Traditional Sensorimotor Approaches to Intervention
Section 1: Overview: the traditional sensorimotor intervention approaches
The Brunnstrom (movement therapy) approach
Proprioceptive neuromuscular facilitation approach
Section 2: Proprioceptive neuromuscular facilitation approach
After studying this chapter, the student or practitioner will be able to do the following:
1 Describe the four general processes of information flow related to control of movement.
2 Define motivational urge, and name the locus of this function in the brain.
3 Trace the flow of information in the central and peripheral nervous systems that leads to purposeful movement.
4 Define the sensorimotor system, its locus in the brain, and its function during motor performance.
5 List the structures that constitute the higher, middle, and lower levels of the central nervous system components for movement.
6 Name the four traditional sensorimotor approaches to intervention and the theorist responsible for each.
7 Name the two models of motor control that form the basis for the sensorimotor approaches to treatment.
8 Briefly describe each of the four traditional sensorimotor approaches to intervention; compare and contrast their similarities and their differences.
9 Understand and apply proprioceptive neuromuscular facilitation as a preparatory method to facilitate client participation in desired occupations.
10 Define proprioceptive neuromuscular facilitation and how this approach facilitates adaptive responses that are performed in daily occupations.
11 Understand the principles of proprioceptive neuromuscular facilitation and how to apply them to enhance client performance.
12 Describe the influence of sensory input on motor learning.
13 Use the proprioceptive neuromuscular facilitation evaluation to determine factors limiting clients’ participation in their occupation.
14 Recognize upper and lower extremity diagonal patterns in daily performance skills.
15 Name the theorists who developed the proprioceptive neuromuscular facilitation approach.
16 Discuss the historical background and current use of neurodevelopmental treatment within occupational therapy.
17 Identify theoretic foundations of neurodevelopmental treatment, as well as current principles of evaluation and intervention.
18 Identify management strategies associated with neurodevelopmental treatment intervention and treatment techniques.
19 Integrate neurodevelopmental treatment within an occupation-centered and client-centered approach to evaluation and intervention.
20 Discuss the relationship between evidence-based practice and neurodevelopmental treatment, and discuss types of evidence available to support the use of neurodevelopmental treatment in occupational therapy.
Overview
Neurologic Considerations for Traditional Sensorimotor Approaches to Intervention
Occupation performance frequently requires precise voluntary movement, which is controlled and monitored by the nervous system. Various structures within the nervous system are coordinated to selectively activate specific muscles to initiate, perform, and complete a desired task or activity. If a movement is performed poorly and thereby compromises performance of a task, feedback occurs through knowledge of the results of the action, and the neurologic commands to the muscles are modified so that accuracy of movement is achieved. Knowledge of the intricate working of the nervous system is of special importance to occupational therapists (OTs) concerned with refinement and improvement of the motor performance of clients with neurologic conditions.3 A brief overview of the flow of information associated with the control of movement is described in the following sections.
Central Nervous System Control of Movement
Firing of motor neurons located in the anterior horn of the spinal cord produces all movements.65 These neurons directly innervate the skeletal muscles. The activity of the spinal or lower motor neurons can be modulated by the segmental spinal circuitry and by the descending influence of the motor neurons located in the motor cortex and brainstem.39,40 These neurons are referred to as upper motor neurons. Two other structures, the basal ganglia and the cerebellum, as well as their associated pathways, are also intimately involved in motor control. Lesions in these structures are associated with characteristic movement disorders.
Production of movement does not begin and end with the upper or lower motor neurons. Many central nervous system (CNS) structures contribute to development of the signals that activate muscles. Although much about control of movement is still unknown, animal and human research suggests that four general processes are related to the flow of information needed to control movement. The four general processes of information flow are motivation, ideation, programming, and execution.8,13 A schematic diagram that indicates the main direction of information flow connecting the various motor centers appears in Figure 31-1.
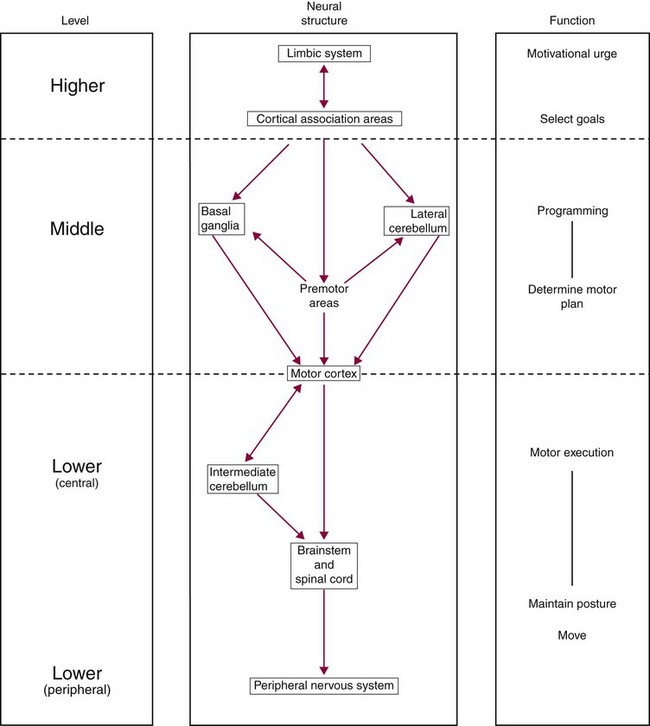
FIGURE 31-1 Schematic representation of the hierarchy of the neural structures involved in motor control. The left column indicates the hierarchic level and the right column the major function of the neural structures shown in the center column during motor performance. (Adapted from Cheney PD: Role of cerebral cortex in voluntary movements: a review, Phys Ther 65[5]:624, 1985.)
The motivation or emotive component of movement is a function of the limbic system.8,59 The motivational urge or impulse to act associated with the limbic system is transformed to ideas by the cortical association areas. This connection of knowledge and affective behavior is also referred to as conation.28 Conation represents the intentional, deliberate, and goal-directed aspect of behavior and is related to the individual’s reason for the motor performance. The association areas of the frontal, parietal, temporal, and occipital lobes are concerned with ideation, or the goal of the movement, and with the programming or movement strategy (plan) that best achieves the goal. Programming of a movement strategy also involves the premotor areas, the basal ganglia, and the cerebellum. The motor program is the procedure or the spatiotemporal order of muscle activation that is needed for smooth and accurate motor performance. The execution level, represented by the motor cortex, the cerebellum, and the spinal cord, is concerned with activation of the spinal motor neurons and interneurons that generate the goal-directed movement and the necessary postural adjustments.
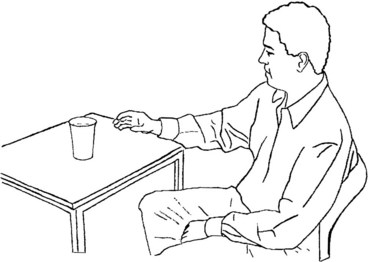
To appreciate the flow of information leading to purposeful movement, consider the actions of your client Carlos, who sustained a right cerebrovascular accident (CVA) with resultant left hemiplegia, is thirsty, and is reaching for a glass of water while seated at a table for support (Figure 31-2). The limbic system, which connects with the areas of the midbrain and brainstem that control vital functions such as hunger and thirst, has registered the need for water.26 This need for drinking water has been conveyed to the cortical association areas, which also received visual, auditory, somatosensory, and proprioceptive information about precisely where the body is in space and where the glass of water is relative to the body.30 This sensory information is needed before the movement is initiated. Strategies or motor plans are formulated to move the arm and hand from their immediate location in space to one in which the glass of water is picked up and moved to the mouth. Motor programs are generated by the association cortex in conjunction with the basal ganglia, lateral cerebellum, and premotor cortex. Once a strategy is selected, the motor cortex is activated. The motor cortex, in turn, conveys the action plan to the brainstem and spinal cord. Activation of the cervical spinal neurons generates a coordinated and precise movement of the shoulder, elbow, wrist, and fingers. Input from the brainstem and cerebellum ensures that the necessary postural adjustments are made by the axial musculature. Sensory information during the movement is necessary to ensure smooth performance of the ongoing movement and to improve subsequent similar movements. Because the motor areas rely heavily on sensory feedback provided by exteroceptors and proprioceptors regarding the accuracy of movement, the structures of the brain that control movement are often referred to as the sensorimotor system. Carlos is able to use his right hand to pick up the glass of water but has compromised postural control. When he is supported, sitting at the table, he is able to complete this task, but when standing and holding his cane in his right hand, he is unable to use his left arm and hand to reach and pick up the glass of water. The resultant motor problems from the right CVA further compromise his ability to perform a bimanual task such as pouring liquid into a glass even when he has the necessary motivational urge or intention for movement.
Given the motivation-ideation-programming-execution scheme of how information is organized through the nervous system, it is obvious that control of voluntary movement involves almost all of the neocortex. Voluntary movement depends on knowledge of where the body is in space, where the body intends to go with respect to this external space, the internal and external loads that must be overcome, and formulation of a strategy or plan to perform the movement. Once a strategy or plan has been formulated, it must be held in memory until execution, at which point appropriate instructions are sent to the spinal motor neurons. The primary functional aspects of the sensorimotor areas involved in motor control are examined in the next section.8,35,59
Sensorimotor Cortex: The sensorimotor cortex is the major integrating center of sensory input and motor output. It is composed of cortical areas located immediately anterior and posterior to the central sulcus (Figure 31-3). The three principal motor regions located in the frontal lobe are the primary motor area, the supplementary motor area, and the premotor area. The two principal sensory regions located in the parietal lobe are the primary somatosensory cortex and the posterior parietal cortex. Each area of the sensorimotor cortex (primary motor cortex, primary somatosensory cortex, posterior parietal cortex, supplementary motor area, and premotor cortex) is arranged in a manner that provides a topographic representation of the contralateral body segments.35,52 Each of these areas is responsible for certain aspects of generating movement. In the previous example of reaching for a glass of water, Carlos had a mental image of his body and its relation to the surrounding space by integrating the information supplied through somatosensory, proprioceptive, and visual input to the posterior parietal cortex. Clients with a lesion in this area demonstrate impairment of body image and its relation to extrapersonal space and, in the extreme situation, neglect of the contralateral body segments.
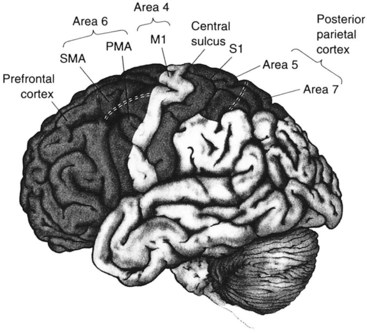
FIGURE 31-3 Areas of the neocortex intimately involved in planning of and instruction for voluntary movement. Areas 4 and 6 constitute the motor cortex. (From Bear MF, Connors BW, Paradiso MA: Neuroscience: exploring the brain, Baltimore, Md, 1996, Williams & Wilkins.)
The posterior parietal cortex integrates and translates sensory information so that the ensuing movements are directed appropriately in extrapersonal space. It is extensively interconnected with the association areas of the frontal lobe that are thought to be involved in determination of the consequences of movement strategies such as moving the arm forward, curling the fingers around the glass, and lifting the glass to the mouth. The fingers begin to curl appropriately before any contact occurs with the glass; therefore, the size and shape of the glass must be recognized before grasping. The prefrontal association areas and the posterior parietal cortex project to the premotor area, which is thought to be concerned with orientation of body segments before initiation of movement. The input of the posterior parietal cortex to the premotor area may be important in the somatosensory guidance of movement.13 Lesions of the premotor area or posterior parietal cortex have been demonstrated to result in the generation of an inappropriate movement strategy.32
Planning of movement is considered to be the function of the supplementary motor area. In animal studies, electrophysiologic recordings of cells in this area indicate that the cells typically increase discharge rates about a second before the observable execution of movement of either hand.69 The same findings have been corroborated in humans with the use of imaging techniques to study patterns of cortical activation. Imaging studies using positron emission tomography monitor changes in local blood flow because an increase in local cerebral blood flow is associated with increased neuronal activity. Under these conditions, when subjects were asked to imagine a movement without actually moving the finger, blood flow to the supplementary motor cortex increased and no comparable increase in blood flow was seen in the primary motor area.55 When subjects were asked to perform a series of finger movements from memory, blood flow to the supplementary motor cortex increased in advance of the movement but not during performance of the movement. Unilateral lesions of the supplementary motor area result in apraxia (loss of the ability to perform movement in the absence of motor or sensory impairments). Another effect of such lesions is an inability to produce the correct sequence of muscle activation for complex motor activities such as speaking, writing, buttoning, typing, sewing, and playing the piano.
The primary somatosensory cortex projection to the primary motor cortex and association areas provides the sensory input needed for motor planning, initiation of movement, and regulation of ongoing movement.20 The primary motor cortex integrates the information that it receives from other areas of the brain and generates the descending command for the execution of movement. Not only is this descending command sent to the brainstem and spinal cord, but a copy of it is also sent to the basal ganglia and cerebellum. The descending command specifies the muscles to be activated and the direction, speed, and required force.13 Lesions of the primary somatosensory cortex typically result in contralateral sensory loss. Movements are uncoordinated because the ability to register sensory feedback during and after the movement is compromised. Damage to the primary motor area results in deficits in motor execution. The client presents the classic picture of contralateral muscle weakness, spasticity, and poor isolation of movement with corresponding loss of function.
Relation to Sensorimotor Intervention Approaches
The CNS structures involved in movement can be grouped functionally into higher, middle, and lower levels. The higher level consists of the limbic system and association areas, where the motivation for action is generated. The sensorimotor areas, along with the basal ganglia and cerebellum, form the middle level, and the lower level consists of the nuclei in the brainstem and spinal cord. Under normal circumstances, an individual’s repertoire of motor activity is varied and complex to meet the unique task and environmental demands. After damage to the CNS regions involved in movement, the coordinated effort between the various levels of motor control is disrupted, and the motor response may be limited or stereotyped. Traditional sensorimotor approaches to intervention can be viewed as targeting the middle sensorimotor level, the motor planning–strategy formulation process, and the lower-level execution process, with the aim of reintegrating, as far as possible, a complete motor control hierarchy. It can easily be seen that a motor-relearning program (discussed in Chapter 32) should also be cognitively oriented and targeted toward achieving a goal or “occupational” task and include all three levels of CNS function related to motor control. This represents the inherent limitation of the traditional sensorimotor approaches. These approaches do not actively engage the client’s volitional intent or motivation to perform a motor act. The limitations of traditional sensorimotor approaches must be considered carefully before selecting this form of intervention for the client.
