Major trauma
PRE-HOSPITAL ASSESSMENT AND INTERVENTION
PRELIMINARY HOSPITAL MANAGEMENT OF MULTIPLE AND SERIOUS INJURIES
Introduction
Major trauma is a relatively rare event in the UK but much more common in other parts of the world, some with higher rates of road traffic collisions (e.g. Saudi Arabia) and others higher levels of personal violence (e.g. South Africa, parts of the USA). Nevertheless, major trauma is the most common cause of death in young people almost everywhere.
For victims who survive the immediate trauma, there are two periods with a particularly high risk of death. The first occurs during the first or ‘golden’ hour after the accident and the second over the next few hours. Survival in the golden hour depends on the severity of injury, the competence of immediate care and the speed of transfer to an accident unit (in the UK, the average time to transport a non-trapped trauma victim to hospital is a surprising 57 minutes). Deaths after the first hour are for the most part avoidable, being largely caused by treatable conditions.
Pre-hospital assessment and intervention
Introduction
The golden hour concept comes from US war experience, popularised by Dr R. Adams Cowley. More recently, following the conflict in Afghanistan, this has been expanded to include the ‘platinum 10 minutes’ during which immediate interventions, particularly in haemorrhage control, may be key determinants of patient survival. Injuries with substantial internal or external bleeding lead to rapid circulatory decompensation; the only effective treatment is expert shock management and surgical arrest of bleeding. Thus, shortening the interval between injury and treatment gives the best chance of survival. The key is rapid essential care at the scene and swift transport to a trauma centre. This strategy is known as scoop and run, as opposed to stay and play, which is best for less severe cases; in these, the risk of physiological derangement caused during transport may be greater than extending the period before hospital treatment.
Assessment at the scene of a road traffic collision
‘Reading the wreckage’ used to foretell patterns and severity of injury to passengers. However, modern cars have sophisticated crumple zones and major vehicle distortion may not cause severe injury, though severe injuries can occur with minor damage. The worst injuries tend to occur in head-on collisions or those affecting the front corners. Some estimate can also be made of whether there was a high- or low-velocity impact. If passengers were killed or thrown out, this indicates a high-velocity impact. Points to check include whether head restraints were in place, whether seatbelts were worn and whether airbags were deployed. For motorcycle crashes, it is best to assume that all victims have pelvic fractures until proved otherwise. When a pedestrian is hit by a car, a ‘bullseye’ fracture of the windscreen indicates a likely severe head injury.
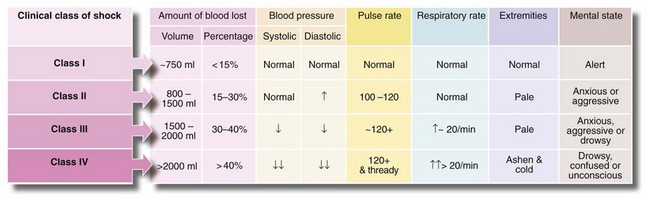
Obvious injuries (e.g. traumatic amputations) are sought in the victims and their level of consciousness and mobility assessed. Trapped wounded need special treatment as they often have long extrication times and need analgesia, intravenous fluids and perhaps sedation to aid release. Trapped patients can quickly become hypothermic and hypovolaemic (see Fig. 15.1).
Preventing secondary injuries and damage
Primary injuries result directly from the trauma. Secondary injuries are an indirect result, e.g. secondary brain damage from hypoxia, fat embolism from fractures, spinal cord damage due to unstable spinal injury. Most are preventable with good immediate care, careful handling, rapid resuscitation and perhaps elective ventilation. Early stabilisation of long bone fractures aids haemodynamic stability, allowing assessment of less urgent head, chest or abdominal injuries.
Pre-hospital care
The guiding principle for the emergency field team is rapid transfer to an appropriate hospital; pre-hospital interventions are limited to essentials. A need for endotracheal intubation is the main intervention to delay transportation but occasionally anaesthetising the patient buys time before direct transfer to a specialised unit.
Airway and breathing: The airway must be assessed and secured first, whilst ensuring the cervical spine is immobilised. If the patient can speak, assume the airway is patent, ventilation is intact and the brain adequately perfused. Agitation, however, may be a sign of hypoxia. In an unconscious or semi-conscious patient, the airway can usually be temporarily secured with a jaw thrust. If tolerated, the patient should then have two nasopharyngeal airways and a Guedel oropharyngeal airway placed to maintain airway patency. Endotracheal intubation is needed if there is inability to maintain or protect the airway or to provide adequate ventilation (Box 15.1). If this proves unattainable, a useful rescue technique is to insert a laryngeal mask (LMA), as used in general anaesthesia; this may avoid the need for a surgical airway. As a last resort, an airway can be achieved using a needle or surgical cricothyroidotomy. In all seriously injured patients, high-flow oxygen therapy (15 L/min) is mandatory.
Spine: In an unconscious patient after a high-impact collision, a cervical spine fracture should be assumed until disproved. If the patient has multiple injuries, the entire spine must be protected from secondary injury during transfer and assessment. After intubation (if needed), the spine is immobilised in a neutral position on a long spinal board. This requires a semi-rigid cervical collar, side head supports and strapping as a minimum (see Fig. 15.2).
Circulation: Two large-bore intravenous cannulas should be inserted. Initial fluid resuscitation should be based upon injuries sustained and physiological parameters. More recent studies indicate that permissive hypotension is often a better strategy than the previous recommendation of rapid indiscriminate crystalloid infusion. If organ perfusion can be maintained, there are advantages in keeping the pressure low in trauma patients. Physiological compensation is effective at systolic pressures between 70 and 85 mmHg, and cerebral perfusion and urinary output are well maintained. Above this pressure, fresh clot is often dislodged (‘pop a clot’) and then bleeding recurs. A further disadvantage of unnecessary fluid resuscitation is that infusing just 750 ml of crystalloid activates cytokines and causes dilutional coagulopathy.
If a patient is unconscious without a palpable radial or pedal pulse, 250–500 ml of fluid is given immediately, followed by small boluses, repeated only until the point at which a pulse returns. This is titration by pulse and has been successfully employed in major trauma and in military campaigns. If intravenous access is unsuccessful, EZ-IO devices (Fig 15.3) are a quick way of inserting a cannula into bone marrow. Procoagulant agents such as tranexamic acid and activated factor VII are increasingly being used early to reduce blood loss following trauma. If a patient is conscious and orientated or unconscious but has a palpable radial pulse, this indicates a systolic of above 90 mmHg and fluid resuscitation is not started.
Transport to hospital
Injured patients need to be transferred rapidly to an appropriate hospital. Most go by ambulance, but transfer by helicopter can be quicker if the severity of injuries requires a major trauma centre. Note that whilst helicopters can cover great distances quickly, they have inherent disadvantages, namely the risk of secondary injury or displacement of lines or tubes during loading, restricted space for ongoing resuscitation and the risk of pneumothorax associated with changes in altitude.
