Spine
When you suffer an attack of nerves you’re being attacked by the nervous system. What chance has a man got against a system?
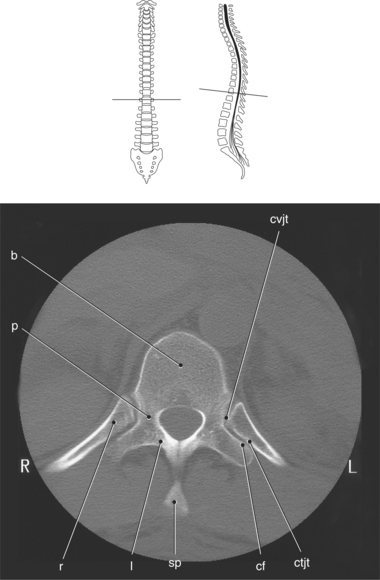
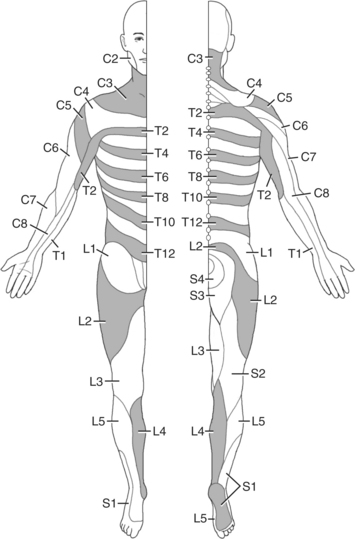
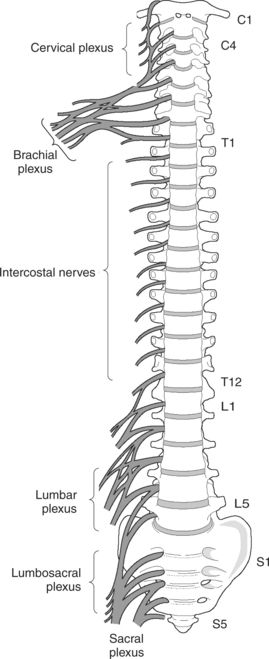
The spine functions to protect the delicate sensory and motor nerves that allow for peripheral sensations and body movement. Sensory or neurologic loss can be a result of injury or pathologic abnormalities of any of the many areas that compose the normal anatomy of this region (Figure 4.1).
VERTEBRAL COLUMN
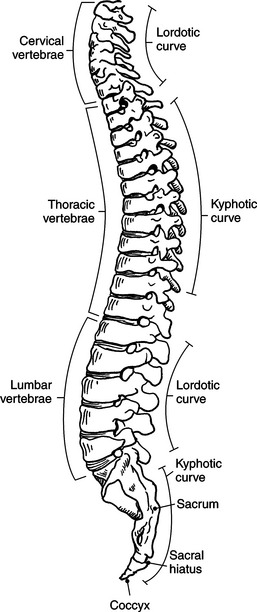
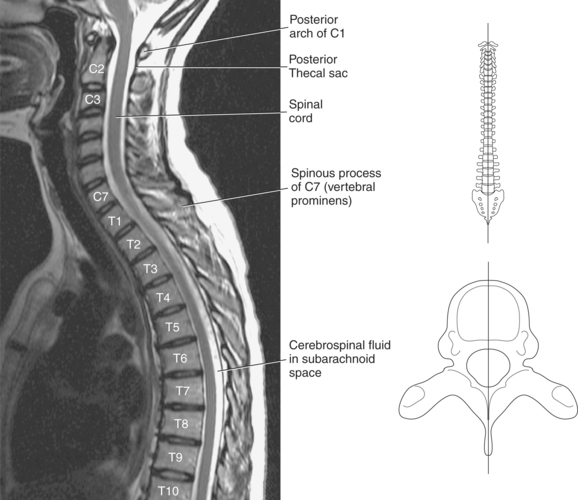
The vertebral column is a remarkable structure that supports the weight of the body, helps to maintain posture, and protects the delicate spinal cord and nerves. It is made up of 33 vertebrae, which can be separated into cervical, thoracic, lumbar, sacral, and coccygeal sections. Curvatures associated with the vertebral column provide spinal flexibility and distribute compressive forces over the spine. The cervical and lumbar sections convex forward, creating lordotic curves, and the thoracic and sacral sections convex backward, creating kyphotic curves (Figure 4.2).
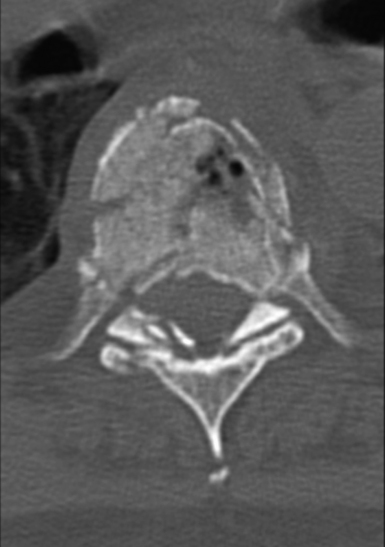
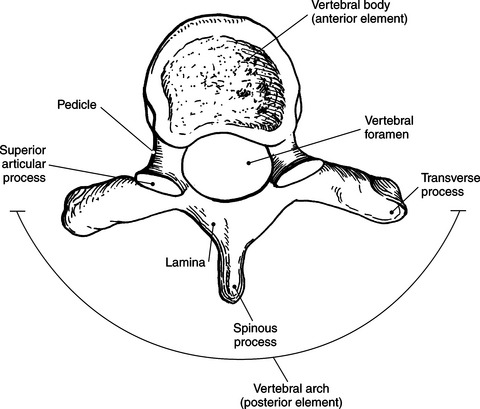
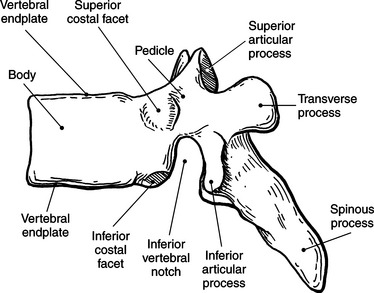
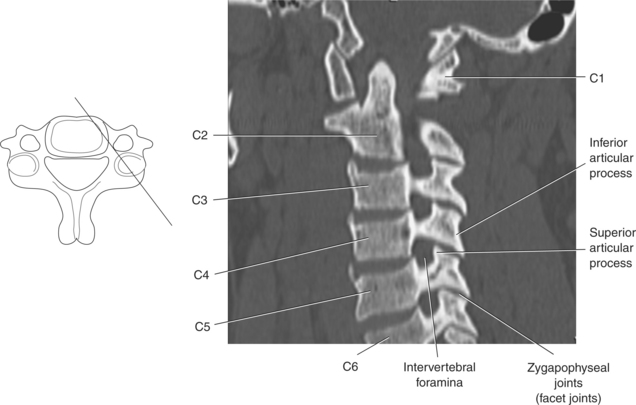
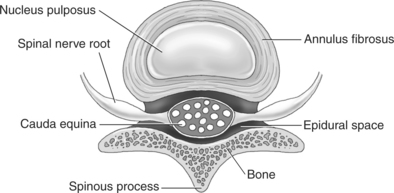
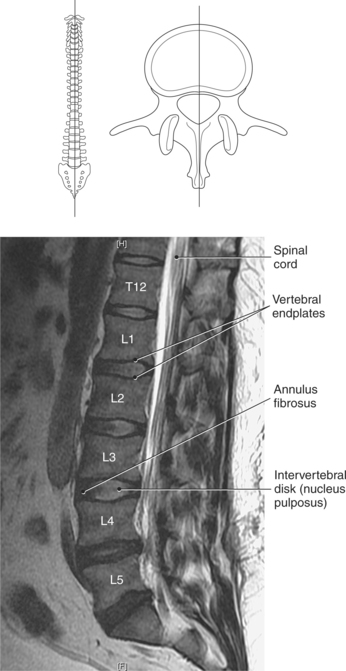
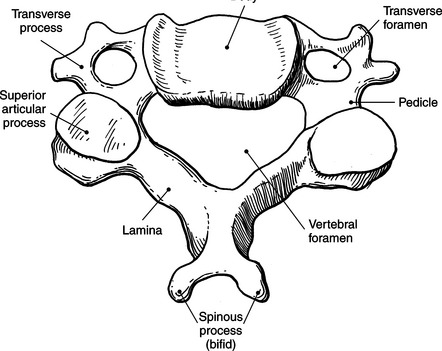
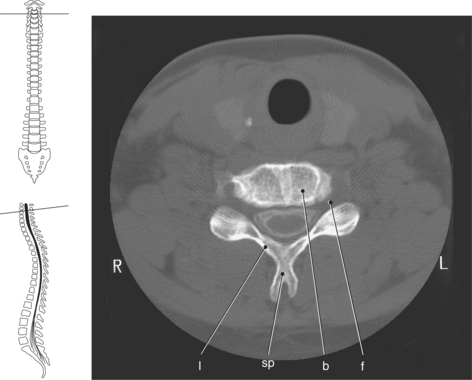
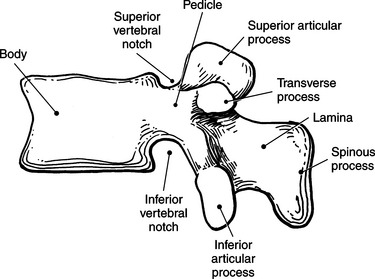
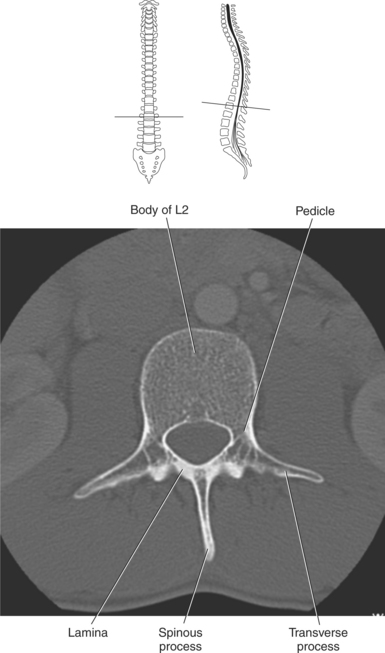
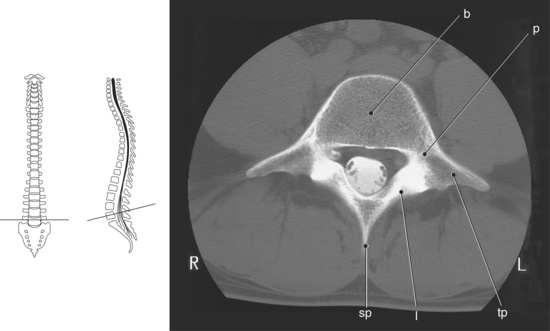
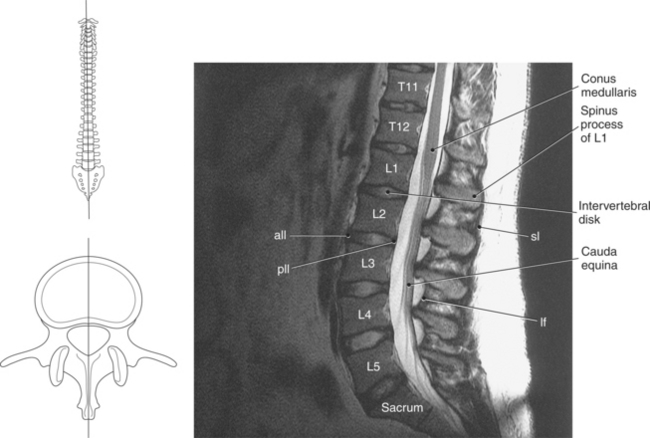
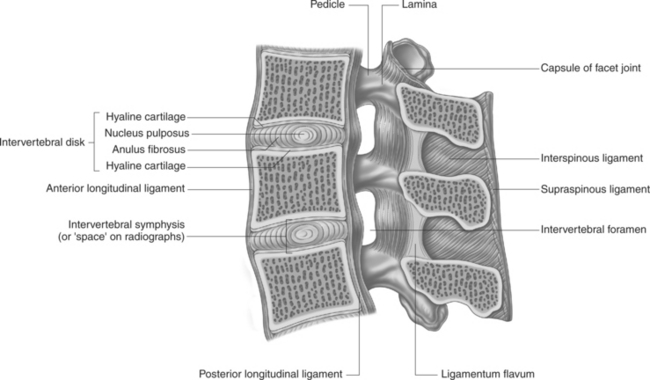
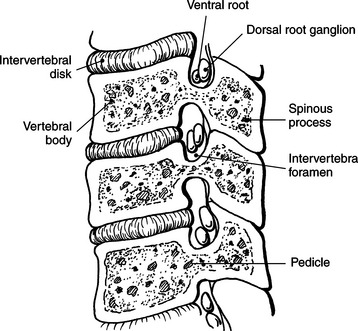
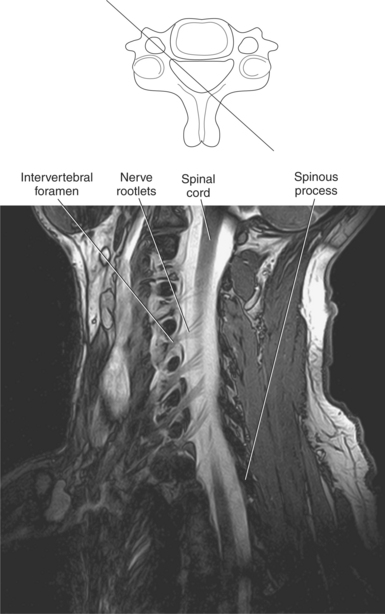
Vertebrae vary in size and shape from section to section, but a typical vertebra consists of two main parts: the body (anterior element) and the vertebral arch (posterior element). The cylindric body is located anteriorly and functions to support body weight (Figures 4.3 and 4.4). The size of the vertebral bodies progressively increases from the superior portion of the vertebral column to the inferior portion of the spine. The compact bone on the superior and inferior surfaces of the body is called the vertebral end plates. Located posteriorly is the ringlike arch that attaches to the sides of the body, creating a space called the vertebral foramen. The succession of the vertebral foramina forms the vertebral canal, which contains and protects the spinal cord. The vertebral arch is formed by pedicles (2), laminae (2), spinous process (1), transverse processes (2), and superior (2) and inferior (2) articular processes (Figures 4.3 through 4.5). The two pedicles project from the body to meet with two laminae that continue posteriorly and medially to form a spinous process. The transverse processes project laterally from the approximate junction of the pedicle and lamina (Figures 4.3 and 4.4). On the upper and lower surfaces of the pedicles is a concave surface termed the vertebral notch (Figure 4.5). When the superior and inferior notches of adjacent vertebrae meet, they form intervertebral foramina, which allow for the transmission of spinal nerves and blood vessels (Figure 4.6). Four articular processes, two superior and two inferior, arise from the junctions of the pedicles and laminae to articulate with adjacent vertebrae to form the zygapophyseal joints (facet joints). These joints give additional support and allow movement of the vertebral column (Figures 4.7 through 4.10). The vertebral bodies are separated by shock-absorbing cartilaginous intervertebral disks. These disks consist of a central mass of soft semi-gelatinous material called the nucleus pulposus and a firm outer portion termed the annulus fibrosus (Figures 4.9 through 4.12).
