Cultural and Spiritual Aspects of Patient Care
Upon completing this chapter, you should be able to:
1 Describe how culture influences health and health care choices.
2 Identify three beliefs or values affecting health care that might be found among patients from the following cultural groups: Hispanic American, Asian American, American Indian, African American, and European American.
3 Plan ways to support the spiritual needs of patients of various religions.
4 Compare ethnic differences of Hispanic Americans and Middle Eastern Muslims.
5 Discuss the ways in which poverty often impedes adequate health care within our country.
6 Describe how religious beliefs and practices may affect health and health care choices.
7 Incorporate major differences in dietary and nutritional choices among cultural and religious groups into patients’ plans of care.
1 Demonstrate cultural competence when caring for a culturally different patient.
2 Plan nursing interventions for a patient whose culture is different from your own.
3 Discuss ways to protect patients’ rights when their culture does not permit the use of a medical intervention.
4 Identify signs of spiritual distress in a patient and plan three interventions to relieve it.
5 Discuss boundaries of professional care for a patient whose religious beliefs are different from yours.
agnostic ( , p. 179)
, p. 179)
atheist ( , p. 179)
, p. 179)
baptized (p. 180)
beliefs (p. 179)
bias ( , p. 184)
, p. 184)
chi’i ( , p. 186)
, p. 186)
circumcision ( , p. 182)
, p. 182)
communion (p. 180)
cultural awareness ( , p. 184)
, p. 184)
cultural competence ( , p. 184)
, p. 184)
cultural sensitivity ( , p. 184)
, p. 184)
culture (p. 178)
curandero ( , p. 186)
, p. 186)
dialects ( , p. 184)
, p. 184)
egalitarian ( , p. 185)
, p. 185)
ethnic (p. 183)
ethnocentrism ( , p. 184)
, p. 184)
faith (p. 179)
generalization ( , p. 184)
, p. 184)
holistic (p. 186)
kosher ( , p. 182)
, p. 182)
matriarchal ( , p. 185)
, p. 185)
patriarchal ( , p. 185)
, p. 185)
personal space (p. 184)
prejudice ( , p. 184)
, p. 184)
race (p. 183)
religion (p. 179)
rituals (p. 179)
shaman ( , p. 187)
, p. 187)
spiritual distress ( , p. 189)
, p. 189)
spirituality (p. 179)
stereotype ( , p. 184)
, p. 184)
subcultures (p. 183)
transcultural nursing (p. 183)
values (p. 179)
worldview (p. 178)
yang (p. 186)
yin (p. 186)
CULTURE, RELIGION, AND SPRITUALITY
Culture and religion have a strong impact on health care because they influence the ways in which people think and behave. Lifestyle choices related to nutrition, exercise, stress management, smoking, and alcohol or drug use are all influenced by culture. Religion or spiritual practice has a definite role in recovery of health for many people.
Culture consists of the values, beliefs, and practices shared by the majority within a group of people. Culture includes the attitudes, roles, behaviors, and religious or spiritual practices accepted and expected by the cultural group. Cultural traditions are carried out and passed on from generation to generation. A group’s worldview is the way in which the group’s people explain life events and view life’s mysteries. This viewdirects the formulation of values, which are those ideas and perceptions seen as good and useful.
Immigration has brought increasing cultural diversity within the United States and Canada, as is seen in the different languages, physical characteristics, skin tones, and attire of people, and the ethnic restaurants and foodstuffs encountered in most cities. Patients from many different cultures are encountered in all types of health care settings (Safety Alert 14-1).
Although the terms religion and spirituality are often used interchangeably, there is a difference. Both have to do with attempting to understand one’s place in the world and life’s meaning or purpose. Spirituality concerns the spirit, or soul, and is an element of religion. It is intangible and may include a belief in a higher power, creative force, or divine being, or a belief in spirits of departed people and the supernatural. Religion is a formalized system of belief and worship. Rituals (ceremonial acts) or practices related to health, illness, birth, and death, and prescribed behavior are part of organized religion and sometimes spirituality. Beliefs are convictions or opinions that one considers to be true. Faith is a belief that cannot be proven, or for which no material evidence exists. A person who does not believe in the existence of God is an atheist. An agnostic is a person who doubts the existence of God, because it cannot be proved or disproved.
