Work Evaluation and Work Programs
History of occupational therapy involvement in work programs
Role of the occupational therapist in work programs
Functional capacity evaluation
Work hardening/work conditioning
Empowering corporate clients: the injury prevention team
Training in risk factor identification/ergonomic evaluation and problem solving
After studying this chapter, the student or practitioner will be able to do the following:
1 Understand the role of occupational therapy in the development of work programs.
2 Describe the different types of work evaluation and work programs that are currently being practiced.
3 Identify the components of an industrial rehabilitation program.
4 Understand the difference between work hardening and work conditioning.
5 Identify the aspects of a well-designed functional capacity evaluation.
6 Explain the importance of reliability and validity in the context of evaluation.
7 Understand the differences between job demands analysis, ergonomic evaluation/hazard identification, and worksite evaluation.
8 Discuss the application of job demands analysis.
9 Discuss basic ergonomic interventions.
10 Describe the components of injury prevention programs.
11 Describe school-to-work transition services.
History of Occupational Therapy Involvement in Work Programs
The therapeutic use of work has always been a core tenet of occupational therapy since the inception of the profession.32 Work programs have their roots in those with mental illness during the moral treatment movement, which started in Europe in the late 18th and early 19th centuries.77 In 1801, Philippe Pinel, one of the founders of moral treatment, first introduced work treatment in the Bicentre Asylum for the Insane. He suggested that “prescribed physical exercises and manual occupations should be employed in all mental hospitals. … Rigorously executed manual labor is the best method of securing good morale. … The return of convalescent patients to their previous interests, to industriousness and perseverance have always been for me the best omen of a final recovery.”80 Later in the 1800s, several psychiatric settings instituted productive activity programs.
In 1914, George Barton, one of the founding fathers of the occupational therapy profession who was disabled by tuberculosis and a foot amputation, established the Consolation House in New York.89 This program enabled convalescents to use occupations to return to productive living.89 Barton stated, “the purpose of work was to divert the mind, exercise the body, and relieve the monotony and boredom of illness.”83
In 1915, Eleanor Clarke Slagle, another founder of the occupational therapy profession, was hired to create a program for persons with mental or physical disabilities to work and become self-sufficient.89 The program was located at Hull House, a settlement house in Chicago, and was funded by philanthropic contributions. The participants involved in the program produced goods such as baskets, needlework, toys, rugs, and cabinets while developing manual skills and receiving wages for their work.
The early leaders of occupational therapy identified the importance of work when defining the profession’s focus and purpose. Adolph Meyer, a psychiatrist who emigrated from Germany at the time and was an early proponent of moral treatment, observed that healthy living involved a “blending of work and pleasure.”61 Dr. Herbert Hall helped establish a medical workshop at Massachusetts General Hospital in Boston, where clients were involved in “work cure.”30 In this workshop, clients produced marketable goods and received a share of the profits. The focus of treatment in these curative workshops was to restore the impaired body part to as normal function as possible, with the goal of returning the client to work.
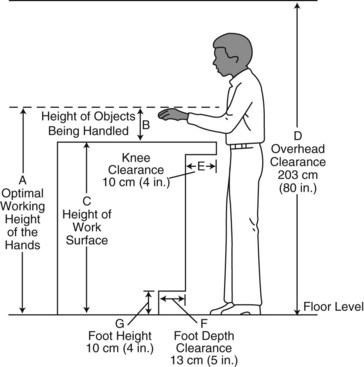
While this curative workshop movement was transpiring on the East Coast, similar programs were developing elsewhere in the United States. For example, at the Los Angeles County Poor Farm, now recognized as Rancho Los Amigos National Rehabilitation Center in Downey, California, “all inmates were requested to do an amount of work that was commensurate with their physical strength and mental capacity, which was determined by the admitting doctor.”27 Inmates used woodworking machinery to build a large amount of furniture that was used at the farm. Commodes, bedside tables, wheelchair tables, park benches, cabinets, and other items were built in the shops. In later years when there was a true occupational therapy department, patients made Navajo-type rugs, rag or braided rugs, brushes, shawls, pottery, pictures, baskets, and leatherwork (Figure 14-1, A). Patients took special occupational therapy classes “which were designed to enable those who are crippled, blinded or otherwise handicapped to make themselves useful” by producing articles that could be used at the County Farm or sold to employees or the California Crafts and Industries Society in Los Angeles (Figure 14-1, B).27
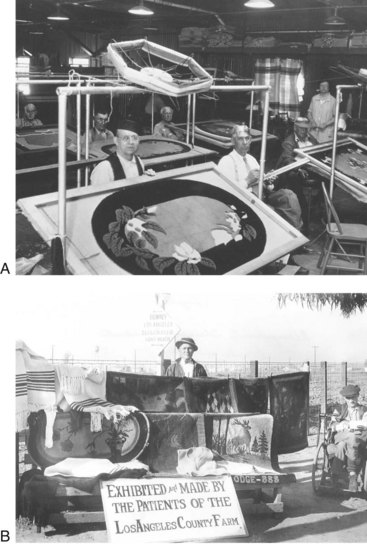
FIGURE 14-1 A, Patients at work weaving rugs in the occupational therapy shop at the Los Angeles (LA) County Poor Farm. B, Patients with a display of their products made at the LA County Poor Farm. (From Fliedner CA: Occupational therapy: for the body and the mind. In Rodgers GM, editor: Centennial Rancho Los Amigos Medical Center 1888-1988, Downey, Calif, 1990, Rancho Los Amigos Medical Center.)
In the early 1900s, the medical profession did not seem to consider vocational readiness programs to be important. The focus of care for persons with physical illnesses was primarily palliative and involved immobilization and bed rest. This attitude shifted after World War I with the need to rehabilitate the large numbers of injured soldiers to help them become functional and gain employment.
The U.S. Federal Board for Vocational Education (FBVE) was created after adoption of the Vocational Education Act of 1917.42 In 1918, the Division of Orthopaedic Surgery in the Medical Department of the Army organized a reconstruction program for disabled soldiers.77 One of the founders of occupational therapy, Thomas Kidner, served as an advisor. This program led to the development of reconstruction aides, who were the precursors to occupational and physical therapists. Treatment involved both handicrafts and vocational education. The reconstruction aides used work activities to return the injured soldiers to military duty or civilian life to the highest degree possible.
In 1920, Congress passed the Civilian Rehabilitation Act of 1920 (Smith-Fess Act, Public Law 66-236). This law provided funds for vocational guidance and training, work adjustment, prostheses, and placement services.42 If therapy was part of a medical treatment program, the law provided payment for occupational therapy services; however, it did not provide payment for physician services. Physicians either provided free services or received payment through state or volunteer contributions. This limited the use of occupational therapy services in vocational rehabilitation to the states that supplemented federal program funds to support services such as the curative workshops.
The Social Security Act of 1935 defined rehabilitation as “the rendering of a person disabled fit to engage in a remunerative occupation.”53 This was the first attempt to provide vocational rehabilitation to the physically handicapped in the community.
In 1937, industrial therapy, called employment therapy, was born.58 The occupational therapist used activities as treatment modalities. It was common for patients to have work assignments in the hospital that matched their experience, aptitude, and interest. Sheltered work environments within the hospital were used, including the hospital laundry, barber shop, and carpenter shop.
The term prevocational started appearing in the literature by the late 1930s. It referred to the use of crafts to develop skills readily transferable to industry.101 Prevocational therapy prepared patients for the work role. Occupational therapists worked as directors, work evaluators, and prevocational therapists in work programs. In the 1940s, prevocational programs and work evaluation were accepted as part of the practice of occupational therapy. Patients in acute care facilities who were physically disabled were transferred to outpatient or rehabilitation prevocational and vocational programs.
World War II brought more opportunities for occupational therapists to become involved in work programs. With the advancement of medicine and pharmacology, many injured soldiers survived their wounds. Federal funding for rehabilitating disabled veterans increased as the government discharged the disabled soldiers. This led to an increase in the development of work programs designed to evaluate and rehabilitate injured veterans.17
In 1943, the Barden-LaFollette Act (Public Law 78-113) modified the original provisions of the Civilian Rehabilitation Act of 1920.42 This new law, called the Vocational Rehabilitation Act, covered many medical services, including occupational therapy and vocational guidance. Services were expanded to those with physical and mental limitations. This law also created the Office of Vocational Rehabilitation, a state and federally funded agency that is still in existence today and provides job training and placement services to people with disabilities. Industrial therapy continued in various settings as a form of vocational rehabilitation.
During the 1950s, many occupational therapists believed that work evaluation belonged to a newly established profession of vocational rehabilitation rather than occupational therapy.58 Occupational therapy involvement declined, and vocational counselors, vocational evaluators, and work adjusters were primarily the leaders in this field. There were, however, still a few occupational therapists who remained active in work programming.
A high point in the development of prevocational exploration and training techniques in the field of occupational therapy occurred in 1960.42 Rosenberg and Wellerson published an article on development of the TOWER (Testing, Orientation, and Work Evaluation in Rehabilitation) system in New York.84 The TOWER system was one of the first work sample programs to use real job samples in a simulated work environment.84 In 1959, Lilian S. Wegg gave the Eleanor Clarke Slagle Lecture on “Essentials of Work Evaluation” based on her experiences at the May T. Morrison Center for Rehabilitation in San Francisco. Wegg promoted the need for both sound testing procedures and training programs.100 Florence S. Cromwell, a president of the American Occupational Therapy Association (AOTA), established norms for disabled populations on certain prevocational tests while evaluating the performance of adults with cerebral palsy at the United Cerebral Palsy Organization.42 Cromwell continued to be an important advocate of work-related therapy in the ensuing decades.
Occupational behavioral theory, which emerged in the mid-1960s and early 1970s, offered a return to the profession’s concern for occupation. Mary Reilly, an early proponent of occupational behavior theory and a 1962 Eleanor Clark Slagle lecturer, believed that productive activity as treatment was the unique contribution of occupational therapy.42 Occupational behavior theory advocated that persons can achieve healthy living only through a balance between work, rest, and play.
The increasing numbers of industries in the late 1970s and early 1980s introduced a whole new arena for occupational therapists: industrial rehabilitation and work hardening.42 Work hardening used actual work tasks in a simulated structured work environment, generally in community-based settings.5 Occupational therapists used their knowledge of neuromuscular characteristics, including range of motion (ROM) and endurance, along with task analysis skills and knowledge of the psychosocial aspects of work in evaluating, planning, and implementing a work-hardening program.
In 1989, the Commission on Accreditation of Rehabilitation Facilities (CARF) developed work-hardening standards requiring an interdisciplinary approach.15 The interdisciplinary team consisted of occupational therapists, physical therapists, psychologists, and vocational specialists.
The Americans With Disabilities Act of 1990 (ADA; Public Law 101-336) was important legislation that opened major markets for occupational therapists.42 Occupational therapists were involved in providing both work training for persons with disabilities and assistance to employers in meeting the requirements of the ADA. This legislation continues to have important implications for work practice.23 (See Chapter 15 for more information on the ADA.)
In 1992, the AOTA defined work as “all productive activities and included life roles such as homemaker, employee, volunteer, student, or hobbyist.”4 This document was replaced in 2000 by the statement “Occupational Therapy Services in Facilitating Work Performance.” This statement asserts that “occupational therapists and occupational therapy assistants contribute to the delivery of services for the promotion and management of productive occupations as well as the prevention and treatment of work-related disability.”2
In 2002, the Occupational Safety and Health Administration (OSHA) unveiled a comprehensive approach to ergonomics to reduce the incidence of musculoskeletal disorders (MSDs) in the workplace. Their four-pronged, comprehensive approach includes guidelines, enforcement, outreach and assistance, and a national advisory committee on ergonomics.
Occupational therapists have traditionally consulted and continue to consult with employers and employees on making recommendations about equipment, posture, and body mechanics to prevent injuries. Ergonomic intervention continues to be an area of many opportunities for occupational therapists who have received additional training and education in the area of ergonomics.
Role of the Occupational Therapist in Work Programs
Occupational therapists and occupational therapy assistants play an important role in helping individuals participate in all aspects of work. According to the Occupational Therapy Practice Framework: Domain and Process, second edition, work is an area of occupation that is defined by Mosey as “activities needed for engaging in remunerative employment or volunteer activities,” including the following: “employment interests and pursuits, employment seeking and acquisition, job performance, retirement preparation and adjustment, volunteer exploration, and volunteer participation.”1 Occupational therapy practitioners provide services to those with limitations in the area of work performance. The occupational therapist focuses on identifying and analyzing the problem and selecting and/or designing appropriate assessments and interventions for solution of the problem. According to the statement “Occupational Therapy Services in Facilitating Work Performance,” “problems in work performance can arise from physical, sensory, cognitive, perceptual, psychological, social, or developmental changes. Therefore, occupational therapy practitioners provide work-related services in a variety of settings, including, but not limited to, acute care and rehabilitation facilities, industrial sites, and office environments, psychiatric treatment centers and in the community.” Two key services are provided in these settings, “evaluation and intervention, which includes consultative, preventive, restorative, and compensatory services.”2 This chapter describes the range of work evaluations and interventions in which occupational therapists are involved in assisting people in actively participating in meaningful work roles.
Industrial Rehabilitation
The range of services provided to injured workers and industry is often encompassed by the terms “industrial” or “occupational rehabilitation.” These terms will be used interchangeably in this chapter. Industrial rehabilitation includes functional capacity evaluation (FCE), vocational evaluation, job demands analysis (JDA), worksite evaluation, pre-employment screening, work hardening/conditioning, on-site rehabilitation, modified/transitional employment, education, ergonomics, wellness, and preventive services. Occupational therapists are integral in providing these services, and this area of practice provides a tangible way for therapists to experience the tremendous reward of seeing lives changed through their efforts. The AOTA has developed a Work and Industry Special Interest Section (WISIS) for those who are involved in or wish to know more about this area of specialization.
Functional Capacity Evaluation
An FCE is an objective assessment of an individual’s ability to perform work-related activity.28,52 These functionally based tests have been used since the early 1970s to assist in making return-to-work decisions and were primarily performed by occupational and physical therapists.38 Today, however, the results of such an evaluation can be used in many different ways and they are performed by a multitude of disciplines. Occupational therapists are remarkably qualified to conduct FCEs because of their education and background in task analysis.2,3 An FCE can be used to set goals for rehabilitation and readiness for return to work, assess residual work capacity, determine disability status, and screen for physical compatibility before hiring a new employee and case closure.75
An FCE usually consists of a review of medical records, an interview, musculoskeletal screening, evaluation of physical performance, formation of recommendations, and generation of a report.45 Evaluation of physical performance usually takes the form of assessing the client’s physiology, both cardiovascular and muscular endurance, during the course of strength, static, and dynamic tasks. The report usually contains information regarding the overall level of work, tolerance for work over the course of a day, individual task scores, job match information, level of client participation (cooperative or self-limited), and interventions for consideration.45,50
A wide variety of FCEs are currently used in practice today, both commercially available systems and evaluations developed by individual therapists or clinics (Box 14-1, Figure 14-2).
FCEs can be (1) all-inclusive when looking at case closure or settlement; (2) job specific when making a match between a person’s abilities and the job description, such as “cashier at XYZ store” or a broader occupational title such as “cashier”; or (3) injury specific, such as an upper extremity evaluation after bilateral carpal tunnel release. Joe, the 26-year-old man with T11 paraplegia, could benefit from a job-specific FCE to determine whether he can meet the physical demands of the alternative job as a laundry attendant.
A well-designed FCE is comprehensive, standardized, practical, objective, reliable, and valid.45,50,86
A comprehensive FCE will include all of the physical demands of work as defined by the Dictionary of Occupational Titles (DOT) published by the U.S. Department of Labor and last revised in 1991 (Box 14-2).97 The main focus of Joe’s FCE will be on the physical demands of work that he can still reasonably do from the wheelchair, such as lifting, sitting, carrying, pushing, pulling, balancing, reaching, handling, fingering, feeling, talking, hearing, and seeing.
It is also important for the individual being tested to understand the correlation between the test items and the functions of the job. The application of meaningful activity can improve individuals’ cooperation during testing and encourage maximum effort. For example, an individual who performs secretarial duties may have difficulty understanding the need to test her ability to climb ladders if she does not actually perform this function during the course of her job.1,75
An FCE needs to be practical in terms of length of testing, cost, space, and report generation.50,75
Standardization in FCEs means having a procedure manual, task definitions and instructions, a scoring methodology, and equipment requirements and set-up.50,52,76 This type of structure helps ensure that individuals are being assessed in a fair and consistent manner and demonstrates the effort to minimize observer bias. Verbal instructions are critical in establishing rapport between the evaluator and the individual being tested. During the initial interview, the tone is set for the course of the evaluation, and the individual’s trust in the evaluator is implicit in maximizing cooperation and effort during the evaluation.50 Objectivity is not limited to weights, distances, heights, or some other numeric quantity; subjective measures can be made objective with operational definitions. Objectivity during the course of an FCE does not exclude clinical judgment and decision making, but it does require the measure to be as free as possible of examiner bias.86 This includes physical performance, as well as client cooperation during testing. Objectivity is accomplished through standardization of the testing protocol and a structured scoring methodology.
