Promoting Urinary Elimination
Upon completing this chapter, you should be able to:
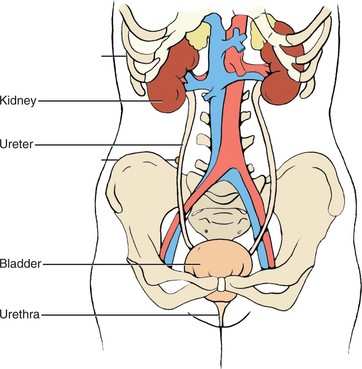
1 Describe the structure and functions of the urinary system.
2 Identify abnormal appearance of a urine specimen.
3 Describe three nursing measures to assist patients to urinate normally.
4 List the purposes and principles of indwelling and intermittent catheterization.
5 Explain the rationale for using a continuous bladder irrigation system.
6 Discuss ways to manage urinary incontinence.
1 Assess a patient’s urinary status.
2 Teach a patient how to obtain a “clean-catch” (midstream) specimen.
3 Perform a urine dipstick test accurately.
4 Assist patients with toileting.
anuria ( , p. 544)
, p. 544)
catheterization ( , p. 554)
, p. 554)
commode chair ( , p. 549)
, p. 549)
condom catheter ( , p. 556)
, p. 556)
Credé’s maneuver ( , p. 554)
, p. 554)
cystitis ( , p. 545)
, p. 545)
dysuria ( , p. 545)
, p. 545)
glycosuria (p. 546)
hematuria ( , p. 546)
, p. 546)
instillation (p. 545)
ketonuria ( , p. 546)
, p. 546)
micturition ( , p. 543)
, p. 543)
nocturia ( , p. 544)
, p. 544)
oliguria ( , p. 545)
, p. 545)
polyuria ( , p. 545)
, p. 545)
proteinuria ( , p. 546)
, p. 546)
pyuria ( , p. 546)
, p. 546)
residual urine ( , p. 544)
, p. 544)
stricture ( , p. 554)
, p. 554)
suprapubic ( , p. 555)
, p. 555)
urinary incontinence ( , p. 544)
, p. 544)
urinary retention ( , p. 544)
, p. 544)
urination ( , p. 544)
, p. 544)
urinometer ( , p. 545)
, p. 545)
urostomy ( , p. 572)
, p. 572)
void ( , p. 542)
, p. 542)
NORMAL URINARY ELIMINATION
The frequency of urination varies. Infants will void (excrete urine) from 5 to 40 times a day. The preschool child may void every 2 hours. The adult voids from 5 to 10 times a day. On average, the adult male voids 300 to 500 mL and the adult female voids 250 mL. There should be at least an hourly urine output of 30 mL. This reflects adequate kidney perfusion. This amounts to 720 mL per 24 hours.
People usually have the urge to void on awakening in the morning, after each meal, at bedtime, and after drinking extra fluid. Urine production is decreased during sleep, and many people can sleep through the night without voiding. Urine is normally sterile, but provides a good medium for the growth of infectious organisms if they are introduced into the bladder.
FACTORS AFFECTING NORMAL URINATION
Urinary elimination is affected by neurologic and muscle development; alterations in spinal cord integrity; the volume of fluid intake; the amount of fluid lost by perspiration, vomiting, or diarrhea; and the amount of antidiuretic hormone (ADH) secreted by the pituitary gland. Anxiety may increase muscle tension and cause a more frequent urge to void. Most people need privacy for urination (expelling urine) to occur freely. Males urinate more easily when standing and females find voiding easier when sitting.
CHARACTERISTICS OF NORMAL URINE
Urine is normally some shade of yellow, with the average being straw colored or amber. The color may darken when the urine is more concentrated. Smoky red or dark brown urine may indicate the presence of blood. Very dark amber urine may be due to the presence of bilirubin. Other color variations may occur from medications the patient is taking or from water-soluble dyes that the patient has consumed in food.
Clarity
Urine should be transparent or only slightly cloudy. Cloudy urine may contain bacteria or large amounts of protein.
Odor
Normal urine smells faintly like ammonia. If the odor is foul, infection may be present. If the odor resembles acetone, ketones are probably present. Other odors may occur depending on what foods the person has eaten or what vitamins have been taken.
Specific Gravity
Specific gravity is the thinness or thickness of the urine. It may be measured by an instrument called the urinometer, an instrument that reads the amount of light the urine absorbs, or by the use of a chemical dipstick. The normal range is 1.010 to 1.030, but conditions such as dehydration and fluid excess may extend the range slightly in either direction.
