CHAPTER 100 Meningitis
CHAPTER 100 Meningitis
ETIOLOGY
Meningitis, inflammation of the leptomeninges, can be caused by bacteria, viruses, or, rarely, fungi. The term aseptic meningitis refers principally to viral meningitis, but a similar picture may be seen with other infectious organisms (Lyme disease, syphilis, tuberculosis), parameningeal infections (brain abscess, epidural abscess, venous sinus empyema), chemical exposure (nonsteroidal anti-inflammatory drugs, intravenous immunoglobulin), autoimmune disorders, and many other diseases.
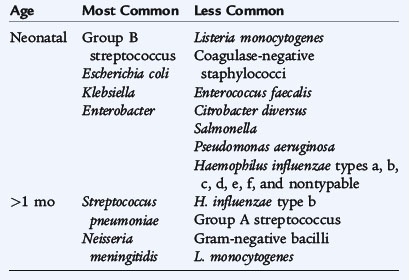
The organisms commonly causing bacterial meningitis (Table 100-1) before the availability of current conjugate vaccines were Haemophilus influenzae, Streptococcus pneumoniae, and Neisseria meningitidis. In the United States, the rate of H. influenzae type b meningitis has declined to less than 5% of its previous rate, and the rate of S. pneumoniae disease has declined substantially after the introduction of targeted vaccines. The bacteria causing neonatal meningitis are the same as the bacteria that cause neonatal sepsis (see Chapter 65). Staphylococcal meningitis occurs primarily in patients who have had neurosurgery or experience penetrating head trauma.
Partially treated meningitis refers to bacterial meningitis complicated by oral antibiotic treatment before the lumbar puncture, which may result in negative cerebrospinal fluid (CSF) cultures, although other CSF findings suggestive of bacterial infection persist. The etiology can be confirmed by antigen detection in the CSF and urine.
Viral meningitis is caused principally by enteroviruses, including coxsackieviruses, echoviruses, and, in unvaccinated individuals, polioviruses. Fecal excretion and transmission are continuous and persist for several weeks. Enteroviruses and arboviruses (St. Louis, LaCrosse, West Nile, California encephalitis viruses) are the principal causes of meningoencephalitis (see Chapter 101). Other viruses that cause meningitis include herpes simplex virus, Epstein-Barr virus, cytomegalovirus, lymphocytic choriomeningitis virus, and human immunodeficiency virus (HIV). Mumps virus is a common cause of viral meningitis in unvaccinated children. Uncommon causes of meningitis include Borrelia burgdorferi (Lyme disease), Bartonella henselae (cat-scratch disease), Mycobacterium tuberculosis, Toxoplasma, fungi (Cryptococcus, Histoplasma, and Coccidioides), and parasites (Angiostrongylus cantonensis, Naegleria fowleri, and Acanthamoeba).
EPIDEMIOLOGY
The incidence of bacterial meningitis is highest among children younger than 1 year of age. Extremely high rates are found in Native Americans, Alaskan Natives, and Australian aboriginals, suggesting that genetic factors play a role in susceptibility. Other risk factors include acquired or congenital immunodeficiencies, hemoglobinopathies such as sickle cell disease, functional or anatomic asplenia, and crowding such as occurs in some households, day care centers, or college and military dormitories. A CSF leak resulting from congenital anomaly or following a basilar skull fracture increases the risk of meningitis, especially that caused by S. pneumoniae.
Enteroviruses cause meningitis with peaks during summer and fall. These infections are more prevalent among low socioeconomic groups, young children, and immunocompromised persons. The prevalence of arboviral meningitis is determined by geographic distribution and seasonal activity of the arthropod (mosquito) vectors. In the United States, most arboviral infections occur during the summer and fall.
CLINICAL MANIFESTATIONS
Preceding upper respiratory tract symptoms are common. Rapid onset is typical of S. pneumoniae and N. meningitidis. Indications of meningeal inflammation include headache, irritability, nausea, nuchal rigidity, lethargy, photophobia, and vomiting. Fever usually is present. Kernig and Brudzinski signs of meningeal irritation are often positive in children older than 12 months of age. In young infants, signs of meningeal inflammation may be minimal with only irritability, restlessness, depressed mental status, and poor feeding. Focal neurologic signs, seizures, arthralgia, myalgia, petechial or purpuric lesions, sepsis, shock, and coma may occur. Increased intracranial pressure is reflected in complaints of headache, diplopia, and vomiting. A bulging fontanelle may be present in infants. Ptosis, sixth nerve palsy, anisocoria, bradycardia with hypertension, and apnea are signs of increased intracranial pressure with brain herniation. Papilledema is uncommon, unless there is occlusion of the venous sinuses, subdural empyema, or brain abscess.
