CARDIOVASCULAR DIAGNOSTIC TESTS
Assessment of the client with a suspected circulatory system disorder, or evaluation of the progress of a disorder, requires that certain cardiovascular tests be performed.
Assessment of cardiac function
Electrocardiography (ECG)
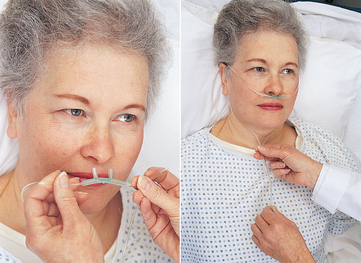
Electrocardiography (ECG) (Fig 23.21) provides a graphical record, or trace, that represents the heart’s electrical action. Cellular activity of the cardiac muscle generates electrical impulses that flow through the heart. This electrical activity can be measured by a system of electrodes placed at specific points on the body surface. The ECG displays the electrical activity as waveforms, which are named P, Q, R, S and T waves. The ECG recording illustrates the rate and rhythm of electrical conduction and cardiac contractions through the heart. Abnormalities indicate enlargement of the chambers, inflammation of the pericardium or damage to the myocardium. Exercise electrocardiography (stress test) measures the cardiovascular effects of controlled physical stress, such as treadmill walking. Ambulatory (Holter) electrocardiography records the heart’s electrical activity for a specified time, for example, 24 hours, as the client performs their usual activities. See Procedural Guideline 23.2.
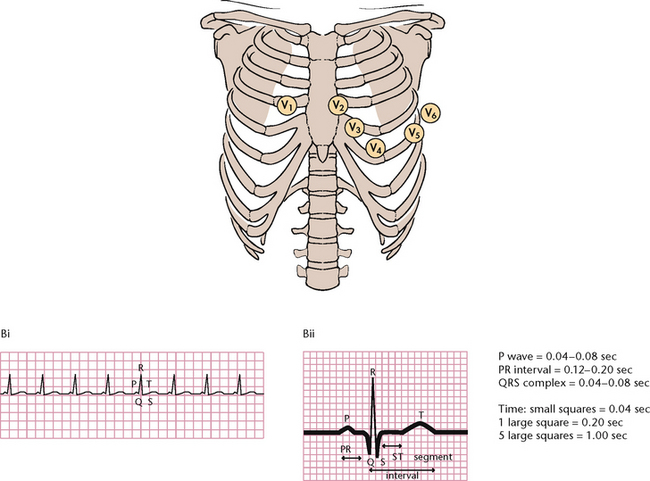
Figure 23.21 Electrocardiogram (ECG) A: Placement of the chest leads B: A normal ECG (i) Regular sinus rhythm. (ii) Detail of an ECG
(A: Lewis et al 2004)
Procedural Guideline 23.2 Performing an ECG
| Review and carry out the standard steps for all nursing procedures/interventions |
Echocardiography
Echocardiography is a painless non-invasive test that directs ultra-high-frequency soundwaves through the chest wall into the heart, which then reflects those waves to a transducer and a recording device. As the sound transects the various heart structures, echoes are produced and recorded. Echocardiography evaluates cardiac structure and function and can reveal valve deformities, septal defects, cardiomyopathy and pericardial effusion.
Nuclear cardiology
Nuclear cardiology involves the use of radioactive tracers to evaluate myocardial blood flow and the status of myocardial cells. An IV injection, for example of the radioisotope thallium-201 or gallium, is administered to the client while they are exercising, and a scan performed to detect thallium uptake. Healthy myocardial tissue absorbs the radioisotope, but ischaemic or necrotic tissue does not.
Cardiac catheterisation
Cardiac catheterisation involves the insertion of a catheter into the right or left side of the heart to obtain information on cardiac pressures, cardiac output, oxygenation and heart valve function. The catheter is inserted through a vein in the arm or the groin and advanced into the vena cava; the passage of the catheter is observed on a fluorescent screen and x-ray films are taken. A contrast medium may be injected through the catheter and x-ray films taken (angiography). For coronary angiography, the catheter is advanced into the aortic arch and positioned into a coronary artery; a contrast medium is then injected to outline the coronary arteries as a series of x-ray films is taken.
Digital subtraction angiography
Digital subtraction angiography is less invasive than conventional angiography and involves injecting contrast dye into the venous system rather than directly into an artery. As the dye circulates through the heart and arterial system, a fluoroscopic image intensifier displays the vessels and focuses the image. A computer then converts the images into numbers. Several vessels can be evaluated with one injection of contrast dye.
Phonocardiography
Phonocardiography graphically records heart sounds produced as blood flows through the heart and great vessels. Microphones are placed on the chest, usually at the apex and base of the heart, and the sounds are picked up and converted into electrical impulses. The impulses are relayed to a recorder, which provides a graph of the heart sounds in wave form.
Central venous pressure
The central venous pressure test measures the functioning of the right atrium. A catheter, which is threaded through the subclavian or jugular vein into or near the right atrium, is connected to a manometer. This procedure enables accurate determination of right atrial blood pressure, which reflects right ventricular pressure. This test is also used to assess blood volume.
Intracardiac pressure monitoring
This test involves the insertion of a balloon-tipped flow-directed catheter, such as the Swan–Ganz catheter, into a large vein and then advancing it until it reaches the right atrium. Once the balloon is inflated, the flow of blood carries the catheter into the pulmonary artery. The procedure permits measurement of both pulmonary artery pressure (PAP) and pulmonary artery wedge pressure (PAWP). In addition, this procedure evaluates pulmonary vascular resistance and tissue oxygenation.
Assessment of peripheral blood vessels
Skin temperature studies
Skin temperature studies may be performed to evaluate skin temperature of the extremities, which helps determine adequacy of blood circulation in arterial disease. Direct skin temperature readings are taken; in arterial disease the temperature in the extremities may be lower than in other body areas. The cold stimulation test may be used to demonstrate Raynaud’s syndrome by recording temperature changes in the client’s fingers before and after their submersion in ice water. Normally digital temperature returns to pre-test level within 15 minutes, but with Raynaud’s syndrome return to pre-test level takes longer than 20 minutes.
Doppler ultrasonography
Doppler ultrasonography involves the transmission of sound waves through the skin, which are reflected from moving blood cells in underlying blood vessels. This test evaluates blood flow in the major veins and arteries in the limbs, and helps to detect peripheral vascular aneurysms and deep vein thrombosis (DVT).
Arteriography
Arteriography (angiography) is the radiographic examination of one or more arteries after injection of a contrast medium into a major artery, usually the femoral artery. Arteriography can demonstrate blood flow status, collateral circulation, vascular anomaly and tumour and aneurysm formation.
Lower limb venography
Lower limb venography is the radiographic examination of a vein after an injection of contrast medium and is often used to assess the condition of the deep leg veins. Venography is the definitive test for DVT but may also be used to distinguish clot formation from other forms of venous obstruction or to locate a suitable vein for arterial bypass grafting.
Assessment of haematological status
Red blood cell (RBC) count
Red blood cell (RBC) (erythrocyte) count is the measurement of the number of erythrocytes found in a microlitre of blood. Together with haematocrit and haemoglobin determinations, this test is most often used to calculate mean corpuscular volume, mean corpuscular haemoglobin and mean corpuscular haemoglobin concentration.
Haematocrit
Haematocrit is a blood test used to measure the percentage of a given volume of blood occupied by erythrocytes.
Erythrocyte indices
Erythrocyte indices involve examination of the size, weight and haemoglobin content of the average erythrocyte (mean corpuscular haemoglobin and mean corpuscular haemoglobin concentration).
Total haemoglobin
Total haemoglobin measures the grams of haemoglobin (Hb) in 100 mL of whole blood.
Stained red cell examination
Stained red cell examination determines abnormalities in the size, shape or structure of erythrocytes.
Reticulocyte count
Reticulocyte count measures the number of reticulocytes present in a sample of blood, which is then expressed as a percentage of the total RBC count. (Reticulocytes are immature erythrocytes.)
Erythrocyte sedimentation rate (ESR)
ESR measures the time required for erythrocytes, in a sample of whole blood, to settle to the bottom of a vertical tube.
Erythrocyte osmotic fragility
Erythrocyte osmotic fragility measures red cell resistance to haemolysis when exposed to a hypotonic solution.
White blood cell (WBC) (leucocyte) count
WBC count is the measurement of the number of white cells found in a microlitre of whole blood. A differential WBC count determines the distribution and morphology of the various WBCs and provides more information about the immune system than the WBC count.
Coagulation
Coagulation function is measured by a wide variety of tests, including:
• Platelet count, which measures the number of circulating thrombocytes (platelets)
• Bleeding time, which measures the duration of bleeding after a standardised skin incision, commonly two small punctures made on the forearm
• Capillary fragility test, which measures the ability of capillaries to remain intact under increased intracapillary pressure. A blood pressure cuff is placed around the upper arm and inflated to midway between the systolic and diastolic pressures. After 5 minutes of sustained pressure, the number of petechiae on a selected area of the forearm are counted
• Clot retraction test, which estimates the quantity and quality of thrombocytes and fibrinogen
• Prothrombin time (PT), which measures the time required for a fibrin clot to form in a citrated plasma sample
• Partial thromboplastin time (PTT), which evaluates the entire coagulation system with the exception of Factors VII and XIII
• Factor VIII activity test, which measures the amount of Factor VIII in the blood and identifies a deficiency of that factor (e.g. as in haemophilia).
Immunoglobulin studies
Immunoglobulin studies evaluate the amount and types of immunoglobulins present.
Total iron-binding capacity (TIBC)
TIBC measures the amount of available transferrin (a protein that binds with iron) in the blood.
Sickle-cell test
Sickle-cell test detects the presence of haemoglobin S in suspected sickle-cell anaemia.
Gastric fluid analysis
Gastric fluid analysis involves measuring the acidity of secretions in the stomach and is used in the diagnosis of pernicious anaemia.
Bone marrow examination
Bone marrow examination provides information about the character, integrity and production of erythrocytes, leucocytes and thrombocytes in the marrow. Bone marrow can be removed by aspiration or needle biopsy. Aspiration of bone marrow involves the removal of a small amount, generally less than 5 mL. Biopsy, performed under local anaesthesia, is done when a larger amount of bone marrow is required. A needle is inserted through the skin and tissue, for example, over the iliac crest, until it reaches bone. The needle is then directed into the marrow cavity, and a sample of bone marrow is withdrawn.
Assessment of the lymphatic system
Lymphangiography is the radiographic examination of the lymphatic system after the injection of a contrast medium into a lymphatic vessel in each foot. X-ray films are taken to demonstrate the filling of the lymphatic vessels and, 24 hours later, to visualise the lymph nodes. Clinical Interest Box 23.5 outlines additional nursing assessment of oxygenation status.
