Nursing and the Health Care System
Upon completing this chapter, you should be able to:
1 Describe Florence Nightingale’s influence on nurses’ training.
2 Explain why nursing is both an art and a science.
3 Indicate how evidence-based practice is helpful in nursing.
4 Trace the growth of nursing in the United States from the Civil War to the present.
5 Discuss the ways in which the desirable attributes of the nurse might be demonstrated.
6 Identify the educational ladder that is available to nurses.
7 Describe educational pathways open to the LPN upon graduation.
8 Compare methods of delivery of nursing care.
9 List four practice settings in which LPNs may find employment.
10 Identify segments within the various levels of health care.
11 Explain how a health maintenance organization and a preferred provider organization differ.
12 Relate how the managed care system has affected your own health care.
1 Write your own definition of nursing.
2 Discuss how the standards of practice for the LPN/LVN are applied in the clinical setting.
3 List the practice areas in the community in which you could be employed as a vocational nurse.
apprenticeship ( p. 2)
p. 2)
aseptically ( , p. 4)
, p. 4)
capitated cost (p. 9)
diagnosis-related groups (DRGs) ( , p. 9)
, p. 9)
evidence-based nursing (p. 4)
health maintenance organizations (HMOs) ( , p. 9)
, p. 9)
implement ( , p. 6)
, p. 6)
integrated delivery network (p. 9)
interventions (p. 3)
invasive procedures ( , p. 3)
, p. 3)
nursing process (p. 6)
nursing theory (p. 4)
practice acts (p. 6)
preferred provider organizations (PPOs) (p. 9)
HISTORICAL OVERVIEW
The art of nursing arose in primitive times when one person simply cared for another who was sick. As family groups banded together into communities, certain individuals extended themselves to care for the ill, the helpless, and the elderly. During this period, nursing consisted of comforting, caring for basic needs, and using herbal remedies.
NURSING IN ENGLAND AND EUROPE
As civilizations appeared, nurses were under the direction of the priest-physicians because illness was often believed to be caused by sin or the gods’ displeasure. With the growth of Christianity, caring for the sick became a function of religious orders. The Christian St. Paul introduced a deaconess named Phoebe, a practical nurse, to Rome. She was the first visiting nurse. Both men and women tended the sick during this period. Nursing became a recognized vocation during the Crusades (1100 to 1200 AD) as hospitals were built to care for the large number of pilgrims needing health care.
The service provided by the religious orders in England changed with the break between King Henry VIII of England and the Catholic Church in the 1500s. The nuns and priests were sent out of the country. The patients in their hospitals were abandoned; the hospitals became the responsibility of the government. Criminals, widows, and orphans were recruited, and in exchange for housing and food, they tended the sick. The drunken nurse-midwives Sairey Gamp and Betsy Prig, as portrayed in Charles Dickens’ 1849 novel Martin Chuzzlewit, were typical of hospital nurses at the time. Health care conditions became very bad.
Florence Nightingale
In the mid-1800s Florence Nightingale, an Englishwoman, felt a calling by God to become a nurse. Nightingale studied in Germany with a Protestant order of women who cared for the sick. She went on to reform and manage a charity hospital for ill governesses. During the Crimean War, Florence Nightingale asked the Secretary of War to allow her to train women to care for the sick and wounded. By cleaning up the wards and improving ventilation, sanitation, and nutrition, her group of 38 nurses lowered the death rate from 60% to 1%. The Nightingale nurses made their rounds after dark with the aid of a lighted oil lamp. The lamp became the official symbol of nursing. Florence Nightingale kept records and statistics that reinforced her theories of care, many of which are still valid today.
Funds were given out of gratitude by the servicemen and their families. These funds were used to begin the first Nightingale training school for nurses, located in England at St. Thomas Hospital. Nightingale based her curriculum on the following beliefs:
• Nutrition is an important part of nursing care.
• Fresh, clean air is beneficial to the sick.
• Sick people need occupational and recreational therapy.
• Nurses should help identify and meet patients’ personal needs, including providing emotional support.
