Evaluation of Sensation and Intervention for Sensory Dysfunction
After studying this chapter, the student or practitioner will be able to do the following:
1 Describe how sensation is positioned within the Occupational Therapy Practice Framework-2 (OTPF-2).
2 Describe and compare the difference in sensory loss because of a cardiovascular accident versus a peripheral nerve repair.
3 Perform a sensory evaluation on a client with a peripheral nerve problem.
4 Instruct a client in an appropriate program for desensitization, describe ways to upgrade the program, and name the criteria that reflect client readiness to have the program upgraded.
5 Explain why people who lack protective sensation are at risk for serious injury and what types of injury are possible.
6 Identify whether a client is a candidate for protective sensory re-education or discriminative sensory re-education based on sensory evaluation findings.
People who have not experienced sensory problems pro-bably take for granted all that sensation contributes to their daily occupational performance. By comparison, people with sensory dysfunction are likely to be acutely aware of the lost picture that normal sensation provides.11
Sensation (also called sensibility) is a body function, a component of the client factors that influences both the motor and processing aspects of performance skills. For this reason, sensation and sensory dysfunction affect clients’ performance in areas of occupation such as activities of daily living (ADLs) and education. For people with carpal tunnel syndrome, as in Mary’s case, the sensory loss involves the thumb, index finger, long finger, and radial half of the ring finger. This distribution of sensory loss makes it difficult to pinch and manipulate small objects with a typical three-point or palmar pinch. It often forces people to oppose their thumb to the pad of their small finger instead.
All clients with sensory dysfunction, regardless of etio-logy, should be evaluated to determine the occupational impact of the loss. The specific sensory tests and interventions may vary according to the diagnosis and prognosis for recovery. The battery of tests selected depends on whether the diagnosis is either central nervous system (CNS) or peripheral nervous system (PNS) in origin. A person with CNS injury is more likely to have deficits in proprioception and stereognosis. A person with PNS injury is more likely to have deficits in touch pressure awareness and two-point discrimination. A client with a history of a cerebrovascular accident (CVA) who then sustains a wrist fracture should be evaluated for proprioception and stereognosis, as well as for pressure threshold and two-point discrimination.
Somatosensory System
The somatosensory system handles sensory input from superficial sources such as the skin and from deep sources such as the musculoskeletal system. Sensation is stimulated by receptors in the periphery of the body, and the sensory information then travels to the brain by way of the spinal cord.
Somatosensory receptors are specialized to respond to stimulation of a specific nature. These receptors are categorized as mechanoreceptors, chemoreceptors, and thermoreceptors. Mechanoreceptors respond to touch, pressure, stretch, and vibration and are stimulated by mechanical deformation. Chemoreceptors respond to cell injury or damage and are stimulated by substances that the injured cells release. Thermoreceptors respond to the stimulation of heating or cooling. Each of these three types of receptors has a subset called nociceptors, which sense pain when stimulated.10
Disturbances in somatosensation may be manifested as paresthesia, hyperalgesia, dysesthesia, or allodynia. Paresthesia is a tingling, electrical, or prickling sensation. Tapping the volar aspect of the wrist may elicit paresthesias in the distribution of the median nerve in a person who has carpal tunnel syndrome. When such tapping elicits paresthesia, it is referred to as a Tinel sign. Hyperalgesia is increased pain and may occur during nerve regeneration. Hypersensitivity is increased sensory pain. Mary experienced hypersensitivity at her incision site following her surgery. Desensitization (discussed in detail later in this chapter) helps normalize the phenomenon of hypersensitivity. In clients with hypersensitivity, application of splint straps and desensitization intervention should be performed in the direction of arm hair growth, not against it, since hair follicle receptors sense hair displacement. Dysesthesia is an unpleasant sensation that may be spontaneous or stimulated. Allodynia is pain in response to a stimulus that is not normally painful.9 An example of allodynia would be seen when a person with complex regional pain syndrome (also referred to as reflex sympathetic dystrophy [RSD]) experiences pain with the mere movement of air wafting over the involved arm.
A dermatome is the area of skin supplied by one spinal dorsal root and its spinal nerve. The affected dermatome correlates with the level of the spinal cord lesion. However, some peripheral nerves have innervation patterns that differ from dermatome patterns. This is due to regrouping of sensory axons in the brachial plexus and in the lumbosacral plexus (Figure 23-1). The clinical significance of such regrouping is that sensory assessment along a dermatomal pattern is more appropriate in clients with CNS lesions, not PNS lesions. This is why clients with CNS lesions, such as CVA, are more likely to be tested for proprioception, stereognosis, and temperature whereas clients with PNS lesions are more likely to be tested for pain, pressure threshold, and two-point discrimination. Vibration testing is sometimes done with a tuning fork or with more sophisticated labor-atory instruments. (For more information on vibration testing, see Bell-Krotoski, Weinstein, and Weinstein.3)
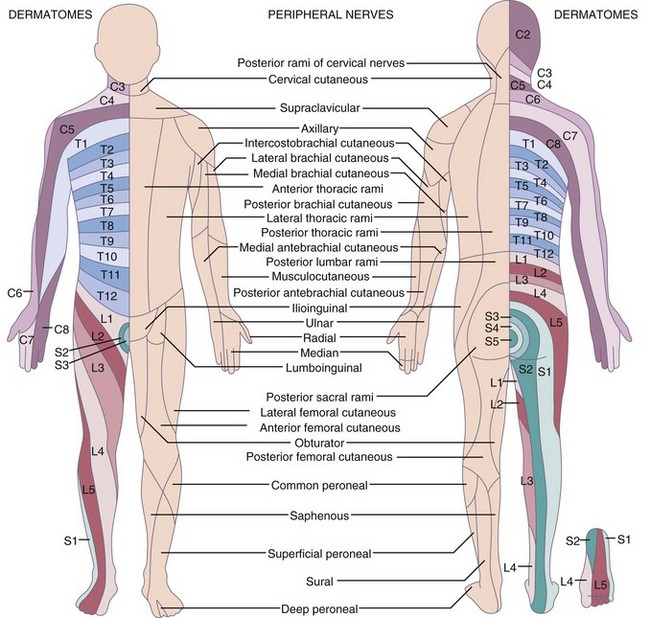
FIGURE 23-1 Cutaneous sensory distribution and dermatomes. (From Lundy-Ekman L: Neuroscience: Fundamentals for Rehabilitation, ed 3, St. Louis, Mo, 2007, Saunders, p 109.)