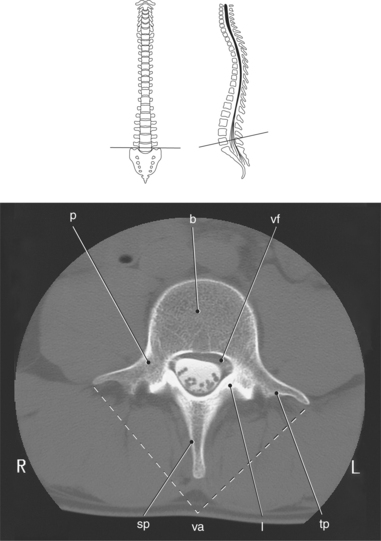
Figure 4.4 Axial CT scan of lumbar vertebra.
Key: p, Pedicle; b, body; vf, vertebral foramen or canal; sp, spinous process; va, vertebral arch; l, lamina; tp, transverse process.
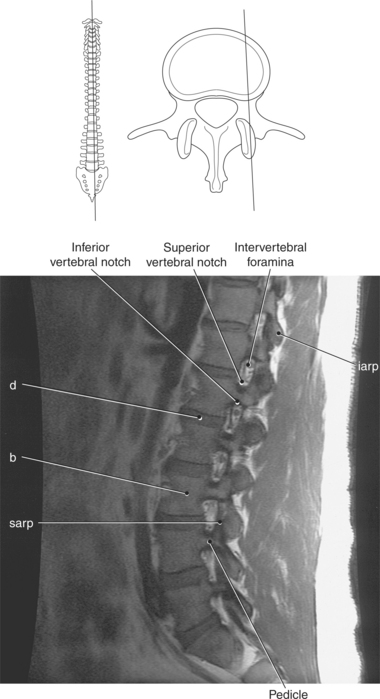
Figure 4.6 Sagittal, T1-weighted MR scan of lumbar vertebrae.
Key: iarp, Inferior articular process; d, disk; b, body; sarp, superior articular process.
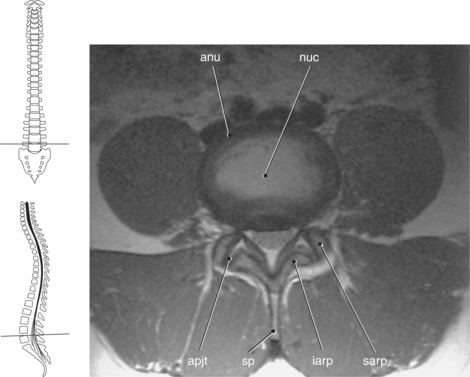
Figure 4.9 Axial, T1-weighted MR scan of lumbar spine with intervertebral disk and zygapophyseal joint.
Key: anu, Annulus fibrosus; nuc, nucleus pulposus; apjt, apophyseal joint; sp, spinous process; iarp, inferior articular process; sarp, superior articular process.
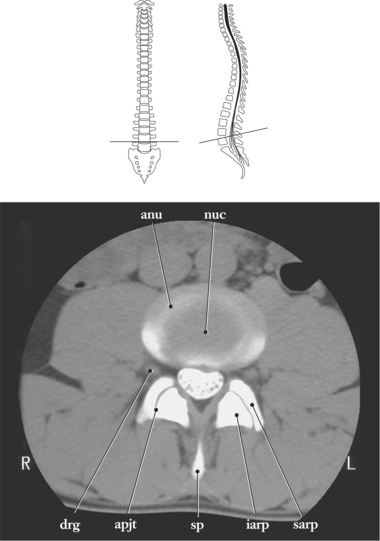
Figure 4.10 Axial CT scan of lumbar spine with intervertebral disk and zygapophyseal joint.
Key: anu, Annulus fibrosus; nuc, nucleus pulposus; drg, dorsal root ganglion; apjt, apophyseal joint; sp, spinous process; iarp, inferior articular process; sarp, superior articular process.
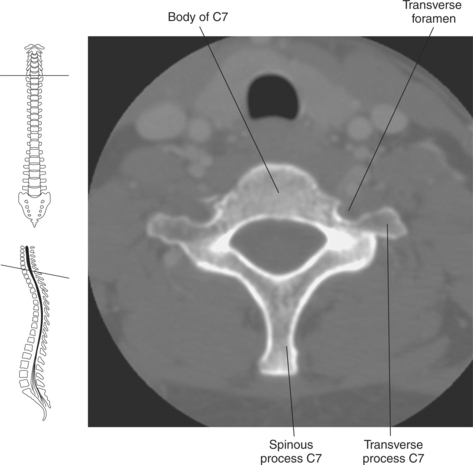
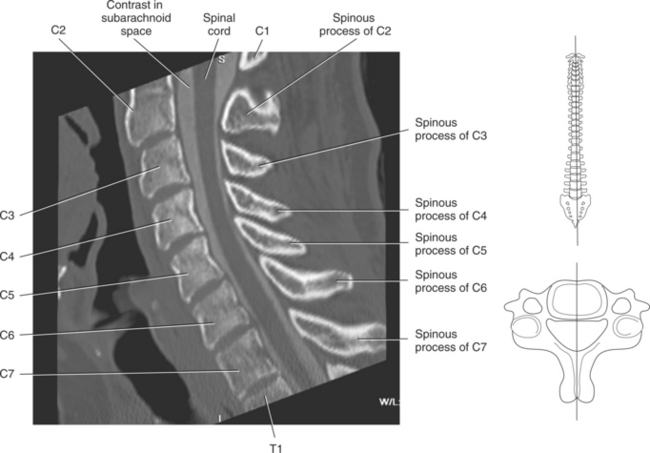
Cervical Vertebrae
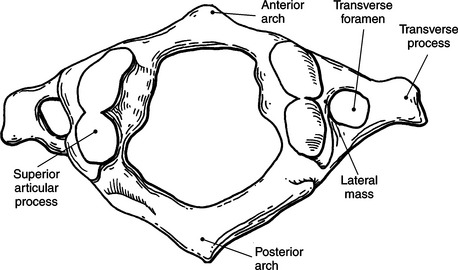
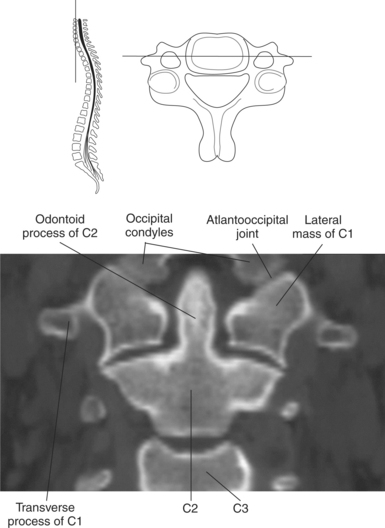
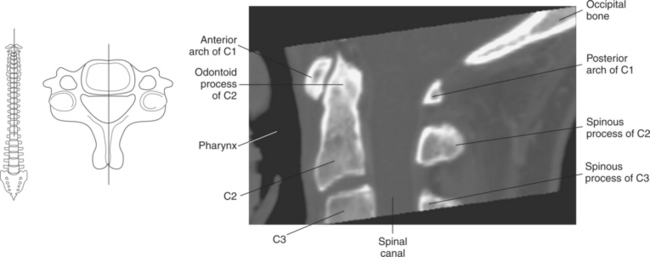
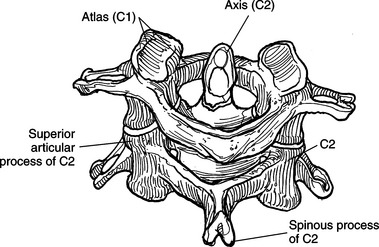
There are seven cervical vertebrae that vary in size and shape to a large degree. Within the transverse process of each cer-vical vertebra is a transverse foramen. These foramina allow passage of the vertebral vessels as they ascend to and descend from the head. The first cervical vertebra is termed the atlas because it supports the head; its large superior articular processes articulate with the occipital condyles of the head to form the atlantooccipital joint. The atlas is a ringlike struc-ture that has no body and no spinous process. It consists of an anterior arch, posterior arch, and two large lateral masses (Figures 4.13 through 4.15). The lateral masses provide the only weight-bearing articulation between the cranium and vertebral column.
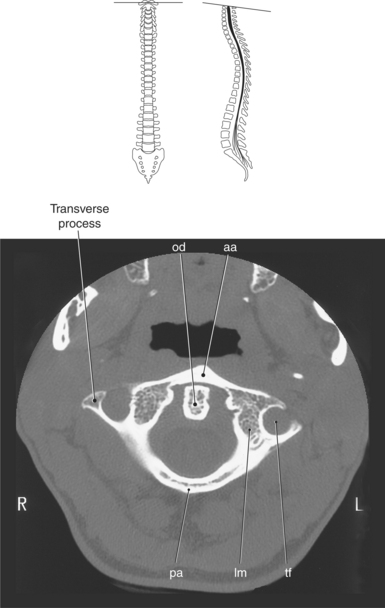
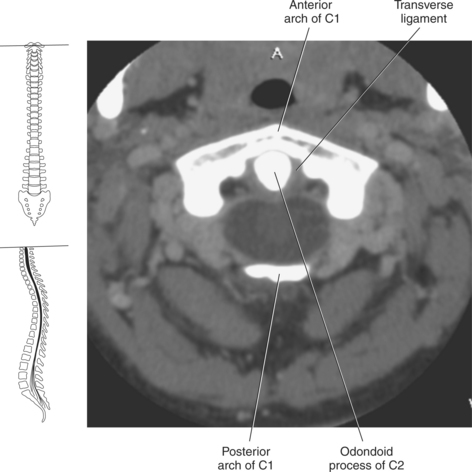
Figure 4.14 Axial CT scan of C1 (atlas).
Key: od, Odontoid process; aa, anterior arch; pa, posterior arch; lm, lateral mass; tf, transverse foramen.
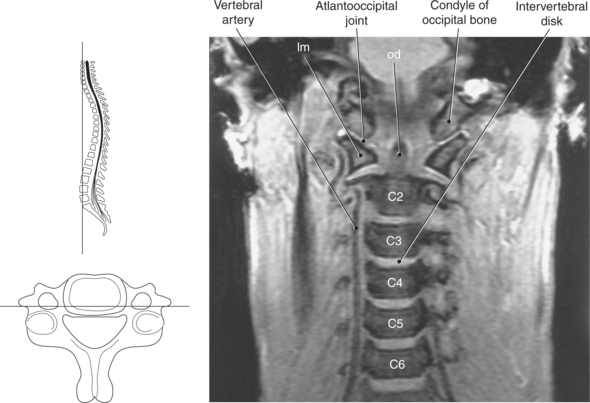
Figure 4.15 Coronal, T1-weighted MR scan of cervical spine.
Key: lm, Lateral mass; od, odontoid process.
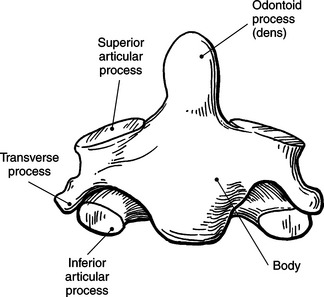
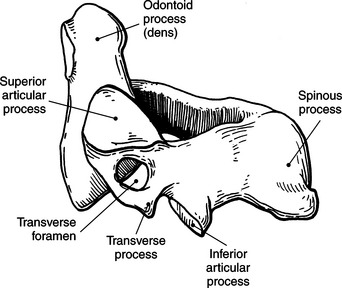
The second cervical vertebra, the axis, has a large odon-toid process (dens) that projects upward from the superior surface of the body. The odontoid process projects into the anterior ring of the atlas to act as a pivot for rotational move-ment of the atlas (Figures 4.16 through 4.18). Lateral to the odontoid process on the upper surface of the body are the superior articular processes, on which the atlas articulates (Figures 4.19 and 4.20). The spinous process of the axis is the first projection to be felt in the posterior groove of the neck. The cervical vertebrae C3-C6 have a unique configuration with their bifid spinous process (Figures 4.21 and 4.22). The seventh cervical vertebra (vertebra prominens) has a long spinous process that is typically not bifid. This spinous process is easily palpable posteriorly at the base of the neck (Figures 4.23 through 4.25).
Thoracic Vertebrae
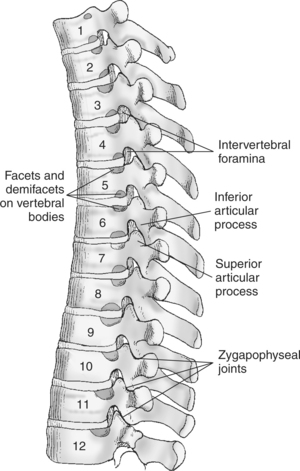
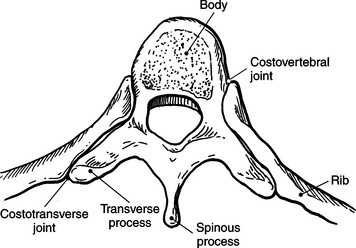
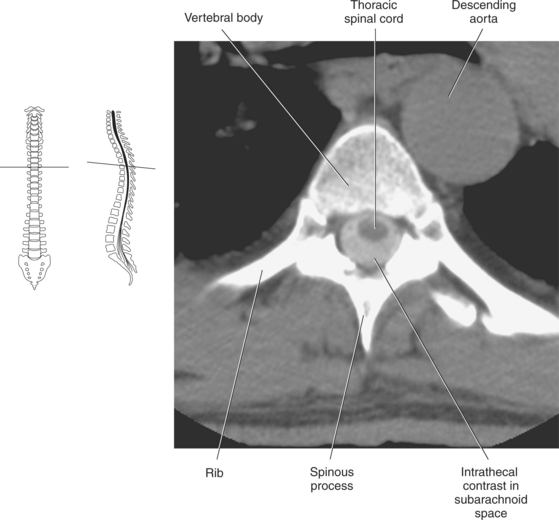
Twelve vertebrae make up the thoracic section. They have typical vertebral configurations except for their characteristic costal facets (demi facets), located on the body and transverse process, that articulate with the ribs. The head of the rib articu-lates with the vertebral bodies at the costovertebral joints, whereas the tubercle of the ribs articulates with the transverse processes at the costotransverse joints. The spinous processes of the thoracic vertebrae are typically long and slender, project-ing inferiorly over the vertebral arches of the vertebrae below (Figures 4.24, 4.26, and 4.27).
