Cardiac and Pulmonary Disease
After studying this chapter, the student or practitioner will be able to do the following:
1 Briefly describe the cardiovascular system and its function.
2 Identify the significance of ischemic heart disease and valvular diseases of the heart.
3 Differentiate between modifiable and nonmodifiable risk factors.
4 Identify signs and symptoms of cardiac distress.
5 Describe the course of action that should be taken if signs and symptoms of cardiac distress are present.
6 List the psychosocial considerations for persons with cardiovascular or pulmonary disease.
7 Describe methods for determining the heart rate and blood pressure.
8 Determine the rate-pressure product given the heart rate and blood pressure.
9 Give a brief overview of the respiratory system, and identify its primary function.
10 Define chronic obstructive pulmonary disease.
11 Identify pulmonary risk factors and psychosocial considerations.
12 Describe dyspnea control postures, pursed-lip breathing, and diaphragmatic breathing.
13 Describe a relaxation technique, and explain its purpose.
14 List interview questions that will help the clinician know what the patient understands about intervention.
15 List the principles of energy conservation.
16 Explain the significance of a metabolic equivalent chart in the progression of activity, and describe how to use it.
In this chapter the term patient is used instead of client to reflect the practice setting and the acute nature of the diagnoses in the individuals described in the case studies.
Individuals with disorders of the cardiovascular or pulmonary system may be severely limited in endurance and performance in areas of occupation, including activities of daily living (ADLs) and instrumental activities of daily living (IADLs). Occupational therapy (OT) services may benefit such individuals and are available throughout the continuum of health care. An understanding of the normal function of the cardiopulmonary system, the pathology of cardiopulmonary disease, common risk factors, clinical terminology, medical interventions, precautions, and standard treatment techniques will guide the occupational therapist in providing effective care and promoting recovery of function in clients with compromised cardiovascular or pulmonary systems.
Every living cell of the body has three major requirements for life: (1) a constant supply of nutrients and oxygen, (2) continual removal of carbon dioxide and other waste products, and (3) a relatively constant temperature. The cardiovascular and pulmonary systems play key roles in meeting these requirements.30
Anatomy and Circulation
The heart and blood vessels work together to maintain a constant flow of blood throughout the body. The heart, located between the lungs, is pear shaped and about the size of a fist. It functions as a two-sided pump. The right side pumps blood from the body to the lungs; the left side simultaneously pumps blood from the lungs to the body. Each side of the heart has two chambers: an upper atrium and a lower ventricle.
Blood flows to the heart from the venous system. Blood enters the right atrium, which contracts and squeezes the blood into the right ventricle. Next, the right ventricle contracts and ejects the blood into the lungs, where carbon dioxide is exchanged for oxygen. Oxygen-rich blood flows from the lungs to the left atrium. As the left atrium contracts, it forces blood into the left ventricle, which then contracts and ejects its contents into the aorta for systemic circulation (Figure 44-1). Blood travels from the aorta to the arteries and through progressively smaller blood vessels to networks of very tiny capillaries. In the capillaries, blood cells exchange their oxygen for carbon dioxide.
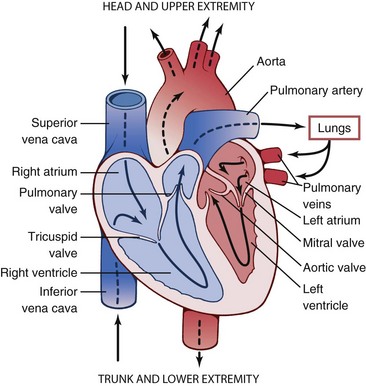
FIGURE 44-1 Anatomy of the heart. (From Thibodeau GA, Patton KT: The human body in health and disease, ed 5, St. Louis, Mo, 2010, Mosby.)
Each of the ventricles has two valves: an input valve and an output valve. The valves open and close as the heart muscle (myocardium) contracts and relaxes. These valves control the direction and flow of blood. The input valves are the mitral, or bicuspid, valve (between the left atrium and ventricle) and the tricuspid valve (between the right atrium and ventricle). The output valves comprise the aortic and pulmonary valves.
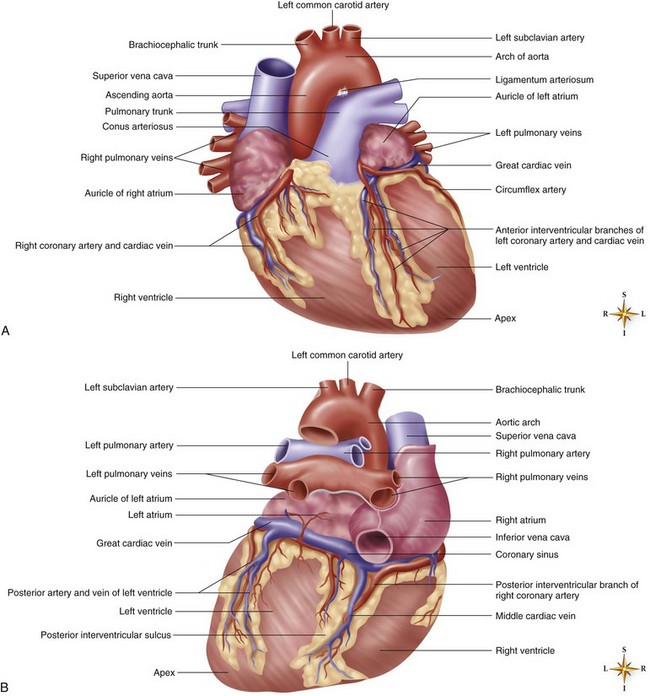
The heart is living tissue and requires a blood supply (through an arterial and venous system of its own), or it will die. Coronary arteries cross over the myocardium to supply it with oxygen-rich blood. The coronary arteries are named for their location on the myocardium (Figure 44-2). Cardiologists generally refer to these arteries by abbreviations, such as “LAD” for “left anterior descending” and “RCA” for “right coronary artery.” The LAD artery is on the left, anterior portion of the heart and runs in a downward direction; it supplies part of the left ventricle. Blockage of this coronary artery will interrupt the blood supply to the left ventricle. Because the left ventricle supplies the body and brain with blood, a heart attack caused by blockage of the LAD artery can have serious consequences.
What Causes the Heart to Contract?
In addition to the ordinary muscle tissue of the heart, the myocardium is composed of two other types of tissue: nodal and Purkinje. These tissues are part of a specialized electrical conduction system that causes the heart to contract and relax (Figure 44-3). An electrical impulse usually originates in the right atrium at a site called the sinoatrial node. The impulse travels along internodal pathways to the atrioventricular node, through the bundle of His, to the left and right bundle branches, and then to the Purkinje fibers. Nerve impulses normally travel this pathway 60 to 100 times every minute, first causing both atria to contract, pushing blood into the ventricles, and then provoking the ventricles to contract. The electrical impulse created by the heart’s conduction system can easily be studied. Electrodes placed on a person’s limbs and chest can pick up the heart’s electrical impulse, which can be translated to paper as an electrocardiogram (ECG). The resulting ECG tracing is frequently used to help diagnose cardiac disease.
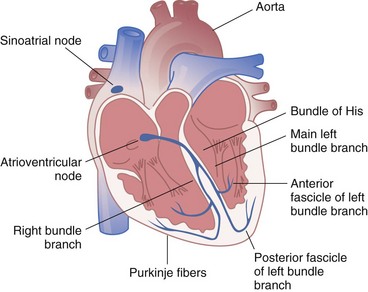
FIGURE 44-3 Cardiac conduction. (From Hall JE, Guyton AC: Guyton and Hall textbook of medical physiology, ed 12, Philadelphia, Pa, 2011, Saunders.)
The sinoatrial node responds to vagal and sympathetic nervous system input.21 This is why the heart rate (HR) increases in response to exercise and anxiety and decreases in response to relaxation techniques, such as deep breathing and meditation. Each cell within the electrical conduction system of the heart can respond to, conduct, resist for a brief period, and generate an electrical impulse. Because of this capacity, electrical impulses causing the heart muscle to contract can be generated from anywhere along the electrical conduction system. This is desirable when part of the conduction system has been damaged and is unable do its job, but it is undesirable when life-threatening conduction irregularities develop.
Cardiac Cycle
HR and blood pressure (BP) determine cardiac output, the amount of blood ejected by the heart each minute. The cardiac cycle occurs in two phases: input (diastole) and output (systole).