Neuropathy is defined as dysfunction of the peripheral nervous system. The typical order of sensory impairment associated with peripheral neuropathy is loss in the following sequence: light touch, cold, heat, and pain. This order is reversed for sensory recovery. Therefore, test for pain perception first and then heat, cold, and light touch.
Superficial Sensation
Pain, temperature, and touch are aspects of superficial sensation, also called cutaneous sensation. When compared with the more proximal body parts, the distal parts have a higher density of receptors and smaller receptive fields. This arrangement contributes to enhanced fingertip sensation, such as the ability to distinguish between one and two stimuli that are close together. The relevance of this in terms of daily occupations is that normal two-point discrimination enables a person to distinguish a dime from a penny without vision, as when one fingers the coins in a pocket or wallet. Figure 23-2 shows normal two-point discrimination values over different locations of the body.
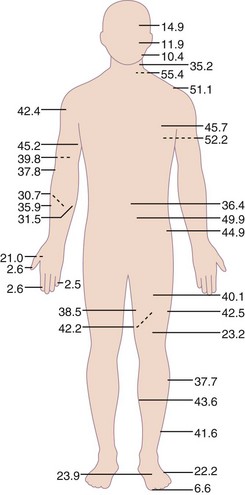
FIGURE 23-2 Normal two-point discrimination values over different locations of the body. (From Lundy-Ekman L: Neuroscience: Fundamentals for Rehabilitation, ed 3, St. Louis, Mo, 2007, Saunders, p 134).
Blisters, altered sweat patterns, calluses, shiny or dry skin, blanching of skin, scars, and wounds are indicators of possible sensory problems and indicate the need to instruct the client in the use of compensatory techniques such as vision during daily occupations. In people with sensory problems, healing is slowed because of decreased nutrition and vascularity. An absence of “wear” marks such as calluses or lack of dirt or grease stains on the hands of a mechanic, for example, may suggest that the hand is not being used. Lack of sweating correlates with lack of discriminative sensation. Nerve damage results in atrophy of soft tissue, which increases the tissue’s susceptibility to injury. Even pinprick testing (see the section on testing pain sensation) might elicit a drop of blood unexpectedly. Occupational therapists should follow universal precautions when performing this test.
Because upper extremity cutaneous sensory fibers and sympathetic nervous system fibers follow the same pathways, sympathetic phenomena may correlate with sensory function. In the upper extremity, the median nerve has more sympathetic fibers than the ulnar nerve, which may explain the increased risk for complex regional pain syndrome (RSD) in clients with median nerve injury. Therefore, it is important to assess Mary for vasomotor function such as blotching of the skin, sudomotor function such as abnormal sweating, pilomotor changes such as no goose bumps, and trophic changes such as atrophy of finger pulp or hair growth.
Before any sensory testing, a history should be obtained through client interview and review of medical reports. The history should include information on name, age, hand dominance, sex, occupation, date of injury, nature of injury, client description of the sensory problem, screening of motor function, and grip and pinch tests if appropriate.
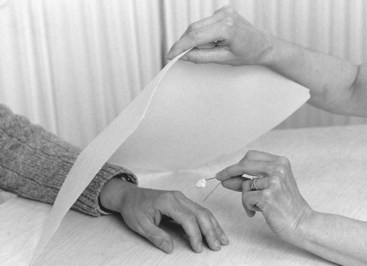
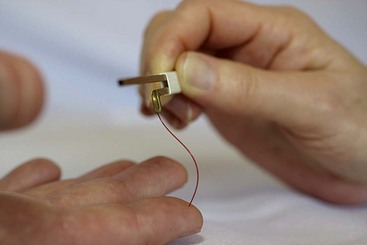
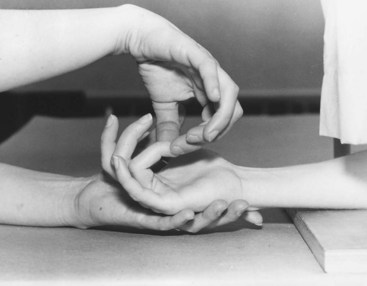
The most accurate sensory evaluation requires an environment free of background noise, good instruments, consistent testing techniques, cooperative clients, and competent testers. It is important to support the client’s hand fully with the examiner’s hand or by resting the client’s hand against putty to prevent it from moving because movement could provide sensory information that interferes with the test being administered (Figure 23-3). For all sensory testing, the client’s vision should be occluded. This is accomplished by asking the client to keep the eyes closed or by occluding the area with other means (Figure 23-4). A hand grid worksheet is used to record the findings (Figure 23-5).

