Chapter 10 Continuing professional development and fitness to practise
Introduction
The term continuing professional development (CPD) is familiar to most people and yet is frequently misunderstood. This chapter is designed to develop an understanding of CPD and to consider the importance to pharmacists of individual active engagement in an ongoing programme of CPD.
A search of the World Wide Web for the phrase ‘continuing professional development’ recently returned more than 30 million hits. The web search showed the phrase is not specific to pharmacy and pharmacists. The results included reference to CPD for teachers, psychotherapists, lawyers, architects, healthcare professionals and many more. Thus, a wide range of people in varying professions all over the world are involved in CPD. These professionals all recognize the value of planned CPD. In most professions CPD is not optional but mandatory. In the UK and many other countries (see Ch. 2) CPD is mandatory for pharmacists. It is relevant to all practising pharmacists, whether experienced and full time or newly qualified and just starting their career. CPD for pharmacists is part of being a professional with an obligation on all to continue to enhance their own knowledge and skills throughout their career and working life.
CPD is related to, and indeed part of, clinical governance (see Ch. 8). Clinical governance is about both continuous quality improvement and being accountable for quality improvement. As such, CPD is an integral part of clinical governance and it involves all healthcare professionals. Those healthcare professionals working in the UK NHS will find there are specific requirements for clinical governance and CPD which are mandatory. The Community Pharmacy Contract (England and Wales) with the NHS states a clear need for community pharmacists to be undertaking and maintaining CPD records within the clinical governance requirements (essential service number eight). In addition to this, the Code of Ethics of the Royal Pharmaceutical Society of Great Britain (RPSGB) places further obligations on pharmacists. Before any service is offered, whether to prescribers, patients or others, a pharmacist must ensure that whoever is delivering the service has a relevant level of competence, skill or knowledge in that area. CPD allows the pharmacist to provide evidence and demonstrate competence.
What is continuing professional development?
CPD means many things to many people. The NHS defines it as ‘a process of lifelong learning for all individuals and teams which meets the needs of patients and delivers the health outcomes and healthcare priorities of the NHS and which enables professionals to expand and fulfill their potential’ (Department of Health 1998). While this definition is accurate, it is somewhat lengthy. An easier option is to consider the three words individually:
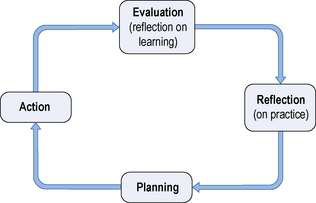
CPD can be defined as the process of reflection, planning, action and evaluation through which pharmacists continuously develop their knowledge, skills, attitudes and behaviours throughout their professional careers. CPD in the UK applies to both pharmacists and registered pharmacy technicians.
The RPSGB began introducing a framework for CPD for pharmacists in 2002. CPD was developed in pharmacy as a response to the profession’s wishes, expressed in a consultation exercise for the Pharmacy in a New Age (PIANA) project in the 1990s, and in response to the requirements of the Health Act 1999.
Today, the concept of CPD remains a relatively new idea and process for pharmacists. Prior to the introduction of the CPD framework, pharmacists had to engage in 30 hours of continuing education each year in line with the professional obligation stated in their code of ethics. This requirement has been replaced with a formal need for CPD records to be completed and retained for the duration of a pharmacist’s career in order to demonstrate the pharmacist is competent to be undertaking the role they are working in at the time.
CPD gives a pharmacist the opportunity to demonstrate to their employer, the NHS, and to patients that they are maintaining and building their own professional capabilities.
Background to CPD
The requirement for formal CPD arose from an increasing pressure on the government to ensure healthcare professions operate in a ‘professional’ manner. Professional accountability has been highlighted by many well documented high-profile reports and incidents. For instance, the Kennedy Report, published in 2001, highlighted gaps in the way the medical profession and the professions allied to medicine kept abreast of changing techniques, knowledge, methods and processes, etc. The report made recommendations for ongoing professional development and suggested CPD should not focus solely on clinical skills but should encompass both attitudes and communication skills.
