Chapter 4 Movement System Syndromes of the Thoracic Spine
Introduction
Thoracic spine pain syndromes are most commonly the result of cumulative microtrauma caused by impairments in alignment, stabilization, and movement patterns. In a normal thoracic spine, balance of the trunk musculature and other contributing tissues (bone, nerve, ligaments, and discs) provides support and control of movement to prevent impairments. The major objective for diagnosis, prognosis, and treatment of thoracic movement system syndromes is to identify all factors that create impairments of the tissues. Thoracic spine diagnoses are determined by direction and magnitude of postural alignment and movements of the thoracic spine that consistently elicit or increase the patient’s symptoms. Individual differences in age, activity level, anthropometrics, and gender assist the physical therapist in (1) understanding the status of the tissues and (2) precisely determining treatment and prognosis.
When a system is multisegmented, as is the case of the human movement system, the greatest degree of motion occurs at the most flexible segment.1 The distribution of motion in the thoracic spine is determined by the mechanical characteristics of the region.2 Following the basic law of physics, movement takes place along the path of least resistance. Thus, because of the increased length of the region (creating a long lever arm) and the angle of the facets (facilitating superior glide and rotation),3 the thoracic region of the spine easily moves into flexion and rotation. To illustrate this concept, consider a young female with a long trunk who develops the habit of bending down to converse with her peers. Thus she develops the movement “habit” of thoracic flexion early in her life. At a later time in this woman’s life, thoracic flexion, coupled with the degenerative process of the aging female spine, creates a structural kyphosis. In the last decades of her life, the unchecked kyphosis becomes so severe that she is predisposed to compression fractures.4-6 Thus the uncorrected habit of thoracic flexion can develop over time into permanent alignment changes.
The most common movement impairments contributing to thoracic spine pain syndromes are related to an imbalance of the trunk and limb musculature creating alterations in the relative flexibility of the thoracic spine. Sustained positions or repetitive movements of the thoracic spine cause microtrauma to the tissues. This microtrauma, if sustained over time, will progress to macrotrauma of the associated spinal structures. Pathology, such as intercostal nerve compromise, disc herniation, osteophyte formation, or compression fracture, will eventually develop as the result of impairments of thoracic spine stability or movement. In addition, upper or lower extremity limb movements during functional activities can impose stress across the thoracic spine. Typically, the movement impairments of the thoracic spine present as excessive or incorrect timing of one or more of the normal motions and positions of flexion, rotation, and extension.
Pain syndromes that develop from movement-related tissue injury require consideration of the mechanisms that cause tissue injury. Factors that affect movement-related tissue injury include (1) excessive joint mobility; (2) impaired timing of the movement relative to the functional requirements; or (3) excessive frequency, duration, or intensity of movement, thus exceeding the tissue’s tolerance to stress.7 Excessive joint mobility will require a precise neuromuscular training program that may include strength training,8 in addition to correction of the impaired movement at the site of pain and the adjoining regions. Patient education for strength training must focus on teaching the patient to control movement within the optimal range of motion (ROM),9 while avoiding excessive frequency of motion for all activities and exercise. Impaired timing of movements present in an individual who moves primarily in the thoracic region without distribution of the motion to other regions of the spine (cervical or lumbar). For example, during forward bending the thoracic spine moves into flexion more rapidly than the lumbar spine (Figure 4-1). Treatment in this circumstance focuses on education regarding reduction of thoracic spine motion by redistribution of the motion to other regions by increasing hip and knee flexion (Figure 4-2).
Finally, excessive frequency, duration, or intensity of movement creates an imbalance of stress on tissues so that tissue recovery is impaired and pain develops. Treatment in this case necessitates reduction of one or more of these factors to protect the tissues. Consideration of the frequency, duration, and intensity of the motion allows the physical therapist to individualize patient education regarding all activities, whether recreational, occupational, or functional. For example, excessive performance of trunk curl exercises increases the stiffness and shortens the abdominal musculature, while simultaneously increasing the length and possibly weakening the thoracic trunk extensors. Weakness of the back extensors has been associated with kyphosis.10-12 Thus reducing the frequency of performance or elimination of trunk curling exercises may be necessary in an individual with a thoracic kyphosis. Likewise, the amount of time spent in a specific position that would flex the spine will contribute to development of a kyphosis. Questioning the individual regarding typical daytime activities can give insight into the amount of time spent sitting or standing. Observation of the patient during “nonclinical” examination times, such as sitting in the waiting room, waiting for the home program to print, or bending down to pick up her purse as she is leaving the clinic, is helpful to determine the presence of habits or body language that perpetuates impaired movement patterns. Some individuals with an overdeveloped and short rectus abdominis (RA) muscle demonstrate thoracic flexion even when they laugh.
The keys to prevention and correction of thoracic spine movement system syndromes are (1) to have the trunk musculature hold the vertebral column in the optimal alignment, (2) to address limb movements that perturb the vertebral column, and (3) to prevent repeated movement at the most flexible thoracic segments during functional activities. To achieve these aims, the impairments in muscle length, stiffness, and performance are addressed. Movement education is provided for motor learning during both trunk and limb motions. In the case of excessive thoracic flexion, the movement of the trunk into forward flexion would be redistributed to increase the motion across the hips instead of across the thoracic region. The habit of flexing primarily in the thoracic region during forward bending needs to be addressed during education regarding common functional activities such as bending, dressing, and lifting tasks. Finally, functional activities are modified to reduce stresses on the thoracic spine segments. For example, sitting alignment is corrected to avoid the position of thoracic flexion, thus decreasing the resting length of the thoracic paraspinal musculature and increasing the resting length of the abdominal musculature.
This chapter presents key principles for examining alignment and movement, determining muscle length, and testing the strength of the musculature of the thoracic spine. The diagnostic categories for the thoracic region are described (Table 4-1). Case examples are provided for the most common movement system syndromes. Associated cervical, scapular, and lumbar region movement system syndromes are mentioned. Syndrome-specific treatment suggestions are provided, including movement system impairment exercises and patient education for functional activities and personal habits.
TABLE 4-1 Thoracic Spine Movement Impairment Syndromes
| Syndrome | Key Findings |
|---|---|
| Rotation-flexion | Pain with postures or motion that flex and rotate the thoracic spine. |
| Flexion | Pain with postures or motion that flex the thoracic spine. In the case of increased kyphosis, pain may occur with correction of the alignment. |
| Rotation-extension | Pain with postures or motion that extend and rotate the thoracic spine. |
| Rotation | Pain with postures or motion that rotate the thoracic spine. |
| Extension | Pain with postures or motion that extend the thoracic spine. |
Alignment of the Thoracic Spine
Normal Standing Alignment
In standing, the normal alignment of the thoracic spine is a flexion curve of 40 degrees, as measured using a Cobb angle.3,13-23 Clinically, a normal thoracic spine has a mild posterior convexity and even distribution of flexion (Figure 4-3). The shape of the thoracic curve is attributed to a slight wedging of the vertebrae.96 A lateral view of a chest x-ray shows that the anterior aspects of the vertebral bodies are slightly smaller than the posterior aspect24 (Figure 4-4). There are no known sex differences in the overall amount of normal thoracic flexion alignment17,25,26; however, with aging, there is an increase in thoracic flexion, with females demonstrating a greater increase than males.17,25

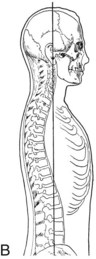
Figure 4-3 A and B, Normal thoracic alignment.
(B, From Kendall FP, McCreary EK, Provance PG: Muscles: testing and function, ed 4, Philadelphia, 1993, Lippincott Williams & Wilkins.)
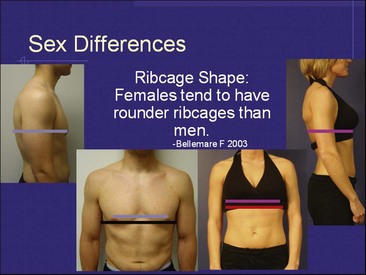
The normal rib cage is slightly rounded in circumference—the superior aspect of the rib cage is more narrow than the inferior aspect. The rib cage is normally symmetrical from side to side. The shape of the rib cage can be attributed to the variation in the length and curvature of the ribs and their anterior attachment to the sternum. The angle formed by the costal margins of ribs 7 to 10 is referred to as the subcostal margin. An ideal subcostal angle of approximately 90 degrees is considered to be a reflection of balance between the length of the internal and external oblique muscles.1-27 Age-related changes of the rib cage have not been well studied; clinical observations indicate that individuals with a thoracic kyphosis, as well as individuals with central obesity, will have a flaring of the lower ribs. Reported sex differences of the rib cage indicate that males tend to have a narrower anterior-to-posterior dimension and a broader medial-to-lateral dimension, whereas females tend to have a more rounded chest wall with a narrower overall diameter28 (Figure 4-5).
Impaired Standing Alignment
Alignment impairments of the thoracic spine can be both postural and structural. Postural impairments are flexible and respond to positional changes or cues to change alignment. Structural alignment impairments are fixed alignments of the boney structures that persist, regardless of the position of the individual. Though structural changes are present, some correction may be possible if connective tissues are extensible. Genetic variation in tissue mobility is a factor in determining the magnitude of alignment change. A structural impairment can be demonstrated with radiographic studies. Attempts to change a structural alignment may increase stress across a region and may worsen a pain syndrome by forcing motion above or below the malaligned segments. For example, cueing an individual with a structural kyphosis to extend the thoracic spine often results in an increase in lumbar or cervical extension. Recognition of a structural impairment and accommodation for the fixed impairment must be made to reduce mechanical stresses and pain. Patients may also present with a combination of structural and postural alignment impairments. In this case, attempts at postural correction may be only partially successful.
There are five categories of impaired thoracic alignment: kyphosis, posterior trunk sway, flat back, rotation, and scoliosis. Thoracic kyphosis is defined as an increase in the flexion curve in the thoracic region3,29 (Figure 4-6). With a sustained postural kyphosis, structural accommodation to the persistent anterior forces on the vertebral bodies results in increasing disc and vertebral body loading, causing a wedging of the thoracic vertebrae.5 In this case, kyphosis that started as a postural fault becomes a structural impairment according to the principles of Wolff’s law. This phenomenon commonly is not painful until a severe kyphosis has developed.
Individuals with a thoracic kyphosis commonly have a lumbar lordosis.29 Specific movement testing may help to determine if the kyphosis-lordosis alignment is (1) structural (fixed), (2) caused by weakness or excessive length of thoracic extensor muscles, or (3) caused by passive stiffness or frequent (habitual) contraction of the abdominal musculature, specifically the RA. Usually, when the kyphosis is structural, the thoracic curvature does not change when the patient is examined in the supine, prone, and quadruped position even when instructed to straighten the thoracic spine. Although a structural kyphosis can occur at any age, older individuals with degenerative changes and osteoarthritis are more likely to have a structural kyphosis.
Scheuermann’s disease, or juvenile kyphosis, is a structural impairment believed to occur as the result of a variation in the growth of the endplates of the vertebral bodies.30 However, the etiology of Scheuermann disease is still unknown. The structural change is a wedge deformity of 5 degrees or more across three consecutive vertebrae31 (Figure 4-7). The lower thoracic or high lumbar regions are most commonly involved, and the thoracic kyphosis is typically greater than 45 degrees.30,32 Individuals with Scheuermann’s disease should avoid positions or exercises that contribute to thoracic flexion. Attempts to overcorrect the thoracic flexion could result in increased lumbar extension. Patient education is important regarding the effect of anterior compressive forces on the spine and minimizing activities that would worsen the condition such as unsupported sitting, trunk curl exercises, and even various weight-training exercises. The patient should also avoid activities that require prolonged trunk flexion.
Figure 4-7 X-ray of Scheuermann’s disease.
(Courtesy of Dr. R. Cairns. From Cassidy JT, Petty RE: Textbook of pediatric rheumatology, ed 5, Philadelphia, 2005, Saunders.)
Osteoporosis is another condition that often results in a thoracic kyphosis because of vertebral compression fractures that result in wedge deformities of the thoracic vertebral bodies.5 The greatest risk factor for development of a compression fracture in an osteoporotic spine is a previous fracture in the same region.33,34 Kyphosis as a result of osteoporotic compression fractures has been reported to be associated with decreased function and quality of life35 and an increased risk for falls.36,37
Posterior trunk sway of the thoracic spine occurs when the upper back is shifted backward and the hips are swayed forward so that typically the shoulders are posterior to the hip joints.29 Generally, individuals with this type of posture have a long kyphosis29; however, the amount and location of the thoracic flexion may vary. Posterior trunk sway results in decreased participation of the trunk extensors and an increase in the use of the RA as an antigravity muscle to control the trunk.38 In this alignment impairment, a thoracic kyphosis can be masked by the change in alignment of the both the lower thoracic spine at the region of the thoracolumbar junction (posterior glide of the vertebrae) and the upper body sway behind the hip joint axis (Figures 4-8 and 4-9).
The flat back posture is one in which the thoracic spine is straight or the degree of flexion is notably less than normal. In severe cases of a flat thoracic spine, there can be the appearance of a thoracic lordosis (Figures 4-10 and 4-11). The flattened thoracic spine can be an assumed posture or structural variation. When the thoracic spine is extended, structural changes are more likely. The individual with a postural flat back will be able to achieve some thoracic flexion. Those with a structural flat back usually cannot achieve full flexion, even with an active effort to curl the trunk.
There is a lack of normal rib cage contour in a structural flat back alignment, which often makes the scapulae more prominent on the thorax. The prominence of the vertebral border of the scapulae can be mislabeled as winging. Grieve39 notes that a flat thoracic spine is common in individuals with a “painful stiffening” of the cervical region, as well as increased complaints of neck and shoulder pain. Individuals with a flat thoracic spine are more likely to have pectus excavatum.40
Rotation of the thoracic spine is almost always an acquired problem that results from repeated movements in one direction. Activities requiring rotation associated with throwing or one-handed sports such as in baseball, softball, volleyball, or tennis can cause rotation of the thorax. Even less vigorous activities such as sitting at a desk and rotating frequently to one side to work on a computer or to answer the phone can also contribute to the thoracic spine becoming rotated. In these individuals, the rotation of the rib cage can be evident in the front view by asymmetry of the rib cage with the side contralateral to the rotation being more prominent. In this type of rotation, there is not the compensatory rotation in the opposite direction with the S-type curve that is the prevailing feature of scoliosis as described below. Some clinicians may refer to this form of rotation which is usually in only one plane as a functional scoliosis though most often the rib deformity is not as marked nor is the lateral flexion of the trunk present.
The last category of impaired thoracic alignment, scoliosis, is present when the thoracic spine and rib cage are rotated. Rotation of the rib cage and/or the thoracic vertebrae may be localized to a few vertebrae or can involve the whole thoracic spine.3 An asymmetrical contour of the rib cage is usually evident from a posterior view and becomes even more obvious in forward bending. The asymmetry may also be evident from an anterior view (Figure 4-12). The asymmetry of the rib cage usually causes an asymmetry in the position of the scapulae. Scoliosis can be postural or structural or a combination of both. Postural scoliosis, sometimes referred to as functional scoliosis,29,41 is considered present when there is an asymmetry in the alignment of the thoracic spine or rib cage that is not fixed. Similar to other alignment impairments, postural scoliosis can be distinguished from structural based on the ability to restore symmetrical alignment. Postural scoliosis can occur as the result of an activity, such as throwing, that would habitually rotate the thoracic spine (Figures 4-13 and 4-14). In a postural scoliosis, there are no structural changes in the shape of the vertebral bodies or ribs.

Figure 4-12 Asymmetrical rib cage. A, Slight appearance and asymmetry. Note arm position in relation to rib cage and pelvis. B, Right side of rib cage more prominent than left. C, Another method demonstrating right rib cage prominence.
Structural scoliosis is defined as a structural impairment of the vertebrae that affects all three planes: frontal, sagittal, and transverse3 (Figure 4-15). Structures that are affected by this asymmetry include not only the vertebral body but also the corresponding ribs and soft tissue structures. Idiopathic scoliosis most commonly presents in adolescence and is believed to have a familial pattern.42 The etiology of idiopathic scoliosis is believed to be multifactorial; possible contributing factors are hormones,43-46 biomechanics,47-50 and motor control.51-55 Increased height and hypokyphosis, or flat spine, which potentially causes improper loading of the spine and thus asymmetrical growth patterns, have also been reported in individuals with idiopathic adolescent scoliosis.47 Locomotor skills, including lateral step, balance strategies, and vibratory sense, have been reported as impaired in individuals with a structural scoliosis.51-55 Currently, it remains unclear if the motor control impairments contribute to the spine malalignment or if the spine malalignment contributes to the motor control impairments.
Rib Cage Alignment Impairments
The most common rib cage alignment impairments are rotational asymmetry or altered rib cage circumference. In the presence of either impairment, the subcostal angle will show a deviation from the normal symmetrical angle of approximately 90 degrees. Widening of the subcostal angle is often accompanied by an outward flare of the lower ribs in obese individuals or those with poor abdominal muscle tone. Overdevelopment of the pectoral muscles in an individual with poor abdominal muscle control can contribute to rib cage malalignment because every time the pectoral muscles are contracted the rib cage is elevated. Conversely, overdevelopment of abdominal musculature can result in narrowing of the subcostal margin; these concepts are discussed in the “Abdominal Muscle Length” section later in the chapter.
Obesity causes increased fat distribution within the chest and abdomen, which can lead to the long-term development of a barrel-shaped chest (Figure 4-16). Changes in trunk shape can be seen even in individuals who have lost weight.56 This change in the contour of the chest wall may cause the scapulae to appear more internally rotated; however, overcorrection of scapular alignment should be avoided because of this change in chest wall shape.
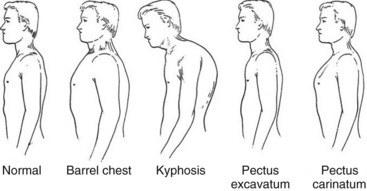
Figure 4-16 Variations in trunk shape.
(From Frownfelter D, Dean E: Cardiovascular and pulmonary physical therapy, ed 4, St Louis, 2006, Mosby.)
Rib cage asymmetry is commonly caused by changes in thoracic spine alignment, as well as muscle length changes in the trunk and shoulder girdle. Thoracic spine rotation will create asymmetry in the subcostal angle, with one side appearing to be closer to midline than the other. As with scoliosis, subcostal angle asymmetry can be structural, postural, or both. Asymmetry of the rib cage can cause approximation of two adjacent ribs, resulting in compression of the intercostal nerves or increased tension at the rib insertion along the sternum or costal cartilage. Common conditions that could result include intercostal neuritis or neuralgia,57-61 costochondritis,62,63 and slipping rib syndrome.63-65 The alignment of the lower ribs is greatly affected by muscular interaction of the external oblique, internal oblique, transversus abdominis, and diaphragm (see the following sections, “Abdominal Muscle Length” and “Muscle Performance”).