Preliminary hospital management of multiple and serious injuries
Organisation of the accident department
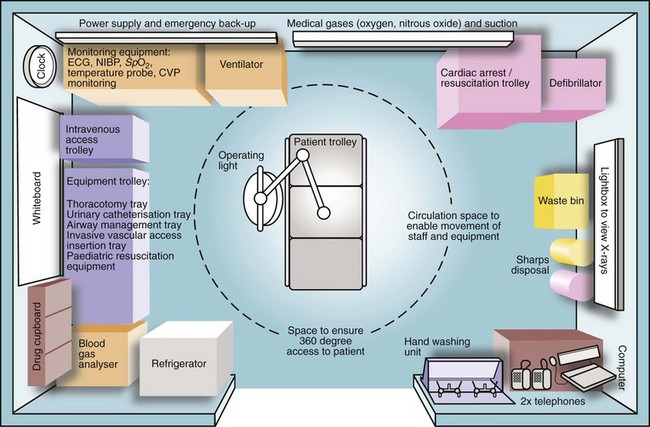
Every accident department should have a major disaster plan (Box 15.2). For any major trauma, the field team or ambulance service informs the receiving trauma unit about the impending arrival of seriously injured patients, plus an estimate of numbers and the nature and severity of injuries. This alerts the surgical and anaesthetic teams to be ready when the patients arrive (Box 15.3). Trauma units have a resuscitation room (see Fig. 15.4) with all necessary equipment so infusion sets can be prepared and drugs laid out.
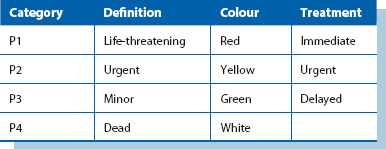
Triage is the process of sorting patients into ‘priority of treatment’ groups on arrival to enable efficient use of resources. The usual categories are shown in Table 15.1.
Success in managing patients with life-threatening multiple injuries depends on good organisation. It involves concurrent activity between several professionals but with one person, often the surgeon, designated team leader. The team leader takes overall medical responsibility as well as coordinating all clinicians.
Initial care in the accident department
When seriously injured patients reach the resuscitation room, the golden hour peak of deaths has passed. The main danger of death is from hypovolaemia (intrathoracic or intraperitoneal haemorrhage, blood loss from fractures) or from an expanding intracranial haematoma.
Immediate priorities after reaching hospital are:
Training has been standardised through Advanced Trauma Life Support (ATLS) courses, originally from the American College of Surgeons and now run in many countries. ATLS principles are simple—the greatest threats to life must be treated first. Mortality at this stage following major trauma is now recognised as associated with three key pathophysiological changes termed the ‘lethal triad’ and comprising coagulopathy, hypothermia and acidosis. Damage control resuscitation has emerged as a means of directly minimising these changes, the key components of which are outlined in Box 15.4.
Assessment of the seriously injured patient: Despite the urgency, primary assessment must be performed systematically as soon as the patient arrives. The primary survey includes a rapid evaluation, resuscitation and crucial life-preserving treatment. Priorities are summarised in Figure 15.5. Meanwhile, regular monitoring takes place (Box 15.5).
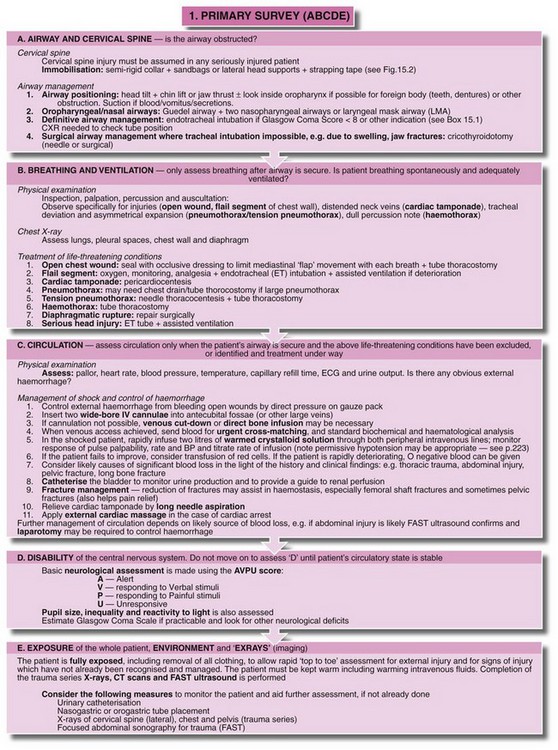
Fig. 15.5 Primary survey and initial resuscitation
Management priorities for the patient with multiple injuries. In practice, anaesthetists usually deal with the airway and intravenous access and monitoring while surgeons evaluate the head and neck, chest, abdomen and pelvis for potential life-threatening injuries
A rapid history is taken whenever practicable, often alongside the secondary survey. A useful mnemonic for this is AMPLE:
Other elements of history come from the field team's notes and include:
• Conscious level of patient when discovered and later changes
• Details of drugs, fluids and other treatments administered at scene
Conscious patients with suspected cervical spine injuries should be moved with extreme caution and no passive movements attempted. The patient should perform active movements; spasm or pain restricts movement in significant injury. To examine the back and perform a rectal examination, the patient should be ‘log-rolled’ by several people.
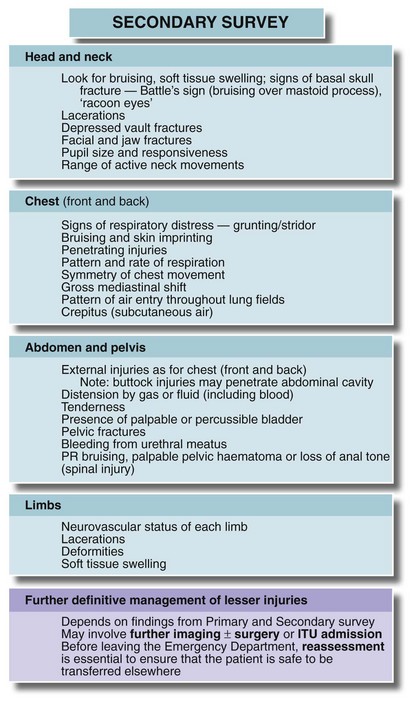
A secondary survey then assesses the potential for life-threatening problems or complications, although urgent initial treatment may delay this. The key clinical features are given in Figure 15.6; individual systems are described later. Up to 20% of multiple injury patients have injuries missed in the early stages so the secondary survey must be repeated.
Recording of events: The time of examination and the clinical findings, plus details of investigations and treatments, must be recorded in the patient's notes, not least for medico-legal purposes.
