Gastroenterology
Background
The main function of the gastrointestinal (GI) tract is to break food down in to a suitable energy source to allow normal physiological function of cells. Needless to say, the process is complex and involves many different organs. Consequently, there are many conditions that affect the GI tract, some of which are acute and self-limiting and respond well to OTC medication and others that are serious and require referral.
General overview of the anatomy of the GI tract
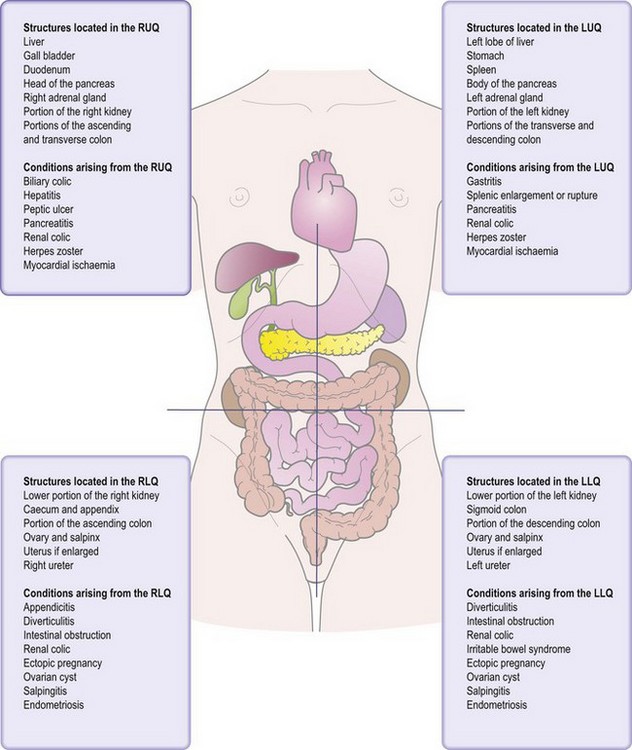
It is vital that pharmacists have a sound understanding of GI tract anatomy. Many conditions will present with similar symptoms and from similar locations, for example abdominal pain, and the pharmacist will need a basic knowledge of GI tract anatomy – and in particular of where each organ of the GI tract is located – to facilitate a correct differential diagnosis.
Stomach
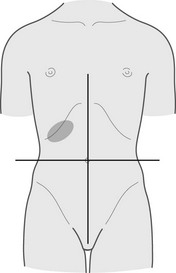
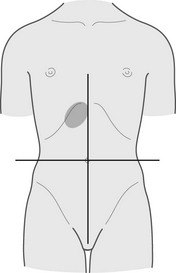
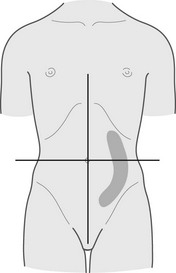
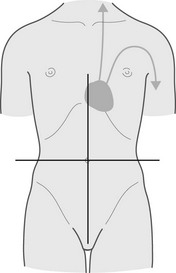
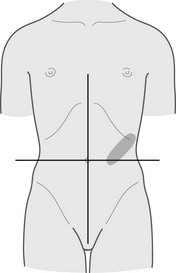
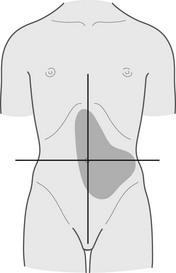
The stomach is roughly ‘J’ shaped and receives food and fluid from the oesophagus. It empties into the duodenum. It is located slightly left of midline and anterior (below) to the rib cage. The lesser curvature of the stomach sits adjacent to the liver.
Liver
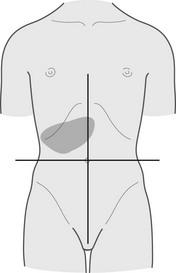
The liver is located below the diaphragm and located mostly right of midline in the upper right quadrant of the abdomen. The liver performs many functions, including carbohydrate, lipid and protein metabolism and the processing of many medicines.
History taking and physical exam
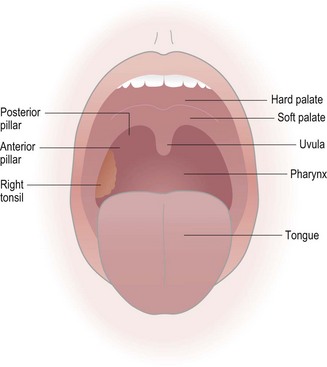
A thorough patient history is essential as physical examination of the GI tract in a community pharmacy is limited to inspection of the mouth. This should allow confirmation of the diagnoses for conditions such as mouth ulcers and oral thrush. A description of how to examine the oral cavity appears in the following section.
Conditions affecting the oral cavity
The process of digestion starts in the oral cavity. The tongue and cheeks position large pieces of food so that the teeth can tear and crush food into smaller particles. Saliva moistens, lubricates and begins the process of digesting carbohydrates (by secreting amylase enzymes) prior to swallowing.
The physical exam
The oral cavity can easily be observed in the pharmacy provided the mouth can be viewed with a good light source, preferably a pen torch (Fig 6.1). The patient will usually present with some form of oral lesion and/or pain in a particular part of the mouth. The pharmacist should examine this area carefully, but the rest of the oral cavity should also be inspected. Checks for periodontal disease (bleeding gums) and other sites of mouth soreness should be performed.
The floor of the mouth and underside of the tongue can be viewed by asking the patient to curl the tongue toward the roof of the mouth; the buccal mucosa is best observed when the patient half opens the mouth.
Mouth ulcers
Aphthous ulcers, more commonly known as mouth ulcers, is a collective term used to describe various different clinical presentations of superficial painful oral lesions that occur in recurrent bouts at intervals between a few days to a few months. The majority of patients (80%) who present in a community pharmacy will have minor aphthous ulcers (MAU). It is the community pharmacists’ role to exclude more serious pathology, for example, systemic causes and carcinoma.
Prevalence and epidemiology
The prevalence and epidemiology of MAU is poorly understood. They occur in all ages but it has been reported that they are more common in patients aged between 20 and 40, and up to 66% of young adults give a history consistent with MAU. Lifetime prevalence is estimated to affect one in five of the general population.
Aetiology
The cause of MAU is unknown. A number of theories have been put forward to explain why people get MAU, including a genetic link, stress, trauma, food sensitivities, nutritional deficiencies (iron, zinc and vitamin B12) and infection, but none have so far been proven.
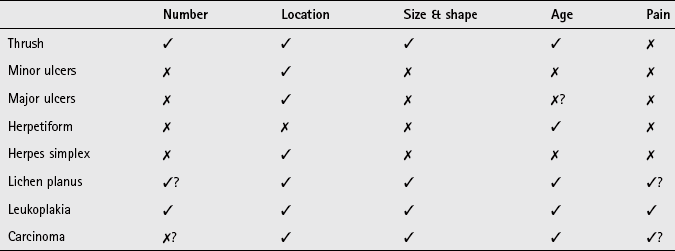
Arriving at a differential diagnosis
There are three main clinical presentations of ulcers: minor, major or herpetiform. Although it is most likely the patient will be suffering from MAU (Table 6.1) it is essential that these and other causes are recognised and referred to the GP for further evaluation.
Table 6.1
Causes of ulcers and their relative incidence in community pharmacy
| Incidence | Cause |
| Most likely | Minor aphthous ulcers (MAU) |
| Likely | Major aphthous ulcers, Trauma |
| Unlikely | Herpetiform ulcers, herpes simplex, oral thrush medicine-induced |
| Very unlikely | Oral carcinoma, erythema multiforme (Steven’s Johnson syndrome), Behçet’s syndrome |
A number of ulcer-specific questions should always be asked of the patient (Table 6.2) and an inspection of the oral cavity should also be performed to help aid the diagnosis.
![]() Table 6.2
Table 6.2
Specific questions to ask the patient: Mouth ulcers
| Question | Relevance |
| Number of ulcers | MAU occur singly or in small crops. A single large ulcerated area is more indicative of pathology outside the remit of the community pharmacist Patients with numerous ulcers are more likely to be suffering from major or herpetiform ulcers rather than MAU |
| Location of ulcers | Ulcers on the side of the cheeks, tongue and inside of the lips are likely to be MAU Ulcers located toward the back of the mouth are more consistent with major or herpetiform ulcers |
| Size and shape | Irregular-shaped ulcers tend to be caused by trauma. If trauma is not the cause then referral is necessary to exclude sinister pathology If ulcers are large or very small they are unlikely to be caused by MAU |
| Painless ulcers | Any patient presenting with a painless ulcer in the oral cavity must be referred. This can indicate sinister pathology such as leukoplakia or carcinoma |
| Age | MAU in young children (<10 years old) is not common and other causes such as primary infection with herpes simplex should be considered If ulcers appear for the first time after adolescence then the diagnostic probability is increased for them to be caused by things other than MAU |
Clinical features of minor aphthous ulcers
The ulcers of MAU are roundish, grey-white in colour and painful. They are small – usually less than 1 cm in diameter – and shallow with a raised red rim. Pain is the key presenting symptom and can make eating and drinking difficult, although pain subsides after three or four days. They rarely occur on the gingival mucosa and occur singly or in small crops of up to five ulcers. It normally takes 7 to 14 days for the ulcers to heal but recurrence typically occurs after an interval of 1 to 4 months (Fig. 6.2).
Conditions to eliminate
Major aphthous ulcers: These are characterised by large (greater than 1 cm in diameter), numerous ulcers, occurring in crops of 10 or more. The ulcers often coalesce to form one large ulcer. The ulcers heal slowly and can persist for many weeks (Fig. 6.3).
Trauma: Trauma to the oral mucosa will result in damage and ulceration. Trauma may be mechanical (e.g. tongue biting) or thermal resulting in ulcers with an irregular border. Patients should be able to recall the traumatic event and have no history of similar ulceration or signs of systemic infection (Fig. 6.4).
Unlikely causes
Herpetiform ulcers: Herpetiform ulcers are pinpoint and occur in large crops of up to 100 at a time. They usually heal within a month and often occur in the posterior part of the mouth, an unusual location for MAU (Fig. 6.5). Both herpetiform and major aphthous ulcers are approximately ten times less common than MAU.
Oral thrush
Oral thrush usually presents as creamy-white soft elevated patches. It is covered in more detail in the next section and the reader is referred to page 139 for differential diagnosis of thrush from other oral lesions.
Herpes simplex
Herpes simplex virus is a common cause of oral ulceration in children. Primary infection results in ulceration of any part of the oral mucosa, especially the gums, tongue and cheeks. The ulcers tend to be small and discrete and many in number. Prior to the eruption of ulcers the person might show signs of systemic infection such as fever and pharyngitis.
Medicine-induced ulcers
A number of case reports have been received of medication causing ulcers. These include cytotoxic agents, nicorandil, alendronate, non-steroidal anti-inflammatory drugs (NSAIDs) and beta-blockers. Ulcers are often seen at the start of therapy or when the dose is increased.
Very unlikely causes
Carcinoma: In 2009, over 6000 cases of oral cancer were confirmed. It is twice as common in men than women. Incidence rates increase sharply beyond 45 years of age. In men the highest incidence is seen in those aged 60–69, and in women it peaks in the over 80s. Smoking and excess alcohol consumption are two major risk factors.
The majority of cancers are noted on the side of the tongue, mouth and lower lip. Initial presentation ranges from painless spots, lumps or ulcers in the mouth or lip area that fail to resolve. Over time these become painful, change colour crust over or bleed. The painless nature of early symptoms leads people to seek help only when other symptoms become apparent. Symptoms therefore can be present for a number of weeks before the patient presents to a health care practitioner. Urgent referral is needed as survival rates increase dramatically if the disease is diagnosed in its early stages.
Erythema multiforme: Infection or drug therapy can cause erythema multiforme, although in about 50% of cases no cause can be found. Symptoms are sudden in onset causing widespread ulceration of the oral cavity. In addition the patient can have annular and symmetric erythematous skin lesions located toward the extremities. Conjunctivitis and eye pain is also common.
Behcet’s syndrome: Most patients will suffer from recurrent, painful major aphthous ulcers that are slow to heal. Lesions are also observed in the genital region and eye involvement (iridocyclitis) is common.
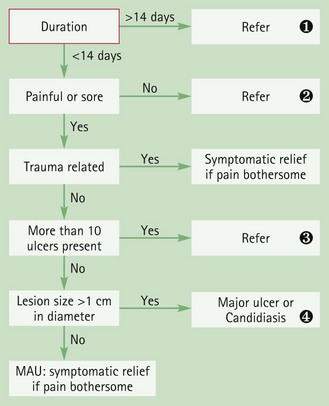
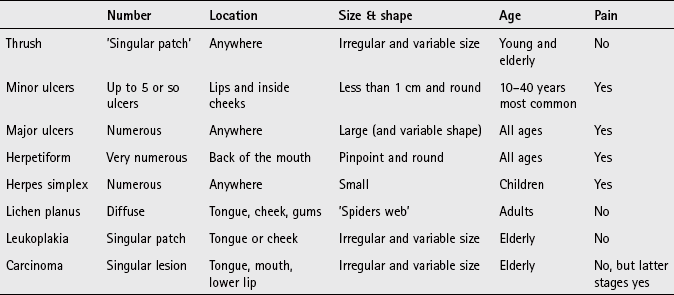
Figure 6.6 will aid the differentiation between serious and non-serious conditions that cause mouth ulcers.
Evidence base for over-the-counter medication
A wide range of products are used for the temporary relief and treatment of mouth ulcers. These products contain corticosteroids, local anaesthetics, antibacterials, astringents and antiseptics. Until, recently, corticosteroids were available OTC (triamcinolone acetonide 0.1% in Orabase and hydrocortisone sodium succinate pellets) but these have been discontinued by the manufacturers. This is unfortunate as a review in BMJ Clinical Evidence found corticosteroids did reduce the duration of pain with MAU (http://exodontia.info/files/BMJ_Clinical_Evidence_2007_Recurrent_Aphthous_Ulcers.pdf; accessed 22 November 2012).
Antibacterial agents (e.g. chlorhexidine)
A number of random controlled trials have investigated antibacterial mouthwashes containing chlorhexidine gluconate. Data from some, but not all studies, have found that they reduced the pain and severity of each episode of ulceration.
Products containing anaesthetic or analgesics
There is very little trial data to support the pain-relieving effect of anaesthetics or analgesics in MAU, apart from choline salicylate. However, these preparations are clinically effective in other painful oral conditions. It is therefore not unreasonable to expect some relief of symptoms to be shown when using these products to treat MAU.
Choline salicylate
Choline salicylate has been shown to exert an analgesic effect in a number of small studies. However, only one study by Reedy (1970) involving 27 patients evaluated choline salicylate in the treatment of oral aphthous ulceration. No significant differences were found between choline salicylate and placebo in ulcer resolution but choline salicylate was found to be significantly superior to placebo in relieving pain.
Practical prescribing and product selection
Prescribing information relating to the medicines used for ulcers reviewed in the section ‘Evidence base for over-the-counter medication’ is discussed and summarised in Table 6.3; useful tips relating to patients presenting with ulcers are given in Hints and Tips Box 6.1.
![]() Table 6.3
Table 6.3
Practical prescribing: Summary of medicines for ulcers
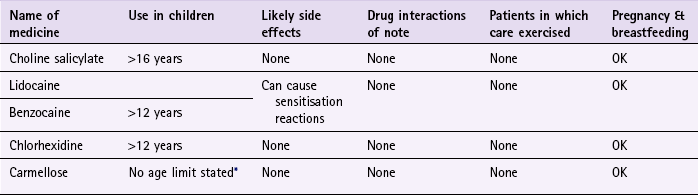
*Children should not be routinely given products as ulcers are rare in this age group.
Antibacterial agents (e.g. chlorhexidine)
Chlorhexidine (e.g. Corsodyl) mouthwash is indicated as an aid in the treatment and prevention of gingivitis and in the maintenance of oral hygiene, which includes the management of aphthous ulceration. Ten mL of the mouthwash should be rinsed around the mouth for about 1 minute twice a day. It can be used by all patient groups, including those who are pregnant and breastfeeding. Side effects associated with its use include reversible tongue and tooth discolouration, burning of the tongue and taste disturbance.
Choline salicylate (Bonjela Cool)
Adults and children over 16 years old should apply the gel, using a clean finger, over the ulcer when needed, but limit this to every 3 hours. It is a safe medicine and can be given to all patient groups. It is not known to interact with any medicines or cause any side effects.
Local anaesthetics (lidocaine e.g. Anbesol range, Iglu gel, Medijel) and benzocaine (e.g. Oralgel & Oralgel Extra Strength).
All local anaesthetics have a short duration of action; frequent dosing is therefore required to maintain the anaesthetic effect. They are thus best used on a when needed basis although the upper limit on the number of applications allowed does vary depending on the concentration of anaesthetic included in each product. They appear to be free from any drug interactions, have minimal side effects and can be given to most patients. A small percentage of patients might experience a hypersensitivity reaction with lidocaine or benzocaine; this appears to be more common with benzocaine.
Carmellose sodium (Orabase Protective Paste)
Orabase can be applied as frequently as requred. It is important that it is dabbed on, and not rubbed on, for it to stick correctly. Also, patients should be discouraged from putting too much on as the excess can peel off leaving the lesion exposed. There are no apparent interactions, and Orabase can be used in all patient groups.
Browne, RM, Fox, EC, Anderson, RJ. Topical triamcinolone acetonide in recurrent aphthous stomatitis. A clinical trial. Lancet. 1968;1:565–567.
MacPhee, IT, Sircus, W, Farmer, ED, et al. Use of steroids in treatment of aphthous ulceration. Br Med J. 1968;2(598):147–149.
Scully, C. Aphthous ulceration. N Engl J Med. 2006;355:165–172.
Truelove, SC, Morris-Owen, RM. Treatment of aphthous ulceration of the mouth. Br Med J. 1958;1:603–607.
Zakrzewska, JM. Fortnightly review: oral cancer. Br Med J. 1999;318:1051–1054.
British Association of Dermatologists. Multi-professional Guidelines for the Management of the Patient with Primary Cutaneous Squamous Cell Carcinoma. http://www.bad.org.uk/Portals/_Bad/Guidelines/Clinical%20Guidelines/SCC%20Guidelines%20Final%20Aug%2009.pdf, 2009.
General site on oral health. http://www.nlm.nih.gov/medlineplus/mouthandteeth.html
The Behçet’s Syndrome Society. http://www.behcets.org.uk/menus/main.asp
The British Dental Health Foundation. http://www.dentalhealth.org.uk/
Oral thrush
Background
Oropharyngeal candidiasis (oral thrush) is an opportunistic mucosal infection and is unusual in healthy adults. If oral thrush is suspected in this population community pharmacists should determine if any identifiable risk factors. A healthy adult with no risk factors generally requires referral to the GP.