Assessment of the upper extremity muscle length and function is needed to determine if muscle imbalance in the shoulder girdle is contributing to upper rib cage postural malalignment.29
Other structural impairments of the rib cage include pectus excavatum, or funnel chest, and pectus carinatum, or pigeon chest (see Figure 4-16). When severe, these conditions can require surgical intervention. Rib cage depression compromising the heart and lungs occurs with severe pectus excavatum.67 Cosmesis is the most common reason for surgery with pectus carinatum.66 Both conditions commonly present with a hypokyphosis and scoliosis67 and are theorized to occur because of overgrowth of costal cartilage.68
Only limited information is available on conservative management of pectus excavatum and pectus carinatum.67,69,70 Physical therapy is believed to be helpful if thoracic or chest wall pain is present in someone with either of these conditions.69,70 Understanding the biomechanical effect of the structural changes on movement may help guide expectations for treatment. With pectus excavatum because there is a fixed depression of the sternum, during inhalation there is insufficient sternal elevation resulting in decreased pump handle motion of the ribs.29,56 On the other hand, pectus carinatum is a deformity of the chest characterized by a protrusion of the sternum and ribs. With pectus carinatum there may be insufficient sternal and rib depression during exhalation. Thus, in both cases, there is the potential to develop a secondary ventilatory impairment as well as affect the length of the abdominal and intercostal musculature. In the case of pectus excavatum, the abdominal and intercostal muscles may be shortened, whereas in the case of pectus carinatum, they may be lengthened. Breathing exercises with emphasis on the specific mechanical deficit can be used to improve ventilatory mechanics in either case.66,70
Normal Sitting Alignment
Ideal sitting alignment for most people is with the spine erect and supported, the shoulders aligned over the hips, the feet supported, and the hips flexed to 90 degrees.1,29 In unsupported sitting, normally, the pelvis is in a slight posterior tilt, resulting in flat lumbar spine but relatively unchanged thoracic and cervical spinal alignment when compared to the standing position.3 Because of the variation in posture and anthropometrics among individuals, no chair or sitting surface is perfect for everyone. For example, a person with a long trunk will require a chair back that is higher than average to maintain adequate support of the spinal column. An individual with a fixed kyphosis should have extra support at the base of the chair back to support the lumbar spine and allow the thoracic spine to rest against the back of the chair (Figures 4-17 and 4-18). In this position, the thorax assumes a vertical alignment, which facilitates good alignment of the cervical spine. Note also that the support at the lumbar spine should not contribute to lumbar extension.1 In an erect unsupported sitting position, there is a significant increase in the activity of internal obliques and thoracic and lumbar paraspinal musculature as compared to the slumped sitting position.38 With prolonged slumped sitting, there is a “flexion relaxation phenomenon” that occurs in the thoracic erector spinae muscles.71,72 Thus, as an individual deviates from an ideal erect position to a more flexed thoracic spine, there is an increased dependence on the passive structures of the spine. Because both erect and relaxed unsupported sitting can be difficult for an individual to maintain, a chair with a back support should be used for prolonged sitting.
Impaired Sitting Alignment
Impaired sitting alignment can be the result of postural alignment impairments, anthropometric variations, and improper environmental factors, including seating surface and work-station configurations. Postural alignment impairments in sitting include a combination of excessive thoracic flexion, rotation, or extension, depending on the habits and alignment of the patient. A patient with thoracic rotation-flexion syndrome may habitually sit with the hips away from the chairback and leaning over onto the armrest. Sitting on one foot or sitting with your legs crossed is a common habit that can contribute to a postural scoliosis and thoracic rotation movement system syndrome. Sitting on the edge of the seat while maintaining the trunk in too erect a position may be noted in individuals with a flat thoracic spine and thoracic extension syndrome. Individuals with a long trunk and short arms are susceptible to leaning over on an armrest because of lack of support while sitting. Individuals with long legs may sit with their knees higher then their hips, causing excessive lumbar and thoracic flexion. Specific seating surface issues need to consider the effect on the thoracic spine. For example, a recliner or low couch may contribute to thoracic flexion. Habitually practicing the piano on a bench without back support may contribute to thoracic extension. The configuration of an office may contribute to thoracic rotation if the patient habitually turns to one side to file, answer the phone, or read the computer monitor. Treatment suggestions for correction of specific sitting postures can be found in the descriptions of the thoracic movement system syndromes and treatment.
Motion of the Thoracic Spine
Clinical examination of thoracic spine and rib cage motion is critical to determine key components of the syndrome and subsequent treatment. Development of a “clinical eye” for impaired thoracic spine and rib cage motion starts with understanding the kinematic principles related to normal motion. Essential aspects of movement that should be considered include the path of instantaneous center of rotation (PICR) for each motion, the normal amount of accessory and physiological motion available at each joint/region, and specific anatomical considerations unique to the thoracic spine and rib cage.
Thoracic Spine Motion
Across the twelve thoracic vertebrae, motion is cumulative, with each segment contributing relatively small degrees of movement for each direction. In comparison, sagittal plane motion of the thoracic spine segments is more limited than in the cervical and lumbar regions. The amount of motion that is available in the upper and middle thoracic regions is limited by the ribs and sternum. The lower thoracic segments have floating ribs that do not limit mobility as much as true ribs, thus contributing to increased sagittal plane motion in the lower thoracic segments.2
During active thoracic flexion and extension, motion should be occurring in all segments; however, the distribution of motion should gradually increase from T1 to T12. Currently, it is accepted that normal thoracic flexion ROM is 30 to 40 degrees, while thoracic extension is 20 to 30 degrees with a combined ROM of 50 to 70 degrees.3 According to White and Panjabi,2 for flexion and extension the contribution of motion from each segment is as follows: The upper thoracic spine (T1 to T5) contributes approximately 4 degrees of motion, the middle thoracic spine (T6 to T10) contributes approximately 6 degrees of motion, and the lower thoracic spine (T11 and T12) contributes 12 degrees of motion (Figure 4-19). According to Panjabi et al,73 the PICR for flexion and extension of the thoracic spine is centered in the body of the inferior vertebrae. During thoracic flexion, there is an anterior-superior translation of the inferior facet of the superior segment, and during extension, there is a posterior-inferior translation of the inferior facet of the superior segment (Figures 4-20 and 4-21). Observation of increased motion at any segment is probably indicative of increased translation at that segment. Research related to the normal amount of in vivo motion is very limited.
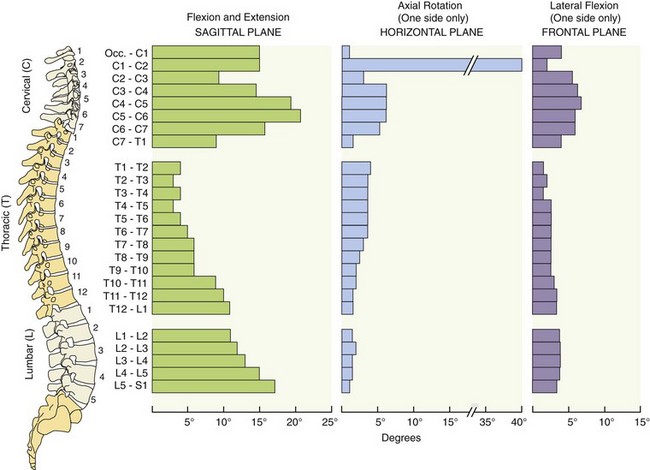
Figure 4-19 Distribution of motion across each segment of the spinal column.
(Styled after White AA, Panjabi MM: Kinematics of the spine. In White AA, Panjabi MM, eds: Clinical biomechanics of the spine, ed 2, Philadelphia, 1990, Lippincott. In Neumann, DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)
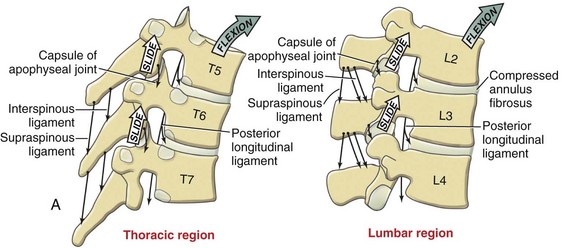
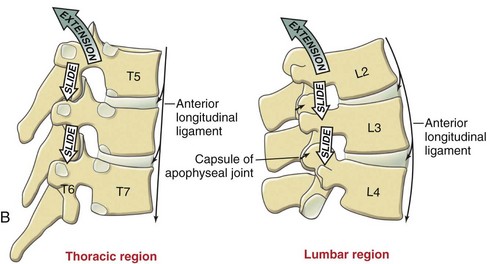
Figure 4-20 A, Thoracic flexion. B, Thoracic extension.
(Modified from Neumann, DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)
(From Neumann, DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)
Because of the approximation of the ribs and the orientation of the facets, the amount of lateral bending in the upper and middle thoracic spine is relatively small. The upper and middle regions of the thoracic spine contribute 6 degrees of motion, whereas the lower segments T11 and T12 contribute 8 to 9 degrees of motion at each segment.2 The total amount of thoracic lateral bending is 25 degrees.3 The PICR for lateral bending is centered in the lateral half of the body of the inferior nonmoving segment, contralateral to the direction of the motion.2 For example, during right lateral flexion, as T8 moves to the right, the PICR will be in the left lateral aspect of T9 vertebral body.
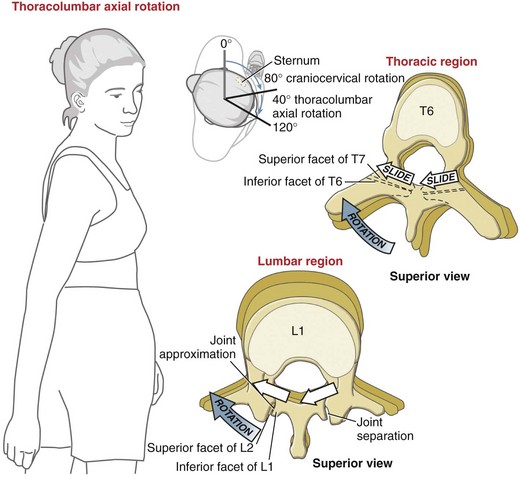
In contrast to lateral flexion, there is a greater amount of rotation ROM available in the thoracic spine. In addition, compared to the lumbar spine, the motion of rotation is greater in the thoracic region. Total amount of unilateral rotation in the thoracic region is 30 to 40 degrees.3,74-76 The upper and middle regions of the thoracic spine demonstrate more rotation ROM than in the lower thoracic region (see Figure 4-19). The angle of the thoracic facets allows increased motion into rotation, especially in the upper and middle thoracic region.2 White and Panjabi report the following values for rotation: T1 to T10 contributes 8 to 9 degrees of motion from each segment, whereas at the thoracolumbar junction, T11 and T12 only contribute 2 degrees of motion per segment.2
Description of the PICR for thoracic rotation differs between sources depending on the study methodology. White and Panjabi’s conclusion that the PICR for rotation is located on the endplate and spinal canal of the inferior vertebrae is based on their literature review.2 Most of the studies included in their review used cadavers with the rib cages removed. Molnar et al77 used geometric modeling of the thoracic spine with ribs attached and concluded that the PICR is in the anterior portion of the spinal canal. Placement of the PICR for rotation in a more anterior location or lateral location would create spinal cord displacement, which is known as the cigar-cutting effect. Because of these relative small axes of motion, when observing the motions of lateral flexion and rotation, one should observe motion being equally distributed across each segment. Rotation of the thoracic spine should be symmetrical and maintain a relatively vertical axis with minimal lateral movement. Any significant lateral “off axis” translation observed during active thoracic rotation would be considered an impairment. Clinically, thoracic rotation is the most common cause of pain syndromes in the thoracic region.2,78-80
The upper thoracic region is believed to demonstrate an ipsilateral coupling pattern of lateral flexion and rotation, similar to the cervical spine, whereas the middle and lower segments demonstrate an inconsistent pattern of coupling.2,3,81 Recent investigators, however, have noted that the coupling pattern of lateral flexion and rotation of the thoracic region remains inconsistent across all regions.82 Generally, end-range of flexion or extension of the thoracic spine will decrease the amount of rotation that is available, resulting in compensatory lateral flexion to gain ROM.39,74 The ease of motion into flexion and anterior translation causes joint surface approximation and soft tissue tension; subsequently, either rotation or lateral flexion can cause relatively large stresses on the soft tissues in the region of the thoracic spine. A movement examination should include the observation of (1) the starting position of the thoracic spine and (2) the relative segmental contributions for rotation and lateral flexion. Based on these observed movement impairments and the effect on the symptoms, a specific treatment program can be developed.
Incidence of degeneration of the thoracic spine is relative low when compared to the lumbar and cervical spines.83,84 This difference in the thoracic region has been attributed to a relatively small PICR for the thoracic spine motions, the load-bearing capacity of the ribs, and the relative small size of the intervertebral discs.83 Lower segments of the thoracic spine are the most common site of degeneration and disc herniation.83,84 Atypical symptoms related to neural compromise have been reported in individuals with thoracic herniation, including extremity, abdominal, pelvic, and chest pain.85-92
Rib Cage Motion
During ventilation, there is a simultaneous change in the rib cage shape across three planes of motion. During maximum inhalation, there is a slight superior and posterior motion of the thoracic vertebrae causing very slight extension, as well as superior anterior expansion of the rib cage81,93 (Figure 4-22). Rotation of the ribs occurs during this superior motion along a 35- to 45-degree axis from the demifacets located on the vertebral bodies and discs. During exhalation, there is a reversal of these motions. Pump-handle motion is the sagittal plane or anterior superior motion of the ribs. Bucket-handle motion is the frontal plane or superior lateral motion of the ribs. Clinical assessment of ventilatory motion should include observation of the lateral and anterior aspects of the rib cage and a posterior view of the thoracic spine. The alignment of the trunk and the flexibility of specific vertebral segments contribute to the development of common movement system syndromes. For example, during inhalation, individuals with a thoracic flexion syndrome and a kyphosis have decreased superior motion of the spine, sternum, and anterior rib cage, with an increase in the lateral motion of the rib cage. Individuals with a swayback alignment have excessive posterior motion of the thoracic spine during ventilation. Individuals with a thoracic extension syndrome with a flat thoracic spine have an increase in the superior posterior motion of the spine and superior anterior motion of the sternum and anterior rib cage. Rotation of the thoracic vertebrae causes rotation of the rib cage. Thus, in the case of scoliosis, the rib cage is asymmetrical. Asymmetrical breathing patterns are common in individuals with scoliosis and have been suggested as contributing to imbalances of the trunk musculature.94
Musculature of the Thoracic Spine and Rib Cage
Muscles of thoracic spine and rib cage are described by their anatomical location: posterior and anterior. Most of the musculature of the thorax is continuous with other regions, specifically the lumbar spine and the upper extremities; however, this discussion is based on the primary role of a muscle or muscle group as it pertains to the thorax.
Posterior Musculature
Muscles Responsible for Thoracic Motion and Stability
The erector spinae muscle group is the most superficial of the spinal extensors. The muscles of the erector spinae are a complex arrangement of muscle that originates from a common tendinous aponeurosis attached to the sacrum and spinous process of the lumbar and lower thoracic spines.95 The erector spinae divides into ascending sections by muscle fibers that blend from section to section, terminating at the cervical spine. The mass of the erector spinae muscle is greatest in the lumbar and thoracic regions. The three thoracic sections of the erector spinae muscles are iliocostalis thoracis, longissimus thoracis, and spinalis thoracis. The iliocostalis thoracis, the most lateral of the thoracic erector spinae muscles, originates not only from the tendinous origin of the sacrum but also from muscle slips that run from the transverse processes of the lumbar and thoracic regions and ribs. Specifically, the iliocostalis thoracis originates from the lower six ribs, ascending to insert into the upper six ribs. The longissimus thoracis, the intermediate muscle of the thoracic erector spinae, has the largest cross-sectional area of the spinal extensors and originates from the erector spinae aponeurosis and spinous processes of lumbar vertebrae and inserts into the transverse processes and ribs of the lower nine ribs. Finally, the spinalis thoracis, the most medial muscle of the erector spinae group, arises from the vertebral spines of the upper lumbar and lowest thoracic vertebrae. The spinalis thoracis muscle fibers blend with the iliocostalis thoracis laterally and semispinalis thoracis superior-laterally before inserting on the spinous processes of the upper thoracic vertebrae.
The complexity of this anatomical arrangement provides insight into the motor control requirements specific to the thoracic erector spinae. In standing, isolated contraction of the thoracic erector spinae extends the thoracic spine without necessarily extending the lumbar spine. Contraction of the lumbar erector spinae without simultaneous contraction of the thoracic erector spinae, contributes to lumbar extension and/or a posterior lower thoracic trunk sway. Thus the thoracic spine can be flexed while the lumbar spine is extended. Another possibility is flexion of the upper thoracic spine with posterior translation/extension at the thoracolumbar junction. Clinically, the differences in regional control of the erector spinae muscles enable the patient to hold the lumbar spine and thoracolumbar junction stable while moving the thoracic spine out of flexion.
From the upright position, bilateral erector spinae contraction extends the spine. When bending forward, the erector spinae work eccentrically until approximately two thirds into the range,96 at which point their activity normally subsides and the trunk motion is controlled by the eccentric activity of the hip extensors. A similar pattern in reverse occurs with the return to the upright position. Erector spinae activity is necessary in the upright position to counter the force of gravity. The thoracic erector spinae have a greater percentage of type I muscle fibers than lumbar erector spinae muscles, suggesting a greater reliance on the thoracic erector spinae for postural support.96,97 Not all authors agree on the contribution of the unilateral erector spinae to thoracic rotation or lateral flexion3,29,80,96; however, recent work using intramuscular electromyography (EMG) has demonstrated that the longissimus thoracis is active during seated ipsilateral trunk rotation and lateral flexion.80,99 The capacity of the longissimus thoracic for torque production during rotation may be greater in the upper thoracic spine than in the lower thoracic spine.80
Contraction of the right longissimus thoracis during left arm movement would help offset the trunk flexion, rotation, and lateral flexion moments.100 Thus, using arm motions to help promote thoracic muscle activity is a useful treatment strategy. Instructions are given to the patient to maintain thoracic spine and rib cage stability while flexing the shoulder. Initially the patient may need to perform this with the elbow flexed to shorten the lever arm and reduce the load. As control improves, the shoulder can be flexed with the elbow in extension or an elastic band can be used for added resistance to the shoulder motion. Alternatively, the patient could lift a weight from counter height and hold it in his hands while maintaining the appropriate thoracic alignment; this could be done using one or both hands, depending on the ability to control the rotatory force.
Thoracic kyphosis creates a shorter lever arm for the erector spinae while placing the muscles in lengthened position, forcing them to generate large extension moments to counter the effects of gravity.101 These large extension moments create increased spinal compression. In addition to the change in muscle force, the center of gravity moves anterior as a result of the thoracic kyphosis, further compounding the situation.101 Clinically, the implications of this are that we must help our patients correct their postural kyphosis and minimize progression, if structural. The patient with structural kyphosis will require greater finesse in exercise and postural correction because compensatory extension in the other areas of the spine must be avoided.
The intermediate layer of spinal extensor muscles is comprised of semispinalis thoracis, the multifidi, and the rotatores. In each of these muscle groups, the number of spinal segments crossed by the muscles progressively decreases when moving from superficial to deep. For example, the semispinalis thoracis will cross six to eight spinal segments, the multifidi cross two to four segments, and the rotatores usually span only one to two segments.3,95 This arrangement permits the smaller muscles to have more precise control over their respective segments. The thoracic rotatores are most developed compared to the other regions in the spine, yet their exact purpose is not fully understood.3,96 These muscles are thought to be more “position sensors than torque producers,”96 so their contribution to motor control in the thoracic spine is important.
Multiple studies have investigated lumbar muscle EMG activity in both normals and subjects with low back pain; however, by comparison, there are very few publications that have examined the muscle activity in the thoracic region. Despite the regional proximity, assumptions that the thoracic spine musculature would behave similarly to the lumbar should not be made because the thoracic spine motion and muscle activity are complicated by the rib cage80 and differences in facet joint orientation.2 In response to arm movement, the multifidus activity in the lumbar spine was independent of force direction102; however, the activity of the thoracic multifidus was dependent on the direction of arm motion so that right arm movement was associated with electromylographic (EMG) activity in the right thoracic multifidus muscles.80 During sitting trunk rotation, the activity of the thoracic multifidus was variable. Bilateral activity of the multifidus occurred in upper thoracic segments during trunk rotation, but no consistent pattern of activity was found for the multifidus in the middle and lower thoracic spine.80 The authors suggest that the multifidus function in the middle and lower thoracic spine may be to control rotational forces.80
The interspinales and intertransversarii are the deepest layer of the posterior spinal muscles. This muscle group is thought to be absent in the thoracic region by some,3 and others report the presence of these muscles in only the upper and lower segments of the thoracic spine.29,95 The significance of these muscles in the thoracic spine is not known.