• There are two conditions to which nursing should be directed: health and illness.
• Nursing is distinct and separate from the practice of medicine and should be taught by nurses.
NURSING IN NORTH AMERICA
Nursing care was sadly lacking during the Civil War in America. The Union government finally appointed Dorothea Dix, a social worker, to organize women volunteers to provide nursing care for the soldiers. These workers were like the nursing assistants of today. Clara Barton took volunteers into the field hospitals to care for soldiers of both armies. She later founded the American Red Cross. Lillian Wald took nursing out into the community, and in 1893 she established the Henry Street Settlement Service in New York City. In the period following the Civil War, nurses’ training was essentially an apprenticeship (learning by doing). Over time, the schooling became more formal and the hospital-based training period lengthened from 6 months to 3 years. Graduates of the training program received a diploma. In an era when women were expected to remain at home and be subservient to men, nurses’ training became a way to obtain further education and employment that could provide independence for women.
In 1892 the New York Young Women’s Christian Association (YWCA) started the Ballard School, which offered a 3-month course in practical nursing. Students were trained to care for infants, children, and the elderly in the home. A legacy left by Thomas Thompson allowed Richard Bradley, the executor of the will, to open a practical nursing school in Brattleboro, Vermont, in 1907. In 1918 a group of women opened the Household Nursing School in Boston to train nurses to care for the sick at home. Later this school was called the Shepard Gill School of Practical Nursing.
The training in the Nightingale schools varied considerably from that of the U.S. nursing schools. The Nightingale program was well organized, with classes held separately from practical experience on the wards. The core curriculum was the same in all schools. Instruction was provided by a trained nurse and was focused on nursing care.
In the United States, the students staffed the hospital and worked without pay. There were no formal classes; education was achieved through work. There was no set curriculum, and content varied depending on the type of cases present in the hospital. Instruction was done at the bedside by the physician and therefore came from a medical viewpoint.
In the 20th century nurses moved out into the community. They worked with the poor in the cities, provided midwifery services, and taught prenatal, obstetric, and child care (Figure 1-1). Nurses were present during wartime, providing essential care on all fronts (Figure 1-2). During World War I, nurses worked behind the lines to care for sick and wounded soldiers (Figure 1-3). Also, the first African American nurses to serve in the U.S. Army paved the way for others to follow (Figure 1-4). World War II created a great demand for nurses in military hospitals, and training programs had to be increased (Figure 1-5). Congress passed a bill to draft nurses, but the declaration of peace occurred before it was enacted. Nurses continue to serve in times of military crisis, as they have for Operation Iraqi Freedom.

FIGURE 1-1 A Red Cross public health nurse poses with her Model T Ford before setting out on her rounds. (Photo courtesy of The American National Red Cross.)

FIGURE 1-2 During the Spanish-American War in 1898, nurses traveled by sea to care for soldiers in need. (Photo courtesy of The American National Red Cross.)

FIGURE 1-3 During World War I, a Red Cross nurse at a field hospital in France bathes the eyes of a gassed patient from the U.S. Army. (Photo courtesy of The American National Red Cross.)
THE ART AND SCIENCE OF NURSING
There are many definitions of nursing, and as you progress through your nursing career, ideas about what nursing is will grow and change. Among the various definitions, the following four common goals appear:
To accomplish these goals, the practical nurse takes on the role of caregiver, educator, collaborator, and manager. Caregiving skills are interventions aimed at restoring and maintaining a person’s health. Interventions are actions taken to improve, maintain, or restore health or prevent illness. An example would be assisting a patient with hygiene tasks such as bathing and brushing the teeth. Today caregiving skills extend to using highly technical equipment for medical therapies and protecting the safety of the patient undergoing invasive procedures (procedures that require entry into the body). Nurses provide both physical and emotional care to patients. By performing various tasks and working closely with the patient, nurses develop a concern for the patient’s well-being. The nurse’s goal is to encourage growth toward wellness so that the patient can once again be self-reliant.