The foundational premise of these traditional sensorimotor approaches posits that clients need to be taught motor strategies or compensatory mechanisms to adapt to the deficits produced by a lesion. Compensatory mechanisms and the shaping of motor programs are brought about by the use of sensory input. The sensorimotor approaches use sensory stimulation to elicit specific movement patterns. Early in the intervention phase, emphasis is placed on the use of external sensory stimuli. Once a movement response is obtained, to reinforce and strengthen the response, the focus shifts to the use of intrinsic sensory information, which thereby encourages voluntary motor control.
The four traditional sensorimotor intervention approaches used historically by occupational therapy practitioners are the Rood approach, the Brunnstrom (movement therapy) approach, the proprioceptive neuromuscular facilitation (PNF) approach, and the neurodevelopmental treatment (Bobath or NDT) approach. These approaches, developed in the 1950s and 1960s, all have their theoretic basis in the reflex and hierarchic models of motor control. Although more contemporary models are currently being used to guide intervention in clients who demonstrate CNS dysfunction, an understanding of these traditional approaches is warranted to appreciate their contributions to clinical practice and to recognize appropriate application of these approaches in selected populations.
Reflex and Hierarchic Models of Motor Control
The reflex and hierarchic models of motor control view movement strategies along a developmental continuum. Two major fundamental assumptions underlie the reflex and hierarchic models.
The basic units of motor control are reflexes. Reflexes are motor responses that occur in response to specific sensory stimuli. Reflexes are automatic, predictable, and stereotypic; they are normal responses seen from early infancy. As the CNS matures, reflexes become integrated and are believed to form the foundation for volitional motor control. Volitional (purposeful) movement is the summation and integration of reflexive movement. When damage to the CNS occurs, a resurgence of reflexive motor activity takes place in addition to an inability to modulate these reflexive movements.
Motor control is hierarchically arranged. In a hierarchic model of motor control, the CNS is believed to have a specific organizational structure, and motor development and function depend on that structure. This hierarchic organization refers to a system in which the higher centers of the brain regulate and exert control over the lower centers of the CNS. The higher centers, specifically the cortical and subcortical areas, are responsible for regulation and control of volitional, conscious movement. The lower levels regulate and control reflexive, automatic, and responsive movement. Based on this conceptualization, when damage to the CNS occurs, it is believed that the damaged area can no longer regulate and exert control over the underlying areas. Motor control, according to this belief, becomes a function of the next lower functioning level of the CNS. Typically, this means a return to more reflexive and primitive movement patterns.
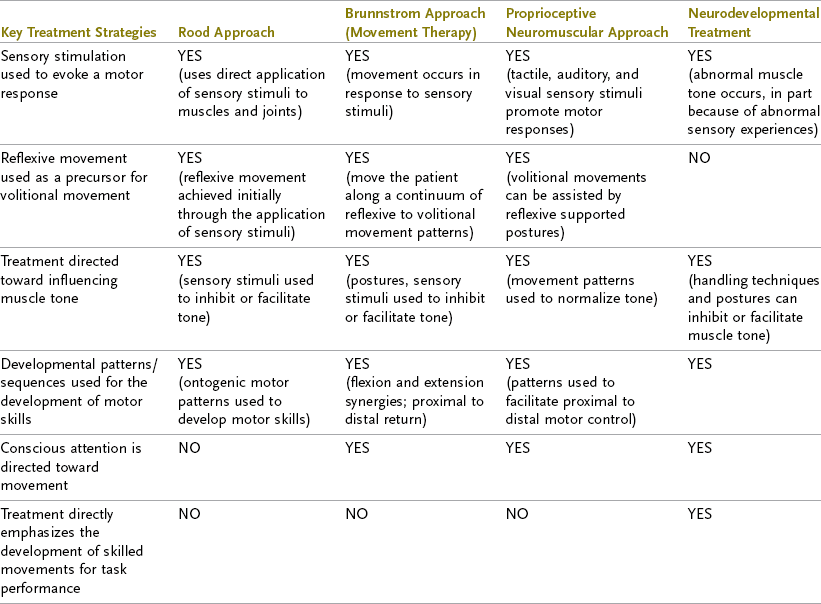
The four traditional sensorimotor intervention strategies rely heavily on these basic assumptions about motor development and motor control. Consequently, the intervention strategies used in these approaches frequently involve the application of sensory stimulation to muscles and joints to evoke specific motor responses, handling and positioning techniques to effect changes in muscle tone, and the use of developmental postures to enhance the ability to initiate and carry out movements. Table 31-1 presents a comparison and summary of the key treatment strategies used in each of the four traditional sensorimotor approaches.
Section 1 The Traditional Sensorimotor Intervention Approaches
The Rood Approach
Margaret Rood drew heavily from both the reflex and the hierarchic models in designing her intervention approach.56–58 Key components of the Rood approach are the use of sensory stimulation to evoke a motor response and the use of developmental postures to promote changes in muscle tone. Sensory stimulation is applied to muscles and joints to elicit a specific motor response. Stimulation has the potential to have either an inhibitory or a facilitatory effect on muscle tone. Types of sensory stimulation described by Rood include the use of slow rolling, neutral warmth, deep pressure, tapping, and prolonged stretch. Examples of how this stimulation may be applied include tapping over a muscle belly to facilitate (increase) muscle tone and applying deep pressure to a muscle’s tendinous insertion to elicit an inhibitory (decreased) effect. Rood also described the use of specific developmental sequences believed to promote motor responses.57 These sequences were proximal to distal and cephalocaudal. Treatment strategies move clients through these developmental sequences.
In current clinical practice, practitioners may use selected principles from Rood’s work as adjunctive or preliminary interventions to prepare an individual to engage in a purposeful activity—for example, application of quick stretch over the triceps before instructing a client to reach for a cup or glass to improve elbow extension.67 A client may be instructed in ways to apply his or her own sensory stimulation to enhance performance of activities of daily living (ADLs). For example, during upper extremity dressing, the OT may ask Carlos to perform a prolonged stretch of the left biceps; this results in a reduction in muscle tone, which may, in turn, increase the ease with which the arm is moved through the sleeve of his shirt.
Limitations in the use of Rood’s approach are numerous and include the passive nature of the sensory stimulation (it is applied “to” an individual) and the short-lasting and unpredictable effect of some of the sensory stimulation. Please refer to the discussion later in this chapter for additional details regarding the Rood approach to intervention.
The Brunnstrom (Movement Therapy) Approach
Signe Brunnstrom, a physical therapist (PT), developed an intervention approach specifically for individuals who had sustained a CVA.9,10 The approach that she designed draws strongly from both the reflex and hierarchic models of motor control. Brunnstrom conceptualized clients who had sustained a CVA as going through an “evolution in reverse.” Spastic or flaccid muscle tone and the presence of reflexive movements that may be evident after a client sustains a CVA are considered part of the normal process of recovery and are viewed as necessary intermediate steps in regaining volitional movement.62 Brunnstrom clearly detailed stages of motor recovery after a CVA (Table 31-2). These stages include the description of flexor synergy patterns and extensor synergy patterns for the upper and lower limbs and are used as descriptors of change following a CVA.23 Carlos currently displays flexor tone dominating his left arm and extensor tone dominating his left leg. This dominating tone interferes with isolated control of his left extremities.
TABLE 31-2
Motor Recovery After a Cerebrovascular Accident*
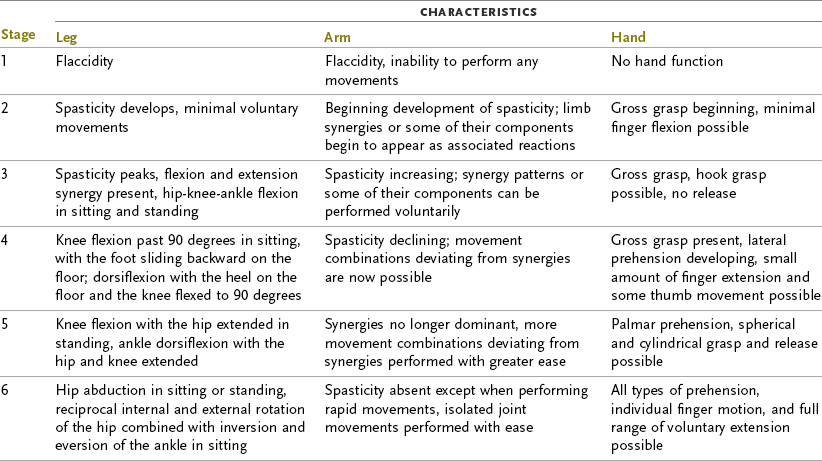
*Recovery of hand function is variable and may not parallel the six recovery stages of the arm.
From Brunnstrom S: Movement therapy in hemiplegia, New York, NY, 1970, Harper & Row.
In the Brunnstrom approach, emphasis is placed on facilitating the progress of the individual by promotion of movement, from reflexive to volitional. In the early stages of recovery this may include the incorporation of reflexes and associated reactions to change tone and achieve movement. For example, to generate reflexive movement in the arm, resistance may be applied to one side of the body to increase muscle tone on the opposite side. This technique is applied until the client demonstrates volitional control over the movement pattern.
Proprioceptive Neuromuscular Facilitation Approach
The PNF approach is grounded in the reflex and hierarchic models of motor control. Developed through the collaborative efforts of a physician, Dr. Herman Kabat, and two PTs, Margaret Knott and Dorothy Voss, in the 1950s, this intervention approach continues to be used but has not been revised since its origins. The major emphasis in this approach is on the developmental sequencing of movement and the balanced interplay between agonist and antagonist in producing volitional movement.74 PNF describes mass movement patterns, which are diagonal in nature, for the limbs and trunk. Intervention strategies use these patterns to promote movement. The use of sensory stimulation, including tactile, auditory, and visual input, is also actively incorporated into treatment to promote a motor response.
In clinical occupational therapy practice, the inclusion of PNF patterns can often be seen in the way that functional activities are designed, especially in the placement of objects during purposeful activities. For example, a client is asked to reach into a shopping bag placed on his left side to retrieve objects that will then be placed in a cabinet on his right side. Specific information regarding the application of PNF is discussed later in Section 2 of this chapter. This approach has been used successfully to increase range of motion (ROM) and for stretching of tightened muscles.64
Neurodevelopmental Treatment Approach
The NDT approach, also known as the Bobath treatment approach, is based on normal development and movement. Berta Bobath, a PT, and her husband Karel Bobath, a physician, provided the initial theoretic foundations of NDT in the 1950s.27 At that time they drew from the hierarchic model of motor control. The primary objectives of NDT are to normalize muscle tone, inhibit primitive reflexes, and facilitate normal postural reactions.5 Improving the quality of movement and helping clients relearn normal movement patterns are key objectives of this approach. To achieve these objectives, therapists use numerous techniques, including handling techniques, weight bearing over the affected limb, use of positions that encourage the use of both sides of the body, and avoidance of any sensory input that may adversely affect muscle tone.16 In clinical practice today, many of these techniques and strategies are used within the context of purposeful activities.
NDT has continued to revise its theoretic framework in response to new evidence on the function of the CNS.27 Discussions on the rationale for NDT include the current understanding of motor systems and motor learning. See Section 3 of this chapter for further descriptions.
Summary
Movement takes place within an occupational context. Emotional needs influence motor strategies. The spinal cord or brainstem can mediate reflexive responses, but interpretation and transformation of sensory signals by all areas of the sensorimotor system are essential for voluntary movement to occur with precision. The primary somatosensory cortex and posterior parietal cortex are primarily responsible for processing sensory information. The premotor area uses sensory information for planning movements, the supplementary motor area is important for bimanual coordination, and the motor cortex is important for execution.
The traditional sensorimotor intervention approaches have their theoretic basis in the reflex and hierarchic models of motor control. These approaches offer a valuable link between neurophysiologic principles and the rehabilitative treatment of clients with CNS dysfunction. In contemporary practice, many of the techniques described in these approaches are used as adjunctive or preliminary techniques or are incorporated into more task-directed treatment activities.
Section 2 Proprioceptive Neuromuscular Facilitation Approach
Based on normal movement and motor development, PNF is more than a technique—it is a philosophy of intervention. Through the case study of Leticia we will discuss the application of PNF in the evaluation and intervention of occupational therapy. Basic principles, diagonal patterns, and more commonly used techniques will be introduced, and their application and presence in routine daily life skills will be demonstrated. PNF addresses the client factors of posture, mobility, strength, effort, and coordination. To use PNF effectively, it is necessary to understand normal development, learn the motor skills to use the techniques, and apply the concepts and techniques to occupational therapy activities.4 This section should form the basis for further reading and training under the supervision of a therapist experienced in PNF.
PNF is based on normal movement and motor development. In normal motor activity the brain registers total movement and not individual muscle action.31 Encompassed in the PNF approach are mass movement patterns that are spiral and diagonal in nature and that resemble the movement seen in functional activities. In this multisensory approach, facilitation techniques are superimposed on movement patterns and postures through manual contact, verbal commands, and visual cues by the therapist. These facilitation techniques and movement patterns can be preparatory methods that prepare the client to participate more effectively in daily occupations or be applied within the performance of a task.
PNF is used as an intervention technique for numerous conditions, including Parkinson’s disease, spinal cord injuries, arthritis, stroke, head injuries, and hand injuries. It has been effectively combined with neuromobilization techniques to reduce sensory deficits in individuals who have sustained a CVA.76
History
PNF originated with Dr. Herman Kabat, physician and neurophysiologist, in the 1940s. He applied neurophysiologic principles, based on the work of Sherrington, to interventions for paralysis secondary to poliomyelitis and multiple sclerosis. In 1948, Kabat and Henry Kaiser founded the Kabat-Keiser Institute in Vallejo, California. Here, Kabat worked with PT Margaret Knott to develop the PNF method of intervention. By 1951 the diagonal patterns and core techniques were established. PNF is now used to treat numerous neurologic, musculoskeletal, and general medical conditions.
In 1952 Dorothy Voss, a PT, joined the staff at the Kaiser-Kabat Institute. She and Knott undertook the teaching and supervision of staff therapists. In 1954 Knott and Voss presented the first 2-week course in Vallejo. Two years later, the first edition of Proprioceptive Neuromuscular Facilitation by Margaret Knott and Dorothy Voss was published by Harper & Row.
During this same period several reports in the American Journal of Occupational Therapy described PNF and its application to occupational therapy intervention.4,12,14,34,71,75 It was not until 1974 that the first PNF course for OTs, taught by Dorothy Voss, was offered. Since then, Beverly Myers, an OT, and others have offered courses for OTs throughout the United States. In 1984, PNF was first taught concurrently to both PTs and OTs at the Rehabilitation Institute in Chicago.49,74 Today, courses are offered throughout the United States, as well as Europe, Asia, and South America.