Although the quadratus lumborum muscle attaches to the twelfth rib, its influence on the thoracic spine is mainly through the stabilization that it provides to the pelvis and lumbar spine.
Extremity Muscles with Spinal Origin
The latissimus dorsi muscle originates from the lumbodorsal fascia; the last three or four ribs; and spinous processes of the sacral, lumbar, and the lower six thoracic vertebrae. The muscle traverses laterally and superiorly to insert on the humerus. With the insertion of the latissimus held relatively stable, bilateral contraction of the muscle will assist with anterior pelvic tilt and spinal extension. If acting unilaterally, contraction of the latissimus produces a rotation moment on the lumbar and lower half of the thoracic spine. According to Porterfield and DeRosa,104 the latissimus dorsi muscle has a long moment arm, thus small forces generated from this muscle can easily influence the mechanics of the spine. Passive tension from the latissimus dorsi muscle should also be considered. Shortness or stiffness of the muscle may induce spinal rotation with unilateral arm motion or spinal extension with bilateral shoulder flexion. Because the latissimus muscle originates from the lower half of the thoracic spine, its effect will be noted in the lower half of the thoracic spine. With stiffness or excessive recruitment of this muscle, there is the potential for extension and/or rotational asymmetry to develop in the lower and midthoracic region.81 Imbalance of the latissimus can contribute to excessive flexibility at the midthoracic level because the lower segments are pulled into rotation while the upper segments remain neutral.
The trapezius and rhomboid muscles are also upper extremity muscles with origins on the thoracic spine. The middle and lower trapezius originate on the thoracic vertebrae, first through fifth and sixth through twelfth, respectively.29 The rhomboid muscles run from the spinous processes of the thoracic vertebrae first to fifth down to the medial border of the scapula. When contracting bilaterally, either the trapezius or the rhomboid muscles can produce an extension moment on the thoracic spine.96 Clinically, this is can be seen in individuals with a flattened thoracic spine; rhomboid muscle contraction is associated with extension of thoracic spine in the interscapular area. Similar to the latissimus, unilateral contraction of the rhomboid and trapezius muscles can cause contralateral rotation of the thoracic spine.
Anterior Musculature
Generally, abdominal muscles are recognized as having a variety of essential functions: support and protect the internal organs, assist with exhalation, and provide both stabilization and movement of the trunk. Probably less understood is what constitutes ideal abdominal performance. There is often an exaggerated emphasis on abdominal strength, especially the RA, and little attention is paid to motor control. The influence of abdominal muscle length on abdominal muscle function is often underappreciated. Assessment of abdominal muscle length, recruitment patterns, and performance are an important part of a thorough thoracic examination. Furthermore, treating patients with pain syndromes by indiscriminately issuing abdominal exercises may perpetuate their thoracic movement impairments.
Abdominal Muscle Length
Ideal abdominal muscle length promotes ideal trunk alignment. Optimal resting length of each of the abdominal muscles holds the spine, rib cage, and pelvis in the correct position. Because passive tension of the abdominal musculature contributes to postural control, the efficiency of maintaining good trunk alignment is greatly enhanced when the abdominal muscles are at ideal length. Consider the effect that a short RA muscle will have on trunk alignment. Individuals with a short RA muscle appear to have a depressed chest, and the thoracic spine will be kyphotic (Figure 4-23) or swayed posterior because the anterior thorax is pulled down toward the anterior rim of the pelvis. This is because the primary action of the RA muscle, which runs from the pubic rim of the pelvis up to the costal margins of the fifth through seventh ribs and xiphoid process, is to curl the trunk by approximating the sternum to the anterior pelvis.29 In athletic populations, the RA muscle is often overdeveloped with “sit-up”-type exercises that lead to shortness or an increased stiffness of the muscle. Shortness of the RA muscle can contribute to movement impairments, as well as alignment impairments, by limiting thoracic extension; individuals may perform lumbar extension as a compensation for the lack of thoracic extension. Although the individual appears to have brought the thorax to a more upright position, what has occurred is an exaggeration of the curves in the thoracic and lumbar spines (see Figure 4-28, B).
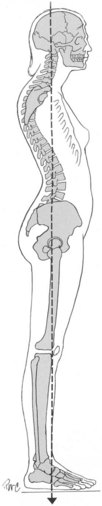
Figure 4-23 Exaggeration of the curves in the thoracic and lumbar spines.
(From Kendall FP, McCreary EK, Provance PG: Muscles: testing and function, ed 4, Philadelphia, 1993, Lippincott Williams & Wilkins.)
As with the RA muscle, the relationship between standing alignment and length of the oblique abdominal muscles should be considered. An individual who habitually stands in a swayback alignment places the fibers of the external obliques in a lengthened position while the fibers of the internal obliques are slightly shortened.29 Habitual assumption of a swayback standing posture shifts the center of mass posterior so that the abdominal muscles, RA and internal obliques muscles in particular, play a greater role in holding the upright position, acting as antigravity muscles.
The length of the internal and external oblique muscles is reflected, in part by the subcostal angle. An ideal subcostal angle of approximately 90 degrees is considered to be a reflection of balance between the internal and external obliques.1 A subcostal angle greater than 90 degrees may indicate shortness of the internal oblique muscles or excessive length of the external oblique muscles, with the latter often the case in individuals who have poor abdominal tone. The individual who routinely has performed abdominal crunches as the main abdominal exercise would be expected to develop shortness or stiffness in the internal oblique (as well as the RA muscle). The result is this individual’s subcostal angle may be greater than 90 degrees. Contraction of the internal oblique muscles that run obliquely in the superomedial direction from the iliac crest to the linea alba and the lower ribs, pulls the thorax toward the pelvis and widens the subcostal angle. Conversely, a narrow subcostal angle could indicate shortness/stiffness of the external oblique muscles. The anterior fibers of the external oblique muscles run inferomedially from the fifth to twelfth ribs toward the linea alba, inguinal ligament, and the anterior pelvic rim. The angle of pull of the external oblique muscles decreases the subcostal angle. The upper fibers of the transversus abdominis muscle may have some ability to narrow the subcostal angle.29
Another form of asymmetry commonly found in the abdominal muscles is an alteration in the resting length of the internal and external obliques on one side compared to the other. An individual who has repeatedly rotated the trunk to the right to perform work duties may develop a postural impairment of rib cage rotation to the right and shortness of the left external oblique muscle compared to the right internal oblique muscle. Additionally, the right internal oblique would be expected to be shorter than the left internal oblique. The subcostal margin would be asymmetrical so that the left subcostal margin would be closer to midline than the right (Figure 4-24). The habit of sitting on one’s foot or leaning over onto the armrest produces lateral trunk flexion, which can also lead to development of length asymmetries in abdominal muscles. The alteration of length depends on the frequency and constancy of assuming such positions, as well as what other activities or positions the individual performs to reverse the lateral trunk flexion/rotation. An individual with poor abdominal muscle tone is probably more likely to develop this postural scoliosis because they lack the normal muscle stiffness that would help to “derotate” the trunk.
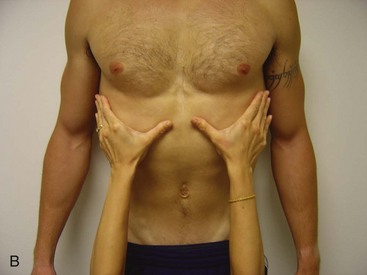
Although the subcostal angle is a useful guide for determining the length of the oblique abdominal muscles, it should not be considered an absolute indicator; variations will occur between individuals because of their body structure, pulmonary dysfunction, or other conditions such as ankylosing spondylitis. The length of the oblique musculature can be assessed further by observing the movement of the rib cage and subcostal angle with inhalation and with full-arm elevation (Figure 4-25). Average rib cage expansion is 5 to 10 cm106 going from maximum exhalation to maximum inhalation; with age, rib cage motion does decrease,106,107 so values on the lower end of normal would be expected in older individuals. Less than 3 cm change in rib cage motion would be considered impaired expansion. Expansion of the rib cage and widening of the subcostal angle during inhalation will be limited by shortness in the abdominal muscles. The limitation in motion will be greater with arms elevated overhead. Failure of the rib cage to expand is a potential sign of shortness in both internal and external oblique muscles. If the subcostal angle does not widen when the subject inhales with the arms overhead, the external oblique muscle is implicated. Limited range of motion and lateral trunk flexion toward the contralateral side may be another indicator of short abdominal muscles. Conclusions about abdominal muscle length should be based on evaluation of the patient’s age, body habitus, activity level, and movement tests.
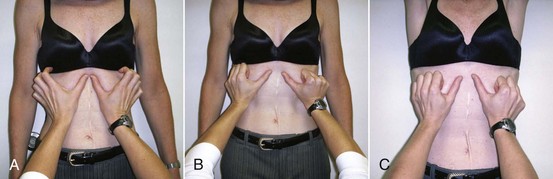
Figure 4-25 Length of the oblique musculature can be assessed further by observing the movement of the rib cage and subcostal angle with inhalation and full-arm elevation. A, At rest with narrow subcostal angle. B, With inhalation, the angle widens. C, Inhalation with arms over the head. The angle does not widen as much as with arms at side.
Development of abdominal muscle shortness can occur by overexercising the muscles or continually adopting postures that allow the abdominal muscle to rest at a shortened length. The general public seems to be under the perception that the abdominal muscles cannot be exercised too much. However, excessive abdominal exercise can lead to muscle imbalances as described previously. The imbalance in the abdominal muscle contributes to movement impairments but may have other consequences. Shortness or stiffness of the oblique abdominal muscles can interfere with the ability of the inspiratory muscles to lift and flare the rib cage. Because the oblique muscles assist with exhalation during strenuous breathing, aerobic activity may perpetuate the muscle shortness. Importantly, an increase in the compression forces on the thoracic spine and rib cage may result from oblique abdominal muscle shortness. Some individuals may be creating greater stresses on their thoracic spine by working on abdominal strengthening exercises.
Muscle Performance
Using the term muscle performance to describe the abdominal function encompasses both parameters of strength and recruitment. Defining abdominal muscle function based only on the results of standard manual muscle testing (MMT), such as the leg lowering test, would dismiss the importance of motor control.108 Stability of the spine and rib cage requires coordinated activation of the abdominal muscles. Modulation of abdominal muscle activity to meet specific functional demands is crucial for appropriate spinal stabilization. Deficits in abdominal muscle motor control have been found in subjects with low back pain109,110; however, it is not known if similar motor control impairments exist in the thoracic spine. Furthermore, it is not clear if the alteration in muscle activation patterns is the cause or the effect of the low back pain. Although little attention has been directed at the relationship between thoracic pain syndromes and abdominal muscle performance, some insights may be gleaned from the work examining their affect on the lumbar spine, but caution is advised in attempting to generalize results across spinal segments.
One of the most important functions of the abdominal muscles is to provide isometric support to resist compensatory spinal motions during extremity motion.1 Porterfield and DeRosa state that ideally the abdominals function as antirotators and antilateral flexors.104 The anatomical arrangement of the internal and external oblique RA and the transverse abdominus muscles is such that when working optimally, they provide stability of the spine and rib cage. During extremity movements, the trunk should be a stable foundation; the abdominal muscles play a major role by countering the rotational moments placed on the thorax and spine during limb movement.100,104 Although the oblique muscles are thought of as rotators and lateral flexors of the trunk, their role in providing stability is achieved by resisting those rotational forces. The abdominal muscles continue to be a major source of trunk stability even when the trunk is in flexion, extension, or lateral flexion.112
During lower extremity movements, the external oblique muscles help prevent anterior pelvic tilt and work with the internal oblique muscles to prevent rotation of the pelvis. When the pelvis is stabilized, the external and internal oblique muscles should control rotation of the rib cage and thoracic spine. A common movement impairment seen in the thoracic region is rotation of the thorax during extremity motion. This impairment can be found even in individuals who do regular abdominal exercise, usually because their exercise strategies have focused on strength and not control. Treatment of the rotational impairment is accomplished by having the patient practice extremity movements while focusing on maintaining rib cage and spine stability. Often, this exercise must be started at a very low level and then progressed as the patient demonstrates the ability to control the motion. For example, a patient with pronounced weakness of the abdominal muscles and excessive flexibility in the thorax may need to start exercising by lying supine, contracting abdominals, and easily moving one arm overhead toward flexion. The patient would stop the motion of the arm when rib cage or spinal motion was detected; initially the patient may move through only a limited ROM but with continued practiced should achieve full flexion. Movements of the arm into horizontal abduction would be considered a progression because the abducted position will tend to rotate the thorax. Higher level exercises may use resistance. Exercise movements that target the latissimus dorsi or serratus anterior will require activity of the external oblique to oppose the forces on the rib cage.1 Lower extremity motions are useful to not only assess abdominal muscle performance and stability of the thorax but also as a method of challenging the muscles.
The TA muscle is often referred to as a muscular corset. The activity of the TA muscle has traditionally been considered to be a spinal stabilizer, in part by increasing intraabdominal pressure (IAP). The role of the TA in spinal stabilization has been shown to be minimal.110a Increasing IAP does increase spinal stiffness,111,113 which can help prevent tissue strain.111 Contraction of the TA muscle does increase IAP via its insertion into the lumbar fascia111; however, its contributions to trunk mechanics may be more complex than that of a corset. The TA muscle has been shown to be active with trunk rotation114 and interestingly, differential activation within portions of the TA.115 Urquhart and Hodges115 used a paradigm of pelvic rotation with the thorax fixed and found that the lower and middle regions of the TA muscle were active during contralateral rotation of the pelvis and the upper fibers during ipsilateral rotation. The authors suggested several possible explanations for the apparent contradictory activity of the TA muscle: (1) stabilization of the linea alba and aponeuroses against the pull of the internal oblique or internal obliques, (2) control of the motion of the rib cage and lumbar spine via insertion onto the lumbodorsal fascia, or (3) the contraction served to increase the intraabdominal pressure.115 These new insights into the function of this muscle correspond to anatomical studies documenting variations in fiber direction within the TA: The upper fibers are oriented horizontally and the middle and lower fibers are angled somewhat inferomedially.116
Another example of regional distinction in the TA muscle was noted during arm movements: Recruitment of the upper portion of the TA muscle was delayed in response to arm movement compared to middle and lower regions.117 Initial investigations into the activity of the TA with extremity movement did not demonstrate differential activity of the muscle dependent on the direction of the arm.118,119 According to Hodges, the activity of the TA would not depend on the direction of force if it contributes to spinal control through modulation of intraabdominal pressure.113
The RA muscle is aligned in such a manner that it does not provide any significant control over rotation.120,121 Therefore exercise programs that emphasize the RA muscle may lead to a compromise in the control of rotation.1 Furthermore, RA muscle exercises are often issued with the intent of targeting either the upper or lower portion of the muscle.122,123 However, in EMG studies, no difference was found between activation of the upper and lower portions of the muscle during common exercise maneuvers.124 Previous studies that may have demonstrated a difference in activity were flawed because the EMG signals were not normalized.
Treatment of thoracic pain syndromes often involves working on trunk muscle control so that both the abdominals and the posterior trunk muscles work synergistically. Instructing the patient to focus on maintaining stability of the spine, rib cage, and pelvis during extremity movements is a useful strategy aimed at improving motor control. This approach is also ideal when considering the length-tension relationship of the abdominals because performing exercises with the trunk in a neutral alignment works the abdominals at their ideal length. Stabilizing the thorax during movements of the extremities is usually easiest in supine and becomes more difficult when the patient moves into sitting, quadruped, or standing.117 When lying supine, the compliance of the rib cage is decreased107; therefore controlling unwanted rib cage motion should be easier for the patient. Exercises can be adapted to meet the specific needs of the patient. It is worth emphasizing that patients may have the ability to generate sufficient force with their abdominals but still lack the precise control needed. The greater the demands the patient places on his or her body, the greater precision needed from the trunk muscles. For example, a competitive tennis player needs to demonstrate the ability to move the arm against resistance while maintaining spine and rib cage stability in standing. In contrast, a sedentary 65-year-old patient may only be able to move one arm up overhead without allowing the rib cage to move while in the supine position.
With nonstructural alignment impairments, the patient should actively correct the alignment and maintain the correction. This can be done intermittently throughout the day and as the patient gains endurance, the alignment correction can be held for longer periods of time. Holding the corrected position will result in the muscles working at the appropriate length. Eventually, the postural correction can be maintained with mostly passive muscle tension. As discussed earlier, thoracic pain syndromes are frequently associated with alterations in tissue properties and the development of excessive flexibility in specific directions. Although some may consider this to be mostly an arthrokinematic dysfunction, reversal of the dysfunction will best be achieved by teaching the patient appropriate trunk muscle recruitment, so the patient can limit or stop the undesired motion.
There are those patients, usually very sedentary, who are unable to readily recruit their abdominal muscles. Having these patients practice abdominal contractions in sitting or standing so that they pull in against the abdominal contents will improve their success. They may spend a week between visits practicing the isolation of abdominal contraction versus inhalation or Valsalva maneuver.
Extensive discussion of the mechanics of breathing is beyond this text; however, a review of the basic kinesiology is warranted. Contraction of the diaphragm will widen the subcostal angle and increase the chest volume as it descends toward the abdomen and compresses the viscera. The increase in chest volume is proportional to the rib cage displacement.125 The resistance of the abdominal muscles, viscera, and the intercostals improves the efficiency of the diaphragm. Optimal performance of the diaphragm relies on a balance between the muscles of ventilation; if the resistance from the intercostals and the oblique abdominal muscles is excessive because of muscle shortness or stiffness, then the diaphragm will be required to work harder during inhalation. Conversely, lack of resistance from abdominal musculature and the intercostals also creates an imbalance that can manifest in two common patterns known as paradoxical breathing. In one pattern, when the diaphragm contracts and there is insufficient resistance from the abdominal muscles, the abdomen bulges outward, limiting the need for rib cage expansion. Such is the case with individuals with abdominal muscle paralysis; contraction of their diaphragm will cause abdominal distention rather than chest expansion. The second type of paradoxical breathing occurs when the abdomen is drawn inward during inhalation, which commonly occurs when there is weakness of the diaphragm and is seen in individuals who are ventilator-dependent.
Clinically, what can be observed in a neurologically intact person is inhalation as a substitute for abdominal muscle contraction. A common error when attempting to contract abdominal muscles by “pulling the belly in” is to inhale by contracting the diaphragm or the accessory muscles of inhalation rather than the abdominals, which are muscles of exhalation. Appropriate contraction of the abdominal muscles should flatten the abdomen, change the firmness of the external obliques, and often narrow the infrasternal angle. Treatment should include education and practice to correct the coordination impairment by having the individual gently blow outward as he or she contracts the abdominal muscles.
The traditional view of intercostal muscle function is that the external intercostal muscles elevate the ribs and therefore are considered inspiratory muscles; the internal intercostals, with fibers angled downward and dorsally, pull the ribs closer together assisting with expiration. Other authors believe that rather than opposing functions, the intercostal muscles work together to stabilize the rib cage against the pull of the diaphragm and the fluctuating pressure in the thorax.96 This belief is supported by EMG activity of both the internal and external intercostals during both phases of ventilation.126,127 The anatomical location of the intercostals may explain what appears to be a dichotomy in their function. The expiratory mechanical advantage of the internal intercostals decreases moving from bottom to top of rib cage and the most anterior portion, often as parasternal intercostals, become inspiratory muscles.128 Although the intercostal muscles are considered primarily ventilatory muscles, EMG studies have demonstrated activity of the intercostals during trunk rotation.129 Using indwelling electrodes placed in the lateral intercostals, Whitelaw129 demonstrated that the internal intercostals were active with ipsilateral rotation and the external intercostals were active during contralateral rotation. The activity in muscles was much greater than the activity during breathing. Although the intercostals may assist with trunk rotation, their operating range and their force-generating capacity would be less than that of the abdominals.