Prevalence and epidemiology
The very young (neonates) and the very old are most likely to suffer from oral thrush. It has been reported that 5% of newborn infants and 10% of debilitated elderly patients suffer from oral thrush. Most other cases will be associated with underlying pathology such as diabetes, xerostomia (dry mouth), patients who are immunocompromised or be attributable to identifiable risk factors such as recent antibiotic therapy, inhaled corticosteroids, and ill-fitting dentures.
Aetiology
It is reported that Candida albicans is found in the oral cavity of 30–60% of healthy people in developed countries (Gonsalves et al 2007). Prevalence in denture wearers is even higher. It is transmitted directly between infected people or via objects that can hold the organism. Changes to the normal environment in the oral cavity will allow C. albicans to proliferate.
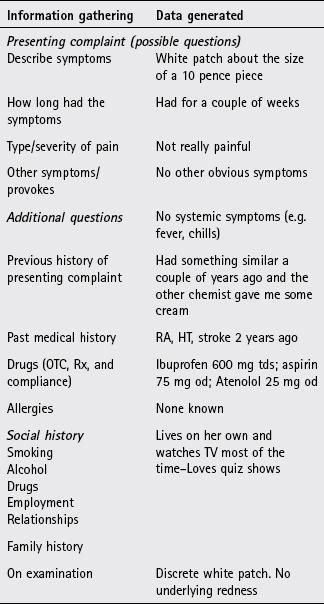
Arriving at a differential diagnosis
Oral thrush is not difficult to diagnose provided a careful history is taken and an oral examination performed. It is the role of the pharmacist to eliminate underlying pathology and exclude risk factors. A number of other conditions need to be considered (Table 6.4) and specific questions asked of the patient (Table 6.5). After questioning the pharmacist should inspect the oral cavity to confirm the diagnosis.
Table 6.4
Causes of oral lesions and their relative incidence in community pharmacy
| Incidence | Cause |
| Most likely | Thrush |
| Likely | Minor aphthous ulcers, medicine induced, ill-fitting dentures |
| Unlikely | Lichen planus, underlying medical disorders, e.g. diabetes, xerostomia (dry mouth) and immunosuppression, major & herpetiform ulcers, herpes simplex |
| Very Unlikely | Leukoplakia, squamous cell carcinoma |
![]() Table 6.5
Table 6.5
Specific questions to ask the patient: Oral thrush
| Question | Relevance |
| Size and shape of lesion | Typically, patients with oral thrush present with ‘patches’. They tend to be irregularly shaped and vary in size from small to large |
| Associated pain | Thrush usually causes some degree of discomfort or pain. Painless patches, especially in people aged over 50, should be referred to exclude sinister pathology such as leukoplakia |
| Location of lesions | Oral thrush often affects the tongue and cheeks, although if precipitated by inhaled steroids the lesions appear on the pharynx |
Clinical features of oral thrush
The classical presentation of oral thrush is of creamy-white soft elevated patches that can be wiped off revealing underlying erythematous mucosa (Fig. 6.7). Pain, soreness, altered taste and a burning tongue can be present. Lesions can occur anywhere in the oral cavity but usually affect the tongue, palate, lips and cheeks. Patients sometimes complain of malaise and loss of appetite. In neonates, spontaneous resolution usually occurs but can take a few weeks.
Conditions to eliminate
Minor aphthous ulcers: Mouth ulcers are covered in more detail on page 134 and the reader is referred to this section for differential diagnosis of these from oral thrush.
Unlikely causes
Lichen planus: Lichen planus is a dermatological condition with lesions similar in appearance to plaque psoriasis. In about 50% of people the oral mucous membranes are affected. The cheeks, gums or tongue develop white, slightly raised painless lesions that look a little like a spider’s web. Other symptoms can include soreness of the mouth and a burning sensation. Occasionally, lichen planus of the mouth occurs without any skin rash.
Underlying medical disorders: As stated previously, oral thrush is unusual in the adult population. Patients are at greater risk of developing thrush if they suffer from medical conditions such as diabetes, xerostomia (dry mouth) or are immunocompromised.
Other forms of ulceration (e.g. major and herpetiform ulcers, herpes simplex): These are covered in more detail on page 135 and the reader is referred to this section for differential diagnosis of these from oral thrush.
Very unlikely causes
Leukoplakia: Leukoplakia is a predominantly white lesion of the oral mucosa that cannot be characterised as any other definable lesion and is therefore a diagnosis based on exclusion (Fig. 6.8). It is often associated with smoking and is a precancerous lesion, although epidemiological data suggests that annual transformation rate to squamous cell carcinoma is approximately 1%. Patients present with a symptomless white patch that develops over a period of weeks on the tongue or cheek. The lesion cannot be wiped off, unlike oral thrush. Most cases are seen in people over the age of 40; it is more common in men. Suspected cases require referral.
Squamous cell carcinoma: Squamous cell carcinoma is covered in more detail on page 137 and the reader is referred to this section for differential diagnosis of these from oral thrush.
Figure 6.9 will aid the differentiation of thrush from other oral lesions.
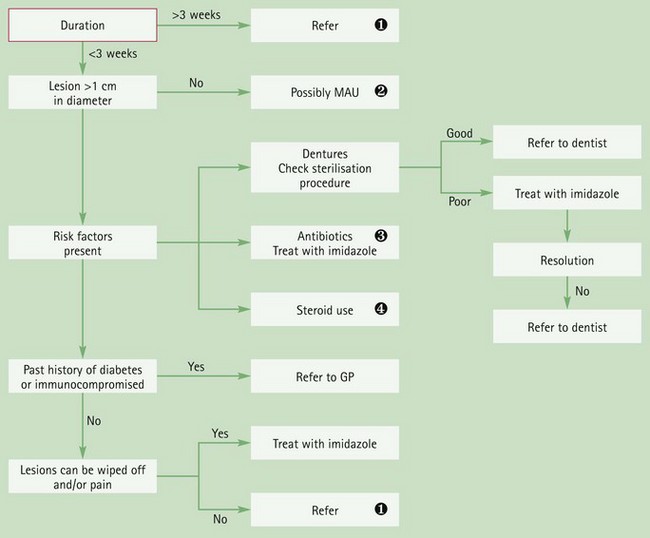
Fig. 6.9 Primer for differential diagnosis of oral thrush.![]() Duration
Duration
Any lesion lasting more than 3 weeks must be referred to exclude sinister pathology.![]() MAU
MAU
See Figure 6.6 for primer for differential diagnosis of mouth ulcers.![]() Antibiotics
Antibiotics
Broad-spectrum antibiotics, e.g. amoxicillin and macrolides, can precipitate oral thrush by altering normal flora of the oral cavity.![]() Inhaled corticosteroids
Inhaled corticosteroids
High-dose inhaled corticosteroids can cause oral thrush. Patients should be encouraged to use a spacer and wash their mouth out after inhaler use to minimise this problem.
Evidence base for over-the-counter medication
Only Daktarin oral gel (miconazole) is available OTC to treat oral thrush. It has proven efficacy and appears to have clinical cure rates between 80 and 90%. In comparative trials, Daktarin appears to have superior cure rates than the POM Nystatin.
Practical prescribing and product selection
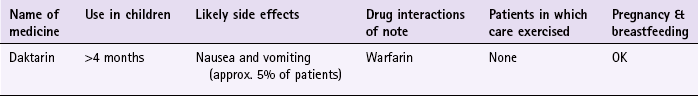
Prescribing information relating to Daktarin Oral gel reviewed in the section ‘Evidence base for over-the-counter medication’ is discussed and summarised in Table 6.6; useful tips relating to the application of Daktarin are given in Hints and Tips Box 6.2.
The dose of gel varies dependent on the age of patient. For adults and children over 6 years, the gel should be applied four times a day and those under six the dose is twice a day. The gel should be applied directly to the area with a clean finger. In May 2008 Jansen-Cilag, the manufacturers of Daktarin, chose to vary the Summary of Product Characteristics (SPC) to recommend that it is not used in infants under 4 months and only with care below the age of 6 months. This change appears to originate from a published report (De Vries et al 2006) documenting a 17-day-old baby who choked when exposed to miconazole oral gel.
It can occasionally cause nausea and vomiting. The manufacturers state that it can interact with a number of medicines, namely mizolastine, cisapride, triazolam, midazolam, quinidine, pimozide, HMG-CoA reductase inhibitors and anticoagulants. However, there is a lack of published data to determine how clinically significant these interactions are except with warfarin. Co-administration of warfarin with miconazole increases warfarin levels markedly and the patient’s (internationalised normalised ratio) INR should be monitored closely. The manufacturers advise that Daktarin should be avoided in pregnancy but published data does not support an association between miconazole and congenital defects. It appears to be safe to use whilst breastfeeding.
Hoppe, JE, Hahn, H. Randomized comparison of two nystatin oral gels with miconazole oral gel for treatment of oral thrush in infants. Antimycotics Study Group. Infection. 1996;24:136–139.
Hoppe, JE. Treatment of oropharyngeal candidiasis in immunocompetent infants: a randomized multicenter study of miconazole gel vs. nystatin suspension. The Antifungals Study Group. Pediatr Infect Dis J. 1997;16:288–293.
Parvinen, T, Kokko, J, Yli-Urpo, A. Miconazole lacquer compared with gel in treatment of denture stomatitis. Scand J Dent Res. 1994;102:361–366.
Gingivitis
Background
Gingivitis simply means inflammation of the gums and is usually caused by an excess build-up of plaque on the teeth. The condition is entirely preventable if regular tooth brushing is undertaken.
Prevalence and epidemiology
It is estimated 50% of the UK population are affected by gum disease and that more than 85% of people over 40 will experience gingival disease. Men more than women tend to suffer from severe gingivitis.
Aetiology
Following tooth brushing, the teeth soon become coated in a mixture of saliva and gingival fluid, known as pellicle. Oral bacteria and food particles adhere to this coating and begin to proliferate forming plaque; subsequent brushing of the teeth removes this plaque build up. However, if plaque is allowed to build up for 3 or 4 days, bacteria begin to undergo internal calcification producing calcium phosphate better known as tartar (or calculus). This adheres tightly to the surface of the tooth and retains bacteria in situ. The bacteria release enzymes and toxins that invade the gingival mucosa, causing inflammation of the gingiva (gingivitis). If the plaque is not removed the inflammation travels downwards, involving the periodontal ligament and associated tooth structures (periodontitis). A pocket forms between the tooth and gum and, over a period of years, the root of the tooth and bone are eroded until such time that the tooth becomes loose and lost. This is the main cause of tooth loss in people over 40 years of age.
A number of risk factors are associated with gingivitis and periodontitis; these include diabetes mellitus, cigarette smoking, poor nutritional status and poor oral hygiene.
Arriving at a differential diagnosis
Gingivitis often goes unnoticed because symptoms can be very mild and painless. This often explains why a routine check-up at the dentist reveals more severe gum disease than patients thought they had. A dental history needs to be taken from the patient, in particular details of their tooth brushing routine and technique, as well as the frequency of visits to their dentist. The mouth should be inspected for tell-tale signs of gingival inflammation. A number of gingivitis-specific questions should always be asked of the patient to aid in diagnosis (Table 6.7).
![]() Table 6.7
Table 6.7
Specific questions to ask the patient: Gingivitis
| Question | Relevance |
| Tooth brushing technique | Overzealous tooth brushing can lead to bleeding gums and gum recession. Make sure the patient is not ‘over cleaning’ their teeth. An electric tooth brush might be helpful for people who apply too much force when brushing teeth |
| Bleeding gums | Gums that bleed without exposure to trauma and is unexplained or unprovoked need referral to exclude underlying pathology |
Clinical features of gingivitis
Gingivitis is characterised by swelling and reddening of the gums, which bleed easily with slight trauma, for example when brushing teeth. Plaque might be visible; especially on teeth that are difficult to reach when tooth brushing. Halitosis might also be present.
Conditions to eliminate
If gingivitis is left untreated it will progress into periodontitis. Symptoms are similar to gingivitis but the patient will experience spontaneous bleeding, taste disturbances, halitosis and difficulty while eating. Periodontal pockets might be visible and the patient might complain of loose teeth. Referral to a dentist is needed for evaluation and removal of tartar.
Evidence base for over-the-counter medication
Put simply, there is no substitute for good oral hygiene. Prevention of plaque build-up is the key to healthy gums and teeth. Twice daily brushing is recommended to maintain oral hygiene at adequate levels. Brushing teeth, with a fluoride toothpaste, to prevent tooth decay, should preferably take place after eating. Flossing is recommended, three times a week, to access areas that a toothbrush might miss. A Cochrane review (Robinson et al 2005) concluded that powered tooth brushes (with rotation oscillation action – where brush heads rotate in one direction and then the other) are more effective than manual brushing at plaque removal.
There is a plethora of oral hygiene products marketed to the public. These products should be reserved for established gingivitis or in those patients who have poor toothbrushing technique.
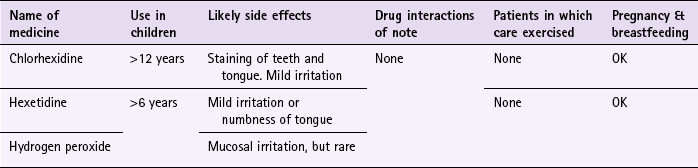
Mouthwashes contain chlorhexidine, hexetidine and hydrogen peroxide. Of these, chlorhexidine in concentrations of either 0.1 or 0.2% has been proven the most effective antibacterial in reducing plaque formation and gingivitis (Ernst et al 1998). In clinical trials it has been shown to be consistently more effective than placebo and comparator medicines, and there appears to be no difference in effect between concentrations. It has even been used as a positive control.
Practical prescribing and product selection
Prescribing information relating to the medicines used for gingivitis reviewed in the section ‘Evidence base for over-the-counter medication’ is discussed and summarised in Table 6.8; useful tips relating to products for oral care are given in Hints and Tips Box 6.3.
All mouthwashes, have minimal side effects and can be used by all patient groups. They are rinsed around the mouth between 30 seconds and 1 minute then spat out.
Chlorhexidine gluconate (e.g. Corsodyl 0.2%, Eludril 0.1%)
The standard dose for adults and children over 12 years old is 10 mL twice a day. Although it is free from side-effects, patients should be warned that prolonged use may stain the tongue and teeth brown. This can be reduced or removed by brushing teeth before use. If this fails to remove the staining then it can be removed by a dentist. Corsodyl is also available as a spray (0.2%) and gel (1%) and used twice a day.
References
Ernst, CP, Prockl, K, Willershausen, B. The effectiveness and side effects of 0.1% and 0.2% chlorhexidine mouthrinses: a clinical study. Quintessence Int. 1998;29:443–448.
Robinson, P, Deacon, SA, Deery, C, et al. Manual versus powered toothbrushing for oral health. Cochrane Database of Systematic Reviews. (Issue 2):2005. [Art. No.: CD002281. DOI: 10.1002/14651858.CD002281.pub2].
Brecx, M, Brownstone, E, MacDonald, L, et al. Efficacy of Listerine, Meridol and chlorhexidine mouthrinses as supplements to regular tooth cleaning measures. J Clin Periodontol. 1992;19:202–207.
Hase, JC, Ainamo, J, Etemadzadeh, H, et al. Plaque formation and gingivitis after mouthrinsing with 0.2% delmopinol hydrochloride, 0.2% chlorhexidine digluconate and placebo for 4 weeks, following an initial professional tooth cleaning. J Clin Periodontol. 1995;22:533–539.
Jones, CM, Blinkhorn, AS, White, E. Hydrogen peroxide, the effect on plaque and gingivitis when used in an oral irrigator. Clin Prev Dent. 1990;12:15–18.
Kelly, M. Adult Dental Health Survey: Oral Health in the United Kingdom 1998. London: TSO; 2000.
Lang, NP, Hase, JC, Grassi, M, et al. Plaque formation and gingivitis after supervised mouthrinsing with 0.2% delmopinol hydrochloride, 0.2% chlorhexidine digluconate and placebo for 6 months. Oral Dis. 1998;4:105–113.
Maruniak, J, Clark, WB, Walker, CB, et al. The effect of 3 mouthrinses on plaque and gingivitis development. J Clin Periodontol. 1992;19:19–23.
The British Dental Association. http://www.bda.org/
The British Fluoridation Society. http://www.bfsweb.org/
The British Dental Health Foundation. http://www.dentalhealth.org.uk/
The American Academy of Periodontology. http://www.perio.org/
Dyspepsia
Background
Confusion surrounds the terminology associated with upper abdominal symptoms and the term dyspepsia is used by different authors to mean different things. It is therefore an umbrella term generally used by healthcare professionals to refer to a group of upper abdominal symptoms that arise from five main conditions:
• non-ulcer dyspepsia/functional dyspepsia (indigestion)
These five conditions represent 90% of dyspepsia cases presented to the GP.
In August 2004, The National Institute for Health and Clinical Excellence (NICE) issued clinical guidance on the management of dyspepsia in adults in primary care (see web sites at end of section). This guidance has specific information on pharmacist management of dyspepsia. This is still current (July 2012) and specific reference is made to this guidance.
Prevalence and epidemiology
The exact prevalence of dyspepsia is unknown. This is largely because of the number of people who self-medicate or do not report mild symptoms to their GP. However, it is clear that dyspepsia is extremely common. Between 25 and 40% of the general population in Western society are reported to suffer from dyspepsia and virtually everyone at some point in their lives will experience an episode. Estimates suggest that 10% of people suffer on a weekly basis and that 5% of all GP consultations are for dyspepsia. The prevalence of dyspepsia is modestly higher in women than men.
Aetiology
The aetiology of dyspepsia differs depending on its cause. Decreased muscle tone leads to lower oesophageal sphincter incompetence (often as a result of medicines or overeating) and is the principal cause of GORD. Increased acid production results in inflammation of the stomach (gastritis) and is usually attributable to Helicobacter pylori infection, or acute alcohol indigestion. The presence of H. pylori is central to duodenal and gastric ulceration – H. pylori is present in 95% of duodenal ulcers and 80% of gastric ulcers. The exact mechanism by which it causes ulceration is still unclear but the bacteria does produce toxins that stimulate the inflammatory cascade. Increasingly common are medicine induced ulcers, most notably NSAIDs and low-dose aspirin.
Finally, when no specific cause can be found for a patient’s symptoms the complaint is said to be non-ulcer dyspepsia. (Some authorities do not advocate the use of this term, preferring the term ‘functional dyspepsia’.)
