 CHAPTER 110 Pneumonia
CHAPTER 110 Pneumonia
ETIOLOGY
Pneumonia is an infection of the lower respiratory tract that involves the airways and parenchyma with consolidation of the alveolar spaces. The term lower respiratory tract infection is often used to encompass bronchitis, bronchiolitis (see Chapter 109), or pneumonia or any combination of the three. Pneumonitis is a general term for lung inflammation that may or may not be associated with consolidation. Lobar pneumonia describes pneumonia localized to one or more lobes of the lung. Atypical pneumonia describes patterns other than lobar pneumonia. Bronchopneumonia refers to inflammation of the lung that is centered in the bronchioles and leads to the production of a mucopurulent exudate that obstructs some of these small airways and causes patchy consolidation of the adjacent lobules. Interstitial pneumonitis refers to inflammation of the interstitium, which is composed of the walls of the alveoli, the alveolar sacs and ducts, and the bronchioles. Interstitial pneumonitis is characteristic of acute viral infections but also may be a chronic process.
Defects in host defenses increase the risk of pneumonia. Lower airways and secretions are sterile as a result of a multicomponent cleansing system. Airway contaminants are caught in the mucus secreted by the goblet cells. Cilia on epithelial surfaces, composing the ciliary elevator system, beat synchronously to move particles upward toward the central airways and into the throat, where they are swallowed or expectorated. Polymorphonuclear neutrophils from the blood and tissue macrophages ingest and kill microorganisms. IgA secreted into the upper airway fluid protects against invasive infections and facilitates viral neutralization.
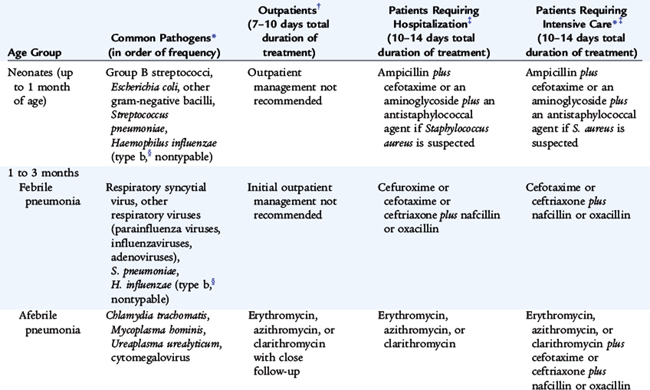
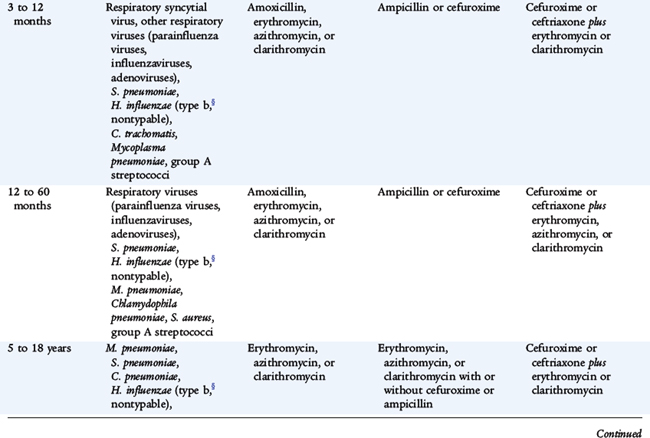
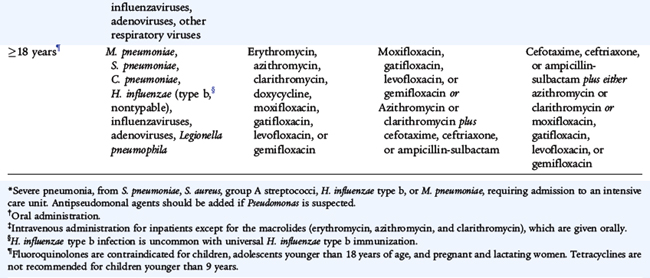
Infectious agents that commonly cause community-acquired pneumonia vary by age (Table 110-1). Most common causes are respiratory syncytial virus (RSV) in infants (see Chapter 109), respiratory viruses (RSV, parainfluenza viruses, influenza viruses, adenoviruses) in children younger than 5 years old, and Mycoplasma pneumoniae in children older than age 5. Streptococcus pneumoniae occurs in children of any age, outside the neonatal period. M. pneumoniae and Chlamydophila pneumoniae are principal causes of atypical pneumonia.