Movement System Syndromes of the Thoracic Spine
Movement system syndromes of the thoracic spine are named for the alignment or movement direction that deviates the most from optimal alignment or movement patterns, as follows:
During an examination, correction of the impaired alignment or movement pattern usually decreases or eliminates the symptoms; however, in many cases of thoracic flexion syndrome, correction of the flexed posture may result in a slight temporary increase in pain. Clinical observation suggests that often even a severe kyphotic posture does not reproduce pain, although the patient may notice some discomfort when modifying the position. Yet, correction of the kyphosis when possible is usually indicated, and even if the patient is unable to fully correct the kyphosis, a partial correction is desirable. In the case of thoracic rotation, modification of the rotation can decrease the symptoms. Correction of excessive thoracic extension can immediately reduce or eliminate the symptoms. In all of the syndromes except the flexion syndromes, alignments or movement impairments that are accompanied by symptoms are weighted more heavily than impairments that do not reproduce pain.
The examination consists of alignment and movement tests of the spine, rib cage, and extremities in a variety of positions. The patient’s preferred strategy for assuming an alignment or performing a movement test is termed the primary test. Those primary tests that produce or increase the patient’s symptoms are followed by a secondary test in which the examiner modifies the movement or alignment and symptom behavior is reported. The location of the patient’s pain should be correlated to the region of impaired motion. For example, in a patient with a flat upper thoracic spine and a kyphotic lower thoracic spine and pain in the upper thoracic region, the patient who complains of increased pain when sitting erect is most likely to have a thoracic extension syndrome. Conversely, a patient with the same postural impairments but with pain in the lower thoracic region will most likely have a thoracic flexion syndrome. Although the results of some tests may be more meaningful when determining the diagnosis, the examination is considered combinatorial (rather than algorithmic) so that all of the results of all key tests are used to verify the movement system diagnosis.
Both scapular muscle strain and cervical dysfunction can create pain in the upper thoracic area. For example, pain along the vertebral border of the scapula is characteristic of a cervical spine syndrome130 (see Chapter 3). Strain of the scapular adductors, consistent with either scapular abduction syndrome or scapular downward rotation syndrome,1 may mimic a thoracic syndrome because of the overlapping regions of pain. Distinguishing the primary source of pain in patients with midthoracic region pain can be difficult because arm motions stress both the thoracic spine and scapular region. However, if the midthoracic pain is reproduced during lower extremity motions, for example, hip abduction-lateral rotation in supine, then the thoracic spine is implicated as the source of pain. It is possible that more than one area is implicated as a source of a patient’s symptoms. A careful systematic examination of the patient will assist in determining the cause of the pain.
Therapists should be aware that the etiology of pain in the thoracic region has a higher likelihood of arising from nonmusculoskeletal sources than other spinal regions.* The therapist must be alert for atypical symptom behavior and other systemic signs or symptoms that the patient may not have associated with the thoracic pain.135,138,139 Suspicion of visceral or systemic pathology warrants a referral to the patient’s physician. Examples of musculoskeletal symptoms suggesting conditions that also warrant a referral to the physician are compression fractures,140,141 possible disc herniation, or lower extremity neurological complaints that may implicate cord involvement.87,136,142 Lower extremity neurological complaints may implicate spinal cord involvement, therefore new or unexplained neurological findings should be assessed by a physician. Additional information on screening for pathology is available through other sources.135 Conversely, there are several cases in the literature of musculoskeletal problems disguising themselves as visceral pathology.80,90,134 Therapists working in conjunction with physicians can be instrumental in identifying musculoskeletal causes of visceral, cardiac, or urogenital symptoms.
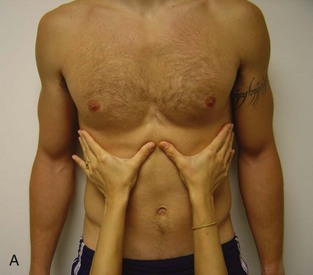
Compressive forces on the thoracic spine have the potential to contribute to symptoms across all of the different thoracic movement system syndromes. For individuals who report a height loss of 3 to 5 cm or more,143-145 there is probably a greater likelihood that compression is a contributing factor to their symptoms. Shortness or hypertrophy of the thoracic paraspinals and overdevelopment of the abdominals will add to spinal compression. Compression forces on the spine are greater in unsupported sitting and standing when compared to a recumbent position. Therefore, if compression is a factor, the patient usually has fewer symptoms when lying down. The effect of compression can be assessed by manually lifting the patient’s rib cage with the patient in the upright position. The therapist’s open hands are placed on each side of the rib cage and while pressing inward, an upward force is applied to the rib cage to help “unload” the spine. If symptoms are reduced with this maneuver, it is likely that compression is contributing to the patient’s symptoms. Location of the hands along the rib cage will be dictated by the symptoms, for example, upper thoracic symptoms would require the hands to be placed closer to the axilla. If the patient has radicular symptoms, hand placement directly over the symptomatic region should be avoided. In the patient with osteopenia, manual rib cage elevation should be done very gently. If osteoporosis is present, manual rib cage elevation should be avoided because of the risk of rib fracture.
In all likelihood, pain syndromes develop because of impairments in motor control, muscle generation of force, and changes in tissue stiffness. In other words, the cause of thoracic pain, similar to low back pain, is multifactorial and in certain patients, one component of dysfunction may be a greater contributing factor than another. Rehabilitation of patients will be most successful if treatment is aimed at restoring normal alignment, movement, and muscle recruitment patterns.
Thoracic Rotation-Flexion Syndrome
Thoracic rotation-flexion syndrome is characterized by pain associated with the movement and postures of thoracic flexion and rotation. Asymmetries of the rib cage with a thoracic kyphosis and/or posterior trunk sway are common alignment impairments observed in this syndrome. Common muscle impairments include asymmetry in the length and recruitment of the trunk muscles, including long thoracic paraspinal muscles and scapulothoracic muscles (middle trapezius, rhomboids); short or stiff shoulder girdle muscles (pectoralis minor and major, latissimus dorsi), and the RA muscle; and asymmetrical length and strength of the oblique abdominal muscles. Motor recruitment dominance of the RA muscle is common in this syndrome. Compression of the spine and asymmetrical approximation of the ribs should be considered contributing factors to pain. There is a paradoxical relationship to the amount of thoracic flexion and the presence of pain; thoracic flexion is easily performed because of the shape of the thoracic facets and the anterior load of the rib cage and upper extremities. Plus, pure thoracic flexion without a rotation component to the motion is commonly not painful. However, excessive posturing or movement into flexion of the thoracic spine is a contributing factor to biomechanical stress that can cause musculoskeletal pain in this region. Creep of the connective tissues of the thoracic spine elongating the posterior elements (posterior longitudinal ligament) while compressing the anterior elements (vertebral bodies and discs) of the spine will occur with prolonged flexion. Thus an individual who spends increased time with the thoracic spine in a flexed position will demonstrate pain when attempting to rapidly improve alignment by straightening the thoracic curve. This individual may be unable to fully correct the posture because the prolonged mechanical stresses have created a structural change at the vertebral bodies, discs, and posterior longitudinal ligament. In addition, rotation occurs early and readily once the thoracic spine is flexed because of the opening of the facets and posterior aspect of intervertebral bodies. Thus flexion with rotation of the thoracic spine would increase not only the anterior forces on the spine but also create asymmetrical compressive forces along the ribs and their attachments into the sternum.
Symptoms and History
Individuals with the thoracic rotation-flexion syndrome complain of pain in the thoracic region, which may radiate into the lateral and anterior rib cage or abdomen. They will note an increase in pain with lying down, reaching, or trunk rotation. Ventilation is affected so that pain occurs with forceful exhalation.134,146-148 Common recreational activities reported by individuals with a rotation-flexion syndrome include any activity that repeatedly places their trunk into flexion and rotation such as crew, squash, golf, diving, and running (asymmetrical arm swing and trunk rotation). Habitual trunk flexion with rotation during functional activities include arranging the desk so that flexion and/or rotation is required to reach the phone, computer, and files or greet incoming customers/clients. Other habits are sitting shifted to one side (leaning toward the mouse pad side of the desk), sitting on one foot, or leaning on an armrest while working, reading, driving, or watching television. Pain with sitting is reduced or abolished when the individual uses a backrest to keep the spine more erect and to avoid asymmetrical postures such as leg crossing, unilateral armrest use, or sitting on one foot. Individuals with a rotation-flexion syndrome may have a history of loss of motion at the glenohumeral joint because of a frozen shoulder or a rotator cuff injury or a history of chest surgery in which the rib cage or sternum has been surgically manipulated.
Key Tests and Signs
Standing Alignment
Thoracic kyphosis with an asymmetry of the rib cage will be the most common alignment impairment found in this syndrome. Sway of the trunk posterior to the axis of the hip combined with thoracic flexion and asymmetry of the rib cage is also commonly observed in individuals with a thoracic rotation-flexion syndrome. The presence of rib cage asymmetry can be noted from either an anterior or posterior view. The shape of the rib cage and its effect on the position of the scapulae should be noted. A posterior rib cage asymmetry may cause the alignment of the scapulae to appear asymmetrical, because the structural base (rib cage) upon which the scapulae are resting is asymmetrical. An anterior rib cage asymmetry may cause the size or shape of the breast to appear asymmetrical.
Scoliosis may be present, although it is more common for scoliosis to present with a loss of the thoracic curve (as in the thoracic rotation-extension diagnosis). Scoliosis with a thoracic flexion alignment impairment occurs in older individuals who have degenerative changes or who have performed trunk-curl exercises. Passive elevation of the rib cage when pain is present unloads the weight of the upper trunk on the thoracic region and relieves symptoms for individuals with pain from compression.
If a structural kyphosis is suspected, observation of the spinal alignment in supine, prone, and a quadruped position should be done. A structural kyphosis is implicated if there is no reduction in the kyphosis in these alternate positions. The quadruped position is an especially useful position for assessing the amount of extension available in the thoracic spine because it allows unloading of the thoracic spine, and this position often relieves the patient’s pain. In this position, it may be helpful to cue the patient to relax the abdominal musculature and lower the apex of the spinal curve. If a structural kyphosis is present, accommodation of the fixed kyphosis is necessary in the treatment planning.
Movement Impairment Analysis
Standing tests
Standing trunk flexion demonstrates excessive flexion and rotation in the thoracic spine; in addition, the presence of a rib hump is more noticeable in a thoracic flexed position compared to standing. The motions of trunk rotation and lateral flexion demonstrate an asymmetry in motion and/or pain with these movements. Either motion may cause a radicular symptom into the chest or abdomen because of neural compromise at either the vertebral foramen or along the length of the ribs. Unilateral shoulder flexion, which is a test for the presence of spine motion during extremity motion, results in variation side to side. Thus, with arm motion there is a resulting motion at the spine and rib cage with or without reproduction of the symptoms. Bilateral shoulder flexion demonstrates an increase in thoracic flexion or sway with unilateral trunk rotation. In the presence of a kyphosis-lordosis alignment impairment (Figure 4-26), rotation may also be present in addition to the increased thoracic and lumbar curves. With both unilateral and bilateral shoulder flexion, pain and motion will be improved if the trunk is supported either by a wall or lying recumbent. The spine will be straighter and aided in the prevention of rotation with the extremity movement. Caution should be used when considering cueing for recruitment of the abdominal musculature for trunk control during this follow-up test, since the increased flexion and spine compression may increase the individual’s pain during arm motion. If the individual presents in an early stage of rehabilitation, protection of the thoracic spine and neural tissue can be achieved by performing supported shoulder flexion while facing the wall. Thus the weight of the upper body can be unloaded by the wall, the thoracic spine can be easily extended without overcorrection. The exercises can be progressed once the patient has advanced to a rehabilitation stage to strengthen the thoracic paraspinal muscles in the same position by active shoulder flexion or flexion without support from the wall.
In the presence of a thoracic rotation-flexion impairment, asymmetrical motion of the rib cage will be noted during ventilation (most commonly during bucket-handle assessment of the rib cage). In addition, because of the positional impairment of sternal depression and dominance of the RA muscle, decreased pump-handle motion compared to the relative amount of bucket-handle motion will also be present.
Supine tests
Pain will commonly be reported when assuming the supine position. Accommodation of the thoracic flexion should be done by providing support for both the cervical and thoracic spine into flexion. Padding may be needed unilaterally to accommodate a structural rotation of the rib cage or spine. A follow-up test of removing some of the support after 5 to 10 minutes in the position should be done to determine if the patient can tolerate the straighter position. Examination of the subcostal margin in the supine position will reveal rib cage asymmetries and give insight in muscle length issues related to the internal oblique, external oblique, and the RA muscle. An increased subcostal margin in both standing and supine may indicate a decreased length of the internal oblique muscles and an increase in the length of the external oblique musculature. An asymmetry of the subcostal margin is commonly present in this category. Approximation of the sternum toward the pubis may be present if there is a marked shortness of the RA muscle. During testing of the abdominal musculature, there will be poor control of the oblique abdominal muscles with rotation of the rib cage and/or thoracic spine during upper or lower extremity movement. Use of inhalation to stabilize the rib cage by contraction of the diaphragm and increasing IAP instead of appropriately recruiting the abdominal musculature is commonly observed. In the presence of sway or sternal depression, increased recruitment of the RA muscle over the lateral abdominal musculature can be seen. In younger individuals, the RA muscle will test strong during trunk curling; however, rotation during the trunk curl demonstrates a unilateral weakness of the oblique abdominal musculature. Unilateral shoulder flexion in the supine position will reveal a rib cage motion or thoracic spine motion that will be most pronounced when moving the arm in a diagonal pattern. Pain with arm motion will commonly decrease with cueing to control the rotational movement by increasing abdominal muscle contraction during the motion. If the patient is in Stage 1 for rehabilitation, the recruitment of the abdominal musculature may increase pain from compressive force on the spine and rib cage. Thus caution should be used during abdominal muscle testing by monitoring closely for an increase or worsening of the presenting symptoms. Hip abduction with lateral rotation in the flexed position is commonly assessed if the individual complains of symptoms during functional activities that require leg motions such as driving and walking. Rotation of the thoracic spine and rib cage and pain noted during the leg motion will be reduced by cueing to recruit the trunk musculature during the activity. Both the thoracic spine extensors (control flexion) and the abdominal musculature (control rotation) may need to be recruited for adequate trunk control during upper and lower extremity motions.
Prone tests
Prone-lying may reduce symptoms in younger more flexible individuals with a thoracic rotation-flexion syndrome. However, older individuals may need increased support in prone to accommodate the amount of thoracic flexion that is present. In the case of a severe kyphosis, prone should not be attempted. Prone lying may also require some lateral trunk support to minimize rotation while in this position. As in the supine position, removal of some of the trunk support can be done after 5 to 10 minutes to see if the individual can tolerate a more extended position of the spine.
Trunk extension in the prone position will test weak in older individuals with a thoracic flexion alignment impairment149-152; however, use of this position for testing and exercise should be done with caution because the erector spinae musculature is not isolated to the thoracic region. Recruitment of the erector spinae in the prone position increases both lumbar and thoracic region extension. Because of the high prevalence of osteoporosis and osteoarthritis in older individuals and the mechanical advantage of the lumbar paraspinals to compress the lumbar region, low back pain may occur during prone trunk extension. If not properly positioned into lumbar and thoracic flexion, an imbalance between the strength and control of the upper thoracic paraspinals (weak and decreased recruitment) compared to the lumbar paraspinals (strong and increased recruitment) can worsen the compression forces at the lower rib cage and thoracolumbar junction.
Single arm raises in the prone position in individuals with a thoracic rotation with extension syndrome can reveal thoracic rotation. Cueing to increase paraspinal muscle recruitment aids in the flexion and rotation control that commonly decreases symptoms. In an individual who is unable to tolerate unilateral arm motions, bilateral symmetrical scapular adduction with shoulder abduction (hands on head, elbows flexed, and elbows extended) can be performed in the various degrees of difficulty.
Quadruped tests
When positioned in the quadruped position, there will be a noticeable amount of thoracic flexion with rotation of the rib cage (hump). Quadruped is commonly a pain-relieving position for individuals with thoracic rotation with flexion because the thoracic spine is suspended between the upper and lower extremities, thus providing a position of unloading. Because of upper extremity muscle weakness and rib cage asymmetries, scapular winging or tilting is commonly present. Rocking back in the quadruped position will reveal an increase in thoracic flexion and rotation. Cueing is needed to relax the abdominal musculature during the rocking motion to prevent flexion of the thoracic spine. Shoulder flexion in quadruped can cause rotation of the thoracic spine and rib cage. Instruction to recruit the latissimus dorsi and thoracic back extensors by an isometric contraction (isometric shoulder extension of the weight-bearing arm toward the ipsilateral knee) reduces the rotation. Inability to perform this correctly in the quadruped position should prompt the therapist to downgrade the activity by performing unilateral shoulder flexion in the prone position. In very active populations, crawling can be assessed to create a more unstable activity that requires trunk rotation. Crawling in individuals with thoracic flexion with rotation will reveal an asymmetry in the trunk rotation.
Functional Activities
Observation of the thoracic spine and rib cage should be done during aggravating functional activities. Specific attention should be paid to the amount of abdominal muscle compared to thoracic paraspinal muscle recruitment during the task. If simply cueing to reduce the motion of flexion with rotation does not decrease the symptoms, timing the movement so that the individual is instructed to first relax their abdominals and then perform the task may reduce the tendency to flex the thoracic spine enough to allow the individual to perform with increased thoracic extension reduce rotation and less pain.
Special Consideration of Treatment of Structural Scoliosis
Caution should be used when prescribing abdominal muscle exercises for individuals with a structural scoliosis because of the compressive effects of the abdominal musculature on the thoracic spine and rib cage. Common impairments that can be observed in older individuals with a structural scoliosis include spine compression with an increase in spine and rib cage rotation that occurs because of excessive abdominal muscle contraction. To address spine compression in an older individual with a structural scoliosis, the therapist should prescribe unloading activities and allow relaxation of the abdominal and trunk musculature. Quadruped rocking, back to the wall with supported shoulder flexion, and inhalation to elevate the ribs and elongate the abdominal musculature should be prescribed.
If pain occurs during asymmetrical sitting positions, the patient should be instructed in correcting the alignment. Avoidance of leaning on armrests, equal weight bearing through the pelvis and femurs, and back support should reduce the pain caused by asymmetrical sitting. In contrast to this, if an individual has scoliosis, pain may occur if they attempt to actively sit in a more symmetrical position. If pain occurs with sitting, instruct the individual to sit without attempting to correct the rotation that is structurally present in the spine. Allowing the individual to sit with the thoracic spine in rotation aligns the boney structures and relieves tissue stresses from forcing a “straight position,” thus decreasing their symptoms with sitting. Pads can be used to distribute the pressure on the back of the chair.
Case Presentation
Thoracic Rotation-Flexion Syndrome
A 23-year-old white female graduate student presents with a 1-year history of burning abdominal pain, located just below her umbilicus. The pain is present with sleeping in sidelying, sitting, driving the car, or using the elliptical machine at the gym. The patient is unaware of a position that relieves her symptoms. She denies any gastrointestinal symptoms (nausea, diarrhea, and so on) occurring at the same time of the pain. The severity of abdominal pain caused her to go to the emergency department twice in the past year. She has had upper and lower gastrointestinal examinations to rule out pathology of this system. Radiological studies of her pelvis and spine are negative. She denies a relationship of the symptoms to her menstrual cycle. Her past recreational history includes 12 years of dance with participation on the dance team during her undergraduate studies. Her initial Oswestry disability score was 46%.
The patient is 5 foot 7 inches tall and weighs 130 pounds. She has a long slender trunk and long arms. When standing, the patient demonstrates a lateral trunk shift to the right with T10, T11, and T12 spinous processes rotated right (indicating left rotation of those segments); a posterior sway of the thoracic spine, with the apex of her thoracic kyphosis at the lower thoracic segments; anterior pelvic tilt; and knee hyperextension. No symptoms reported in standing.