The most important aspects of an FCE are reliability and validity of the testing protocol. Two types of reliability are deemed to be important in an FCE: interrater and test-retest reliability.52 Interrater reliability in an FCE means consistency; if two therapists administer the same test to the same client, will they get the same results?45 King and Barrett state that “test-retest reliability or intra-rater reliability refers to the stability of a score derived from one administration of an FCE to another when administered by the same rater.”45 Being able to establish reliability is the first step in determining the validity or accuracy of the results.86 If there is not agreement between evaluators, it is difficult to determine whose results are correct.45 Once reliability has been proved, validity can be assessed. The term validity is used in many ways, often with significance placed on issues surrounding sincerity of effort. In scientific terms, validity means accuracy; in other words, does the FCE provide results that truly describe how the client can perform at work?50,86
There are several types of validity, with content, criterion (both concurrent and predictive), and construct validity having the most impact on the results of an FCE.45,50 Content validity is the easiest to establish in an FCE because this measure refers to whether the evaluation tests the physical demands of work, as defined by a panel of experts, by job analysis, or by a recognized document such as the DOT.50,52,75,97
Criterion validity refers to whether conclusions can be drawn from the measures taken, and in an FCE this refers to whether a person can actually perform at the level demonstrated during testing.45,50,52 Criterion validity is often determined by comparing the methodology in question with a “gold standard”—another instrument that has been proved to be reliable and valid.45,50,52 This is difficult to do in an FCE because there are a limited number of available assessments with proven reliability and validity to compare against and because other methods, such as comparing the person’s tested ability with the actual work level, can be seriously flawed.50,52,56 Criterion validity includes concurrent and predictive validity.
Concurrent validity refers to the ability of a test to measure existing abilities, and in an FCE this would be demonstrated by the test’s ability to determine which clients can perform at a given level and which clients cannot perform at a given level.45,50,52
Predictive validity is indicated by the test’s capacity to predict future ability and has great value in an FCE by determining who can safely return to work and remain without injury.45,50,59 The first FCE to be studied for validity and published in peer-reviewed literature was developed by the occupational therapist Susan Smith and has served as an important contribution to the knowledge base.92 Without reliability and validity, a referral source cannot know whether the results of the evaluation would vary if the individual were tested by another therapist or whether the results are accurate.45,50,52
Vocational Evaluations
Work evaluations, or vocational evaluations, are “a comprehensive process that systematically uses work, real or simulated, as the focal point for vocational assessment and exploration to assist individuals in their vocational development.”25 According to CARF, the following factors are addressed in the traditional vocational evaluation model: physical and psychomotor capacities; intellectual capacities; emotional stability; interests, attitudes, and knowledge of occupational information; aptitudes and achievements (vocational and educational); work skills and work tolerances; work habits; work-related capabilities; and job-seeking skills.35 These assessments can last from 3 to 10 consecutive days, depending on the goals of the assessment. Vocational evaluators generally conduct these types of assessments in private vocational agencies; however, some occupational therapists have been involved in conducting these evaluations in public and private medical or nonmedical settings as well. Vocational rehabilitation, worker’s compensation, and long-term disability carriers pay for these services, but most medical plans do not.
Standardized work samples such as the Valpar Component Work Sample System or the Jewish Employment Vocational Services are used to assess specific skills in the areas of data or things (Figure 14-3). Dexterity tests such as the Bennett Hand Tool, Crawford Small Parts, and Purdue Pegboard are used to evaluate motor skills (Figure 14-4).35 When no standardized work samples are available to assess the specific skills needed for a particular occupation, specially designed situational assessments are also used to create real-life work situations that are related to actual work tasks that would be conducted on particular jobs. For example, a person who is interested in working as a floral arranger could have her motor skills evaluated to see whether she has the coordination, energy, and strength and effort to grip and manipulate tools to cut the stems of flowers and plants and arrange them in floral containers. Individuals can also be evaluated in real worksites and perform actual job tasks that one would perform on the job.

FIGURE 14-3 A, Valpar and JEVS work samples. B, Valpar 9 Total Body Range of Motion work sample, which is used to evaluate functional abilities such as standing, bending, crouching, reaching, and gross manipulation and handling. C, The Valpar 10 Tri-Level Measurement is used to evaluate a person’s ability to follow a multistep sequence to inspect metal parts with various jigs and tools.
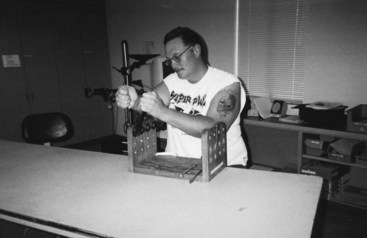
FIGURE 14-4 The Bennett Hand Tool is a dexterity test to assess a person’s ability to use hand tools.
There are generally two different types of vocational evaluation: a general vocational evaluation and a specific vocational evaluation. A general vocational evaluation is a comprehensive assessment to evaluate a person’s potential to do any type of work. For an individual who has never worked, does not have a job to return to, or cannot return to the previous job because of a disability, this type of evaluation is beneficial in determining one’s aptitudes, abilities, and interests to explore all reasonable options for work. For example, Henry, the roofer who experienced a traumatic brain injury from a fall while working, could benefit most from a general vocational evaluation to explore other options for employment. A general vocational evaluation could help identify other vocational interests and abilities by exploring a person’s cognitive and motor skills and physical and mental tolerances that could be applied to a different occupation. A specific vocational evaluation assesses a person’s readiness to return to a particular occupation. For a person who has suffered a stroke and wants to return to work as a general office clerk, a specifically tailored vocational evaluation to assess the person’s ability to return to this particular type of work can be done. Clerical work samples and specially designed situational assessments that gauge the person’s ability to multitask, pay attention to detail, file, answer a telephone, and take messages can be incorporated as an integral component of the vocational evaluation.
Job Demands Analysis
Assessing the physical demands of a job by JDA is often beneficial in the rehabilitation process inasmuch as recommendations for initiation or return to work require objective information about both the client’s abilities and the job itself. A well-written job description that includes the essential tasks of the job, physical requirements, cognitive aptitudes, educational requirements, equipment operated, and environmental exposure assists in selecting suitable candidates for employment, setting compensation packages, and making appropriate return-to-work decisions after an injury.8
A JDA does not need to be confused with ergonomic evaluations or identification and abatement of hazards. A JDA seeks to define the actual demands of the job, whereas ergonomic evaluations and hazard assessment focus more on work practice and risk for injury secondary to postural or manual material-handling extremes or excesses.7 Certainly, these areas can overlap, but it is important to be clear about the differences and the reasons behind the request for information and to use suitable methods for each.7
Approaches to a JDA include questionnaires, interviews, observations, and formal measurement.7 It is common to interview incumbents or supervisors about the job requirements.75 Such an informal approach often leads to narrative descriptions with little functional information and questionable accuracy of demand estimates.36,62,75 As with other types of assessment, it is important to have an objective process for analyzing the demands of the job. In the context of attempting to make return-to-work decisions based on matching the results of an FCE with the job description, many FCEs include a JDA component.50 However, these are often subjective interviews with the client and can lack accuracy regarding the physical demands.
The occupational therapist who was working with Joe contacted the employer and conducted a JDA to obtain a complete picture of the job demands and requirements of the laundry attendant position. The occupational therapist spoke to the supervisor, as well as to other employees while they were performing the actual job at the worksite. Being able to actually observe the job being done in the real work environment allowed the occupational therapist to gather the information needed to adequately assess Joe’s ability to carry out the essential functions of this job.
A standardized classification system is crucial to ensure consistency in terminology and among professionals. The DOT defines the physical demands of work and defines occupations in the United States (Tables 14-1 through 14-3).97 It provides definitions of the overall level of work, strength demands, and frequencies of the physical demands.97,98 Many countries around the world also refer to the DOT as their primary reference for generic occupational descriptions.
TABLE 14-1
Definitions for Overall Level of Work
| Level of Work | Definition |
| Sedentary | Exerting up to 10 lb of force occasionally or a negligible amount of force frequently to lift, carry, push, pull, or otherwise move objects, including the human body. Sedentary work involves sitting most of the time but may involve walking or standing for brief periods. Jobs are sedentary if walking and standing are required only occasionally but all other sedentary criteria are met |
| Light | Exerting up to 20 lb of force occasionally, up to 10 lb of force frequently, or a negligible amount of force constantly to move objects. Physical demand requirements are in excess of those for sedentary work. Even though the weight lifted may be only a negligible amount, a job should be rated light work (1) when it requires a significant degree of walking or standing, (2) when it requires sitting most of the time but entails pushing or pulling arm or leg controls, or (3) when the job requires working at a production rate pace entailing constant pushing or pulling of material even though the weight of the material is negligible. Note: The constant stress and strain of maintaining a production rate pace, especially in an industrial setting, can be and is physically demanding on a worker even though the amount of force exerted is negligible |
| Medium | Exerting 20-50 lb of force occasionally, 10-25 lb of force frequently, or greater than negligible and up to 10 lb of force constantly to move objects. Physical demand requirements are in excess of those for light work |
| Heavy | Exerting 50-100 lb of force occasionally, 25-50 lb of force frequently, or 10-20 lb of force constantly to move objects. Physical demand requirements are in excess of those for medium work |
| Very heavy | Exerting force in excess of 100 lb of force occasionally, in excess of 50 lb of force frequently, or in excess of 20 lb of force constantly to move objects. Physical demand requirements are in excess of those for heavy work |
Data compiled from US Department of Labor, Employment and Training Administration: Revised dictionary of occupational titles, vols I and II, ed 4, Washington, DC, 1991, US Government Printing Office; and US Department of Labor, Employment and Training Administration: The revised handbook for analyzing jobs, Indianapolis, Ind, 1991, JIST Works.
TABLE 14-2
Definitions of Physical Demand Frequencies
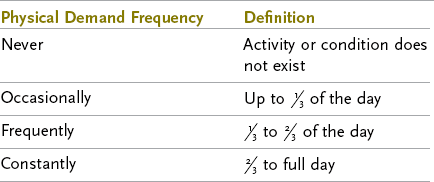
Data compiled from US Department of Labor, Employment and Training Administration: Revised dictionary of occupational titles, vols I and II, ed 4, Washington, DC, 1991; and US Government Printing Office; US Department of Labor, Employment and Training Administration: The revised handbook for analyzing jobs, Indianapolis, Ind, 1991, JIST Works.
TABLE 14-3
Strength Demands of Work: Frequency of Force Exertion or Weight Carried
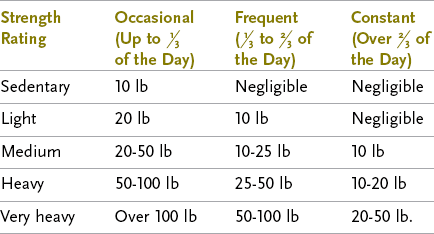
Data from US Department of Labor, Employment and Training Administration: Revised dictionary of occupational titles, vols I and II, ed 4, Washington, DC, 1991, US Government Printing Office.
The DOT was last revised in 1991, and in the early 1990s the U.S. government made the decision to not revise the DOT again but instead create a new format for classifying occupations.26 The intent was to create a more generic classification system or framework for defining work. The American Institutes of Research (AIR) was awarded a contract by the Utah Department of Employment Security on behalf of the U.S. Department of Labor, and they developed O*NET, an online, searchable database for information about occupations. Although the format includes an enormous amount of data, its definitions can make it difficult for rehabilitation professionals to use in a qualitative fashion.74 O*NET, however, is not intended to take the place of the DOT but rather to provide a more structured approach for “career exploration.”74 It is recommended that both the DOT and O*NET be consulted when obtaining occupational information.26
In terms of recent legislation that has an impact on employment law, both the ADA and the Equal Employment Opportunities Commission (EEOC) define essential tasks as being the reason that the job exists.6,7 The ADA further defines essential tasks as those that are highly specialized (i.e., the reason that the incumbent was hired to perform the job) and that there are a limited number of people available at the job site to perform the tasks.6 During the course of a JDA it is important to distinguish between tasks that are essential and those that are not. This can be challenging because it is a nontraditional way for both the employee and the employer to look at the job. It is important that both hiring and return-to-work decisions be based on job descriptions that define the essential tasks to be congruent with both the ADA and EEOC language.
Jobs are composed of the tasks that are performed, the physical demands that make up the tasks, and the frequency with which the physical demands are performed, including weights handled, forces exerted, and distances both ambulated and reached.7 The frequency of each physical demand must be weighted appropriately for the given duration of each task because there is often a significant difference in the amount of time spent on each task during the workday. For example, the job of “loader” in ABC warehouse is composed of two tasks: (1) loading crates with boxes and (2) wrapping the crate with packing tape when loaded. The loader completes 48 cycles of loading and taping in an 8-hour shift, with loading the crate taking approximately 80% of the work shift. The boxes weigh 10 lb each. To correctly assess the overall level of work, the amount of weight lifted must be determined, as well as the frequency of the manual materials handling.
Task 1 is composed of the physical demands of lifting, carrying, stooping, walking, reaching, handling, and standing. Task 2 is composed of walking, reaching, handling, fingering, and standing. To correctly sum the amount of the physical demands for the job of loader, one must determine how much time is spent on each physical demand within each task and then account for the proportion of the time that the task is performed during the workday. This type of assessment can be performed manually, as well as with the application of various software protocols available in the marketplace.
Whatever methods are selected, clinicians should strive to provide an accurate picture of the job and its requirements, with an emphasis on functional demands for easier application in the rehabilitation continuum.
Work Hardening/Work Conditioning
The idea of using work for rehabilitation is at the very core of occupational therapy. In the 1970s, the idea of occupational rehabilitation developed from the necessity of improving strategies to control work-related injuries.19,44,51,73 Work hardening was first illustrated conceptually by Leonard Matheson, a psychologist at Rancho Los Amigos who worked very closely with Linda Dempster, an occupational therapist, in developing his material.44,51,73 The goal was then and still remains rehabilitation of injured workers, maximization of their function, and returning them to work as quickly and safely as possible. The delivery system for this type of rehabilitation has evolved over time from a lengthy hospital-based program, to structured interdisciplinary programs in outpatient settings, to the more progressive partnership between outpatient intervention and transitional work, as well as to rehabilitation occurring at the workplace in company-sponsored clinics. In the 1980s, CARF developed guidelines for work-hardening programs and offered certification for a fee through adherence to their guidelines and periodic surveys.19,44,51,73 In 1991, a committee from the American Physical Therapy Association (APTA) developed another set of principles for clinics that wanted to follow recognized standards but did not desire to undertake the CARF accreditation process.19,44,51
Work hardening refers to formal, multidisciplinary programs for rehabilitating an injured worker.19,44,51,73 The disciplines represented on the team can often include occupational and physical therapists and assistants, psychologists, vocational evaluators and counselors, licensed professional counselors, addiction counselors, exercise physiologists, and dieticians.19,44,51 The programs typically range from 4 to 8 weeks and consist of an entry and exit evaluation (usually an FCE or a derivative thereof), a job site evaluation, graded activity, both work simulation and strength and cardiovascular conditioning, education, and individualized goal setting and program modification, with the goal of return to work at either full or modified duty.19,44,51 Actual equipment from the job is preferred during the work simulation to maximize cooperation of the worker and more closely replicate the actual demands of the job.44 Work conditioning is more often defined as physical conditioning alone, which covers strength, aerobic fitness, flexibility, coordination, and endurance and generally involves a single discipline.19,42,44 Both approaches involve evaluation of the worker to establish a baseline from which to plan treatment and measure progress.
Motivational issues are a constant concern and are often thought to be at the forefront of unsuccessful return to work.91 Maladaptive behavior regarding return to work can develop in an injured worker as a result of depression, financial issues, family pressures, and feelings of being manipulated by the “system.”91 This can lead to employer mistrust, interest in litigation, and a need to exaggerate symptoms. Fraud on the part of the injured worker is also an issue.91 Employer indifference is a concern and can have a remarkable impact on a worker’s attitude toward returning to the job.91 Surveys of attitudes among employers have indicated that activity on the part of the employer can affect costs; as many as 90% of respondents indicated that how well the employee perceived that he or she was treated at the time of the injury was associated with decreased costs as a result of the injury.91
Think about Lorna, the upholsterer who is experiencing hand problems, and the difficulties that she is experiencing at work. An occupational therapist could evaluate her symptoms and her job description and make suggestions to the employer about modifying her job demands so that she can continue to work during treatment. This demonstrates to Lorna that her well-being matters and can help her have a positive outcome with treatment.
Ensuring a positive outcome for the injured worker requires early intervention and a customized plan of treatment to address the various areas affected by the injury, including both physical and psychosocial.91 Incorporation of a multidisciplinary team allows the patient to have the benefit of many areas of expertise working toward his or her common good. Intervening and initiating the rehabilitation program as soon as possible following the injury dramatically increase the chance for successful return to work. Based on a study of 5620 worker’s compensation beneficiaries, there was a 47% return-to-work rate in workers referred to rehabilitation within the first 3 months after injury, with a cost savings of 71%. When referred during months 4 through 6, the rates dropped to 33% for return to work and 61% for cost savings. For those referred beyond 12 months after injury, only 18% returned to work and cost savings dropped to 51%.91
Transitional work and modified duty programs involve a combination or a progression of acute rehabilitation and return to work at a level consistent with the individual’s current ability, with the goal of returning to work at full duty or maximizing the individual’s work capacity. An example of transitional duty would have a worker performing work-conditioning activities under supervision in an outpatient clinic from 8 to 10 a.m., going to the worksite and performing the less physically demanding portions of his job from 11 a.m. to 1 p.m., breaking for lunch, and then returning to the “lighter” duties of the job for the duration of the shift. More regular duty activities are added under supervision as the worker’s skill and strength improve, with eventual return to full duty. This type of structure provides a much better environment for the worker to be involved in the work culture and allows coworkers and supervisors to participate in job modification and overall recovery of the injured worker.91 Modified duty follows a similar path but typically does not include the clinical portion of the day. There are challenges to return to work at less than full duty, however, with some employers not wanting workers to return to the site unless they are at “100%.” It is imperative to demonstrate the benefit to the company and the employee, both economically and psychologically, of early transitional return to the long-term success of returning the employee to the workforce.