Spiritual and religious beliefs (or nonbelief) are learned in the family or culture of a child. Over time, faith matures into a way of thinking that influences lifestyle, behavior, attitudes, and beliefs about life, health, illness, and death. Religious and spiritual beliefs change over time and may be especially affected by changes in health. During illness, and especially in the face of death, religious and spiritual beliefs may be strengthened, questioned, or rejected. Health care decisions may be influenced by beliefs regarding health as a gift, or illness or disease as a punishment. There also may be religious prohibitions or requirements for treatment. Some people with spiritual beliefs may see illness or disease as displeasure of the spirits that requires special rituals and ceremonies to remove the displeasure. Prayer and meditation often are used along with a scientific medical regimen by spiritual and religious people.
MAJOR RELIGIONS IN THE UNITED STATES AND CANADA
Many different religions flourish in the United States and Canada. People who identify themselves as Christians are the majority. Until recently, people of the Jewish faith were the second largest group, but rapid increases in the numbers of people who are Muslims now make that religion second largest. All three religions have a faith in one God who created the world and has revealed himself at some point in history. Smaller numbers of people in the United States and Canada, particularly among the Southeast Asian, Chinese, Korean, Indian, and Japanese populations, may believe in the religions of Buddhism, Hinduism, Confucianism, or Taoism (Daoism). Religious beliefs and rituals are interwoven into a group’s culture. However, not all members of a particular cultural group are of the same religion. It is important to inquire about the spiritual life of each individual patient.
CHRISTIANITY
The largest religion in the world is Christianity, with its three main divisions: Roman Catholic, Eastern Orthodox, and the Protestant faiths. Christians believe in eternal life, as promised in the New Testament of the Bible in the message of Jesus. Death is viewed as a transition to a life with God. The administration of the sacraments, particularly the sacraments of baptism and Holy Communion, is very important to most Roman Catholics. A priest or a religious leader should be called if the patient desires a sacrament. Catholic and Eastern Orthodox beliefs related to health care are presented in Box 14-1.
Protestant denominations began when a rift developed between King Henry VIII of England and the Roman Catholic Church and when religious leaders such as Martin Luther objected to some practices of the Roman Catholic Church. The Anglican and Lutheran churches and other Protestant denominations were founded. There are a great many Protestant denominations. The Protestant religious leader is usually called a minister or pastor. Some denominations with considerably different beliefs and practices are Christian Science, Jehovah’s Witnesses, The Church of Jesus Christof Latter-day Saints (Mormon), Unitarian Universalist Association, and the Unification Church. The Bible provides guidance and solace for Christians.
Most Protestant patients seek and accept health care. However, because of the diversity of denominations and their beliefs, it is essential to perform a spiritual assessment to ascertain what needs and concerns the patient might have. Prayer, reading of scripture and devotionals, and attendance at church services are the main religious activities of Protestant patients.
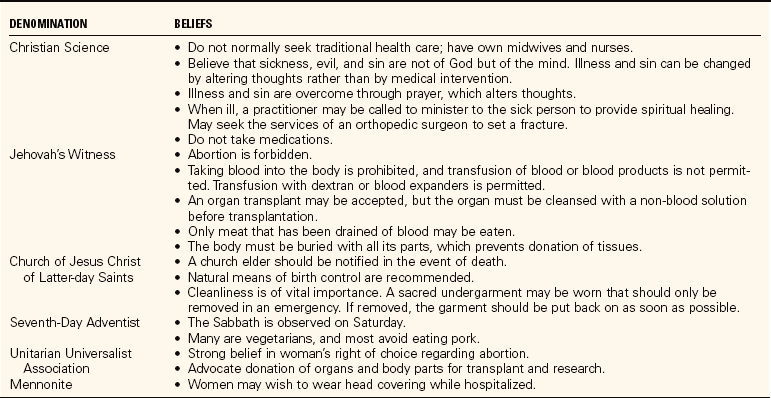
Many Protestant patients may wish to have Holy Communion while hospitalized. Some denominations believe in the anointing of the sick. The pastor or minister should be contacted for the patient desiring these sacraments. Abortion is generally opposed by most Protestant denominations except if the mother’s life is in danger. Birth control decisions are generally left up to the individual family. The religious groups whose beliefs differ from some of the main beliefs described and in specific areas relevant to health care are presented in Table 14-1. Some protestant denominations forbid the use of alcohol, tobacco, tea, coffee, and caffeine substances because they are considered drugs. Beliefs of individuals within each denomination vary, and specific spiritual assessment regarding the various issues relevant to health care is essential.