FIGURE 23-3 Ways to support the hand during sensory testing. A, In the examiner’s hand. B, In putty. (From Callahan AD: Sensibility assessment for nerve lesions-in-continuity and nerve lacerations. In Mackin EJ, Callahan AD, Skirven TM, et al, editors: Rehabilitation of the hand and upper extremity, ed 5, St. Louis, Mo, 2002, Mosby.)
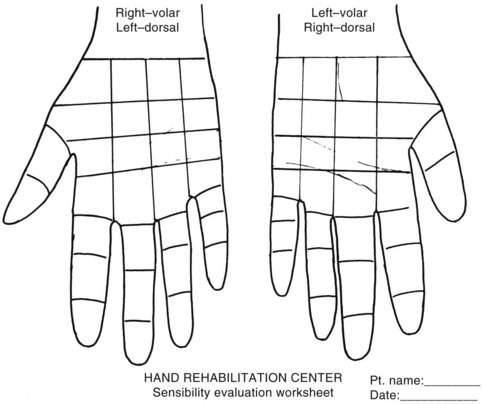
FIGURE 23-5 Hand grid worksheet. (From Callahan AD: Sensibility assessment for nerve lesions-in-continuity and nerve lacerations. In Mackin EJ, Callahan AD, Skirven TM, et al, editors: Rehabilitation of the hand and upper extremity, ed 5, St. Louis, Mo, 2002, Mosby.)
Sensory screening is a time-saving method to determine some parameters of the sensory loss experienced. When screening the hand, specific sites can be used to reflect larger portions of the hand innervated by the same nerve. For screening Mary’s median nerve function, test the thumb tip, index tip, and index proximal phalanx. For screening ulnar nerve function, test the distal and proximal ends of the small finger and the proximal ulnar aspect of the palm. For screening the radial nerve, test the thumb web space.2 (See Figure 23-6 for a picture of the sensory distribution of the hand.)
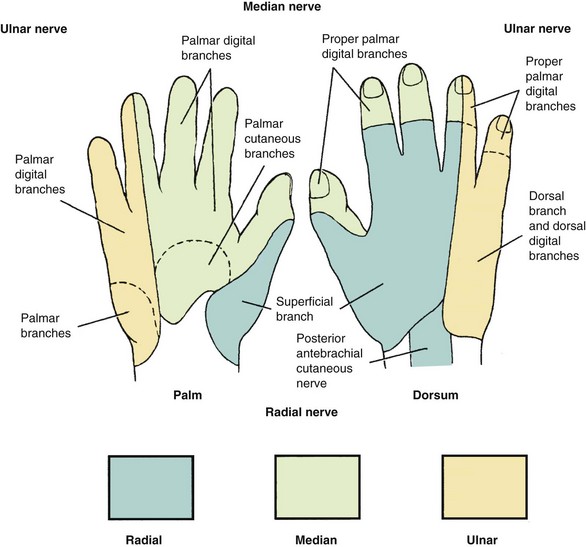
FIGURE 23-6 Sensory distribution of the hand. (From Trumble TE: Principles of hand surgery and therapy, ed 2, Philadelphia, 2000, Saunders, p 14.)
Pain Sensation
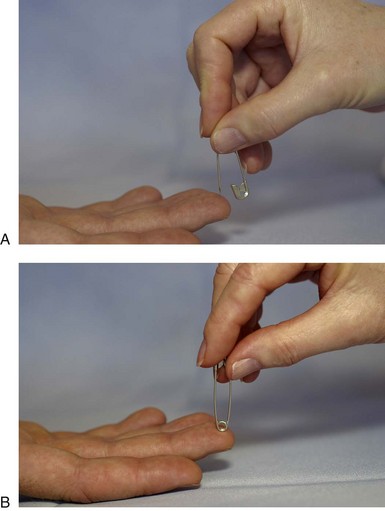
Pain is an unpleasant sensory and perceptual experience that is associated with either actual or potential cellular damage. The experience of pain is subjective and multidimensional.7 Pain can be tested by pinching the digit firmly or by pinprick. Intact pain sensation is indicative of protective sensation. The pinprick test can be used to rule out a digital nerve laceration. Be sure to use universal precautions (see Chapter 9).
Test for Pain (Protective Sensation):
• Using a sterilized safety pin, assess the amount of pressure required to elicit a pain response on the uninvolved hand. This is the amount of pressure that the examiner will use on the involved side.
• Alternate randomly between the sharp and dull sides of the safety pin and ensure that each spot has one sharp and one dull application (Figure 23-7).
Temperature Awareness
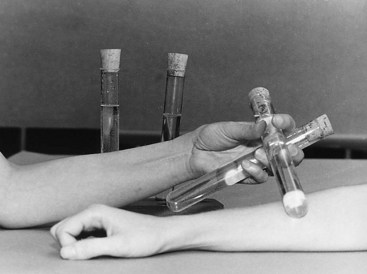
Temperature awareness is a test for protective sensation. Thermal receptors detect warmth and cold. In the clinic, it is important to test temperature sensation before applying heat or cold modalities to avoid burn injuries. Thermal receptors are also critical for a person to be able to determine safe water temperature for bathing. A client who lacks temperature awareness must learn compensatory strategies such as testing the water temperature with an unaffected body part. Many clinicians use only the pinprick test as sufficient evidence of protective sensation.
