13 Rabbit conjunctivitis
PRESENTING SIGNS
The owner’s usual complaint is of a red eye, but frequently it is also sore, and often quite significant discharge is present. Rabbits of any age or breed can be affected and one or both eyes can be involved. If the rabbit is housed with others these too could be affected. The rabbit is usually clinically well, although some might be eating less, and some will have a nasal discharge and the owner might report noisy breathing.
CASE HISTORY
The condition is usually sudden in onset, and often one eye is affected initially, closely followed by the other. There is frequently no relevant previous history, although sometimes the condition will coincide with a change in management – different bedding, feeding from different containers, a change in placement of the outdoor run, or the introduction of a new rabbit to the household. Some rabbits will have a history of previous ocular or respiratory infections.
CLINICAL EXAMINATION
General clinical examination can be variable. In many animals it will be normal but a significant number will have evidence of respiratory disease – nasal discharge, increased respiratory rate and effort, mild pyrexia and so on. Sometimes the rabbit will be thin. As with all rabbits which are presented to the surgery their teeth should be checked!
On ophthalmic examination the affected eye(s) will be obviously red and inflamed. Thus marked conjunctival hyperaemia will be present, usually affecting both bulbar and palpebral conjunctiva, and moderate chemosis is frequently also present. Sometimes the conjunctiva is so swollen that visualization of the eye itself is difficult. Moderate blepharospasm is present, frequently with significant lid swelling as well as hyperaemia. The lids should be checked for signs of entropion which can occur in young rabbits and will cause secondary conjunctival hyperaemia. An ocular discharge is almost always present but can be very variable in nature. Initially it is usually serous but rapidly becomes mucopurulent and can be very thick and sticky – adhering to the eyelids and medial canthal skin and sometimes causing local skin excoriation.
The cornea should always be stained with fluorescein to check for evidence of corneal ulceration but this can be difficult in very painful eyes with excessive chemosis. A slight miosis can be present but in general intraocular examination is unremarkable.
CASE WORK-UP
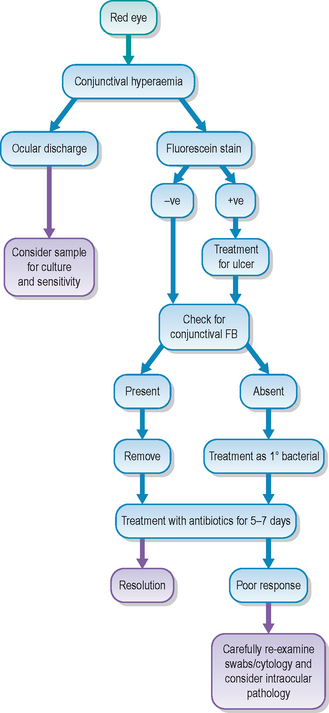
Although swabs for bacterial culture and sensitivity are not usually taken from rabbits on initial presentation – empirical treatment is usually tried first – it is certainly something to consider: they can always be discarded if necessary but cannot be retaken after the eye has been cleaned up! Cytology can also be considered.
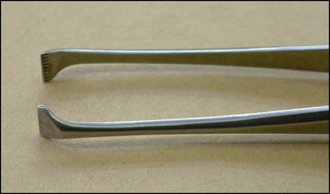
It is important to check for any foreign body – fragments of hay, straw and sawdust frequently become trapped in the conjunctival fornix or behind the third eyelid. Topical anaesthetic drops are applied to the eye and to a cotton bud. The latter can be gently rolled in the lower and upper fornix and will attract any debris. Flush copiously with sterile saline – a 5 ml syringe with a cut-off nasolacrimal cannula on the end is ideal for flushing the fornix. The third eyelid can be grasped with atraumatic forceps – von Graefe forceps (Figure 13.1) are ideal since they grip well without damaging the conjunctiva – and it is gently elevated to check behind for any foreign matter.
Since the main differential for conjunctivitis in rabbits is dacryocystitis, it is sensible to flush the nasolacrimal duct on initial presentation. The procedure for doing this is described in the case on rabbit dacryocystitis (Chapter 19, p. 115). Flushing at initial presentation will not only differentiate conjunctivitis from the more serious nasolacrimal duct involvement but will also immediately establish drainage such that any build up of discharge is less likely to block the duct and actually cause a secondary dacryocystitis should the rabbit not respond to its initial treatment.
It is important to keep the rabbit comfortable and regular removal of any ocular discharge will be beneficial – especially if this is sticky and building up such that the rabbit cannot open its eye. Soft, gauze-free swabs soaked with sterile saline are ideal. The rabbit will be treated with either drops or ointment. If the latter, it is sensible to change the bedding to shredded paper rather than straw or sawdust to reduce the risk of further damage as debris adheres to the ointment as well as the ocular discharge!
