Ear
The Ear – Tiny Yet Complex Like a Maze
The ear (Auris) contains the sensory apparatus and nerve cells of two sensory systems that arise from a common embryonic system (the otic placode), but serve very different purposes: hearing and equilibrium or balance. The small, delicate, membranous, convoluted organs, which carry the sensory cells of both modalities, are located in the membranous labyrinth (see below). In turn, the labyrinth is positioned inside the petrous part of the temporal bone (Pars petrosa ossis temporalis), the bony pyramid that separates the posterior and medial cranial fossa. The sensory nerve, the N. vestibulocochlearis [VIII], emerges from the inner ear.
In humans (as in terrestrial vertebrates) a former (the first) pharyngeal groove (also named bronchial groove, pharyngeal cleft, or bronchial cleft) plus surrounding bones and muscles are part of the construction of the acoustic part of the ear – this includes the sound-conducting apparatus, the middle ear and the outer ear. In fish, a pharyngeal groove is a typical “breathing hole”; water “inhaled” through the mouth is expelled from the pharynx via the branchial hole. The “ear-branchial cleft” of terrestrial animals does not longer open, since a very thin membrane, the tympanic membrane (Membrana tympanica), closes it off. If the tympanic membrane had a hole, one could theoretically breathe “through the ears”, since a continuous opening would exist that connects the external acoustic (auditory) meatus to the pharynx. Practically, this is not possible because the ducts are too narrow. However, divers with ruptured tympanic membranes can experience difficulties due to influx of water into the pharynx.
Outer Ear (Auris externa)
The outer ear extends from the auricle (Auricula) to the external acoustic (auditory) meatus (Meatus acusticus externus) up to the tympanic membrane. In other words, it is the “outer part” of the former branchial cleft.
Auricles of rabbits or horses are flexible, foldable, and are used for directional hearing. In humans, only some flexibility is conserved, whereas folding and motility of the outer ear are lost. Despite the presence of remnants of these ear muscles, they are usually too weak to support significant movement of the auricle. Nevertheless, the Concha, made of elastic cartilage, assists in directional hearing in humans.
The external acoustic (auditory) meatus is 3–4 cm in length and S-shaped. It consists of a distal cartilaginous component, which continues as an osseous canal in the petrous part of the temporal bone. The osseous canal ends at the tympanic membrane. Immediately above and below to the external acoustic meatus is the temporomandibular joint. One can feel the deformation of the cartilaginous component when chewing, especially if one inserts the fifth finger into the external acoustic meatus.
Middle Ear (Auris media)
The tympanic membrane marks the lateral margin of the middle ear, which is located inside the petrous part of the temporal bone. The middle ear is a contorted mucosal space connected to other cavities. Various nerve pathways run within the walls and the cavity of the middle ear, where the three auditory ossicles are attached. The “inner part” of the above-mentioned former branchial cleft is connected through the auditory (EUSTACHIAN) tube (Tuba auditiva) with the Pharynx.
The auditory tube is lined by a mucous membrane, descending inferiorly and anteriorly of the tympanic cavity. The Tuba auditiva is located in an osseous meatus in the petrous part of the temporal bone and is supported by elastic cartilage towards the pharynx, where its pharyngeal orifice is shaped like a trumpet bell. The Tuba auditiva serves to equalise the air pressure between the middle ear and the surroundings, which is particularly evident during flying and mountain climbing.
The actual tympanic cavity (Cavitas tympani) in the petrous part of the temporal bone contains the three auditory ossicles (Ossicula auditus), Malleus, Incus, and Stapes. These ossicles are connected by flexible joints and are mounted to the wall of the tympanic cavity by ligaments to form a V-shaped lever that transmits the vibrations of the tympanic membrane (to which the Malleus is attached) to the oval window (which holds the base of the Stapes, see below). In addition, two muscles (M. tensor tympani, M. stapedius) are attached to the Malleus and the Stapes. They regulate the “tension level” of the bony chain and, thus, the efficiency of sound transmission. The branches of the two cranial nerves, the N. facialis [VII] and the N. glossopharyngeus [IX], run within the mucosal layer of the walls of the tympanic cavity; the Chorda tympani, a branch of the N. facialis [VII], descends through the tympanic cavity. These nerve branches are not directly associated with hearing and balance – they supply other regions by passing through the tympanic cavity and petrous part of the temporal bone. A branch of the N. facialis [VII] innervates the M. stapedius (see above); the branches of the N. glossopharyngeus [IX] (Plexus tympanicus) supply the mucous membranes of the tympanic cavity.
The air-filled tympanic cavity extends in an interior and posterior direction into the multi-chambered, also air-filled Cellulae mastoideae in the mastoid process of the occipital bone (which is palpable just behind and below the auricle).
Inner Ear (Auris interna)
The inner ear is referred to as the labyrinth and is also located in the petrous part of the temporal bone, just superior (vestibular apparatus) and medial (cochlea) of the tympanic cavity. A membranous and bony labyrinth can be distinguished.
The membranous labyrinth is a closed tube system. It is filled with a liquid, the endolymph, and contains the sensory organs. Its complex structure consists of three semicircular canals (Canales semicirculares) which contain sensory modalities registering accelerated rotation. Sensory modalities (Sacculus and Utriculus) of linear acceleration and static position are located in the region of the vestibule (Vestibulum).
The bony labyrinth is a cavity in the petrous part of the temporal bone. It surrounds the membranous labyrinth and its shape is identical, but bigger in size. Thus, the resulting space between the two labyrinths is filled with a liquid called perilymph. This perilymphatic space opens via two membranous windows towards the middle ear: the Fenestra vestibuli (ovalis) and the Fenestra cochleae (rotunda). The Stapes is secured in the oval window and the vibrations of the stapedial foot cause the perilymph to oscillate.
The Cochlea records the vibrations of the lymph, which are conferred by the sound-conducting apparatus of the ear. The Cochlea is the actual auditory organ. The action potentials arising from the sensory modalities of the equilibrium and the auditory organ are conducted via the N. vestibulocochlearis [VIII] which enters the labyrinth from the posterior cranial fossa via the internal acoustic meatus (Meatus acusticus internus).
→Dissection Link
Auricle (pinna, Auricula), external acoustic meatus, and tympanic membrane are usually not dissected. The anterior and posterior semicircular canals are displayed by chipping open the bone with a chisel. Both semicircular canals are, in part, deeply embedded in the petrous bone. Usually, the horizontal semicircular canal is only demonstrated. The Meatus acusticus externus is exposed along the course of the Nn. facialis [VI] and vestibulocochlaris [VIII] up to the Ganglion geniculi, to the Cochlea and vestibular system, respectively. Next the branching of the N. petrosus major from the Ganglion geniculi is visualised. For illustration of the Cochlea, the anterior surface of the petrous bone, located medially to the internal acoustic meatus, is removed with a chisel approximately 1–2 mm parallel to the bone surface. The roof of tympanic cavity is now opened. The Malleus and Incus become visible. For visualisation of the Stapes, special preparations are required (and therefore this is usually only demonstrated). Starting at the Ganglion geniculi, the N. facialis [VII] is traced with care and attention must be paid to the Chorda tympani which runs in the opposite direction in between Malleus and Incus.
Overview
Development
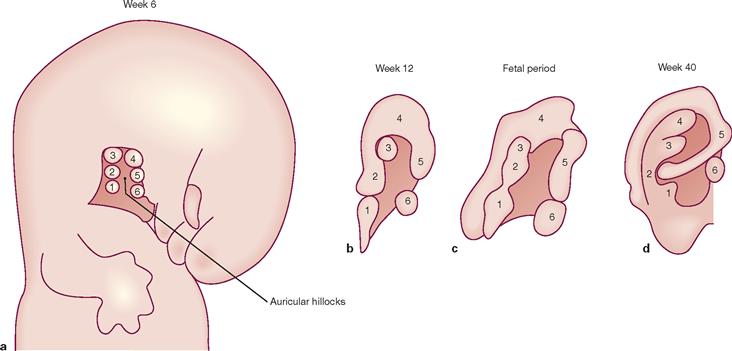
Figs. 10.1a to d Development of the auricle from the six auricular hillocks, right side. [21]
The merger of the auricular hillocks (1–6) is a complex process and, thus, developmental abnormalities are not infrequent. The primordial auricles start to develop at the base of the neck. As the mandible develops, the auricles move cranially to reach their normal position on both sides of the head at the level of the eyes. Ears positioned deeper in the head frequently are associated with (often chromosomal) developmental abnormalities. The external acoustic canal derives from the posterior part of the first pharyngeal groove which extends inwards as a cone-shaped tube to reach the entodermal epithelial lining of the tympanic cavity (Recessus tubotympanicus). At the beginning of week 9, epithelial cells located at the floor of the external acoustic meatus proliferate to generate a cellular plate, the meatal plug, which normally degenerates by 7 months of fetal development. A persistent plate in the external acoustic meatus is a cause of congenital deafness.
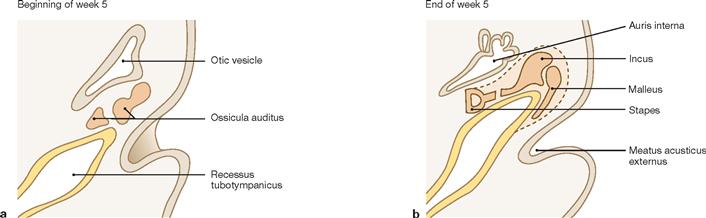
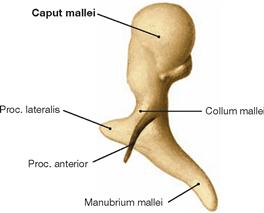
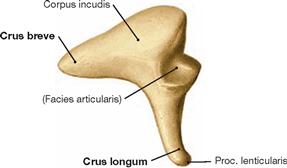
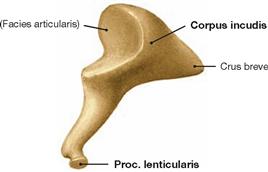
Figs. 10.2a and b Differentiation of the auditory ossicles, Ossicula auditus. [21]
At the beginning of week 5, mesenchymal tissue of the first and second branchial (pharyngeal) arches initiates the formation of auditory ossicles. The first branchial arch (also named manchibular arch) generates the Malleus and Incus as derivatives of MECKEL’s cartilage as well as the M. tensor tympani which is innervated by the first branchial nerve, the N. mandibularis [V/3]. The second branchial arch generates the Stapes, a derivative of REICHERT‘s cartilage. The Stapes can be moved by the M. stapedius which is innervated by the second branchial nerves nerve, the N. facialis [VII].