The Pharmacists and Pharmacy Technicians Order 2007 in the UK initiated the final steps for mandatory CPD for practising pharmacists registered with the RPSGB. This means that pharmacists must keep a record of their development which shows they are ‘actively’ keeping up to date with the knowledge they use day to day. By keeping up to date they are able to demonstrate ongoing competence in their current role, or roles that they wish to pursue in the future.
The RPSGB format for recording CPD involves keeping a written record of an activity or event, demonstrating that the pharmacist has learned from a situation relevant to their professional role.
Pharmacists gain from taking ownership of their CPD, since CPD is a personal activity: it is specific to each pharmacist. No two pharmacists will have the same CPD records. CPD is designed to help pharmacists structure and plan ways to ensure that their skills are constantly being updated and renewed. CPD puts pharmacists in control of their learning.
CPD cycle
CPD is defined as a systematic, ongoing, cyclical process of self-directed learning. It should enable pharmacists to do their job more effectively and involves employers as well as individuals.
CPD is a four-stage process which helps the pharmacist plan their learning and track, record and reflect on learning and development. The learning may be clinical or related to a skill, attitude or behaviours associated with the pharmacist’s role. The four stages are often depicted as a cyclical process. The RPSGB recording system is based on the four stages of the CPD cycle.
The four stages of the cycle are shown in Figure 10.1 and involve:
Reflection on practice
Reflection involves the pharmacist spending time reflecting on current performance and how work is undertaken. The reflection time aids in the pharmacist identifying personal learning and development needs. The pharmacist is the best person to identify their own personal learning needs. Reflection involves the pharmacist thinking about how daily tasks are carried out, the areas in which the pharmacist feels knowledge or skills are weak or events have happened which indicate a pharmacist needs to improve knowledge or skills in that area.
Sometimes a particular situation or event will draw the attention of the pharmacist to a weakness in knowledge, ability or systems of work which, if not addressed, could cause further problems. This is called a critical incident (see Ch. 9).
When reflecting, there are several questions the pharmacist may ask:
Other ways of identifying learning needs or knowledge, skill, attitude or behaviour gaps is for the pharmacist to consider the following activities:
When identifying learning needs, the pharmacist must remember to keep the learning need simple. A learning need broken down into bite-size pieces is easier to address. The process of reflecting on what a pharmacist does not know or is unable to do results in identification of training needs.
Planning
Having identified learning needs, the pharmacist next needs to plan what can be done to meet these learning needs and how it can be achieved. At this stage, if several learning needs have been identified the pharmacist will have to prioritize learning. When prioritizing, the pharmacist needs to consider the impact of the learning on one’s self, on colleagues, on the organization worked for and on the patient.
If the pharmacist has identified more than one learning need then it may be that more than one CPD cycle needs to be started. When planning actions to meet learning objectives, the pharmacist needs to consider:
Additionally, at this stage the pharmacist needs to consider what the consequence of not undertaking the learning would be. If the pharmacist realizes that the learning need is no longer urgent or important, then it is appropriate not to take it any further.
When considering how to meet learning needs, there are a number of ways that learning can be undertaken. The RPSGB suggests pharmacists be creative and not limit themselves to formal or certificated courses. Pharmacists may wish to consider the following methods (this list is not exhaustive):
It is important to recognize pharmacists all learn in different ways and all have preferences. It may be worthwhile considering options which may have not been considered before.
Action
At this stage of the cycle, once the plan is complete for what needs to happen, it is time for the pharmacist to put the plan into action and commence learning. Action is simply carrying out the plan. While this sounds simple, the time taken to undertake the learning needs to be built into the plan and the timetable adhered to.
While undertaking the actions, the pharmacist should throughout be asking:
As these questions are answered, a record should be made of what has been learned.