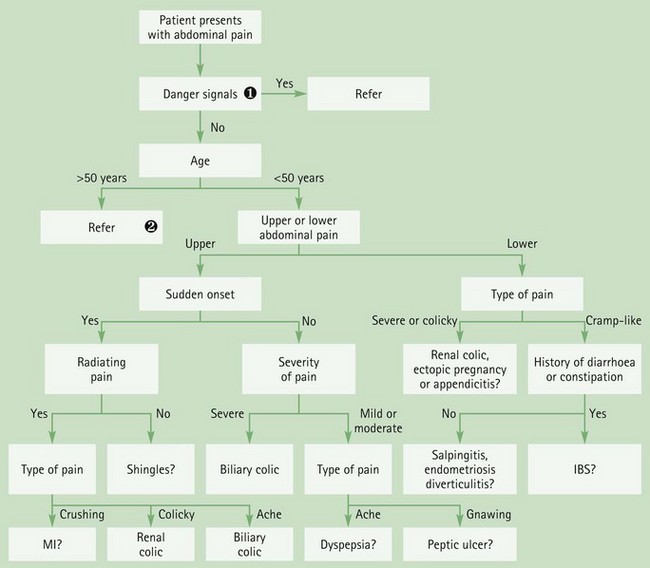
Arriving at a differential diagnosis
Overwhelmingly, patients who present with dyspepsia are likely to be suffering from GORD, gastritis or non-ulcer dyspepsia (Table 6.9). Research has shown that even those patients who meet NICE guidelines for endoscopical investigation are found to have either gastritis/hiatus hernia (30%), oesophagitis (10–17%) or no abnormal findings (30%). It has also been reported that a medical practitioner with an average list size will only see one new case of oesophageal cancer and one new case of stomach cancer every four years. Despite these statistics, a thorough medical and drug history should be taken to enable the community pharmacist to rule out serious pathology. ALARM symptoms (see Trigger points for referral), which would warrant further investigation are surprisingly common and it is important that patients exhibiting these symptoms are referred. A number of dyspepsia specific questions should always be asked of the patient to aid in diagnosis (Table 6.10).
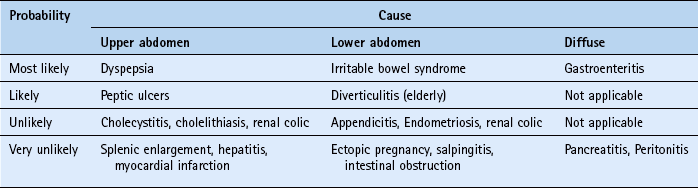
Table 6.9
Causes of upper GI symptoms and their relative incidence in community pharmacy
| Incidence | Cause |
| Most likely | Non-ulcer dyspepsia |
| Unlikely | Medicine induced, peptic ulcers, irritable bowel syndrome |
| Very unlikely | Gastric and oesophageal cancers, atypical angina |
![]() Table 6.10
Table 6.10
Specific questions to ask the patient: Dyspepsia
| Question | Relevance |
| Age | The incidence of dyspepsia decreases with advancing age and therefore young adults are likely to suffer from dyspepsia with no specific pathologic condition, unlike patients over 50 years of age, in which a specific pathologic condition becomes more common |
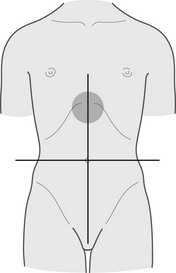
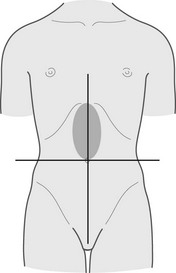
| Location | Dyspepsia is experienced as pain above the umbilicus and centrally located (epigastric area). Pain below the umbilicus will not be due to dyspepsia Pain experienced behind the sternum (breastbone) is likely to be heartburn If the patient can point to a specific area of the abdomen then it is unlikely to be dyspepsia |
| Nature of pain | Pain associated with dyspepsia is described as aching or discomfort. Pain described as gnawing, sharp or stabbing is unlikely to be dyspepsia |
| Radiation | Pain that radiates to other areas of the body is indicative of more serious pathology and the patient must be referred. The pain might be cardiovascular in origin, especially if the pain is felt down the inside aspect of the left arm |
| Severity | Pain described as debilitating or severe must be referred to exclude more serious conditions |
| Associated symptoms | Persistent vomiting with or without blood is suggestive of ulceration or even cancer and must be referred Black and tarry stools indicate a bleed in the GI tract and must be referred |
| Aggravating or relieving factors | Pain shortly after eating (1 to 3 hours) and relieved by food or antacids are classic symptoms of ulcers Symptoms of dyspepsia are often brought on by certain types of food, for example caffeine containing products and spicy food |
| Social history | Bouts of excessive drinking are commonly implicated in dyspepsia. Likewise, eating food on the move or too quickly is often the cause of the symptoms. A person’s job is often a good clue to whether these are contributing to their symptoms |
Clinical features of dyspepsia
Patients with dyspepsia present with a range of symptoms commonly involving:
Although, dyspeptic symptoms are a poor predictor of disease severity or underlying pathology, retrosternal heartburn is the classic symptom of GORD.
Conditions to eliminate
Peptic ulceration: Ruling out peptic ulceration is probably the main consideration for community pharmacists when assessing patients with symptoms of dyspepsia. Ulcers are classed as either gastric or duodenal. They occur most commonly in patients aged between 30 and 50, although patients over the age of 60 account for 80% of deaths even though they only account for 15% of cases. Typically the patient will have well localised mid-epigastric pain described as ‘constant’, ‘annoying’ or ‘gnawing/boring’. In gastric ulcers the pain comes on whenever the stomach is empty, usually 30 minutes after eating and is generally relieved by antacids or food and aggravated by alcohol and caffeine. Gastric ulcers are also more commonly associated with weight loss and GI bleeds than duodenal ulcers. Patients can experience weight loss of 5 to 10 kg and although this could indicate carcinoma, especially in people aged over 40, on investigation a benign gastric ulcer is found most of the time. NSAID use is associated with a three- to fourfold increase in gastric ulcers.
Duodenal ulcers tend to be more consistent in symptom presentation. Pain occurs 2 to 3 hours after eating and pain that wakes a person at night is highly suggestive of duodenal ulcer. If ulcers are suspected referral to the GP is necessary as peptic ulcers can only be conclusively diagnosed by endoscopy.
Medicine-induced dyspepsia: A number of medicines can cause gastric irritation leading to or provoking GI discomfort or they can decrease oesophageal sphincter tone resulting in reflux. Aspirin and NSAIDs are very often associated with dyspepsia and can affect up to 25% of patients. Table 6.11 lists other medicines commonly implicated in causing dyspepsia.
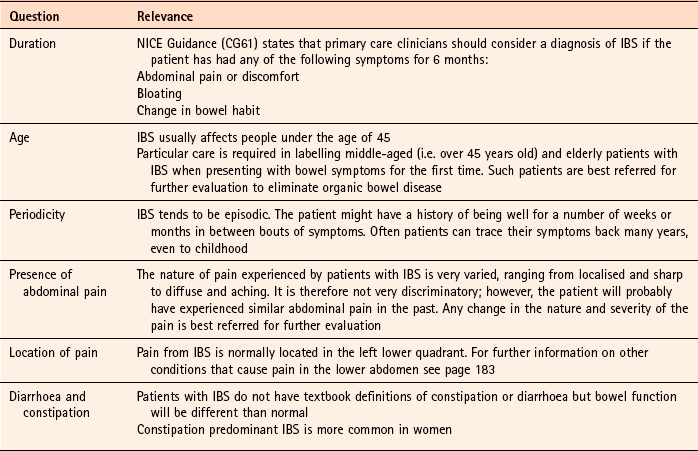
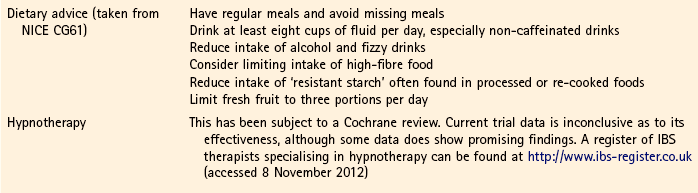
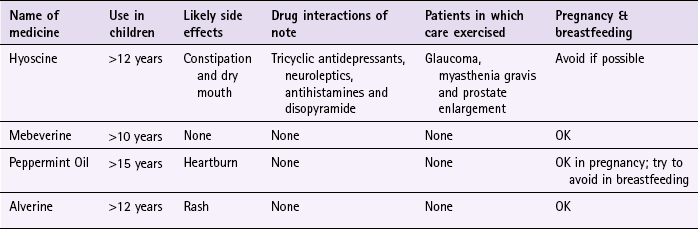
Irritable bowel syndrome: Patients younger than 45, who have uncomplicated dyspepsia and also lower abdominal pain and altered bowel habits are likely to have irritable bowel syndrome (IBS). For further details on IBS see page 168.
Very unlikely causes
Gastric carcinoma: Gastric carcinoma is the third most common GI malignancy after colorectal and pancreatic cancer. However, only 2% of patients who are referred by their GP for an endoscopy have malignancy. It is therefore a rare condition and community pharmacists are extremely unlikely to encounter a patient with carcinoma. One or more ALARM symptoms should be present plus symptoms such as nausea and vomiting.
Oesophageal carcinoma: In its early stages, oesophageal carcinoma might go unnoticed. Over time, however, as the oesophagus becomes constricted, patients will complain of difficulty in swallowing and experience a sensation of food sticking in the oesophagus. As the disease progresses weight loss becomes prominent despite the patient maintaining a good appetite.
Atypical angina: Not all cases of angina have classical textbook presentation of pain in the retrosternal area with radiation to the neck, back or left shoulder that is precipitated by temperature changes or exercise. Patients can complain of dyspepsia-like symptoms and feel generally unwell. These symptoms might be brought on by a heavy meal. In such cases antacids will fail to relieve symptoms and referral is needed.
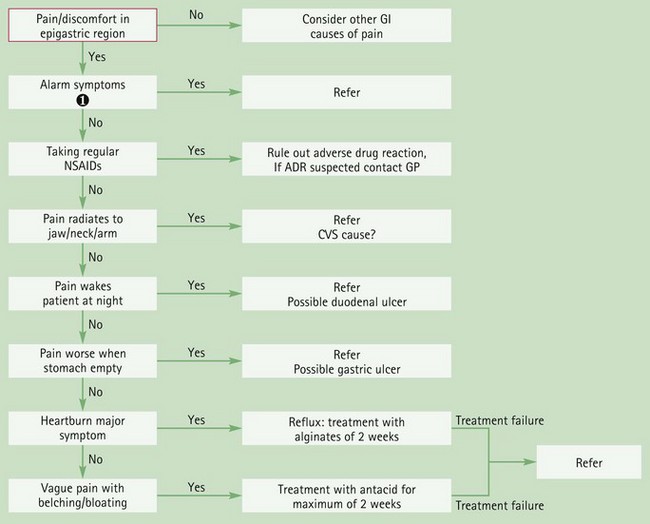
Figure 6.10 will aid differentiation of the causes of dyspepsia.
Evidence base for over-the-counter medication
In accordance with NICE guidelines the group of patients that should be treated by pharmacists are classed as having ‘uninvestigated dyspepsia’ (i.e. those that have not had endoscopical investigation). OTC treatment options consist of antacids, H2 antagonists and proton pump inhibitors (PPIs). Before treatment is instigated lifestyle advice should be given where appropriate. Although there is no strong evidence that dietary changes will lessen dyspepsia symptoms, a general healthier lifestyle will have wider health benefits. The patient should be assessed in terms of diet and physical activity:
It might also be possible to identify factors that precipitate or worsen symptoms. Commonly implicated foods that precipitate dyspepsia are spicy or fatty food, caffeine, chocolate and alcohol. Bending is also said to worsen symptoms.
Antacids
Antacids have been used for many decades to treat dyspepsia and have proven efficacy in neutralising stomach acid. However, the neutralising capacity of each antacid varies dependent on the metal salt used. In addition, the solubility of each metal salt differs, which affects their onset and duration of action. Sodium and potassium salts are the most highly soluble, which makes them quick but short acting. Magnesium and aluminium salts are less soluble so have a slower onset but greater duration of action. Calcium salts have the advantage of being quick acting yet have a prolonged action.
It is therefore commonplace for manufacturers to combine two or more antacid ingredients together to ensure a quick onset (generally sodium salts e.g. sodium bicarbonate) and prolonged action (aluminium, magnesium or calcium salts).
Alginates
For patients suffering from GORD an alginate product should be first-line treatment. When in contact with gastric acid the alginate precipitates out, forming a sponge-like matrix that floats on top of the stomach contents. Alginate preparations are also commonly combined with antacids to help neutralise stomach acid. In clinical trials alginate-containing products have demonstrated superior symptom control compared to placebo and antacids. However, PPIs and H2 antagonists do have superior efficacy to alginates.
H2 antagonists
Two H2 antagonists are currently available OTC in the UK; ranitidine and famotidine. Cimetidine was also available OTC but withdrawn by the manufacturer and nizatidine has exemption from POM control but currently there is no marketed product.
H2 antagonists are effective at POM doses but OTC licensed indications use lower doses. The question is, at these lower doses are they still effective? There is a paucity of publicly available trial data supporting their use at non-prescription doses. Famotidine appears to have the greatest body of accessible trial data. A number of trials have been conducted in patients suffering from heartburn and who regularly self-medicate with antacids. Famotidine was shown to be more effective than placebo and equally effective to antacids. No trials involving ranitidine could be found on public databases that involved patients taking OTC doses.
However, the inhibitory effects of OTC doses of ranitidine on gastric acid have been investigated in healthy volunteers. Trials showed conclusively that ranitidine, and its comparator drug famotidine, did significantly raise intragastric pH compared to placebo, although antacids (calcium carbonates) had a significantly quicker onset of action but with shorter duration.
Proton pump inhibitors
A number of trials have compared PPIs with H2 antagonists for non-ulcer dyspepsia and GORD-like symptoms (Moayyedi et al 2006; Talley et al 2002; van Pinxteren 2006). Results indicate that PPIs, even at half the standard POM dose, are generally superior to H2 antagonists in treating dyspeptic symptoms.
Summary
Antacids will work for the majority of people presenting at the pharmacy with mild dyspeptic symptoms. They can be used as first-line therapy unless heartburn predominates then an alginate or alginate/antacid combination can be used. H2 antagonists appear to be equally effective to antacids but are considerably more expensive. Proton pump inhibitors are the most effective and could be considered first-line, especially for those patients that suffer from moderate to severe or recurrent symptoms. Like H2 antagonists they are expensive in comparison to simple antacids and might influence patient choice or pharmacist recommendation.
Practical prescribing and product selection
Prescribing information relating to the medicines used for dyspepsia reviewed in the section ‘Evidence base for over-the-counter medication is discussed and summarised in Table 6.12.
![]() Table 6.12
Table 6.12
Practical prescribing: Summary of medicines for dyspepsia
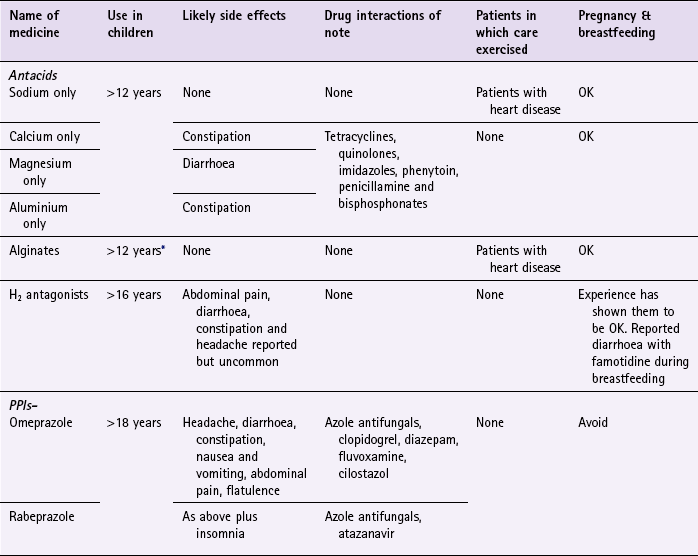
*Certain products can be given to children but dyspepsia unusual in children and it might be prudent to refer such patients to their GP.
Antacids
The majority of marketed antacids are combination products containing two, three or even four constituents. The rationale for combining different salts together appears to be twofold. First, to ensure the product has quick onset (containing sodium or calcium) and a long duration of action (containing magnesium, aluminium or calcium). Second, to minimise any side effects that might be experienced from the product. For example, magnesium salts tend to cause diarrhoea and aluminium salts constipation, however, if both are combined in the same product then neither side effect is noticed. Useful tips relating to antacids are given in Hints and Tips Box 6.4.
Antacids can affect the absorption of a number of medications via chelation and adsorption. Commonly affected medicines include tetracyclines, quinolones, imidazoles, phenytoin, penicillamine and bisphosphonates. In addition, the absorption of enteric-coated preparations can be affected due to antacids increasing the stomach pH. The majority of these interactions are easily overcome by leaving a minimum gap of 1 hour between the respective doses of each medicine.
Most patient groups can take antacids, although patients on salt-restricted diets (e.g. patients with coronary heart disease) should ideally avoid sodium-containing antacids. In addition, antacids should not be recommended in children because dyspepsia is unusual in children under 12. Indeed, most products are licensed for use only for children aged 12 and over. However, there are a few exceptions (e.g. Acidex, Topal), which have product licences for use in children.
Alginates (e.g. the Gaviscon range)
Products containing alginates are combination preparations that contain an alginate with antacids. They are best given after each main meal and before bedtime, although they can be taken on a when-needed basis. They can be given during pregnancy and breastfeeding and to most patient groups but, as with antacids, patients on salt-restricted diets should ideally avoid sodium-containing alginate preparations. They are reported not to have any side effects or interactions with other medicines.
H2 antagonists
Sales of H2 antagonists are restricted to adults and children over the age of 16. They possess no clinically important drug interactions and side effects are rare. Safety concerns were raised on deregulation of H2 antagonists about the potential to mask serious underlying conditions and the possibility of increased adverse reactions. These fears appear to have been unfounded as follow-up studies and post marketing surveillance has not shown any increase in risk associated with greater availability. Indeed, H2 antagonists are now available as general sales list medicines. They have been used in pregnancy and breastfeeding, with ranitidine having been used most. Data suggests that there are no significant increases in any major malformations in pregnancy and can be used whilst breastfeeding and manufacturers of OTC products advise patients to speak to the doctor or pharmacist before taking.