TABLE 110-1 Etiologic Agents and Empirical Antimicrobial Therapy for Pneumonia in Patients without History of Recent Antibiotic Therapy
Additional agents occasionally or rarely cause pneumonia. Severe acute respiratory syndrome (SARS) is due to SARS-associated coronavirus (SARS-CoV). Avian influenza, also known as bird flu, is a highly contagious viral disease of poultry and other birds that is caused by influenza A (H5N1). There were outbreaks among humans in South East Asia in 1997 and 2003–2004 with high mortality rates. Hantavirus cardiopulmonary syndrome is caused by Sin Nombre virus, which is carried by Peromyscus maniculatus (the deer mouse) and transmitted to humans by aerosolized rodent excreta. Legionnaires’ disease caused by Legionella pneumophila is a rare cause of pneumonia in children.
Chlamydia trachomatis and less commonly Mycoplasma hominis, Ureaplasma urealyticum, and cytomegalovirus (CMV) cause a similar respiratory syndrome in infants 1 to 3 months of age with subacute onset of an afebrile pneumonia with cough and hyperinflation as the predominant signs. These infections are difficult to diagnose and to distinguish from each other. In adults, these organisms are carried primarily as part of the genital mucosal flora. Women who harbor these agents may transmit them perinatally to newborns.
Causes of pneumonia in immunocompromised persons include gram-negative enteric bacteria, mycobacteria (M. avium complex), fungi (aspergillosis, histoplasmosis), viruses (CMV), and Pneumocystis jirovecii (carinii). Pneumonia in patients with cystic fibrosis usually is caused by Staphylococcus aureus in infancy and Pseudomonas aeruginosa or Burkholderia cepacia in older patients.
EPIDEMIOLOGY
Immunizations have had a great impact on the incidence of pneumonia caused by pertussis, diphtheria, measles, Haemophilus influenzae, and S. pneumoniae. Where used, bacille Calmette-Guérin (BCG) for tuberculosis also has had a significant impact. More than 4 million deaths each year in developing countries are due to acute respiratory tract infections. Risk factors for lower respiratory tract infections include gastroesophageal reflux, neurologic impairment (aspiration), immunocompromised states, anatomic abnormalities of the respiratory tract, residence in residential care facilities for handicapped children, and hospitalization, especially in an intensive care unit (ICU) or requiring invasive procedures.
CLINICAL MANIFESTATIONS
Age is a determinant in the clinical manifestations of pneumonia. Neonates may have fever only with subtle or absent physical findings of pneumonia (see Chapter 65). The typical clinical patterns of viral and bacterial pneumonias usually differ between older infants and children, although the distinction is not always clear for a particular patient. Fever, chills, tachypnea, cough, malaise, pleuritic chest pain, retractions, and apprehension, because of difficulty breathing or shortness of breath, are common in older infants and children.
Viral pneumonias are associated more often with cough, wheezing, or stridor; fever is less prominent than with bacterial pneumonia. Bacterial pneumonias typically are associated with higher fever, chills, cough, dyspnea, and auscultatory findings of lung consolidation. Atypical pneumonia in young infants is characterized by tachypnea, cough, crackles on auscultation, and often concomitant chlamydial conjunctivitis. Other signs of respiratory distress include flaring of the alae of the nose, intercostal and subcostal retractions, and grunting. All significant pneumonias have localized crackles and decreased breath sounds; a pleural effusion may cause dullness to percussion.