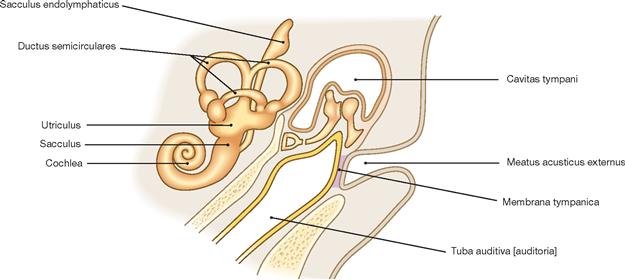
Fig. 10.3 Structures of the inner, middle, and outer ear at the time of birth. [21]
Up to 8 months of pregnancy, the initially cartilaginous auditory ossicles are embedded in mesenchyme. Gradually, this mesenchyme is replaced by an entoderm-derived mucosal lining which covers the complete tympanic cavity.
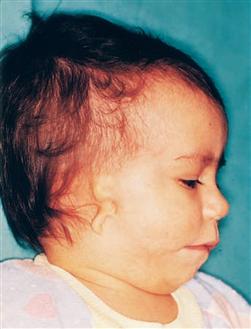
Fig. 10.5 Child with a small rudimentary auricle (microtia). [20]
Second degree auricular dysplasia. The auricle is small and severely disfigured. This often includes the external acoustic meatus.
Outer ear
Ear, overview
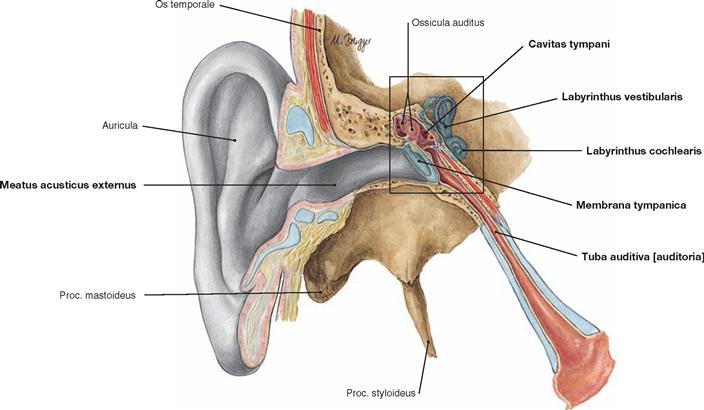
Fig. 10.6 Parts of the ear, Auris, right side; longitudinal section through the acoustic meatus, middle ear, and auditory tube; frontal view.
Presentation of the auricle (Auricula), external acoustic meatus (Meatus acusticus externus), tympanic membrane (Membrana tympanica, ear drum), tympanic cavity (Cavitas tympani), auditory ossicles (Ossicula auditus), cochlear labyrinth (Labyrinthus cochlearis), and vestibular labyrinth (Labyrinthus vestibularis).
Sound waves initiate oscillation of the tympanic membrane (aerotympanal conduction). The auditory ossicles transmit the vibrations to the oval window of the inner ear (→ Fig. 10.27) and match the low air impedance (→ Fig. 10.17) with the high fluid impedance of the liquid-filled inner ear (impedance matching). In addition, the inner ear can also sense vibrations of skull bones (bone conduction). Within the inner ear, the sound energy propels as a wave (migrating wave). Sensory cells of the inner ear convert the sound energy into electric impulses which are transmitted via the N. cochlearis to specific regions of the brain. The vestibular organ serves the perception of rotational and linear accelerations. Motion of the endolymph contained within the vestibular organ results in the deflection of cilia on the surface of sensory cells which are in contact with afferent fibres of the N. vestibularis.
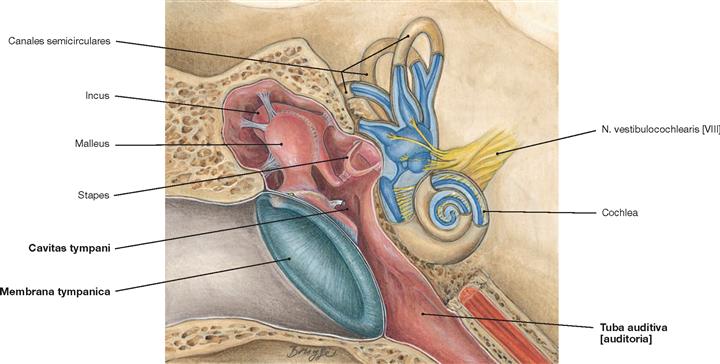
Fig. 10.7 Middle and inner ear, Auris media and interna, right side; enlarged section of Figure → 10.6; frontal view.
Depicted are the tympanic membrane, the three auditory ossicles in the tympanic cavity (Cavitas tympani): hammer-shaped Malleus, anvil-shaped Incus, and stirrup-like Stapes as well as parts of the membranous labyrinth (Labyrinthus membranaceus, blue).
Auricle
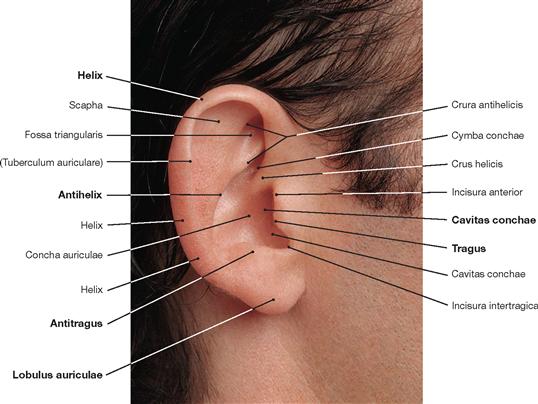
Fig. 10.8 Auricle, Auricula, right side; lateral view.
The basic framework of the auricle consists of elastic cartilage. The skin on the lateral surface of the auricle is fixed to the perichondrium and cannot be moved; on the rear side of the auricle, the skin is movable. Subcutaneous fat tissue is lacking. The earlobe (Lobulus auriculae) is free of cartilage.
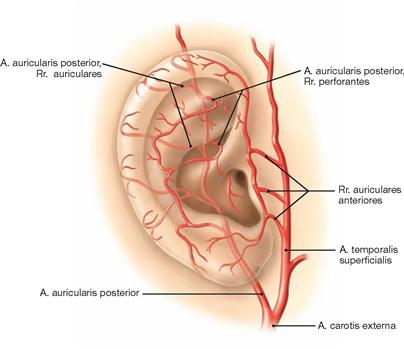
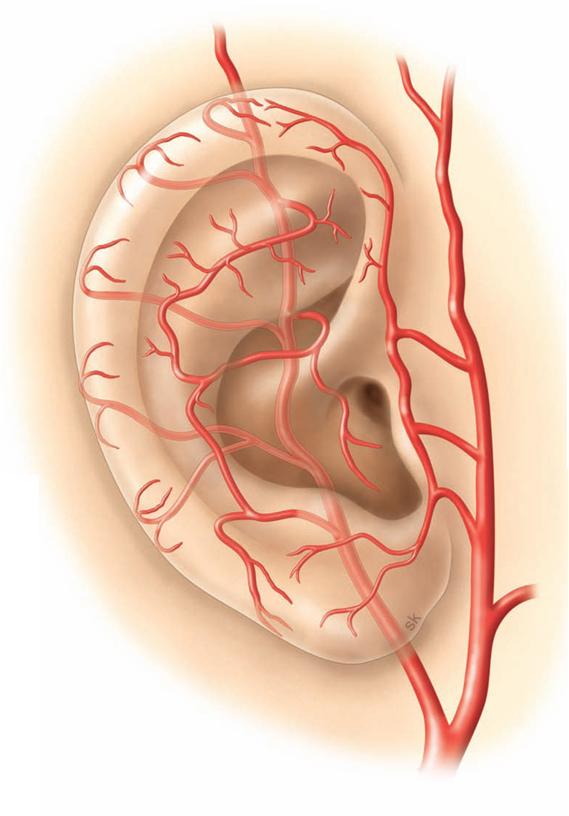
Fig. 10.9 Arteries of the auricle, Auricula, right side; lateral view. [8]
Due to its exposed location, the auricle is highly vascularized (protection against freezing, suitable for heat convection). The supplying ar-teries are branches of the A. carotis externa (A. auricularis posterior, A. temporalis superficialis).
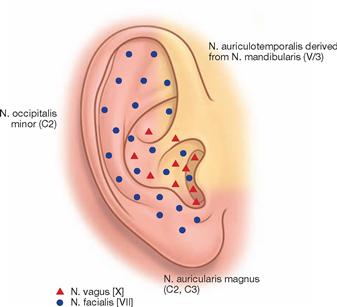
Fig. 10.10 Sensory innervation of the auricle, Auricula, right side; lateral view. [8]
The sensory innervation of the auricle is supplied by the N. auriculotemporalis (from the N. mandibularis [V/3]) in front of the ear, the Plexus cervicalis (N. auricularis magnus, N. occipitalis minor) for the region behind and below the ear, the N. facialis [VII] for the auricle itself (what part of the N. facialis [VII] exactly is involved is not entirely clear), and the N. vagus [X] for the entrance (aditus) to the external acoustic meatus.
Auricle and external acoustic meatus
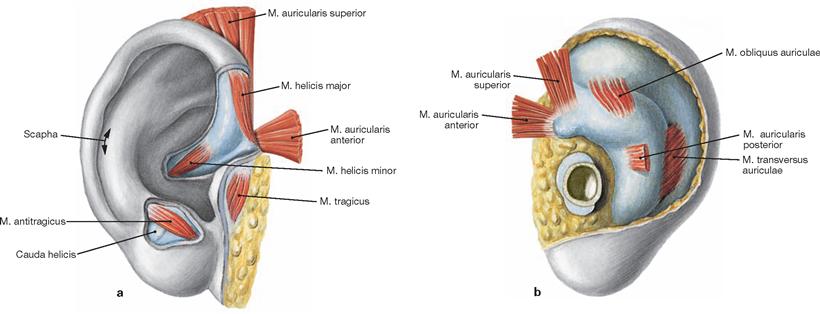
Figs. 10.11a and b Muscles, Mm. auriculares, and cartilage of the auricle, Auricula, right side.