The patient demonstrated thoracic motion that was greater than hip motion with forward bending and reproduced her abdominal pain. The secondary test of corrected forward bending abolished her symptoms but required upper extremity support during forward bending to increase her ability to flex her hips and decrease the amount of thoracic flexion. On return from forward bending, the patient reported central lower thoracic pain with no abdominal symptoms. Corrected return from forward bending did not reproduce her pain. (During this point in the examination, the patient noted that she commonly would use trunk extension to attempt to relieve her abdominal pain.)
The patient demonstrated lateral abdominal pain (2/10) with sidebending in both directions. Sidebending left demonstrated greater ROM compared to right sidebending. The secondary test of supported sidebending at the apex of her curve abolished her pain bilaterally.
During the single leg stance test on the right lower extremity, the patient demonstrated trunk shift right with rotation left, an increase in the posterior sway of the trunk and increased abdominal pain. Correction of these alignment faults abolished her pain. To correct the movement impairments, the patient supported her trunk by using bilateral upper extremity support on the wall, while being cued to keep her trunk still during motion of her leg.
The patient demonstrated less than 3 cm of rib cage expansion with primarily bucket-handle motion. No symptoms were produced during this test.
On assuming the sitting position the patient demonstrated a slumped posture with a trunk shift to the right. Trunk flexion in sitting increased her pain to 2/10, and trunk extension in sitting reduced her pain to 0/10.
From the corrected position, the patient demonstrated thoracic flexion with rotation during terminal knee extension in sitting; however, no symptoms were produced.
The patient demonstrated a right trunk shift and reproduced her abdominal pain when performing active hip flexion with either leg (2/10) while in the sitting position.
The patient reported no symptoms in supine. Shoulder flexion was through full ROM without detectable rib cage changes. During single knee to chest, her upper trunk rotated but not her pelvis nor were her symptoms reproduced.
In the sidelying position, the patient reported an increase in her symptoms to 4/10. The abdominal pain abolished with support of the rib cage by a thin pillow.
The patient noted central 2/10 thoracic pain with initial prone lying. Positioning of the chest and lumbar spine with pillows to decrease lumbar extension and thoracic flexion reduced the symptoms to 0/10. The patient demonstrated left rotation of the thoracic segments T10 to T12 in the prone position. Palpation of the thoracic erector spinae musculature was positive for sensitivity to touch and a hyperemic reaction T10 to T12. Posterior to anterior spring testing of the lower thoracic and upper lumbar segments revealed decreased motion at the (L) facets and spinous process of T10 to T12 compared to the adjacent lumbar segments (L1 to L2). No abdominal pain was produced with spring testing.
In the quadruped position, the patient reported 1/10 abdominal pain that abolished with correction of the assumed position of thoracic flexion with right trunk shift and left rotation. Arm lift in the quadruped position reproduced her abdominal pain, and the patient’s rotation and shift was increased. The patient was unable to correct the thoracic movement in this position.
The patient consistently sat in thoracic flexion with her legs crossed and tended to lean on the right armrest of the chair. In addition, when observing her driving position, the patient demonstrated the same alignment impairments by consistently shifting toward the center console of the car.
The patient’s movement system diagnosis was thoracic rotation-flexion syndrome. The tissue impairment was considered Stage 2 because she did not have continuous symptoms and the symptoms could be modified in most positions during the examination. Her prognosis was good to excellent because of the ability to modify her symptom during the examination, her age, and general good health. Negative moderators were her lack of awareness of specific positions that would improve her symptoms and the amount of time that she spends sitting during the day.
The patient was seen once a week for 4 weeks, and then decreased to once every other week for an additional 3 more visits. Treatment included instruction in correct performance of functional activities, including bending, sleeping, sitting, driving a car, and aerobic exercise. She was also instructed in a home exercise program to improve the recruitment of her thoracic paraspinal muscles and improve the control of her trunk musculature during the examination items that had produced thoracic flexion, sidebending, and rotation.
During the first visit the patient was instructed to sleep with a support under her rib cage to provide positioning out of trunk sidebending while in the sidelying position. In addition, the use of pillows between her knees aided in control of trunk rotation by placing the pelvis in a neutral position. The patient was also instructed not to cross her legs, to avoid leaning on the armrests of chairs, and to maintain a more erect trunk by keeping her back supported by the back of the chair and her buttocks as far back in the seat as possible.
Initially, to improve the recruitment of her thoracic paraspinal muscles and improve her alignment impairments, she was given bilateral shoulder flexion exercises in standing with her hands and forearms supported on a wall and unilateral shoulder flexion in prone with her upper extremity off the supporting surface. To improve her trunk control during leg motions, she was given supported single leg stance with an emphasis on keeping her trunk still during leg motions. In addition, quadruped rocking and in standing trunk flexion supporting herself with her hands on a counter was given to unload the thoracic spine and improve hip flexion while decreasing the overall amount of thoracic spine flexion.
On subsequent visits, standing alignment was reviewed with a mirror to provide visual feedback of her trunk sway. The home exercise program was progressed to shoulder flexion in quadruped (corrective exercises for both flexion and rotation trunk control problems), shoulder flexion with her back to the wall (to progress load for paraspinal strengthening), and prone trunk extension with positioning to avoid lower lumbar extension (to strengthen thoracic paraspinal muscles without causing a secondary lumbar extension impairment).
At 1 month, the patient reported absence of abdominal pain with sitting and sleeping; however, she would occasionally notice pain during aerobic exercise. At this point the patient was instructed to avoid trunk rotation and bending into the elliptical machine during her workout activities. In addition, during a discussion regarding an appropriate means of abdominal strengthening, the patient reported she had started performing sit-ups after 30 minutes on the elliptical machine. Lower leg and upper extremity motions while keeping her trunk still were performed to demonstrate the abdominal muscle recruitment during these tasks; the patient was given an explanation as to why trunk curling activities were most likely contributing to her pain syndrome. At this stage of her care, light weights were added to the shoulder flexion exercises to increase the demands on the paraspinal and trunk musculature.
At the time of her last visit, the patient reported no abdominal pain for the past month; she had been consistently performing her home program 3 times a week with daily implementation of the functional activity changes. She was able to perform 45 minutes on the elliptical trainer and indicated that she understood that she had to avoid trunk curling activities in the future. Spring testing in prone of the lower thoracic vertebral structures was negative. Her Oswestry disability score was 0%.
Thoracic Flexion Syndrome
Although the thoracic flexion syndrome is associated with movements and postures of flexion, the movement is not always painful; however, prevention of excessive thoracic flexion is key to preventing other pain syndromes. Excessive flexion predisposes an individual to increased thoracic spine compression, as well as neck and lumbar spine impairments. A thoracic kyphosis and/or posterior trunk sway are common alignment impairments observed in this syndrome. Common muscle impairments include long thoracic paraspinal and scapulothoracic muscles (middle trapezius and rhomboids); short or stiff anterior axioscapular and axiohumeral muscles (pectoralis minor and major and latissimus dorsi, especially in an individual with a kyphosis lordosis), and the RA muscle. Motor recruitment dominance of the RA muscle is common in this syndrome.
If active thoracic flexion and taking a deep breath is painful, compression fracture of the spine should be considered. There is a paradoxical relationship with the amount of thoracic flexion and the presence of pain. An individual may be predisposed to thoracic flexion because of the shape of the thoracic facets and the flexion moment created by the head, shoulders, and rib cage. Usually, thoracic flexion without a rotation component to the motion is not painful. However, excessive flexion of the thoracic spine is a contributing factor to biomechanical stress that can cause musculoskeletal pain in this region. Elongating the posterior elements (posterior longitudinal ligament and other connective tissues) while compressing the anterior elements (vertebral bodies and discs) of the spine is a consequence of the prolonged flexion. An individual who maintains prolonged thoracic flexion may have pain when attempting to decrease the curve and is usually unable to correct his or her alignment because of the structural changes that have developed.
Symptoms and History
In this syndrome, the pain in the thoracic region usually increases when reaching with both arms, lying in the supine position or when trying to straighten the thoracic spine after prolonged flexion. Ventilation will be affected so that pain occurs with forceful exhalation.134,146-148 Individuals with a flexion syndrome often participate in activities that cause flexion such as bending to garden, prolonged reading, or watching television. Habitual trunk flexion during functional activities is commonly observed in individuals with this syndrome. These individuals sit slouched (leaning toward the mouse pad) or with their hips not fully back into the seat. Pain with sitting is reduced or abolished when the individual is instructed to use the backrest of the chair to keep the spine straight or support the trunk by using the armrests on the chair. Younger individuals with a flexion syndrome report a history of excessive abdominal strengthening exercises. In addition, the current postural trend for students is to sit in thoracic and lumbar flexion.
Key Tests and Signs
Standing Alignment
Thoracic kyphosis with sternal depression is the most common alignment impairment. Sway of the trunk posterior to the axis of the hip combined with thoracic flexion is also common. The patient may have a wide subcostal margin (infrasternal angle). It is important to note the shape of the rib cage and its effect on the position of the scapulae. The scapulae will be more abducted and internally rotated and demonstrate less posterior tilt during shoulder flexion because of the shape of the rib cage. Passive elevation of the rib cage when pain is present will unload the weight of the upper trunk and relieve symptoms for individuals with a contributing factor of compression.
Movement Impairment Analysis
Standing tests
Standing trunk flexion demonstrates excessive flexion in the thoracic spine. The motions of trunk rotation and lateral flexion do not demonstrate an asymmetry in motion and/or pain with these movements. Unilateral and bilateral shoulder flexion, which is a test for presence of spine motion during extremity motion, demonstrates an increase in thoracic flexion or sway. In the presence of a kyphosis-lordosis alignment impairment, lumbar extension with thoracic flexion may be noted. With both unilateral and bilateral shoulder flexion, pain and motion are improved if the trunk is provided support either from a wall or lying recumbent, thus allowing the spine to be straighter. Caution should be used when considering cueing for recruitment of the abdominal musculature for trunk control during this follow-up test because increased flexion and spine compression may add to the individual’s pain during arm motion. If the individual is in an early stage of rehabilitation, protection of the thoracic spine can be achieved by performing supported bilateral shoulder flexion while facing the wall, thus unloading the weight of the upper body by the support of the wall. The thoracic flexion can be decreased by having the patient extend a few degrees and gradually progress the program once the patient has advanced to Stage 2. The program would consist of strengthening the thoracic paraspinal muscles by performing active shoulder flexion from the facing the wall position and then without the wall for support. In the presence of thoracic flexion during ventilation the pump-handle motion of the rib cage is decreased compared to the relative amount of bucket-handle motion.
Supine tests
To avoid pain in the supine position, a support for both the cervical and thoracic spine should be used. Removal of some of the support after 5 to 10 minutes usually indicates that the patient can tolerate the straighter position. The subcostal margin indicates a wide subcostal angle that is consistent with a decrease in the length of the internal oblique muscles and an increase in the length of the external oblique musculature. Approximation of the sternum toward the pubis may be present if there is a marked shortness of the RA muscle. There is poor control of the lateral abdominal musculature. The patient will inhale as an attempt to contract the abdominal muscles instead of appropriate recruitment of the abdominal muscles, which contribute to exhalation. In the presence of trunk sway or sternal depression, increased recruitment of the RA muscle over the lateral abdominal musculature can be observed. In younger individuals, the RA muscle tests strong during trunk curling; however, in the older adult the internal obliques with the RA may test weak during the trunk curl. The trunk curl is rarely used to assess the performance of the internal oblique muscles in the older individual. Therefore assessment of the relative performance of the abdominals versus the pectoral muscles is best assessed by using arm motions. Unilateral shoulder flexion in the supine position reveals rib cage motion or thoracic spine motion that will be most pronounced when moving the arm in a diagonal pattern. If the patient is in Stage 1 for rehabilitation, as following abdominal surgery or a trauma to the thorax, the recruitment of the abdominal musculature may increase the pain caused by compressive force on the spine and rib cage. Thus caution should be taken during abdominal muscle testing, monitoring closely for an increase or worsening of the presenting symptoms.
Prone tests
The prone position may reduce symptoms in younger more flexible individuals but may increase the symptoms in older less flexible individuals. In the case of a severe kyphosis, prone testing should not be attempted. If the patient is positioned in prone on pillows, removal of some of the trunk support can be done after 5 to 10 minutes to see if the individual can tolerate a more extended position of the spine.
Trunk extension in the prone position tests weak in older individuals with a thoracic flexion alignment impairment149-152; however, use of this position for testing and exercise should be done with caution since the erector spinae musculature is not isolated to the thoracic region. These individuals also have excessive cervical extension or an anterior translation of the cervical spine. Recruitment of the erector spinae muscle in the prone position increases both lumbar and thoracic region extension. Because of the high prevalence of osteoporosis, osteoarthritis, and spinal stenosis in older individuals and the mechanical advantage of the lumbar paraspinals to compress the lumbar region, low back pain may occur during this prone trunk extension. If not properly positioned into lumbar and thoracic flexion, an imbalance between the strength and motor control of the upper thoracic paraspinal muscles (weak and decreased recruitment) compared to the lumbar paraspinals (strong and increased recruitment) can worsen the compression forces at the lower rib cage and thoracolumbar junction.
Quadruped tests
When positioned in quadruped, there will be a noticeable amount of thoracic flexion. Quadruped is commonly a pain-relieving position for individuals with thoracic flexion because the thoracic spine is suspended between the upper and lower extremities, thus providing a position of unloading. Because of upper extremity muscle weakness, scapular winging or tilting commonly is present. Rocking back in the quadruped position reveals an increase in thoracic flexion. Cueing is needed to relax the abdominal musculature to prevent activation during motion, which would cause an increase in the flexion moment of the thoracic spine.
Sitting tests
A prolonged slumped or flexed position of the thoracic spine has been related to increased pain in the thoracic, cervical, and lumbar regions.16,78,153,154 As noted earlier, individuals with long legs may sit with their knees higher than their hips, causing lumbar and thoracic flexion. Reducing the angle so that the knees are not higher than the hip by using a higher chair or a cushion would make it easier to avoid lumbar and thoracic flexion. Correction of the sitting position of thoracic flexion should eliminate any symptoms associated with the alignment fault. The patient may also need to modify the position when working at a desk to avoid thoracic flexion. In addition, the individual’s vision should be checked to see if it is partially responsible for the slouching behavior. The habit of leaning forward may be the result of individuals not being able to see what is positioned in front of them. Interestingly, a slouched sitting posture has been reported to be associated with a decrease in shoulder ROM and strength.155 Therefore it is important to assess reaching by mimicking the typical activities an individual would perform while sitting at the desk. If pain occurs with reaching during sitting in a slouched position, the patient should be instructed to correct the alignment before reaching forward. Individuals with a marked fixed kyphosis usually sit in lumbar extension. Often, a support behind the lumbar spine or not positioning the buttocks against the back of the chair will decrease the symptoms in sitting.
Functional Activities
Observation of the thoracic spine and rib cage should be done during aggravating functional activities. Specific attention should be paid to the pattern of abdominal muscle activity compared to thoracic paraspinal muscle activity during the task. If simply cueing to reduce the motion of flexion does not decrease the symptoms, then the individual should be instructed to first relax the abdominal muscles before performing the task so that the amount of thoracic extension will increase and there will be less thoracic rotation.
Treatment
Treatment of osteoporosis includes load-bearing exercises to stimulate bone growth.156 Weakness of the back extensors is common in individuals with an osteoporotic kyphosis,10,12 thus exercise prescription should include strengthening exercises for the thoracic paraspinal musculature. Consideration should be given to the biomechanical stresses applied to the adjacent spinal regions when developing a strengthening program for the thoracic back extensors. Classically, a prone trunk extension exercise is prescribed to improve the strength of the paraspinal musculature in this population152 (Figure 4-27). Careful observation of the spine during the prone extension exercise is critical for determining the region of the spine that is moving. Commonly, lumbar extension is performed to a greater extent than thoracic extension, thus increasing the compressive forces at the lumbar spine resulting in pain152 (Figure 4-28). An alternative to the classic back extensor strengthening exercise is to exercise in a functional position. Sitting and standing with the spine aligned against a wall improves alignment and unloads the weight of the upper trunk. Motions of the upper extremity, shoulder flexion or abduction, can then be used to facilitate contraction of the paraspinal musculature157 (Figure 4-29). Spine compression and abdominal muscle shortness are contributing factors to the osteoporotic kyphosis, thus deep breathing while appropriately aligned on the wall should be done to increase abdominal muscle length1,29 and decompress the thoracic spine.93 Because of the compressive forces on the spine with contraction of the abdominal musculature, care should be taken with strengthening abdominal muscle in individuals with osteoporosis. Generally, patients with a swayback alignment of their trunk are cued to contract their abdominals only enough to hold a corrected alignment of their trunk, while patients with a kyphosis are advised to avoid abdominal muscle contraction in standing.
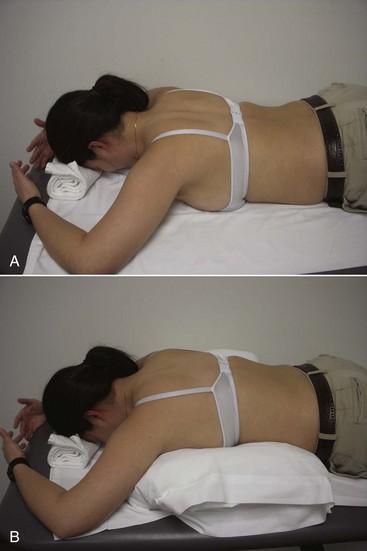
Figure 4-27 Starting position for prine arm lifts. A, Insufficient support under thorax allows thoracic extension. B, Increased support places thoracic spine in more ideal alignment.
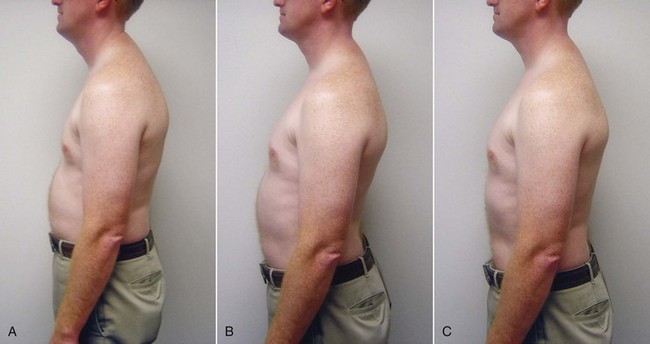
Figure 4-28 A, Kyphosis. B, Lumbar extension greater than thoracic extension. C, Improved thoracic alignment without lumbar extension.
Older individuals with a total C-curve of both the thoracic and lumbar spines, as well as a flat abdomen, have excessive abdominal muscle activity and markedly diminished back extensor activity. Even in the prone position, while performing shoulder flexion from the overhead position, the abdominal muscles contract rather than the back extensor muscles. Every effort needs to be made to change this recruitment pattern. Therefore these individuals need to avoid any type of abdominal muscle exercise and standing in the swayback position that makes the abdominal muscles the antigravity muscle group.
Thoracic Rotation-Extension Syndrome
Symptoms and History
The thoracic rotation-extension syndrome causes pain in the thoracic region that may radiate into the lateral and anterior rib cage or the abdomen. Symptoms may be pain, numbness, or burning. Trunk extension and/or rotation produce symptoms so that motions of unilateral shoulder flexion or reaching are painful because of these associated trunk motions. Similarly, a deep inhalation can cause pain because of associated thoracic rotation-extension.133,145,158 Positions and alignments that cause rotation or extension forces on the thoracic spine, such as sidelying or sitting up in an exaggerated position of trunk extension, can also cause pain.
Racquet sports, gymnastics, and ballet are activities that may have contributed to the development of the rotation-extension syndrome. Occupations that require working with the arms overhead can also contribute to the development of the syndrome. Patients with the diagnosis of thoracic rotation-extension may report a history of loss of motion at the glenohumeral joint. The loss of glenohumeral motion could cause the patient to substitute thoracic spine motion of extension and/or rotation as a substitute for loss of motion at the shoulder joint.