CLINICAL INTEREST BOX 23.5 Nursing assessment—oxygenation status
NURSING A CLIENT WITH A RESPIRATORY AND/OR CARDIAC SYSTEM DISORDER
A holistic approach to nursing care should be delivered to clients with a respiratory or cardiac system disorder. Specific nursing actions and medical management will vary depending on the disorder; however, the main aims of nursing care are to:
• Maintain fluid and nutritional status
• Facilitate normal and effective breathing
• Promote efficient gas exchange
• Promote comfort and relieve pain
• Provide psychological support
• Promote and maintain mobility
A client with a respiratory system disorder will commonly experience problems such as a change in breathing pattern and discomfort associated with breathing. Clients with cardiac disorders may experience multi-system problems associated with circulation, including pain or discomfort with exercise, difficulty breathing, palpitations and fatigue. Nursing activities include alleviating discomforts associated with exercise and breathing, administering oxygen, positioning, monitoring the client and their vital signs and helping the client with cardiovascular and breathing exercises. As well as planning care to meet specific needs, nurses must also consider the client’s other needs, such as nutrition, fluid intake, skin integrity, elimination and the need for comfort.
Promoting a clear airway
One of the most important aspects of care is the maintenance or restoration of a clear airway, which includes measures directed at removing secretions. Commonly an inflammatory respiratory tract disorder results in the production of excessive secretions, made more tenacious by dehydration caused by tachypnoea, mouth breathing and pyrexia. The client may experience difficulty in maintaining a patent airway; some of the following steps may assist them in expectorating secretions.
Adequate hydration
Dehydration can make secretions more viscous and difficult to expectorate, so an adequate fluid input is important. Unless contraindicated, the client should be encouraged to drink at least 2–3 L a day. In certain conditions such as cardiac failure fluid may need to be restricted to 1500 mL or less. The nurse should assess fluid balance by measuring fluid input and output and by observing for signs of oedema. Weighing the client, for example, each day, is another way of assessing their fluid status. If they are unable to tolerate sufficient fluids orally because of dyspnoea, nausea and/or vomiting or the presence of an oxygen mask that can make drinking more difficult, alternative fluids may be administered by the IV route if necessary.
Maintaining nutritional status
Commonly a client with a cardiovascular disorder will be prescribed a diet that aims to reduce serum cholesterol and triglyceride levels. Sodium intake may also be reduced, for example, in the control and prevention of hypertension. If the client with either a respiratory or a cardiovascular disorder is obese, a weight-reduction diet is generally prescribed. The diet generally should be low in total fat content, particularly saturated fats, and low in sodium. Kilojoules may be reduced to correct or prevent obesity, and alcohol should be restricted, as it can raise kilojoule intake and serum lipid levels. Beverages and foods containing caffeine should be restricted, as caffeine is a metabolic stimulant that can worsen tachycardia, hypoxaemia and dysrhythmias.
In specific blood disorders the client may be prescribed a diet high in one or more nutrients, for example, a diet high in iron is generally prescribed in the treatment of iron-deficiency anaemia. When a specific diet is prescribed the dietitian consults with the client to plan the diet and to ensure that they understand any dietary modifications or restrictions.
It is important that nurses are aware of the type of diet that has been prescribed and ensure that the client receives the correct tray at mealtimes. Nurses encourage the client to follow the diet and may need to assist at mealtimes, for example, if the client is unable to eat meals independently. (Information on assisting at mealtime is provided in Chapter 28.)
Cessation of smoking
If the client is a smoker, they should be encouraged to stop smoking. Cigarette smoke impairs function of the cilia, and smoking generally aggravates any existing respiratory and cardiac disorder (see Clinical Scenario Box 23.1).
Clinical Scenario Box 23.1
My dad was a heavy smoker—2 packets a day. Then he had a pulmonary embolism (PE) which caused him to collapse 4 days after an emergency appendectomy. Dad spent 7 days in intensive care. Smoking was considered a major cause of the PE. This was such a shock to both dad and the family that he made the decision to give up smoking.
Now 20 years later, dad remains on warfarin, wears anti-embolic stockings and has not had a cigarette since his hospitalisation.
Gabrielle, daughter and RN
Nebulisation and humidification
As well as drinking adequate fluid, additional fluid may be administered directly into the airways by means of humidifiers, inhalations or nebulisers. Nebulisation or humidification reduces the viscosity of secretions, facilitating easy expectoration. Physiotherapy may be used concurrently. (Information on the use of humidifiers and nebulisers is provided later in this chapter.)
Positioning
If a client with a respiratory condition experiences dyspnoea, they should be assisted into a more upright position. This facilitates alveolar expansion, as gravity allows more blood to perfuse the bases of the lung, improving the ventilation/perfusion (V/Q) ratio. Nurses should ensure that sufficient pillows are placed so that the client’s back, neck, head and arms are well supported, or that the head of the bed is elevated.
Medication
Medications may be prescribed to reduce pain, loosen secretions, relieve bronchospasm, increase cilia beating speed, combat infection, increase or decrease coughing, relieve pulmonary oedema, alter blood pressure and cholesterol levels or correct dysrhythmias. Medications may be given by inhalation, orally or by intramuscular or IV routes. The types of medications prescribed may include analgesics, decongestants, antihistamines, antibiotics, bronchodilators or expectorants.
Oronasopharyngeal suction
If coughing is ineffective in removing secretions, suction may be necessary. Oronasopharyngeal suction removes secretions from the pharynx by means of a suction catheter inserted through the mouth or nostril. This technique is used to maintain a patent airway and is indicated for a client who is unable to clear their airway effectively with coughing and expectoration (see Procedural Guideline 23.3).
Procedural Guideline 23.3 Oronasopharyngeal suction
| Review and carry out the standard steps for all nursing procedures/interventions |
| Intervention | Rationale |
|---|---|
| Explain the procedure to the client and provide privacy | Reduces anxiety and embarrassment |
| If possible, position the client in a sitting position or with the neck extended | Promotes lung expansion and effective coughing. Facilitates catheter insertion |
| Perform hand hygiene. Put on gloves | Prevents cross-infection |
| Attach collection bottle to the suction unit, attach connecting tubing, connector and catheter | Equipment must be assembled and checked for function before the procedure starts |
| Turn on the suction and dip the tip of the catheter into the water | Lubricates the catheter to facilitate insertion |
| With the suction off (e.g. by using the Y-connector), gently introduce the catheter into the mouth or nostril. If the oral route is used, the client’s tongue may be depressed with a tongue depressor | Suction during insertion may damage the mucosa. Facilitates insertion of the suction catheter |
| Ensure that suction pressure is below 120 mmHg. Apply suction as the catheter is withdrawn, rotating the catheter as it is being withdrawn | Pressure above 120 mmHg may damage the mucosa. Rotating motion prevents tissue trauma and obtains maximal volume of secretions |
| Apply suction for a maximum of 8–10 seconds, or less in the young or critically unwell client, then remove from the airway. Allow the client time to rest between suctioning | Suctioning for longer than 10 seconds can cause tissue trauma and hypoxia |
| If secretions are tenacious, dip the tip of the catheter in water and apply suction. If a specimen is required for virology or bacterial studies, use of normal saline is recommended | |
| Repeat the procedure, if necessary, until the mucous obstruction has been removed | Promotes a clear airway |
| After suctioning, instruct the client (if able) to take several slow deep breaths | Relieves hypoxia and promotes relaxation |
| Dip the catheter into the water and apply suction | Clears catheter and connecting tubing |
| Discard the catheter, water and gloves. Attend to the rest of the equipment. Perform hand hygiene | Prevents cross-infection |
| Assist the client into a position of comfort | Promotes rest and relaxation |
| Wash and dry hands | Prevents cross-infection |
| Document and report the procedure, including observations of the aspirate | Appropriate care can be planned and implemented |
Chest physiotherapy
Chest physiotherapy assists the client to mobilise and eliminate secretions, re-expand airways and alveoli and promotes the efficient use of the muscles of ventilation. Chest physiotherapy includes postural drainage, chest percussion and vibration, coughing and deep-breathing exercises.
Postural drainage
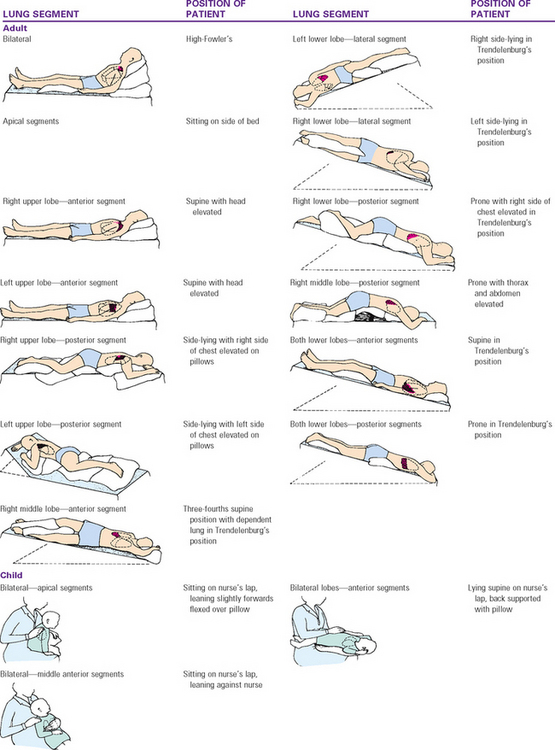
Postural drainage (Fig 23.22) encourages pulmonary secretions to empty by gravity into the bronchioles, bronchi or trachea, so that they may be expectorated. The client with a respiratory disorder is assisted to assume positions that promote drainage from the affected parts of the lungs. Effectiveness of the technique largely depends on positioning that allows drainage by gravity. Postural drainage should be avoided immediately before or after meals, to prevent nausea and aspiration of food or vomitus.
Percussion and vibration
Percussion and vibration are employed to help loosen respiratory secretions and are commonly used in conjunction with postural drainage. Percussion is performed by rhythmic tapping using cupped hands over the affected segments of the lungs. Care should be afforded to clients with osteoporosis, fractures or recent surgery. Vibration is performed by placing the hands over the affected area and shaking, so that the chest wall is vibrated while the client is forcibly exhaling. To ensure sufficient force is being used the client can be asked to vocalise and a vocal fremitus should be heard.
After postural drainage, percussion and vibration, the client should be asked to cough to remove the loosened secretions. This is performed by a physiotherapist or allied health assistant. Oral hygiene should be attended to after the procedure because the expectorated secretions may have an offensive taste or odour.
Promoting comfort and relieving pain
In many disorders of the circulatory system the aim is to increase the client’s activity progressively without pain. Comfort is promoted if the client is provided with a bed made to meet their specific needs.
The client may experience pain, for example, as a result of myocardial infarction or peripheral vascular dysfunction, so relief of pain is an important aspect in the promotion of comfort. In certain respiratory conditions such as pleurisy, severe pain may increase on inspiration. The presence of indwelling tubes, wires or cannulas all contribute to further discomfort. Pain-relieving measures such as the administration of adequate analgesic medication are implemented so that the client is able to rest comfortably, sleep without discomfort and perform the activities of daily living without experiencing pain or significant side effects of the medication. The client is also advised on what precautions to take to avoid pain, which includes identifying any precipitating factors such as physical exertion or emotional stress. The incidence of pain can generally be reduced by careful planning of activity, modifying risk factors and use of prophylactic measures.