Industrial rehabilitation programs will continue to change as the tides of economy, industry needs, and legislation move forward. Occupational therapists are key in directing the changes that lie ahead.
Worksite Evaluations
Worksite evaluations are on-the-job assessments to determine whether an individual can return to work after onset of a disability or whether a person can benefit from reasonable accommodations to maintain employment.41,95 For example, a man who worked at a manufacturing company as a machine operator incurs a stroke and the employer is willing to take him back as long as he can meet the physical and cognitive demands of the job. An occupational therapist can go to the worksite to evaluate the person’s ability to safely and adequately operate the machinery and carry out the essential functions of the job. Consider another example. A person who previously worked as an office clerk without any difficulty is now experiencing extreme fatigue, pain, and muscle weakness with repetitive tasks as a result of post-polio syndrome. This person could benefit from a worksite evaluation to identify reasonable accommodations to allow her to continue working at this job while minimizing her symptoms. Several factors are assessed at the worksite with the worker present: the essential functions of the job, the functional assets and limitations of the worker, and the physical environment of the workplace.55
A worksite evaluation is usually conducted after a job analysis has been done. Larger companies may already have information on job analyses done on specific jobs. If a job analysis has not been done, the occupational therapist can conduct a job analysis if the employer is willing, or a job description could be obtained from the employer before going out to the worksite. If there is no written job description, a phone call to the supervisor/manager of the worker should be made to obtain verbal information regarding the essential functions of the job and the physical and cognitive requirements for the job. After this information is obtained, the occupational therapist schedules a time with the employer and the worker to meet at the worksite. This is exactly what happened with Joe as he prepared to switch from the job of janitor to laundry attendant at the hotel and spa. After the occupational therapist conducted the job analysis, Joe met with both the occupational therapist and the employer at the worksite for the worksite evaluation.
When the occupational therapist meets the employer and worker at the worksite, the occupational therapist assesses the work, the worker, and the workplace.47 The evaluation begins with an analysis of the essential functions that may require accommodation.95 The occupational therapist should have an idea of what these functions are based on the information obtained before going to the worksite. The desired outcome of the work tasks should be emphasized, not just the process of performing the essential function.95 The occupational therapist should find out certain details, such as how the outcome will be affected if a particular task is done incorrectly, in a different sequence, or omitted; whether there are quotas, standards, or time constraints that must be met79; and whether the frequency with which a task is done will affect the outcome.
Activity analysis is a useful tool for evaluating a person at the worksite.11 It can be used to address all areas, including motor, sensory, cognitive, perceptual, emotional and behavioral, cultural, and social. When assessing a person’s ability to carry out the essential functions of the job, the occupational therapist has expertise in breaking down the tasks and determining the parts of the task with which the worker is having difficulty or may have difficulty over the course of a workday. The occupational therapist can suggest accommodations to allow the worker to carry out the essential functions of the job.
The final step in the worksite evaluation is to assess the work environment. The environment outside the immediate work area should be evaluated (parking if driving or access to public transportation; access into the building, break room, and restroom), as well as the workstation itself. All work areas that the worker may use need to be investigated to identify obstacles and solutions to increase accessibility. The location and placement of machines, supplies, and equipment that the worker needs to access should be assessed, as well as other environmental factors such as lighting, temperature, and noise level.
Taking photographs or video recordings at the worksite can be very useful; however, permission must be obtained from the employer as well as the worker to do so. The occupational therapist should also bring a tape measure to measure the height of work surfaces, width of doorways, and other factors, depending on the person’s needs. Drawing a layout of the work area to scale on graph paper is also very helpful, especially when the worker is in a wheelchair. Critical measurements can be recorded on the diagram.
The outcome of the worksite evaluation is to determine whether the person can safely and adequately carry out the essential functions of the job with or without any reasonable accommodations. Ergonomic principles (addressed in the following section) should be considered and applied when recommending reasonable accommodations. The process of identifying reasonable accommodations requires cooperation between the person with the disability, the employer, and the occupational therapist.79 Each person has valuable insights and information to contribute to the process of identifying the best accommodations. The Job Accommodation Network (JAN) is a service provided by the Office of Disability Employment Policy (ODEP) of the U.S. Department of Labor’s and is the best resource for assisting employers and disabled workers in making reasonable accommodations (http://askjan.org).87 Their Website points out that most job accommodations are not usually expensive. According to the JAN, more than half of all accommodations cost nothing. The JAN offers one-on-one guidance on workplace accommodations, the ADA, and self-employment options for people with disabilities. JAN consultants can be contacted both over the phone and online. JAN’s toll-free number is (800)526-7324. The occupational therapist analyzes the need for modification of the equipment that the worker is using or modification of the workplace to help the person perform with greater efficiency, effectiveness, and safety.5
After the worksite evaluation is completed, a report is prepared and sent to the qualified employee, the referring party, and the employer. The problem areas that relate to the essential job functions should be listed clearly, as well as the accommodations necessary to solve them. If training is necessary to use a recommended accommodation, sources for the training should be identified. If commercially available equipment is recommended, exact model numbers, local sources, and approximate expenses should be provided.95 If custom equipment needs to be fabricated, sources, cost estimates, and the amount of time required to fabricate the equipment should be included as well. The report should summarize the findings of the evaluation and the accommodations that were recommended.
After Joe’s worksite evaluation, it was determined that he could safely and dependably carry out the essential functions of the job from his wheelchair. Just one accommodation was recommended and implemented. Since it gets very hot in the laundry room and Joe is sensitive to the heat, the employer agreed to purchase additional fans to ventilate the room better, as well as allow the door to the laundry room to be propped open. The employer agreed to schedule Joe’s shift in the evening or early morning when it was cooler to avoid having to work in the heat of the day.
The occupational therapy practitioner thus evaluates the worker, the work, the workplace, and the relationship among them. Therapeutic intervention is used when deficits in performance are found. The occupational therapist can modify the way that the worker performs the work or modify the work environment to allow the worker to perform optimally.
Ergonomics
All aspects of the domain of occupational therapy must be in harmony for people to fully engage in the occupation of work. The activity demands of the job and the context in which the job is performed must fit with the employee’s abilities and physical/psychosocial makeup. Any mismatch between the activity demands of the job and context, individual client factors, and performance patterns will interfere with successful execution of the appropriate performance skills required to do the job.
Occupational therapists use the science of ergonomics to assist clients in fully engaging in the occupation of work. Ergonomics addresses human performance and well-being in relation to one’s job, equipment, tools, and environment. The goal of ergonomics is to improve the health, safety, and efficiency of both the worker and the workplace.67 The term ergonomics is derived from the Greek words ergos, meaning “work,” and nomos, meaning “laws”—hence the laws of work.20 The Polish educator and scientist Wojciech Jastrzebowski (1799-1882) introduced the term ergonomics in the literature about 150 years ago.19 However, the concept of ergonomics—that there is some connection between physical well-being and the type of work performed—is as old as humanity: “From the very first tool of the Stone Age, humans have tried to find better ways of working, taking advantage of human talents and making up for human shortcomings.”56
The idea behind ergonomics is that every worker brings his or her own unique set of performance skills, performance patterns, and client factors to the workplace. Many times work settings and work processes are designed to satisfy space and budget limitations and the demands of productivity and aesthetics. When these designs fail to take into account the people who will be using the work setting and process, injury and inefficiency can result. Finding a way to match individual employees’ strengths and limitations with the context and activity demands of a job can improve both worker safety and workplace productivity.
The principles of ergonomics help address a variety of work-related issues. Common issues include workplace and work process design, work-related stress, the disabled and aging workforces, tool and equipment design, architectural design, and accessibility. Ergonomic intervention can be applied proactively, preventing problems before they occur, or reactively, adjusting the worker-job-context “fit” when problems do occur. Many occupational therapists use ergonomic principles as part of their comprehensive rehabilitation or wellness and prevention client-centered programs. A few occupational therapists specialize in ergonomics and become professional ergonomists.
With regard to ergonomic services, the occupational therapist’s client base may include the individual worker, workers in the context of employee groups, and/or the employer itself. The environment for an occupational therapist providing ergonomic services is generally at the client’s place of work. These occupational therapists must become skilled in navigating what can be an unfamiliar business world with its unique lingo, social norms, and traditions. However, an occupational therapist providing ergonomic services shares a similar focus with occupational therapists in all areas of practice, that is, a focus on marketing and sale of the product (in ergonomics—wellness), cost-effectiveness, definable outcomes, and client satisfaction.
Occupational therapists are not the only professionals suited to specialize in the field of ergonomics. Ergonomics professionals come from a variety of backgrounds. It is not unusual to see ergonomists who have been academically trained in industrial hygiene, engineering, safety, business administration, human resources, medicine, physical/occupational rehabilitation, psychology, architecture, epidemiology, or computer science.18 For the occupational therapist, the road to becoming a professional ergonomist can take many paths. Box 14-3 outlines a variety of methods for acquiring advanced knowledge and certification in the field of ergonomics.
For occupational therapists interested in the field of ergonomics, the holistic nature of occupational therapy training is an asset. The occupational therapist immediately understands that the goal of ergonomic intervention, or achieving a perfect fit between an individual worker and his or her job and context, is never simplistic. In the domain of occupational therapy, the worker component is composed of performance skills, performance patterns, and client factors (Box 14-4). The job component is composed of activity demands, both of the job tasks and of tools/equipment. Engaging in the occupation of work occurs in a variety of contexts, including the environment and organization, as well as the worker’s personal, cultural, social, and spiritual contexts.
Observing independent aspects of the domain offers the observer limited insight. Rather, it is the interactions between the various aspects of the domain that reveal the whole picture. This way of looking at worker performance via the interactions of all aspects of the domain of occupational therapy is known as system theory. Rannell Dahl, MS, OTR, explains that the “components of work systems are workers, job tasks, tools and equipment, work environments, and organizational structure, and the interactions among these components.”18 Dahl offers an excellent schematic of this concept of the ergonomics work system (Figure 14-5).
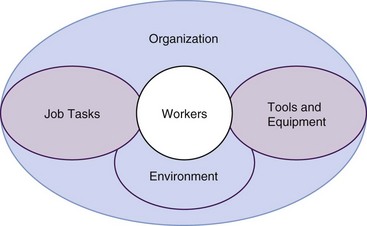
FIGURE 14-5 Dahl’s ergonomics work system. (From Dahl R: Ergonomics. In Kornblau B, Jacobs K, editors: Work: principles and practice, Bethesda, Md, 2000, American Occupational Therapy Association.)
In his groundbreaking text Conceptual Aspects of Human Factors, David Meister explained that in human factors (ergonomics), the system concept is the belief that human performance in work can be meaningfully conceptualized only in terms of organized wholes. He emphasized the fundamental Gestalt ideas that “the whole is more than the sum of its parts, that the parts cannot be understood if isolated from the whole, and that the parts are dynamically interrelated or interdependent.”59 Occupational therapists understand that one can conceive of worker performance only in terms of the interaction between performance skills, performance patterns, context, activity demands, and client factors. The Occupational Therapy Practice Framework: Domain and Process supports this concept: “Engagement in occupation as the focus of occupational therapy intervention involves addressing both subjective (emotional and psychological) and objective (physically observable) aspects of performance. Occupational therapy practitioners understand engagement from this dual and holistic perspective and address all aspects of performance when providing interventions” (p. 628).1
Occupational therapist Jeffrey Crabtree adds that it is “the subjective meaning of the interactions in the human-work-machine-environment model [that] is central to occupational therapy and ergonomics.”16
The system theory does not discount the importance of the adequacy of independent aspects of the domain of occupational therapy. The quality of the work system can suffer if there are deficiencies or deviations in performance skills, performance patterns, context, activity demands, or individual client factors. Dahl explains that each component of the ergonomics work system (see Figure 14-5) “has its own set of characteristics that affect the performance of the work system”18 as a whole. It is here that ergonomic assessment and intervention seek to make a difference in the quality of our clients’ engagement in the occupation of work. The ergonomic practitioner modifies and strengthens certain aspects of the system with the goal of enhancing the overall quality of the work system interactions (i.e., improving the fit between the worker and his or her job).
Although it is beyond the scope of this chapter to comprehensively review the complete array of ergonomic design considerations, the following is a discussion of selected ergonomic design principles. There are, however, a multitude of resources for occupational therapists interested in learning more about the science of ergonomics. The authors of this chapter direct you to the references listed at the end of the chapter. Additionally, readers may be interested in the ergonomics information available through OSHA (www.osha.gov) and NIOSH (www.cdc.gov/niosh/).
When discussing ergonomic design it is important to understand that it is the relationship between the worker and work equipment, tools, or processes that is the problem, not any particular characteristic on either side. This can be confusing to an employer who orders expensive ergonomic tools and equipment for his or her workers and is disappointed when the workers continue to suffer work-related injuries and illnesses. The specialists in ergonomics must explain to their clients that a tool or piece of equipment is never in itself ergonomic; rather, it is the fit between a particular piece of equipment, tool, or process and the intended user of that equipment, tool, or process that creates a proper ergonomic situation.
Workstations
There are three major types of workstations: seated, standing, and combination sit/stand. The type of task being performed dictates the best choice. Seated workstations are best for fine assembly and writing tasks and when all required task items can be supplied and handled within comfortable arm’s reach in the seated work space. Items handled in a seated workstation should not require hands to work more than 6 inches (15 cm) above the work space, and the items handled should not weigh more than 10 lb (4.5 kg). For this reason, the height of the work surface should be above elbow height for precision work. Standing workstations are appropriate for all kinds of work tasks but are preferred when downward force must be exerted (i.e., packaging and wrapping tasks) and when frequent movement or multilevel reaching is required around the work area. Items weighing more than 10 lb (4.5 kg) should be handled in a standing workstation. Work surface heights for heavy work should be 4 to 6 inches (10 to 15 cm) below elbow height for heavy work. The combination sit/stand workstation is best for jobs consisting of multiple tasks, some best done sitting and some best done standing.22 Figure 14-6 shows the recommended dimensions for both a seated workstation and a standing workstation.
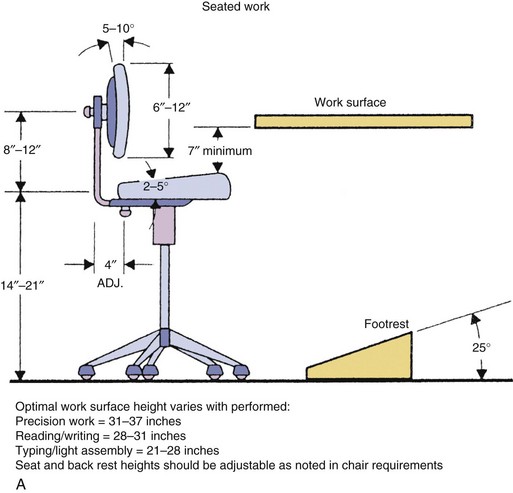
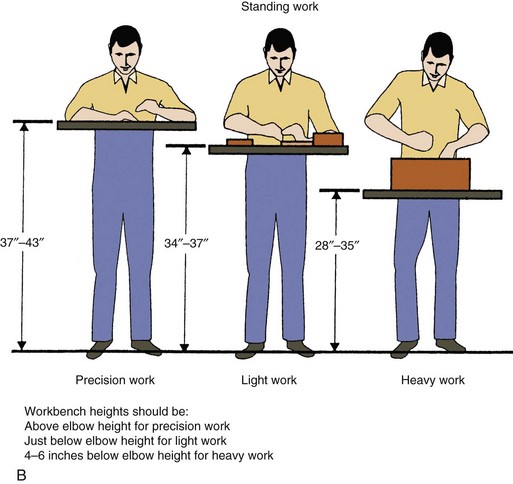
FIGURE 14-6 Recommended dimensions of workstations. A, Seated work. B, Standing work. (From Cohen AL, Gjessing CC, fine LJ, Bernard BP, McGlothlin JD: Elements of ergonomics programs: a primer based on workplace evaluations of musculoskeletal disorders, Washington, DC, 1997, US Government Printing Office.)
Seating
If seating is required, the design of the chair is of paramount importance for worker comfort and support. Poor seating leads to poor working posture. The result can be fatigue, musculoskeletal injury, and/or poor work performance. Although chair preference is highly variable among the population, there are some basic characteristics to consider. Chairs should be easily adjustable for height, backrest position, and seat pan tilt. Appropriate lumbar support is important. Seats upholstered in woven fabric are cooler and more comfortable in warmer work environments.22 Chair casters should match the flooring (i.e., hard floor versus carpet casters). A seat pan that is too deep will cut into the back of the leg and compromise lower extremity circulation. Sitting in a chair without the feet supported will also cause pressure on the back of the legs. When the worker is seated at the workstation and performing a task, both feet should be supported on the floor or a footrest. Choosing a seat pan with a front-edge “waterfall” design will also decrease pressure on the back of the legs. Armrests are an area of controversy but should generally be provided when the work task requires the arms to be held away from the body.37 Figure 14-7, A, illustrates the recommended chair characteristics for generalized seated workstations. Figure 14-7, B, illustrates a seated position for computer users.