Key Tests and Signs
Often, patients with this syndrome have asymmetry in the thoracic spine and rib cage. The malalignment may be localized over a few segments or a structural scoliosis. From a posterior view, the spinous processes of the thoracic vertebrae may demonstrate lateral curvature and a rib hump may be present. If the rotation malalignment is in the upper thoracic region, the rib hump may not be obvious because of the scapulae; however, scapular asymmetry is likely. Loss of the normal thoracic sagittal curve is apparent in the posterior view in a few segments or the entire thoracic spine, and often the scapulae appear to wing because of the loss of the normal thoracic curve. Patients who habitually hold their spines in extension can often lessen their symptoms by relaxing thoracic paraspinal muscles and allowing the thoracic spine to flex. Minimal or no change in the thoracic curve will occur when the flat thoracic spine is structural.
From the anterior view, the chest or rib cage may be asymmetrical. The subcostal margin is often flared outward more on one side than the other. The subcostal angle may be wide (>110 degrees), and the rib cage appears to be flared. In such patients, the abdominal muscles will not be stiff or strong enough to counter the pull from the pectoral muscles so overhead movements of the upper extremities cause the rib cage elevation and thoracic spine extension.
Movement Impairment Analysis
The tests described here are considered to be key tests for thoracic rotation-extension syndrome. The tests are listed according to the order they are performed during the examination.
Standing tests
The tests are (1) trunk flexion, (2) trunk rotation, (3) trunk lateral flexion, (4) trunk extension, (5) shoulder flexion, and (6) deep inhalation.
Trunk flexion
The amount of flexion available in the thoracic spine is often less than the expected 30 to 40 degrees of flexion.2,3 During the return to the upright position, pain may be reported. Cueing the patient to avoid excessive extension and/or rotation during the return from forward bending decreases the symptoms.
Trunk rotation
Asymmetrical rotation is accompanied by complaints of pain. Pain may occur with rotation to either side. The axis of rotation appears to be shifted to one side, producing a twisting motion rather than a motion about a relatively straight line, typically at or close to the painful region.
Trunk or thoracic lateral flexion
Asymmetry and pain can also be noted with lateral flexion to either or both sides. During lateral thoracic flexion, the location and amount of spinal motion is assessed. If pain and a pivot point of motion are observed, the therapist manually stabilizes the segments of increased motion as the patient repeats lateral flexion. Improvement in symptoms while trying to redistribute the motion helps confirm the rotation aspect of the diagnosis.
Thoracic extension
Thoracic extension motion reproduces or increases the patient’s pain. Excessive extension range may be observed in a few segments of the thoracic spine.
Shoulder flexion
Unilateral shoulder flexion is considered a positive test if symptoms are reproduced or the thoracic spine is observed to laterally flex, rotate, or extend. If the primary test is positive, during the secondary test the patient is cued to stabilize the thoracic spine or it is manually stabilized during shoulder motion. The accuracy of the diagnosis is further supported if the patient reports a decrease in symptoms with the modified movement.
Supine tests
The tests are (1) shoulder flexion and (2) shoulder diagonal motion. Lying supine may produce a decrease in pain as a result of relaxation of the thoracic paraspinal muscles and decreased compression. If the patient has a large posterior rib hump, there may be an increase in symptoms unless the rotation can be accommodated. A small folded towel placed under the rib cage on the opposite side or manually supporting the rib cage should decrease the pain.
Shoulder flexion
Unilateral shoulder flexion will cause asymmetrical rib cage motion. During bilateral shoulder flexion, the rib cage is often observed to elevate excessively and the motion may be asymmetrical. If the patient reports pain with this test, the same motion should be repeated with contraction of the abdominals or manual stabilization of the rib cage.
Arm diagonal movement
Movement of the arm from a vertical position toward the horizontal on a diagonal line (as if stretching the sternal fibers of pectoralis major) produces rib cage motion. The ribs are observed to deviate toward the side of the moving arm, which is most easily seen by visually monitoring the caudal portion of the sternum and rib angle. Typically, one side is noted to move less than the other or not at all. The secondary test is the same arm motion performed with abdominals contracted to limit the excessive rib cage motion or manual stabilization of the rib cage.
Prone tests
The movement tests are (1) shoulder flexion (arm lift) and (2) trapezius muscle tests. The patient may report a decrease of pain when assuming the prone position because of relaxation of the thoracic paraspinal muscles and a decrease in compressive forces on the spine. A pillow placed under the chest may improve symptoms further.
Shoulder flexion
Unilateral shoulder flexion will cause thoracic rotation. When both arms are lifted off the supporting surface, thoracic extension and pain are produced. The secondary test requires the patient to recruit their abdominal muscles to limit any extension or rotation of the spine. Manual assistance from the therapist may help improve the movement or a pillow can be placed under the thorax and the bilateral shoulder flexion repeated.
Quadruped tests
Movement tests are (1) rocking backward, (2) shoulder flexion, and (3) crawling. Commonly, the patient assumes a position of thoracic extension and rotation or lateral flexion. Correction of extension alignment will reduce symptoms.
Rocking backward
The thoracic spine may extend and/or rotate. As the patient rocks backward, the therapist may need to monitor by palpation the area of the thoracic spine that is believed to be causing the pain to detect the motion.
Treatment
The treatment emphasis of the rotation-extension syndrome is to prevent extension and/or rotation motions of the thoracic spine in all positions and during motions of the trunk and the extremities. The patient’s daily routines and habits, such as sitting positions and body language, should be reviewed and observed to identify contributing factors. Those activities that the patient reports as painful are especially important to simulate in the clinic. For example, if the patient reports pain with running, observation of his or her running pattern will probably reveal asymmetrical arm swing and thoracic extension. The patient should correct this by allowing the thoracic spine to move toward flexion and limiting the arm swing.
Commonly, patients with the diagnosis of thoracic rotation-extension need to be cued to relax their thoracic paraspinal muscles and allow the thoracic spine to slightly flex. This extension posture is usually seen in both standing and sitting, but the position of rotation or lateral flexion occurs more often in sitting than standing. An example is the receptionist who sits erect in her chair and rotates to greet people as they approach her from the side. She should be cued to use the backrest on her chair and allow her trunk to relax into the chair and rotate the chair rather than rotating in her thoracic spine. When sitting, patients also need to refrain from leaning over onto an armrest or sitting on one of their legs that is bent under them.
Exercise Program
The home exercise program should focus on balance of trunk muscle activity, which often necessitates avoiding strengthening the trunk extensors. Frequently, the performance of the abdominal muscles is not optimal, so improving the strength and recruitment of the obliques is indicated. Abdominal activity is beneficial to help control the rotation forces on the rib cage and spine, as well as help balance the paraspinal activity; some patients seem to maintain spinal stability by excessive paraspinal muscle activity. Unilateral arm or leg movements are good exercises for recruiting the abdominal muscles to control the rotation of the trunk and to counter the extension of the thoracic spine.
Prone exercises are also useful for learning to control rotation and extension motions of the thoracic spine. Initially, the patient may need to lay over two pillows to position the thoracic spine in flexion (see Figure 4-27); eventually they can work toward using only one pillow under their chest. Prone unilateral arm movements, such as sliding the arm along a surface toward shoulder flexion or arm lifts, are often more challenging for patients than arm diagonals in supine and therefore should be monitored closely. To effectively stabilize the thorax during the exercise, the patient should be cued to make their trunk stiff and to activate their abdominals.
Quadruped rocking back is also a useful exercise, with the focus on controlling the motion so that the thoracic spine is not rotating or extending as the patient rocks backs. Often, the patient will flex both lumbar and thoracic spines rather than isolating the flexion to thoracic region. It may be helpful to provide manual contact over the posterior lumbar area to promote neutral spine position and gentle pressure at the sternum to promote slight thoracic flexion. A more challenging exercise in the quadruped position than rocking backward is unilateral shoulder flexion. If the patient is unable to control thoracic extension or rotation with the hips at 90 degrees of flexion, increasing the hip flexion angle during the unilateral shoulder flexion makes it easier to perform.
As mentioned earlier, compression may be an underlying source of symptoms with this diagnosis, as well as the others. Positioning strategies taught to the patient include sitting with arms supported on armrests or pillows or a lap board on the patient’s lap to help alleviate the compression. The patient may find it helpful to face the wall and rest his/her hands and forearms on the wall at head level, the emphasis is to let the upper extremities help support the weight of trunk and reduce the activity of the posterior thoracic muscles (Figure 4-30, A). Additionally, the quadruped and recumbent positions are useful in decreasing the compression of the spine.
Case Presentation
Thoracic Rotation-Extension Syndrome
Symptoms and History
A 34-year-old female was referred to physical therapy for treatment of right shoulder pain. The patient reported a sudden onset of pain in the right scapular region 10 days before her initial visit. Pain progressively worsened over the next few days; she reported breathing was painful at the times when pain was at its worst. She rated her pain as 9/10 at worst and 0 at best using the 0- to 10-point pain scale. Her pain had started to lessen over the 2 days before her initial physical therapy visit so that at the time of initial examination, she reported no pain. The patient attributed the improvement in symptoms to taking time off work and reducing her activity level over the previous week. Her pain was still quite bothersome at night and would interfere with her sleep. During the day, she reported being somewhat guarded with movements and if she twisted or “moved the wrong way,” she would get a sharp jab of pain. Lying supine and rolling over onto her side increased pain. Once in a sidelying position, she usually could become more comfortable. Driving was also uncomfortable, and when questioned, the patient admitted to leaning on the console while driving.
The patient was working as a postdoctoral fellow in molecular biology; this work required her to work under a fumigating hood or at a laboratory bench. When sitting at work, she would often have to sit on an elevated stool without back support. Her main computer was a laptop that she carried back and forth with her on a daily basis. She had not been exercising for the past few months, but 3 to 4 months before she had trained for and completed a 5K race. The patient enjoyed knitting as a pastime but even that was painful during the 2 weeks before her visit.
Patient’s goals were to resolve pain and return not only to normal work and self-care activities but also to be able to resume some type of exercise. She was concerned that she may need to permanently restrict activities to avoid exacerbating the pain.
Alignment Analysis
Patient was 5 foot 3 inches tall and weighed 142 pounds. She had mild kyphosis in the lower thoracic spine, and the upper thoracic spine was flat. The thorax was rotated and laterally flexed to the right and the right iliac crest was higher than the left. The right scapula was abducted with vertebral border 4 inches from the spine; the left scapula was resting in neutral abduction/adduction. Scapular depression was also noted on the right, corresponding to the right clavicle being aligned horizontally. In the seated position, the patient would assume a slouched posture.
Movement Analysis
Cervical ROM was pain-free, and the range was considered to be normal. The most significant movement impairment noted during cervical movements was an increase in posterior translation with cervical extension. Trunk forward flexion and lateral flexion were pain-free. Flexion ROM was greater in the lower than in the upper thoracic spine. Rotation to the right was greater in range than rotation to the left, and vague discomfort was present with rotation to the right. Extension of the trunk also produced mild discomfort in the right upper thoracic area, which was the area of her chief complaint. Extension occurred mostly in the upper thoracic spine rather than in the lumbar spine. During trunk rotation and extension, the patient had difficulty isolating motion to the spine, so she moved the scapula while moving the spine. This combination of thoracic and scapular motion made isolating the source of symptoms more difficult.
Assessment of breathing pattern revealed an increase in pump-handle motion, whereas the bucket-handle motion was diminished.
The patient did not note any pain at this time with deep inhalation. Shoulder flexion did not produce symptoms, and range was normal. A movement impairment of scapular depression was noted (right greater than left). A secondary test was not performed because of the lack of symptom reproduction. Palpation of the musculature in the scapular region did not produce pain.
Active shoulder flexion created rotation in the rib cage. With right shoulder flexion, rib cage rotation occurred almost immediately when she initiated shoulder flexion and caused discomfort; with left shoulder flexion, rotation occurred later in the range and was not as pronounced. During the secondary test, the rib cage was manually stabilized during shoulder flexion and the symptoms were eliminated. Patient was unable to improve the movement pattern using her own abdominal contraction.
Arm diagonal movements were assessed by having the patient move the arm from 90 degrees of humeral flexion outward and down toward horizontal as if stretching the sternal portion of the pectoralis major. Rotation of the rib cage was noted during with arm movement (right greater than left); minimal pain was reported with this movement.
Hip abduction lateral rotation from a hip-flexed position also revealed poor abdominal control because of the pelvic rotation noted with leg movement, however, no pain was reported. The patient did note mild pain moving from supine to sidelying and prone positions. When turning from supine to her side, she moved into a partial sit-up by pushing back with her arm, then as she moved toward her side, she twisted her thoracic spine. Immediate modification of her rolling method resulted in a pain-free motion.
The patient was positioned over a pillow in the prone position, which did not reproduce any pain. Manual muscle testing of scapular muscles was performed with the patient lying with the pillow under her chest. Strength of the middle trapezius on the right was 4-/5, left 3/5; lower trapezius on the right was 3+/5, on the left 3/5. No pain was produced during tests if the examiner supplied fixation with a hand on opposite side of thorax.29 Rhomboid strength was 5/5 bilaterally.
The patient was cued to perform bilateral arm lifts with her hands clasped on top of her head. The upper thoracic spine was observed to extend, and the patient was noted to push into cervical flexion so that she pressed her forehead into the supporting towel roll. With cueing to contract her abdominal muscles for stabilization and to avoid extending the upper back, the patient could improve her performance.
The patient was diagnosed with a thoracic rotation-extension syndrome. Movements or positions of thoracic rotation reproduced her pain. In particular, rotation moments on the rib cage caused pain. Supporting factors for the extension diagnosis are the flat upper thoracic alignment, extension of upper thoracic spine during trunk extension and prone tests, and pain in the upper thoracic region. The poor abdominal muscle control was a contributing factor to both the rotation and extension movement impairments. The kyphosis in the lower thoracic spine was suspected to contribute to the extension in the upper thoracic spine as compensation. Although strain of the trapezius muscle had been considered as a possible source of the pain, the lack of pain with palpation and during strength testing did not support the hypothesis.
Significant time was spent educating the patient on postural corrections. Key corrections included sitting with back support as often as possible, avoiding twisting or rotation of the trunk, and stopping sidebending onto the arm of the chair or the console of the car. The patient found it comfortable to support her arms on pillows while seated, so this was encouraged to help unload the weight of upper extremities off the thoracic region. This support was particularly helpful while knitting.
Bed mobility and transfers were practiced with patient. She was taught to avoid twisting her spine as she moved from one position to another, which helped her avoid symptoms. On her first visit the patient was instructed in (1) wall slides with scapular elevation; (2) prone, with a pillow under her thorax, arm lifts with her hands on her head with instruction to avoid thoracic extension and to contract her abdominal muscles; and (3) hip abduction with lateral rotation in supine.
Her exercise program was designed to improve abdominal muscle performance to help avoid thoracic extension and to control rotation. Improving scapular muscle performance was also to assist in reducing the asymmetrical rotation of her thoracic spine. On the patient’s second visit, she was overcorrecting her spinal alignment so that rather than just gently lifting her chest to correct the lower thoracic flexion, she was extending her spine forcefully and causing pain. The overcorrection also occurred during the wall slide exercise and prone arm lifts. Postural correction was practiced with the patient in sitting and standing using a mirror for visual feedback. She was able to reproduce the corrected alignment. Once the patient could distinguish the correct position, she was able to limit the thoracic extension during the wall slides as well. The prone exercise was modified having the patient place two pillows under her thorax so that the upper thoracic spine was placed in slight flexion. Verbal cues for abdominal recruitment were also provided, and the patient could perform the exercise correctly without pain.
Sleeping continued to be disturbed; specifically, the patient awoke with pain when she was changing positions. She remembered pushing her elbow down into the bed while rolling to sidelying from supine. Bed mobility was again practiced with the emphasis on “log rolling” so that her shoulders, trunk, and hips rotated at the same time. Patient was advised to practice rolling a few times each day so that during the night, the correct strategy for rolling would be more automatic.
Over the next month the patient was seen once each week, during which time her exercise program was progressed. Additions to her program included (1) practicing transfers sit to supine to sidelying without allowing lateral flexion or rotation of the trunk, (2) rolling to each side while using hands to hold knees toward chest and keeping head supported, (3) supine bilateral then unilateral shoulder flexion without allowing the rib cage to rotate, and (4) arm diagonals. She also continued with hip abduction lateral rotation from hip flexion with addition of a 2-pound weight at the knee to create a greater load on the obliques, prone arm lifts, and wall slides with scapular elevation.
Shoulder flexion in supine was first given to the patient with instructions to flex both arms at the same time and use abdominal muscles to prevent the rib cage from elevating. Bilateral motion was easier because the patient did not have to prevent rotation. She was eventually progressed to performing the exercise with one arm at a time. Patient was not able to control trunk sufficiently to perform shoulder flexion in the quadruped position.
The patient was seen for 5 visits over a 10-week period. At her final visit, she reported resolution of her pain unless she twisted without thinking about how she was moving, but this occurred only occasionally. She had resumed all of her regular responsibilities both at work and at home. She was able to sleep through the night without awakening even with a change of position. Driving was pain-free, although she did have to remind herself to avoid leaning onto the console when she drove the car. The patient also reported that she felt her strength in her arms and trunk had improved.
Thoracic Rotation Syndrome
Thoracic rotation syndrome is characterized by pain associated with the movement and postures of thoracic rotation. Asymmetries of the rib cage are the common alignment impairments observed in this syndrome. Common muscle impairments include asymmetry in the length and recruitment of the trunk muscles, including thoracic paraspinal and scapulothoracic muscles (middle trapezius rhomboids), short or stiff anterior scapulohumeral muscles (pectoralis minor and major, latissimus dorsi), and asymmetrical length and strength of the oblique abdominal muscles. Approximation of the ribs resulting from rotation and/or compression from stiffness or shortness of the abdominal muscles should be considered a contributing factor to pain. In addition, thoracic rotation impairments occur in position of both thoracic flexion and extension.
Symptoms and History
Individuals with the rotation syndrome complain of pain in the thoracic region, which may radiate into the lateral and anterior rib cage or abdomen. They note an increase in pain with reaching or trunk rotation. The most common recreational activities reported by individuals with rotation syndrome include any activity that repeatedly places their trunk into rotation, including tennis, softball, sailing, squash, and running (asymmetrical arm swing and trunk rotation). Habitual trunk rotation during functional activities are commonly observed in individuals with this syndrome and include arrangement of their desk so that rotation is required to reach the phone, computer, or files and/or to greet incoming customers/clients; sitting shifted to one side (leaning toward the mouse pad side of desk); sitting on one foot; or leaning on an armrest while working, reading, driving, and watching television. Pain with sitting is reduced or abolished when the individual is instructed to use the backrest to keep the spine straight and to avoid asymmetrical postures, leg crossing, unilateral armrest use, and sitting on one foot. Commonly, individuals with a rotation syndrome report a history of chest surgery in which the rib cage or sternum have been surgically manipulated.
Movement Impairment Analysis
Thoracic rotation with an asymmetry of the rib cage will be the most common alignment impairment found in this diagnosis. The presence of a rib cage asymmetry can be noted from either an anterior or posterior perspective. It is important to note the shape of the rib cage and its effect on the position of the scapulae. A posterior rib cage asymmetry may cause the alignment of the scapulae to appear asymmetrical, when in fact the structural base (rib cage) that the scapulae are resting on is asymmetrical. An anterior rib cage asymmetry may cause the size or shape of the breast to appear asymmetrical. See the preceding Case Presentation, “Thoracic Rotation-Flexion Syndrome” for discussion on the affect of scoliosis on this diagnosis.