LABORATORY AND IMAGING STUDIES
Bacterial flora of the upper respiratory tract is not an accurate reflection of the causes of lower respiratory tract infection, and good quality sputum is rarely obtainable from children. In otherwise healthy children without life-threatening disease, invasive procedures to obtain lower respiratory tissue or secretions usually are not indicated. Serologic tests are not useful for the most common causes of bacterial pneumonia.
The white blood cell (WBC) count with viral pneumonias is often normal or mildly elevated, with a predominance of lymphocytes, whereas with bacterial pneumonias the WBC count is elevated (>20,000/mm3) with a predominance of neutrophils. Mild eosinophilia is characteristic of infant C. trachomatis pneumonia. Blood cultures should be performed to attempt to diagnose a bacterial cause of pneumonia. Blood cultures are positive in 10% to 20% of bacterial pneumonia and are considered to be confirmatory of the cause of pneumonia if positive for a recognized respiratory pathogen. Urinary antigen tests are especially useful for L. pneumophila (Legionnaires’ disease).
Relatively accurate for the diagnosis of viral respiratory pneumonia are cultures or rapid viral antigen detection of upper respiratory secretions, but neither rules out concomitant bacterial pneumonia. M. pneumoniae should be suspected if cold agglutinins are present in peripheral blood samples; this may be confirmed by Mycoplasma IgM or more specifically polymerase chain reaction (PCR). CMV and enterovirus can be cultured from the nasopharynx, urine, or bronchoalveolar lavage fluid. The diagnosis of M. tuberculosis is established by tuberculin skin test, blood interferon assays, and analysis of sputum or gastric aspirates by culture, antigen detection, or PCR.
The need to establish an etiologic diagnosis of pneumonia is greater for patients who are ill enough to require hospitalization, immunocompromised patients, patients with recurrent pneumonia, or patients with pneumonia unresponsive to empirical therapy. For these patients, bronchoscopy with bronchoalveolar lavage and brush mucosal biopsy, needle aspiration of the lung, and open lung biopsy are methods of obtaining material for microbiologic diagnosis.
When there is effusion or empyema, performing a thoracentesis to obtain pleural fluid can be diagnostic and therapeutic. Evaluation differentiates between empyema and a sterile parapneumonic effusion caused by irritation of the pleura contiguous with the pneumonia. Gram stain and culture may lead to microbiologic diagnosis. The pleural fluid should be cultured for bacteria, mycobacteria, fungi, and viruses. If the fluid is grossly purulent, removal reduces the patient’s toxicity and associated discomfort and may facilitate more rapid recovery. If the accumulation is large and impairs the ability of the lung to expand, removal of the fluid improves pulmonary mechanics and gas exchange.
Frontal and lateral radiographs are required to localize the diseased segments and to visualize adequately infiltrates behind the heart or the diaphragmatic leaflets. There are characteristic radiographic findings of pneumonia, although there is much overlap that precludes definitive diagnosis by radiography alone. Bacterial pneumonia characteristically shows lobar consolidation, or a round pneumonia, with pleural effusion in 10% to 30% of cases (Fig. 110-1). Viral pneumonia characteristically shows diffuse, streaky infiltrates of bronchopneumonia (Fig. 110-2). Atypical pneumonia, such as with M. pneumoniae and C. pneumoniae, shows increased interstitial markings or bronchopneumonia (Fig. 110-3). The chest radiograph may be normal in early pneumonia, with appearance of an infiltrate during the treatment phase of the disease when edema fluid is greater. Hilar lymphadenopathy is uncommon with bacterial pneumonia, but may be a sign of tuberculosis, histoplasmosis, or an underlying malignant neoplasm. Decubitus views or ultrasound should be used to assess size of pleural effusions and whether they are freely mobile. Computed tomography (CT) is used to evaluate serious disease, pleural abscesses, bronchiectasis, and delineating effusions. Unusual etiologies or recurrent pneumonias require special considerations (Table 110-2). Lung abscesses, pneumatoceles, and empyema all require special management.