Principles of Intervention
Voss presented 11 principles of intervention at the Northwestern University Special Therapeutic Exercise Project in 1966. These principles were developed from concepts in the fields of neurophysiology, motor learning, and motor behavior and are still essential to the practice of PNF today.72
All human beings have potentials that have not been fully developed. This philosophy is the underlying basis of PNF. Therefore, during evaluation and intervention planning, the client’s abilities and potentials are emphasized. For example, a client who has weakness on one side of the body can use the intact side to assist the weaker part. Likewise, a client who has hemiplegia with a flaccid arm can use the intact head, neck, and trunk musculature to begin reinforcement of the weak arm in weight-bearing activities.
Normal motor development proceeds in a cervicocaudal and proximodistal direction. The cervicocaudal and proximodistal direction is followed in evaluation and intervention. When severe disability is present, attention is first directed to the head and neck region, with its visual, auditory, and vestibular receptors, and then to the upper part of the trunk and extremities. If the superior region is intact, an effective source of reinforcement for the inferior region is available.74 The proximodistal direction is followed by developing adequate function in the head, neck, and trunk before developing function in the extremities. This approach is of particular importance in interventions that facilitate fine motor coordination in the upper extremities. Unless adequate control exists in the head, neck, and trunk region, fine motor skills cannot be developed effectively. For example, Leticia needs to strengthen her head, neck, and trunk muscles to regain adequate postural control before she can adequately perform the fine motor tasks required in her job, such as cutting with scissors. This illustrates how addressing a specific client factor of postural control can influence occupational performance.
Early motor behavior is dominated by reflex activity. Mature motor behavior is supported or reinforced by postural reflexes. As humans mature, primitive reflexes are integrated and available for reinforcement to allow progressive development, such as rolling, crawling, and sitting. Reflexes have also been noted to have an effect on changes in tone in the extremities. Hellebrandt, Schade, and Carns studied the effect of the tonic neck reflex and the asymmetric tonic neck reflex on changes in tone and movement in the extremities of normal adults.25 They found that head and neck movement significantly affected arm and leg movement. In applying this finding to intervention, for example, weak elbow extensors can be reinforced with the asymmetric tonic neck reflex by having the client look toward the side of weakness. Likewise, the client can be assisted in assuming postures with the influence of reflex support. For example, Leticia can use the body-on-body righting reflex to support her ability to assume sitting upright on the edge of the bed from a side-lying position when she gets up in the morning.
Early motor behavior is characterized by spontaneous movement, which oscillates between extremes of flexion and extension. These movements are rhythmic and reversing in character. During intervention it is important to attend to both directions of movement. When the occupational therapy practitioner is working with a client on getting up from a chair, attention must also be given to sitting back down. Often with an injury, the eccentric contraction (e.g., sitting down) is lost and becomes very difficult for the client to regain. If not properly treated, the client may be left with inadequate motor control to sit down smoothly and thus may “drop” into a chair. This eccentric control would be particularly important for Leticia because she is required to sit in low chairs at her children’s school. Similarly, in training for ADLs the client must learn how to get undressed and dressed.
Developing motor behavior is expressed in an orderly sequence of total patterns of movement and posture. In a normal infant the sequence of total patterns is demonstrated through the progression of locomotion. The infant learns to roll, to crawl, to creep, and finally to stand and walk. Throughout these stages of locomotion the infant also learns to use the extremities in different patterns and within different postures. Initially, the hands are used for reaching and grasping within the most supported postures, such as supine and prone. As postural control develops, the infant begins to use the hands in side-lying, sitting, and standing positions. During intervention, to maximize motor performance, clients should be given opportunities to work in a variety of developmental postures. Use of the extremities in total patterns requires interaction with component patterns of the head, neck, and trunk. For example, when swinging a tennis racquet in a forehand stroke, the arm and the head, neck, and trunk move in the direction of the swing. Without the interaction of the distal and proximal components, movement becomes less powerful and less coordinated.
The growth of motor behavior has cyclic trends, as evidenced by shifts between flexor and extensor dominance. The shifts between antagonists help develop muscle balance and control. One of the main goals of the PNF intervention approach is to establish a balance between antagonists. Developmentally, the infant establishes this balance before creeping (i.e., when rocking forward [extensor dominant] and backward [flexor dominant] on hands and knees). Postural control and balance must be achieved before movement can begin in this position. During intervention it is important to establish a balance between antagonistic muscles by first observing where imbalance exists and then facilitating the weaker component. For example, if a client who has sustained a stroke demonstrates flexor synergy (flexor dominant), extension should be facilitated.
Normal motor development has an orderly sequence but lacks a step-by-step quality. Overlapping of skills occurs. A child does not perfect performance of one activity before beginning another, more advanced activity. When trying to ascertain in which total pattern to position the client, normal motor development should be heeded. If one technique or developmental posture is not effective in obtaining the desired result, it may be necessary to try the activity in another developmental posture. For example, if a client who has ataxia, such as Leticia, is unable to perform a fine motor task while sitting, it may be necessary to practice skills in a more supported posture, such as prone on the elbows or with her elbows supported on a surface such as a table. Just as the infant reverts to a more secure posture when attempting a complex fine motor task, so must the client. On the other hand, if the client has not perfected a motor activity such as walking on level surfaces, he or she may benefit from attempting a higher-level activity such as walking up or down stairs, which in turn can improve ambulation on level surfaces. It is natural for the client to move up and down the developmental sequence, and this allows multiple and varied opportunities for practicing motor activities. The cognitive demands of the task in relation to the developmental posture must also be considered. When the client’s position is varied, either by changing the base of support or by shifting weight on different extremities, the quality of visual and cognitive processing is influenced.1
Locomotion depends on the reciprocal contraction of flexors and extensors, and maintenance of posture requires continual adjustment for nuances of imbalance. Antagonistic pairs of movements, reflexes, and muscles and joint motion interact as necessary with the movement or posture. This principle restates one of the main objectives of PNF—to achieve a balance between antagonists. An example of imbalance is a client with a head injury who is unable to maintain adequate sitting balance for a tabletop cognitive activity because of a dominance of trunk extensor tone. Another example is a client who has hemiplegia with tight finger flexors secondary to a flexor-dominant tone in the hand. During intervention, emphasis is placed on correcting the imbalances. In a client with spasticity, first the spasticity is inhibited and then the antagonistic muscles, reflexes, and postures are facilitated.
Improvement in motor ability is dependent on motor learning. Multisensory input from the therapist facilitates motor learning in the client and is an integral part of the PNF approach. For example, the therapist may work with a client on a shoulder flexion activity such as reaching into a cabinet for a cup. The therapist may say, “Reach for the cup,” to add verbal input. This approach also encourages the client to look in the direction of the movement to allow vision to enhance the motor response. Thus, tactile, auditory, and visual input is used. Motor learning has occurred when these external cues are no longer needed for adequate performance.
Frequent stimulation and repetitive activity are used to promote and retain motor learning and to develop strength and endurance. Just as a therapist who is learning PNF needs the opportunity to practice the techniques, a client needs the opportunity to practice new motor skills. With practice, habits will be formed that support motor performance in occupation. In the process of development an infant constantly repeats a motor skill in many settings and developmental postures until it is mastered, as becomes apparent to anyone who watches a child learning to walk. Numerous attempts fail, but efforts are repeated until the skill is mastered. After the activity is learned, it becomes part of the child. He or she is able to use the activity automatically and deliberately as the occasion demands.74 The same is true for a person learning to play the piano or to play tennis. Without the opportunity to practice, motor learning cannot occur successfully. Just as Leticia’s students may be given homework to help them practice the material that they learn in school, Leticia will also need to be given a home program that encourages her to practice the postures and movements facilitated in therapy.
Goal-directed activities coupled with techniques of facilitation are used to hasten learning of total patterns of walking and self-care activities. When facilitation techniques are applied to self-care, the objective is improved functional ability, but improvement is achieved by more than instruction and practice. Correction of deficiencies is accomplished by direct application of manual contact and techniques to facilitate a desired response.29 During an intervention session, this approach may mean applying stretch to the finger extensors to facilitate release of an object or providing joint approximation through the shoulders and pelvis of a client who has ataxia to provide stability while the client is standing to wash dishes. With repetition of appropriate facilitation techniques, Leticia will have the opportunity to feel more normal movement and need to rely less on the therapist’s external input.
Motor Learning
Motor learning requires a multisensory approach. The auditory, visual, and tactile systems are all used to achieve the desired response. The correct combination of sensory input in each client should be ascertained, implemented, and altered as the client progresses. The developmental level of the client and the ability to cooperate should also be taken into consideration.74 The approach used with a client who has aphasia differs from that used with a client who has a hand injury. For example, verbal instructions would be better understood by the client with a hand injury than the client with aphasia. Less verbal and more tactile and gestural cues would be appropriate with the client who has aphasia. Similarly, the approach used with a child varies greatly from that used with an adult. Interventions with Leticia must take into consideration her visual deficits in addition to any cognitive impairment that remains as a result of her head injury.
Auditory System
Verbal commands should be brief and clear. It is important to time the command so that it does not come too early or too late in relation to the motor act. Tone of voice may influence the quality of the client’s response. Buchwald states that tones of moderate intensity evoke gamma motor neuron activity and that louder tones can alter alpha motor neuron activity.11 Strong, sharp commands simulate a stress situation and are used when maximal stimulation of motor response is desired. A soft tone of voice is used to offer reassurance and to encourage a smooth movement, as in the presence of pain (e.g., when techniques are used to increase mobility in Leticia’s left wrist). When a client is giving the best effort, a moderate tone can be used.74
Another effect of auditory feedback on motor performance was studied by Loomis and Boersma.40 They used a “verbal mediation strategy” to teach wheelchair safety before clients with right CVA transferred out of the chair. Loomis and Boersma taught clients to say aloud the steps required to leave the wheelchair safely and independently. They found that only clients who used verbal mediation learned the wheelchair drill sufficiently to perform safe and independent transfers. These clients also had better retention of the sequence of steps, which suggests that verbal mediation is beneficial in reaching independence with better sequencing and fewer errors.
When Leticia first arrived in therapy, she suffered considerable pain at the site of her wrist fracture. Early PNF intervention should use soft verbal commands when activities that involve wrist mobility are performed. In contrast, when facilitating Leticia’s ability to perform assumption of postures (i.e., moving from side lying to tall kneeling), more forceful, sharp commands may be needed.
Visual System
Visual stimuli assist in initiation and coordination of movement. Visual input should be monitored to ensure that the client is tracking in the direction of movement. For example, the therapist’s position is important because the client often uses the therapist’s movement or position as a visual cue. If the therapist desires Leticia to move in a forward direction, the therapist should be positioned diagonally in front of the client. In addition to the therapist’s position, placement of the occupational therapy activity should also be considered. Using one of her children’s favorite board games, the therapist could place it in front and to the left of Leticia to achieve the goal of increased head, neck, and trunk rotation. Because occupational therapy is activity oriented, an abundance of visual stimuli is offered to the client.
Special consideration will need to be given to the use of vision when working with Leticia. Her stronger head and neck musculature can be used to reinforce oculomotor control. Total body and extremity diagonal patterns can be used to reinforce eye teaming.
Tactile System
Developmentally the tactile system matures before the auditory and visual systems.17 Furthermore, the tactile system is more efficient because it has temporal and spatial discrimination abilities, as opposed to the visual system, which can make only spatial discriminations, and the auditory system, which can make only temporal discriminations.22 Affolter stated that during development, processing of tactile-kinesthetic information can be considered fundamental for building cognitive and emotional experience.2 Looking at and listening to the world do not result in change; however, the world cannot be touched without some change taking place. A Chinese proverb often cited in PNF courses reinforces this viewpoint: “I listen and I forget, I see and I remember, I do and I understand.”
It is important for the client to feel movement patterns that are coordinated and balanced. This is particularly important for clients with ataxia, such as Leticia. With the PNF approach, tactile input is supplied through manual contact with the therapist to guide and reinforce the desired response. This approach may involve gently touching the client to guide movement, using stretch to initiate movement, and providing resistance to strengthen movement. The type and extent of manual contact depend on the client’s clinical status, which is determined through evaluation and re-evaluation. For example, the use of stretch or resistance in an individual with musculoskeletal instability may be contraindicated, as in the early healing phases of Leticia’s fractures. Likewise, stretch or resistance should not be used if they cause increased pain or an imbalance in tone.
To increase speed and accuracy in motor performance, the client needs the opportunity to practice. Through repetition, habit patterns that occur automatically without voluntary effort are established. The PNF approach uses the concepts of part-task practice and whole-task practice. In other words, to learn the whole task, emphasis is placed on the parts of the task that the client is unable to perform independently. The term stepwise procedures is descriptive of the emphasis on a part of the task during performance of the whole.74 Performance of each part of the task is improved by combining practice with appropriate sensory cues and techniques of facilitation. For example, a client learning to transfer from a wheelchair to a tub bench may have difficulty lifting the leg over the tub rim. This part of the task should be practiced, with repetition and facilitation techniques involving the hip flexors, during performance of the transfer. When the transfer becomes smooth and coordinated, it is no longer necessary to practice each part individually. It is also unnecessary for the therapist to provide continued facilitation.
Leticia has difficulty getting down on the floor to play games with her children. During intervention she should be provided with facilitation and practice in moving from sitting on a chair to tall kneeling to side sitting on the floor. She will initially require considerable manual facilitation by the therapist to move through and achieve these various movement patterns. As she develops more skill, the therapist will reduce and adjust the intensity of the tactile input.
In summation, several components are necessary for motor learning to occur. In the PNF intervention approach, these components include multisensory input from the therapist’s verbal commands, visual cues, and manual contact. Touch is the most efficient form of stimulation and provides the opportunity for the client to feel normal movement. Current motor-learning theory argues that for motor learning to occur, the client cannot be a passive recipient of intervention. Therefore, the client needs opportunities to practice motor skills in the context of functional life situations. Initially, the therapist’s manual contact and sensory input are needed. These should be decreased, however, as the client demonstrates and learns skilled movement. The amount of feedback from the therapist should also be decreased as the client learns to rely on his or her own internal feedback system for error detection and correction.
Assessment
Assessment of the client requires astute observational skills and knowledge of normal movement. An initial assessment is performed to determine the client’s abilities, deficiencies, and potential. After the intervention plan is established, ongoing assessment of the client is necessary to ascertain the effectiveness of intervention and to make modifications as the client changes.