Providing psychological support
Anxiety and fear are common responses to hospitalisation. A client who is experiencing a major respiratory or cardiovascular dysfunction, such as myocardial infarction, pneumonia or blood dyscrasias, often becomes extremely anxious, apprehensive and depressed about dyspnoea, pain, disability, loss of independence and dying. The client and their significant others may experience great concern about the alterations in lifestyle imposed by their disorder. Nurses provide psychological support by establishing and maintaining a trusting relationship with the client and their significant others and by encouraging them to express their feelings and concerns. They should be encouraged to discuss any lifestyle adjustments that may be necessary and they should be offered guidance on how to cope with change.
Stress and anxiety can be reduced if the client’s symptoms, such as pain or dyspnoea, are alleviated, and the nurse should try to provide an environment that is as stress-free as possible. The client should be provided with sufficient information about their illness, as knowledge helps to diminish anxiety and apprehension and assists them to develop effective coping skills. All procedures, treatments and monitoring techniques being implemented are explained so that the client understands the treatment. The client should be encouraged to participate in their care as much as possible and, when appropriate, to gradually assume responsibility for self-care to prevent loss of independence. The client should be informed about support groups and community resources such as rehabilitation classes, which may be helpful when they are discharged from hospital.
Maintaining skin integrity
A client with a respiratory, cardiac, peripheral vascular, blood or lymphatic disorder is at risk of impaired skin integrity. Decreased peripheral perfusion and oxygenation can result in skin breakdown. With poor arterial circulation the tissues lack adequate oxygen and nutrients and this can lead to cellulitis, ulcers, poor wound healing and necrosis. Maintenance of skin integrity includes:
• Assessing the skin for any signs of breakdown
• Keeping the skin clean and dry
• Protecting the extremities from exposure to extremes of temperature and from trauma
• Position changes to avoid prolonged pressure on the skin
• The use of accessories (e.g. a sheepskin) to reduce pressure, and promoting mobility
Preventing skin breakdown includes keeping the feet clean and dry, avoiding rough drying movements, using creams or lotions that prevent drying and cracking, avoiding scratching itchy areas on the legs or feet, providing nail care by a podiatrist and protecting the feet with socks, slippers or well-fitting shoes.
Promoting and maintaining mobility
Maintenance of mobility is necessary to prevent the complications of immobility, such as decubitus ulcers, venous stasis and pulmonary complications. Problems of immobility should be counteracted with position changes, range-of-motion (ROM) exercises and coughing and deep-breathing exercises. Ambulation of the client as soon as possible is important to prevent the complications of immobility.
In the initial stages of illness, such as immediately after myocardial infarction, the client’s level of activity may be reduced to a minimum. As their tolerance increases, their level of physical activity gradually increases. The client should understand the importance of adequate physical exercise, which provides the necessary muscle contraction for movement of arterial blood and lymph to and from the peripheral areas of the body. Exercise or activity programs are generally implemented gradually, and the client is encouraged to rest after the exercise periods. As the client’s condition improves, moderate exercise is encouraged as long as pain is not induced.
Preventing infection
A client with any of the disorders mentioned previously may be susceptible to infection as a result of nosocomial infections, altered nutritional status, medications such as steroids, invasive procedures and changes in immune status. Measures to prevent infection must be implemented, such as good handwashing techniques, and aseptic techniques for any procedure. Precautions must be taken to prevent damage to the skin or mucous membranes, as injured tissues create a portal for bacterial invasion. If the client’s WBC count is low (leucopenia), it may be necessary to use protective isolation techniques to protect them against infection. The client must be monitored closely to detect the early manifestations of infection so that appropriate treatment can be prescribed.
Promoting effective breathing and aeration
In addition to the measures employed to promote a clear airway, other measures may be necessary to maintain adequate ventilation. Breathing exercises may be used by the client to promote and maintain optimal pulmonary ventilation, and oxygen may be prescribed to supplement that being obtained from the atmosphere.
Breathing exercises
When respiratory system disorders produce ineffective breathing patterns and inadequate ventilation, the client may be educated to perform deep-breathing exercises.
Deep breathing
Deep, or diaphragmatic, breathing uses the diaphragm and abdominal muscles to fully ventilate the lungs. The client should be assisted into a sitting position to promote optimal alveolar expansion. One hand is placed on the chest and the other hand is placed on the abdomen. If the client is breathing correctly the hand on the abdomen should rise with inhalation and fall with exhalation; the hand on the chest should remain still. The client is educated to inhale deeply and slowly, pushing the abdomen out, to promote optimal distribution of air to the alveoli. Clients may also be educated to exhale through pursed lips, while contracting their abdomen. Exhalation through pursed lips improves ventilation pressures and encourages a slow deep-breathing pattern. Abdominal contraction pushes the diaphragm upwards, exerts pressure on the lungs and helps to empty them.
Breathing exercises are performed according to the client’s condition; for example, short sessions may be indicated if the client becomes fatigued easily. The duration and frequency with which deep-breathing exercises are performed vary; they may, for example, be performed for 1 minute, with gradual progression to a 10-minute exercise period four times daily.
Incentive spirometry
Incentive spirometry (Fig 23.23) uses a breathing device to encourage the client to achieve maximal ventilation. The device measures peak respiratory flow or respiratory volume, and induces the client to take a deep breath and hold it for several seconds. Incentive spirometry benefits the client, as it establishes alveolar hyperinflation for a longer time than is possible with a normal deep breath.
Promoting efficient gas exchange
Any disorder of the respiratory system may result in impaired gas exchange. Depending on the extent to which it interferes with ventilation and perfusion, hypercapnia, hypocapnia and/or hypoxaemia may develop. The aim of management of these conditions is to maintain adequate oxygenation and removal of carbon dioxide. In addition to the measures already described, which promote a clear airway and effective breathing, other measures may be necessary, including the insertion of an artificial airway and/or mechanical ventilation. (Information on both these topics is provided later in this chapter.) The nurse must observe the client for the signs and symptoms of impaired gas exchange (see Table 23.4). Clinical Interest Box 23.6 outlines the cardiopulmonary health promotion for young to older adults.
Table 23.4 Impaired gas exchange
| Condition | Possible cause | Manifestations |
|---|---|---|
| Respiratory acidosis (hypercapnia) | Hypoventilation as a result of chronic obstructive pulmonary disease, pneumonia, drugs or trauma | Flushed warm skin, hypertension, tachycardia, headaches, drowsiness, confusion, irritability, coma |
| Respiratory alkalosis (hypocapnia) | Hyperventilation as a result of acute asthma, cerebral trauma or congestive cardiac failure | Diaphoresis, pallor, tachypnoea, tingling and numbness in the limbs, or around the mouth, carpopedal spasm (tetany) and convulsions |
| Hypoxia | Obstructive lung diseases, and restrictive lung diseases (e.g. chronic bronchitis, emphysema, sarcoidosis) | Pallor or cyanosis, tachypnoea, tachycardia, breathlessness, headaches, irritability, confusion |
CLINICAL INTEREST BOX 23.6 Cardiopulmonary health promotion for young to older adults
• Eat a low-fat, low-salt, kilojoule-appropriate diet
• Monitor cholesterol and triglyceride levels
• Engage in regular aerobic exercise
• Use stress-reduction techniques
• Avoid second-hand smoke and other pollutants
• Use a filter mask when exposed to occupational hazards
• Get an annual influenza vaccine if at risk of developing influenza
(Crisp & Taylor 2009:962)
Specific Interventions
Specific nursing interventions relevant to caring for a client with a respiratory system disorder include:
• Collecting specimens of sputum
• Obtaining nasal or throat swabs
Collecting sputum
Sputum is a mucous secretion produced by the mucous membranes that line the respiratory tract. Mucous secretion increases in response to inflammation, infection or congestion. Laboratory examination of sputum may be necessary to determine whether any microorganisms, blood or malignant cells are present. The nurse should observe the sputum, noting the amount, consistency, colour and presence of blood or odour. Sputum is normally clear in colour but may turn white if the client smokes or has a viral infection; yellow, rust-coloured or green to dark-brown sputum may indicate the presence of an infection. It may be tinged with blood or contain streaks of blood that can suggest inflammations, dryness or infections or conditions such as pulmonary oedema or carcinoma. The consistency varies from watery to mucoid to tenacious.
When a specimen of sputum is required it is best collected early in the morning before any food or fluid is given, as this ensures that there is an accumulation of secretions to be obtained. To avoid the risk of cross-infection with airborne microorganisms the nurse should stand beside rather than in front of a client when collecting the sputum specimen. Sputum for laboratory testing should be free of saliva and food particles (see Procedural Guideline 23.4).
Procedural Guideline 23.4 Collection of sputum
| Review and carry out the standard steps for all nursing procedures/interventions |
| Intervention | Rationale |
|---|---|
| Explain the procedure to the client, ensuring that they understand it is sputum and not saliva that is required. Label the container appropriately | Reduces anxiety. Saliva will produce inaccurate test results |
| Perform hand hygiene and don gloves | Prevents cross-infection |
| Assist the client to a sitting position | Facilitates coughing and expectoration |
| Instruct the client to cough and to expectorate into a sterile container | A sterile container ensures that the specimen is not contaminated |
| Place the lid on the labelled container, wipe the outside of the container and perform hand hygiene | Prevents cross-infection |
| Despatch the specimen, together with the request form, to the laboratory as soon as possible. Ensure that the container is clearly labelled with the relevant information | Proliferation of microorganisms occurs if the specimen is not despatched as soon as possible after collection. Avoids errors |
| Offer the client oral hygiene | Reduces bad taste or halitosis in mouth |
Nasopharyngeal and throat swabs
Laboratory examination of secretions from the nasopharynx or throat may be necessary to determine the presence of pathogenic microorganisms. Collection of a specimen involves swabbing the inflamed tissues and collecting any exudate with a sterile cotton-wool-tipped swab. The nurse should refer to the healthcare institution’s policy manual for information about the type of applicator, culture tube and transport medium to use (see Procedural Guideline 23.5).
Procedural Guideline 23.5 Collecting a nasopharyngeal or throat swab
| Review and carry out the standard steps for all nursing procedures/interventions |
| Intervention | Rationale |
|---|---|
| Explain the procedure to the client. Inform them that they may experience the urge to sneeze or gag during the swabbing. Label the container appropriately | Reduces anxiety and promotes cooperation to minimise trauma |
| Assist the client, if possible, to a sitting position | Facilitates collection of the specimen |
| Perform hand hygiene and don gloves | Prevents cross-infection |
| If a nasopharyngeal swab is to be obtained, request the client to blow their nose | Clears the nasal passages |
| Request the client to tilt their head back | Facilitates collection of the specimen |
| To obtain a swab of the nasopharynx, gently pass the swab through the nostril until it reaches the posterior pharyngeal wall | Gentle insertion prevents tissue damage |
| Rotate, then withdraw the swab. To obtain a swab of the throat request the client to open their mouth, depress the tongue with a tongue depressor and use a torch to illuminate the throat | Facilitates access and visualisation |
| Ask the client to say ‘ah’. Pass the swab over the tonsils, posterior pharyngeal wall and posterior edge of the soft palate | Raises the uvula to expose proper site of collection |
| Place the swab in the culture tube immediately and close the end of the tube. Perform hand hygiene | Prevents cross-infection and contamination of the specimen |
| Despatch the specimen, together with the request form, to the laboratory as soon as possible. Ensure that the container is clearly labelled with the relevant information | Proliferation of microorganisms occurs if the specimen is not despatched and refrigerated as soon as possible after collection |
Clinical Scenario Box 23.2
Mr Williams, a 76-year-old chronic smoker diagnosed 30 years prior with emphysema, is a long-term client in your facility. During the previous 2 days his respiratory effort has increased, and his skin colour, previously pink, has now developed central and peripheral cyanosis that appears to be worsening. He has developed diaphoresis, his blood pressure has increased marginally and he is complaining of a headache.