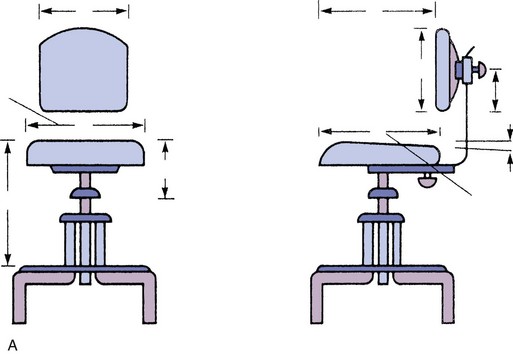
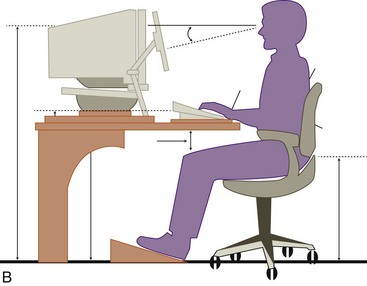
FIGURE 14-7 A, Recommended chair characteristics. Dimensions are given from both front and side views for width (A), depth (E), vertical adjustability (D), and angle (I) and for backrest width (C), height (F), and vertical (H) and horizontal (G) adjustability relative to the chair seat. The angle of the backrest should be adjustable horizontally from 12 to 17 inches (30 to 43 cm) by either a slide adjust or a spring and vertically from 7 to 10 inches (18 to 25 cm). Adjustability is needed to provide back support during different types of seated work. The seat should be adjustable within at least a 6-inch (15-cm) range. The height of the chair seat above the floor with this adjustment range will be determined by the workplace, with or without a footrest. B, Proper seated position for a computer user. (A, From Eggleton E, editor: Ergonomic design for people at work, vol 1, New York, NY, 1983, Van Nostrand Reinhold; B, from Occupational Safety and Health Administration: Working safely with video display terminals, Washington, DC, 1997, US Government Printing Office, available at: www.osha.gov/ Publications/osha3092.pdf.)
Visualizing the Job Task
Visual factors to consider are the location of task items and lighting. Again, recommendations depend on the type of task being performed. The goal is clear, direct viewing without straining the eyes or neck. Tasks should be located as directly in front of the worker as possible. Tasks requiring close-range viewing should be positioned 6 to 10 inches (15 to 25 cm) above the work surface. Minimum and maximum viewing distances depend on the size of the object being viewed. Bifocal eyeglass wearers have difficulty observing any object closer than 7 inches (18 cm) in front of the body that is above eye level or near the floor. Additionally, bifocal wearers have difficulty focusing on signs or dials located 24 to 36 inches (61 to 91 cm) in front of them.20
Three basic lighting factors need to be considered for performance of work: quantity, contrast, and glare. Lighting should be adequate for the worker to perform the job task, but not so bright that it causes discomfort. General work environment illumination is typically provided by sunlight and light fixtures at 50 to 100 foot-candles (ft-c). Computer users may find that this amount of illumination washes out the display screen and causes eyestrain. The recommended illumination level for computer workstations is 28 to 50 ft-c. Too much contrast between the task items and the surrounding areas can also stress the eyes. Therefore, the illuminance between the task items, equipment, horizontal work surface, and surrounding areas should be minimized. Finally, the color and finish of the workstation walls and equipment, as well as the arrangement of the lighting sources, should all be designed to avoid reflective glare on the job task (Figure 14-8).72
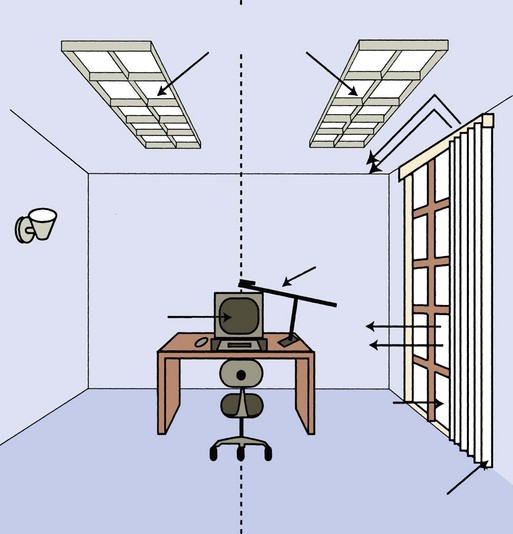
FIGURE 14-8 Lighting position considerations for computer workstations. Most of these lighting position principles can be applied to workstations in general. (From Occupational Safety and Health Administration: Working safely with video display terminals, Washington, DC, 1997, US Government Printing Office, available at: www.osha.gov/Publications/osha3092.pdf.)
Tools
Tools should be designed to protect the worker from hand vibration, extreme temperatures, and soft tissue compression. Therefore, handles on tools are essential. “A properly designed tool handle should isolate the hand from contact with the tool surface, enhance tool control and stability, and serve to increase the mechanical advantage while reducing the amount of required exertion.”81 Since the average worker’s hand is 4 inches (10 cm) across, the length of the tool handle must be at least 4 inches to avoid unnecessary pressure on the palm of the hand. Handles of scissors and pliers should be spring-loaded to avoid trauma to the back and sides of the hands.81
Tool design should minimize muscular effort and awkward posturing of the upper extremity. Whenever possible, opt for power tools to minimize the human effort required. Choose tool shapes that allow the wrist to stay straight and the elbow to stay bent and close to the body during use. The shape of the tool will depend on the job task and work surface (Figure 14-9). Tools that weigh between 10 and 15 lb (4 to 6.5 kg) cannot be held in a horizontal position more than a couple of minutes without the worker experiencing pain and fatigue. Suspension systems and counterweights should be designed for use with heavy hand tools.81
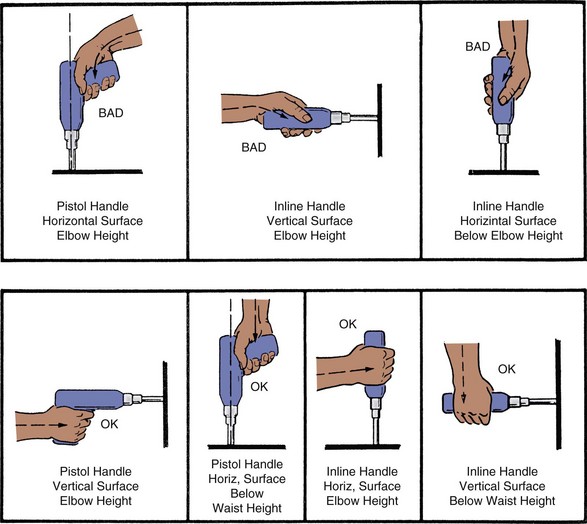
FIGURE 14-9 Hand tool design and wrist posture. (From Armstrong T: An ergonomic guide to carpal tunnel syndrome, Akron, Ohio, 1983, American Industrial Hygiene Association.)
Whole-body vibration can cause back pain and performance problems when the workstation vibrates, as in the case of long-distance truck drivers and in production industries using high-powered drills or saws in the work area.14 Hand-arm vibration has been linked to vascular compromise, peripheral nerve damage, muscular fatigue, bone cysts, and central nervous system disturbances.29 The effects of hand tool vibration should be minimized as much as possible. Use antivibration tools at low speeds when available. Ensure that tool handles and gloves fit the workers’ hands. Train workers to grip tool handles as lightly as possible and allow the tool to do all the work instead of the worker adding force behind the tool. Encourage frequent rest breaks and educate workers that smoking increases the risk for vibration-related hand problems.18,29
Materials Handling
Concerns regarding handling materials center on back injury and include lifting, pushing, pulling, bending, and twisting. The heavier the material, the more risk for injury. Low back injuries are seldom the result of a single traumatic episode but rather the result of repeated microtrauma that ultimately leads to injury.33 Therefore, workstation and work process design becomes integral for the safety of materials handling workers.
Design considerations for heavy lifting include the use of mechanical assist devices whenever feasible (e.g., use of a Hoyer lift for moving immobile patients in the hospital). When mechanical assist devices are not available, training in proper lifting technique and proper body mechanics is important to promote worker safety. Providing workers with back support is controversial, but many believe that the use of an elastic back support “has a preventative function, protecting the tissues … thus making injury less common.”46 Training workers and providing them with back support is only effective, however, when “supervisors and managers encourage the use of safe procedures and write policies that enforce them.”85
The following suggestions are useful for addressing safe handling of materials. Design workstations to keep large items that require lifting off the floor. Provide platforms that will keep items at mid-thigh height to allow workers to stand nearly erect for lifting. Provide foot clearance so that workers can get as close to the item as possible when lifting and face the load head-on. Adjustable lift tables are excellent for this purpose. Objects should be against the torso during the lift to minimize force on the spine. Workers should never be forced to twist their torsos to lift an object. Use carts or conveyors to transport heavy materials instead of carrying them. Orient packages for easy pick-up and provide adequate handles or handhold cutouts on packages.18
As stated earlier, these ergonomic design principles can be applied proactively to work situations to prevent problems before they even occur. For many occupational therapists, however, introduction to ergonomic considerations comes secondarily as part of a comprehensive rehabilitation program for injured workers. Following a work-related injury, ergonomic intervention is essential to the client’s successful re-engagement in the occupation of work. Without the ergonomic intervention aspect, the rehabilitation process cannot be considered complete.
A significant amount of effort goes into the rehabilitation of an injured worker. Physical injuries require the attention of a medical doctor to prescribe rest, medications, and rehabilitative therapies. The occupational therapist will provide acute care of the injuries by fabricating splints, instructing workers in stretching and strengthening exercise, and using physical agent modalities such as heat and ice to calm the soft tissues in preparation for functional rehabilitative activities. Other aspects of the occupational therapy plan include educating the injured worker about the nature of the injury and training in general body mechanics and personal injury management strategies to help prevent recurrence of injury on return to work. In some cases, the injured worker will require specialized conditioning before return to work and will be referred to a work-hardening program.
When the client is ready to return to work, it is important to remember that an injured worker cannot be safely returned to the same job without ergonomic intervention.
It seems obvious that returning an injured worker to the same conditions that caused the injury will certainly result in reinjury if not eliminated before the employee’s return to work. However, ergonomic intervention is sometimes overlooked as an integral part of the rehabilitation program. The goal of ergonomic evaluation and intervention in an injured employee’s work environment is to eliminate factors that contributed to the injury in the first place. If we do not eliminate the major cause of the original injury, it will not be long before the worker suffers a recurrence. If that happens, we have failed as occupational therapists to provide a successful rehabilitation process.
Ergonomic Evaluation
The ergonomic evaluation is an important assessment and intervention tool when used as part of a comprehensive rehabilitation or injury prevention program. This tool can be used along the entire continuum of prevention services. Ergonomic evaluation can be performed during workstation and work methods planning to assist in efforts to prevent worker injury. Ergonomic evaluation can also be performed for workers in whom symptoms of a work-related musculoskeletal disorder (WMSD) develop and for workers who come to therapy for rehabilitation and are ready to return to work, the goal being to prevent reinjury. Finally, ergonomic assessment can be useful in modifying a job in preparation for a disabled worker’s return to work with the goal of preventing further injury related to the disability.
The ergonomic evaluation should begin with the occupational therapist scheduling a time to meet with both the worker(s) to be assessed and the direct supervisor of the work area. The evaluation should be scheduled during the normal work hours of the worker(s). The goal is to obtain the best understanding of what actually occurs during a typical work shift, so the conditions should be closely approximated. It is extremely important that the actual worker(s) be present. The purpose of the evaluation is to look at the fit between the specific worker(s) and the specific job methods, equipment, and set-up. If any element is missing, the evaluation is of little or even no value.
Ideally, the occupational therapist evaluator will arrive at the worksite and meet first with the direct supervisor of the work area to be evaluated. The supervisor will be asked to give an overview of the circumstances leading up to the request for ergonomic evaluation. The occupational therapist will want to know what kinds of injuries are occurring in the work area, when the problem started, and how many employees have been affected. The supervisor will be able to review how the organization has dealt with the problem to date. Frequently, the supervisor will also describe what sorts of psychosocial and environmental influences may be affecting the situation. Occasionally, an ergonomic assessment is requested before any problems occur at all. The supervisor may explain that the employer is just trying to be proactive. In either case, this brief encounter with the supervisor will give an observant occupational therapist evaluator a very good feel for the organization’s management culture and organizational priorities.
Following the supervisor interview, the occupational therapist evaluator will want to see the work area and meet the employees. The supervisor may give the evaluator a brief tour of the work area and describe the job tasks and methods that occur there. If the supervisor has identified any problem areas (areas that the supervisor thinks are contributing to injury), the supervisor should be encouraged to point these out. This part of the evaluation will give the evaluator an understanding of how management views the situation. Next, the evaluator will ask to meet with the workers.
Once alone with the worker(s) it is important to establish some level of trust. The evaluator will explain to the workers(s) why the organization has asked for an ergonomic evaluation. It should be explained that the purpose of the evaluation is to make the job safer and more comfortable for the worker(s). The worker(s) should be encouraged to give the evaluator a tour of the work area and to explain their job tasks. If there are any discrepancies between management’s understanding of the job situation and the workers’ understanding of the same, the evaluator must seek definitive clarification.
Finally, the worker(s) should be asked to begin performing the job as normally as possible. The evaluator will explain that he/she will be watching and perhaps videotaping or taking notes. The evaluator should assure the worker(s) that the information that is being recorded will be used to develop strategies to make the job tasks safer and more comfortable to perform. The evaluator must stress that he or she wants the workers(s) to do the job just like any other day. The evaluator will not begin analysis of the work methods until at least 10 minutes has elapsed to allow the workers time to fall into a more normal work pattern.
The ergonomic workstation and work methods assessment should focus on identifying known risk factors for MSD. It is often very useful to videotape the work area and work methods performed. Recording the worker(s) performing their job tasks will allow the evaluator to return to his or her office and further analyze the data. If the evaluator plans to videotape any work areas or work methods, he or she should ask permission from the company before taping. It is becoming increasingly more difficult to gain permission for in-house videotaping because of confidentiality and trade secrets concerns. However, some companies are still willing to allow videotaping for the purpose of ergonomic evaluation. Always obtain prior written permission allowing you to videotape in-house. Box 14-5 suggests a protocol for videotaping jobs for the purpose of ergonomic evaluation.
In light of these concerns, it may be helpful to develop an ergonomic checklist to assist in performing the on-site evaluation. The checklist should include the most common ergonomic risk factors and be tailored to the specific needs and conditions of the workplace that the occupational therapist intends to evaluate. Figure 14-10 is an example of a typical ergonomic risk factor identification checklist. Figure 14-11 is an example of a checklist for computer workstation evaluation. Figure 14-12 is a typical hand tool risk factor checklist.
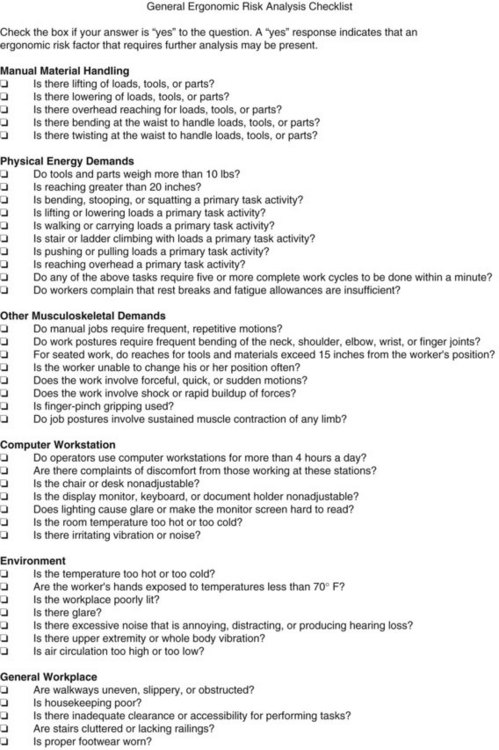
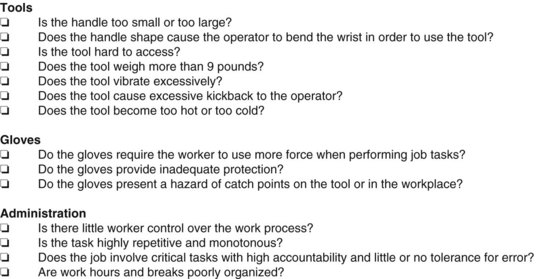
FIGURE 14-10 General ergonomic risk analysis checklist. (From Cohen AL, Gjessing CC, fine LJ, Bernard BP, McGlothlin JD: Elements of ergonomics programs: a primer based on workplace evaluations of musculoskeletal disorders, Washington, DC, 1997, US Government Printing Office.)
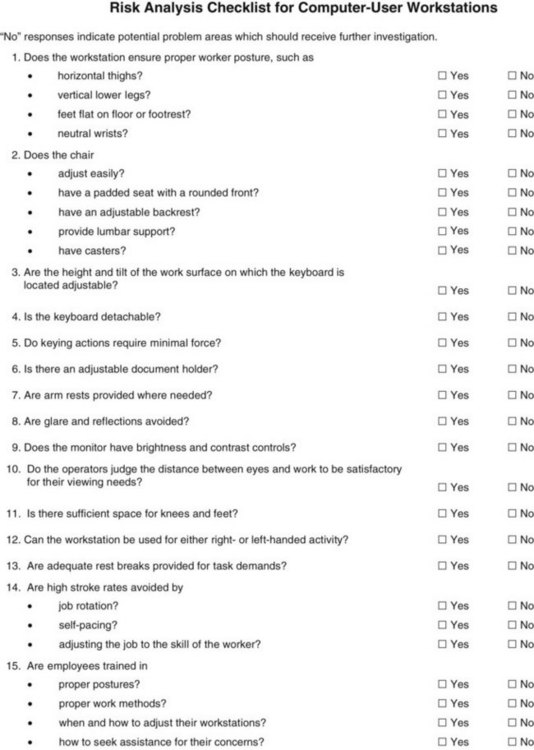
FIGURE 14-11 Risk analysis checklist for computer workstations. (From Cohen AL, Gjessing CC, fine LJ, Bernard BP, McGlothlin JD: Elements of ergonomics programs: a primer based on workplace evaluations of musculoskeletal disorders, Washington, DC, 1997, US Government Printing Office.)