Test for Temperature Awareness (Protective Sensation):
• Apply test tubes or metal cylinders filled with hot or cold fluid randomly to areas of the involved hand (Figure 23-8).
Testing for Touch Sensation
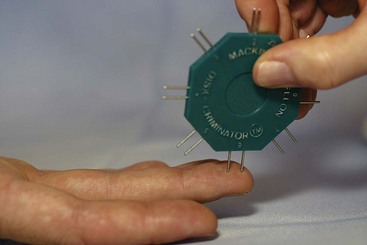
Two-Point Discrimination: Two-point discrimination and touch pressure testing with monofilaments are tests of different aspects of sensation. Two-point discrimination is a test for receptor density and is a good test to use for mapping improvement following nerve repair. Moving two-point discrimination returns before static two-point discrimination and is an indicator of recovery that is typically noticed before static two-point discrimination improves. One criticism concerns potential variability in the force of application during testing. Nonetheless, good intertester reliability has been reported with the Disk-Criminator tool.13
Test for Static Two-Point Discrimination:
• Use a device such as the Disk-Criminator or Boley gauge with blunt testing ends (Figure 23-9).
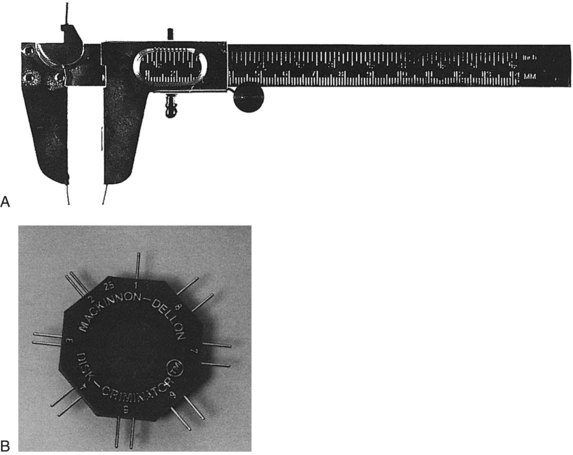
FIGURE 23-9 Boley gauge (A) and Disk-Criminator (B) for testing static and moving two-point discrimination.
• Test only the fingertips because this is the primary area of the hand used for exploration of objects.
• Begin with a distance of 5 mm between the testing points.
• Randomly test one or two points on the radial and ulnar aspects of each finger for 10 applications (Figure 23-10).
• Pressure is applied lightly; stop just when the skin begins to blanch.
• The client responds accurately to 7 of 10 applications at that number of millimeters of distance between the two points.
• 1 to 5 mm indicates normal static two-point discrimination.
• 6 to 10 mm indicates fair static two-point discrimination.
• 11 to 15 mm indicates poor static two-point discrimination.
Test for Moving Two-Point Discrimination:
• Begin with distance of 8 mm between points.
• Randomly select one or two points, and move proximal to distal on the distal phalanx parallel to the longitudinal axis of the finger so that the adjacent digital nerve is not stimulated (see Figure 23-10).
• The pressure applied is just enough for the client to appreciate the stimulus.
• If client responds accurately, decrease the distance between the points and repeat the sequence until you find the smallest distance that the client can perceive accurately.
Touch Pressure
Light touch is perceived by receptors in the superficial skin. Pressure (or deeper touch) is perceived by receptors in the subcutaneous and deeper tissues. Light touch is important for fine discriminatory hand use, whereas deep pressure is important as a form of protective sensation. Touch pressure testing examines the spectrum from light touch to deep pressure. Touch pressure testing is a good test to use for clients with nerve entrapment such as carpal tunnel syndrome. Many clinicians test two-point discrimination and the touch pressure of their hand therapy patients. Having intact light touch pressure awareness is an indicator of better sensation than having only intact deep touch pressure awareness. It is interesting to note that light touch pressure awareness has to be intact for two-point discrimination to be testable because the two-point discrimination test uses light touch.
Touch pressure is tested with a set of 20 monofilaments. These monofilaments are of varying thickness with numbers that represent a mathematic formula of the force required to bow them when applied perpendicularly. They are color-coded to correspond to five threshold categories. Clinicians will frequently use an abbreviated set of five monofilaments, one for each of these categories.
• Begin with monofilament 1.65.
• Apply the monofilament for 1 to 1.5 seconds at the pressure needed to bow the monofilament (applied perpendicularly) (Figure 23-11).
• Hold the pressure for 1 to 1.5 seconds.
• Lift the monofilament in 1 to 1.5 seconds.
• The proper amount of pressure is achieved when the filament bends.
• Repeat this three times in the same spot for monofilaments 1.65 to 4.08; monofilaments higher than 4.08 are applied only once.
• Randomly select areas of the hand to test, and change the interval of time between the application of monofilaments.
• If the client does not perceive the monofilament, proceed to the next (thicker) monofilament and repeat the sequence until monofilament 6.65.
• If the client does perceive the monofilament, record this number on the hand grid and proceed to the next area of the hand.
• The client responds to at least one of the three applications of the monofilament.
• Green (1.65 to 2.83) indicates normal light touch.