The PNF assessment follows a sequence from proximal to distal. First, vital and related functions are considered, such as breathing, swallowing, voice production, facial and oral musculature, and visual-ocular control. Any impairment or weakness in these functions is noted. Because Leticia fatigues quickly, breathing patterns and efficiency need to be closely evaluated as she engages in her daily activities.
The head and neck region is observed after vital functions. Deficiencies in this area directly affect the upper part of the trunk and extremities. Head and neck positions are observed in varying postures and total patterns during functional activities. It is important to note (1) dominance of tone (flexor or extensor), (2) alignment (midline or shift to one side), and (3) stability and mobility (more or less needed).49
After observation of the head and neck region, the assessment proceeds to the following parts of the body: upper part of the trunk, upper extremities (UEs), lower part of the trunk, and lower extremities (LEs). Each segment is assessed individually in specific movement patterns, in addition to during developmental activities in which the body segments interact. For example, shoulder flexion can be observed in an individual UE movement pattern, in addition to during a total developmental pattern such as rolling.
During assessment of developmental activities and postures, the following issues should be addressed:
• Is more stability or mobility needed?
• Is there a balance between the flexors and extensors, or is one more dominant?
• Is the client able to move in all directions?
• What are the client’s major limitations (e.g., weakness, incoordination, spasticity, and contractures)?
• Is the client able to assume a posture and maintain it? If not, which total pattern or postures are inadequate?
• Are the inadequacies more proximal or distal?
• Which sensory input does the client respond to most effectively—auditory, visual, or tactile?
• Which techniques of facilitation does the client respond to best?
When applying these questions to Leticia’s evaluation, the following observations can be made. First, Leticia will need to work on developing stability to diminish the effects of her ataxia. She is not dominated by either flexor or extensor tone but, when fatigued, has more difficulty maintaining an upright posture. She will therefore need to have facilitation of the head, neck, and trunk extensors when fatigued. She can move in all directions but has less stability when walking backward. Her major limitations are poor motor control and rigidity, but prevention of a wrist contracture is also a concern. Leticia is having difficulty assuming kneeling, sitting, and standing postures because of her instability. Once in an upright posture, she can maintain it for a few minutes, but fatigue then sets in. She will therefore need to build endurance in more supported lower developmental postures. When moving into more upright postures, she will need PNF techniques to build strength and endurance. Her inadequate proximal control and trunk rigidity affect her ability to effectively use her extremities, especially in higher developmental positions. Visual sensory input may not be the best to start with because of her diplopia; however, facilitation of oculomotor control using PNF techniques will be of benefit as she progresses. The facilitation techniques that Leticia responds to best are rhythmic stabilization, stabilizing reversals, and approximation.
Finally, the client is observed during self-care and other ADLs to determine whether performance of individual and total patterns is adequate within the context of a functional activity. The client’s performance may vary from one setting to another. After the client leaves the structured setting of the occupational or physical therapy clinic for the less structured home or community environment, deterioration of motor performance is not unusual. Thus, the intervention plan must accommodate the practice of motor performance in a variety of settings in locations appropriate to the specific activity.
Intervention Implementation
After assessment, an intervention plan is developed that includes goals that the client hopes to accomplish. The techniques and procedures that have the most favorable influence on movement and posture are used. Similarly, appropriate total patterns (developmental postures) and patterns of facilitation are selected to enhance performance.
Diagonal Patterns
The diagonal patterns used in the PNF approach are the mass movement patterns observed in most functional activities. Part of the challenge in occupational therapy assessment and intervention is recognition of the diagonal patterns in ADLs. Knowledge of the diagonals is necessary for identifying areas of deficiency. Two diagonal motions are present for each major part of the body: head and neck, upper and lower parts of the trunk, and extremities. Each diagonal pattern has a flexion and extension component, together with rotation and movement away from or toward the midline.
The head, neck, and trunk patterns are referred to as (1) flexion with rotation to the right or left and (2) extension with rotation to the right or left. These proximal patterns combine with the extremity diagonals. The UE and LE diagonals are described according to the three movement components at the shoulder and hip: (1) flexion and extension, (2) abduction and adduction, and (3) external and internal rotation. Voss introduced shorter descriptions for the extremity patterns in 1967 and referred to them as diagonal 1 (D1) flexion/extension and diagonal 2 (D2) flexion/extension.72 The reference points for flexion and extension are the shoulder and hip joints of the UEs and LEs, respectively.
The movements associated with each diagonal and examples of these patterns seen in self-care and other ADLs are presented in the following sections. Note that during functional activities, not all components of the pattern or full ROM are necessarily seen. Furthermore, the diagonals interact during functional movement, changing from one pattern or combination to another, when they cross the transverse and sagittal planes of the body.48
1. UE D1 flexion (shoulder flexion-adduction–external rotation): Scapula elevation, abduction, and rotation; shoulder flexion, adduction, and external rotation; elbow in flexion or extension; forearm supination; wrist flexion to the radial side; finger flexion and adduction; and thumb adduction (Figure 31-4, A). Examples in functional activity: hand-to-mouth motion in feeding, tennis forehand, combing the hair on the left side of the head with the right hand (Figure 31-5, A), and rolling from supine to prone.
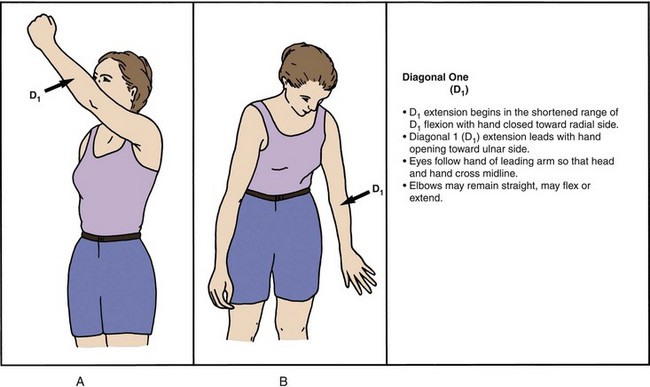
FIGURE 31-4 A, Upper extremity D1 flexion pattern. B, Upper extremity D1 extension pattern. (From Myers BJ: Unit I: PNF diagonal patterns and their application to functional activities, videotape study guide, Chicago, Ill, 1982, Rehabilitation Institute of Chicago.)
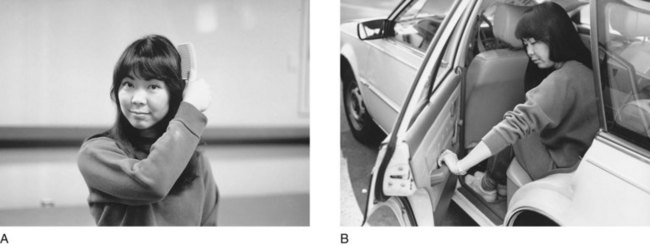
FIGURE 31-5 A, Upper extremity D1 flexion pattern used to comb the hair, opposite side. B, Upper extremity D1 extension pattern used to push a car door open.
2. UE D1 extension (shoulder extension-abduction–internal rotation): Scapula depression, adduction, and rotation; shoulder extension, abduction, and internal rotation; elbow in flexion or extension; forearm pronation; wrist extension to the ulnar side; finger extension and abduction; and thumb in palmar abduction (Figure 31-4, B). Examples in functional activity: pushing a car door open from the inside (Figure 31-5, B), tennis backhand stroke, and rolling from prone to supine.
3. UE D2 flexion (shoulder flexion-abduction–external rotation): Scapula elevation, adduction, and rotation; shoulder flexion, abduction, and external rotation; elbow in flexion or extension; forearm supination; wrist extension to the radial side; finger extension and abduction; and thumb extension (Figure 31-6, A). Examples in functional activity: combing the hair on the right side of the head with the right hand (Figure 31-7, A), lifting a racquet in a tennis serve, and back stroke in swimming. The D2 flexion pattern would be emphasized in Leticia’s left UE to facilitate supination and wrist extension, which are weak secondary to her wrist fracture.
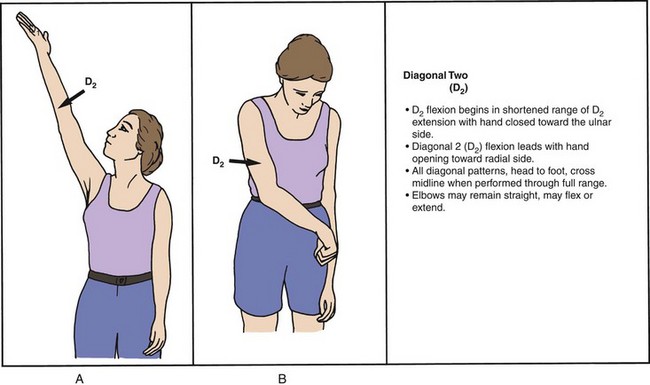
FIGURE 31-6 A, Upper extremity D2 flexion pattern. B, Upper extremity D2 extension pattern. (From Myers BJ: Unit I: PNF diagonal patterns and their application to functional activities, videotape study guide, Chicago, Ill, 1982, Rehabilitation Institute of Chicago.)
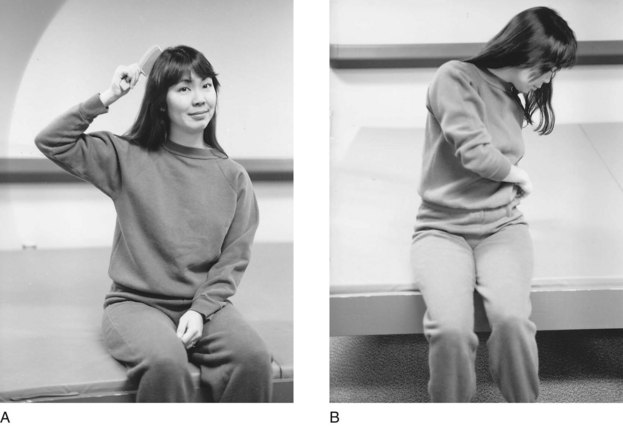
FIGURE 31-7 A, Upper extremity D2 flexion pattern used to comb the hair, same side. B, Upper extremity D2 extension pattern used to button trousers, opposite side.
4. UE D2 extension (shoulder extension-adduction–internal rotation): Scapula depression, abduction, and rotation; shoulder extension, adduction, and internal rotation; elbow in flexion or extension; forearm pronation; wrist flexion to the ulnar side; finger flexion and adduction; and thumb opposition (see Figure 31-6, B). Examples in functional activity: pitching a baseball, hitting a ball during a tennis serve, and buttoning pants on the left side with the right hand (see Figure 31-7, B). The rotational component in LE D1 flexion and extension parallels the UE patterns.
5. LE D1 flexion (hip flexion-adduction–external rotation): Hip flexion, adduction, and external rotation; knee in flexion or extension; and ankle and foot dorsiflexion with inversion and toe extension. Examples in functional activity: kicking a soccer ball, rolling from supine to prone, and putting on a shoe with the legs crossed (Figure 31-8, A).
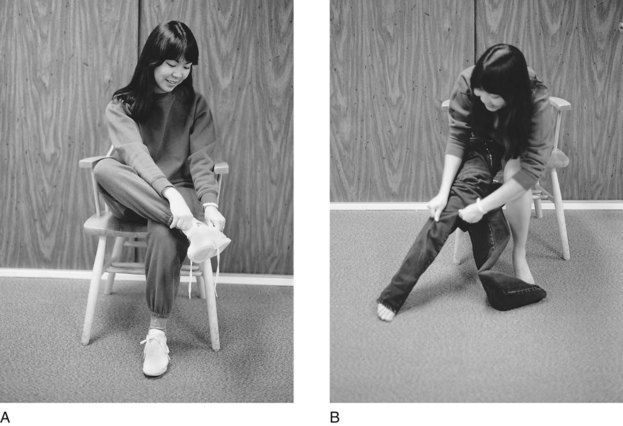
FIGURE 31-8 A, Lower extremity D1 flexion pattern demonstrated when crossing the leg to put on a shoe. B, Lower extremity D1 extension pattern used when pulling on trousers.
6. LE D1 extension (hip extension-abduction–internal rotation): Hip extension, abduction, and internal rotation; knee in flexion or extension; and ankle and foot plantar flexion with eversion and toe flexion. Examples in functional activity: putting a leg into pants (Figure 31-8, B) and rolling from prone to supine. The rotational component of LE D2 flexion and extension is opposite that in the UE patterns.
7. LE D2 flexion (hip flexion-abduction–internal rotation): Hip flexion, abduction, and internal rotation; knee in flexion or extension; and ankle and foot dorsiflexion with eversion and toe extension. Examples in functional activity: karate kick (Figure 31-9, A) and drawing the heels up during the breaststroke in swimming.
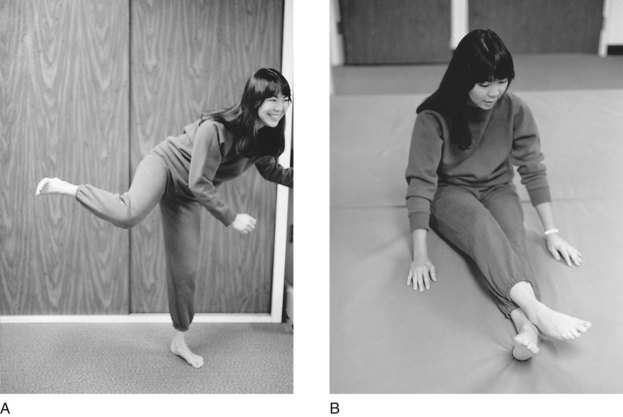
FIGURE 31-9 A, Lower extremity D2 flexion pattern shown in a karate kick. B, Lower extremity D2 extension pattern used in long sitting with the legs crossed.
8. LE D2 extension (hip extension-adduction–external rotation): Hip extension, adduction, and external rotation; knee in flexion or extension; and ankle and foot plantar flexion with inversion and toe flexion. Examples of functional activity: push-off in gait, the kick during the breaststroke in swimming, and long sitting with the legs crossed (Figure 31-9, B).
Bilateral Patterns: Movements in the extremities may be reinforced by combining diagonals in bilateral patterns as follows:
1. Symmetric patterns: Paired extremities perform similar movements at the same time (Figure 31-10, A). Examples: bilateral symmetric D1 extension, such as pushing off a chair to stand (Figure 31-11, A); bilateral symmetric D2 extension, such as starting to take off a pullover sweater (Figure 31-11, B); and bilateral symmetric D2 flexion, such as reaching to lift a large item off a high shelf (Figure 31-11, C). Bilateral symmetric UE patterns facilitate trunk flexion and extension.