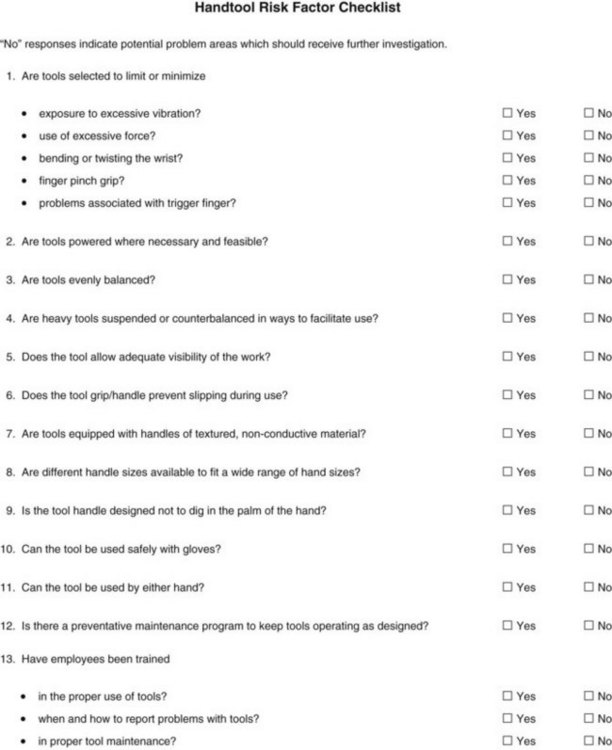
FIGURE 14-12 Hand tool risk factor checklist. (From Cohen AL, Gjessing CC, fine LJ, Bernard BP, McGlothlin JD: Elements of ergonomics programs: a primer based on workplace evaluations of musculoskeletal disorders, Washington, DC, 1997, US Government Printing Office.)
Risk factors to look for include the following:
1. Forceful exertions: Heavy lifting, pushing, pulling, twisting, gripping, or pinching. Handling heavy tools, equipment, or products. Difficulty maintaining control of equipment or tools or lifting and moving an object of asymmetric size. Also using inappropriate or inadequate tools.
2. Repetition: Performing the same motion or series of motions continually or frequently for an extended period (Table 14-4).
TABLE 14-4
High-Risk Repetition Rates for the Upper Extremity
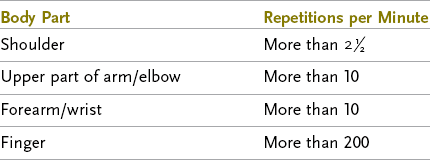
From Kilbom A: Repetitive work of the upper extremity; Part II: the scientific basis for the guide, Int J Ind Erg 14:59, 1994.
3. Awkward or static posturing, either repetitively or for prolonged periods: Assuming positions that place stress on the body, such as reaching above shoulder height, kneeling, squatting, leaning over a work surface, using a knife or keyboard with the wrists bent, twisting the torso while lifting, or looking at a computer monitor off to one side, which causes the neck to twist all day. Also, sitting all day at a desk with poor posture.
4. Contact stress: Pressing the body or part of the body (such as a hand or forearm) against hard or sharp surfaces and edges (e.g., using the hand as a hammer, resting the forearms on a sharp desk edge while typing, and using pliers with the handle pressing into the palm).
5. Excessive vibration: For example, from power tools or sitting in a truck cab all day while driving.
6. Cold temperatures: Either working in cold temperature or handling cold tools or products (e.g., construction workers outside during winter handling metal tools and equipment or meat packers or butchers handling frozen meat).
Once the workstation and work methods risk factors have been identified and the worker(s) have had a chance to familiarize themselves with the occupational therapist, focus should turn to the psychosocial aspects of the job. Frequently, these factors will surface during the evaluation process without any prompting whatsoever. Factors such as workload and productivity stressors, quality of the relationship between the worker(s) and other coworkers and the supervisor, genuine job task enjoyment, and overall health and fitness cannot be overlooked. Work-related musculoskeletal injury is never the result of any one factor; rather, it is the accumulation of a variety of risk factors and situations that ultimately result in injury. Occupational therapists look at the entire occupational profile to determine what is occurring.
Finally, it is important to ask the workers for their perspective on problem areas or risk factors in their work area. If their perspective matches what has been identified in the ergonomic evaluation of the work area and work methods, the workers should be encouraged to share their ideas for correcting the problem. Although the occupational therapist is the expert in workstation and work methods analysis, the on-site workers know their job better than anyone. The workers have probably spent hours formulating and discussing how they would change things if ever given the chance. Ask them. Often, one will find a wealth of knowledge and many useful ideas for reducing or eliminating risk factors in the people who perform the job. It is important to exercise caution before using each suggestion. As the expert, it is the occupational therapist’s responsibility to ensure that the changes implemented will serve to reduce and prevent injury. Sometimes, worker-driven suggestions inadvertently cause new problems if not assessed appropriately by the ergonomic consultant.
Following the on-site evaluation, the occupational therapist returns to his or her office to analyze the data and prepare a report. The report will be shared with whomever requested the ergonomic evaluation. The report should contain an introduction explaining the background and purpose of the ergonomic evaluation, a description of the actual work area and work methods assessment, and finally the evaluator’s findings and recommendations with clear and comprehensive information regarding how to implement the recommendations and resources for securing and purchasing any equipment or services. Job tasks found to contain several risk factors for the development of WSMD have the greatest risk for injury and should be addressed first by the company. Recommendations will focus on ways to eliminate or reduce risk factors (Table 14-5).
TABLE 14-5
Combating Ergonomic Risk Factors
| Risk Factor | Suggestions for Improvement |
| Using Excessive Force | Reduce Force Required to Perform Activity |
| Occupational therapist lifts/transfers heavy clients several times daily | Use Hoyer lift or get help from coworker |
| Employee uses heavy drill in a manufacturing plant | Suspend tools from ceiling with tension wire |
| Chef has difficulty cutting chicken in restaurant kitchen | Provide equipment to sharpen knives after every shift |
| Repetition | Reduce Prolonged Exposure to Repetitive Activity |
| Multiple scans required to activate grocery scanner | Implement program for regular preventive maintenance on scanners |
| Executive secretary required to type 5 hours in an 8-hour workday | Alternate typing task every 30 minutes with other office tasks such as making phone calls and filing |
| Awkward/Static Posturing | Reduce or Eliminate Awkward/Static Posturing |
| Medical transcriptionist types with her head turned to the right to see computer screen | Move computer monitor on desk so that it is directly in line with the computer keyboard and worker’s face as she looks straight ahead |
| Same medical transcriptionist sits in same position all day to type | Require worker to stand and gently march in place for 60 seconds after every 30 minutes of typing; provide timer to remind worker |
| Grocery store checkout clerk bends at waist and grabs case of soda from bottom of cart with right hand several times daily | Teach body mechanics for proper lift technique and use of two-hand power grip |
| Contact Stress | Reduce or Eliminate Contact Stress |
| Typist rests her forearms on sharp desk edge to type | Provide soft wrist rest until budget allows purchase of new desk with rounded edges |
| Jewelry maker uses pliers with short handle to twist wires; end of handle rests in palm of hand | Provide pliers with longer handle that is gently curved to fit hand |
| Teacher uses side of fist to punch stapler several times daily | Provide electric stapler |
| Excessive Vibration | Reduce Vibration |
| Drill vibrates in hand of assembly line worker in manufacturing plant | Wrap handle of power tool in vibration-dampening tape and have the worker wear antivibration gloves that fit correctly (to avoid grasping tighter than necessary to handle tool) |
| Cold Temperature | Reduce Exposure to Cold |
| Construction workers outside in winter handle cold metal equipment and tools | Wrap tool and equipment handles with neoprene and provide workers with thermal gloves to wear; make sure that gloves fit the workers correctly to avoid grasping objects tighter than necessary |
| Meat and deli team at grocery store handle frozen foods frequently | Provide well-fitting thermal gloves to wear when handling frozen items and provide grasping tool to use for handling smaller frozen packages |
Lorna benefited from a worksite evaluation. The occupational therapist went to her worksite to observe her and the other workers perform some of the essential functions of the job in their actual work environment. Risk factors were identified, such as excessive force from pinching and pulling the fabric tightly over the padded wooden frame and from using the heavy staple gun. A significant amount of force is required to push the heavy furniture to the next workstation. Her work tasks are repetitive, for example, pulling the trigger of the staple gun and pushing and pulling the fabric and furniture all day long. Lorna and the other workers were observed to have awkward posturing with frequent bending, twisting, and squatting to move the bulky furniture around to staple the fabric down.
Lorna’s employer was open to the suggestions that the occupational therapist made and was willing to make the appropriate accommodations. A special tool with a padded and curved handle to fit the shape of most hands was purchased to allow the workers to use a grasp-release motion to activate a material clamp rather than using the fingers so forcefully to pinch and pull the fabric. To lessen the amount of bending, twisting, and squatting required, it was recommended that the company purchase commercially available platforms on wheels to easily move the wooden furniture frames around. Additionally, the platforms contain a simple hydraulic lift that elevates the frame to whatever height is needed for easy stapling. The occupational therapist researched and located a resource for purchase of this helpful equipment, which facilitated the employer’s timely implementation of the worksite recommendations. Worksite evaluations and ergonomic interventions can also be important aspects of a comprehensive injury prevention program, as discussed in the next section.
Injury Prevention Programs
For decades, the majority of occupational therapy practice has been in the area of rehabilitation. Occupational therapists are unquestionably skilled in facilitating client independence during and/or following an injury, illness, or disease. Though not an entirely new concept, we are now recognizing occupational therapy’s potential to facilitate and perpetuate independence before or even in avoidance of these events. As we move into the 21st century, increasing numbers of occupational therapists are broadening their practices to include wellness and prevention.
Support for this movement is ubiquitous. The 1994-1996 landmark University of Southern California’s Well Elderly Study supports occupational therapy’s preventive intervention role in enhancing physical and mental health, occupational functioning, and life satisfaction.40 The Occupational Therapy Practice Framework: Domain and Process, second edition, provides further support and lists health promotion, performance maintenance, and disability prevention as occupational therapy intervention approaches that facilitate “participation in life through engagement in occupations.”1 Finally, in 2004, AOTA President Carolyn Baum, PhD, OTR/L, FAOTA, identified several prevention-related businesses as “hot” occupational therapy emerging practice areas.57
With regard to occupational therapy and work, prevention can take on three forms: primary prevention, secondary prevention, and tertiary prevention. Primary prevention efforts help protect healthy workers against a targeted condition before the condition occurs. Interventions are directed to an entire workforce to prevent a specific work-related medical problem. Secondary prevention emphasizes early identification of and intervention for asymptomatic workers who have risk factors for the development of work-related medical problems, as well as identification and treatment of workers with mild medical symptoms in the early reversible stages of injury. The goal is to identify risk factors so that they can be minimized or eliminated and to reverse any medical problems that might be developing. Tertiary prevention occurs after a worker suffers nonreversible injury, illness, or disease. Interventions include treatment of the medical problem, attempts to restore maximum function in the workplace, and prevention of injury, illness, or disease-related complications. The goal is to return the affected worker to gainful employment within the confines of the medical problem and to prevent further injury. Once a permanent work-related injury occurs, primary and secondary prevention measures have failed. However, early risk factor detection and intervention through secondary prevention may have minimized the severity of the permanent injury.85,99
Most occupational therapists are familiar with the process of tertiary prevention of work-related medical problems. Typically, the occupational therapist becomes involved after a worker suffers an injury and it becomes the therapist’s job to help the client regain maximum function in the workplace and prevent further injury. Occupational therapists are also commonly involved in secondary prevention efforts. Workers are referred with mild work-related medical conditions and intervention is planned to reverse the symptoms. When these clients get ready to return to work, the occupational therapist may assist the client in identification and modification of risk factors to reduce the risk for reinjury. Worksite evaluation and ergonomic intervention are generally part of the process for successfully re-engaging these workers.
Worksite evaluation and ergonomic intervention can also be part of a comprehensive primary prevention program designed to prevent work-related injury, illness, and disease.
Helping employers improve worker fitness, job comfort, and workplace safety reduces work-related medical problems. It can also lead to improved employee morale and increased productivity.39 Occupational therapists, acting as consultants, can assist corporate clients in establishing injury prevention programs. This is one way that occupational therapists can incorporate the concepts of wellness and health promotion into their daily practices.
Occupational therapist Michael Melnick wrote that “the success or failure of a prevention program has less to do with specific activities implemented and more to do with the methods of implementation.”60 Melnick outlines the four characteristics that are common among successful injury prevention programs: ongoing management support, supervisor “buy in,” employee participation, and ongoing support and reinforcement.60 Melnick explains that successful prevention programs are grounded in the consultant’s ability to instill in the corporate client a culture of safety and wellness. The focus should be on the process of implementing safety and wellness activities and not on the activities themselves.
One common reason that an occupational therapist might be asked to consult with an industrial client is to control the severity and incidence of WMSDs. WMSDs are a class of soft injuries affecting the muscles, tendons, and nerves. Other names for WMSDs are cumulative trauma disorders, overuse syndromes, and repetitive strain disorders. WMSDs come on slowly and develop over time. They are thought to be the result of repeated microtrauma to a body and occur when the body is denied the opportunity to adequately rest and repair itself. Common diagnoses within the class of WMSDs include carpal tunnel syndrome, de Quervain tendinitis, lateral epicondylitis, and some types of back injuries.81
According to the Bureau of Labor Statistics, WMSDs accounted for 29% of all workplace injuries requiring time away from work in 2007 (reference page info: retrieved from the Bureau of Labor Statistics—www.bls.gov/opub/ted/2008/dec/wk1/art02.htm-on September 27, 2010). Employers pay more than $45 billion annually in worker’s compensation and other expenses associated with these disorders.4 These statistics indicate that WMSDs are at a crisis level in the workplace. However, the financial losses to industry and the economy pale in comparison to the physical and emotional pain and suffering endured by today’s injured workers.
Lorna and several of her coworkers were experiencing WMSDs. Their employer agreed to implement an in-house ergonomics program and injury prevention program at the recommendation of the occupational therapy consultant. An ergonomic team was developed that consisted of the company’s chief financial officer, the stapling station supervisor, the employee health nurse, the safety manager, the occupational therapist consultant, and three employees who worked in the stapling station, including Lorna.
There are a multitude of resources available for prevention consultants interested in helping corporate clients develop effective programs for evaluating and addressing musculoskeletal concerns in the workplace. OSHA and NIOSH are excellent starting points. Box 14-6 offers information on these two government entities and provides a partial listing of their ergonomic and injury prevention resource materials.
It is important to remember that every corporate client is unique and that the consultant’s recommendations must work within the corporate culture, goals, and budget constraints. Melnick also reminds us that we must help our corporate clients recognize that “injury prevention consultants do not reduce injuries. This would occur only if the consultant stepped in and performed each worker’s job. Rather, prevention consultants help companies reduce their losses by guiding them through various activities.”60
As a guiding framework, however, the injury prevention consultant will want to incorporate the following elements into the corporate plan:
• A process for the organization to initially identify the potential risk for musculoskeletal problems or other risk factors in the workplace
• A strategy for showcasing management’s commitment to addressing problems and encouraging open worker involvement in problem-solving activities
• Skill training to ensure that management and workers can evaluate work areas and work methods for risk factors that could lead to musculoskeletal problems
• Protocols for gathering data to identify jobs or work conditions that are most problematic and at-risk by using strategies such as ergonomic evaluation
• A strategy for developing effective controls for identified risk factors that if left untouched, could lead to musculoskeletal injury
• Protocols for outcomes assessment to see whether the musculoskeletal injury risk factor controls have actually reduced or eliminated the problem
• A plan for establishing a health care management program that emphasizes the importance of early detection and treatment of MSDs since early identification and treatment of these disorders almost always reduce the severity of injury and disability and their associated costs
• A plan for minimizing future risk factors for musculoskeletal injury when new work processes and work areas are in development since it is less costly to build good design into the workplace than it is to redesign or retrofit later
The essential elements of musculoskeletal injury prevention programs listed above are based on recommendations from both OSHA and NIOSH.14,68–71 In the 1990s and early 2000s, these two entities developed guidelines and recommendations for public and private sector organizations seeking to establish in-house musculoskeletal injury prevention programs. These informational documents are available through OSHA and NIOSH and are an invaluable resource for occupational therapists wanting to offer prevention consulting services to address WMSDs.
Empowering Corporate Clients: The Injury Prevention Team
Corporate clients initially realize they may have a problem with WMSDs in a variety of ways. Signs of potential problems include worker reports of frequent aches and pains via employee health visits or organized symptom surveys, injury and illness trends among workers performing the same job tasks, and identification of injury risk factors as a result of preventive ergonomic job analysis.14 Figure 14-13 presents an example of a typical symptom survey used by companies to screen for potential work-related musculoskeletal problems. Once an organization recognizes that it has a problem with WMSDs, it must develop a strategy to address the problem. At this point, corporate clients frequently seek an injury prevention consultant to “make the problem go away.”