Evaluation (reflection on learning)
As with all development, evaluating what learning has been undertaken and how it has been undertaken is important. During the evaluation process, pharmacists should consider a series of questions:
In some cases pharmacists may find that what has been learned is not what they set out to learn. In this case the pharmacist needs to revisit the original learning need and consider if the requirement to undertake further actions is still necessary for their practice. If the pharmacist decides the learning need is still valid, then this will lead the pharmacist into a new CPD cycle or alternatively the pharmacist can go back a couple of steps in the cycle and add in different actions.
If the pharmacist does not have the learning need any longer because it is no longer relevant or it has been overtaken by other priorities or events, then the pharmacist may exit the CPD cycle there.
Assessing whether the learning undertaken has been effective
A further question that the pharmacist needs to ask is: ‘Can my practice now be shown to have improved as a result of the learning experience or is further learning required?’ Realistically, true evaluation may not occur for some weeks or months, since an opportunity to apply learning may not occur sooner.
Scheduled learning vs unscheduled learning
The CPD cycle is a circle – each stage flows into the next. There are three entry points into the cycle – ‘Reflection on practice’, ‘Planning’ and ‘Action’. The exit (end point) is always ‘Evaluation’, when the impact of the learning undertaken is reviewed.
Scheduled learning is another term given to CPD which enters the process at ‘Reflection on practice’. This is when someone or something leads the pharmacist to identify a learning need or knowledge gap and plan ways that the pharmacist can meet this need or gap. This can be as simple as someone asking the pharmacist a question that the pharmacist does not know the answer to.
Unscheduled learning is learning that starts from ‘Action’. This is learning that happens unexpectedly through someone or something. It is learning that was not planned and has not happened consciously.
All entry points into the CPD cycle are valid. Ordinarily a pharmacist would have a mixture of cycles, some starting at ‘Reflection’ or ‘Planning’, which indicates the pharmacist is thinking about his practice and planning appropriate actions, and some entries starting at ‘Action’, which indicates the pharmacist is receptive to new ideas and concepts as they arise.
Recording CPD
The CPD four-stage cyclical process should be documented to demonstrate learning is being undertaken which meets the needs of the individuals and the organizations in which the pharmacist works. The RPSGB has issued guidance stating the requirement to record CPD in a specially designed format. The RPSGB gives additional guidance stating how much CPD a pharmacist records is dependent on personal development needs. It is advised that a pharmacist focus on the quality of the process and recording rather than the quantity.
Generally a pharmacist needs to aim to record at least one CPD entry each month, although ordinarily most pharmacists will undertake greater CPD daily in the course of professional work.
The time taken to undertake a CPD cycle may be hours, days, weeks, months or, for some learning needs, years. The length of time taken to record a CPD cycle is about 30 minutes. This time includes the pharmacist recording the cycle and the thinking during the process. It is worth acknowledging that initially it may take longer than 30 minutes but as a pharmacist becomes more familiar and experienced in the process this time should reduce.
The CPD framework described is designed specifically for use by both pharmacists and technicians registered with the RPSGB. The framework was piloted with 500 pharmacists in all branches of the profession. Many of these pharmacists found that CPD was not an onerous burden and in fact it increased their personal satisfaction from work.
The RPSGB is of the view that pharmacists will need to submit their CPD records periodically for review to the RPSGB or equivalent regulatory body. This periodic review is likely to be every 3–5 years. The method of review will involve evaluating the records against a set of evaluation criteria.
In summary, CPD describes any activity – whether formal course, informal query from a patient or personal study – that helps a pharmacist do their job better, resulting in a more competent service to customers, line manager, colleagues and the organization, and helps the pharmacist progress faster in their career. CPD is a cyclical process. For everyone, the need for the updating of knowledge and skills is a continuous one. Pharmacists moving from one post to another may need new skills. Pharmacists may find job descriptions change over time and new developments in practice need to be implemented, which may also require new skills and knowledge. Learning does not stop after the first degree course, or after the pre-registration year or after completing a postgraduate qualification. Learning continues throughout life. What CPD does is to focus that learning on the needs of the individuals and the organizations which employ them.