Rudimentary muscles can sometimes be found attached to the auricle (some people manage to wag their ears). These are facial muscles (innervation by the N. auricularis posterior of the N. facialis [VII]) which are part of a rudimentary sphincter system still found in many animals. Horses, for example, move the auricle such that the external acoustic meatus faces the sound waves. During hibernation, hedgehogs and bears use this sphincter function to occlude the external acoustic meatus and block out unwanted noise.![]()
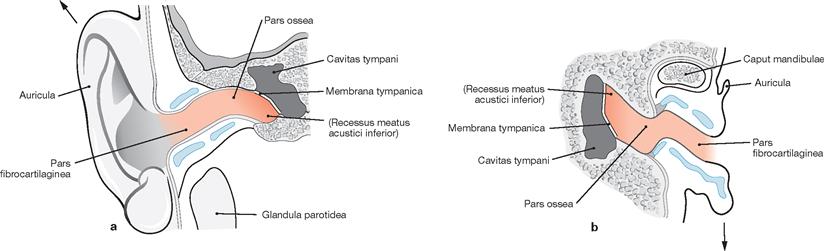
Figs. 10.12a and b External acoustic meatus, Meatus acusticus externus, right side; schematic drawing.
The external acoustic meatus is S-shaped and is formed by the Pars tympanica of the Os temporale. The auricle has to be pulled up and backwards in order to inspect the tympanic membrane with a reflecting otoscopic mirror or a microscope (otoscopy). This will straighten the cartilaginous part of the external acoustic meatus and allow the (at least partial) view at the tympanic membrane. Innervation of the external acoustic meatus (not shown) is through the N. meatus acustici externi of the N. auriculotemporalis (anterior and superior wall), the R. auricularis of the N. vagus [X] (posterior and partially inferior wall), and via the Rr. auriculares of the N. facialis [VII] and the N. glossopharyngeus [IX] (posterior wall and tympanic membrane).
Arrows: direction of pull on the auricle by the examiner to straighten the external acoustic meatus and allow a view at the tympanic membrane.
Tympanic membrane
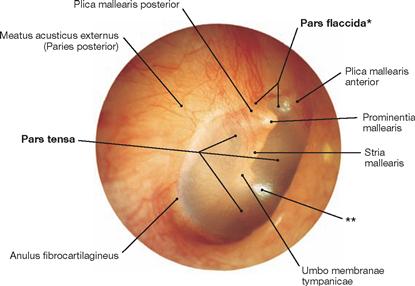
Fig. 10.13 Tympanic membrane, Membrana tympanica, right side; lateral view; otoscopic image.
In its anterior, inferior, and posterior aspects, the Meatus acusticus externus is demarcated by the Pars tympanica of the Os temporale. In its superior aspect, the bony ring is interrupted by the Incisura tympanica (attachment point for the Pars flaccida of the tympanic membrane). With the exception of the Incisura tympanica, the otherwise circular Sulcus tympanicus is located within the Pars tympanica (the Pars tensa of the tympanic membrane is attached here through the fibrous cartilaginous Anulus fibrocartilagineus).
* clinical term: SHRAPNELL’s membrane
** typically positioned light reflex
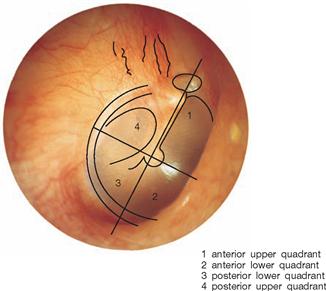
Fig. 10.14 Tympanic membrane, Membrana tympanica, right side, quadrant scheme. Lateral view.
Illumination of the pearl-coloured tympanic membrane usually results in a triangular light reflex in the anterior lower quadrant, which allows conclusions on the tension of the tympanic membrane.
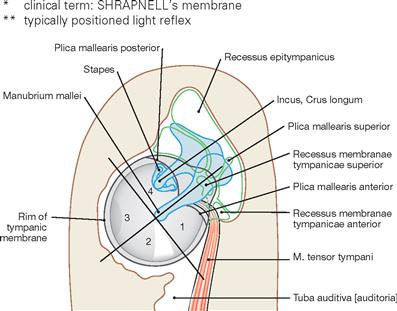
Fig. 10.15 Tympanic membrane, Membrana tympanica, and recessus of the tympanic cavity, Cavitas tympani, right side, quadrant scheme; lateral view; schematic drawing.
The quadrant scheme is of practical clinical relevance. The auditory ossicles are located in the upper quadrants. In addition, the Chorda tympani and the attaching tendon of the M. tensor tympani are localized here (→ Fig. 12.148).
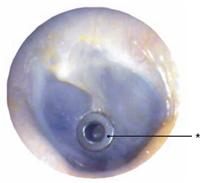
Fig. 10.16 Tympanostomy tube (grommet) in the anterior lower quadrant.
To avoid injury of structures of the middle ear, a paracentesis (myringotomy; small surgical incision of the tympanic membrane) is performed in the anterior or posterior lower quadrant, respectively. Longer-term ventilation of the tympanic cavity is ensured by inserting a grommet into the incision.
* grommet
Middle ear
Auditory ossicles
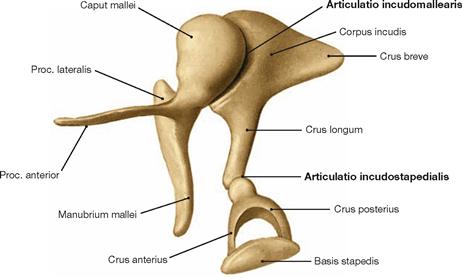
Fig. 10.17 Auditory ossicles, Ossicula auditus, right side; superomedial view.
The auditory bones of the anditory ossicular chain are connected in series. They are linked by true joints (Articulatio incudomallearis – a saddle joint – and Art. incudostapedialis – a spheroidal joint). The chain of auditory ossicles transmits the energy of the sound waves from the tympanic membrane to the perilymph of the inner ear. This involves the transformation from lower air impedance to the much higher fluid impedance of the inner ear lymph. This requires the amplification of the sound waves (impedance matching), which is accomplished by the size difference between the tympanic membrane (55 mm2) and the oval window (3.2 mm2; 17-times) and the lever action of the auditory ossicles (1.3-times). Thus, the acoustic pressure amplifies by 22-fold.
Tympanic cavity
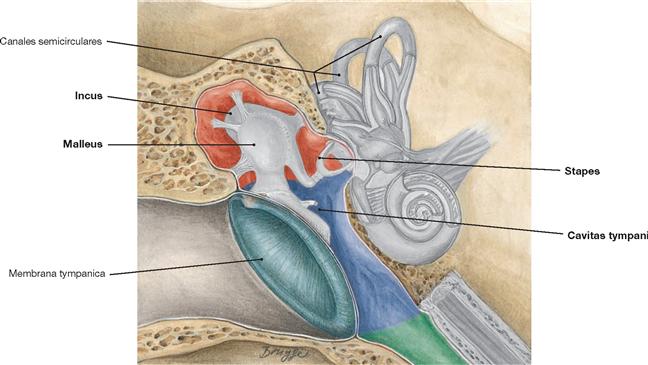
Fig. 10.23 Different levels of the tympanic cavity, Cavitas tympani, right side; frontal view.
From a clinical standpoint, the tympanic cavity divides into three sections named according to their topographic relationship to the tympanic membrane:
• The epitympanum (red; Recessus epitympanicus, epitympanic recess, attic), contains the suspension apparatus and the majority of the ossicles and, through the Antrum mastoideum, connects with the mastoid cells.
• The mesotympanum (blue) contains the Manubrium mallei, the Proc. lenticularis of the incus, and the tendon of the M. tensor tympani.
• The hypotympanum (green; Recessus hypotympanicus) leads into the Tuba auditiva [auditoria].
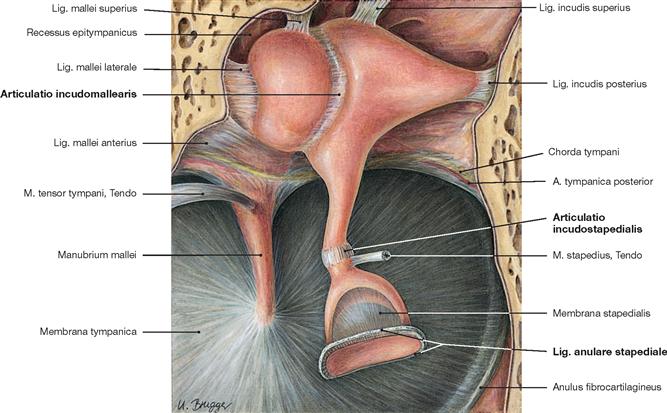
Fig. 10.24 Joints and ligaments of the auditory ossicles, Articulationes and Ligg. ossiculorum auditus, right side; superomedial view.
Ligaments fasten the Malleus and Incus in the epitympanum. The Art. incudomallearis (saddle joint) connects both auditory ossicles. The Art. incudostapedialis (spheroidal joint) connects the Stapes with the Incus. The base of the Stapes (Basis stapedis) is secured to the oval window by the Lig. anulare stapediale (syndesmosis). All structures in the tympanic cavity, including the Chorda tympani, are lined with mucosa of the middle ear.
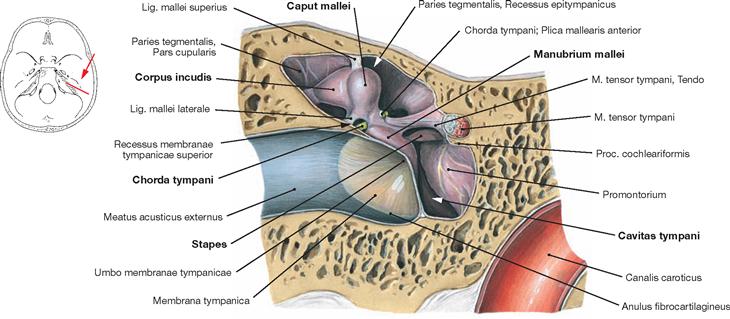
Fig. 10.25 Tympanic cavity, Cavitas tympani, right side; frontal section; frontal view.