• Blue (3.22 to 3.61) indicates diminished light touch.
• Purple (3.84 to 4.31) indicates diminished protective sensation.
• Red (4.56 to 6.65) indicates loss of protective sensation.
• Untestable indicates an inability to feel the largest monofilament.
Proprioception
Conscious proprioception derives from receptors found in muscles, tendons, and joints and is defined as awareness of joint position in space. It is through cerebral integration of information about touch and proprioception that objects can be identified by tactile cues and pressure. If proprioception is impaired, it may be difficult to gauge how much pressure to use when holding a paper cup.
• Hold the lateral aspect of the elbow, wrist, or digit.
• Move the body part into flexion or extension (Figure 23-12).
The term kinesthesia is sometimes used interchangeably with the term proprioception but can also be defined as awareness of joint movement. Some therapists make a distinction between these two terms and test for kinesthesia by moving the unaffected limb into a certain posture and having the client copy the movement with the affected side while the eyes are closed.
Stereognosis
Stereognosis is the use of both proprioceptive information and touch information to identify an item with the vision occluded. Without stereognosis, it is impossible to pick out a specific object such as a coin or a key from one’s pocket, use a zipper that fastens behind you, or pick up a plate from a sink of sudsy water.
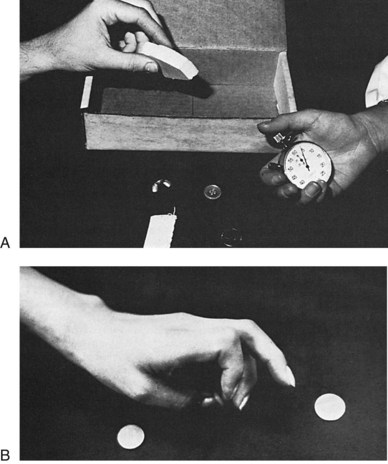
The Dellon modification of the Moberg Pickup Test is a good test for stereognosis for clients with injuries involving the median and/or ulnar nerves. This test requires the client to have the ability to participate motorically, so motor loss or weakness should be factored into the choice of this assessment. This test is based on the Moberg Pickup Test, which is a timed motor test that does not require identification of objects.
The Dellon Modification of the Moberg Pickup Test:
• Begin with a group of 12 standardized items: wing nut, large nut, hex nut, small square nut, screw, key, nickel, dime, washer, safety pin, paper clip, and nail.
• If the ulnar nerve is not involved, tape the ulnar two fingers to the client’s palm if possible.
• The client places the items one at a time into a box as quickly as possible (Figure 23-13).
• Test 2 (initiate test 2 only if the client’s deficits do not appear to be too severe during test 1).
Localization of Touch
Localization of touch is considered to be a test of functional sensation because there is high correlation between this test and the test for two-point discrimination. Localization of touch is an important test to perform following nerve repair since it helps determine the client’s baseline and projected functional prognosis. This test can be done with a constant (static) touch or a moving touch. Localization of touch is thought by many to reflect a cognitive component of the client’s abilities. Because it is considered to be a test of tactile discrimination that requires cortical processing, it is different from touch pressure testing.
Test for Localization of Touch:
• Apply the finest monofilament that the client can perceive to the center of a corresponding zone on the hand grid.
• Once the client feels a touch, have him or her open his or her eyes and use the index finger to point to the exact area where the stimulus was felt.
• Place a dot on the hand grid for a correct response.
• Place an arrow from the site of the actual stimulation to the identified site if the stimulus is identified incorrectly.
• Correct identification of the area within 1 cm of actual placement indicates intact touch localization.2
Somatotopic Arrangement
Sensory information is received and organized somatotopically in the primary somatosensory cortex. The homunculus (Figure 23-14) is a diagram that shows the arrangement and proportions of cortical areas representing the surface of the body. Areas with large cortical representation indicate a high density of sensory receptors. As indicated in Figure 23-14, somatotopic arrangement is such that axons providing information from the index finger are situated closer to those from the thumb than to those from the foot. Elegant research studies have elucidated the relevance of somatotopic arrangement to therapeutic strategies for normalizing impaired sensation. These strategies are effective because of the brain’s plasticity.16
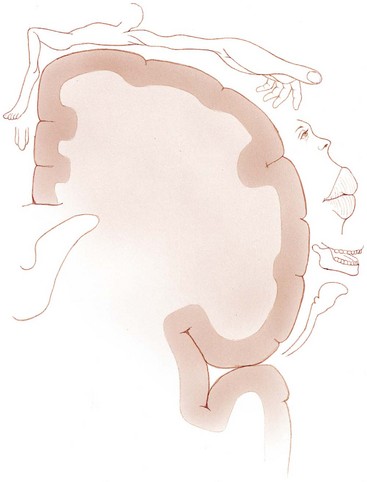
FIGURE 23-14 Homunculus. (From Lundy-Ekman L: Neuroscience: fundamentals for rehabilitation, ed 3, St. Louis, Mo, 2007, Saunders.)
Within the somatosensory cortex there is an inherent capacity for plasticity involving the circuitry.5 Topographic reorganization of the cerebral cortex occurs following injury and can be influenced by sensory input and by learning and experience. This has been described eloquently by the neurologist and author Frank R. Wilson as a dynamic interplay of the sensorimotor and cognitive worlds.19 Referred sensations and phantom pain (pain felt in a part removed from its point of origin) in amputees are examples of cortical reorganization.