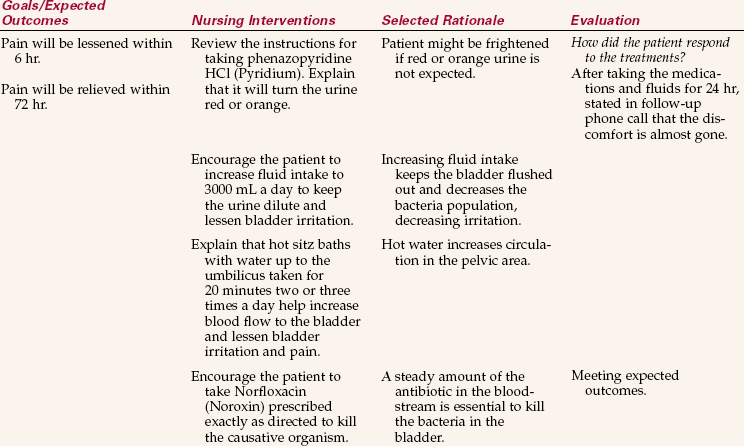
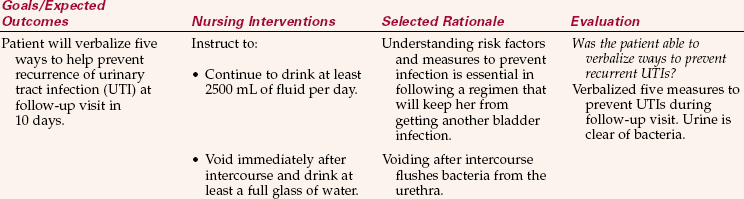
ALTERATIONS IN URINARY ELIMINATION
Alterations in urinary elimination patterns are listed in Box 29-1. A common urinary tract infection is cystitis (inflammation of the bladder). Cystitis may be caused by irritation of highly concentrated urine, pathogenic bacteria, injury, or instillation (putting in a solution) of an irritating substance. A break in aseptic technique when inserting or caring for an indwelling catheter is a frequent cause of cystitis. Escherichia coli is often the bacterium responsible for cystitis, especially in females. Symptoms of cystitis are frequency, urgency, dysuria, (painful urination), burning, malaise, foul-smelling urine, and a slight temperature elevation. Health Promotion Points 29-1 and Complementary & Alternative Therapies 29-1 include useful information to help your patients prevent cystitis.
APPLICATION of the NURSING PROCESS
Obtain a history of the patient’s usual pattern of urinary elimination. Inquire if there are ever incidences of incontinence. Ask if there is a need to urinate frequently, burning when urinating, or a sense of urgency in finding a toilet quickly. Does the patient need to get up to urinate at night frequently? Have there been changes in the appearance of the urine? At what times of the day does the patient usually void? Is the bladder usually completely emptied or is there a need to void again in less than 2 hours? How much fluid is taken in a 24-hour period? Does the patient have a urinary catheter in place? Is there a history of previous urinary problems? What is the patient’s total 24-hour intake and output? Is it normal? Assess the patient’s mobility to determine if it is safe to allow ambulation to the bathroom unassisted. Note when the patient last voided. Each patient should void at least every 8 hours unless an indwelling catheter is in place. If voided amounts are small and intake is normal, gently palpate the bladder to see if it is distended. To do this, feel with the palm of the hand for a bulge indicating a full bladder above the symphysis pubis.
Voided Specimen for Urinalysis.: Inspection of the urine is the next step in the assessment. Various types of specimens may be collected depending on the patient’s symptoms. For a simple voided specimen for urinalysis, ask the patient to void into a clean bedpan, urinal, collection bottle, or plastic “hat” collection device placed inside the front of the toilet (Figure 29-3). Provide privacy for the patient. Explain to the female how to hold the urine bottle or cup so that it surrounds the urethra. She should stand in a slightly squatting position, or sit over the toilet and hold the collection container steady to catch the urine as she voids. Explain to both men and women that only about 1½ inches of urine is needed. It is not necessary to fill the container. If the specimen is to go to the laboratory, transfer it to the specimen container, label it properly, and send it to the laboratory within 5 to 10 minutes. Urine that stands for 15 minutes or more changes characteristics, and the urinalysis will not be accurate. Box 29-2 shows some common abnormalities found by urinalysis.

FIGURE 29-3 Urine collection devices: fracture pan (left front), standard bedpan (right front), urinal (left rear), and in-toilet “hat” (right rear).
Dipstick tests, containing chemical reagents, are routinely performed in most physicians’ offices and outpatient clinics. They may test for a variety of components, including glucose, ketones, protein, blood, specific gravity, pH, nitrate, bilirubin, and leukocytes. If a dipstick test is to be performed, follow the directions on the side of the bottle of test strips. Exact timing for checking each component is essential for accuracy of the result (Figure 29-4).
Midstream (Clean-Catch) Urine Specimen.: This procedure is used to obtain a specimen for a culture and sensitivity test when a urinary tract infection is suspected. The purpose is to obtain a specimen that is relatively free from external contamination (Patient Teaching 29-1).
Specimen from an Indwelling Catheter.: A specimen may be obtained from the self-sealing port of an indwelling catheter system or from the lumen of a latex catheter (Steps 29-1, Figure 29-5).
Sterile Catheterized Specimen.: When a sterile specimen is ordered and the patient does not have an indwelling catheter in place, the patient is catheterized with a straight catheter (no balloon) that may be attached to a small collection bag, or the urine may be collected by placing the distal end of the catheter into a sterile specimen container.