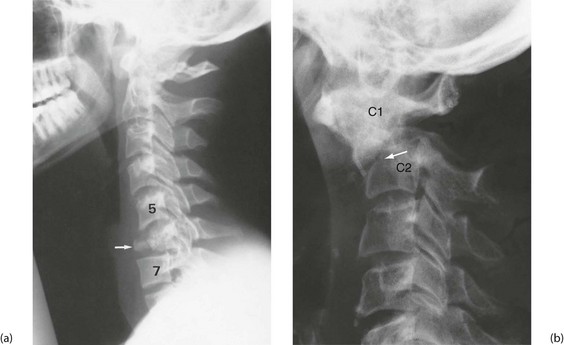
X-rays and other investigations: In major trauma, the cervical spine (see below, Fig. 15.10), chest and pelvis are X-rayed in the resuscitation room. The chest films must be good enough to exclude major chest wall, mediastinal and lung injuries and provide a baseline if the patient later deteriorates. Polytrauma patients, or patients with serious head injury should have rapid assessment and stabilisation before swift transfer for trauma CT scan. Patients should not be moved to the CT scanner until they are stable—the machine is known as the ‘donut of death’ in ATLS parlance.
Focused abdominal sonography for trauma, or FAST (see Abdominal injuries, below), is performed in the emergency department for suspected abdominal injuries and bleeding. Initial blood tests include haemoglobin and group and cross-match or antibody screen and ordering of an appropriate amount of blood. In a desperate emergency, universal donor blood (group O, Rh negative) can be transfused. Evidence from recent conflicts has demonstrated the advantages of early administration of blood products in reducing the risk of haemodilution and coagulopathy. Emergency departments are increasingly using ‘blood packs’ which include several units of packed red cells, fresh frozen plasma and platelets. These may be transfused in a 1 : 1 : 1 ratio or in a goal-directed manner, guided by coagulation testing and thromboelastography. Plasma electrolytes and glucose are measured, plus arterial blood gases if there is suspicion of respiratory failure.
Abdominal injuries
Introduction
Abdominal and thoracic injuries often coexist, so it is logical to think in terms of torso trauma. Major torso injuries are a common cause of death at the trauma scene, for example from avulsion of the thoracic aorta, cardiac injury or massive liver injury. Immediate diagnosis and urgent laparotomy or thoracotomy offers almost the only hope of survival, but the injury is often too extensive or time too short to intervene.
The site and signs of external injury provide clues to internal injuries. This is obvious with penetrating injuries but is also true of blunt injuries. For example, trauma to the left upper abdominal quadrant or lower ribs is often coupled with splenic rupture; similarly for the liver with right-sided injuries. Lower abdominal injuries may injure the bladder, and loin trauma the kidney. Central anterior chest trauma can damage the heart whilst clavicular area injury may traumatise the brachial plexus or subclavian blood vessels.
Abdominal injuries are rare compared with head and chest injuries and mortality can be low with prompt and appropriate management. When death occurs, it is usually from massive haemorrhage arising from bursting of liver or spleen or from penetration of major arteries or veins, particularly with gunshot wounds. Note that unrecognised injuries are the principal avoidable cause of death.
Areas of the abdomen other than the main peritoneal cavity may be wounded; pelvic viscera lie within a bony cage but extend low enough to be injured by buttock or perineal wounds. Similarly, retroperitoneal viscera may seem protected but are vulnerable to flank or back wounds, or to deep anterior stab wounds or any gunshot wounds. This area is not easily palpated and diagnosis requires cross-sectional imaging.
Overall, 20% of patients with closed abdominal trauma require operation. In penetrating injuries, 30% with stab wounds require operation and close to 100% of those with gunshot wounds.
Diagnosis of abdominal injuries
Clinical diagnosis is unreliable in blunt injuries because overt signs of bleeding or hollow viscus perforation may not develop until hours after injury. If the patient is stable but the accident involved high energy transfer or other significant injuries are present, early CT scanning should be performed.
Clinical observation: If surgical intervention is not needed, regular nursing observations and serial clinical examination by a doctor should be performed for signs of peritonitis or intra-abdominal bleeding. Note that significant injuries almost always become manifest within 24 hours.
Focused abdominal sonography for trauma (FAST): FAST reliably detects free intra-abdominal fluid and concentrates on five areas, the ‘five Ps’—Perihepatic, Perisplenic and Pelvic in the abdomen and Pleural and Pericardial in the chest. It is, of course, user-dependent.
CT scanning for abdominal injuries: CT can identify injuries to all solid abdominal and retroperitoneal organs (liver, spleen, pancreas and kidney), bowel perforations (indirectly by detecting free gas and fluid), diaphragmatic rupture, retroperitoneal blood and pelvic and spinal fractures. This may allow conservative management of less severe splenic and liver injuries. CT is also valuable for defining the extent and configuration of complex pelvic fractures.
Penetrating abdominal wounds
Stab wounds and other sharp abdominal wounds
Stab wounds may or may not penetrate the peritoneal cavity. They often cause little damage unless the blade penetrates the retroperitoneal area and injures great vessels or pancreas. It used to be thought that all abdominal stab wounds required surgical exploration but current policy in most cases is more conservative management. A large series from Baragwanath Hospital, Soweto, South Africa, demonstrated that 70% of patients, or more, could safely be managed by observation in hospital for 24 hours, and operated upon only if there were signs of deterioration. However, haemodynamically unstable patients and those with extensive or potentially contaminated penetrating wounds must be explored surgically without delay.
For most patients, the first step is to determine whether the peritoneum has been breached, by exploring the wound under local anaesthesia. If it has, then laparoscopy, ultrasonography or CT scanning can be employed to explore intra-abdominal viscera. If the peritoneum is intact and/or imaging is negative (as in most cases), conservative management with careful monitoring is appropriate. However, about one-third who later proved to have significant injury were initially free of signs, emphasising the need for repeated clinical and radiographic reassessment.
Bullet and other missile injuries
The severity of internal injury depends on the path and mass of the missile and especially on its velocity. Low-velocity wounds (e.g. hand-gun bullets) cause damage confined to the wound track, whereas high-velocity (i.e. rifle) bullet wounds injure widely and deeply. This is because the much higher kinetic energy is dissipated in the tissues. In addition, cavitation is caused and debris is sucked into the wounds, causing contamination with clothing and soil. If a bullet hits bone, secondary missiles cause further injury. The size of the entry wound is often small because of elastic recoil of the skin and is no guide to the extent of injury. Given the unpredictable extent of injuries, all gunshot wounds must be surgically explored to check for visceral organ, intestinal and vascular damage. Buttock wounds should be treated in the same way.