ISLAM
Islam is one of the fastest growing religions in the world. It is most prevalent in the Middle East, Africa, South Asia, and parts of Eastern Europe. It emphasizes equality of the races and social classes and attempts to promote brotherhood for all. The prophet Muhammad, who made Mecca the focal point of this religion, is believed to have received revelations from God through the angel Gabriel during meditation in the seventh century. Muhammad began preaching that there is only one God, Allah. Visions experienced by Muhammad during his life were written in the Koran and include instructions and guidance about how to live a good life and thereby achieve salvation. An imam is a Muslim religious prayer leader, and the main place of worship is the mosque (Figure 14-1).
Women may not have the independence in a traditional Islamic family that the American assumes as a norm, and some women may not be allowed to make decisions about their health care. Sometimes the woman’s husband or father must be present to give consent for treatment. Beliefs and practices related to health care are listed in Box 14-2.
JUDAISM
Judaism has several branches: Orthodox, Conservative, Reform, and Reconstructionist. The religious leader in Judaism is called a rabbi, and the main place of worship is the synagogue (temple). Judaism began when the one God revealed himself to the nomadic tribes of the Middle East (in the region that is now Israel) thousands of years before the birth of Christ. Strict rules regarding hygiene, diet, sexual mores, and religious ceremony were passed down orally and later written down in the Torah, which is the basis for the Christian Old Testament. Orthodox Jews follow the most strict interpretation of Jewish law. Food is prepared according to Jewish dietary laws during slaughter, processing, and packaging and is then labeled kosher. Jewish religious laws may be relaxed during illness, but it is still very important to consult with the patient to be sure that nursing care does not cause spiritual distress. There are rituals regarding care of a dead body and burial, and the rabbi should be consulted.
Circumcision is a Jewish religious ritual performed by a man called a mohel on the eighth day of a boy’s life. It involves the ceremonial removal of the penile foreskin. Box 14-3 presents the major Jewish beliefs to be considered when planning health care.
HINDUISM, BUDDHISM, AND TAOISM
Many Hindus are vegetarians because most believe that eating meat involves harming a living creature, which is contrary to their beliefs. Illness or disease is seen as the result of the misuse of the body or a consequence of sin committed in a previous life. There is a strong belief that life is controlled by God and that the individual has little control over what happens. Within the family, the eldest woman is considered the authority on health and healing matters. She should be consulted and included in any patient teaching. Ayurvedic medicine, founded in India, follows principles of “hot” and “cold” to balance the diet as needed for the season and the disease state.
Buddhists do not believe in healing through faith, but believe spiritual peace and liberation from anxiety through following Buddha’s teachings are important in promoting health and recovery. Taoists believe that illness or disease is due to an imbalance in yin and yang.
The Asian diet consists of less meat and more vegetables than that of other Americans. Meats are sliced, diced, or shredded and added in small quantities to vegetables. A variety of sauces and spices are used in cooking. “Hot” or “cold” foods are consumed during illness or disease to regain balance within the body (see Nutrition, p. 185). Many religions have dietary rules (Table 14-2).
Table 14-2
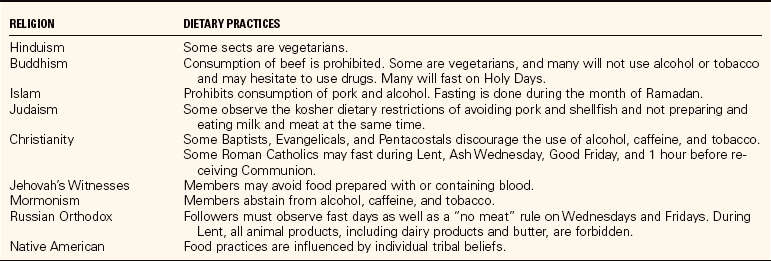
From Potter, P.A., & Perry, A.G. (2005). Fundamentals of Nursing (6th ed., p. 561). St. Louis: Elsevier Mosby.
CULTURAL GROUP CHARACTERISTICS
The main characteristics that differentiate cultural groups from one another are nationality, race, color, gender, age, and religious affiliation (Purnell and Paulanka, 2003). Race is a biologic way of categorizing people. Race is based on physical characteristics such as skin color and texture, facial characteristics, and body proportions. Although there has been considerable blending of race in various parts of the world, there are three basic races: white (people from Europe, western Russia, North Africa, the Middle East, and southwest Asia), Negro (most Africans), and Mongoloid (northern and eastern Asians, Pacific Islanders, and some American Indians). Various ethnic groups are found within a race; these groups are usually differentiated by geographic, religious, social, or language differences (Purnell and Paulanka, 2003).