24-Hour Urine Specimen.: All urine voided during the 24-hour period is collected in the designated container and stored on ice if necessary. The laboratory analysis is done to determine the amount of a specified chemical that is excreted through the urine in a 24-hour period. If some urine is accidentally thrown out, the test is invalid and must be started over. A sign should be posted over the bed and over the toilet indicating that all urine is to be saved. The patient’s bladder should be empty at the beginning and at the conclusion of the test. The patient empties the bladder just before beginning the collection and the urine is discarded. At the ending time, the patient voids and the urine is added to the collection container. Check with the laboratory before beginning the test to be certain the right container with preservative is on hand and to see whether the specimen must be kept cold during the 24-hour period (see Chapter 24).
Urinary Collection Bag.: This device is used to obtain a urine specimen from an infant or toddler. It attaches to the skin by an adhesive backing and is placed so that it surrounds the genitals. When sufficient urine has collected in the bag for a specimen, the bag is carefully removed and the urine is poured into a specimen container.
Nursing Diagnosis
Nursing diagnoses for patients with problems of urinary elimination are as follows:
• Urinary elimination, impaired
• Urinary incontinence (urge, stress, total, reflex, overflow, or functional)
• Injury, risk for (to kidney from urine blockage)
• Self-care deficit, toileting
The specific defining characteristics are added to the diagnosis stem for the individual patient.
Planning
The data gathered during assessment will give you the information needed to plan time to assist the patient needing help with toileting. If a patient has been prone to urinary tract infections (UTIs), you can specifically plan to increase fluids, unless they are contraindicated, at set intervals and to reinforce patient teaching regarding ways to prevent further UTIs. You should plan for time to collect any needed urine specimens, and should tell the patient that one will be needed sufficiently ahead of time for the patient to be able to produce the urine. When you are planning care for your patient, remember to be culturally sensitive in helping your patient to achieve toileting needs (Cultural Cues 29-1).
For the patient prone to urinary retention, you can plan to note the amount of each voiding and to palpate the bladder for distention if output falls below normal.
If the patient is in need of assistive devices for toileting, place a bedpan and/or urinal in the bedside stand or obtain an order for the device needed. Discharge planning includes ensuring that arrangements are made before the patient goes home for devices such as grab bars by the toilet, a commode chair (chair with a container inserted to catch urine or feces), or a raised toilet seat (Figure 29-6).
Keep in mind that urinary elimination is usually an independent function and it is embarrassing to most people to have assistance. The insertion of a catheter causes a disturbance in body image even if the catheteris temporary. Plan to show extra sensitivity when caring for these patients. Some examples of expected outcomes can be found in Nursing Care Plan 29-1.
Implementation
Assisting patients with urinary elimination is a basic nursing function. Patients who can ambulate can be assisted to the bathroom to use the toilet. Others may use a commode chair. This is a chair with an opening in the seat and a large receptacle beneath it. It is usually placed by the bedside or a short distance away. The patient is transferred from the bed to the commode and then back again. The receptacle is emptied after each use. The commode chair is used for bowel movements as well as urination. Another assistive device is a raised toilet seat. This is usually a frame device that fits over the toilet bowl and has a toilet seat attached to it at a higher point than is usual. Patients who have difficulty with hip flexion or who have had a hip replacement need to use such a device.
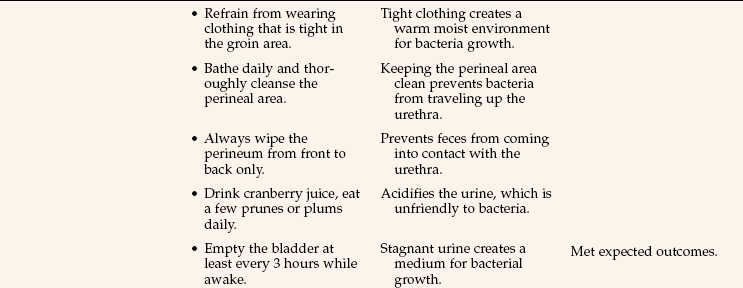
Patients on bed rest are provided with a bedpan for elimination. It is made of metal or plastic (see Figure 29-3). Each patient has an individual bedpan stored in the bedside stand during the hospital stay. The female uses it for both urine and bowel elimination, whereas the male uses it for bowel elimination only. The bedpan should be covered if it must be carried outside the patient’s room. Paper towels or a small hand towel may be used.
The fracture pan (see Figure 29-3) is used when patients are unable to sit on a regular-sized bedpan. It is smaller in surface area and height than the regular bedpan. It is used for patients with musculoskeletal problems. The flat end with the wide rim is placed under the patient’s buttocks. It is placed under the patient by separating the patient’s legs and slipping the pan under the buttocks. A little powder on the flat rim helps when the patient is unable to raise the hips to assist. The greater depth at the front of the pan helps keep the urine from spilling on the bed. Remove the pan carefully so that urine is not spilled on the bed. Skill 29-1 presents instructions on how to place and remove a bedpan.
