CHAPTER 115 Vulvovaginitis
CHAPTER 115 Vulvovaginitis
ETIOLOGY
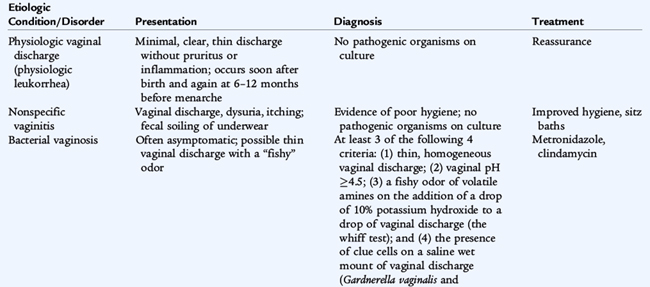
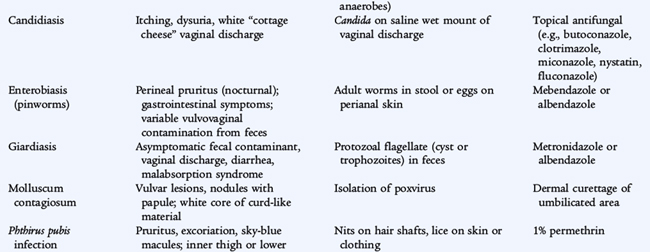
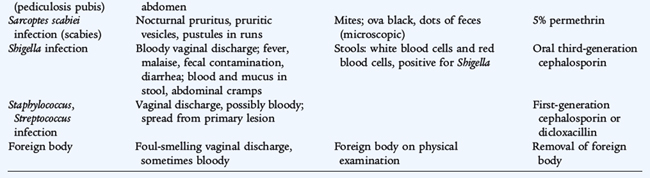
Vulvovaginitis, which is inflammation of the vulva or the vagina or both, is the most common gynecologic problem in children. Low prepubertal levels of estrogen result in thin, atrophic vaginal epithelium that is susceptible to bacterial invasion. At puberty, estrogen increases, and the pH of the vagina becomes more acidic. There are several specific causes of vulvovaginitis (Table 115-1) including sexually transmitted infections (STIs) such as Trichomonas vaginalis and herpes simplex virus (HSV) (see Chapter 116). Nonspecific vaginitis results from overgrowth of normal aerobic vaginal flora that is associated with poor hygiene. Bacterial vaginosis is caused by Gardnerella vaginalis, which interacts synergistically with vaginal anaerobes, including Bacteroides, Mobiluncus, and Peptostreptococcus.
EPIDEMIOLOGY
Nonspecific vaginitis is the most common cause of vulvovaginitis in young girls. G. vaginalis is often present as part of the normal vaginal flora in preadolescent girls, but is more common in girls who are sexually active. Candida is much less common in preadolescent girls than in women.
CLINICAL MANIFESTATIONS
The primary symptoms of vulvovaginitis are vaginal discharge, erythema, and pruritus. A thin, gray, homogeneous discharge with a fishy odor suggests bacterial vaginosis. A white cottage cheese discharge suggests Candida. Bloody discharge suggests group A streptococcus or Shigella. Foul-smelling discharge suggests a foreign body.
LABORATORY AND IMAGING STUDIES
Wet mount microscopic examination, prepared by mixing vaginal secretions with normal saline solution, and culture may be used to confirm a specific diagnosis (see Table 115-1). Clue cells are vaginal epithelial cells that are covered with G. vaginalis and have a granular appearance. Vaginal cultures for G. vaginalis are not useful. Candida may be identified by saline wet mount or by culture.
DIFFERENTIAL DIAGNOSIS
Noninfectious causes of vulvovaginitis include physical agents (foreign body, sand), chemical agents (bubble bath, soap, detergent), and vulvar skin disease (atopic dermatitis, seborrhea, psoriasis). Physiologic vaginal discharge or physiologic leukorrhea of desquamated vaginal cells and mucus occurs normally in girls soon after birth, with discharge lasting for about 1 week, and again at 6 to 12 months before menarche. There is minimal, clear, thin discharge without pruritus or inflammation. No treatment is necessary.
TREATMENT
The treatment of vulvovaginitis depends on the etiology (see Table 115-1). Treatment of nonspecific vaginitis includes improving perineal hygiene and sitz baths two to three times a day as needed. The recommended treatment for bacterial vaginosis is oral metronidazole. Imidazole creams and vaginal tablets and suppositories all are effective for the treatment of acute vulvovaginal candidiasis. Douching or vaginal irrigation is not beneficial and is not recommended.