Lumbar Vertebrae
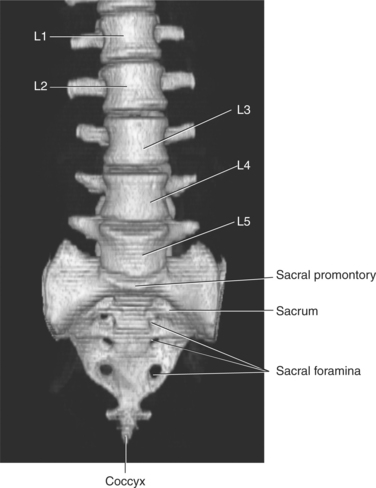
The lumbar section typically consists of five vertebrae. Their massive bodies increase in size from superior to inferior (Figure 4.28). The largest of the lumbar vertebrae, L5, is characterized by its massive transverse processes. The entire weight of the upper body is transferred from the fifth lumbar vertebra to the base of the sacrum across the L5-S1 disk (Figures 4.29 through 4.32).
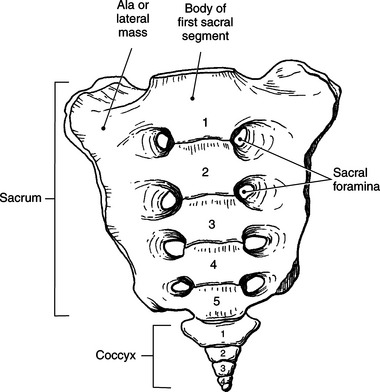
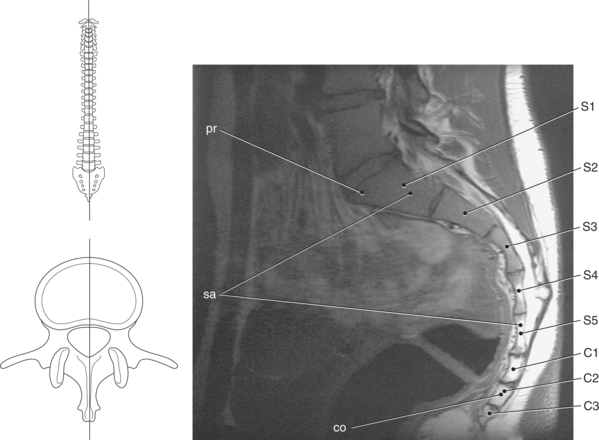
Sacrum and Coccyx
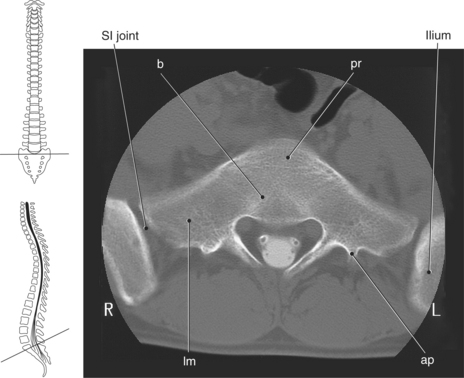
The sacral section consists of five vertebrae that fuse to form the sacrum. Their transverse processes combine to form the lateral masses (ala), which articulate with the pelvic bones at the sacroiliac joints. Located within the lateral masses are the sacral foramina that allow for the passage of nerves (Figures 4.33 and 4.34). The first sacral segment has a promi-nent ridge located on the anterior surface of the body termed the sacral promontory (Figures 4.35 and 4.36). This bony land-mark is used to separate the abdominal cavity from the pelvic cavity. The spinous process of the fifth sacral segment is absent, leaving an opening termed the sacral hiatus (Figure 4.2). Located at the sides of the sacral hiatus are the inferior articular processes of the fifth sacral segment that project downward as the sacral cornu. Located inferior to the fifth sacral segment is the coccyx, which consists of three to five small fused bony segments (Figures 4.33 and 4.35). Superior projections off of the first coccygeal segment, called cornu, have ligamentous attachments to the sacral cornu that provide additional stability to the articulation between the sacrum and coccyx. The coccyx represents the most inferior portion of the vertebral column.
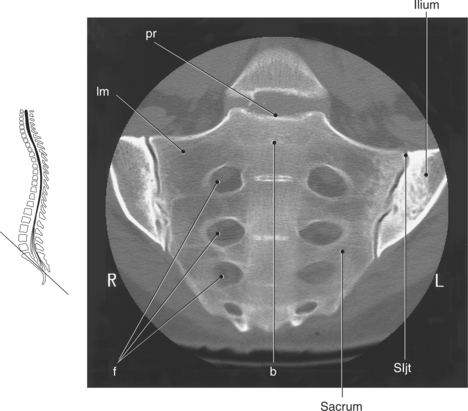
Figure 4.34 Coronal CT scan of sacrum and coccyx.
Key: pr, Sacral promontory; lm, lateral mass; f, sacral foramina; b, body of S1; SIjt, sacroiliac joint.
LIGAMENTS
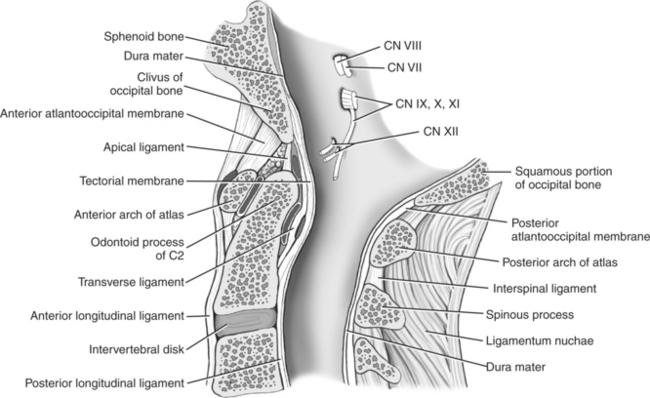
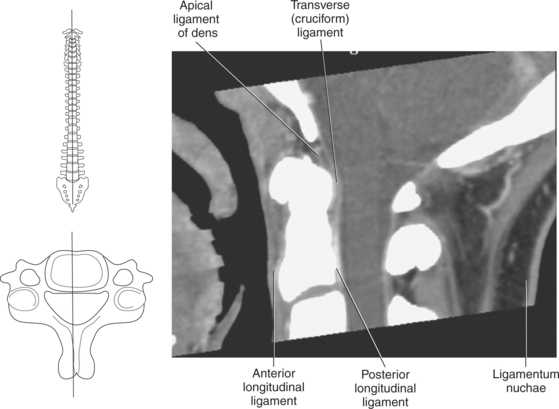
Specific ligaments of the spine serve to connect the cervical vertebrae and the cranium to provide mobility and protection for the head and neck. The apical ligament is a midline struc-ture that connects the apex of the odontoid process to the anterior margin of the foramen magnum (Figures 4.37 through 4.39). The alar ligaments are two strong bands that extend obliquely from the sides of the odontoid process, upward to the lateral margins of the occipital condyles to limit rotation and flexion of the head (Figures 4.40 and 4.41). The trans-verse ligament extends across the ring of C1 to form a sling over the posterior surface of the odontoid process. It has a small band of longitudinal fibers that ascend to attach to the anterior margin of the foramen magnum and inferiorly to attach to the body of the axis. The transverse ligament func-tions to hold the odontoid process of C2 against the anterior arch of C1 (Figures 4.40, 4.42, and 4.43). The transverse liga-ment is sometimes called the cruciform ligament because of its crosslike appearance.
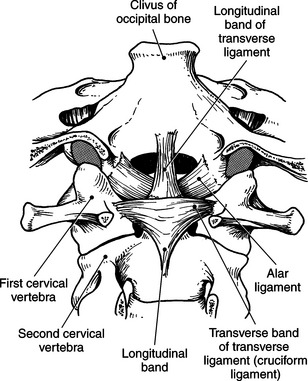
Figure 4.40 Posterior view of alar ligaments.
Key: lm, Lateral mass; od, odontoid process; al, alar ligament; tl, transverse ligament.
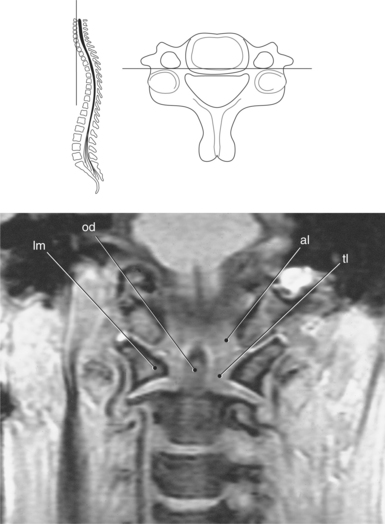
Figure 4.41 Coronal, T1-weighted MR scan of alar and transverse ligaments.
Key: ln, ligamentum nuchae; dr, dorsal root; vr, ventral root; tl, transverse ligament.
Another important ligament of the cervical region is the ligamentum nuchae, which serves as an attachment point for muscles. This expansive ligament extends from the external occipital protuberance of the cranium to the spinous processes of the cervical vertebrae (Figures 4.37 through 4.39). The liga-mentum nuchae continues inferiorly as the supraspinous liga-ment. The supraspinous ligament is a narrow band of fibers that runs over and connects the tips of the spinous processes from the seventh cervical vertebra to the lower lumbar vertebrae (Figures 4.44 through 4.46).
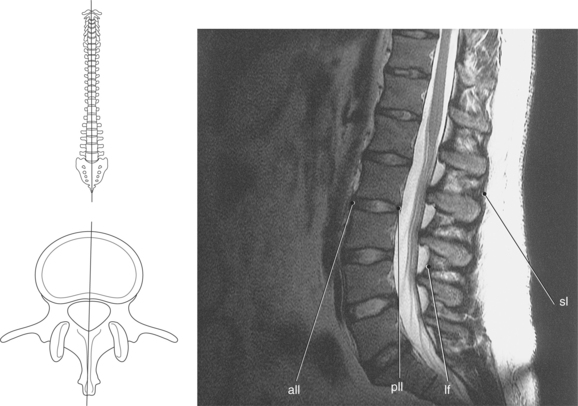
Figure 4.46 Midsagittal, T2-weighted MR scan of lumbar spine demonstrating spinal ligaments.
Key: all, Anterior longitudinal ligament; pll, posterior longitudinal ligament; lf, ligamentum flava; sl, supraspinous ligament.
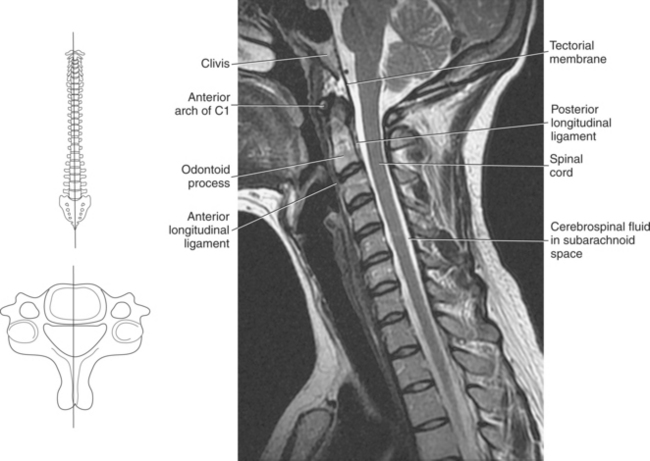
In addition to the ligaments listed above, the stability of the suboccipital region of the spine is reinforced with the atlanto-occipital and tectorial membranes. The atlanto-occipital membrane consists of an anterior and posterior portion that serves to connect the arches of the atlas with the occipital bone. The anterior atlantooccipital membrane passes from the anterior arch of the atlas and connects to the anterior margin at the base of the occipital bone. This ligament is the superior extension of the anterior longitudinal ligament. The posterior atlantooccipital membrane extends from the pos-terior margin of the foramen magnum to the posterior arch of the atlas, closing the posterior portion of the vertebral canal between the skull and C1 (Figure 4.37). The tectorial membrane is a broad ligament that extends from the clivus of the occipital bone to the posterior body of the axis, covering the dens, transverse, apical, and alar ligaments. The tectorial membrane forms the anterior boundary of the vertebral canal and is continuous with the posterior longitudinal ligament (Figures 4.37 through 4.39).
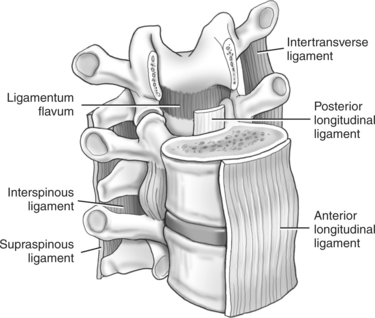
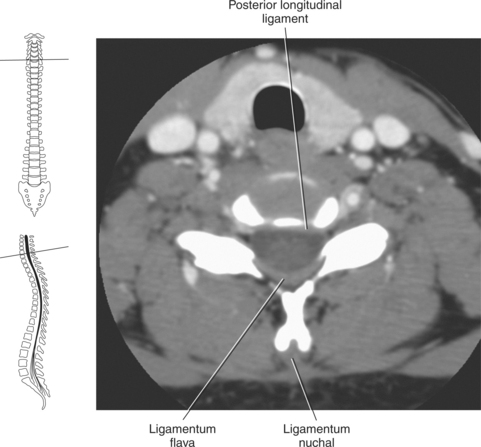
Several ligaments enclose the vertebral column to help protect the spinal cord and maintain stability of the vertebral column. Two of the larger ligaments are the anterior and posterior longitudinal ligaments (Figure 4.44). The anterior longitudinal ligament is a broad fibrous band that extends downward from C1 along the entire anterior surface of the vertebral bodies to the sacrum. This ligament connects the anterior aspects of the vertebral bodies and intervertebral disks to maintain stability of the joints and to help prevent hyper-extension of the vertebral column. It is thicker in the thoracic region than in the cervical and lumbar regions, providing additional support to the thoracic spine. The posterior longitudinal ligament is narrower and slightly weaker than the anterior longitudinal ligament. It lies inside the vertebral canal and runs along the posterior aspect of the vertebral bodies (Figures 4.44 through 4.49). Unlike the anterior longitudinal ligament, the posterior longitudinal ligament is attached only at the intervertebral disk and adjacent margins. It is separated from the middle of each vertebra by epidural fat that provides passage of the basivertebral veins. The posterior longitudinal ligament runs the entire length of the vertebral column beginning at C2. This ligament helps to prevent posterior protrusion of the nucleus pulposus and hyperflexion of the vertebral column.