Neuroplasticity
Our brain has the plasticity to mechanically induce neuronal reorganization. One aspect of this phenomenon, called neuroplasticity, includes the processes of habituation, learning, memory, and cellular recovery following an injury. Along with changes in synaptic connections, there are also changes in non-neuronal cells. Some concepts of neuroplasticity are as follows5,11:
• Sensory perception is a dynamic process that is experienced by the CNS.
• Receptor morphology is affected by hand use. The axiom of “use it or lose it” is particularly applicable here. Immobilization or disuse (such as a casted fracture or a highly guarded upper extremity posture) contributes to retrogressive modifications in receptors. Conversely, promoting normal use may stimulate new receptors.15
• Because there is overlap of the receptive fields of various nerve fibers, a single stimulus can excite different receptors.
Neurons may die following CNS injuries such as spinal cord lesions and strokes. The nervous system accommodates for injuries with behavioral, physiologic, and anatomic changes. Over time, the CNS can adapt by altering the strength of neural transmission through modifications in the structure and function of neurons and synapses. It is very exciting clinically to realize that occupational therapists facilitate recovery through functional activities and involvement in occupation resulting in somatosensory reeducation.11
Desensitization
The existence or persistence of hypersensitivity will often limit use of the affected body part and may prevent sensory re-education from proceeding, so it is important to address this problem early if possible. Desensitization for hypersensitivity is a form of treatment that aims to elicit habituation and thereby reduce the client’s hypersensitivity and improve function. Habituation is a decrease in a response following repeated benign stimuli. There is a reduction in the excitatory neurotransmitters released, and if the stimulation continues over a prolonged period, a permanent change consisting of a reduction in the number of synaptic connections will occur.4
Desensitization uses graded stimulation with procedures and modalities that are slightly aversive but tolerable. The stimuli are upgraded to be slightly more noxious as the client’s tolerance increases.18 Lois Barber, an occupational therapist and pioneer in hand splinting and hand therapy, developed a desensitization approach that exposes the hypersensitive area to textures such as sandpaper, contact particles such as rice, and vibration.1 Treatment is performed for 10-minute intervals, three or four times a day (Figure 23-15). Clients can be very creative at incorporating desensitization into their daily routine. For example, they may find that rubbing the hand on their textured shirt or corduroy pants is desensitizing and can be performed easily throughout the day.
Sensory Re-education
Stimulation and use of a body part affect the cortical map.12 Passage of time, use of the involved hand, and training all help promote improved functional sensibility.8 Children have greater capacity for neural regeneration and neuroplasticity than older people do. Motivation and the ability to concentrate enhance the results of sensory re-education.
Sensory re-education has been shown to improve the sensation of fingertip replantations even without repair of the nerves.14 Anne Callahan, an occupational therapist and prolific author in the field of hand therapy, has identified two groups of clients for sensory re-education, with guidelines differing according to the group. The two groups are candidates for protective sensory re-education and candidates for discriminative sensory re-education.
Protective Sensory Re-education
People who lack protective sensation are at risk for serious injury since they cannot feel pinprick or hot or cold exposure. Blisters may develop after holding objects and people do not realize it until they visually examine the hand. Following a CVA, a person with left hemiparesis and left neglect may inadvertently move the left hand on top of a stove burner during a cooking task. If the client lacks protective sensation, he or she will be burned without feeling the painful sensory stimulus of the hot stove. The same frequently happens to individuals with C6 quadriplegia. Protective sensation in their thumb, index finger, and long finger may be intact, whereas sensation in their ring and little fingers is absent.
Callahan identified the following instructions for protective sensory re-education of these clients6:
• Protect from being exposed to sharp items or to cold or heat.
• Try to soften the amount of force used when gripping an object.
• Use built-up handles on objects whenever possible to distribute gripping pressure over a greater surface area.
• Do not persist in an activity for prolonged periods. Instead, change the tool used and rotate the work task often.
• Visually examine the skin for edema, redness, warmth, blisters, cuts, or other wounds. This is important because tissue heals more slowly when a nerve injury has occurred.
• If there is tissue injury or damage, be very careful in treating and try to avoid infection.
• Maintain skin suppleness as much as possible by applying moisturizing agents.
Discriminative Sensory Re-education
Clients are candidates for discriminative sensory training if they have intact protective sensation with recognition of at least 4.31 on the touch pressure monofilament test. A client who is not able to localize the stimulus but can feel it is still a candidate for discriminative sensory re-education. A client with a brain insult or nerve injury resulting in reduced discriminative sensation will be unable to fasten a bra in the back, braid her own hair, or locate a wallet in a bag or pocket with the vision occluded. Discriminative sensory re-education can be graded by initially using grossly dissimilar objects such as a spoon and a penny and progressing over time to more similar objects such as a dime and a penny.
When planning discriminative sensory re-education intervention, it works best to identify short-term goals that are achievable and that will enhance function despite the sensory loss. If the client has motor involvement and cannot manually manipulate the stimulus, the stimulus can be moved over the hand instead. Discriminative sensory re-education involves training in both localization and graded discrimination.