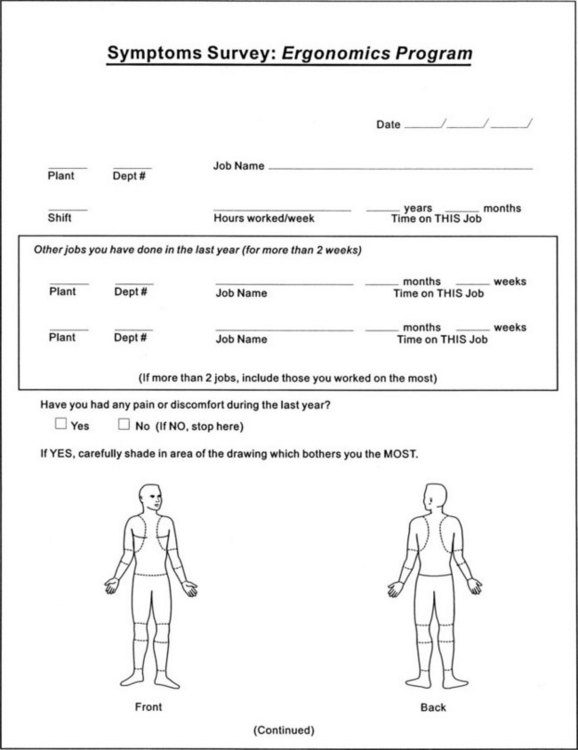
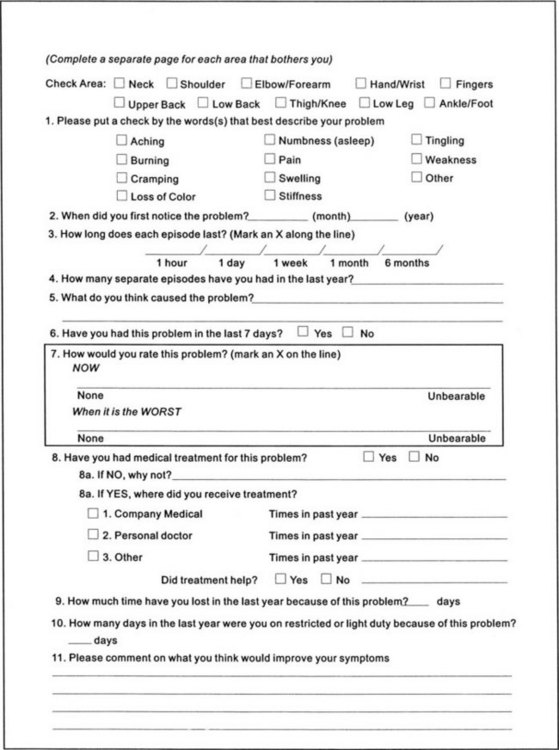
FIGURE 14-13 Symptom surveys are sometimes used as screening tools in companies that suspect problems with work-related musculoskeletal disorders. Workers are asked to voluntarily fill out the survey. The surveys are analyzed for trends indicating similar musculoskeletal symptoms within certain work groups. If workers from a specific work group tend to have similar complaints, the job tasks and workstations should be analyzed further. (From Cohen AL, Gjessing CC, fine LJ, Bernard BP, McGlothlin JD: Elements of ergonomics programs: a primer based on workplace evaluations of musculoskeletal disorders, Washington, DC, 1997, US Government Printing Office.)
Corporate clients frequently seek injury prevention specialists in the hope of achieving a quick and definitive fix. However, controlling WMSDs needs to be an ongoing process of control and management. The injury prevention consultant must work toward empowering the corporate client to maintain a successful injury prevention program consistently over time. The consultant must ensure that the client company has the knowledge and skills to follow through with the program. The role of the injury prevention consultant is to help the organization put together a team and a strategy for ongoing identification and control of risk factors for musculoskeletal injury.
In the same way that occupational therapists teach individuals to be self-sufficient in performing activities of daily living, they can also teach their corporate clients to be self-sufficient in controlling risk factors for musculoskeletal injury in the work environment. This client-centered approach has occupational therapy intervention focused on the corporate client’s priority of controlling work-related injuries and their associated costs. The occupational therapy intervention plan is the development of a corporate in-house injury prevention team. Another name for this team is the ergonomics team.
Usually, the injury prevention consultant will decide with corporate management who will be a part of the ergonomics team. Ideally, the team will be composed of representatives from management, front-line supervisors, production workers, labor unions, employee health, safety and/or industrial hygiene, engineering, and the injury prevention/ergonomic consultant. The exact makeup of the team will vary depending on the nature of the organization and corporate structure. The team meets and formulates a strategy for developing and implementing the injury prevention program.
Initial meetings will typically focus on the nature and scope of reported injuries and the effects that these injuries have had on production, worker’s compensation and associated costs, employee retention, and employee morale. An analysis of existing medical, safety, and insurance records can be conducted for the purpose of identifying injuries associated with MSDs. Health care team members should be encouraged to present medical record and injury information in a way that protects the confidentiality of individual workers. The team can then determine incidence rates of MSDs and look at trends that indicate problem work areas or job tasks.
Once the scope of the problem has been analyzed, the team will decide on a plan of attack for prevention of injury. In general, the magnitude and location of existing problems will suggest the magnitude and direction of the initial team efforts. The consultant will want to direct the corporate client to address the most grievous and resource-draining problems first. If on analysis of the data the problems seem widespread and involve a large percentage of the workforce, the plan of attack will probably be an aggressive company-wide program. On the other hand, if the problems seem to be isolated to just a few work areas or employees, the initial plan would probably be more focused and direct.14
Management Commitment
The industrial safety and health literature stresses that support of management in injury prevention efforts is crucial for successful implementation and outcomes.14 The consultant will want to ensure that management commitment to the process is genuine. If there is a lack of sincere top-level support for the injury prevention program, a consultant would be wise to pass on his or her involvement. Consultants are judged on their record of success. Prevention efforts without management support are destined to fail.
A good injury prevention consultant knows that employees want to see evidence of management support for all new programs. One of several ways to assist corporate clients in demonstrating support to the workforce is to encourage management to issue policy statements that give injury prevention efforts equal priority with productivity standards and cost control. Management should also meet with employee or union representatives (who should ideally be part of the ergonomics team) to discuss new policy and injury prevention program plans and show evidence of committing resources to implement the injury prevention program. Goals should be set and timelines established for meeting these goals, with specific people assigned responsibility and held accountable for overseeing various aspects of the program. Finally, information about the program should be disseminated to the entire workforce, from planning, to implementation, to evaluation. Employees want and need to feel that they are a part of the organization’s commitment to safety.10,14
Training in Risk Factor Identification/Ergonomic Evaluation and Problem Solving
Research has identified specific physical activity demands that place people at risk for the development of WMSDs: repetition, force, awkward or static posturing, prolonged direct pressure on soft tissue, vibration, exposure to cold, and inappropriate or inadequate hand tools.14,68–71,81 Additionally, psychosocial stressors at work can contribute to the development of WMSDs.14 Although this is an area in need of further study, these types of stressors can include excessive volume or productivity expectations, work that is “too difficult” or beyond the intellectual or emotional capacity of the employee, or a superior who does not express appreciation for a job well done. It is the combination of physical and psychosocial risk factors that the ergonomics team must address as part of an injury prevention program for WMSDs.
The ergonomics team will probably have the injury prevention consultant perform the first ergonomic evaluations at the workplace and present the first suggestions for improvement. However, key members of the injury prevention team should receive training in performing these evaluations themselves and training on how to formulate solutions. In this way, the evaluation part of the process is not reliant on an outside source. The goal, eventually, is to have the injury prevention consultant step out of the picture and leave behind a self-sufficient team of in-house experts to implement an ongoing process of risk factor identification for control of MSDs.
Figure 14-10 is an example of a general ergonomic injury risk analysis checklist. Members of the injury prevention team could be trained to use this tool to screen a variety of jobs for risk factors for musculoskeletal injury. Similarly, Figure 14-11 is an example of a job-specific screening tool. This checklist helps evaluators identify risk factors for musculoskeletal injury in computer users. Figure 14-12 is a hand tool analysis checklist. The injury prevention consultant or ergonomics team members could choose to modify any of these screening tools to match jobs specific to the organization.
The NIOSH publication “Elements for Ergonomics Programs 12” lists several objectives for team member training. A successfully trained team member will be able to do the following:
• Recognize risk factors for musculoskeletal injury and understand basic methods for their control
• Identify signs and symptoms of musculoskeletal injury in workers
• Understand the company’s injury prevention program thoroughly and everyone’s role and responsibility from top-level management to front-line worker
• Know the company’s procedure for reporting identified risk factors and signs and symptoms of musculoskeletal injury
• Demonstrate the ability to perform a basic ergonomic evaluation for identifying risk factors for musculoskeletal injury
• Recommend ways to control injury risk factors based on collaboration with employees, management, and other members of the ergonomics team
• Select ways to implement and evaluate the control measures
• Demonstrate skill in team building, consensus development, and problem solving
Some companies will decide to extend training to other members of the workforce. General training can be provided to employees who may potentially be exposed to hazards for musculoskeletal injury. Training can include how to recognize and report early signs and symptoms of musculoskeletal injury, information on identifying risk factors for musculoskeletal injury both at work and outside work, and strategies for workers to protect themselves from the development of musculoskeletal injury. Supervisors should receive the same training as workers, as well as training in techniques to reinforce proper body mechanics and other important aspects of the injury prevention program.71
Training the ergonomics team in skills required to sustain the injury prevention program is a substantial aspect of the consultant’s role. The consultant selects or designs the training and training materials to be understandable to the layperson in accordance with the participants’ educational levels and literacy ability. Consideration of language skills is also important, and attempts should be made to provide materials in the primary language of the employee.14 Outside training courses are also valuable in bringing perspective to the organization’s situation. Interaction with other companies’ course attendees provides opportunities for company-to-company networking. Many resources exist for locating appropriate training courses, including NIOSH and OSHA.
Developing Risk Factor Controls
The ergonomic evaluations will identify known risk factors for the development of MSDs. Risk factors might include forceful exertions, awkward or static posturing, repetition, contact stressors, vibration, exposure to cold, and/or psychosocial stressors. These identified risk factors will be brought back to the ergonomics team for discussion. Once high-risk areas or tasks have been identified, the task of the team then becomes formulating ways to reduce or eliminate the risk factors for musculoskeletal injury.
At this point it is important to use as many front-line production workers in the problem-solving process as possible. Workers know their jobs better than anyone and may have already formulated some ideas about improving the work area or work methods. Promoting worker involvement at this point has several benefits: enhanced worker motivation and job satisfaction, added team problem-solving capabilities, greater acceptance of workplace change, and greater knowledge of the work and organization.12,14,48,49,66
When workers present ideas for risk factor modification, it is essential that the injury prevention consultant and the in-house ergonomics team ensure that these potential solutions are appropriate and do not carry with them any potential for creating new problems. Union representatives should ensure that the suggested solutions do not violate employee-management understandings and contracts. Engineering’s role is to evaluate suggested solutions for practical and physical feasibility. Management’s role is to provide input regarding the organizational and financial appropriateness of the suggested solutions.
There are a variety of ways to reduce or eliminate risk factors for musculoskeletal injury. The 1991 OSHA publication Ergonomics Program Management Guidelines for Meatpacking Plants outlines a variety of risk factor control strategies applicable to most any workplace situation. These strategies can be categorized as either engineering controls, work practice controls, administrative controls, or use of personal protective equipment.71
Engineering controls include strategies for designing or modifying the workstation, work methods, and/or tools. The goal is to eliminate or reduce excessive exertion, awkward postures, and repetition. Workstations should be designed or modified to accommodate the actual worker at that workstation. If more than one person uses a workstation, elements of the workstation should be adjustable to fit each worker and be comfortable for the workers to use. Work methods should be designed or modified to minimize static and awkward posturing, repetitive motions, and excessive force. Tools and handles should be designed for a specific job and minimize contact stress, vibration, and forceful motions/gripping by the workers’ hands.71
Work practice controls include policies and procedures for safe and proper performance of tasks that are understood by all and enforced by supervisors. Workers should receive training in proper body mechanics, tool maintenance, and use of workstation adjustability features. New workers and those who have been away for awhile should be allowed adequate break-in periods to condition and recondition their bodies for the physical demands of the job. Supervisors and management should constantly monitor the use and effectiveness of work practice controls and make adjustments in techniques, line speed, and staffing as needed to maintain a safe and healthy work environment.71
Selection and use of personal protective equipment should be in line with the overall injury prevention program. Equipment should be available in a variety of sizes to accommodate the size differences among workers. Proper fit is especially important for gloves because improperly fitting gloves can reduce blood flow and sensory feedback and lead to slippage and use of excessive grip and pinch force. Protection against extreme cold (<40° F) is required to protect joints and soft tissues. Back braces and upper extremity splints should not be considered personal protective equipment. These devices are part of the medical management aspect of the program and should be used only with the advice and under the supervision of the health care team.71
Finally, administrative controls must be an option in situations in which musculoskeletal risk factors cannot be adequately reduced or eliminated via engineering controls, work practice controls, and the use of personal protective equipment. Administrative controls reduce the duration, frequency, and severity of exposure to risk factors. Methods include decreasing production rates, limiting overtime work, providing periodic rest breaks throughout the day, increasing staffing levels, and using job rotation/job enlargement to other jobs and tasks that involve the use of different muscle-tendon groups.71
When the team comes to a consensus on which methods to use to reduce or eliminate the risk factors for musculoskeletal injury, it is time to formulate a plan and implement the proposed solutions. However, before any changes are made, it is important to again solicit employee feedback regarding these plans, especially from employees who are not involved in the ergonomics team. Most people are resistant to change; it is human nature. Soliciting and sincerely listening to feedback improve employee buy-in for the proposed changes. Additionally, this feedback might identify implementation problems that the ergonomics team overlooked. Even the best idea for improving the comfort and safety of a job cannot be successfully implemented without employee support. Performing this step in the process is well worth the time and effort.
Medical Management Strategies
In addition to identifying risk factors for musculoskeletal injury and implementing plans to reduce or eliminate these risk factors, it is important for the ergonomics team to develop a medical management plan. Initiating early conservative medical treatment is key to minimizing serious disorder and dysfunction.63 Workers should be trained to identify early symptoms of MSDs so that they can seek medical care. The employee health staff should formulate guidelines for the management of employees with early symptoms of MSDs. This plan might include oral anti-inflammatories, splinting, rotation to light duty or time off work, and occupational therapy. The physician and/or employee health nurse will usually lead the effort in developing medical management guidelines for the organization.
As occupational therapists, it is important to understand the role and implications of upper extremity splinting of work-related injuries. The health care team should think about the possible ramifications of prescribing an upper extremity splint to a worker who plans to remain on the job. It is true that splinting helps rest the injured body part and that this can be helpful for recovery from a musculoskeletal injury. However, when a worker is restricted from moving, for example, the wrist during work, the result is often that the elbow or shoulder will compensate by positioning itself awkwardly to get the task accomplished. Splinting during work may protect the wrist, but the result could be injury to the elbow, shoulder, neck, or back. Therefore, splints should not be used at work unless the health care team understands the worker’s job tasks and can ensure that using the splint will not place stress on other parts of the body.
Outcomes Assessment and Preventing Future Problems
Finally, once the ergonomics team has implemented both efforts at controlling risk factors for musculoskeletal injury and the medical management process, the entire injury prevention program must be evaluated for effectiveness. Outcomes measures are useful in determining whether the program is working and to what extent. If the program does not seem to be working to any significant degree, the team will continue to modify its efforts until the incidence of WMSDs has declined to acceptable levels. The injury prevention program should be considered an ongoing process rather than a short-term solution to an identified incident or problem work area. Most ergonomics teams find that as soon as one problem work area is under control, another problem is identified that requires the focus of the team’s efforts.
The occupational therapist is an invaluable resource for helping organizations develop in-house injury prevention programs to control risk factors related to the development of musculoskeletal injury. The occupational therapist’s basic training in occupational performance analysis, problem identification, intervention planning and implementation, and outcomes assessment makes the fields of ergonomics and injury prevention ideally suited for practitioners of our profession. The NIOSH and OSHA are valuable resources for occupational therapists interested in working in ergonomics and injury prevention.
Pre-Employment Testing
A frequent use of functional testing includes assessing a person’s ability to meet certain physical requirements before being hired for a job.78 Some pre-employment testing may consist of isometric strength testing, ROM testing, or actual measurement of a person’s ability to perform selected tasks from the job description. Pre-employment screening can be an integral part of a company’s comprehensive injury prevention and management strategy.78 Because of their training in task analysis and holistic approach, occupational therapists are excellent candidates for assisting companies in expanding plans to more effectively manage employee injuries.