During the input phase, blood flows through the atria and into the ventricles. The atria contract and push more blood into the ventricles. Once the pressure inside the ventricles is equal to the pressure in the atria, the input valves (tricuspid in the right ventricle and mitral [or bicuspid] in the left ventricle) close. The ventricles then contract, which results in rapidly increasing ventricular pressure. When the pressure inside the ventricles exceeds the pressure in the blood vessels beyond, the output valves (pulmonary in the right and aortic in the left) open, and diastolic BP is attained.
The ventricles continue to contract and squeeze blood under greater and greater pressure into the pulmonary and body circulation. Systolic BP is attained when pressure in the emptying ventricles falls below pressure in the blood vessels beyond, which causes the output valves to close.
Ischemic Heart Disease
Ischemic heart disease (ischemia) occurs when a part of the heart is temporarily deprived of sufficient oxygen to meet its demand. The most common cause of cardiac ischemia is coronary artery disease (CAD). CAD is the most common type of heart disease and the leading cause of death in the United States in both men and women.33 CAD usually develops over a period of many years without causing symptoms. The internal wall of an artery can become injured. Once the wall is damaged, it becomes irregular in shape and more prone to collect plaque (fatty deposits such as cholesterol). Platelets also gather along the arterial wall and clog the artery, thereby creating a lesion in the same manner in which rust can clog a pipe. The artery gradually narrows and thus allows a smaller volume of blood to pass through it. This disease process is called atherosclerosis.
If a coronary artery is partially or completely blocked, the part of the heart supplied by that artery may not receive sufficient oxygen to meet its needs. Persons with partial blockage of a coronary artery may be free of symptoms at rest but have angina, a type of chest pain, with eating, exercise, exertion, or exposure to cold. Angina varies from individual to individual and has been described as squeezing, tightness, fullness, pressure, or a sharp pain in the chest. The pain may also radiate to other parts of the body, usually the arm, back, neck, or jaw. Angina has also been confused with indigestion. Rest or medication (or both) will frequently relieve angina. Usually, no permanent heart damage results. Angina is a warning sign that should not be ignored. It is a sign that CAD is present—that the individual may be a candidate for a heart attack.
Chest pain that is not relieved by rest or nitroglycerin indicates a myocardial infarction (MI), or heart attack. A patient who has this type of pain should seek emergency medical help immediately. Individuals who attribute their symptoms to anxiety and stress are more likely to delay emergency care.42 In the case of Franklin, his substernal chest pain was a warning sign that one or more of his coronary arteries were blocked. The blood flow to the heart muscle was interrupted, and starved of the necessary oxygen, Franklin’s heart began to die. MI is significant because part of the heart muscle dies as a result of lack of oxygen. If a substantial section of the heart is damaged, it will stop pumping (cardiac arrest).
Restrictions in activity are prescribed for the first 6 weeks after a heart attack because newly damaged heart muscle, like any injured body tissue, is easily reinjured.14 During a heart attack, metabolic waste products accumulate in the damaged myocardium and make it irritable and prone to electrical irregularities such as premature ventricular contractions. A delicate balance of rest and activity must be maintained to allow the damaged area of myocardium to heal while also maintaining the strength of the healthy part of the heart. OT is frequently recommended to guide the patient toward a safe level of activity, or participation in occupation, during this acute period of recovery. Franklin requires guidance from the therapist in recognizing signs of fatigue, determining when rest breaks are needed, and choosing activities that can be performed safely.
At approximately 6 weeks after an MI, scar tissue forms and the risk of extending the MI decreases. The scarred part of the heart muscle is not elastic and does not contract with each heartbeat. Therefore, the heart does not pump as well. A graded exercise program will help strengthen the healthy part of the myocardium and improve cardiac output.43
CAD can also lead to congestive heart failure (CHF). Similarly, infections can lead to CHF. This disease process develops over time with the heart becoming progressively weaker. CHF occurs when the heart is unable to pump effectively enough to meet the demand and fluid backs up into the lungs or the body. The fluid buildup in the lungs causes shortness of breath. Fluid overload is serious because it puts a greater workload on the heart as the heart strains while attempting to clear the excess fluid, which may result in further congestion. Heart size is often enlarged in persons with CHF because the heart muscle thickens (hypertrophy) from working so hard. Diuretics can be prescribed for persons with CHF to promote fluid loss through the urinary system. Low-sodium diets and fluid restrictions reduce the overall amount of fluid in the body. CHF cannot be cured, but with diet, medications, and rest, people with this condition can live longer and participate more fully in life.
Once an acute exacerbation of CHF is controlled, gradual resumption of activity will promote improved function. If activity is resumed too quickly, another acute episode may follow. Patients who have difficulty resuming their former level of activity may self-limit their recovery. OT can guide clients with acute CHF toward an optimal level of function via graded self-care tasks. “About 5.7 million people in the United States have heart failure, and it results in about 300,000 deaths each year.”35
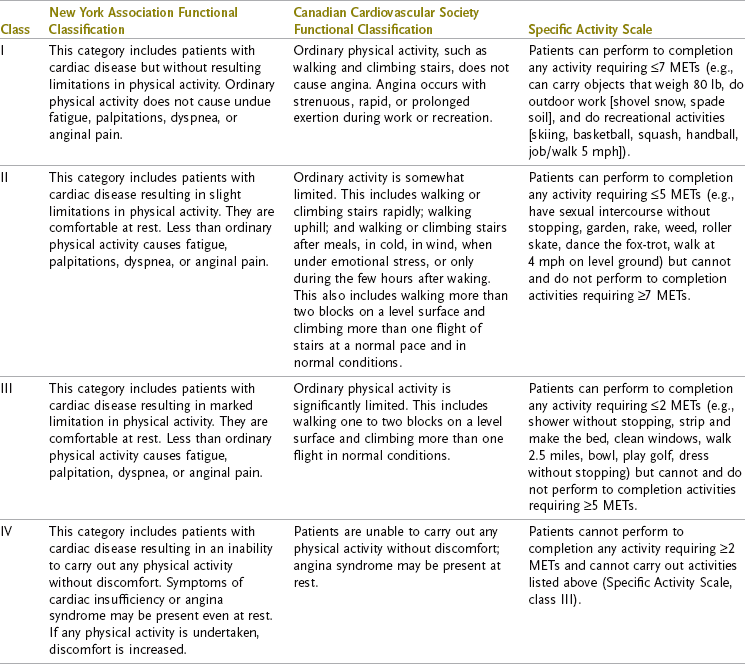
Table 44-1 delineates the four functional classifications of heart disease. OT can be of great benefit to persons with stage III and IV heart disease and can provide preventive programs for persons with stages I and II.
Valvular Disease
The heart valves, which are responsible for controlling the direction and flow of blood through the heart, may become damaged by disease or infection. Two complications result from valvular disease: volume overload and pressure overload. A fibrous mitral valve will fail to close properly, and blood will be regurgitated back to the atria when the left ventricle contracts. Volume overload results when fluid accumulates in the lungs, thereby causing shortness of breath. Volume overload increases the potential for atrial fibrillation, which results in irregular and ineffective contractions in both atria. Blood flow through the heart slows, and blood clots (emboli) may develop in the ventricles. Many cerebrovascular accidents are caused when emboli ejected from the left ventricle enter the circulatory system of the brain.
If the aortic valve fails to close properly (aortic insufficiency), CHF or ischemia may result. Another disorder of the aortic valve is aortic stenosis (narrowing), which results in pressure overload. The left ventricle, which must work harder to open the sticky valve, becomes enlarged, and cardiac output decreases. Ventricular arrhythmia (irregular rhythm of heartbeats), cerebral insufficiency, confusion, syncope (fainting), and even sudden death may result from aortic stenosis. Surgery to repair or replace the damaged valves is frequently recommended.
Cardiac Risk Factors
Many scientific studies have been conducted to determine the causes of heart disease. The most famous of these, the Framingham study,10 helped identify many factors that put an individual at risk for atherosclerosis. Risk factors are divided into three major categories: those that cannot be changed (heredity, male gender, and age), those that can be changed (high blood pressure, cigarette smoking, cholesterol levels, and an inactive lifestyle), and contributing factors (diabetes, stress, and obesity). Other factors that contribute to CAD include sleep apnea, high levels of triglycerides, and high levels of C-reactive protein.34 The more risk factors that an individual has, the greater the individual’s risk for CAD. All team members—the physician, nurse, physical therapist, case manager, social worker, nutritionist, and occupational therapist—should support the patient’s attempts to reduce risk factors.