Localization: Localization of moving touch tends to return before localization of constant touch. Retraining is done for both. With the client’s eyes closed, the eraser end of a pencil or the therapist’s finger is used to touch the client’s hand in the midline of one zone of the hand grid. This makes documentation easier and the intervention more accurate and consistent and minimizes afferent activity from adjacent areas of the skin. The stimulus is applied with either a moving or a constant touch. The client is told to open his or her eyes and point to the area that was touched. Interestingly, it has been shown that activity in the visual cortex is enhanced when touch of the hand is added to the visual stimulation, as long as the touch is provided on the same side as the visual stimulation.17 If the answer was incorrect, the process is repeated. The steps are repeated again with the eyes closed. The full process is then repeated in a new area. As the client improves, the stimulus is changed to a lighter and smaller touch.
Graded Discrimination: Stimulation is graded from that requiring gross discrimination to that requiring fine discrimination. Levels of difficulty in discrimination are represented by sequencing of the following three categories: (1) same or different, (2) how they are the same or different, (3) identification of the material or object.
The stimulus is applied to the skin in an area corresponding to the hand grid. Either the hand or the stimulus is moved to provide input. As earlier, the eyes are closed, then opened, and then closed for the retraining steps. Various textures can be used, such as different grades of sandpaper fabric or objects such as nuts and bolts or coins (Figure 23-16).
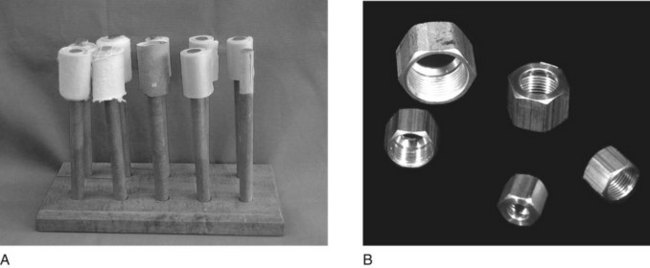
FIGURE 23-16 A, Different grades of sandpaper. B, Nuts and bolts used for graded discrimination sensory re-education. (A, From Callahan AD: Therapist’s management of peripheral injuries. In Mackin EJ, Callahan AD, Skirven TM, et al, editors: Rehabilitation of the hand and upper extremity, ed 5, St. Louis, Mo, 2002, Mosby; B, from Fess EE: Sensory reeducation. In Mackin EJ, Callahan AD, Skirven TM, et al, editors: Rehabilitation of the hand and upper extremity, ed 5, St. Louis, Mo, 2002, Mosby.)
Another version of discriminative training involves tracing a geometric shape or a letter or number on the fingertip or small area of the hand. This can be applied with a fingertip or the end of an instrument such as a small dowel or a pencil eraser. The client tries to identify the figure.
Difficulty is increased by adding the requirement of fingering for motor stimulation if appropriate and by occluding vision. Discriminative training can include identifying objects out of a box, retrieving objects from rice or sand, or performing ADLs with the eyes closed (Figure 23-17). Progress can be determined by improvement in the number of accurate responses, better mapping of areas of localization, increased speed of completing motor tasks, better status of two-point discrimination, and improved level of function involving ADLs overall.
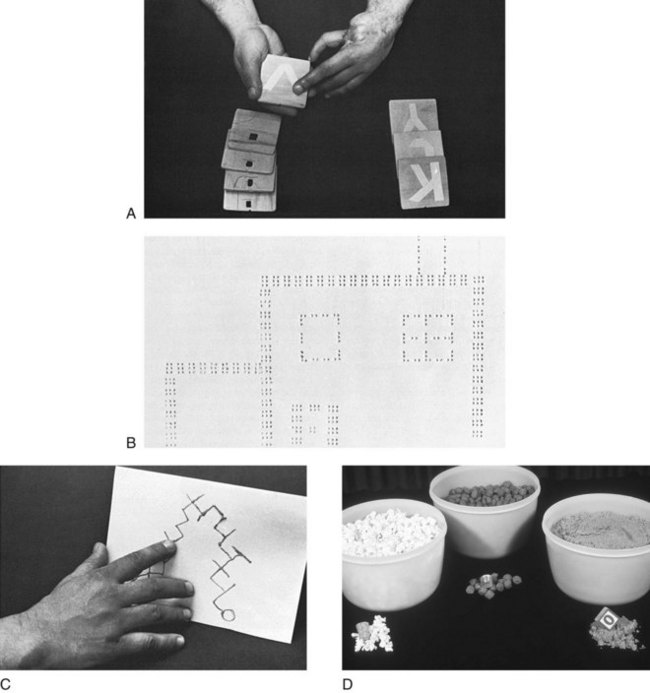
FIGURE 23-17 A, Identifying letters. B, Braille designs. C, Tracing the fingertip over finger mazes. D, Retrieving objects from containers filled with contact particles such as rice or beans for graded sensory re-education. (A-C, From Callahan AD: Therapist’s management of peripheral injuries. In Mackin EJ, Callahan AD, Skirven TM, et al, editors: Rehabilitation of the hand and upper extremity, ed 5, St. Louis, Mo, 2002, Mosby; D, from Fess EE: Sensory reeducation. In Mackin EJ, Callahan AD, Skirven TM, et al, editors: Rehabilitation of the hand and upper extremity, ed 5, St. Louis, Mo, 2002, Mosby.)