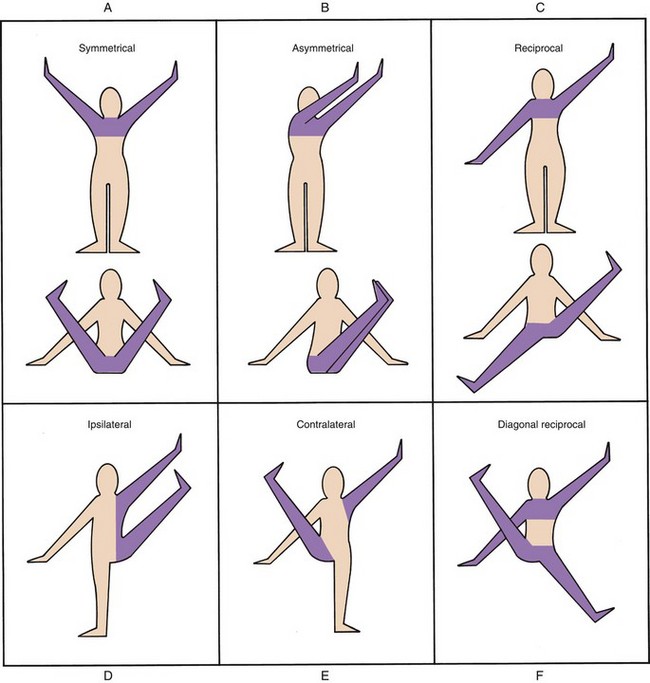
FIGURE 31-10 A, Symmetric patterns. B, Asymmetric patterns. C, Reciprocal patterns. D, Ipsilateral pattern. E, Contralateral pattern. F, Diagonal reciprocal pattern. (From Myers BJ: Unit I: PNF diagonal patterns and their application to functional activities, videotape study guide, Chicago, Ill, 1982, Rehabilitation Institute of Chicago.)
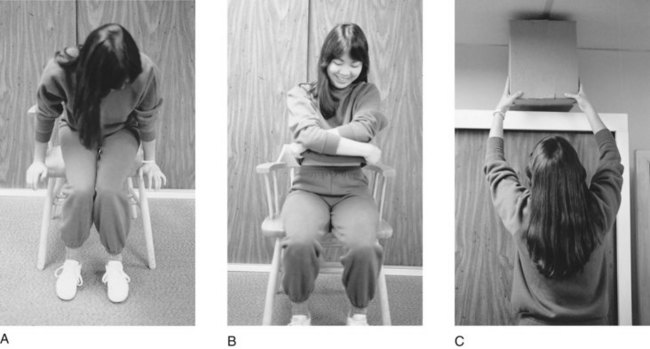
FIGURE 31-11 A, Upper extremity bilateral symmetric D1 extension pattern shown when pushing off from a chair. B, Upper extremity bilateral symmetric D2 extension pattern used when starting to take off a pullover shirt. C, Upper extremity bilateral symmetric D2 flexion pattern used when reaching to lift a box off a high shelf.
2. Asymmetric patterns: Paired extremities perform movements toward one side of the body at the same time, which facilitates trunk rotation (see Figure 31-10, B). The asymmetric patterns can be performed with the arms in contact, such as in the chopping and lifting patterns in which greater trunk rotation is seen (Figures 31-12 and 31-13). Furthermore, with the arms in contact, self-touching occurs. This is frequently observed in those with pain or in reinforcement of a motion when greater control or power is needed.74 This phenomenon is observed in a baseball player at bat and in a tennis player who uses a two-handed backhand to increase control and power. Asymmetric patterns with the arms in contact would be beneficial for Leticia to control ataxia. Examples of asymmetric patterns are bilateral asymmetric flexion to the left with the left arm in D2 flexion and the right arm in D1 flexion, such as when putting on a left earring (Figure 31-14), and bilateral asymmetric extension to the left with the right arm in D2 extension and the left arm in D1 extension, such as when zipping a left-sided zipper.
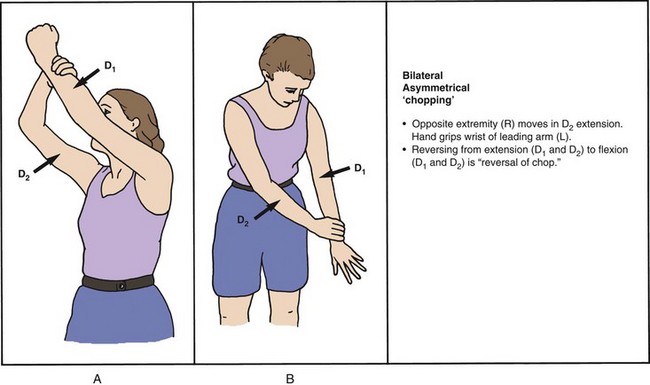
FIGURE 31-12 Bilateral asymmetric chopping. (From Myers BJ: Unit I: PNF diagonal patterns and their application to functional activities, videotape study guide, Chicago, Ill, 1982, Rehabilitation Institute of Chicago.)
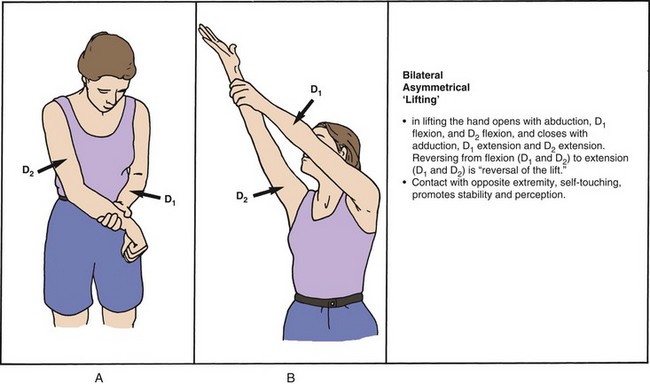
FIGURE 31-13 Bilateral asymmetric lifting. (From Myers BJ: Unit I: PNF diagonal patterns and their application to functional activities, videotape study guide, Chicago, Ill, 1982, Rehabilitation Institute of Chicago.)
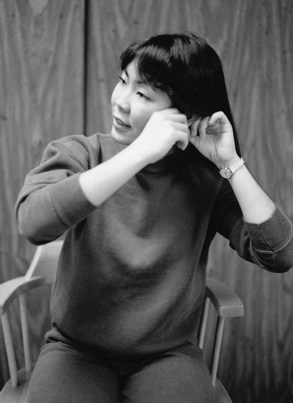
FIGURE 31-14 Putting on earring requires use of the upper extremity bilateral asymmetric flexion pattern.
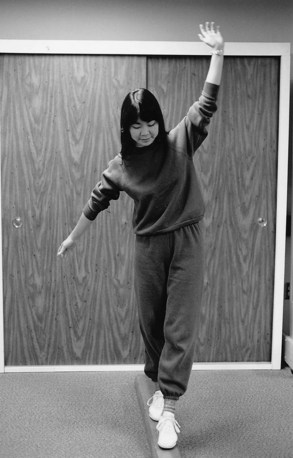
3. Reciprocal patterns: Paired extremities move in opposite directions simultaneously, either in the same diagonal or in combined diagonals. If paired extremities perform movements in combined diagonals (see Figure 31-10, C), a stabilizing effect occurs on the head, neck, and trunk because movement of the extremities is in the opposite direction while the head and neck remain in the midline. During activities requiring high-level balance, reciprocal patterns with combined diagonals come into play, with one extremity in D1 extension and the other extremity in D2 flexion. Examples are pitching in baseball, sidestroke in swimming, and walking a balance beam with one extremity in a diagonal flexion pattern and the other in a diagonal extension pattern (Figure 31-15). In contrast, reciprocal patterns in the same diagonal, such as D1 in arm swing during walking, facilitate trunk rotation. Leticia needs to work with reciprocals of D1 to improve her rhythm of arm swing and trunk rotation during walking.
Combined Movements of the Upper and Lower Extremities: Interaction of the UEs and LEs results in (1) ipsilateral patterns, with extremities on the same side moving in the same direction at the same time; (2) contralateral patterns, with extremities on opposite sides moving in the same direction at the same time; and (3) diagonal reciprocal patterns, with contralateral extremities moving in the same direction at the same time while the opposite contralateral extremities move in the opposite direction (see Figure 31-10, D, E, and F).
Combined movements of the UEs and LEs are observed in such activities as crawling and walking. Awareness of these patterns is important in the assessment of a client’s motor skills. The ipsilateral patterns are more primitive developmentally and indicate a lack of bilateral integration. Less rotation is also observed in ipsilateral patterns. Therefore, the goal in intervention is to progress from ipsilateral to contralateral to diagonal reciprocal patterns.
The use of diagonal patterns has several advantages in intervention. First, crossing of the midline occurs. This movement is of particular importance in the remediation of perceptual motor deficits such as unilateral neglect, in which integration of both sides of the body and awareness of the neglected side are intervention goals. Second, each muscle has an optimal pattern in which it functions. For example, a client who has weak thumb opposition benefits from active movement in D2 extension. Similarly, D1 extension is the optimal pattern for ulnar wrist extension. Leticia should work on D2 flexion after her Colles wrist fracture is stable. This pattern will increase ROM and strengthen supination and radial wrist extension. Third, the diagonal patterns use groups of muscles, which is typical of the movement seen in functional activities. For example, when eating, the hand-to-mouth action is accomplished in one mass movement pattern (D1 flexion) that uses several muscles simultaneously. Therefore, movement in the diagonals is more efficient than movement performed at each joint separately. Finally, rotation is always a component in the diagonals (e.g., trunk rotation to the left or right and forearm pronation and supination). With an injury or with the aging process, rotation is frequently impaired and can be facilitated by movement in the diagonals. During intervention, attention should be given to the placement of activities so that movement occurs in the diagonal. For example, if a client is working on a wood-sanding project, trunk rotation with extension can be facilitated by placing the project on an inclined plane in a diagonal. Leticia can incorporate rotational movements into homemaking activities such as unloading the dishwasher.
Total Patterns
In PNF, developmental postures are also called total patterns of movement and posture.47 Total patterns require interaction between the proximal (head, neck, and trunk) and distal (extremity) components. The assumption of postures is important, as is the maintenance of postures. When posture cannot be sustained, emphasis should be placed on the assumption of posture.73 For example, before a client can be expected to sustain a sitting posture, he or she must have ability in the lower developmental total patterns of movement, such as rolling and moving from side lying to side sitting.
Active assumption of postures can be included in occupational therapy activities. For example, a reaching and placing activity could be set up so that the client must reach for the object in the supine posture and place the object in the side-lying posture. The use of total patterns can also reinforce individual extremity movements. For example, in an activity such as wiping a tabletop, wrist extension is reinforced when the client leans forward over the supporting arm. This would be a way to make homemaking activities part of Leticia’s home exercise program for her wrist in the later stages of recovery.
Several facts support the use of total patterns in the PNF intervention approach.47 First, total patterns of movement and posture are experienced as part of the normal developmental process in all human beings. Therefore, recapitulation of these postures is meaningful to the client and acquired with less difficulty. Second, movement in and out of total patterns and the ability to sustain postures enhance components of normal development, such as reflex integration and support, balance between antagonists, and development of motor control in a cephalocaudal, proximodistal direction. Third, the use of total patterns improves the ability to assume and maintain postures, which is important in all areas of occupation.
The sequence and procedures for assisting clients in the developmental postures were developed by Voss. In 1981 Myers developed a videotape that shows use of the sequence and procedures in occupational therapy.47 This video demonstrates more information on application of the total patterns and postures in occupational therapy.
Procedures
PNF techniques are superimposed on movement and posture. Among these techniques are basic procedures considered essential to the PNF approach. Two procedures, verbal commands and visual cues, were discussed previously. Other procedures are described in the following sections.
Manual contact refers to placement of the therapist’s hands on the client. Such contact is most effective when applied directly to the skin. Pressure from the therapist’s touch is used as a facilitating mechanism and serves as a sensory cue to help the client understand the direction of the anticipated movement.74 The amount of pressure applied depends on the specific technique being used and on the desired response. The location of manual contact is chosen according to the groups of muscles, tendons, and joints responsible for the desired movement patterns. If a client is having difficulty reaching back to comb her hair because of scapular weakness, the desired movement pattern is D2 flexion. Manual contact should be on the posterior surface of the scapula to reinforce the muscles that elevate, adduct, and rotate the scapula.
Stretch is used to initiate voluntary movement and enhance speed of response and strength in weak muscles. This procedure is based on Sherrington’s neurophysiologic principle of reciprocal innervation.65 When a muscle is stretched, the Ia and II fibers in the muscle spindle send excitatory messages to the alpha motor neurons that innervate the stretched muscle. Inhibitory messages are sent to the antagonistic muscle simultaneously.17
When stretch is used in the PNF approach, the part to be facilitated is placed in the extreme lengthened range of the desired pattern (or where tension is felt on all muscle components of a given pattern). This range is the completely shortened range of the antagonistic pattern. Special attention is directed to the rotatory component of the pattern because it is responsible for elongation of the fibers of the muscles in a given pattern. After the correct position for the stretch stimulus has been achieved, stretch is superimposed on the pattern. The client should attempt the movement at the exact time that the stretch reflex is elicited. The use of verbal commands also should coincide with the application of stretch to reinforce the movement. Discrimination should be exercised with use of stretch to prevent an increase in pain or muscle imbalance.
Traction facilitates the joint receptors by creating a separation of the joint surfaces. It is thought that traction promotes movement and is used for pulling motion.74 In activities such as carrying a heavy suitcase or pulling open a jammed door, traction can be felt on the joint surfaces. Although traction may be contraindicated in clients with acute symptoms, such as after surgery or a fracture, it can sometimes provide relief of pain and promote greater ROM in painful joints.
Approximation facilitates joint receptors by creating compression of the joint surfaces. It promotes stability and postural control and is used for pushing motion.74 Approximation is usually superimposed on a weight-bearing posture. For example, to enhance postural control in the prone-on-elbows posture, approximation may be given through the shoulders in a downward direction. As part of a home program to enhance proximal stability, Leticia could play board games on the floor with her children in weight-bearing positions such as prone on elbows or side sitting. A weighted vest could be used in place of the therapist’s manual contact to provide approximation.