Famotidine (PepcidTwo): The dose for famotidine is 10 mg (one tablet) at the onset of symptoms; however, if symptoms persist an additional dose can be repeated after 1 hour. The maximum dose is 20 mg (two tablets) in 24 hours. A dose can be taken 1 hour prior to consuming food or drink that are known to bring on symptoms. PepcidTwo is a combination of famotidine, calcium carbonate and magnesium hydroxide. The antacid component of the product provides quick onset of action helping to relieve symptoms before famotidine exerts its action, which can take 2 hours.
Ranitidine (e.g. Zantac range, Gavilast and Gavilast P, Ranzac): Dosing for ranitidine (Zantac 75) is similar to famotidine in that one tablet should be taken straight away but if symptoms persist then a further tablet should be taken 1 hour later. The maximum dose is 300 mg (four tablets) in 24 hours. The General Sales List versions of ranitidine (Zantac 75 Relief and Ranzac), have slightly different license in that they cannot be used for prevention of heartburn and the maximum dose is only two tablets in 24 hours.
Omeprazole (Zanprol): Zanprol is licensed for the relief of reflux-like symptoms (e.g. heartburn) associated with acid-related dyspepsia in patients aged over 18 years of age. The initial dose is two 10 mg tablets once daily. Once symptoms improve the dose can be reduced to one tablet (10 mg). If symptoms return then the dose can be stepped back up to 20 mg. Patients should be referred to their GP if symptoms do not resolve in 2 weeks or they need to use omeprazole for more than 4 weeks continuously. Omeprazole can cause a number of common side effects (>1 in 100), which include headache, diarrhoea, constipation, abdominal pain, nausea and vomiting and flatulence. Drug interactions with omeprazole are possible because it is metabolised in the liver by cytochrome P450 isoenzymes. These include ‘azole’ antifungals (decrease in azole bioavailability), diazepam (enhanced diazepam side effects), fluvoxamine (increased omeprazole levels), cilostazol (increased cilostazol levels – and UK manufacturers advise against co-administration) and clopidogrel (reduced clopidogrel levels). Other interactions listed in the manufacturer’s literature include phenytoin and warfarin but their clinical significance appears low.
It appears to be safe in pregnancy and excreted in only small amounts of breast milk and is not contraindicated when used as a POM medicine, however for pharmacy use it is not recommended.
Rabeprazole (Pariet Pharmacy): The MHRA have recently approved the deregulation of rabeprazole from POM to P. Its product license is very similar to that of omeprazole: it has a license for the short-term symptomatic treatment of GORD-like symptoms (e.g. heartburn) in adults aged 18 and over; if symptoms have not been controlled within 2 weeks or if continuous treatment for more than 4 weeks is required, then the patient should be referred to their doctor; and it should be avoided in pregnant and breastfeeding women. The dose is one 10 mg tablet each day. Side effects commonly seen include insomnia, headaches, dizziness, cough, diarrhea, vomiting, nausea, abdominal pain and constipation. It interacts with oral ‘azole’ medicines and on theoretical grounds should not be co-administered with atazanavir.
References
Moayyedi, P, Soo, S, Deeks, J, et al. Pharmacological interventions for non-ulcer dyspepsia. Cochrane Database of Systematic Reviews. (Issue 4):2006. [Art. No.: CD001960. DOI: 10.1002/14651858.CD001960.pub3.].
Talley, NJ, Moore, MG, Sprogis, A, et al. Randomised controlled trial of pantoprazole versus ranitidine for the treatment of uninvestigated heartburn in primary care. Med J Aust. 2002;177(8):423–427.
van Pinxteren, B, Sigterman, KE, Bonis, P, Lau, J, et al. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease. Cochrane Database of Systematic Reviews. (Issue 3):2006. [Art. No.: CD002095. DOI: 10.1002/14651858.CD002095.pub3].
Castell, DO, Dalton, CB, Becker, D, et al. Alginic acid decreases postprandial upright gastroesophageal reflux. Comparison with equal-strength antacid. Dig Dis Sci. 1992;37:589–593.
Dowswell, T, Neilson, JP. Interventions for heartburn in pregnancy. Cochrane Database of Systematic Reviews. (Issue 4):2008. Art. No.: CD007065. DOI: 10.1002/14651858.CD007065.pub2
Drake, D, Hollander, D. Neutralizing capacity and cost effectiveness of antacids. Ann Intern Med. 1981;94:215–217.
Feldman, M. Comparison of the effects of over-the-counter famotidine and calcium carbonate antacid on postprandial gastric acid. A randomized controlled trial. JAMA. 1996;275:1428–1431.
Halter, F. Determination of neutralization capacity of antacids in gastric juice. Z Gastroenterol. 1983;21:S33–S40.
Netzer, P, Brabetz-Hofliger, A, Brundler, R, et al. Comparison of the effect of the antacid Rennie versus low dose H2 receptor antagonists (ranitidine, famotidine) on intragastric acidity. Ailment Pharmacol Ther. 1998;12:337–342.
Reilly, TG, Singh, S, Cottrell, J, et al. Low dose famotidine and rantidine as single post-prandial doses: a three-period placebo-controlled comparative trial. Ailment Pharmacol Ther. 1996;10:749–755.
Smart, HL, Atkinson, M. Comparison of a dimethicone/antacid (Asilone gel) with an alginate/antacid (Gaviscon liquid) in the management of reflux oesophagitis. J R Soc Med. 1990;83:554–556.
NICE Guidance on management of dyspepsia in primary care. http://publications.nice.org.uk/dyspepsia-cg17.
British Society of Gastroenterology. http://www.bsg.org.uk/
CORE. research charity. http://www.corecharity.org.uk/.
American Gastroenterological Association. http://www.gastro.org/
Diarrhoea
Background
Diarrhoea can be defined as an increase in frequency of the passage of soft or watery stools relative to the usual bowel habit for that individual. It is not a disease but a sign of an underlying problem such as an infection or gastrointestinal disorder. It can be classed as acute (less than 7 days), persistent (more than 14 days) or chronic (lasting longer than a month). Most patients will present to the pharmacy with a self-diagnosis of acute diarrhoea. It is necessary to confirm this self-diagnosis because patients’ interpretations of their symptoms might not match up with the medical definition of diarrhoea.
Prevalence and epidemiology
The exact prevalence and epidemiology of diarrhoea is not well known. This is probably due to the number of patients who do not seek care or who self-medicate. However, acute diarrhoea does generate high GP consultation rates. It has been reported that children under the age of 5 years have between one and three bouts of diarrhoea per year and adults, on average, just under one episode of diarrhoea per year. Many of these cases are thought to be food related.
Aetiology
The aetiology of diarrhoea depends on its cause. Acute gastroenteritis, the most common cause of diarrhoea in all age groups, is usually viral in origin. In the UK rotavirus and small round structured virus (SRSV) are the most common identified causes of gastroenteritis in children, and in adults, Campylobacter followed by rotavirus are the most common. Other pathogens identified include Escherichia coli, Salmonella, Shigella; viruses such as adenovirus; and the protozoa Cryptosporidium and Giardia. Viral causes tend to cause diarrhoea by blunting of the villi of the upper small intestine decreasing the absorptive surface. Bacterial causes of diarrhoea are normally a result of eating contaminated food or drink and cause diarrhoea by a number of mechanisms. For example, enterotoxigenic E. coli produce enterotoxins that affect gut function with secretion and loss of fluids; enteropathogenic E. coli interferes with normal mucosal function; and enteroinvasive E. coli, Shigella and Salmonella species cause injury to the mucosa of the small intestine and deeper tissues.
Other organisms, for example Staphylococcus aureus and Bacillus cereus, produce preformed enterotoxins which on ingestion stimulate the active secretion of electrolytes into the intestinal lumen.
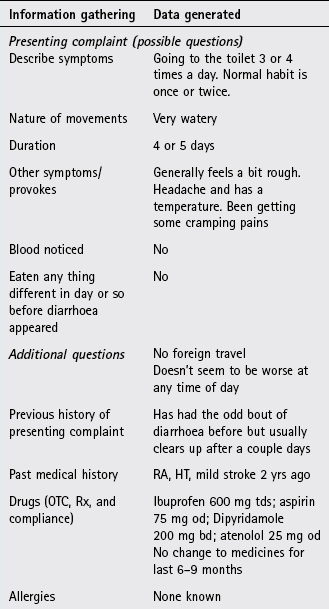
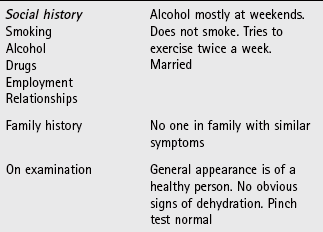
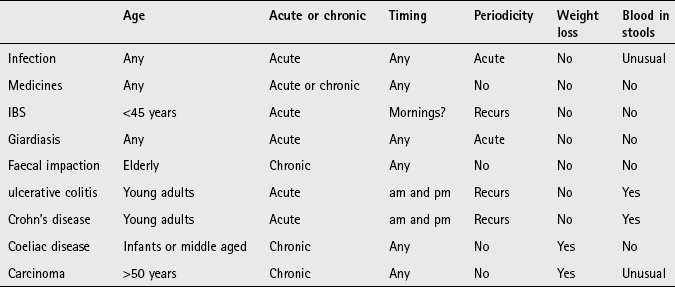
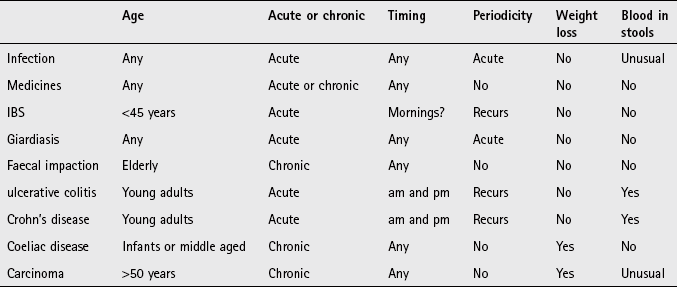
Arriving at a differential diagnosis
The most common causes of diarrhoea are viral or bacterial infection (Table 6.13) and the community pharmacist can appropriately manage the vast majority of cases. The main priority is identifying those patients that need referral and how quickly they need to be referred. Dehydration is the main complicating factor, especially in the very young (see page 297) and very old. A number of diarrhoea specific questions should always be asked of the patient to aid in diagnosis (Table 6.14).
Table 6.13
Causes of diarrhoea and their relative incidence in community pharmacy
| Incidence | Cause |
| Most likely | Viral and bacterial infection |
| Likely | Medicine induced |
| Unlikely | Irritable bowel syndrome, giardiasis, faecal impaction |
| Very unlikely | Ulcerative colitis and Crohn’s disease, colorectal cancer, malabsorption syndromes |
![]() Table 6.14
Table 6.14
Specific questions to ask the patient: Diarrhoea
| Question | Relevance |
| Frequency and nature of the stools | Patients with acute self-limiting diarrhoea will be passing watery stools more frequently than normal Diarrhoea associated with blood and mucus (dysentery) requires referral to eliminate invasive infection such as Shigella, Campylobacter, Salmonella or E. coli O157 Bloody stools is also associated with conditions such as inflammatory bowel disease |
| Periodicity | A history of recurrent diarrhoea of no known cause should be referred for further investigation |
| Duration | A person who presents with a history of chronic diarrhoea should be referred. The most frequent causes of chronic diarrhoea are IBS, inflammatory disease and colon cancer |
| Onset of symptoms | Ingestion of bacterial pathogens can give rise to symptoms in a matter of a few hours (toxin producing bacteria) after eating contaminated food or up to 3 days later. It is therefore important to ask about food consumption over the last few days, establish if anyone else ate the same food and to check the status of his or her health |
| Timing of diarrhoea | Patients who experience diarrhoea first thing in the morning might well have underlying pathology such as IBS Nocturnal diarrhoea is often associated with inflammatory bowel disease |
| Recent change of diet | Changes in diet can cause changes to bowel function, for example when away on holiday. If the person has recently been to a non-Western country then giardiasis is a possibility |
| Signs of dehydration | Mild (<5%) dehydration can be vague but include tiredness, anorexia, nausea and light-headedness Moderate (5 to 10%) dehydration is characterised by dry mouth, sunken eyes, decreased urine output, moderate thirst and decreased skin turgor (pinch test of 1 to 2 seconds or longer) |
Clinical features of acute diarrhoea
Symptoms are normally rapid in onset, with the patient having a history of prior good health. Nausea and vomiting might be present prior to or during the bout of acute diarrhoea. Abdominal cramping, flatulence and tenderness is also often present. If rotavirus is the cause the patient might also experience viral prodromal symptoms such as cough and cold. Acute infective diarrhoea is usually watery in nature with no blood present. Complete resolution of symptoms should be observed in 2 to 4 days. However, diarrhoea caused by the rotavirus can persist for longer.
Conditions to eliminate
Medicine-induced diarrhoea: Many medicines (both POM and OTC) can induce diarrhoea (Table 6.15). If medication is suspected as the cause of the diarrhoea the GP should be contacted and an alternative suggested.
![]() Table 6.15
Table 6.15
Examples of medicines known to cause diarrhoea (defined as very common [>10%] or common [1–10%])
| α-blocker | Prazosin |
| ACE inhibitor | Lisinopril, perindopril |
| Angiotensin receptor blocker | Telmisartan |
| Acetylcholinesterase inhibitor | Donepezil, galantamine, rivastigmine |
| Antacid | Magnesium salts |
| Antibacterial | All |
| Antidiabetic | Metformin, acarbose |
| Antidepressant | SSRIs, clomipramine, venlafaxine |
| Anti-emetic | Aprepitant, dolasetron |
| Anti-epileptic | Carbamazepine, oxcarbamazepine, tiagabine, zonisamide, pregabalin, levetiracetam |
| Antifungal | Caspofungin, fluconazole, flucytosine, nystatin (in large doses), terbinafine, voriconazole |
| Antimalarial | Mefloquine |
| Antiprotozoal | Metronidazole, sodium stibogluconate |
| Antipsychotic | Aripiprazole |
| Antiviral | Abacavir, emtricitabine, stavudine, tenofovir, zalcitabine, zidovudine, amprenavir, atazanavir, indinavir, lopinavir, nelfinavir, saquinavir, efavirenz, ganciclovir, valganciclovir, adefovir, oseltamivir, ribavirin, fosamprenavir |
| Beta-blocker | Bisoprolol, carvedilol, nebivolol |
| Bisphosphonate | Alendronic acid, disodium etidronate, ibandronic acid, risedronate, sodium clodronate, disodium pamidronate, tiludronic acid |
| Cytokine inhibitor | Adalimumab, infliximab |
| Cytotoxic | All classes of cytotoxics |
| Dopaminergic | Levodopa, entacapone |
| Growth hormone antagonist | Pegvisomant |
| Immunosuppressant | Ciclosporin, mycophenolate, leflunomide |
| NSAID | All |
| Ulcer healing | Proton pump inhibitors |
| Vaccines | Pediacel (5 vaccines in 1), haemophilus, meningococcal |
| Miscellaneous | Calcitonin, strontium ranelate, colchicines, dantrolene, olsalazine, anagrelide, nicotinic acid, pancreatin, eplerenone, acamprosate |
Reproduced with permission from R Walker and C Whittlesea, Clinical pharmacy and therapeutics, 5th edition, 2011, Churchill Livingstone.
Unlikely causes
Irritable bowel syndrome: Patients younger than 45 with lower abdominal pain and a history of alternating diarrhoea and constipation are likely to have IBS. For further details on IBS see page 168.
Giardiasis: Giardiasis, a protozoan infection of the small intestine, is contracted through drinking contaminated drinking water. It is an uncommon cause of diarrhoea in Western society. However, with more people taking exotic foreign holidays, enquiry about recent travel should be made. The patient will present with watery and foul-smelling diarrhoea accompanied with symptoms of bloating, flatulence and epigastric pain. If giardiasis is suspected the patient must be referred to the GP quickly for confirmation and appropriate antibiotic treatment.
Faecal impaction: Faecal impaction is most commonly seen in the elderly and those with poor mobility. Patients might present with continuous soiling as a result of liquid passing around hard stools and mistakenly believe they have diarrhoea. On questioning, the patient might describe the passage of regular poorly formed hard stools that are difficult to pass. Referral is needed as manual removal of the faeces is often needed.
Very unlikely causes
Ulcerative colitis and Crohn’s disease: Both conditions are characterised by chronic inflammation at various sites in the GI tract and follow periods of remission and relapse. They can affect any age group, although peak incidence is between 20 and 30 years of age. In mild cases of both conditions, diarrhoea is one of the major presenting symptoms, although blood in the stool is usually present. Patients might also find that they have urgency, nocturnal diarrhoea and early morning rushes. In the acute phase patients will appear unwell and have malaise.
Malabsorption syndromes: Lactose intolerance is often diagnosed in infants under 1 year old. In addition to more frequent loose bowel movements symptoms such as fever, vomiting, perianal excoriation and a failure to gain weight might occur.
Coeliac disease has a bimodal incidence: first, in early infancy when cereals become a major constituent of the diet, and second, during the fourth and fifth decades. Steatorrhoea (fatty stools) is common and might be observed by the patient as frothy or floating stools in the toilet pan. Bloating and weight loss in the presence of a normal appetite might also be observed.
Colorectal cancer: Any middle-aged patient presenting with a longstanding change of bowel habit must be viewed with suspicion. Persistent diarrhoea accompanied by a feeling that the bowel has not really been emptied is suggestive of neoplasm. This is especially true if weight loss is also present.
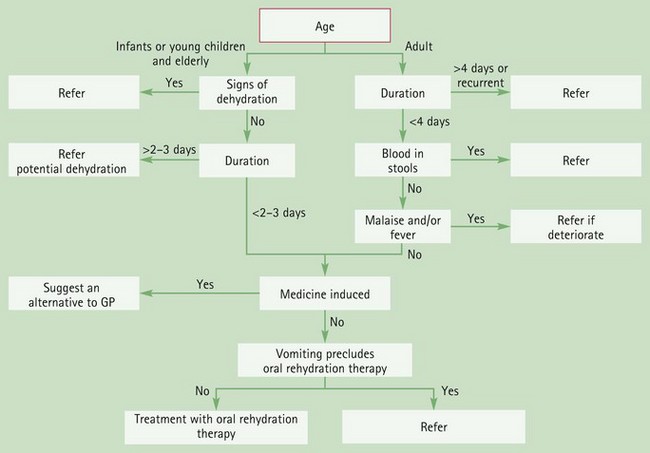
Figure 6.11 will aid differentiation of diarrhoeal cases that require referral.