Medical Management
A heart attack is a medical emergency, and treatment with aspirin and oxygen is usually initiated before diagnosis. Nitroglycerin and other measures to control chest pain are included in these early measures.37 After emergency treatment, heart attack survivors are typically managed in a coronary care unit, where they are closely observed for complications. Approximately 90% of persons who have suffered an MI will have arrhythmia.4 Heart failure, the development of blood clots (thrombosis and embolism), aneurysms, rupture of part of the heart muscle, inflammation of the sac around the heart (pericarditis), and even death are potential outcomes of MI. Close medical management is imperative.
Generally, patients are managed for 2 to 3 days after MI in an intensive care unit. Once their condition is stabilized, they graduate to a monitored hospital bed. Patients typically stay 4 to 6 days in the hospital after an acute MI. Vital signs are monitored closely while activity is gradually increased. OT personnel may be called on to monitor the patient’s response to activity and educate the patient about the disease process, risk factors, and lifestyle modification.
Various surgical procedures can correct the circulatory problems associated with CAD. Balloon angioplasty, also called percutaneous transluminal coronary angioplasty (PTCA), and coronary artery bypass grafting (CABG) are most common. During PTCA, a wire mesh tube, called a stent, may be implanted into the coronary artery to keep the artery open.9
In PTCA, a catheter is inserted into the femoral artery and guided through the circulatory system into the coronary arteries. Radioactive dye is injected into the arteries, and the site of the lesion is pinpointed. A balloon is then inflated at the site of the lesion to push the plaque against the arterial wall. When the balloon is deflated and the catheter removed, improved circulation to the myocardium usually results. Ensuring that the patient rests in bed for 8 hours after PTCA helps prevent hemorrhage from the femoral artery.
If a lesion is too diffuse or if an artery reoccludes after PTCA, CABG may be performed. The diseased section of the coronary arteries is bypassed with healthy blood vessels (taken from other parts of the body), thus improving the coronary circulation. In performing CABG, the surgeon usually opens the chest wall by cracking the sternum and spreading the ribs to gain access to the heart. Postsurgical precautions to prevent trauma to the new graft sites, incisions, and sternum generally last about 8 weeks after surgery and include the following: avoiding Valsalva maneuvers (e.g., straining during a bowel movement), avoiding rapid movement of the upper part of the body, adhering to a 10-lb lifting restriction, wearing compressive hose, refraining from driving (which creates problems because of upper body torque), and traveling in a seat without an airbag when riding in a car. “Following CABG, 85 percent of people have significantly reduced symptoms, less risk of future heart attacks, and a decreased chance of dying within 10 years.”32
Arrhythmias that cannot be controlled with medication may be managed by the insertion of a pacemaker in the chest. Wires are run from the pacemaker to specific spots on the heart. The pacemaker delivers a small electrical impulse to the heart muscle and sets the pace of the heart’s electrical conduction. The impulse may be set to deliver a regular impulse or to send an impulse only if the heart rate drops below a certain number of beats per minute (demand). Modern pacemakers can monitor physiologic responses such as BP and temperature. Implantable cardioverter-defibrillators (ICDs) may also be used to treat cardiac arrhythmias. An ICD can both pace the heart muscle and deliver a high-energy impulse to reset the heart muscle if certain dangerous arrhythmias develop.
When the heart’s pumping ability has become too compromised by CHF or cardiomyopathy, a heart transplant or heart-lung transplant may be considered. After the healthy tissue of a recently deceased person is harvested, the patient’s diseased organ (or organs) is removed, and the harvested tissue is transplanted into the patient’s body. Transplant patients are typically maintained on special medication to decrease the risk for organ rejection. Nearly 50% of all heart transplant recipients survive for 10 years. Most recipients resume normal lifestyles, but only about 40% return to work.36
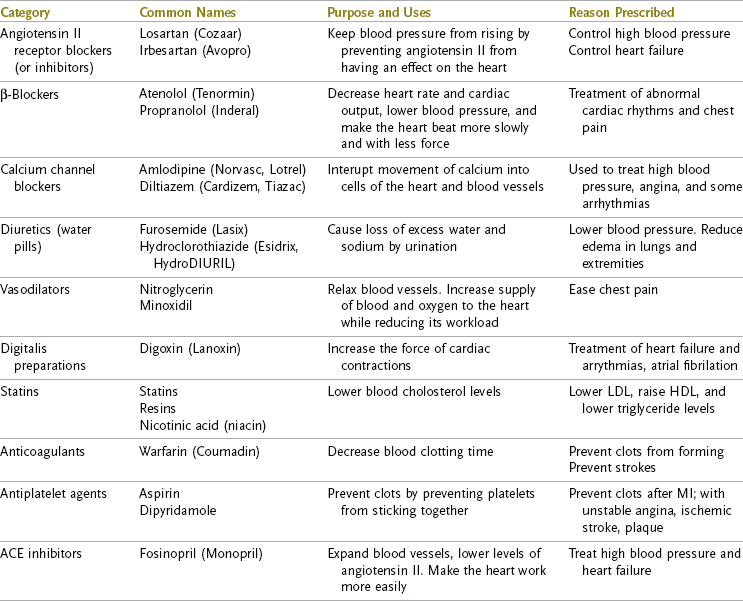
Cardiac Medications
Knowledge of the purpose and side effects of cardiac medication promotes understanding of the patient’s response to activity. Table 44-2 lists common cardiac medications.
Psychosocial Considerations
Persons who have experienced MI pass through a number of phases of adjustment to their disability. Fear and anxiety develop initially as patients confront their mortality. Sedatives may be prescribed to reduce stress and allow rest so that the cardiovascular system can begin to heal. Once stabilized, patients must confront the reality of their physical limitations.15
As patients begin to resume more normal activities, such as self-care and walking around the ward, feelings of helplessness may begin to subside. Patients feel more secure when familiar coping mechanisms allow them to respond to the stress, but some former coping mechanisms (e.g., smoking, drinking, consuming fatty foods) are harmful and should be discouraged and replaced by newly learned coping strategies, often those taught by the occupational therapist and other members of the intervention team. Typically, the nutritionist directs the patient toward healthy food choices, the physical therapist provides guidance toward exercise, and the nurse oversees management of medications.
Denial is common in patients with cardiac disease. Patients in denial must be closely monitored during the acute phase of recovery. Persons in denial may ignore all precautions and could stress and further damage their cardiovascular systems.
Depression is common 3 to 6 days after MI and may last many months.3 Increased morbidity and mortality, reduced modification of risk factors, and reduced quality of life have been associated with depression in cardiac patients.24 Clinical evidence supports psychosocial counseling after MI that focuses on improving self health appraisal, improving social support, and establishing an effective means of coping to improve quality of life.47 The patient’s family must be included in the education so that their misconceptions and anxieties do not compound the patient’s fears. In Franklin’s case, his fear of dying in the facility, as his father did before him, could influence him to resist any activity.
Cardiac Rehabilitation
During the first 1 to 3 days after MI, stabilization of the patient’s medical condition is usually attained. This acute phase is followed by a period of early mobilization. Phase 1 of treatment, inpatient cardiac rehabilitation, includes monitored low-level physical activity, including self-care; reinforcement of cardiac and postsurgical precautions; instruction in energy conservation and graded activity; and establishment of guidelines for appropriate activity levels at discharge. Through monitored activity, the ill effects of prolonged inactivity can be averted while medical problems, poor responses to medications, and atypical chest pain can be addressed.
Phase 2 of treatment, outpatient cardiac rehabilitation, usually begins at discharge. During this phase, exercise can be advanced while the patient is closely monitored on an outpatient basis. Community-based exercise programs follow in phase 3. Some individuals require treatment in their place of residence because they are not strong enough to tolerate outpatient therapy.
Health care costs can be significantly reduced and positive health effects can result from comprehensive cardiac rehabilitation.23 Additional research indicates reduced mortality in selected patients who have undergone cardiac rehabilitation after acute MI.41 Cardiac rehabilitation has also been found to benefit patients with left ventricular dysfunction by improving physical work capacity.18 Patients who acquire skills in relaxation and control of breathing after MI have been found to require fewer hospitalizations and less expensive medical management even 5 years after the MI.48 Early and accurate identification of the signs and symptoms of cardiac distress and modification of treatment to remedy distress are imperative to the well-being of the patient. If the clinician observes any of the signs of cardiac distress (Table 44-3) during treatment, the proper response is to stop the activity, allow the patient to rest, seek emergency medical help if the symptoms do not resolve, report the symptoms to the team, and modify future activity to decrease the workload on the heart.