Major cultural groups within the United States and Canada are European Americans, American Indians, African Americans, Hispanic Americans, Asian/Pacific Islander Americans, and Arab Americans. Subcultures are smaller groups within the culture whose members have similar views and goals in addition to or in place of those of the main culture. A subculture may be based on a variety of characteristics such as socioeconomic status, education, occupation, political beliefs, sexual orientation, or residence in a rural versus urban area. Those living in poverty, a socioeconomic state, become a subculture because of the shared beliefs and practices of the poor. Their orientation is day-to-day survival with little hope for the future. There may be unstable family relationships, alcohol and drug abuse, and often elderly grandparents caring for young children. Emotional and physical disorders may prevent some within this group from meeting their basic needs for shelter, food, and clothing and they become homeless.
The poor and the homeless are more likely to suffer from illnesses and diseases such as malnutrition and tuberculosis, and chronic disorders may become worse because they go untreated. Because of lack of funds, lack of transportation, and/or lack of access to health care, the poor do not attend to preventive health practices and may not receive care for acute illnesses.
TRANSCULTURAL NURSING
Transcultural nursing is a term used by Dr. Madeline Leininger to describe care that recognizes cultural diversity and is sensitive to the cultural needs of the patient and family. It is based on the fact that although there is diversity or differences among cultures, there are also universal patterns of behavior. Dr. Leininger described human caring as what all people need most to grow, remain well, avoid illness, and survive or face death (Leininger, 1991). Thus human caring is part of every culture, but it may be expressed in different ways.
DEVELOPING CULTURAL COMPETENCE
Nurses must develop cultural awareness and cultural sensitivity in order to deliver culturally competent care. Cultural awareness involves knowledge of a people’s history and ancestry and an appreciation for their artistic expressions, foods, and celebrations. Cultural sensitivity is refraining from using offensive language, respecting accepted patterns of communication, and refraining from speaking in ways that are disrespectful of a person’s cultural beliefs (Figure 14-2). Cultural competence involves knowing yourself, examining your own values, attitudes, beliefs, and prejudices. Keeping an open mind and trying to look at the world through the perspectives of culturally diverse peoples is another aspect of cultural competence. Learn all you can about other cultures. Literature written by authors from other cultures can provide a wealth of information and insight into others’ views of the world. Respect differences among people, recognizing that every group has its strengths and weaknesses. Be willing and open to learning by getting to know people. Learn to communicate effectively, being sensitive to the affect, body movements, use of personal space, and gestures of others (Narayan, 2003). Don’t make judgments about cultural behaviors and practices that are different from yours. Be resourceful and creative in fitting nursing interventions into the belief system of the patient. Consider your nursing actions carefully when interacting with a patient from another culture (Cultural Cues 14-1).

FIGURE 14-2 Nurse giving traditional greeting to a Hindu patient. This method of greeting honors the spirit within each of us.
Care must be taken not to let ethnocentrism affect one’s attitude toward a patient. Ethnocentrism is the tendency of human beings to think that their ways of thinking, believing, and doing things are the only way or the only right way. Beliefs that greatly differ from one’s own are seen as strange and are therefore considered wrong.
A generalization identifies common trends, patterns, and beliefs of a group. Generalizations may be true for the group, but not necessarily for a particular individual in the group. Additional information must be sought from the individual patient to determine whether the generalization is true. It is also essential not to stereotype a patient. A stereotype is a set opinion or belief about the group that is applied to an individual. “Hispanics like hot peppers” is a stereotype. Although many Hispanics may like hot peppers, this is not true of all Hispanic people. Stereotypes can be negative or positive, but they all ignore the uniqueness of the patient.
Bias or prejudice (positive or negative attitude or opinion that is unsupported by evidence) should not affect the quality of care a patient receives. All patients should be given the same level of care regardless of race, socioeconomic status, gender, age, spiritual/religious orientation, or personal habits.
CULTURAL AND ETHNIC DIFFERENCES
Particular areas in which cultural difference is evident are communication, view of time, organization of the family, nutrition, issues related to death and dying, and health care beliefs (Purnell and Paulanka, 2003).