Health teaching and counseling are functions of the practical nurse and are directed toward promoting wellness and preventing illness. Teaching about medi cations and how to aseptically (without introducing infectious material) change dressings are examples of this role. Emotional support and comfort are incorporated in care, and the nurse is an advocate for the patient during times of health-related stress.
The licensed practical nurse (LPN) or licensed vocational nurse (LVN) collaborates with the registered nurse (RN) and other members of the health care team to provide continuity of care. Care for the patient is planned jointly by all members of the health care team. Minor tasks such as taking vital signs or giving a bed bath may be assigned to the nursing assistant or other ancillary personnel.
Therapeutic communication techniques facilitate a patient’s ability to cope. Active listening is a therapeutic technique that helps the patient consider possible solutions when a problem occurs. Establishing a good nurse-patient relationship is necessary to gain the patient’s trust so that teaching and other communications are well received.
Initially nursing was an art’it consisted of performing certain acts of care skillfully, with intuition and creativity. Over time, a scientific base was combined with the art of nursing. From this body of knowledge, the nurse can choose interventions that are most likely to produce desired outcomes for the patient.
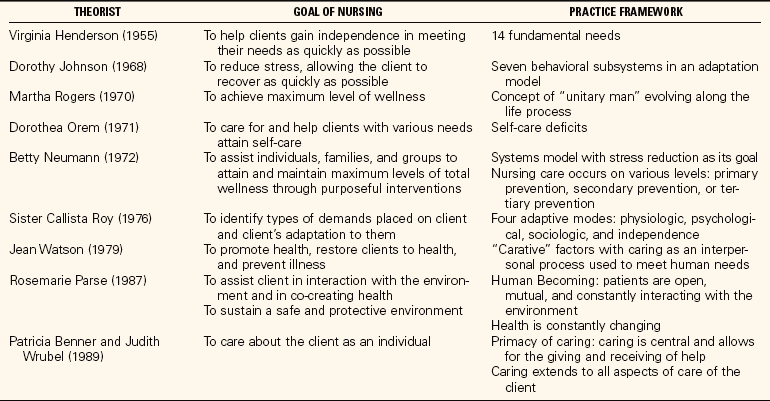
As this scientific base for nursing has developed, various scholars have proposed theories concerning the process of nursing. A nursing theory is a statement about relationships among concepts or facts, based on existing information. Nursing theorists generally base their beliefs on the relationships among humans, environment, health, and nursing. Table 1-1 provides a brief explanation of some of the major nursing theories. A particular theory may be the basis of a nursing school’s curriculum structure and part of its philosophy of how nursing care is delivered. Nursing strives to maintain recognition as a profession. For this reason, ongoing research is essential to add to the scientific knowledge base.
EVIDENCE-BASED PRACTICE
The promotion of evidence-based nursing has become stronger around the world over the last decade. It involves the “integration of best research evidence with clinical expertise and patient values to facilitate clinical decision making” (DiCenso et al., 2005). Students are being taught the skills to discriminate between high-quality and flawed research and to interpret the study results. Nurses are being strongly encouraged to seek evidence for their practice throughout their careers. Evidence-based practice is using the best scientific evidence from research to guide decision making (Benefield, 2002). Evidence-based nursing is used to help determine “best practices.” Best practices are optimal techniques, procedures, or programs identified by one or more organizations that improve care effectiveness or efficiency while providing positive patient outcomes (Huffman, 2005). Clinical field experience and evidence-based research are used to establish the best practices for patient care.
CURRENT NURSING PRACTICE
As nursing has grown and changed to meet the needs of society, laws have been made and standards set that govern the practice of the profession. In 2004 the American Nurses Association (ANA) revised the Standards of Nursing Practice (see Appendix 1). These standards for the professional registered nurse protect the nurse, the patient, and the health care agency where nursing care is given. The practical nurse follows standards as written by the National Federation of Licensed Practical Nurses to deliver safe, knowledgeable, nursing care (Box 1-1, Appendix 4). The National Association for Practical Nurse Education and Service (NAPNES) has formulated an additional set of standards for practical nurses (see Chapter 3). In Canada, another set of similar standards guides the practice of nursing (Box 1-2).