TABLE 44-3
Signs and Symptoms of Cardiac Distress
| Sign/Symptom | What to Look For |
| Angina | Look for chest pain that may be described as squeezing, tightness, aching, burning, or choking. Pain is generally substernal and may radiate to the arms, jaw, neck, or back. More intense or longer-lasting pain forewarns of greater ischemia. |
| Dyspnea | Look for shortness of breath with activity or at rest. Note the activity that brought on the dyspnea and the amount of time that it takes to resolve. Dyspnea at rest with a resting respiratory rate of greater than 30 breaths per minute is a sign of acute congestive heart failure. The patient may require emergency medical help. |
| Orthopnea | Look for dyspnea brought on by lying supine. Count the number of pillows that the patient needs to breathe comfortably during sleep (1, 2, 3, or 4 pillows needed to relieve orthopnea). |
| Nausea/emesis | Look for vomiting or signs that the patient feels sick to the stomach. |
| Diaphoresis | Look for cold, clammy sweat. |
| Fatigue | Look for a generalized feeling of exhaustion. The Borg Rate of Perceived Exertion Scale is a tool used to grade fatigue (see Box 44-1). Cerebral signs—ataxia, dizziness, confusion, and fainting (syncope)—are all signs that the brain is not getting enough oxygen. |
| Orthostatic | Look for a drop in systolic blood pressure and hypotension of greater than 10 mm Hg with a change in position from supine to sitting or sitting to standing. |
Box 44-1, the Borg Rate of Perceived Exertion Scale, is a tool used to measure perceived exertion. The patient is shown the scale before an activity and instructed that a rating of “6” means no exertion at all and a rating of “19” indicates extremely strenuous activity, equal to the most strenuous activity that the patient has ever performed. After the activity has been completed, the patient is asked to appraise his or her feelings of exertion as accurately as possible and give the activity a rating.
Patients’ perceptions of their illness can have an impact on their ability to make the changes in lifestyle necessary for healthy living after an acute coronary event. Individualized intervention plans that address the unique physical, social, and psychologic concerns of the patient improve the integration of lifestyle changes and functional improvement.20,26,28
Monitoring Response to Activity
When the patient’s response to an activity is being assessed, symptoms provide one indication that the patient is or is not tolerating the activity. HR, BP, rate-pressure product (RPP), and ECG readings are other measures that may be used to evaluate the cardiovascular system’s response to work.
Heart Rate
HR, or the number of beats per minute, can be monitored by feeling the patient’s pulse at the radial, brachial, or carotid sites. The radial pulse is located on the volar surface of the wrist, just lateral to the head of the radius. The brachial pulse is found in the antecubital fossa, slightly medial to the midline of the forearm. The carotid pulse, located on the neck lateral to the Adam’s apple, should be palpated gently; if overstimulated, it can cause the HR to drop below 60 beats per minute (bradycardia). To determine HR, the clinician applies the second and third fingers (flat, not with the tips) to the pulse site. If the pulse is even (regular), the clinician counts the number of beats in 10 seconds and multiplies the finding by 6. The thumb should never be used to take a pulse because it has its own pulse.
All clinicians who assess HR, as well as patients, should be able to note the evenness (regularity) of the heartbeat. HR can be regular or irregular. An irregular heartbeat may be described as regularly irregular, which means that there is a consistent irregular pattern (e.g., every third beat is premature), or it may be described as irregularly irregular, which means that there is no pattern to the premature or skipped beats. HR irregularities include skipped beats, delayed beats, premature beats, and beats originating from outside the normal conduction pathway in the heart. Although an irregular HR is not normal, many individuals function quite well with an irregular rate. Clinicians should note the client’s normal rate pattern, as well as any variations. A sudden change in HR from regular to irregular should be reported to the physician. An ECG or other diagnostic test may be ordered on the basis of such findings. When the HR is irregular, the number of beats should be counted for a full minute. Patients can be taught to take their own pulse and monitor the response of HR to activity. As a general rule, HR should rise in response to activity.
Blood Pressure
BP is the pressure that the blood exerts against the walls of any vessel as the heart beats. It is highest in the left ventricle during systole and decreases in the arterial system with distance from the heart.49 A stethoscope and BP cuff (sphygmomanometer) are used to indirectly determine BP. The BP cuff is placed snugly (but not tightly) around the upper part of the patient’s arm just above the elbow, with the bladder of the cuff centered above the brachial artery. The examiner inflates the cuff while palpating the brachial artery to 20 mm Hg above the point at which the brachial pulse is last felt. With the earpieces of the stethoscope angled forward in the examiner’s ears, the dome of the stethoscope is placed over the patient’s brachial artery. Supporting the patient’s arm in extension with the pulse point of the brachial artery and the gauge of the stethoscope at the patient’s heart level, the examiner deflates the cuff at a rate of approximately 2 mm Hg per second. Listening is imperative when recording BP. The first two sounds heard correspond to systolic BP. The examiner continues to listen until the last pulse is heard and diastolic BP is attained.
Physicians usually indicate treatment parameters for the HR and BP of patients in medical facilities. Parameters are frequently written in abbreviations, such as “Call HO if SBP > 150 < 90; DBP > 90 < 60; HR > 120 < 60.” (In other words, “Call the house officer or physician on call if systolic BP is greater than 150 or less than 90, if diastolic BP is greater than 90 or less than 60, and if HR is greater than 120 or less than 60.”).
HR and BP will fluctuate in response to activity, and cardiac output is affected by both HR and BP. Measurement of the RPP can give a more accurate indication of how well the heart is pumping. The RPP is the product of HR and systolic BP (RPP = HR × SBP). It is usually a five-digit number but is reported in three digits by dropping the last two (for example, HR 100 × SBP 120 = 12,000 = RPP 120). During any activity, the RPP should rise at peak and return to baseline in recovery (after 5 to 10 minutes of rest).
Correctly reading and interpreting an ECG is a skill that requires hours of learning and practice for proficiency. Electrocardiography is not available in most nonacute settings. The reader is referred to Dubin’s Rapid Interpretation of EKGs,11 which is an excellent resource for persons unfamiliar with the subject.
There are many similarities in the evaluation and treatment of persons with cardiac disease and those with pulmonary dysfunction. A review of the pulmonary system and its disease processes follows.
Anatomy and Physiology of Respiration4,29,31
While the heart provides oxygen-rich blood to the body and transports carbon dioxide and other waste products to the lungs, the respiratory system exchanges oxygen for carbon dioxide. The cardiac and pulmonary systems are interdependent. If no oxygen were delivered to the bloodstream, the heart would soon stop functioning for lack of oxygen; conversely, if the heart were to stop pumping, the lungs would cease functioning for lack of a blood supply. All body tissues depend on the cardiopulmonary system for their nutrients.
The respiratory system supplies oxygen to the blood and removes waste products, primarily carbon dioxide, from the blood. Air enters the body via the nose and mouth and travels through the nasopharynx to the larynx or voice box. From there, the air continues downward into the lungs by way of the trachea or windpipe. The trachea consists of ribbed cartilage approximately 10 cm long. When the trachea or pharynx becomes blocked, a small incision may be made in the trachea to allow air to pass freely into the lungs. This procedure is called a tracheotomy.
The trachea divides into two main bronchi that carry air into the left and right lungs. The bronchi continue to branch off into smaller tubes, called bronchioles. Bronchioles are segmented into smaller passages called the alveolar ducts. Each alveolar duct is divided and leads into three or more alveolar sacs. The entire respiratory passageway from bronchi to alveolar sacs is often referred to as “the pulmonary tree” because its structure is much like that of an upside-down tree, with the alveolar sacs representing the leaves.
Each alveolar sac contains more than 10 alveoli. A very fine, semipermeable membrane separates the alveolus from the capillary network. Across this membrane, oxygen is transported and exchanged for carbon dioxide. Carbon dioxide is exhaled into the air after traveling upward through the “pulmonary tree” (Figure 44-4).