Maximal resistance is a procedure that involves Sherrington’s principle of irradiation—namely, that stronger muscles and patterns reinforce weaker components.65 This procedure is frequently misunderstood and applied incorrectly. The procedure is defined as the greatest amount of resistance that can be applied to an active contraction while allowing full ROM to take place or that can be applied to an isometric contraction without defeating or breaking the client’s hold.74 Maximal resistance is not the greatest amount of resistance that the therapist can apply. The objective is to obtain maximal effort on the part of the client because strength is increased by movement against resistance that requires maximal effort.24
If the resistance applied by the therapist results in uncoordinated or jerky movement or if it breaks the client’s hold, too much resistance has been given. Movement against maximal resistance should be slow and smooth. To use this technique effectively, the therapist must sense the appropriate amount of resistance. For clients with neurologic impairment or pain, the resistance may be very light, and light resistance is probably maximal for the client’s needs. The therapist’s manual contact may offer light resistance that actually assists by providing the client with a way to track the desired movement. In the presence of spasticity, resistance may increase existing muscle imbalance and thus needs to be monitored. For example, if an increase in finger flexor spasticity is noted with resisted rocking in the hands-knees position, resistance should be decreased or eliminated or an alternative position used.
Techniques
Specific techniques are used in conjunction with these basic procedures. A few have been selected for discussion. These techniques are divided into three categories: those directed to the agonists, those that are a reversal of the antagonists, and those that promote relaxation.74
Techniques Directed to the Agonists: The use of repeated contractions is a technique based on the assumption that repetition of an activity is necessary for motor learning and helps develop strength, ROM, and endurance. The client’s voluntary movement is facilitated with stretch and resistance by performing isometric and isotonic contractions. Repeated contractions could be used to increase trunk flexion with rotation in a client who has difficulty reaching to put on a pair of shoes from the sitting position. The client bends forward as far as possible. At the point where active motion weakens, the client is asked to “hold” with an isometric contraction. This action is followed by isotonic contractions, facilitated by stretch, as the client is asked to “reach toward your feet.” This sequence is repeated until either fatigue is evident or the client is able to reach the feet. The pattern can be reinforced further by asking the client to hold with another isometric contraction at the end of the sequence.
Rhythmic initiation is used to improve the ability to initiate movement, which may be a problem in clients with Parkinson’s disease or apraxia. This technique involves voluntary relaxation, passive movement, and repeated isotonic contractions of the agonistic pattern. The verbal command is, “Relax and let me move you.” As relaxation is felt, the command is, “Now you do it with me.” After several repetitions of active movement, resistance may be provided to reinforce the movement. Rhythmic initiation allows the client to feel the pattern before beginning active movement. Thus, the proprioceptive and kinesthetic senses are enhanced.
Techniques Involving Reversal of Antagonists: Reversal-of-antagonist techniques use a characteristic of normal development—namely, that movement is reversing and changes direction. These techniques are based on Sherrington’s principle of successive induction, according to which the stronger antagonist facilitates the weaker agonist.65 The agonist is facilitated through resistance to the antagonist. The contraction of the antagonist can be isotonic, isometric, or a combination of the two. These techniques may be contraindicated in clients in whom resistance of antagonists increases symptoms such as pain and spasticity. For example, facilitation of finger extension (agonist) would not be achieved effectively through resistance applied to spastic finger flexors (antagonist). In this situation, finger extension may be better facilitated through the use of repeated contractions, in which the emphasis is only on the extensor surface.
Slow reversal is an isotonic contraction (against resistance) of the antagonist followed by an isotonic contraction (against resistance) of the agonist. Slow reversal–hold is the same sequence, but with an isometric contraction at the end of the range. For a client who has difficulty reaching his or her mouth for oral hygiene because of weakness in the D1 flexion pattern, the slow-reversal procedure is as follows: an isotonic contraction against resistance in D1 extension with the verbal command, “Push down and out,” followed by an isotonic contraction of D1 flexion against resistance with the verbal command, “Pull up and across.” An increase or buildup of power in the agonist should be felt with each successive isotonic contraction. Slow reversal used in conjunction with repeated contractions could be applied to trunk movement patterns to help Leticia overcome her rigidity and improve the balance of antagonists. This sequence of techniques could also be used to increase Leticia’s wrist ROM and strength once her fracture is stable.
Stabilizing reversals are characterized by alternating isotonic contractions opposed by enough resistance to prevent motion. In practice, the therapist provides resistance to the client in one direction while asking the client to oppose the force, with no motion allowed. Once the client is fully resisting the force, the therapist gradually moves the resistance in another direction. Each time that the client is able to respond to the new resistance, the therapist moves the hand to resist a new direction, with directions reversed as often as needed to achieve stability. This technique is used to increase stability, balance, and muscle strength.
Rhythmic stabilization is used to increase stability by eliciting simultaneous isometric contractions of antagonistic muscle groups. Cocontraction results if the client is not allowed to relax. This technique requires repeated isometric contractions, which leads to increased circulation or the tendency for the client to hold his or her breath, or both. Therefore, rhythmic stabilization may be contraindicated in clients with cardiac involvement, and no more than three or four repetitions should be done at a time with any clients.
In rhythmic stabilization, manual contact is applied to both agonist and antagonist muscles, with resistance given simultaneously. The client is asked to hold the contraction against graded resistance. Without allowing the client to relax, manual contact is switched to the opposite surfaces. Rhythmic stabilization is useful in clients lacking postural control because of ataxia or proximal weakness. Used intermittently during an activity requiring postural stability, such as meal preparation in a standing posture, this technique enhances muscle balance, endurance, and control of movement. Rhythmic stabilization techniques were found to be effective in improving postural control and reducing pain in individuals who had chronic low back pain.36
Because these two stabilizing techniques can be superimposed on activity-based movements, they could be used to facilitate Leticia’s ability to perform numerous daily activities. For example, rhythmic stabilization could be used to improve trunk endurance and stability when Leticia experiences fatigue while standing at the sink to wash dishes.
Relaxation Techniques: Relaxation techniques are an effective means of increasing ROM, particularly in clients with pain or spasticity, which may be increased by passive stretch.
Contract-relax involves passive motion to the point of limitation in movement patterns. This is followed by an isotonic contraction of the antagonist pattern against maximal resistance, with only the rotational component of the diagonal movement allowed. This action is followed by relaxation and then by further passive movement into the agonistic pattern (e.g., contract-relax could involve passive motion to the point of limitation of D2 flexion, which would be followed by an isotonic contraction of D2 extension and then by further passive movement into D2 flexion). This procedure is repeated at each point in the ROM in which limitation is felt to occur.74 Contract-relax is used when no active range in the agonistic pattern is present. However, the ultimate goal is active movement through the full range. Therefore, once relaxation and increased ROM occur, active movement should be facilitated. The contract-relax technique has been demonstrated to be an effective means to gain ROM when compared with passive stretch, but the mechanism underlying this technique is not clear.46
Hold-relax is performed in the same sequence as contract-relax but involves an isometric contraction (no movement allowed) of the antagonist, followed by relaxation and then active movement into the agonistic pattern. It has been recommended that the static contraction be held for 3 seconds to achieve the greatest improvement in ROM.64 Because this technique involves an isometric contraction against resistance, it is particularly beneficial in a client with pain or acute orthopedic conditions. For a client with reflex sympathetic dystrophy (RSD) who has pain during shoulder flexion, abduction, and external rotation, the therapist asks the client to hold against resistance in the D2 extension pattern and then to initiate active movement into the D2 flexion pattern. This technique is beneficial for a client with RSD during self-care activities such as shampooing the hair and zipping a shirt in back.
Slow reversal–hold-relax begins with an isotonic contraction, followed by an isometric contraction, relaxation of the antagonistic pattern, and then active movement of the agonistic pattern. When the client has the ability to move the agonist actively, the technique is preferred. For example, to increase active elbow extension in a client with tight elbow flexors, the therapist asks the client to perform D1 flexion with elbow flexion as resistance is applied. When the ROM is complete, the client is asked to hold with an isometric contraction, followed immediately by relaxation. When relaxation is felt, the client moves actively into D1 extension with elbow extension. This technique helps increase elbow extension for such activities as reaching to lock the wheelchair brakes or picking up an object off the floor.
Rhythmic rotation is effective in decreasing spasticity and increasing ROM. The therapist passively moves the body part in the desired pattern. When tightness or restriction of movement is felt, the therapist rotates the body part slowly and rhythmically in both directions. After relaxation is felt, the therapist continues to move the body part into the newly available range. This technique is effective in preparing a paraplegic client with LE spasticity or clonus to don a pair of pants. The technique is also effective in preparing for splint fabrication on a spastic extremity.
Summary
The PNF approach emphasizes the client’s abilities and potential so that strengths assist weaker components. Strengths and deficiencies are assessed and addressed during intervention within total patterns of movement and posture. Carefully selected techniques are superimposed on these total patterns to enhance motor response and facilitate motor learning.
PNF uses multisensory input. Coordination and timing of sensory input are important in eliciting the desired response from the client. The client’s performance should be monitored, and sensory input should be adjusted accordingly.
To use PNF effectively, the therapist must understand the developmental sequence and the components of normal movement. The therapist must learn the diagonal patterns and how they are used for ADLs, must know when and how to use the techniques of facilitation and relaxation, and must be able to apply patterns and techniques of facilitation to occupational therapy evaluation and intervention. Attaining these skills requires observation and practice under the supervision of a therapist experienced in the PNF approach.
Section 3 Neurodevelopmental Treatment Approach
Historical Context of the Neurodevelopmental Treatment Approach
“Neurodevelopmental treatment,” as it is currently referred to in the United States, originally began as the “Bobath concept,” a treatment approach developed by Berta and Karel Bobath in the 1940s. Berta Bobath received her early training as a remedial gymnast at the Anna Herrmann School of gymnastics in Germany, where she stayed on as an instructor of gymnastics after graduation.63 She described the focus of her educational program at Anna Herrmann:
We were taught about the analysis of normal movements and various ways of relaxation. We learned to feel and evaluate degrees of relaxation not only on tight muscles but its effect on the strength and activity of their antagonists. This was done by a special way of handling a person, inducing movements in response to being moved (p. 8).
In the 1930s, when the Nazis came to power in Germany, Berta Bobath lost her job as a gymnastics instructor because the school would not retain a Jewish teacher. Berta subsequently moved to London and eventually worked at the Princess Louise Hospital.
Based on her background and skills in analyzing normal movement, Berta Bobath was repeatedly asked to see special cases of both children with cerebral palsy and adults with hemiplegia. At the time, it was assumed that individuals with upper motor neuron (UMN) lesions could not recover from their motor deficits. Because of her background in dance, her training in posture and analysis of movement, and probably also her “heretical or eccentric” (p. viii) views,68 Mrs. Bobath did not ascribe to this belief. She began by repositioning these clients into more neutral and symmetric alignments. She examined the impact of her handling on their tone and ability to move. Berta described the basis of her approach as “…the inhibition of released and exaggerated abnormal reflex action, the counteraction of abnormal patterns, and the facilitation of more normal automatic voluntary movements.”63
After much experience and success with her techniques, Berta eventually studied to become a physiotherapist and passed the examination in 1950. Dr. Karel Bobath, Berta’s husband and a psychiatrist, became interested in the approach and spent much of his career studying and explaining the neurophysiology behind Berta’s observations.
Together, Berta and Karel Bobath are credited with development of the Bobath concept and the NDT approach. They established the first Bobath Centre in London in 1951 and soon began training other physiotherapists in her approach to the treatment of children with cerebral palsy and adults with hemiplegia. Today, courses on this approach are taught both nationally and internationally to OTs and PTs, speech-language pathologists, and in some countries, nurses, physicians, and teachers.27 Information regarding continuing education courses in the United States (for OTs) can be found at the Neuro-Developmental Treatment Association Website, www.ndta.org.
Several contemporary authors describe NDT as a treatment approach that is based on a hierarchic view of the nervous system, given the time period in which it was established. Although it is true that the accepted view of the nervous system at the time that the approach began was a hierarchic model, it does not appear true, or consistent with the writings of the Bobaths and other historians, that the approach was originally based on a hierarchic perspective. The approach was based on Berta’s experiences—her skilled observations of alignment, posture, and movement—which were then interpreted in light of the reflex-hierarchic model of the time.54,63 This inductive sequence, from observations to development of theory, is discussed in many historical accounts of the approach. Even though dynamic models of CNS function and specifically motor control did not exist at the time, contemporary dynamic perspectives seem to support Berta’s original observations and experiences more accurately than reflex-hierarchic models do. Her handling resulted in changes in tone and movement capacities that seem unlikely (or could not have resulted) if the client’s tone and movement patterns were exclusively reflexive in nature. Her handling tapped into a dynamic system controlling motor output that is reflected in contemporary models.66
Whether the original NDT approach was founded on a reflex-hierarchic perspective or simply explained in terms of that model, it was clearly suggested as a “living concept” from its inception27 that consisted of concepts that were intended as “working hypotheses” (p. 9). Dr. Bobath used this terminology to stress the need for the approach to change over time with new information. Because it was grounded in an understanding of and appreciation for normal movement rather than pathology, he emphasized that the approach would continue to evolve as the understanding of normal movement advances through new discoveries and development of theories.
Berta’s Developing Theory: Original Concepts and Changes over Time
The Philosophy of Neurodevelopmental Treatment: Deeply engrained in an NDT-trained therapist’s methods are the philosophic underpinnings of the approach stemming from its opposition to the prevailing perspectives in the 1950s. When Berta began working with people with UMN lesions, most people believed that these individuals would not recover, and practices reflected this perspective. Individuals either were not provided rehabilitation services or were provided a compensatory approach exclusively. Any remedial intervention was from an orthopedic frame of reference—primarily stretching and strengthening—and therefore did not address the neurologic basis underlying the movement problems.27,54 Contrary to these views and practices and related to her clinical observations and experiences, Berta Bobath believed that these individuals could regain control of movement if given the right opportunities.
Part of the NDT philosophy is a belief in recovery (i.e., in the client’s potential). This belief in recovery was coupled with a belief in the influence that normal movement could have on a person’s quality of life. In the Foreword to Berta Bobath’s first book, Dr. P.W. Nathan very eloquently exposed some of the philosophic underpinnings of the approach, the essence of which remain today50:
Whether the doctor knows he is doing so or not, he chooses either a policy of persuading the client to use the hemiplegic limbs and re-train his affected side, or else a policy of encouraging the client to neglect the hemiplegic side and to use the unaffected side for all tasks previously done by the limbs of both sides. The choice affects only the upper limb and the general posture of the client. There is no choice about the lower limb; the client has to learn to use it. That being so, it is best for him to learn to use it properly. If the client gives in to this neurological disorder, he will become an invalid. If he learns to retrain his hemiplegic side, he returns to life (p. v).