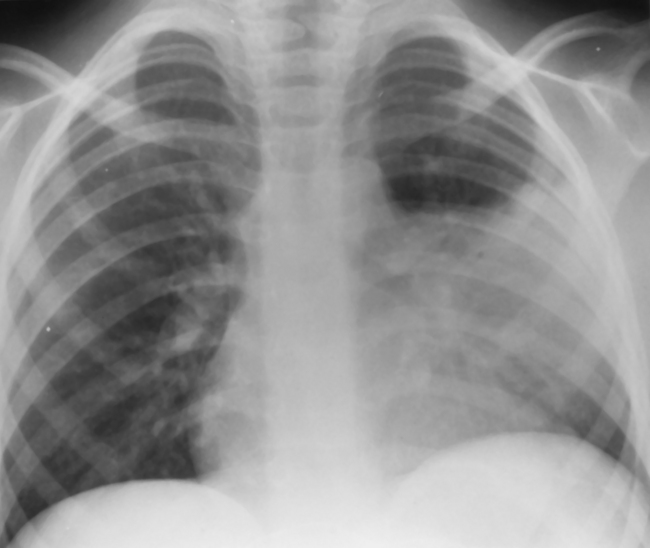
FIGURE 110-1 Acute lobar pneumonia of the lingula in a 6-year-old child with high fever, cough, and chest pain. Frontal chest radiograph shows airspace consolidation, which obliterates the silhouette of the heart border on the left. The left hemidiaphragm is mildly elevated as a result of splinting.
(From Markowitz RI: Diagnostic imaging. In Jenson HB, Baltimore RS [eds]: Pediatric Infectious Diseases: Principles and Practice, 2nd ed. Philadelphia, WB Saunders, 2002, p 133.)

FIGURE 110-2 Diffuse viral bronchopneumonia in a 12-year-old boy with cough, fever, and wheezing. Frontal chest radiograph shows bilateral, perihilar, peribronchial thickening and shaggy infiltrate. Focal airspace disease representing consolidation or atelectasis is present in the medial portion of the right upper lobe. The findings are typical of bronchopneumonia.
(From Markowitz RI: Diagnostic imaging. In Jenson HB, Baltimore RS [eds]: Pediatric Infectious Diseases: Principles and Practice, 2nd ed. Philadelphia, WB Saunders, 2002, p 132.)

FIGURE 110-3 Mycoplasma pneumoniae infection (atypical pneumonia) in a 14-year-old boy with malaise, dry cough, and mild shortness of breath for 1 week. Frontal chest radiograph shows a diffuse pattern of increased interstitial markings, including Kerley lines. The heart is normal, and there are no focal infiltrates. Cold agglutinins were markedly elevated, and the patient responded to erythromycin. This radiographic pattern of reticulonodular interstitial disease is observed in 25% to 30% of patients with pneumonia caused by Mycoplasma pneumoniae.
(From Baltimore RS: Pneumonia. In Jenson HB, Baltimore RS [eds]: Pediatric Infectious Diseases: Principles and Practice, 2nd ed. Philadelphia, WB Saunders, 2002, p 808.)
DIFFERENTIAL DIAGNOSIS
Complete physical examination is important to identify other foci of disease or associated findings that may suggest an etiology. Mucosal congestion and inflammation of the upper airway suggest a viral infection. Tachypnea can be caused by airway inflammation resulting in obstruction or by pneumonia resulting in inadequate gas exchange and hypoxia. Generalized or peripheral cyanosis indicates hypoxia with severe diffuse or multilobular pneumonia or a large pleural effusion. With a young infant, apneic spells may be the first sign of pneumonia.
Asymmetry or shallow breathing may be due to splinting from pain. Low diaphragms by percussion indicate air trapping, which is common in asthma, but also frequently accompanies viral lower respiratory infections. Poor diaphragmatic excursion may indicate hyperexpanded lungs or an inability for expansion because a large consolidation is causing poor lung compliance. Hyperexpansion may push the diaphragm and liver downward. Dullness to percussion may be due to lobar or segmental infiltrates or pleural fluid. Auscultation may be normal in early or very focal pneumonia, but the presence of localized crackles, rhonchi, and wheezes may help one to detect and locate pneumonia. Distant breath sounds may indicate a large, poorly ventilated area of consolidation or pleural fluid.