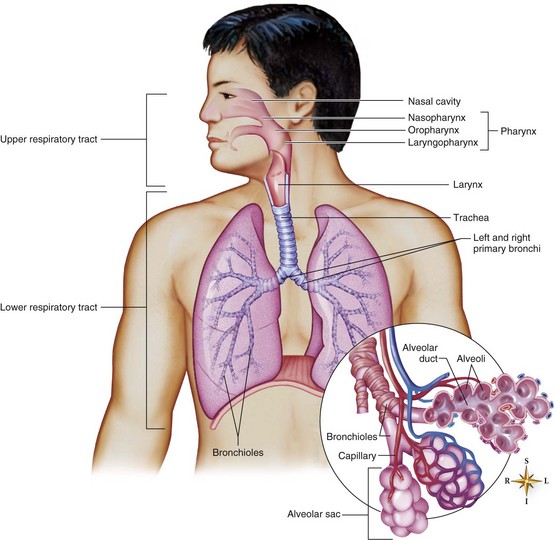
FIGURE 44-4 Major structures of the respiratory system. (From Patton KT, Thibodeau GA: Anatomy & physiology, ed 7, St. Louis, Mo, 2010, Mosby.)
With the exception of the nose and mouth, all the airways are lined with cilia and coated with mucus. Mucus and cilia provide a filtering shield that protects the fragile airway respiratory structures from dust and germs.
The musculature of the thorax helps in inspiration and expiration. During inspiration, the muscle power for breathing air into the lungs is provided primarily by the diaphragm. Originating from the sternum, ribs, lumbar vertebrae, and lumbocostal arches, the diaphragm forms the inferior border of the thorax. The muscle fibers of the diaphragm insert into a central tendon. Innervated by the left and right phrenic nerves, the diaphragm contracts and domes downward when stimulated. This downward doming of the diaphragm enlarges the volume of the thorax and causes a drop in pressure in the lungs relative to the air in the environment. Air then enters the lungs to equalize inside and outside pressure. Accessory muscles, the intercostals and scalenes, are also active during inspiration. The intercostals maintain alignment of the ribs, and the scalene helps elevate the rib cage.
At rest, expiration is primarily a passive relaxation of the inspiratory musculature. The lungs help draw the thorax inward as the inspiratory muscles relax. Forced expiration requires active contraction of the abdominal muscles to compress the viscera and squeeze the diaphragm upward in the thorax. Expiration can be further forced by flexing the torso forward and pressing with the arms on the chest or abdomen. As the volume of the thorax decreases, air is forced out of the lungs.
Accessory muscles in the neck and collarbone region can be recruited to assist in respiration when lung disease is active or other respiratory musculature is impaired.
Innervation of the Respiratory System
Breathing is mostly involuntary. A person does not have to think to take a breath. The autonomic nervous system has control over breathing. With anxiety and increased activity, the sympathetic nervous system will automatically increase the depth and rate of inspiration.
Inspiration and expiration have a volitional component. Volitional control allows us to control our breathing as we swim and to play the harmonica. Additionally, receptors within and outside the lungs can, when stimulated, cause changes in the depth and rate of breathing. Although the pons, medulla, and other parts of the brain provide the central control for breathing, they adjust their response to input from receptors in the lungs, the aorta, and the carotid artery.
Chronic Lung Disease2,4,38
Common chronic disorders of the lungs for which pulmonary rehabilitation is typically prescribed include chronic obstructive pulmonary disease (COPD) and asthma.4 COPD is characterized by “damage to the alveolar wall and inflammation of the conducting airways”2 and includes emphysema, peripheral airway disease, and chronic bronchitis. COPD has been diagnosed in more than 15 million Americans, including Harriet.
Emphysema is a condition in which the alveoli become enlarged or ruptured, usually because of a restriction during expiration or a decrease in elasticity of the lungs.49 Chronic emphysema is most prevalent in men between the ages of 45 and 65 who have a history of chronic bronchitis, smoking, working in areas with high levels of air pollution, or exposure to cold, damp environments. Persons with chronic bronchitis experience shortness of breath (dyspnea) on exertion, and as the disease progresses, dyspnea occurs at rest.
Inflammation, fibrosis (thickening of the connective tissue), and narrowing of the terminal airways of the lungs are the physiologic changes that occur with peripheral airway disease. Smoking and other environmental pollutants irritate the airways, which leads to the development of abnormal terminal airways. Coughing and spitting up mucus from the lungs are common clinical manifestations of this disorder. The disease process may never progress beyond this initial phase, or it may evolve into emphysema and full-fledged COPD.
Chronic bronchitis is diagnosed after a 2-year period of repeated episodes, lasting longer than 3 months, of mucus-producing cough of unknown origin. A direct relationship exists between the development of chronic bronchitis and a history of cigarette smoking. Clinical manifestations of the disease increase as the pack-year history increases. Pack-year history is calculated by multiplying the number of packs of cigarettes consumed per day by the number of years of smoking. Harriet began smoking at the age of 20. She is 64 years old now. Therefore, her pack-year history is 64 − 20 = 44 × 1 pack/yr = 44 pack-years. As with other forms of COPD, the onset of physical disability is typically gradual, with dyspnea on exertion representing the initial phases of disability and devolving to shortness of breath at rest.
Asthma is characterized by irritability of the bronchotracheal tree and is typically episodic in onset. Persons suffering from asthma experience wheezing and shortness of breath that may resolve spontaneously or necessitate the use of medication for calming the airway. Persons with asthma may be free of symptoms for periods between the episodes of wheezing and dyspnea. Some individuals appear to have a genetic predisposition to asthma. Allergenic causes of asthma may include pollen and respiratory irritants such as perfume, dust, and cleaning agents. Bronchospasm occurring with exposure to cold air or induced by exercise is sometimes the first clinical manifestations of asthma. Irritation of the airway leads to narrowing of the air passages and interferes with ventilation of the alveolar sacs. If obstruction of the airway is significant enough, a reduction in oxygen levels in the bloodstream will result in hypoxemia.13 If left untreated, a severe asthmatic episode may result in death.
Pulmonary Risk Factors
Cigarette smoking is the primary cause of COPD, and smoking cessation will slow the progression of disability in persons with COPD.39 Because cigarette smoke is a pulmonary irritant, it may also be a causative agent in asthmatic episodes. Other environmental irritants, such as air pollution, chemical exposure, and dust, are contributory risk factors in the development of COPD and asthma.
Medical Management
COPD is a progressive, chronic disease. The onset of the disease is insidious. When patients initially seek medical attention, they are frequently seen in a physician’s clinic rather than at a medical center. Besides evaluating the patient’s medical history and symptoms and performing a physical examination, the physician will assess the patient’s history of smoking and occupational exposure to respiratory irritants. Blood work and an x-ray examination will be performed to further assess the patient’s clinical status. Medications prescribed for persons with pulmonary disease include anti-inflammatory agents (e.g., steroids and cromolyn sodium), bronchodilators (e.g., albuterol and theophylline) to help open the airway, and expectorants (e.g., iodides and guaifenesin) to help loosen and clear mucus. Flu shots and pneumonococcal vaccines are recommended. Oxygen therapy may also be prescribed at a specific flow rate. Occasionally, persons receiving oxygen therapy may be tempted to increase the liter-per-minute flow in the erroneous thinking that more is better. This can result in retention of carbon dioxide and lead to failure of the right side of the heart.
Persons in acute respiratory distress may initially be managed with a ventilator before being weaned to oxygen. Ventilators provide mechanical assistance to the process of inspiration and do not increase the number of healthy alveolar sacs. Ventilators will not slow the end-stage disease process of COPD. Mechanical ventilation is frequently prescribed for persons with an acute exacerbation of the disease process caused by pneumonia, influenza, or CHF.
When a patient’s endurance decreases sufficiently to impair performance of ADLs, the physician may refer the patient to OT. Regrettably, the client is not likely to be seen by an occupational therapist or receive an assessment of occupational lifestyle as the first line of defense.
Signs and Symptoms of Respiratory Distress
Dyspnea is probably the most obvious sign of a breathing difficulty. In the most severe form of dyspnea, the patient is short of breath even at rest. Clients with this level of dyspnea are unable to utter a short phrase without gasping for air. When reporting that a client has dyspnea, the practitioner should note the precipitating factors and associated circumstances; for example, “Harriet becomes short of breath when washing her face while seated in front of the sink.”
Other signs that the body is not getting enough oxygen include extreme fatigue, a nonproductive cough, confusion, impaired judgment, and cyanosis (bluish skin color caused by insufficient oxygen in the blood).