Key Principles of Neurodevelopmental Treatment: The NDT approach is now widely described as a problem-solving approach to the restoration of movement and participation for individuals with UMN lesions, specifically cerebral palsy and hemiplegia.27 The approach is aimed at restoration of function through identifying and correcting underlying impairments that interfere with movement and participation in everyday activities. The emphasis is on regaining normal movement and postural control, as well as quality of movement in general. Compensations are discouraged.21 Clinicians studying the approach are instructed in Berta’s belief in the potential of the hemiplegic side to recover movement and her emphasis on addressing the whole body and the whole person. According to Tallis,68 the “fundamental ethos of Bobath [remains today as]…the client as partner, rehabilitation tailored to the client’s current situation, and rehabilitation as a 24/7 activity” (p. xi).
Although the basic principles of intervention remain the same, ideas regarding the nature of a client’s movement deficits and how movement is controlled and learned have evolved over time in response to scientific advances. Primary changes in the approach can be tied to discoveries in neuroscience and motor-learning research, specifically a dynamic and interactive understanding of the way in which movement is controlled and executed and feedback is used. In the most recent edition of her book on adult hemiplegia, Bobath outlined the major problems of the client as abnormal coordination of movement and abnormal postural tone and control.7 Current findings suggest that deficits in motor performance result from the combined “neurological dysfunction due to damage of the CNS, musculoskeletal changes, and learned movement strategies.”21 Intervention is no longer directed at reducing spasticity. Merely reducing spasticity will not foster improvements in the client’s motor control. However, there appear to be other aspects of hypertonicity that are non-neural in nature, and these non-neural influences on hypertonicity may result from muscle length, joint alignment, and recruitment patterns that tend to be amenable to handling strategies. Motor output is organized around task goals, and therefore motor skills are practiced in function as much as possible. Errors are required for motor learning, as is active participation on the part of the client; consequently, passive movement of the client is minimized and handling is graded to ensure increasing autonomy on the part of the client.
Using Neurodevelopmental Treatment to Restore Participation in Occupation
Within the last several years there has been a fair amount of controversy in the literature not only about the efficacy of NDT, which is addressed in the next section, but also about the approach itself.15,42,43 Given the changes in the NDT approach over time, questions arise regarding which aspects of the approach have remained constant. What are the current NDT strategies used to promote recovery of functional movement and therefore participation in occupation? What makes something NDT versus an entirely new approach to intervention? Because NDT has changed over time, other approaches have evolved from NDT, and NDT is used in combination with other approaches, it can be challenging to specify exactly which specific strategies are NDT. Physiotherapists who use the Bobath concept were surveyed and agreed that the following interventions are definitely or probably part of the approach: facilitation, mobilization, practicing motor skills for certain activities, practicing activities themselves, and teaching caregivers how to position the client.70 Based on review of the literature and the content of Neuro-Developmental Treatment Association–approved courses (ndta.org), the next section represents a distillation of contemporary evaluation and intervention using the NDT approach.
It should also be mentioned that the NDT approach is incorporated into occupational therapy evaluation and intervention to address problems of motor control and functional movement. It does not provide a thorough lens with which to view the dynamics of occupational problems in context. NDT should be used in concert with other theoretic models to provide a comprehensive occupational therapy program. It should also be combined, as appropriate, with other interventions found to be successful in current research to effectively manage the client’s needs and responses.
Returning to Charlotte, as the OT observed her attempts to dress, including pull on pants and pull on a sweater, it was apparent that the flexor tone in her right UE compromised performance. Even while seated, Charlotte tended to lean to the left side and did not sit with a symmetric posture. Her right scapula was downwardly rotated and she had significant lateral flexion of her trunk on the right side with a weight shift to the left in sitting and standing.
Evaluation: Based on a top-down approach to intervention, an OT using the NDT approach would begin with an occupational history interview. Grounded in the occupational profile and the client’s goals, the therapist would then observe the client’s performance in various occupations. Charlotte was unable to effectively and efficiently dress herself in a reasonable amount of time. She also had difficulty preparing a simple meal, particularly obtaining cooking equipment from the lower cupboards and spices from an upper cupboard. When reaching into a cupboard she had limited trunk extension, and her weight was shifted to the left when she was standing at the counter. Based on NDT, this observation would include assessment of not only the client’s level of assistance and the amount of movement present but also the quality of movement and postural control.
Specifically, the clinician would assess the following:
1. The client’s ability to maintain alignment in postures required for the occupation. As mentioned earlier, Charlotte did not use a symmetric posture in standing or sitting, and this had a negative impact on her efficiency in dressing and meal preparation tasks.
2. The “normal” or typical motor performance skills required for the tasks or activities that will be addressed. NDT-trained therapists analyze movement in terms of the whole body and the stability-mobility relationships between body segments during a task.
3. The client’s alignment and movement while performing the basic motor skills necessary for everyday activity, such as reaching, sit-to-stand, and transferring, as well as while performing occupational goals.
4. Underlying impairments that might be contributing to movement dysfunction. Ryerson and Levit outline the four primary impairments resulting from CNS lesions as “changes in muscle strength, muscle tone, and muscle activation, and changes in sensory processing” (p. 18).60 It is these impairments that result in the compensatory movements observed following CNS lesions and also, without intervention, often result in secondary impairments such as “changes in orthopedic alignment and mobility, changes in muscle and tissue length, edema, and pain” (p. 31). Impairments are typically assessed in upright postures and during functional activity and through observation, handling, and the patient’s subjective report. A common method for assessing tone is placing, in which the therapist guides the limb and asks the client to hold against gravity. If tone is too low, the client cannot hold the limb against gravity; if it is too high, the therapist will feel resistance during placing.6
Intervention: Because Bobath believed that you cannot “superimpose normal patterns on abnormal ones”6 (p. 59) and because there is a desire to minimize abnormal patterns of movement from the beginning, therapists are encouraged to overlap evaluation and intervention.33 Although “normal” movement has been emphasized since the inception of the approach, more recent descriptions emphasize efficient and functional movement while minimizing compensations.45 Intervention typically includes facilitation of the normal motor performance skills involved in a task, as well as practice of tasks themselves—or occupations—with manual guidance or handling.38 An OT will also use the NDT framework when providing compensatory strategies to promote modified independence in necessary and valued occupations while remediating motor skills. Compensations based on an NDT approach stress incorporating the hemiplegic side as much as possible; avoiding repetition of abnormal movement patterns with the hemiplegic side, many of which lead to orthopedic impairments over time; and neutral/symmetric alignment during activities, which reinforces the other two.60
After analyzing the client’s movement problems and tendencies, both outside of and within the occupational goal, intervention is structured according to the following sequence: preparation → movement → function. These steps overlap within an intervention session, as well as structure the series of sessions overall. Preparation encompasses all the activities that are necessary for the client to actively work on the motor skills required for the task and the task itself. Preparation might include the following:
1. Careful analysis of the movement components required for the task or occupational goal by the therapist. A helpful way to organize this analysis is by using segments of the body and analyzing the flow of movement that occurs within body segments and between body segments. The OT realized that sitting with most of the weight shifted to the left side further compromised Charlotte’s ability to easily dress herself in a front-closing blouse. This asymmetric sitting position made it difficult for Charlotte to position the sleeve of the blouse to her right side and place her right arm in the sleeve. The OT then used manual cues and handling to help Charlotte experience sitting in a symmetric posture before donning the blouse. By helping Charlotte experience this upright and symmetric posture, she was then able to hold the position for a short period before attempting to dress. Her improved sitting posture allowed greater freedom of movement.
2. Set-up of the environment to promote active participation on the part of the client, as well as attention to the client’s starting alignment for activity. Within the kitchen, it was suggested that Charlotte place her right hand on the counter while she was preparing a meal. This position fostered a symmetric standing position at the counter. It was also suggested that Charlotte use her right arm to help stabile a bowl when stirring food.
3. Mobilization to give the client access to the ROM required for the task. Charlotte had significant flexor tone in her right arm and downward rotation of her right scapula. Before working on various activities it was suggested that Charlotte sit at the table with her hands clasped together and forearms resting on the table. She would then lean on her elbows by shifting her trunk forward and then shift her trunk backward.6 This movement of her trunk effectively mobilized her scapula, particularly her right scapula, on the trunk before attempting to dress or prepare a meal.
Following preparation, the therapist will structure the session to work on specific motor skills required for the task. Frequently, these skills are partially addressed outside the occupation itself in preparation for practice of the whole task, which is congruent with the motor-learning guidelines regarding part- and whole-task practice.19 Along with verbal cues, demonstration, and structure of the environment, facilitation of motor skills is done with handling. In handling, the therapist uses his or her body in contact with the client’s to promote more efficient movement and avoid unwanted motor responses or alignments (Figure 31-16). Specifically, therapists use handling to add to the sensorimotor information that the client experiences during performance of task, to make the client more aware of his or her body and incorporate the hemiplegic side, and to assist in the coordination and timing of movement patterns.45 Continuing education courses and textbooks based on the NDT approach instruct clinicians on precise choices for hand placement that result in desired movement outcomes. These choices are referred to as key points of control. Although the therapist uses manual handling and guiding, the client should be active in the process. Handling and guiding should be graded to provide just enough assistance and input to give the client a feel for a more efficient movement pattern and then be gradually withdrawn as the client progresses and is able to do more of the movement pattern and task independently.21
Intervention for limb movements is also graded from closed chain patterns of movement to open chain patterns. A closed chain movement occurs when the distal part of a joint, or “chain” of joints, is fixed and the proximal part is moving.53 An example of a closed chain pattern for the UE would be incorporating the arm in a weight-bearing alignment for postural support and to assist with balance during an activity such as standing at a counter while bearing weight on one hand for support and reaching overhead into a cupboard for an item (Figure 31-17). The weight-bearing arm must be active. Clinicians using an NDT approach would include the UE in weight bearing as part of the base of support to assist with postural control and also to promote sensory input and isometric and eccentric control in the limb. Use of the weight-bearing or closed chain strategy requires muscle activity in the arm, not passive positioning. It is often combined with movement over the base of support to encourage active extension of the UE for balance.
Positioning the UE with the hand in contact with a stable surface can also be useful for mobilization and stretching of the distal part of the UE and to grade facilitation of isolated movement patterns in the arm. During mobilization and stretching, particularly of the wrist and hand, moving the arm on a fixed hand allows the therapist to stretch the extrinsic finger, thumb, and wrist flexors (Figure 31-18). Muscle lengthening may lead to decreases in hypertonicity. In addition, when promoting isolated movement of the UE, for example, in reaching patterns of shoulder flexion with elbow extension, the distal contact offers the limb support and decreases the resistance or demand on the proximal musculature required for the task. Similar to handling and other forms of sensory input and feedback, this support must be gradually withdrawn for muscle strengthening and motor learning to occur. The sequence of facilitation should proceed to incorporation of the learned movement patterns into the occupation or functional task. Handling is gradually decreased as the patient is able to complete the efficient movement patterns.
Neurodevelopmental Treatment and Evidence-Based Practice
Evidence-based practice is a clinical reasoning process that combines the best available research, a clinician’s expertise, and the client’s preferences and values to make decisions about intervention in individual cases and provide the most effective and efficient care.61 The best available research for clinical decision making regarding the effectiveness of specific interventions is a systematic review of randomized clinical trials or a randomized clinical trial.18 Few studies have addressed the effect of NDT on client outcomes. At the present time, a great majority of the evidence for the effectiveness of NDT is at a lower level on the evidence scale—it is primarily the expertise of many practitioners, clients, and caregivers, who could be considered experts in their own living experiences with the condition and who report positive outcomes as a result of incorporating NDT principles and management strategies into their intervention.
The limited number of systematic reviews and clinical trials addressing the effectiveness of the NDT approach has yielded mix results. One systematic review of the literature by Kollen and colleagues examined 16 studies encompassing 813 clients and concluded that “there was no evidence of superiority of Bobath on sensorimotor control of upper and lower limb, dexterity, mobility, activities of daily living, health-related quality of life, and cost-effectiveness”37 (p. e89). Findings by Luke, Dodd, and Brock indicated that although the Bobath concept was found to have slightly better results than other approaches or no intervention at all in reducing shoulder pain and tone, the Bobath concept was one approach among several that did not demonstrate “superiority of one approach over the other at improving upper limb impairment, activity or participation”41 (p. 888). Similarly, Paci, in his review of 15 trials, found no evidence to support NDT as an optimal type of treatment, but also no conclusive support for idea that the approach is not effective.51 Researchers agree that additional higher-level research, with more rigorous methodologies that define and detail NDT methods, is needed to provide evidence-based guidelines for practice. To systematize such research, Tyson, Connell, Busse, and Lennon outlined a “typical treatment package’” for future clinical trials (p. 454) based on their study of physiotherapists using the Bobath concept.70 The focus of the intervention package would be “facilitation, mobilization, practicing the components of movement, practicing a few whole activities, and teaching clients and carers on how to position the client” (p. 454). It has also been suggested that researchers study specific intervention techniques, rather than the NDT concept or approach as a whole.70
NDT is not alone in lacking evidence. As stated by Mayston, “the reality is that there is only partial evidence to support current modalities such as task-specific training, constraint-induced movement therapy, treadmill training and muscle strengthening”44 (p. 184). The present evidence for use of the NDT approach consists of widespread clinical observations and expertise, along with limited clinical trials and systematic reviews. Despite a lack of high-level evidence supporting its efficacy, according to the authors of one systematic literature review, “in the Western world, the Bobath Concept or neuro-developmental treatment is the most popular treatment approached used in stroke rehabilitation.”37 This evidence, though useful and substantial, is not enough to warrant continued and isolated use of this approach as research demonstrating more effective and/or efficient methods at higher levels of evidence becomes available. Based on dynamic models exposing the integration of multiple systems within and outside the person that contribute to the control of movement, as well as occupational performance, contemporary clinical reasoning and intervention planning for individuals with UMN lesions must consider the complex web of factors contributing to function and integrate all available resources and intervention methods, supported by evidence, that contribute to effectively restoring participation in desired occupations.
1. What are the four general processes of information flow related to control of movement?
2. Define motivational urge and name the locus of this function in the brain.
3. Trace the flow of information in the central and peripheral nervous systems that leads to purposeful movement.
4. What is the sensorimotor system?
5. List the areas of the sensorimotor cortex.
6. List the structures that constitute the higher, middle, and lower levels of the CNS components for movement.
7. Name the four traditional sensorimotor approaches to treatment and the theorist responsible for each.
8. Which two models of motor control form the basis for the sensorimotor approaches to treatment?
9. Briefly describe each of the four traditional sensorimotor approaches to treatment. Compare and contrast their similarities and differences.
10. List some techniques used by therapists to influence or modify motor responses in each of the traditional sensorimotor approaches.