Describe the most appropriate oxygen delivery method and flow rate applicable in this situation and what complications may occur as a result of oxygen therapy.
Oronasopharyngeal suction
Oronasopharyngeal suction may be required when secretions or foreign substances are causing an obstruction to the client’s airway. Suction is indicated for the client who is unable to clear the airway effectively with coughing and expectoration, such as the severely debilitated or unconscious client. The removal of excess secretions and mucus from the airway aids breathing, promotes pulmonary gas exchange and prevents the accumulation of secretions that may cause secondary atelectasis or pneumonia. Suctioning is achieved by means of a catheter, which is introduced through the mouth or nose into the pharynx.
The basic equipment consists of:
• Wall suction or portable suction apparatus
• Water suitable for flushing the catheter and tubing in a small container
Suction equipment is usually kept in readiness at the bedside if there is an indication that it may be needed frequently, as an emergency measure or as part of the healthcare institution’s policies. In general the pressure is set at 80–120 mmHg for an adult (and considerably lower for a child), depending on the diameter of the catheter and the viscosity of the secretions. The medical officer will prescribe the level of suction to be used. If using the nasal route, suctioning should be alternated between the left and right nostrils to reduce trauma to the one nostril. It may also be necessary to lubricate the tip of the catheter with a sterile water-soluble lubricant before insertion into the nostril. (See Clinical Interest Box 23.7.)
Inhalation therapy
Various forms of inhalation therapy may be prescribed for a client with a respiratory disorder, including humidified air or oxygen, and nebulised air or oxygen. These can be administered by aerosol devices, electric nebulisers and humidifiers or an intermittent positive-pressure ventilator.
Electrical humidifiers and nebulisers
Water vapour may be provided by means of a humidity cot, tent or via a mask or tube attached to the client. Various electrical devices can provide both humidification and nebulisation, depending on the fitting used. The device has water fed by a sterile container to an electrically warmed core that heats up the fluid contained in it as it passes through a chamber. The warmed water vapour is delivered to the client via large-bore corrugated tubing and the oxygen concentration can be regulated from room air to 100% oxygen by means of an oxygen venturi-type diluter. The client inhales the vapour through a nebuliser-type mask.
Nebulisation provides a very visible mist of large water droplets that are delivered into the airways. Nebulisation is used to treat atelectasis and airway infections and to loosen and decrease the viscosity of secretions to facilitate expectoration. It can be delivered through a mask or tracheotomy tube. Humidification provides water vapour in an almost invisible fine mist of small droplets that can travel further into the airways than by nebulisation by virtue of the droplet size and weight. Humidification is used to provide humidity to prevent stasis of mucus, tissue dehydration and to reduce drying, inflammation and irritation of the air passages. These devices provide precise control of oxygen delivery and protection against cross-contamination by means of a sterile pre-filled container of solution, such as sterile water or normal saline.
Other similar devices are used in positive-pressure ventilators, such as Bird or Bennet ventilators, to deliver humidity or medication to a client on a ventilator or during intermittent positive-pressure breathing therapy. Nurses should know their role and responsibilities regarding inhalation therapy and administration of medications, and should be familiar with the healthcare facility’s infection-control guidelines. The nurse should check the devices hourly for leaks, cracks and oxygen concentration. Bedding and clothing are changed as soon as they become damp. Care should also be taken to observe the skin surrounding the mask for signs of breakdown.
Mechanical and electrical nebulisers are used to deliver moisture or medication as a fine mist into the airways of clients with conditions such as asthma or emphysema. Bronchodilators are commonly prescribed in the management of asthma. The devices operate off mains or 12-volt power and are generally used by clients at home. Care must be taken to ensure that the device is placed on a stable surface, and regular maintenance of the filters is required.
Gas-driven nebulisers are used with compressed air or oxygen to deliver nebulised vapour or medication. The prescribed solution is inserted into the nebuliser, either alone or together with a prescribed amount of sterile water or saline, and one end of the oxygen tubing is attached to the nebuliser, which is directly connected to a nebuliser mask. The other end of the tubing is attached to an oxygen regulator and then to the pressurised gas source, which is turned on to check for proper misting. To produce particles of the correct size and to better ensure their arrival at the most distal airways, a flow rate of 10 L/min is generally required. The client is instructed to breathe deeply, slowly and evenly through the mouthpiece or mask and to hold their breath for 2–3 seconds at the end of inhalation to receive the full benefit of the medication. The client should be encouraged to cough and expectorate.
Steam inhalations are not generally used because of the risk of burns and the improved effectiveness in providing fluids by other means.
Mechanical ventilation
Mechanical ventilation is sometimes indicated for a client with a respiratory system disorder. Mechanical ventilation artificially assists or controls respiration and it is indicated to correct or prevent gas transport abnormalities. To maintain adequate pulmonary blood gas exchange, an endotracheal or tracheostomy tube is inserted (see below) and connected to the ventilator.
A variety of ventilators are available, which may be one of two main types: pressure controlled or volume controlled. With the pressure-controlled ventilator the gas is delivered to the lungs until a predetermined pressure is reached, then inspiration is terminated. With a volume-controlled ventilator a set volume of gas is delivered with each inspiration. The ventilation rate may be preset, controlled by the client, or may be a combination of both.
Care of a client receiving mechanical ventilation should be provided by nursing staff who are qualified and experienced to provide it. A client who requires mechanical ventilation is generally nursed in an ICU, as they require constant physical attention and emotional support.
THE CLIENT WITH AN ARTIFICIAL AIRWAY
The placement of an artificial airway is indicated to relieve obstruction, to facilitate suctioning of the lower respiratory tract, to prevent aspiration or to allow for mechanical ventilation. Artificial airways include the oropharyngeal airway, the endotracheal tube and the tracheostomy tube.
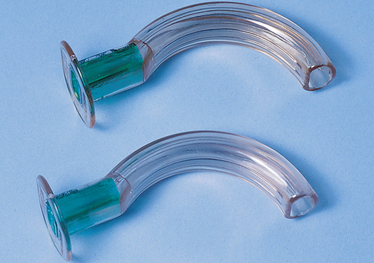
Oropharyngeal airway
An oropharyngeal airway (Fig 23.24) is a curved rubber or plastic device inserted into the mouth to the posterior pharynx to establish or maintain a patent airway. The airway allows air to pass around and through the tube and facilitates oropharyngeal suctioning. It is used for the short term only, such as in the immediate post-anaesthetic period. If a client requires respiratory assistance for a longer period, an endotracheal or tracheostomy tube is generally used.
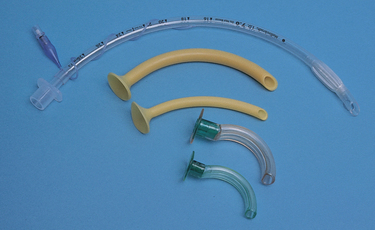
Endotracheal tube
An endotracheal tube is a flexible cuffed tube inserted via the mouth or nostril through the larynx into the trachea (Fig 23.25). Endotracheal intubation establishes and maintains a patent airway, prevents aspiration by sealing the trachea off from the digestive tract, facilitates the removal of tracheobronchial secretions and provides a means whereby optimal ventilation can be achieved. Endotracheal intubation may be required in an emergency or may be required for a short or long term.
The tube is inserted by a medical officer, who uses a laryngoscope to visualise the trachea and facilitate the passage of the tube. Most endotracheal tubes in adults have a cuff, which is inflated with air to provide a seal that prevents the leakage of air around the tube when the client is ventilated. Uncuffed tubes are generally used in infants and children unless there is excessive leakage of air past the tube. To avoid inadvertent removal or displacement of the tube, string and tape may be applied to secure the tube in position. Continuous expert care is required after endotracheal intubation to ensure airway patency and to prevent complications. A client who has been intubated is generally nursed in an ICU and receives constant physical attention and emotional support.
Tracheostomy
A tracheostomy (Fig 23.26) is a surgical creation of an external opening into the trachea, and may be performed as an emergency temporary measure or as a permanent measure. A tracheostomy tube may be inserted into the tracheostomy to provide a patent airway, prevent aspiration of secretions, allow removal of tracheobronchial secretions by suction and permit the use of a mechanical ventilation device. A tracheostomy tube is a short curved tube fitted with a flange that assists in stabilising the tube. Tracheostomy tubes are available in a range of styles, materials and sizes, and some are fitted with an inflatable cuff.
NURSING A CLIENT WITH AN ARTIFICIAL AIRWAY
The care of a client with an artificial airway—whether it has been inserted for a short or long term—involves many physical actions and the provision of emotional support. The main aspects of care include:
• Continued assessment of airway status
• Maintenance of correct cuff pressure to prevent tissue ischaemia and necrosis
• Continued monitoring for complications
Nursing a client with a tracheostomy
When caring for a client with a tracheostomy, the following should always be available at the bedside in case of accidental dislodgement or obstruction of the tube:
A client with an artificial airway will be apprehensive about asphyxiation or choking, which can be further increased by an impaired ability to communicate their needs to others. The client’s ability to effectively remove secretions by coughing may be grossly impaired. When unable to cough or expectorate secretions, suctioning must be performed. In the first few days after the insertion of a tracheostomy tube the procedure is uncomfortable and frightening, and the client must be provided with an explanation of the suctioning technique before it is performed. The nurse should be aware of their role in, and the regulations and the healthcare facility’s, procedures and policies regarding tracheostomy suctioning. A suggested method of tracheostomy suctioning is outlined in Procedural Guideline 23.6.
Procedural Guideline 23.6 Tracheostomy suctioning
| Review and carry out the standard steps for all nursing procedures/intervention |
| Intervention | Rationale |
|---|---|
| Explain the procedure and provide privacy. The client should be informed that suctioning may cause transient coughing or gagging | Reduces anxiety and embarrassment |
| Place the equipment within easy reach | Facilitates performance of the procedure in an organised manner |
| Remove any humidification (or ventilation) device | Allows access to the tracheostomy tube |
| Perform hand hygiene and put on gloves | Prevents cross-infection |
| Attach the catheter to the suction tubing and set suction pressure to 80–120 mmHg | Pressure above 120 mmHg may damage the tracheal mucosa |
| Ask the client to cough and breathe slowly and deeply | Coughing helps loosen secretions, and deep breathing helps to minimise hypoxia |
| If necessary, or prescribed, the client’s lungs are hyperoxygenated before aspiration | Helps to prevent hypoxia |
| Insert the catheter without suction into the tracheostomy tube | Prevents hypoxia and tracheal mucosa trauma |
| Report immediately if there is any difficulty in inserting the catheter into the tube | The tube may be partially blocked with secretions |
| When suctioning is completed, the client may need to be hyperoxygenated again. Replace any humidification device | Prevents hypoxia and promotes relaxation. Re-establishes delivery of humidity |
| Dispose of the gloves and suction catheter appropriately, perform hand hygiene | Prevents cross-infection |
| Document and report on the procedure | Appropriate care can be planned and implemented |
The basic equipment for tracheostomy suctioning is:
• Sterile ‘Y’ suction catheters
• Wall or portable suction apparatus
• Container of sterile or tap water for clearing the catheter (depending on the institution’s policy)
Care of the tracheostomy and tracheostomy tube is performed to minimise contamination and to decrease the possibility of obstruction by secretions. Tracheostomy care, which is performed using sterile equipment and aseptic technique to prevent infection, involves cleansing of the inner cannula and the area around the stoma. The frequency with which the care is provided may vary depending on the amount of secretions present, and may be as frequent as every ½ hour to 1 hour or may only be required once every 8 hours.