Evidence base for over-the-counter medication
Acute infectious diarrhoea still remains one of the leading causes of death in developing countries, despite advances in its treatment. In developed and Western countries diarrhoeal disease is primarily of economic and socially disruptive significance. Goals of OTC treatment in the UK are therefore concentrated on relief of symptoms.
Before considering treatment it is important to stress to patients the importance of hand washing. Interventions that promote hand washing can reduce diarrhoea episodes by about one-third.
Oral rehydration solution (ORS)
ORS represents one of the major advances in medicine. It has proved to be a simple highly effective treatment, which has decreased mortality and morbidity associated with acute diarrhoea in developing countries. The formula recommended by the World Health Organization (WHO) contains glucose (75 mmol/L), sodium (75 mmol/L), potassium (20 mmol/L), chloride (65 mmol/L) and citrate (10 mmol/L) in an almost isotonic fluid. Until recently, the WHO oral rehydration solution contained 90 mmol/L sodium but a systematic review (Hahn et al 2002) concluded that ORS with a reduced osmolarity compared to the standard WHO formula were associated with fewer complications in children with mild to moderate diarrhoea. Based on this, and other findings, the WHO oral rehydration solution now has a reduced osmolarity of 245 mm/L, which contains 75 mmol of sodium. A number of similar preparations are available commercially in the form of sachets that require reconstitution in clean water before use; however, commercially available solutions in the UK contain lower sodium concentrations as diarrhoea tends to be isotonic, and therefore replacement of large quantities of sodium is less important.
Rice-based ORS
In many developing countries a glucose substitute was added to electrolytes because of glucose unavailability. These products were found to be quite successful. Clinical trials have subsequently shown rice-based ORS to be highly efficacious, well tolerated and potentially more effective than conventional ORS.
Loperamide
Loperamide is a synthetic opioid analogue and is thought to exert its action via opiate receptors slowing intestinal tract time and increasing the capacity of the gut. It has been extensively researched, with many published trials investigating its effectiveness in acute infectious diarrhoea. The majority of well-designed double-blind placebo-controlled trials have consistently shown it to be significantly better than placebo and comparable to diphenoxylate. Loperamide is also available compounded with simeticone. However, there is little evidence of better efficacy in terms of diarrhoeal symptoms with the combination.
Bismuth subsalicylate
Bismuth-containing products have been used for many decades. Its use has declined over time as other products have become more popular. However, bismuth subsalicylate has been shown to be effective in treating traveller’s diarrhoea. A review paper by Steffen (1990) concluded that bismuth subsalicylate was clinically superior to placebo, decreasing the number of unformed stools and increasing the number of patients who were symptom free. However, two of the trials reviewed showed bismuth subsalicylate to be significantly slower in symptom resolution than its comparator drug loperamide.
Kaolin and morphine
The constipating side effect of opioid analgesics can be used to treat diarrhoea. However, kaolin and morphine products have no evidence of efficacy and should not be recommended. It remains a popular home remedy, especially with the elderly.
Rotavirus vaccine
In 2006, two new oral vaccines (Rotarix, and RotaTeq) were licensed by the European Medicines Agency and the US Food and Drug Administration. Clinical trials have shown them to be effective (Soares-Weiser et al 2012).
From 2013, the rotavirus vaccine will be added to the routine UK childhood vaccination schedule.
Summary
Since diarrhoea results in fluid and electrolyte loss it is important to re-establish normal fluid balance and so ORS is first line treatment for all age groups, especially children and the frail elderly. Loperamide is a useful adjunct in reducing the number of bowel movements but should be reserved for those patients who will find it inconvenient to have to go to the toilet.
Practical prescribing and product selection
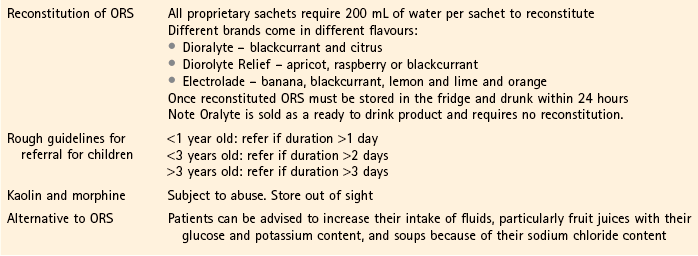
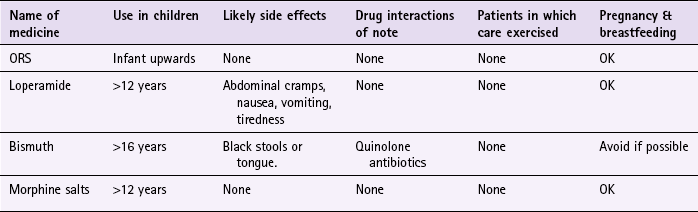
Prescribing information relating to the medicines used for diarrhoea reviewed in the section ‘Evidence base for over-the-counter medication’ is discussed and summarised in Table 6.16; useful tips relating to patients presenting with diarrhoea are given in Hints and Tips Box 6.5.
ORS (Dioralyte, Dioralyte Relief (rice-based), Electrolade, Oralyte)
ORS can be given to all patient groups, has no side effects or drug interactions. The volume of solution given is dependent on how much fluid is lost. As infants and the elderly are more at risk of developing dehydration they should be encouraged to drink as much ORS as possible. In adults, 2 L of ORS should be given in the first 24 hours, followed by unrestricted normal fluids with 200 mL of rehydration solution per loose stool or vomit. The solution is best sipped every 5–10 min rather than drunk in large quantities less frequently. In infants, 1 to  times the usual feed volume should be given.
times the usual feed volume should be given.
Loperamide (e.g. Diocalm Ultra, Diah-Limit, Imodium range)
The dose is two capsules immediately, followed by one capsule after each further bout of diarrhoea. It has minimal CNS side effects, although CNS depressant effects and respiratory depression have been reported at high doses. OTC doses are therefore limited to 16 mg a day and cannot be used in children under 12. The excellent safety record of loperamide has seen it granted General Sales List status, although abdominal cramps, nausea, vomiting, tiredness, drowsiness, dizziness and dry mouth have been reported. Loperamide is available in a range of formulations, such as dispersible tablets, melt-tabs and liquid.
Bismuth (Pepto-Bismol Liquid 87.6 mg/5 mL bismuth subsalicylate and Chewable tablet 262.5 mg)
Pepto-Bismol should only be given to people over the age of 16. The dose is 30 mL or two tablets taken every 30 min to 1 hour when needed, with a maximum of eight doses in 24 hours. Bismuth subsalicylate is well tolerated and has a favourable side-effect profile, although black stools are commonly observed (caused by unabsorbed bismuth compound). Occasional use is not known to cause problems during pregnancy and breastfeeding but the manufacturers state it should not be used. Bismuth can decrease the bioavailability of quinolone antibiotics therefore a minimum 2-hour gap should be left between doses of each medicine.
Morphine (e.g. Kaolin and morphine, Diocalm Dual Action)
Morphine is generally well tolerated at OTC doses, with no side effects reported. The products can be given to all patient groups, including pregnant and breastfeeding women. There are no drug interactions of note. Morphine is available as a non-proprietary product (Kaolin and morphine) and J Collis Browne’s products.
References
Soares-Weiser, K, MacLehose, H, Bergman, H, et al. Vaccines for preventing rotavirus diarrhoea: vaccines in use. Cochrane Database of Systematic Reviews. (Issue 2):2012. [Art. No.: CD008521. DOI: 10.1002/14651858.CD008521.pub2].
Steffen, R. Worldwide efficacy of bismuth subsalicylate in the treatment of travelers’ diarrhea. Rev Infect Dis. 1990;12:S80–S86.
American Academy of Pediatrics [AAP] Committee on Quality Improvement SoAG. Practice Parameter. The management of acute gastroenteritis in young children. Pediatrics. 1996;97:4224–4433.
Amery, W, Duyck, F, Polak, J, et al. A multicentre double-blind study in acute diarrhoea comparing loperamide (R 18553) with two common antidiarrhoeal agents and a placebo. Curr Ther Res Clin Exp. 1975;17:263–270.
Chassany, O, Michaux, A, Bergman, JF. Drug-induced diarrhoea. Drug Safety. 2000;22:53–72.
Cornett, JWD, Aspeling, RL, Mallegol, D. A double blind comparative evaluation of loperamide versus diphenoxylate with atropine in acute diarrhea. Curr Ther Res. 1977;21:629–637.
Ejemot-Nwadiaro, RI, Ehiri, JE, Meremikwu, MM, et al. Hand washing for preventing diarrhoea. Cochrane Database of Systematic Reviews. (Issue 1):2008. Art. No.: CD004265. DOI: 10.1002/14651858.CD004265.pub2
Gavin, N, Merrick, N, Davidson, B. Efficacy of glucose-based oral rehydration therapy. Pediatrics. 1996;98:45–51.
Hahn, S, Kim, Y, Garner, P. Reduced osmolarity oral rehydration solution for treating dehydration caused by acute diarrhoea in children. Cochrane Database of Systematic Reviews. (Issue 1):2002. Art. No.: CD002847. DOI: 10.1002/14651858.CD002847
Islam, A, Molla, AM, Ahmed, MA, et al. Is rice based oral rehydration therapy effective in young infants? Arch Dis Child. 1994;71:19–23.
Molla, AM, Sarker, SA, Hossain, M, et al. Rice-powder electrolyte solution as oral-therapy in diarrhoea due to Vibrio cholerae and Escherichia coli. Lancet. 1982;1(8285):1317–1319.
Nelemans, FA, Zelvelder, WG. A double-blind placebo controlled trial of loperamide (Imodium) in acute diarrhea. J Drug Res. 1976;2:54–59.
Patra, FC, Mahalanabis, D, Jalan, KN, et al. Is oral rice electrolyte solution superior to glucose electrolyte solution in infantile diarrhoea? Arch Dis Child. 1982;57:910–912.
Selby, W. Diarrhoea – differential diagnosis. Aust Fam Physician. 1990;19:1683–1686.
Soares-Weiser, K, Goldberg, E, Tamimi, G, et al. Rotavirus vaccine for preventing diarrhoea. Cochrane Database of Systematic Reviews. (Issue 1):2004. Art. No.: CD002848. DOI: 10.1002/14651858.CD002848.pub2
Steffen, R. Worldwide efficacy of bismuth subsalicylate in the treatment of travelers’ diarrhea. Rev Infect Dis. 1990;12:S80–S86.
National Association for Colitis and Crohn’s disease (NACC) – Crohn’s and Colitis UK. http://www.nacc.org.uk
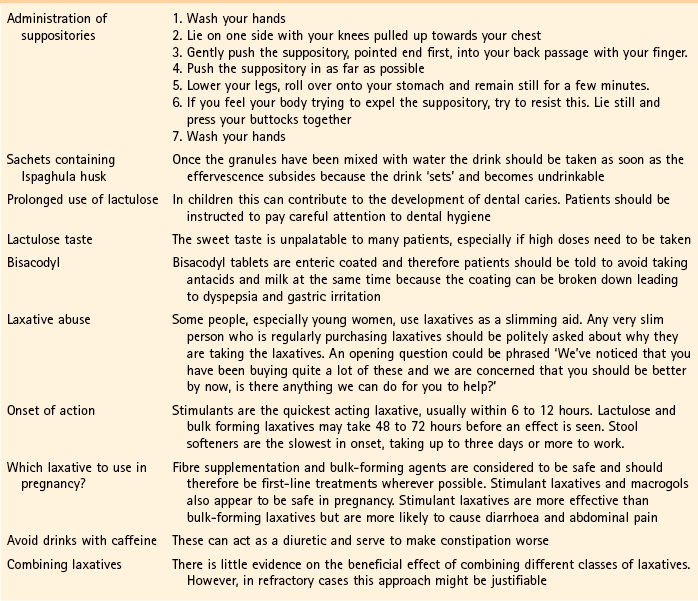
Constipation
Background
Constipation, like diarrhoea, means different things to different people. Constipation arises when the patient experiences a reduction in their normal bowel habit accompanied with more difficult defecation and/or hard stools. In Western populations 90% of people defecate between three times a day and once every three days. However, many people still believe that anything other than one bowel movement a day is abnormal.
Prevalence and epidemiology
Constipation is very common. It occurs in all age groups but is especially common in the elderly. It has been estimated that 25 to 40% of all people over the age of 65 have constipation. The majority of the elderly have normal frequency of bowel movements but strain at stool. This is probably a result of sedentary lifestyle, a decreased fluid intake, poor nutrition, avoidance of fibrous foods and chronic illness. Women are two to three times more likely to suffer from constipation than men and 40% of women in late pregnancy experience constipation.
Aetiology
The normal function of the large intestine is to remove water and various salts from the colon, drying and expulsion of the faeces. Any process that facilitates water resorption will generally lead to constipation. The commonest cause of constipation is an increase in intestinal tract transit time of food which allows greater water resorption from the large bowel leading to harder stools that are more difficult to pass. This is most frequently caused by a deficiency in dietary fibre, a change in lifestyle and/or environment and medication. Occasionally, patients ignore the defecatory reflex as it maybe inconvenient for them to defecate.
Arriving at a differential diagnosis
The first thing a pharmacist should do is to establish the patient’s current bowel habit compared to normal. This should establish if the patient is suffering from constipation. Questioning should then concentrate on determining the cause because constipation is a symptom and not a disease and can be caused by many different conditions. Constipation does not usually have sinister pathology and the commonest cause in the vast majority of non-elderly adults will be a lack of dietary fibre (Table 6.17). However, constipation can be caused by medication and many disease states including neurological disorders (e.g. multiple sclerosis, Parkinson’s disease), metabolic and endocrine conditions (diabetes, hypothyroidism) and neoplasm. A number of constipation-specific questions should always be asked of the patient to aid in diagnosis (Table 6.18).
Table 6.17
Causes of constipation and their relative incidence in community pharmacy
| Incidence | Cause |
| Most likely | Eating habits/lifestyle |
| Likely | Medication |
| Unlikely | Irritable bowel syndrome, pregnancy, depression, functional disorders (children) |
| Very unlikely | Colorectal cancer, hypothyroidism |
![]() Table 6.18
Table 6.18
Specific questions to ask the patient: Constipation
| Question | Relevance |
| Change of diet or routine | Constipation usually has a social or behavioural cause. There will usually be some event that has precipitated the onset of symptoms |
| Pain on defecation | Associated pain when going to the toilet is usually due to a local anorectal problem. Constipation is often secondary to the suppression of defecation because it induces pain. These cases are best referred for physical examination |
| Presence of blood | Bright red specks in the toilet or smears on toilet tissue suggest haemorrhoids or a tear in the anal canal (fissure). However, if blood is mixed in the stool (melaena) then referral to the GP is necessary. A stool that appears black and tarry is suggestive of an upper GI bleed |
| Duration (chronic or recent?) | Constipation lasting 6 weeks or more is said to be chronic. If a patient suffers from longstanding constipation and has been previously seen by the GP then treatment could be given. However, cases of more than 14 days with no identifiable cause or previous investigation by the GP should be referred |
| Lifestyle changes | Changes in job or marital status can precipitate depressive illness that can manifest with physiological symptoms such as constipation |
Clinical features of constipation
Besides the inability to defecate, patients might also have abdominal discomfort and bloating. In children, parents might also notice the child is more irritable and have a decreased appetite. Specks of blood in the toilet pan might be present and are usually due to straining at stool. In the vast majority of cases blood in the stool does not indicate sinister pathology. Those patients presenting with acute constipation with no other symptoms apart from very small amounts of bright red blood can be managed in the pharmacy, however, if blood loss is substantial (stools appear tarry, red or black) or the patient has other associated symptoms such as malaise, abdominal distension and is over 40 years old then referral is needed.
Conditions to eliminate
Medicine-induced constipation: Many medicines are known to cause constipation. Most exert their action by decreasing gut motility, although opioids tend to raise sphincter tone and reduce sensitivity to rectal distension. A detailed medication history should always be sought from the patient and Table 6.19 lists the commonly implicated medicines that cause constipation.
![]() Table 6.19
Table 6.19
Examples of medicines known to cause constipation (frequency defined as very common [>10%] or common [1–10%])
| α-blocker | Prazosin |
| Antacid | Aluminium and calcium salts |
| Anticholinergic | Trihexyphenidyl, hyoscine, oxybutynin, procyclidine, tolterodine |
| Antidepressant | Tricyclics, SSRIs, reboxetine, venlafaxine, duloxetine, mirtazapine |
| Anti-emetic | Palonosetron, dolasetron, aprepitant |
| Anti-epileptic | Carbamazepine, oxcarbazepine |
| Antipsychotic | Phenothiazines, haloperidol, pimozide and atypical antipsychotics such as amisulpride, aripiprazole, olanzapine, quetiapine, risperidone, zotepine, clozapine |
| Antiviral | Foscarnet |
| Beta-blocker | Oxprenolol, bisoprolol, nebivolol; other βετα-blockers tend to cause constipation more rarely |
| Bisphosphonate | Alendronic acid |
| CNS stimulant | Atomoxetine |
| Calcium channel blocker | Diltiazem, verapamil |
| Cytotoxic | Bortezomib, buserelin, cladribine, docetaxel, doxorubicin, exemestane, gemcitabine, irinotecan, mitoxantrone, pentostatin, temozolomide, topotecan, vinblastine, vincristine, vindesine, vinorelbine |
| Dopaminergic | Amantadine, bromocriptine, cabergoline, entacapone, tolcapone, levodopa, pergolide, pramipexole, quinagolide |
| Growth hormone antagonist | Pegvisomant |
| Immunosuppressant | Basiliximab, mycophenolate, tacrolimus |
| Lipid-lowering agent | Cholestyramine, colestipol, rosuvastatin, atorvastatin (other statins uncommon), gemfibrozil |
| Iron | Ferrous sulphate |
| Metabolic disorders | Miglustat |
| Muscle relaxant | Baclofen |
| NSAID | Meloxicam; other NSAIDs, e.g. aceclofenac, and COX-2 inhibitors reported as uncommon |
| Smoking cessation | Bupropion |
| Opioid analgesic | All opioid analgesics and derivatives |
| Ulcer healing | All proton pump inhibitors, sucralfate |
Reproduced with permission from R Walker and C Whittlesea, Clinical pharmacy and therapeutics, 5th edition, 2011, Churchill Livingstone.
Unlikely causes
Irritable bowel syndrome: Patients younger than 45 with lower abdominal pain and a history of alternating diarrhoea and constipation are likely to have IBS. For further details on IBS see page 168.
Pregnancy: Constipation is common in pregnancy, especially in the third trimester. A combination of increased circulating progestogen, displacement of the uterus against the colon by the fetus, decreased mobility and iron supplementation all contribute to an increased incidence of constipation whilst pregnant. Most patients complain of hard stools rather than a decrease in bowel movements. If a laxative is used a bulk-forming laxative should be recommended.
