Abdomen
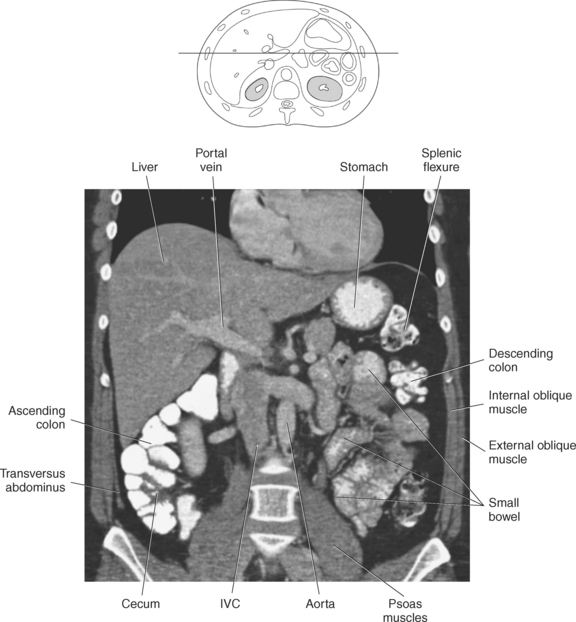
The abdominal cavity houses many critical structures that have a large array of functions. It is for this reason that cross-section imaging of the abdomen is so essential in visualizing these various organs and body systems (Figure 7.1). This chapter demonstrates cross-section anatomy of the following structures:
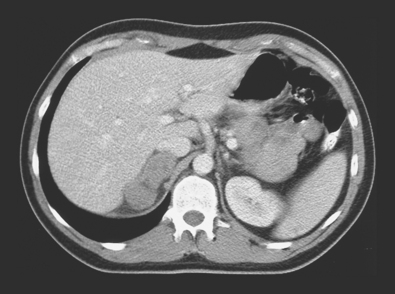
Figure 7.1 Axial CT scan of abdomen with right adrenal mass associated with an abnormal retrocaval lymph node.
ABDOMINAL CAVITY
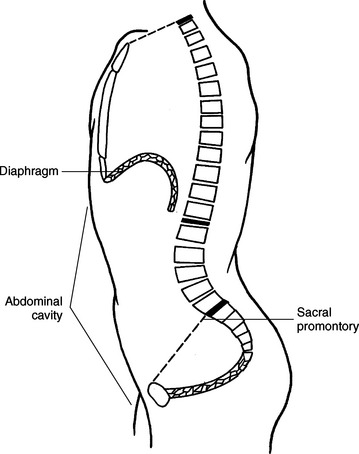
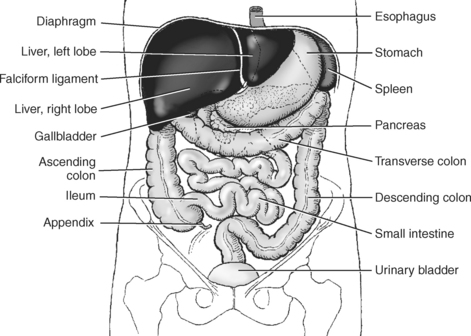
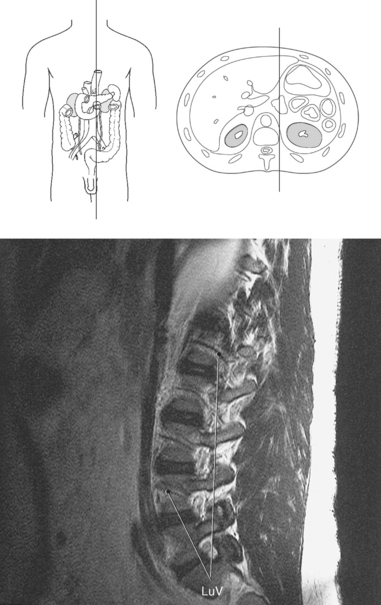
The abdominal cavity is the region located between the diaphragm and sacral promontory (Figure 7.2). The abdominal and pelvic cavities are commonly divided into four quadrants or nine distinct regions (see Chapter 1). Contents of the abdominal cavity include the liver, gallbladder and biliary system, pancreas, spleen, adrenal glands, kidneys, ureters, stomach, intestines, and vascular structures.
Peritoneum
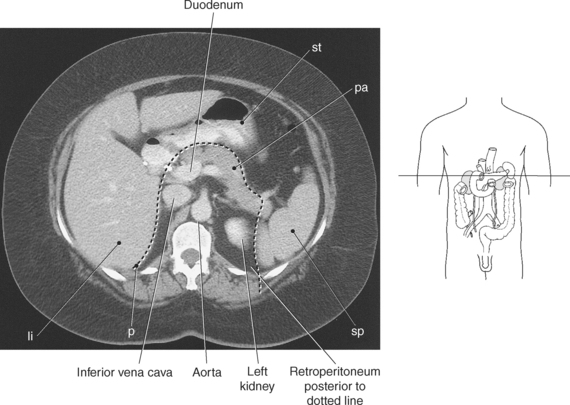
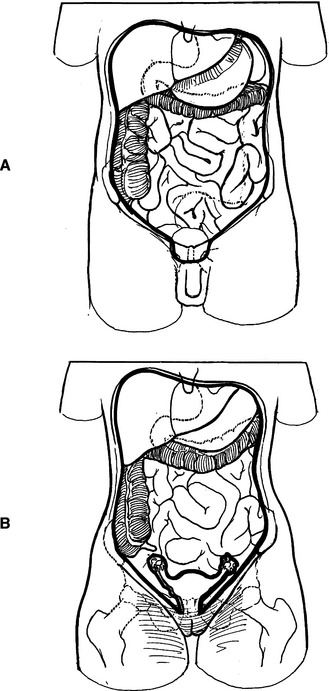
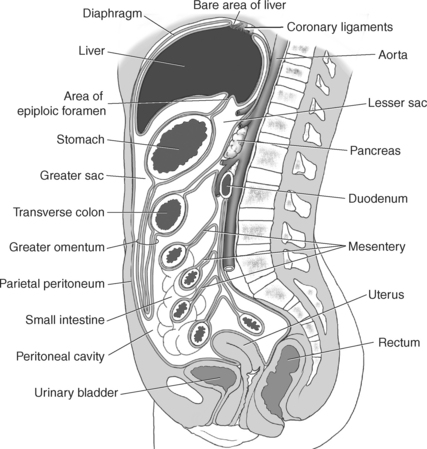
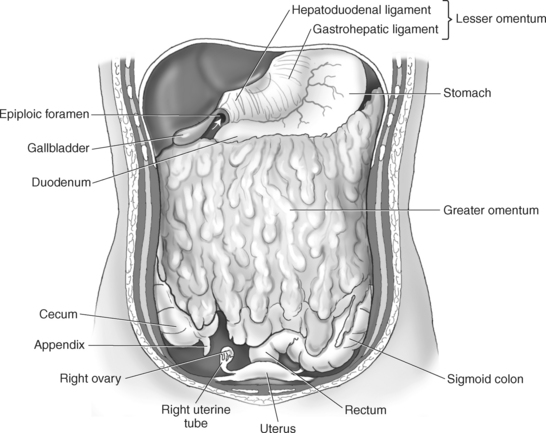
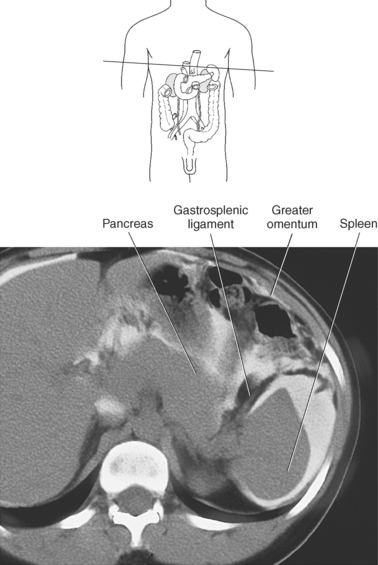
The walls of the abdominal cavity are lined by a thin serous membrane called the peritoneum. This membrane is divided into two layers: the parietal peritoneum, which lines the abdominal walls, and the visceral peritoneum, which covers the organs (Figures 7.3). The two layers of peritoneum are separated by a film of serous fluid for lubrication to allow organs to move against each other without friction. The peritoneum forms a cavity that encloses the following organs of the abdomen: liver (except for the bare area), gallbladder, spleen, stomach, ovaries, and majority of intestines (Figures 7.4 and 7.5). In males, the peritoneal cavity is a closed cavity, but in females it communicates with the exterior through the uterine tubes, uterus, and vagina (Figure 7.6, A and B). The peritoneal cavity consists of the greater sac and lesser sac (omental bursae). The greater sac is located between the inner surface of the anterior abdominal wall and the outer surface of the abdominal viscera. It is bounded between the parietal and visceral peritoneum. The greater sac communicates with the lesser sac through the epiploic foramen (of Winslow). The lesser sac is located primarily between the posterior surface of the stomach and the posterior abdominal wall (Figures 7.3 and 7.7 through 7.9)
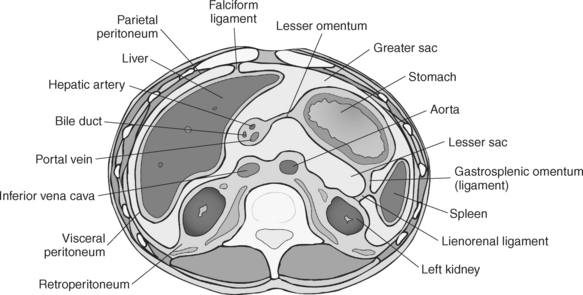
Figure 7.3 Axial view of abdomen with greater and lesser sac, falciform, gastrosplenic, and lienorenal ligaments.
Key: li, Liver; p, peritoneum; pa, pancreas; st, stomach; sp, spleen.
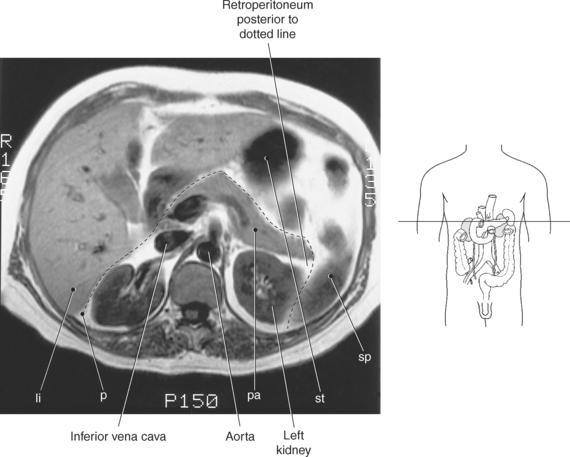
Figure 7.4 Axial, T1-weighted MR scan of peritoneal and retroperitoneal structures (separated by dotted line).
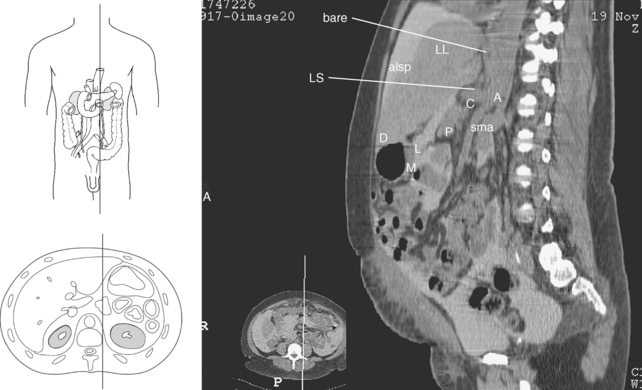
Figure 7.8 Sagittal CT reformat of abdomen with lesser sac and peritoneal spaces.
Key: bare, Bare area of liver; LS, lesser sac; alsp, anterior left subphrenic space; LL, liver; D, duodenum; L, lesser sac; M, mesocolon; P, pancreas; sma, superior mesenteric artery; C, celiac artery; A, aorta.
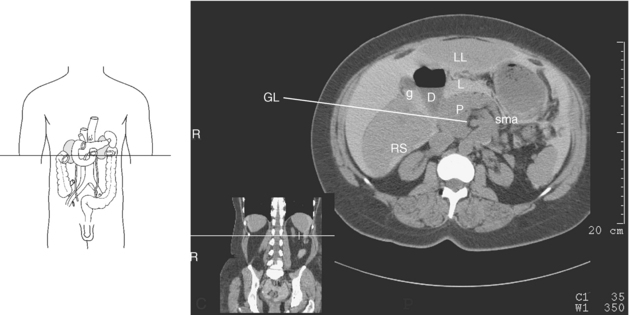
Figure 7.9 Axial CT scan of abdomen and peritoneal spaces.
Key: GL, gastrohepatic ligament; LL, liver; L, lesser sac; g, gallbladder; D, duodenum; P, pancreas; sma, superior mesenteric artery; RS, right subhepatic space.
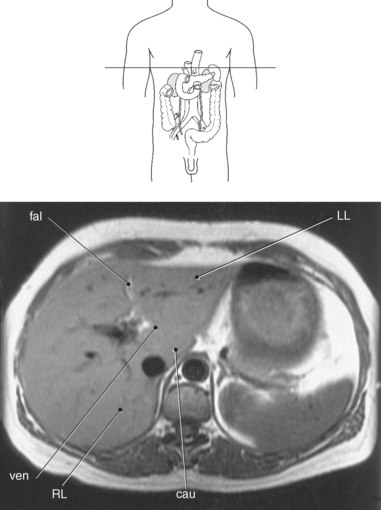
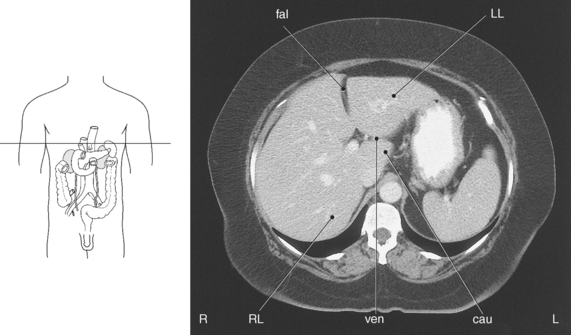
Numerous folds of peritoneum extend between organs, serving to hold them in position and at the same time enclose the vessels and nerves proceeding to each part. These folds or double layers of peritoneum are termed mesentery, omenta, and peritoneal ligaments. The mesentery is a double layer of peritoneum, which encloses the intestine and attaches it to the abdominal wall. An omentum is a mesentery or double layer of peritoneum that is attached to the stomach. The normal omentum is usually imperceptible on routine scans, visible only when fluid is present. The greater omentum is a fat-laden fold of peritoneum that drapes down from the greater curvature of the stomach and connects the stomach with the spleen, and transverse colon, whereas the lesser omentum attaches the duodenum and lesser curvature of the stomach to the liver (Figures 7.10 through 7.13). Numerous peritoneal ligaments serve to connect an organ with another organ or abdominal wall. These peritoneal ligaments are not ligaments in the classic sense but are distinct regions of mesentery connecting the structures for which they are named. Three regions of the greater omentum that are characterized as peritoneal ligaments include gastrocolic, gastrosplenic, and gastrophrenic. These ligaments attach the greater omentum to the transverse colon, hilum of the spleen and greater curvature and fundus of the stomach, diaphragm, and esophagus (Figures 7.3, 7.11, and 7.12). Ligaments of the lesser omentum include the hepatogastric and hepatoduodenal, which serve to connect the stomach and duodenum to the liver. Ligaments associated specifically with the liver are the round ligament (ligamentum teres), which represents the obliterated umbilical vein and attaches the internal surface of the umbilicus within the free inferior margin of the falciform ligament. The falciform ligament extends from the liver to the anterior abdominal wall and diaphragm and forms a plane that divides the liver anatomically into right and left lobes (Figures 7.14 and 7.15). The coronary ligaments surround the superior pole of the liver and attach the liver to the diaphragm, forming the margins of the bare area (Figures 7.7, 7.8, and 7.16). Additional peritoneal ligaments are described in Table 7.1.
TABLE 7-1
| LIGAMENTS | LOCATION |
| Gastrocolic ligaments | Apron portion of the greater omentum attached to the transverse colon |
| Gastrosplenic ligaments (gastrolienal ligament) | The left portion of the greater omentum that connects the hilum of the spleen to the greater curvature and fundus of the stomach |
| Splenorenal (lienorenal) igament | Connecting the spleen and kidneyl |
| Gastrophrenic ligament | Superior portion of greater omentum attached to the diaphragm and posterior aspect of the fundus and esophagus |
| Hepatorenal ligament | Connects the liver with the kidney |
| Hepatoesophageal ligament | Connects the liver with the esophagus |
| Hepatogastric ligament | Connects the liver with the lesser curvature of the stomach |
| Hepatoduodenal ligament | Connects the superior region of the duodenum to the liver |
| Falciform ligament | Extends from the liver to the anterior abdominal wall and diaphragm |
| Round ligament (ligamentum teres) | Remnant of the left umbilical vein, lying in the free edge of the falciform ligament |
| Coronary ligaments (superior and inferior) | Reflections of the peritoneum that surround the bare area of the liver |
| Triangular (left and right) | Where the layers of the coronary ligament meet to the left and right, respectively |
| Phrenocolic ligament | Attaches the left flexure of the colon and the diaphragm. |
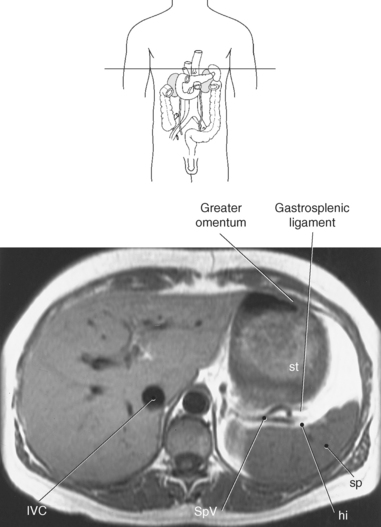
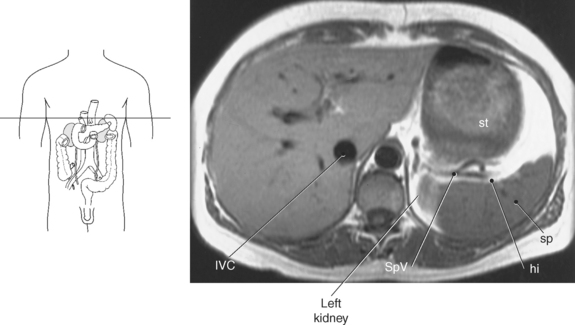
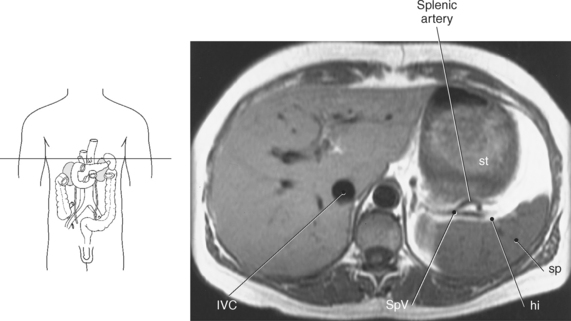
Figure 7.11 Axial, T1-weighted MR scan of abdomen with greater omentum and gastrosplenic ligament.
Key: IVC, inferior vena cava; SpV, splenic vein; st, stomach; sp, spleen; hi, hilum.
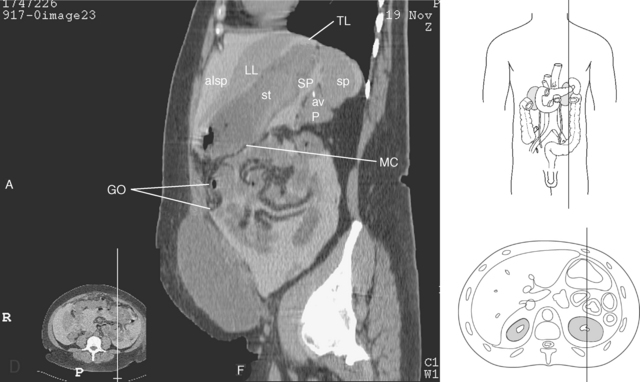
Figure 7.13 Sagittal CT reformat of abdomen with greater omentum and peritoneal spaces.
Key: GO, greater omentum; TL, triangular ligaments; alsp, anterior left subphrenic space; SP, splenic recess; av, splenic artery and vein; MC, mesocolon.
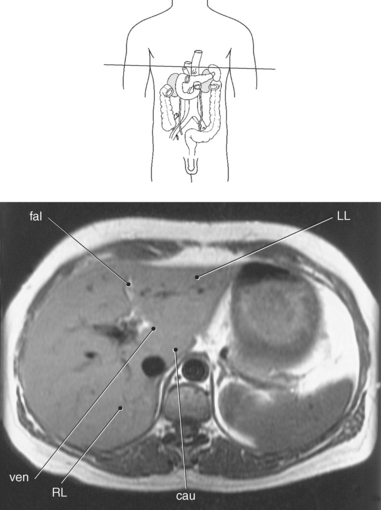
Figure 7.14 Axial, T1-weighted MR scan of abdomen with falciform ligament.
Key: fal, Falciform ligament; LL, left lobe of liver; ven, ligamentum venosum; RL, right lobe of liver; cau, caudate lobe of liver.
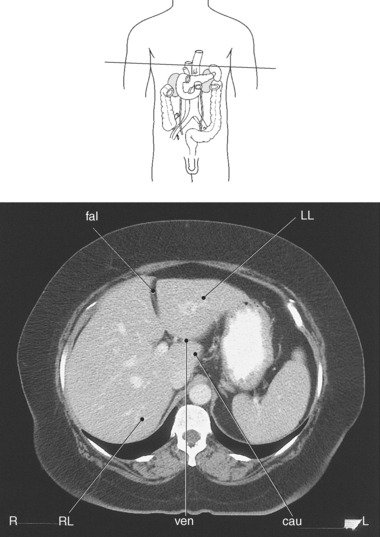
Figure 7.15 Axial CT scan of abdomen with falciform ligament.