LABORATORY AND IMAGING STUDIES
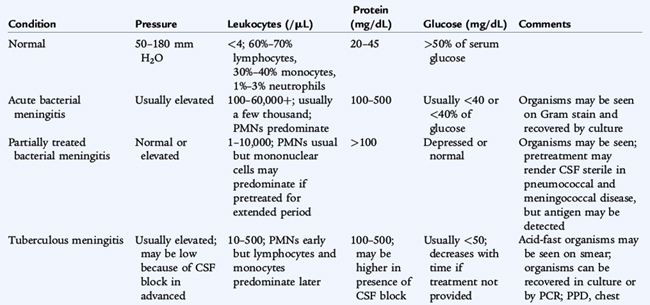
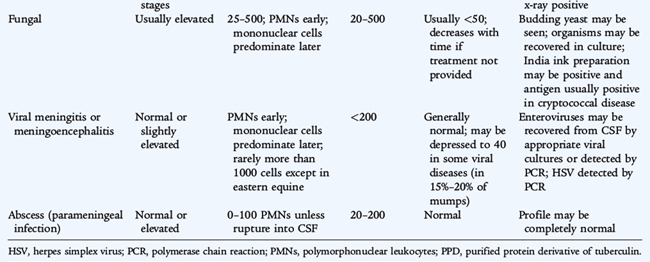
If bacterial meningitis is suspected, a lumbar puncture should be performed unless there is evidence of cardiovascular instability or of increased intracranial pressure, other than a bulging fontanelle (because of the risk of herniation). Routine CSF examination includes a white blood cell count, differential, protein and glucose levels, and Gram stain (Table 100-2). CSF should be cultured for bacteria and, when appropriate, fungi, viruses, and mycobacteria. The polymerase chain reaction test is used to diagnose enteroviruses and herpes simplex virus; it is more sensitive and more rapid than viral culture. Leukocytosis is common on the complete blood count. Blood cultures are positive in 90% of cases of bacterial meningitis. An electroencephalogram may confirm an encephalitis component (see Chapter 101).
DIFFERENTIAL DIAGNOSIS
Many disorders may show signs of meningeal irritation and increased intracranial pressure, including the infectious causes of meningitis, encephalitis, hemorrhage, rheumatic diseases, and malignancies. Seizures are associated with meningitis, encephalitis, and intracranial abscess or can be the sequelae of brain edema, cerebral infarction or hemorrhage, or vasculitis.
TREATMENT
Treatment of bacterial meningitis focuses on sterilization of the CSF by antibiotics (Table 100-3) and maintenance of adequate cerebral and systemic perfusion. Because of increasing resistance of S. pneumoniae to both penicillin and cephalosporins, cefotaxime (or ceftriaxone) plus vancomycin should be administered until antibiotic susceptibility testing is available. Cefotaxime or ceftriaxone are adequate to treat N. meningitidis and H. influenzae types a through f. For infants younger than 2 months of age, ampicillin is added to cover the possibility of Listeria monocytogenes and Escherichia coli. Duration of treatment is 10 to 14 days for S. pneumoniae, 5 to 7 days for N. meningitidis, and 7 to 10 days for H. influenzae.
TABLE 100-3 Initial Antimicrobial Therapy by Age for Presumed Bacterial Meningitis
| Age | Recommended Treatment | Alternative Treatments |
|---|---|---|
| Newborns (0–28 days) | Cefotaxime or ceftriaxone plus ampicillin with or without gentamicin | |
| Infants and toddlers (1 mo–4 yr) | Ceftriaxone or cefotaxime plus vancomycin | Cefotaxime or ceftriaxone plus rifampin |
| Children and adolescents (5–13 yr) and adults | Ceftriaxone or cefotaxime plus vancomycin | Cefepime or ceftazidime plus vancomycin |
Dexamethasone therapy (0.6 to 0.8 mg/kg daily in two to three divided doses for 2 days), as adjunctive therapy initiated just before or concurrently with the first dose of antibiotics, significantly diminishes the incidence of hearing loss and neurologic deficits resulting from H. influenzae meningitis. In addition, it improves outcomes in both children and adults with pneumococcal meningitis.
Supportive therapy involves treatment of dehydration, shock, disseminated intravascular coagulation, syndrome of inappropriate antidiuretic hormone (SIADH) secretion, seizures, increased intracranial pressure, apnea, arrhythmias, and coma. Adequate cerebral perfusion must be maintained in the presence of cerebral edema.
COMPLICATIONS AND PROGNOSIS
SIADH secretion may complicate meningitis and necessitates monitoring of urine output and fluid administration. Computed tomography or magnetic resonance imaging commonly detects subdural effusions with S. pneumoniae and H. influenzae meningitis. Most effusions are sterile and asymptomatic, and they do not necessitate drainage unless associated with increased intracranial pressure or focal neurologic signs. Persistent fever is common during treatment, but it also may be related to infective or immune complex–mediated pericardial or joint effusions, thrombophlebitis, drug fever, or nosocomial infection. A repeat lumbar puncture is not indicated for fever in the absence of other signs of persistent central nervous system infection.
Even with appropriate antibiotic therapy, the mortality rate for bacterial meningitis in children is significant: 25% for S. pneumoniae, 15% for N. meningitidis, and 8% for H. influenzae. Of survivors, 35% have sequelae, particularly after pneumococcal infection, including deafness, seizures, learning disabilities, blindness, paresis, ataxia, or hydrocephalus. All patients with meningitis should have hearing evaluation before discharge and at follow-up. Poor prognosis is associated with young age, long duration of illness before effective antibiotic therapy, seizures, coma at presentation, shock, low or absent CSF white blood cell count in the presence of visible bacteria on Gram stain of the CSF, and immunocompromised status.
Rarely, relapse may occur 3 to 14 days after treatment, possibly from parameningeal foci or resistant organisms. Recurrence may indicate an underlying immunologic or anatomic defect that predisposes the patient to meningitis.
PREVENTION
Routine immunizations against H. influenzae and S. pneumoniae are recommended for children beginning at 2 months of age. Vaccines against N. meningitidis are recommended for young adolescents, college freshmen, military personnel, and travelers to highly endemic areas (see Chapter 94). Chemoprophylaxis is recommended for close contacts of persons with N. meningitidis infection plus the index case as well as for close contacts of persons with H. influenzae disease and the index case. Treatment with rifampin, ciprofloxacin, or ceftriaxone is recommended.