When a company is looking at the overall impact of an employee injury on the bottom line, it goes much further than simply the cost associated with the injury itself. It extends beyond the medical costs to include the employee’s compensation, benefit package payments, training of replacement personnel, replacement personnel wages, and overtime payment for existing personnel if they are needed for coverage. This does not include the indirect costs of diminished productivity during the period when coverage is being arranged. The total impact can be quite staggering. The cost of developing an employment screening process is significant; however, the cost savings to the company can be dramatic.78
The EEOC’s Uniform Guidelines on Employee Selection Procedures sets forth guidelines for the structure and function of human resource departments within companies and businesses. The guidelines also address how an organization can select and manage employees and places strong emphasis on the necessity of policies and procedures being job related.24,78 The EEOC also mandates that an employer’s selection process not have adverse impact on any group of people and must not discriminate on the basis of race, color, religion, sex, or national origin, as established by Title VII of the Civil Rights Act of 1964.24,78 Meeting these criteria requires that the selection procedures demonstrate validation, be of business necessity, and be a bona fide occupational requirement.24,78 To be compliant with the ADA, pre-employment screening must be based on an accurate job description, test only the essential functions (although not every function need be assessed), and have high face validity (often referred to as content validity—tests what you really want to know) or closely mirror the aspects of the job that is being tested.6,78 Dynamic testing (actually replicating physical tasks from the job) is recommended and can be conducted on-site at the company or off-site and needs to use equipment from the job as it is available.78 It is vital that companies take the time to thoroughly develop their screening process to be able to defend why the screening was considered necessary, maintain awareness and vigilance in the development phase of good test design, and be prepared to explain and demonstrate the applicability of the screening to the job in question.78
Pre-employment testing can also occur at several points in the hiring process; however, many health care providers and legal experts recommend conducting such testing after an offer of employment has been extended.31,54 With post-offer screening (POS), the most advantageous progression is to interview the applicant and determine whether the person is an acceptable candidate for employment.78 A conditional offer is extended to the applicant based on the applicant’s ability to meet a variety of conditions, such as passing a drug screen, acceptable background check, and physical testing. A problem with pre-offer testing is that Title 29 of the Code of Federal Regulations specifically states that medical examination is permissible “after making an offer of employment to a job applicant.”13 Monitoring blood pressure or the heart rate or inquiring about past medical history is considered to be part of a medical examination and is precluded in pre-offer testing.78
Anything that a therapist does in the way of evaluating an applicant might be deemed medical simply because an occupational therapist is a medical professional. It is also important to look critically at any testing that is considered to be general strength testing because it has been found to be a poor predictor of potential for injury.21,65,78 Normative databases are of little use in making hiring decisions, too, since according to both the ADA and the EEOC, it does not matter whether the applicant falls into the 5th percentile or the 95th percentile; the only thing of importance is whether the applicant can perform the tasks of the job.6,24
If the applicant passes the screening, he or she is hired and begins working. If the applicant does not pass, the employer must assess whether the applicant has a disability as defined under the ADA (see Chapter 15).6 If the applicant does, the employer must determine whether reasonable accommodation can be offered to the applicant so that that the individual may be able to perform the job. Reasonable accommodation means providing accommodation in such a way that the employer is not placed under undue financial strain for the accommodation to be implemented. If the company can and does offer accommodation to the applicant, the hiring process is completed and the employment begins. If the company cannot offer reasonable accommodation or if the applicant does not have a disability yet fails the screening, the employer can choose to rescind the offer of employment, examine opportunities for alternative placement elsewhere in the company, or offer remediation of some type and allow the applicant to retest if certain criteria are met.78 For example, if a nondisabled applicant does not pass the lifting portion of a POS and otherwise meets the employment criteria, the company might elect to allow the applicant 2 weeks to improve strength with the goal of returning for a retest screen in an attempt to pass the lifting portion.
Suppose Henry (the roofer in the case study) had difficulty balancing on one leg as a result of an early childhood accident but that this balance problem was not something that was readily apparent. If a POS were conducted on Henry before being hired at the roofing company and balance was a component of testing for working as a roofer, his difficulty could have been detected and Henry could have been denied the job or offered alternative placement. Either way Henry would have been protected from a fall that would radically change his life.
A company does not have to test applicants for every job. Typically, it is suggested that a company survey all of its injuries and determine where the majority of injuries are occurring and if they are occurring within the first 6 months of hiring. If so, this company is a good candidate for implementing a physical screen as part of the hiring process. Once it is determined which jobs are going to be selected for testing, the physical demands of the job must be evaluated. This can be done by survey, questionnaire, or observation (either direct or video).7 The job description must include information that is functional in terms of physical demands, describe the essential tasks of the job, and be presented in such language that one can test for an individual’s ability to perform them.7 In the case of a company requesting that existing job descriptions be used for development of the screen, it is extremely important to document that the company provided the job descriptions and that the therapist does not assume any liability for errors in their accuracy.
Physical demand items can then be selected for testing during screening based on either the difficulty or the frequency of the item. It is not necessary to test all of the physical demands for each job. For instance, a job might include carrying 10 lb a distance of 10 feet twice a day and lifting 40 lb from pallet height to waist height 200 times per day. Testing the ability to lift 40 lb would be a better selection for testing, for if the applicant is able to lift 40 lb from pallet height to waist height, it is likely that he or she will also be able to carry 10 lb a distance of 10 feet. It is important to select a method of testing the tasks that is reliable and valid and demonstrates job applicability, whether choosing from a standardized battery of physical demand tests or developing job-specific tasks to improve the applicant’s understanding of the relevance of the task and defensibility of hiring decisions.24,78
After tasks are selected, implementation can begin. It is suggested that a statistically significant sample of incumbents be tested to ensure that the correct demands have been selected and that the minimum requirements for each demand have been set appropriately. Once pilot testing is complete, the screening can be administered consistently to all applicants for a given job. It is also recommended that the screening process be monitored to ensure that fair and nondiscriminatory selection of applicants is occurring and that modifications in the screening process can occur as needed.78
Transition Services from School to Work
Occupational therapy practitioners can make a valuable contribution to students with disabilities who are transitioning from school to the community. The 1997 amendments to the Individuals with Disabilities Education Act (IDEA) of 1990 specified that transition planning is to be part of the Individualized Education Program (IEP). Representatives from community agencies that provide post-school services, such as state-sponsored vocational rehabilitation, must join the education team. Related services such as occupational therapy are formal contributors to the transition planning for students who need these type of services.94 Transition services are defined by the IDEA as “a coordinated set of activities for a student designed within an outcome-oriented process, which promotes movement from school to post-school activities, includes postsecondary education, vocational training, integrated employment (including supported employment), continuing and adult education, adult services, independent living, or community participation.”93 Occupational therapy’s unique focus on occupational performance can be a strong asset to the transition team.
The three main roles that an occupational therapist will participate in are transition-related evaluation, service planning, and service implementation. The occupational therapist contributes vital information about students’ performance abilities and needs in any of the transition domains: domestic, vocational, school, recreational, and community.
Transition-Related Evaluation
Effective transition-related evaluation primarily uses nonstandardized interviews, situational observation, and activity analysis approaches. These approaches are top-down, which means that they first consider what the student wants or needs to do and secondarily identify the occupational performance issues that are causing difficulties.7 The transition team helps the student identify a positive, shared vision for the future. This can include living alone or with others in the community, attending post-secondary schools or training programs, working in a paid or volunteer job, using community services, and participating in activities of interest. The occupational therapist and other members of the team work together to identify the student’s present interests and abilities within the context in which performance is expected or needed. The evaluation process also allows the team to identify areas in which the student is likely to need ongoing support and resources to achieve his or her vision and goals for the future.
Service Planning
In a collaborative transition team, the team members collectively share information and write down the student’s goals.94 The team members do not record discipline-specific goals that focus on remediating the student’s underlying deficits. The occupational therapist, for example, does not need to write specific goals addressing cognitive, motor, or psychosocial skills. Instead, two or more group members gather together to write the goals and work collaboratively with the student to accomplish the goals. A student with limited movement in her arms and hands may have the goal of being able to complete written assignments. The occupational therapist may take the lead in evaluating the effectiveness of using alternative writing methods such as assistive technology. Recommendations are made to the student and the team. If the team supports the recommendations, the team would assign responsibility for obtaining the equipment, as well as provide training to the student and other team members. Rainforth and York-Barr define collaboration as “an interactive process in which persons with varied life perspectives and experiences join together in a spirit of willingness to share resources, responsibility, and regards in creating inclusive and effective educational programs and environments for students with unique learning needs.”82
Program Implementation
The occupational therapist provides services in collaboration with the student and his or her teachers, parents, employers, coworkers, and others as necessary to address the student’s goals in the domestic, vocational, school, recreation, and community areas. Occupational therapy personnel (including the occupational therapist and the occupational therapy assistant) deliver transition services in the student’s natural environments. Therefore, occupational therapy may provide intervention in the student’s school, workplace, home, or any other relevant setting in the community. Collaborative problem solving with others involved in the student’s environment is essential to help the student use alternative methods to complete the necessary activities. For example, an occupational therapist may introduce and train the teacher in using assistive technology to help a student be able to access the computer at school to do written assignments. The occupational therapy practitioner may provide direct or consultative services to help minimize discrepancies in the student’s abilities and the demands of any environment. Evaluating whether the student reaches his or her goals should be the outcome measure to evaluate the effectiveness of occupational therapy services.
Work Readiness Programs
Many times, people who have survived a major accident or illness cannot return to their prior employment and need to explore other options for employment. For example, Henry can no longer carry out the job demands of a roofer. Henry may really want to return to some type of meaningful work but needs guidance and direction to explore what his present abilities and work skills are so that he can set some realistic vocational goals.
A work readiness program is designed to help individuals who desire to work identify vocational options that match their interests, skills, and abilities. At Rancho Los Amigos National Rehabilitation Center in Downey, California, an occupational therapist developed and implemented an ongoing work readiness program as part of the Occupational Therapy Vocational Services. This is a 6-week program that meets three times a week for 2 hours. It consists primarily of group sessions with a few individual sessions. Topics addressed include the following: work habits, goals, interests, work skills, vocational exploration, job hunting strategies, and community resources. Instruction, group discussion, and hands-on exploration of work skills via standardized work samples and situational assessments are used to help people explore their readiness to work and discover their potential for pursuing training for a different occupation. Each person’s program is individualized to address specific goals and interests. For example, Henry may be interested in working with a computer. He would be given the opportunity to do different work-related tasks using a computer so that he could see whether he has an aptitude for this type of work. If Henry was not familiar with the types of jobs that a person could do with a computer, he would learn how to do vocational research by using various reference books in the library or on the Internet.
A work readiness program can help people identify specific goals to pursue and develop a plan to help them work toward their goals. This program can help a person prepare for returning to work, but it does not provide a job for the participant. At the completion of the program, if a person demonstrates readiness to work, he or she can be referred to the State Department of Rehabilitation for assistance in job training and job placement. After completing a work readiness program, the occupational therapist can provide valuable information on a person’s skills, aptitudes, and interests to assist the rehabilitation counselor in developing a feasible plan for the worker. While Henry was attending the work readiness program, he identified the goal of becoming a computer support technician. Based on the vocational testing and research that he did during the program, this was determined to be a reasonable goal for him to pursue. He was referred to the State Department of Rehabilitation for job training and job placement in his new career.
Community-Based Services
Historically, work-related programs took place within medical model clinics, such as rehabilitation programs or settings designed for work intervention, as opposed to the site where the worker actually performed his or her role.90 Today, work programs are increasingly being located in the community in which the participant resides or within the work setting itself.90 This trend toward increased community practice is probably due to changes in the field of occupational therapy and external forces influencing the practice. Current thinking in occupational therapy recognizes that “occupational dysfunction is multidimensional, resulting from the interplay of biological, psychological, and ecological factors.”90 Decreasing reimbursement in medical model settings has resulted in occupational therapists exploring other options for reimbursement in the community.
Funding for most community-based programs is derived from grants or contracts through local, state, or federal governments, as well as foundations. Grants are funds that are awarded for a specific purpose and a specific period, usually for research or a service project, “based on a submission of a creative original proposal.”90 Contracts also provide funding for research or service projects; however, the funding agency defines the scope of the project and requests bids from competing organizations in the community. The majority of funding for community-based programs comes from foundations; “foundations are operated by philanthropic families, corporations, or community agencies that have reserved significant amounts of money for the purpose of supporting charitable organizations and programs to address specific community needs.”90 Many associations and civic groups, such as the United Way, American Head Injury Foundation, Kiwanis Club, and others, provide funding for community projects related to specific areas of interest. It is important to note that community-based programs should develop a broad financial base with multiple funding sources for programs to “survive and thrive” in the long run.
Community Rehabilitation Programs
There are almost 600 community rehabilitation programs (CRPs) with federal contracts under the Javits-Wagner-O’Day (JWOD) program according to NISH, formerly the National Industries for the Severely Handicapped. These community-based nonprofit organizations train and employ individuals with severe disabilities (primarily developmental disabilities and blindness) and provide quality goods and services to the federal government. The CRPs subcontract work from various industries to allow individuals with severe disabilities the opportunity to be productive, earn a competitive wage, and contribute to society. See the NISH Website (www.NISH.org) for more details. These programs receive most of their funding from regional centers or the Office of Vocational Rehabilitation. Although most of these programs are run by non–occupational therapy personnel, this is an area that some occupational therapists may want to explore for future involvement. There is a great need for these types of programs for individuals with other severe, chronic disabilities (such as brain and spinal cord injuries), but creative funding needs to be obtained to support them.
Homeless Shelter Programs
An emerging practice area for occupational therapists is working with persons who are homeless. Because of the increasing number of persons experiencing homelessness, Congress enacted the Stewart McKinney Homeless Assistance Act of 1987 (Public Law 100-77).34 This act was designed to meet the needs of those who are homeless by providing funds for emergency shelters, food, health care, housing, education, job training, and other community services. The act funded a Department of Labor project to plan, implement, and evaluate the effectiveness of a comprehensive spectrum of employment, training, and other support services to help persons who are homeless to locate and sustain employment. Based on the Job Training for the Homeless Demonstration Program (JTHDP), which consisted of 63 organizations across the United States that provided comprehensive services for persons who were homeless from September 1988 to November 1995, the Department of Labor created a best practices guide.90 Box 14-7 lists the findings of the JTHDP, which recommended that a sponsoring agency provide the core services or that the agency develop linkages with other local human service providers to assist persons who are homeless in obtaining and sustaining employment.
Occupational therapists have the skills to design and implement programs that incorporate the JTHDP recommendations for best practices. Client-centered job readiness and job-training programs can and have been developed for community service agencies to address the concerns of persons who are homeless. This population desires intervention services that are “sensitive, respectful, and responsive to their self-identified needs.”10
Occupational therapy practitioners work with those who are homeless, as well as with agencies providing services for people who are homeless, to build skills for accessing resources, solving problems by identifying strengths and assets, and learning to critically analyze situations for win-win situations for employers and the persons who are homeless.
Welfare-to-Work Programs
Congress passed the Personal Responsibility and Work Opportunity Reconciliation Act (Public Law 104-193) in 1996 to move people from welfare to work.10 It required welfare recipients to find work after receiving 2 years of public assistance. The Balanced Budget Act of 1997 (Public Law 105-33) provided funds for welfare-to-work grants. These grants are for training long-term recipients of welfare or public assistance to enter the job market in unsubsidized jobs. People who are most difficult to place because of multiple barriers to work, such as low academic skills, poor work history, or those who need substance abuse treatment, are the target of these grants. A substantial percentage of welfare recipients have learning problems, mental health and substance use disorders, and issues of domestic violence interfering with their sustained employability.90
Welfare-to-work programs are another innovative practice area for occupational therapists. Therapists who are interested in entering this area of practice must find out which agencies within the local or state communities control the welfare-to-work funds. Occupational therapists can subcontract with these agencies and collaborate with them. This information can be accessed from the National Governors Association (NGA) Center for Best Practices welfare reform Website.64 Private foundations that are involved in the welfare-to-work programs may also be a source of entry for occupational therapists.
There are many barriers that a person receiving welfare must face to enter into competitive employment. Lack of transportation, lack of childcare, problems with domestic violence, illiteracy, lack of housing, substance abuse, and medical needs can interfere with a welfare recipient’s ability to obtain and retain a job.10 Successful welfare-to-work programs attempt to break these barriers down. For example, programs combine basic education and job development, provide refurbished cars for transportation to work, and provide one-on-one mentoring for improving self-sufficiency. Transitioning welfare recipients to the workplace presents a challenging practice area for occupational therapists to use their creativity to design and deliver effective services to help clients set goals, explore vocational options, and introduce them to different community resources to achieve successful and continued employment.43
Ticket to Work
The Ticket to Work and Work Incentives Improvement Act was enacted in December 1999. This law created a voluntary program for recipients of Supplemental Security Income (SSI) and Social Security Disability Insurance (SSDI) to receive job-related support services and encourage beneficiaries to return to work and pursue their employment goals.96 Those who have tickets can go to any Employment Network (EN), an organizational entity (state or local, public or private) that has contracted with the Social Security Administration (SSA) to coordinate and deliver employment services, vocational rehabilitation services, and/or other support services under the Ticket to Work Program. Interested individuals can contact MAXIMUS, a private company contracted by the SSA to oversee and process support to sustain ongoing Ticket to Work Program operations. They can be reached toll free at 1-866-968-7842 or contacted via the Website www.yourtickettowork.com or www.ssa.gov/work. The Ticket to Work Program creates opportunities for occupational therapists to serve on advisory panels, work as program managers, or provide employment support services.43
Future Trends
The population of older workers is increasing, whereas the population of younger workers between 25 and 44 is decreasing.88 According to the Bureau of Labor Statistics, between 1977 and 2007, employment of workers 65 and older increased 101% as compared with 59% for total employment (16 and older).9 It is predicted that there will be a shortage of younger workers to replace the baby boomers when they retire, thereby creating a gap in the labor market. One proposal to fill this gap would be to employ more people with disabilities.88 Occupational therapists can work with human resource managers to educate and provide resources for workplace accommodations. The Society for Human Resource Management has recently partnered with the Office of Disability Employment Policy (ODEP).88 This collaboration reveals that human resource professionals are seeking support and services for hiring and accommodating workers with disabilities.