The various types of pneumonia—lobar pneumonia, bronchopneumonia, interstitial and alveolar pneumonias—need to be differentiated on the basis of radiologic or pathologic diagnosis. Pneumonia must be differentiated from other acute lung diseases, including lung edema caused by heart failure, allergic pneumonitis, and aspiration, and autoimmune diseases, such as rheumatoid disease and systemic lupus erythematosus. Radiographically, pneumonia must be differentiated from lung trauma and contusion, hemorrhage, foreign body obstruction, and irritation from subdiaphragmatic inflammation.
TREATMENT
Therapy for pneumonia includes supportive and specific treatment and depends on the degree of illness, complications, and knowledge of the infectious agent likely causing the pneumonia. Age, severity of the illness, complications noted on the chest radiograph, degree of respiratory distress, and ability of the family to care for the child and to assess the progression of the symptoms all must be taken into consideration in the choice of ambulatory treatment over hospitalization (Table 110-3). Most cases of pneumonia in healthy children can be managed on an outpatient basis.
TABLE 110-3 Factors Suggesting Need for Hospitalization of Children with Pneumonia
Adapted from Baltimore RS: Pneumonia. In Jenson HB, Baltimore RS (eds): Pediatric Infectious Diseases: Principles and Practice. Philadelphia, WB Saunders, 2002.
Although viruses cause most community-acquired pneumonias in young children, in most situations experts recommend empirical antibiotic treatment for the most probable treatable causes (see Table 110-1). Exceptional situations include lack of response to empirical therapy, unusually severe presentations, nosocomial pneumonia, and immunocompromised children susceptible to infections with opportunistic pathogens (Table 110-4). In contrast to pneumococcal meningitis, presumed pneumococcal pneumonia can be treated with high-dose cephalosporin therapy even with high-level penicillin resistance. Vancomycin can be used if the isolate shows high-level resistance and the patient is severely ill. For infants 4 to 18 weeks old with afebrile pneumonia most likely caused by C. trachomatis, a macrolide is the recommended treatment.
TABLE 110-4 Antimicrobial Therapy for Pneumonia Caused by Specific Pathogens*
| Pathogen | Recommended Treatment | Alternative Treatment |
|---|---|---|
| Streptococcus pneumoniae† | Ceftriaxone, cefotaxime, penicillin G, or penicillin V | Cefuroxime axetil, erythromycin, clindamycin, or vancomycin |
| Group A streptococci | Penicillin G | Cefuroxime, cefuroxime axetil, or erythromycin |
| Group B streptococci | Penicillin G | |
| Haemophilus influenzae type b | Ceftriaxone, cefotaxime, ampicillin-sulbactam, or ampicillin | Cefuroxime, cefuroxime axetil |
| Mycoplasma pneumoniae | Erythromycin, azithromycin, or clarithromycin | Doxycycline (in patients older than 9 years of age)‡ Fluoroquinolone (in patients older than 18 years) |
| Gram-negative aerobic bacilli (except P. aeruginosa) | Cefotaxime (or ceftriaxone) with or without an aminoglycoside | Piperacillin-tazobactam plus an aminoglycoside§ |
| P. aeruginosa | Ceftazidime with or without an aminoglycoside§ | Piperacillin-tazobactam plus an aminoglycoside§ |
| Staphylococcus aureus | Nafcillin, cephazolin, clindamycin (for MRSA) | Vancomycin (for MRSA) |
| Chlamydophila pneumoniae | Erythromycin, azithromycin, or clarithromycin | Doxycycline (in patients older than 9 years of age)‡ Fluoroquinolone (in patients older than 18 years) |
| Chlamydia trachomatis (afebrile pneumonia in infants) | Erythromycin, azithromycin, or clarithromycin | |
| Herpes simplex virus | Acyclovir |
MRSA, methicillin-resistant Staphylococcus aureus; TMP-SMX, trimethoprim-sulfamethoxazole.