EPIDEMIOLOGY
Management errors and bacterial infections are the most common causes for conjunctivitis in rabbits. Overhead hay nets should be avoided as debris can fall into the eyes, causing conjunctivitis. Poor quality straw bedding can have the same effect. If the rabbit’s hutch is not cleaned frequently a build up of ammonia and so on can decrease air quality and trigger irritation and then conjunctivitis. Overcrowding can also be an issue in some cases.
Pasteurella spp. are considered the most frequent primary bacterial infection in rabbits, causing conjunctivitis, dacryocystitis, abscesses and respiratory infections. Staphylococcal spp. are also frequently isolated with occasional reports of Haemophilus spp. The underlying bacterial type cannot be distinguished clinically – hence the need for culture and sensitivity testing. Viral causes are also encountered – the myxoma virus has various strains and the actual presentation will be different according to the strain involved. Typically lid swelling (blepharoedema) is dramatic and considered pathognomonic for myxomatosis, but early symptoms might be just a conjunctivitis (unfortunately followed by a swift death in many animals).
TREATMENT OPTIONS – MEDICAL
Most initial medication will consist of broad spectrum antibiotic drops or ointment. Gentamicin and fusidic acid are both licensed in rabbits. Drops have the advantage of not clogging up the lids and encouraging debris to stick, but have the disadvantage of requiring more frequent application. Even if the conjunctiva seems very inflamed, steroid-containing topical medication is not required as a primary medication. Systemic administration of enrofloxacin is sometimes also advocated. Most rabbits will respond within a few days – if not, then further thorough examination is required with sampling if necessary. Affected rabbits should always be isolated and kept in clean, warm, dry, dust-free surroundings until fully recovered.
PROGNOSIS
The prognosis for rabbits with conjunctivitis only is generally good, providing the underlying cause is identified and corrected quickly. However, if the condition is neglected, then a secondary dacryocystitis will rapidly develop and the long-term management of this can be challenging and frustrating. Similarly, if a foreign body is present but undetected, it can easily cause corneal ulceration and, if not removed, can even result in corneal perforation. Many rabbit owners are aware of these risks and so will present their pets timely but unfortunately some are ignorant of the potential seriousness of an untreated conjunctivitis.
The rabbit lived with a neutered male rabbit and a guinea-pig in a large outside hutch with access to grass. It was reportedly fit and well and had never suffered from ocular problems before. The owners noticed that the left eye was red and a watery discharge was present. They bathed it for 48 hours but there was no improvement and the right eye then started to look a bit red. Hence they sought veterinary attention. The in-contact animals were unaffected. There had been no change in the management of the animals.
CLINICAL SIGNS
General clinical examination was unremarkable – the rabbit was of a suitable weight and no noticeable dental disease was observed on a brief oral examination. The left eye was uncomfortable and held half closed. Marked tear overflow was present with some nasofacial dermatitis. The discharge was mainly serous but some mucopurulent matter was present in the conjunctival fornix ventromedially. The conjunctiva was extremely hyperaemic – particularly the palpebral rather than bulbar regions (Figure 13.3). The eyelid margins were thickened. No corneal ulceration was present and intraocular examination appeared normal. Mild conjunctival hyperaemia was present in the right eye but no significant discharge was noted.
WORK-UP
The left eye was gently bathed with sterile saline. A drop of topical anaesthesia (proxymetacaine) was applied to the eye and the fornix was carefully flushed again to ensure that no pieces of plant matter or similar foreign body were present – none were found. The bulbar surface of the nictitans membrane was also similarly checked with no foreign material identified. Since the rabbit was very good to handle, it was decided to flush the nasolacrimal duct. No obstruction was present and clear saline was obtained from the nose, ruling out dacryocystitis as a possible diagnosis. No work-up was undertaken for the right eye.
TREATMENT
The rabbit was treated with topical gentamicin drops three times daily bilaterally, and the owner instructed to gently bathe any discharge prior to applying the medication. Soft white paraffin (Vaseline) was advised to be applied once daily to the sore patch of skin ventromedial to the eye but no topical or systemic antibiosis was deemed necessary to treat the dermatitis. The rabbit was kept separate from its companions.
Five days later there had been no improvement in the left eye – still very inflamed with the mucopurulent discharge – while the right eye had deteriorated with more conjunctival hyperaemia and now a serous discharge from this eye. It was suggested that swabs were taken for culture and sensitivity, and the nasolacrimal duct flushing repeated bilaterally. However, the owners did not want any additional expense and so instead treatment was changed to fusidic acid twice daily bilaterally. Within 48 hours both eyes were much improved – minimal conjunctival hyperaemia, resolution of the lid swelling in the left eye and a significant reduction in the ocular discharge.
OUTCOME
The fusidic acid was continued for another 5 days (a full week in total), by which time both eyes appeared normal. It is assumed that a bacterial infection was present, with resistance to gentamicin. This could suggest a Gram-positive organism such as Staphylococcus spp. which have commonly been isolated from rabbits with conjunctivitis. However, without bacterial culture and sensitivity testing this is speculative. Thankfully the condition responded well and the rabbit did not develop dacryocystitis (the owners had been warned of this possibility right from the outset).