The tympanic cavity is an air-filled hollow space within the middle ear and contains the auditory ossicles. The tympanic cavity is located directly behind the tympanic membrane and is aerated and drained by the Tuba auditiva [auditoria] (EUSTACHIAN tube) which also serves in pressure equalization. The spatial distance between the epitympanum and hypotympanum is 12–15 mm and the depth is 3–7 mm, with an inner volume of approximately 1 cm3.
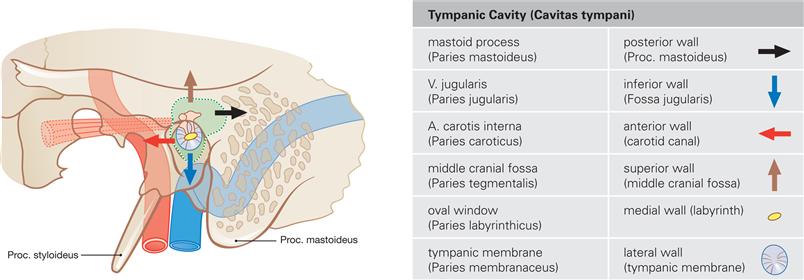
Fig. 10.26 Topographical relationships between the tympanic cavity, Cavitas tympani, and adjacent structures, right side; lateral view; schematic drawing.
A thin bony plate (Tegmen tympani, Paries tegmentalis) separates the epitympanum cranially from the middle cranial fossa. The anterior wall of the mesotympanum (Paries caroticus) is in close proximity to the A. carotis interna. The tympanic membrane makes up the entire lateral wall (Paries membranaceus). The Tuba auditiva [auditoria] enters the tympanic cavity in the inferior wall section. The posterior wall (Paries mastoideus) borders the mastoid process (Proc. mastoideus). In its posterior upper section, a direct connection exists to the pneumatic spaces of the mastoid (Aditus ad antrum). The medial wall (Paries labyrinthicus; → Figs. 10.27 and 10.28) separates the Cochlea from the tympanic cavity. The inferior wall of the tympanic cavity (Paries jungularis) belongs to the hypotympanum and separates the tympanic cavity from the V. jugularis interna. Here, the bone is very thin and partially air-filled.
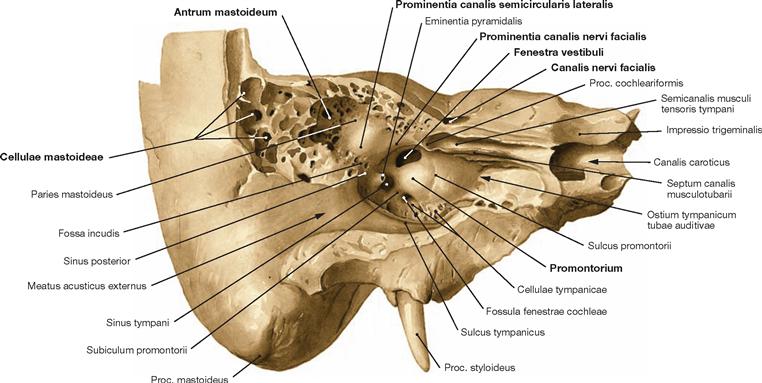
Fig. 10.27 Medial wall, Paries labyrinthicus, of the tympanic cavity, Cavitas tympani, right side; vertical section in the longitudinal axis of the petrous part of the temporal bone; frontolateral view.
Above the oval window, the lateral semicircular canal bulges out the wall of the tympanic cavity to form the Prominentia canalis semicircularis lateralis. The N. facialis [VII] passes through the Canalis nervi facialis which is located within the medial wall. This canal creates the horizontal Prominentia canalis nervi facialis in the medial wall. The Tuba auditiva [auditoria] initiates at the Ostium tympanicum tubae auditivae. Located along the superior aspect of the Tuba auditiva [auditoria], the Septum canalis musculotubarii separates the auditory tube from the Semicanalis musculi tensoris tympani. Typically pneumatised (Cellulae mastoideae), the mastoid process (Proc. mastoideus) connects with the tympanic cavity through the Antrum mastoideum.
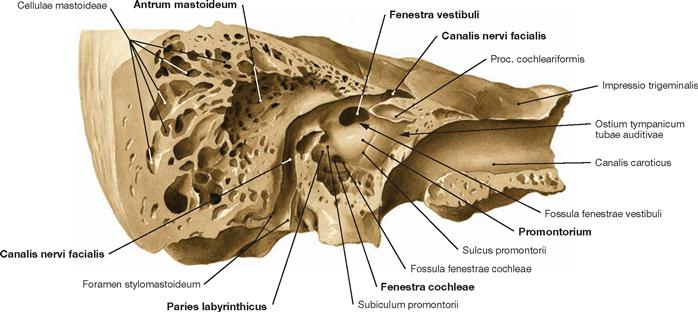
Fig. 10.28 Medial wall, Paries labyrinthicus, of the tympanic cavity, Cavitas tympani, right side; anterolateral view; after removal of the lateral wall and the adjacent parts of the anterior and superior walls; facial canal and carotid canal opened.
The medial walls separates the tympanic cavity from the inner ear (labyrinth) and has two openings:
• the oval window (Fenestra vestibuli) with the base of the Stapes affixed to it by the Lig. anulare stapediale
• located more inferiorly, the round window (Fenestra cochleae) occluded by the Membrana tympanica secundaria.
In the space between oval and round window, the basal cochlear turn creates a prominent bulge in the medial wall of the tympanic cavity, named the Promontorium.
Tympanic cavity, topography
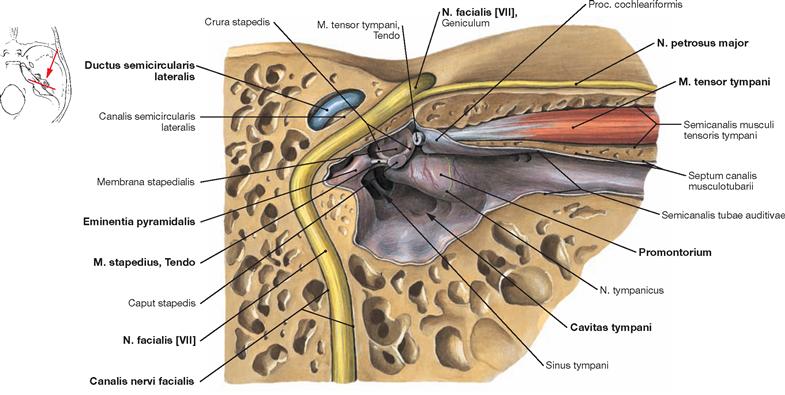
Fig. 10.29 N. facialis [VII], tympanic cavity, Cavitas tympani, and auditory tube, Tuba auditiva [auditoria], right side; vertical section in the longitudinal axis of the petrous part of the temporal bone; frontal view; facial canal opened.
The N. facialis [VII] is composed of two branches, the actual N. facialis and the N. intermedius. Both branches combine deep in the facial canal (Canalis nervi facialis) to form the N. intermediofacialis (henceforth referred to as N. facialis [VII]). It arches around the tympanic cavity and generates the Prominentia nervi facialis in the medial wall of the tympanic cavity. Beneath thereof, the Eminentia pyramidalis protrudes into the cavity. It houses the M. stapedius innervated by the N. facialis (→ Fig. 12.152). The tendon of the M. stapedius exits the Eminentia pyramidalis and inserts at the inferior lateral aspect of the stapedial head.
Function of the M. stapedius: It attenuates vibrations at the oval window by slightly tilting the stapes, thus, decreasing the transmission of sound waves and protecting the sensory cells of the inner ear from excessive noise.
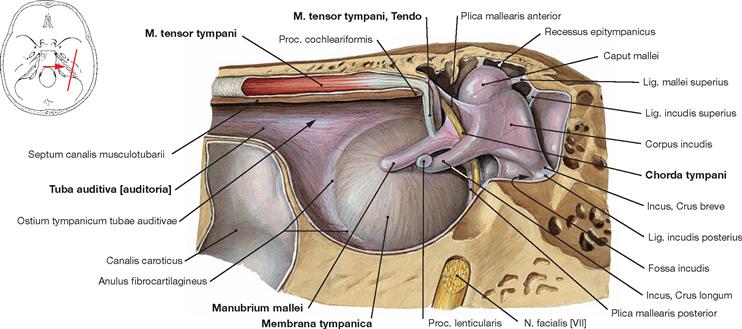
Fig. 10.30 Lateral wall, Paries membranaceus, of the tympanic cavity, Cavitas tympani, right side; medial view.
The Canalis musculotubarius enters the tympanic cavity from the front. It is composed of two bony semicanals (Semicanales), separated by a bony septum, and contains the M. tensor tympani and the Tuba auditiva [auditoria]. At the Proc. cochleariformis, the tendon of the M. tensor tympani makes a right angle turn and inserts at the Manubrium mallei.
Function of the M. tensor tympani: It increases the tension of the tympanic membrane by pulling at the Manubrium mallei. This results in the chain of auditory ossicles to become more rigid and this improves their ability to transmit high-frequency sound waves. Shortly before the end of the Canalis nervi facialis, the Chorda tympani leaves the N. facialis [VII], runs backwards through its own bony canal into the tympanic cavity and, embedded in mucosa, courses through the centre of the tympanic cavity between Malleus and Crus longum of the Incus. The Chorda tympani exits the cranial base through the Fissura sphenopetrosa (or Fissura petrotympanica).
N. facialis [VII], topography
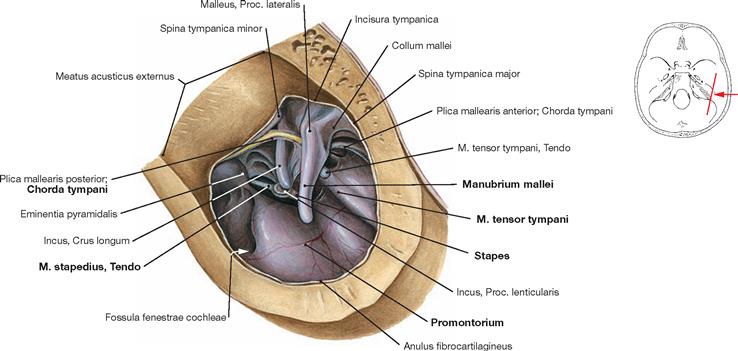
Fig. 10.31 Tympanic cavity, Cavitas tympani, right side; lateral view after removal of the tympanic membrane and the mucosal layer around the Chorda tympani.