Some tracheostomy tubes have an inner replaceable tube that can be changed as part of routine daily care (e.g. 4-hourly to daily). It is essential that a spare inner tube is kept close at hand and replaced if the inner tube becomes blocked. The inner tube is cleaned using a suitable solution and dried and made accessible for future use. Many tracheostomy tubes are fitted with an inflatable cuff. Regular deflation of a cuffed tube is performed to prevent tracheal necrosis and stenosis. The frequency and length of time for cuff deflation varies depending on the type of tube used and the condition of the client.
To prevent the trachea or lower airways from drying and bleeding, a humidification connector, a ‘Swedish nose’, may be applied. It consists of a single or dual barrel that encloses the tube’s orifice; humidity is provided by rolled absorptive paper filters pre-moistened with normal saline. If secretions are present on the outside of the suction catheter, additional sterile saline may be required to be instilled into the tracheostomy tube to loosen secretions and maintain the patency of the tracheostomy tube.
Communication is a significant problem and to alleviate anxiety and apprehension an alternative means of communication should be provided. A pad and pencil should be available, the client’s call bell or buzzer must always be within easy reach and must be answered promptly. If unable to write, the client can be educated to use a series of gestures or sign language as an alternative method of communicating their needs. Alternatively, for clients with uncuffed tubes a speaking valve can be employed, or they can be educated how to cover the tube with their finger to occlude the airway on expiration and allow for limited communication. If the artificial airway is a temporary measure, the client should be informed that their voice will recover when the tube is removed. Before deflation, the tube and oronasopharynx are aspirated. When the cuff is inflated, only sufficient air is inserted to occlude the escape of air from around the sides of the tube.
The client should be provided with information about their progress and any procedures that are to be performed. They should be encouraged to participate in their own care as much as possible to reduce any sense of dependency, and the significant others should be involved in the care. The client may be discharged from hospital with a tracheostomy tube in situ. As soon as possible, they and the significant others are educated in self-care so that they feel comfortable and confident about caring for their tracheostomy. The client should be provided with information about relevant support groups such as tracheostomy associations that they may wish to contact.
Before the permanent removal of a tracheostomy tube the client will require sufficient information and emotional support, as they may feel that they will not be able to breathe without the tube. The tube may be removed when the client is able to maintain independent respiratory function, is able to breathe through the upper respiratory tract and has satisfactory protective reflexes such as the cough reflex.
To prepare the client for permanent removal of the tracheostomy tube a fenestrated tube may be inserted. This type of tube has an opening in the outer cannula that allows the client to breathe around as well as through the tube. Thus, they are able to adjust gradually to removal of the tube. Alternatively the tube may be occluded or ‘corked’ by an adhesive tape to determine the client’s ability to cope without the tube. With uncuffed tubes this is routinely achieved to enhance communication by allowing the client to occlude the tube with their fingers while speaking. By covering the tube, they may be able to speak, breathe normally through the upper airway and expectorate secretions.
Before the tube is removed, suction is applied to remove tracheal and pharyngeal secretions. The cuff is then deflated and the tube removed. Generally a dry occlusive dressing is placed over the stoma and the client closely monitored for the first 24 hours. Healing and reduction in the tracheostomy can take 12 months or longer and care must be taken during this time to prevent aspiration and infections. After a period of time, when the client’s airway is stable, the stoma can be surgically sutured together (see Procedural Guideline 23.7).
Procedural Guideline 23.7 Tracheal stoma care
| Review and carry out the standard steps for all nursing procedures/interventions |
| Intervention | Rationale |
|---|---|
| Explain the procedure and provide privacy | Reduces anxiety and embarrassment |
| Open a sterile dressing pack and place any additional equipment within easy reach | Facilitates performance of the procedure in an organised manner |
| Perform hand hygiene | Prevents cross-infection |
| Remove any humidification (or ventilation) device | Allows access to the tracheostomy tube |
| Suction the tracheostomy tube (refer to Procedural Guideline 23.6) | Removes secretions from the airway |
| Remove and discard the tracheostomy dressing into a suitable waste receptacle | Correct disposal prevents cross-infection |
| For a newly formed stoma, use a sterile drape around the tracheostomy site | Provides a sterile field around the stoma |
| Put on sterile gloves | Prevents cross-infection |
| Cleanse the skin around the stoma and the flanges of the tube using gauze and appropriate solution. Take care not to let solution or strands of gauze enter the tube or stoma | Removes accumulated secretions and crusts. These may be aspirated into the lungs |
| Inspect the surrounding area and stoma site for inflammation or skin breakdown | Signs of impaired healing or infection require immediate attention |
| Apply a sterile tracheostomy dressing | Protects the stoma site |
| Replace the tracheostomy tapes if they are soiled or loose. Whenever possible, two people should be present to change the tapes | Tracheostomy tube must be secured in position. Soiled tapes predispose the client to infection. Prevents accidental dislodgement of the tube |
| Replace any humidification device | Re-establishes delivery of humidity |
| Remove gloves, dispose of the equipment appropriately, perform hand hygiene | Prevents cross-infection |
| Assist the client into position and place the call bell within reach | Promotes comfort and relaxation |
| Document and report on the procedure | Appropriate care can be planned and implemented |
Complications of tracheostomy
The insertion of an artificial airway can result in several complications:
• Infection due to altered ciliary function or colonisation of the airway with bacteria
• Tracheal necrosis and stenosis due to excessive pressure on the trachea from the cuff
• Partial or complete airway obstruction (e.g. due to an accumulation of secretions in the tube)
• Psychological effects, such as frustration at being unable to communicate as usual.
THE CLIENT WITH THORACIC DRAINAGE TUBES
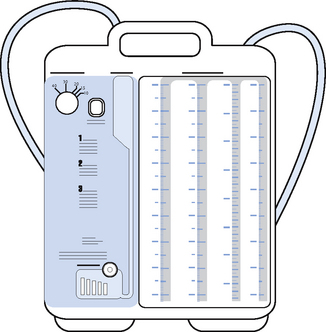
Insertion of chest drainage tubes (Figs 23.27 and 23.28) permits the drainage of air or fluid from the pleural space which, if not removed, alters intrapleural pressure and causes lung collapse. Ventilation is adversely affected by any disruption of the intrapleural pressure, which may be caused by surgery, trauma or pulmonary disease. Insertion of chest tubes drains the excess air or fluid and enables the lungs to function normally.
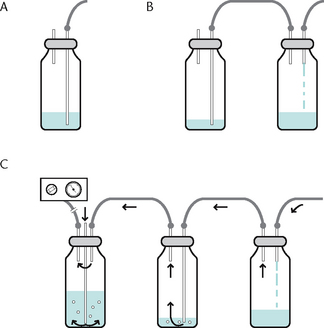
Figure 23.27 Chest tube drainage A: One-bottle system B: Two-bottle system C: Three-bottle system with suction
Chest drainage tubes may be inserted at the time of surgery while a client is anaesthetised, or they may be inserted using local anaesthetic. Because the procedure is painful, a conscious client is generally given analgesic medication about 30 minutes before tube insertion. The procedure is performed by a medical officer, using sterile equipment and aseptic technique. The insertion site is selected according to the client’s condition, and one or more tubes may be inserted at the same time.
Underwater seal drainage
After insertion the chest tube is connected to a drainage system that permits drainage out of the pleural space and prevents back-flow into that space. The tubing leads to a collection system positioned well below the level of the client’s chest. This dependent position facilitates the removal of air or fluid from the pleural cavity and prevents back-flow. To prevent the entry of air into the pleural cavity the distal end of the tubing is submerged underwater. This provides a closed water-seal drainage system. The depth of water that the tube is placed under determines the water pressure used to create a seal, for example 5 cm, and is ordered by a medical officer.
Some commercially available systems of underwater seal drainage, for example the Pleur-evac® system, are available already assembled and are disposed of after use. Other types of thoracic drainage systems include the one-, two- or three-bottle systems. The one- and two-bottle systems are primarily gravity systems, which can be provided with suction to facilitate drainage. Such systems provide a water seal and can be connected to suction. A medical officer is required to order the application of suction, which is used to facilitate faster drainage of air or fluids. A low-flow suction regulator device is used to ensure that the suction provides a minimal bubbling effect.
NURSING A CLIENT WITH A CHEST DRAIN
The aim of closed-chest underwater seal drainage is to promote lung expansion by facilitating drainage of air and fluid. Care of the client includes:
• Nursing them in an upright position when possible, to facilitate optimal lung expansion and to promote drainage by gravity
• Providing adequate explanation and emotional support to reduce anxiety. The client may tend to restrict their breathing and movement for fear of dislodging the tube, so it is essential to explain that the tube is secured in position with tape and/or sutures
• Administering adequate analgesic medication to decrease discomfort. It may be necessary to administer analgesic medication 30–45 minutes before physiotherapy, to promote pain relief and relaxation
• Encouraging the client to breathe deeply and cough frequently (e.g. hourly, to help drain the pleural space and expand the lungs)
• Regularly assessing the client’s respiratory status. The client should be observed for discomfort and any difficulty in breathing, and it is important to observe whether their chest is expanding symmetrically. The ventilations are assessed at regular intervals (e.g. hourly, for rate, rhythm and character)
• Maintaining the water seal and preventing air leakage, which is essential to prevent entry of air into the pleural space. The fluid level in the drainage bottle should be checked frequently (e.g. hourly) and sterile water added if necessary to ensure that the distal end of the water seal tube remains submerged at the ordered level
• Taking precautions to prevent separation of the connections, such as taping the joints and securing the tube to the client’s clothing. Care must be taken to ensure that the underwater seal system remains below the client’s chest to prevent fluid or air re-entering the pleural cavity, which can cause subsequent pneumothorax or empyema
• Securing the drainage system to the bed or placing it securely on the floor to protect it from toppling over and from accidental breakage. If the system is accidentally disconnected or broken, air will enter the pleural space and the lungs may collapse. It is general practice to have two chest clamps in plain view at the bedside for any client with a chest drain; in the event of disconnection, the two clamps are applied immediately to the chest tube, and assistance is summoned immediately.
There is some controversy surrounding this emergency measure, as some authorities believe that clamping a chest tube could result in a tension pneumothorax. It is essential that the nurse be aware of the healthcare institution’s measures to be taken should accidental disconnection of the system occur. If a chest tube is accidentally dislodged or falls out, the client is asked to exhale forcefully and the opening on the skin surface is sealed with an airtight dressing until the tube can be reinserted.