Closed (blunt) abdominal injuries
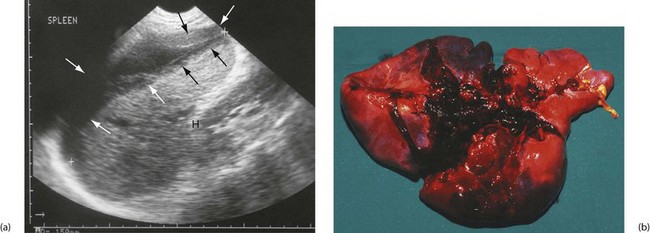
Closed abdominal injuries usually result from road traffic collisions, falls, sporting contact injuries and accidents involving horses. Following substantial blunt injury, about 20% will require laparotomy. The spleen is the most vulnerable organ, especially in left-sided injuries (see Fig. 15.7). Liver injury requires greater impact force, usually from the front or right side. Pancreatic and duodenal injuries are uncommon and usually result from a heavy central abdominal impact, transsecting the pancreas or retroperitoneal duodenum across the vertebral bodies. This most commonly occurs in children falling across the handlebars of bicycles. The kidneys are vulnerable to punches or kicks in the loins.
Bowel is damaged by rapid deceleration or crushing, and is particularly vulnerable at sites where freely mobile bowel becomes attached to the retroperitoneum, i.e. at each end of the transverse colon, at the duodeno-jejunal flexure and in the ileocaecal area. A full bladder, common after a bout of heavy drinking, may rupture into the peritoneal cavity (or sometimes retroperitoneally) after abdominal impact. The bladder and urethra are also liable to be torn in displaced pelvic fractures. The clinical features and investigation of closed abdominal injuries are shown in Box 15.6.
Injuries to specific solid organs
Spleen (Fig. 15.7): The spleen is the most commonly injured organ in blunt abdominal trauma. The organ should be preserved wherever possible because of the dangers of post-splenectomy infection and sepsis. In one study, 2.4% of all post-splenectomy patients suffered sepsis and more than 50% of those were fatal.
CT scanning enables accurate assessment and classification of the extent of injury. Haematomas and capsular tears not extending deeply can often be managed conservatively. More severe injuries are treated by urgent laparotomy and where possible, splenic repair (splenorrhaphy) by direct suture, fibrin glue or absorbable mesh bags. Segmental resection or splenic artery ligation can be done, but 50% of splenic substance must be preserved for useful function. Whenever splenic preserving techniques are employed, a period of careful observation for up to 10 days is required as catastrophic secondary haemorrhage can occur.
Liver: Isolated small liver injuries may be treated by surgical repair or local resection but paradoxically, major injuries are often best treated conservatively. This is because control of deep hepatic vessels may prove impossible, particularly bleeding from hepatic veins entering the IVC. Patients with severe liver injuries should be discussed with a regional hepato-pancreatico-biliary (HPB) or liver unit. Conservative management involves large-volume blood transfusions until abdominal tamponade stops the bleeding. If operation is performed and a major liver injury is found and haemorrhage cannot be arrested, the liver should be packed with large pieces of surgical gauze, the abdomen closed and the patient stabilised. Ideally the patient should be transferred to an HPB centre as extensive liver surgery may be necessary when the packs are removed at a ‘second look’ laparotomy 24–48 hours later.
Injuries to small bowel are dealt with by simple suture or, if mesenteric vascular supply is impaired, by resection and anastomosis. Conventional treatment for right-sided colon injuries is resection and anastomosis of colon to ileum. Localised injuries to other parts of the colon without substantial faecal contamination can usually be resected and joined end to end. After knife or gunshot wounds, simple repair gives good results if there is minimal peritoneal contamination. Extensive injuries with contamination require exteriorisation of the damaged bowel ends to the abdominal wall (see Ch. 27).
High-velocity penetrating injuries wreak havoc on the gut, causing devascularisation and multiple perforations. All necrotic or ischaemic tissue must be excised. The immediate dangers are peritonitis and systemic sepsis from contamination. Exteriorisation of viable bowel ends is mandatory and planned re-exploration usual.
Lower urinary tract injuries
Intraperitoneal rupture of the bladder is treated by laparotomy and suturing, with a urethral catheter left in situ for 5–7 days. Extraperitoneal bladder rupture is treated conservatively, with prolonged urethral or suprapubic catheterisation. Urethral tears require specialist urological management. If the urethral wall is partly intact on urethrography, it can be treated, at least initially, by suprapubic catheterisation. Complete urethral avulsion injuries are usually treated by suprapubic catheterisation, with formal repair after inflammation has settled.
Damage control laparotomy
Major trauma patients sometimes have extensive and complex intra-abdominal injuries. In an unstable patient, prolonged surgery to manage these definitively greatly exacerbates the lethal triad of coagulopathy, hypothermia and acidosis. Damage control laparotomy can be employed here as a life-saving procedure that should be completed within an hour. Haemorrhage is controlled by temporary clamping, then packing or ligating vessels. Hollow viscus injuries are stapled or resected without anastomosis. The abdomen is temporarily closed and arrangements made for definitive surgery in 24–48 hours following resuscitation.
Chest injuries
The types of chest injury, their clinical features and their treatment are summarised in Table 15.2.
Table 15.2
Types of chest injury and their management
| Nature of the injury | Clinical features | Treatment |
| Sternal fracture | Anterior chest pain and tenderness; ‘clicking’ on palpation; arrhythmia and ECG changes | Consider cardiac contusion or tamponade; FAST scan; 24h ECG; cardiac enzymes |
| Rib fractures | Localised pain on respiration or coughing; tenderness over fractures; usually visible on chest X-ray | Analgesia, intercostal blocks, physiotherapy, prophylactic antibiotics in chronic bronchitics |
| Flail chest, i.e. multiple rib fractures producing a mobile segment | Respiratory embarrassment; ‘paradoxical’ indrawing of the flail segment on inspiration | Intercostal block analgesia; endotracheal intubation and ventilation if hypoxic |
| Pneumothorax, i.e. air in pleural cavity causing lung collapse | Unilateral signs: loss of chest movement and breath sounds, percussion note resonant; sometimes chest wall emphysema; confirmed by chest X-ray | Intercostal drain with underwater seal |
| Sucking chest wound, i.e. open pneumothorax with mediastinum ‘flapping’ from side to side with each respiration | Gross respiratory embarrassment, audible sucking of air through chest wound | Sealing of chest wound with impermeable dressing; intercostal drainage |
| Tension pneumothorax, i.e. expanding pneumothorax causing progressive mediastinal shift to the opposite side and tracheal deviation | Signs of pneumothorax with disproportionate and increasing respiratory distress and hypoxaemia | Urgent chest drainage |
| Lung contusion | Deteriorating respiratory function; opacification of affected lung field on chest X-ray | Oxygenation, physiotherapy, mechanical ventilation if severe |
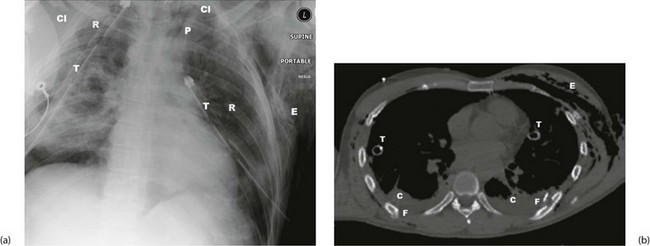
| Rupture of bronchus (uncommon) | Respiratory distress, surgical emphysema in the neck; suggested by air in mediastinum on chest X-ray (see Fig. 15.9a); confirmed by bronchoscopy | Operation by thoracic trained surgeon |
| Rupture of oesophagus (very rare) | May have surgical emphysema in neck and pneumomediastinum on CXR but diagnosis often missed until mediastinitis or empyema develops | Surgical repair if recognised early; surgical drainage and diversion if late |
| Haemothorax, i.e. blood in the pleural cavity Usually arises from chest wall injury—rib fracture, lung parenchyma or minor venous injury. Most are self-limiting. Arterial injuries less common and likely to need thoracotomy |
Dull percussion note, breath sounds absent, tachycardia and hypotension due to blood loss | Most have stopped bleeding by the time of examination and only tube drainage is required Dark, venous bleeding more likely to cease spontaneously than bright arterial bleeding Tube must be large enough to drain without clotting, ideally 32–36°F; placed in sixth intercostal space in mid-axillary line If patient haemodynamically stable, admit and observe. If continuing drainage of 200 ml+ per hour over 4 hours, should undergo thoracotomy |
| Cardiac tamponade, i.e. bleeding into pericardial cavity (usually penetrating trauma) | Hypotension, inaudible heart sounds, distended neck veins with systolic waves; enlarged, rounded heart shadow on chest X-ray; confirmed with ultrasound | Long needle aspiration via epigastric approach; operation if tamponade recurs |
| Cardiac contusion | Often arrhythmia or ECG changes similar to myocardial infarction | Conservative management |
| Rupture of aorta (usually from deceleration injury)—fatal unless false aneurysm develops in mediastinum | Back pain, hypotension; systolic murmur or signs of tamponade in some cases; characteristic widening of mediastinum on chest X-ray; diagnosis confirmed by arteriography | Urgent thoracotomy and Dacron graft or minimal-access stent graft if available |
| Rupture of diaphragm, linear split usually in left diaphragm with herniation of gut into chest (penetrating or abdominal crush injury) | Respiratory distress, bowel sounds heard in the chest; diagnosis by chest X-ray and confirmed by barium meal; many cases only discovered much later; diagnosis may be made by laparoscopy or at laparotomy | Repair of diaphragm, usually via abdominal approach |
General principles
Chest injuries are a common cause of death in patients with multiple injuries, although the death rate has fallen dramatically wherever seatbelt wearing is compulsory. Seatbelts, however, often cause typical sash pattern bruising obliquely across the chest, and minor rib and sternal fractures (Fig. 15.8). Serious chest injuries may be present without external injury, particularly tearing of mediastinal contents (aorta, bronchi and oesophagus). Diagnosis goes hand in hand with urgent resuscitation. Good-quality chest X-rays (or CT scans) are essential and usually reveal the diagnosis (see Fig. 15.9).
Mechanisms of chest injury include penetrating trauma, blunt impact and crushing injuries, deceleration injuries and rupture of the diaphragm caused by abdominal compression. Less than 10% of chest injuries require surgical intervention but early recognition of these may be life-saving.
Thoracostomy (open and tube)
Following trauma, chest drains are usually placed in the fourth or fifth intercostal space on the mid-axillary line. The technique is shown in Figure 31.6, p. 402. Bilateral open thoracostomy is often used in pre-hospital care in ventilated patients (particularly during helicopter transfer) as a precursor to formal chest drain insertion.
Vascular trauma
Veins and arteries may be damaged by penetrating or blunt trauma. Gunshot wounds are more likely to damage vessels than stab wounds, and blunt injuries can damage arterial walls causing occlusion. Iatrogenic injuries are becoming common with the rise in radiological and minimal access procedures, and hip replacements. Damaged vessels bleed or impair distal circulation, or both.
Bleeding
Bleeding may be revealed (visible), or concealed and the rate of loss determines the presentation and risk of death. Concealed haemorrhage often occurs in the chest, abdomen or pelvis or in limb muscles with fractures; blood from facial fractures may be swallowed and unrecognised.
Ischaemia
Trauma that interrupts arterial flow to a limb or organ causes ischaemia, leading to potential limb or organ loss, stroke, bowel necrosis, and consequent multiple organ dysfunction. Skeletal muscle can survive ischaemia for 3–6 hours and still recover but peripheral nerves are sensitive and deficits can result from brief ischaemia.
If arterial supply is restored after delay, the release of inflammatory mediators, lactic acid and potassium into the circulation can cause reperfusion syndrome. In limbs, this can lead to compartment syndrome, and can also initiate a systemic inflammatory response with myocardial and other organ dysfunction.
Patterns of vascular injury
Laceration is the most common. Completely severed arteries contract, limiting haemorrhage, but partially transsected arteries continue bleeding. Veins are unlikely to retract.
Blunt trauma causes crushing, stretching or shearing injures to vessels. Intimal flaps can lead to thrombosis or dissection. Thrombosis may propagate down the vessel or embolise distally. Arterial ‘spasm’ alone does not cause limb ischaemia—the cause is thrombosis or vessel wall damage and requires urgent investigation.
False aneurysm: An arterial puncture (e.g. femoral artery catheterisation or a stab wound) may cause bleeding that is enclosed by connective tissue, forming a pulsatile mass of clot known as a false aneurysm. This often presents days or weeks later. Distal flow is usually conserved and diagnosis can be confirmed by duplex Doppler ultrasound. First-line treatment is usually ultrasound-guided compression to cause thrombosis of the leak. If this fails, or for larger defects, suturing or patching may be needed.
Arteriovenous fistula: An injury to an artery and an adjacent vein can cause an arteriovenous (AV) fistula, which may eventually rupture or lead to cardiovascular compromise. These present some days or weeks after the injury. In a limb, the patient complains of a swelling with dilated superficial veins. On examination, there is a machinery-type murmur heard and diagnosis is confirmed by angiography. Treatment is by dividing the fistula and repairing the vein and artery, sometimes with a flap of fascia interposed.
Diagnosis of vascular injury
Clinical signs: Visible bleeding from a traumatic wound with signs of hypovolaemia make the diagnosis obvious. In limbs, palpable distal pulses are the most reliable sign of intact distal circulation. Hand-held Doppler probes can be misleading in detecting distal pulses and in ankle pressure measurement.
The following ‘hard’ signs of vascular injury indicate a need for urgent operative intervention, often without prior investigation:
Patients with the following ‘soft’ signs of vascular injury do not require urgent investigation or exploration; they should be admitted, investigated as needed and observed over 24 hours.
Investigation: In expert hands, Duplex ultrasound can detect intimal tears, thrombosis, false aneurysms and arteriovenous fistulae, but angiography by direct puncture, CT angiography or on the operating table remains the gold standard for investigation and mapping of vascular injury. Arteriography may be needed to show the extent of injury in a stable patient with equivocal signs; to exclude injury where there are no hard signs but suspicion of vascular injury; in limb fractures with absent pulses; in injury by high-velocity missiles or multiple fragment injuries; and in blunt trauma. Angiography may be used to treat certain injuries by embolisation or stenting where expertise is available.
Management of vascular injury
The priorities in managing vascular injury are arrest of life-threatening haemorrhage and restoration of normal circulation. Temporary bleeding control is usually achievable by pressure over the site of injury, NOT with tourniquets.
Direct exploration of an actively bleeding wound is usually inadvisable because of poor visibility and the technical difficulty of achieving control. Far better to obtain proximal control, if necessary via a separate incision, isolating and clamping the artery before exploring the wound. Sometimes the artery distal to the wound needs clamping remotely too.
With proximal and distal clamps in situ, the wound is explored, debrided and the extent of arterial and venous damage assessed. Generally, large veins should be repaired first to allow drainage as soon as the artery is repaired. A cut or lacerated artery may be amenable to direct repair or to patching, if direct suturing would narrow the lumen. More extensive damage may require an interposition graft, usually autologous long saphenous vein, or sometimes synthetic graft material. Before repair, proximal then distal clamps are released in turn to check for adequate blood flow. If inadequate, a Fogarty balloon catheter is passed to extract thrombus and heparinised saline instilled.
Compartment syndrome: Delayed revascularisation of a limb risks compartment syndrome (see Ch. 17, p. 235). Prophylactic fasciotomy should be performed at the time of repair in these circumstances, particularly if the patient is ventilated or has an epidural, as these mask the symptoms of developing compartment syndrome.
Damage control in vascular injury
Vessel ligation: In extreme conditions, most vessels can be ligated. The common and external carotid, subclavian, axillary or internal iliac can be ligated with little consequence, but internal carotid ligation carries a 10–20% risk of stroke, and ligation of external iliac, common or superficial femoral arteries has a high risk of causing critical limb ischaemia. Coeliac axis arteries can be ligated, but not the superior mesenteric which would lead to bowel ischaemia. Almost any vein can be ligated, including the inferior vena cava (but this causes lower limb oedema).
Interventional radiology in vascular injury
Interventional radiology is increasingly used in trauma as a means of controlling haemorrhage without need for a surgical procedure. In pelvic fractures, angiography and embolisation has become the gold standard for control of bleeding from iliac vessels; this remains the only firm indication for interventional radiology in unstable patients. In stable patients, embolisation can be used to control bleeding from solid organs (e.g. in splenic laceration) and covered stents can be deployed across major vessel disruptions (e.g. traumatic rupture of the thoracic aorta).
Orthopaedic trauma
This section contains a brief introduction to the main points of fracture management, followed by detail on spinal and pelvic injuries.
• Pain—major orthopaedic injuries are extremely painful so good analgesia and early reduction is an important part of treatment, contributing to early mobilisation and reducing the potential for deep venous thrombosis (DVT)
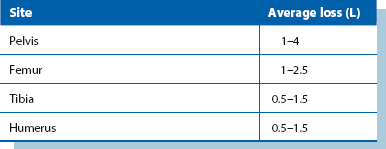
• Blood loss—internal blood loss from fractures is often substantial (see Table 15.3), particularly if there are multiple fractures, and blood volume needs to be appropriately replaced. In pelvic fractures, external fixation may reduce blood loss
• Deformity—obvious deformity should be corrected as soon as possible using temporary splinting. This treats pain and may assist vascular supply and limit blood loss
• Vascular and neurological integrity—where limbs are involved, this should be checked and appropriate investigation and intervention arranged
• Definitive fixation of fractures may be needed early or may have to be deferred until other life-threatening injuries have been dealt with
Introduction: A fracture is when there is a break in continuity of a bone. Fractures are classified so patterns of injury can be recognised, and the best treatment of any subtype agreed by consensus. Fracture patterns are linked to anatomical location, and mechanism and energy of injury. Eponymous fracture classifications are used in some countries, whereas objective systems such as the Swiss AO system (Arbeitsgemeinschaft Osteosynthesefragen) prevail elsewhere (see Box 15.7).
Bone is strong in compression but weaker in resisting torsional or bending forces. A footballer landing on one foot loads the tibia in compression and this is stable, but with a twisting force in addition, torsion is applied and it fractures. A pure bending force when falling from a height onto a forearm causes fracture, as the energy is applied where the bone is weakest. As velocity increases, high energy transfer collisions can fracture the bone in multiple places (Force = Mass × Velocity2).
Fracture healing: Fractures heal by restoring bone continuity. Cancellous bone heals more quickly than cortical bone and some movement at fracture sites stimulates healing. Healing needs a good blood supply so rates of healing are more rapid in children.
Healing can be considered in five stages: first, the bone ends bleed causing a haematoma, and periosteum is stripped from bone. Soft tissues may also be damaged. Second, acute inflammation and cell division begins within 8 hours. Third, osteoblasts proliferate in periosteum and callus forms. This is a heterogenous mixture of woven bone (from osteoblasts) and hyaline cartilage from chondroblasts. Osteoclasts resorb dead bone. In stage four, orderly lamellar bone replaces woven bone and the fracture becomes united. Lastly, during remodelling, the bone recovers its normal shape and any medullary cavity is restored.
Principles of fracture management: These include reduction, immobilisation and later, rehabilitation. The need for reduction depends on the fracture. Rotational, valgus or varus deformity usually needs correcting and intra-articular fractures need precise anatomical reduction. Reduction can be performed as a closed or open procedure.
Immobilisation by external or internal methods is then needed until fractures unite. External methods include plaster casts, traction and external fixation. Internal methods include plates, intramedullary nails and K-wires.
Initial management of fractures: First aid minimises pain and reduces the risk of secondary damage. Broken bones are usually acutely painful and deviation causes pressure on skin and neurovascular structures. Initial treatment in the field involves assessing overlying wounds and applying dressings, reducing fractures into an immobilising splint or plaster and later, confirming the diagnosis with X-rays. These steps resuscitate the limb and soft tissues. They also reduce pain by limiting movement at the fracture site.
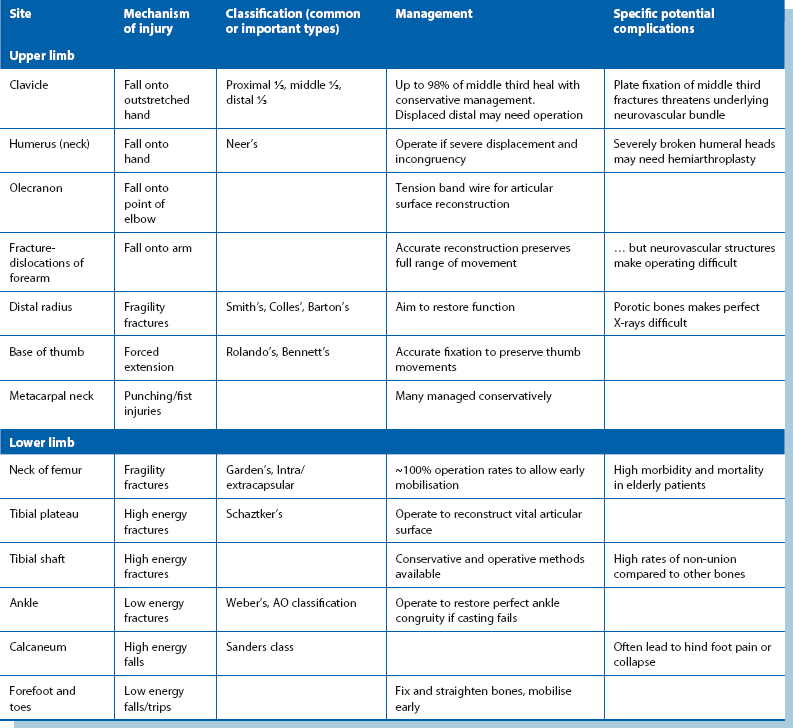
Definitive management of fractures (see Table 15.4): Fractures were able to heal long before orthopaedic surgery existed, but learning how to restore the anatomy and hold bones immobile while they healed was a major advance. Definitive management nowadays may be operative (open) or non-operative (closed). Operative treatment may not accelerate healing so the extra risks need to be justified. Complications include: infection, non-union, implant failure and refracture.
The main indications for operative treatment are: fracture types that require open reduction, unstable fractures, intra-articular fractures (to stabilise anatomical reduction), multiple injuries, elderly patients (to allow early mobilisation), long bone fractures (tibia, femur and humerus), where blood vessels or nerves need repair (to access and protect the repair), where conservative management has failed, and pathological fractures. A local capability of performing this surgery with low complication rates is also important.
Open (compound) fractures: These must all be assumed to be contaminated. First aid treatment is the same as for closed fracture, but open fractures require early operation, ideally within 6 hours of injury. At operation the wound is cleaned, devitalised tissue is debrided and the fracture stabilised. Small clean wounds can be sutured but large or dirty wounds should be left open and closed by delayed primary suture after about 5 days.
Pathological fractures: These occur in:
• Generalised bone diseases, e.g. osteoporosis or metabolic bone diseases (osteomalacia, hyperparathyroidism, Paget's disease)
• Localised benign bone disorders, e.g. chronic infection, solitary bone cysts, fibrous cortical defects or chondromas
• Malignant disease: metastatic cancers, myelomatosis, primary malignant bone tumours
Complications of fractures (see Box 15.8): The likelihood of complications depends on the mechanism of injury and the amount of force through the area at the moment of fracture. Sharp bone ends can perforate or crush nearby structures such as muscles, skin, blood vessels and rarely nerves; hyperextension of the knee can damage popliteal nerves. Prompt recognition and fracture reduction is crucial as fracture deformity continues to provoke inflammation and damage.
Malunion can lead later to disordered mechanical forces in the rest of the limb and back, and may cause osteoarthritis in nearby joints. Displaced intra-articular fractures with an irregular joint surface markedly increases friction, leading to post-traumatic osteoarthritis. Delayed union leads to long periods of disuse, and the entire limb can suffer from muscle atrophy, osteoporosis and joint contractures if not treated early. For Compartment syndrome, see Chapter 17, p. 235.
Specific fractures
Common upper limb fractures: The most common and their usual management are:
• Metacarpal neck—often left to heal in mildly angulated position
• Base of thumb metacarpal—fragments accurately reduced and fixed
• Distal radius—deformity reduced and fixed, e.g. Colles type
• Olecranon process—articular process reconstructed and fixed
These fractures each have typical patterns of presentation. For example, distal radius fractures are often in bone weakened by osteoporosis, and a simple fall from standing can cause an angulated and deforming fracture needing surgery. Conversely, entirely normal bone in the metacarpal neck can be fractured in young adults fighting with fists.
Common lower limb fractures: The most common lower limb fractures are:
Fragility fractures due to osteoporosis far outnumber the others and affect a large number of older patients. Femoral neck fracture still carries a high mortality. Operative treatment carries risks but is still the best method of restoring mobility and preventing death from other causes. Nevertheless death rates of 10–30% at 1 year are common.
Dealing with fragility hip fractures presents a challenge. Conservative treatment is rare nowadays, as spending 6 or more weeks in bed leads to high rates of venous thromboembolism, respiratory infection, pressure ulcers and death. These patients are often frail, with impaired cardiovascular and respiratory function, so surgical treatment requires anaesthetic risk assessment and optimising general health. There is a trend in the UK towards involving a dedicated care-of-the-elderly physician in assessing and managing all these patients. This, together with physiotherapists, dedicated theatres to minimise delays, modern surgical stabilisation techniques and skilled anaesthesia, provides optimum care and better outcomes.
Fracturing lower limb long bones in healthy adults requires substantial force. Typical patterns of tibial and femoral shaft fractures occur in motor vehicle accidents, falls from height and high energy collisions on the sports field.
Ankle fractures occur in all age groups, caused by accidental slips and falls. The shape of the talus means that twisting the foot plus body weight exerting downward force can easily break the ankle even with normal bone. Operative or non-operative treatments can be used to fix a broken distal tibia and fibula or ankle joint, depending on the fracture configuration.
Pelvic fractures: The pelvis is a strong structure and very large forces are needed to fracture it. Most pelvic fractures occur in high energy collisions; if the bony pelvis is disrupted, the soft organs and viscera are also threatened. Pelvic fractures often occur with substantial injuries to the trunk and limbs. The bony pelvis is effectively a ring, and disruption depends on there being at least two fractures or joint separations with consequent instability. The pelvis can be crushed in an antero-posterior, lateral or vertical direction or a combination of all three. Life-threatening internal bleeding from arterial or, most importantly, venous injury to the iliac vessels often accompanies pelvic fractures.
Clinical indications of likely pelvic fracture include:
• Haematuria or in males, signs of urethral injury, e.g. high-riding prostate on rectal examination, scrotal haematoma or blood at urethral meatus
• Rectal bleeding, or a large haematoma or palpable fracture line on rectal examination
• Haematomas of the proximal thigh, above the inguinal ligament, over the perineum or in the flank
A plain AP pelvic X-ray reveals 90% of injuries. If a fracture is present or suspected and the patient stable, a pelvic CT scan is the best imaging for pelvic anatomy (including hip dislocation and acetabular fracture) and shows the extent of pelvic, retroperitoneal and intraperitoneal bleeding. Rapid assessment, then temporary stabilisation with a fabric pelvic-binder applied in the accident department may help arrest the bleeding, but transfusion and angiographic embolisation may be needed.
Spinal fractures (Fig. 15.10): These may be pathological or not. The most common pathological fracture is a fragility (crush) fracture in osteoporotic bone, typically in lumbar spine bodies in older patients. Up to 90% of patients in their 80s are believed to have sustained a vertebral fragility crush fracture. These cause pain and disability but do not benefit from surgical treatment and take time to settle. Pathological fractures through metastatic deposits are a common new presentation of a known neoplasm or of an undiagnosed primary.
Non-pathological spinal fractures usually occur with high energy trauma, but vertebrae can be crushed in healthy adults after a vertical fall from standing height. Any patient suffering sufficient trauma should be assumed to have a spinal injury until proven otherwise. Most attention is directed to the vulnerable cervical spine (see below), but the entire spinal column should be assessed.
The cervical spine may be cleared clinically, without need for radiology, if the following conditions are met:
• Patient alert and orientated
• No abnormal neurological signs
• No significant other injury that may distract the patient from complaining about the spine
• On examination: no bruising or deformity around the neck, no tenderness and a normal pain-free range of active movement
A cervical spine CT scan should be performed (usually with a CT head) if the criteria are not met. Thoracolumbar spine imaging is indicated if there is pain, bruising, swelling, deformity or abnormal neurological signs attributable to the region. A fracture anywhere in the spine is an indication for full spinal imaging. Unconscious patients cannot be assessed clinically and require radiological clearance of the whole spine (i.e. exclusion of injuries). If in doubt, spinal immobilisation devices are left in place, logrolling for movement and high frequency nursing care is continued while seeking detail about the fracture.
The spine has a key role in structural support and fractures are classified to judge stability. Fractures occur in flexion/extension, compression and/or rotation. Understanding altered vertebral anatomy helps decide whether operation is needed. Damage to the spinal cord or peripheral nerves in the vertebral canal causes limb paralysis. This can occur at the moment of trauma and may be an irretrievable neurological injury, no matter what spinal stabilisation is provided. However, the injured spinal cord can enter a period of spinal shock lasting 24–72 hours and sometimes recovery is seen after this. Spinal shock is an old term for a period of altered distal function with loss of sphincteric control and reflexes which may result from inadequate tissue perfusion secondary to the spinal injury interrupting autonomic control, leading to bradycardia and hypotension. Management of spinal shock is a period of observation, with protection against pressure ulcers and urinary retention, until the spinal cord settles to a stable state of injury, with neurological deficits at and distal to the level of injury.
Common ligamentous injuries
The notion of a sprain versus a ligamentous tear or rupture is important to clarify. A ligament can be injured but retain its functional length without elongation. This causes an acutely painful inflammatory response known as a sprain. Greater energy during injury results in collagen fibre disruption and loss of tensile strength to the point where the ligament tears. Sprains usually resolve without surgical intervention, whereas tears may result in the ligament becoming permanently longer.
Most sprains occur at the ankle and wrist. Both joints have very strong interconnected ligamentous structures. With acute ankle injury, the area rapidly becomes painful and oedematous, but weight bearing may be possible initially as structure remains intact. Later, increasing pain makes weight bearing impossible and medical attention is usually sought. Once a sprain is diagnosed, the management is pain relief, elevation to reduce oedema, initial splintage and rest. Early mobilisation at 1–2 weeks is usually encouraged to prevent stiffness, and movement of the sprained ligament encourages vascularisation and a healing response.
Dislocations: Certain joints can sublux or dislocate after a ligament sprain or rupture. Subluxation is when there is partial loss of congruity between articular surfaces and dislocation is when there is total loss of congruity. Some joints are predisposed to this by their shape and inherent mobility. Sometimes a systemic disease such as the collagen disorder Ehlers–Danlos syndrome, or muscle weakness in muscular dystrophy contributes instability enough for joints to dislocate.
Shoulder dislocation at the glenohumeral joint, and patella dislocation at the patella-femoral joint are common. Both joints have little bony congruity with flat convexities resting in a dish-shaped socket.
Prompt recognition of a dislocation followed by rapid reduction or relocation of joint components is ideal. Reducing the dislocation reduces pain and relieves pressure on nearby structures, including stabilising ligaments and neurovascular structures. Pain usually causes muscle spasm around the site, so good analgesia is needed for reduction in a conscious patient. Skilled emergency room staff can often reduce a dislocated joint if no fracture is present.
Damage control orthopaedics
Advances in understanding physiological responses to severe injury have prompted surgeons to re-examine the management of polytrauma. Long operations soon after a high energy injury definitely increase the threat to life. Open fixation of broken bones causes additional trauma, particularly if there is an enthusiastic desire to fix all fractures in one theatre visit. Such interventions may also cause fat embolism which can lead to respiratory collapse and death. A short surgical intervention after resuscitation could often be justified, but lengthy fixation of all broken bones has been abandoned in favour of temporary stabilisation with external fixators; this is known as damage control orthopaedics. The patient can then be managed or supported for the next 48–72 hours in a high dependency setting whilst the physiological ‘storm’ is optimised. External fixators can then be exchanged for definitive plates or intramedullary rods between days 3 and 10.
Paediatric trauma
Paediatric trauma is more complicated to manage because of the physiological differences between adults and children. Airway management and venous access can be challenging and children are more prone to hypothermia, especially if small, so it is important that paediatric specialists form part of the trauma team. Assessment of major trauma still follows ATLS protocols. Children can appear to compensate for profound hypovolaemia without hypotension, but once deterioration occurs, it is often rapid and irreversible. Potential physical and mental effects of trauma in children must be considered as many are left with long-term disability. Child protection may also need to be considered in some presentations of injury.
Patterns of injury are also different from adults because of differences in anatomy (e.g. bladder injury due to shallow pelvis), physiology (e.g. higher risk of secondary brain injury due to greater cerebral blood flow) and mechanism of injury (e.g. duodenal contusion from handlebar impact). In general, children sustain proportionately greater energy in blunt trauma than adults owing to their small size. Bone elasticity and increased visceral mobility means severe soft tissue or solid organ injury can occur without a fracture.
In orthopaedic injury, operative stabilisation of fractures is achieved using special implants and techniques. Interfering with the growth plate (physis) can cause growth arrest, so any metalwork must be placed away from the physis.