CHAPTER 119 Ocular Infections
CHAPTER 119 Ocular Infections
ETIOLOGY
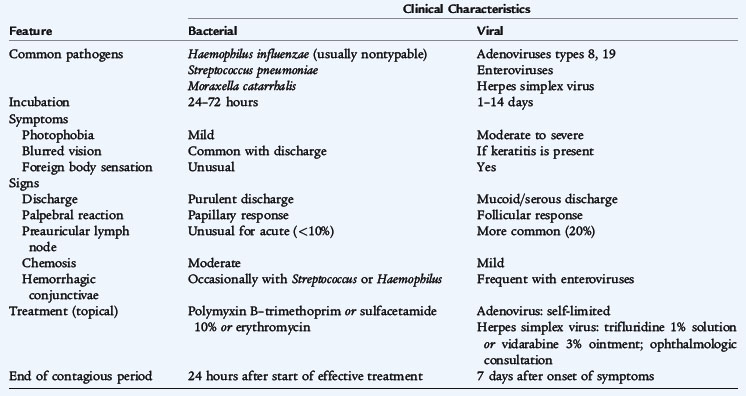
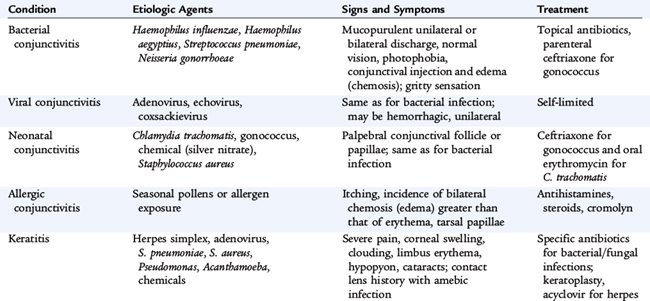
Acute conjunctivitis is usually a bacterial or viral infection of the eye characterized by a rapid onset of symptoms that persists for a few days. The most common causes of bacterial conjunctivitis are nontypable Haemophilus influenzae, Streptococcus pneumoniae, and Mycoplasma catarrhalis (Table 119-1). Other causes include Neisseria gonorrhoeae and Pseudomonas aeruginosa, which is associated with extended-wear soft contact lenses. Viral conjunctivitis most commonly is caused by adenoviruses, which cause epidemic keratoconjunctivitis, and less frequently by coxsackieviruses and other enteroviruses. Keratitis, or inflammation of the cornea, is not commonly associated with conjunctivitis but occurs with N. gonorrhoeae, herpes simplex virus (HSV), and adenovirus infections.
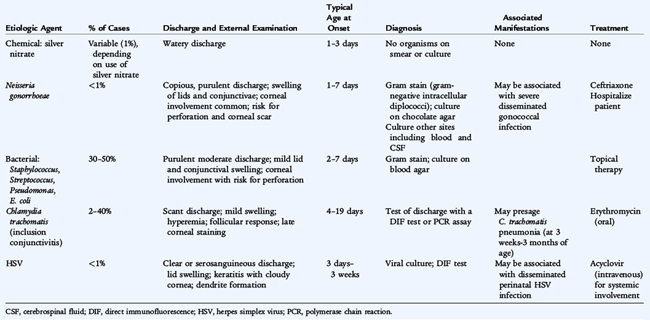
Neonatal conjunctivitis, or ophthalmia neonatorum, is purulent conjunctivitis during the first 10 days of life, usually acquired during birth. The common causes of neonatal conjunctivitis, in order of decreasing prevalence, are: silver nitrate if used for gonococcal prophylaxis, Chlamydia trachomatis, common bacterial causes of conjunctivitis, Escherichia coli, other gram-negative enteric bacilli, and N. gonorrhoeae. Neonatal conjunctivitis also can occur as a part of perinatal HSV infection.
EPIDEMIOLOGY
Conjunctivitis is common in young children, especially if they come in contact with other children with conjunctivitis. Predisposing factors for bacterial infection include nasolacrimal duct obstruction, sinus disease, ear infection, and allergic children who rub their eyes frequently. Conjunctivitis occurs in 1% to 12% of neonates. A mild to moderate chemical conjunctivitis commonly is present from 24 to 48 hours of age in most newborns who receive ophthalmic silver nitrate as gonococcal prophylaxis. Neonatal acquisition of C. trachomatis occurs in approximately 50% of infants born vaginally to infected mothers. In infants with perinatal acquisition of C. trachomatis, the risk of chlamydial conjunctivitis, also called inclusion conjunctivitis, is 25% to 50%.
CLINICAL MANIFESTATIONS
Symptoms include redness, discharge, matted eyelids, and mild photophobia. Physical examination findings include chemosis, injection of the conjunctiva, and edema of the eyelids. Corneal involvement suggests gonococcal or herpetic infection. Herpetic corneal lesions appear as dendritic or ameboid ulcers or, more commonly, in recurrent infection, as a deep keratitis. Unilateral conjunctivitis with ipsilateral otitis media is often caused by nontypable H. influenzae.
The timing and manifestations of neonatal conjunctivitis are helpful in identifying the cause (Table 119-2). N. gonorrhoeae causes severe conjunctivitis with profuse purulent discharge. Chlamydial conjunctivitis usually occurs in the second week of life but may appear 3 days to 6 weeks after delivery. There is mild to moderate inflammation with purulent discharge issuing from one or both eyes.
LABORATORY AND IMAGING STUDIES
Cultures are not routinely obtained because bacterial conjunctivitis is usually self-limited or responds quickly to antibiotic treatment. If gonococcal conjunctivitis is suspected, especially in neonates, Gram stain and culture must be obtained. In these infants, further testing of blood or other sites of infection should be cultured. Additional testing for chlamydia, human immunodeficiency virus (HIV), and syphilis should be performed as well.
