 CHAPTER 32 Maintenance Fluid Therapy
CHAPTER 32 Maintenance Fluid Therapy
BODY COMPOSITION
Water is the most plentiful constituent of the human body. Total body water (TBW) as a percentage of body weight varies with age. The fetus has a high TBW, which gradually decreases to about 75% of birth weight for a term infant. Premature infants have a higher TBW content than term infants. During the first year of life, TBW decreases to about 60% of body weight and basically remains at this level until puberty. At puberty, the fat content of females increases more than males, who acquire more muscle mass than females. Because fat has low water content, and muscle has high water content, by the end of puberty TBW in males remains at 60%, but it decreases to 50% of body weight in females. During dehydration, TBW decreases and is a smaller percentage of body weight.
TBW has two main compartments: intracellular fluid (ICF) and extracellular fluid (ECF). In the fetus and newborn, the ECF volume is larger than the ICF volume. The normal postnatal diuresis causes an immediate decrease in the ECF volume. This decrease in ECF volume is followed by continued expansion of the ICF volume because of cellular growth. By 1 year of age, the ratio of the ICF volume to the ECF volume approaches adult levels. The ECF volume is 20% to 25% of body weight, and the ICF volume is 30% to 40% of body weight (Fig. 32-1). With puberty, the increased muscle mass of males results in a higher ICF volume than females.
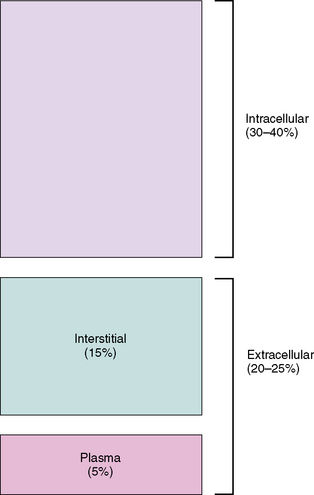
FIGURE 32-1 Compartments of total body water, expressed as percentage of body weight, in an older child or adult.
(From Greenbaum LA: Pathophysiology of body fluids and fluid therapy. In Kliegman RM, Behrman RE, Jenson HB, et al: Nelson Textbook of Pediatrics, 18th ed. Philadelphia, 2007, Elsevier Science, p 268.)
The ECF is divided further into plasma water and interstitial fluid (see Fig. 32-1). Plasma water is about 5% of body weight. The blood volume, given a hematocrit of 40%, is usually 8% of body weight, although it is higher in newborns and young infants. In premature newborns, it is around 10% of body weight. The volume of plasma water can be altered by pathologic conditions, including dehydration, anemia, polycythemia, heart failure, abnormal plasma osmolality, and hypoalbuminemia. The interstitial fluid, normally 15% of body weight, can increase dramatically in diseases associated with edema, such as heart failure, protein-losing enteropathy, liver failure, and nephrotic syndrome.
The composition of solutes in the ICF and ECF is different. Sodium and chloride are the dominant cation and anion in the ECF. Potassium is the most abundant cation in the ICF, and proteins, organic anions, and phosphate are the most plentiful anions in the ICF. The dissimilarity between the anions in the ICF and the ECF is determined largely by the presence of intracellular molecules that do not cross the cell membrane, the barrier separating the ECF and the ICF. In contrast, the difference in the distribution of cations—sodium and potassium—is due to the activity of the Na+, K+-ATPase pump, which uses cellular energy to actively extrude sodium from cells and move potassium into cells.
REGULATION OF INTRAVASCULAR VOLUME AND OSMOLALITY
Proper cell functioning requires close regulation of plasma osmolality and intravascular volume; these are controlled by independent systems for water balance, which determines osmolality, and sodium balance, which determines volume status. Maintenance of a normal osmolality depends on control of water balance. Control of volume status depends on regulation of sodium balance.
The plasma osmolality is tightly regulated between 285 and 295 mOsm/kg. Modification of water intake and excretion maintains a normal plasma osmolality. In the steady state, water intake and water produced from oxidation balances water losses from the skin, lungs, urine, and gastrointestinal tract. Only water intake and urinary losses can be regulated. A small increase in the plasma osmolality stimulates thirst. Urinary water losses are regulated by the secretion of antidiuretic hormone (ADH), which increases in response to an increasing plasma osmolality. ADH, by stimulating renal tubular reabsorption of water, decreases urinary water losses. Control of osmolality is subordinate to maintenance of an adequate intravascular volume. When significant volume depletion is present, ADH secretion and thirst are stimulated, regardless of the plasma osmolality.