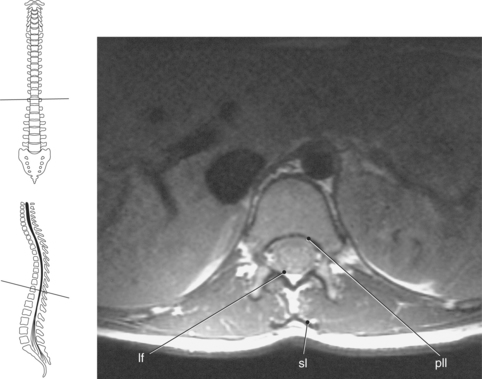
Figure 4.48 Axial, T1-weighted MR scan of thoracic spine demonstrating spinal ligaments.
Key: lf, Ligamentum flava; sl, supraspinous ligament; pll, posterior longitudinal ligament.
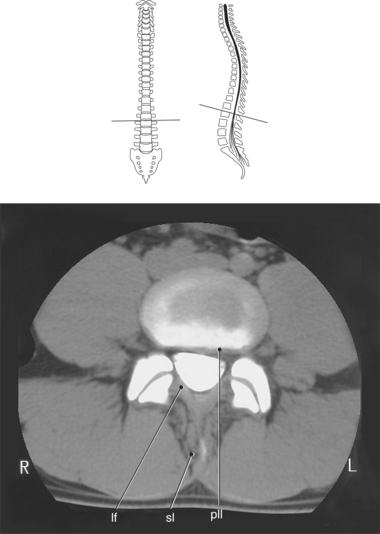
Figure 4.49 Axial CT scan of lumbar vertebra demonstrating spinal ligaments.
Key: lf, Ligamentum flava; sl, supraspinous ligament; pll, posterior longitudinal ligament.
The ligamentum flava are strong ligaments (consisting of yellow elastic tissue) present on either side of the spinous process. They join the laminae of adjacent vertebral arches, helping to preserve the normal curvature of the spine (Figures 4.44 through 4.49).
MUSCLES
Muscles of the back can be separated into three groupings or layers; the superficial layer (splenius muscles), the intermediate layer (erector spinae group), and the deep layer (transversospinal group). The muscle groups that run the length of the spine can be divided into regions according to their location: capitis, cervicis, thoracis, and lumborum (Table 4.1).
TABLE 4-1
| MUSCLE | ORIGIN | INSERTION |
| Splenius | ||
| Splenius capitis | Ligamentum nuchae and spinous processes of C7-T3 | Mastoid process of temporal bone |
| Splenius cervicis | Spinous processes of T3-T6 | Transverse processes of C1-C4 |
| Erector spinae | ||
| Iliocostalis | ||
| Iliocostalis cervicis | Angles of 4th to 7th ribs | Transverse processes of C4-C6 |
| Iliocostalis thoracis | Angles of 7th to 12th ribs | Angles of ribs 1 to 6: transverse process of C7 |
| Iliocostalis lumborum | Sacrum and iliac crest, spinous processes of lumbar vertebrae | Angles of ribs 7 to 12 |
| Longissimus | Transverse processes of C3-T3 | Mastoid process of temporal bone |
| Longissimus capitis | Transverse processes of T1-T6 | Transverse processes of C2-C5 |
| Longissimus cervicis | Transverse processes of lumbar vertebrae | Transverse processes of all thoracic vertebrae, tubercles of inferior 10 ribs |
| Longissimus thoracis | Fibers blend with semispinalis capitis muscles | Fibers blend with semispinalis capitis muscles |
| Spinalis | ||
| Spinalis capitis | Lower ligamentum nuchae and spinous process of C7 | Spinous process of C2 |
| Spinalis cervicis (inconsistent) | Spinous processes of T11-L2 | Spinous processes of T1-T8 |
| Spinalis thoracis | ||
| Transversospinal | ||
| Semispinalis | ||
| Semispinalis capitis | Transverse processes of C7-T6; articular processes of C4-C6 | Occipital bone between superior and inferior nuchal lines |
| Semispinalis cervicis | Transverse processes of T2-T6 | Spinous processes of C2-C5 |
| Semispinalis thoracis | Transverse processes of T6-T10 | Spinous processes of C6-T4 |
| Multifidus | Transverse processes of thoracic vertebrae and articular processes of four inferior cervical vertebrae, sacrum, and posterior superior iliac spine | Spinous processes of C1-L5 |
| Rotatores | Transverse processes of T2-T12; poorly developed in cervical and lumbar regions | Lamina of T1-T11; poorly developed in cervical and lumbar regions |
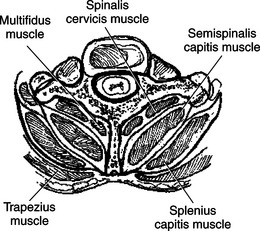
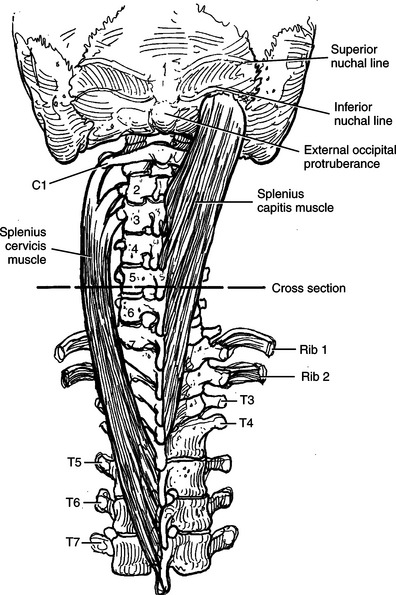
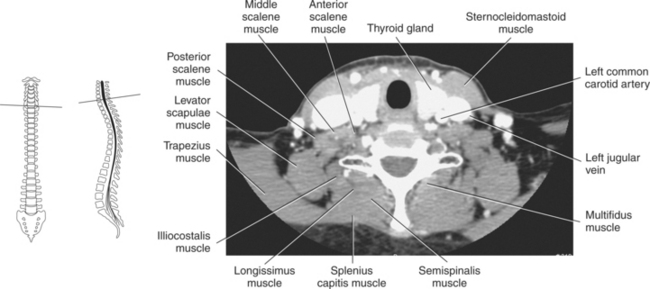
Superficial Layer
The splenius muscles are located on the lateral and posterior aspect of the cervical and upper thoracic spine. These bandage-like muscles originate on the spinous processes of C7-T6 and the inferior half of the ligamentum nuchae. They are divided into a cranial portion, splenius capitus, that inserts on the mastoid process of the temporal bone and a cervical portion, splenius cervicis, that inserts on the transverse processes of C1-C4 (Figures 4.50 through 4.53). Together they act to extend the head and neck.
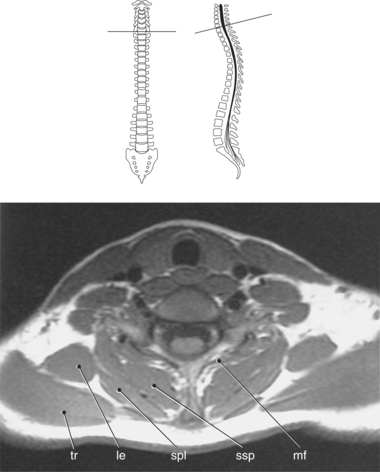
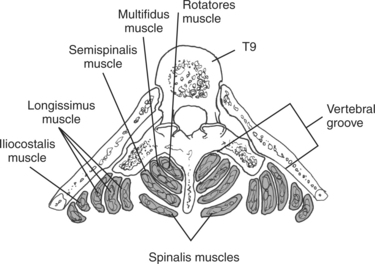
Intermediate Layer
The intermediate muscle group, the erector spinae muscle group, consists of massive muscles that form a prominent bulge on each side of the vertebral column. The erector spinae muscle group is the chief extensor of the vertebral column and is arranged in three vertical columns, the iliocostalis layer (lateral column), longissimus layer (intermediate column), and the spinalis layer (medial column) (Figures 4.54 and 4.55). This muscle group arises from a common broad tendon from the posterior part of the iliac crest, sacrum, and inferior lumbar spinous processes. The iliocostalis muscles run superiorly to attach to the angles of the ribs and transverse processes of C7 to C4. The longissimus muscles run superiorly to insert into the tips of the transverse processes of the thoracic and cervical regions, the angles of the ribs, and the mastoid process. The narrow spinalis muscle group extends from the spinous processes of the upper lumbar and lower thoracic regions to the spinous processes of the superior thoracic region. The cervicis and capitis portion of the muscle are inseparable from the semispinalis of the transversospinal group (Figures 4.55 through 4.57).
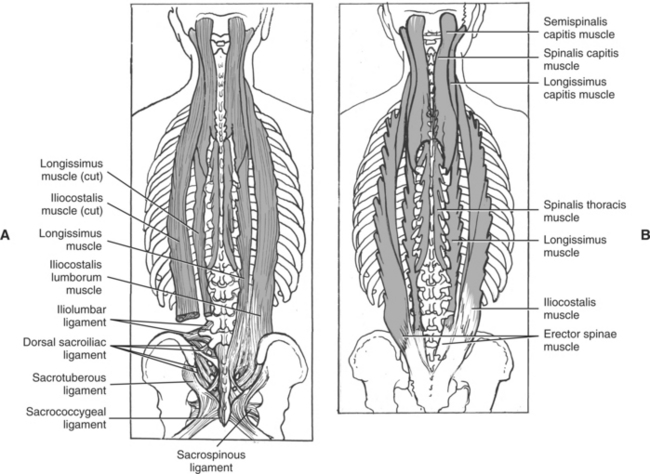
Figure 4.54 A, Posterior view of longissimus and iliocostalis muscles of the erector spinae muscle group.B, Posterior view of spinalis muscle of the erector spinae muscle group.
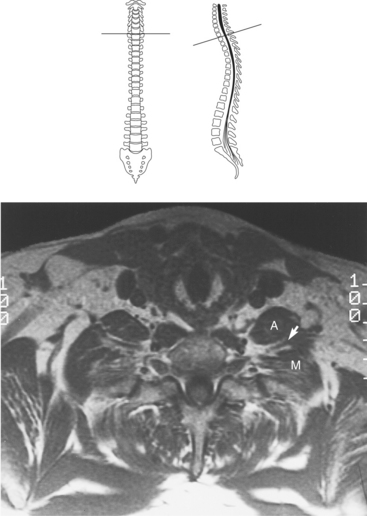
Deep Layer
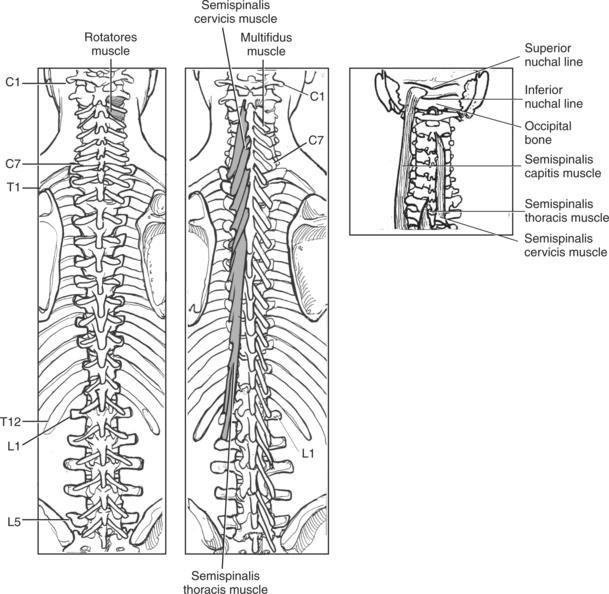
The transversospinal muscles consist of several short muscles that are located in the groove between the transverse and spinous processes of the vertebrae. They can be separated into the semispinalis, multifidus, and rotatores with a primary function to flex and rotate the vertebral column (Figures 4.55 through 4.58). The semispinalis muscles arise from the thoracic and cervical transverse processes and insert on the occipital bone and spinous processes in the thoracic and cervical regions. The semispinalis muscles form the largest muscle mass in the posterior portion of the neck. The multifidus muscles consist of many fibrous bundles that extend the full length of the spine and are the most prominent in the lumbar region. The deepest of the transversospinal muscles are the rotatores, which connect the lamina of one vertebra to the transverse process of the vertebra below. They are best developed in the thoracic region.
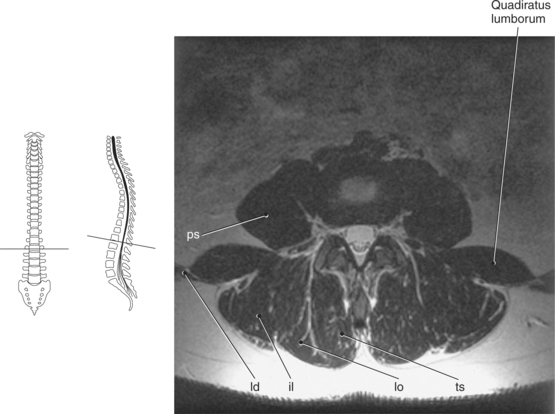
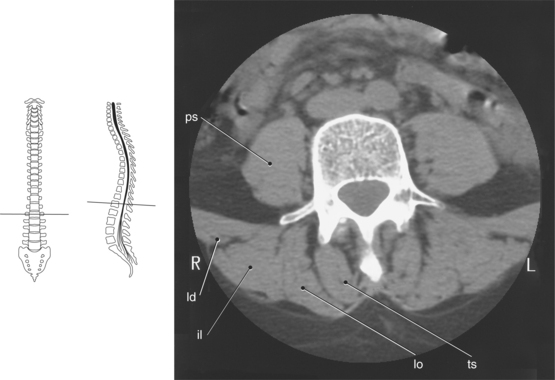
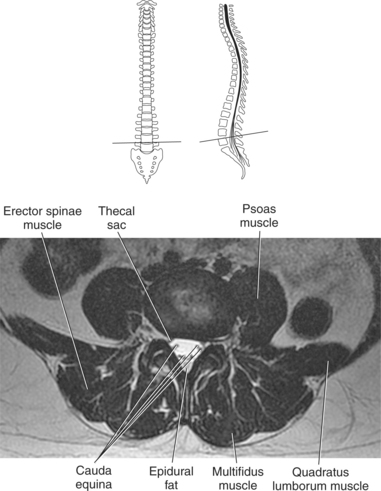
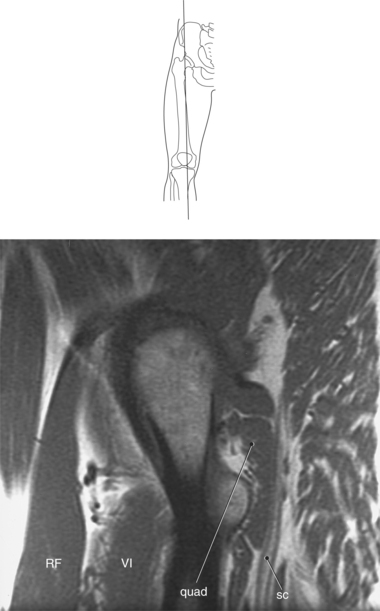
Two additional muscles that are commonly visualized in the lumbar region of the spine are the quadratus lumborum and the psoas muscles, which are considered abdominal muscles (Figures 4.59 through 4.61). Further information on these muscles can be found in Chapter 7.