Nurse practice acts have been established in each of the states of the United States and in the provinces of Canada to regulate the practice of nursing. Each state has a regulatory body that makes and enforces rules and regulations for the nursing profession. The practice acts generally define activities in which nurses may engage, state the legal requirements and titles for nursing licensure, and establish the education needed for licensure. The practice acts are designed to protect the public, and they define the legal scope of practice. Policy and procedure books are established by each facility that hires nurses. These books define which procedures each professional can perform in that facility as well as specify step-by-step guidelines for the way that facility wants a procedure performed.
The nursing process emerged during the 1970s and 1980s as an organized, deliberate, systematic way to deliver nursing care. The nursing process provides a way to implement (to put into action) caregiving, and it combines the science and the art of nursing. The nurse focuses on the patient as an individual, identifies health care needs and strengths of the patient, establishes and implements a plan of action to meet those needs, and evaluates the outcomes of the plan. It is a circular process involving ongoing assessment. The nursing process is presented in depth in Unit Two: The Nursing Process.
NURSING EDUCATION PATHWAYS
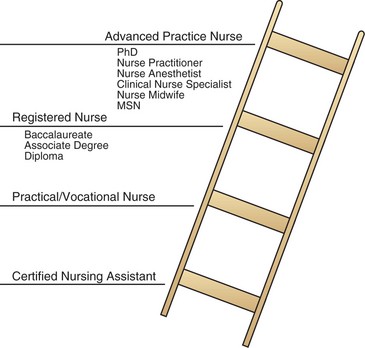
Formal education has been another way to build a professional image for nursing. Nursing education has been mostly moved from hospital training schools into institutions of higher learning. There are two levels of entry into nursing: practical (or vocational) nursing and professional (registered) nursing. Often a student studies to become a certified nursing assistant before going up the “ladder” to practical/vocational training. Each educational program produces graduates with skills for a particular level of entry into practice. A nursing assistant program is short, averaging 6 to 8 weeks. Basic personal care and basic nursing skills are taught. The practical nursing program generally takes 12 to 18 months to complete. The professional nursing program (RN) requires 2 to 5 years of education, depending on the type of degree sought (Figure 1-6). If the student has already obtained a practical/vocational nursing license, the program may require only one more year to become an RN.
PRACTICAL NURSING
Practical nursing was created to fill a gap left by nurses who enlisted in the military services during World War II. Programs were developed to train practical nurses to care for well people and those who were mildly or chronically ill or past the acute stage of illness. Registered nurses could then concentrate on the acutely ill. A need for practical nurses continued after the war, and the National Association for Practical Nurse Education and Service (NAPNES) was formed to standardize practical nurse education and to establish licensure criteria for graduates. Practical nursing programs are offered in vocational schools, hospitals, proprietary schools, and community colleges. Graduates take the National Council Licensure Examination for Practical Nurses (NCLEX-PN®) after program completion. Successfully passing the exam and obtaining licensure allows the use of the initials LVN or LPN after one’s name. Practical nurses provide direct patient care under the supervision of a registered nurse, physician, or dentist. Many community colleges have structured the practical nurse curriculum so that graduates can easily enter the second year of the registered nursing program. This type of curriculum is considered a “ladder program.” Many LPN/LVN programs require that the entering student be a certified nursing assistant (Figure 1-7).
After completion of an LPN/LVN curriculum and/or licensure, the graduate can seek certification by NAPNES in pharmacology and long-term care. The pharmacology examination can be taken online. Pharmacology certification is for 5 years and can then be renewed.
REGISTERED NURSING
Graduates of three different educational programs are qualified to take the registered nurse licensure exam (NCLEX-RN®): a hospital-based diploma program, a 2-year associate degree program at a community college, or a 4-year baccalaureate nursing program at a college or university. Registered nurses may provide bedside care or care in the community, or supervise others in managing care of multiple patients.