DIFFERENTIAL DIAGNOSIS
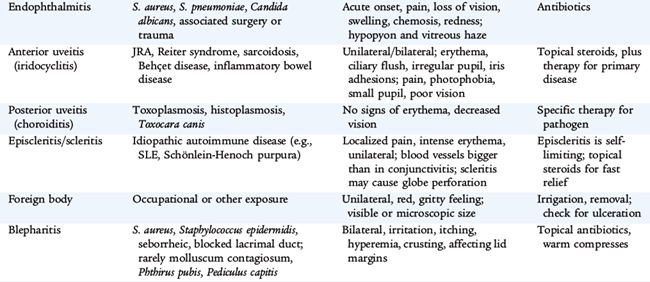
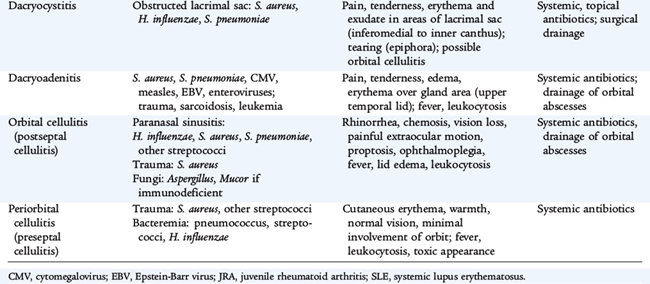
Distinguishing bacterial from viral conjunctivitis by presentation and appearance is difficult (see Table 119-1). Vesicular lid lesions, if present, suggest the diagnosis of HSV. Hyperpurulent conjunctivitis characterized by reaccumulation of purulent discharge within minutes is characteristic of N. gonorrhea infection. The differential diagnosis is delineated in Table 119-3.
Blepharitis is associated with staphylococcal infections, seborrhea, and meibomian gland dysfunction. The child complains of photophobia, burning, irritation, and a foreign body sensation that causes the child to rub the eyes. Eyelid hygiene with an eyelid scrub routine is the initial step in treatment.
Hordeola are acute suppurative nodular inflammatory lesions of the eyelids associated with pain and redness. External hordeola or styes occur on the anterior eyelid, in the Zeis glands, or in the lash follicles and usually are caused by staphylococci. Internal hordeola occur in the meibomian glands and may be infected with staphylococci or may be sterile. If the meibomian gland becomes obstructed, the gland secretions accumulate, and a chalazion develops. Hordeola usually respond spontaneously to local treatment measures, but may recur.
Dacryocystitis is an infection or inflammation of the lacrimal sac, which is usually obstructed, and is most commonly caused by Staphylococcus aureus or coagulase-negative staphylococci. A mucopurulent discharge can be expressed with gentle pressure on the nasolacrimal sac. Treatment usually requires probing of the nasolacrimal system to establish communication.
Endophthalmitis is an emergent, sight-threatening infection that usually follows trauma, surgery, or hematogenous spread from a distant focus. Causative organisms include coagulase-negative staphylococci, S. aureus, S. pneumoniae, Bacillus cereus, and Candida albicans. Examination is difficult because of severe blepharospasm and extreme photophobia. A hypopyon and haze may be visible on examination.
TREATMENT
The lids should be treated as needed with warm compresses to remove accumulated discharge. Acute bacterial conjunctivitis is frequently self-limited, but topical antibiotics hasten resolution. Antibiotics are instilled between the eyelids four times a day until the discharge and chemosis subside. Recommended treatment includes topical ciprofloxacin solution, sulfacetamide 10% solution trimethoprim–polymyxin B solution, and erythromycin ointment. Gonococcal conjunctivitis in adults is treated with a single intramuscular (IM) dose of ceftriaxone (1 g) plus azithromycin (to treat possible concominant chlamydial infection).
The treatment of ophthalmia neonatorum depends on the cause (see Table 119-2). Gonococcal ophthalmia neonatorum is treated with a single dose of ceftriaxone (25–50 mg/kg intravenous [IV] or IM; maximum dose 125 mg). These infants should be hospitalized. Antibiotic treatment also is recommended for newborns to mothers with untreated gonorrhea. The mother and infant should be tested for chlamydial infection. Chlamydial conjunctivitis is treated with oral erythromycin for 14 days, partly to reduce the risk of subsequent chlamydial pneumonia.
COMPLICATIONS AND PROGNOSIS
The prognosis for bacterial and viral conjunctivitis is excellent. The major complication is keratitis, which can lead to ulcerations and perforation. This complication is uncommon except with N. gonorrhoeae infection. Complications of neonatal conjunctivitis are uncommon except with N. gonorrhoeae and HSV infections. Chlamydial conjunctivitis may progress in infants to chlamydial pneumonia, which typically develops from 4 to 12 weeks of age (see Chapter 110).
PREVENTION
Careful hand washing is important to prevent spread of conjunctivitis. Bacterial conjunctivitis is considered contagious for 24 hours after initiating effective treatment. Children may return to school, but treatment measures must be continued until there is complete clinical resolution.
All infants should receive prophylaxis for gonococcal ophthalmia neonatorum. Silver nitrate 1% is used frequently but usually causes a chemical conjunctivitis. Alternative methods are equally effective and less irritating and include a single application of erythromycin 0.5% ointment or tetracycline 1% ointment. Prophylaxis is administered to all newborns, whether delivered vaginally or by cesarean section, as soon as possible after delivery.