The structures of the tympanic cavity covered by mucosa are shown.
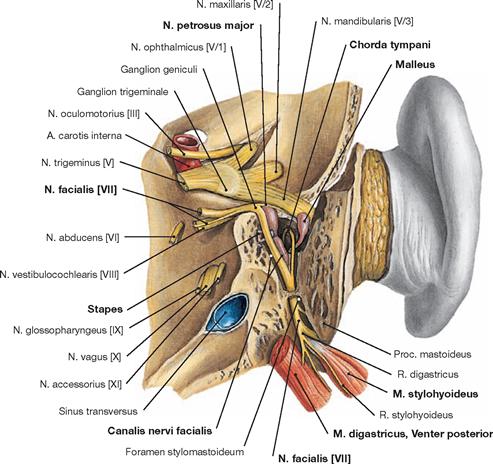
Fig. 10.32 N. facialis [VII] in the petrous part of the temporal bone, Os temporale, Pars petrosa, right side; posterior view; petrous bone partially removed; facial canal and tympanic cavity opened.
After removal of the Proc. mastoideus and opening of the facial canal and the tympanic cavity, the entire course of the N. facialis [VII] and its branches in the bony canal become visible (→ Fig. 12.148).
Auditory tube
N. facialis [VII], topography
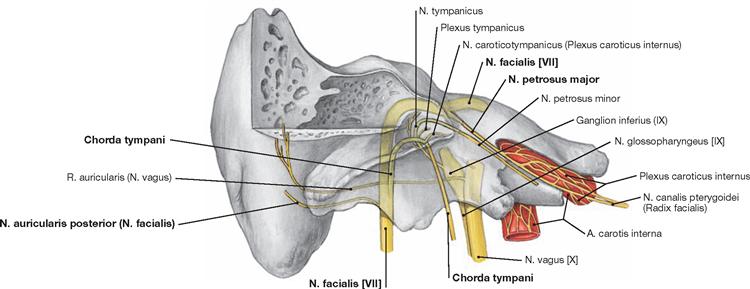
Fig. 10.33 N. facialis [VII], N. glossopharyngeus [IX], and N. vagus [X], right side; frontal view; petrous bone partially removed; nerves are shown transparently.
The N. petrosus major is the first branch to leave the N. facialis [VII] at the Ganglion geniculi. The N. petrosus major projects frontomedially and exits the Os temporale at the Hiatus nervi petrosi majoris below the Dura mater on the Facies anterior of the Pars petrosa ossis temporalis. This nerve provides preganglionic parasympathetic fibres to the Ganglion pterygopalatinum for the innervation of lacrimal and nasal glands. Shortly after passing through the Foramen stylomastoideum, the N. facialis [VII] releases the N. auricularis posterior for the innervation of the auricle. Shown are also the R. auricularis of the N. vagus [X] for the sensory innervation of the external acoustic meatus and the N. tympanicus which branches off the N. glossopharyngeus shortly before this cranial nerve passes through the Foramen jugulare. Together with branches derived from a sympathetic network (Plexus caroticus internus, Nn. caroticotympanici) surrounding the A. carotis interna, the N. tympanicus participates in the formation of a neuronal plexus in the mucosal layer of the Promontorium. This Plexus tympanicus innervates the entire mucosa of the middle ear as well as the mucosal layer of the Tuba auditiva [auditoria] and the mastoid process.
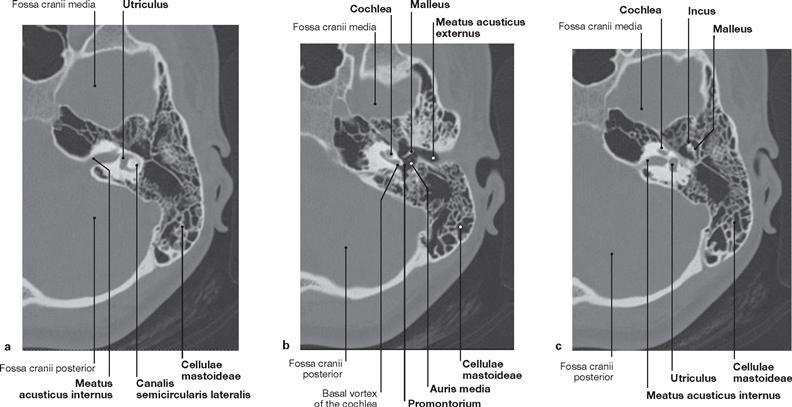
Figs. 10.34a to c Temporal bone, Os temporale, with middle and inner ear, left ear; computed tomographic section (CT), inferior view. [10]
High-resolution CT is able to visualize in detail all structures of the middle and inner ear. For example, this imaging technique allows for the evaluation of the internal acoustic [auditory] meatus, the pneumatisation of the mastoid process, the positioning of the auditory ossicles, and the labyrinth.
Auditory tube
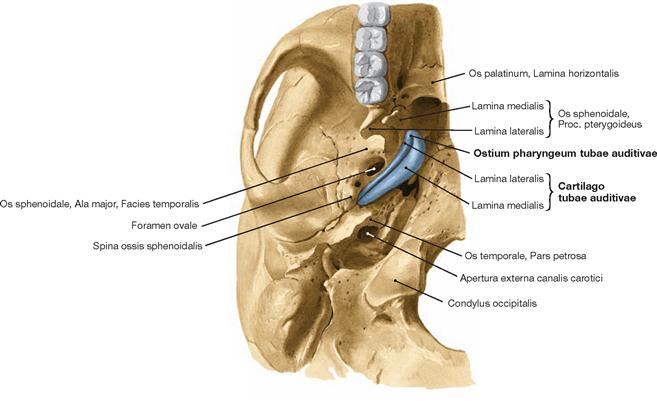
Fig. 10.35 Cartilage of the auditory tube, Cartilago tubae auditivae, right side; inferior view; exposed at the base of the skull.
Projecting in an oblique angle from a cranial posterolateral to a frontomedial caudal position, the approximately 4 cm long auditory tube (Tuba auditiva [auditoria], EUSTACHIAN tube) connects the tympanic cavity with the nasopharynx (nasal part of the pharynx). It serves in pressure equalisation. The requirement for optimal transmission of sound waves is equal air pressure in both the tympanic cavity (the tympanic membrane is impermeable to air) and the external acoustic meatus compartment. If this is not the case, e.g. during the ascent or descent flight of a plane, impaired hearing results.
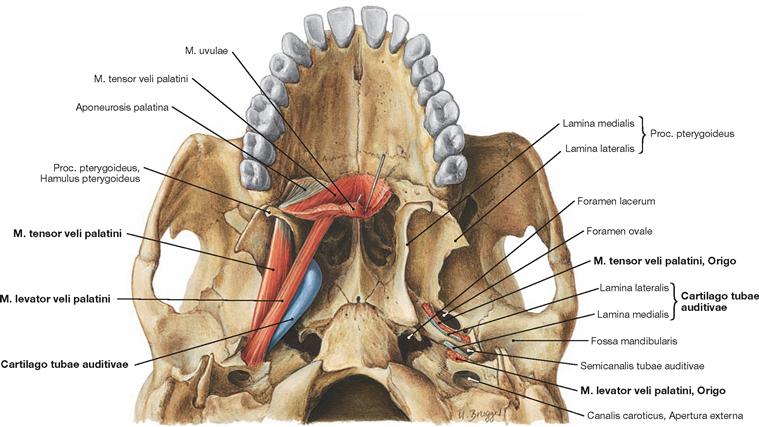
Fig. 10.36 M. levator veli palatini, M. tensor veli palatini, and cartilage of the auditory tube, Cartilago tubae auditivae; inferior view.
The Tuba auditiva [auditoria] (bony part not shown) initiates at the Ostium tympanicum tubae auditivae of the anterior wall of the tympanic cavity (Paries caroticus) and ends at the Ostium pharyngeum tubae auditivae which protrudes in the posterior lateral aspect of the nasopharynx. One can distinguish a bony part (Pars ossea) and a cartilaginous part (Pars cartilaginea) twice the length of the bony part. The latter consists of a trough-shaped elastic cartilage (Cartilago tubae auditivae) in an upside-down position with connective tissue (Lamina membranacea) on its medial side, thus creating a slit-like canal. Contractions of the Mm. tensor und levator veli palatini during swallowing result in the opening of the Tuba auditiva [auditoria].![]()
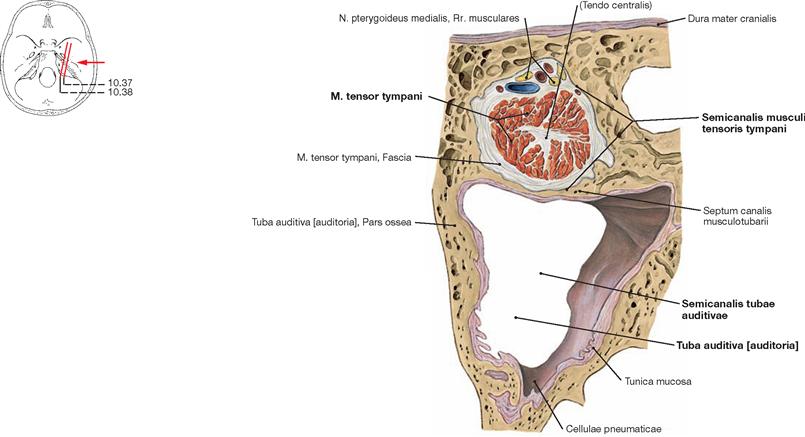
Fig. 10.37 Auditory tube, Tuba auditiva [auditoria], right side; cross-section through the Canalis musculotubarius at the level of the Pars ossea; lateral view.
The osseous part of the Tuba auditiva [auditoria] is located in a triangular bony canal (Semicanalis tubae auditivae of the Canalis musculotubarius) of the Pars petrosa ossis temporalis. Separated by a thin bony layer lies the M. tensor tympani in the Semicanalis musculi tensoris tympani of the Canalis musculotubarius.