COMMUNICATION
An obvious cultural difference among people is language. In a large city, there may be many different languages spoken by various groups as well as differing dialects (regional variations of the language with different pronunciation, grammar, or word meanings). Nonverbal communication patterns differ among cultural groups’for example, degree of eye contact that is acceptable, amount of personal space (space acceptable between two people when conversing) that is appropriate, acceptable touching, and meaning of gestures such as head nodding. The Vietnamese avoid eye contact when talking with someone they consider an authority figure or who is older (Lindsay, Narayan, and Rea, 1998). The American Indian may find sustained direct eye contact rude or disrespectful. In European American culture, 18 inches is the usual space between people that is comfortable when they are talking together. Asians, people from the Middle East, and Hispanics tend to stand closer together when they converse. In some cultures, it is not acceptable to disagree with a superior, which may result in an outward appearance of agreement by people even though they do not agree with what is being said.
Learning key phrases in other languages frequently encountered, or using translation lists of common questions or symptoms, is helpful. A skilled interpreter is needed, however, to obtain assessment data and convey instructions. Most health agencies have people available to interpret when needed. A good interpreter knows the language and the customs of the patient and is knowledgeable about the health care system. One should avoid the use of family members as interpreters whenever possible because the patient may be reluctant to talk through a family member because of modesty or because of privacy concerns. AT&T has a language line service for over-the-phone interpretation of more than 140 languages. It is available 24 hours a day, 7 days a week at 1-800-752-6096. This is not as good a solution as an interpreter who is present, but it helps until one can be found.
VIEW OF TIME
Orientation to time varies from one culture to another, and attitudes about time can cause misunderstanding. An orientation toward the future is a European American dominant cultural value in the United States. There is a sense of time urgency (not enough time), and importance is placed on punctuality and schedules. Other cultures, notably the Hispanic American and the African American, do not have this same view of time. The focus in these cultures is on the here and now, and there is not a feeling of urgency to be someplace right on time. Generally, this applies to social occasions rather than business or medical appointments.
A second consideration of time is whether the culture is mostly concerned with the past, present, or future. Past-oriented cultures attach considerable importance to traditions. Ancestor worship may occur. Some people believe the past is unimportant and the future unpredictable; they live in the present. Future-oriented cultures place a high value on change where their circumstances will be improved. A balance of all three views is prevalent for many individuals. It is important to know the patient’s view of time.
ORGANIZATION OF THE FAMILY
Family households may be male dominated (patriarchal), may be female dominated (matriarchal), or may share equality between men and woman (egalitarian). Knowing the family dominance pattern is important because the head of the household usually plays a role in the health care decisions for the patient. There are very specific roles within some cultures for men and women. Men may be expected to provide for the family and protect its members, manage the finances, and deal with issues in the outside world. The expected female role may be to take care of the children, maintain the home environment, and perform all household tasks. These cultural differences must be respected without trying to impose an egalitarian viewpoint, which is prevalent in the United States.
The position of the elderly varies considerably from one culture to another. In some cultures, the elderly are considered wise and are revered. They are provided for by their children when they are no longer able to care for themselves. In other cultures, although the elderly are loved, when self-care becomes a problem, they may be cared for outside the home.
Extended family members may all live together in some cultures, and there may be several generations under the same roof. In other cultures each couple, with or without children, has its own living space apart from the extended family members.
NUTRITION
What people eat or avoid is influenced by culture. Food has much symbolic and social meaning. People learn from their family culture what foods are “good for you” or should be avoided or used for specific illnesses or diseases. Certain foods are associated with celebrations, and others with comfort and nurture. When a patient is in a health care facility, food choices may be very limited, and changes from the usual time and rituals of eating may occur. Foods are categorized in some cultures (Asian, Hispanic, Middle Eastern) as “hot,” “cold,” or “cool,” based not on their temperature, but on their effect in the body. Each culture has its own set of foods that are viewed as “hot” or “cold.” That effect is used to counteract illness or disease’cold foods are used to treat “hot” illnesses or diseases, and hot foods are used to treat “cold” illnesses or diseases. Because of these beliefs, many patients would not think of drinking ice water when ill.
Family members can often provide food for the patient that fits within the medical orders. Such additions to the health care facility diet not only meet nutritional needs but also provide security and belonging for a patient who may feel frightened and ill at ease in the health care facility setting.