Key: fal, Falciform ligament; LL, left lobe of liver; ven, ligamentum venosum; RL, right lobe of liver; cau, caudate lobe of liver.
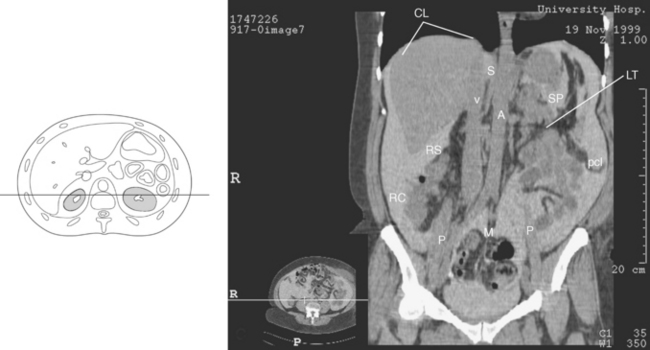
Figure 7.16 Coronal CT reformat of liver and coronary ligaments.
KEY: CL, coronary ligaments; S, superior recess of the lesser sac; v, vena cava; A, aorta; SP, splenic recess; RS, right subhepatic space; LT, ligament of Treitz; pcl, phrenicocolic ligament; RC, paracolic space; P, psoas muscles; M, mesentery of small bowel.
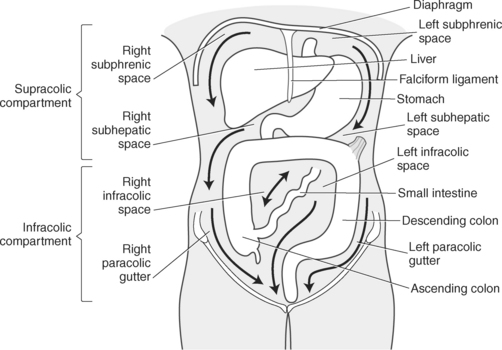
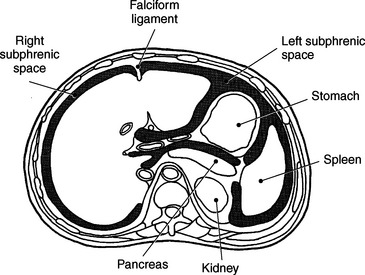
Peritoneal Spaces
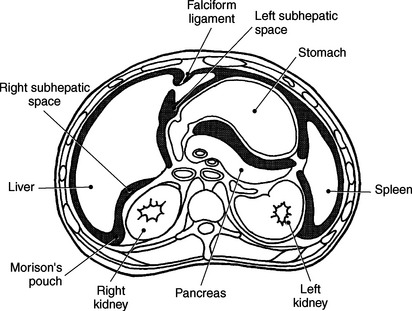
The peritoneal cavity contains potential spaces resulting from folds of peritoneum that extend from the viscera to the abdominal wall. These spaces can be divided into the supracolic and infracolic compartments (Figure 7.17). The supracolic compartment is located above the transverse colon and contains the right and left subphrenic spaces and right and left subhepatic spaces. The subphrenic spaces are located between the diaphragm and the anterior portion of the liver. They are divided into right and left compartments by the falciform ligament (Figures 7.18 and 7.19). The subhepatic spaces are located posterior and inferior between the liver and the abdominal viscera. The right subhepatic space, located between the liver and kidney, contains Morison’s pouch, which is the deepest point of the abdominal cavity in a supine patient and a common site for collection of fluid (Figures 7.20 and 7.21).
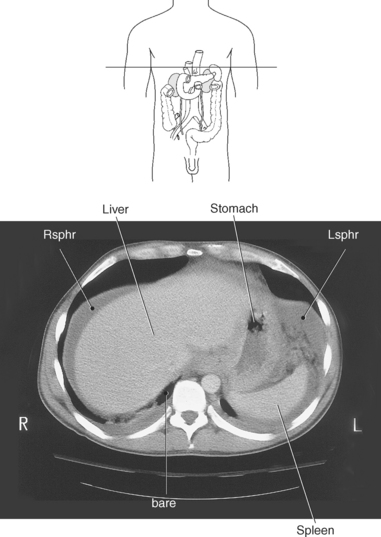
Figure 7.19 Axial CT scan of abdomen with subphrenic spaces.
Key: Rsphr, Right subphrenic compartment; Lsphr, left subphrenic compartment; bare, bare area of liver.
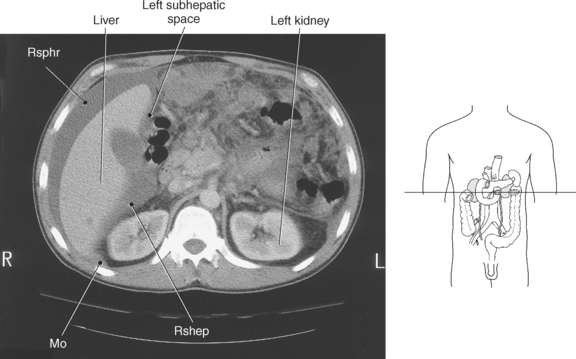
Figure 7.21 Axial CT scan of abdomen with subhepatic spaces and Morison’s pouch.
Key: Rsphr, Right subphrenic compartment; Mo, Morison’s pouch; Rshep, right subhepatic space.
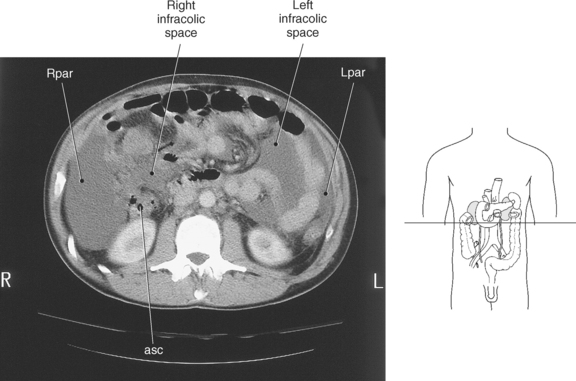
Below the transverse colon is the infracolic compartment, which consists of the right and left infracolic spaces and the paracolic gutters. The right and left infracolic spaces are divided by the mesentery of the small intestine. The right and left paracolic gutters are troughlike spaces located lateral to the ascending and descending colon (Figures 7.17 and 7.22 and Table 7.2). The deeper right gutter is a common site for free fluid collections.
TABLE 7-2
Peritoneal and Retroperitoneal Spaces
| SPACE | LOCATION |
| Peritoneal Spaces | |
| Supracolic Compartment | Above Transverse Colon |
| Subphrenic space | Between diaphragm and anterior liver |
| Right | Right and left spaces divided by falciform |
| Left | ligament |
| Subhepatic space | Posterior and inferior to liver |
| Right | Between right lobe of liver and kidney; contains Morison’s pouch |
| Left | Between left lobe of liver and kidney; includes lesser omentum |
| Infracolic Compartment | Below Transverse Colon |
| Infracolic spaces | |
| Right and left | Divided by mesentery of small intestine |
| Paracolic gutters | |
| Right | Between ascending colon and right abdominal wall |
| Left | Between descending colon and left abdominal wall |
| Retroperitoneal Spaces | |
| Pararenal Spaces | |
| Anterior | Between renal (Gerota’s) fascia and posterior surface of peritoneum |
| Posterior | Between renal (Gerota’s) fascia and muscles of posterior abdominal wall |
| Perirenal Space | |
| Right Left |
Around kidney and adrenal glands; completely enclosed by renal (Gerota’s) fascia |
Retroperitoneum
Structures located posterior to the peritoneum, yet lined by it anteriorly, are considered to be in the retroperitoneum and include the kidneys, ureters, adrenal glands, pancreas, duodenum, aorta, inferior vena cava, bladder, uterus, and prostate gland. In addition, the ascending and descending colon and most of the duodenum are situated in the retroperitoneum (Figures 7.3 through 7.5)
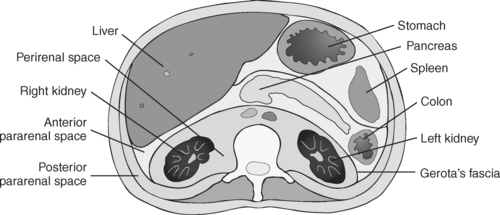
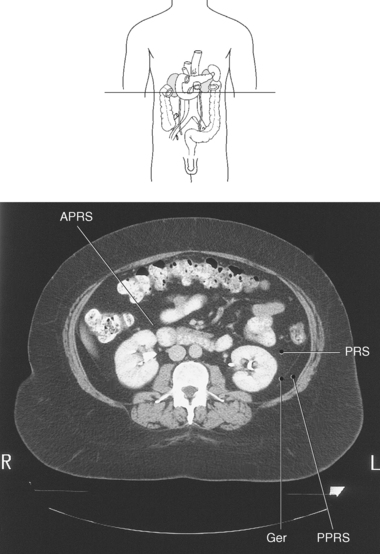
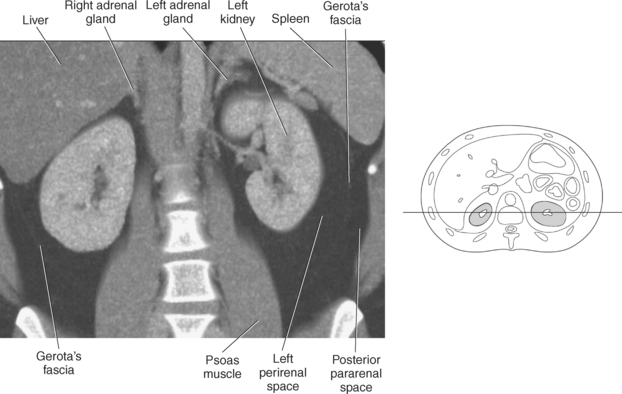
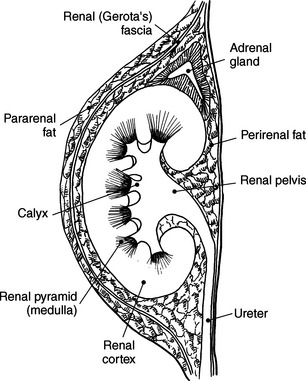
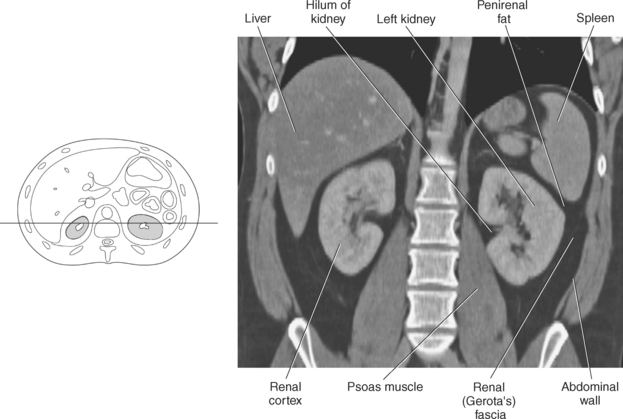
Retroperitoneal Spaces
The retroperitoneum can be divided into compartments or spaces that include the anterior and posterior pararenal spaces and left and right perirenal spaces (Figure 7.23). The anterior pararenal space is located between the anterior surface of the renal fascia (Gerota’s fascia) and the posterior position of the peritoneum. It contains the retroperitoneal portions of the ascending and descending colon, the pancreas, and the duodenum. The posterior pararenal space is located between the posterior renal fascia and the muscles of the posterior abdominal wall. There are no solid organs located in this space, just fat and vessels (Figures 7.24 and 7.25). The left and right perirenal spaces are the areas located directly around the kidneys and are completely enclosed by renal fascia. The perirenal spaces contain the kidneys, adrenal glands, lymph nodes, blood vessels, and perirenal fat. The perirenal fat separates the adrenal glands from the kidneys and provides cushioning for the kidney (Figure 7.26 and Table 7.2).
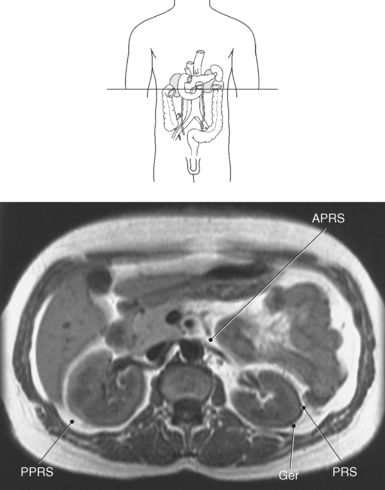
Figure 7.24 Axial, T1-weighted MR scan of abdomen with kidneys and pararenal spaces.
Key: APRS, Anterior pararenal space; PPRS, posterior pararenal space; Ger, Gerota’s fascia; PRS, perirenal space.
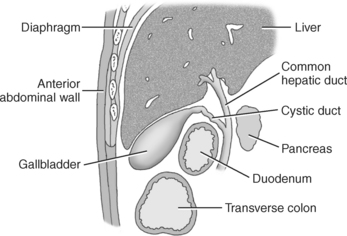
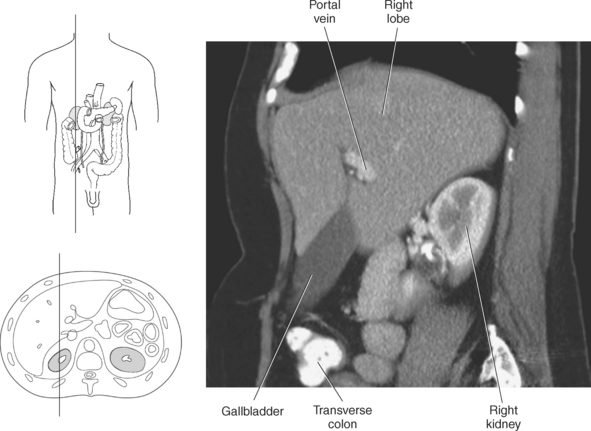
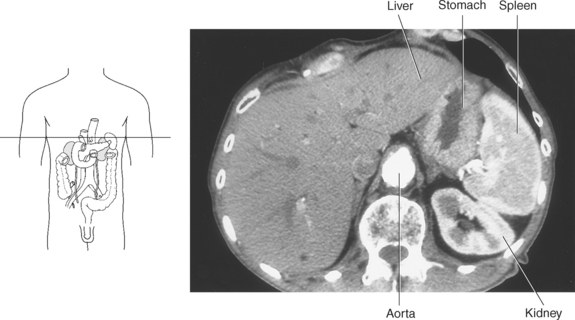
LIVER
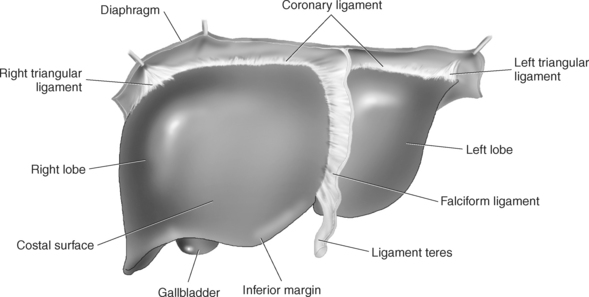
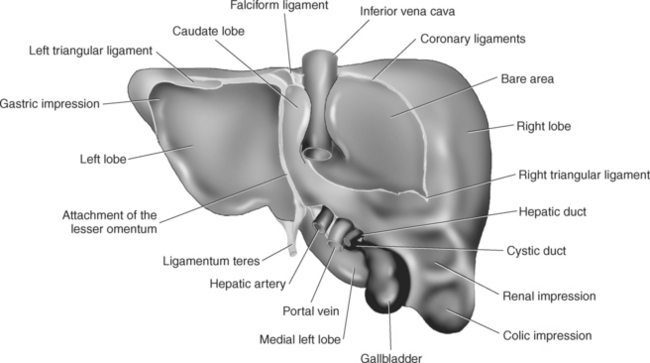
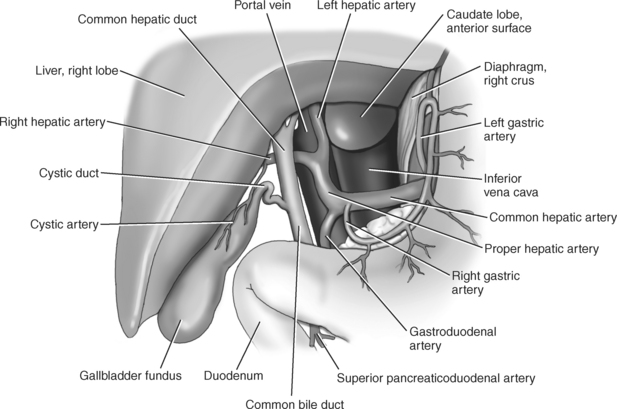
The liver is a large, complex organ with numerous functions that include metabolic regulation, hematologic regulation, and bile production. It is the largest organ of the abdomen, occupying a major portion of the right hypochondriac and epigastric regions, sometimes extending into the left hypochondriac and umbilical regions. The liver is bordered superiorly, laterally, and anteriorly by the right hemidiaphragm (Figures 7.27 and 7.28). The medial surface is bordered by the stomach, duodenum, and transverse colon; the inferior surface is bordered by the hepatic flexure of the colon; and the posterior surface is bordered by the right kidney (Figure 7.29). The liver is surrounded by a strong connective tissue capsule (Glisson’s capsule) that gives shape and stability to the soft hepatic tissue. It is also entirely covered by peritoneum except for the gallbladder fossa, the surface apposed to the inferior vena cava (IVC), and the bare area (liver surface between the superior and inferior coronary ligaments) (Figures 7.7, 7.8, 7.19, and 7.28).
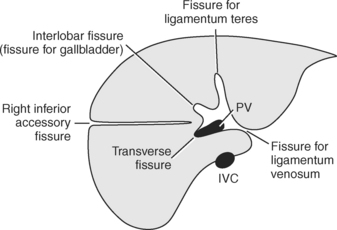
Within the liver there are several main grooves or fissures that are useful in defining the lobes and boundaries of the hepatic segments. The umbilical fissure (fissure for ligamentum teres) divides the left hepatic lobe into medial and lateral segments. The fissure for the ligamentum venosum separates the caudate lobe from the left lobe, and the transverse fissure (portal) contains the horizontal portions of the right and left portal veins. The interlobar fissure (main lobar fissure), also called the fissure for the gallbladder, divides the right from left lobes of the liver (Figure 7.30). The hilum of the liver, the porta hepatis, is located on the inferomedial border of the liver. It is the central location for vessels to enter and exit the liver (Figure 7.28).
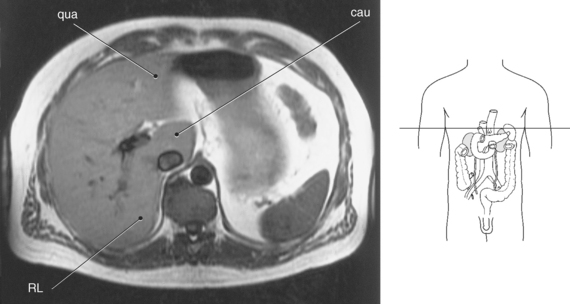
Surface Anatomy
The liver can be divided into lobes according to surface anatomy or into segments according to vascular supply. The four lobes commonly used for reference based on surface anatomy are the left, right, caudate, and quadrate. The left lobe is the most anterior of the liver lobes, extending across the midline. It is separated from the right lobe by the interlobar fissure, an imaginary line drawn through the gallbladder fossa and the middle hepatic vein to the inferior vena cava. The smallest lobe is the caudate lobe, which is located on the inferior and posterior liver surface, sandwiched between the IVC and the ligamentum venosum. The quadrate lobe is located on the anteroinferior surface of the left lobe between the gallbladder and the ligamentum teres. The round, cordlike, ligamentum teres is a remnant of the fetal umbilical vein and runs along the free edge of the falciform ligament. The falciform ligament provides the structural support that attaches the upper surfaces of the liver to the diaphragm and upper abdominal wall (Figures 7.27, 7.28, 7.29, and 7.31 through 7.34).