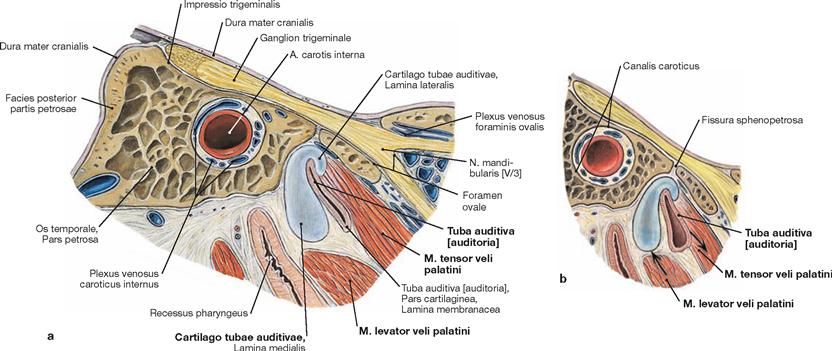
Figs. 10.38a and b Auditory tube, Tuba auditiva [auditoria], right side; cross-section at the level of the lateral part of the Pars cartilaginea; lateral view.
Swallowing involves the contraction of the Mm. tensor and levator veli palatini. Contraction of the M. tensor veli palatini causes a pull at the Pars membranacea and the upper rim of the cartilaginous part of the auditory tube resulting in a dilation of the tube lumen. Contraction of the M. levator veli palatini causes the muscle to bulge out and this muscle belly pushes against the cartilaginous part of the tube from below. As a result, the slit-shaped lumen bends such that it causes the lumen of the auditory tube to dilate. Occlusion of the auditory tube involves the M. salpingopharyngeus (not shown).
Inner ear
Bony labyrinth
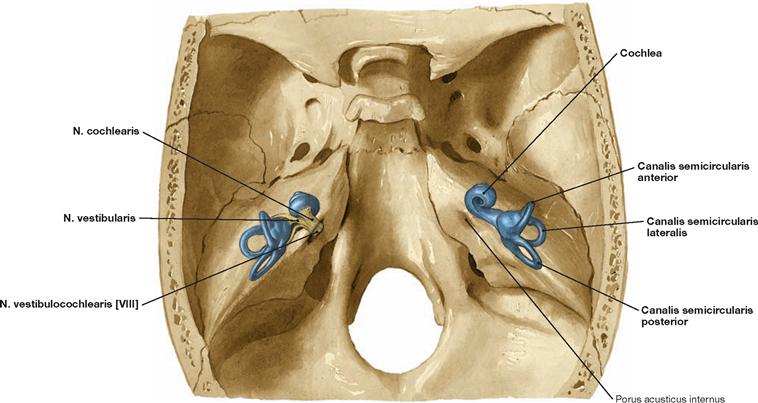
Fig. 10.39 Inner ear, Auris interna, and N. vestibulocochlearis [VIII]; superior view; inner ear projected onto the petrous part of the temporal bone illustrating its natural position.
The tip of the Cochlea is pointed anterolateral. The semicircular canals (Canales semicirculares) position in a 45o angle in relation to the main planes of the skull (frontal, sagittal, and horizontal planes). This is important information to know when examining CT scans of the skull.
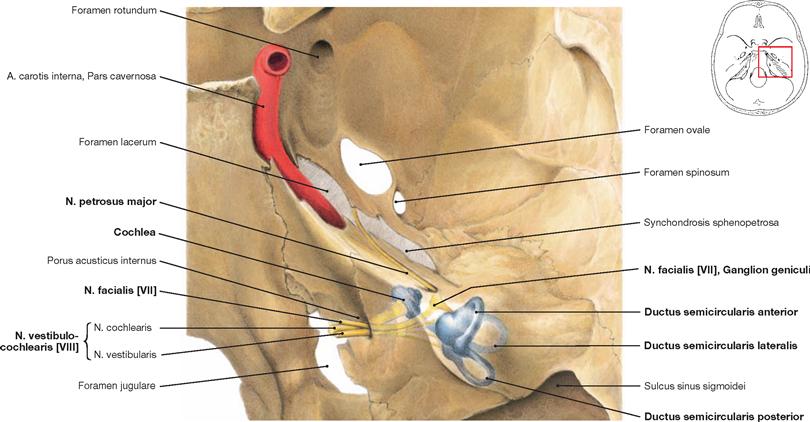
Fig. 10.40 Inner ear, Auris interna, with N. facialis [VII] and N. vestibulocochlearis [VIII], right side; superior view onto the petrous part of the temporal bone.
When entering the Porus acusticus internus, the N. facialis [VII] and its intermedius part position on top of the N. vestibulocochlearis [VIII] (in clinical terms often referred to as N. statoacusticus), which is composed of the Nn. cochlearis and vestibularis. The nerves distribute within the petrous bone. The N. cochlearis arches forward to the cochlea. The N. vestibularis arches backward and, just before reaching the labyrinth, divides into a Pars superior for the anterior and lateral semicircular canals and the saccule as well as into a Pars inferior for the utricle and the posterior semicircular canal. The perikarya of the neurons of both parts are jointly located in the Ganglion vestibulare. The N. facialis [VII] runs above and in between the cochlea and vestibular organ in the facial canal. At the outer facial knee, the facial nerve bends downward in an almost 90o angle. The N. petrosus major branches off the N. facialis [VII] at the Ganglion geniculi. The nerve runs in a duplication of the dura on top of the petrous bone towards the Foramen lacerum and contains preganglionic parasympathetic fibres for the innervation of lacrimal and nasal glands.
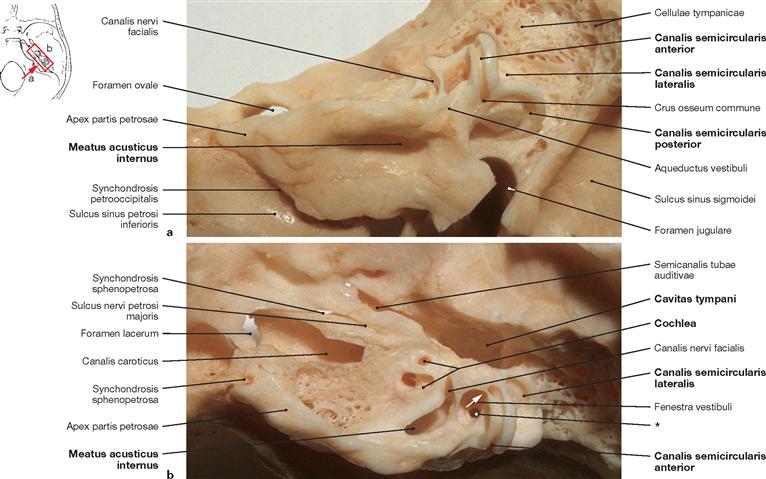
Figs. 10.41a and b Bony labyrinth, Labyrinthus osseus, right side; hollowed out of the petrous part of the temporal bone; posterior and superior view (a), superior view (b).
The inner ear (Auris interna) is a complex of bony canals and ampullary extensions in the Pars petrosa of the Os temporale (bony labyrinth). Contained within it is a system of membranous tubes and sacs, known as membranous labyrinth. It harbours the vestibular and cochlear organ (Organum vestibulocochleare).
* opening of the Canaliculus posterior
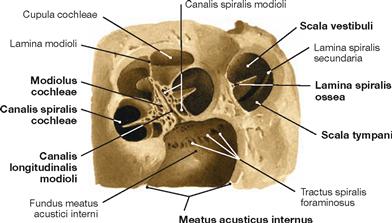
Fig. 10.42 Spiral canal of the cochlea, Canalis spiralis cochleae, right side; superior view; opened along the axis of the modiolus.
The Cochlea consists of a spiral canal (Canalis spiralis cochleae) of 2½ turns around a central modiolus (Modiolus cochleae). The Ganglion spirale cochleae, containing the perikarya of the bipolar neurons of the N. cochlearis, is located within the Canales spiralis and longitudinalis modioli. Originating from the modiolus, the Lamina spiralis ossea protrudes into the cochlear canal.
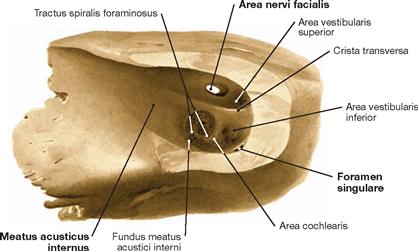
Fig. 10.43 Internal acoustic meatus, Meatus acusticus internus, and fundus of the internal acoustic meatus, Fundus meatus acustici interni, right side; medial view; after partial removal of the posterior wall.
The internal acoustic meatus initiates at the Porus acusticus internus and projects laterally for approximately 1 cm. Here it ends in a perforated bony plate. The N. facialis [VII] and N. vestibulocochlearis [VIII] run in this 1 cm long segment.
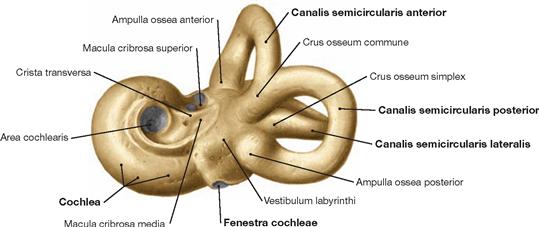
Fig. 10.44 Bony labyrinth, Labyrinthus osseus, right side; view from an oblique posterior angle; the osseous lining of the membranous labyrinth has been hollowed out of the petrous part of the temporal bone.
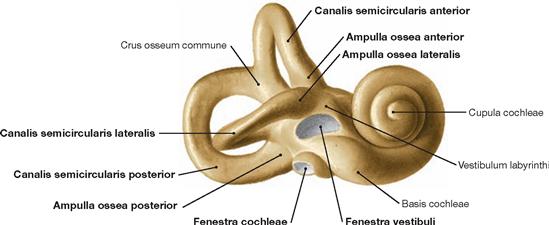
Fig. 10.45 Bony labyrinth, Labyrinthus osseus, right side; lateral view; the osseous lining of the membranous labyrinth has been hollowed out of the petrous part of the temporal bone.