Diploma schools decreased as the desire to improve the professional image of nursing through more formal education occurred. Hospitals could no longer afford to provide the expensive diploma programs. Diploma nurses are very well trained in skills compared with the students of other programs. They spend a far greater number of clinical hours working directly with patients, but they do not get as broad a base of scientific knowledge as college-educated nurses receive.
Associate degree programs attract the majority of registered nurse students. The associate degree nurse is considered a technical nurse and is not specifically prepared to work in a management position, although many do. Graduates of these programs have 2 years of clinical experience along with their academic classes.
Baccalaureate nursing programs prepare nurses who have managerial skills as well as bedside nursing skills. These graduates are considered professional nurses. The push toward professionalism for nursing has caused the ANA to propose that the baccalaureate degree be necessary for entry into professional nursing practice. There has been considerable controversy over this proposal because the many registered nurses who graduated from diploma or associate degree programs feel that their jobs may be threatened by such a proposal. To date, most employers do not distinguish between the various educational programs of the registered nurse, and view graduates of all three programs as the same. Another concern is that, if the more expensive and longer program is required to become a professional registered nurse, employers would have to pay higher salaries. The nursing shortage has also tempered the thrust for all nurses to be baccalaureate prepared since the program is twice as long.
ADVANCED PRACTICE NURSING
Graduate programs are available in nursing for both master’s and doctorate degrees. Nurses who pursue higher education are prepared as specialists in the various clinical branches of nursing, in research, or in administration. Another form of advanced education is the nurse practitioner program. Registered nurses continue their training in a specialty such as family practice, pediatrics, maternity, psychiatry, adult health nursing, or geriatrics, and once licensed can practice more independently than as a registered nurse. Nurse practitioners usually provide care in an outpatient, ambulatory care, or community-based setting. In many states they can treat patients on their own and write prescriptions under the direction of a physician. A certified nurse-midwife (CNM) is a registered nurse with further training in midwifery. Certification is by examination through the American College of Nurse-Midwives.
The ANA set up a separate American Nurses Credentialing Center to enhance the professional image of nursing. Registered nurses who have experience in a particular specialty may take a comprehensive examination. Passing the exam provides the nurse with certification of expertise in that specialty. Certification is also available for the practical nurse under a program developed by NAPNES.
DELIVERY OF NURSING CARE
Various systems of delivering nursing care have been tried through the years. Today various adaptations are devised to meet the specific needs of the patients and nurses. Functional nursing care was the first care delivery system for the practical nurse. Practical nurses performed a series of tasks such as administration of medication and treatments. Care was rather fragmented. Team nursing evolved in the 1950s and extended into the mid-1970s. A registered nurse was the team leader who coordinated care for a group of patients. Work tasks were assigned to the other members of the team, the practical nurses and the nurses’ aides. This system worked fairly well as long as there was excellent communication among the members and the team leader evaluated care delivered. Total patient care came next, in which one nurse carried out all nursing functions for the patient, including medication administration. This was an effort to provide less fragmented care for the patient.
Primary nursing appeared in the late 1960s and 1970s. In this system, one nurse plans and directs care for a patient over a 24-hour period. This method eliminated fragmentation of care between shifts. When the primary nurse is off duty, an associate nurse takes over the care and planning. Today, primary nursing is often modified with the use of cross-trained personnel assigned to help with duties. To increase the level of productivity, ancillary workers supervised by the RN are trained in multiple functions, such as clerical and housekeeping tasks and vital sign measurement and phlebotomy. This system has not been entirely satisfactory. Presently, because research is showing better patient outcomes with more of the care being delivered by nurses, there is a trend back to total patient care.
PRACTICE SETTINGS
Practical nurses work in areas where there is supervision by a registered nurse, physician, or dentist. Community nursing, school nursing, and public health nursing presently are primarily the arena of the professional registered nurse. Practice settings for the LPN/LVN include the following:
• Hospitals: Restorative care is provided to ill or injured patients
• Extended care facilities: Facilities for intermediate or long-term care where personal care and skilled care is provided for those requiring rehabilitation or custodial care
• Physicians’ offices: Ambulatory patients receive preventive care or treatment of an illness or injury
• Ambulatory clinics: Ambulatory patients come for preventive care or treatment of an illness or injury; often treatment by specialty groups is available on site
• Renal dialysis centers: Patients with kidney failure receive renal dialysis treatments
• Hospices: Supportive treatment is provided for patients who are terminally ill
• Home health agencies: In-home care is provided to patients by nurses who visit the home
• Neighborhood emergency centers: Minor emergency care is provided to patients within the community setting
As the role of the practical nurse expands, employment in other practice settings is possible.