Depression: Upwards of 20% of the population will suffer from depression at sometime. Many will present with physical as well as emotional symptoms. It has been reported that a third of all patients suffering from depression present with gastrointestinal complaints in a primary care setting. Core symptoms of persistent low mood and loss of interest in most activities should trigger referral.
Functional causes in children: Constipation in children is common and the cause can be varied. Constipation is not normally a result of organic disease but stems from poor diet or a traumatic experience associated with defecation, for example, unwillingness to defecate due to association of prior pain on defecation.
Very unlikely causes
Colorectal cancer: Colorectal carcinomas are rare in patients under the age of 40. However, the incidence of carcinoma increases with increasing age and any patient over the age of 40 presenting for the first time with a marked change in bowel habit should be referred. Sexes appear to be equally affected. The patient might complain of abdominal pain, rectal bleeding and tenesmus. Weight loss – a classical textbook sign of colon cancer – is common but observed only in the latter stages of the disease. Therefore a patient is unlikely to have noticed marked weight loss when visiting a pharmacy early in disease progression.
Hypothyroidism: The signs and symptoms of hypothyroidism are often subtle and insidious in onset. Patients might experience weight gain, lethargy, cold intolerance, coarse hair and dry skin as well as constipation. Hypothyroidism affects ten times more women than men and peak incidence is in the fifth or sixth decade. Constipation is often less pronounced than lethargy and cold intolerance.
Figure 6.12 will aid differentiation between common causes of constipation and more serious causes.
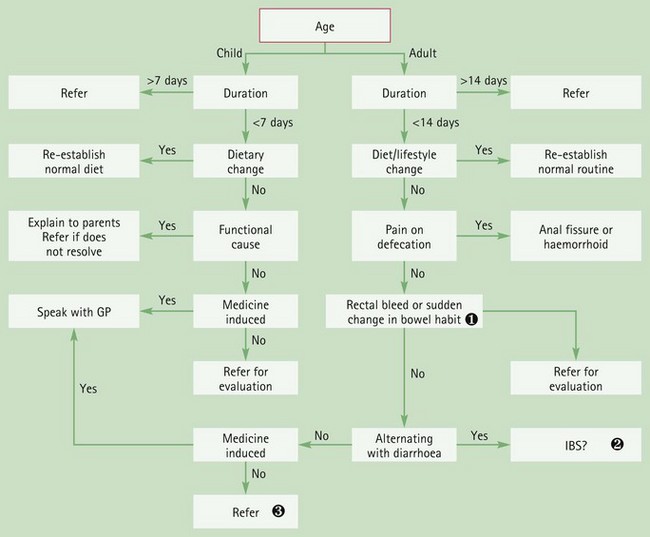
Fig. 6.12 Primer for differential diagnosis of constipation.![]() Patients with unexplained constipation of recent onset accompanied with rectal bleeding should be referred for further investigation; most likely a colonoscopy or sigmoidoscopy and stool culture to eliminate carcinoma
Patients with unexplained constipation of recent onset accompanied with rectal bleeding should be referred for further investigation; most likely a colonoscopy or sigmoidoscopy and stool culture to eliminate carcinoma![]() See Fig. 6.13 for primer for differential diagnosis of IBS.
See Fig. 6.13 for primer for differential diagnosis of IBS.![]() If no obvious cause of constipation can be found referral to the GP is needed for further evaluation.
If no obvious cause of constipation can be found referral to the GP is needed for further evaluation.
Evidence base for over-the-counter medication
For uncomplicated constipation, non-drug treatment is advocated as first-line treatment for all patient groups as simple dietary and lifestyle modifications (increasing exercise) will relieve the majority of acute cases of constipation. Advice includes increasing fluid and fibre intake. Dietary fibre increases stool bulk, stool water content and colonic bacterial load. Fibre intake should be increased to approximately 30 g day in the form of fruit, vegetables, cereals, grain foods and wholemeal bread. It is important to remind patients that adequate fluid intake (2 L per day) is needed when following a high-fibre diet and patients might experience excessive gas production, colicky abdominal pain and bloating. Effects of a high-fibre diet are usually seen in 3 to 5 days.
If medication is required, four classes of OTC laxatives are available: bulk-forming agents, stimulants, osmotics and stool softeners. Despite their widespread use surprisingly few well-designed trials have substantiated clinical efficacy.
A systematic review in 1997 (Tramonte et al) identified 36 trials involving 1815 participants that met their inclusion criteria and involved 25 different laxatives representing all four classes of laxative. Twenty of the trials compared laxative against placebo or regular diet, 13 of which demonstrated statistically significant increases in bowel movement. The remaining 16 trials compared different types of laxatives with each other. The review concluded that laxatives do increase the number of bowel movements and, in 9 of 11 trials studying overall symptom control, laxatives did perform significantly better than placebo. Unfortunately, because of a lack of comparative trial data, the review could not conclude which laxative was most efficacious. A further review of laxative effect in elderly patients suffering with chronic constipation also failed to determine superior clinical effect between laxative classes. The findings from the Tramonte paper was reviewed in 2005 by the centre for reviews and dissemination which supported them.
Practical prescribing and product selection
Prescribing information relating to the medicines used for constipation reviewed in the section ‘Evidence base for over-the-counter medication’ is discussed and summarised in Table 6.20; useful tips relating to these medicines are given in Hints and Tips Box 6.6.
![]() Table 6.20
Table 6.20
Practical prescribing: Summary of medicines for constipation
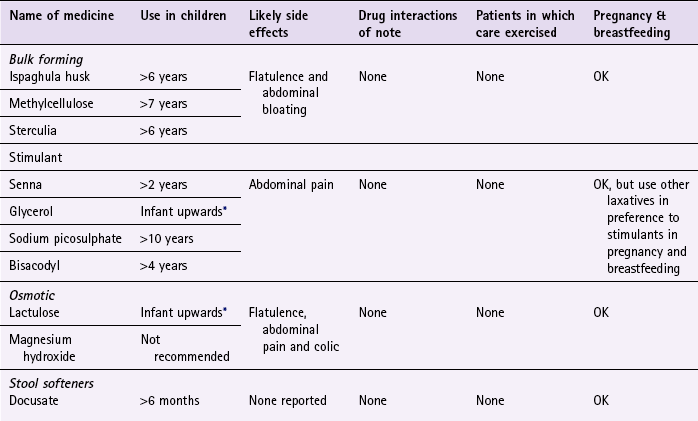
*If prescribing to children less than 6 years of age then the pharmacist must be competent in prescribing laxatives for children.
Prescribing laxatives in children should ideally be left to those healthcare professionals experienced in managing childhood constipation (BNF edition 63). OTC products are licensed for use in young children but in accordance with good practice those children younger than 6 years old who have failed to respond to dietary intervention should be referred to their GP. The text below does however make reference to dosing in children younger than 6.
Bulk-forming laxatives (e.g. ispaghula husk, methylcellulose and sterculia)
Bulk-forming laxatives exert their effect by mimicking increased fibre consumption, swelling in the bowel and increasing faecal mass. In addition, they also encourage the proliferation of colonic bacteria and this helps further increase faecal bulk and stool softness. Patients should be advised to increase their fluid intake whilst taking bulk-forming medicines. Their effect is usually seen in 12 to 36 hours but can take as long as 72 hours. Side effects commonly experienced include flatulence and abdominal distension. They are well tolerated in pregnancy and breastfeeding and have no teratogenic effects. They appear to have no drug interactions of any note.
Ispaghula husk
Ispaghula husk is widely available as either granules (Fibrelief, Fybogel, Isogel, Ispagel) or powder (Regulan). All have to be reconstituted with water prior to taking. The dose for adults and children over 12 years old can range from one to six sachets a day depending on the brand used and the severity of the condition. Fybogel is probably the most familiar branded product used OTC in the UK – adults should take 1 sachet or 2 level 5 mL spoonfuls twice a day and for children aged between 6 and 12,  to one 5 mL spoonful twice daily.
to one 5 mL spoonful twice daily.
Methylcellulose (Celevac)
Methylcellulose is only available as Celevac tablets. The adult dose is three to six tablets twice daily, and for children aged between 7 and 12, the dose is two tablets twice a day. Each dose should be taken with at least 300 mL of liquid.
Sterculia (Normacol and Normacol Plus granules or sachets)
Both products contain 62% sterculia but Normacol Plus also contains 8% frangula. The dose for both products is the same. Adults and children over 12 should take either one or two sachets or heaped 5 mL spoonfuls, once or twice daily after meals. For children aged between 6 and 12 the dose is half that of the adult dose.
The granules should be placed dry on the tongue and swallowed immediately with plenty of water or a cool drink. They can also be sprinkled onto, and taken with, soft food such as yoghurt.
Stimulant laxatives (e.g. bisacodyl, glycerol, senna, sodium picosulfate)
Stimulant laxatives increase GI motility by directly stimulating colonic nerves. It is this action that, presumably, causes abdominal pain and is the main side effect associated with stimulant laxatives. Additionally, stimulant laxatives are associated with the possibility of nerve damage in long-term use and are the most commonly abused laxatives. Their onset in action is quicker than other laxative classes, with patients experiencing a bowel movement in 6 to 12 hours when taken orally. They can be taken by all patient groups, have no drug interactions and are safe in pregnancy and breastfeeding. However, because of their stimulant effect on uterine contractions they are best avoided in pregnancy if possible.
Bisacodyl (Dulcolax)
Bisacodyl is available as either tablets or suppositories and can be given to patients aged over 4 years old. The dose for children aged between 4 and 10 years is 5 mg (one tablet or one paediatric suppository) and for adults and children over 10 years the dose is 5 to 10 mg (one to two tablets or one Dulcolax 10 mg suppository).
Glycerol suppositories
Glycerol suppositories are normally used when a bowel movement is needed quickly. The patient should experience a bowel movement in 15 to 30 minutes. Varying sizes are made to accommodate use in different ages. The 1-g suppositories are designed for infants, the 2-g for children and the 4-g for adults.
Senna (e.g. Senokot)
Senna is available as syrup, tablets or granules. Dosing of proprietary products differs from those recommended in the BNF and BNF-C. Proprietary products recommend BNF/BNF-C starting doses. These are: adults and children over 12 should take 15 mg each day, preferably at bedtime; children over 6 the dose is half that of the adult dose (7.5 mg, e.g Senokot syrup).
Sodium picosulfate (e.g. Dulcolax Pico)
Adults and children over 10 years old should take 5 to 10 mg at night.
Osmotic laxatives (e.g. lactulose, macrogols and magnesium salts)
These act by retaining fluid in the bowel by osmosis or by changing the pattern of water distribution in the faeces. Flatulence, abdominal pain and colic are frequently reported. They can be taken by all patient groups, have no drug interactions and safely used in pregnancy and breastfeeding.
Lactulose: Lactulose is given twice daily for all ages. The dose for adults is initially 15 mL, for children aged between 5 and 18 the dose is 5–20 mL, those aged between 1 and 5 the dose is 2.5–10 mL and children under 1 year of age 2.5 mL. It has been reported that up to 20% of patients experience troublesome flatulence and cramps, although these often settle after a few days. It may take 48 hours or longer for it to work.
Macrogols (e.g. Movicol, Dulcobalance): Macrogols are available as powders that are reconstituted with water. They are licensed for chronic constipation and should therefore not be routinely recommended by pharmacists because treatment should be only instigated in those presenting with acute constipation. Section 1.6.4 of the BNF highlights doses for the respective products.
Stool softeners (liquid paraffin and docusate sodium)
Liquid paraffin has been traditionally used to treat constipation. However, the adverse side-effect profile of liquid paraffin now means it should never be recommended because other, safer and more effective medications are available.
Docusate sodium: Docusate sodium is a non-ionic surfactant that has stool-softening properties that allows penetration of intestinal fluids into the faecal mass. It also has weak stimulant properties. Docusate is available as either capsules (Dioctyl) or solution (Docusal). It can be given from children aged 6 months and over. Children between the age of 6 months and 2 years should take 12.5 mg (5 mL of Docusal paediatric solution) three times a day. For children aged between 2 and 12 the dose is 12.5 to 25 mg (5 to 10 mL) three times a day. Adults and children over 12 years old should take up to 500 mg daily in divided doses. In contrast to liquid paraffin, docusate sodium seems to be almost free of any side effects. Docusate sodium can be given to all patient groups.
Borum, ML. Constipation: evaluation and management. Primary Care. 2001;28:577–590.
Gattuso, JM, Kamm, MA. Adverse effects of drugs used in the management of constipation and diarrhoea. Drug Saf. 1994;10:47–65.
Gerber, PD, Barrett, JE, Barrett, JA, et al. The relationship of presenting physical complaints to depressive symptoms in primary care patients. J Gen Intern Med. 1992:170–173.
Herz, MJ, Kahan, E, Zalevski, S, et al. Constipation: a different entity for patients and doctors. Fam Pract. 1996;13:156–159.
Higgins, PDR, Johnson, JF. Epidemiology of constipation in North America: a systemic review. Am J Gast. 2004;99:750–759.
Jewell, D, Young, G. Interventions for treating constipation in pregnancy. Cochrane Database of Systematic Reviews. (Issue 2):2001. Art. No.: CD001142. DOI: 10.1002/14651858.CD001142
Leng-Peschlow, E. Senna and its rational use. Pharmacology. 1992;44:S1–52.
Paraskevaides, EC. Fatal lipid pneumonia and liquid paraffin. Br J Clin Pract. 1990;44:509–510.
Petticrew, M, Watt, I, Brand, M. What’s the ‘best buy’ for treatment of constipation? Results of a systematic review of the efficacy and comparative efficacy of laxatives in the elderly. Br J Gen Pract. 1999;49:387–393.
Talley, NJ, Fleming, KC, Evans, JM, et al. Constipation in an elderly community: a study of prevalence and potential risk factors. Am J Gastroenterol. 1996;9:19–25.
Irritable bowel syndrome
Background
IBS is one of the commonest GI tract conditions seen in primary care. It can be defined as a functional bowel disorder (i.e. absence of abnormality) in which abdominal pain and bloating is associated with a change in bowel habit. The diagnosis is suggested by the presence of longstanding colonic symptoms without any deterioration in the patient’s general condition.
Prevalence and epidemiology
IBS is common. Adult prevalence rates in Western countries are reported to be between 10 and 20%, with approximately twice as many women than men affected. It most commonly affects people between 20 and 30 years old but recent trends indicate that there is a significant prevalence of IBS in older people.
Aetiology
No anatomic cause can be found to explain the aetiology of IBS but it is now clearly understood to be multifactorial. Many factors can contribute to disease expression and include motility dysfunction, diet and genetics. In a small proportion of cases symptoms appear after bacterial gastroenteritis. Psychological factors also influence symptom reporting and consultation and some studies have shown patients who suffer from higher levels of stress or depression experience worse symptoms when compared to other patients. Flare-up of symptoms has also been associated with periods of increased stress. Symptoms of diarrhoea and constipation appear to be linked with hyperactivity of the small intestine and colon in response to food ingestion and parasympathomimetic drugs. Excessive parasympathomimetic activity might account for mucus associated with the stool.
Arriving at a differential diagnosis
IBS is essentially a diagnosis of exclusion and a careful and thorough history of the patient is essential. Diagnostic aids, such as rectal examination and biopsy, which can be used by GPs are of limited use. A number of IBS-specific questions should always be asked of the patient to aid in diagnosis (Table 6.21).
Clinical features of IBS
IBS is characterised by abdominal pain or discomfort, located especially in the left lower quadrant of the abdomen, which is often relieved by defecation or the passage of wind. Altered defecation, either constipation or diarrhoea, with associated bloating is also normally present. People with IBS can present with ‘diarrhoea predominant’, ‘constipation predominant’ or alternating symptom profiles. During bouts of diarrhoea, mucus tends to be visible on the stools. Patients might also complain of increased stool frequency but pass normal or pellet-like stools. Diarrhoea on wakening and shortly after meals is also observed in many patients.
Conditions to eliminate
Since the major presenting symptom of IBS is an alteration in defecation, it is necessary to differentiate IBS from acute and chronic causes of constipation and diarrhoea. For further information on differentiating these conditions from IBS please refer to page 160 (for constipation) and page 154 (for diarrhoea).
Figure 6.13 will aid differentiation of IBS from other abdominal conditions.
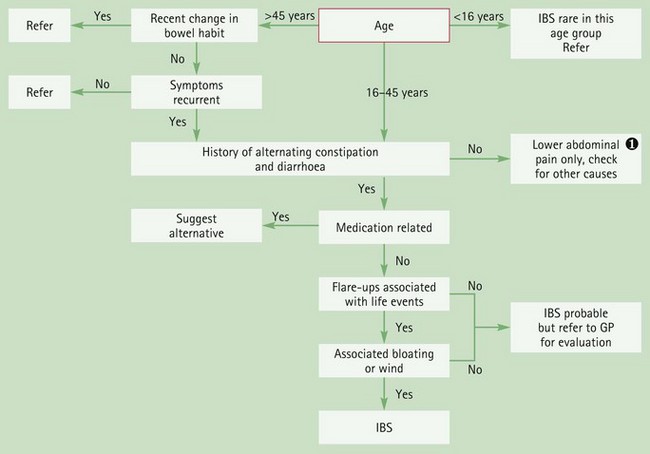
Fig. 6.13 Primer for differential diagnosis of irritable bowel syndrome.![]() Lower abdominal pain
Lower abdominal pain
See Fig. 6.29 for primer for differential diagnosis of abdominal pain.
Evidence base for over-the-counter medication
Before medicines are recommended it might be useful to discuss if stress is a factor and if this can be avoided. In addition, dietary modification has shown to be effective for some patients. (see Hints and Tips Box 6.7) If diet is deemed a major contributor toward symptoms then food avoidance can be tried. Suspected food products must be excluded from the diet for a minimum of 2 weeks and then gradually reintroduced to determine if the food item triggers symptoms.
Antispasmodics are considered first-line pharmacological intervention for IBS, although the evidence base for them is weak; these include mebeverine, alverine, hyoscine and peppermint oil. In addition, bulk-forming and stimulant laxatives can be used to treat constipation-predominant IBS and loperamide for diarrhoea-predominant IBS. Both laxatives and diarrhoeals can be taken on a regular basis using the lowest effective dose. The following text only concentrates on the evidence for those products specifically marketed for the treatment of IBS.