Fitness to practise
Pharmacy in the UK is in a period of regulatory change. Regulations regarding fitness to practise in pharmacy have recently been implemented. It is well recognized throughout the pharmacy profession that this form of regulation is necessary in order to maintain and develop public confidence in pharmacists and other healthcare professions. In the past there has been a concern over disparity between regulation of different professions. Some professions being ‘over-regulated’ and others ‘under-regulated’ has impaired public confidence.
The UK Government in 2007 published a document entitled Trust, Assurance and Safety – The Regulation of Health Professionals in the 21st Century. This outlined proposals to ensure patient, public and professional confidence in the healthcare professionals’ watchdogs to improve patient safety and ensure the fair treatment of healthcare professionals. Further proposals also suggested healthcare professionals will be required to prove their fitness to practise every 5 years. How this will impact on pharmacists and what role CPD has to play in proving fitness to practise and revalidation is very much in its embryonic stages.
Within the pharmacy profession, moves for additional broader regulation have commenced through the Pharmacists and Pharmacy Technicians Order 2007 which aims to bring pharmacist regulation into line with other professions. The main provisions in the order are as follows:
Declaration of fitness to practise
Pharmacists are required to make an annual fitness to practise declaration to the RPSGB. The declaration signed by practising pharmacists confirms their commitment to the Code of Ethics, to work under the standards and guidance published by the RPSGB and to undertake CPD. The declaration also confirms that the signatory has not been or is not the subject of any regulatory, civil or criminal proceedings or investigations relevant to their fitness to practise. Non-practising pharmacists sign a declaration to confirm they will not practise.
Pharmacists who fail to make an annual declaration are sent a letter by the RPSGB advising them that a note will be made on their file, and that until a declaration is received they will not be eligible for a letter of good standing or a certificate of current professional statement; this includes a complete fitness to practise check for inclusion in NHS pharmaceutical provider lists. Following the receipt of the letter the pharmacist has 2 months to provide a declaration; failure to do so will lead to an automatic removal of name from the Pharmaceutical Register.
In addition to the annual declaration pharmacists have a responsibility under the Code of Ethics to promptly declare to relevant parties, including the RPSGB, their employer and other relevant authority, any circumstances following completion of a declaration that may call into question their fitness to practise. The RPSGB states that pharmacists have a responsibility to notify their profession to the police should they be charged with any offence.
Roles of the statutory committees in fitness to practise
The Pharmacists and Pharmacy Technicians Order 2007 for fitness to practise has established three new statutory committees: the Investigating Committee, the Health Committee and the Disciplinary Committee (see Ch. 8).
In the past, the RPSGB had powers to consider allegations of misconduct and to make decisions and recommendations based on the misconduct. Under the changes introduced by the Pharmacists and Pharmacy Technicians Order 2007, the RPSGB is able to consider a wider range of allegations, including those relating to a registrant’s physical and mental health. The Pharmacists and Pharmacy Technicians Order 2007 provides the RPSGB’s new statutory committees with a wider range of sanctions and options for disposal. The new Investigating Committee has the power, in certain circumstances and where the allegation is admitted, to accept written undertakings. The Disciplinary and Health Committees have the power to impose conditions on registration and to suspend a person’s name from the register for a period of up to 1 year, as well as the power to direct removal from the register.
Conclusion
In summary, the Pharmacists and Pharmacy Technicians Order 2007 states the fitness to practise guidance for pharmacists and pharmacy technicians in respect of standards of conduct, practice and performance, and the need to disclose information will change from time to time. It is important for all practising pharmacists to be engaged in regular CPD regarding updating their knowledge of practice, regulation and legislative changes within their field of work.