• Maintaining patency of the drainage system, which is essential to facilitate expansion of the lung. The system must be checked hourly for loose connections and for fluctuation in the water-seal bottle. As the client inhales, the fluid should rise in the water-seal tube, and as they exhale the level should fall back (this is termed ‘swinging’)
• Ensuring that, if the system is connected to suction, the fluid line in the water-seal tube remains constant. During exhalation, bubbling is normally present in the water-seal bottle. Gently bubbling in a suction control bottle indicates that the correct level of suction has been achieved
• Observing the tubing for, and keeping it free from, kinks. Kinking of the tubing will obstruct the flow of air or fluid. To prevent kinking, or dependent loops of tubing, the tubing should be coiled flat on the bed and may be attached to the edge of the bed with tape and a safety pin. The tubing should fall in a straight line from the coil to the drainage bottle, to facilitate flow. The nurse should ensure that the client is able to move freely without pulling or lying on the tubing
• Double-clamping the chest tube near the site of insertion when it is necessary to replace a drainage system bottle. The bottle, and, if necessary, the connection tubing, is replaced and the clamps removed. The tubes should not be clamped for longer than 2 minutes, as a tension pneumothorax may result when air or fluid is prevented from escaping. As a safety precaution, two nurses should be present whenever a drainage bottle or system is being replaced
• Protecting the insertion site by an occlusive dressing (e.g. Opsite). Using sterile equipment and aseptic techniques to prevent infection, the dressing is renewed in accordance with the healthcare institution’s policy
• Assessing and documenting the colour, volume and type of drainage. Any alteration in the amount, colour or flow of drainage must be reported immediately. Sudden cessation of flow of drainage may indicate a malfunction of the system or disconnection of the tubing. A gradual reduction in flow may indicate occlusion by blood or proteins, that the tube position has moved in the pleural cavity or that the chest has reinflated.
Removal of a chest drain tube is performed by the medical officer. Generally the tube is clamped for up to 24 hours before removal, and a chest x-ray is performed immediately beforehand to determine lung expansion. If the client develops respiratory distress or a pneumothorax, the clamps are removed and the tube left in place. Analgesic medication is usually administered 30–45 minutes before tube removal. The tube is removed swiftly and immediately covered with an occlusive dressing to provide an airtight seal. In some cases the site is closed with purse string sutures that are tightened during removal.
One hour after the removal of the tube an x-ray is taken to ensure that there has been no ingress of air during or after the removal. The insertion site is checked regularly for sounds of air leakage and the client is observed for manifestations of pneumothorax, infection, subcutaneous emphysema and respiratory distress.
NURSING PRACTICE AND OXYGEN ADMINISTRATION
Nursing staff must be educated to adequately administer oxygen therapy. oxygen therapy is the delivery of oxygen to the client by some device or equipment in concentrations greater than that found in normal room air (room air is 21%). oxygen therapy is not a cure and does not remove the underlying disease or condition but aims to decrease the workload of the cardiopulmonary system and to protect the client from tissue hypoxia. Regardless of the mode of delivery the client must be able to maintain a patent airway, or an artificial airway must be established.
It is important for nursing staff to assess, initiate and monitor oxygen delivery systems within the prescribed parameter. An exception to this would be in an emergency when no client should be denied adequate oxygenation. In such cases oxygen should be given first and documented later.
Assessment
A client’s respiratory status is assessed to ascertain whether they are receiving an adequate supply of oxygen and excreting sufficient carbon dioxide to meet their body’s needs. A respiratory assessment should consider the following:
• Observing the client for signs and symptoms of hypoxaemia and respiratory distress
• Identifying any deviations from normal and by assessing their ventilations.
Assessing the respiratory status and identifying any actual or potential problems is assisted by obtaining information from the client regarding:
• Allergic reactions such as coughing, watery eyes, sneezing or shortness of breath that may occur as a result of exposure to allergens such as dust mites, pet hair or pollen
• Exposure to environmental air pollutants such as chemical wastes, smoke or dust
• History of tobacco and inhaled recreational drugs
• Presence of a cough and the volume, quality and quantity of sputum
Signs and symptoms of hypoxaemia and respiratory distress
The client should be observed for signs and symptoms of hypoxaemia which is defined as a diminished availability of oxygen to the body tissues. Hypoxaemia may result from disorders that limit the volume of air entering the lungs, or from obstructive lung diseases such as asthma and emphysema. The signs and symptoms of hypoxia and respiratory distress include:
• Cyanosis. Cyanosis is a bluish discolouration of the skin and mucous membranes due to inadequate oxygenation, and can be either peripheral or central. Peripheral cyanosis results in local vasoconstriction and is usually visible in the nail beds and the lips. Central cyanosis is the result of more severe hypoxia and affects all body organs. It is most visible in highly vascular areas such as the lips, nail beds, tip of the nose, the external ear and the underside of the tongue. In people with naturally dark brown or black skin, cyanosis is most accurately detected by inspecting the mucosa inside the mouth
• Elevated blood pressure and pulse rate
• Shortness of breath (dyspnoea), fatigue and intolerance to exercise
• Abnormal respiratory rate, depth or rhythm
• Sighing, gasping, breath holding
• Use of accessory muscles during breathing (e.g. sub-sternal recession, tracheal tugging, shoulder shrugging and intercostal muscles during expiration)
• Apprehension, aggression, non-compliance or agitation
Assessment of a client with chronic respiratory disorder
A person with a chronic respiratory disorder should also be assessed for a barrel-shaped chest, which is an increase in the antero-posterior diameter of the chest wall, commonly associated with air trapping, as in atelectasis or chronic obstructive airways disease. Clients with chronic hypoxaemia may experience the same symptoms as above but may have clubbing of the fingers, where the angle of the nail bed increases to over 85 degrees, caused by an increase in capillary numbers to supply poorly perfused tissue, with subsequent increase in size.
Meeting a client’s need for oxygen
Breathing is an automatic activity, but rate and depth can be changed voluntarily. Normally room air at normal atmospheric pressure, such as at sea level, provides sufficient oxygen to meet metabolic needs of the body. However, admission to hospital, or a respiratory condition, may affect a client’s normal pattern of breathing. For example, if a person has an infection or is apprehensive or anxious, they may experience temporary breathing difficulties. In these instances measures to promote the return of normal breathing are performed. Nurses provide clients with adequate information to allay some of the anxiety relating to their condition, investigations and hospitalisation. The nurse should also attempt to ensure that the room is ventilated adequately and at a comfortable temperature.
Clients who experience breathing difficulties due to a clinical condition may require assistance to meet any increase in either oxygen demands or carbon dioxide retention. Some methods include, for example, positioning in a more upright position, nebulisation, humidification, physiotherapy (which may include deep-breathing and coughing exercises) and mobilisation. Clients who suffer from an oxygen deficiency will commonly require administration of oxygen to supplement that being obtained from the atmosphere.
Administering oxygen
To prevent or reverse hypoxia and to improve tissue oxygenation, oxygen may be administered via a number of devices. Oxygen is a drug; it is prescribed by a medical officer who determines the concentration, route and length of time that it is to be administered. To promote the safety and comfort of the client receiving oxygen therapy, the nurse should be aware of certain principles relevant to the administration of oxygen:
• Hypoxaemia can result from insufficient oxygen flow or delivery. Equipment and connections must be checked at regular intervals (e.g. hourly) to ensure that it is functioning properly. If signs or symptoms of hypoxaemia occur they must be reported immediately, as adjustment to the concentration being administered may be necessary, or alternative investigations or treatment implemented
• Although oxygen is not normally combustible, it does support combustion and it is essential to implement safety precautions to reduce the risk of fire. Smoking is prohibited in the vicinity, and measures are taken to prevent sparks, which may be given off by electrical or mechanical items. Inflammable substances such as oil or alcohol should not be used near or on the oxygen equipment
• Administration of any gas can dry and irritate mucous membranes; this is particularly so with nasal prongs. In some healthcare institutions the gas is humidified by passing it through a sterile water humidification system before administration
• Oxygen is colourless and odourless, so accurate gauges on gas cylinders and oxygen concentrators are used to indicate the volume of oxygen remaining or rate of flow. An oxygen regulator limits the flow of the gas. Care must be taken to ensure that connections on the regulator are tight, otherwise a reduced volume or concentration will be administered
• Oxygen toxicity is a hazard with prolonged administration or concentrations over 50%. The client’s capillary, venous or arterial blood gases are commonly measured during oxygen therapy and the concentration of oxygen or method of delivery can be adjusted. Damage and inflammation to airways, blood vessels and nervous tissue may result in acute respiratory distress syndrome (ARDS)
• Nosocomial infections can occur using oxygen therapy, particularly with the use of non-sterile oxygen bubble humidifiers. Masks, tubing, cannulae and catheters are for single client use and are discarded on discharge. Care must be taken to clean the mask or nebuliser regularly (e.g. every 8 hours).
The nurse must know how to check that the equipment is functioning correctly and that all connections are secure and do not leak. Cleaning and disposal of equipment is done as per the individual healthcare institution’s infection-control guidelines.
Oxygen delivery equipment
Oxygen is often piped to a wall outlet or, less commonly, is supplied via a portable cylinder or oxygen concentrator and may be delivered to the client via an oxygen regulator using one of several devices. Oxygen is prescribed in litres per minute or in percentage as FiO2 (fraction of inspired oxygen such as 80% or 0.08). The mode chosen for the delivery of oxygen is dependent on the client’s clinical condition, concentration of oxygen required, degree of ventilatory support required and the client’s ability to comply with the therapy.
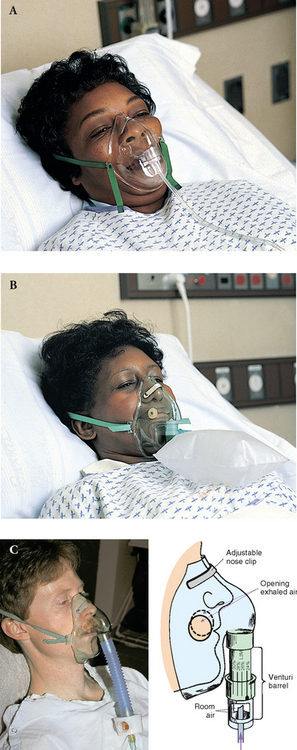
Nasal cannula
A nasal cannula (nasal prongs) (Fig 23.29) is made from a soft plastic material and contains two short prongs that fit into the nostrils. It may be secured in position by an adjustable ring or strap around the back of the head or taped onto the cheeks to prevent dislodgement. Because it does not enclose the nose or mouth, the cannula is comfortable and convenient for the person and there is less risk of aspiration of vomitus than a mask. The cannula is connected to the oxygen supply and the oxygen turned on at a low flow rate, with the flow checked before positioning it in the nares. The prongs are inserted following the natural curve of the nostrils, and the tubes are positioned over each ear and around the back of the head. The ring or strap is adjusted to maintain the position of the prongs, and care is taken to ensure that the strap is not too tight. An over-tight strap can cause pressure on the nostrils, the nose, the upper lip and cheeks. When the cannula has been positioned correctly, the flow of oxygen is adjusted to the prescribed rate. Minimum flow is 0.25 L/min to a maximum of 3 L/min. Higher volumes increase irritation and drying of the nasal mucosa. The oxygen concentration that the client receives is undeterminable and is reduced if the client mouth-breathes, eats or drinks.