Antispasmodics
The Cochrane review by Ruepert (2011) concluded that antispasmodics as a class of medicines when compared to placebo provided a statistically significant benefit for abdominal pain, global assessment and IBS symptom score. However, as the authors acknowledge, antispasmodics are pharmacologically diverse and in their review it was not possible to include all compounds (due to limited number of studies) at sub-group analysis. Therefore, in this review, it was not possible to determine the individual effectiveness of certain OTC antispasmodics available in the UK. No data was reviewed for alverine and only one trial was included that considered mebeverine. In that trial (Kruis et al 1986) no statistically significant effect for improvement of global assessment was found for mebeverine. Similarly, for hyoscine no statistically significant effect for improvement of global assessment was found. The only OTC product which the review found evidence of efficacy was peppermint oil. For peppermint oil a statistically significant effect for improvement of global assessment and effect for improvement of IBS symptom score was found.
Alternative treatments
Herbal remedies for IBS have been subject to a Cochrane review (Liu et al 2006). Seventy-five trials were reviewed involving 71 different herbal medicines versus placebo or conventional pharmacological treatment. When compared against placebo, STW 5 and STW5-II, Padma Lax, Tongxie Yaofang, and Ayurvedic preparation showed significant improvement of global symptoms. Compared with conventional therapy (in 65 trials testing 51 different herbal medicines) 22 herbal medicines demonstrated a statistically significant benefit for symptom improvement. Most trials were however deemed to be of poor methodological quality and authors concluded that findings should be interpreted with caution.
Probiotics, such as Lactobacillus and Bifidobacterium have also been promoted for IBS. A systematic review identified 18 studies using probiotics either alone or in combination for the treatment of IBS (Moayyedi et al 2010). The results suggested probiotics significantly improved IBS symptoms and there was no apparent difference across the probiotics. However, the authors noted that there was potential publication bias in the review, with an over-representation of small, positive studies, and therefore these estimates of efficacy are likely to be overestimates. The authors concluded that probiotics appear to be effective in IBS, however the size of the effect and the effectiveness of individual probiotics is still to be established.
Practical prescribing and product selection
Prescribing information relating to the medicines used for IBS reviewed in the section ‘Evidence base for over-the-counter medication’ is discussed and summarised in Table 6.22; useful tips relating to the treatment of patients with IBS are given in Hints and Tips Box 6.7.
All marketed products can be given to children (see individual entries) but anyone aged under 16 suspected of having IBS should be referred to a doctor as IBS in this age group is unusual.
Hyoscine butylbromide (Buscopan IBS Relief)
The recommended starting dose for adults is one tablet three times a day, although this can be increased to two tablets four a day if necessary. It is not recommended for children under the age of 12. It is a quaternary derivative of hyoscine so it does not readily cross the blood–brain barrier and therefore sedation is not normally encountered, although it might cause dry mouth and constipation. Because of its anticholinergic effects it is best avoided with other medicines that also have anticholinergic effects, for example, antihistamines, tricyclic antidepressants, neuroleptics, and disopyramide. It can be given during pregnancy and breastfeeding but avoided if possible. It should also be avoided in patients with glaucoma, myasthenia gravis and prostate enlargement.
Mebeverine (Colofac IBS)
Adults and children 10 years and over should take one tablet three times a day, preferably 20 minutes before meals. Mebeverine is not known to interact with other medicines, has no cautions in its use and can be given in pregnancy and breastfeeding although there is a lack of detailed studies. It is associated with very few side effects although allergic reactions have been reported.
Alverine (Spasmonal)
Adults and children over 12 should take one or two capsules three times a day before food. Like mebeverine, it is not known to interact with other medicines, has no cautions in its use and can be given in pregnancy and breastfeeding. It has no interactions with other medicines and can be used by all patient groups. Rash is the commonest side effect, although nausea, headache, dizziness, itching and allergic reactions have been reported.
Peppermint oil (e.g. Colpermin IBS Relief)
Adults and children aged over 15 can take peppermint oil. The dose is one capsule three times a day before food, which can be increased to two capsules three times a day in severe symptoms. It often causes heartburn and rarely allergic rashes have been reported. It is safe to use in pregnancy but can decrease breast milk production. It has no drug interactions and can be used by all patient groups.
References
Kruis, W, Weinzierl, M, Schussler, P, et al. Comparison of the therapeutic effect of wheat bran, mebeverine and placebo in patients with the irritable bowel syndrome. Digestion. 1986;34:196–201.
Liu, JP, Yang, M, Liu, Y, et al. Herbal medicines for treatment of irritable bowel syndrome. Cochrane Database of Systematic Reviews. (Issue 1):2006. [Art. No.: CD004116. DOI: 10.1002/14651858.CD004116.pub2].
Moayyedi, P, Ford, AC, Talley, NJ, et al. The efficacy of probiotics in the treatment of irritable bowel syndrome: a systematic review. BMJ. 2010;59(3):325.
Ruepert, L, Quartero, AO, de Wit, NJ, et al. Bulking agents, antispasmodics and antidepressants for the treatment of irritable bowel syndrome. Cochrane Database of Systematic Reviews. (Issue 8):2011. [Art. No.: CD003460. DOI: 10.1002/14651858.CD003460.pub3].
Agrawal, A, Whorwell, PJ. Irritable bowel syndrome: diagnosis and management. Br Med J. 2006;332:280–283.
Jamieson, DJ, Steege, JF. The prevalence of dysmenorrhea, dyspareunia, pelvic pain, and irritable bowel syndrome in primary care practices. Obstet Gynecol. 1996;87:55–58.
Poynard, T, Regimbeau, C, Benhamou, Y. Meta-analysis of smooth muscle relaxants in the treatment of irritable bowel syndrome. Aliment Pharmacol Ther. 2001;15:355–361.
Ritchie, JA, Truelove, SC. Treatment of irritable bowel syndrome with lorazepam, hyoscine butylbromide, and ispaghula husk. BMJ. 1979;1(6160):376–378.
Tudor, GJ. A general practice study to compare alverine citrate with mebeverine hydrochloride in the treatment of irritable bowel syndrome. Br J Clin Pract. 1986;40:276–278.
Webb, AN, Kukuruzovic, R, Catto-Smith, AG, et al. Hypnotherapy for treatment of irritable bowel syndrome. Cochrane Database of Systematic Reviews. (Issue 4):2007. Art. No.: CD005110. DOI: 10.1002/14651858.CD005110.pub2
Whitehead, WE, Crowell, MD, Robinson, JC, et al. Effects of stressful life events on bowel symptoms: subjects with irritable bowel syndrome compared with subjects without bowel dysfunction. Gut. 1992;33:825–830.
Irritable Bowel Syndrome Self Help and Support Group. http://www.ibsgroup.org
NICE Guidelines. Irritable bowel syndrome in adults: diagnosis and management of irritable bowel syndrome in primary care. http://guidance.nice.org.uk/CG61.
Haemorrhoids
Background
Haemorrhoids (piles) are the most common problem affecting the anorectal region. Patients might feel embarrassed talking about symptoms and it is therefore important that any requests for advice are treated sympathetically and away from others to avoid embarrassment.
Prevalence and epidemiology
The exact prevalence of haemorrhoids is unknown but it is estimated that one in two people will experience at least one episode at some point during their lives. Haemorrhoids can occur at any age but are rare in children and adults under the age of 20. It affects both sexes equally and is more common with increasing age; especially in people aged between 45 to 65 years of age. There is a high incidence of haemorrhoids in pregnant women.
Aetiology
The cause of haemorrhoids is probably multifactorial with anatomical (degeneration of elastic), physiological (increased anal canal pressure) and mechanical (straining at stool) processes implicated. Haemorrhoids have been traditionally described as engorged veins of the haemorrhoidal plexus. The analogy of varicose veins of the anal canal is often used but is misleading. Current thinking favours the theory of prolapsed anal cushions. Anal cushions maintain fine continence and are submucosal vascular structures suspended in the canal by a connective tissue framework derived from the internal anal sphincter and longitudinal muscle. Within each of the three cushions is a venous plexus that is fed by arteriovenous blood supply. Veins in these cushions fill with blood when sphincters inside them relax and empty when the sphincters contract. Fragmentation of the connective tissue supporting the cushions leads to their descent. The prolapsed anal cushion has impaired venous return resulting in venous stasis and inflammation of the cushion’s epithelium.
Haemorrhoids are classified as either internal or external. This distinction is an anatomical one. Superior to the anal sphincter there is an area known as the dentate line. At this junction epithelial cells change from squamous to columnar epithelial tissue. Above the dentate line haemorrhoids are classed as internal and below, external. Furthermore internal haemorrhoids are graded according to severity: grade I, do not prolapse out of the anal canal; grade II, prolapse on defecation but reduce spontaneously; grade III, require manual reduction; and grade IV, cannot be reduced.
Arriving at a differential diagnosis
In the first instance most patients with anorectal symptoms will self-diagnose haemorrhoids and often self-treat due to embarrassment about symptoms. Bleeding tends to cause the greatest concern and often instigates the patient to seek help. Invariably, rectal bleeding is of little consequence but should be thoroughly investigated to exclude sinister pathology. A number of haemorrhoid-specific questions should always be asked (Table 6.23).
![]() Table 6.23
Table 6.23
Specific questions to ask the patient: Haemorrhoids
| Question | Relevance |
| Duration | Patients with haemorrhoids tend to have had symptoms for some time before requesting advice. However, patients with symptoms that have been constantly present for more 3 weeks should be referred |
| Pain | Pain associated with haemorrhoids tends to occur on defecation. It can occur at other times, for example when sitting. Pain is usually described as a dull ache Sharp or stabbing pain at the time of defecation can suggest an anal fissure or tear |
| Rectal Bleeding | Slight rectal bleeding is often associated with haemorrhoids. Blood appears bright red and might be visible in the toilet bowl or on the surface of the stool. The presence of blood is usually a direct referral sign but if the cause is haemorrhoids this could be treated unless the patient is unduly anxious in which case referral is appropriate Blood mixed in the stool has to be referred to eliminate a GI bleed Large volumes of blood or blood loss not associated with defecation must be referred to eliminate possible carcinoma |
| Associated symptoms | Symptoms associated with haemorrhoids are usually localised, for example anal itching. Other symptoms such as nausea, vomiting, loss of appetite and altered bowel habit should be viewed with caution and underlying pathology suspected. Referral would be needed |
| Diet | A lack of dietary fibre that leads to constipation is a contributory factor to haemorrhoids. The passage of hard stools and straining during defecation can cause haemorrhoids. Find out about the patient’s diet and current bowel habits |
Clinical features of haemorrhoids
Symptoms experienced by the patient are dependent upon the severity or type of haemorrhoid and can include bleeding, perianal itching, mucus discharge and pain. Often patients are asymptomatic until the haemorrhoid prolapses. Any blood associated is bright red and is most commonly seen as spotting around the toilet pan, streaking on toilet tissue or visible on the surface of the stool. Symptoms are often intermittent and each episode usually lasts from a few days to a few weeks.
Internal haemorrhoids are rarely painful, whereas external haemorrhoids often cause pain due to the cushion becoming thrombosed. Pain is described as a dull ache that increases in severity when the patient defecates leading to patients ignoring the urge to defecate. This can then lead to constipation, which in turn will lead to more difficulty in passing stools and further increase the pain associated with defecation.
Conditions to eliminate
Localised anal itching can result from dermatitis (or even threadworm infection). If pruritus is the major presenting symptom then the most likely cause is contact dermatitis often caused by toiletries.
Medication
As constipation is a contributory factor in the manifestation of haemorrhoids, those medicines that are prone to causing constipation should, if possible, be avoided. Table 6.19 lists those medicines that are commonly known to cause constipation.
Conditions causing rectal bleeding
A number of conditions can present with varying degrees of rectal bleeding. However, other symptoms should be present which will allow them to be excluded.
Anal fissure
Anal fissures are common, with the 20–30-year-old age group most affected. Symptoms often follow a period of constipation and are normally caused by straining at stool. Pain can be intense on defecation and can last between a few minutes and a few hours after defecation. Bright red blood is commonly seen. Non-urgent referral is necessary for confirmation of the diagnosis. In the meantime the patient should be instructed to eat more fibre and increase their fluid intake.
Ulcerative colitis and Crohn’s disease
Other symptoms besides blood in the stool are usually present with ulcerative colitis and Crohn’s disease. These tend to be stools that are watery, abdominal pain in the lower left quadrant, weight loss and fever. Patients will appear unwell and also find that they have urgency, nocturnal diarrhoea and early morning rushes. In the acute phase patients will have malaise.
Upper GI bleeds
Erosion of the stomach wall or upper intestine is normally responsible for GI bleeds and is often associated with NSAID intake. The colour of the stool is related to the rate of bleeding. Stools from GI bleeds can be tarry (indicating a bleed of 100 to 200 mL of blood) or black (indicating a bleed of 400 to 500 mL of blood). Urgent referral is needed.
Colorectal cancer
Rectal carcinoma is most common in the 50–70-year-old age group and is characterised by rectal bleeding, a change in bowel habit and tenesmus. Rectal bleeding tends to be persistent and steady though slight for all tumours. Colorectal bleeds depend on the site of tumour, for example sigmoid tumours lead to bright red blood in or around the stool. Any patient over 40 years of age with persistent rectal bleeding and a change of bowel habit must be urgently referred. If over 60 years then persistent rectal bleeding alone is sufficient to refer. NICE have produced referral guidelines for doctors for suspected cases of colorectal cancer (http://www.nice.org.uk/guidance/CG27, accessed 8 November 2012).
Figure 6.14 will aid the differentiation of haemorrhoids.
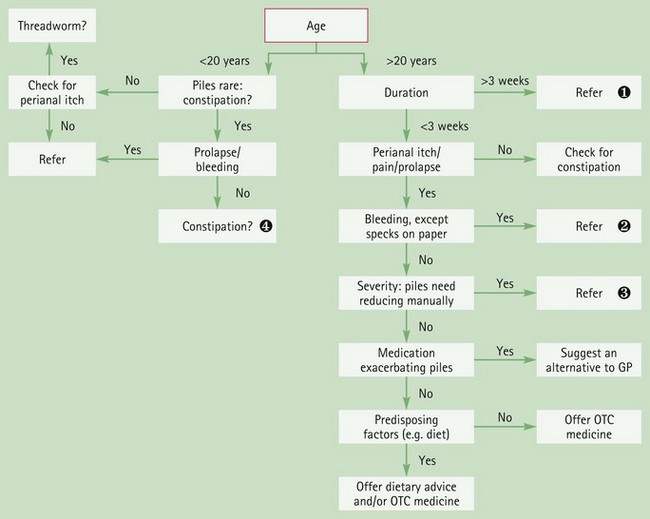
Fig. 6.14 Primer for differential diagnosis of haemorrhoids.![]() Duration
Duration
Patients with long-standing symptoms that have not been seen previously by the GP should be referred to eliminate any underlying pathology. In the vast majority of cases no sinister findings will result.![]() Rectal bleeding
Rectal bleeding
In the majority of cases rectal bleeding is a sign of referral.
However, in cases where sinister pathology has been excluded and only mild local bleeding has occurred the pharmacist could instigate treatment.![]() Severity
Severity
Medication is unlikely to help any patient who has to manually reduce haemorrhoids. Referral for other treatments is recommended.![]() Constipation
Constipation
See Fig. 6.12.
Evidence base for over-the-counter medication
Reviews by Alonso-Coelle et al (2005, 2006a, b) have concluded that general measures to prevent constipation will help to decrease straining during defecation, ease the symptoms of haemorrhoids and reduce recurrence. Patients should therefore be asked about their normal diet to determine fibre intake. Those with diets low in fibre should be encouraged to increase their fibre and fluid intake; this will help produce softer stools and reduce constipation. Patients should try to eat more fruit, vegetables, bran, and wholemeal bread. If this is not possible then fibre supplementation with a bulk-forming laxative could be recommended. Bulk-forming laxatives will take 2–3 days to relieve constipation and may take up to 6 weeks to improve symptoms of haemorrhoids.
Pharmacological Intervention
Numerous products are marketed for the relief and treatment of haemorrhoids. These include a wide range of therapeutic agents and commonly include anaesthetics, astringents, anti-inflammatories and protectorants. Most products contain a combination of these agents.
The inclusion of such a diverse range of chemical entities appears to be based largely on theoretical grounds rather than any evidence base. Extensive literature searching found only one published trial regarding the efficacy of any marketed product (Ledward 1980); however, this trial suffered from serious methodological flaws.
Anaesthetics (lidocaine, benzocaine and cinchocaine)
No trials appear to have been conducted using local anaesthetics in the treatment and relief of symptoms for haemorrhoids. However, anaesthetics have proven efficacy when used on other mucosal surfaces; their use could therefore be justifiably recommended. Their action is short lived and will produce temporary relief from perianal itching and pain. They require frequent application and might therefore cause skin sensitisation.
Astringents (allantoin, bismuth, zinc, Peru balsam)
Astringents are included in haemorrhoid preparations on the theoretical basis that they precipitate surface proteins thus producing a protective coat over the haemorrhoid. There appears to be no evidence to support this theory. Certain proprietary products only contain astringents and at best will provide a placebo effect.
Anti-inflammatories (hydrocortisone)
Steroids have proven effectiveness in reducing inflammation and would therefore be useful in reducing haemorrhoidal swelling, however trials with OTC products containing hydrocortisone appear not to have taken place.
Protectorants (e.g. shark liver oil)
Protectorants are claimed to provide a protective coating over the skin and thus produce temporary relief from pain and perianal itch. These claims cannot be substantiated and as with astringents any benefit conveyed by a protectorant is probably a placebo effect. In addition, there is also an ethical dimension to using a product with no efficacy sourced from sharks.
Other agents
Sclerosing agents (lauromacrogol), and wound-healing agents (yeast cell extract) can also be found in some products. There is no evidence supporting their effectiveness.
Flavonoids
Dietary supplementation with flavonoids is a common alternative treatment that is popular in continental Europe and the Far East. As an adjunct, their use has been shown to reduce acute symptoms and secondary haemorrhage after haemorrhoidectomy.
Summary
With so little data available on their effectiveness it is impossible to say whether any product is a credible treatment for haemorrhoids, and many medical authorities regard them as little more than placebos. A Cochrane review is underway to assess the efficacy of topical products and may give a more definitive answer (Kopljar et al 2011). Until such time, it seems prudent to recommend products containing a local anaesthetic or hydrocortisone as they do have proven effectiveness in other similar conditions.
Treatment should only be recommended to patients with mild haemorrhoids. Any person complaining of prolapsing haemorrhoids, which need reducing by the patient should be referred, because these patients might require non-surgical intervention with sclerotherapy or rubber band ligation. If these fail to cure the problem then a haemorrhoidectomy might be performed.