DEATH AND DYING
It is important to become knowledgeable about rituals concerning death and bereavement so that cultural taboos can be avoided. In some cultures, the body must be buried whole; for others, cremation is preferred. Pacific Islanders leave a window open when someone dies, so that the soul can leave (Lester, 1998). Learn cultural views about autopsy before approaching a family on this issue. There may be cultural rituals for preparing the body for burial. Expressions of grief are also culturally based. In some cultural and ethnic groups it is appropriate to display emotions, and in others one is expected to bear the grief of the loss in silence.
HEALTH CARE BELIEFS
Beliefs about health, disease, illness, and treatment are culturally based. In cultural groups who believe the world is dominated by supernatural forces, people feel that one’s fate depends on the action of a god or gods. They are at the mercy of the spiritual force. Religion is an integral part of culture and often plays a very important part in the treatment of the patient.
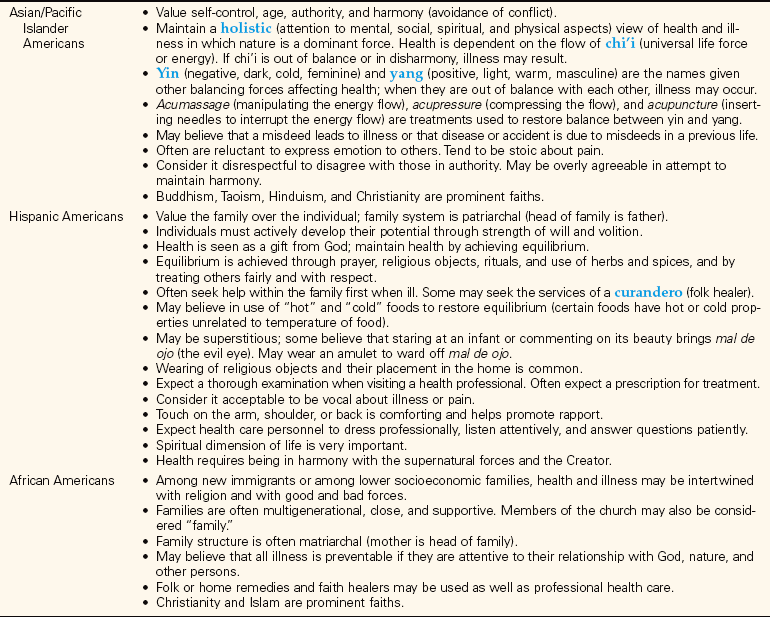
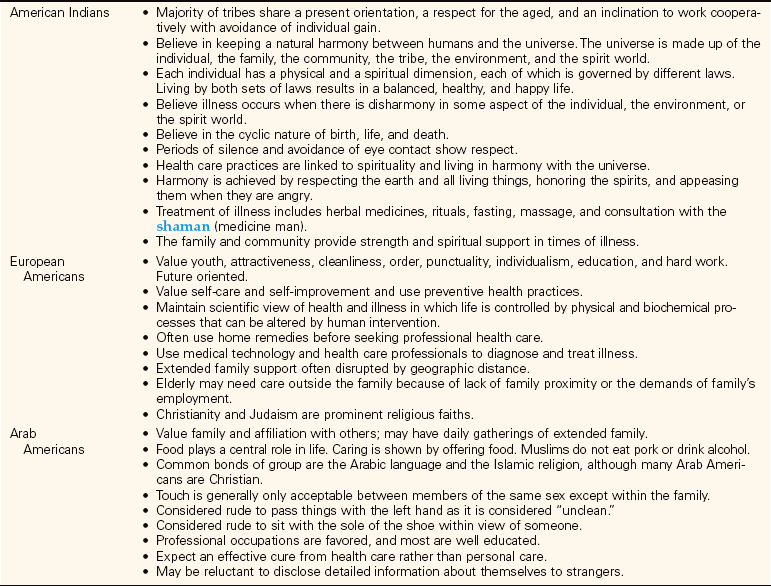
All cultures have an element of folk or home remedy medicine that is handed down through families for treatment of common illnesses. Folk medicine relies on home remedies and self-care practices. Folk medicine is often used first before consulting a health care professional, or it may be used along with seeking professional assistance for an illness. Treating a cough with a particular type of tea with honey and lemon is an example of a folk medicine remedy. The use of the tea may be continued even after going to the clinic and receiving a prescription for antibiotics for a lung infection. Knowing how a patient’s family usually treats the type of illness the patient has is important in understanding any reluctance the patient has in following the professionally prescribed regimen for the illness. Although the scientific view of health care is the majority view in the United States, it may not be the belief of a person raised in another culture. Table 14-3 presents values, practices, and beliefs of various cultures.