Psychosocial Considerations
Because COPD is a progressive, debilitating physical illness, it is not surprising that the psychosocial effects of the disease are considerable. Chan identified five themes related to barriers preventing engagement in occupation for people with COPD: uncertainty about progression of the disease, attributing the cause of the disease to external factors, progressing restriction in activity and isolation, anxiety and depression, and passive acceptance.6 Persons with anxiety and depression are more inclined to experience relapses after initial emergency department visits,8 and 96% of patients with COPD have reported disabling anxiety.1 Other patients with COPD complain of faintness or difficulty concentrating.12 Training in progressive muscle relaxation can be a successful tool for controlling the dyspnea and anxiety and for lowering the HR.44
Most cardiac and respiratory disease processes are preventable. Individuals with these diseases may lack basic skills in coping and setting limits with themselves or with others. The therapist’s role includes encouraging the patient to engage in activities that will develop his or her skills and promoting resumption of occupations that bring value, meaning, and participation back into the patient’s life. With these skills, the patient begins to see himself or herself as a person actively making choices to get better. By working with Harriet on ways to engage with her dog when she does not have the endurance to take a walk, the occupational therapist not only teaches energy conservation but also conveys this information in a meaningful manner to the patient.
Most persons with end-stage COPD realize that they will die as a result of their disease. Fear of death from suffocation is misplaced. Persons with such concerns should be referred to their physician, who can reassure them that individuals with CO2 retention die peacefully in their sleep.19
Pulmonary Rehabilitation
The goal of pulmonary rehabilitation is to stabilize or reverse the disease process and return the patient’s function and participation in activity/occupation to the highest capacity. A multidisciplinary rehabilitation team working with the patient can design an individualized intervention program to meet this end. Accurate diagnosis, medical management, therapy, education, and emotional support are components of a pulmonary rehabilitation program. OT personnel are frequently part of the patient’s team, which is headed by the patient and also includes the physician, nurse, and the patient’s family and social supports. Respiratory therapists, dietitians, physical therapists, social workers, and psychologists may also be team members. Roles of team members vary slightly among facilities. Knowledge of specialized pulmonary treatment techniques is imperative for each team member when treating persons with pulmonary disease.
Intervention Techniques
Dyspnea Control Postures: Adopting certain postures can reduce breathlessness. In a seated position, the patient bends forward slightly at the waist while supporting the upper part of the body by leaning the forearms on a table or the thighs. In a standing position, relief may be obtained by leaning forward and propping oneself on a counter or shopping cart.
Pursed-Lip Breathing: Pursed-lip breathing (PLB) is thought to prevent tightness in the airway by providing resistance to expiration. This technique has been shown to increase use of the diaphragm and decrease accessory muscle recruitment.5 Persons with COPD sometimes instinctively adopt this technique, whereas others may need to be taught it. Instructions for PLB are as follows:
Diaphragmatic Breathing: Another breathing pattern, which calls for increased use of the diaphragm to improve chest volume, is diaphragmatic breathing. Many persons learn this technique by placing a small paperback novel on the abdomen just below the xiphoid process (base of the sternum or breastbone). The novel provides a visual cue for diaphragmatic movement. The patient lies supine and is instructed to inhale slowly and make the book rise. Exhalation through pursed lips should cause the book to fall.
Relaxation: Progressive muscle relaxation in conjunction with breathing exercises can be effective in decreasing anxiety and controlling shortness of breath. One technique involves tensing muscle groups while slowly inhaling and then relaxing the muscle groups while exhaling twice as slowly through pursed lips. It is helpful to teach the patient a sequence of muscle groups to tense and relax. One common sequence involves tensing and relaxing first the face; followed by the face and the neck; then the face, neck, and shoulders; and so on, down the body to the toes. A calm, quiet, and comfortable environment is important for the novice in learning any relaxation technique. Biofeedback in conjunction with relaxation therapy promotes more timely mastery of relaxation skills.17
Other Treatments and Considerations: Physical therapists are generally called on to instruct patients in chest expansion exercises, a series of exercises intended to increase the flexibility of the chest. Percussion and postural drainage use gravity and gentle drumming on the patient’s back to loosen secretions and help drain the secretions from the lungs. By isometrically contracting the arms and hands while they are placed on the patient’s thorax, the therapist may transmit vibration to the patient. Vibration is performed during the expiratory phase of breathing and helps loosen secretions. Percussion and postural drainage may, however, be contraindicated in acutely ill patients and those who are medically unstable.
Humidity, pollution, extremes of temperature, and stagnant air have deleterious effects on persons with respiratory ailments. The therapist and patient should take these factors into consideration when planning activity.
Migliore’s guidelines for the management of dyspnea provide a clinical progression and direction for the integration of dyspnea control techniques with progression of activity.27
Individuals with chronic respiratory or cardiovascular limitations are frequently restricted in their ability to perform ADLs. OT intervention can promote improvements in the client’s life management skills and quality of life.
Evaluation
A review of the medical record will identify the patient’s medical history (diagnosis, severity, associated conditions, and secondary diagnoses), social history, test results, medications, and precautions.
Patient Interview
It is common courtesy and good medical practice to begin every encounter with a patient by introducing oneself and explaining the purpose of the evaluation or intervention. Good interviewing skills, including asking the right questions, listening to the patient’s response, and observing the patient while responding, are considered integral aspects of the therapeutic use of self. Thoughtful, probing questions will help the patient and therapist identify areas of concern and lay the groundwork for establishing mutually agreeable goals. The therapist should observe the patient for signs of anxiety, shortness of breath, confusion, difficulty comprehending, fatigue, abnormal posture, reduced endurance, reduced ability to move, and stressful family dynamics. Interview questions should not only seek clarification of information that was unclear in the medical record but also clarify the patient’s understanding of his or her condition and treatment.
A patient with a history of angina should be asked to describe what the angina feels like. If the patient has also had an MI, the patient should be asked whether he or she can differentiate between the angina and the MI chest pain. Clarification of symptoms before treatment can prove invaluable should symptoms arise.
Asking patients to describe a typical day, to identify activities that bring on shortness of breath or angina, and to tell how their physical limitations interfere with the activities or occupations that they need to do or most enjoy doing will reveal problems that are meaningful and relevant to the patient.
Clinical Evaluation
The purpose of clinical assessment is to establish the patient’s present functional ability and limitations. The content of an occupational therapist’s clinical evaluation will vary from patient to patient and from setting to setting. Clients with impairments in the cardiovascular system will require monitoring of HR, BP, signs and symptoms of cardiac distress, and possibly ECG readings during an assessment of tolerance to postural changes and during a functional task. Table 44-4 provides a summary of appropriate versus inappropriate responses to activity. Individuals with disorders involving the respiratory system should be monitored closely for signs and symptoms of respiratory distress. If an oxygen saturation monitor is available, the patient’s range of motion, strength, and sensation may be grossly assessed within the context of the ADL assessment. The patient’s cognitive and psychosocial status will become apparent to a skilled clinician via interview and observation.
TABLE 44-4
Cardiovascular Response to Activity
| Appropriate | Inappropriate | |
| Heart rate (HR) | Increases with activity to no more than 20 beats/min above the resting heart rate | HR more than 20 beats/min above the resting heart rate (RHR) with activity, RHR ≥120, HR drops or does not rise with activity |
| Blood pressure (BP) | Systolic blood pressure (SBP) rises with activity | SBP ≥220 mm Hg postural hypotension (≥10-20–mm Hg drop in SBP, decrease in SBP with activity |
| Signs and symptoms | Absence of adverse symptoms | Excessive shortness of breath, angina, nausea and vomiting, excessive sweating, extreme fatigue (RPE ≥15), cerebral symptoms |
After completing the evaluation, the clinician has sufficient information to formulate an intervention plan. In establishing the intervention goals and objectives, the clinician verifies that the patient agrees with the intervention plans and projected outcome.
Intervention
Client goals, present clinical status, recent occupational performance history, response to current activities and occupations, and prognosis all help guide the progression of intervention for persons with cardiovascular or respiratory impairment. Clients with significant cardiac or pulmonary impairment, limited recent ability to participate in occupation, inappropriate responses to activities and occupations or orthostatic change, and a poor prognosis will progress very slowly. Individuals with little impairment of the heart or lungs, a recent history of normal occupational performance, appropriate responses to orthostatic change and activities and occupations, and a good prognosis will progress rapidly by comparison.