Practical prescribing and product selection
Prescribing information relating to the medicines used for haemorrhoids reviewed in the section ‘Evidence base for over-the-counter medication’ is discussed and summarised in Table 6.24.
![]() Table 6.24
Table 6.24
Practical prescribing: Summary of haemorrhoid products
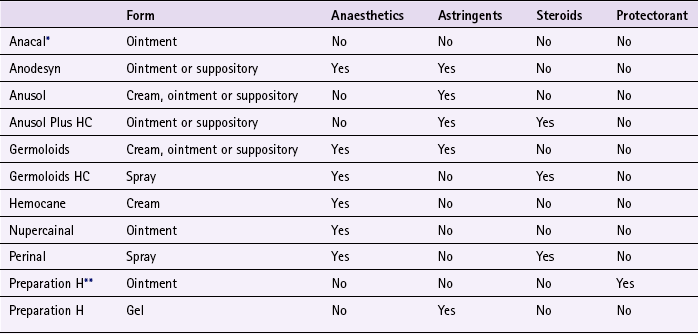
*contains a sclerosing agent.
**contains yeast cell extract.
The product licenses of products for haemorrhoids allow all patient groups, except children under 12, to use them. (Note-good practice dictates that people under 20 years old with suspected haemorrhoids should be referred.) They do not interact with any other medicines and can be used in pregnancy and breastfeeding. The standard dose for any formulation is twice daily, plus application after each bowel movement. Minimal side effects have been reported and are usually limited to slight irritation. Products that contain hydrocortisone are subject to several licensing restrictions: they are restricted to use in patients over a certain age (Perinal spray 14 years, Germoloids spray 16 years and Anusol Plus products 18 years); no longer than a week’s duration and not for use in pregnant or lactating women.
References
Alonso-Coello, P, Guyatt, GH, Heels-Ansdell, D, et al. Laxatives for the treatment of hemorrhoids. Cochrane Database of Systematic Reviews. (Issue 4):2005. [Art. No.: CD004649. DOI: 10.1002/14651858.CD004649.pub2].
Alonso-Coello, P, Mills, E, Heels-Ansdell, D, et al. Fiber for the treatment of hemorrhoids complications: a systematic review and meta-analysis. Am J Gastroenterol. 2006;101:181–188.
Alonso-Coello, P, Zhou, Q, Martinez-Zapeta, MJ, et al. Meta-analysis of flavonoids for the treatment of haemorrhoids. Br J Surg. 2006;93(8):909–920.
Ledward, RS. The management of puerperal haemorrhoids: A double blind clinical trial of Anacal rectal ointment. The Practitioner. 1980;224:660–661.
Kopljar, M, Balduzzi, S, Patrlj, L, et al. Topical treatment for hemorrhoids. Cochrane Database of Systematic Reviews. (Issue 11):2011. [Art. No.: CD009443. DOI: 10.1002/14651858.CD009443. (Protocol)].
Abdominal pain
Background
Abdominal pain is a symptom of many different conditions, ranging from acute self-limiting problems to life threatening conditions such as ruptured appendicitis and bowel obstruction. However, the overwhelming majority of cases will be of a non-serious nature, self-limiting and not require medical referral. The most common conditions that present to community pharmacies are dyspepsia affecting the upper abdomen and IBS affecting the lower abdomen. These are covered in more detail on pages 146 and 168. However, other conditions will present with abdominal pain (Fig. 6.15 and Table 6.25) and these are covered in this chapter.
Prevalence and epidemiology
The prevalence and epidemiology of abdominal pain within the population is determined by those conditions that cause it. As so many conditions can give rise to abdominal pain it is likely that the majority of the population will, at some point, suffer from abdominal pain. For example, one study found that 40% of the UK population had suffered from dyspepsia during the previous 12 months and gastroenteritis, which is commonly associated with abdominal pain, is extremely common.
Aetiology
Abdominal pain does not only arise from the GI tract but also from the cardiovascular and musculoskeletal system. Therefore the aetiology of abdominal pain is dependent on its cause. GI tract causes include poor muscle tone leading to reflux (e.g. lower oesophageal sphincter incompetence), infections that cause peptic ulcers (from H. pylori) and mechanical blockages causing renal and biliary colic. Cardiovascular causes include angina and myocardial infarction whereas musculoskeletal problems often involve tearing of abdominal muscles.
Arriving at a differential diagnosis
The main role of the community pharmacist is to identify patients in whom symptoms suggest more serious pathology, so that they can be further evaluated. This is not easy, as many abdominal conditions do not present with classical textbook symptoms and patients tend to present to the pharmacist early in the course of the disease, often before the presenting symptoms have assumed the more usual description. The low prevalence of serious disease and overlapping symptoms with minor illness makes the task even more difficult. Single symptoms are poor predictors of final diagnosis (except for reflux oesophagitis, in which the presence of heartburn is highly suggestive). It is therefore important to look for ‘symptom clusters’ and to use knowledge of the incidence and prevalence of conditions to determine if referral is needed. This necessitates taking a very careful history and not relying on a single symptom to label a patient with a particular problem. Specific questions relating to abdominal pain should be asked (Table 6.26).
![]() Table 6.26
Table 6.26
Specific questions to ask the patient: Abdominal pain
| Question | Relevance |
| Location of pain | Knowing the anatomical location of abdominal structures is helpful in differential diagnosis of abdominal pain (Fig. 6.13) |
| Presence only of abdominal pain/discomfort | In general, patients without other symptoms rarely have serious pathology. The symptoms are usually self-limiting and often no cause can be determined |
| Nature of the pain | Heartburn is classically associated with a retrosternal burning sensation Cramp-like pain is seen in diverticulitis, IBS, salpingitis and gastroenteritis Colicky pain (pain that comes and goes) has been used to describe the pain of appendicitis, biliary and renal colic and intestinal obstruction Gnawing pain is associated with pancreatitis and pancreatic cancer and boring pain with ulceration |
| Radiating pain | Abdominal pain that moves from its original site should be viewed with caution Pain that radiates to the jaw, face and arm could be cardiovascular in origin Pain that moves from a central location to the right lower quadrant could suggest appendicitis Pain radiating to the back may suggest peptic ulcer or pancreatitis |
| Severity of pain | Non-serious causes of abdominal pain generally do not give rise to severe pain. Pain associated with pancreatitis, biliary and renal colic and peritonitis tends to be severe (subjective scores higher than 6 out of 10) |
| Age of patient | With increasing age, abdominal pain is more likely to have an identifiable and serious organic cause. Appendicitis is the only serious abdominal condition that is much more common in young patients |
| Onset & duration | In general, if no identifiable cause can be found, abdominal pain with sudden onset is generally a symptom of more serious conditions. For example, peritonitis, appendicitis, ectopic pregnancy, renal and biliary colic. Pain that lasts more than 6 hours is suggestive of underlying pathology |
| Aggravating or ameliorating factors | Biliary colic can be aggravated by fatty foods Vomiting tends to relieve pain in gastric ulcers Pain in duodenal ulcer is relieved after ingestion of food Pain in salpingitis, pancreatitis and appendicitis are often made worse by movement |
| Associated symptoms | Vomiting, weight loss, melaena, altered bowel habit and haematemesis are all symptoms that suggest more serious pathology and require referral |
Conditions affecting the upper abdomen
Dyspepsia/gastritis: Patients with dyspepsia present with a range of symptoms that commonly involve vague abdominal discomfort (aching) above the umbilicus (Fig. 6.16) associated with belching, bloating, flatulence, feeling of fullness and heartburn. It is normally relieved by antacids and aggravated by spicy foods or excessive caffeine. Vomiting is unusual. For further information on dyspepsia see page 146.
Splenic enlargement or rupture: If the spleen is enlarged, generalised left upper quadrant pain associated with abdominal fullness and early feeding satiety is observed (Fig. 6.17). Referred pain to the left shoulder is sometimes seen. The condition is rare and is nearly always secondary to another primary cause, which might be an infection, a result of inflammation or haematological in origin.
Right upper quadrant pain
Acute cholecystitis and cholelithiasis: Acute cholecystitis (inflammation of the gall bladder) and cholelithiasis (presence of gall stones in the bile ducts, also called biliary colic) are characterised by persistent, steady severe pain (Fig. 6.18). Pain can vary from sharp, cramping or dull in nature. Classically, the onset is sudden and starts a few hours after a meal and frequently waking the patient in the early hours of the morning. The pain can also be felt in the epigastric area and radiate to the tip of the right scapula in cholelithiasis. Fatty foods often aggravate the pain. The incidence increases with increasing age and is most common in people aged over 50. It is also more prevalent in women than men.
Hepatitis: Liver enlargement from any type of hepatitis will cause discomfort or dull pain around the right rib cage (Fig. 6.19). Associated early symptoms are general malaise, tiredness, skin rash and nausea. The most common causes of acute hepatitis are alcohol abuse and viral infection.
Ulcers: Ulcers are classed as either gastric or duodenal. They occur most commonly in patients aged 30 to 50 years old and are more common in men than women. Symptoms are variable but typically the patient will have localised mid epigastric pain (Fig. 6.20) described as ‘constant’, ‘annoying’ or ‘gnawing/boring’.
With gastric ulcers, symptoms are inconsistent but the pain usually comes on whenever the stomach is empty – usually 15 to 30 minutes after eating – and is generally relieved by antacids or food and aggravated by alcohol and caffeine. NSAID use is associated with a three- to fourfold increase in gastric ulcers.
Duodenal ulcers tend to be more consistent in symptom presentation. Pain occurs 2 to 3 hours after eating and pain that wakes a person at night is highly suggestive of duodenal ulcer.
Pain affecting both right and left upper quadrants
Acute pancreatitis: Pain of pancreatitis develops suddenly and is described as agonising with the pain being centrally located that often radiates into the back (Fig. 6.21). Pain reaches its maximum intensity within minutes and can last hours or days. Vomiting is common but does not relieve the pain. Early in attack patients might get relief from the pain by sitting forwards. It is commonly seen in alcoholics and it is likely that the patient will have a history of long-term heavy drinking. Patients are very unlikely to present in a community pharmacy due to the severity of the pain but a mild attack could present with steady epigastric pain sometimes centred close to the umbilicus and can be difficult to distinguish between other causes of upper quadrant pain.
Renal colic: Urinary calculi (stones) can occur anywhere in the urinary tract, although most frequently stones get lodged in the ureter. Pain begins in the loin, radiating round the flank into the groin and sometimes down the inner side of the thigh (Fig. 6.22). Pain is severe and colicky in nature. Attacks are spasmodic and tend to last minutes to hours and often leave the person prostrate with pain. Symptoms of nausea and vomiting might also be present. It is more common in men and usually occurs between the ages of 30 and 50 years old.
Myocardial ischaemia: Angina and myocardial infarction (MI) cause chest pain that can be difficult to distinguish initially from epigastric/retrosternal pain caused by dyspepsia (Fig. 6.23). However, pain of cardiovascular origin often radiates to the neck, jaw and inner aspect of the left arm. Typically, angina pain is precipitated by exertion and subsides after a few minutes once at rest. Pain associated with MI will present with characteristic deep crushing pain. The patient will appear pale, display weakness and be tachycardic. Cardiovascular pain should respond to sublingual glyceryl trinitrate therapy.
Herpes zoster (shingles): Pain associated with herpes zoster typically occurs once the rash has erupted, although it can precede the rash by several days. Pain that precedes the rash and is right sided can be confused with appendicitis (Fig. 6.24).
Conditions affecting the lower abdomen
The most common causes of lower abdominal pain are muscle strains, IBS, appendicitis, and salpingitis in women. Apart from appendicitis, all these conditions can present in either quadrant.
Irritable bowel syndrome: Pain is most often observed in the left lower quadrant (Fig. 6.25); however, the discomfort can be vague and diffuse and about one-third of patients exhibit upper abdominal pain. The pain is described as ‘cramp-like’ and is recurrent. Alternating diarrhoea and constipation and mucus coating the stools is also often present. For further information on IBS see page 168.
Diverticulitis: The incidence of diverticulitis increases with increasing age. It is most prevalent in the elderly and is characterised by constant pain and local tenderness. Pain is more commonly seen in the left lower quadrant (Fig. 6.26) but can be suprapubic and occasionally right lower quadrant. Pain tends to be cramp-like in nature. Fever is a prominent feature and altered bowel habit is usual with diarrhoea more common than constipation.
Intestinal obstruction: Intestinal obstruction is most prevalent in people over the age of 50. It has sudden and acute onset. The pain is described as colicky and can be experienced anywhere in the lower abdomen. Constipation and vomiting are prominent features.
Appendicitis: Classically, the pain starts in the mid-abdomen region, around the umbilicus, before migrating to the right lower quadrant after a few hours (Fig 6.27), although right-sided pain is experienced from the outset in about 50% of patients. The pain of appendicitis is described as colicky or cramp-like but after a few hours becomes constant. Movement tends to aggravate the pain and vomiting might also be present. Appendicitis is most common in young adults, especially young men.
Conditions affecting women
Generalised lower abdominal pain (Fig. 6.28) can be experienced in a number of gynaecological conditions:
• Ectopic pregnancy: these are usually experienced between weeks 5 and 14 of the pregnancy. Patients suffer from persistent moderate to severe pain that is sudden in onset. Referred pain to the tip of the scapula is possible. Most patients (80%) experience bleeding ranging from spotting to the equivalent of a menstrual period. Diarrhoea and vomiting is often also present.
• Salpingitis (inflammation of the fallopian tubes): occurs predominantly in young, sexually active women, especially those fitted with an IUD. Pain is usually bilateral, low and cramping. Pain starts shortly after menstruation and can worsen with movement. Malaise and fever are common.
• Endometriosis: patients experience lower abdominal aching pain that usually starts 5 to 7 days before menstruation begins and can be constant and severe. The pain often worsens at the onset of menstruation. Referred pain into the back and down the thighs is also possible.
Diffuse abdominal pain
A number of conditions will present with diffuse abdominal pain over the four quadrants. The most common cause of diffuse pain seen by the pharmacist is gastroenteritis. Other causes include peritonitis and pancreatitis.
Gastroenteritis: Other symptoms of nausea, vomiting and diarrhoea will be more prominent in gastroenteritis than abdominal pain. The patient might also have a fever and suffer from general malaise.
Peritonitis: Although the pain of acute peritonitis can be diffuse, severe pain in the upper abdomen is often present. This is accompanied by intense rigidity of the abdominal wall producing a ‘board like’ appearance; fever and vomiting might also be present. Urgent referral is required due to associated complications.
Figure 6.29 will aid in the differentiation of the different types of abdominal pain.
Evidence base for over-the-counter medication and practical prescribing and product selection
The two conditions that have abdominal pain/discomfort as one of the major presenting symptoms and can be treated OTC are dyspepsia and IBS. For further information on products used to treat these conditions, please refer to pages 151 and 171.
Bagshaw, EJ. Abdominal pain protocol: right upper quadrant pain. Lippincotts Prim Care Pract. 1999;3:486–492.
Guthrie, E, Thompson, D. Abdominal pain and functional gastrointestinal disorders. Br Med J. 2002;325:701–703.
Kalloo, AN, Kantsevoy, SV. Gallstones and biliary disease. Prim Care. 2001;28:591–606.
Lucenti, MJ, Nadel, ES, Brown, DF. Right lower quadrant pain. J Emerg Med. 2001;21:431–434.
Miiller, SK, Alpert, PT. Assessment and differential diagnosis of abdominal pain. Nurse Pract. 2006 Jul;31(7):38–45. 47
The following questions are intended to supplement the text. Two levels of questions are provided; multiple choice questions and case studies. The multiple choice questions are designed to test factual recall and the case studies allow knowledge to be applied to a practice setting.
Multiple choice questions
6.1. Which one of the following symptoms is most indicative of renal colic
a. Loin pain radiating to the groin
b. Left lower quadrant pain radiating to loin area
c. Right lower quadrant pain radiating to loin area
6.2. In the treatment of constipation which one of the following statements is true?
a. Bulk-forming laxatives usually act within 12 to 24 hours
b. Senna tablets should be avoided in nursing mothers
c. Fybogel is not suitable for a patient with coeliac disease
d. Lactulose should not be taken by diabetics
e. Liquid paraffin has been linked with causing lipid pneumonia
6.3. A man asks for the best thing to stop diarrhoea as he is going on holiday and he doesn’t want to be caught short. Which of the following is the first-line treatment to be recommended?
6.4. Antacids that contain aluminium, calcium or magnesium salts inhibit the intestinal absorption of which of the following?
6.5. What condition predisposes patients to oral thrush?
6.6. Abdominal pain that starts centrally then moves to the right lower quadrant is indicative of?
6.7. Which condition is least likely to cause rectal bleeding?
6.8. Mrs Jones, a 44-year-old woman, asks for advice on a sore spot on the inside of her cheek. Based solely on the sex of the patient and age, what is the most likely diagnosis?
Questions 6.9 to 6.11 concern the following conditions:
Select, from A to E, which statement best relates to the conditions above:
Questions 6.12 to 6.14 concern the following OTC medications:
6.12. Is most suitable for treating heartburn, which tends to get worse when lying down
6.13. Is most suitable to treat abdominal discomfort caused by trapped gas
6.14. Could be used to relieve constipation, as well as indigestion
Questions 6.15 to 6.17: for each of these questions one or more of the responses is (are) correct. Decide which of the responses is (are) correct. Then choose:
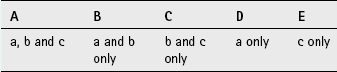
6.15. When questioning a patient seeking advice for nausea and gastrointestinal upset, which of the following symptoms would indicate the need for direct referral to the general practitioner?
6.16. A common presentation of minor aphthous ulcers is
6.17. Which symptoms in a patient presenting with constipation should be referred?
Questions 6.18 to 6.20: these questions consist of a statement in the left-hand column followed by a statement in the right-hand column. You need to:
A If both statements are true and the second statement is a correct explanation of the first statement
B If both statements are true but the second statement is NOT a correct explanation of the first statement
C If the first statement is true but the second statement is false
D If the first statement is false but the second statement is true
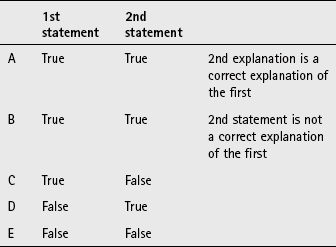
| First statement | Second statement |
| 6.18 IBS is common in people under the age of 40 | It can be caused by stress |
| 6.19 Gingivitis is caused by plaque build up | It is characterised by swollen and red gums |
| 6.20 Heartburn causes retrosternal pain | Sphincter incompetence is responsible for symptoms |