Methods of treatment of illness or disease from cultures that believe in holistic health care are slowly becoming integrated into the Western science-based practice of medicine. Alternative therapies such as massage, acupuncture, and chiropractic adjustment are being recommended along with the use of prescription medications and other standard medical treatments. More and more evidence is pointing to a connection between mind and body that influences health, and more emphasis on the use of prayer and meditation is beginning to occur (Patient Teaching 14-1).
SUSCEPTIBILITY TO DISEASE
Certain diseases are passed from parent to child through the genes that determine a person’s characteristics. Nurses should be alert for signs of disorders that are common to a particular culture or race. People of African or Mediterranean background are predisposed to sickle cell trait or sickle cell anemia, a blood disorder that is passed from parents to child. Keloid formation (abnormal scar tissue formation) and sarcoidosis (fibrous nodules that can interfere with function) are also more common in African Americans. People of Eastern European Jewish ancestry may carry the trait for a fatal neurologic disorder of infancy called Tay-Sachs disease. Lactase deficiency’the absence of an enzyme needed to digest lactose, a sugar found in milk and milk products’is common in people of Hispanic, African, Chinese, Thai, and American Indian origin.
Diabetes is more common among the Hispanic and American Indian populations because of a genetic susceptibility. Hypertension is prevalent among the African American group and some Pacific Islanders. A part of obtaining knowledge for cultural competence is to learn about various disorders that are predominant in a particular group.
APPLICATION of the NURSING PROCESS
Consider the general aspects of the patient’s culture and spiritual orientation before beginning the assessment. What are the social customs of this culture? What are the nonverbal communication patterns? Is eye contact considered polite or rude? Is touch acceptable? What taboos are there regarding touch? What is the appropriate personal space between people when talking in this culture? Begin the introduction in English unless you speak the patient’s language. Obtain an interpreter if one is needed, and then begin the general assessment (Focused Assessment 14-1).
A frequently overlooked area of assessment has to do with spiritual/religious assessment. Observe for the presence of religious or spiritual objects such as a cross, Star of David, Bible, rosary beads, prayer shawl or cap, feathers or amulets, crystals, or books on spirituality. Listen for references to church, temple, or mosque; religious or spiritual activities; or God. See Focused Assessment 14-1 for an assessment of the spiritual dimension of the patient.
Nursing Diagnosis
Some nursing diagnoses specifically related to cultural and spiritual problems or differences might be as follows:
Spiritual distress may be related to feelings of guilt and unworthiness if the patient views illness as punishment for wrongdoing or sin. Other aspects of spiritual distress are feelings of abandonment, anger, despair, or hopelessness as the patient questions the presence of God. Fear of death also causes spiritual distress. The need to seek forgiveness, either from significant people in the patient’s life or from God, is often expressed. Spiritual distress may also be related to a conflict between one’s religious or spiritual beliefs and medical treatment or the inability to attend or actively participate in religious services or spiritual rituals.
Planning
While planning, consider the patient’s family and social support system as well as the belief in culturally traditional health care practices. Write individual expected outcomes for the selected nursing diagnoses. Integrate the patient’s cultural practices related to the illness and treatment into the planned interventions as much as possible. Expected outcomes related to the above nursing diagnoses might be that the patient will:
• Express comfort with the designed plan of care.
• Express needs and opinions through an interpreter.
• Cope with cultural differences of agency routines.
• Develop, reestablish, or continue the spiritual practices that nurture a relationship with God or a higher power.
• Express comfort with her relationship to God and significant others.
• State that she feels at peace.
• Identify and employ spiritual supports: prayer, reading, visits from religious/spiritual representative, engagement in religious/spiritual rituals.
Implementation
Implement care with consideration of the patient’s usual cultural and spiritual practices. Enlist various family members to assist with the patient’s care if that is desirable within the culture (Figure 14-3). Show courtesy and respect for the patient as an individual (Cultural Cues 14-2).

FIGURE 14-3 Observe and respect the way in which extended family members view being involved in the health care decision making.
Developing a therapeutic caring relationship permits patients to express their fears, concerns, and distress and allows the nurse to identify spiritual interventions. One’s own spiritual or religious beliefs must be set aside when they differ from those of the patient. One helpful intervention is to assist the patient to use prayer and meditation to reduce spiritual distress. At the patient’s request, praying with or for the patient can be very comforting. Reading scripture is also calming for many. The Psalms are particularly supportive and are part of the Christian, Jewish, and Islamic traditions.