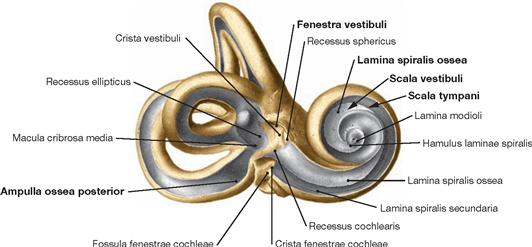
Fig. 10.46 Bony labyrinth, Labyrinthus osseus, right side; anterolateral view; cavities have been hollowed out.
The bony labyrinth consists of the Vestibulum, three bony semicircular canals (Canales semicirculares ossei), the bony cochlea (Cochlea), and the internal acoustic meatus (Meatus acusticus internus). Cochlea and semicircular canals originate from the Vestibulum which connects with the tympanic cavity through the oval window.
Membranous labyrinth
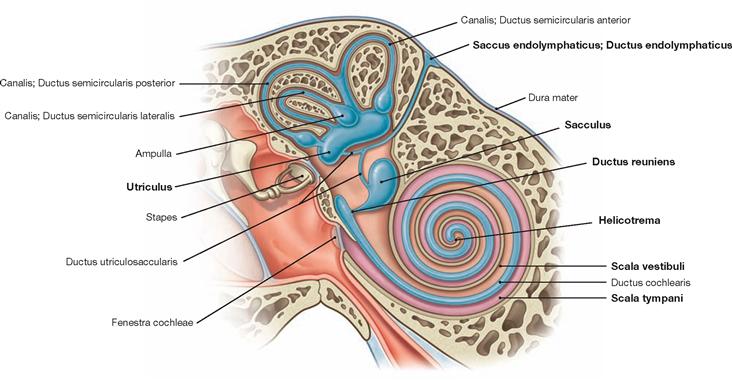
Fig. 10.47 Membranous labyrinth, Labyrinthus membranaceus, right side; longitudinal section through the petrous part of the temporal bone; frontal view, schematic drawing. [8]
The membranous labyrinth contains potassium rich and sodium poor endolymph. A perilymphatic space filled with perilymph separates the membranous labyrinth from the bony labyrinth. According to its function, the membranous labyrinth divides into a vestibular and cochlear compartment. The vestibular labyrinth includes the Sacculus and Utriculus located in the vestibulum, the Ductus utriculosaccularis, the three semicircular canals, and the Ductus endolymphaticus with the Saccus endolymphaticus. The latter is located on the rear side of the petrous bone and represents an epidural sac for the resorption of the endolymph. The cochlear labyrinth forms the Ductus cochlearis. The Ductus reuniens connects the vestibular and cochlear labyrinths.
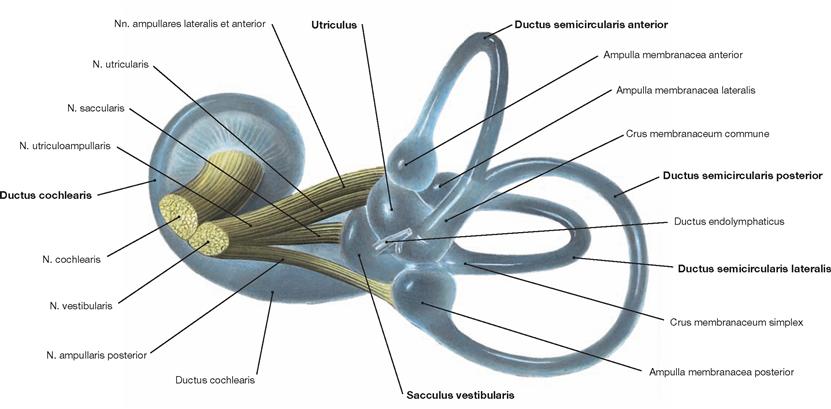
Fig. 10.48 N. vestibulocochlearis [VIII] and membranous labyrinth, Labyrinthus membranaceus; semi-schematic overview, dorsal view.
The membranous labyrinth includes the Ductus cochlearis, the Sacculus, the Utriculus as well as the three membranous semicircular canals (Ductus semicirculares). The latter ones connect with the Utriculus. At the border to the Utriculus, each Ductus semicircularis develops an ampulla-shaped dilation (Ampulla membranacea). At one end, the superior and posterior semicircular canal unite to form one common canal (Crus commune). Each ampulla contains sensory epithelium (Crista ampullaris, not shown).
Blood supply and innervation of the membranous labyrinth
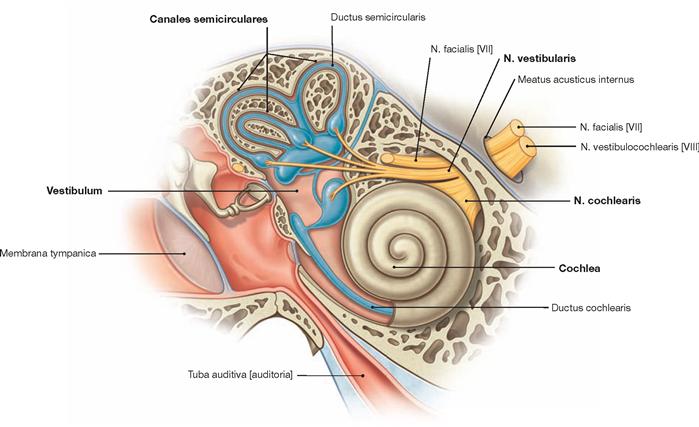
Fig. 10.49 Innervation of the inner ear, Auris interna, right side; longitudinal section through the petrous part of the temporal bone; frontal view, schematic drawing. [8]
The inner ear is composed of the compact bone of the petrous bone surrounding the bony labyrinth (Labyrinthus osseus) and, enclosed within it, the membranous labyrinth (Labyrinthus membranaceus), which resembles a system of membranous tubes.
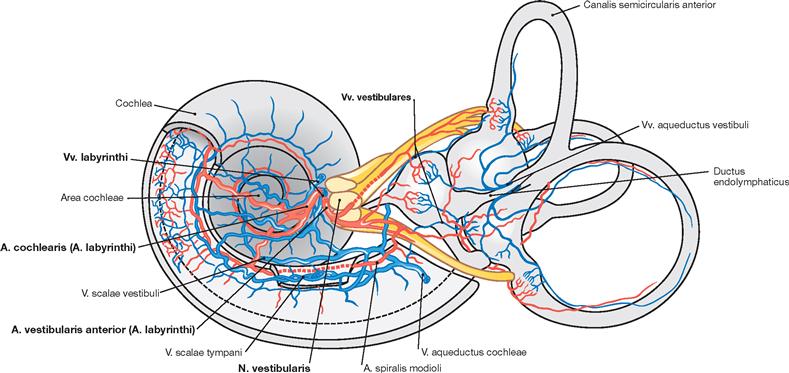
Fig. 10.50 Blood supply and innervation of the inner ear, Auris interna, of the right side; medial view. (according to [2])
The branches of the A. labyrinthi (→ Fig. 12.96) provide the complete blood supply to the inner ear; the Vv. labyrinthi drain the venous blood. A. and V. inferior anterior cerebelli project into the internal acoustic meatus for a few millimeters (not shown) before the A. and Vv. labyrinthi branch off to provide blood supply to the labyrinth (caveat: the A. labyrinthi is a terminal artery).
Cochlea
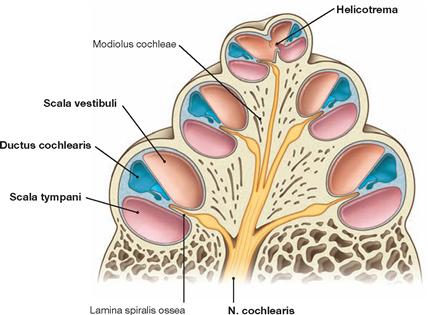
Fig. 10.51 Spiral canal of the cochlea, Cochlea; cross-section; schematic drawing. [8]
The REISSNER’s membrane and the basilar membrane divide the Canalis spiralis cochleae into three spaces:
• The Scala vestibuli stretches from the Vestibulum to the Helicotrema and is filled with perilymph.
• The Ductus cochlearis is filled with endolymph.
• The Scala tympani extends from the Helicotrema to the round window in the medial wall of the tympanic cavity and is filled with perilymph. Scala vestibuli and Scala tympani join at the helicotrema.
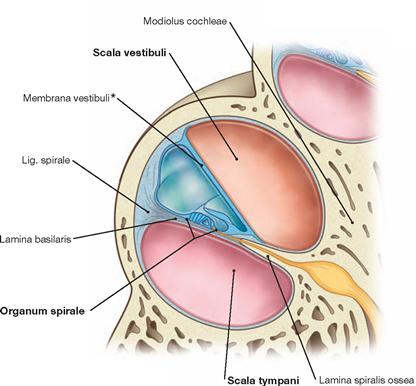
Fig. 10.52 Spiral canal of the cochlea, Cochlea; cross-section through a turn of the Organum spirale; schematic drawing. [8]
The basilar membrane (Lamina basilaris) forms the base of the Ductus cochlearis and supports the cochlear organ (Organ of CORTI or CORTI’s organ). The Stria vascularis at the lateral bony wall of the Cochlea pro-duces the endolymph.
* REISSNER’s membrane
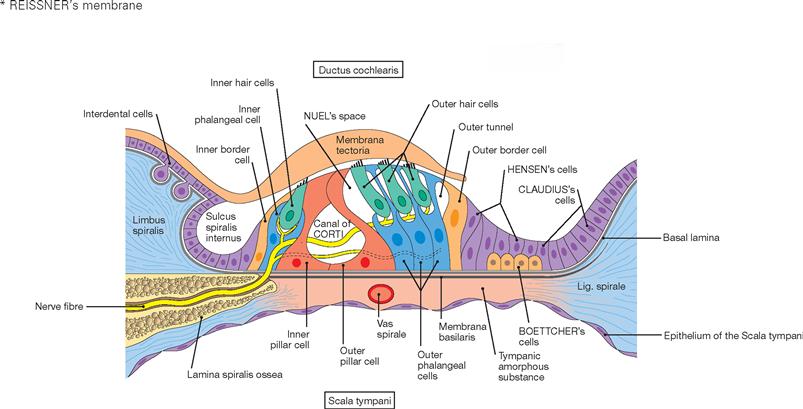
Fig. 10.53 Organum spirale (Organ of CORTI); schematic drawing. [24]
This is a simplified presentation of the complex afferent and efferent innervation of the hair cells.