Volume depletion and volume overload may cause significant morbidity and mortality. Because sodium is the principal extracellular cation and is restricted to the ECF, adequate body sodium is necessary for maintenance of intravascular volume. The kidney determines sodium balance because there is little homeostatic control of sodium intake, although salt craving occasionally occurs, typically in children with chronic renal salt loss. The kidney regulates sodium balance by altering the percentage of filtered sodium that is reabsorbed along the nephron. The renin-angiotensin system is an important regulator of renal sodium reabsorption and excretion. The juxtaglomerular apparatus produces renin in response to decreased effective intravascular volume. Renin cleaves angiotensinogen, producing angiotensin I, which angiotensin-converting enzyme converts into angiotensin II. The actions of angiotensin II include direct stimulation of the proximal tubule to increase sodium reabsorption and stimulation of the adrenal gland to increase aldosterone secretion, which increases sodium reabsorption in the distal nephron.
Volume expansion stimulates the synthesis of atrial natriuretic peptide, which is produced by the atria in response to atrial wall distention. Along with increasing glomerular filtration rate, atrial natriuretic peptide inhibits sodium reabsorption, facilitating an increase in urinary sodium excretion.
MAINTENANCE FLUIDS
Maintenance intravenous (IV) fluids are used in children who cannot be fed enterally. Along with maintenance fluids, children may require concurrent replacement fluids if they have excessive ongoing losses, such as may occur with drainage from a nasogastric tube. In addition, if dehydration is present, the patient also needs to receive deficit replacement (see Chapter 33).
Maintenance fluids are composed of a solution of water, glucose, sodium, potassium, and chloride. This solution replaces electrolyte losses from the urine and stool, as well as water losses from the urine, stool, skin, and lungs. The glucose in maintenance fluids provides approximately 20% of the normal caloric needs of the patient. This percentage is enough to prevent the development of starvation ketoacidosis and diminishes the protein degradation that would occur if the patient received no calories. Glucose also provides added osmoles, avoiding the administration of hypotonic fluids, which may cause hemolysis.
Maintenance fluids do not provide adequate calories, protein, fat, minerals, or vitamins. Because of inadequate calories, a child on maintenance IV fluids loses 0.5% to 1% of real weight each day. Patients should not remain on maintenance therapy indefinitely; parenteral nutrition (see Chapter 34) should be used for children who cannot be fed enterally for more than a few days. Parenteral nutrition is especially important in a patient with underlying malnutrition.
Daily water losses are measurable (urine and stool) and not measurable (insensible losses from the skin and lungs). Failure to replace these losses leads to a thirsty, uncomfortable child and, ultimately, a dehydrated child. Table 32-1 provides a system for calculating 24-hour maintenance water needs based on the patient’s weight. Sodium and potassium are given in maintenance fluids to replace losses from urine and stool.
TABLE 32-1 Body Weight Method for Calculating Maintenance Fluid Volume and Rate
| Body Weight (kg) | Volume Per Day | Hourly Rate |
|---|---|---|
| 0–10 | 100 mL/kg | 4 mL/kg/hr |
| 11–20 | 1000 mL 50 mL/kg for each 1 kg >10 kg | 40 mL/hr 2 mL/kg/hr × (wt − 10) |
| >20 | 1500 mL 20 mL/kg for each 1 kg >20 kg* | 60 mL/hr 1 mL/kg/hr × (wt − 20)† |
* The maximum total fluid per day is normally 2400 mL.
† The maximum fluid rate is normally 100 mL/hr.
After calculation of water needs and electrolyte needs, children typically receive either 5% dextrose (D5) in ¼ normal saline (NS) plus 20 mEq/L of potassium chloride (KCl) or D5 in ½ NS plus 20 mEq/L of KCl. Children weighing less than 10 kg do best with the solution containing ¼ NS (38.5 mEq/L) because of their high water needs per kilogram. In contrast, larger children and adults may receive the solution with ½ NS (77 mEq/L). These guidelines assume that there is no disease process present that would require an adjustment in either the volume or the electrolyte composition of maintenance fluids. (Children with renal insufficiency may be hyperkalemic or unable to excrete potassium and may not tolerate 20 mEq/L of KCl.) In children with complicated pathophysiologic derangements, it may be necessary to adjust the electrolyte composition and rate of maintenance fluids empirically based on electrolyte measurements and assessment of fluid balance.