Standing tests
Standing trunk flexion demonstrates excessive rotation in the thoracic spine; in addition, the presence of a rib hump is more noticeable in a thoracic-flexed position compared to standing. The motions of trunk rotation and lateral flexion demonstrate an asymmetry or are excessive in a selected group of thoracic segments, with pain with these movements. Either motion may cause a radicular symptom into the chest or abdomen as a result of neural compromise at either the vertebral foramen or along the length of the ribs. Unilateral shoulder flexion, a test for presence of spine motion during extremity motion, results in a side-to-side variation so that arm motion results in a motion at the spine, with or without reproduction of the presenting symptoms. Bilateral shoulder flexion demonstrates unilateral trunk rotation. With both unilateral and bilateral shoulder flexion, pain and motion are improved if the trunk is provided support, either from a wall or lying recumbent, which aids in prevention of rotation with the extremity movement. Recruitment of the abdominal musculature for trunk control during this follow-up test may be needed to control the rotational forces on the spine. In an early stage of rehabilitation, protection of the thoracic spine and neural tissue can be achieved by performing supported shoulder flexion while facing the wall. Thus some of the weight of the upper body is supported by the wall, and the rotation of the thoracic spine can be corrected. Progress can be made once the patient has advanced to Stage 2 to strengthen the thoracic paraspinal muscles in the same position by active shoulder flexion or by lifting the hands off the wall after performing shoulder flexion sliding the hands up the wall. Asymmetrical motion of the rib cage is noted during ventilation (most commonly during bucket-handle assessment of the rib cage).
Supine tests
Pain will commonly be reported when assuming the supine position. Support of the rib cage by appropriate padding can be used unilaterally to accommodate a structural rotation of the rib cage or spine. Examination of the subcostal margin in the supine position reveals rib cage asymmetries and gives insight into muscle length issues related to the internal oblique and external oblique muscles. An increased subcostal margin in standing and supine would indicate a decreased length of the internal oblique and an increased length of the external oblique musculature.
During testing of the abdominal musculature, there is poor control of the oblique abdominal muscles with rotation of the rib cage and/or thoracic spine during lower extremity movement. Unilateral shoulder flexion in the supine position reveals rib cage motion or thoracic spine motion that is most pronounced when moving the arm in a diagonal pattern. Pain with arm motion commonly decreases with cueing to control the rotational movement by increasing abdominal muscle contraction during the motion. If the patient is in Stage 1 of rehabilitation, the recruitment of the abdominal musculature may increase pain because of compressive force on the spine and rib cage. Thus caution should be taken during abdominal muscle testing, monitoring closely for an increase or worsening of the presenting symptoms. Hip abduction with lateral rotation in the flexed position is commonly assessed if the individual complains of symptoms during functional activities that requires lower extremity motions such as running and walking. Rotation of the thoracic spine and rib cage and pain noted during the lower extremity motion is reduced by cueing to recruit the trunk musculature during the activity. Both the thoracic spine extensors and the abdominal musculature may need to be recruited for adequate trunk rotation control during upper and lower extremity motions.
Prone tests
The prone positioning may reduce symptoms in younger more flexible individuals with a thoracic rotation syndrome. However, the spines of older individuals may need increased support in prone to accommodate the amount of thoracic flexion present. Prone lying may also require some lateral trunk support to minimize rotation while in this position.
In individuals with a thoracic rotation diagnosis, unilateral shoulder flexion with scapular posterior tilt starting with the shoulder already in the flexed position while in the prone position will reveal thoracic rotation. Instructing the patient to increase paraspinal muscle recruitment or abdominal muscle recruitment will aid in controlling the rotation and usually decrease the symptoms. In an individual who is not able to tolerate unilateral arm motions, bilateral symmetrical scapular posterior tilt and adduction with shoulder flexion can be performed by increasing the degrees of difficulty such as hands on head, arms bent, or arms straight.
Quadruped tests
When positioned in quadruped, there may not be a noticeable amount rotation of the rib cage (hump); however, rocking backward or shoulder flexion in quadruped may reveal trunk rotation. Quadruped is commonly a pain relieving position for individuals with thoracic rotation because the thoracic spine is suspended between the upper and lower extremities and thus in an unloaded position. Because of upper extremity muscle weakness and rib cage asymmetries, scapular winging or tilting will commonly be present. As initially noted, rocking back in the quadruped position will reveal an increase in rotation, while cueing is needed to relax the abdominal musculature to prevent any contraction of the abdominal muscles during motion, that would cause an increase in the rotation of the thoracic spine. Shoulder flexion in quadruped will cause rotation of the thoracic spine and rib cage, and cueing recruits the latissimus dorsi and thoracic back extensors by an isometric contraction (draw the heel of the weight-bearing hand toward the ipsilateral knee). Shoulder isometric extension will reduce the rotation. Inability to perform this correctly in the quadruped position should prompt the therapist to downgrade the activity by performing unilateral shoulder flexion in the prone position. In very active populations, crawling can be assessed to create a more unstable activity that requires trunk rotation. Crawling in individuals with thoracic rotation will reveal an asymmetry in the trunk rotation during this task.
Functional Activities
Observation of the thoracic spine and rib cage should be done during aggravating functional activities. Specific attention should be paid to the amount of abdominal muscle recruitment compared to thoracic paraspinal muscle recruitment during the task. If simply cueing to reduce the motion of rotation does not decrease the symptoms, timing the movement so that the individual is instructed to first relax the abdominals and then perform the task may reduce the mechanical load enough to allow the individual to perform with decreased compression and reduce rotation and pain.
Thoracic Extension Syndrome
Symptoms and History
Individuals with thoracic extension syndrome have an altered flexibility of the thoracic spine so that extension occurs too easily. Thoracic extension occurs most often in the interscapular region but can occur in the lower thoracic segments or the thoracolumbar junction. The symptoms associated with thoracic extension syndrome are usually confined to these same areas; however, patients may have a greater distribution of their symptoms. According to Bogduk,159 pain from the thoracic spine is quasisegmental; the location of pain may be representative of the source of pain with an accuracy of one to two segments.
The habit of holding an erect posture in both sitting and standing is characteristic of individuals with this syndrome, and both positions are associated with pain. The habitual contraction of the spinal extensors contributes to altered flexibility in the thoracic spine so that extension occurs too easily. This syndrome occurs more commonly in younger rather than older people, especially those who participate in dance or gymnastics and who work with their arms overhead.
In some patients, the entire spinal column is flattened so that all of the normal curves of the spine are decreased. The upper thoracic spine, most often between the scapulae, may actually appear to be in some extension. The ability of the thoracic spine to extend may be related to some anomaly of the thoracic vertebrae. Normally, extension is limited by the superior facet impinging onto the vertebrae below, as well as the contact of the spinous processes. Because this syndrome is often associated with overactivity of both thoracic paraspinals and scapular adductors, an impairment of scapular adduction can be present as well.
Key Tests and Signs
The key tests for thoracic extension syndrome are as follows and are listed in the order they are performed during the examination.
Standing tests
The tests performed in standing are (1) trunk flexion, (2) trunk extension, (3) trunk rotation, (4) lateral flexion, and (5) ventilation.
Trunk flexion
The amount of flexion available in the thoracic spine is often less than the expected 30 to 40 degrees of flexion.2,3 If the extension impairment involves the upper thoracic spine, the loss of flexion ROM may not be noticeable because normally the upper thoracic spine contributes less than half of the available range2 (see Figure 4-19). During the return to the upright position, pain may be reported and careful observation may reveal that extension is exaggerated at some segments, usually in the painful area. The distribution of motion between segments is thought to transition gradually, so obvious motion occurring at a few segments would be considered faulty. Cueing the patient to avoid excessive extension during the return from forward bending will improve symptoms.
Sitting test
In a sitting test, assessment of a individual’s preferred alignment and modification of alignment are performed. The patient will most often sit with the spine held very erect. Cues to relax his or her spine and allow it to slightly flex should decrease the pain. Further relief may be obtained by supporting the spine in the flexed position with the backrest of the chair.
Supine tests
The patient may report a decrease of pain when assuming the supine position as a result of relaxation of the thoracic paraspinals; the reduction of compression on the spine may possibly aid in pain reduction. Assessment of abdominal performance typically reveals weakness.
Shoulder flexion
During bilateral shoulder flexion, the rib cage is often observed to elevate excessively. The patient may be able to feel extension of the involved thoracic segments. If the patient reports pain with this test, the same motion should be repeated with contraction of the abdominals or manual stabilization of the rib cage.
Prone tests
The following movement tests are assessed with the patient in the prone position: (1) shoulder flexion (arm lift) and (2) assessment of trapezius muscle performance. With both movement tests, the impairment and symptoms would be expected to occur more consistently when both arms are lifted off the surface. As with supine, the effect of position on symptoms is assessed. The patient may report a decrease of pain on assuming the prone position caused by relaxation of the thoracic paraspinal muscles and a decrease in compressive forces on the spine. A pillow placed under the chest may improve symptoms further.
Shoulder flexion
Shoulder flexion performed unilaterally might cause thoracic extension; however, when both arms are lifted off the surface, thoracic extension and pain are produced. The secondary test requires the patient to recruit their abdominal muscles to limit extension of the spine. Manual assistance from the therapist may help improve the movement.
Trapezius muscle test
A dominance of the rhomboid muscles may be observed during a middle trapezius test so that the scapula moves toward downward rotation when the patient must support the weight of the arm. With middle and lower trapezius testing, extension of the upper or midthoracic spine may be noted as well. Although the trapezius muscle may test strong during an isolated test, the inability of the patient to control the thoracic spine extension during the test or exercise attempt is the most important finding.
Quadruped tests
In the quadruped position, both alignment and movement tests are performed. Commonly, the patient will assume a position of thoracic extension, and the scapulae will be prominent on the posterior thorax. The patient may appear to be “hanging” on their shoulders and scapulae.
Shoulder flexion.
Movement of the arm into shoulder flexion may produce mild extension of the thoracic spine in those individuals whose relative flexibility into thoracic extension is greatly exaggerated. This motion may not cause pain because the spine is not subjected to the same compression forces as with standing.
Treatment
The treatment priority for thoracic extension syndrome is to restrict movement of the spine into extension during the patient’s activities. This will be most effective if the patient learns to recognize spinal extension and the extremity movements that induce extension moments on the thoracic region. For example, if the patient routinely has pain associated with styling her hair because arm elevation induces thoracic extension, then it is necessary to teach the patient to hold gentle flexion in the thoracic spine while elevating the arms.
Patients with the diagnosis of thoracic extension syndrome typically exhibit habitual thoracic extension. Instruction to relax the thoracic paraspinals and slightly flex the thoracic spine improves symptoms. Initially, pain will be an indication of faulty positioning; however, long-term management requires that the patient develop an awareness of spinal posture.
If compression is contributing to symptoms, positioning strategies, such as sitting with arms supported, are encouraged. In standing, the patient can help reduce compressive forces by resting the hands and forearms on the wall at head level and relaxing the trunk, so that the upper extremities help support the weight of trunk and reduce the activity of the posterior thoracic muscles. Recumbent positions or quadruped are frequently pain relieving and should be used to help control symptoms.
Exercise Program
The home exercise program should focus on improving the motor control of the thoracic region and reversing the trend of excessive flexibility into thoracic extension or rib cage elevation. Failure to avoid thoracic extension postures and movements will perpetuate the pain problem. Exercises that may be useful when trying to improve the motor control are similar to those listed for treatment of the thoracic rotation-extension syndrome, with the obvious difference being that rotation is not a problem. Often, abdominal muscle activity is emphasized as a means to control or stop the spinal extension. The abdominal muscles may be weak (insufficient contractile elements) or their recruitment pattern is impaired. The corrective exercise is to engage the abdominal muscles to limit thoracic extension or excessive elevation of the rib cage during arm elevation. This exercise can be practiced in standing, sitting, or quadruped.
Conclusion
Movement system syndromes of the thoracic spine are most commonly caused by impairments in alignment, stabilization, and movement patterns. Pain syndromes that develop from movement-related tissue injury require consideration of the mechanics that cause tissue injury. This chapter presented key principles for examining alignment, movement, and muscle impairments of the thoracic region. Emphasis was placed on a structured examination, key tests for diagnosis, and treatment for the specific impairments. The emphasis of treatment of movement related syndromes is on education regarding changes in alignment, muscle recruitment, and reduction of thoracic movement by redistribution of motion to other regions. The ultimate goal is to achieve optimal alignment and movement patterns that are consistent with kinesiology. Malalignments and altered movement patterns of the thoracic spine also play a key role in problems of the cervical spine, shoulder, and lumbar spine. Thus optimizing thoracic alignment and trunk control is important in many, if not most, of the musculoskeletal pain syndromes and not just when pain is present in the thoracic spine region.
1 Sahrmann S. Diagnosis and treatment of movement impairment syndromes. St Louis: Mosby; 2002.
2 White AAIII, Panjabi M. Clinical biomechanics of the spine, ed 2. Philadelphia: Lippincott-Raven; 1990.
3 Neumann DA. Kinesiology of the musculoskeletal system: foundations of rehabilitation. St Louis: Mosby; 2002.
4 Harrison DE, Colloca CJ, Harrison DD, et al. Anterior thoracic posture increases thoracolumbar disc loading. Eur Spine J. 2005;14(3):234-242.
5 Keller TS, Harrison DE, Colloca CJ, et al. Prediction of osteoporotic spinal deformity. Spine. 2003;28(5):455-462.
6 Silverman SL. The clinical consequences of vertebral compression fracture. Bone. 1993;13(2):S27-S31.
7 Mueller MJ, Maluf KS. Tissue adaptation to physical stress: a proposed “Physical Stress Theory” to guide physical therapist practice, education, and research. Phys Ther. 2002;82(4):383-403.
8 Russek LN. Hypermobility syndrome. Phys Ther. 1999;79(6):591-599.
9 Russek LN. Examination and treatment of a patient with hypermobility syndrome. Phys Ther. 2000;80(4):386-398.
10 Sinaki M, Itoi E, Rogers JW, et al. Correlation of back extensor strength with thoracic kyphosis and lumbar lordosis in estrogen-deficient women. Am J Phys Med Rehabil. 1996;75(5):370-374.
11 Sinaki M, Nwaogwugwu NC, Phillips BE, et al. Effect of gender, age, and anthropometry on axial and appendicular muscle strength. Am J Phys Med Rehabil. 2001;80(5):330-338.
12 Sinaki M, Lynn SG. Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study. Am J Phys Med Rehabil. 2002;81(4):241-246.
13 Willner S. Spinal pantograph: a non-invasive technique for describing kyphosis and lordosis in the thoracolumbar spine. Acta Orthop Scand. 1981;52(5):525-529.
14 Mellin G. Measurement of thoracolumbar posture and mobility with a Myrin inclinometer. Spine. 1986;11(7):759-762.
15 Gajdosik RL, Albert CR, Mitman JJ. Influence of hamstring length on the standing position and flexion range of motion of the pelvic angle, lumbar angle, and thoracic angle. J Orthop Sports Phys Ther. 1994;20(4):213-219.
16 Christie HJ, Kumar S, Warren SA. Postural aberrations in low back pain. Arch Phys Med Rehabil. 1995;76(3):218-224.
17 Fon GT, Pitt MJ, Thies ACJr. Thoracic kyphosis: range in normal subjects. AJR Am J Roentgenol. 1980;134(5):979-983.
18 Singer KP, Jones TJ, Breidahl PD. A comparison of radiographic and computer-assisted measurements of thoracic and thoracolumbar sagittal curvature. Skel Radiol. 1990;19(1):21-26.
19 Itoi E, Sinaki M. Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age. Mayo Clin Proc. 1994;69(11):1054-1059.
20 Jackson RP, Mcmanus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low-back-pain matched for age, sex, and size—a prospective controlled clinical-study. Spine. 1994;19(14):1611-1618.
21 Korovessis PG, Stamatakis M, Baikousis A. Unrecognized laceration of main bronchus caused by fracture of the T6 vertebra. Eur Spine J. 1998;7(1):72-75.
22 Korovessis P, Stamatakis M, Baikousis A. Segmental roentgenographic analysis of vertebral inclination on sagittal plane in asymptomatic versus chronic low back pain patients. J Spinal Disord. 1999;12(2):131-137.
23 Tuzun C, Yorulmaz I, Cindas A, et al. Low back pain and posture. Clin Rheumatol. 1999;18(4):308-312.
24 Mirza SK, White AAIII. Anatomy of intervertebral disc and pathophysiology of herniated disc disease. J Clin Laser Med Surg. 1995;13(3):131-142.
25 Carr AJ, Jefferson RJ, Turner-Smith AR, et al. An analysis of normal back shape measured by ISIS scanning. Spine. 1991;16(6):656-659.
26 Crawford MB, Toms AP, Shepstone L. Defining normal vertebral angulation at the thoracolumbar junction. AJR Am J Roentgenol. 2009;193(1):W33-W37.
27 Zoeller R, Sahrmann SA, Kuhnline M, et al. Changes in the infrasternal angle with abdominal muscle contractions. Phys Ther. 1993;73:S104.
28 Bellemare F, Jeanneret A, Couture J. Sex differences in thoracic dimensions and configuration. Am J Respir Crit Care Med. 2003;168(3):305-312.
29 Kendall F. Muscles: testing and function with posture and pain, ed 5. Baltimore: Lippincott Williams & Wilkins; 2005.
30 Lowe TG, Line BG. Evidence-based medicine: analysis of Scheuermann kyphosis. Spine. 2007;32(Suppl 19):S115-S119.
31 Tribus CB. Scheuermann’s kyphosis in adolescents and adults: diagnosis and management. J Am Acad Orthop Surg. 1998;6(1):36-43.
32 Poolman RW, Been HD, Ubags LH. Clinical outcome and radiographic results after operative treatment of Scheuermann’s disease. Eur Spine J. 2002;11(6):561-569.
33 Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 2002;359(9321):1929-1936.
34 Kanis JA, Borgstrom F, De Laet C, et al. Assessment of fracture risk. Osteoporos Int. 2005;16(6):581-589.
35 Kotz K, Deleger S, Cohen R, et al. Osteoporosis and health-related quality-of-life outcomes in the Alameda County Study population. Prev Chronic Dis. 2004;1(1):A05.
36 Sinaki M, Brey RH, Hughes CA, et al. Significant reduction in risk of falls and back pain in osteoporotic-kyphotic women through a Spinal Proprioceptive Extension Exercise Dynamic (SPEED) program. Mayo Clin Proc. 2005;80(7):849-855.
37 Sinaki M, Brey RH, Hughes CA, et al. Balance disorder and increased risk of falls in osteoporosis and kyphosis: significance of kyphotic posture and muscle strength. Osteoporos Int. 2005;16(8):1004-1010.
38 O’Sullivan PB, Grahamslaw KM, Kendell M, et al. The effect of different standing and sitting postures on trunk muscle activity in a pain-free population. Spine. 2002;27(11):1238-1244.
39 Grieve GP. Common vertebral joint problems. London: Longman Group Limited; 1981.
40 Stubgen JP. Rigid spine syndrome: a noninvasive cardiac evaluation. Pediatr Cardiol. 2008;29(1):45-49.
41 Omey ML, Micheli LJ, Gerbino PG. Idiopathic scoliosis and spondylolysis in the female athlete. Tips for treatment. Clin Orthop Relat Res. 2000;372:74-84.
42 Wynne-Davies R. Familial (idiopathic) scoliosis. A family survey. J Bone Joint Surg Br. 1968;50(1):24-30.
43 Burwell RG, Dangerfield PH, Moulton A, et al. Etiologic theories of idiopathic scoliosis: autonomic nervous system and the leptin-sympathetic nervous system concept for the pathogenesis of adolescent idiopathic scoliosis. Stud Health Technol Inform. 2008;140:197-207.
44 Bagnall KM, Raso VJ, Hill DL, et al. Melatonin levels in idiopathic scoliosis. Diurnal and nocturnal serum melatonin levels in girls with adolescent idiopathic scoliosis. Spine. 1996;21(17):1974-1978.
45 Hilibrand AS, Blakemore LC, Loder RT, et al. The role of melatonin in the pathogenesis of adolescent idiopathic scoliosis. Spine. 1996;21(10):1140-1146.