TODAY’S HEALTH CARE SYSTEM
In times past, most medical care was provided by physicians in private practice. With the technological advances in medicine and the flood of new drugs on the market, health care costs have risen dramatically. Although the use of magnetic resonance imaging (MRI) and computed tomography (CT) provides much more data than a standard radiograph, both cost much more. Microsurgical techniques allow procedures that would not have been possible 20 years ago. The elderly are living longer and needing more years of medical care and many prescription drugs.
Diagnosis-related groups (DRGs) were created by Medicare in 1983 as an attempt to contain health care costs. The DRG system means that a hospital receives a set amount of money for a patient who is hospitalized with a certain diagnosis. If a patient is admitted with pneumonia, only a certain number of days of hospitalization are allowed and will be paid for by Medicare. If the patient has other known problems, they are mentioned when he is admitted. It is to the advantage of the hospital and physician to indicate all possible diagnoses when the patient enters the hospital. If the patient with pneumonia also has diabetes, the length of stay is likely to be longer. Adding this diagnosis at admission provides an extra measure of money for the patient’s care. Private insurance companies have adjusted their payments in many instances to be more in line with what Medicare will pay for the same problem. This system has created a large amount of paperwork for all health care agencies and caregivers. In 2008 Medicare will stop paying hospitals for care related to preventable hospital-acquired conditions. This means that if a patient contracts an infection as a result of poor catheter care or poor aseptic techniques while in the hospital, the hospital will not be paid for the care and extra days the patient is there to clear the infection. To clearly prove patient needs and proper care, nursing documentation of patient assessment and identified need become very important.
In December of 2003, Congress passed the controversial Medicare Prescription Drug Modernization and Improvement Act, which is meant to supply financial relief to seniors who take multiple prescription drugs. The way the law is written and the intricacies of the program have caused many problems. About 6 million low-income and disabled persons found their drug coverage reduced from former levels. Many retirees have been forced to go from private insurance–funded prescription coverage to this new government program. Although beneficial to low-income participants, it provides only modest relief for middle-income seniors. Medicare recipients have the option to forego traditional Medicare coverage and receive vouchers for private insurance coverage, mainly from health maintenance organizations, that will provide some prescription drug coverage. There will be very high deductibles for the drug coverage. Legislative work is underway to correct problems with the Medicare Prescription Drug Program.
LEVELS OF HEALTH CARE
An emphasis on managing health care rather than on managing illness is coming to the forefront. There is more focus on maintaining wellness and on providing preventive care. The integrated delivery network is a set of providers and services organized to deliver coordinated care to promote wellness, care for illness, and promote rehabilitation. This type of network performs these services for a set or capitated cost, meaning that they are paid a set fee for every patient enrolled in the network each year.
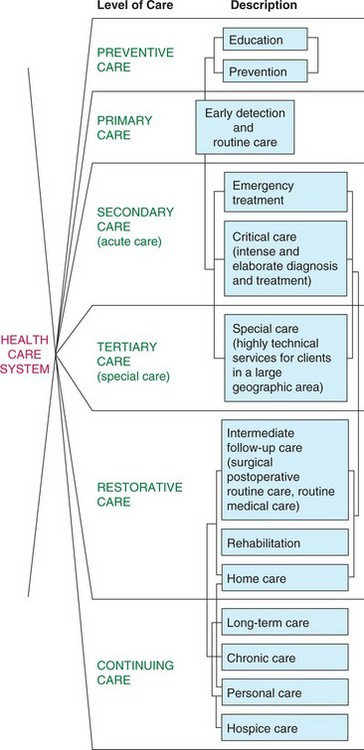
There are six levels of care within the health care system: preventive, primary, secondary, tertiary, restorative, and continuing care (Figure 1-8). The levels of care show the scope of services and settings where patients receive care across the spectrum of health and illness. Box 1-3 depicts the types of specific services available within the various levels of care.