For the ambulatory patient who needs urinary output recorded, place a plastic “hat” device toward the front of the toilet bowel between the bowl and the seat. The inside is graduated so that you can record the amount of output after each voiding and then empty, rinse, and replace the container so that it is ready for the next voiding.
Whatever method is used for urinary elimination, provide an opportunity for hand hygiene (Cultural Cues 29-2). The patient is made comfortable with side rails replaced and the call bell within reach.
Assisting with Use of a Urinal: When a male is unable to use a urinal unassisted, the nurse helps. If the patient can stand by the side of the bed, this is the most desirable position. The male urinal is a plastic or metal bottle with a round neck, a handle, rectangular sides, and a flat base (see Figure 29-3). It may or may not have a lid. The urinal can be used by the patient who is confined to bed, in any one of four positions: lying supine, lying on either the right or the left side, or in Fowler’s position. Provide privacy by closing the door or the privacy curtain, don gloves, lower the side rail, and ask the patient to spread his legs. Hold the urinal by the handle and direct it at an angle between the legs so that the flat side rests on the bed. Lift the penis and place it well within the urinal. After urination, carefully remove the urinal and empty it immediately, measuring and recording the urine voided. Be sure the penis is dry. Clean the urinal and return it to the proper place.
Assisting a Patient to Urinate: Patients often have difficulty urinating after surgery and anesthesia, childbirth, or other trauma to the perineum. All efforts are made to help the patient void naturally before resorting to catheterization (insertion of a tube into the bladder). Some methods of helping patients initiate the voiding reflex are as follows:
• Run water in a nearby sink so the patient hears the sound.
• Have the patient deep breathe, relax, and visualize a peaceful place with a bubbling brook.
• Assist the male to stand by the side of the bed (with a physician’s order).
• Have the female blow through a straw in a glass of water, causing bubbling, while sitting on the toilet or bedpan.
• Pour warm water over the perineum while the patient attempts to void. Measure the water volume so you can subtract it from the total volume to determine how much the patient voided.
• With a physician’s order, gently but firmly use Cred é’s maneuver over the bladder (massage from top of bladder to bottom by starting above the pubic bone and rocking the palm of the hand steadily downward).
• Obtain an order for a sitz bath and have the patient sit in the warm water. Encourage the patient to void while in the bath. Cleanse the perineum afterward.
When a patient cannot empty the bladder naturally for a period longer than 8 hours, a bladder scan may be performed using an ultrasound machine designed for that purpose (Figure 29-7). If the bladder contains a large amount of urine, an order is obtained for catheterization. The bladder scan can also disclose the amount of residual urine in the bladder after a patient voids. This tells the physician whether the bladder is emptying sufficiently. If needed, the physician orders either a straight “in-and-out” catheterization or the insertion of an indwelling (Foley) catheter. Other reasons for catheterization include
• Preparing a patient for a surgical procedure or obstetric delivery
• Keeping the genitalia and perineum clean after obstetric or surgical procedures
• Dilating a urethral stricture (narrowed lumen)
• Splinting the urethra following surgery on the urethra
• Measuring the amount of residual urine in the bladder (this is also accomplished by a using a portable ultrasound bladder scanner)
• Monitoring hourly urine output or to obtain exact measurements of total output
• Performing irrigation or instillation and drainage of chemotherapeutic solutions into the bladder
• Assisting with the re-toning of the bladder muscle after surgery on the bladder
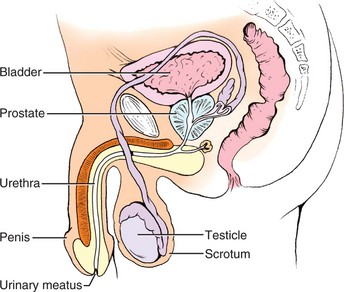
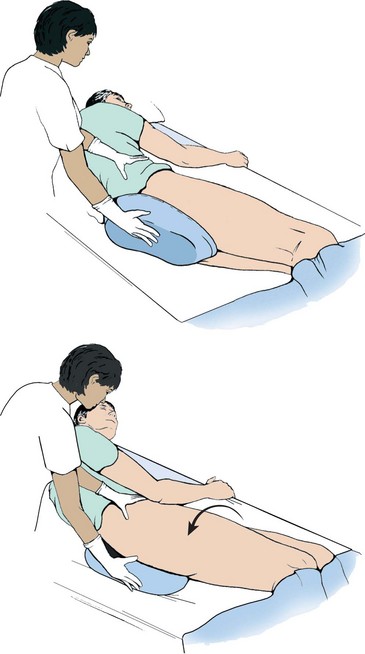
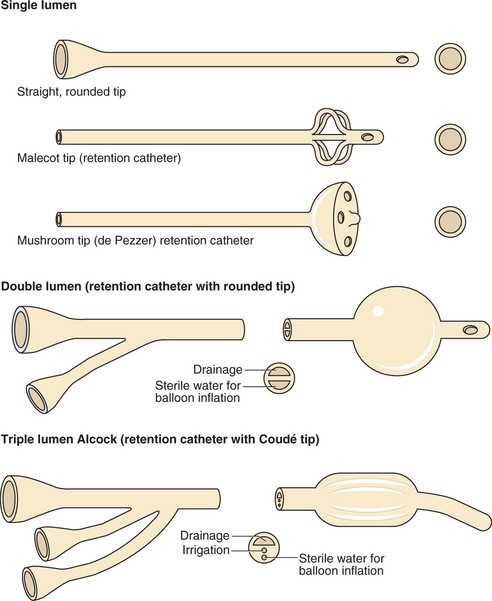
Types of Urinary Catheters: Catheters come in several sizes and shapes and are either rubber or plastic. Some are Teflon coated. They are sized by the French system, with the average size used for an adult female being 14 to 16 Fr. and for the male 18 to 20 Fr. (Figure 29-8). A straight catheter (e.g., the Robinson) is used to relieve retention when a patient is temporarily unable to void, or to obtain a sterile specimen. The Foley is the most common indwelling catheter, the type that remains in the bladder for an extended period. It is sometimes referred to as a “retention” catheter because it is retained in the bladder. A Foley catheter has two lumens, one to drain urine and one for inflation of the balloon that holds the catheter in the bladder to prevent it from slipping out the urethra. The balloon usually holds 5 to 10 mL of sterile water. This catheter is used for continuous drainage, particularly postoperatively, and can also be used for suprapubic (above the pubic bone) drainage.