The organ of CORTI represents the actual cochlear organ. Cochlear sensory cells (hair cells) together with different supporting cell types rest on the basilar membrane and a gelatinous membrane (Membrana tectoria) covers their apical cell surface. The organ of CORTI stretches along the whole length of the Ductus cochlearis.
Hearing and equilibrium
Mechanoelectrical sound conduction and equilibrium (balance) organ
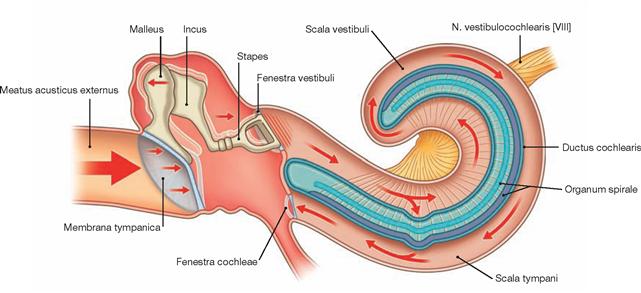
Fig. 10.54 Mechanoelectrical sound conduction. [8]
Sound propagates by sound waves which reach the outer ear (auricle and external acoustic meatus) and are transmitted by the tympanic membrane and the chain of auditory ossicles through the base of the Stapes to the perilymph. Vibrations at the oval window initiate movements of perilymph causing migrating waves running along the walls of the Ductus cochlearis (particularly the basilar membrane). These waves cause a deflection of the basilar membrane and the organ of CORTI. Consequently, stereocilia of the inner hair cells deflect. The sensory cells transduce this biomechanic event into a receptor potential (mechanoelectrical transduction).
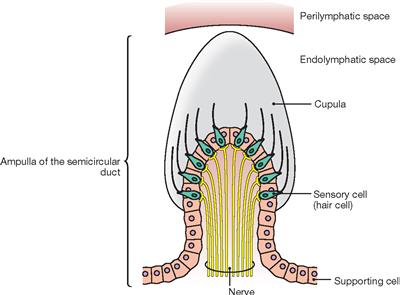
Fig. 10.55 Structure of the Crista ampullaris. (according to [25])
The vestibular labyrinth is filled with endolymph and consists of the Sacculus (Macula sacculi – vertical linear acceleration), Utriculus (Macula utriculi – horizontal linear acceleration), and the three semicircular canals (Cristae ampullares with their Cupulae – rotational acceleration). The sensory cells of the vestibular organ possess a long kinocilium and stereocilia which extend into a gelatinous substance (Cupula). Movements of the Cupula result in the deflection of these cellular processes on the surface of the sensory cells. This presents a stimulus for the synaptic activation of afferent fibres of the N. vestibularis.
Hearing and equilibrium
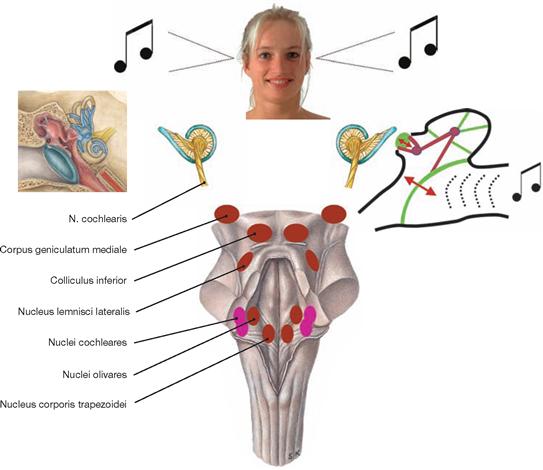
Fig. 10.56 Hearing.
Primary nuclei (purple): Nuclei cochlearis anteriores and posteriores; other nuclei (brown): upper olivary complex, Nuclei lemnisci, Colliculi inferiores, Corpora geniculata medialia. The neuronal network of primary and secondary groups of nuclei constitutes the auditory pathway and is shown in → Figure 10.58. The chain of auditory ossicles amplifies the amplitude of the sound waves physically.
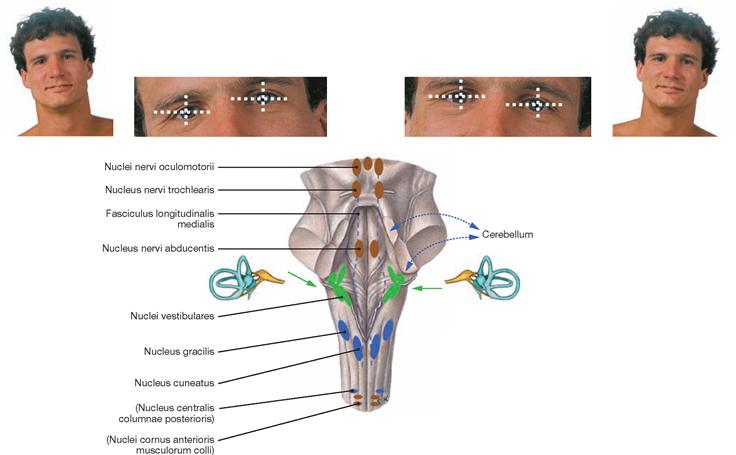
Fig. 10.57 Control of equilibrium and stabilisation of the visual field.
Afferent fibres originate in the muscles of the eye, the equilibrium organ, and the muscles of the neck; efferent fibres modulate the mus-cles of the eye and the body. The cerebellum plays a predominant role in this coordination.
Auditory pathway
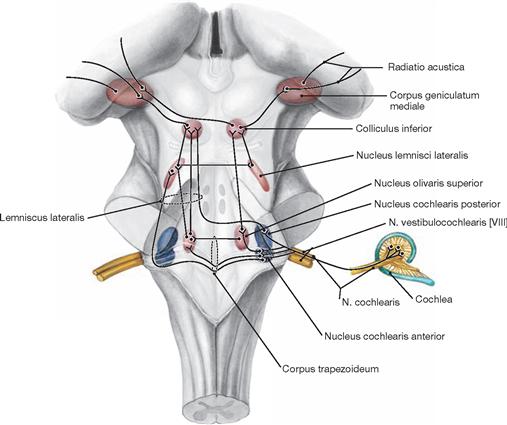
Fig. 10.58 Auditory pathway; overview.
The function of the ascending auditory pathway is to transmit acoustic signals to the brain, to process this information centrally, and to create an acoustic awareness.
1. neuron: bipolar cells in the Ganglion spirale cochleae
• After exiting the small apertures of the Tractus spiralis foraminosus deep within the internal acoustic meatus, the fibres form the N. cochlearis unite with the N. vestibularis at the floor of the internal acoustic meatus to form the N. vestibulocochlearis [VIII].
• Fibres from the basal cochlear part traverse to the Nucleus cochlearis posterior and those from the apical parts terminate in the Nucleus cochlearis anterior.
2. neuron: multipolar cells of the Nuclei cochleares
• The fibres from the Nucleus cochlearis anterior pass mainly to the olivary complex on the same or opposite side.
• Apart of the fibres crosses to the opposite side and, without synapsing, run in the Lemniscus lateralis to the Colliculus inferior.
• Fibres that reach the olivary complex on the same side, either ascend to the Nucleus lemnisci lateralis, synapse, cross to the opposite side, synapse again, and then reach the Colliculus inferior or they ascend directly in the Lemniscus lateralis to reach the Colliculus inferior.
3. or 4. neuron: From the Colliculus inferior connections are made to the Corpus geniculatum mediale.
4. or 5. neuron: The acoustic radiation (Radiatio acustica) connects the Corpus geniculatum mediale with the transverse temporal HESCHL’s gyri or convolutions and the WERNICKE’s centre in the temporal lobe.
Equilibrium (balance) pathway
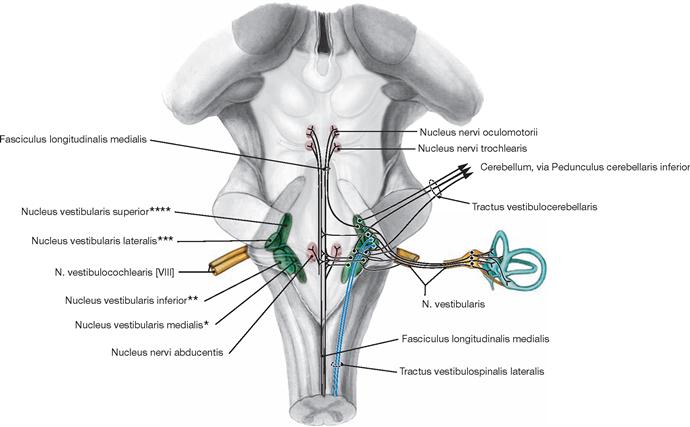
Fig. 10.59 Equilibrium (balance) pathway; overview.
The equilibrium (balance) pathway coordinates eye movements and movements of the torso, neck, and extremities.
• The afferent fibres of the Ganglion vestibulare mainly project into the Nucleus vestibularis medialis (SCHWALBE’s nucleus), the Nu-cleus vestibularis superior (nucleus of BEKHTEREV), and the Nucleus vestibularis inferior (ROLLER’s nucleus).
• Afferent fibres of the Cristae ampullares of the semicircular canals mainly course to the nucleus of BEKHTEREV and SCHWALBE’s nucleus as well as into the vestibulocerebellum via the direct sensory cerebellar pathway.
• Afferent fibres of the Utriculus project into the medial vestibular nu-cleus, afferent fibres of the Sacculus project into the lateral vestibular nucleus.
• The lateral vestibular nucleus (DEITERS’ nucleus) also receives collateral fibres from the vestibular pathways and, in particular, connections from the Cerebellum.
2. neuron: from the vestibular nuclei efferent fibres project
• to the Cerebellum (Tractus vestibulocerebellaris)
• to the spinal cord (Tractus vestibulospinalis)
• to the nuclei controlling the extraocular muscles (Fasciculus longitudinalis medialis)
• to the Thalamus (via the Tractus vestibulothalamicus to the Nucleus ventralis posterior inferior and from there via the Radiatio thalami to the Gyrus postcentralis)
* SCHWALBE’s nucleus
** ROLLER’s nucleus
*** DEITERS’ nucleus
**** nucleus of BEKHTEREV