Nasal catheter
An intranasal oxygen catheter (see the Teleflex® catheter, Fig 23.30) is made from a soft plastic material and contains a series of holes at the distal ends. The approximate length to be inserted is estimated by holding the catheter in a straight line from the tip of the client’s nose to their earlobe, and marking the catheter with an indelible pen to ensure that the insertion length can always be seen. The tip of the catheter may be lubricated with sterile water or a water-soluble lubricant to facilitate insertion. Before insertion, the catheter is connected to the oxygen supply and the oxygen turned on at a low flow rate. As with nasal prongs, oxygen concentration varies with factors such as mouth-breathing. The catheter can induce gastric distension if forced into the stomach.

Figure 23.30 Intranasal oxygen catheter
(Teleflex, EndoTest, ISIS and Rüsch are trademarks or registered trademarks of Teleflex Incorporated or its affiliates. © 2012 Teleflex Incorporated. All rights reserved.)
The catheter is gently inserted through one nostril into the nasopharynx to the pre-measured length. Using hypoallergenic tape, the catheter may be secured to the nose or cheek, avoiding traction on the nostril, which could cause skin breakdown. When the catheter has been positioned correctly, the flow of oxygen is adjusted to the prescribed rate. As it is an invasive device, the catheter may cause irritation of the mucosa, so it is usual to remove it after about 8 hours and insert a clean one into the other nostril. Rotating the site reduces the risks of mucous membrane irritation and skin breakdown at the tip of the nose.
Face mask
Face masks (Fig 23.31) are available in several styles and sizes. They are made from a lightweight vinyl material and are designed to fit over the nose and mouth, secured in position by an elastic band around the head. As the mask covers both the nose and the mouth, it is confining and impedes activities such as eating, drinking and communication as well as potentiating the risk of aspiration of vomitus.
Minimum flow rates for masks is normally 5 L/min, as a lower flow rate is not adequate to clear the mask of exhaled carbon dioxide and can cause hypercapnia (CO2 retention). Depending on the style, a mask can deliver oxygen from 28% at 4 L/min to 100% concentration at higher flow rates. A mask is commonly used when the client requires higher concentrations and more accurate amounts of oxygen, such as when the client is mouth-breathing, eating, talking or is able to breathe only through the mouth. Oxygen masks are recognisable by the presence of multiple small holes on the sides of the mask, as opposed to nebuliser masks, which have one large-diameter hole each side.
The style and size of a mask is assessed by measuring from the chin to the top of the nose, and an appropriate size is selected. The mask is connected to the oxygen supply via a flexible plastic tube, and the oxygen turned on to check that there are no leaks at a low flow rate. The mask is placed over the nose, mouth and chin, and the elastic strap secured around the back of the head; some masks have pliable metal straps that can be used to mould the mask to the client’s face shape. The strap is adjusted to ensure that the mask is firmly positioned but not uncomfortable, and the flow of oxygen adjusted to the prescribed rate. It is important that the mask fits closely but is not uncomfortable, and the nurse should ensure that there is no leakage of oxygen from the top of the mask. Leakage of oxygen from the top of the mask can flow across the eyes, causing dryness and irritation of the delicate tissues. Masks can create pressure areas on the skin and can be made more comfortable by applying self-adhesive foam to the edges in contact with skin.
Head box
A head box may be used to deliver oxygen to an infant and consists of a transparent plastic box that fits over the head or shoulders. The infant can be observed easily, and high concentrations of oxygen can be administered.
The concentration of oxygen to be delivered to the client will be specified by the medical officer and depends on the delivery device used and the rate at which the oxygen flows. Oxygen can be delivered from concentrations of 21% to 100%, and the flow rate adjusted by oxygen regulators from 0.25 L/min (low flow) to 3 L/min (high flow). The flow rate is adjusted by turning the valve on the flow meter (Fig 23.32) and observing the ball or dial that indicates the number of litres per minute at which the oxygen is flowing.
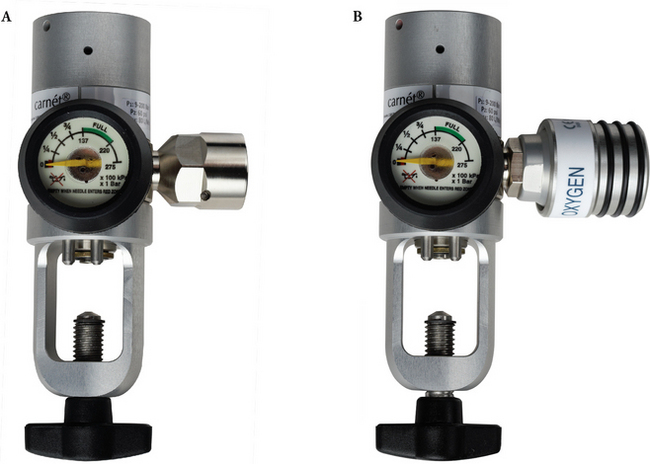
Figure 23.32 Oxygen regulators A: an example of an Australian standard regulator B: an example of a New Zealand standard regulator
(Images of Carnét® Oxygen Pressure Regulators (AS and BS) courtesy of BOC Limited, a member of the Linde group)
Whenever oxygen is to be administered the nurse should refer to the directions that accompany the device, to ensure that the correct concentration of oxygen is delivered to the client.
Mechanical ventilation
In specific situations a client may require oxygen to be administered via a mechanical ventilator. These devices may use either positive or negative pressure.
Positive pressure
Intermittent positive-pressure ventilation (IPPV) devices push atmospheric or oxygen rich air into the client’s airways to promote adequate lung expansion. Commonly, IPPV is performed via an endotracheal or tracheostomy tube and allows effective control of ventilation and oxygenation. The flow of air to the lungs is set at a predetermined pressure and, as the pressure is attained, the flow is stopped, pressure is released and the person exhales. Types of IPPV devices include:
• Positive end-expiratory pressure (PEEP): maintains a positive pressure in the lungs at the end of the client’s respiratory cycle, by increasing pressure within airways
• Continuous positive airway pressure (CPAP) is a device that maintains a certain amount of pressure to maintain the patency of large and small airways and alveoli. CPAP devices are commonly used with a tight-fitting face mask or over a tracheostomy.
Measures to promote the comfort and safety of the client receiving oxygen
There are a number of measures that nurses should consider when caring for a client receiving oxygen. Such measures include:
• Constantly monitoring the equipment to ensure that it is functioning correctly. The nurse should check the flow rate and ensure that the prescribed concentration of oxygen is being delivered to the client. Connections on regulators, concentrators and humidifiers should be checked to ensure their tightness and that they are free of leaks. Measures should be taken to prevent the oxygen tubing becoming twisted, kinked or disconnected, to facilitate a free flow of oxygen to the client
• Prevention of infection. In the past, oxygen that was delivered by an oxygen mask, nasal cannula or nasal catheter was humidified to prevent drying of the mucous membranes. Normal practice in most healthcare agencies is to use only sterile methods of humidification and dispose of the equipment according to infection-control or manufacturer’s guidelines to reduce the potential for nosocomial infections. Oxygen masks and cannulas provide sufficient atmospheric water to humidify the oxygen
• Reducing any anxiety that the client or their significant others experience related to the administration of oxygen. Some people may feel that the administration of oxygen is a sign that the client’s condition is deteriorating, and clients using face masks may experience anxiety related to having both their nose and their mouth covered. The nurse should explain the purpose of the oxygen and the equipment that is being used. Some people may be educated to use the equipment independently and thus feel they have some control over the situation. Frequent visits to the client, prompt attention to their needs and efficient handling of the equipment will help to reduce their anxiety
• Informing the client of the importance of maintaining the delivery device in the correct position, as changing its position may alter the amount of oxygen being delivered
• Assisting the client to meet their hygiene needs. The skin under the tubing, elastic straps or mask should be kept dry to promote comfort and to reduce the risk of skin breakdown caused by humidity or perspiration. Both the client’s face and face mask should be wiped dry at least every 2 hours, and the skin under the delivery device checked for signs of pressure or irritation. Oral and nasal hygiene needs should be met and a water-based cream or balm may be applied to the lips or nares to prevent dryness and discomfort
• Replacing the mask with a nasal cannula if necessary, while the client is eating or having their oral hygiene needs met
• Measuring the client’s temperature by the tympanic or axillary route rather than the oral route, as placement of the thermometer in the mouth may cause further ventilatory distress
• Monitoring the client’s condition constantly to assess the effectiveness of the treatment. The client should be observed for signs of hypoxia or oxygen toxicity. Hypoxia may occur if the oxygen concentration is inadequate or if the equipment is not functioning properly. Oxygen toxicity is more likely to occur if the client is receiving high concentrations (e.g. over 50%), which can be detrimental to the central nervous system. Manifestations of oxygen toxicity include nausea, muscle twitching, dizziness, restlessness and irritability, convulsive seizures and coma. Prolonged administration of high concentrations of oxygen may also cause damage to the linings of the bronchi and alveoli, resulting in pulmonary congestion or collapse of lung tissue. Any indications of hypoxaemia, hypercapnia (CO2 retention) or toxicity must be reported immediately, as the concentration of oxygen being administered may need to be adjusted. It should also be noted that people with chronic obstructive airways disease, such as emphysema, may have an ‘oxygen drive’, in which their respiratory rate is controlled by decreasing levels of oxygen, as opposed to the normal regulation of respiratory rate, which is due to an increasing CO2 level. These clients are never prescribed high-flow oxygen, as it reduces their respiratory drive and rate and increases hypercapnia
• Observing the client closely after oxygen therapy has been discontinued, as the therapy may need to be resumed if signs of hypoxia become evident.
Handling the oxygen equipment. The equipment used to deliver oxygen to the person should be cared for in the manner specified in the healthcare institution’s policy manual. Most of the delivery devices are disposable, which reduces the risk of cross-infection.
Education
Planning for a client’s discharge from hospital is of particular importance if their respiratory disorder is chronic or recurrent. The client must be provided with sufficient information because, by understanding their condition and how to manage the symptoms, they will be better able to cope with chronic respiratory disease. The client should be encouraged to pursue as normal a lifestyle as possible and should be given information about:
• The importance of avoiding factors that may precipitate or exacerbate their condition, such as extremes of temperature, exposure to allergens or environmental irritants, fatigue or emotional stress
• The importance of avoiding close contact with clients who have a respiratory tract infection
• The importance of contacting their medical officer at the first sign of a respiratory tract infection
• The nature and correct use of any prescribed medications, nebulisers or aerosol therapy
• Public health education about smoking and its relationship to lung cancer and chronic obstructive pulmonary disease; the means of preventing droplet-spread infection; and the effects of air pollutants on the respiratory tract
• Immunisation against infections such as pertussis, influenza and TB
• How and when to use oxygen, which a client may need to have immediate access to at all times
• When to contact their medical officer or go to hospital (e.g. if the measures implemented at home fail to sufficiently control their symptoms).