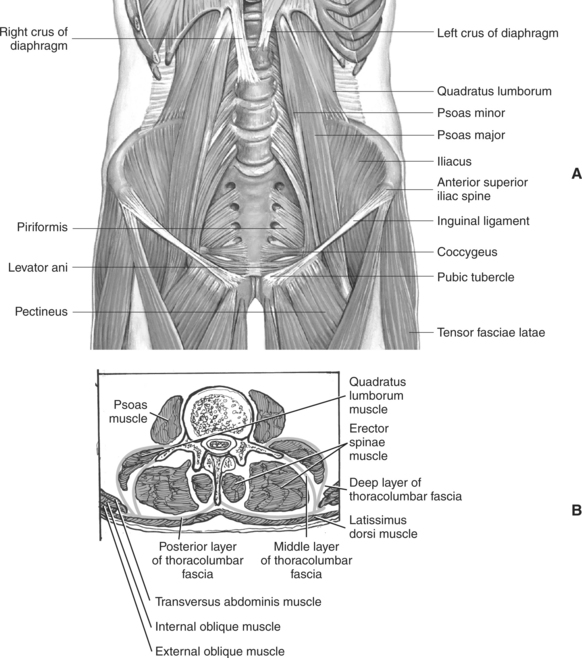
Figure 4.59 A, Coronal view of quadratus lumborum and psoas muscles. B, Axial view of quadratus lumborum and psoas muscles.
SPINAL CORD
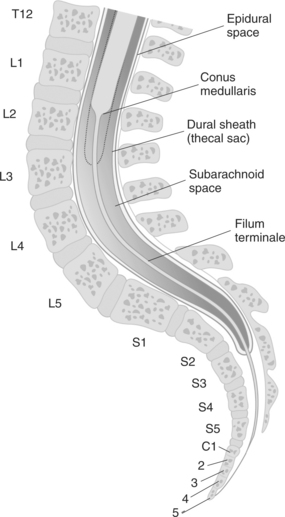
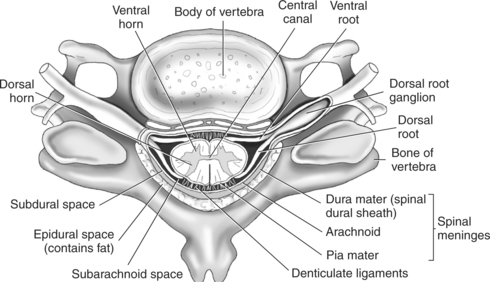
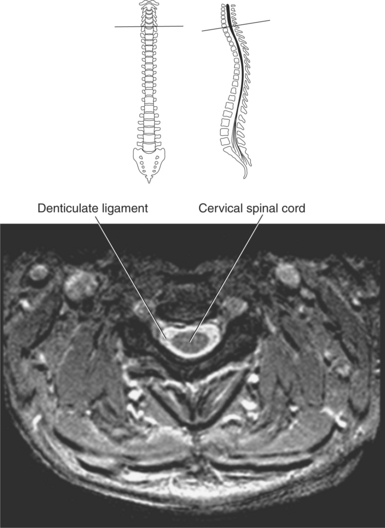
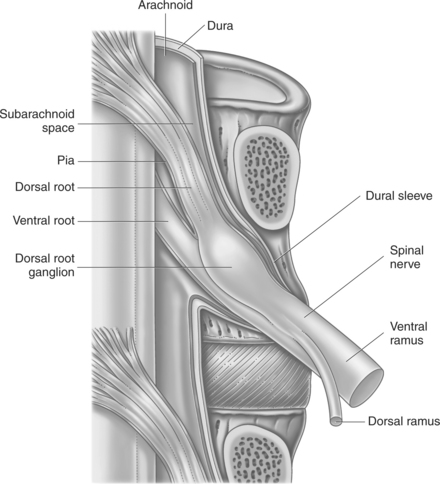
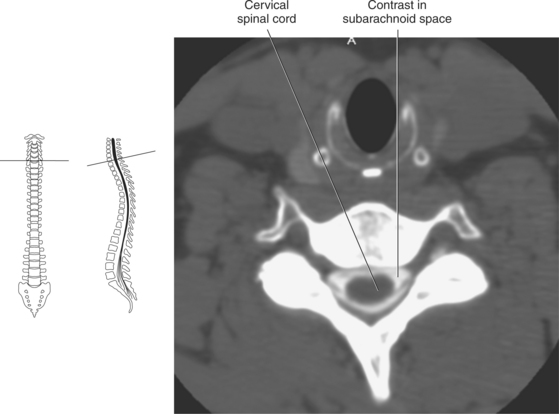
Throughout its length, the delicate spinal cord is surrounded and protected by cerebrospinal fluid, which is contained in the thecal sac formed by the spinal meninges (Figure 4.62). The spinal meninges are continuous with the cranial meninges and can be broken into the same three layers: dura, arachnoid, and pia. The dura mater is the tough outer layer that extends to S2, creating the thecal sac (Figures 4.63 and 4.64). The spinal dura mater adheres to the posterior longitudinal liga-ment and is separated from the vertebral column by an epidural space that contains fat and vessels. Each spinal nerve is surrounded by dura mater that extends through the inter-vertebral foramen. The arachnoid mater is the thin trans-parent membrane that is attached to the inner surface of the dura mater. A potential space called the subdural space runs between the arachnoid and dura mater. The arachnoid mater is connected to the pia mater by numerous delicate strands creating the spiderlike appearance associated with the arach-noid mater. The space between the arachnoid mater and pia mater is the subarachnoid space, which is filled with cerebro-spinal fluid and the blood vessels that supply the spinal cord (Figures 4.62, 4.65, and 4.66). The pia mater is a highly vascular layer that closely adheres to the spinal cord. At the distal end of the spinal cord, approximately L1, the pia mater continues as a long slender strand called the filum terminale. The filum terminale descends through the subarachnoid space to the inferior border of the thecal sac, where it is reinforced by the dura mater. After leaving the thecal sac, it eventually exits the sacral canal through the sacral hiatus and attaches to the coccyx, providing an anchor between the spinal cord and the coccyx (Figures 4.62 and 4.63). In addition, lateral extensions of the pia mater leave the spinal cord to form 21 pairs of denticulate ligaments that attach to the dura, preventing lateral movement of the spinal cord within the thecal sac (Figures 4.65 and 4.67).
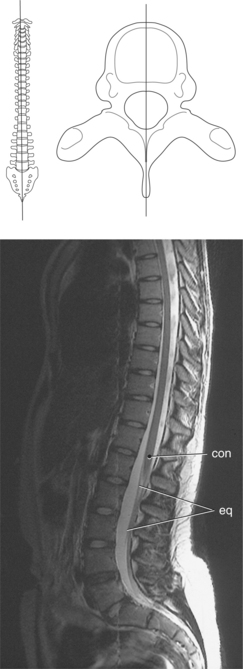
Figure 4.64 Midsagittal, T2-weighted MR scan of thecal sac, conus medullaris, and filum terminale.
Key: con, Conus medullaris; eq, cauda equina.
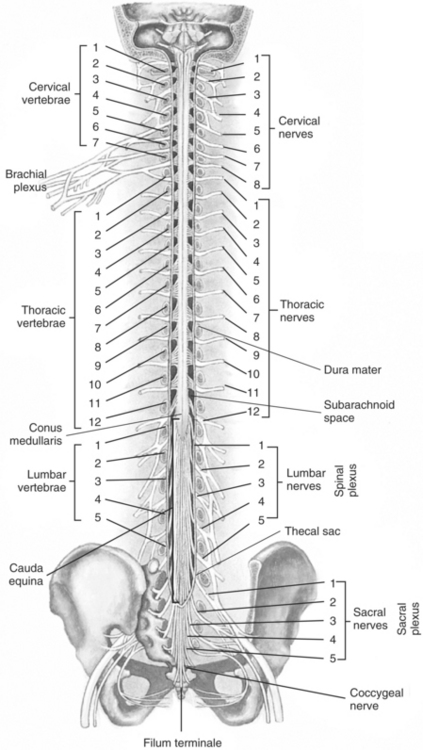
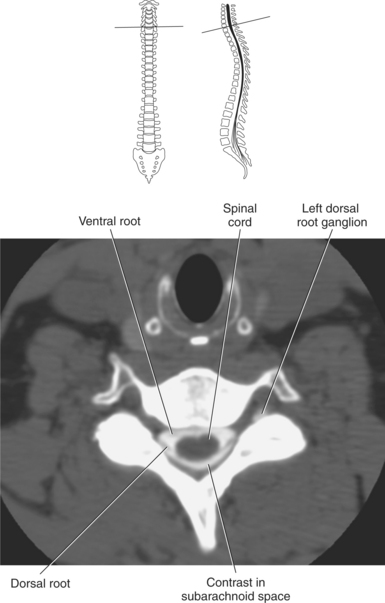
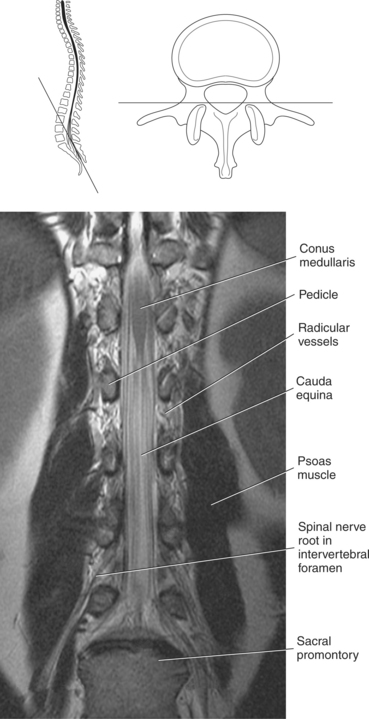
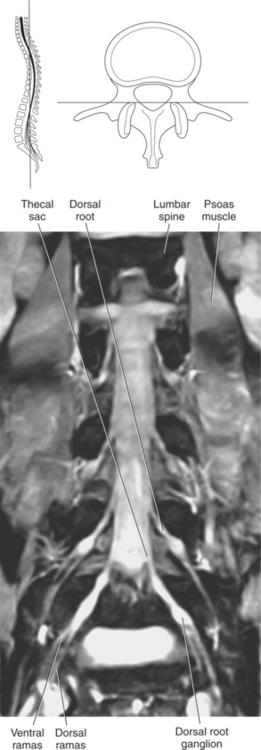
Spinal Cord and Nerve Roots
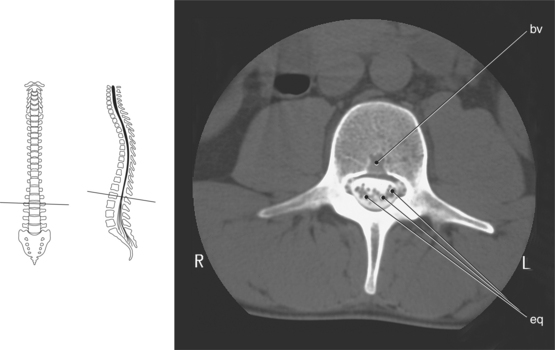
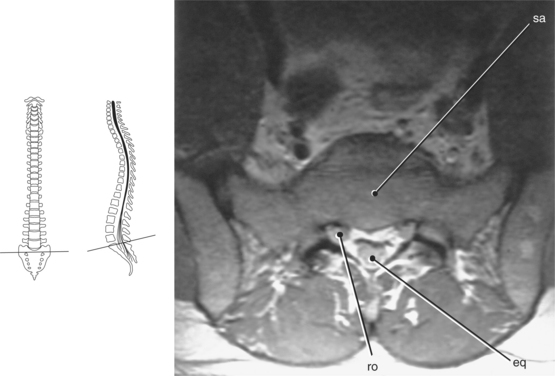
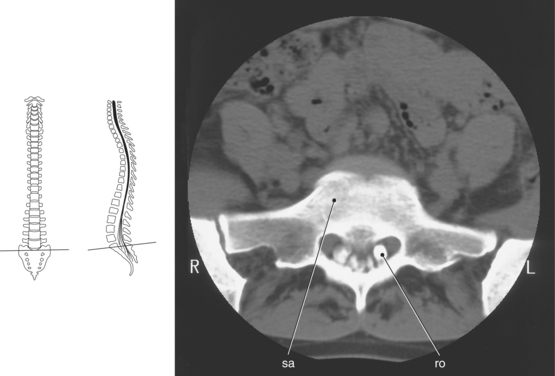
The spinal cord functions as a large nerve cable that connects the brain with the body. It begins as a continuation of the medulla at the inferior margin of the brainstem and extends to approximately the first or second lumbar vertebra. The spinal cord tapers into a cone-shaped segment called the conus medullaris (Figures 4.62, 4.64, and 4.68 through 4.70). The conus medullaris is the most inferior portion of the spinal cord and is located at approximately the level of the first or second lumbar vertebra. At the termination of the spinal cord, nerves continue inferiorly in bundles. This grouping of nerves has the appearance of a horse’s tail and is termed the cauda equina, exiting through the lumbosacral foramina (Figures 4.62, 4.68, 4.71, and 4.72).
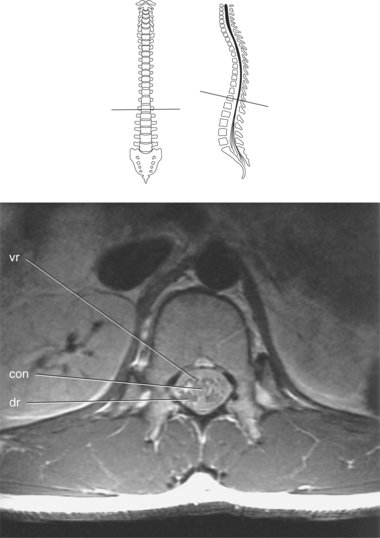
Figure 4.69 Axial, T1-weighted MR scan of conus medullaris.
Key: vr, Ventral root; con, conus medullaris; dr, dorsal root.
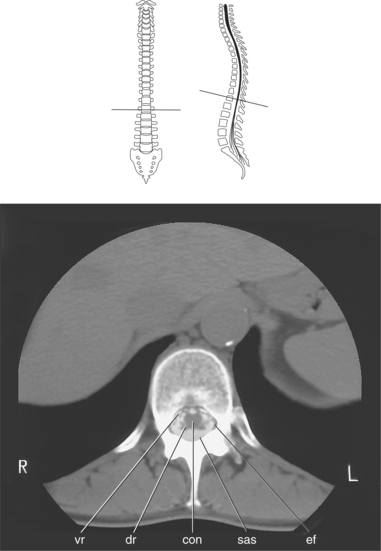
Figure 4.70 Axial CT scan of conus medullaris.
Key: vr, Ventral root; dr, dorsal root; con, conus medullaris; sas, subarachnoid space; ef, epidural fat.