The Coudé catheter, a variation of the Robinson catheter, is curved and has a rounded or bulbous tip that is easier to insert into the male urethra when the prostate is enlarged.
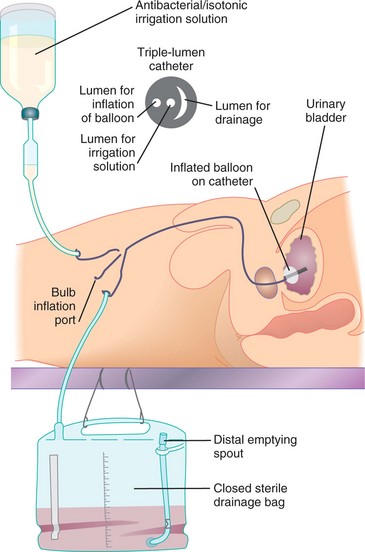
The Alcock catheter, used for continuous bladder irrigation following prostate or bladder surgery, is a Foley-type catheter with two eyes. It has three lumens, one for urine drainage, one for inflation of the balloon, and one for the instillation of the irrigation fluid.
The de Pezzer catheter, which has a tip shaped like a mushroom, is used for suprapubic drainage. The Malecot catheter, which has a large single tube with a tip shaped like wings, is often used as a nephrostomy tube; it is placed into the pelvis of the kidney.
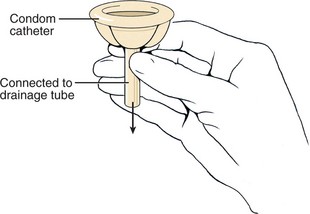
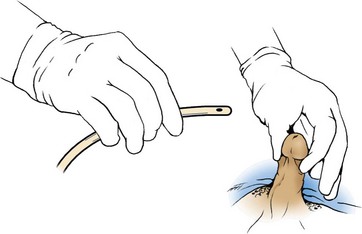
A condom catheter consists of a condom with a tube attached to the distal end that is attached to a drainage bag. It is used to provide continuous urine drainage for the male in a noninvasive manner. It is applied to the penis and, since it is noninvasive, it is less likely to predispose to urinary tract infection.
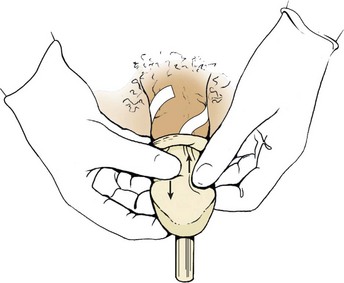
When applying a condom catheter, care must be taken not to apply the sheath too tightly. This can cause a decreased blood flow to the penis. The sheath must be checked frequently for signs of moisture accumulation as this can lead to skin breakdown. Unless applied carefully and correctly, a condom catheter will leak. Read the directions that come with the specific catheter and follow the steps in Skill 29-2.
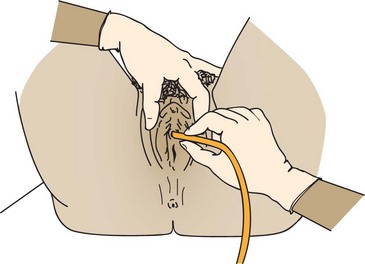
Performing Catheterization: Explain the procedure and elicit the patient’s cooperation (Communication Cues 29-1). Sterile equipment and strict aseptic technique must be used to catheterize a patient. Any break in aseptic technique causing contamination must be corrected before continuing with the procedure. Each catheter kit is suitable for catheterizing a male or female. The procedure for male and female catheterization is similar except for variations in the positioning, draping, and cleansing of the urinary meatus. In the male, the catheter is inserted farther (about 7 to 8 inches). When inserting a catheter, gently insert until you see the urine flow and then insert 1 to 2 more inches. This will ensure the balloon will not damage the urethra during inflation. Skill 29-3 and Skill 29-4 (p. 563) give the steps for catheterization of the female patient and the male patient, respectively. The Foley catheter system should be maintained as a closed system to lessen the risk of infection. The procedure for inserting a straight or Foley catheter is similar. The difference is that with the Foley, the balloon must be inflated and there is a connecting tube to a drainage bag. Information on straight catheterization is presented in the Special Considerations at the end of Skills 29-3 and 29-4.
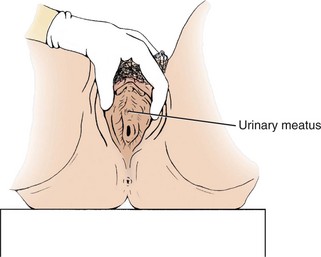
It is a good idea to identify the urethral meatus in the female before beginning the procedure. This may be done before gathering the equipment or just before opening the sterile catheterization kit. When the patient is in the dorsal recumbent position and draped, put on exam gloves, use adequate light, and spread the labia minora to reveal the inner anatomy. The urethral meatus is usually slightly above the vaginal opening and often looks like a dimple or fold in the mucous membrane.
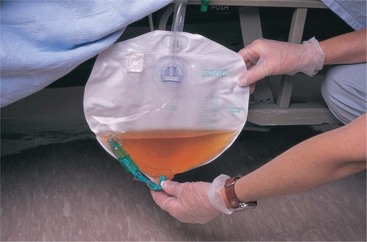
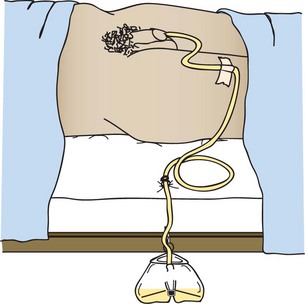
The catheter is taped to the thigh of the female, preferably the inner thigh, and to the top of the thigh or the abdomen of the male. Allow a little slack in the catheter before taping it to the skin so that there is not constant tension on the internal sphincter by the balloon. All patients with an indwelling catheter are placed on intake and output recording.
The perineum is cleaned during the daily bath, and the external portion of the catheter is washed at that time if it is soiled. No special cleansing of the urinary meatus is recommended. Box 29-3 provides suggestions for caring for the patient with an indwelling catheter.
Removal of an Indwelling (Foley) Catheter: Removal of an indwelling catheter requires a physician’s order. The patient is kept on intake and output recording for 12 to 24 hours after catheter removal to ensure that the bladder is draining adequately. Steps 29-2 give the steps and rationale for this removal.
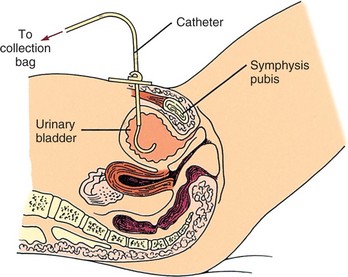
The Suprapubic Catheter: A suprapubic catheter may be used for urine drainage following gynecologic and bladder surgery. It is inserted through the abdominal wall by the surgeon. The suprapubic catheter is sutured to the skin at the time of insertion (Figure 29-10).
Intermittent Self-Catheterization: Intermittent self-catheterization is used for patients who regularly experience incontinence or urinary retention. In accordance with 2009 National Patient Safety Goals, patients should be taught and encouraged to participate in their own care (Patient Teaching 29-2). Often these patients have a spinal cord problem that prevents proper function of the nerves that control the bladder and urinary sphincters. This procedure, most often performed outside of the hospital, is a “clean” rather than a “sterile” procedure and does not require the use of a sterile catheter.
Bladder Irrigation or Instillation: Irrigation or instillation is performed on patients with indwelling catheters to
• Wash out residual urine or sediment from the bladder
• Remove clots and stop oozing of blood after prostate or bladder surgery
• Soothe irritated bladder tissues and promote healing
• Ensure that the lumen of the indwelling catheter is open and draining
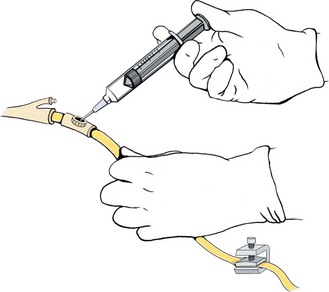
Bladder irrigation or instillation is best done via the injection port on the drainage tubing. The tubing is clamped distal to the port and the medication or solution is introduced via a needle placed in the port. The solution is then allowed to drain. If medication is instilled, the catheter is clamped for a designated period of time before unclamping it so drainage can occur. For irrigation, continue instilling 30 to 50 mL of solution, depending on the medical order, and allow it to drain until the return is clear (Skill 29-5).
Continuous irrigation is performed after prostate or bladder surgery via the “three-way” indwelling (Foley) catheter system where the irrigation solution is hooked up to the irrigation port of the catheter. The solution container is positioned on an intravenous (IV) pole. Using sterile technique, solution is run through the tubing to remove air and then the tubing is connected to the irrigation port of the catheter. When using a three-way catheter consult the package instructions to determine which port should be attached to the irrigating solution and which port is designated for the drainage bag connection. (Note: The inner lumen with the largest diameter should be used for the drainage because of the potential for clots or debris that are washed from the bladder.) The third port is for inflating the “balloon” and will appear similar to a standard Foley catheter port. The order is checked for the flow rate. Generally, the irrigation solution is set to flow just fast enough to prevent clots from forming in the bladder (Figure 29-11). The return should be pink to light red. The irrigation solution container is changed at least every 24 hours.
When the drainage system must be opened for irrigation, strict asepsis must be maintained. Take special care not to contaminate the end of the drainage tubing or the end of the catheter.
The amount of solution to be introduced is ordered by the physician. If there is no specific amount ordered, follow agency procedure. All irrigation fluid is subtracted from the amount of output.
Assisting the Patient Who Is Incontinent: There are at least six types of incontinence: urge, stress, total, overflow, functional, and reflex (Box 29-4). The effect on the patient is much the same. The incontinent patient suffers a body image disturbance over the loss of a normal function. There is risk of skin breakdown from moisture and waste products in the urine, as well as worry over being wet and smelling of urine. There is also the risk of infection because urine is a good medium for bacterial growth. Urinary incontinence may be temporary or it may be permanent.
Management and treatment of incontinence is complex; some patients may have more than one form of incontinence. For example, stress incontinence is often accompanied by urge incontinence. For some patients, better and quicker assistance to the toilet will resolve the problem. For others, continence training may help(Steps 29-3) (Assignment Considerations 29-1). Regularly performing Kegel exercises may greatly reduce or stop incontinence in patients (Patient Teaching 29-3). Several surgical procedures can be used for patients who choose to correct a specific physiologic problem. For those incontinent patients for whom there is no cure, such as people with neurologic damage that prevents sphincter control, you must help the patient stay dry and clean and preserve his dignity (Legal & Ethical Considerations 29-1). Condom catheters are often used for the incontinent male. Adult briefs containing material similar to diapers are used for females. Absorbent pads similar to sanitary napkins may be used for either sex.
Urinary Diversion Care: Urinary diversion is necessary when the bladder must be removed or bypassed for some reason. When urinary diversion is performed, one or both ureters are implanted into the abdominal wall, the bowel, or a portion of bowel that forms a pouch. When the ureter exits on the abdominal wall, discharging urine through the opening, it is called a urostomy (opening through which urine drains). The nurse is concerned with collection of the draining urine and care of the skin around the urostomy. Unless the urostomy is constructed with an internal pouch and valve, urine drains constantly. This presents a challenge when changing the urostomy bag. Place a tampon in the opening while you clean the skin and prepare the clean urostomy bag. The urostomy with an internal pouch is emptied by the insertion of a catheter. Urine contains ammonia, which is very irritating to the skin, and a skin barrier is applied before attaching the collection appliance. Because bowel ostomies are more common than urostomies, particulars of skin care and changing the ostomy bag (appliance) are presented in Chapter 30.
Evaluation
Review the expected outcomes written during the planning phase in order to properly evaluate the effectiveness of interventions for the patient’s problems. Determining whether the patient can urinate normally without urgency, dysuria, or frequency, plus a urinalysis performed after treatment is complete or when a Foley catheter is removed, indicates whether infection has been eliminated or avoided. Noting intake and output records and comparing them from day to day indicates whether fluid intake is sufficient and output is adequate. Noting the condition of skin in the perineal area of the patient who has been incontinent provides information as to whether measures to protect the skin are sufficient. Evidence that the patient has had fewer episodes of incontinence over a period of days indicates that the continence training program is helpful. Checking the appearance of the urine for normal characteristics is another evaluation tool.
Obtain feedback for all patient teaching performed. Can the patient tell you measures to take to prevent urinary tract infection? Can the patient needing intermittent catheterization self-catheterize successfully? Does the patient, or the family member of the patient at home, know how to care for the catheter and empty the collection bag properly? Is the patient in the long-term care facility who has functional incontinence now receiving the needed assistance? Nursing Care Plan 29-1 provides some specific examples of evaluative statements for expected outcomes on the plan.
Documentation: When a patient voids normally and without problems in adequate amounts, include a short note of “voiding quantity sufficient.” If a patient has been having a problem with some aspect of urinary elimination, the number of voidings per day is charted along with the urinary output and the appearance of the urine. When a patient is catheterized, a note is made regarding the appearance of the urine returned from the catheter and any problems encountered during the procedure. The size and type of catheter are charted and the amount of water instilled in the Foley balloon is noted. A description of the urine should be documented on the computer or chart flow sheet or nurse’s notes at least once a day when a patient has an indwelling catheter, along with assessment data that indicate no urinary tract infection is present (unless one was present before the catheter was inserted).
For the incontinent patient, a note regarding the number of times the patient voided normally is made along with a description of the time and circumstances of any incontinent voidings. The assessment of the skin in the perineal area is charted at least once a shift.