* Oral outpatient therapy may be used for mild illness. Intravenous inpatient therapy should be used for moderate to severe illness.
† Antibiotic should be chosen on the basis of antibiotic susceptibility of the isolate or susceptibility of the prevalent isolates in the community.
‡ Appropriate fluoroquinolones include moxifloxacin, gatifloxacin, levofloxacin, and gemifloxacin. Fluoroquinolones are contraindicated for children, adolescents younger than 18 years of age, and pregnant and lactating women. Tetracyclines are not recommended for children younger than 9 years.
§ Aminoglycoside dosing should be guided by serum antibiotic concentrations after a steady state has been reached.
COMPLICATIONS AND PROGNOSIS
Bacterial pneumonias frequently cause inflammatory fluid to collect in the adjacent pleural space, causing a parapneumonic effusion or, if grossly purulent, an empyema. Small effusions may not require any special therapy. Large effusions may restrict breathing and require drainage. Air dissection within lung tissue results in a pneumatocele, or air pocket. Scarring of the airways and lung tissue may leave dilated bronchi, resulting in bronchiectasis and increased risk for recurrent infection.
Pneumonia that causes necrosis of lung tissue may evolve into a lung abscess. Lung abscess is an uncommon problem in children and usually is caused by aspiration or infection behind an obstructed bronchus. The most commonly involved sites are the posterior segments of the upper lobes and the superior segments of the lower lobes, where aspirated material drains when the child is recumbent. Anaerobic bacteria usually predominate, along with various streptococci, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Staphylococcus aureus. Chest radiograph or CT scan reveals a cavitary lesion, often with an air-fluid level, surrounded by parenchymal inflammation. If the cavity communicates with the bronchi, organisms may be isolated from sputum. Diagnostic bronchoscopy may be indicated to exclude a foreign body and obtain microbiologic specimens. Lung abscesses usually respond to appropriate antimicrobial therapy with clindamycin, penicillin G, or ampicillin-sulbactam.
Most children recover from pneumonia rapidly and completely, although radiographic abnormalities may take 6 to 8 weeks to return to normal. In a few children, pneumonia may persist longer than 1 month or may be recurrent. In such cases, the possibility of underlying disease must be investigated further, such as with tuberculin skin test, sweat chloride determination for cystic fibrosis, serum immunoglobulin and IgG subclass determinations, bronchoscopy to identify anatomic abnormalities or foreign body, and barium swallow for gastroesophageal reflux.
Severe adenovirus pneumonia may result in bronchiolitis obliterans, a subacute inflammatory process in which the small airways are replaced by scar tissue, resulting in a reduction in lung volume and lung compliance. Unilateral hyperlucent lung, or Swyer-James syndrome, is a focal sequela of severe necrotizing pneumonia in which all or part of a lung has increased translucency radiographically and has been linked to adenovirus type 21.
PREVENTION
Annual influenza vaccine is recommended for all children 6 to 18 years of age (see Chapter 94). Children 6 months to 5 years of age are at higher risk for influenza complications. Trivalent inactivated vaccine or the live, attenuated influenza vaccine can be used for persons 2 to 49 years of age. Some trivalent vaccines are licensed for use beginning at 6 months of age. Universal childhood vaccination with conjugate vaccines for H influenzae type b and S. pneumoniae have greatly diminished the incidence of these pneumonias. The severity of RSV infections can be reduced by use of palivizumab in high-risk patients (see Chapter 109).
Reducing the duration of mechanical ventilation and administering antibiotics judiciously reduces the incidence of ventilator-associated pneumonias. The head of the bed should be raised to 30 to 45 degrees for intubated patients to minimize risk of aspiration, and all suctioning equipment and saline should be sterile. Hand washing before and after every patient contact and use of gloves for invasive procedures are important measures to prevent nosocomial transmission of infections. Hospital staff with respiratory illnesses or who are carriers of certain organisms, such as methicillin-resistant S. aureus, should comply with infection control policies to prevent transfer of organisms to patients. Treating sources of aerosols, such as air coolers, can prevent Legionella pneumonia.