Management of Temporomandibular Disorders
Patients frequently consult a dentist because of pain or dysfunction in the temporomandibular region. The most common causes of temporomandibular disorders (TMDs) are muscular disorders, which are commonly referred to as myofascial pain and dysfunction. These muscular disorders are generally managed with a variety of reversible nonsurgical treatment methods.
Other causes of temporomandibular pain or dysfunction originate primarily within the temporomandibular joint (TMJ). These causes include internal derangement, osteoarthritis, rheumatoid arthritis, chronic recurrent dislocation, ankylosis, neoplasia, and infection. Although most of these disorders respond to nonsurgical therapy, some patients may eventually require surgical treatment. If a successful result is to be achieved, management of these patients requires a coordinated plan between the general dentist, oral and maxillofacial surgeon, and other health care providers.
EVALUATION
The evaluation of the patient with temporomandibular pain, dysfunction, or both is like that in any other diagnostic workup. This evaluation should include a thorough history, a physical examination of the masticatory system, and problem-focused TMJ radiography.
Interview
The patient’s history may be the most important part of the evaluation because it furnishes clues for the diagnosis. The history begins with the chief complaint, which is a statement of the patient’s reasons for seeking consultation or treatment. The history of the present illness should be comprehensive, including an accurate description of the patient’s symptoms, chronology of the symptoms, description of how the problem affects the patient and information about any previous treatments (including the patient’s response to those treatments). To have patients complete a general questionnaire is often useful to help provide information about the history of their problem. The use of a visual analog pain scale may also help obtain an understanding of the patient’s perception of the severity of their pain.
Examination
The physical examination consists of an evaluation of the entire masticatory system. The head and neck should be inspected for soft tissue asymmetry or evidence of muscular hypertrophy. The patient should be observed for signs of jaw clenching or other habits. The masticatory muscles should be examined systematically. The muscles should be palpated for the presence of tenderness, fasciculations, spasm, or trigger points (Fig. 30-1).
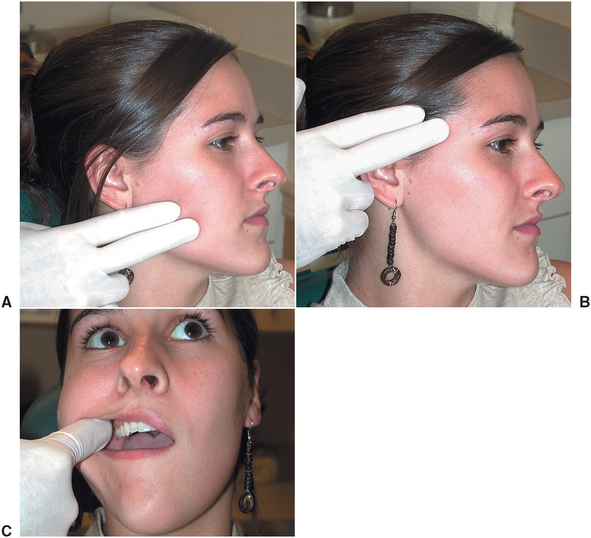
FIGURE 30-1 Systematic evaluation of muscles of mastication. A, Palpation of masseter muscle. B, Palpation of temporalis muscle. C, Palpation of temporalis tendon attachment on coronoid process and ascending ramus.
The TMJs are examined for tenderness and noise (Fig. 30-2). The location of the joint tenderness (e.g., lateral or posterior) should be noted. If the joint is more painful during different areas of the opening cycle or with different types of functions, this should be recorded. The most common forms of joint noise are clicking (a distinct sound) and crepitus (i.e., scraping or grating sounds). Many joint sounds can be easily heard without special instrumentation or can be felt during palpation of the joint; however, in some cases auscultation with a stethoscope may allow less obvious joint sounds, such as mild crepitus, to be appreciated.
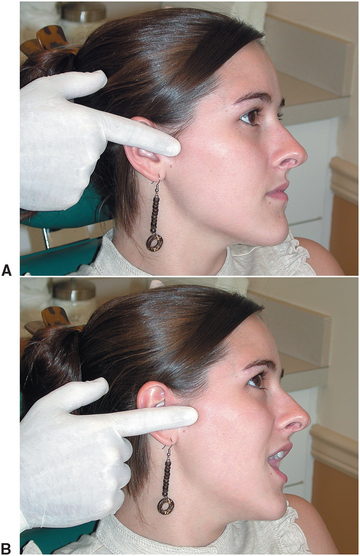
FIGURE 30-2 Evaluation of temporomandibular joint for tenderness and noise. Joint is palpated laterally in closed position (A) and open position (B).
The mandibular range of motion should be determined. Normal range of movement of an adult’s mandible is about 45 mm vertically (i.e., interincisally) and 10 mm protrusively and laterally (Fig. 30-3). The normal movement is straight and symmetric. In some cases, tenderness in the joint or muscle areas may prevent opening. The clinician should attempt to ascertain not only the painless voluntary opening but also the maximum opening that can be achieved with gentle digital pressure. In some cases the patient may appear to have a mechanical obstruction in the joint causing limited opening but with gentle pressure may actually be able to achieve near normal opening. This may suggest muscular rather than intracapsular problems.
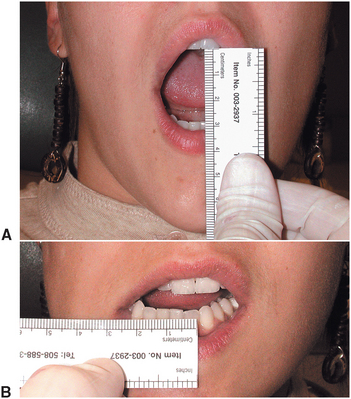
FIGURE 30-3 Measurement of range of jaw motion. A, Maximum voluntary vertical opening. B, Evaluation of lateral excursive movement (should be approximately 10 mm). Protrusive movements should be similar to excursion.
The dental evaluation is also important. Odontogenic sources of pain should be eliminated. The teeth should be examined for wear facets, soreness, and mobility, which may be evidence of bruxism. Although the significance of occlusal abnormalities is controversial, the occlusal relationship should be evaluated and documented. Missing teeth should be noted, and dental and skeletal classification should be determined. The clinician should note any centric relation and centric occlusion discrepancy or significant posturing by the patient. The examination findings can be summarized on a TMD evaluation form and included in the patient’s chart. In many cases a more detailed chart note may be necessary to document adequately all of the history and examination findings described previously.
Radiographic Evaluation
Radiographs of the TMJ are helpful in the diagnosis of intraarticular, osseous, and soft tissue pathologic conditions. The use of radiographs in the evaluation of the patient with TMD should be based on the patient’s signs and symptoms instead of routinely ordering a standard set of radiographs. In many cases the panoramic radiograph provides adequate information as a screening radiograph in evaluation of TMD. A variety of other radiographic techniques are available that may provide useful information in certain cases.
Panoramic Radiography
One of the best overall radiographs for screening evaluation of the TMJs is the panoramic radiograph. This technique allows visualization of both TMJs on the same film. Because a panoramic technique provides a tomographic-type view of the TMJ, this can frequently provide a good assessment of the bony anatomy of the articulating surfaces of the mandibular condyle and glenoid fossa (Fig. 30-4); and other areas, such as the coronoid process, can also be visualized.1 Many machines are equipped to provide special views of the mandible, focusing primarily on the area of the TMJs. These radiographs can often be completed in the open and closed position.
Tomograms
The tomographic technique allows a more detailed view of the TMJ.2 This technique allows radiographic sectioning of the joint at different levels of the condyle and fossa complex, which provides individual views visualizing the joint in “slices” from the medial to the lateral pole. These views eliminate bony superimposition and overlap and provide a relatively clear picture of the bony anatomy of the joint.
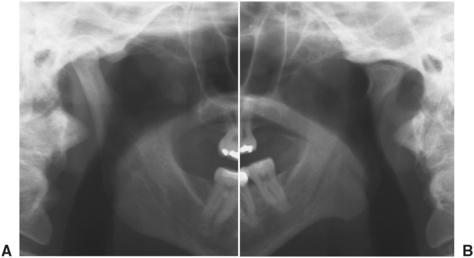
Temporomandibular Joint Arthrography
This imaging method was the first technique available that allowed visualization (indirect) of the intraarticular disk. Arthrography involves the injection of contrast material into the inferior or superior spaces of a joint, after which the joint is radiographed.3 Evaluation of the configuration of the dye in the joint spaces allows evaluation of the position and morphology of the articular disk (Fig. 30-5). This technique also demonstrates the presence of perforations and adhesions of the disk or its attachments. With the availability of more advanced, less invasive techniques, arthrography is rarely used.
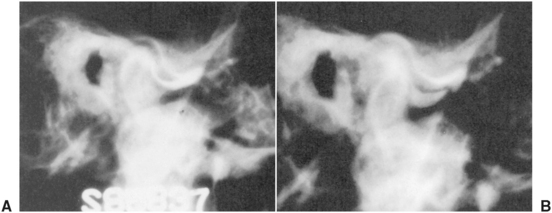
FIGURE 30-5 Arthrogram shows dye in inferior and superior joint spaces. Anatomy and location of disk is indirectly interpreted from dye pattern observed after injection of joint spaces above and below disk. This arthrogram demonstrates anterior disk displacement without reduction. A, Closed position. B, Open position.
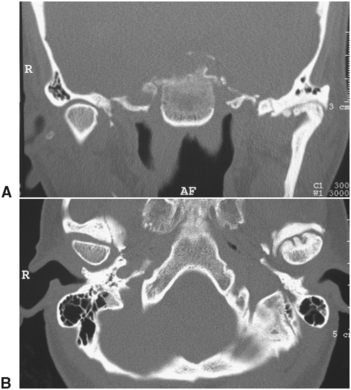
Computed Tomography
Computed tomography (CT) provides a combination of tomographic views of the joint, combined with computer enhancement of hard and soft tissue images.4 This technique allows evaluation of a variety of hard and soft tissue pathologic conditions in the joint. CT images provide the most accurate radiographic assessment of the bony components of the joint (Fig. 30-6). CT scan reconstruction capabilities allow images obtained in one plane of space to be reconstructed so that the images can be evaluated from a different view. Thus evaluation of the joint from a variety of perspectives can be made from a single radiation exposure.
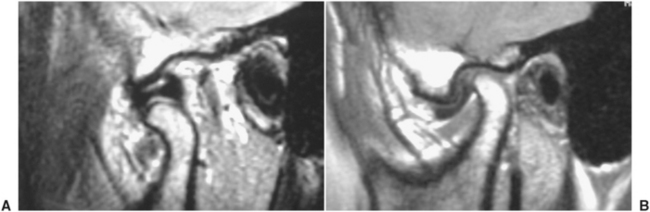
Magnetic Resonance Imaging
The most effective diagnostic imaging technique to evaluate TMJ soft tissues is magnetic resonance imaging (MRI; Fig. 30-7).5 This technique allows excellent images of intraarticular soft tissue, making MRI a valuable technique for evaluating disk morphology and position. MRI images can be obtained showing dynamic joint function in a cinematic fashion, providing valuable information about the anatomic components of the joint during function. The fact that this technique does not use ionizing radiation is a significant advantage.
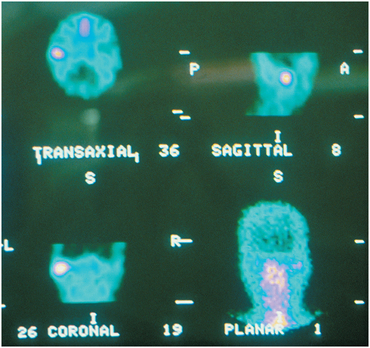
Nuclear Imaging
Nuclear medicine studies involve intravenous injection of technetium-99, a γ-emitting isotope that is concentrated in areas of active bone metabolism. Approximately 3 hours after injection of the isotope, images are obtained using a gamma camera. Single-photon emission computerized tomography images can then be used to determine active areas of bone metabolism (Fig. 30-8).6 Although this technique is extremely sensitive, the information obtained may be difficult to interpret. Because bone changes, such as degeneration, may appear identical to repair or regeneration, this technique must be evaluated cautiously and in combination with clinical findings.
Psychological Evaluation
Many patients with temporomandibular pain and dysfunction of long-standing duration develop manifestations of chronic pain syndrome behavior. This complex may include gross exaggeration of symptoms and clinical depression.7,8 The comorbidity of psychiatric illness and temporomandibular dysfunction can be as high as 10% to 20% of patients seeking treatment.9 A third of these patients is suffering from depression at the time on initial presentation, whereas more than two thirds have had a severe depressive episode in their history.10 Psychiatric disorders may elicit somatic components through parafunctional habits resulting in dystonia and myalgia, and individuals with chronic pain commonly have a higher incidence of concomitant anxiety disorders.11–13 Behavioral changes associated with pain and dysfunction can be elicited in the history through questions regarding functional limitation that results from the patient’s symptoms.14 If the functional limitation appears to be excessive compared with the patient’s clinical signs or the patient appears to be clinically depressed, further psychological evaluation may be warranted.15
CLASSIFICATION OF TEMPOROMANDIBULAR DISORDERS
Myofascial pain and dysfunction (MPD) is the most common cause of masticatory pain and limited function for which patients seek dental consultation and treatment. The source of the pain and dysfunction is muscular, with masticatory muscles developing tenderness and pain as a result of abnormal muscular function or hyperactivity. The muscular pain is frequently, but not always, associated with daytime clenching or nocturnal bruxism. The cause of MPD is multifactorial. One of the most commonly accepted causes of MPD is bruxism resulting from stress and anxiety, with occlusion being a modifying or aggravating factor. MPD may also occur because of internal joint problems, such as disk displacement disorders or degenerative joint disease (DJD).
Patients with MPD generally complain of diffuse, poorly localized, preauricular pain that may also involve other muscles of mastication, such as the temporalis and medial pterygoid muscles. In patients with nocturnal bruxism, the pain is frequently more severe in the morning. Patients generally describe decreased jaw opening with pain during functions such as chewing. Headaches, usually bitemporal in location, may also be associated with these symptoms. Because of the role of stress, the pain is often more severe during periods of tension and anxiety.
Examination of the patient reveals diffuse tenderness of the masticatory muscles. The TMJs are frequently nontender to palpation. In isolated MPD, joint noises are usually not present. However, as mentioned previously, MPD may be associated with a variety of other joint problems that may produce other TMJ signs and symptoms. The range of mandibular movement in patients with MPD may be decreased and is associated with deviation of the mandible toward the affected side. The teeth frequently have wear facets. However, the absence of such facets does not eliminate bruxism as a cause of the problem.
Radiographs of the TMJs are usually normal. Some patients have evidence of degenerative changes, such as altered surface contours, erosion, or osteophytes. These changes, however, may result from or be unassociated with the MPD problem.
Disk Displacement Disorders
In a normally functioning TMJ the condyle functions in a hinge and a sliding fashion. During full opening the condyle not only rotates on a hinge axis but also translates forward to a position near the most inferior portion of the articular eminence (Fig. 30-9). During function the biconcave disk remains interpositioned between the condyle and fossa, with the condyle remaining against the thin intermediate zone during all phases of opening and closing.

FIGURE 30-9 Normal disk and condyle relationship. A, Biconcave disk is interpositioned between fossa and condyle in closed position. B, When condyle translates forward, thin intermediate zone stays in consistent relationship with condyle. C, Maximum open position.
Anterior Disk Displacement with Reduction
In anterior disk displacement the disk is positioned anterior and medial to the condyle in the closed position. During opening the condyle moves over the posterior band of the disk and eventually returns to the normal condyle and disk relationship, resting on the thin intermediate zone. During closing the condyle then slips posteriorly and rests on the retrodiskal tissue, with the disk returning to the anterior, medially displaced position (Fig. 30-10).

FIGURE 30-10 Anterior disk displacement with reduction. A, Biconcave disk is situated anterior to articulating surface of condyle. When condyle translates forward, it eventually passes over thickened posterior band of disk, creating clicking noise. B, After click occurs, disk remains in appropriate relationship with condyle through remainder of opening cycle. C, Maximum opening position. When mandible closes, condyle and disk relationship return to position as shown in A.
Examination of the patient usually reveals joint tenderness, and muscle tenderness may also exist. Joint noise (i.e., clicking) is commonly heard with opening, when the condyle moves from the area posterior to the disk into the thin concave area in the middle of the disk. In some cases, clicking can be heard or palpated during the closing cycle. Maximal opening can be normal or slightly limited, with the click occurring during the opening movement. Anatomically, the opening click corresponds to the disk reducing to a more normal position. The closing click (i.e., reciprocal click) corresponds to the disk failing to maintain its normal position between the condylar head and the articular eminence and slipping forward to the anteriorly displaced position. Crepitus may be present and is usually a result of articular movement across irregular surfaces.
The images obtained from plain TMJ radiography in patients with anterior disk displacement may be normal or may demonstrate slight bone abnormalities. MRI images usually demonstrate anterior displacement of the disk.
Anterior Disk Displacement Without Reduction
In this type of internal derangement the disk displacement cannot be reduced, and thus the condyle is unable to translate to its full anterior extent, which prevents maximal opening and causes deviation of the mandible to the affected side (Fig. 30-11).

FIGURE 30-11 Anterior disk displacement without reduction. A, Disk that has been chronically anteriorly displaced now has amorphous shape rather than distinct biconcave structure. B, When condyle begins to translate forward, disk remains anterior to condyle. C, In maximum open position, disk tissue continues to remain anterior to condyle, with posterior attachment tissue interposed between condyle and fossa.
In these patients no clicking occurs because they are unable to translate the condyle over the posterior aspect of the disk. This lack of translation may result in restricted opening, deviation to the affected side, and decreased lateral excursions to the contralateral side. Some evidence suggests that the limitation of motion may not be directly related to the actual displacement of the disk but rather to the adherence of the disk to the fossa, causing a restriction of the sliding function of the joint.16
Radiographic evaluation of disk displacement without reduction is similar to findings in anterior disk displacement with reduction. Plain TMJ radiography may appear normal, whereas CT scans and MRIs generally demonstrate anteromedial disk displacement. However, in this disorder, images taken in the maximal open position continue to show anterior disk displacement within the open position.
Degenerative Joint Disease (Arthrosis, Osteoarthritis)
DJD includes a variety of anatomic findings, including irregular, perforated, or severely damaged disks in association with articular surface abnormalities, such as articular surface flattening, erosions, or osteophyte formation (Fig. 30-12). The mechanisms of TMJ degenerative diseases are not clearly understood but are thought to be multifactorial. Current concepts of DJD incorporate three possible mechanisms of injury: (1) direct mechanical trauma, (2) hypoxia reperfusion injury, and (3) neurogenic inflammation.17
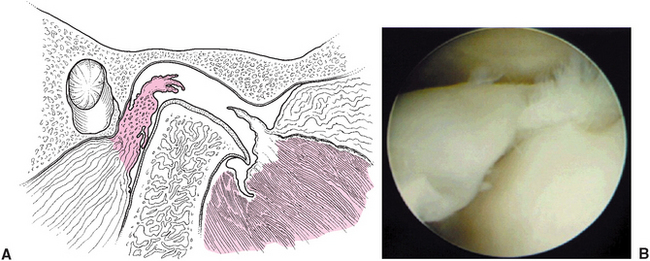
FIGURE 30-12 A, Degenerative joint disease demonstrates large perforation of disk tissue and erosion and flattening of articulating surfaces of condyle and fossa. B, Arthroscopic visualization of disk perforation with exposure of condyle in superior joint space.
Mechanical trauma may result from significant and obvious trauma to the joint or much less obvious microtrauma, such as excessive mechanical loading. The excessive stress produced in the joint can lead to molecular disruption and the generation of free radicals, with resulting oxidative stress and intracellular damage. Excess loading can also affect local cell populations and reduce the reparative capacity of the joint.
The hypoxia-reperfusion theory suggests that excessive intracapsular hydrostatic pressure within the TMJ may exceed the blood vessel perfusion pressure, resulting in hypoxia.
This type of increased intracapsular pressure has been clearly demonstrated in patients during clenching and bruxing.18 When the pressure in the joint is decreased and perfusion is reestablished, free radicals are formed. These free radicals may interact with other substances in the joint (e.g., hemoglobin) to produce even more damage.
Neurogenic inflammation results when a variety of substances are released from peripheral neurons. It is hypothesized that in cases of disk displacement, the compression or stretching of the nerve-rich retrodiskal tissue may result in release of proinflammatory neuropeptides.17,19 The release of cytokines results in the release and activation of a variety of substances including prostaglandins, leukotrienes, and matrix-degrading enzymes. These compounds not only have a role in the disease process but also may serve as biologic markers that may help to diagnose and eventually treat pathologic conditions of the joint.20,21 It must be emphasized that it is impossible to predict the progression of pathologic conditions of the joint.
Patients with DJD frequently experience pain associated with clicking or crepitus located directly over the TMJ. Usually, an obvious limitation of opening is present, and symptoms usually increase with function. Radiographic findings are variable but generally exhibit decreased joint space, surface erosions, osteophytes, and flattening of the condylar head. Irregularities in the fossa and articular eminence may also be present.
Systemic Arthritic Conditions
A variety of systemic arthritic conditions are known to affect the TMJ. The most common of these is rheumatoid arthritis. Other processes, such as systemic lupus, can also affect the TMJ. In these cases, symptoms are rarely isolated to the TMJs, and several other signs and symptoms of arthritis are usually present in other areas of the body.
In the case of rheumatoid arthritis, an inflammatory process results in abnormal proliferation of synovial tissue in a so-called pannus formation (Fig. 30-13).
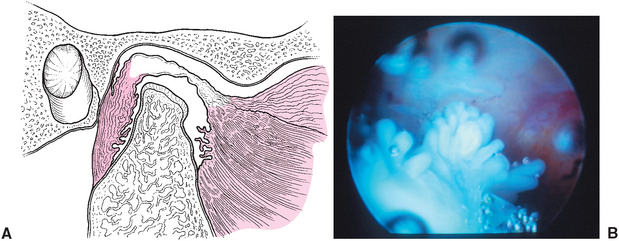
FIGURE 30-13 A, Changes seen in rheumatoid arthritis of temporomandibular joint. These changes include proliferation of synovial tissue, creating resorption in anterior and posterior areas of condyle. Irregularities of disk tissue and articulating surface of condyle eventually occur. B, Arthroscopic view of synovial hyperplasia.
TMJ symptoms that result from rheumatoid arthritis may occur at an earlier age than those associated with DJD. As opposed to DJD, which is usually unilateral, rheumatoid arthritis (and other systemic conditions) usually affects the TMJs bilaterally.
Radiographic findings of the TMJ initially show erosive changes in the anterior and posterior aspects of the condylar heads. These changes may progress to large eroded areas that leave the appearance of a small, pointed condyle in a large fossa. Eventually, the entire condyle and condylar neck may be destroyed. Laboratory tests, such as rheumatoid factor and erythrocyte sedimentation rate, may be helpful in confirming the diagnosis of rheumatoid arthritis.
Chronic Recurrent Dislocation
Dislocation of the TMJ occurs frequently and is caused by mandibular hypermobility. Subluxation is a displacement of the condyle, which is self-reducing and generally requires no medical management. A more serious condition occurs when the mandibular condyle translates anteriorly in front of the articular eminence and becomes locked in that position (Fig. 30-14). Dislocation may be unilateral or bilateral and may occur spontaneously after opening the mouth widely, such as when yawning, eating, or during a dental procedure. Dislocation of the mandibular condyle that persists for more than a few seconds generally becomes painful and is often associated with severe muscular spasms.
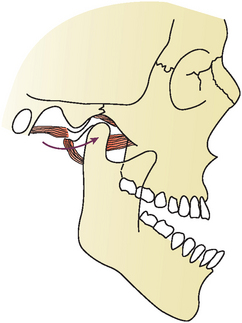
FIGURE 30-14 Diagram demonstrating hypermobility of joint allowing dislocation of condyle anterior to articular eminence.
Dislocations should be reduced as soon as possible. This reduction is accomplished by applying downward pressure on the posterior teeth and upward pressure on the chin, accompanied by posterior displacement of the mandible. Usually reduction is not difficult. However, muscular spasms may prevent simple reduction, particularly when the dislocation cannot be reduced immediately. In these cases, anesthesia of the auricular temporal nerve and the muscles of mastication may be necessary. Sedation to reduce patient anxiety and provide muscular relaxation may also be required. After reduction the patient should be instructed to restrict mandibular opening for 2 to 4 weeks. Moist heat and nonsteroidal antiinflammatory drugs (NSAIDs) are also helpful in controlling pain and inflammation.
Ankylosis
Intracapsular ankylosis, or fusion of the joint, leads to reduced mandibular opening that ranges from partial reduction in function to complete immobility of the jaw. Intracapsular ankylosis results from a fusion of the condyle, disk, and fossa complex as a result of the formation of fibrous tissue, bone fusion, or a combination of the two (Fig. 30-15). The most common cause of ankylosis involves macrotrauma, most frequently associated with condylar fractures. Other causes of ankylosis include previous surgical treatment that resulted in scarring and, in rare cases, infections.
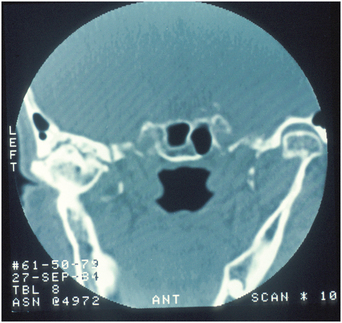
FIGURE 30-15 Bony ankylosis. Computed tomography scan imaging illustrating partial bony fusion of condyle and glenoid fossa.
Evaluation of the patient reveals severe restriction of maximal opening, deviation to the affected side, and decreased lateral excursions to the contralateral side. If the ankylosis is the result primarily of fibrous tissue, jaw mobility will be greater than if the ankylosis is a result of bone fusion.
Radiographic evaluation reveals irregular articular surfaces of the condyle and fossa, with varying degrees of calcified connection between these articulating surfaces.
Extracapsular Ankylosis
Extracapsular ankylosis usually involves the coronoid process and temporalis muscle. Frequent causes of extracapsular ankylosis are coronoid process enlargement, or hyperplasia, and trauma to the zygomatic arch area. Infection around the temporalis muscle may also produce extracapsular ankylosis (Fig. 30-16).

FIGURE 30-16 Extracapsular ankylosis resulting from coronoid hypertrophy. Elongation of coronoid process results in impingement against the posterior aspect of the maxilla during opening, limiting mandibular range of motion.
Patients initially have limitation of opening and deviation to the affected side. In these cases, complete restriction of opening is rare, and limited lateral and protrusive movements can usually be performed, indicating no intracapsular ankylosis. Panoramic radiography generally demonstrates the elongation of a coronoid process. A submental vertex radiograph may be useful in demonstrating impingement caused by a fractured zygomatic arch or zygomaticomaxillary complex.
Neoplasia
Neoplasms in the TMJ are rare. Neoplasms can occasionally result in restriction of opening and joint pain. Tumors within the TMJ may result in an abnormal condyle and fossa relationship or an intracapsular ankylosis. A complete discussion of the neoplastic processes known to occur in the TMJ area is beyond the scope of this chapter.
Infections
Infections in the TMJ area are rare, even in the case of trauma or surgical intervention in this area. In third world countries where antibiotic therapy of middle ear infections is not available, extension of infectious processes may occasionally involve the TMJ and result in intracapsular ankylosis.
REVERSIBLE TREATMENT
Although the cause of temporomandibular pain and dysfunction can arise from several different sources, initial treatment is frequently aimed at nonsurgical methods of reducing pain and discomfort, decreasing inflammation in muscles and joints, and improving jaw function. In some cases, such as ankylosis or severe joint degeneration, surgical treatment may be the preferred initial course of therapy. However, in most cases—including MPD, disk displacement disorders, and degenerative and systemic arthritic disorders—a nonsurgical, reversible treatment phase may provide significant reduction in pain and improvement in function. Most patients with MPD and internal derangements do well without any type of long-term or invasive treatment. In the case of anterior disk displacement without reduction (i.e., closed lock), most patients experience a gradual progression of increased opening and decreased discomfort without extensive treatment. This is apparently the result of physiologic and anatomic adaptation of tissue within the joint. It appears that in many patients the posterior attachment tissue undergoes fibrous adaptation and adequately serves as interpositioning tissue between the condyle and fossa.22 This is often termed pseudodisk adaptation (Fig. 30-17). This pseudodisk formation, combined with other normal healing capabilities of joints, is most likely responsible for clinical improvement in many patients.
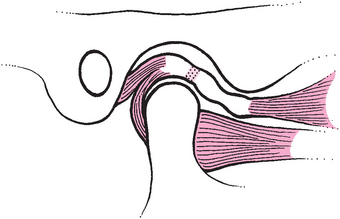
FIGURE 30-17 Anteriorly displaced disk results in stress on retrodiskal tissue. Subsequent fibrosis provides adaptation, producing a functional, although anatomically different, interpositional disk.
Patient Education
The first step in involving patients in their own treatment is to make them aware of the pathologic condition producing their pain and dysfunction and to describe the prognosis or possible progression of their pain and dysfunction. Many problems of masticatory pain and dysfunction stabilize or improve with conservative therapy, despite patients’ concerns that they may be on a continually deteriorating course. In the case of a patient with MPD, a precise, confident explanation should attempt to assure the patient that muscular pain usually improves with minimal treatment. The clinician should also explain that although symptoms may recur on occasion, they generally can be controlled with the treatment (described later in this chapter).
In some cases, such as DJD, the patient should be made aware of the long-term spectrum of outcomes of this problem. Warning signs of further deterioration, including increased pain, limitation of motion, and increased joint noise, should be emphasized to the patient.
Patients who have an awareness of the factors associated with their pain and dysfunction can actively participate in their own improvement. Myofascial pain often results from parafunctional habits or muscular hyperactivity resulting from stress and anxiety. Patients who are aware of these factors are often able to control their activity and thereby reduce discomfort and improve function. Biofeedback devices provide information to patients to help them control their muscular activity. For example, the output from surface electrodes over the masseter or temporalis muscle can be used to indicate clenching or grinding during daytime activity.23 Electromyographic recordings can also be useful in evaluating nocturnal bruxism and associated pain and can be used to monitor the effectiveness of splint therapy and medication to control muscular hyperactivity. Other forms of stress control, such as physical exercise, reducing exposure to stressful situations, and psychological counseling, can also be explored. When the patient becomes aware of the relationship between personal actions and the symptoms of pain and dysfunction, behavior modification can follow.
Modification of diet combined with home exercise routines are also an important part of the patient’s educational process. Patients who experience temporomandibular pain or dysfunction frequently find that it is most apparent when chewing hard food. Temporary alteration of the diet to a softer consistency may result in a significant reduction in symptoms. A gradual progression to a more normal diet over a period of 6 weeks may be sufficient to reduce joint or muscle symptoms. Aggravating factors including chewing of gum, fingernails, or ice should be reviewed, and cessation or limitation of these activities should be encouraged.
Medication
Pharmacologic therapy is an important aspect of nonsurgical management of TMD. Medications typically used in the treatment of TMDs include NSAIDs; (2) occasionally, stronger analgesics; (3) muscle relaxants; and (4) antidepressants.
NSAIDs not only reduce inflammation but also serve as an excellent analgesic. Categories of nonsteroidal antiinflammatory medications include propionic acid derivatives (ibuprofen, naproxen), salicylates (aspirin, diflunisal), and acetic acid compounds (indomethacin, sulindac). These medications can be effective in reducing inflammation in muscles and joints and in most cases provide satisfactory pain relief. These drugs are not associated with severe addiction problems, and their use as an analgesic is strongly preferred over narcotic medications. Dosing of antiinflammatory medications is most effective when they are administered on a time-regulated schedule rather than on a pain-dependent schedule. Patients should be instructed to take the medicine regularly, obtaining an adequate blood level that should then be maintained for a minimum of 7 to 14 days. Discontinuation or tapering of the medicine can then be attempted.
The cyclooxygenase-2 (COX-2) inhibitors such as celecoxib (Celebrex) have gained popularity in the treatment of inflammation and pain. Prostaglandins produced by COX-1 activity appear to be required for normal physiologic function, whereas those produced by COX-2 activation mediate pain and inflammation. The COX-2 inhibitors are intended to reduce pain and inflammation without affecting prostaglandin-dependent functions. Some COX-2 inhibitors have recently been associated with the potential for significant side effects including cardiac complications, and they should be used with the appropriate caution and monitoring of the patient. Consultation with the patient’s physician may be warranted.
Analgesic medicines for patients with TMJ disorders may range from acetaminophen to potent narcotics. One important principle of treatment for all pain and dysfunction in patients is to remember that the problem may be chronic and that medication could produce long-term addiction. Because of the sedative and depressive effects of narcotics and their potential for addiction, these medications should be restricted to short-term use for episodes of severe, acute pain or in a postoperative setting. In such instances, medications such as acetaminophen with codeine should be sufficient. This medication should not be used for longer than 10 days to 2 weeks if possible.
Muscle relaxants may provide significant improvement in jaw function and relief of masticatory pain through control of dystonia. However, muscle relaxants have a significant potential for depression and sedation and can produce long-term addiction. In many patients with acute pain or exacerbation of muscular hyperactivity, muscle relaxants can be considered for short periods, such as 10 days to 2 weeks. The lowest effective dose should be used. Diazepam (Valium), carisoprodol (Soma), cyclobenzaprine (Flexeril), and tizanidine (Zanaflex) are examples of commonly used muscle relaxants. Pharmacologic therapy often provides adequate relief of muscular symptoms in patients with TMD.
Antidepressants, most commonly tricyclic antidepressants used in low doses, appear to be useful in the management of patients with chronic pain.24,25 Tricyclic antidepressants prevent the reuptake of amine neurotransmitters, such as serotonin and norepinephrine, causing an inhibition of pain transmission. Recently, anecdotal evidence has suggested that these antidepressants may be effective in decreasing nocturnal bruxism. It appears that nighttime bruxing may be in part a result of disruption of normal sleep patterns.26,27 Amitriptyline (Elavil) used in small doses (10 to 25 mg at bedtime) may improve sleep patterns, decrease bruxism, and result in decreased joint and muscle pain.
Medications that must be administered by injection may occasionally be helpful in managing muscular and joint pain and inflammation. Recently, the use of botulinum toxin A has shown promise in decreasing masticatory muscle hyperactivity.28,29 Botulinum toxin (Botox) is a neurotoxin produced by the bacterium Clostridium botulinum. This neurotoxin produces a paralytic effect on muscles by inhibiting the release of acetylcholine at the neuromuscular junction. In very low doses, Botulinum toxin can be safely administered by injection directly into the affected muscle area, decreasing muscle contraction activity and the associated pain (Fig. 30-18). The effect of Botulinum toxin is temporary, lasting from a few weeks to several months. In many cases, injection of Botulinum toxin must be repeated to obtain long-term pain relief.
Injection of local anesthetic combined with steroids into the temporalis tendon and the joint has been shown to be an effective way to decrease pain and inflammation. Tendinitis in areas such as the insertion of the temporalis tendon along the ascending ramus and coronoid process often responds favorably to trigger point injection. Local anesthetic provides temporary relief of pain, and steriods exert their effect through the inhibition of proinflammatory cytokines.30 There continues to be some debate about the long-term effect of steroids in the joint and the possibility that further degeneration may be associated with steroid injection.31 Further research is required in this area.
Physical Therapy
Physical therapy can be useful in the management of patients with temporomandibular pain and dysfunction. A variety of techniques have been used successfully as adjunctive therapy for treatment of temporomandibular dysfunction. The most common modalities used include range of motion exercises, relaxation training, ultrasound, spray and stretch, and pressure massage.32,33
Although the patient is generally encouraged to reduce the functional load placed on the joint and muscles, it is important to remember that maximizing range of motion is also an important aspect of treatment of all TMDs.34 Limited mandibular range of motion may lead to problems in the TMJ and muscles of mastication. The lack of mobility may limit the lubrication of the joint via changes in the synovial membrane and contribute to degenerative changes of the articular surfaces. Limited muscular movement can result in fibrosis, further restriction of motion and an increase in pain. Physical therapy is initially implemented through a home regimen. These exercises include gentle stretching exercises done within pain tolerance through passive opening or active exercise routines. Establishing a baseline is a valuable resource to gauge progress and can be measured via the number of fingers positioned between the incisal edges or dispensing a plastic ruler. Simple methods for passive therapy include stretching by exerting a scissor effect with the thumb and forefinger or interval increases in tongue blades placed between the upper and lower teeth (Fig. 30-19). The force is exerted until resistance or pain is encountered and is maintained for several seconds. Appliances are also available that provide easy and efficient methods for improving jaw mobility through passive exercise. Consultation with a physical therapist may be required to provide a regimen to assist in overcoming persistent immobilization.35,36

FIGURE 30-19 Jaw exercising. A, Passive stretch applied through scissoring of thumb and forefinger. B, Physical therapy through Therabite appliance to increase range of jaw motion.
Relaxation training, although perhaps not physical therapy in the strictest sense, can be effective in reducing symptoms caused by muscular pain and hyperactivity. During the educational phase, patients are made aware of the contribution of stress and muscular hyperactivity to pain. Relaxation techniques can be used to reduce the effects of stress on muscle and joint pain. Electromyographic monitoring of the patient’s muscular activity can be used as an effective teaching tool by providing instant feedback demonstrating relaxation therapy, reduction of muscular hyperactivity, and the resultant improvement in symptoms of pain.
Ultrasound is an effective way to produce tissue heating with ultrasonic waves, which alter blood flow and metabolic activity at a deeper level than that provided by simple surface moist-heat applications.37 The effect of ultrasonic tissue heating is theoretically related to increase in tissue temperature, increase in circulation, increase in uptake of painful metabolic by-products, and disruption of collagen cross-linking, which may affect adhesion formation. All of these effects may result in a more comfortable manipulation of muscles and a wider range of motion. In addition, intraarticular inflammation may also be reduced with ultrasonic applications. Ultrasonic treatments are usually provided by a physical therapist in combination with other treatment modalities.
Spray and stretch is an effective method for improving range of motion. The theory behind spray and stretch is the concept that significant superficial skin stimulation can produce an overriding or distracting effect on pain input that originates in the muscles and joints.38 By spraying a vapocoolant material, such as fluoromethane, over the lateral surface of the face, the muscles of mastication can be passively or actively stretched with a reduced level of pain.
Friction massage involves the use of firm cutaneous pressure sufficient to produce a temporary degree of ischemia. This ischemia and the resultant hyperemia have been described as a method for inactivation of trigger points, which are areas responsible for pain referred to muscles in the head and neck area.38 More frequently, this technique may be useful in disrupting small fibrous connective tissue adhesions that may develop within the muscles during healing after surgery and injury or as a result of prolonged muscular shortening from restricted motion.
Physical therapists and other practitioners sometimes use transcutaneous electrical nerve stimulation (TENS) to provide pain relief for chronic pain patients when other techniques have been unable to eliminate or reduce pain symptoms. The exact mechanism of action of TENS is not completely understood. The technique was initially based on the concept that stimulation of superficial nerve fiber with TENS may be responsible for overriding pain input from structures such as masticatory muscles and the TMJs. Interestingly, many patients who use TENS units experience pain relief that is longer in duration than the time during which the unit is actually applied. This may be a result of the release of endogenous endorphin compounds that can provide extended periods of decreased pain.
Each of the physical therapy modalities may be useful in the reduction of TMJ pain and increasing range of motion. The low cost of physical therapy compared with other medical treatment, the likelihood that some benefit will occur, and the minimal risk associated with these techniques are strong arguments for frequent use of physical therapy in the management of patients with TMD.
Splint Therapy
Occlusal splints are generally considered a part of the reversible or conservative treatment phase in the management of patients with TMD. Splint designs vary; however, most splints can be classified into two distinct groups: (1) autorepositioning splints and (2) anterior repositioning splints.
Autorepositioning Splints
The autorepositioning splint, also called anterior guidance splints, superior repositioning splints, or muscle splints. The splints are most frequently used to treat muscle problems or eliminate TMJ pain when no specific internal derangement or other obvious pathologic condition can be identified. However, these splints may be used in some cases, such as anterior disk displacement or DJD, in an attempt to unload or reduce the force placed directly on the TMJ area. These splints are designed to provide a flat surface with even contact in all areas of the occlusion. The splint provides full-arch contact without working or balancing interferences and without ramps or deep interdigitation that would force the mandible to function in one specific occlusal position (Fig. 30-20). This splint allows the patient to seek a comfortable muscle and joint position without excessive influence of the occlusion. Nitzan18 has shown that properly designed splints can be effective in reducing intraarticular pressure. An example of this type of splint would be in a patient with a Class II malocclusion and significant overjet who continually postures forward to obtain incisor contact during mastication. Many of these patients complain of muscular symptoms and describe a feeling that they do not have a consistent, repeatable bite relationship. Wearing an autorepositioning splint allows full-arch dental contact with the condyles in a more posterior retruded position, which frequently results in reduction of muscle and joint symptoms.
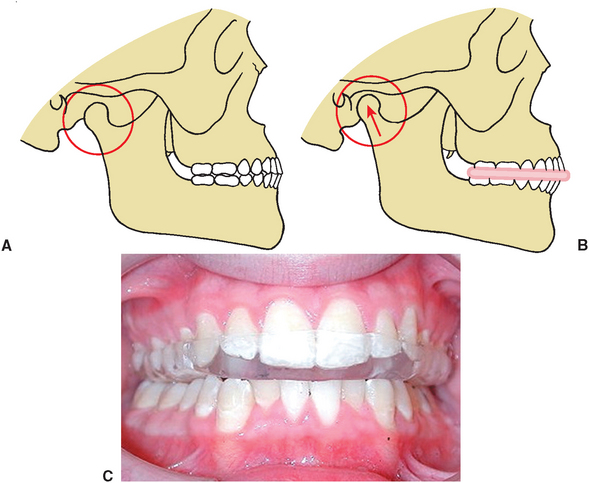
FIGURE 30-20 Autorepositioning splint. A, Diagram representing maximum interdigitation obtained with condyle slightly down and forward. B, Repositioning of mandible by eliminating forced interdigitation of teeth results in posterior and superior repositioning of condyle. C, Clinical photograph of occlusal splint.
Anterior Repositioning Splints
Anterior repositioning splints are constructed so that an anterior ramping effect forces the mandible to function in a protruded position (Fig. 30-21). This type of splint is most useful in providing temporary relief and, in rare cases, a long-term cure for anterior disk displacement with reduction. In these cases the anterior position is determined by protrusion of the mandible necessary to produce the proper disk and condyle relationships (after the protruding or opening click has occurred).
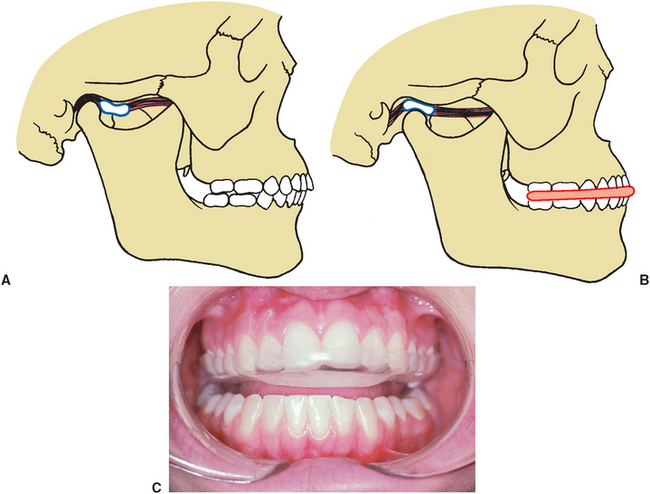
FIGURE 30-21 Anterior repositioning splint. A, Diagram of anteriorly displaced disk. B, Disk interposition between condyle and articular eminence, with anterior repositioning splint in place. Anterior position of mandible allows function with condyle in appropriate condyle and disk relationship. C, Clinical photograph of anterior repositioning splint.
The splint is usually worn 24 hours a day for several months. Theoretically, after the disk is repositioned for a long period, the posterior ligaments may shorten and maintain the disk in proper relationship to the condyle. Despite theoretical expectations, these splints are generally ineffective in producing permanent reduction of disk displacement. However, even when the splints are not curative, they often provide significant relief of discomfort in the acute stages of TMJ dysfunction.
PERMANENT OCCLUSION MODIFICATION
After completion of a course of reversible treatment, many patients may be candidates for permanent modification of the occlusion. This permanent modification appears to be most appropriate when patients have had significant improvement in masticatory function and reduction in pain as a result of temporary alteration of occlusal position with splint therapy. Permanent occlusion modification may include occlusal equilibration, prosthetic restoration, orthodontics, and orthognathic surgery. Although the relationship between occlusion abnormalities and TMD is unclear, it does appear that permanent modification of the occlusion in indicated patients may provide long-term improvement in symptoms of pain and dysfunction.
TEMPOROMANDIBULAR JOINT SURGERY
Despite the fact that many patients with internal pathologic conditions of the joint improve with reversible nonsurgical treatment, some patients eventually require surgical intervention to improve masticatory function and decrease pain. Several techniques are currently available for correction of a variety of TMJ derangements.
Arthrocentesis
Arthrocentesis is a minimally invasive technique that involves placing ports (needles or small cannulas) into the TMJ to lavage the joint and to break up fine adhesions. Most patients undergoing arthrocentesis do so with intravenous sedation and an auriculotemporal nerve block. Several techniques have been described for TMJ arthrocentesis.16,39 The most common method involves initially placing one needle into the superior joint space (Fig. 30-22). A small amount of lactated Ringer’s solution is injected to distend the joint space and release fine adhesions that may be limiting disk mobility. With the joint insufflated, a second needle is placed into the superior joint space, allowing thorough lavage with large amounts of fluid (approximately 200 ml).
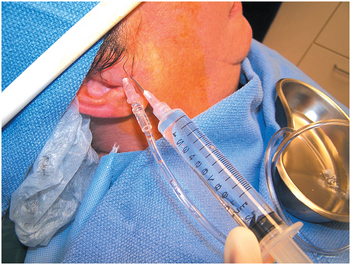
FIGURE 30-22 Arthrocentesis. Port placement into superior joint space paralleling the external auditory meatus to allow lavage and lysis of fine adhesions.
During the arthrocentesis the jaw can be gently manipulated. At the conclusion of the procedure, steroids, local anesthesia, or a combination of both can be injected into the joint space before the needles are withdrawn. Discomfort after the procedure is managed with mild analgesics or NSAIDs. Some type of exercise regimen or physical therapy is accomplished during the recovery period.
Many types of internal pathologic conditions of the joint appear to respond well to arthrocentesis. The most common use appears to be in patients with anterior disk displacement without reduction. Treatment appears to be effective, with results similar to or better than other types of arthroscopic and open surgical procedures. Nitzan39 demonstrated that arthrocentesis produced significant improvement in incisal opening and reduction of pain in patients with persistent and severe closed lock.
The success seen with arthrocentesis has several potential explanations. When disk displacement occurs, negative pressure may develop within the joint, causing a “suction cup” effect between the disk and fossa. Distending the joint obviously eliminates the negative pressure. In some cases of more chronic disk displacement, some adhesion may develop between the disk and fossa. With arthrocentesis the distention under pressure can release these adhesions. Capsular constriction may occur as a result of joint hypomobility and can be stretched with pressure distention. Finally, there may be an accumulation of some of the chemical mediators described previously. The simple flushing action in the joint may eliminate or decrease biochemical factors contributing to inflammation and pain.
Arthroscopy
Arthroscopic surgery has become one of the most popular and effective methods of diagnosing and treating TMJ disorders.40 The technique involves placement of a small cannula into the superior joint space, followed by insertion of an arthroscope to allow direct visualization of all aspects of the glenoid fossa, superior joint space, and superior aspect of the disk. Arthroscopic evaluation enables the surgeon to visualize the joint and therefore contributes to the diagnosis of the internal pathologic condition of the joint. Lysis of adhesions and lavage of the joint are also completed.
More sophisticated arthroscopic operative techniques have been developed, increasing the ability of the surgeon to correct a variety of intracapsular disorders. Current surgical techniques usually involve the placement of at least two cannulas into the superior joint space. One cannula is used for visualization of the procedure with the arthroscope, whereas instruments are placed through the other cannula to allow instrumentation in the joint (Fig. 30-23). Instrumentation used through the working cannula includes forceps, scissors, sutures, medication needles, cautery probes, and motorized instrumentation such as burs and shavers. Laser fibers can also be used to eliminate adhesions and inflamed tissue and incise tissue within the joint. Disk manipulation, disk attachment release, posterior band cautery, and suture techniques have been developed in an attempt to reposition or stabilize displaced disks.41 Although it appears that attempts to reposition displaced disks do not result in anatomic restoration of normal disk position, patients undergoing this type of treatment appear to have significant clinical improvement after arthroscopic surgery.42
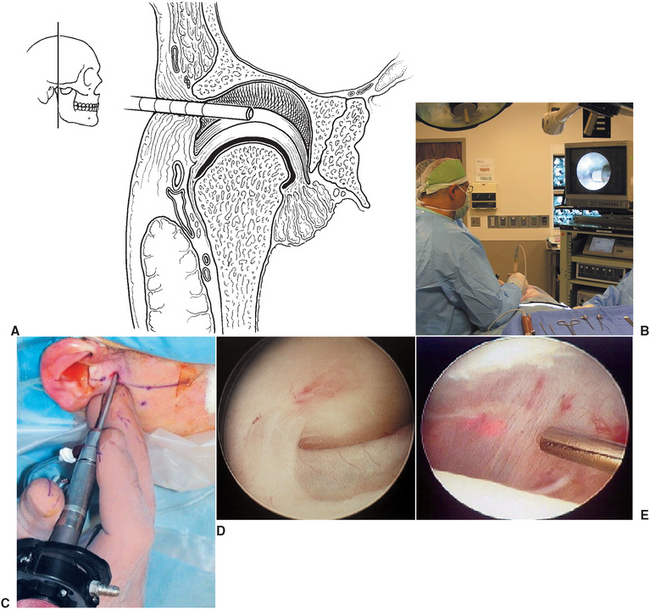
FIGURE 30-23 Temporomandibular joint arthroscopy. A, Diagram depicting arthroscope placement in superior joint space. B, Operating room orientation for arthroscopy. C, Arthroscope orientation for visualization of the temporomandibular joint. D, View of superior joint space with disk inferiorly and fibrous adhesions limiting disk mobility. E, Instrumentation through a second port (radio frequency, laser, motorized shaver) allows surgical manipulation within the joint space.
Arthroscopic surgery has been advocated for treatment of a variety of TMJ disorders, including internal derangements, hypomobility as a result of fibrosis or adhesions, DJD, and hypermobility. The removal of disks with gross perforations can be accomplished with the arthroscope while preserving the surrounding synovial tissue for lubrication.43 The efficacy of arthroscopic treatment appears to be similar to that of open joint procedures, with the advantage of less surgical morbidity and fewer and less severe complications.41–44
As with most TMJ surgical procedures, patients are placed on some type of physical therapy regimen and often continue splint therapy to help decrease loading on the joint during healing.45
Disk-Repositioning Surgery
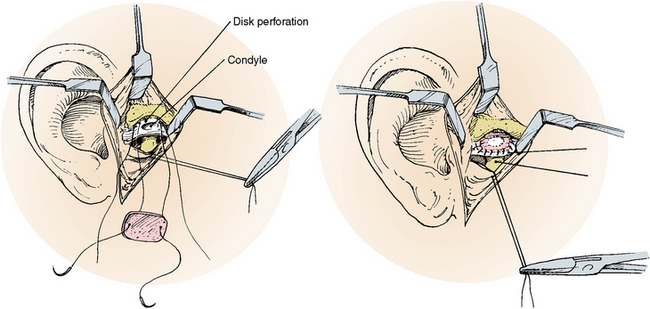
Open joint procedures are generally reserved for individuals who have not responded favorably to other measures. Open surgical exploration of the TMJ traditionally proceeds after conservative techniques have been maximized. Disk plication and repositioning through an variety of open approaches has been a common surgical procedure performed to correct anterior disk displacement that has not responded to nonsurgical treatment and that most frequently results in persistent painful clicking joints or closed locking. Although these disorders are often managed surgically with arthrocentesis or arthroscopy, many surgeons still prefer this type of surgical correction. In this operation, the displaced disk is identified and repositioned into a more normal position by removing a wedge of tissue from the posterior attachment of the disk and suturing the disk back to the correct anatomic position (Fig. 30-24). In some cases this procedure is combined with recontouring of the disk, articular eminence, and mandibular condyle. After surgery, patients generally begin a nonchew diet for several weeks, progressing to a relatively normal diet in 3 to 6 months. A progressive regimen of jaw exercises is also instituted in an attempt to obtain normal jaw motion within 6 to 8 weeks after surgery.
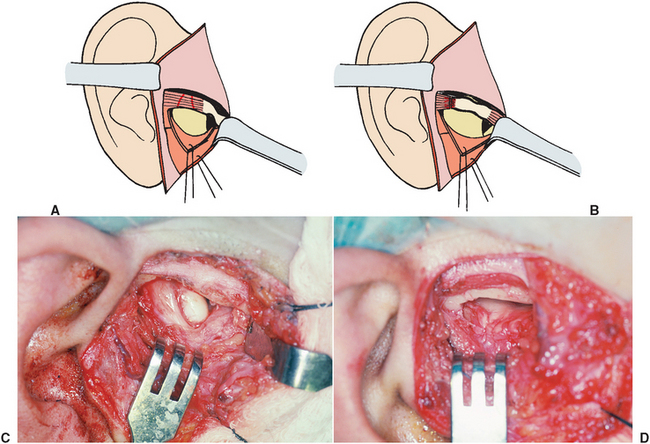
FIGURE 30-24 Open temporomandibular joint surgery. A, Preauricular incision through skin subcutaneous tissue and temporomandibular joint capsule, exposing anteriorly displaced disk. B, Wedge of tissue is removed from posterior attachment area, and disk is repositioned and sutured into its correct position. C, Displaced disk anterior to mandibular condyle. D, Disk repositioning and plication via open arthrotomy.
In general, the results of open arthroplasty have been favorable, with a majority of patients experiencing less pain and improved jaw function.46 Unfortunately, this surgery does not produce improvement in all patients, with 10% to 15% of patients describing no improvement or a worsening of the condition.
Disk Repair or Removal
In some cases the disk is so severely damaged that the remnants of disk tissue must be removed. Diskectomy without replacement was one of the earliest surgical procedures described for treatment of severe TMJ internal derangements.47 With current technology, the diskectomy procedure can be performed through arthroscopic techniques to minimize scar tissue formation and preserve lubrication provided by the synovium. Although this technique has been widely used, there seems to be a wide variation in clinical results, with some joints showing minimal anatomic changes and significant clinical improvement and some joints demonstrating severe degenerative changes with continued symptoms of pain and dysfunction.
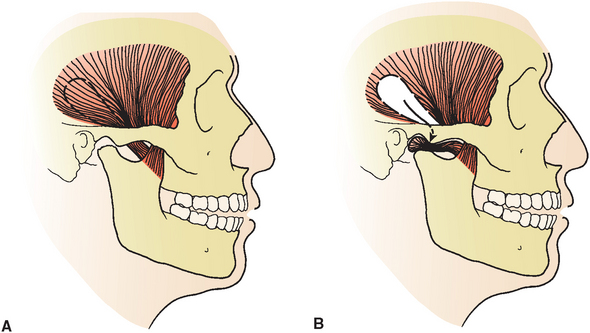
In advanced internal pathologic conditions of the joint, the disk may be severely damaged and perforated but may have adequate remaining tissue so that a repair or patch procedure can be accomplished. Autogenous grafting techniques include the use of dermis, auricular cartilage, or temporalis fascia.48,49 Dermis harvested from the abdomen or upper lateral thigh placed into the joint functions as an interpositional disk (Fig. 30-25). The dermal graft with associated adipose tissue provides lubrication and coverage of the articular surfaces.
Another alternative to the use of a free graft involves rotation of a temporalis muscle flap into the joint to provide interpositional tissue between the condyle and fossa.50 The posterior fibers of the temporalis are mobilized from the temporal bone with an anterior pedicle originating from the coronoid process (Fig. 30-26). The maintenance of the anterior aspect of the temporalis muscle provides a blood supply to the flap, enhancing viability. The fascia, muscle, and periosteum are ligated to prevent separation and are rotated under the zygomatic arch. The flap is positioned over the condyle and sutured to the residual retrodiskal tissue. The preservation of the overlying fascia may aid in continued lubrication of the obliterated joint.
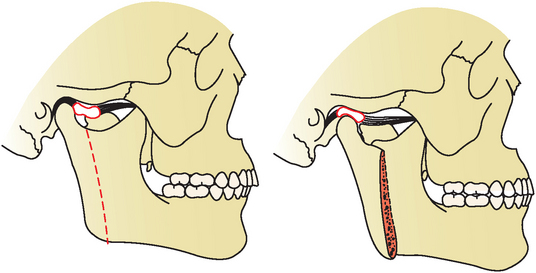
Condylotomy for Treatment of Temporomandibular Joint Disorders
The condylotomy is an osteotomy completed in a manner identical to the vertical ramus osteotomy described in Chapter 25 (Fig. 30-27). When used for treatment of TMJ problems, the osteotomy is completed, but no wire or screw fixation is placed, and the patient is placed into intermaxillary fixation for a period ranging from 2 to 6 weeks. The theory behind this operation is that muscles attached to the proximal segment (i.e., segment attached to the condyle) will passively reposition the condyle, resulting in a more favorable relationship between the condyle, disk, and fossa.51,52
This technique has been advocated primarily for treatment of disk displacement with or without reduction. DJD and subluxation or dislocation have also been suggested as possible indications for use of this technique. Although this method of surgical treatment has been controversial, it appears to provide significant clinical improvement in a variety of TMJ disorders.
Total Joint Replacement
In some cases, a pathologic condition of the joint results in destruction of joint structures and in loss of vertical dimension of the condyle and posterior ramus, malocclusion, limited opening, and severe pain. In these cases, reconstruction or replacement of condylar and fossa components of the TMJ may be necessary. Surgical techniques may involve replacement of the condyle or fossa but most commonly include both elements.
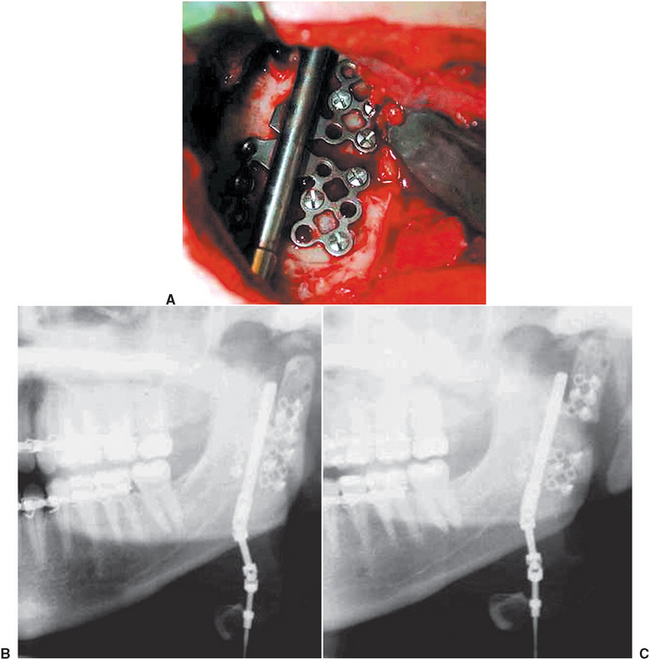
One method of joint reconstruction involves grafting autogenous tissue using a costochondral bone graft.53 These grafts are most frequently used in growing individuals but also can be used effectively in the treatment of a variety of adult disorders. Figure 30-28, B, shows the use of a costochondral graft for replacement of a severely degenerated mandibular condyle. In this situation the graft replaces only the condylar portion of the joint and does not address significant abnormalities of the fossa. Problems with costochondral grafting include recurrent ankylosis, degenerative changes of the graft, and (in some cases) excess and asymmetric growth of the graft.
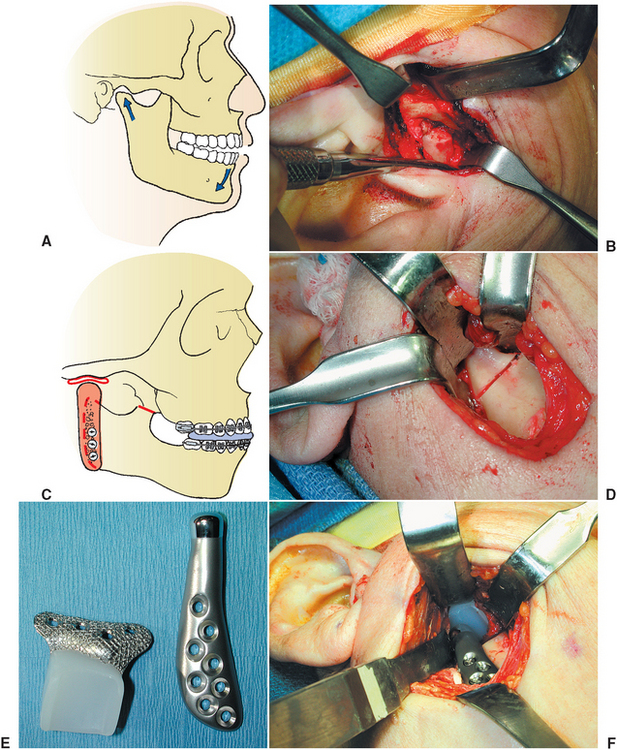
FIGURE 30-28 Total joint replacement. A, Illustration showing severe degenerative joint disease resulting in open bite malocclusion caused by resorption of condyle. B, Exposure via a preauricular approach confirms severe degeneration of the condyle. C, Illustration of costochondral bone graft placed along posterior aspect of mandible to reconstruct severely damaged condyle. This technique is usually reserved for growing patients. D, Bone cut for condylectomy completed with sagittal saw while protecting important adjacent neurovascular structures. E, Custom condylar and fossa prosthesis fabricated from a stereolithic model. F, Positioning of condyle and fossa in total joint reconstruction.
In the past, several types of prosthetic joint replacement have been available.54 Long-term results of prosthetic joint replacements have been disappointing because of a variety of engineering and biologic problems. However, for many patients with significant destruction of TMJ structures who have had poor results from other surgical treatment, no other viable surgical options exist. In these cases the joint destruction results in severe pain, limited motion or complete ankylosis, and severe malocclusions.
Total joint replacement in severe TMJ disease, such as a severely degenerative or multiply operated joint with excessive scarring, aims to restore function through improved range of motion and reduction in pain. Older joint prostheses met with limited success because of the excessive scar tissue associated with multiple previous open joint surgeries, mechanical failure, and foreign body reaction from wear debris. Newer-generation joint prostheses have improved engineering, better biocompatibility, and materials with greater wear resistance. Total joint replacement can be completed with standard preformed fossa and condyle parts or with custom fabrication of joint components. Custom joints are generated from a stereolithic model based on three-dimensional CT scan imaging of the articular fossa and mandibular anatomy (Fig. 30-28, C).
Access to the joint and ramus are achieved through a preauricular and retromandibular incision, respectively. A nerve simulator is used during the dissection to ensure preservation of the facial nerve to the muscles of facial expression. Soft tissue dissection is completed to expose the TMJ capsule, condyle, coronoid, and ramus. Removal of the diseased condyle is completed, followed by débridement of the articular fossa. The joint fossa and condylar prosthesis are placed after the occlusion has been established with maxillomandibular fixation and secured with bone screws. The established occlusion is verified while maintaining sterility of the surgical field. Manipulation of the mandible intraoperatively allows for evaluation of joint function in the absence of muscular influences.
These recent advantages have provided significant improvement in the outcome after total joint replacement.55,56
DISTRACTION OSTEOGENESIS
The loss of vertical ramus height is a consequence of a condylar pathologic condition and may result in asymmetry and malocclusion, as well as dysfunction and pain. Severe alteration of condylar anatomy may result from a variety of conditions such as hemifacial microsomia, growth disturbances, trauma, or a pathologic condition. Until recently, skeletally immature patients were treated primarily with costochondral grafts.57 The need for donor site surgery and unpredictable results including asymmetric growth and ankylosis yielded less than ideal results in many patients. More recently, distraction osteogenesis has been used successfully to reconstruct the mandibular condyle.58
Distraction osteogenesis of the mandibular condyle involves exposing the mandibular ramus, usually through an extraoral approach. The distractor is temporary stabilized on the lateral surface of the mandible, an osteotomy of the posterior ramus is completed, and the distraction appliance is attached to the osteotomized (condyle) segment and to the stable portion of the ramus (Fig. 30-29). Following an initial latency period of 5 to 7 days, the distraction appliance is activated, producing approximately 1 mm of bone movement per day. This process creates regenerate bone formation in response to distraction of the condylar segment. Range of motion is maintained during distraction, and control of the occlusion and molding of the regenerate can be completed with elastic traction guidance. The consolidation period is typically calculated as 3 times the period of distraction. During this time the structural integrity over the regenerate is maintained with the distraction appliance. A second intervention is required to remove the distractor, and a stabilizing bone plate can be placed over the regenerate gap. Surgical access to remove the distractor is through the existing incision. The reestablishment of vertical ramus height and increased mandibular continuity allows for reestablishment of symmetry and occlusion. Finalizing the occlusion often requires orthodontic detailing or equilibration to aid in providing a stable, balanced interdigitation.
REFERENCES
1. Blaschke, DD, White, SC. Radiology. In Sarnat BG, Laskin DM, eds.: The temporomandibular joint: biological diagnosis and treatment, ed 3, Springfield, IL: Charles C Thomas, 1980.
2. Blair, GS, Chalmers, IM, Leggat, TG, et al. Circular tomography of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1973;35:416.
3. Dolwick, MF, Katzberg, RW, Helms, CA, et al. Arthrotomographic evaluation of the temporomandibular joint. J Oral Surg. 1979;37:793.
4. Helms, CA, Morrish, RB, Jr., Kircos, LT, et al. Computed tomography of the meniscus of the temporomandibular joint: preliminary observations. Radiology. 1982;145:719.
5. Manzione, JV, Katzberg, RW, Tallents, RH, et al. Magnetic resonance imaging of the temporomandibular joint. J Am Dent Assoc. 1986;113:398.
6. Oesterreich, FU, Jend-Rossmann, I, Jend, HH, et al. Semi-quantitative SPECT imaging for assessment of bone reaction to internal derangements of the temporomandibular joint. J Oral Maxillofac Surg. 1987;45:1022.
7. Sternback, RA, Varieties of pain games. Bonica, JJ, eds. Advances in neurology: international symposium on pain, vol 4. New York: Raven, 1973.
8. Yap, AU, Chua, EK, Tan, KB, et al. Relationship between depression/somatization and self-reports of pain and disability. J Orofac Pain. 2004;18:220–225.
9. Green, CS. Orthodontics and temporomandibular disorders. Dent Clin North Am. 1988;32:529–538.
10. Kinney, RK, Gatchel, RJ, Ellis, E, et al. Major psychological disorders in chronic TMD patients: implications for successful management. J Am Dent Assoc. 1992;123:49–54.
11. Rugh, JD. Psychological components of pain. Dent Clin North Am. 1987;31:579–594.
12. Moss, RA, Adams, HE. The assessment of personality, anxiety and depression in mandibular pain dysfunction subjects. J Oral Rehabil. 1984;11:233–237.
13. Katon, W, Egan, K, Miller, D. Chronic pain: lifetime psychiatric diagnosis and family history. Am J Psychiatry. 1985;142:1156–1160.
14. Turner, JA, Whitney, C, Dworkin, SF, et al. Do changes in patients beliefs and coping strategies predict temporomandibular disorder treatment outcomes? Clin J Pain. 1995;11:177–188.
15. Rugh, JD, Solberg, WK. Psychological implications in temporomandibular pain and dysfunction. Oral Sci Rev. 1976;7:3.
16. Nitzan, DW, Samson, B, Better, H. Long-term outcome of arthrocentesis for sudden onset, persistent severe closed lock of the temporomandibular joint. J Oral Maxillofac Surg. 1997;55:151.
17. Milam, SB, Schmitz, JP. Molecular biology of temporomandibular joint disorders: proposed mechanisms of disease. J Oral Maxillofac Surg. 1995;53:1445.
18. Nitzan, DW. Intraarticular pressure in the functioning human temporomandibular joint and its alteration by uniform elevation of the occlusal plane. J Oral Maxillofac Surg. 1994;52:671.
19. Holmlund, A, Ekblom, A, Hansson, P, et al. Concentrations of neuropeptide substance P, neurokinin A, calcitonin gene-related peptide, neuropeptide Y, and vasoactive intestinal polypeptide in synovial fluid of human temporomandibular joint: a correlation with symptoms, signs, and arthroscopic findings. Int J Oral Maxillofac Surg. 1991;20:228.
20. Israel, HA, Saed-Nejad, R, Ratliffe, A. Early diagnosis of osteoarthrosis of the temporomandibular joint: correlation between arthroscopic diagnosis and keratan sulfate levels in the synovial fluid. J Oral Maxillofac Surg. 1991;49:708.
21. Quinn, JH, Bazan, NG. Identification of prostaglandin E2 and leukotriene BA4 in the synovial fluid of painful dysfunctional temporomandibular joints. J Oral Maxillofac Surg. 1990;48:968.
22. Blaustein, D, Scappino, RP. Remodeling of the temporomandibular joint disk and posterior attachment in disk displacement specimens in relation to glycosaminoglycan content. Plast Reconstr Surg. 1986;78:756.
23. Riggs, RR, Rugh, JD, Borghi, W. Muscle activity of MPD and TMJ patients and nonpatients. J Dent Res. 1982;61:277. [(abstract).].
24. Plesh, O, Curtis, D, Levine, J, et al. Amitriptyline treatment of chronic pain in patients with temporomandibular disorders. J Oral Rehabil. 2000;27:834–841.
25. Kreisberg, MK. Tricyclic antidepressants: analgesic effect and indications in orofacial pain. J Craniomandib Disord. 1988;2:171–177.
26. Raigrodski, AJ, Mohamed, SE, Gardiner, DM. The effect of amitriptyline on pain intensity and perception of stress in bruxers. J Prosthodont. 2001;10:73–77.
27. Cohen, SP, Mullins, R, Abdi, S. The pharmacologic treatment of muscle pain. Anesthesiology. 2004;101:495–526.
28. Erg-King, T, Jankovic, J. Treating severe bruxism with botulinum toxin. J Am Dent Assoc. 2001;131:211.
29. Von Lindern, JJ. Type A botulinum toxin in the treatment of chronic facial pain associated with temporomandibular dysfunction. Acta Neurol Belg. 2001;101:39.
30. Kopp, S, Carlsson, GE, Haraldson, T, et al. Long-term effect of intraarticular injections of sodium hyaluronate and corticosteroid on temporomandibular joint arthritis. J Oral Maxillofac Surg. 1987;45:929.
31. Poswillo, D. The effects of intraarticular deposition of betamethasone in the goat temporomandibular joint: discussion. J Oral Maxillofac Surg. 1995;52:1440.
32. Medlicott, MS, Harris, SR. A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training, and biofeedback in the management of temporomandibular disorder. Phys Ther. 2006;86:955–973.
33. Sturdivant, J, Fricton, JR. Physical therapy for temporomandibular disorders and orofacial pain. Curr Opin Dent. 1991;1:485–496.
34. Maloney, G. Effect of a passive jaw motion device on pain and range of motion in TMD patients not responding to flat plane intraoral appliances. J Craniomandibular Pract. 2002;20:55–56.
35. Hertling, D, Kessler, R. Management of common musculoskeletal disorders: physical therapy principles and methods, ed 2. Philadelphia: JB Lippincott, 1990.
36. Richardson, JK, Iglarsh, AI. Clinical orthopaedic physical therapy. Philadelphia: WB Saunders, 1994.
37. Griffin, JE, Karselis, GD, Terrence, C. Ultrasonic energy in physical agents for physical therapists. Springfield, IL: Charles C Thomas, 1979.
38. Travell, JG, Simons, DJ. Myofacial muscles in myofascial pain and dysfunction: the trigger point manual. Baltimore: Williams & Wilkins, 1983.
39. Nitzan, DW. Arthrocentesis for management of severe closed lock of the temporomandibular joint: current controversies in surgery for internal derangement of the temporomandibular joint. Atlas Oral Maxillofac Surg Clin North Am. 1994;6:245.
40. Sanders, B, Buoncristiani, R. Diagnostic and surgical arthroscopy of the temporomandibular joint: clinical experience with 137 procedures over a two year period. J Craniomandib Disord. 1987;1:202.
41. McCain, J, Podrasky, A, Zabiegalskin, NA. Arthroscopic disc repositioning and suturing: a preliminary report. J Oral Maxillofac Surg. 1992;50:568.
42. Moses, J, Sartoris, D, Glass, R, et al. The effect of arthroscopic surgical lysis and lavage of the superior joint space on TMJ disk position and mobility. J Oral Maxillofac Surg. 1989;47:674.
43. Mazzonetto, R, Spagnoli, DB. Long-term evaluation of arthroscopic diskectomy of the temporomandibular joint using holmium YAG laser. J Oral Maxillofac Surg. 2001;59:1018–1023.
44. Zeitler, D, Porter, B. A retrospective study comparing arthroscopic surgery with arthrotomy and disc repositioning. In: Clark G, Sanders B, Bertolami C, eds. Advances in diagnostic and surgical arthroscopy of the temporomandibular joint. Philadelphia: WB Saunders, 1993.
45. Bertolucci, LE. Postoperative physical therapy in temporomandibular joint arthroplasty. Cranio. 1992;10:211–220.
46. Dolwick, MF. Disc preservation surgery for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg. 2001;59:1047.
47. McKenna, SJ. Discectomy for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg. 2001;59:1051.
48. Tucker, MR, Jacoway, JR, White, RP, Jr. Use of autogenous dermal graft for repair of TMJ meniscus perforations. J Oral Maxillofac Surg. 1986;44:781.
49. Tucker, MR, Kennady, MC, Jacoway, JR. Autogenous auricular cartilage implantation following discectomy in the primate temporomandibular joint. J Oral Maxillofac Surg. 1990;48:38.
50. Sanders, B, Buoncristiani, RO. Temporomandibular joint arthrotomy: management of failed cases. Oral Maxillofac Surg Clin North Am. 1989;1:944.
51. Bell, WH, Yamaguchi, Y, Poor, MR. Treatment of temporomandibular joint dysfunction by intraoral vertical ramus osteotomy. Int J Adult Orthodon Orthognath Surg. 1990;5:9.
52. Hall, HD, Navarro, EZ, Gibbs, SJ. One- and three-year prospective outcome study of modified condylotomy for treatment of reducing disk displacement. J Oral Maxillofac Surg. 2000;58:7–17.
53. Lindqvist, C, Jokinen, J, Paukku, P, et al. Adaptation of autogenous costochondral grafts used for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 1988;46:465.
54. Kent, JN, Misiek, DJ, Akin, RK, et al. Temporomandibular joint condylar prosthesis: a ten-year report. J Oral Maxillofac Surg. 1983;41:245.
55. Mercuri, LG. The use of alloplastic prostheses for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58:70.
56. Mercuri, LG. Considering total temporomandibular joint replacement. Cranio. 1999;17:44.
57. Ko, EW, Huang, C, Chen, Y. Temporomandibular joint reconstruction in children using costochondral grafts. J Oral Maxillofac Surg. 1999;57:789–800.
58. Stucki-McCormick, SU. Reconstruction of the mandibular condyle using transport distraction osteogenesis. J Craniofacial Surg. 1997;8:48–53.