Summary
The most appropriate sensory tests for Mary would be touch pressure, two-point discrimination, and the Dellon modification of the Moberg Pickup Test. Test for touch pressure first since light touch must be intact for two-point discrimination to be tested. The Dellon modification of the Moberg Pickup Test is particularly appropriate for Mary because it looks at sensory function of the digits that carpal tunnel syndrome is affecting. Mary is a good candidate for both desensitization of the hypersensitive incision scar and discriminative sensory re-education to stimulate neural recovery. For instance, Mary could practice putting her earrings on in front of a mirror and grading the size of the earrings/fasteners. Tell Mary that typical recovery after successful carpal release includes decreased hypersensitivity as the desensitization program progresses. She should expect improving ability to feel and manipulate small objects as sensory recovery proceeds proximally to distally, with the fingertips being the last to recover. Deeper pressure will be felt before lighter pressure, and it will be easier to discern a nickel before she can discern a dime with vision occluded; this will progress as two-point discrimination improves.
1. What is the typical order of sensory recovery following peripheral nerve injury?
2. Explain why the fingertips have enhanced sensation when compared with more proximal body parts.
3. Name three signs that represent altered sympathetic nervous system status.
4. Explain how desensitization works.
5. What are the two categories of sensory re-education and how do they differ?
Acknowledgment
We thank Colleen G. West, MS, OTR/L, Genevieve Lebel, OTR/L, Shawn A. McGoogan, OTR/L, and Alex Pereda, MOT, OTR/L, for their review and feedback regarding this manuscript.
References
1. Barber, LM. Desensitization of the traumatized hand. In: Hunter JM, Schneider LH, Mackin EJ, Callahan AD, eds. Rehabilitation of the hand. ed 3. St. Louis, Mo: Mosby; 1990:721–730.
2. Bell-Krotoski, JA. Sensibility testing with the Semmes-Weinstein monofilaments. In: Mackin EJ, Callahan AD, Skirven TM, et al, eds. Rehabilitation of the hand and upper extremity. ed 5. St. Louis, Mo: Mosby; 2002:194–213.
3. Bell-Krotoski, J, Weinstein, S, Weinstein, C. Testing sensibility, including touch-pressure, two-point discrimination, point localization, and vibration. J Hand Ther. 1993;6:114–123.
4. Burleigh-Jacobs, A, Stehno-Bittel, L. Neuroplasticity. In: Lundy-Ekman L, ed. Neuroscience: fundamentals for rehabilitation. ed 2. Philadelphia, Pa: Saunders; 2002:67–80.
5. Calford, MB. Mechanisms for acute changes in sensory maps. Adv Exp Med Biol. 2002;508:451–460.
6. Callahan, AD. Sensibility assessment: prerequisites and techniques for nerve lesions in continuity and nerve lacerations. In: Hunter JM, Mackin EJ, Callahan AD, eds. Rehabilitation of the hand: surgery and therapy. ed 4. St. Louis, Mo: Mosby; 1995:129–152.
7. Engel, JM. Evaluation and pain management. In: Pendleton HM, Schultz-Krohn W, eds. Occupational therapy: practice skills for physical dysfunction. ed 6. St. Louis, Mo: Mosby; 2006:646–655.
8. Fess, EE. Sensory reeducation. In: Mackin EJ, Callahan AD, Skirven TM, et al, eds. Rehabilitation of the hand and upper extremity. ed 5. St. Louis, Mo: Mosby; 2002:635–639.
9. Koman, LA, Smith, BP, Smith, TL. Reflex sympathetic dystrophy (complex regional pain syndromes—types 1 and 2). In: Mackin EJ, Callahan AD, Skirven TM, et al, eds. Rehabilitation of the hand and upper extremity. ed 5. St. Louis, Mo: Mosby; 2002:1695–1706.
10. Lundy-Ekman, L. Somatosensory system. In: Lundy-Ekman L, ed. Neuroscience: fundamentals for rehabilitation. ed 3. St. Louis, Mo: Saunders; 2007:105–128.
11. Malaviya, GN. Sensory perception in leprosy—neurophysiological correlates. Int J Leprosy. 2003;71(2):119–124.
12. Merzenich, MM, Jenkins, WM. Reorganization of cortical representations of the hand following alterations of skin inputs induced by nerve injury, skin island transfers, and experience. J Hand Ther. 1993;6(2):89–104.
13. Novak, CB. Evaluation of hand sensibility: a review. J Hand Ther. 2001;14(4):266–272.
14. Ozcelik, IB, Tuncer, S, Purisa, H, et al. Sensory outcome of fingertip replantations without nerve repair. Microsurgery. 2008;28:524–530.
15. Rosen, B, Balkenius, C, Lundborg, G. Sensory re-education today and tomorrow: a review of evolving concepts. Br J Hand Ther. 2003;8(2):48–56.
16. Rosen, B, Bjorkman, A, Lundborg, G. Improved sensory relearning after nerve repair induced by selective temporary anaesthesia—a new concept in hand rehabilitation. J Hand Surg Eur Vol. 2006;31(2):126–132.
17. Shimojo, S, Shams, L. Sensory modalities are not separate modalities: plasticity and interactions. Curr Opin Neurobiol. 2001;11:505–509.
18. Skirven, TM, Callahan, AD. Therapist’s management of peripheral nerve injuries. In: Mackin EJ, Callahan AD, Skirven TM, et al, eds. Rehabilitation of the hand and upper extremity. ed 5. St. Louis, Mo: Mosby; 2002:599–621.
19. Wilson, FR. The hand: how its use shapes the brain, language, and human culture. New York: Pantheon Books; 1998.