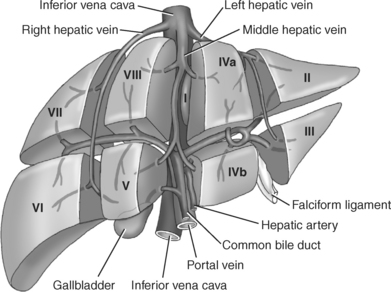
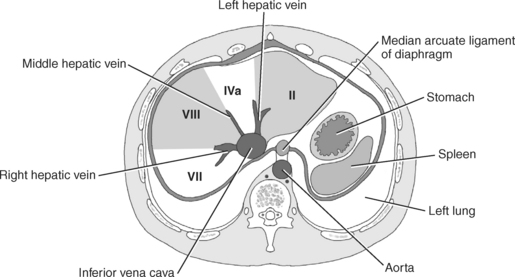
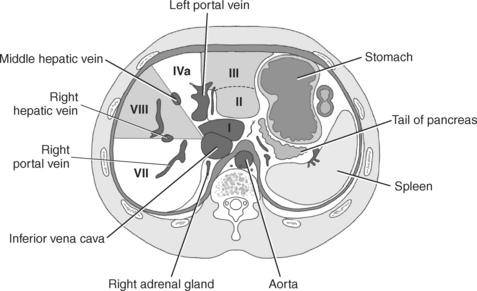
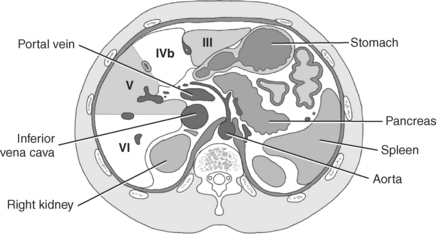
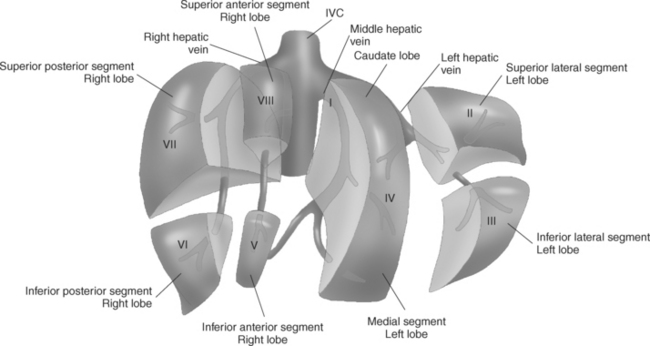
Segmental Anatomy
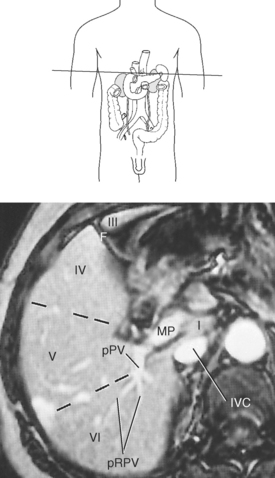
Current practice favors dividing the liver into eight segments, according to its vascular supply, which can aid in surgical resection. According to the French anatomist Couinaud, the liver can be divided into segments based on the branching of the portal and hepatic veins. The three main hepatic veins divide the liver longitudinally into four sections (Figure 7.35). The middle hepatic vein divides the liver into right and left lobes. The right lobe is divided into medial and lateral sectors by the right hepatic vein, and the left lobe is divided into medial and lateral sectors by the left hepatic vein. Each section is then subdivided transversely by the right and left portal veins, creating nine segments numbered counterclockwise from the IVC. Each segment can be considered functionally independent with its own hepatic artery, portal vein, and bile duct and drained by a branch of the hepatic vein (Figures 7.36 through 7.47).
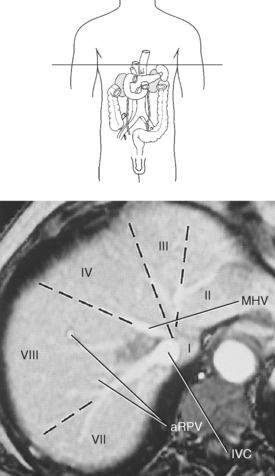
Figure 7.37 Axial, T1-weighted MR scan of liver segments.
Key: MHV, Middle hepatic vein; IVC, inferior vena cava; aRPV, tributaries of anterior branch of right portal vein.
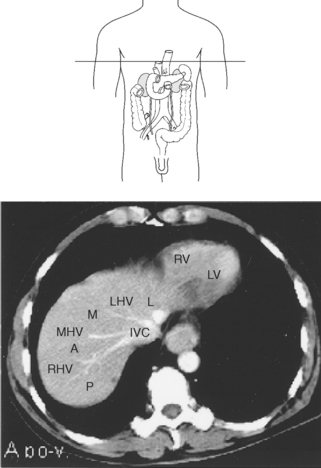
Figure 7.38 Axial CT scan of liver segments.
Axial, T1-weighted MR scan of liver segments.
Key: MHV, Middle hepatic vein; IVC, inferior vena cava; RV, right ventricle of heart; LV, left ventricle of heart; L, lateral segment of left lobe; LHV, left hepatic vein; M, medial segment of left lobe; MHV, middle hepatic vein; A, anterior segment of right lobe; RHV, right hepatic vein; P, posterior segment of right lobe; IVC, inferior vena cava.
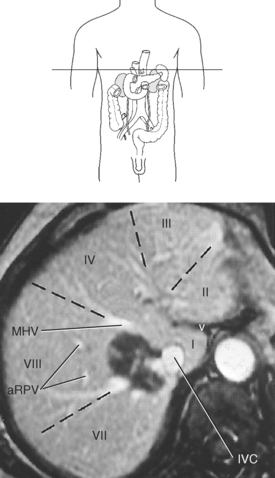
Figure 7.40 Axial, T1-weighted MR scan of liver segments.
Key: v, Ligamentum venosum; MHV, middle hepatic vein; IVC, inferior vena cava; aRPV, anterior branches of right portal vein.
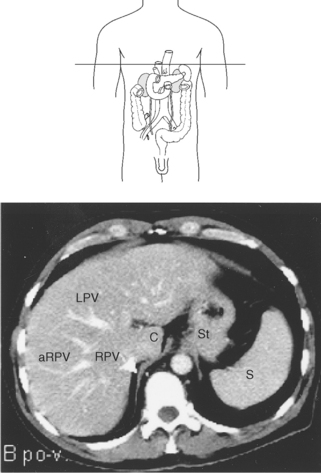
Figure 7.41 Axial CT scan of liver segments.
Key: LPV, left portal vein; aRPV, anterior branches of right portal vein; RPV, right portal vein; C, caudate lobe; St, stomach; S, spleen.
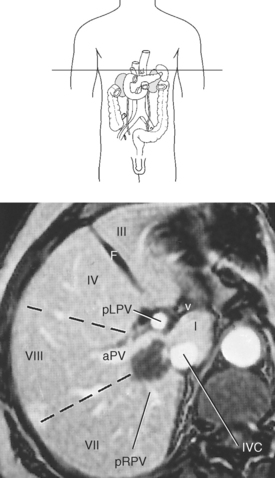
Figure 7.43 Axial, T1-weighted MR scan of liver segments.
KEY: F, Falciform ligament; pLPV, proximal left portal vein; IVC, inferior vena cava; pRPV, posterior branch of right portal vein; v, ligamentum venosum; pRPV, posterior branches of right portal vein.
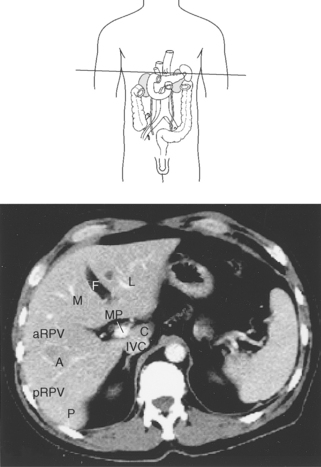
Figure 7.44 Axial CT scan of liver segments.
KEY: F, Falciform ligament; A, anterior segment of right lobe; IVC, inferior vena cava; pRPV, posterior branch of right portal vein; M, medial segment of left lobe; L, lateral segment of left lobe; MP, main portal vein; C, caudate lobe; aRPV, anterior branches of right portal vein; A, anterior segment of right lobe; pRPV, posterior branches of right portal vein; P, posterior segment of right lobe.
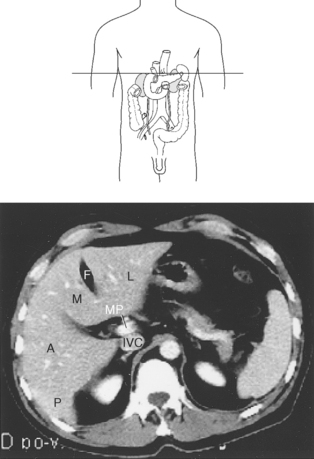
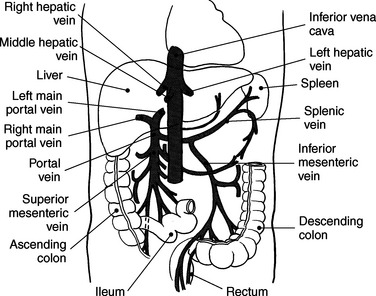
Portal Hepatic System
The liver receives nutrient-rich blood from the gastrointestinal tract via the portal hepatic system (Figures 7.35 and 7.48). The major vessel of this system is the portal vein, which is formed in the retroperitoneum by the union of the superior mesenteric and splenic veins, posterior to the neck of the pancreas (Figures 7.49 through 7.52). It passes obliquely to the right, posterior to the hepatic artery within the lesser omentum, and enters the liver at the porta hepatis. At the porta hepatis, the portal vein branches into right and left main portal veins that then follow the course of the right and left hepatic arteries (Figures 7.53 and 7.54). The right portal vein first sends branches to the caudate lobe, then divides into anterior and posterior branches that subdivide into superior and inferior branches to supply the right lobe of the liver. The left portal vein initially courses to the left, then turns medially toward the ligamentum teres. It branches to supply the lateral segments (segments II and III) of the left lobe and the superior and inferior segmental branches of segment IV.
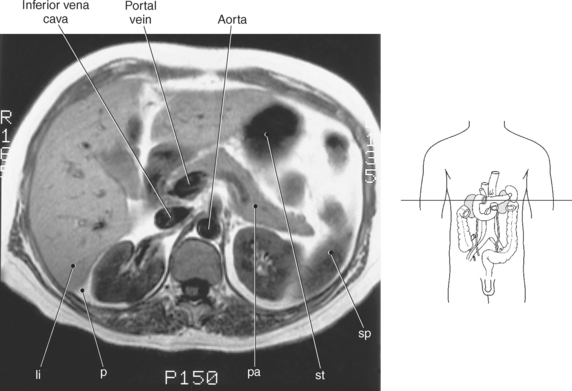
Figure 7.49 Axial, T1-weighted MR scan of liver and portal vein.
Key: li, Liver; p, peritoneum; pa, pancreas; st, stomach; sp, spleen.
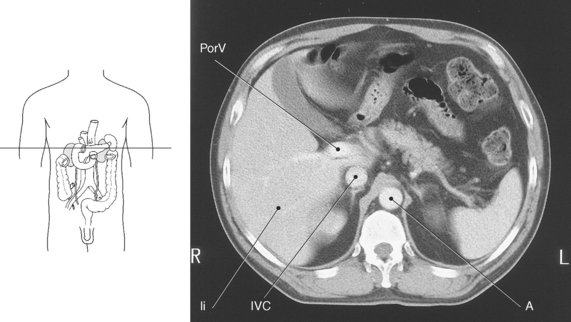
Figure 7.50 Axial CT scan of liver and portal vein.
Key: PorV, Portal vein; li, liver; IVC, inferior vena cava; A, aorta.
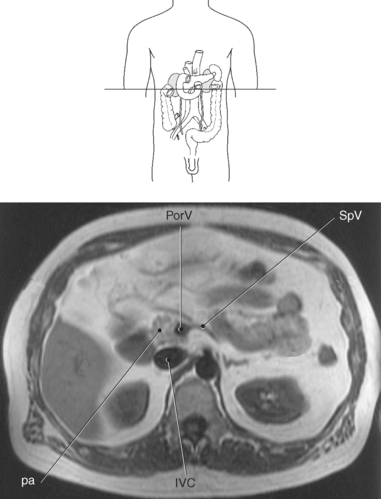
Figure 7.51 Axial, T1-weighted MR scan of abdomen with portal and splenic veins.
Key: PorV, Portal vein; IVC, inferior vena cava; SpV, splenic vein; pa, pancreas.
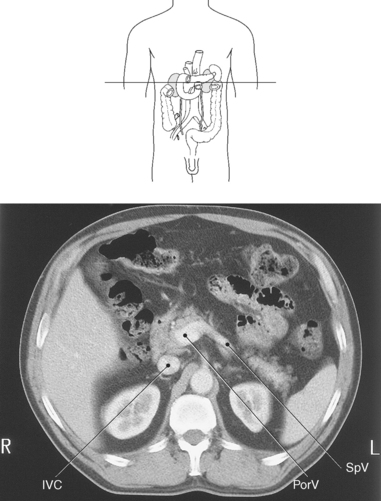
Figure 7.52 Axial CT scan of abdomen with portal and splenic veins.
Key: PorV, Portal vein; IVC, inferior vena cava; SpV, splenic vein.
Vasculature
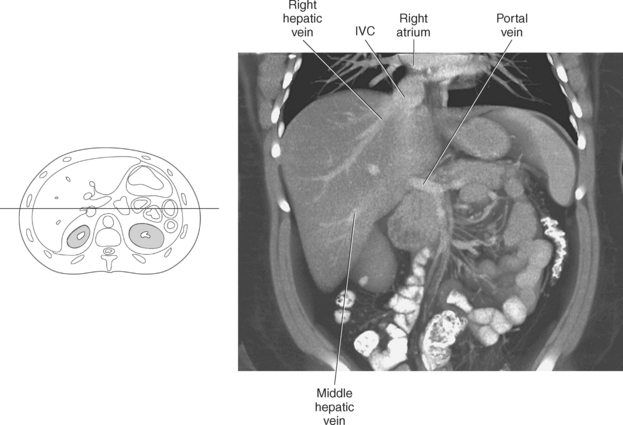
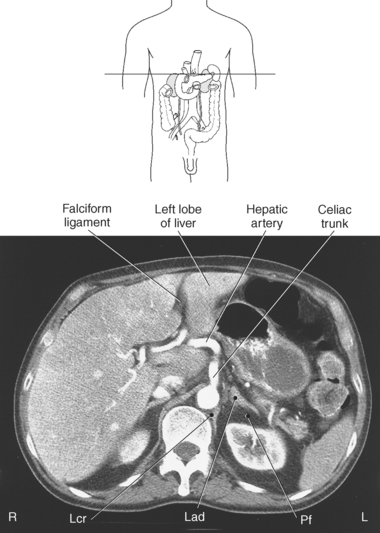
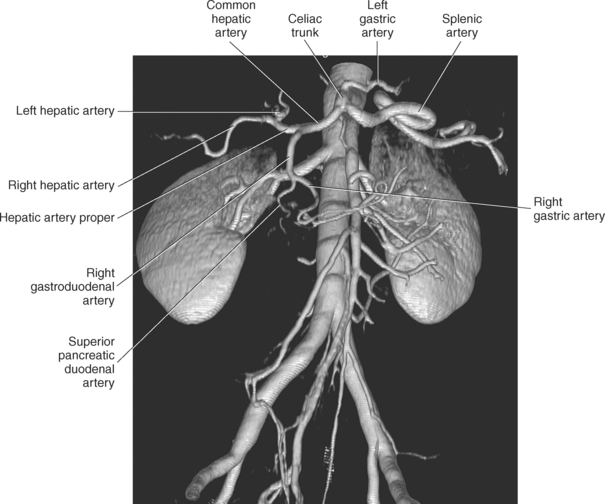
The liver is unusual in that it has a dual blood supply, receiving arterial blood (20%-25%) from the common hepatic artery and nutrient-rich venous blood (75%-80%) from the portal vein. The common hepatic artery usually arises as one of the three branches off the celiac artery, coursing to the right to enter the lesser omentum anterior to the portal vein (Figures 7.55 through 7.58). It branches into the right gastric and gastroduodenal arteries just above the duodenum and continues in the hepatoduodenal ligament as the proper hepatic artery. While within or just before entering the porta hepatis, the proper hepatic artery divides into left and right hepatic arteries that continue to branch and supply the lobes of the liver. The right hepatic artery is larger than the left and supplies the majority of the right lobe of the liver. It passes posterior to the uncinate process of the pancreas and runs along the posterior wall of the bile duct into the right hepatic lobe. The left hepatic artery is located between the lesser curvature of the stomach and approaches the liver in the lesser omentum and branches to supply the caudate, quadrate, and medial and lateral segments of the left lobe of the liver (Figure 7.59). The venous drainage of the liver occurs via the small interlobar and intersegmental hepatic vessels that merge into the three major hepatic veins, emptying directly into the IVC, just below the diaphragm (Figure 7.60). The right hepatic vein, the largest, lies between the right anterior and posterior hepatic segments, drains segments V, VI, and VII, and enters the IVC at the right lateral aspect. The middle hepatic vein lies in the interlobar fissure, drains segments IV, V, and VIII, then enters the IVC at the anterior or right anterior surface. The smallest hepatic vein, the left hepatic vein, courses between the medial and lateral segments of the left lobe, drains segments II and III, then enters the left anterior surface of the IVC (Figures 7.61 and 7.62). Frequently, the middle and left hepatic veins converge to form a common trunk before emptying into the IVC just below the diaphragm. The IVC lies in a groove along the posterior wall of the liver and ascends into the thoracic cavity through the caval hiatus of the diaphragm and enters the right atrium of the heart (Figures 7.61 through 7.64).
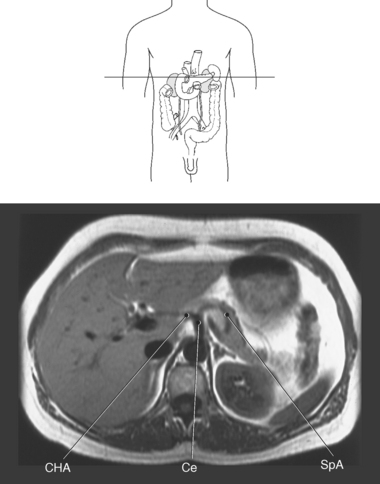
Figure 7.57 Axial, T1-weighted MR scan of abdomen with celiac trunk and hepatic artery.
Key: CHA, Common hepatic artery; Ce, celiac axis; SpA, splenic artery.
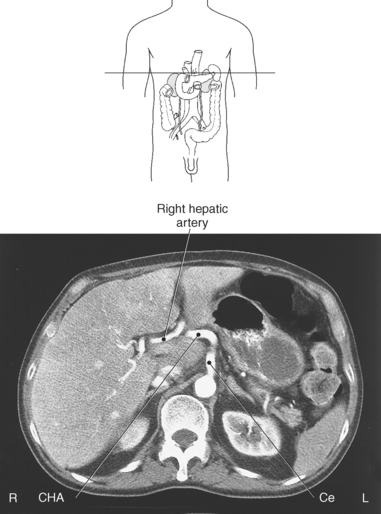
Figure 7.58 Axial CT scan of abdomen with celiac trunk and hepatic artery.
Key: CHA, Common hepatic artery; Ce, celiac axis.
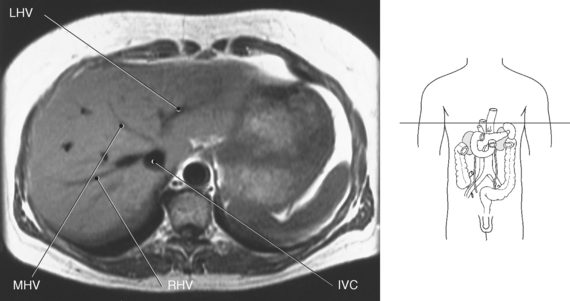
Figure 7.61 Axial, T1-weighted MR scan of abdomen with hepatic veins.
Key: LHV, Left hepatic vein; MHV, middle hepatic vein; RHV, right hepatic vein; IVC, inferior vena cava;.
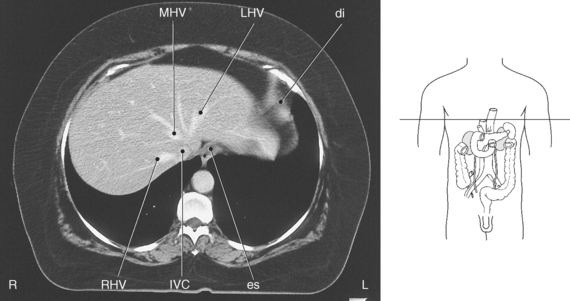
Figure 7.62 Axial CT scan of liver with hepatic veins.
Key: LHV, Left hepatic vein; MHV, middle hepatic vein; RHV, right hepatic vein; IVC, inferior vena cava; di, diaphragm; es, esophagus.
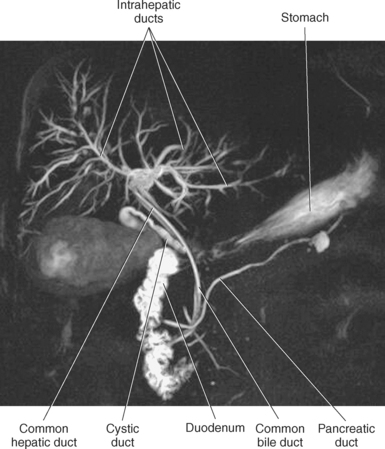
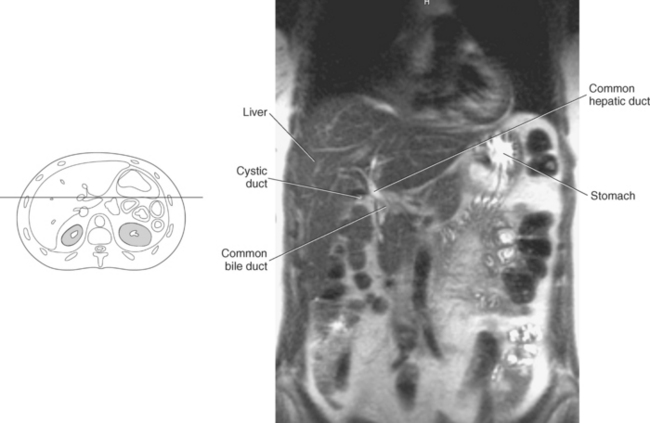
GALLBLADDER AND BILIARY SYSTEM
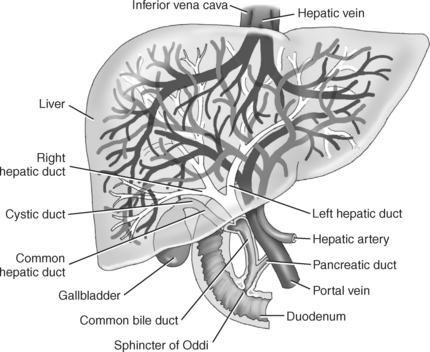
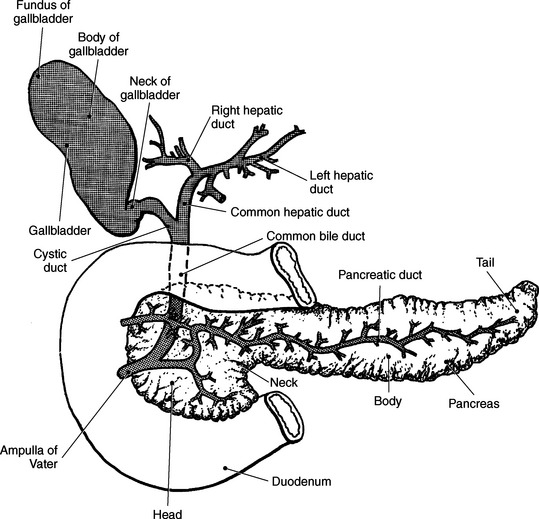
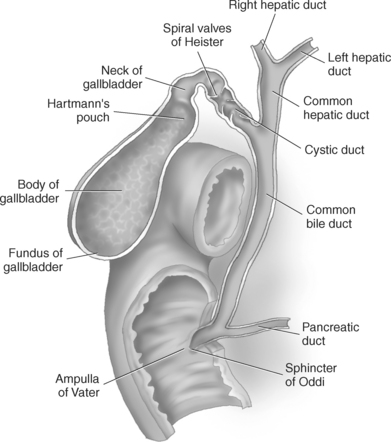
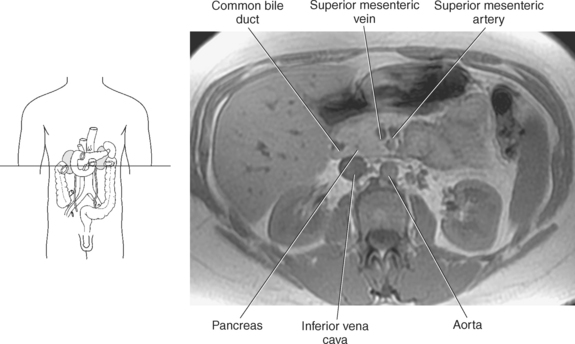
The biliary system is composed of the gallbladder and bile ducts (both intrahepatic and extrahepatic) that serve to drain the liver of bile and then store it until it is transported to the duodenum to aid in digestion (Figure 7.65). The hollow pear-shaped gallbladder is located in the gallbladder fossa on the anteroinferior portion of the right lobe of the liver, closely associated with the main lobar fissure. It functions as the reservoir for storing and concentrating bile before being transported to the duodenum. The gallbladder can be divided into a fundus, body, and neck (Figures 7.66 to 7.71). The fundus is the rounded distal portion of the gallbladder sac that is frequently in contact with the anterior abdominal wall. The widest portion, the body, gently tapers superiorly into the neck. The narrow neck lies to the right of the porta hepatis and continues as the cystic duct. The neck contains circular muscles that create spiral folds within the mucosa that are called the spiral valves of Heister (Figure 7.67). These valves are especially prominent at the bend formed by the neck and cystic duct, a common area for gallbladder impaction during acute or chronic cholecystitis. The gallbladder has a muscular wall that contracts when stimulated by cholecystokinin, forcing bile through the extrahepatic biliary system into the duodenum. Bile, formed within the liver, is collected for transport to the gallbladder by the intrahepatic bile ducts. The intrahepatic bile ducts run beside the hepatic arteries and portal veins throughout the liver parenchyma. The intrahepatic ducts merge into successively larger ducts as they follow a course from the periphery to the central portion of the liver, eventually forming the right and left hepatic ducts (Figures 7.65 to 7.68). The right and left hepatic ducts unite at the porta hepatis to form the proximal portion of the common hepatic duct (CHD), which marks the beginning of the extrahepatic biliary system (Figure 7.66). The CHD is located anterior to the portal vein and lateral to the hepatic artery in its caudal descent from the porta hepatis. As the CHD descends in the free border of the lesser omentum, it is joined from the right by the cystic duct to form the common bile duct (CBD). The CBD continues a caudal descent along with the hepatic artery and portal vein within the hepatoduodenal ligament (Figure 7.65). It curves slightly to the right, away from the portal vein, then courses posterior and medial to the first part of the duodenum behind the head of the pancreas (Figures 7.69 through 7.76). The CBD follows a groove on the posterior surface of the pancreatic head, then pierces the medial wall of the second part of the duodenum along with the main pancreatic duct (duct of Wirsung) through the ampulla of Vater (Figure 7.66). The ends of both ducts are surrounded by the circular muscle fibers of the sphincter of Oddi (Figure 7.67).
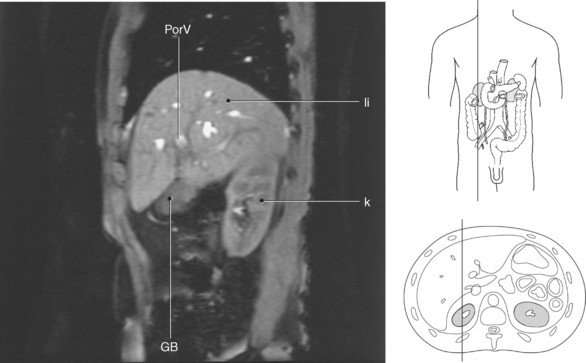
Figure 7.70 Sagittal, T2-weighted MR scan of liver and gallbladder.
Key: PorV, Portal vein; li, liver; k, kidney; GB, gallbladder.
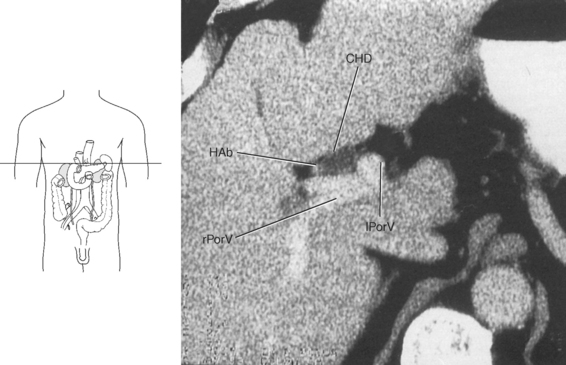
Figure 7.74 Axial CT scan of abdomen and common bile duct.
Key: CHD, Common hepatic duct; HAb, hepatic artery branch; lPorV, left branch of portal vein; rPorV, right branch of portal vein.
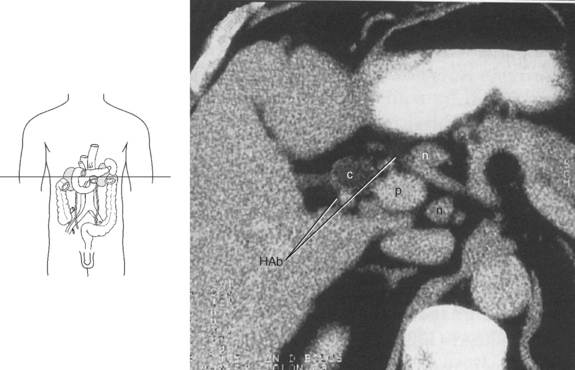
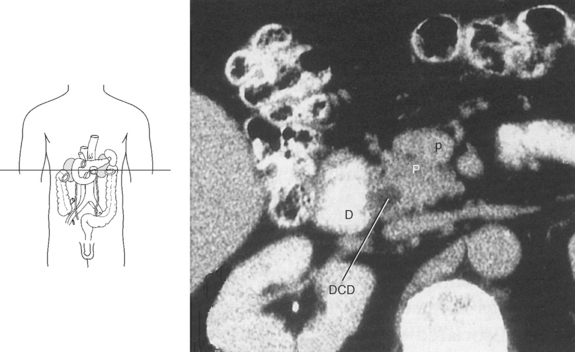
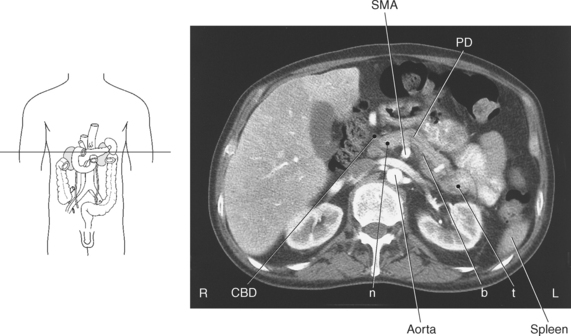
PANCREAS
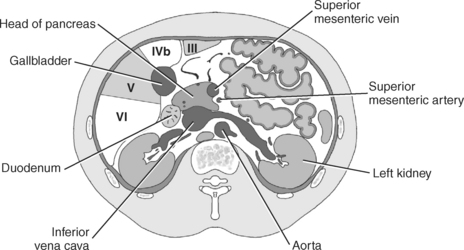
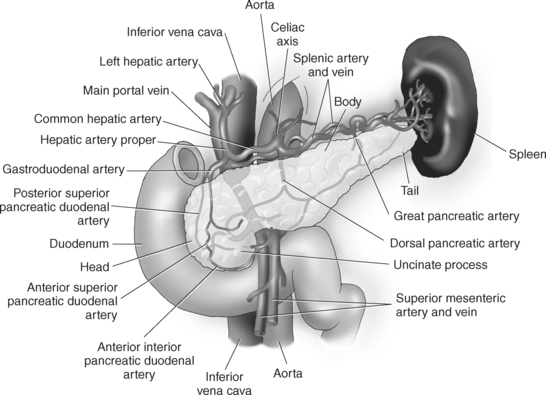
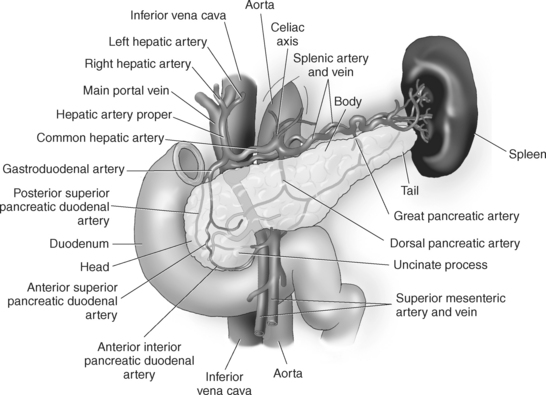
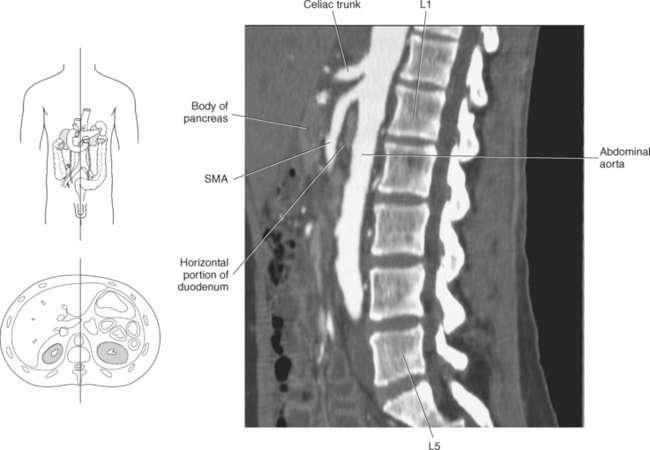
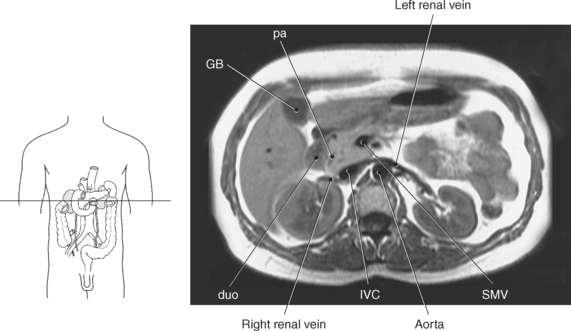
The pancreas is a long, narrow retroperitoneal organ that lies posterior to the stomach and extends transversely at an oblique angle between the duodenum and splenic hilum. The pancreas can be divided into the head, uncinate process, neck, body, and tail (Figure 7.77). The broad, flat head of the pancreas lies inferior and to the right of the body and tail, nestled in the curve of the second portion of the duodenum at approximately the level of L2-L3. The head is anterior to the IVC and renal veins. Two vessels can be commonly seen running through the head: the common bile duct in the right posterior aspect and the gastroduodenal artery in the anterior aspect (Figures 7.78 and 7.79). The uncinate process is a medial and posterior extension of the head, lying between the superior mesenteric vein and inferior vena cava (Figure 7.77). The neck, the constricted portion of the gland, is located between the pancreatic head and body. Located just posterior to the neck is the portal splenic confluence, where the portal vein is formed by the merging of the superior mesenteric and splenic veins (Figure 7.77). The body is the largest and most anterior portion of the pancreas, extending transversely to the left, anterior to the aorta and superior mesenteric artery (Figures 7.80 and 7.81). The splenic vein runs along the posterior surface of the body on its route to the portal splenic confluence. The body tapers superiorly and posteriorly into the pancreatic tail. The tail extends into to the left anterior pararenal space, anterior to the left kidney, to end at the splenic hilum (Figures 7.77 and 7.80 through 7.82). The pancreas has both an endocrine (insulin, glucagon) and exocrine (digestive enzymes) function. It delivers its endocrine hormones into the draining venous system and its enzymes into the small intestines. The endocrine hormones help control plasma glucose concentration. Insulin’s chief role is to regulate cellular absorption and utilization of glucose, thereby affecting carbohydrate, protein and lipid metabolism in body tissues. Glucagon, acting in opposition to insulin, tends to raise plasma sugar levels by increasing the rate of glycogen breakdown and glucose synthesis in the liver. Pancreatic enzymes include amylase for the digestion of starch, lipase for the digestion of lipids, peptidases for protein digestion, and sodium bicarbonate to neutralize gastric acid. The pancreatic enzymes are carried to the duodenum via a system of ducts. The main pancreatic duct (duct of Wirsung) begins in the tail and runs the length of the gland to the ampulla of Vater, where it empties, together with the common bile duct, into the duodenum through the sphincter of Oddi (Figures 7.66 and 7.82). The arterial supply of the pancreas comes from branches of the celiac and superior mesenteric arteries. Venous blood drains from the pancreas into the portal vein via the superior mesenteric or splenic vein. The pancreas is unencapsulated and has a distinct lobulated appearance, making identification easy in cross section.
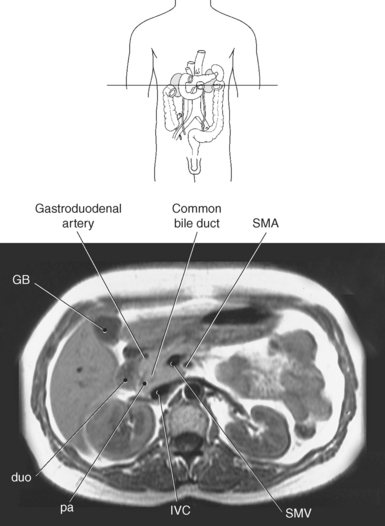
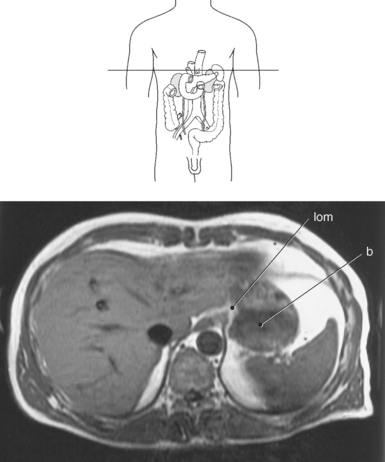
Figure 7.78 Axial, T1-weighted MR scan of abdomen with head of pancreas and duodenum.
Key: GB, Gallbladder; duo, duodenum; pa, pancreas; IVC, inferior vena cava; SMV, superior mesenteric vein; SMA, superior mesenteric artery.
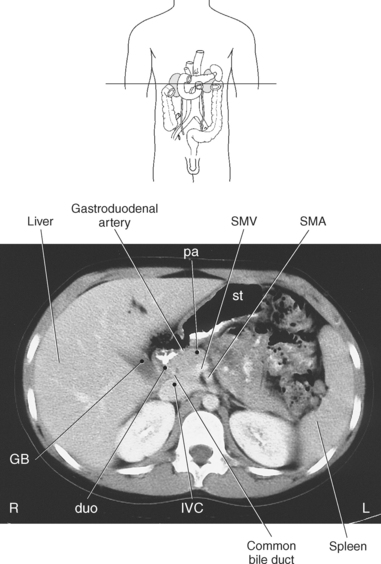
Figure 7.79 Axial CT scan of abdomen with head of pancreas and duodenum.
Key: GB, Gallbladder; duo, duodenum; pa, pancreas; IVC, inferior vena cava; SMV, superior mesenteric vein; st, stomach; SMA, superior mesenteric artery;.
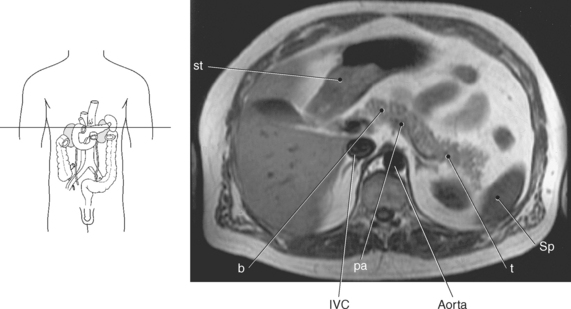
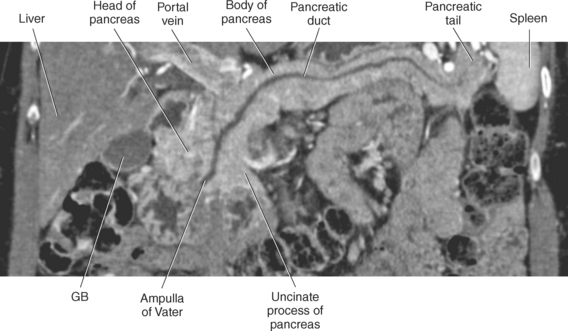
Figure 7.80 Axial, T1-weighted MR scan of pancreas.
Key: pa, pancreas; IVC, inferior vena cava; st, stomach; b, body of pancreas; t, tail of pancreas; Sp, spleen.
SPLEEN
The spleen is the largest lymph organ in the body composed of lymphoid tissue. The cellular components of the spleen create a highly vascular, spongy parenchyma called red and white pulp. The red pulp contains large quantities of blood, and the white pulp contains lymphoid tissue and white blood cells. The spleen is an intraperitoneal organ that is covered entirely with peritoneum except at its small bare area at the splenic hilum. It is located posterior to the stomach in the left upper quadrant of the abdomen, protected by the ninth through eleventh ribs. The spleen is bordered on its medial side by the left kidney, splenic flexure of the colon, and pancreatic tail. The posterior border of the spleen is in contact with the diaphragm, pleura, left lung, and ribs. The spleen is attached to the greater curvature of the stomach and the left kidney by the gastrosplenic and lienorenal ligaments, respectively (Figure 7.83). The spleen receives its arterial blood from the splenic artery and is drained via the splenic vein. The splenic artery and vein enter and exit the spleen at the splenic hilum between the gastric and renal depressions (Figures 7.84 and 7.85). The spleen is a highly vascular organ that functions to produce white blood cells, filter abnormal blood cells from the blood, store iron from red blood cells, and initiate the immune response. Normal splenic parenchyma is homogeneous; however, immediately after intravenous contrast injection, the spleen can have a heterogeneous appearance on early arterial phase images (Figure 7.85).
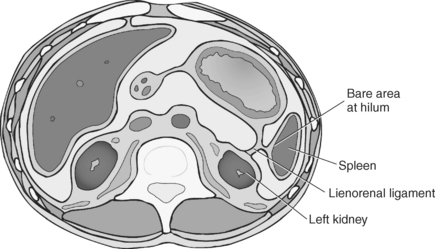
Figure 7.83 Axial view of the abdomen with greater and lesser sac, falciform and gastrosplenic and lienorenal ligaments.
ADRENAL GLANDS
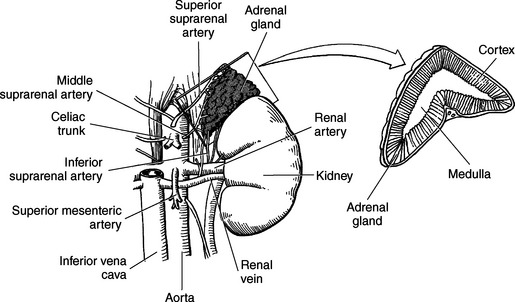
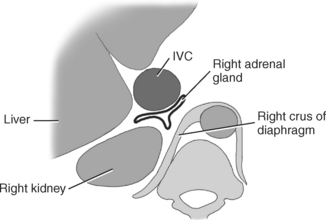
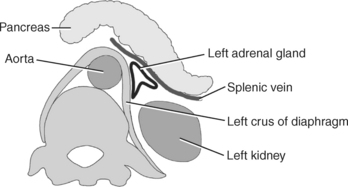
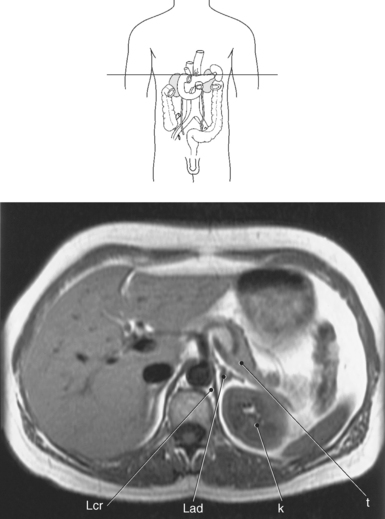
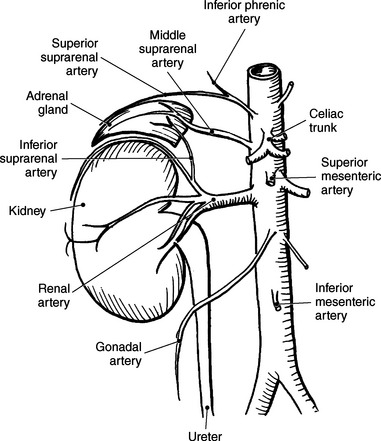
The paired adrenal (suprarenal) glands are retroperitoneal organs located superior to each kidney (Figures 7.86 and 7.87). They are separated from the superior surface of the kidneys by perirenal fat and are enclosed, along with the kidneys, by Gerota’s fascia (Figure 7.88). The right adrenal gland is located just posterior to the IVC, medial to the posterior segment of the right hepatic lobe, and lateral to the right crus of the diaphragm. It is generally lower and more medial than the left adrenal gland and commonly appears as an inverted V on cross section (Figures 7.89 through 7.91). The left adrenal gland lies anteromedial to the upper pole of the left kidney. It is located in a triangle formed by the aorta, pancreatic tail, and left kidney (Figure 7.92). It commonly appears as a triangular or Y-shaped configuration (Figures 7.93 and 7.94). The posterior surfaces of both the right and left glands border the crus of the diaphragm. Each adrenal gland has an outer cortex and an inner medulla that function independently (Figure 7.86). The adrenal cortex produces more than two dozen steroids, collectively called adrenocortical steroids or just corticosteroids. The corticosteroids are broken into three main categories: glucocorticoids, which affect glucose metabolism; mineralocorticoids, which regulate sodium and potassium levels; and androgens and estrogens, which are responsible for promoting normal development of bone and reproductive organs. The adrenal medulla produces the hormones epinephrine and norepinephrine, which accelerate metabolism and energy and are responsible for the body’s “fight or flight” response. The adrenal glands receive arterial blood from the superior, middle, and inferior adrenal arteries. The drainage of the right gland is via a short suprarenal vein that empties directly into the IVC. The left gland is drained by the left suprarenal vein, which empties into the left renal vein.
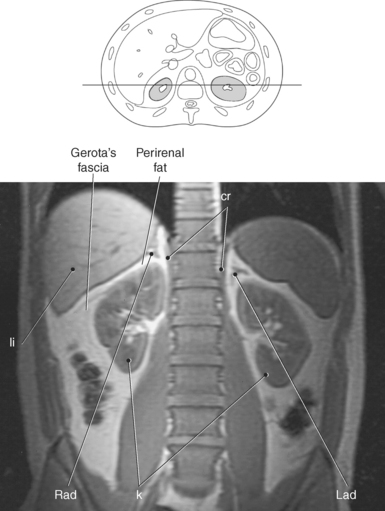
Figure 7.88 Coronal, T1-weighted MR scan with adrenal glands.
Key: cr, Crus; li, liver; Rad, right adrenal gland; k, kidney; Lad, left adrenal gland.
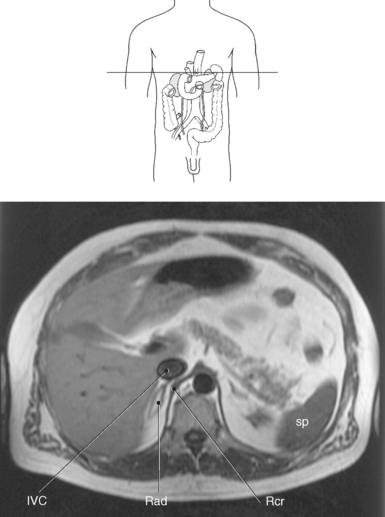
Figure 7.90 Axial, T1-weighted MR scan of right adrenal gland.
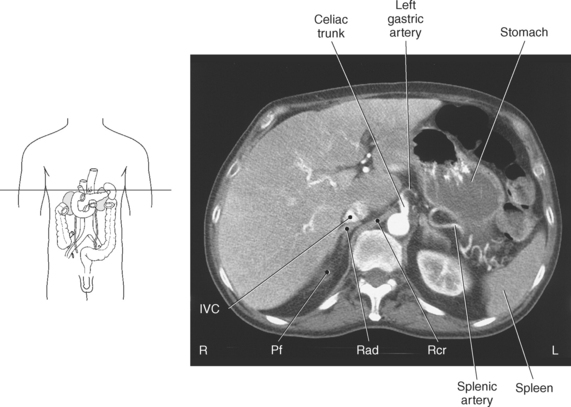
Key: IVC, Inferior vena cava; Rad, right adrenal gland; Rcr, right crus; sp, spleen.
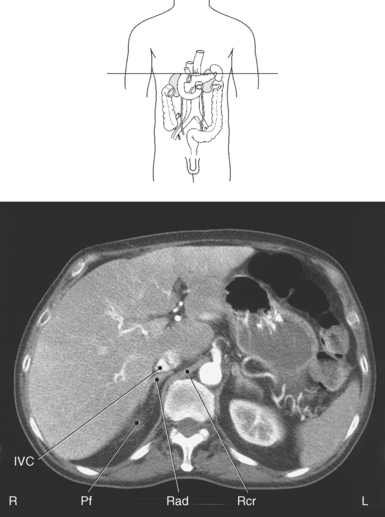
Figure 7.91 Axial CT scan of right adrenal gland.
Key: IVC, Inferior vena cava; Rad, right adrenal gland; Rcr, right crus; Pf, perirenal fat.
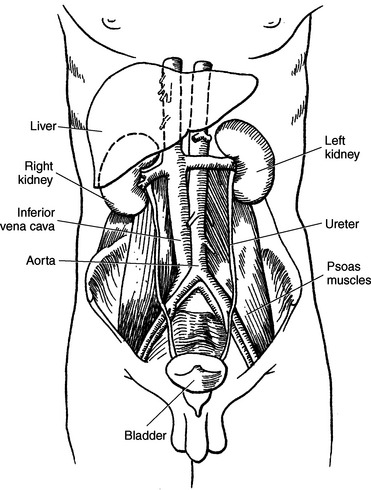
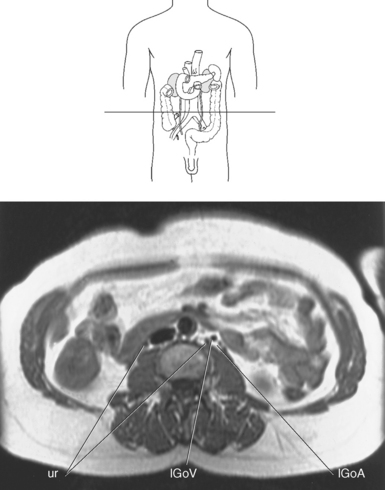
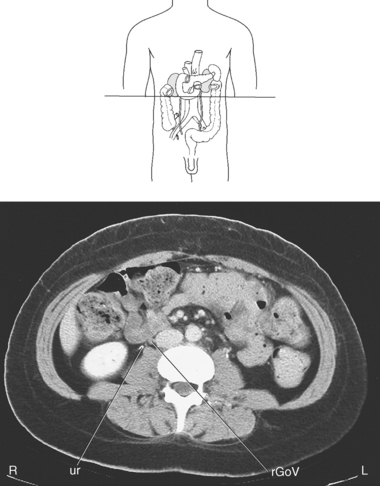
URINARY SYSTEM
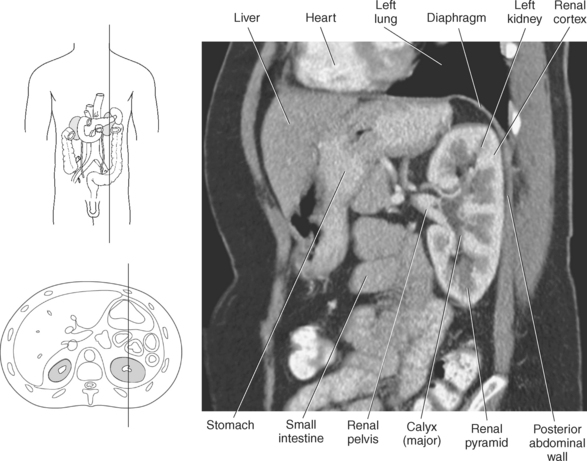
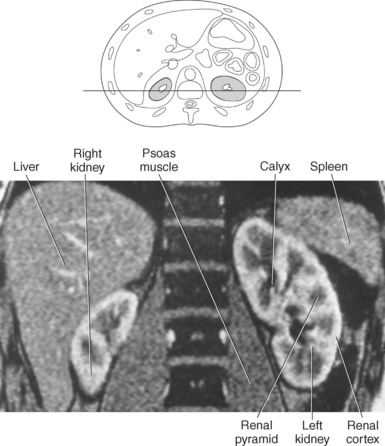
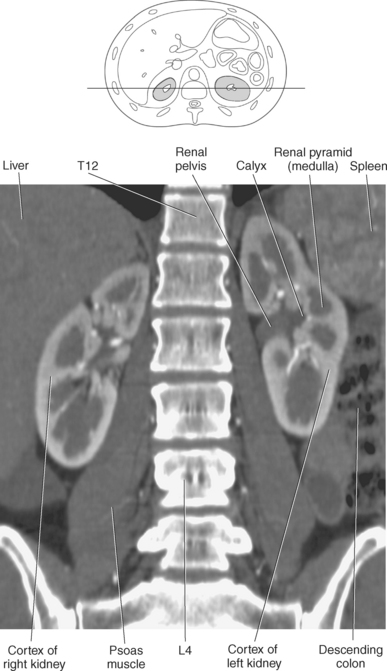
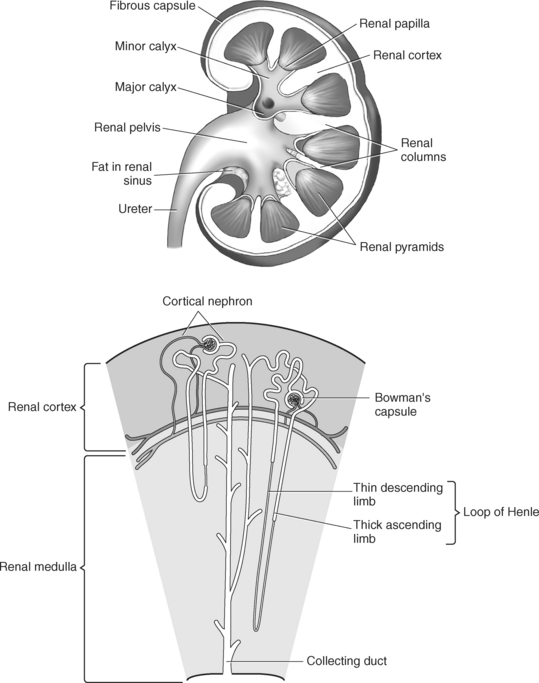
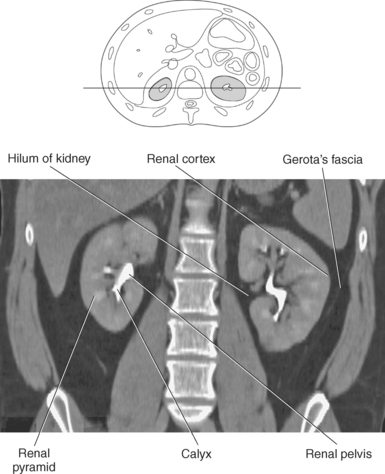
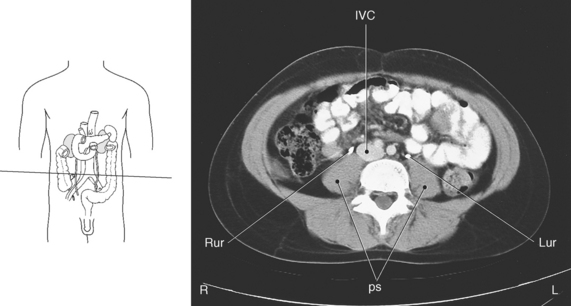
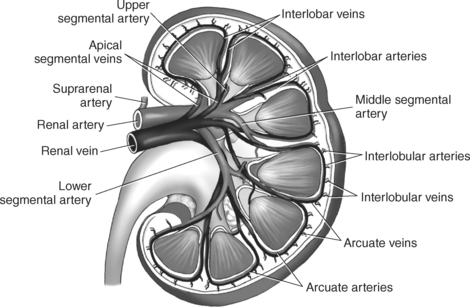
The structures of the urinary system include the kidneys, ureters, bladder, and urethra. Those that are located within the abdomen are the kidneys and ureters (Figure 7.95). The bladder and urethra are located in the pelvis and are discussed in Chapter 8. The kidneys are retroperitoneal bean-shaped organs that lie in the paravertebral gutters against the posterior abdominal wall (Figure 7.96). They lie at an oblique orientation, with the upper poles more medial and posterior than the lower poles. They are located on each side of the spine between T12 and L4 and are embedded in perirenal fat (Figure 7.97). The right kidney is usually slightly lower due to displacement by the liver (Figures 7.98 and 7.99). Each kidney is composed of an outer cortex and an inner medulla. The renal cortex comprises the outer one third of the renal tissue and has extensions between the renal pyramids of the medulla. The cortex contains the functional subunit of the kidney, the nephron, which consists of the glomerulus and convoluted tubules and is responsible for filtration of urine (Figure 7.100). The renal medulla consists of segments called renal pyramids that radiate from the renal sinus to the outer surface of the kidney. The striated-appearing pyramids contain the loops of Henle and collecting tubules and function as the beginning of the collecting system. Arising from the apices of the pyramids are the cup-shaped minor calyces. Each kidney has 7 to 14 minor calyces that merge into 2 or 3 major calyces. The major calyces join to form the renal pelvis, which is the largest dilated portion of the collecting system and is continuous with the ureters (Figure 7.100). The fat-filled cavity surrounding the renal pelvis is called the renal sinus.
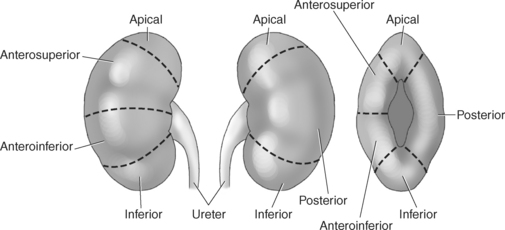
Surrounding the kidneys and perirenal fat is another protective layer called the renal fascia (Gerota’s fascia). The renal fascia functions to anchor the kidneys to surrounding structures in an attempt to prevent bumps and jolts to the body from injuring the kidneys. In addition, the renal fascia acts as a barrier, limiting the spread of infection that may arise from the kidneys. The medial indentation in the kidney is called the hilum; it allows the renal artery and vein and ureters to enter and exit the kidney (Figures 7.97 and 7.101 through 7.104). The kidneys can be divided into five segments according to their vascular supply: apical, anterosuperior (upper anterior), anteroinferior (middle inferior), inferior, and posterior (Figure 7.105). The segmental classification helps with surgical planning for partial nephrectomies. The ureters are paired muscular tubes that transport urine to the urinary bladder. Each ureter originates at the renal pelvis and descends anteriorly and medially to the psoas muscles, just anterior to the transverse processes of the lumbar spine (Figures 7.104 through 7.106). The ureters then enter the posterior wall of the bladder at an oblique angle (Figure 7.107). The primary function of the urinary system is to filter blood, produce and excrete urine, and help maintain normal body physiology.
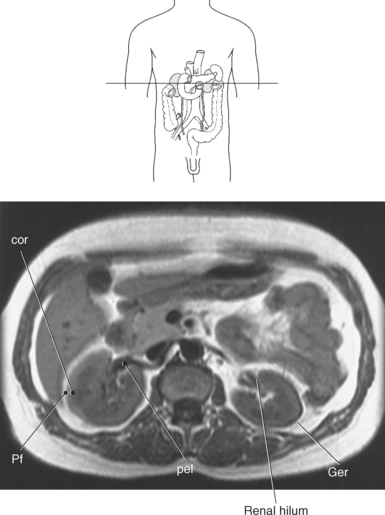
Figure 7.103 Axial, T1-weighted MR scan of kidney.
Key: cor, Renal cortex; Pf, perirenal fat; pel, renal pelvis; Ger, Gerota’s fascia.
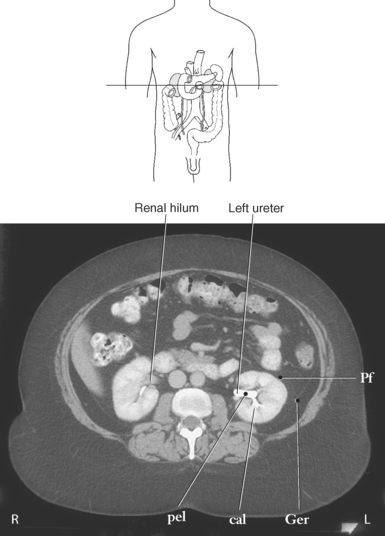
Figure 7.104 Axial CT scan of kidney.
Key: Pf, perirenal fat; pel, renal pelvis; cal, calyx; Ger, Gerota’s fascia.
STOMACH
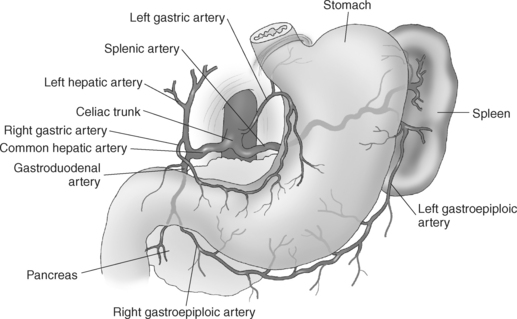
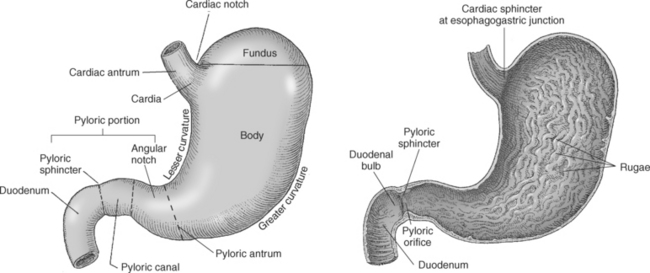
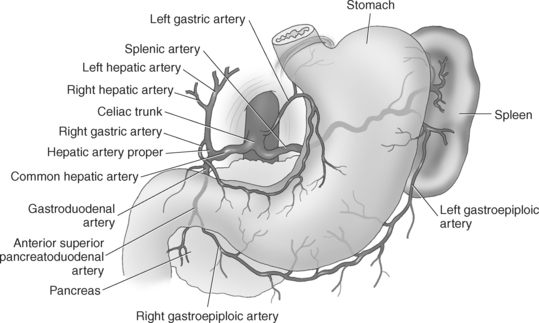
The stomach is the dilated portion of the digestive system that acts as a food reservoir and is responsible for the early stages of digestion. It has four major functions: (1) storage of food, (2) mechanical breakdown of food, (3) dissolution of chemical bonds via acids and enzymes, and (4) production of intrinsic factor. The stomach is located under the left dome of the diaphragm, with the superior portion joining the esophagus at the cardiac orifice (cardiac sphincter), creating the esophagogastric junction (Figures 7.108 through 7.110). The stomach has two borders called the lesser and greater curvatures. Between the two curvatures is the largest portion of the stomach, termed the body (Figures 7.111 to 7.113). On the superior surface of the body is a rounded surface called the fundus (Figure 7.110). The inferior portion (pyloric antrum) empties into the duodenum through the pyloric sphincter (Figure 7.114). The anterior surface is in contact with the diaphragm, anterior abdominal wall, and left lobe of the liver. Located posterior to the stomach is the gastric portion of the spleen, the left adrenal gland and kidney, and the body and tail of the pancreas. When empty, the inner surface of the stomach creates prominent folds called rugae that allow the stomach to expand with the ingestion of food (Figures 7.108 and 7.110). The average adult produces 2 to 3 L per day of gastric juices that contain mucus, hydrochloric acid, intrinsic factor, and the digestive enzymes of pepsinogen and lipase. The stomach can hold up to 3 L of food, which it mixes with digestive juices to form chyme. The stomach is one of the most vascular organs within the body. The arterial blood is supplied by branches of the gastric, splenic, and gastroduodenal arteries (Figure 7.55). Venous drainage corresponds to the arterial supply. The gastric veins usually drain directly into the portal vein or into the superior mesenteric vein.
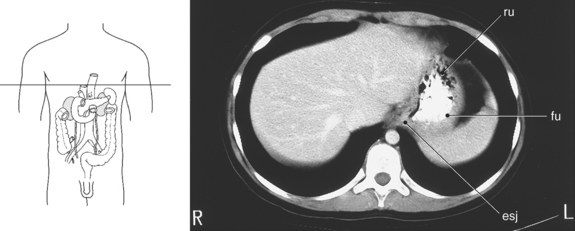
Figure 7.110 Axial CT scan of esophagogastric junction.
Key: ru, Rugae; fu, fundus of stomach; esj, esophagogastric junction.
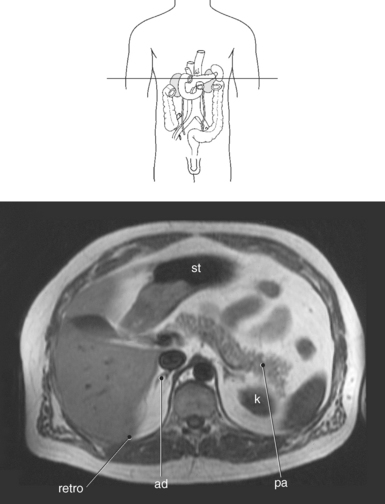
Figure 7.111 Axial, T1-weighted MR scan of stomach.
Key: st, stomach; k, kidney; retro, retroperitoneum; ad, adrenal gland; pa, pancreas.
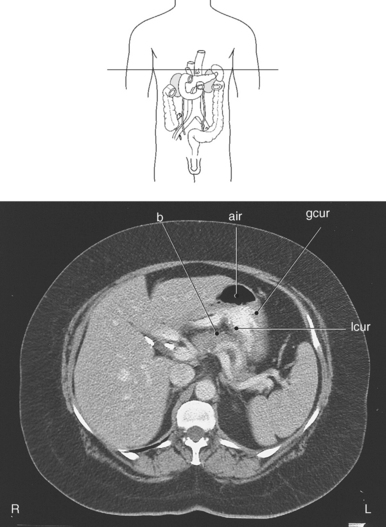
Figure 7.112 Axial CT scan of stomach.
Key: b, body of pancreas; air, air; gcur, greater curvature; lcur, lesser curvature.
INTESTINES
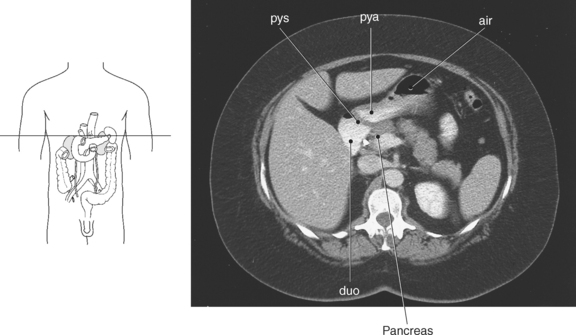
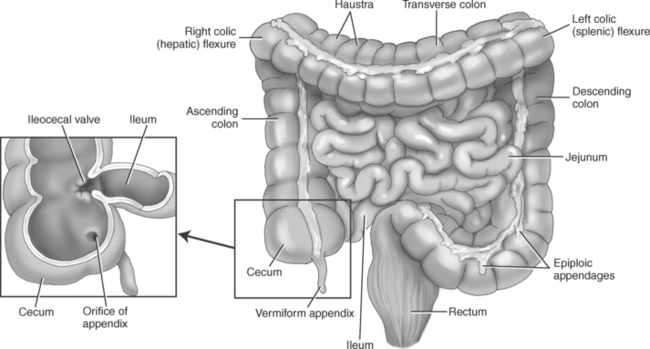
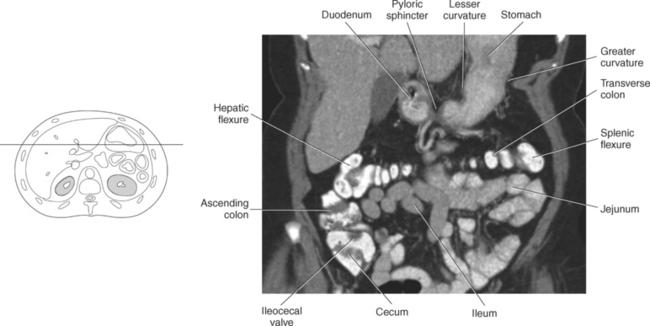
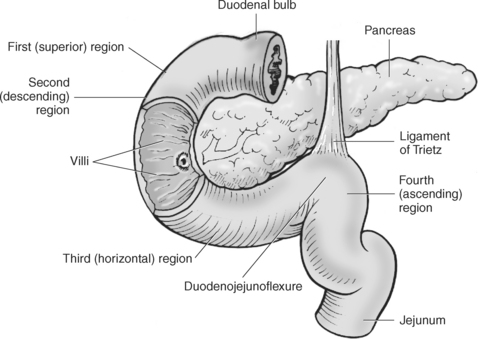
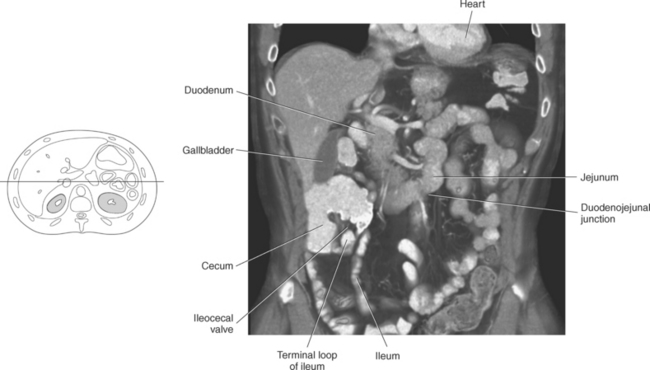
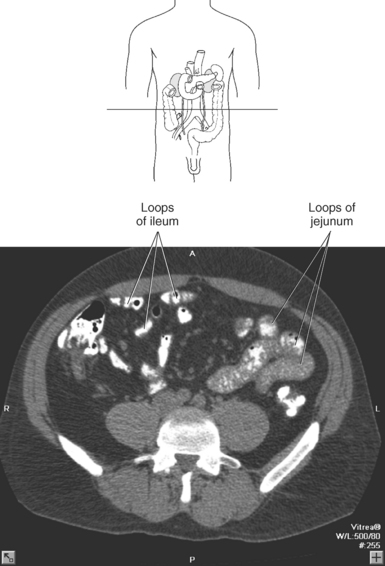
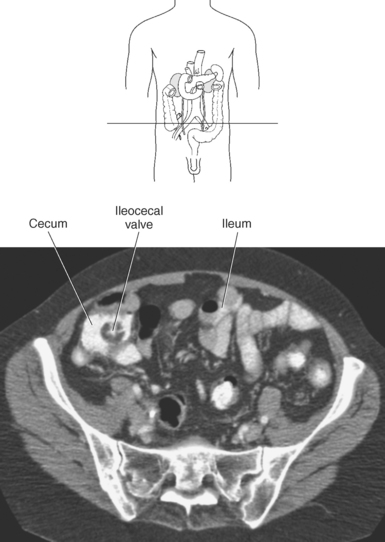
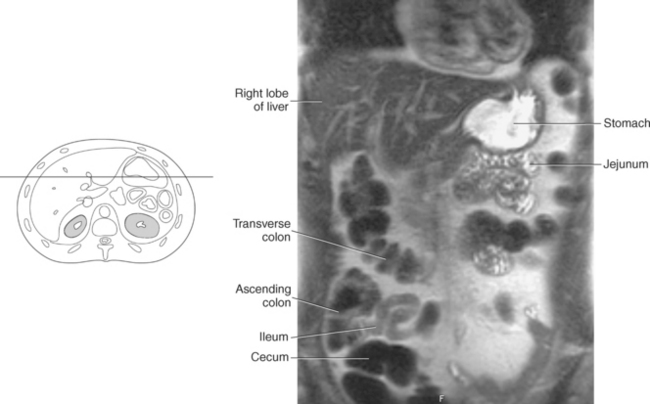
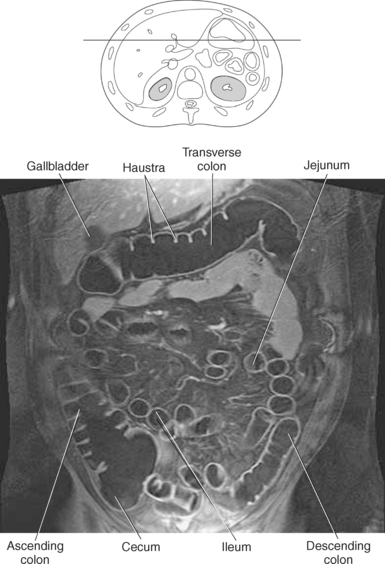
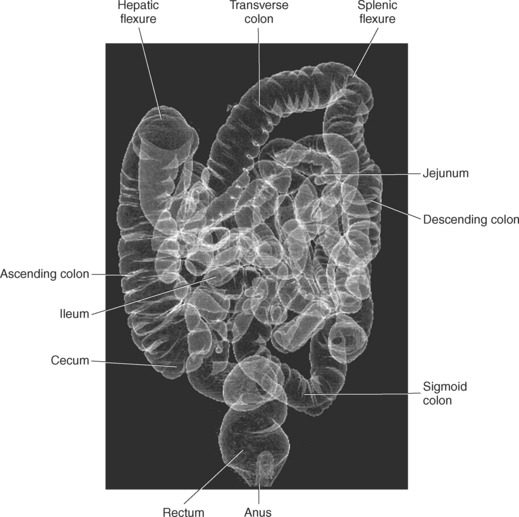
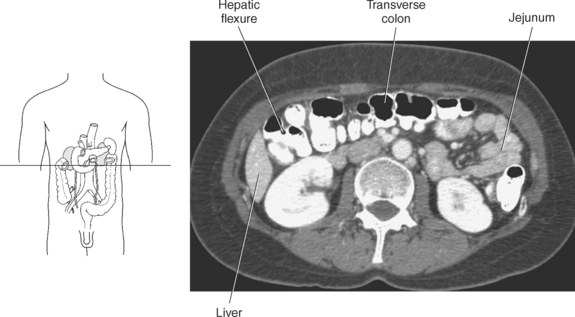
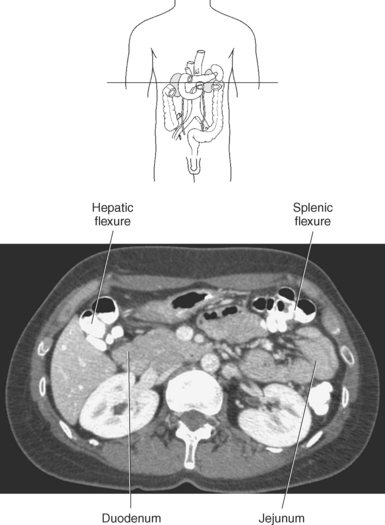
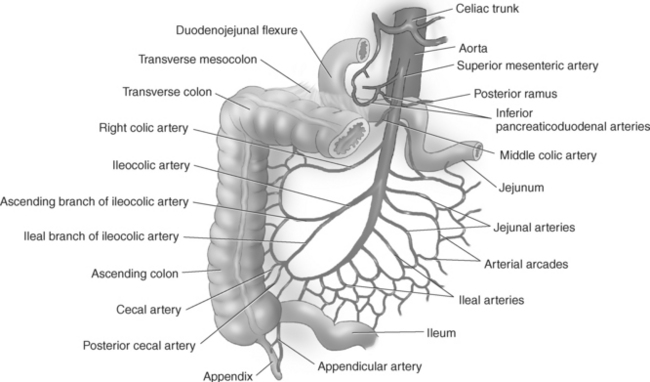
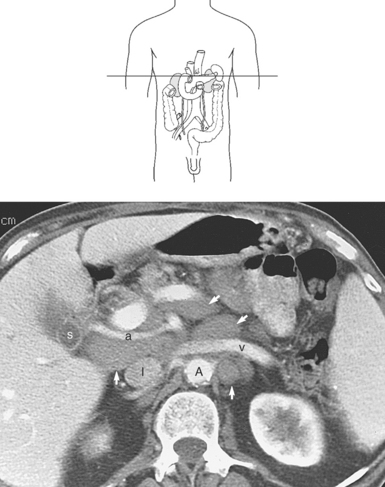
The small intestine (small bowel) is located between the pylorus and ileocecal valve and consists of loops of bowel averaging 6 to 7 meters in length. It can be subdivided into the duodenum, jejunum, and the ileum (Figures 7.115 and 7.116). The proximal portion of the small intestine is the duodenum, which begins at the gastric pylorus and curves around the head of the pancreas, forming the letter C (Figures 7.113 through 7.117). The duodenum is mostly retroperitoneal, making it less mobile than the rest of the small intestine. Although quite short, the duodenum is divided into four portions. The first (superior) portion is formed by the first 2 inches of the duodenum, the conical-shaped duodenal bulb. It is the most common site for peptic ulcer formation. The second (descending) portion is formed by the next 4 inches of duodenum that descends along the right side of the vertebral column; it contains the ampulla of Vater and receives pancreatic and biliary drainage. The third (horizontal) portion is about 10 cm long and runs horizontally in front of the third lumbar vertebra. In its horizontal course from right to left, the third portion of the duodenum runs anterior to the superior vena cava (SVC), aorta, and inferior mesenteric artery and posterior to the superior mesenteric artery. The fourth (ascending) portion is about 2.5 cm in length and ascends on the left side of the aorta to the level of the L2 vertebra, where it meets up with the jejunum at the duodenojejunal flexure. The duodenojejunal flexure is fixed in place by the ligament of Treitz, a suspensory ligament created from the connective tissue around the celiac axis and left crus of the diaphragm (Figure 7.117). This location marks the entry of the small bowel into the peritoneal cavity. The remainder of the small intestine, the jejunum and ileum, is suspended from the posterior abdominal wall by a fan-shaped mesentery. The jejunum is approximately 2.5 meters long and occupies the left upper abdomen or umbilical region of the abdomen (Figures 7.115 through 7.119). This section of small bowel is where the bulk of chemical digestion and nutrient absorption occurs. The jejunum contains numerous circular folds that give it a feathery appearance on barium or computed tomography (CT) examinations. The lower three fifths of the small intestine, the ileum, is the longest portion of the small intestine, averaging 3.5 meters long and located in the right lower abdomen (Figures 7.115, 7.116, and 7.119 through 7.121). It is in the ileum that intrinsic factor from the stomach combines with vitamin B12 for absorption in the terminal ileum. Vitamin B12 is essential for normal red blood cell (RBC) formation and nervous system function. The loops of ileum terminate at the ileocecal valve, a sphincter that controls the flow of material from the ileum into the cecum of the large intestine (Figures 7.118, 7.122, and 7.123). The mesentery serves as a route for blood vessels, lymphatics, and nerves to reach the small intestine. The segments of the small intestine receive blood from branches of the superior mesenteric artery and are drained by branches of the superior mesenteric vein.
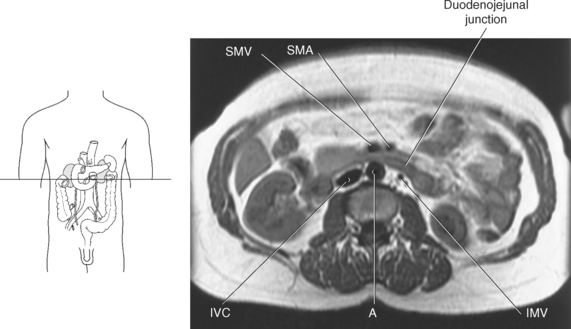
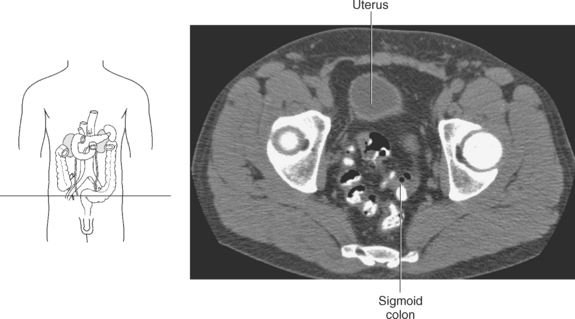
Figure 7.118 Axial, T1-weighted MR scan at duodenojejunal junction.
Key: SMV, superior mesenteric vein; SMA, superior mesenteric artery; IVC, inferior vena cava; A, aorta; IMV, inferior mesenteric vein.
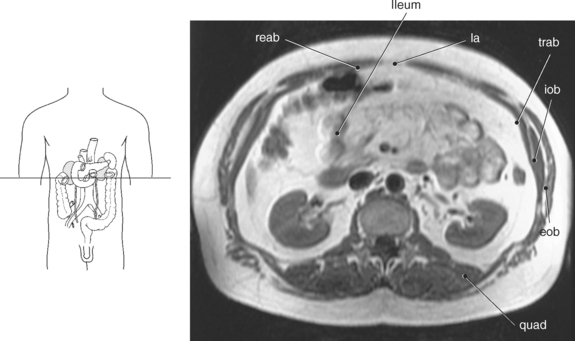
Figure 7.120 Axial, T1-weighted MR scan with ileum.
Key: reab, rectus abdominis; la, linea alba; trab, transverse abdominis; iob, internal oblique; eob, external oblique; quad, quadratus lumborum.
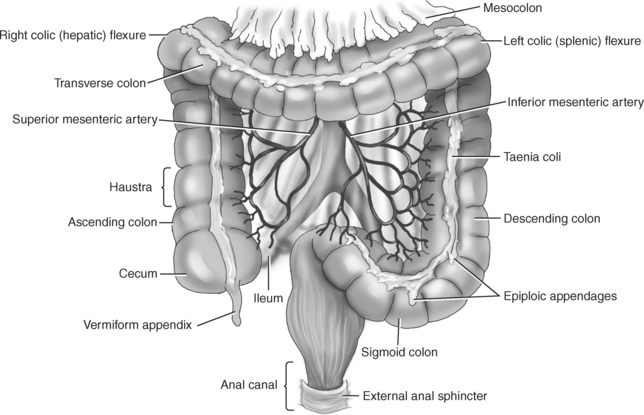
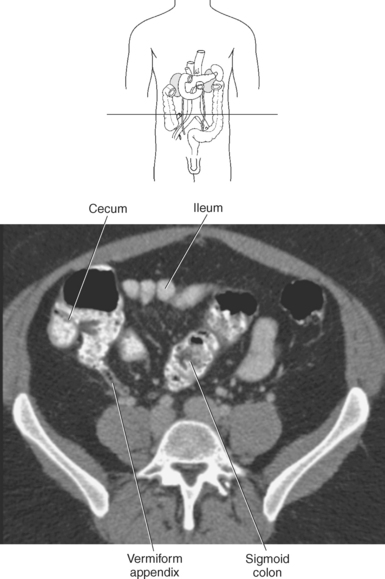
The large intestine (large bowel) lies inferior to the stomach and liver and almost completely frames the small intestine (Figures 7.115 and 7.123). The large intestine has a larger diameter and thinner walls than the small intestine and is approximately 1.5 meters long, starting at the ileocecal junction and ending at the anus. The outer, longitudinal muscle of the large intestine forms three thickened bands called taenia coli that gather the cecum and colon into a series of pouchlike folds called haustra. On the outer surface of the large intestine are small fat-filled sacs of omentum called the epiploic appendages. The three main divisions of the large intestine are the cecum, colon, and rectum (Figure 7.123). The cecum is a pouchlike section of the proximal portion of the large intestine located at the ileocecal valve. The slender vermiform appendix attaches to the posteromedial surface of the cecum (Figures 7.123 through 7.125). The colon is the longest portion of the large intestine and can be subdivided into four distinct portions: ascending, transverse, descending, and sigmoid (Figures 7.126 and 7.127). The ascending colon is retroperitoneal and commences at the cecum, ascending the right lateral wall of the abdomen to the level of the liver. It then curves sharply to the left, creating the hepatic flexure (Figures 7.123, 7.128, and 7.129). The hepatic flexure marks the beginning of the transverse colon. The transverse colon travels horizontally across the anterior abdomen toward the spleen, where it bends sharply downward, creating the splenic flexure and the beginning of the descending colon (Figures 7.130 and 7.131). The transverse colon is located within the peritoneal cavity and is the largest and most mobile portion of the large intestine, making its position quite variable in the patient. The descending colon is retroperitoneal and continues inferiorly along the left lateral abdominal wall to the iliac fossa, where it curves to become the S-shaped sigmoid colon posterior to the bladder (Figure 7.123). The sigmoid colon joins the rectum, which is the terminal portion of the colon (Figures 7.132 and 7.133). The rectum is considered a pelvic organ and is covered in greater detail in Chapter 8. The superior and inferior mesenteric arteries and veins supply and drain blood from the large intestine. The major functions of the large intestine include the reabsorption of water and the storage and elimination of fecal material.
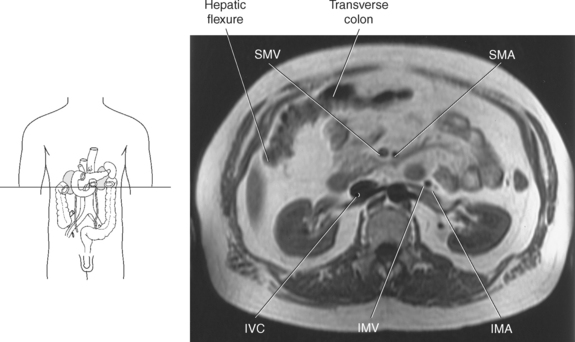
Figure 7.128 Axial, T1-weighted MR scan of hepatic flexure and transverse colon.
Key: SMV, Superior mesenteric vein; SMA, superior mesenteric artery; IVC, inferior vena cava; IMV, inferior mesenteric vein; IMA, inferior mesenteric vein.
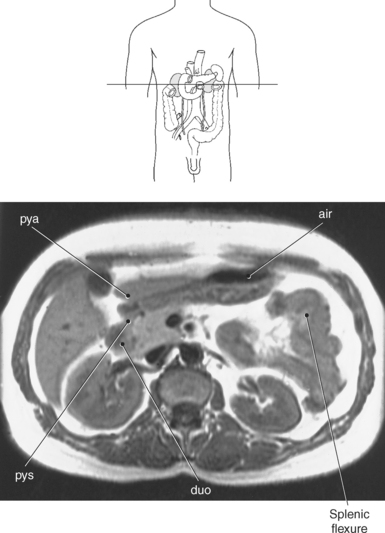
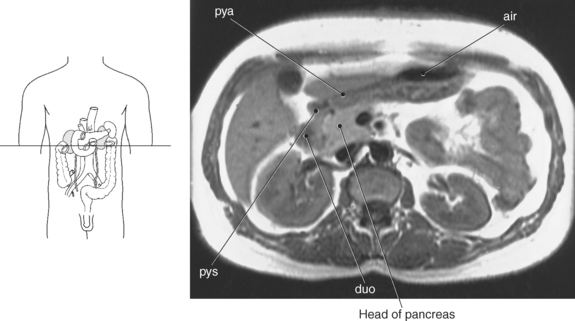
Figure 7.130 Axial, T1-weighted MR scan of splenic flexure.
Key: pya, pyloric antrum; air, air in stomach; pys, pyloric sphincter; duo, duodenum.
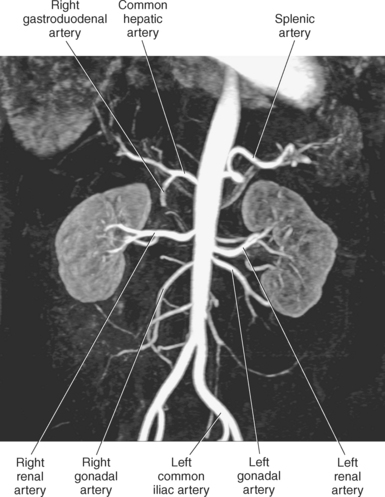
ABDOMINAL AORTA AND BRANCHES
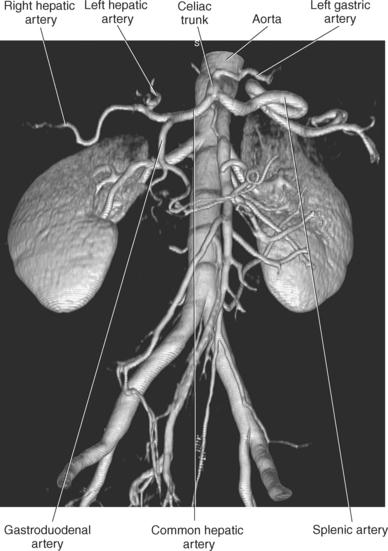
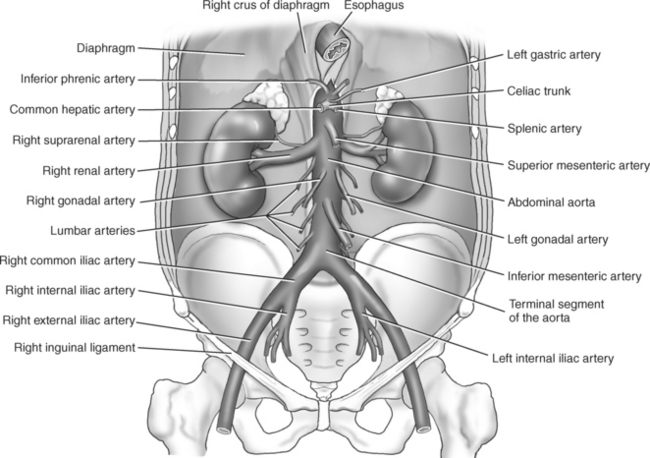
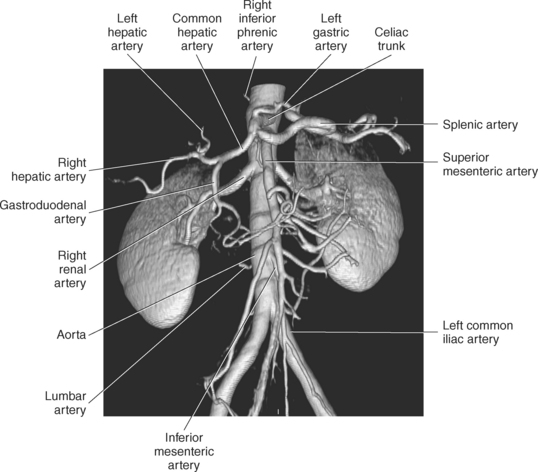
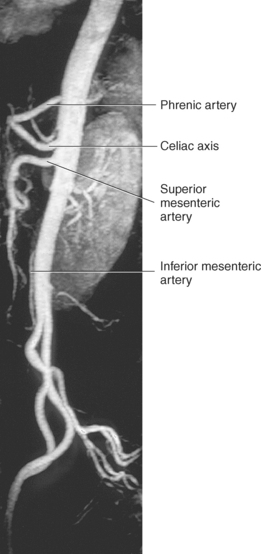
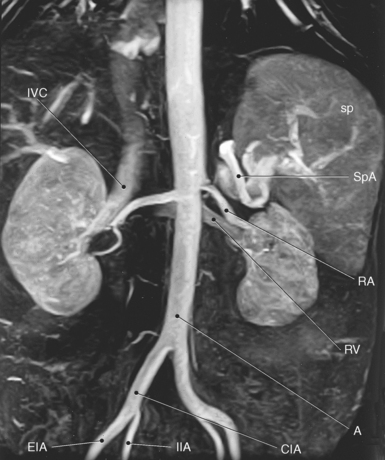
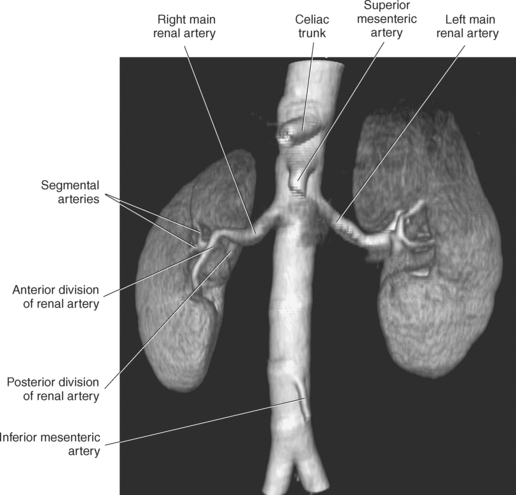
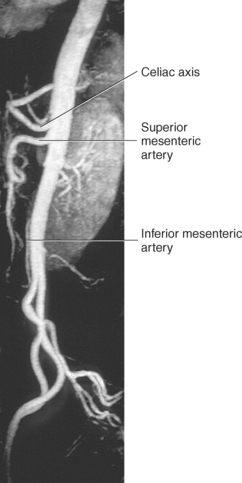
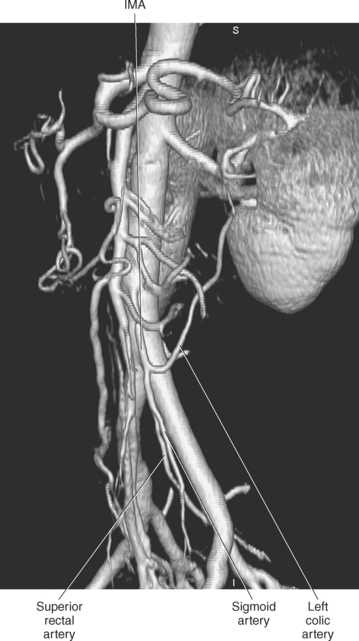
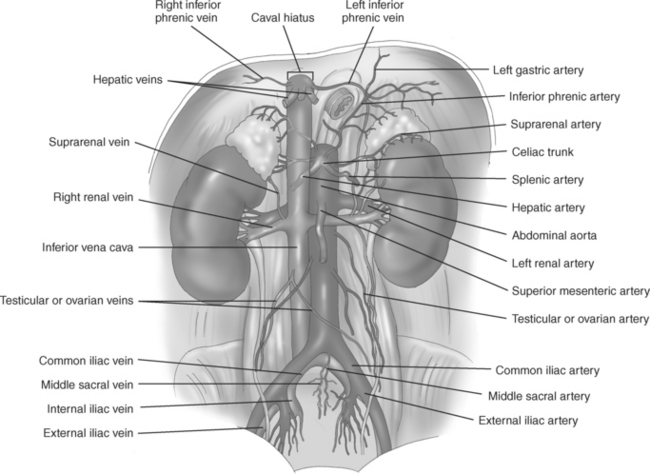
The abdominal aorta is a retroperitoneal structure beginning, as an extension of the thoracic aorta, at the aortic hiatus of the diaphragm. The abdominal aorta has a gradual diminishment of its diameter as it descends the abdomen just left of the midline next to the vertebral bodies. It delivers blood to all the abdominopelvic organs and structures. At approximately the level of L4, the abdominal aorta bifurcates into the right and left common iliac arteries. The branches of the abdominal aorta can be divided into the paired (dorsal) parietal branches, including the inferior phrenic and lumbar arteries; paired visceral branches, including the suprarenal, renal, and gonadal arteries; and unpaired (ventral) visceral branches that include the celiac trunk, splenic, superior mesenteric, and inferior mesenteric arteries (Figures 7.134 through 7.136). Each of these branches has a typical configuration that is described within this text; however, many normal variations of these vessels may occur.

Figure 7.135 MR angiogram of abdominal aorta.
Key: IVC, Inferior vena cava; k, kidney; IIA, internal iliac artery; EIA, external iliac artery; CIA, common iliac artery; A, aorta; RV, renal vein; RA, renal artery; SpA, splenic artery; sp, spleen.
Paired Parietal (Dorsal) Branches
The parietal (dorsal) branches supply the diaphragm and trunk wall and include the inferior phrenic and lumbar arteries. The paired inferior phrenic arteries are first to branch from the lateral surface of the abdominal aorta just as it descends through the aortic hiatus. The right inferior phrenic artery passes upward on the right side behind the IVC, and the left inferior phrenic artery passes behind the stomach and the abdominal part of the esophagus (Figures 7.134 and 7.137). The phrenic arteries extend to supply the inferior surface of the diaphragm and dispatch the superior suprarenal arteries to the upper pole of the suprarenal glands (Figure 7.138).
Four pair of lumbar arteries arise from the posterior wall of the abdominal aorta at the level of L1-L4 (Figures 7.134 and 7.136). The lumbar arteries supply the posterior abdominal wall, lumbar vertebrae, and the inferior end of the spinal cord (see Chapter 4 for branches of the lumbar arteries). Extending from the dorsal wall of the aorta, somewhat above the aortic bifurcation, is the median sacral artery, which continues caudally in front of the sacrum. It gives off the fifth pair of lumbar arteries as lateral branches and terminates anterior to the apex of the coccyx.
Paired Visceral Branches
The middle suprarenal arteries exit the lateral walls of the aorta near the base of the superior mesenteric artery. These arteries course laterally and slightly superiorly to supply the adrenal glands. The superior suprarenal arteries are branches of the inferior phrenic arteries, and the inferior suprarenal arteries extend from the renal arteries (Figures 7.134 and 7.138).
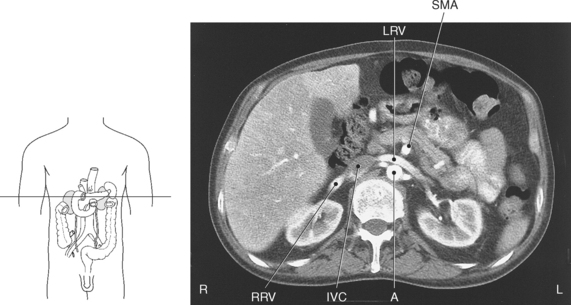
Renal Arteries
The two large renal arteries arise from the lateral walls of the aorta just below the superior mesenteric artery. Each vessel travels horizontally to the hilum of the corresponding kidney (Figures 7.134 through 7.136). Because of the position of the aorta on the left side of the vertebral column, the right renal artery is slightly longer than the left renal artery. The right renal artery passes posterior to the inferior vena cava and right renal vein on its course to the right kidney (Figure 7.139). Typically, the left kidney is higher than the right kidney, which means the left renal artery is generally slightly superior to the right (Figure 7.140). As each renal artery reaches the renal hilum, it typically divides into anterior and posterior branches from which five segmental arteries—apical, upper, middle, lower, and posterior—arise (Figures 7.141 through 7.143). Each segmental artery further divides into lobar arteries, one for each pyramid and adjoining cortex.
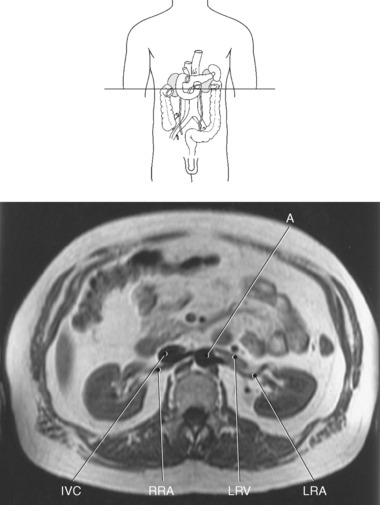
Figure 7.139 MRA of abdomen with renal arteries and veins.
Key: A, Aorta; IVC, inferior vena cava; RRA, right renal artery; LRV, left renal vein; LRA, left renal artery.
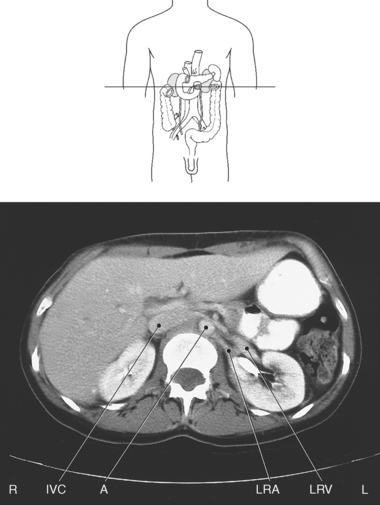
Figure 7.140 Axial CT scan of abdomen with renal arteries and veins.
Key: A, Aorta; IVC, inferior vena cava; LRV, left renal vein; LRA, left renal artery.
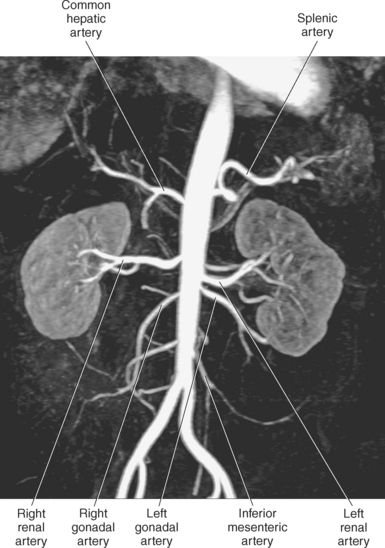
Gonadal Arteries
The gonadal arteries originate from the anterior wall of the aorta just inferior to the renal arteries. They descend along the psoas muscles to reach their respective organs (Figures 7.134, 7.144, and 7.145). In the male, the gonadal arteries are termed the testicular arteries, which supply the testes and scrotum, whereas the gonadal arteries in the female are termed the ovarian arteries and supply the ovaries, uterine tubes, and uterus.
Unpaired Visceral Branches
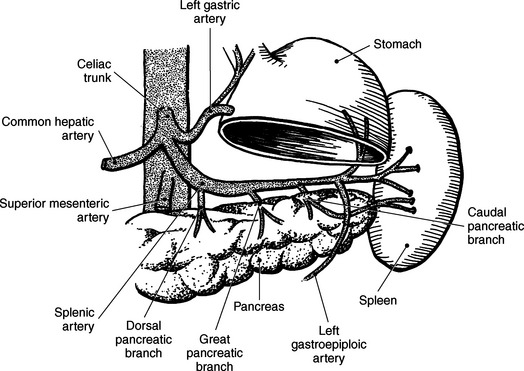
The celiac trunk is a very short vessel that leaves the anterior wall of the aorta just after the aorta passes through the diaphragm. The short celiac trunk divides into three branches: left gastric, common hepatic, and splenic arteries (Figures 7.146 through 7.148). Variations of the celiac trunk are not rare; occasionally the hepatic artery will branch from the superior mesenteric artery.
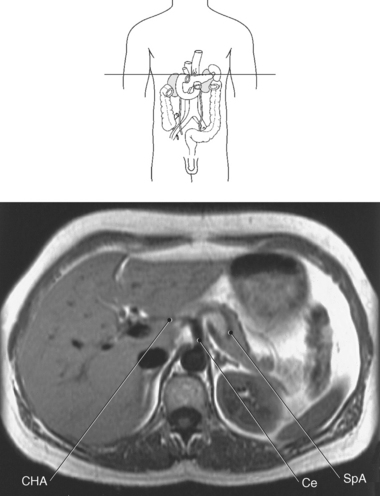
Figure 7.147 Axial, T1-weighted MR scan of abdomen with celiac trunk.
Key: CHA, common hepatic artery; Ce, celiac axis; SpA, splenic artery.
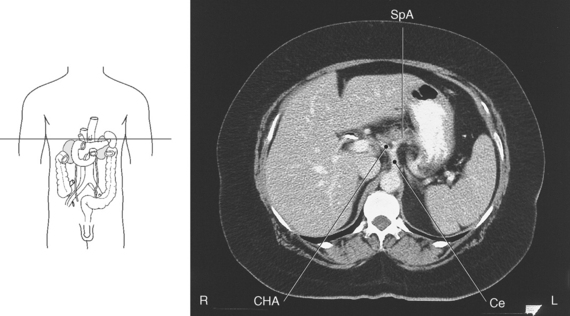
Figure 7.148 Axial CT scan of abdomen with celiac trunk.
Key: SpA, splenic artery; CHA, common hepatic artery; Ce, celiac axis.
The left gastric artery courses superiorly and leftward within the lesser omentum to supply the cardiac region of the stomach then passes along the lesser curvature toward the pylorus, giving off esophageal and gastric branches to supply the abdominal esophagus and adjacent anterior and posterior walls of the body of the stomach. The left gastric artery continues toward the right to anastomose with the right gastric artery, which is a branch of the hepatic artery (Figures 7.146 and 7.149 through 7.152).
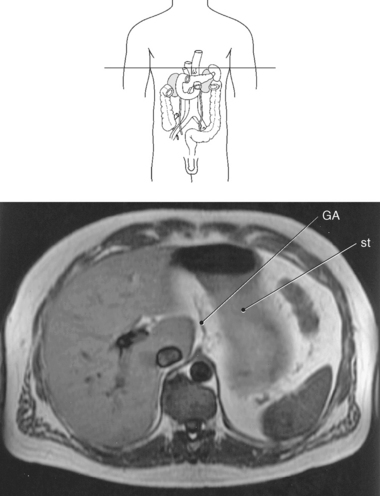
Figure 7.149 Axial, T1-weighted MR scan of abdomen with gastric artery.
Key: GA, left gastric artery; st, stomach.
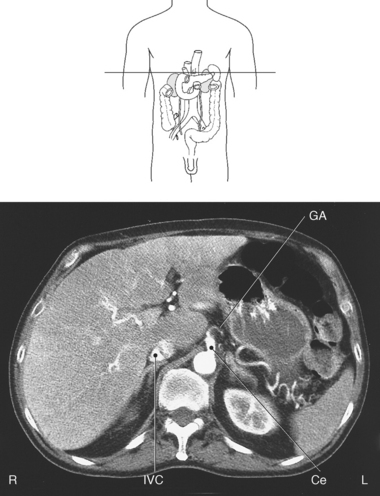
Figure 7.150 Axial CT scan of abdomen with gastric artery.
Key: Ce, celiac axis; GA, left gastric artery; IVC, inferior vena cava.
The common hepatic artery crosses to the right toward the superior aspect of the duodenum and divides into the hepatic artery proper and the gastroduodenal artery (Figures 7.146 through 7.148 and 7.151 and 7.152). The hepatic artery proper ascends obliquely to the right in the hepatoduodenal ligament, adjacent to the portal vein and common bile duct, and divides near the porta hepatis into the right and left hepatic branches and usually gives off the right gastric artery (Figures 7.146, 7.151, and 7.152). The right hepatic branch dispatches the cystic artery to the gallbladder and divides into the anterior and posterior segmental arteries to supply the segments of the right and caudate lobes of the liver. The left branch also gives off an artery to the caudate lobe, as well as medial and lateral segmental arteries to supply the segments of the left lobe and the intermediate branch to the quadrate lobe. The right gastric artery, which can also come from the common hepatic or gastroduodenal arteries, supplies the lower part of the lesser curvature of the stomach and anastomoses with the left gastric artery within the lesser curvature of the stomach (Figures 7.146 and 7.151). The gastroduodenal artery descends behind the pylorus to give off many branches, including the anterior and posterior superior pancreaticoduodenal arteries, which supply the superior part of the duodenum and head of the pancreas, and the right gastroepiploic (gastro-omental) artery. The right gastroepiploic artery passes in the greater omentum, anastomoses with the left gastroepiploic artery on the inferior surface of the greater curvature, and dispatches numerous gastric branches to the anterior and posterior walls of the pyloric and body portions of the stomach (Figures 7.146, and 7.151 through 7.153).
The splenic (lienal) artery is the largest branch of the celiac trunk and passes to the left behind the stomach and along the upper border of the pancreas, within the splenorenal ligament, to the hilum of the spleen. At the point where the splenic artery courses near the border of the pancreas, it gives off numerous pancreatic branches that supply the body and tail of the pancreas, including the dorsal, great, and caudal pancreatic arteries (Figure 7.154). Just before the splenic artery terminates into numerous splenic branches, it gives rise to the left gastroepiploic (gastro-omental) artery, which gives off epiploic and gastric branches to the greater omentum and anterior and posterior walls of the fundus of the stomach (Figures 7.146 and 7.151 through 7.156).