Progression and Energy Costs
The energy costs of an activity or occupation and the factors that influence energy costs can further guide the clinician in the safe progression of activity or participation in occupation. Oxygen consumption suggests how hard the heart and lungs are working and is indicative of the amount of energy needed to complete a task. Resting quietly in bed requires the lowest amount of oxygen per kilogram of body weight, roughly 3.5 mL O2/kg body weight. This can also be expressed as 1 basal metabolic equivalent (MET). As activity increases, more oxygen is needed to meet the demands of the task. For instance, dressing requires 2.5 METs, or roughly twice the amount of energy that lying in bed requires (Table 44-5). Franklin had a 2.5 MET for seated bathing and dressing. Guided by a MET table, the patient’s response to activity or occupation, the prognosis, and the patient’s goals, the occupational therapist will be able to determine a logical intervention progression. As a general rule, once a patient tolerates an activity (e.g., seated sponge bathing) with appropriate responses, the patient may progress to the next higher MET-level activity (e.g., standing sponge bath).
TABLE 44-5
Basal Metabolic Equivalent Table of Self-Care and Homemaking Tasks
| MET Level | Activities of Daily Living | Instrumental Activities of Daily Living, Work, Play, and Leisure |
| 1-2 | Eating, seated25; transfers, bed to chair; washing face and hands; brushing hair25; walking 1 mph | Hand sewing7; machine sewing; sweeping floors6; driving automatic car, drawing, knitting45 |
| 2-3 | Seated sponge bath,45 standing sponge bath,45 dressing and undressing,22 seated warm shower,45 walking 2-3 mph, wheelchair propulsion 1.2 mph | Dusting,25 kneading dough,7 hand-washing small items,7 using electric vacuum,25 preparing a meal,22 washing dishes,45 golfing45 |
| 3-4 | Standing shower, warm22; bowel movement on toilet7; climbing stairs at 24 ft/min45 | Making a bed22; sweeping, mopping, gardening45 |
| 4-5 | Hot shower,22 bowel movement on bedpan,22 sexual intercourse45 | Changing bed linen25; gardening, raking, weeding; rollerskating16; swimming 20 yards/min45 |
| 5-6 | Sexual intercourse,45 walking up stairs at 30 feet/min45 | Biking 10 mph on level ground45 |
| 6-7 | Walking with braces and crutches | Swimming breaststroke45; skiing, playing basketball, walking 5 mph, shoveling snow, spading soil45 |
The duration of sustained physical activity must be taken into account when activity guidelines are being determined. Obviously, persons who have difficulty performing a 2-MET activity must still use a commode (3.6 METs) or bedpan (4.7 METs) for their bowel management. This is possible because a person can perform at a higher than usual MET level for brief periods without adverse effects.
At 5 METs, sexual activity is frequently a grave concern to persons with impaired cardiovascular function and to their partners. Sexual intercourse is intermittent in its peak demands for energy. Patients are frequently able to return to sexual intercourse once they can climb up and down two flights of steps in 1 minute with appropriate cardiovascular responses.46 Providing the patient with information about when it is safe to resume sexual activity can reduce anxiety surrounding the resumption of sexual intercourse. Anxiety may be further decreased through discussion of sexual activity guidelines with the patient and partner and identification of various forms of romantic intimacy, such as hand holding and kissing, when intercourse is not feasible. Besides instructing the patient to monitor HR and symptoms of cardiac distress before and after intercourse, the therapist should inform the patient and partner that cardiac medications might affect the patient’s libido. The patient should be encouraged to inform the physician of problems related to sexual activity. In many cases the physician can adjust the patient’s medications to control symptoms (see Chapter 12 for additional appropriate clinical interventions).
Energy Conservation
When patients are taught methods to conserve their energy resources, they will be able to perform at a higher functional level without expending more energy. The principles of energy conservation and work simplification are based on knowledge of the ways in which specific factors cause various cardiovascular responses. Ogden identified six variables that increase oxygen demand: increased rate, increased resistance, increased use of large muscles, increased involvement of the trunk musculature, raising one’s arms, and isometric work (straining).40 Upper extremity activity has also been shown to require greater cardiovascular output than lower extremity activity, and standing activity requires more energy than seated activity. Extremes of temperature, high humidity, and pollution make the heart work harder. By applying this information, a skilled clinician can suggest modifications in activity that will decrease the amount of energy needed for the task.
Energy conservation training should be individualized for each patient. Time management is an invaluable tool for energy conservation. Time management involves learning to plan one’s activity or participation in occupation so that tasks requiring high energy expenditure are interspersed with lighter tasks and rest breaks are scheduled throughout the day, especially after meals. The most important part of educating the client is incorporating his or her active involvement in planning the day. Client involvement increases the likelihood of realistic goal attainment. Rather than prescribing how Harriet might sequence her ADLs, IADLs, and rest breaks throughout her typical day, the therapist might engage her in a conversation about what works or does not work well for her in her current performance patterns. The therapist would then ask probing questions, such as “Have you tried taking your shower at a different time of day?” and “Would laying your clothes out the night before help your morning go more smoothly?” Such a client-centered approach engages the patient in the process of designing realistic performance patterns that incorporate principles of energy conservation according to his or her own circumstances and values. Through such collaboration, the therapist demonstrates respect for the patient’s needs and increases the likelihood that changes will be implemented successfully.
Written material may augment energy conservation instruction. However, until the patient has successfully applied energy conservation principles to activity, the therapist should expect little follow-through with energy conservation recommendations. Practice and practical application of skills are critical to changing behavior.
The specific pulmonary rehabilitation intervention techniques of PLB, diaphragmatic breathing, dyspnea control postures, and relaxation techniques were discussed earlier in this chapter. Exhaling with exertion is another breathing principle for persons with compromised cardiac or pulmonary function. Franklin might be taught to exhale when having a bowel movement rather than holding his breath and straining. Harriet might be taught to exhale when lifting or lowering her pet’s water bowl. This technique is more energy efficient and helps control systolic BP responses to activity. It is important for the patient to practice these skills during treatment. Therapeutic support is often critical in learning.
Lifestyle Modification
Modification of lifestyle is a key component in improving cardiovascular health. Exercise education should include the benefits of exercise; a graded program of increased activity and participation in occupation; stretching, strengthening, and aerobic activity; guidelines for monitoring HR, BP, and rate of perceived exertion; cool down; safety issues related to clothing, environmental factors, and warning signs; a plan for resuming exercise if it is skipped for a period; and emergency guidelines. Although the physical therapist typically designs and oversees the exercise program, the occupational therapist can provide valuable insight into forms of exercise that might be meaningful to the patient. Modification of diet may be addressed by the dietitian but can readily be reinforced during meal preparation activities. To stop smoking, refrain from excessive alcohol consumption, and stop abusing drugs are challenging goals for clients who have developed these habits. Support groups, counseling, and medical management play key roles in successful cessation or modification of these risk factors. Occupational therapists believe that enabling the client’s participation in rounds of personally meaningful and healthy occupations can also play a key role in supporting health and controlling such risk factors.
Patient and Family Education
As members of the health care team, occupational therapists share the responsibility for patient and family education. The team must instruct the patient and family members in cardiac or pulmonary anatomy, the disease process, management of symptoms, risk factors, diet, exercise, and energy conservation and must reinforce the teaching. Inclusion of family members in an education program provides support indirectly to the client through the family unit. Such support is critical when the client depends on the assistance of a family member to accomplish everyday tasks.
Summary
Healthy persons are able to meet the varying demands of their bodies for oxygen because their heart and respiratory rates adjust to meet oxygen demand. When either the cardiovascular or the pulmonary system (or both) is compromised, the ability to perform normal activities or occupations declines. This chapter is intended to guide the occupational therapist in the treatment of clients with impairment of the heart or lungs and in designing programs to maximize clients’ independent performance in areas of occupation to support participation in context. The two case studies presented in this chapter and related information portray the range of problems involving client factors, contextual issues, performance skills, and performance patterns that typically interfere with the client’s ability to perform customary activities and occupations.
1. Describe the heart, including its size, anatomy, and functional parts.
2. Name the heart valves, and give their locations and functions.
3. Discuss the relationship between the coronary arteries and health of the heart.
4. List and describe the symptoms of cardiac distress.
5. What are the typical psychosocial responses to a diagnosis of heart disease?
6. How is cardiac response to activity monitored? How does the therapist know that a change in level of activity is warranted?
7. Describe the functional parts of the pulmonary system.
8. What is COPD, and what is its significance for occupational performance?
9. What can the OT practitioner do to help prevent or reduce the incidence of COPD?
10. Demonstrate the recommended dyspnea control postures.
11. Compare pursed-lip breathing with diaphragmatic breathing. When should one be used rather than the other?
12. Describe the appropriate evaluation content and approach for patients with cardiac and pulmonary problems.
13. What is a MET, and what is the clinical value of a MET table for occupational therapists?
14. How would you teach energy conservation techniques to the following individuals, all of whom have cardiac or pulmonary disease?