11. How are the sensorimotor approaches used in current clinical practice?
12. In clients with pain, what tone of voice should be used when giving verbal commands?
13. Discuss the significance of auditory, visual, and tactile input in motor learning.
14. Which UE diagonal pattern is used for the hand-to-mouth phase of eating? For zipping front-opening pants?
15. Discuss the advantages of using the chop and lift patterns.
16. Which trunk pattern is used when donning a left sock?
17. List three advantages of using the diagonal patterns.
18. What is the developmental sequence of total patterns?
19. If a client needs more stability, which of the following total patterns should be chosen: side lying or prone posture on elbows?
20. Which PNF technique facilitates postural control and cocontraction?
32. Discuss the neurophysiologic principles of Sherrington on which the PNF techniques of facilitation are based.
33. What is an effective technique to prepare a client with UE flexor spasticity to don a shirt?
34. Define maximal resistance.
35. Name two PNF techniques that facilitate initiation of movement.
36. What are the key principles of the NDT approach?
37. What is the difference between a closed and open kinetic chain?
38. Identify a task in which you would use a closed kinetic chain and a task in which you would use an open kinetic chain.
References
1. Abreu, BF, Toglia, JP. Cognitive rehabilitation: a model for occupational therapy. Am J Occup Ther. 1987;41(7):439.
2. Affolter, F. Perceptual processes as prerequisites for complex human behavior. Int Rehabil Med. 1981;3(1):3.
3. American Occupational Therapy Association. Occupational therapy practice framework: domain and process, 2nd edition. Am J Occup Ther. 2008;62:625–683.
4. Ayres, AJ. Proprioceptive neuromuscular facilitation elicited through the upper extremities. I. Background, II. Application, III. Specific application to occupational therapy. Am J Occup Ther. 1955;9(1):1.
5. Bobath, B. Adult hemiplegia: evaluation and treatment, ed 3. London, UK: Heinemann; 1991.
6. Bobath, B. Adult hemiplegia: evaluation and treatment, ed 2. London, UK: Heinemann; 1978.
7. Bobath, B. Adult hemiplegia: evaluation and treatment, ed 3. Boston, Mass: Butterworth-Heinemann; 1990.
8. Brooks, VB. The neural basis of motor control. New York, NY: Oxford University Press; 1986.
9. Brunnstrom, S. Motor behavior in adult hemiplegic patients. Am J Occup Ther. 1961;15(1):6.
10. Brunnstrom, S. Movement therapy in hemiplegia. New York, NY: Harper & Row; 1970.
11. Buchwald, J. Exteroceptive reflexes and movement. Am J Phys Med. 1967;46(1):141.
12. Carroll, J. The utilization of reinforcement techniques in the program for the hemiplegic. Am J Occup Ther. 1950;4(5):211.
13. Cheney, PD. Role of cerebral cortex in voluntary movements: a review. Phys Ther. 1985;65(5):624.
14. Cooke, DM. The effects of resistance on multiple sclerosis patients with intention tremor. Am J Occup Ther. 1958;12(2):89.
15. Damiano, D. Pass the torch, please!. Dev Med Child Neurol. 2007;49:723.
16. Eggers, O. Occupational therapy in the treatment of adult hemiplegia. Rockville, Md: Aspen; 1987.
17. Farber, SD. Neurorehabilitation: a multisensory approach. Philadelphia, Pa: Saunders; 1982.
18. Fineout-Overholt, E, Melnyk, B, Schultz, A. Transforming health care from the inside out: Advancing evidence-based practice in the 21st century. J Prof Nurs. 2005;21(6):335–344.
19. Fletcher, L, Cornall, C, Armstrong, S. Moving between sitting and standing. In: Raine S, Meadows L, Lynch-Ellerington M, eds. Bobath concept: theory and clinical practice in neurological rehabilitation. Oxford, UK: Blackwell; 2009:83–116.
20. Fromm, C, Wise, SP, Evarts, EV. Sensory response properties of pyramidal tract neurons in the precentral motor cortex and postcentral gyrus of the rhesus monkey. Exp Brain Res. 1984;54(1):177.
21. Graham, J, Eustace, C, Brock, K, et al. The Bobath concept in contemporary clinical practice. Topics Stroke Rehabil. 2009;16(1):57–68.
22. Hagbarth, KE. Excitatory and inhibitory skin areas for flexor and extensor mononeurons. Acta Physiol Scand. 1952;26(suppl 94):1.
23. Hashimoto, K, Higuchi, K, Nakayama, Y, Abo, M. Ability for basic movement as an early predictor of functioning related to activities of daily living in stroke patients. Neurorehabil Neural Repair. 2007;21:353–357.
24. Hellebrandt, FA. Physiology. In: Delorme TL, Watkins AL, eds. Progressive resistance exercise. New York, NY: Appleton, Century, Crofts, 1951.
25. Hellebrandt, FA, Schade, M, Carns, ML. Methods of evoking the tonic neck reflexes in normal human subjects. Am J Phys Med. 1962;4(90):139.
26. Holstege, G. The emotional motor system. Eur J Morphol. 1992;30(1):67.
27. Howle, JM. Neuro-developmental treatment approach: theoretical foundations and principles of clinical practice. Laguna Beach, Calif: Neuro-Developmental Treatment Association; 2002.
28. Huitt, W, Conation as an important factor of mind. Educational Psychology Interactive, Valdosta, Ga, Valdosta State University, 1999. Retrieved July 2005 from, http://chiron.valdosta.edu/whuitt/col/regsys/conation.html.
29. Humphrey, TL, Huddleston, OL. Applying facilitation techniques to self care training. Phys Ther Rev. 1958;38(9):605.
30. Huss, AJ. Sensorimotor approaches. In: Hopkins H, Smith H, eds. Willard and Spackman’s occupational therapy. Philadelphia, Pa: Lippincott, 1978.
31. Jackson, JH, Selected writings. vol 1, London, UK, Hodder & Staughton (edited by J Taylor), 1931.
32. Jeannerod, M. The neural and behavioral organization of goal-directed movements. Oxford, UK: Clarendon Press; 1988.
33. Johnson, P. Assessment and clinical reasoning in the Bobath concept. In: Raine S, Meadows L, Lynch-Ellerington M, eds. Bobath concept: theory and clinical practice in neurological rehabilitation. Oxford, UK: Blackwell Publishing, Ltd; 2009:43–63.
34. Kabat, H, Rosenberg, D. Concepts and techniques of occupational therapy for neuromuscular disorders. Am J Occup Ther. 1950;4(1):6.
35. Kandel ER, Schwartz JH, Jesell TM, eds. Principles of neural science, ed 4, New York, NY: Elsevier, 2000.
36. Kofotolis, N, Kellis, E. Effects of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility, and functional performance in women with chronic low back pain. Phys Ther. 2006;86:1001–1012.
37. Kollen, BJ, Lennon, S, Lyons, B, et al. The effectiveness of the Bobath concept in stroke rehabilitation: what is the evidence? Stroke. 2009;40(4):e89–e97.
38. Lennon, S, Ashburn, A. The Bobath concept in stroke rehabilitation: a focus group study of the experienced physiotherapists’ perspective. Disabil Rehabil. 2000;22(15):665–674.
39. Levy, CE, Nichols, DS, Schmalbrock, PM. Functional MRI evidence of cortical reorganization in upper-limb stroke hemiplegia treated with constraint-induced movement therapy. Am J Phys Med Rehabil. 2000;80:4.
40. Loomis, JE, Boersma, FJ. Training right brain damaged patients in a wheelchair task: case studies using verbal mediation. Physiother Can. 1982;34(4):204.
41. Luke, C, Dodd, K, Brock, K. Outcomes of the Bobath concept on upper limb recovery following stroke. Clin Rehabil. 2004;18:888–898.
42. Mayston, MJ. Motor learning now needs meaningful goals [letter]. Physiotherapy. 2000;86(9):492–493.
43. Mayston, MJ. Fusion not feuding [letter]. Physiother Res Int. 2001;6(4):265–266.
44. Mayston, MJ. Raine: a response. Physiother Res Int. 2006;11(3):183–186.
45. Meadows, L, Williams, J. An understanding of functional movement as a basis for clinical reasoning. In: Raine S, Meadows L, Lynch-Ellerington M, eds. Bobath concept: theory and clinical practice in neurological rehabilitation. Oxford, UK: Blackwell; 2009:23–42.
46. Mitchell, UH, Myrer, JW, Hopkins, JT, et al. Neurophysiological reflex mechanisms’ lack of contribution to the success of PNF stretches. J Sport Rehabil. 2009;18:343–357.
47. Myers, BJ. Assisting to postures and application in occupational therapy activities [videotape]. Chicago, Ill: Rehabilitation Institute of Chicago; 1981.
48. Myers, BJ. PNF: patterns and application in occupational therapy [videotape]. Chicago, Ill: Rehabilitation Institute of Chicago; 1981.
49. Myers BJ: Proprioceptive neuromuscular facilitation: concepts and application in occupational therapy as taught by Voss. Notes from course at Rehabilitation Institute of Chicago, September 8-12, 1980.
50. Nathan, P. Forward. In: Bobath B, ed. Adult hemiplegia: evaluation and treatment. London, UK: William Heinemann, 1970.
51. Paci, M. Physiotherapy based on the Bobath concept for adults with post-stroke hemiplegia: a review of effectiveness studies. J Rehabil Med. 2003;35:2–7.
52. Penfield, W. The excitable cortex in conscious man. Liverpool, UK: Liverpool University Press; 1958.
53. Prentice, WE. Open- versus closed-kinetic-chain exercise in rehabilitation. In Prentice WE, ed.: Rehabilitation techniques for sports medicine and athletic training, ed 4, New York, NY: McGraw-Hill, 2004.
54. Raine, S. The Bobath concept: developments and current theoretical underpinning. In: Raine S, Meadows L, Lynch-Ellerington M, eds. Bobath Concept. Oxford, UK: Blackwell; 2009:1–22.
55. Roland, P, Larsen, B, Lassen, NA, et al. Supplementary motor area and other cortical areas in organization of voluntary movements in man. J Neurophysiol. 1980;43(1):118.
56. Rood, M. Neurophysiological mechanisms utilized in the treatment of neuromuscular dysfunction. Am J Occup Ther. 1956;10:4.
57. Rood, M. Occupational therapy in the treatment of the cerebral palsied. Phys Ther Rev. 1952;32:220.
58. Rood, M. The use of sensory receptors to activate, facilitate and inhibit motor responses, automatic and somatic, in developmental sequence. In: Sattely C, ed. Approaches to the treatment of patients with neuromuscular dysfunction. Dubuque, Iowa: William C Brown, 1962.
59. Rothwell, JC. Control of human voluntary movement, ed 2. London, UK: Chapman & Hall; 1994.
60. Ryerson, S, Levit, K. Functional movement reeducation. Philadelphia, Pa: Churchill Livingstone; 1997.
61. Sackett, D, Straus, S, Richardson, W, et al. : Evidence-based medicine: how to practice and teach EBM, ed 2. New York, NY: Churchill Livingstone; 2000.
62. Sawner, K, LaVigne, J. Brunnstrom’s movement therapy in hemiplegia: a neurophysiological approach, ed 2. Philadelphia, Pa: Lippincott; 1992.
63. Schleichkorn, J. The Bobaths; a biography of Berta and Karel Bobath. Tucson, Ariz: Therapy Skill Builders; 1992.
64. Sharman, MJ, Cresswell, AG, Riek, S. Proprioceptive neuromuscular facilitation stretching: mechanisms and clinical implications. Sports Med. 2006;36:929–939.
65. Sherrington, C. The integrative action of the nervous system, ed 2. New Haven, Conn: Yale University Press; 1961.
66. Shumway-Cook, A, Woolacott, MH. Motor control: translating research into clinical practice, ed 3. Philadelphia, Pa: Lippincott Williams & Wilkins; 2007.
67. Stockmeyer, S. An interpretation of the approach of Rood to the treatment of neuromuscular dysfunction, NUSTEP proceedings. Am J Phys Med. 1967;46(1):900.
68. Tallis, R. Forward. In: Raine S, Meadows L, Lynch-Ellerington M, eds. Bobath Concept. Oxford, UK: Blackwell; 2009:viii–ix.
69. Tanji, J, Taniguchi, K, Saga, T. Supplementary motor area: neuronal response to motor instructions. J Neurophysiol. 1980;43(1):60.
70. Tyson, S, Connell, L, Busse, M, Lennon, S. What is Bobath? A survey of UK stroke physiotherapists’ perceptions of the content of the Bobath concept to treat postural control and mobility problems after stroke. Disabil Rehabil. 2009;31(6):448–457.
71. Voss, DE. Application of patterns and techniques in occupational therapy. Am J Occup Ther. 1959;8(4):191.
72. Voss, DE. Proprioceptive neuromuscular facilitation. Am J Phys Med. 1967;46(1):838.
73. Voss, DE. Proprioceptive neuromuscular facilitation: the PNF method. In: Pearson PH, Williams CE, eds. Physical therapy services in the developmental disabilities. Springfield, Ill: Charles C Thomas, 1972.
74. Voss, DE, Ionta, MK, Myers, BJ. Proprioceptive neuromuscular facilitation, ed 3. Philadelphia, Pa: Harper & Row; 1985.
75. Whitaker, EW. A suggested treatment in occupational therapy for patients with multiple sclerosis. Am J Occup Ther. 1950;4(6):247.
76. Wolny, T, Saulicz, E, Gnat, R, Koksz, M. Butler’s neuromobilizations combined with proprioceptive neuromuscular facilitation are effective in reducing of upper limb sensory in late-stage stroke subjects: a three-group randomized trial. Clin Rehabil. 2010;24:810–821.
Adler, SS, Beckers, D, Buck, M. PNF in practice: an illustrated guide. Berlin, Germany: Springer-Verlag; 1993.
Goloszewski, S, Kremser, C, Wagner, M, et al. Functional magnetic resonance imaging of the human motor cortex before and after whole-hand electrical stimulation. Scand J Rehabil Med. 1999;31:165.
Kunkel, A, Kopp, B, Muller, G, et al. Constraint-induced movement therapy for motor recovery in chronic stroke patients. Arch Phys Med Rehabil. 1999;80:624.
Kwalkel, GW, Wagenaar, RC, Twisk, JW, et al. Intensity of leg and arm training after primary middle-cerebral artery stroke: a randomized trial. Lancet. 1999;354:191.
Thornborough, JR. Pretest key concepts neuron function. New York, NY: McGraw-Hill; 1994. p 103
Weiss, PL, Naveh, Y, Katz, N. Design and testing of a virtual environment for patients with unilateral spatial neglect to cross a street safely. Occup Ther Int. 2003;10:39.