Summary
The human body requires oxygen and nutrients in order to survive. The circulatory system is the means by which every cell in the body is supplied with oxygen and nutrients, and the means by which the cells’ waste products are transported to various organs for excretion. The circulatory system consists of the cardiovascular and the lymphatic systems. The cardiovascular system is composed of the blood, the blood vessels and the heart. The lymphatic system consists of lymph, lymphatic capillaries, vessels, nodes and ducts.
Blood is a viscous substance composed of a fluid (plasma) in which three types of formed elements are suspended—erythrocytes, leucocytes and platelets—each of which has specific functions. The overall functions of blood are to transport oxygen, nutrients and other substances to the cells, transport wastes away from the cells, protect the body against infection, distribute heat evenly throughout the body and prevent a loss of blood by means of a clotting mechanism. Blood is pumped by the heart into the major arteries, which then form increasingly smaller arteries and eventually arterioles. Arterioles are continuous, with a network of minute vessels called capillaries. Blood then enters small veins or venules, which join to form veins. The veins unite to form the major veins, which transport the blood back to the heart. Blood is in constant circulation around the body, in either the systemic, pulmonary or portal circulation. The lymphatic vessels pass through one or more nodes, the functions of which are to filter and destroy microorganisms and to produce lymphocytes, antibodies and antitoxins.
The heart is a hollow muscular organ situated in the thoracic cavity. It pumps deoxygenated blood to the lungs, and oxygenated blood to all parts of the body.
The act of breathing allows the passage of oxygen and carbon dioxide to and from the lungs, while the cardiovascular system transports these substances to and from the cells. Ventilation is controlled by centres in the brainstem that are sensitive to CO2 level, while certain factors such as a client’s clinical condition, disease, physical activity or emotions affect the rate, rhythm and depth of breathing. Diffusion is the process by which oxygen and CO2 molecules are transported between the alveoli and the capillary network, and into and out of cells. Diffusion abnormalities can result from cardiac abnormalities such as cardiac failure causing pulmonary oedema, or respiratory disorders that cause a reduction in the amount of functioning lung tissue or fibrosis of the alveolar walls.
Respiratory dysfunction results from inadequate ventilation, from abnormalities of diffusion through the pulmonary membrane or inadequate transport from the lungs to the tissues. In addition to abnormalities of the lungs or respiratory structures, dysfunction of other body systems such as the cardiac system can adversely affect respiratory function, and vice versa. The major manifestations of respiratory system disorders are chest pain, cough, voice change, dyspnoea, altered ventilations, hypoxia and thoracic skeletal abnormalities. Disorders of the respiratory system can be classified as those occurring from multiple causes, from infection, as a result of neoplasms or obstruction or as a result of injury. Specific diagnostic tests used to assess function of the systems include full blood examinations, urea and electrolytes, ultrasound, pulmonary function tests, oximetry, chest x-ray, lung scan, blood gas analysis, cultures, sputum cytology, skin tests, bronchoscopy and thoracentesis.
Care of the client with a respiratory system disorder includes promoting a clear airway, promoting local hydration, proper positioning, administration of medications, oronasopharyngeal suction, chest physiotherapy and the administration of oxygen. The nurse may be required to obtain a specimen of sputum for laboratory examination, to obtain a nasal or throat swab or to administer inhalation therapy. A client with a specific disorder of the respiratory system may require the insertion of an artificial airway, and/or mechanical ventilation. The insertion of chest tubes may be necessary to promote the drainage of air or fluid from the pleural space. Care of clients with cardiac or lymphatic disorders include similar care to that of a respiratory client but may also include fluid restrictions, weighing and attention to chest or limb pain and skin integrity. Specific disorders of the circulatory system may require surgical intervention, which includes pacemaker implantation and heart or bone marrow transplantation.
Some clients require the administration of oxygen, which can be delivered using one of the various devices available. Whenever oxygen is being administered, the nurse must promote the client’s safety and comfort as part of assisting them to meet their need for oxygen. Legislation exists to protect the client against environmental pollution. The aims are to ensure that clients in their place of work are not exposed to high levels of respiratory tract pollutants and irritants, and to control the processing, handling and sale of foods that may otherwise be responsible for the transmission of diseases.
The community health nurse, who plays a major role in illness prevention, health maintenance and health promotion, can make a significant contribution in reducing the incidence of cardiac and respiratory disease through the planning and implementation of community education programs.
1. A 36-year-old male professional cyclist is admitted to accident and emergency with a provisional diagnosis of spontaneous right-sided pneumothorax. What clinical features would you expect to see in this client? Describe the nursing procedures that would be performed to alleviate the client’s respiratory distress.
2. Mrs Peters, 78, has cardiac failure from a 23-year history of chronic hypertension. She is prescribed one Lasix (frusemide) daily to promote diuresis but continues to drink more than her allowable daily limit, and her lower peripheries appear oedematous. She says she drinks because the ‘Lasix makes her thirsty’, and she cannot stop herself drinking. What nursing measures could you put in place to reduce her input and her thirst to prevent further oedema?
3. Mr Ahmed has recently migrated to Australia to join his family. He has presented at the local medical clinic because he has become increasingly tired, has had a persistent cough and has been losing weight. What questions would be important to ask when conducting the nursing history?
1. Discuss the structure and function of the respiratory and cardiovascular systems and how they interact together.
2. Explain the process of respiration.
3. Explain the process of ventilation.
5. List some of the common clinical features of respiratory disease.
6. List some of the most common manifestations of cardiovascular disease.
7. Describe the differences in cardiac pain for angina and myocardial infarction.
8. What are the main aims of nursing care for a client with a respiratory or cardiovascular disorder?
9. Describe the nursing care for a client receiving oxygen therapy.
References and Recommended Reading
Barnett M. A practical guide to the management of a tracheostomy. Journal of Community Nursing. 2008;22(12):24–26.
Berman A, Snyder S, Kozier B, et al. Kozier and Erb’s Fundamentals of Nursing. Vol 2. 2nd edn. Pearson, Frenchs Forest, NSW, 2012.
Crisp J, Taylor C. Potter & Perry’s Fundamentals of Nursing, 3rd edn., Sydney: Elsevier, 2009.
deWit SC. Fundamental Concepts and Skills for Nursing, 2nd edn. Philadelphia: WB Saunders, 2005.
Dougherty L, Lister S. The Royal Marsden Hospital Manual of Clinical Nursing Procedures, 8th edn. UK: Wiley-Blackwell, 2011.
Earis JE, Pearson MG. Respiratory Medicine. London: Times Mirror International Publishers, 1995.
Elliot M, Tate R, Page R. Do clinicians know how to use pulse oximetry? A literature review and clinical applications. Australian Critical Care. 2006;19(4):139–144.
Giles TL, Lasserson TJ, Smith B, et al. Continuous positive airway pressure for obstructive sleep apnea in adults. Cochrane Database Systematic Reviews. 2006;3:CD001106. [Cochrane summary]
Guyatt GH, McKim DA, Weaver B, et al. Development and testing of formal protocols for oxygen prescribing. American Journal of Respiratory and Critical Care Medicine. 2001;163(4):942–946.
Hargrave-Huttel RA. Medical Surgical Nursing, 3rd edn. Philadelphia: Lippincott, 2001.
Hawley R, King J, Weller BF. Australian Nurses’ Dictionary, 5th edn. Sydney: Baillière Tindall, 2012.
Joanna Briggs Institute Evidence Based Nursing and Midwifery. Vital signs. Best Practice. 3(3), 1999.
Jones I. Cardiac Care: an Introductory Text. London & Philadelphia: Whurr, 2006.
Kapit W, Meisami ME. The Physiology Coloring Book, 2nd edn. San Francisco: Benjamin Cummings, 2000.
Lemmi FO, Lemmi CAE. Physical Assessment Findings. Philadelphia: CD-ROM, WB Saunders, 2000.
Lewis SM, Heitkemper MM, Dirksen SR. Medical–Surgical Nursing. Assessment and Management of Clinical Problems, 6th edn. St Louis: Mosby, 2004.
Marieb EN. Essentials of Human Anatomy & Physiology. San Francisco: Pearson/Benjamin Cummings, 2009.
Marieb EN, Hoehn K. Human Anatomy and Physiology, 8th edn. San Francisco: Pearson, 2010.
Martin L. (nd) PaO2, SaO2 and oxygen content. Online. Available: www.lakesidepress.com/pulmonary/ABG/PO2.htm.
Mir MA. Atlas of Clinical Diagnosis, 2nd edn. Edinburgh: Saunders, 2003.
Nolan JD. Prehospital and resuscitative airway care: should the gold standard be reassessed? Current Opinion in Critical Care. 2001;7(6):413–421.
Oh H, Seo W. A meta-analysis of the effects of various interventions in preventing endotracheal suction-induced hypoxemia. Journal of Clinical Nursing. 2003;12(6):912–924.
Peackock WFIV, Tiffany BR. Cardiac Emergencies. New York: McGraw-Hill Medical Publishing, 2006.
Pedersen CM, Rosendahl-Nielsen M, Hjermind J, et al. Endotracheal suctioning of the adult intubated client—what is the evidence? Intensive Critical Care Nurse. 2009;25(1):21–30.
Potter PA, Perry AG. Fundamentals of Nursing, 7th edn. St Louis: Mosby, 2008.
Potter PA, Perry AG, et al. Fundamentals of Nursing, 8th edn. St Louis: Mosby, 2013.
Santos C, Ferrer M, Roca J, et al. Pulmonary gas exchange response to oxygen breathing in acute lung injury. American Journal of Respiratory and Critical Care Medicine. 2000;161:26–31.
Tollefson J. Clinical Psychomotor Motor Skills, 4th edn. Southbank: Thomson, 2011.
Tortora GJ, Grabowski SR. Principles of Anatomy and Physiology, 9th edn. New York: Wiley & Sons, 2000.
Zitelli BJ, Davis HW. Atlas of Paediatric Physical Diagnosis, 3rd edn. St Louis: Mosby, 1997.
American Association for Respiratory Care, www.aarc.org.
American Journal of Respiratory and Critical Care Medicine, http://ajrccm.atsjournals.org.
American Lung Organisation (oxygen therapy), www.lungusa.org/site/c.dvLUK9O0E/b.23013/k.82B3/Oxygen_Therapy_Fact_sheet.htm.
Australian Resuscitation Council, www.resus.org.au.
Children’s Virtual Hospital (electric airway: upper airway problems in children), www.vh.org/pediatric/provider/pediatrics/ElectricAirway/ElectricAirway.html.
eMedicine (altitude illness—pulmonary syndromes), www.emedicine.com/emerg/topic795.htm
Joanna Briggs Institute www.joannabriggs.edu.au (use the search function to find a variety of research evidence)
Oxygen therapy: the first 150 years. http://thesis.library.adelaide.edu.au/uploads/approved/adt-SUA20060503.162655/public/02whole.pdf.
Pleur-evac setup, www.medtrng.com/blackboard/chest_tube_care_and_monitoring.htm.
The four most important equations in clinical practice, www.globalrph.com/martin_4_most.htm.