Baby boomers represent one of the largest percentage of the working population.88 As they age, employers may need to be sensitive to workers in whom multiple disabilities develop that have an impact on their job performance. Changes in the workplace offer new opportunities for occupational therapists to help aging workers stay employed with their functional limitations. As older workers retire, occupational therapists can help individuals plan for their retirement and explore ways to remain active in the community by participation in leisure pursuits or volunteer activities. Occupational therapists can help older individuals identify their strengths and abilities and provide community resources to allow meaningful participation in valued occupations.
Summary
This chapter provides an overview of the varying types of work programs in which occupational therapists are currently practicing, as well as identifies and discusses areas for further involvement. There are tremendous opportunities for occupational therapists and certified occupational therapy assistants to expand their role and involvement in hospitals, schools, industrial settings, and the community in general in the area of work practice. Occupational therapy practitioners are challenged to take a proactive approach in advocating the need for and benefit of these types of work-related programs in all communities to help restore the worker role in many people’s lives.
1. How has involvement of occupational therapy in work programs evolved over the years?
2. What is the role of occupational therapy in work programs?
3. Describe the difference between an FCE and a vocational evaluation.
4. What components are usually included in an FCE report?
5. Describe the difference between work hardening and work conditioning.
6. List the common applications of the results of a JDA.
7. What interventions are used to determine whether someone is capable of returning to a specific occupation after an injury?
8. Discuss the ergonomic design considerations for workstations, seating, visualizing job tasks, tools, and materials handling.
9. List and discuss the eight important elements of corporate injury prevention plans.
10. Why are occupational therapists good candidates for assisting companies in the development of injury management programs?
11. Name and describe some innovative types of work programs in which occupational therapists can be involved in the community.
References
1. American Occupational Therapy Association. Occupational therapy practice framework: domain and process, 2nd Ed. Am J Occup Ther. 2008;62(6):625–683.
2. American Occupational Therapy Association. Statement: occupational therapy services in facilitating work performance. Am J Occup Ther. 2005;59:676–679.
3. American Occupational Therapy Association. Statement: occupational therapy services in facilitating work performance. Am J Occup Ther. 2000;54(6):626–628.
4. American Occupational Therapy Association. Occupational therapy services in work practice. Am J Occup Ther. 1992;46(12):1086.
5. American Occupational Therapy Association. Work hardening guidelines. Am J Occup Ther. 1986;40(12):841.
6. Americans with Disabilities Act. Technical assistance manual. Washington, DC: Equal Employment Opportunity Commission; 1992.
7. Baum, CM, Law, M. Occupational therapy practice: focusing on occupational performance. Am J Occup Ther. 1997;51(4):277.
8. Bohr, PC. Work analysis. In: King PM, ed. Sourcebook of occupational rehabilitation. New York, NY: Plenum Press, 1998.
9. Bureau of Labor Statistics. Retrieved online from www.bls.gov/, 2010. [on October 2].
10. Callahan, SR. Understanding health-status barriers that hinder the transition from welfare to work. Washington, DC: National Governors Association Center for Best Practices, Health Policy Status Division; 1999.
11. Canelon, MF. An on-site job evaluation performed via activity analysis. Am J Occup Ther. 1997;51(2):144.
12. Cascio, WF. Applied psychology in personnel management. Englewood Cliffs, NJ: Prentice-Hall; 1991.
13. Code of Federal Regulations, Title 29, Vol 4. Revised as of July 1, 2003. Part 1630: Regulations to implement the equal employment provisions of the Americans with Disabilities Act. Section 1630.14, Washington DC.
14. Cohen, AL, Gjessing, CC, Fine, LJ, Bernard, BP, McGlothlin, JD. Elements of ergonomics programs: a primer based on workplace evaluations of musculoskeletal disorders. Washington DC: US Government Printing Office; 1997.
15. Commission on Accreditation of Rehabilitation Facilities. Standards manual for organizations serving people with disabilities. Tucson, AZ: CARF; 1989.
16. Crabtree, J. The end of occupational therapy. Am J Occup Ther. 1998;52(3):205.
17. Cromwell, FS. Work-related programming in occupational therapy: its roots course and prognosis. Occup Ther Healthcare. 1985;2(4):9.
18. Dahl, R. Ergonomics. In: Kornblau B, Jacobs K, eds. Work: principles and practice. Bethesda, Md: American Occupational Therapy Association, 2000.
19. Darphin, LE. Work-hardening and work-conditioning perspectives. In: Isernhagen SJ, ed. The comprehensive guide to work injury management. Gaithersburg, Fla: Aspen, 1995.
20. Davis, H, Rodgers, S, Using this book for ergonomics in industry: introduction. Rodgers S, technical editor. Eggleton, E, eds. Ergonomic design for people at work, New York, NY, Van Nostrand Reinhold, 1983;vol 1:.
21. Deuker, JA, Ritchie, SM, Knox, TJ, Rose, SJ. Isokinetic trunk testing and employment. J Occup Med. 1994;36(1):42.
22. Rodgers S, technical editor. Eggleton, E, eds. Ergonomic design for people at work, vol 1. New York, NY: Van Nostrand Reinhold, 1983.
23. Ellexon, M. What every rehab professional in the U.S.A. should know about the ADA. Miami, Fla: ADA Consultants; 1992.
24. Equal Employment Opportunity Commission. Uniform guidelines on employee selection procedures. Washington, DC: EEOC; 1978.
25. Eser, G. Overview of vocational evaluation. Las Vegas, Nev: Stout University Training Workshop; 1983.
26. Field, JE, Field, TF. COJ 2000 with an O*NETTM 98 Crosswalk. Athens, Ga: Elliot & Fitzpatrick; 1999.
27. Fliedner, CA. Occupational therapy: for the body and the mind. In: Rodgers GM, ed. Centennial Rancho Los Amigos Medical Center 1888-1988. Downey, Calif: Rancho Los Amigos Medical Center, 1990.
28. Gibson, L, Strong, J. A conceptual framework of functional capacity evaluation for occupational therapy in work rehabilitation. Aust Occup Ther J. 2003;50(2):64–71.
29. Grubbs, R, Hamilton, A. Criteria for a recommended standard: occupational exposure to hand-arm vibration. Washington DC: US Government Printing Office; 1989.
30. Hall, H, Buck, M. The work of our hands. New York, NY: Moffat Yard & Co; 1919.
31. Harbin, G, Olson, J. Post-offer, pre-placement testing in industry. Am J Ind Med. 2005;47(4):296–307.
32. Harvey-Krefting, L. The concept of work in occupational therapy: a historical review. Am J Occup Ther. 1985;39(5):301.
33. Hepper, E, et al. Back school. In Kirkaldy-Willis WH, Burton CV, eds.: Managing low back pain, ed 3, New York, NY: Churchill Livingstone, 1992.
34. Herzberg, GL, et al. Work and the underserved: homelessness and work. In: Kornblau BK, Jacobs K, eds. Work: principles and practice. Bethesda, Md: American Occupational Therapy Association, 2000.
35. Holmes, D. The role of the occupational therapist-work evaluator. Am J Occup Ther. 1985;39(5):308.
36. Homan, NM, Armstrong, TJ. Evaluation of three methodologies for assessing work activity during computer use. Am Ind Hyg Assoc J. 2003;64(1):48–55.
37. IBM ergonomics handbook. New York, NY: IBM Corp, 2000.
38. Isernhagen, SJ. Advancements in functional capacity evaluation. In: D’Orazio BP, ed. Back pain rehabilitation. Boston, Mass: Butterworth, 1993.
39. Isernhagen, SJ. Corporate fitness and prevention of industrial injuries. In: Rothman J, Levine R, eds. Prevention practice: strategies for physical therapy and occupational therapy. Philadelphia, Pa: Saunders, 1992.
40. Jackson, J, Carlson, M, Mandel, D, Zemke, R, Clark, F. Occupation in lifestyle redesign: the Well Elderly Study Occupational Therapy Program. Am J Occup Ther. 1998;52(5):326.
41. Jacobs, K. Preparing for return to work. In Trombly K, ed.: Occupational therapy for physical dysfunction, ed 4, Baltimore, Md: Williams & Wilkins, 1995.
42. Jacobs, K, Baker, NA. The history of work-related therapy in occupational therapy. In: Kornblau BL, Jacobs, K, eds. Work: principles and practice. Bethesda, Md: American Occupational Therapy Association, 2000.
43. Johannson, C. Top 10 emerging practice areas to watch in the new millennium. OT Pract. 2000. [Jan 31].
44. King, PM. Work hardening and work conditioning. In: King PM, ed. Sourcebook of occupational rehabilitation. New York, NY: Plenum Press, 1998.
45. King, PM, Barrett, T. A critical review of functional capacity evaluations. Phys Ther. 1998;78(8):852.
46. Kirkaldy-Willis, WH. Energy stored for action: the elastic support and bodysuit. In Kirkaldy-Willis WH, Burton CV, eds.: Managing low back pain, ed 3, New York, NY: Churchill Livingstone, 1992.
47. Kornblau, B. The occupational therapist and vocational evaluation. Work Programs Special Interest Section Newsletter. 1996;10:1.
48. LaBar, G. Safety at Saturn: a team effort. Occup Hazards. 1994;56(3):41.
49. Lawler, EE. High involvement management. San Francisco, Calif: Jossey-Bass; 1991.
50. Lechner, DE. Functional capacity evaluation. In: King PM, ed. Sourcebook of occupational rehabilitation. New York, NY: Plenum Press, 1998.
51. Lechner, DE. Work hardening and work conditioning interventions: do they affect disability? Phys Ther. 1994;74(5):102.
52. Lechner, D, Roth, D, Stratton, K. Functional capacity evaluation in work disability. Work. 1991;1:37.
53. Legislative Committee, National Rehabilitation Association. Meeting the nation’s needs by the expansion of the program of vocational rehabilitation of physically handicapped persons. Occup Ther Rehabil. 1937;16(3):186.
54. Littleton, M. Cost-effectiveness of prework screening program for the University of Illinois at Chicago physical plant. Work. 2003;21(3):243–250.
55. MacFarlane, B. Job modification. Work Special Interest Section Newsletter. 1988;2(1):1.
56. MacLeod, D, et al. The ergonomics manual: guidebook for managers, supervisors, and ergonomic team members. Minneapolis, Minn: Comprehensive Loss Management; 1990.
57. Malugani, M. Emerging areas in OT. Monster Worldwide http://content.monster.com, 2004. [on the AOTA website 12/24/04].
58. Marshall, EM. Looking back. Am J Occup Ther. 1985;39(5):297.
59. Meister, D. Conceptual aspects of human factors. Baltimore, Md: Johns Hopkins Press; 1989.
60. Melnick, M. Injury prevention. In: Kornblau B, Jacobs K, eds. Work: principles and practice. Bethesda, Md: American Occupational Therapy Association, 2000.
61. Meyer, A. The philosophy of occupational therapy. Am J Occup Ther. 1977;31(10):639.
62. Mikkelson, S, Vilstrup, I, Lassen, CF, et al. Validity of questionnaire self-reports on computer, mouse and keyboard usage during a four week period. Occup Environ Med. 2007;64(8):541–547.
63. Mosely, LH, et al. Cumulative trauma disorders and compression neuropathies of the upper extremities. In: Kasdan ML, ed. Occupational hand and upper extremity injuries and diseases. Philadelphia, Pa: Hanley & Belfus, 1991.
64. National Governors Association Center for Best Practices. Welfare reform (online) Available at http://www.nga.org/portal/site/nga/menuitem.1b7ae943ae381e6cfcdcbeeb501010a0/?vgnextoid=4bb8aa9c00ee1010VgnVCM1000001a01010aRCRD&vgnextfmt=print.
65. Newton, M, Waddell, G. Trunk strength testing with iso-machines: Part I. Review of a decade of scientific evidence. Spine. 1993;18(7):801.
66. Noro, K, Imada, AS. Participatory ergonomics. Bristol, Pa: Taylor & Francis; 1991.
67. O’Callaghan, J. Primary prevention and ergonomics: the role of rehabilitation specialists in preventing occupational injury. In: Rothman J, Levine R, eds. Prevention practice: strategies for physical therapy and occupational therapy. Philadelphia, Pa: Saunders, 1992.
68. Occupational Safety and Health Administration. Ergonomics for the prevention of musculoskeletal disorders: guidelines for nursing homes. Washington, DC: US Government Printing Office; 2003.
69. Occupational Safety and Health Administration. Ergonomics for the prevention of musculoskeletal disorders: guidelines for poultry processing. Washington, DC: US Government Printing Office; 2004.
70. Occupational Safety and Health Administration. Ergonomics for the prevention of musculoskeletal disorders: guidelines for retail grocery stores. Washington, DC: US Government Printing Office; 2004.
71. Occupational Safety and Health Administration. Ergonomics program management guidelines for meatpacking plants. Washington, DC: US Government Printing Office; 1990.
72. Occupational Safety and Health Administration. Working safely with video display terminals. Washington, DC: US Government Printing Office; 1997.
73. Ogden-Niemeyer, L, Jacobs, K. Definition and history of work hardening. In: Ogden-Niemeyer L, Jacobs, K, eds. Work hardening state of the art. Thorofare, NJ: Slack, 1989.
74. O*NET. http://online.onetcenter.org/, 2006. [Retrieved August 12, 2010, from].
75. Owens, LA, Buchholz, RL. Functional capacity assessment, worker evaluation strategies, and the disability management process. In: Shrey DE, Lacerte M, eds. Principals and practices of disability management in industry. Winter Park, Fla: GR Press, 1995.
76. Page, J. Functional capacity evaluation-making the right decision. RehabPro. 9(4), 2001.
77. Patterson, C. A historical perspective of work practice services. In: Pratt J, Jacobs K, eds. Work practice: international perspectives. Boston, Mass: Butterworth, 1997.
78. Perry, L. Preemployment and preplacement testing. In: King PM, ed. Sourcebook of occupational rehabilitation. New York: Plenum Press, 1998.
79. Peterson, W, Perr, A. Home and worksite accommodations. In: Galvin JC, Scherer J, eds. Evaluating, selecting and using appropriate assistive technology. Gaithersburg, Md: Aspen, 1996.
80. Pinel, P. A treatise on insanity. New York, NY: Hafner; 1962.
81. Putz-Anderson V, ed. Cumulative trauma disorders: a manual for musculoskeletal diseases of the upper limbs. Bristol, Pa: Taylor & Francis, 1988.
82. Rainforth, B, York-Barr, J. Collaborative teams for students with severe disabilities: integrating therapy and educational services, 2. Baltimore, Md: Brookes; 1997.
83. Reed, K. The beginnings of occupational therapy. In: Hopkins HL, Smith HD, eds. Willard and Spackman’s occupational therapy. Philadelphia, Pa: Lippincott, 1993.
84. Rosenberg, B, Wellerson, T. A structured pre-vocational program. Am J Occup Ther. 1960;14:57.
85. Rothman, J, Levine, R. Prevention practice: strategies for physical therapy and occupational therapy. Philadelphia, Pa: Saunders; 1992.
86. Rothstein, J, Echternach, J. Primer on measurement: an introductory guide to measurement issues featuring the APTA’s standards for tests and measurements in physical therapy practice. Alexandria, Va: American Physical Therapy Association; 1993.
87. Ryan, DJ. Job search handbook for people with disabilities. Indianapolis, Ind: Job Information Seeking and Training (JIST) Publishing; 2000.
88. Sabata, D, Endicott, S. Workplace changes: seizing opportunities for persons with disabilities in the workplace. Work Programs Special Interest Section Q/Am Occup Ther Assoc. 2007;21:2.
89. Sabonis-Chafee, B. Occupational therapy: introductory concepts. St. Louis: Mosby; 1989.
90. Scaffa, ME, et al. Future directions in community-based practice. In: Scaffa ME, ed. Occupational therapy in community-based practice settings. Philadelphia, Pa: FA Davis, 2001.
91. Shrey, DE. Worksite disability management and industrial rehabilitation: an overview. In: Shrey DE, Lacerte M, eds. Principals and practices of disability management in industry. Winter Park, Fla: GR Press, 1995.
92. Smith, SL, Cunningham, S, Weinberg, R. The predictive validity of the functional capacities evaluation. Am J Occup Ther. 1986;40:564.
93. Snodgrass, JE. Getting comfortable: developing a clinical specialty in ergonomics has its own challenges and rewards. Rehab Manag. 2004. [July:24].
94. Spencer, K. Transition from school to adult life. In: Kornblau B, Jacobs K, eds. Work: principles and practice. Bethesda, Md: American Occupational Therapy Association, 2000.
95. Symons, J, Veran, A. Conducting worksite evaluations to identify reasonable accommodations. In: Hamil J, ed. Integrating assistive technology into your practice, AOTA on-line course. Bethesda, Md: American Occupational Therapy Association, 2000.
96. The Work Site. Ticket to work fact sheet (online). Available at www.ssa.gov.
97. US Department of Labor, Employment and Training Administration. Revised dictionary of occupational titles, vols I and II, ed 4. Washington, DC: US Government Printing Office; 1991.
98. US Department of Labor, Employment and Training Administration. The revised handbook for analyzing jobs. Indianapolis, Ind: Job Information Seeking and Training (JIST); 1991.
99. US Preventive Services Task Force. Guide to clinical preventive services, ed 2. Washington, DC: US Government Printing Office; 1996.
100. Wegg, LS. The essentials of work evaluation. Am J Occup Ther. 1960;14:65.
101. Young, ES. Setting up an industrial program for the tuberculosis. Occup Ther Rehabil. 1939;18(3):163.