• A 40-year-old female marathon runner
• A 50-year-old homemaker and adoptive mother of eight (including three children younger than 6 years)
• A 60-year-old air conditioner repairman
• A 72-year-old man who says his main pleasures are riding thoroughbreds, drinking good Kentucky bourbon, smoking cigars, and enjoying the company of lovely women
References
1. Agle, DP, Baum, GL. Psychological aspects of chronic obstructive pulmonary disease. Med Clin North Am. 1977;61(4):744.
2. American Thoracic Society. Definitions and classifications of chronic bronchitis, asthma, and pulmonary emphysema. Am Rev Respir Dis. 1962;85:762.
3. Bragg, TL. Psychological response to myocardial infarction. Nurs Forum. 1975;14(4):383.
4. Brannon, FJ, Foley, MW, Starr, JA, Saul, LM. Cardiopulmonary rehabilitation: basic theory and application, ed 3. Philadelphia, Pa: Davis; 1997.
5. Breslin, EH. The pattern of respiratory muscle recruitment during pursed-lip breathing. Chest. 1992;101(1):75.
6. Chan, SCC. Chronic obstructive pulmonary disease and engagement in occupation. Am J Occup Ther. 2004;58:408–415.
7. Colorado Heart Association. Exercise equivalent (pamphlet). Boston, Mass: Cardiac Reconditioning & Work Evaluation Unit, Spaulding Rehabilitation Center; 1970.
8. Dahlén, I, Janson, C. Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest. 2002;122:1933.
9. Dangas, G, Kuepper, F. Cardiology patient age, restenosis: repeat narrowing of a coronary artery: prevention and treatment. Circulation. 2002;105(22):2586.
10. Dawber, TR. The Framingham study, the epidemiology of atherosclerotic disease. Cambridge, Mass: Harvard University Press; 1980.
11. Dubin, D. Rapid interpretation of EKGs, ed 6. Tampa, Fla: Cover Publishing; 2000. [updated 2007].
12. Dudley, DL, Glaser, EM, Jorgenson, BN, Logan, DL. Psychosocial concomitants to rehabilitation in chronic obstructive pulmonary disease. Part 2: psychosocial treatment. Chest. 1980;77(4):544–551.
13. Farzan, S. A concise handbook of respiratory diseases, ed 4. Reston, Va: Reston Publishing; 1997.
14. Froom, P, Gofer, D, Boyko, V, Goldbourt, U. Risk for early ischaemic event after acute myocardial infarction in working males. Int J Occup Med Environ Health. 2002;15:43–48.
15. Goldberger, E. Essentials of clinical cardiology. Philadelphia, Pa: Lippincott; 1990.
16. Goldman, L, Hashimoto, B, Cook, EF, Loscalzo, A. Comparative reproducibility and validity of systems for assessing cardiovascular functional class: advantages of a new specific activity scale. Circulation. 1981;64:1227–1234.
17. Green, E. Biofeedback techniques for deep relaxation. Psychophysiology. 1969;6(3):371.
18. Greenland, P. Efficacy of supervised cardiac rehabilitation programs for coronary patients: update 1986-1990. Cardiopulm Rehabil. 1991;11:190.
19. Hodgkin, JE, Celli, BR, Connors, GL. Pulmonary rehabilitation guidelines to success, ed 3. Philadelphia, Pa: Lippincott Williams & Wilkins; 2000.
20. Jette, DC, Downing, J. The relationship of cardiovascular and psychological impairments to the health status of patients enrolled in cardiac rehabilitation programs. Phys Ther. 1996;76(2):130–139. [discussion 140-148].
21. Kinney, M. Andreoli’s comprehensive cardiac care, ed 8. St. Louis, Mo: Mosby; 1995.
22. Kottke, FJ. Common cardiovascular problems in rehabilitation. In: Krusen FH, Kottke FJ, Elwood PM, eds. Handbook of physical medicine and rehabilitation. Philadelphia, Pa: Saunders, 1971.
23. Levin, LA, Perk, J, Hedback, B. Cardiac rehabilitation: a cost analysis. J Intern Med. 1991;230(5):427.
24. Lichtman, JH, Bigger, JT, Jr., Blumenthal, JA, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–1775.
25. Maloney, FP, Moss, K. Energy requirements for selected activities. Denver, Colo: Department of Physical Medicine, National Jewish Hospital (unpublished); 1974.
26. Mckenna, K, Mass, F, Tooth, L. Predictions of quality of life after angioplasty. Scand J Occup Ther. 1998;5:173–179.
27. Migliore, A. Management of dyspnea guidelines for practice for adults with chronic obstructive pulmonary disease. In Occupational therapy in health care. Binghamton, NY: Haworth Press; 2004.
28. Mithal, M, Mann, WC, Granger, CV. The role of coronary heart disease (CHD) in functional limitation in community dwelling elders. Phys Occup Ther Geriatr. 2001;19(3):33–46.
29. Mythos for SoftKey. BodyWorks 4.0: human anatomy leaps to life. Cambridge, Mass: SoftKey International; 1993-1995.
30. National Institutes of Health. Available at http://health.nih.gov/category/HeartandCirculation. [December 1, 2010].
31. National Institutes of Health. Available at http://health.nih.gov/category/LungsandBreathing. [December 8, 2010].
32. National Institutes of Health. Available at http://www.nhlbi.nih.gov/health/dci/Diseases/cabg/cabg_whatis.html. [December 7, 2010].
33. National Institutes of Health. Available at http://www.nhlbi.nih.gov/health/dci/Diseases/Cad/CAD_WhatIs.html. [December 3, 2010].
34. National Institutes of Health. Available at http://www.nhlbi.nih.gov/health/dci/Diseases/Cad/CAD_WhoIsAtRisk.html. [December 7, 2010].
35. National Institutes of Health. Available at http://www.nhlbi.nih.gov/health/dci/Diseases/Hf/HF_WhatIs.html. [December 3, 2010].
36. National Institutes of Health. Available at http://www.nhlbi.nih.gov/health/dci/Diseases/ht/ht_whatis.html. [December 7, 2010].
37. National Institutes of Health. Available at http://www.nhlbi.nih.gov/health/dci/Diseases/HeartAttack/HeartAttack_Treatments.html. [December 7, 2010].
38. National Institutes of Health. Available at http://www.nhlbi.nih.gov/health/dci/Diseases/hlw/hlw_lungdis.html. [December 10, 2010].
39. Nemery, B, Moavero, NE, Brasseur, L, Stănescu, DC. Changes in lung function after smoking cessation: an assessment from a cross-sectional survey. Am Rev Respir Dis. 1982;125(1):122–124.
40. Ogden, LD. Guidelines for analysis and testing of activities of daily living with cardiac patients. Downey, Calif: Cardiac Rehabilitation Resources; 1981.
41. Oldridge, NB, Guyatt, GH, Fischer, ME, Rimm, AA. Cardiac rehabilitation after myocardial infarction. JAMA. 1988;260(7):945–950.
42. Perkins-Porras, L, Whitehead, D, Strike, P, Steptoe, A. Causal beliefs, cardiac denial and pre-hospital delays following the onset of acute coronary syndromes. J Behav Med. 2008;31(6):498–505.
43. Hambrecht, R, Gielen, S, Linke, A, et al. Effects of exercise training on left ventricular function and peripheral resistance in patients with chronic heart failure: a randomized trial. JAMA. 2000;283(23):3095–3101.
44. Renfroe, KL. Effect of progressive relaxation on dyspnea and state anxiety in patients with chronic obstructive pulmonary disease. Heart Lung. 1988;17(4):408.
45. Santa Clara Valley Medical Center. Graded activity sheets. San Jose, Calif: Santa Clara Valley Medical Center; 1994.
46. Scalzi, C, Burke, L. Myocardial infarction: behavioral responses of patient and spouses. In: Underhill SL, et al, eds. Cardiac nursing. Philadelphia, Pa: Lippincott, 1982.
47. Sheikh, A, Marotta, S. Best practices for counseling in cardiac rehabilitation settings. J Counsel Dev. 2008;86(1):111–120.
48. van Dixhoorn, JJ, Duivenvoorden, HJ. Effect of relaxation therapy on cardiac events after myocardial infarction: a 5-year follow-up study. J Cardiopulm Rehabil. 1999;19(3):178.
49. Venes, D, Thomas, CL, Taber, CW. Taber’s cyclopedic medical dictionary, ed 19. Philadelphia, Pa: Davis; 2001.