Documentation of all patient teaching is done in the nurse’s notes or on a patient education flow sheet. All diagnostic tests and specimens obtained and sent to the lab are noted on the daily activity flow sheet. Urostomy care is documented on the flow sheet as well. A note regarding the condition of the stoma and the surrounding skin should be placed in the nurse’s notes.
If a bladder irrigation or instillation is performed, it is documented in the nurse’s notes stating the amount of solution instilled, whether aseptic technique was maintained, the time the fluid remained in the bladder, the amount and description of the outflow, and any problems encountered. When an indwelling catheter is removed, document the time, date, and amount of urine in the drainage bag. Add a note as to the time by which the patient should void (within 8 hours). Document any problems the patient has voiding after catheter removal.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. A patient underwent a hernia repair in the same-day surgery department. He is awake and alert, but has not been able to void since he returned from surgery 4 hours ago. He cannot be discharged until he voids. He has had 1000 mL of IV fluid. Which intervention would be the most likely to help this patient to urinate?
1. Give more liquids by mouth.
3. Assist him to stand by the side of the bed to void.
4. Call the physician and obtain an order for a Foley catheter.
2. The physician prescribes phenazopyridine HCl (Pyridium) for a patient with cystitis. What is a correct teaching point for this medication?
1. The medication helps to flush the bladder.
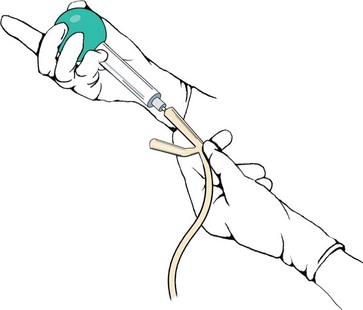
2. The medication acidifies the urine.
3. The nurse is obtaining a urine specimen for a patient who has an existing Foley catheter. Below are the steps for the procedure. Place these steps (1 though 6) in the correct order.
_______1. Wipe the aspiration port of the drainage tubing with an alcohol pad.
_______2. Aspirate 3 mL of urine by gently pulling back on the plunger.
_______3. Clamp the catheter below the aspiration port.
_______4. Empty the syringe into the sterile container; needle should not touch the container.
_______5. Close and label the container. Unclamp the catheter.
_______6. Insert a 25-gauge needle attached to a syringe into the aspiration port.
4. Which statement by the patient indicates a need for additional patient teaching about cystitis?
1. “I should increase fluids, including orange and grapefruit juice.”
2. “I should avoid use of bubble bath and feminine hygiene sprays.”
5. The nurse has just collected a midstream urine specimen from a patient. Which urine characteristic would be of the greatest concern?
6. A patient in a long-term facility has a retention catheter in place. The nurse identifies Risk for infection as a nursing diagnosis. Which urine abnormality supports the choice of this diagnosis?
7. A patient is admitted with urinary retention. There is an order to insert a Foley catheter into his bladder. He attempts to void and passes 100 mL of urine. Before catheterization, the nurse should:
1. use a condom catheter with a leg bag.
2. wait 2 hours and have him try to void again.
3. have him drink 2 to 3 glasses of water.
4. perform a bladder scan to determine amount of urine retained.
8. The nurse is catheterizing a male patient, who is confused. He moves several times during the procedure despite repeated verbal instructions to remain calm, quiet, and still. Which nursing diagnosis is the priority related to the presence of the catheter for this patient?
9. The nurse is catheterizing a male patient. Resistance is met. The nurse should:
1. apply more pressure with a twisting motion to insert the catheter.
2. obtain a new sterile kit and try again with a sterile Coudé catheter.
3. ask him to take a deep breath and slowly exhale as the catheter is inserted.
4. discontinue the procedure and try again after the patient relaxes.
10. A fracture pan is generally used for a patient who has:
11. Which urine characteristic suggests that the patient might be dehydrated?
12. The patient complains of urinary frequency, urgency, and burning. Which nursing action should be done first?
1. Obtain an order for a urinalysis.
2. Check the patient’s temperature.
13. The purpose of clamping the catheter tubing when irrigating the bladder is to:
1. prevent urine from draining into the bag.
2. hold the solution in the bladder.
14. Which of the following statements by the patient indicates that she understands how to perform the clean-catch method for a urine specimen?
1. “I should clean my genital area first, pee into the cup, and then re-clean myself.”
2. “I should fill the cup completely and save it in the refrigerator.”
3. “I should keep the contents of the kit sterile at all times.”
4. “I should clean myself first, pee a little into the toilet, and then pee into the cup.”
15. The patient had a resection of the prostate gland yesterday and has a three-way catheter for continuous irrigation. The draining urine is very red. This means that the nurse needs to:
1. notify the physician immediately.
2. increase the rate of flow of the irrigation solution.
16. A 24-hour urine specimen is ordered for a patient. The UAP discards some of the urine that should have been saved. Which is the most appropriate nursing action?
1. Verbally reprimand the nursing assistant.
2. Make a note to extend the urine collection period.
17. A nurse is caring for a patient who is incontinent. What is the priority action?