46 Machida M, Dubousset J, Yamada T, et al. Serum melatonin levels in adolescent idiopathic scoliosis prediction and prevention for curve progression—a prospective study. J Pineal Res. 2009;46(3):344-348.
47 Smith RM, Pool RD, Butt WP, et al. The transverse plane deformity of structural scoliosis. Spine. 1991;16(9):1126-1129.
48 Shohat M, Shohat T, Nitzan M, et al. Growth and ethnicity in scoliosis. Acta Orthop Scand. 1988;59(3):310-313.
49 Dickson RA. The etiology and pathogenesis of idiopathic scoliosis. Acta Orthop Belg. 1992;58(Suppl 1):21-25.
50 Cheng S, Sipila S, Taaffe DR, et al. Change in bone mass distribution induced by hormone replacement therapy and high-impact physical exercise in post-menopausal women. Bone. 2002;31(1):126-135.
51 Bruyneel AV, Chavet P, Bollini G, et al. Lateral steps reveal adaptive biomechanical strategies in adolescent idiopathic scoliosis. Ann Readapt Med Phys. 2008;51(8):630-641.
52 Bruyneel AV, Chavet P, Bollini G, et al. Dynamical asymmetries in idiopathic scoliosis during forward and lateral initiation step. Eur Spine J. 2009;18(2):188-195.
53 Lao ML, Chow DH, Guo X, et al. Impaired dynamic balance control in adolescents with idiopathic scoliosis and abnormal somatosensory evoked potentials. J Pediatr Orthop. 2008;28(8):846-849.
54 Mallau S, Bollini G, Jouve JL, et al. Locomotor skills and balance strategies in adolescents idiopathic scoliosis. Spine. 2007;32(1):E14-E22.
55 Olafsson Y, Odergren T, Persson HE, et al. Somatosensory testing in idiopathic scoliosis. Dev Med Child Neurol. 2002;44(2):130-132.
56 Frownfelter D, Dean E. Cardiovascular and pulmonary physical therapy, ed 4. St Louis: Mosby; 2006.
57 Santos PS, Resende LA, Fonseca RG, et al. Intercostal nerve mononeuropathy: study of 14 cases. Arq Neuropsiquiatr. 2005;63(3B):776-778.
58 Carnett JB. The simulation of gall-bladder disease by intercostal neuralgia of the abdominal wall. Ann Surg. 1927;86(5):747-757.
59 Carnett JB, Bates W. The treatment of intercostal neuralgia of the abdominal wall. Ann Surg. 1933;98(5):820-829.
60 Hardy PA. Post-thoracotomy intercostal neuralgia. Lancet. 1986;1(8481):626-627.
61 Defalque RJ, Bromley JJ. Poststernotomy neuralgia: a new pain syndrome. Anesth Analg. 1989;69(1):81-82.
62 Selbst SM. Chest pain in children. Am Fam Physician. 1990;41(1):179-186.
63 Gregory PL, Biswas AC, Batt ME. Musculoskeletal problems of the chest wall in athletes. Sports Med. 2002;32(4):235-250.
64 Monnin JL, Pierrugues R, Bories P, et al. The slipping rib syndrome: a cause of diagnostic errors in abdominal pain. La Presse Medicale. 1988;17(1):25-29.
65 Udermann BE, Cavanaugh DG, Gibson MH, et al. Slipping rib syndrome in a collegiate swimmer: a case report. J Athl Train. 2005;40(2):120-122.
66 Coelho MS, Guimaraes PS. Pectus carinatum. J Bras Pneumol. 2007;33(4):463-474.
67 Mavanur A, Hight DW. Pectus excavatum and carinatum: new concepts in the correction of congenital chest wall deformities in the pediatric age group. Conn Med. 2008;72(1):5-11.
68 Nakaoka T, Uemura S, Yano T, et al. Does overgrowth of costal cartilage cause pectus excavatum? A study on the lengths of ribs and costal cartilages in asymmetric patients. J Pediatr Surg. 2009;44(7):1333-1336.
69 Schoenmakers MAGC, Gulmans VAM, Bax NMA, et al. Physiotherapy as an adjuvant to the surgical treatment of anterior chest wall deformities: a necessity? J Pediatr Surg. 2000;35(10):1440-1443.
70 Canavan PK, Cahalin L. Integrated physical therapy intervention for a person with pectus excavatum and bilateral shoulder pain: a single-case study. Arch Phys Med Rehabil. 2008;89(11):2195-2204.
71 O’Sullivan P, Dankaerts W, Burnett A, et al. Evaluation of the flexion relaxation phenomenon of the trunk muscles in sitting. Spine. 2006;31(17):2009-2016.
72 Callaghan JP, Dunk NM. Examination of the flexion relaxation phenomenon in erector spinae muscles during short duration slumped sitting. Clin Biomech. 2002;17(5):353-360.
73 Panjabi MM, Krag MH, Dimnet JC, et al. Thoracic spine centers of rotation in the sagittal plane. J Orthop Res. 1984;1(4):387-394.
74 Edmondston SJ, Aggerholm M, Elfving S, et al. Influence of posture on the range of axial rotation and coupled lateral flexion of the thoracic spine. J Manipulative Physiol Ther. 2007;30(3):193-199.
75 Grice AS. Radiographic, biomechanical and clinical factors in lumbar lateral flexion: part I. J Manipulative Physiol Ther. 1979;2:26-34.
76 Panjabi MM, Oxland TR, Yamamoto I, et al. Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load-displacement curves. J Bone Joint Surg Am. 1994;76(3):413-424.
77 Molnar S, Mano S, Kiss L, et al. Ex vivo and in vitro determination of the axial rotational axis of the human thoracic spine. Spine. 2006;31(26):E984-E991.
78 McDonnell MK, Sahrmann S. Movement impairment syndromes of the thoracic and cervical spine. In: Grant R, editor. Physical therapy of the cervical and thoracic spine. New York: Churchill Livingstone, 2002.
79 Spitznagle TM. Musculoskeletal chronic pelvic pain. In: Carriere B, Feldt C, editors. The pelvic floor. Stuttgart: Georg Thieme Verlag, 2010.
80 Lee LJ, Coppieters MW, Hodges PW. Differential activation of the thoracic multifidus and longissimus thoracis during trunk rotation. Spine. 2005;30(8):870-876.
81 Oatis CA. Kinesiology: the mechanics & pathomechanics of human movement. Philadelphia: Lippincott Williams & Williams; 2004.
82 Sizer PS, Brismee JM, Cook C. Coupling behavior of the thoracic spine: a systematic review of the literature. J Manipulative Physiol Ther. 2007;30(5):390-399.
83 McInerney J, Ball PA. The pathophysiology of thoracic disc disease. Neurosurg Focus. 2000;9(4):e1.
84 Oppenheim JS, Rothman AS, Sachdev VP. Thoracic herniated discs: review of the literature and 12 cases. Mount Sinai J Med. 1993;60(4):321-326.
85 Wilke A, Wolf U, Lageard P, et al. Thoracic disc herniation: a diagnostic challenge. Man Ther. 2000;5(3):181-184.
86 Yelland MJ. Back, chest and abdominal pain. How good are spinal signs at identifying musculoskeletal causes of back, chest or abdominal pain? Aust Fam Physician. 2001;30(9):908-912.
87 Xiong Y, Lachmann E, Marini S, et al. Thoracic disk herniation presenting as abdominal and pelvic pain: a case report. Arch Phys Med Rehabil. 2001;82(8):1142-1144.
88 Rohde RS, Kang JD. Thoracic disc herniation presenting with chronic nausea and abdominal pain. A case report. J Bone Joint Surg Am. 2004;86(2):379-381.
89 Jorgensen LS, Fossgreen J. Back pain and spinal pathology in patients with functional upper abdominal pain. Scand J Gastroenterol. 1990;25(12):1235-1241.
90 Hamberg J, Lindahl O. Angina pectoris symptoms caused by thoracic spine disorders. Clinical examination and treatment. Acta Medica Scand Suppl. 1981;644:84-86.
91 Fruergaard P, Launbjerg J, Hesse B, et al. The diagnoses of patients admitted with acute chest pain but without myocardial infarction. Eur Heart J. 1996;17(7):1028-1034.
92 Frobert O, Fossgreen J, Sondergaard-Petersen J, et al. Musculoskeletal pathology in patients with angina pectoris and normal coronary angiograms. J Intern Med. 1999;245(3):237-246.
93 Leong JC, Lu WW, Luk KD, et al. Kinematics of the chest cage and spine during breathing in healthy individuals and in patients with adolescent idiopathic scoliosis. Spine. 1999;24(13):1310-1315.
94 Massery M. Multi system consequences of impaired breathing mechanics and/or postural control. In Frownfelter D, Dean E, editors: Cardiovascular and pulmonary physical therapy evidence and practice, ed 4, St Louis: Mosby, 2005.
95 Williams PL, Warwick R, Dyson M, et al. Gray’s anatomy, ed 37. New York: Churchill Livingstone; 1989.
96 From Oatis CA. Kinesiology: the mechanics & pathomechanics of human movement, ed 2. Philadelphia: Lippincott Williams & Williams; 2009.
97 Mannion AF, Dumas GA, Cooper RG, et al. Muscle fibre size and type distribution in thoracic and lumbar regions of erector spinae in healthy subjects without low back pain: normal values and sex differences. J Anat. 1997;190:505-513.
98 Lee DG. The thorax: an integrated approach, ed 2. Orthopedic Physical Therapy Products; 2003.
99 Lee LJ, Coppieters MW, Hodges PW. Anticipatory postural adjustments to arm movement reveal complex control of paraspinal muscles in the thorax. J Electromyogr Kinesiol. 2009;19(1):46-54.
100 Hodges PW, Richardson CA. Relationship between limb movement speed and associated contraction of the trunk muscles. Ergonomics. 1997;40(11):1220-1230.
101 Briggs AM, Greig AM, Wark JD, et al. A review of anatomical and mechanical factors affecting vertebral body integrity. Int J Med Sci. 2004;1(3):170-180.
102 Moseley GL, Hodges PW, Gandevia SC. Deep and superficial fibers of the lumbar multifidus muscle are differentially active during voluntary arm movements. Spine. 2002;27(2):E29-E36.
103 Phillips S, Mercer S, Bogduk N. Anatomy and biomechanics of quadratus lumborum. Proceedings of the Institution of Mechanical Engineers. Part H. J Engineer Med. 2008;222(2):151-159.
104 Porterfield JA, DeRosa C. Mechanical low back pain: perspectives in functional anatomy. Philadelphia: Saunders; 1991.
105 McGill SM. A revised anatomical model of the abdominal musculature for torso flexion efforts. J Biomech. 1996;29(7):973-977.
106 Moll JM, Wright V. An objective clinical study of chest expansion. Ann Rheum Dis. 1972;31(1):1-8.
107 Estenne M, Yernault JC, De Troyer A. Rib cage and diaphragm-abdomen compliance in humans: effects of age and posture. J Appl Physiol. 1985;59(6):1842-1848.
108 Jull GA, Richardson CA. Motor control problems in patients with spinal pain: a new direction for therapeutic exercise. J Manipulative Physiol Ther. 2000;23(2):115-117.
109 Hodges PW, Richardson CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. J Spinal Disord. 1998;11(1):46-56.
110 Hodges PW, Richardson CA. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehabil. 1999;80(9):1005-1012.
110a Grenier SC, McGill SM. Quantification of lumbar stability by using two different abdominal activation strategies. Arch Phys Med Rehabil. 2007;88(1):54-62.
111 McGill S. Low back disorders: evidence-based prevention and rehabilitation. Champaign, IL: Human Kinetics Publishers; 2002.
112 Brown SH, McGill SM. How the inherent stiffness of the in vivo human trunk varies with changing magnitudes of muscular activation. Clin Biomech. 2008;23(1):15-22.
113 Hodges PW. Core stability exercise in chronic low back pain. Orthop Clin North Am. 2003;34(2):245-254.
114 Cresswell AG, Grundstrom H, Thorstensson A. Observations on intra-abdominal pressure and patterns of abdominal intra-muscular activity in man. Acta Physiologica Scand. 1992;144(4):409-418.
115 Urquhart DM, Hodges PW. Differential activity of regions of transverses abdominis during trunk rotation. Eur Spin J. 2005;14:393-400.
116 Urquhart DM, Barker PJ, Hodges PW, et al. Regional morphology of the transversus abdominis and obliquus internus and externus abdominis muscles. Clin Biomech. 2005;20:233-241.
117 Urquhart DM, Hodges PW, Story IH. Postural activity of the abdominal muscles varies between regions of these muscles and between body positions. Gait Posture. 2005;22(4):295-301.
118 Hodges PW, Richardson CA. Transversus abdominis and the superficial abdominal muscles are controlled independently in a postural task. Neurosci Lett. 1999;265(2):91-94.
119 Hodges PW, Cresswell AG, Daggfeldt K, et al. Three dimensional preparatory trunk motion precedes asymmetrical upper limb movement. Gait Posture. 2000;11(2):92-101.
120 Urquhart DM, Hodges PW, Allen TJ, et al. Abdominal muscle recruitment during a range of voluntary exercises. Man Ther. 2005;10(2):144-153.
121 Andersson EA, Grundstrom H, Thorstensson A. Diverging intramuscular activity patterns in back and abdominal muscles during trunk rotation. Spine. 2002;27(6):E152-E160.
122 Parfrey KC, Docherty D, Workman RC, et al. The effects of different sit- and curl-up positions on activation of abdominal and hip flexor musculature. Appl Physiol Nutr Metabol. 2008;33(5):888-895.
123 Bird M, Fletcher KM, Koch AJ. Electromyographic comparison of the ab-slide and crunch exercises. J Strength Conditioning Res. 1920;2:436-440.
124 Lehman GJ, McGill SM. Quantification of the differences in electromyographic activity magnitude between the upper and lower portions of the rectus abdominis muscle during selected trunk exercises. Phys Ther. 2001;81(5):1096-1101.
125 Fitting JW. Clinical significance of abnormal rib cage abdominal motion. Eur Respir J. 1988;1(6):495-497.
126 Whitelaw MA, Markham DR. Patterns of intercostal muscle activity in humans. J Appl Physiol. 1989;67(5):2087-2094.
127 Dimarco AF, Romaniuk JR, Supinski GS. Action of the intercostal muscles on the rib cage. Respir Physiol. 1990;82(3):295-306.
128 De Troyer A, Kirkwood PA, Wilson TA. Respiratory action of the intercostal muscles. Physiol Rev. 2005;85(2):717-756.
129 Whitelaw WA, Ford GT, Rimmer KP, et al. Intercostal muscles are used during rotation of the thorax in humans. J Appl Physiol. 1992;72(5):1940-1944.
130 Cloward RB. Cervical diskography. A contribution to the etiology and mechanism of neck, shoulder and arm pain. Ann Surg. 1959;150:1052-1064.
131 Abbott J. Pelvic pain: Lessons from anatomy and physiology. J Emerg Med. 1990;8(4):441-447.
132 Howard FM, El-Minawi AM, Sanchez RA. Conscious pain mapping by laparoscopy in women with chronic pelvic pain. Obstet Gynecol. 2000;96(6):934-939.
133 Deep K, Bhalaik V. Pain as a presenting feature of acute abdomen in spinal injuries. Injury. 2003;34(1):33-34.
134 Lum-Hee N, Abdulla AJ. Slipping rib syndrome: an overlooked cause of chest and abdominal pain. Int J Clin Pract. 1997;51(4):252-253.
135 Goodman CC, Snyder TK. Differential diagnosis for physical therapists: screening for referral, ed 4. St Louis: Saunders Elsevier; 2007.
136 Bruckner FE, Greco A, Leung AW. ‘Benign thoracic pain’ syndrome: role of magnetic resonance imaging in the detection and localization of thoracic disc disease. J Royal Soc Med. 1989;82(2):81-83.
137 Fruth SJ. Differential diagnosis and treatment in a patient with posterior upper thoracic pain. Phys Ther. 2006;86(2):254-268.
138 Nicholas JJ, Christy WC. Spinal pain made worse by recumbency: a clue to spinal cord tumors. Arch Phys Med Rehabil. 1986;67(9):598-600.
139 Saha E, Dziadzio M, Irving K, et al. Unusual cause of painful shoulder in an elderly woman with rheumatoid arthritis. Clin Rheumatol. 2007;26(9):1549-1551.
140 Cortet B, Roches E, Logier R, et al. Evaluation of spinal curvatures after a recent osteoporotic vertebral fracture. Joint Bone Spine. 2002;69(2):201-208.
141 Sutherland CJ, Miller F, Wang GJ. Early progressive kyphosis following compression fractures. Two case reports from a series of “stable” thoracolumbar compression fractures. Clin Orthop Relat Res. 1983;173:216-220.
142 Wong-Chung JK, Naseeb SA, Kaneker SG, et al. Anterior disc protrusion as a cause for abdominal symptoms in childhood discitis. A case report. Spine. 1999;24(9):918-920.
143 Moayyeri A, Luben RN, Bingham SA, et al. Measured height loss predicts fractures in middle-aged and older men and women: the EPIC-Norfolk prospective population study. J Bone Miner Res. 2008;23(3):425-432.
144 Gunnes M, Lehmann EH, Mellstrom D, et al. The relationship between anthropometric measurements and fractures in women. Bone. 1996;19(4):407-413.
145 Eggertsen R, Mellstrom D. Height loss in women caused by vertebral fractures and osteoporosis. Ups J Med Sci. 2007;112(2):213-219.
146 Arroyo JF, Vine R, Reynaud C, et al. Geriatrics advisor. Slipping rib syndrome: don’t be fooled. Geriatrics. 1995;50(3):46-49.
147 Meuwly JY, Wicky S, Schnyder P, et al. Slipping rib syndrome: a place for sonography in the diagnosis of a frequently overlooked cause of abdominal or low thoracic pain. J Ultrasound Med. 2002;21(3):339-343.
148 Porter GE. Slipping rib syndrome: an infrequently recognized entity in children: a report of three cases and review of the literature. Pediatrics. 1985;76(5):810-813.
149 Sinaki M, Grubbs NC. Back strengthening exercises: quantitative evaluation of their efficacy for women aged 40 to 65 years. Arch Phys Med Rehabil. 1989;70(1):16-20.
150 Sinaki M, Wahner HW, Bergstralh EJ, et al. Three-year controlled, randomized trial of the effect of dose-specified loading and strengthening exercises on bone mineral density of spine and femur in nonathletic, physically active women. Bone. 1996;19(3):233-244.
151 Sinaki M, Itoi E, Wahner HW, et al. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone. 2002;30(6):836-841.
152 Hongo M, Itoi E, Sinaki M, et al. Effect of low-intensity back exercise on quality of life and back extensor strength in patients with osteoporosis: a randomized controlled trial. Osteoporos Int. 2007;18(10):1389-1395.
153 Straker LM, O’Sullivan PB, Smith AJ, et al. Relationships between prolonged neck/shoulder pain and sitting spinal posture in male and female adolescents. Man Ther. 2008;14(3):321-329.
154 Straker LM, O’Sullivan PB, Smith AJ, et al. Sitting spinal posture in adolescents differs between genders, but is not clearly related to neck/shoulder pain: an observational study. Aust J Physiother. 2008;54(2):127-133.
155 Kebaetse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80(8):945-950.
156 Wolff I, van Croonenborg JJ, Kemper HC, et al. The effect of exercise training programs on bone mass: a meta-analysis of published controlled trials in pre- and postmenopausal women. Osteoporos Int. 1999;9(1):1-12.
157 Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine. 1996;21(22):2640-2650.
158 Ozgocmen S, Cimen OB, Ardicoglu O. Relationship between chest expansion and respiratory muscle strength in patients with primary fibromyalgia. Clin Rheumatol. 2002;21(1):19-22.
159 Bogduk N. Innervation and pain patterns of the thoracic spine. In Grant R, editor: Physical therapy of the cervical and thoracic spine, ed 3, New York: Churchill Livingstone, 2002.