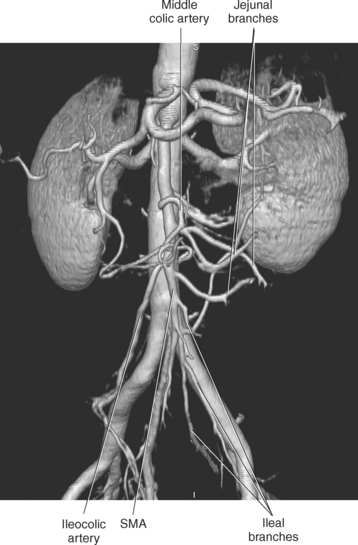
Superior Mesenteric Artery
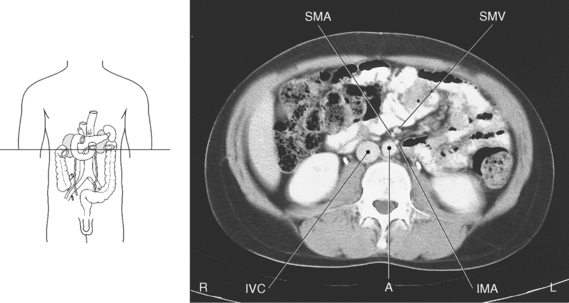
The large superior mesenteric artery branches just below the celiac trunk at approximately the level of L1 (Figures 7.134, 7.157, and 7.158). It descends behind the body of the pancreas, then over the horizontal portion of the duodenum to course in the mesentery to the ileum (Figures 7.157, 7.159, and 7.160). The artery supplies the head of the pancreas and the majority of the small and large intestines. Branches of the superior mesenteric artery include the inferior pancreaticoduodenal artery, jejunal arteries, ileal arteries, middle colic artery, right colic artery, and ileocolic artery (Figure 7.161). The inferior pancreaticoduodenal artery extends to the head of the pancreas and duodenum, then divides into the posterior ramus anastomosing with the posterior superior pancreaticoduodenal artery and the anterior ramus, which anastomoses with the anterior superior pancreaticoduodenal artery. The jejunal and ileal arteries extend to supply the jejunum and ileum, except the end segment near the cecum. The middle colic artery reaches the transverse colon and the right colic artery passes to the ascending colon. The ileocolic artery courses behind the peritoneum across the right ureter into the right iliac fossa and divides to supply a portion of the ascending colon, the cecum, vermiform appendix, and terminal portion of the ileum (Figures 7.162 and 7.163).
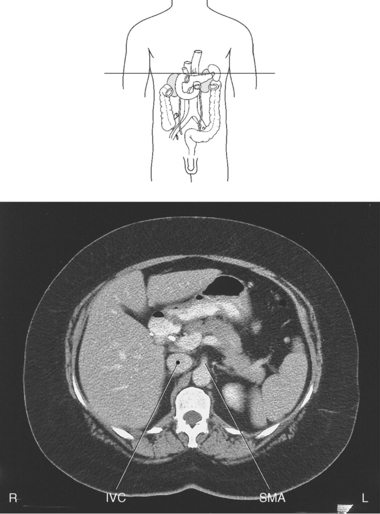
Figure 7.158 Axial CT scan with superior mesenteric artery.
KEY: IVC, Inferior vena cava; SMA, superior mesenteric artery.
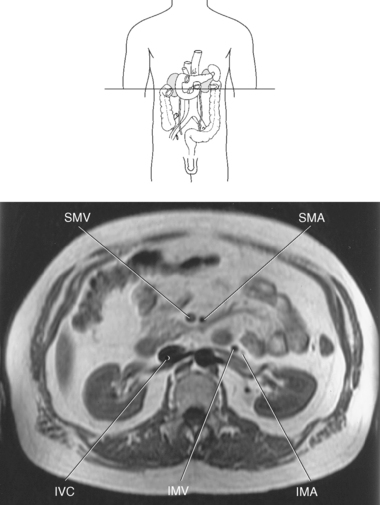
Figure 7.159 Axial, T1-weighted MR scan of superior mesenteric vessels.
KEY: IVC, Inferior vena cava; SMA, superior mesenteric artery; SMV, superior mesenteric vein; IMV, inferior mesenteric vein; IMA, inferior mesenteric vein.
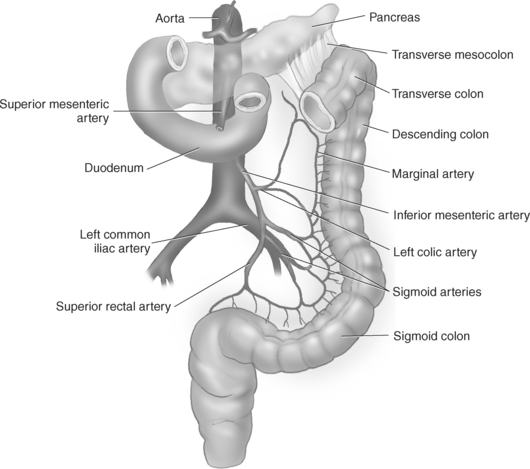
Inferior Mesenteric Artery
The inferior mesenteric artery arises 3 to 4 cm above the bifurcation of the aorta at approximately the level of L3-L4. It descends in front of the abdominal aorta and then to the left, where it gives off the left colic artery, sigmoid arteries, and the superior rectal arteries (Figures 7.159, 7.160, and 7.164). The left colic artery is a retroperitoneal structure that passes along the posterior body wall on the anterior surface of the left psoas and quadratus lumborum muscles. It bifurcates into ascending and descending branches that supply the walls of the left third of the transverse colon and the entire descending colon. The sigmoid branches (2 or 3) course within the mesentery to supply branches to the terminal descending colon and to the sigmoid colon. The superior rectal artery crosses the common iliac artery and vein as it descends to branch and supply the rectum (Figures 7.165 through 7.166).
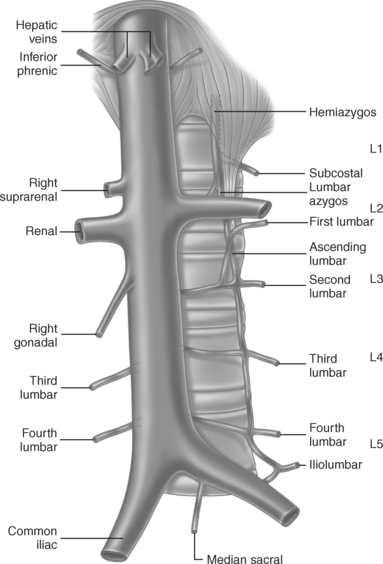
INFERIOR VENA CAVA AND TRIBUTARIES
The IVC is the largest vein of the body (Figure 7.167). It carries blood to the heart from the lower limbs, pelvic organs and the abdominal viscera, and abdominal wall. The IVC is formed by the union of the common iliac veins at approximately the level of L5. It courses superiorly through the retroperitoneum along the anterior aspect of the vertebral column and to the right of the aorta (Figures 7.159 and 7.160). As the IVC ascends the abdominal cavity, it passes the posterior surface of the liver and pierces the diaphragm at the caval hiatus to enter the right atrium of the heart. The IVC receives many tributaries throughout its course in the abdomen that include the inferior phrenic, lumbar, right gonadal, renal, right suprarenal, and hepatic veins (Figure 7.167).
Inferior Phrenic Veins
The inferior phrenic veins extend from the inferior surface of the diaphragm. The left inferior phrenic vein is often doubled and drains into either the left suprarenal vein or to the left renal vein. The right inferior phrenic vein drains directly into the inferior vena cava (Figure 7.167).
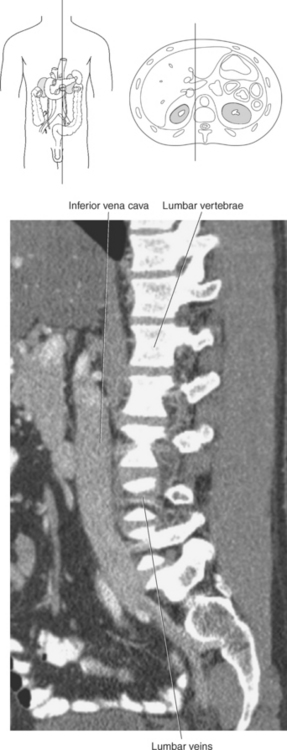
Lumbar Veins
The lumbar veins consist of four pairs of vessels that collect blood from the posterior abdominal wall from the level of L1 to L4 (Figures 7.168 through 7.170). They receive veins from the vertebral plexuses and then travel horizontally along the transverse processes deep to the psoas muscles. The lumbar veins on the left are typically longer than those on the right because they must cross over the vertebral column to drain into the IVC. The arrangement of these veins varies, with some entering the lateral walls of the IVC and others emptying into the common iliac vein or are united on each side by a vertical connecting vein termed the ascending lumbar vein. Typically, the right ascending lumbar vein continues as the azygos vein and the left ascending lumbar vein continues as the hemiazygos vein. Additionally, a diminutive median sacral vein may accompany the median sacral artery. It typically drains into the left common iliac vein but may also drain into the junction of the common iliac veins (Figure 7.167).
Gonadal Veins
The gonadal veins, ovarian in females and testicular in males, ascend the abdomen along the psoas muscle, anterior to the ureters. The right gonadal vein enters the anterolateral wall of the IVC just below the opening for the right renal vein, whereas the left gonadal vein empties into the left renal vein (Figures 7.144, 7.145, and 7.167).
Renal Veins
Blood leaves the kidney by way of interlobular veins that carry blood from the renal cortex to the arcuate veins, which carry blood from the medulla to the interlobar veins. The interlobar veins join to form the renal vein at the renal hilum (Figure 7.141). The renal veins pass anterior to the renal arteries to empty into the IVC at about the level of L2. The left renal vein passes posterior to the superior mesenteric artery and anterior to the aorta on its route from the left kidney to enter the left lateral wall of the IVC. It receives the left gonadal vein, left inferior phrenic vein, and generally the left suprarenal vein. The shorter right renal vein is typically lower than the left renal vein as it travels its short course to enter the right lateral wall of the IVC (Figures 7.167, 7.171, and 7.172).
Suprarenal Veins
The right suprarenal vein courses from the medial side of the right suprarenal gland to empty directly into the IVC. The left suprarenal vein courses from the inferior pole of the left suprarenal gland to empty directly into the left renal vein or left inferior phrenic vein (Figures 7.167 and 7.168).
Hepatic Veins
The three short hepatic veins (right, middle, left) begin as smaller vessels that collect blood from the liver parenchyma. The hepatic veins course from the inferior aspect of the liver to the superior aspect of the liver, where they empty into the IVC just below the diaphragm. In general, the right and left hepatic veins drain the right and left lobes of the liver, respectively, whereas the middle hepatic vein drains the medial segment of the left lobe and the anterior portions of the right (see Liver section, Figures 7.61, 7.62, and 7.167).
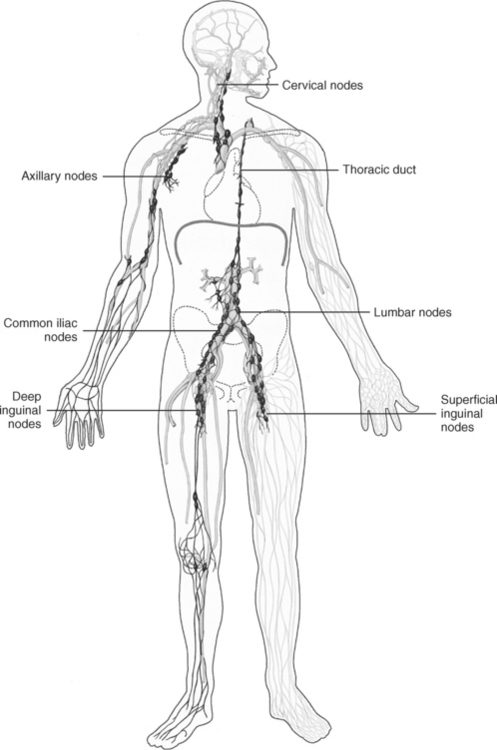
LYMPH NODES
Many lymph nodes exist within the abdominal cavity. Abdominal lymph nodes occur in chains along the main branches of the arteries of the intestine and abdominal aorta. Most abdominal lymph nodes appear as small oblong soft tissue masses oriented parallel to their accompanying vessels and may be difficult to visualize in cross section unless they are enlarged as a result of an abnormality. Typically, lymph nodes are considered enlarged if their short axis diameter is greater than 1 cm. Abdominoaortic nodal groups surround the aorta and IVC and visceral lymph nodes drain adjacent organs that include the mesenteric hepatic, splenic, and pancreaticoduodenal nodal groups. Lymph from the abdominal cavity empties into the lumbar trunk, which drains lymph from the legs, lower abdominal wall, and the pelvic organs; and the intestinal trunk, which drains organs located within the abdominal cavity. These trunks then join the thoracic duct and ultimately enter the venous system (Figures 7.173 through 7.175).
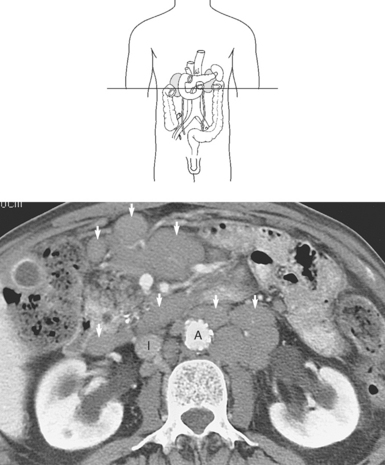
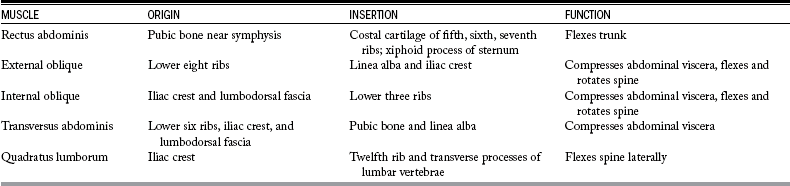
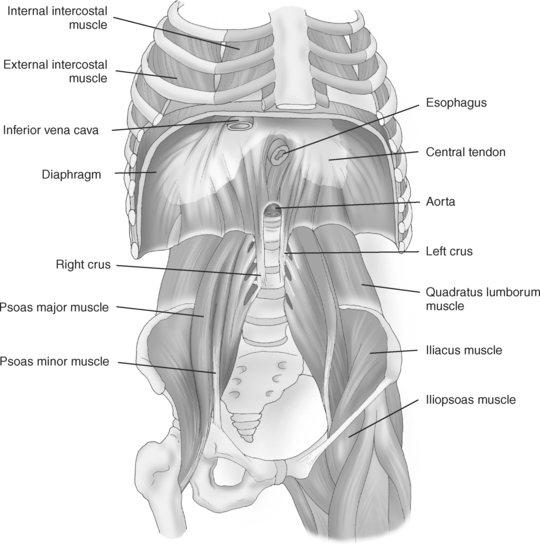
MUSCLES OF THE ABDOMINAL WALL
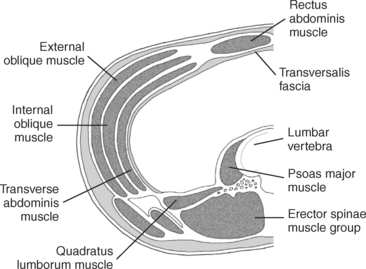
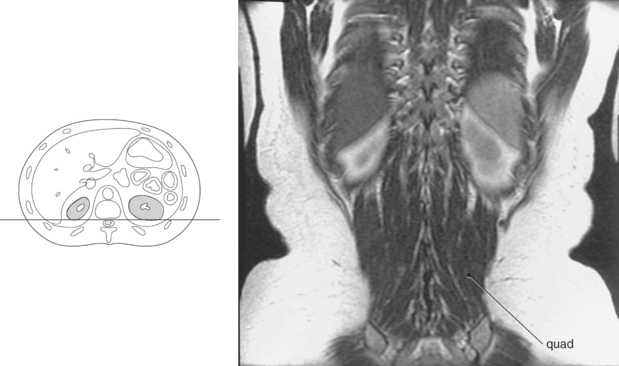
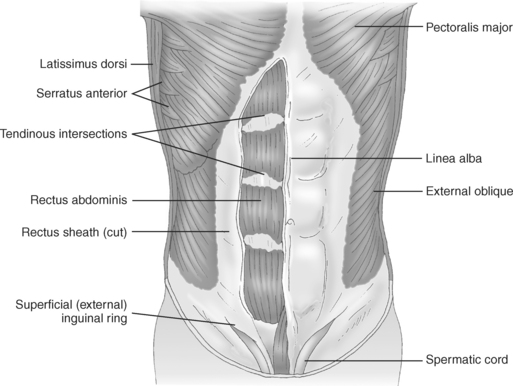
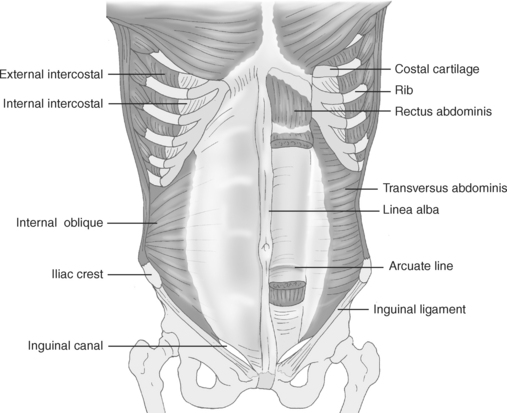
The abdominal wall is formed superiorly by the diaphragm and is inferiorly continuous with the pelvic cavity at the pelvic inlet. Posteriorly, the abdominal wall is formed by the five lumbar vertebrae, twelfth pair of ribs, upper portion of the pelvis, quadratus lumborum muscles, and psoas muscles (Figure 7.176). The quadratus lumborum muscle forms a large portion of the posterior abdominal wall. It extends from the iliac crest to the inferior border of the twelfth rib and transverse processes of the lumbar vertebrae to aid in lateral flexion of the vertebral column. The large psoas muscles extend along the lateral surfaces of the lumbar vertebrae to insert on the lesser trochanter of the femur and act to flex the thigh and trunk (Figures 7.177 through 7.180). Anteriorly, the abdominal wall is formed by the lower portion of the thoracic cage and by layers of muscles that include the rectus abdominis, external oblique, internal oblique, and transversus abdominis (Figures 7.181 and 7.182). The paired rectus abdominis muscles, visualized on the anterior surface of the abdomen and pelvis, originate from the pubic symphysis and extend vertically to the xiphoid process and costal cartilage of the fifth, sixth, and seventh ribs. They function to flex the lumbar vertebrae and support the abdomen (Figures 7.177 and 7.179). The anterior surface of the rectus muscle is crossed by three tendinous intersections that course transversely, forming individual muscle bellies that can contract separately (Figure 7.181). A longitudinal band of fibers that forms a central anterior attachment for the muscle layers of the abdomen is the linea alba, which extends from the xiphoid process of the sternum to the pubic symphysis. The linea alba is formed, at the midline, by the interlacing of fibers from the rectus abdominis and oblique muscles (Figures 7.178, 7.179, and 7.182). The external and internal oblique muscles are located on the outer lateral portion of the abdomen and extend from the cartilages of the lower ribs to the level of the iliac crest (Figures 7.177, 7.179, and 7.181 through 7.183). The oblique muscles work together to flex and rotate the vertebral column and compress the abdominal viscera. The external oblique is the most extensive of the three broad abdominal muscles and contains a triangular opening, the superficial inguinal ring, that allows for the passage of the spermatic cord or round ligament of the uterus (Figure 7.181). The inguinal ligament is a fibrous band formed by the thickened inferior border of the aponeurosis of the external oblique muscle. It extends from the anterior superior iliac spine to the pubic tubercle and gives origin to the lowermost fibers of the internal oblique and transversus abdominis muscles (Figure 7.182). The transversus abdominis muscle lies deep to the internal oblique muscles. Its fibers extend transversely across the abdomen to provide maximum support for the abdominal viscera. The transversus abdominis muscle extends from the lower six costal cartilages, lumbar fascia, iliac crest, and inguinal ligament to insert into the xiphoid process, linea alba, and pubic symphysis (Figures 7.177, 7.179, and 7.183 and Table 7.3).
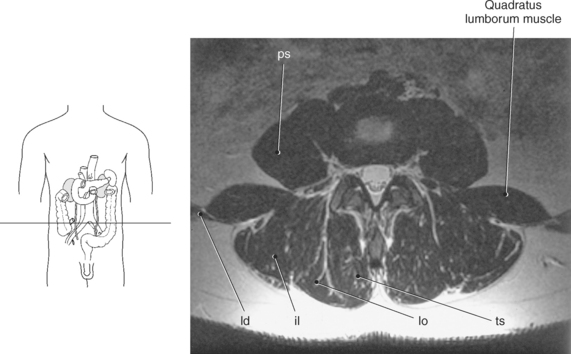
Figure 7.178 Axial, T1-weighted MR scan of psoas and quadratus lumborum muscles.
Key: ps, psoas muscles; ld, latissimus dorsi; il, iliocostalis muscle; lo, longissimus muscle; ts, transversospinal muscles.
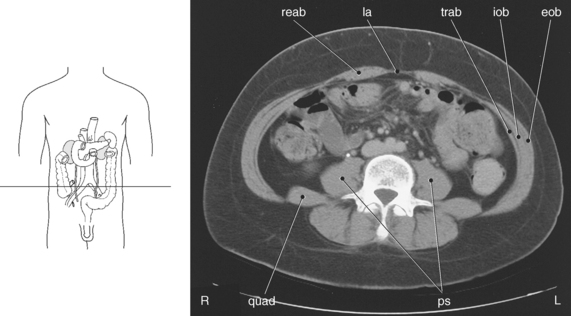
Figure 7.179 Axial CT scan of psoas and quadratus lumborum muscles.
Key: ps, psoas muscles; reab, rectus abdominis; la, linea alba; trab, transverse abdominis; iob, internal oblique; eob, external oblique; quad, quadratus lumborum.