Religious objects may be very important to the patient. Be sure that items such as a medal or crucifix, rosary beads, Bible, Koran, prayer shawl and cap, or prayer rug are respected and within reach (Figure 14-4). If these must be removed during surgical procedures, assure the patient that they will be restored as soon as possible after the surgery. In some hospitals, special arrangements can be made to keep the item with the patient throughout the surgery or procedure.
Evaluation
Evaluation is based on achievement of the expected outcomes and should not be based on whether treatment is successful from the standpoint of the nurse’s cultural orientation. Transcultural nursing is successful when a mutual understanding and trust develop between the patient and the nurse. Nurses must be sensitive to the cultural and spiritual aspects of their patients in order to give holistic care. Nurses can contribute to a positive health care experience for all people when they seek to learn about the patient as a unique individual and advocate for the rights of patients to choose health care practices that fit with their cultural or spiritual background.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. Culturally competent care is best defined as:
1. generalized care that will not offend any particular cultural group.
2. care delivered by nurses who have a thorough understanding of their own cultural heritage.
3. care adapted to the patient’s cultural beliefs and values.
4. care that only imposes the nurse’s own cultural norms when they will not interfere with the patient’s.
2. Which of the following cultural groups is likely to believe in treating “hot” illnesses with “cold” foods and vice versa?
3. Of the following cultural groups, which is likely to use the services of curanderos?
4. A patient who is Islamic says she cannot sign the surgical consent form without her husband’s consent. You would respond:
1. “Only you, the patient, can sign the surgical consent.”
2. “But, you said he agreed that you should have the surgery.”
3. “I have to ask you to sign this consent form now.”
4. “Call me when your husband gets here and you have talked with him.”
5. An elderly Japanese patient who does not speak English is admitted to the surgical unit after major abdominal surgery, with no family member present. The nurse cannot speak the patient’s language. To assess for pain, the nurse should:
1. look for nonverbal indicators of pain: grimacing, moaning, or restlessness.
2. obtain the services of a translator to devise question-and-answer cards regarding pain.
3. wait for the family to come to ask the patient about pain.
4. use pantomime and gestures to get the patient to indicate his pain level.
6. A person who is an Orthodox Jew may be hesitant to eat hospital food because:
1. hospital food tastes terrible.
2. kosher-prepared foods are served in this hospital.
3. special foods are used to treat specific diseases.
4. separate dishes and utensils are used for meat and milk foods, and there is concern that the hospital may not keep separate sets of dishes and utensils for this purpose.
7. A patient who is Roman Catholic asks to have the priest come to hear her confession and administer communion before she goes to surgery. The priest arrives the evening before the patient is scheduled for the operating room but after normal visiting hours. The nurse should:
1. suggest that the priest return after surgery because the patient has been medicated and is drowsy.
2. provide privacy for the priest to hear confession and administer communion.
3. inform the priest that the patient has not attended confession for a long time.
4. offer to stay with the patient and the priest during the visit to assist the priest.
8. Hindus believe that illness or disease is caused by: (Select all that apply.)
1. a lack of piety and attention to the rituals of Hinduism.
2. misusing the body in some way.
9. A patient says to the nurse, “Is God punishing me with all this pain?” To continue with a spiritual assessment, the nurse could best respond:
1. “God often punishes people for sins. What sins have you committed?”
2. “God doesn’t punish people with pain’you have cancer of the bone that is causing your pain.”
3. “I’ll see if the doctor will order more pain medication. You don’t need to suffer with this pain.”
10. When an Islamic Arab American dies in the hospital, you know: (Select all that apply.)
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
Rosa Souza is a 76-year-old patient of Mexican origin preparing for surgery of an abdominal tumor for which she had previously been treated by a curandero. She is Roman Catholic, wears religious medals, and reads from her Spanish Bible. Her family (husband, two daughters, one son, and several grandchildren) is often present, surrounding the bedside. She will be having surgery in several days.
1. What assessments are important for Mrs. Souza from a cultural or spiritual viewpoint? What questions would you ask?
2. What religious activities might be important for Mrs. Souza.? How can you determine these?
3. Discuss the significance of limiting visitors to allow Mrs. Souza to rest versus accommodating large numbers of family at the bedside.