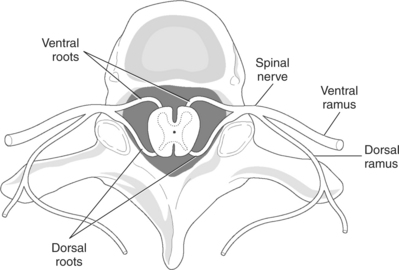
The spinal cord is composed of white and gray matter. The white matter comprises the external borders of the cord and is more abundant. The gray matter is composed of nerve cells and runs the entire length of the cord. It is centrally located and surrounds the central canal, which contains cerebrospinal fluid and is continuous with the ventricles of the brain (Figures 4.65 and 4.73). In cross section, the gray matter has the appearance of a butterfly. The two posterior projections are the dorsal horns, and the two anterior projections are the ventral horns (Figure 4.65). The dorsal horns contain neurons and sensory fibers that enter the cord from the body periphery via the dorsal roots. These are called the afferent (sensory) nerve roots (Figures 4.66 and 4.74). The dorsal root ganglion, an oval enlargement of the dorsal root that contains the nerve cell bodies of the sensory neurons, is located in the inter-vertebral foramen (Figures 4.65, 4.66, and 4.75 through 4.79). The ventral horns contain the nerve cell bodies of the efferent (motor) neurons. The efferent (motor) nerve roots exit the spinal cord via the ventral root to be distributed throughout the body. Just outside the intervertebral foramina, the ventral and dorsal roots unite to form the 31 pairs of spinal nerves. Eight of these nerve pairs correspond to the cervical region, 12 belong to the thoracic section, 5 correspond to the lumbar region, 5 correspond to the sacrum, and 1 belongs to the coccyx (Figures 4.80 through 4.82). Each spinal nerve provides a specific cutaneous distribution that can be demonstrated on a dermatome map (Figure 4.83).
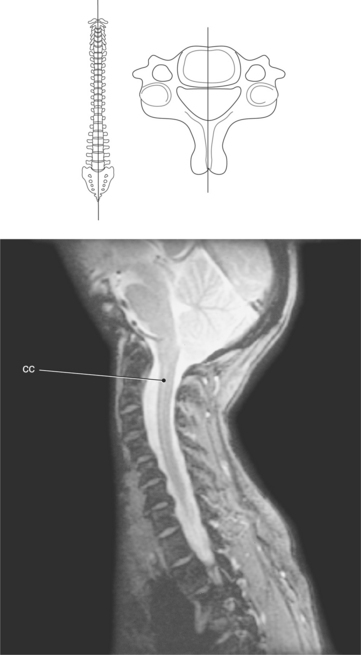
Figure 4.73 Sagittal, T2-weighted MR scan of cervical spine and central canal.
Key: cc, Central canal.
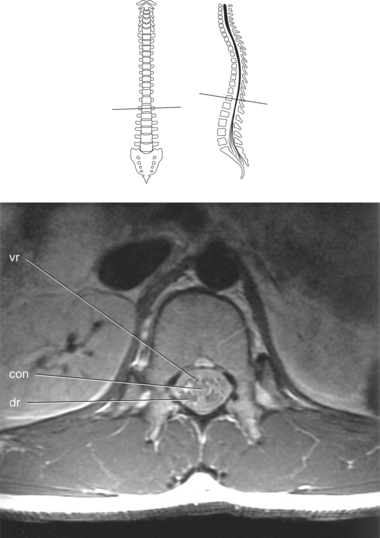
Figure 4.74 Axial, T1-weighted MR scan of spinal cord with ventral and dorsal roots.
Key: vr, ventral root; con, conus medullaris; dr, dorsal root.
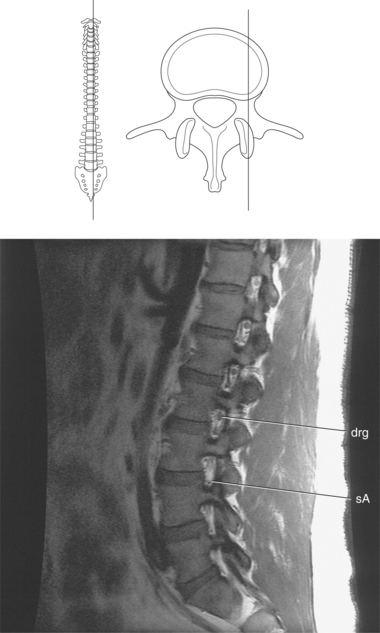
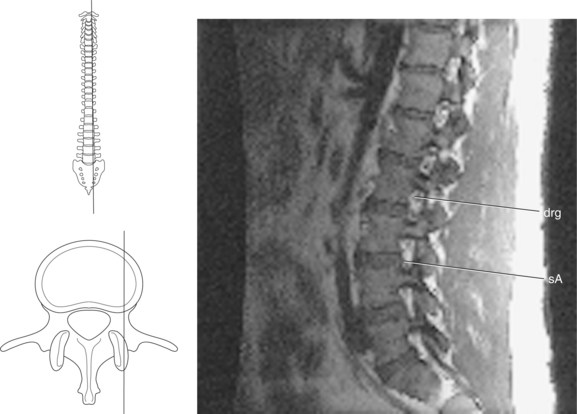
Figure 4.76 Sagittal, T1-weighted MR scan of lumbar spine with neural foramina.
Key: drg, Dorsal root ganglion; sA, spinal artery.
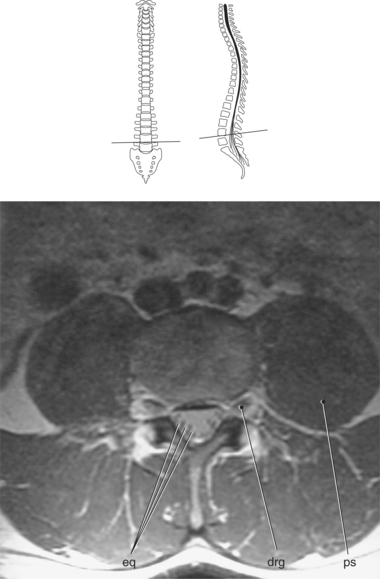
Figure 4.77 Axial, T1-weighted MR scan of lumbar vertebra with dorsal root ganglion.
Key: eq, cauda equina; drg, Dorsal root ganglion; ps, psoas muscle.
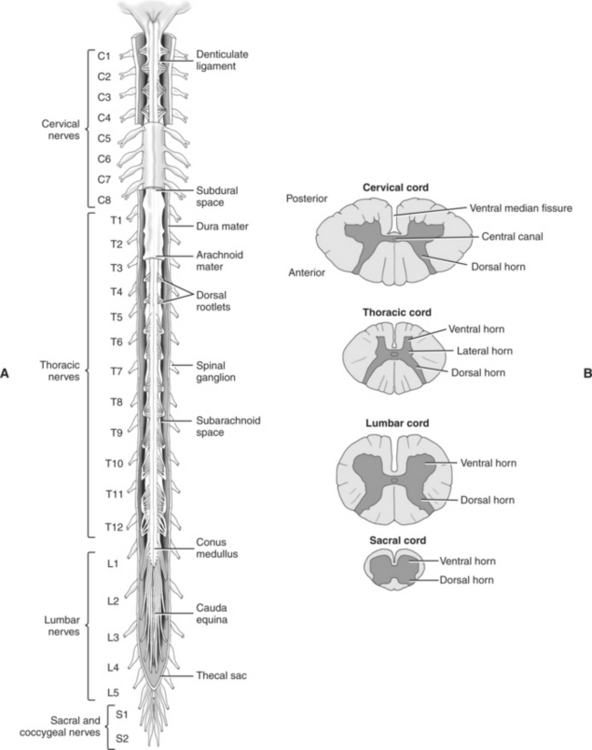
Figure 4.80 A, Posterior view of spinal cord and meninges. B, Transverse sections through spinal cord.
PLEXUSES
The spinal cord is enlarged in two regions by the cell bodies of nerves that extend to the extremities. The cervical enlarge-ment extends from the vertebral bodies of approximately C3-C7, and the lumbosacral enlargement occurs within the lower thoracic region. Cross-section images of the spinal cord at various levels have considerable differences in size and shape because of the changing proportion of gray and white matter (Figures 4.80, and 4.84 through 4.89).
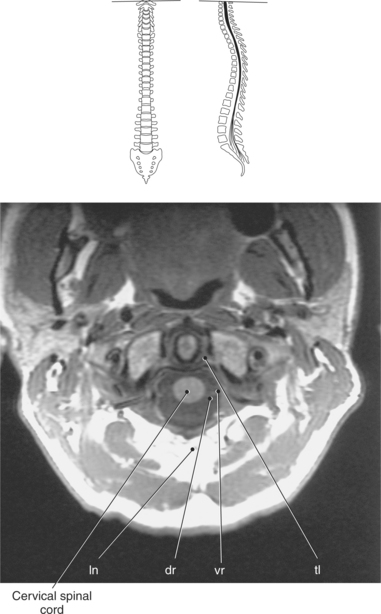
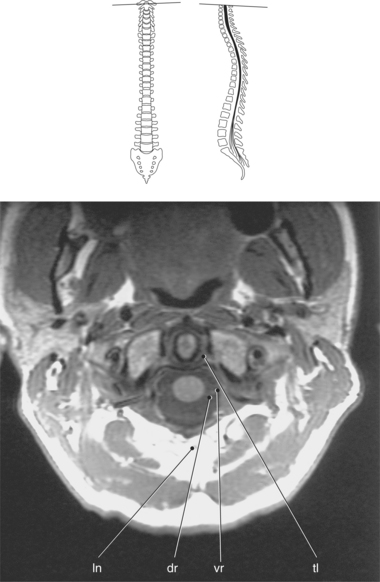
Figure 4.84 Axial, T1-weighted MR scan of cervical spinal cord.Key: ln, Ligamentum nuchae; dr, dorsal root; vr, ventral root; tl, transverse ligament.
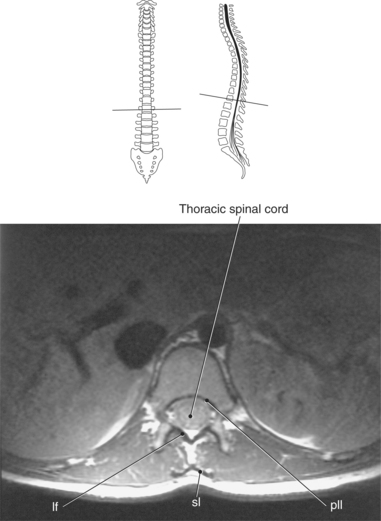
Figure 4.86 Axial, T1-weighted MR scan of thoracic spinal cord.
Key: lf, Ligamentum flava; sl, supraspinous ligament; pll, posterior longitudinal ligament.
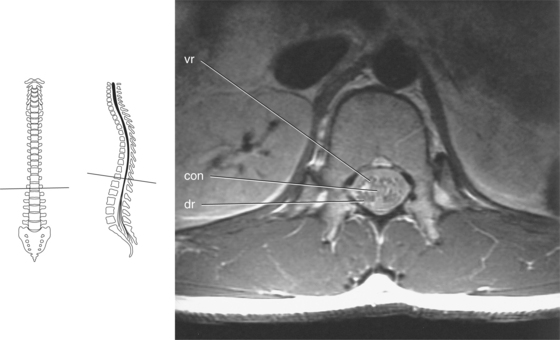
Figure 4.88 Axial, T1-weighted MR scan of spinal cord at conus T-12.
Key: vr, Ventral root; con, conus medullaris; dr, dorsal root.
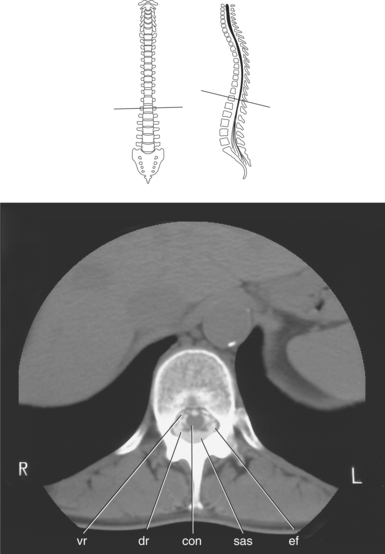
Figure 4.89 Axial CT scan of lumbar spinal cord at conus T-12.
Key: vr, Ventral root; dr, dorsal root; con, conus medullaris; sas, subarachnoid space with contrast; ef, epidural fat.
Shortly after emerging from the spinal cord, each nerve divides into dorsal and ventral rami that contain both motor and sensory fibers (Figure 4.90). The dorsal rami of all spinal nerves extend posteriorly to innervate the skin and muscles of the posterior trunk. The ventral rami of T2-T12 pass anteriorly as the intercostal nerves to supply the skin and muscles of the anterior and lateral trunk. The ventral rami of all other spinal nerves form complex networks of nerves called plexuses. These plexuses serve the motor and sensory needs of the muscles and skin of the extremities. The four major nerve plexuses are the cervical, brachial, lumbar, and sacral (Figure 4.91).
Cervical Plexus
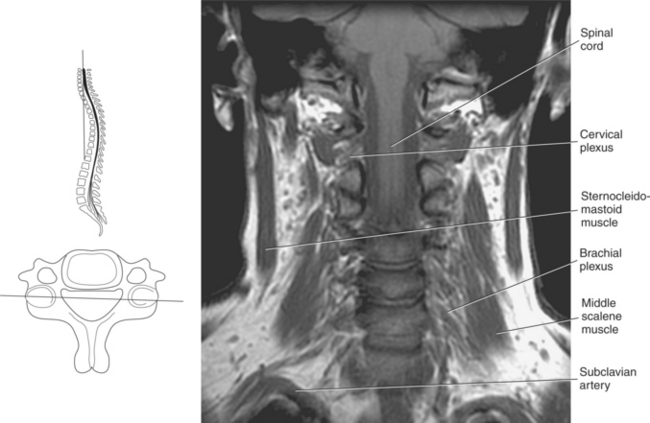
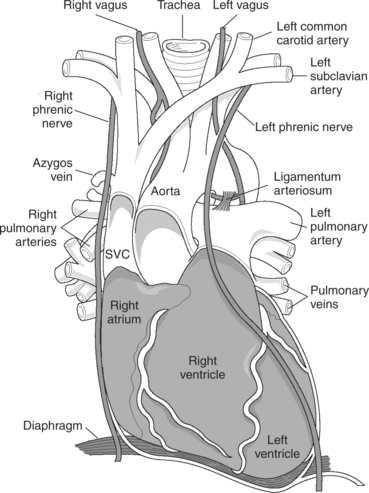
The cervical plexus arises from the upper four ventral rami of C1-C4 to innervate from the neck, lower part of the face and ear, the side of the scalp, and the upper thoracic area. The major motor branch of this plexus is the phrenic nerve, which is formed by the branches of C3, C4, and upper division of C5. This nerve descends vertically down the neck and passes into the superior thoracic aperture. The phrenic nerve continues inferiorly to the diaphragm, together with the pericardiophrenic vessels, through the anterior hilum between the mediastinal pleura and the pericardium. The left and right phrenic nerves can be slightly different in lengths. The right phrenic nerve runs along the lateral wall of the superior vena cava and right atrium of the heart. The left phrenic nerve courses lateral to the left ventricle of the heart (Figures 4.91 through 4.94).
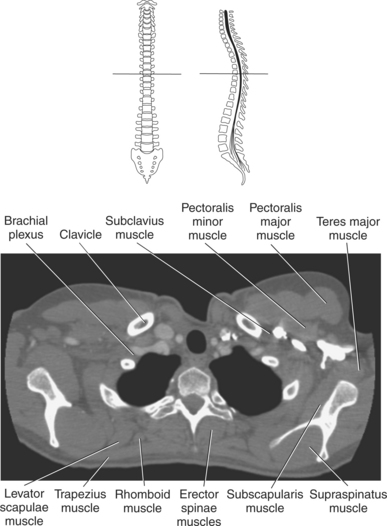
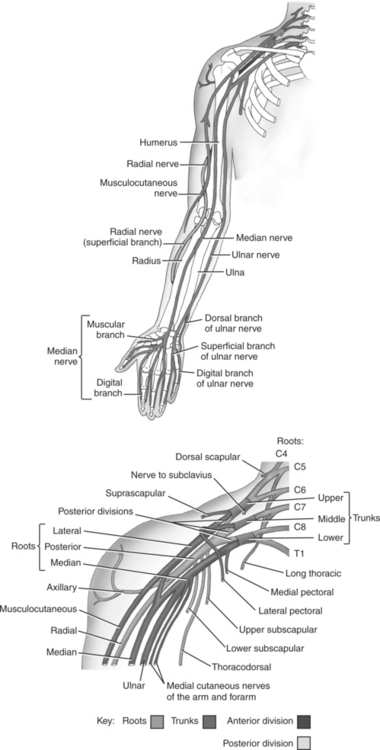
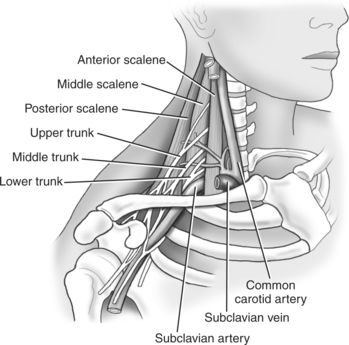
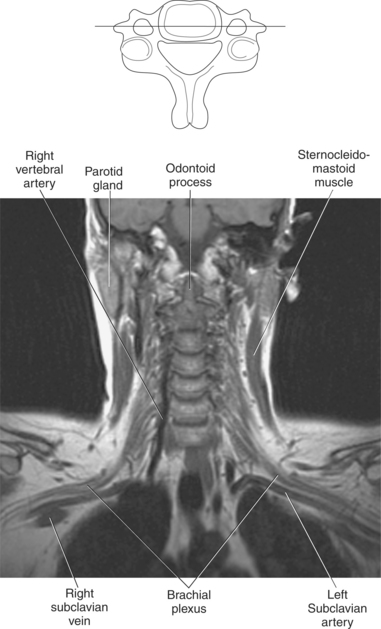
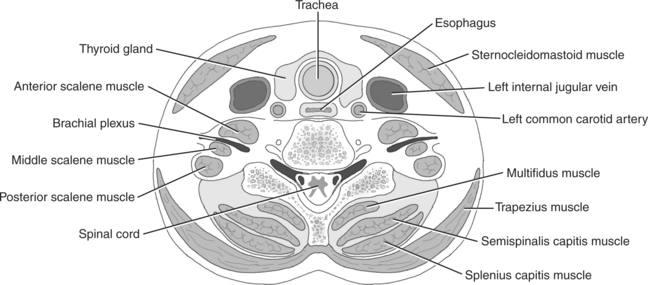
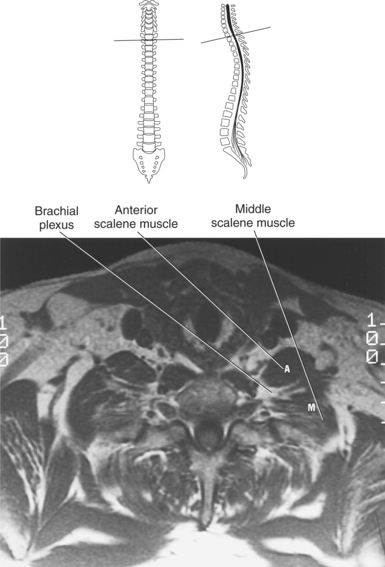
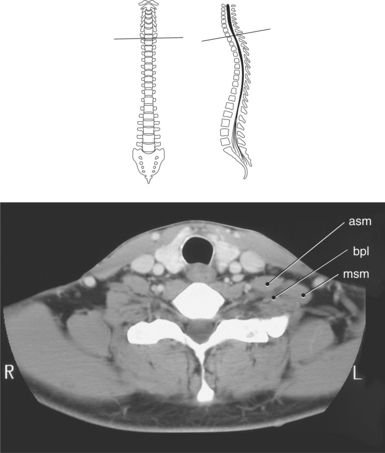
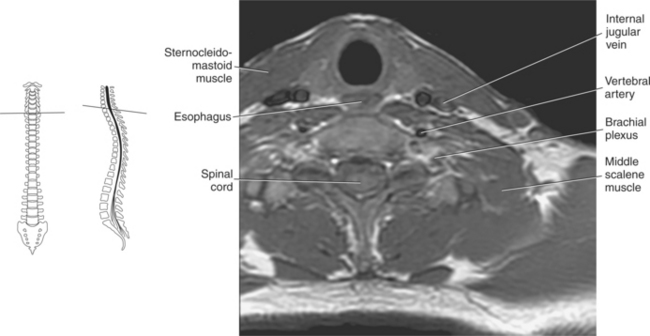
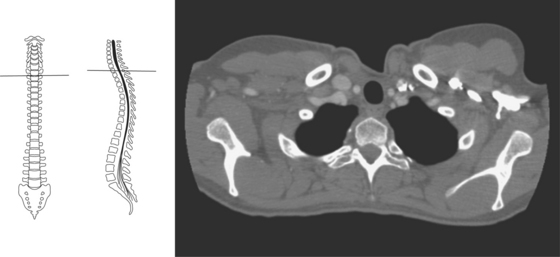
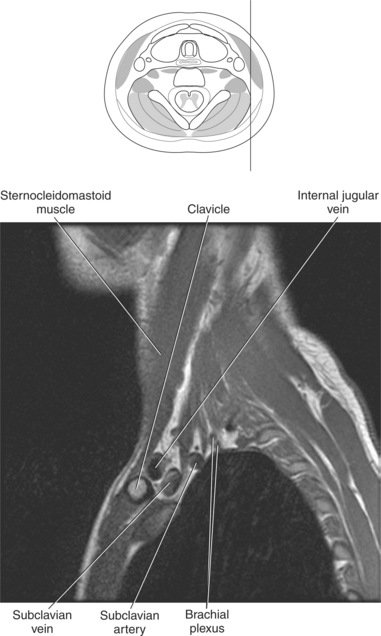
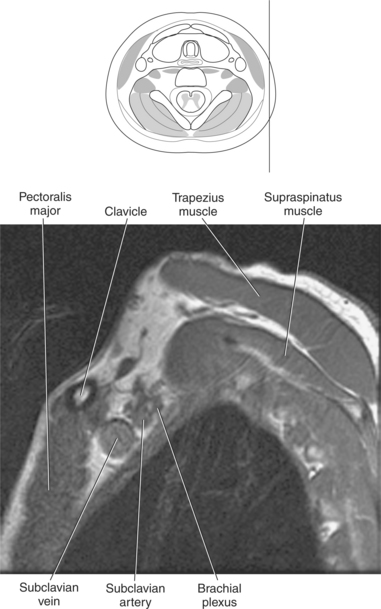
Brachial Plexus
The brachial plexus is a large, complex network of nerves arising from the five ventral rami of C5-C8 and T1. The roots of the brachial plexus emerge between the anterior and middle scalene muscles, where they continue laterally and inferiorly to divide into three cords just posterior to the clavicle (Figures 4.95 and 4.96). The cords extend through the axilla to form five terminal branches: the musculocutaneous, axil-lary, median, radial, and ulnar nerves. These nerves provide innervation for the muscles of the upper extremity and shoulder (Figures 4.95 through 4.104).
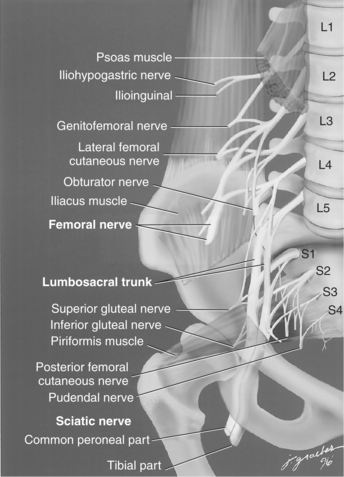
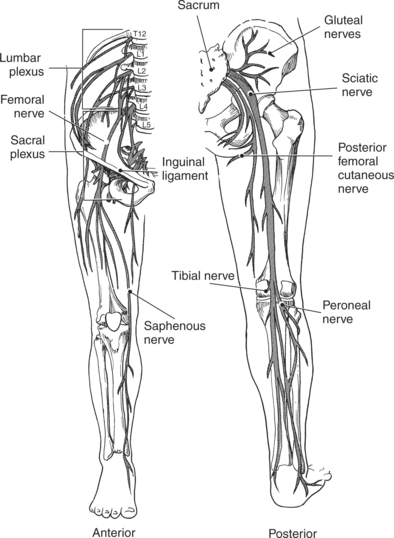
Lumbar Plexus
The lumbar plexus arises from the ventral rami of T12 and L1-L4. The lumbar plexus is situated on the posterior abdominal wall, between the psoas major muscle and the trans-verse processes of the lumbar vertebrae. In general, it serves the lower abdominopelvic region and anterior and medial muscles of the thigh. The femoral nerve is the largest branch of the lumbar plexus descending beneath the inguinal ligament. At the level of the lesser trochanter the femoral nerve divides into several branches, the largest being the saphenous nerve, which descends along the medial aspect of the leg to the ankle accompanied by the great saphenous vein. The saphenous nerve innervates the anterior lower leg, some of the ankle, and part of the foot (Figures 4.105 through 4.108).
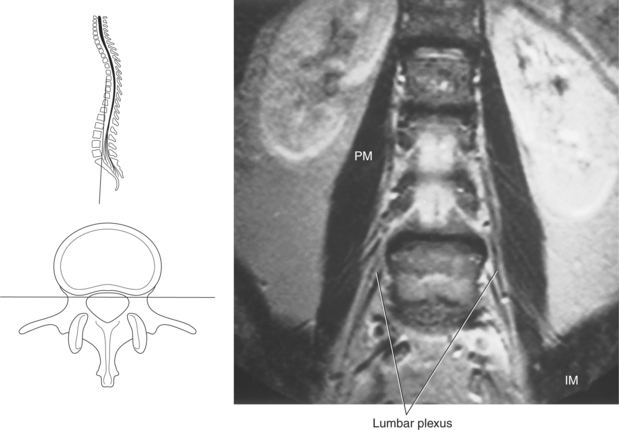
Figure 4.107 Coronal, T1-weighted MR scan of lumbar plexus.
Key: PM, Pectoralis major muscle; IM, iliacus muscle.
Sacral Plexus
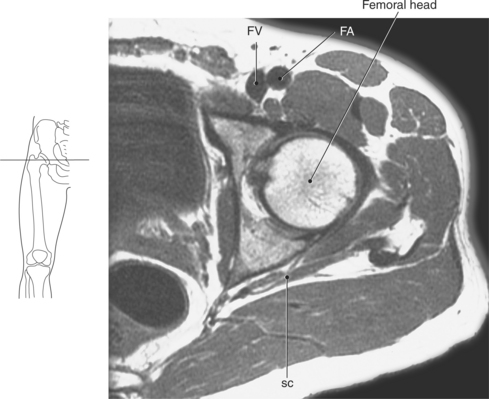
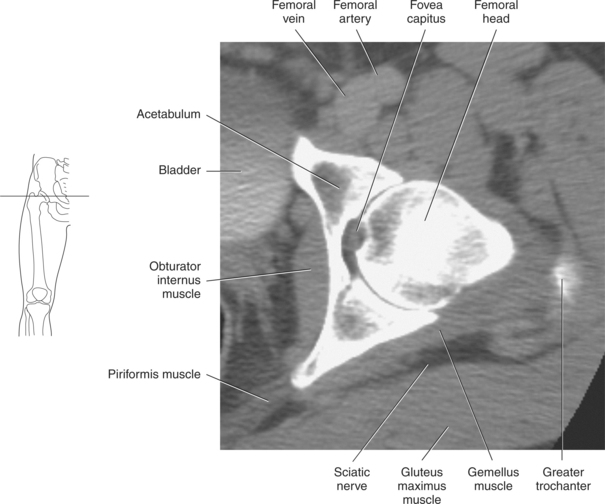
Arising from L4-L5 and S1-S4, the nerves of the sacral plexus innervate the buttock, posterior thigh, and feet. These nerves converge toward the inferior sacral foramina to unite into a large flattened band. Most of this nerve network continues into the thigh as the sciatic nerve, which is the largest nerve in the body. The sciatic nerve exits the pelvis through the greater sciatic foramen and continues to descend vertically along the posterior thigh. In its course it divides into the tibial and peroneal nerves, which innervate the posterior aspect of the lower extremity. The sacral plexus lies against the postero-lateral wall of the pelvis between the piriformis muscle and internal iliac vessels, just anterior to the sacroiliac joint (Figures 4.105, 4.106, and 4.109 through 4.113).
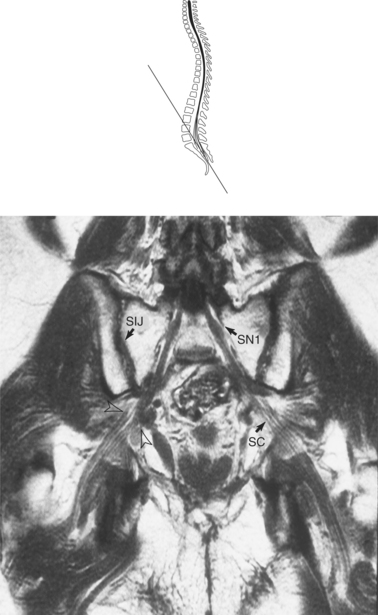
Figure 4.109 Coronal, T1-weighted MR scan of sacroiliac joints and sacral plexus.
Key: SIJ, Sacroiliac joint; SN1, S1 nerve; SC, sciatic nerve.
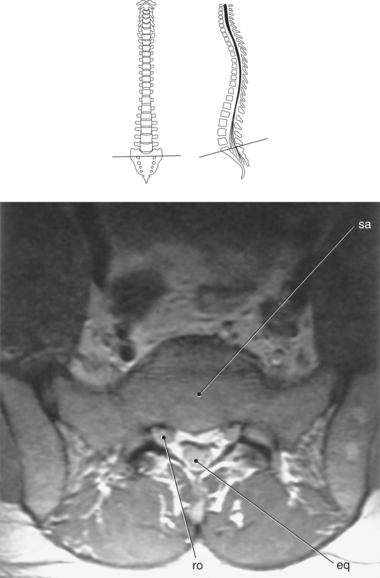
Figure 4.110 Axial, T1-weighted MR scan of sacrum and sacral plexus.
Key: sa, sacrum; eq, cauda equina; ro, root sleeve.
VASCULATURE
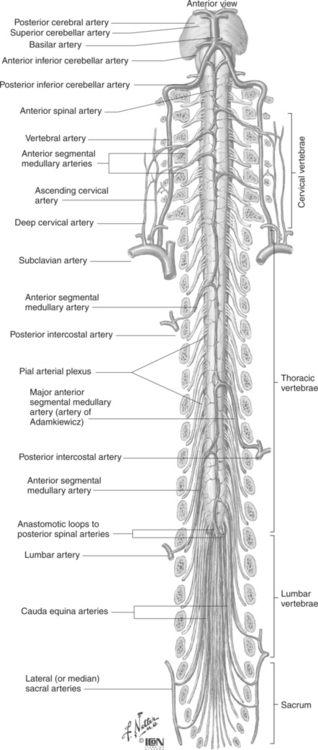
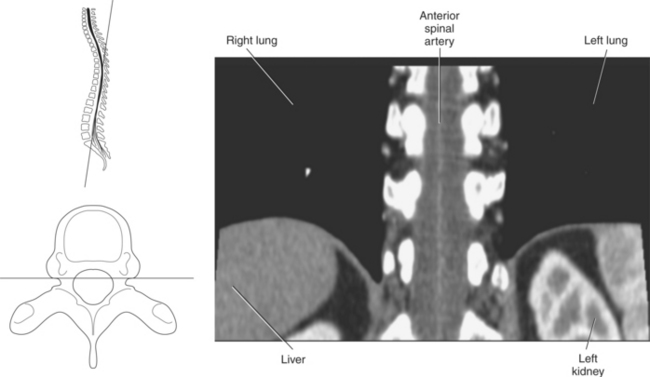
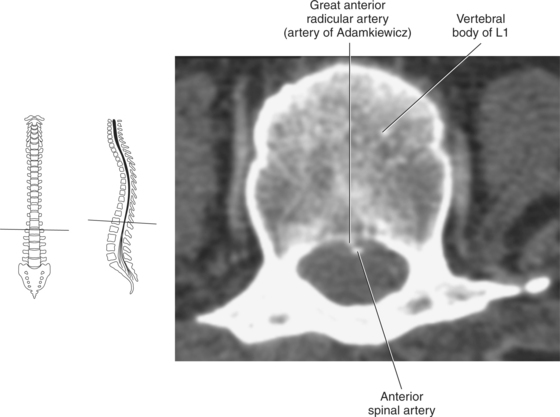
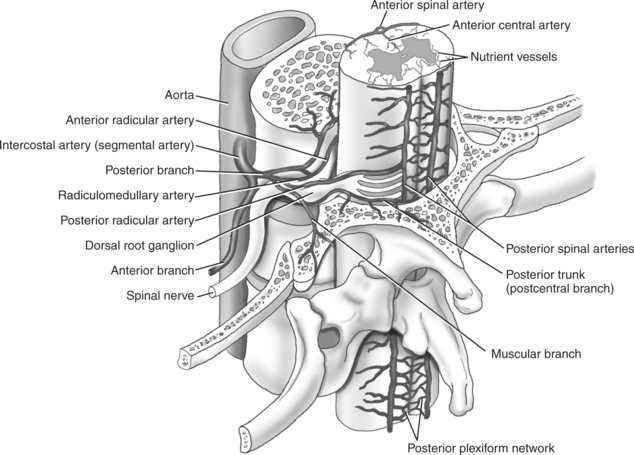
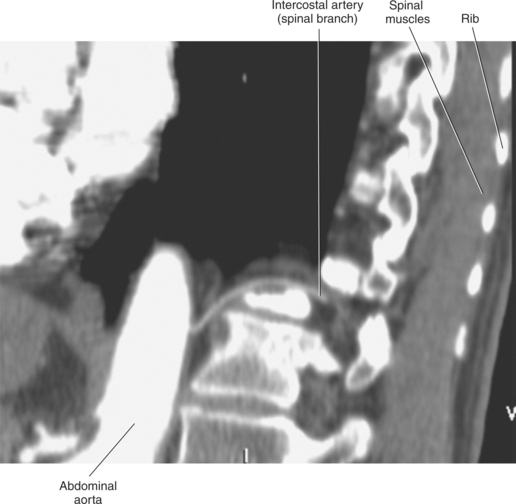
The spinal cord is supplied by a single anterior spinal artery, by a paired posterior spinal arteries, and from a series of spinal branches. The anterior spinal artery is formed, just caudal to the basilar artery, by the union of two small branches of the vertebral arteries (Figure 4.114). It runs the entire length of the spinal cord in the anterior median fissure and supplies the anterior two thirds of the spinal cord (Figures 4.115 and 4.116). Although the anterior spinal artery is quite small in diameter, it is widest in the cervical and lumbar enlargements and is much reduced in the thoracic region. The posterior spinal arteries arise as small branches of either the vertebral or the posterior inferior cerebellar arteries and descend along the dorsal surface of the spinal cord (Figure 4.117). The posterior one third of the spinal cord is supplied by the posterior spinal arteries. There exist frequent anastomoses joining the two posterior spinal arteries with each other and with the anterior spinal artery. The spinal branches arise at various levels from the vertebral, deep cervical, posterior intercostal, lumbar, and lateral sacral arteries. The spinal branches enter the spinal canal through the intervertebral foramen (Figures 4.117 and 4.118). After giving off an anterior and posterior branch to the wall of the vertebral canal, the spinal branch divides into anterior and posterior radicular arteries that pass along the ventral and dorsal roots into the spinal cord (Figure 4.114). The anterior radicular arteries contribute blood to the anterior spinal artery, and the posterior radicular arteries contribute blood to the posterior spinal arteries. The largest of the radi-cular arteries is the great anterior radicular artery (artery of Adamkiewicz), which arises in the lower thoracic and upper lumbar region typically between T12 and L3 (Figures 4.114 and 4.116). This vessel makes a major contribution to the anterior spinal artery and provides the main blood supply to the inferior two thirds of the spinal cord.
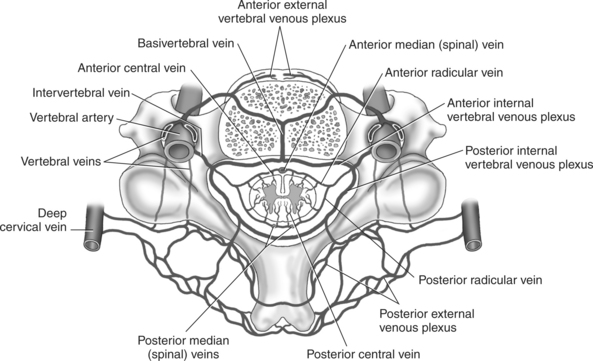
Spinal Veins
The veins that drain the spinal cord follow the same segmental organization as their arterial counterparts. The central gray matter of the cord is drained by the anterior and posterior central veins located in the anterior median fissure and posterior sulcus, respectively. The outer white matter is drained by small radial veins that encircle the spinal cord within the pia mater. The venous blood collected by these tiny veins drains into the anterior and posterior median (spinal) veins created by the longitudinal venous channels within the pia mater on the anterior and posterior surfaces of the spinal cord (Figure 4.119). The anterior median vein parallels the anterior spinal artery, and the posterior median vein typically presents as the largest vascular structure on the posterior surface of the spinal cord. The anterior and posterior median veins drain into the anterior and posterior radicular veins that parallel the ventral and dorsal nerve roots and even-tually empty into the intervertebral veins that accompany the spinal nerves through the intervertebral foramina.
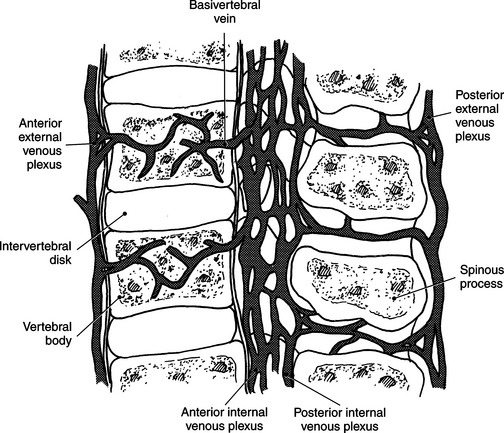
Veins of the Vertebral Column
The veins of the vertebral column form an extensive network of internal and external venous plexuses, named according to their corre-sponding location to the vertebral column (Figures 4.119 and 4.120). The internal venous plexuses lie within the vertebral canal in the epidural space and are divided into anterior and posterior internal plexuses. The anterior internal venous plexuses are found on either side of the anterior longitudinal ligament, and the single posterior internal venous plexus lies anterior to the ligamentum flavum.
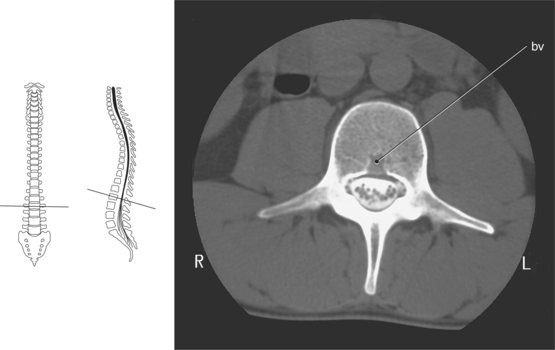
The valveless external venous plexuses communicate freely with the vertebral veins and intracranial venous sinuses and are located at the outer surfaces of the vertebral column. They can be divided into the anterior and posterior external plexuses. The anterior external plexuses run directly in front of the vertebral bodies and the posterior external plexuses run along the posterior aspect of the vertebral arches (Figure 4.121). The anterior sections of the internal and external plexuses com-municate via a network of veins that drain the vertebral bodies called the basivertebral veins. The basivertebral veins emerge from the posterior surfaces of the vertebral bodies, creating large channels that join with the anterior internal venous plexuses (Figure 4.122). The internal and external venous plexuses, along with the radicular veins, drain into the inter-vertebral veins, ending in the vertebral, intercostal, lumbar, and sacral veins.
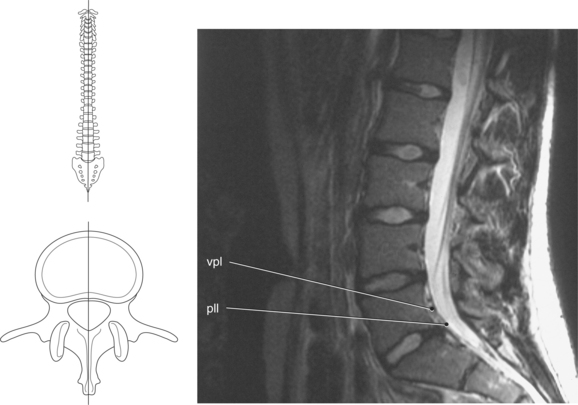
Figure 4.121 Sagittal, T2-weighted MR scan of lumbar spine showing internal venous plexus.
Key: vpl, Venous plexus; pll, posterior longitudinal ligament.
Agur, AM. Grant’s atlas of anatomy. Baltimore: Williams & Wilkins, 1996.
Ballinger, PW. Merrill’s atlas of radiographic positions and radiologic procedures, ed 10. St. Louis: Mosby, 2003.
English, AW. Wolf-Heidegger’s atlas of human anatomy, ed 5. Basel, Switzerland: Karger, 2000.
Frick, H, Leonhardt, H, Starck, D, et al. Human anatomy 1. New York: Thieme Medical Publishers, 1991.
Frick, H, Leonhardt, H, Starck, D, et al. Human anatomy 2. New York: Thieme Medical Publishers, 1991.
Gray, H. Gray’s anatomy, ed 15. New York: Barnes & Noble, 1995.
Harnsberger, HR. Handbook of head and neck imaging, ed 2. St. Louis: Mosby, 1995.
Hayman, LA. Clinical brain imaging: normal structure and functional anatomy. St. Louis: Mosby, 1992.
Hendelman, WJ. Student’s atlas of neuroanatomy. Philadelphia: Saunders, 1994.
Jacob, S. Atlas of human anatomy. Philadelphia: Churchill Livingstone, 2002.
Larsen, WJ. Anatomy: Development function clinical correlations. Philadelphia: Saunders, 2002.
Leblanc, A. Atlas of hearing and balance organs. New York: Springer-Verlag, 1999.
Mancuso, AA. Workbook for MRI and CT of the head and neck, ed 2. Baltimore: Williams & Wilkins, 1989.
Martini, FH. Fundamentals of anatomy and physiology, ed 3. Englewood Cliffs, NJ: Prentice-Hall, 1995.
Mosby’s medical, nursing, and allied health dictionary, ed 6. Mosby: St. Louis, 2002.
Netter, FH. The Ciba collection: nervous system. Summit, NJ: Ciba Pharmaceutical Products, 1957.
Orrison, WW, Lewine, JD, Sanders, JA, et al. Functional brain imaging. St. Louis: Mosby, 1995.
Osborn, AG. Diagnostic neuroradiology. St. Louis: Mosby, 1994.
Osborn, AG, Tong, KA. Handbook of neuroradiology: brain and skull, ed 2. St. Louis: Mosby, 1996.
Palastanga, N, Field, D, Soames, R, et al. Anatomy and human movement, ed 4. Philadelphia: Butterworth-Heinemann, 2002.
Standring, S. Gray’s anatomy, ed 39. Philadelphia: Churchill Livingstone, 2005.
Som, PM, Curtin, HD. Head and neck imaging, ed 3. St. Louis: Mosby, 1996.
Stark, DD, Bradley, WG. Magnetic resonance imaging, ed 3. St. Louis: Mosby, 1999.
Taveras, JM. Neuroradiology, ed 3. Baltimore: Williams & Wilkins, 1996.
Valvassori, GE, Mahmood, FM, Carter, BL. Imaging of the head and neck. New York: Thieme Medical Publishers, 1995.
Warner, JJ. Atlas of neuroanatomy: with systems organization and case correlations. Philadelphia: Butterworth-Heinemann, 2001.