HEALTH MAINTENANCE ORGANIZATIONS
The need to decrease the high cost of medical care has caused health care providers to group together to provide services. Health maintenance organizations (HMOs), a type of group practice, enroll patients for a set fee per month. They provide a limited network of physicians, hospitals, and other health care providers from which to choose. Two national HMOs are Kaiser Permanente and Family Health Plan (FHP). The patient or employer pays a monthly fee for the insurance, and a small copayment may be required from the patient for each visit. Patients must be referred by their primary physician for diagnostic tests, hospitalization (including emergency room visits), and consultation with a specialist. Part of the philosophy of the HMO is that because the patient does not pay the full cost for each visit, earlier treatment will be sought and serious illness can be avoided. One goal of the HMO is to keep patients healthy and out of the hospital.
PREFERRED PROVIDER ORGANIZATIONS
Large businesses and insured groups may contract with preferred provider organizations (PPOs). PPOs offer a discount on fees in return for a large pool of potential patients. Using PPOs allows insurance companies to keep their premium rates lower and in turn makes insurance coverage of employees less expensive for employers. Patients then choose a physician from the list of those associated with the PPO. There are usually a larger number of physicians to choose from in a PPO than in an HMO.
THE MANAGED CARE ENVIRONMENT
There is considerable controversy about the effectiveness of this managed care approach to health care. Patients find that they cannot establish a long-term relationship with a physician because employers’ contracts with PPOs change frequently, and HMOs find that physicians frequently leave for employment elsewhere. Patients resent having to see their primary physician before seeing other specialists.
Nurses must constantly think critically about cost containment while trying to give optimal care to patients. Vigilant assessment with documentation is more important than ever in order to catch beginning complications before they become serious. Budgeting issues for every department and unit in a health care agency concern each employee. The nurse who forgets to discontinue a heating pad the patient is no longer using, or forgets to charge for an item taken from the supply cart, is costing the nursing unit and the health care agency money. Documentation is exacting because every treatment and each use of equipment must be documented with evidence showing it is needed.
In an effort to cut costs, many hospitals are cross-training personnel to fulfill more than one function. Unit secretaries may be training to be electrocardiography (ECG) monitor technicians or housekeeping staff may be trained to perform tasks usually done by nursing assistants, such as taking vital signs. Fewer nurses are found on nursing units than before, and they care for a larger number of patients. Nurses must learn to be good managers and to maximize use of ancillary personnel in order to accomplish their work.
Health care agencies are beginning to find that nurses are very necessary to the agency and can provide a much better quality of care than ancillary workers. With time, a balanced ratio of qualified, licensed personnel to patients will again occur.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. When nursing was taken out into the community, nursing education was essentially:
2. The American Red Cross was founded by __________________________, as an outgrowth of service during the _______________________ war. (Fill in the blanks.)
3. In setting up her nurses’ training, Florence Nightingale carried out her belief that: (Select all that apply.)
1. recreational therapy is essential to recovery.
2. large classes are detrimental to learning.
3. nursing should be taught by nurses.
4. proper nutrition is essential to recovery from illness.
5. any woman could be trained to be a nurse.
4. Inherent in any definition or philosophy of nursing are several core concepts. The core concepts include: (Select all that apply.)
6. One main difference between a licensed practical nurse and a registered nurse is that the licensed practical nurse:
1. usually is responsible for giving medications.
2. performs only noninvasive procedures.
7. Which of the following nursing education programs prepares a nurse for a management role?
8. Which one of the following would be an example of collaborative practice?
1. Showing the patient how to cleanse a wound
2. Speaking with the social worker about the patient’s insurance problems
3. Administering each of a patient’s prescribed medications
4. Asking the nursing assistant to take the vital signs on three patients
9. An advantage to the patient of a managed health care system is: