CHAPTER 37 Mental health
At the completion of this chapter and with further reading, students should be able to:
• Understand the continuum of mental health and mental illness
• Identify factors that influence the development of mental health
• Reflect on the causes and impact of stigma on people with mental illness
• Understand the roles of the mental health nurse and the mental health team
• Gain an overview of the care issues involved when clients experience anxiety, depression, aggressive, self-destructive, hyperactive or confused behaviour
• Develop an awareness of some of the basic legal and ethical issues in the field of mental health nursing
Mental health nursing is a specialised field of nursing. A variety of educational programs is aimed at preparing mental health nurses (MHNs) to work specifically and effectively with clients who have mental health disorders. A nurse who has not undertaken a course specific to mental health nursing may be required to assist in caring for a client with a mental illness. The nurse may be required to work in a psychiatric unit or ward within a general hospital, or to assist in caring for a client who has been admitted to a general medical or surgical ward with a physical illness but has a concurrent mental health problem. It is therefore important that every nurse has a basic understanding of mental health, mental illness and the principles of care related to clients who are experiencing a disturbance in mental wellbeing. It is not the aim of this chapter to provide the reader with comprehensive knowledge and skills to care for clients with mental health disorders. Rather, this chapter aims to introduce nurses to the basic concepts of mental health nursing, some of the theoretical frameworks that underpin psychiatric care and to raise awareness of some legal and ethical issues that confront mental health nurses. The texts and online resources listed at the end of this chapter provide more detailed information.
I would wake up in the morning feeling like I didn’t want to face the day. There was a black cloud hanging over me. I wanted to stay in bed and shut out the world. I felt at these times that I was in an absolute pit of hopelessness and despair about life and I didn’t want to go on. I was a burden to myself and my family. My sister took me to see my doctor and I was admitted to a psychiatric hospital. I didn’t want to be there because I believed no one could help me. After some time the nursing care and antidepressant medication I was prescribed helped me to slowly climb out of my pit of despair. One day I found myself enjoying looking at the autumn leaves falling and I knew that I was getting better. Now I understand that depression is a severe illness and I will look for help when I feel myself slipping back.
CONCEPTS OF MENTAL HEALTH AND MENTAL ILLNESS
Perhaps the most important aspect of understanding mental illness is being able to define the difference between mental illness and mental health. This first section aims to help nurses gain an understanding of mental health and mental illness and the factors that impact on both.
What is mental health?
The concept of mental health is difficult to define, as mental health is much more complex than merely the absence of a mental illness. There are numerous definitions of what constitutes mental health. It has been defined as a state in which people are able to cope with, and adjust to, the recurrent stresses of everyday living in an acceptable way (Watkins 2002). It has also been defined as the ability of people to cope well with stress both internal and external (Antai-Otong 2007). According to Barkway, ‘a person can enjoy mental health regardless of whether or not they are diagnosed with a mental illness if they have a positive sense of self, personal and social support with which to respond to life’s challenges, meaningful relationships with others, access to employment and recreation activities, sufficient financial resources and suitable living arrangements’ (cited in Elder et al 2009:120). For most people the feelings associated with mental health will be present sometimes and not others and will vary in intensity at different times. According to this view, then, mental health is a state that can change frequently and that can fluctuate according to specific circumstances. Touhy & Jett (2009) capture the concept of fluctuation in this definition:
Mental health is like a violin with strings of interaction, behaviour, affect (mood) and intellect. All of this together may produce a pleasant or stimulating melody, or they may be discordant and irritating. The tune constantly changes. No one is entirely mentally unhealthy and no one is fully mentally healthy at all times.
The terms mental health and mental illness are often used interchangeably but they should not be: the difference between the two needs to be clear (Elder et al 2009). The American Psychiatric Association (APA) defines mental illness or mental disorder as an illness or a syndrome with psychological or behavioural manifestations and/or impairment in functioning due to a social, psychological, genetic, physical/chemical or biological disturbance (Shives 2005:12).
Clinical Interest Box 37.1 illustrates some differences between mental health and mental illness.
CLINICAL INTEREST BOX 37.1 Some differences between mental health and mental illness
(Compiled from Varcarolis et al 2010)
| Signs of mental health | Signs of mental illness |
|---|---|
| Happiness | Major depressive episode |
| Control over behaviour | Control disorder: undersocialised, aggressive |
| Shows repetitive and persistent pattern of aggressive conduct in which the basic rights of others are violated | |
| Appraisal of reality | Schizophrenic disorder |
| Effectiveness in work | Adjustment disorder with work (or academic inhibition) |
| Shows inhibition in work or academic functioning whereas previously there was adequate performance | |
| Healthy self-concept | Dependent personality disorder |
| Satisfying relationships | Borderline personality disorder |
| Effective coping strategies | Substance dependence |
| Repeatedly self-administers substances despite significant substance-related problems (loss of employment, family and social networks) |
Development of mental health
According to Shives (2008) the factors that influence the development of mental health relate to three main areas: inherited characteristics, nurturing during childhood and life circumstances.
Inherited characteristics
It is believed by some theorists that the ability to maintain a mentally healthy and positive outlook on life is in part connected to a person’s genetic make-up, just as inherited defective genes are thought to predispose particular people to illnesses such as schizophrenia and depression.
Nurturing during childhood
Nurturing during childhood relates primarily to the relationships that develop between children, their parents and their siblings. It is thought that positive relationships, those that promote feelings of being loved, secure and accepted, facilitate the development of children into mature and mentally healthy adults. It is thought that negative relationships may result when children experience maternal deprivation, parental rejection, serious sibling rivalry and early communication failures. Such relationships are more likely to result in a poor sense of self-worth and a lower level of mental health (Shives 2008). The quest for a sense of self begins in childhood; children who have positive nurturing experiences are more likely to have a stronger sense of identity than those who have negative nurturing experiences (Watkins 2002).
Life circumstances
Life experiences can influence mental health from birth onwards. Positive life experiences include pleasurable times and success at school and with friends, a good job, financial security and good physical health. Negative experiences include poverty, poor physical health, unemployment and unsuccessful personal relationships (Shives 2008).
Different people will react to childhood experiences and life circumstances in different ways. Some, despite negative circumstances, will develop positive strategies for coping and will not become mentally ill. Generally it is people who have not achieved a strong sense of identity who are more prone to mental illness (Watkins 2002). Perhaps this is most clearly understood when considering the mental health of Indigenous populations. It is not difficult to imagine how the effects of colonisation, the removal of children from their families, the loss of traditional lifestyle and cultural practices and the resulting social disruption may impact negatively on mental wellbeing. It is generally understood that the difficulties involved in belonging and adjusting to two different cultural contexts can make it difficult to establish a strong sense of identity. The difficulties faced by Indigenous people have led to some serious mental health concerns. For example, there are worrying levels of depression, substance misuse, self-harm, harm to others and suicide in Aboriginal people in Australia that are at higher rates than in the non-Indigenous population (Australian Bureau of Statistics (ABS) and Australian Institute of Health and Welfare (AIHW) 2011).
Nurses working with Indigenous people can better empathise and not negatively judge behavioural signs of mental ill-health if they recognise that it often stems from deep mental anguish and spiritual sorrow relating to the effects of European invasion (Brown 2001).
What is mental illness?
Just as it is difficult to arrive at a precise definition of mental health, so too is it difficult to succinctly define mental illness because it is often related to what a given society considers is normal or acceptable behaviour and, as with mental health, mental illness is a matter of degree.
What society considers normal
People tend to evaluate the behaviour of others based on their own social, cultural, ethical and behavioural standards. Therefore, behaviour that is regarded by one person as acceptable and normal may be perceived by another person as totally unacceptable. In addition, what is accepted as normal in a society may change over time. For example, homosexuality was previously considered a diagnosable clinical mental disorder but is now no longer classified as a mental disorder (Antai-Ojong 2003). When a person’s behaviour is in question it is appropriate to ask ‘Who is qualified to decide whether this behaviour is acceptable or not?’ and ‘What is the meaning and relevance of this behaviour in relation to the context in which it is occurring and to the person’s society, religion and culture?’
In every society and cultural group there are different interpretations of certain behaviours and events. For example, in western psychiatric terms, visual or auditory hallucinations (images or sounds that are seen or heard by an individual but by no one else) are viewed as abnormal and a sign of mental illness, whereas in some cultures these happenings are viewed as experiences of symbolic and spiritual importance and those experiencing them may be revered as visionaries rather than mentally ill (Varcarolis et al 2010).
A matter of degree
Anxiety, fear, anger, sadness and the need to be alone are feelings commonly identified in mental illness but they are normal feelings experienced at different levels of intensity by most people at various times. Depending on the intensity of the emotions, people may not feel as mentally healthy as they do at other times but will not necessarily be classified as mentally ill. It is when the feelings are exaggerated and extend over longer periods of time than deemed normal that the person is likely to seek professional help and be diagnosed as having a mental illness. For example, a diagnosis of a depressive disorder is likely when sadness or feelings of being ‘down in the dumps’ become deep, long-lasting feelings of despair that the person cannot escape from without professional help. Mental illness or mental disorder are therefore terms used to designate changes from normal mental functioning that are sufficient to become, and be diagnosed as, a clinical disorder. Broadly, mental illness can be defined as a state in which an individual exhibits disturbances of emotions, thinking and/or action, but it can be defined in a multitude of ways.
Clinical Interest Box 37.2 provides a range of definitions of mental illness.
CLINICAL INTEREST BOX 37.2 Definitions of mental illness
• Mental illness is a term that refers to all the different types of mental disorders. These include disorders of thought, mood or behaviour that cause distress and result in a reduced ability to function psychologically, socially, occupationally or interpersonally (Mayo Foundation for Medical Education and Research 2002)
• A disease that causes mild to severe disturbances in thought and/or behaviour, resulting in an inability to cope with life’s ordinary demands and routines (National Mental Health Association (USA) 2012)
• A disorder causing abnormal behaviour more often than in most people (Shives 2005)
• Psychopathology exhibiting frequent irresponsibility, the inability to cope, being at odds with society and an inaccurate perception of reality (Shives 2005)
• The absolute absence or constant presence of a specific behaviour that has social implications regarding its acceptance (Shives 2005)
• The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM) is a classification system for mental illness. In the fourth edition (DSM-IV), mental illness is defined as being a clinically significant behaviour or psychological syndrome or pattern that occurs in an individual and that is associated with present distress (e.g. painful symptom) or disability (i.e. impairment in one or more areas of functioning) or with a significantly increased risk of suffering death, pain, disability or an important loss of freedom. In addition, this syndrome or pattern must not be merely an expectable culturally sanctioned response to a particular event, for example, the death of a loved one. Whatever its original cause, it must currently be considered a manifestation of a behavioural, psychological or biological dysfunction in the individual. Neither deviant behaviour (e.g. political, religious or sexual) nor conflicts that are primarily between the individual and the society are mental disorders unless the deviance or conflict is a symptom of a dysfunction in the individual, as described above (American Psychiatric Association 2002).
There is no clear line that divides mental health from mental illness; the two grade into one another.
Table 37.1 provides some areas of comparison between the two but it should be noted that, while these are general traits that mentally healthy or mentally ill people tend to share, different types of mental illness manifest with different effects and with different levels of intensity. In addition, mentally healthy people may experience more than one type of mental dysfunction at different periods in their lives.
Table 37.1 Areas of comparison between mental health and mental illness*
| Attribute | The mentally healthy person | The mentally ill person |
|---|---|---|
| Self-concept | ||
| Relationships | Inability to cope with stress can result in disruption, disorganisation, inappropriate responses and unacceptable behaviour that make it difficult to meet the expectations of others in work or social environments. This means that there may be an inability to establish or maintain meaningful relationships. These factors may result in a limited social support network | |
| Outlook on life | Optimistic and positive view, sense of purpose and satisfaction | Tends to a pessimistic negative view of present and future |
| Coping and adaptation | Able to tolerate stress and return to normal functioning after stressful events. Can cope with feelings such as frustration and aggression without becoming overwhelmed | Can feel overwhelmed by even minor levels of stress and may react with maladaptive behaviour |
| Judgment/decision making | Uses sound judgment to make decisions and is able to problem solve | May display poor judgment and avoid problems rather than attempting to solve them |
| Characteristics/traits | Can delay gratifcation | May feel an urgency to have personal wants and needs met immediately and may demand immediate gratifcation |
| Level of functioning | ||
| Perceptions | Able to differentiate between what is imagined and what is real because can test assumptions by considered thought. Can change perceptions in light of new information | May be unable to perceive reality |
* It should be noted that these are general points only. Different types of mental illness manifest with different effects and, while there are traits that mentally healthy people tend to share, many mentally healthy people may experience several areas of dysfunction at different periods in their lives. Mental illness may occur as a temporary inability to cope; it may occur episodically with long periods of mental health in between; or it may occur as a chronic condition that is constantly present.
Signs and symptoms of mental illness
Symptoms of mental illness occur on a continuum and range from minimal to severe (Antai-Ojong 2003). A person usually receives a diagnosis of having a mental illness when the level of mental distress causes them to seek professional help or when others in society perceive that they need professional psychiatric help. It is important to recognise that, in relation to the differences between mental health and mental illness, there is a ‘grey’ area into which all individuals may enter from time to time. Those with a severe and long-term psychiatric disorder may dip back into relative mental health and reality-based living for a while and, similarly, sometimes the stresses of everyday living are so overwhelming that the most well-adjusted ‘normal’ person may experience marked irrational thoughts, feelings and actions. Therefore, as in the case of physical illness such as diabetes, heart disease or cancer, anyone can develop a mental illness. A mental illness is not the fault of the person affected, and the cause may be related to a combination of biological, psychological and sociocultural factors.
Symptoms of mental illness include changes in personal habits, social withdrawal and changes in mood and thinking. While particular symptoms occur with specific disorders, there are warning signs that indicate the presence of a mental health problem. Clinical Interest Box 37.3 provides examples of early warning symptoms of mental illness that may occur in children, adolescents and adults.
CLINICAL INTEREST BOX 37.3 Warning signs and symptoms of mental illness
People may have one or two of these or other symptoms at any one time. This does not necessarily mean there is cause for alarm, but it is advisable they be assessed professionally. A combination of multiple symptoms is a strong signal that professional assessment and help should be sought as soon as possible.
In younger children
• Decline in standard of performance in school work or activities that does not pick up again over time
• The child is not managing or coping with tasks as expected at their developmental age
• Suggestions from teachers that there may be a learning difficulty, a behavioural problem or a problem making friends
• Persistent crying, waking at night or nightmares
• Persistent disobedience or aggression
• Excessive anxiety (e.g. preoccupation with fears of burglars, barking dogs, parents getting killed)
• Constant fighting with other children, and reports from school of the child being ‘angry or disruptive’
• Refusal to go to bed, inability to sleep or a need to sleep with, or close to, parents
• Decreased interest in playing
• The child tries to stimulate themself in various ways (e.g. hair pulling, rocking of the body, head banging)
• The child constantly says things that indicate low self-esteem (e.g. ‘I’m dumb’, ‘I never do anything right’, ‘No one likes me’, ‘I’m too skinny’, or too fat, too tall, too ugly, etc)
In older children and adolescents
• Frequently asks or hints at the need for help
• Fears or phobias that interfere with normal activities
• Change in sleeping/eating/hygiene habits
• Isolating self from others excessively
• Involved in beating up others
• Inability to cope with problems and usual daily activities
• Excessive complaints about physical aches and pains
• Defiance of authority, truancy, theft and/or acts of vandalism
• Demonstrates ritualistic behaviours (e.g. preparing for bed, a meal or going out) using routines that are exact, precise and never vary
• Provocatively sexual behaviour that is not appropriate
• Participates in mutilating or killing animals
• Persistent and prolonged low mood (a major concern, especially if accompanied by poor appetite or thoughts and talk of death or signs of self-mutilation)
In adults
• Prolonged periods of sadness/low mood and apathy
• Feelings of extreme highs and lows
• Unrealistic or excessive fears
• Marked changes to eating/sleeping/hygiene or other habits
• Strong feelings of anger/outbursts of violent behaviour
• Increasing inability to cope with usual activities of everyday life
• Denial of anything being wrong even in light of obvious problems
• Numerous unexplained physical ailments
• Thoughts/talk about suicide or homicide (professional help needed immediately)
(American Psychiatric Association 2002; National Mental Health Association (USA) 2012)
Who is most at risk of developing a mental illness?
Anyone can develop a mental illness but some groups of people in society are particularly at risk. Clinical Interest Box 37.4 identifies groups of people at greater risk of mental illness.
CLINICAL INTEREST BOX 37.4 People at risk of mental illness
Anyone can develop a mental illness, but people at particular risk include:
• Adolescents: adolescents face a period of enormous physical, psychological and social change. Some adolescents may not have sufficient resources to cope with the demands placed on them at this challenging stage of life and to complete the developmental tasks necessary to move successfully from adolescence to adulthood. Erik Erikson’s theory of personality development (Erikson & Erikson 1997) is one that is useful to explore in relation to life stages and developmental tasks
• New parents: new parents face a multitude of stressors (things that trigger a stress response) as well as many pleasures connected with a new baby. Stressors may include conflict over the acceptance of the pregnancy, transition from being a couple to being parents, loss of financial income, a baby’s constant demands and anxiety about the infant’s welfare
• Women: women face factors such as a disadvantaged status in society, internal conflict arising from decisions about whether to pursue a career, become a home-maker or try to achieve both, or being subjected to domestic violence or abuse. These are social factors that may possibly predispose some women to mental illness
• Older adults (male and female): older adults may face many stressors, including loss of work role status because of retirement, reduced income, fear of declining physical and mental abilities, relocation, death of a partner and/or friends and siblings of similar age. The effect of these multiple losses may accumulate and leave some older adults at risk of mental illness
• Refugees and migrants: these people may experience a grief reaction on leaving their homeland, friends and family to live in a country where the cultural practices, values and beliefs are different and where they may be considered of low status and worth. It may be difficult for some migrants to work successfully through their grief because of language barriers, the stress from job and financial uncertainty and lack of support from relatives and friends left behind. Some refugees and migrants may experience problems of adjustment, isolation and loneliness, each of which may contribute to mental illness. In some cases refugees have experienced torture and trauma in their country of origin, which creates a high risk of developing a posttraumatic stress disorder (Griffiths et al 2003)
• Physically or intellectually impaired persons: factors such as isolation, lack of meaningful relationships, social restrictions caused by disabilities, poor self-esteem and negative stigmatising community attitudes towards people with disabilities are all aspects of experience that can elevate the risk of mental illness, particularly anxiety and depression (Dewer & Barr 1996)
Many people from all age groups and of different social, educational and cultural backgrounds cope with highly stressful events and accumulative stressors.
Classification of mental disorders
There are more than 200 classified forms of mental illness. These include:
• Cognitive disorders (e.g. dementia, delirium)
• Substance-related disorders (e.g. alcohol abuse or dependence, drug abuse or dependence)
• Anxiety disorders (e.g. phobias, panic disorder, obsessive disorder)
• Schizophrenia and other psychotic disorders (e.g. paranoid or catatonic-type schizophrenia)
• Mood disorders (e.g. depression, bipolar disorder (mixed mood))
• Personality disorders (e.g. antisocial personality disorder, dependent personality disorder)
Diagnosis
The APA’s Diagnostic and Statistical Manual of Mental Disorders (DSM) is a respected and influential classification system under which a mental illness is determined according to the symptoms experienced and the clinical features of the illness. The International Classification of Disease (ICD) is produced by the World Health Organization and is mainly used In Europe. It also assists with diagnosis and classification. In Australia, New Zealand and the United States the fourth edition of the DSM (DSM-IV-TR) is most commonly used. (DSM-V is due for publication in May 2013.)
There are many categories of classification but mental illness is mainly classified within the following areas:
• Thought disorders, such as schizophrenia, which disrupt the ability to think and perceive things clearly and logically and can impair a person’s perception of reality
• Mood disorders, which affect how a person feels and can result in persistent low mood (depression) or cycles of low mood and euphoria (bipolar disorder)
• Behavioural disorders, which involve people acting in potentially destructive ways, including eating disorders such as anorexia nervosa and bulimia
• Mixed disorders, which have components of two or more of the other categories (Mayo Foundation for Medical Education and Research 2002).
Diagnosis according to the DSM (IV) has the benefit that clients may feel great relief when they have a diagnosis that helps them make sense of what is happening to them, and a medical diagnosis can guide clinical treatment. But this diagnostic system has a disadvantage in that a diagnosis can also be a label that has negative connotations; for example, a label of schizophrenia or a personality disorder is associated with significant social stigma. Diagnostic labels describe certain types of behaviour but they indicate very little about the nature or causes of the experience.
Mental health nurses develop nursing diagnoses in response to the client’s experience, emotions and behaviours. Nursing care responds holistically to the client’s biological, psychosocial, spiritual and environmental needs and specifically addresses the client’s feelings and behavioural responses to those feelings, many of which are common across several different medically classified conditions. Examples of some nursing diagnoses commonly used in mental health nursing are provided in Clinical Interest Box 37.5.
CLINICAL INTEREST BOX 37.5 Examples of identification of issues by nurses used in mental health nursing
• Impaired social interaction: insufficient or excess quantity or ineffective quality of social interactions
• Ineffective coping: inability to form a valid appraisal of the stressors, inability to use available resources
• Chronic low self-esteem: long-standing negative feelings about self or own capabilities
• Self-care deficit: impaired ability to perform or complete activities of daily living (e.g. hygiene, toileting, nutrition)
• Imbalanced nutrition, less than body requirements: intake of nourishment insufficient to meet the body’s metabolic needs
• Powerlessness: perception that one’s own actions will not significantly affect an outcome; a perceived lack of control over a current situation
• Disturbed thought processes: disruption in cognitive abilities and activities
• Disturbed sensory perceptions: alteration in the amount or patterning of incoming stimuli accompanied by a diminished/exaggerated/distorted/impaired response to the stimuli (often used for clients who are experiencing delusions, hallucinations or illusions or have impaired awareness of self/environment)
• Impaired verbal communication: diminished, delayed or impaired ability to understand or transmit verbal messages
• Dysfunctional grieving: prolonged unsuccessful use of strategies and responses by which people attempt to work through the process of grieving
• Risk for injury: potential for injury as a result of environmental conditions interacting with the client’s adaptive and defensive resources
• Risk for self-directed violence; risk for other-directed violence: existence of the potential for an individual to be physically, emotionally or sexually harmful to self or others
• Risk for suicide: potential for self-inflicted life-threatening injury
A mental disorder can be categorised as temporary, episodic or chronic/enduring, according to the way it manifests:
• Temporary: a temporary inability to cope; for example, a single experience of depression. The vague definition of ‘a nervous breakdown’ is a common non-medical term for this kind of isolated non-recurring illness
• Episodic: an illness that occurs episodically; for example, recurrent episodes of a disabling condition such as bipolar disorder (once known as manic depression) or schizophrenia. While the condition is disabling when it occurs, the person affected can often enjoy a comparatively normal life for much, if not most, of the time
• Chronic/enduring: a constant disabling and unrelenting illness that is extremely challenging for the affected person and their families to deal with; for example, a chronic type of schizophrenia or bipolar disorder or irreversible dementia can be disabling.
Although use of the terms psychosis and neurosis to describe particular illnesses is no longer favoured, nurses need to be aware of the meanings associated with each as the terms are still used in some contexts. The terms are out of favour because symptoms ascribed to each condition can occur in the other, and this causes confusion. The term psychosis refers to disorders that are so marked and incapacitating that the person who is afflicted is out of touch with reality and lacks insight into the illness and the associated behaviours, which may be unusual or bizarre. Psychosis was the term traditionally used to describe disorders such as schizophrenia and bipolar disorder, in which the symptoms experienced were quite different to those experienced by other people and included delusions and hallucinations (Elder at al 2009). Clinical Interest Box 37.6 provides explanations and examples of delusions and hallucinations.
CLINICAL INTEREST BOX 37.6 Delusions and hallucinations*
(Fortinash & Holoday Worret 2007; Shives 2005)
| Delusion: a fixed thought or belief that is not reality based or true, is not consistent with the person’s level of education and development or cultural background, and is not amenable to reason. It is categorised as a thought disorder |
| Type | Example |
|---|---|
| Somatic delusions (a false belief involving a body part or function) | A young woman believes her body is rotting away from the inside, her heart is made of ice and is gradually melting because she doesn’t deserve to live |
| Nihilistic delusions (false feeling that the self, others or the world is non-existent) | A client refuses to eat, saying there is no need for him to eat because he has no body |
| Delusions of persecution (oversuspiciousness: the person falsely believes themself to be the object of harassment) | A client believes the staff belong to a cult, are watching his every move and are out to get him. He is afraid to go to sleep for fear of what the staff might do to him |
| Delusions of control (false belief that one is being controlled by an external source) | A client believes her feelings, thoughts and actions are being controlled by aliens who send messages to her via the television, instructing her on what to do |
| Delusions of grandeur (exaggerated beliefs about personal importance or powers) | A client believes he is God and controls the universe |
| Delusions of self-depreciation (beliefs of unworthiness) | A client believes she is ugly and sinful, saying, ‘I don’t deserve to be loved—look at me—it shows that I am full of sin’ |
| Hallucinations: sensory perceptions that are not founded on any external stimuli. They may involve any of the five senses. They are most commonly visual or auditory | |
| Type | Example |
|---|---|
| Visual hallucination | A client tells you that he sees his deceased wife in different areas of his home |
| Auditory hallucination | A 16-year-old client tells you she hears voices in her head saying derogatory things such as, ‘You are worthless, you don’t deserve to live’ |
| Gustatory (taste) hallucination | A middle-aged client with organic brain syndrome complains of a constant metallic taste in his mouth |
| Olfactory hallucination | A 30-year-old client states that she smells ‘rotten garbage’ in her bedroom although no one else can smell anything unusual or unpleasant |
| Tactile hallucination | A middle-aged woman undergoing symptoms of alcohol withdrawal reports feeling ants crawling all over her body although no ants are present |
* Clients can experience delusions and hallucinations together. For example, a client may hear her dead daughter’s voice, see her standing close by and be convinced that she caused her daughter’s death despite of evidence to the contrary that her daughter died as a result of injuries received in a car accident when on holiday with a friend.
Unlike people suffering from a psychotic disorder, those with what used to be termed a neurosis have insight into their condition. For example, a person who has an obsessive-compulsive disorder may experience persistent and intrusive thoughts (obsessions) about personal cleanliness. To decrease the level of anxiety the person may wash their hands hundreds of times a day, even if their hands become red and raw (compulsion to act). When they are extreme, such thoughts and acts may be so unusual and disrupt the person’s life to the degree that to the observer the person is mentally ill. Unlike those experiencing a psychotic disorder, the affected person is aware that the behaviour is abnormal (there is insight into the behaviour and the illness). Despite their condition, people who have what was once classified as a neurosis can often continue to function in society, whereas a person who is psychotic cannot function effectively (Varcarolis et al 2010). Nursing diagnosis should always be developed through the lens of a client-centred approach which respects the client’s social and individual experience of their illness.
Theoretical models and causation of mental illness
Historically the medical profession was prominent in the care of people with mental illness and as a result there has been, and still is, a strong focus on identifying physical causes of mental illness. However, others have looked at psychological, sociocultural, interpersonal and human development factors and there are now many theoretical models used to explain the presence of a mental disorder. Mental health nurses select concepts from the various relevant models that best explain the client’s behaviours, problems and needs. They then draw on these concepts as a basis for client assessment and then for planning, conducting and evaluating care (Varcarolis et al 2010). The following provide very basic examples of a small selection of theoretical models. To work effectively in the area of mental health, however, nurses need a deep and sound understanding of a wide range of models.
The medical or biological model
This model explains mental illness as being caused by physiological malfunction in the body. Physical causes can be separated into acquired and non-acquired factors. Acquired causes include head injury, cerebral infection and substance misuse. Non-acquired causes include genetic transmission, electrical conductivity changes in the brain or alterations to the production and/or activity of neurotransmitters (Elder et al 2009). There is evidence to support biological explanations. For example, studies indicate that depression and schizophrenia may be linked to abnormal neurotransmitter function, and that genetic factors may be linked to both (Elder et al 2009). A medical approach to treating mental illness tends to focus primarily on medication and sometimes includes electroconvulsive therapy (ECT), both of which aim to correct chemical imbalance in the body believed to be caused by abnormal neurotransmitter function in the brain. Emil Kraepelin (1856–1926) is a theorist associated with the origins of the medical model.
Psychological and psychodynamic models
The psychoanalytical model, first conceptualised by Sigmund Freud (1856–1939), is possibly the best known model in this group. Freud’s model viewed human personality as developing predominantly within the first 5 years of life and focused mostly on unconscious, non-rational and instinctual parts of human behaviour (Varcarolis et al 2010). Freud attributed disrupted behaviour in the adult to developmental tasks that were not accomplished successfully at earlier developmental stages. For example, within this theoretical framework a mental illness may be linked to a failure during adolescence to move successfully from dependence on parents to independence. Freud’s mode of treatment was psychoanalysis, which aimed to bring unconscious problems to conscious awareness.
Carl Jung (1875–1961), Melanie Klein (1882–1960) and Erik Erikson (1902–1994) are some of the theorists who expanded on Freud’s thinking about the nature of human development and behaviour. Erikson’s theory has provided nurses with a developmental model that encompasses the entire life span. Erikson studied healthy personalities and focused on human strengths as well as weaknesses, emphasising how people who failed to achieve developmental milestones at various life stages could rectify these failures at later stages (Elder et al 2009).
It was Freud who identified the manner in which humans develop and used defence mechanisms to ward off anxiety that might otherwise be overwhelming and incapacitating (Varcarolis et al 2010). Defence mechanisms prevent conscious awareness of threatening feelings and can be a helpful response in adapting to stress, but their overuse can be a sign of maladaptation to stress and an indicator of mental ill-health. They are particularly relevant in understanding stress-vulnerability and stress-adaptation models of health and illness. Stress-vulnerability/adaptation models recognise that throughout life there is a need for everyone to adapt to change, for example, to adjust to school and then work life, to living with a partner or to becoming a parent or a grandparent and then to retirement and perhaps the death of a spouse. The model views that some people find it more difficult than others to adapt to life’s changes and to cope effectively with the stressors that change can bring. When life results in a stressful situation or there is an accumulation of multiple stressors, people who have been unable to develop and establish adequate coping skills and coping resources are at the highest risk of developing a mental illness.
Social and interpersonal models
Social/interpersonal models draw attention to the impact of factors within a person’s social environment on mental wellbeing. The basic concept is that negative social factors such as low status, low levels of support, isolation and poverty contribute to and increase the risk of developing a mental illness such as depression (Elder et al 2009).
Interpersonal models encompass the premise that internal conflict within one’s personality and particular behaviours may be derived from unresolved conflicts within personal relationships, sometimes during early life experiences. This model also encompasses the premise that an individual’s wellbeing is dependent on the amount of stress experienced and the effectiveness of personal coping strategies in dealing with that stress. Karen Horney (1885–1952), Harry Stack Sullivan (1892–1949) and Hildegard Peplau (1909–1999), a nurse theorist, are some of the important theorists who have conducted research related to social and interpersonal factors and mental health.
Cognitive behaviour models
Cognitive behaviour models stem from the assumption that behavioural responses are learned. Ivan Pavlov (1849–1936) developed the understanding of learned behaviours when he found that when a bell was repeatedly rung each time dogs were given food the dogs began to salivate just at the sound of the bell. This conditioned reflex was termed classic conditioning and is acknowledged as a form of learning that applies to humans, learning in which a previously neutral stimulus comes to elicit a given response through association. For example, behavioural theorists would suggest that children who observe parents responding to every minor stress with anxiety would soon learn the response and would develop a similar pattern of behaviour (Elder et al 2009). According to the behavioural model, this early learning experience would be considered a significant factor in the cause of an anxiety disorder and limited constructive coping strategies in later life.
BF Skinner (1904–1990) added to behavioural theory by introducing the concept of operant conditioning. Operant conditioning refers to the use of reinforcers to motivate the repetition of particular behaviours. The use of positive reinforcement (the continual rewarding of desired behaviours) forms the basis of behaviour modification therapy used to help motivate clients to change undesirable behaviours. It has been effective for clients with phobias, alcohol addiction and a variety of other conditions (Elder et al 2009).
Aaron Beck was one of the early founders of cognitive behaviour therapy (CBT), now a common and often very successful form of psychological treatment. It is based on the view that dysfunctional behaviour is linked to dysfunctional thinking, and that thinking processes are shaped by underlying beliefs. For example, the client with depression believes, ‘I am no good at anything, I’m worthless, and nobody likes me’. Cognitive behaviour therapy is based on helping clients recognise, challenge and change dysfunctional thinking. Beck’s work has primarily focused on helping people with depression but he has expanded the use of CBT to include working with people who have complex disorders such as borderline personality disorder and schizophrenia, and there are distinct signs of success (Elder et al 2009).
Mental health, like physical health, is clearly affected by a multitude of factors. Consequently, mental health nurses and psychiatrists are concerned with all the aspects of people’s lives that distinguish them as human beings. The mental health nurse uses knowledge from the psychosocial and biophysical sciences, and theories of stress vulnerability, personality and behaviour, to develop a framework on which to base the art of nursing. The mental health nurse is an integral part of the interdisciplinary team required to meet the needs of clients who have a mental illness.
THE PROVISION OF CARE
The multidisciplinary team
Many people may be involved in assisting a person who is experiencing a disruption or potential disruption to their mental health. Mental healthcare commonly employs an interdisciplinary team approach to care management. The client’s care, according to individual needs, is planned and implemented by a team composed of mental health nurses, psychiatric social workers, counsellors, clinical psychologists, general or specialist medical officers (depending on the client’s physical status) and pharmacists. Additional team members may be required and, depending on individual needs, these may include: a dietitian; an occupational therapist; a recreational, art, music or dance therapist; complementary healthcare therapist; and a chaplain or other spiritual support person. (See Clinical Interest Box 37.7.)
CLINICAL INTEREST BOX 37.7 Some members of the healthcare team
• The psychiatrist: a physician whose specialty is mental disorders and who is responsible for diagnosis and treatment. A psychiatrist has the legal power to prescribe and to write treatment orders and, as such, is often the team leader
• The mental health nurse: a nurse with experience and expertise in clinical psychiatry, who promotes a holistic approach to care
• The clinical psychologist: a psychologist who has undertaken specialised education in the area of mental health and whose function includes applying and interpreting psychological tests and the implementation of specific therapies such as behaviour modification programs and sexual, marital or family therapy
• The psychiatric social worker: a social worker in the field of mental health, whose function includes assisting the client to prepare a support system that will help maintain their mental health on discharge into the community from an inpatient facility. A social worker may liaise with employers, contacts in day-treatment centres and those providing training and educational programs. The social worker may also assist the client to locate and access sources of financial aid and accommodation
• Occupational, recreational, art, music and dance therapists: according to their specialist areas of expertise, these various therapists assist clients to gain skills that assist them to cope more effectively, to gain or retain employment, to use leisure time in a way that promotes their mental wellbeing and to express their emotions in healthy ways
(Stuart & Laraia 2001; Varcarolis et al 2010)
It should never be forgotten that the most important member of the team is the client, and often clients know what they need to promote their own recovery. Some clients have reflected on the times when they have been at their most vulnerable. For example, some clients who have experienced admissions to acute-care settings have identified that what they need most at times of severe mental distress is somewhere they can feel safe and supported, somewhere they can relax and calm down and someone to be with them who will listen and really hear them (Watkins 2002). While the client may feel the need for medication, it is not appropriate or helpful to implement other therapeutic interventions, such as group therapy, recreational therapy or family therapy, until the client is feeling less distressed and can collaborate in decisions about what sort of interventions will be most helpful. Skilled helping involves actively listening to the client and working collaboratively with the client to achieve a process of recovery. (See Ch 6 for information concerning active listening as a therapeutic measure.) The therapeutic process involves health professionals, including nurses, as facilitators who use their knowledge to help the client become more resourceful and self-reliant. This helping relationship needs to be a participative but never a directive process (Watkins 2002). The model of helping relationships established by Carl Rogers (1961) and the model of skilled helping established by Gerard Egan (1994) are client-centred models of caring on which mental health nurses can reliably base their therapeutic interactions with clients.
Responsibilities of the mental health nurse
Mental health nursing may be described as an interpersonal process in which the nurse uses the presence of self, interpersonal communication skills and a knowledge of physiology, psychology and sociology to help clients in mental distress. A combined understanding of biological processes and psychodynamic processes is essential for the mental health nurse because many people with mental illness have a concurrent physical problem, and the two are often interconnected (Elder et al 2009).
Mental health nurses are very involved in psychiatric inpatient services and in community mental health services. They play a major role in education and health promotion, as well as in the provision of continuing care and counselling for people with mental health problems. For some experienced mental health nurses the role may include conducting specific psychological therapies such as cognitive behaviour therapy, solution focused therapy and acceptance and commitment therapy.
Nursing care aims to help clients cope with the experience of mental illness, prevent relapse and to promote a return to mental health through a successful rehabilitation program. The primary aims of mental health nursing (Watkins 2002) are to help individual clients to:
• Identify and clarify their needs and problems
• Create a better future for themselves (e.g. empower clients by developing self-help strategies)
• Create strategies to enable them to move forward (e.g. clients can become stuck in a particular way of responding to situations).
Rehabilitation is important for people who have been discharged from a psychiatric ward or unit. Some people need minimal support but others represent a population of chronically ill clients who return to hospital periodically over many years and require support in several different areas of their lives. The community mental health nurse and other members of the community mental health team may be involved in:
• Individual and family therapy
• Medical care for concurrent physical problems
• Vocational training and support (Shives 2008).
Recovery and mental illness
The concept of recovery has been apparent for the last few decades and is manifest mainly in policy at various levels such as health services management, practitioners and consumer/survivors of healthcare services (Edward et al 2011). Many consumer/survivors, some of whom were mental health professionals, began to speak about their experiences of mental illness and their individual journey of recovery which led to the development of the consumer-recovery movement (Deegan 1988; Lovejoy 1984). In the United States the consumer-recovery movement was boosted by William Anthony, a rehabilitation expert who challenged the state health system on their vision of recovery that was based on a belief that mental illness was essentially a ‘chronic’ condition with very little hope of getting back to full health (Anthony 2000). According to Anthony (2000), mental health services need to be grounded in the idea that people can recover from mental illness, and that the construction of the service delivery system must be based on this knowledge. From that period of time most western countries adopted an approach to recovery that is based on practices and principles of autonomy and self-determination.
Contemporary mental health nursing care is now based on the recovery principles that refer to the person’s rights to self-determination and inclusion in community life regardless of their diagnosis of mental illness. Recovery principles are based on an approach that hope is central to recovery and that shifting the focus from symptom management and diagnostic labels to one which keeps people well gives their lives value and meaning. Personal and social recovery is the primary focus of contemporary mental health nursing care.
Facilitating development of constructive coping mechanisms
The nurse’s role in stress and stress management has some specific points that need to be highlighted here. To recognise and deal with stress, individuals need to be provided with information about, and helped to recognise:
• Issues and events related to health and illness, and the importance of adhering to sound health practices (e.g. adequate nutrition, sleep, exercise and relaxation) as a way of promoting mental wellbeing
• The dimensions of potential stressors, possible outcomes and the client’s own established positive and negative coping mechanisms and coping resources
• Their existing strengths and develop and maximise their abilities in problem solving, tolerating stress and dealing effectively with interpersonal relationships
• Where and how to gain access to additional coping resources (e.g. vocational training, support groups and counselling).
There is a wide variety of activities that clients may find helpful in promoting coping, but there is no one right or best activity. What works for one person may not work for another. Nurses have a responsibility to provide clients with information and options, but only the client can know what feels appropriate, so the choice of what activities to attempt or to become involved with should ultimately rest with the client. Clinical Interest Box 37.8 provides examples of constructive coping strategies, coping resources and destructive coping mechanisms.
CLINICAL INTEREST BOX 37.8 Examples of constructive coping strategies, coping resources and destructive coping mechanisms
Coping resources
Destructive coping mechanisms
• Always being submissive to others and so failing to get own needs met
• Excessive use of alcohol and/or other drugs or overeating (seeking comfort in substances)
• Promiscuity (seeking love and acceptance in a way that does not improve self-esteem)
• Overuse of defence mechanisms to cope with unacceptable or ambivalent feelings. Defence mechanisms commonly used in a maladaptive manner (Stuart & Laraia 2001) include:
(Beyond Blue, www.beyondblue.org.au); (Stuart & Laraia 2001; Varcarolis et al 2010)
The nurse’s role in educating the public and reducing stigma
One particularly important facet of the community mental health nurse’s role is educating the public about mental illness to reduce the stigma that for many mentally ill people is the biggest hurdle to overcome (Watkins 2002). There is a general lack of knowledge in the community about what constitutes mental illness and about the prognoses of mental disorders; this ensures that mental illnesses are often surrounded by mystery, misinformation and stigma (Weir & Oei 1996). Despite positive interventions in recent years, people suffering from mental illness remain among the most stigmatised, discriminated against, marginalised, disadvantaged and vulnerable members of society (Johnstone 2001) (see Clinical Scenario Box 37.1).
Clinical Scenario Box 37.1
The stigma of mental illness
John was diagnosed with schizophrenia 2 years ago. Getting a diagnosis was such a relief, because then we knew what had caused such a big change in him. The nurses taught us about the illness and now, because we know what to look for, we pick up the early warning signs. He knows where to get help and most of the time he avoids a relapse.
John’s pretty much in control of his illness now, but the thing that’s upset him and us most is the way some people have treated him. He lost his part-time job in the supermarket and even one of his lecturers at college told him he should consider leaving his engineering course because of it. Even my own sister won’t have him babysit his young cousins anymore. John now feels it is not safe to tell anyone about it. How do you think that makes him feel? If it was diabetes that made him ill I wonder if people would have reacted the same.
Several myths about mental illness create fear of those affected and this fear serves to increase stigmatising behaviours and attitudes. For example, there is a widely held perception that people with mental illness are often out of control, unpredictable and may pose a threat. The truth is that most people with mental illness do not behave in this way; however, severe mental distress is often highlighted in the media, and this links images of dangerous behaviour with mental illness in the minds of the public (Watkins 2002). In addition, single, isolated and often very minor criminal acts committed by mentally ill people tend to be sensationalised by the media, contributing to negative stereotypes (Jewell & Posner 1996). Overall, violence in society associated with mental illness is not significant (Elder et al 2009). The Sane Australia Stigmawatch website monitors misuse, misrepresentation or inappropriate references to mental illness in the media (Elder et al 2009).
The lack of accurate knowledge about mental illness that leads to fear, mistrust and sometimes violence against people living with mental illness and their families can also serve to:
• Lower the morale and self-esteem of people living with mental illness
• Prevent people with mental illness from admitting the problem and seeking professional help
• Prevent people with mental illness from gaining paid employment
• Limit the participation of people with mental illness in community activities and force them into a reclusive lifestyle
• Cause families and friends to turn their backs on the mentally ill person when support is most needed.
The picture is not always as dismal as this. Many mental healthcare users are themselves excellent ambassadors for people with mental illness. By calling themselves consumers or clients they have empowered themselves to become advocates for other people experiencing mental health disorders. Mental healthcare users or consumers now have a vital role to play in participating and planning the delivery of mental health services (Happell & Roper 2003). Consumer advocacy groups now exist in every state and territory of Australia and in New Zealand to promote participation of consumers in planning, implementation and evaluation of mental health services. Accordingly, many consumers live and work within a local community, use the same facilities (e.g. shops, library, cinema, sports centres) as everyone else, are accepted by the people within the community and experience no harassment and attract no hostility from the local residents (Markowitz 2007). All nurses can play a part in highlighting and reducing stigma by:
• Acknowledging the person by using respectful language; for example, never referring to someone as a manic depressive, but rather referring to them as a person with a bipolar disorder
• Discouraging the use of disrespectful language; for example, terms such as schizo, lunatic, crazy, nut case or barmy. The nurse can advocate for people with mental illness by alerting someone to the fact that they are expressing a stigmatising attitude. Many people do this automatically without realising the hurt they are causing and the negative impact on the person with the illness or their family members
• Emphasising the person’s abilities rather than their limitations
• Avoiding representing a successful person with a mental illness as superhuman.
In part it is the way people with mental disturbance were treated in the past that influences current perceptions of mental illness and the associated stigma. The next section provides a brief overview of historical perspectives relevant to understanding societal attitudes today.
HISTORICAL PERSPECTIVES AND MENTAL HEALTHCARE
In the past, when emotions, thoughts or actions were deemed to be abnormal, the terms madness and insanity were linked to those affected. Reasons for the perceived abnormalities were once attributed to a variety of factors such as the influences of magic, witchcraft, possession by the devil or evil spirits, loss of the soul or punishment by the gods. Healing methods included exorcism, magical ritual and incantation (Videbeck 2001). Later it was proposed that an imbalance of ‘body humours’ was responsible—body humours being blood, black bile, yellow bile and phlegm—and such imbalances were corrected by bloodletting. During the medieval period, beliefs returned again to those connected with magic and demonology but also included beliefs that the moon influenced madness (lunacy). Some of those perceived as mad or lunatics were flogged, tortured and starved and those whose illness resulted in violent behaviour were shackled in prisons or put out to sea as a means of ridding them from society. Fear and lack of knowledge resulted in significant cruelty.
In the late 19th and early 20th centuries, those with behaviours which were not manageable, who were misunderstood or were simply not acceptable in society were placed in custodial care inside large public mental hospitals or asylums. It can only be imagined how being confined and isolated inside large institutions might have caused feelings of abandonment and rejection. During this period doctors classified the symptoms of mental illness but had limited understanding of the sources of mental anguish (Wilson & Kneisl 1996).
Increased understanding of mental distress was promoted by the psychological, psychosocial and interpersonal theories to explain behaviour espoused by theorists such as Freud, Erikson and Stack Sullivan. The introduction of psychotropic drugs, such as chlorpromazine (Largactil) in the 1950s, helped staff members manage large numbers of clients with challenging behaviours, who were often accommodated in crowded conditions in the large institutions. In the 1990s (the time known as the decade of the brain) biological, scientific and technological concepts combined to expand on earlier understandings of mental illness. As a result, advanced brain-imaging techniques now allow direct viewing of the structure and function of the living brain while it is functioning (Wilson & Kneisl 1996).
In the latter part of the 20th century the negative impact of institutionalisation for people with mental illness was recognised. This recognition was in part the stimulus that shifted public policy to one of deinstitutionalisation and community-based care for people with mental illness. The push towards community-based mental health services also came from the human rights movement and the philosophy of normalisation for people with disabilities of all kinds. (Ch 39 explains more about the principles of normalisation and people with disabilities.) The discovery of psychotropic drugs in the 1950s also contributed to the current predominance of care in the community because these agents helped to modify challenging behaviours (Jewell & Posner 1996).
Mental healthcare today
Mainstreaming of mental healthcare has resulted in the provision of psychiatric care to consumers in general hospitals with an inpatient psychiatric unit, hostels and other residential care facilities and sometimes in forensic centres for the mentally impaired who have committed crimes. However, mental healthcare is primarily provided in the community and in Australia the community setting has become the place where most consumers receive their care.
Nurses may meet with clients in a variety of community settings, including:
Current healthcare policy promotes not admitting people to a treatment centre unless essential, and, when it is necessary for clients to be admitted to treatment centres, they are discharged back into the community as early as possible. Ideally, community-based mental health services provide appropriate networks of supports and resources for those who need it. The aim of service providers is to ensure that there are caring interventions aptly suited to assist each person to rehabilitate successfully and to cope well in society. The policy of community-based care has enabled many of those who once lived in psychiatric institutions to resettle successfully in the community and to be well supported. It is important to remember that the environment in which the consumer is seen affects the therapeutic relationship. In community settings the mental health nurse enters the home of the consumer as a guest, engaging with the consumer on a more relational and contextual basis.
Unfortunately, however, there are other instances in which the deinstitutionalisation process has not been supported with adequate community care. The result of this is that some people who experience mental ill-health have merely been relocated to substandard boarding houses or other semi-institutionalised accommodation, or face homelessness (Grigg et al 2004).
While there are still many problems for mentally ill people and health professionals to contend with and resolve, there is now more cause for optimism in relation to mental illness than in the past. Success rates for the treatment of many common mental disorders such as bipolar disorder, major depression and schizophrenia now equal or exceed the success rates for many other medical disorders (Goldberg 2007).
While this chapter does not aim to inform the nurse about the range of treatments available to assist clients with specific disorders, the next section provides a summary of possible nursing responses to some common emotional and behavioural problems that challenge clients with mental illness. The terminology used in mental healthcare, some of which is contained in the next section, is extensive and different from terms used in other areas of nursing. Some of the more common terminology is defined in Table 37.2.
Table 37.2 Terms associated with mental illness
| Addiction | Physical or emotional dependence, or both, on a substance, such as alcohol or other drugs |
| Affect | Current, observable state of emotion, feeling or mood such as sadness, anger or elation |
| Aggression | Forceful behaviour that may be physical or verbal, as well as subtle manipulation |
| Akathisia | A condition of excessive restlessness that causes a person to move about constantly, fdget or pace. This can be a side effect of certain medications used in psychiatry |
| Anhedonia | Reduced or complete inability to feel pleasure from activities previously enjoyed |
| Amnesia | Loss of memory of events for a period of time that may range from a few hours to many years |
| Anxiety | A feeling of apprehension, dread or unexplained discomfort, associated with a sense of helplessness, arising from internal conflict |
| Apathy | Lack of feeling, emotion, concern or interest |
| Asylum | A place of safety or sanctuary; a refuge from the stresses of life. Historically the term asylum was associated with institutions that provided custodial care for people with a mental illness. Unfortunately, they were often associated not with the real meaning of asylum but with mistreatment and cruelty |
| Autism | Preoccupation with the self and inner experiences; a process of introspective thinking that is often rich in fantasy |
| Behaviour | Any human activity, either physical or mental. Some behaviour can be observed while other behaviour can only be inferred |
| Behaviour modifcation | A method of changing or controlling behaviour through the application of techniques based on the principles of classical conditioning |
| Bipolar disorder | A type of mood disorder that causes alternating periods of low and high moods; a combination of depression and mania |
| Body image | The conscious and unconscious attitudes a person has towards their body (e.g. feelings about size, function and appearance) |
| Catatonia | A state characterised by muscular rigidity and immobility (stuporose type) and which, at times, is interrupted by episodes of extreme agitation (excited type) and is usually associated with schizophrenia |
| Compensation | Process by which a person makes up for a defciency in their self-image by strongly emphasising some feature of themself that they regard as an asset |
| Compulsion | An uncontrollable persistent urge to perform an act repetitively in an attempt to relieve anxiety. Compulsive behaviour often accompanies obsessions and may be directly linked to them |
| Confabulation | The fabrication of experiences or situations recounted in a plausible way to fill in and cover gaps in the memory. Used most often as a defence mechanism and most commonly by people with head injuries, dementia, amnesic disorders or alcoholism, especially those with Korsakoff’s syndrome |
| Confusion | A cluster of abnormalities constituting disturbances of judgment, orientation, memory, affect and cognition |
| Coping mechanisms | Any effort directed towards stress management. They can be unconscious (defence) mechanisms that protect the individual against anxiety, or conscious attempts to solve a problem that is creating stress |
| Deinstitutionalisation | A shift in the location of treatment from large public hospitals to community settings |
| Delusion | A fxed false belief resistant to modifcation. A delusion of grandeur is a false belief that one has great prestige, power or money, which may be manifested in the belief that the individual is a famous person. A delusion of persecution is an individual’s belief that they are in danger, being harassed, are under investigation or are at the mercy of some powerful force. A somatic delusion is a belief that one’s body is changing and responding in an unusual way |
| Dementia | A mental disorder characterised by a gradual onset of usually irreversible cognitive impairments |
| Depression | A mood state that may be mild or short lived or more severe and persistent. The latter, a mood disorder, is characterised by extreme sadness, feelings of hopelessness, low self-worth and little or no conviction that things can ever improve |
| Disorientation | Lack of awareness of the correct time, place or person |
| Electroconvulsive therapy (ECT) | A therapeutic procedure in which an electric current is briefly applied to the brain to produce a seizure. This is used in treatment of severe symptoms that do not respond to other measures, most commonly used in the treatment of severe depression |
| Hallucination | A sensory experience that is not the result of an external stimulus; may be visual, auditory, tactile, gustatory or olfactory |
| Hyperactive | Excessively or unusually active |
| Illusion | Misperceptions and misinterpretations of real external stimuli; may be visual or auditory or, less commonly, olfactory or tactile |
| Labile | Subject to frequent or unpredictable changes: the term is commonly used with reference to emotions |
| Mania | A mood characterised by an intense feeling of elation or irritability, often accompanied by increased activity, rapid speech and poor judgment |
| Mood disorder | A group of disorders in which the predominant feature is disturbance in mood |
| Nervous breakdown | A non-medical term sometimes used by the public to describe an episode of overwhelming distress or depression |
| Obsession | A persistent thought, idea or impulse that cannot be eliminated from consciousness by logical effort |
| Obsessive-compulsive disorder | An anxiety disorder characterised by intense, unwanted and distressing recurrent thoughts (obsessions) and repeated behaviours (compulsions) that are beyond the affected person’s ability to control |
| Panic attack | A period of sudden intense anxiety, often associated with feelings of impending disaster and accompanied by strong physiological symptoms, including shortness of breath, pounding heart or palpitations and dizziness |
| Paranoia | A serious personality distortion in which the person is markedly suspicious and mistrusting of others and may be convinced that they wish to harm them |
| Phobia | An intense fear of some situation, person or object, so that the danger is magnifed out of proportion and may result in a panic attack |
| Psychosis | A state in which a person’s mental capacity to recognise reality, communicate and relate to others is impaired. Delusions and hallucinations are often present |
| Psychotic | A person who is psychotic experiences delusions and hallucinations that cause disorganised thinking, unusual behaviours and a loss of touch with reality |
| Schizophrenia | A complex condition caused by brain dysfunction that results in hallucinations and delusions, distorted thinking and other disturbances |
| Suicidal ideation | Thoughts of suicide with an intention to end one’s life |
| Tardive dyskinesia | A side effect of some antipsychotic medications that manifests with a variety of involuntary muscle movements including those that affect the face, jaw and tongue, the trunk and the extremities of the body. The involuntary movements are irreversible. They are also referred to as extrapyramidal side effects |
CARE OF CLIENTS WITH SPECIFIC EMOTIONAL OR BEHAVIOURAL CHALLENGES
Here we address some of the more common mental states that clients being cared for in non-psychiatric hospital settings may experience. Information is provided on caring for a person who is anxious, depressed, aggressive, displaying self-destructive behaviour, hyperactive, confused or disoriented.
The client experiencing anxiety
Anxiety is an internal feeling usually experienced as an unpleasant or uncomfortable emotion and which is frequently associated with conflicts and frustrations. While a certain mild degree of anxiety can be beneficial when it stimulates motivation and energy, severe anxiety can be devastating and is the basis of many mental health disorders. Anxiety differs from fear in that anxiety attacks the person at a deeper level than fear, and the source of the anxiety may be unknown. Sometimes, in extreme anxiety, a person may experience panic attacks that result in markedly disturbed behaviour. The person may be unable to process what is happening in the environment and may lose touch with reality. During a panic attack behaviour may be erratic, uncoordinated and impulsive. There are three different forms of panic attack: ‘out of the blue’ attacks, which are not brought on by a trigger; situation-bound attacks which are brought on by exposure to a trigger; and situation-predisposed attacks that are comparable to situation-bound but which do not happen every time the person is exposed to a trigger.
Anxiety invades the very centre of a person’s being. Severe anxiety is profound and persistent and can erode and destroy a person’s sense of self-esteem and self-worth that contribute to a sense of being fully human (Varcarolis et al 2010).
Anxiety is experienced in a wide variety of situations and is generally the result of a threat to a person’s self-esteem or physical integrity. Threats to self-esteem include factors such as interpersonal difficulties, change in job status, social or cultural group pressures, a change in role or confusion over one’s identity. Threats to physical integrity include factors such as decreased ability to perform the activities of daily living, for example, as a result of injury or illness, or lack of basic requirements such as food, shelter and clothing. Mild and moderate levels of anxiety can alert the person to the fact that something is wrong and may be the stimulus to take appropriate action. Severe levels of anxiety interfere with problem-solving abilities, so that those affected have difficulty finding effective solutions to problems. For example, someone who experiences panic attacks may use unproductive relief behaviours to avoid the attacks from occurring, such as refraining from leaving the house to avoid the risk of a panic attack when driving the car, at work or at the supermarket. Unproductive relief behaviours perpetuate the cycle of anxiety (Varcarolis et al 2010).
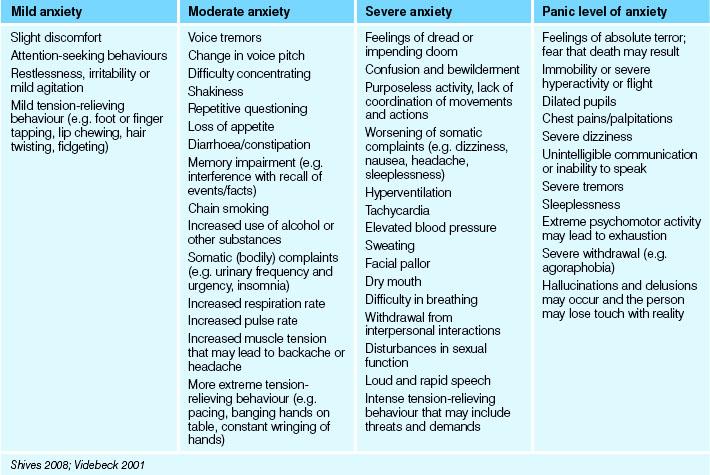
Whether the source is known or unrecognised, anxiety can produce physiological responses, behavioural changes and emotional reactions. The type and extent of response depends on the level of anxiety experienced. Table 37.3 lists some physiological and other responses to different levels of anxiety. Emotional reactions are usually apparent in the person’s descriptions of their experience. For example, they may state that they feel apprehensive, irritable, angry, depressed, helpless, on edge, unable to concentrate or remember things or they may feel detached from events and the environment. The person may experience angry outbursts or a tendency to cry frequently.
Specific treatment and care of a person experiencing anxiety depends on the level of anxiety experienced and the effects on the individual, but generally interventions are directed towards reducing intense anxiety to a more manageable level and helping the person to develop self-help strategies to prevent overwhelming anxiety. Cognitive behaviour therapy (CBT), for example, helps clients develop strategies for controlling their anxiety and reducing the incidence of panic attacks. Minor tranquillisers such as diazepam (Valium), lorazepam (Ativan) and clorazepate (Tranxene) are sometimes prescribed to suppress the client’s feelings of anxiety but, as medications do not cure the condition and there are problems with dependence, long-term use is not advocated (Healy 2002).
• Establishing and maintaining a trusting relationship
• Attempting to identify the cause (stressors) of the anxiety and encouraging the client to take effective action
• Facilitating open and honest communication about the client’s anxiety and/or problems
• Identifying existing coping mechanisms and coping resources
• Discussing with the client ways of resolving conflicts
• Providing information about, and teaching, constructive coping strategies that can help to manage stress.
The most common coping mechanisms taught and encouraged are:
• Skills for establishing and maintaining relationships
• Community living skills (Schwecke 2003).
Care during a panic attack
Care during a panic attack can take the form of:
• Remaining with the person during the attack and speaking in a calm confident voice using short and simple sentences
• Ruling out that the person is not experiencing a cardiac incident
• Telling the person to take slow deep breaths and to breathe in and out through their nose. Place their hand on their diaphragm to focus their attention on their breathing and reduce the breath rate to 10 per minute until the anxiety recedes
• Following the panic attack, telling the person what they have experienced is a panic attack; reassure the person that they can get help to manage panic attacks
• Referring the person to their general practitioner for a full physical assessment to rule out a physical cause.
In addition, strategies to help tolerate and decrease the effects of anxiety can be taught, although these address the effects rather than the cause of anxiety. These strategies include complementary therapies such as visualisation techniques, guided imagery, meditation and relaxation training.
An understanding of the types and levels of anxiety and defensive patterns of behaviour used in response to anxiety is basic to effective psychiatric nursing care. Hildegard Peplau was a nurse theorist whose conceptual model of anxiety provides a firm basis on which nurses can plan interventions for clients experiencing anxiety. Nurses would benefit from reviewing the work of Peplau (1991) and other psychiatric nursing texts to enhance their knowledge of the relationship between anxiety and mental illness and the range of treatment options available.
The client experiencing depression
Depression is an emotional state that most people experience at one time or another. It can manifest anywhere along a continuum from intermittent feelings of sadness to a persistent deep sense of unending despair accompanied by hallucinations and delusions (Shives 2008). At the onset of depression the mood begins with a feeling of sadness that may be described as ‘feeling down in the dumps’. As depression worsens, sad feelings deepen until those affected feel gloomy and dejected much of the time. At this level of depression people may describe the experience with statements such as ‘I have no joy in my life anymore’ or ‘I just feel unhappy’. For some people the depressed mood can deepen even further until there is a persistent feeling of utter desolation. Severely depressed people have a sense of hopelessness about the past and the present, and the future looks black and bleak. The heavy feelings of despondency, wretchedness and acute misery are relentless. People affected feel desperately low and worthless, and this experience is accompanied by a sense of despair so profound that they do not believe the feelings will ever lift (Elder et al 2009).
Feelings of sadness and even intense grief, such as might be felt at the death of a loved one, are normal reactions to the various losses encountered by most people during their lives. Sadness and depression in such cases may be transitory, with the person moving through a grieving process and recovering successfully after the loss. Sometimes recovery after a significant loss does not occur and the person moves into a level of persistent and severe depression that does not resolve without professional assistance. This would be termed dysfunctional grieving. In some cases sadness, moderate and severe depression can occur without the person affected being able to identify a particular trigger for the low mood. Depression caused by biochemical imbalance is an example of this (Shives 2008).
Feelings of depression are so common that depression is known as the ‘common cold’ of psychiatry. It can occur at any age, even in very small children. Children with parents diagnosed with a depressive disorder have a higher risk of experiencing depression than others, and certain events may predispose young people to develop depressive symptoms (Keltner et al 2003). These events include:
• Loss of parents through divorce
• Death of other individuals close to them (e.g. grandparents, siblings, other relatives or friends)
• Move to a new neighbourhood or town
• Academic difficulties or failure
• Physical illness or injury that entails a stay in hospital.
Depression has a wide range of signs and symptoms but even so some people are able to hide their depression from others. Clinical Interest Box 37.9 lists the common signs and symptoms of depression. For some people depression may also be accompanied by anxiety. Some people experience alternating moods of depression and elation that can be disruptive to their lives. The periods of elation may be accompanied by significant hyperactivity. Such conditions are categorised as bipolar affective (mood) disorders, whereas mood disorders that have only the one dimension of depression without periods of elation are termed unipolar (Videbeck 2001).
CLINICAL INTEREST BOX 37.9 Signs and symptoms of depression
Signs and symptoms of depression vary according to the severity of the low mood but may include:
• Non-verbal cues (sad facial expression, crying, slumped posture)
• Disturbed sleep patterns (e.g. insomnia or sleeping for much longer periods than usual)
• Self-criticism and expressions of guilt feelings
• Low self-esteem that may result in thoughts of self-harm or self-destruction
• Indecisiveness and poor concentration
• Psychomotor retardation or marked reduced mental or physical activity (slow dragging gait, slowed speech pattern and slow, flat, lifeless, colourless verbal responses, lack of concern and apathy about maintaining personal appearance)
• Psychomotor agitation (some people with depression experience significant anxiety that may manifest as restlessness, pacing or constant walking or constant purposeless movements such as pulling at hair or wringing of hands)
• Appetite disturbance and marked loss of weight
• Headaches, chest pains, gastrointestinal disturbances and other physical manifestations
• Increased consumption of substances such as nicotine, alcohol and non-prescribed drugs
• Anhedonia (inability to feel any pleasure when participating in activities that previously were pleasurable)
Particular signs that may be associated with depression in children and adolescents include:
• Frequent, vague, non-specific physical complaints such as headaches, muscle aches, stomach aches or tiredness
• Frequent absences from school or poor performance in school
• Efforts to run away from home, or talk of this
• Outbursts of shouting, complaining, unexplained irritability or crying
• Lack of interest in playing with friends
• Extreme sensitivity to rejection or failure
• Increased irritability, hostility or anger
(Keltner et al 2011; National Institute of Mental Health 2000; Varcarolis et al 2010)
Care of a depressed client is directed towards first addressing immediate safety needs in those at risk of self-harm. This will require hospitalisation and frequent or constant observation of those so seriously depressed as to be actively contemplating suicide. Antidepressant medication, when necessary, is started immediately, but the symptomatic relief is not generally achieved for at least several days, and possibly up to 4 weeks after therapy starts. Other specific interventions include individual, family, group, cognitive and behavioural psychotherapy (Keltner et al 2003; Shives 2008). The major goals are to lift the client’s mood, improve self-esteem, identify and reduce the impact of any major identified stressors, promote the development of constructive coping mechanisms, assist the client to regain interest and motivation in life and also to address any concurrent problems associated with physical health. General care involves:
• Establishing and maintaining a trusting relationship
• Helping the person, when the acute phase is resolved, to recognise and express emotions (e.g. through verbal and nonverbal communication)
• Helping the client to set realistic goals
• Encouraging the client to establish and maintain social contact and interpersonal relationships
• Encouraging visits by family or significant others, to reduce any feeling of isolation
• Promoting physical health and wellbeing (e.g. adequate exercise, sleep and nutrition)
• Providing information concerning measures that may reduce and help manage stress
• Identifying existing coping mechanisms and coping resources
• Assisting the client to develop and enhance constructive coping mechanisms, including decision-making and problem-solving skills.
Table 37.4 outlines nursing interventions and care for the client with depression.
Table 37.4 Key nursing interventions and principles of care for clients with depression
Adapted from Keltner et al 2011
People who are depressed are very vulnerable and this may be, in part, why they often withdraw and isolate themselves. This can make it very challenging for the nurse needing to establish effective communication. Clinical Interest Box 37.10 provides some strategies for promoting effective communication with clients who have depression.
CLINICAL INTEREST BOX 37.10 Strategies for promoting effective communication with clients who have depression
Acceptance
Spend time with the client and accept the person without judgment. People who have depression are not always able to express feelings and may express them through behaviour that is unusual or even bizarre. The nurse should be careful not to make or imply any criticism of the client’s behaviour because people with depression have low self-esteem and are particularly vulnerable to feelings of disapproval that may be interpreted as rejection.
Openness and honesty
Because people with depression are less able than others to tolerate disappointment, the nurse should be truthful at all times and never make promises that for any reason might not be kept. Nor should the nurse offer false reassurance.
It is important for the nurse to develop a trusting relationship with the client and this will only be achieved with honesty. For example, a client may wish to share something private with the nurse but not want the nurse to tell anyone else about what is disclosed. The nurse builds trust by telling the client that significant information will need to be shared with other members of the healthcare team. The client learns to trust the nurse as a professional whose main concern is shown to be the client’s own best interest.
Empathy
Any attempts to cheer up a depressed client may be perceived as a failure to understand their feelings or difficulties. Inappropriate approaches such as this may cause the client to withdraw further from interactions and may increase their isolation and depression.
Empathy means facilitating the client to express feelings of pain and inner distress and to respond in a way that indicates recognition and understanding of that pain and distress.
Tolerance
People with depression may be unable to make even the simplest decision (e.g. where to sit, what clothing to select and put on). The nurse needs to understand how low mood slows physical as well as mental responses and that the psychomotor retardation is part of the illness, not a deliberate act. It is impossible for clients with depression to ‘shake themselves out of it’ and it is not therapeutic to try to badger people with depression into activity. Tolerance is also required for clients with depression who experience psychomotor agitation.
Underlying anxiety in the depressed client may also manifest as hyperactivity or anger and hostility that may be directed towards the nurse. Clients sometimes shock themselves at the hostile and sometimes hateful things they say to others during periods of depression. It is a normal response for the nurse to feel some frustration and irritation or even anger towards clients at times, but the nurse must be mindful that the client’s behaviour is an outward reflection of inner anguish and that to be therapeutic they must remain patient. To assist in this the nurse must reflect on, and implement, the strategies needed to maintain personal mental wellbeing. This may include discussing feeling responses to clients with a colleague.
Depression is a major problem in older adults and may also be accompanied by worry and anxiety. Symptoms of depression in the older age group are relatively common but often go undetected. This may be because sadness is considered a normal response to the losses associated with ageing, such as physical decline, loss of social role and loss of a spouse, and it may not be recognised when normal sadness and grief has developed into clinical depression requiring treatment. In addition, the complexities of physical illness, the side effects of medication and the symptoms of dementia may combine with symptoms of depression; making diagnosis of what is happening complex and difficult (Keltner et al 2011). It is very important for nurses working with older clients, particularly those with dementia, to be alert for, and report, changes such as unusual expressions of sadness, voicing the wish to die, decrease in appetite, reduced enjoyment, loss of interest in activities or other symptoms that may indicate the presence of depression. Clinical Interest Box 37.11 lists some issues relating to the mental health of older adults.
CLINICAL INTEREST BOX 37.11 Mental health issues in older adults
• The older person is vulnerable to emotional and mental stress from many losses, including the loss of a spouse, loss of social roles and resources, decreased income and loss of status and socialisation associated with paid employment
• Physical health problems such as chronic illness, disability, visual problems, falls and incontinence
• Disorders common in the older population include depression, paranoid reactions and dementias
• Depression is the most common emotional disorder in the older population
• Paranoia may be related to depression and/or neurological disorders. It is also associated with sensory deficits and loneliness
• Of the dementias, the Alzheimer’s type is the most common non-reversible dementia
• The risk of suicide increases with age, with men aged 75 and over being particularly vulnerable
• Family carers of people with dementia are more likely than other family carers to experience emotional health problems such as stress, exhaustion and depression
The client experiencing feelings of anger and hostility
Anger is a feeling experienced by most people at certain times. It generally occurs in response to fear, confusion or frustration. Anger often occurs in response to the anxiety a person feels when a threat is perceived. Most people have little difficulty in handling mild anger, which is experienced as annoyance and usually subsides quickly. Feelings of anger, disappointment and frustration may be expressed verbally or non-verbally, for example, by cursing or kicking a car when it won’t start. When a person is very frustrated, such as when they are unable to attain an important goal, anger may become more intense. A person experiencing intense anger may try to disperse the unpleasant feeling through an angry outburst or an act of aggression. Occasionally a person may be so consumed by feelings of anger that they become violent and pose a threat to themselves and to others nearby.
Nurses may encounter anger in the course of providing nursing care; for example, a person whose health is disrupted becomes frustrated, and frustration can lead to anger. Sometimes people express their anger through verbal or physical abuse towards others, including staff members. Therefore it is important that nurses are aware of the reasons why a person may be angry, of their own responses to outbursts of angry feelings, and of how to help an individual to express anger in an appropriate manner. Anger may be the result of various stressors. Some of the factors that may cause anger or aggression in people who are in hospital for any reason include:
• A feeling of loss of control and/or independence
• A sense of isolation from family and familiar environment
• A feeling of loss of identity or individuality
• Feelings of fear and discomfort because of inadequate privacy
• Anxiety about the possible outcomes of illness (e.g. altered body image).
Some of the specific risk factors leading to a potential for aggression in clients with mental illness have been identified (Watkins 2002) as:
• A diagnosis of an illness with paranoid features (paranoia can lead to fears that induce aggressive acts aimed at defending against a perceived threat; for example, the belief that someone is plotting against you or trying to harm or kill you can lead to lashing out at that person defensively)
• Deterioration in family and/or social relationships
• A previous history of aggression or violence and declared threats of violence
• Developmental history of exposure to aggression and violence
• Non-adherence to a medication regimen
• Failure to learn to delay gratification of wants (e.g. extreme frustration when need is not met immediately)
• Failure to learn alternative strategies other than aggressive responses
Aggressive outbursts may occur when a person is unable to find a solution to a problem that is causing fear, confusion or frustration. Aggressive action may be directed towards the person or object perceived as the source of the frustration, or at other persons or objects in the vicinity. Displacement is a defence mechanism whereby an individual discharges pent-up feelings, such as anger, on a person or object other than the one that aroused the feelings (Varcarolis et al 2010). Approaches for dealing with anger and hostile behaviour in the mental healthcare environment are outlined in Table 37.5. Nurses may apply the principles of these approaches, when necessary and appropriate, in any healthcare setting.
Table 37.5 Approaches for dealing with anger and hostile behaviour in the mental healthcare environment
| Action | Rationale |
|---|---|
| Accept the client but make it clear that certain behaviours are not acceptable | This is a non-judgmental approach that informs the client that they are accepted as a person but that certain aspects of their behaviour are not appropriate |
| Acknowledge the person’s anger and their right to their feelings | This demonstrates respect and acceptance of the client |
| Allow expression of the anger in appropriate safe ways; for example, voicing angry feelings verbally, discharging anger in non-destructive acts (e.g. not damaging property or person) | Anger is self-limiting and it may be better to let it run its course than to forcibly try to stop an angry person. Attempting to stop the person’s expression of anger can restimulate the aggressive feelings and lead to a continuance of displayed anger |
| Try to remain calm (self-talk and relaxation techniques such as deep breathing and muscle relaxation can help with this). Provide psychological containment by staying in the same calm ‘gear’ and avoiding any tendency to retaliate or placate | Retaliation or trying to placate an angry person can stimulate the client to higher levels of aggression. Clients need their feelings to be acknowledged and understood; retaliation and appeasing do not achieve this |
| Be aware of your body language—try not to communicate threatening non-verbal signals (e.g. keep your hands in a low position) | Raised hands may be interpreted as a threatening gesture, particularly by clients who are experiencing paranoia, confusion or disorientation and such a gesturing may be interpreted as indicating a failure to understand the client’s feelings and point of view |
| Do not try to defend the person or situation the client is feeling angry about | |
| Set limits and be frm and consistent in treatment approaches. Encourage the client to take control by raising awareness of options at times of angry feelings (e.g. time-out, walking/talking with nurse, medication). The client should also be aware of the outcomes if self-restraint is not demonstrated | A client at risk of aggressive outburst is helped to remain in control if limits on what is acceptable are clear and alternative options for dealing with feelings are provided; for example, exercise, informing and seeking help from a nurse or other therapist when feelings are surfacing |
| Later, when the client is calm, assist to explore the immediate cause of the anger and anything that precipitated the aggressive response | Recognition of triggers can assist with problem solving |
| Help the client engage in problem solving and exploring alternative ways of handling their feelings | Engaging the client in solving their own problems is empowering because it informs the client that they can take responsibility for their actions |
| Be supportive and provide positive feedback when the client controls hostile or aggressive behaviour | Positive reinforcement is a way of helping people to modify unwanted behaviour |
| Accept that some anger may be displaced or projected on to you | The defence mechanisms of displacement and projection serve to reduce the anxiety and the threat to self caused by the intense emotions. Understanding this helps the nurse to avoid taking the hostility personally |
| Don’t take unnecessary risks. If a person’s anger is not subsiding but is in danger of escalating into destructive or violent acts, take whatever action is necessary to protect yourself and others (e.g. remove yourself and others from the area, seek assistance from others) | Nurses have rights in relation to workplace safety. Apart from the risk of personal harm to the nurse or others, the client who causes harm can later feel devastated by what has happened. Such an occurrence can be extremely destructive to the person’s self-esteem and to the therapeutic process |
| Debrief with colleagues after the incident and seek any additional support that you feel you require | Dealing with aggression is challenging and can be frightening. Debriefng is a way of relieving the associated stress and can serve to identify ways for nurses to reduce risks and improve responses in the future |
Preventing aggression and violence is important for the wellbeing of clients and others. Assertive behaviour is one constructive way of dealing with anger. To be assertive is to stand up for oneself while taking into account other people’s interests and feelings. It takes time to develop the ability to be assertive when people are in the habit of being subservient or responding to situations they are unhappy with by being aggressive. It is within the role of mental health nurses to conduct training for clients who will be helped by developing assertiveness skills.
The client who is at risk of self-destructive behaviour
Self-destructive behaviour is that which results in physical harm and, sometimes, in the person’s own death by suicide. Self-destructive behaviour includes self-mutilation and any form of suicidal activity.
Self-mutilation
Deliberate self-mutilation results from overwhelming mental distress and is the deliberate destruction of body tissue usually without conscious intent of suicide (Antai-Otong 2003). Self-mutilation may occur once or it may become repetitive. It may or may not be impulsive. It is a behaviour associated with a range of mental health disorders (Elder et al 2009) including:
• Childhood and physical and sexual abuse
• Borderline personality disorder
• Cognitive impairment disorders
Self-mutilation may involve skin cutting, severe skin scratching or burning, head banging, self-biting, eyeball pressing, tearing out hair, self-punching or inserting dangerous objects into body orifices such as the vagina or rectum. It may involve skin carving (words, designs, symbols), bone breaking or interfering with healing by picking at wounds. Very rarely, extremely serious acts of self-mutilation occur, such as eye enucleation or amputating fingers, toes or genital organs. Other behaviours that may be considered self-destructive include involvement in unsafe sex, irresponsible gambling or spending, substance misuse, driving recklessly and binge eating (Elder et al 2009; Varcarolis et al 2010). The reason for self-mutilation is not totally clear but various explanations are possible. It may be:
• A maladaptive coping mechanism that raises low self-esteem by denying helplessness or powerlessness
• A self-punishing act that helps relieve unconscious feelings of guilt
• Risk-taking behaviour that, when overcome, raises self-esteem
• A way to reconnect to feeling real and alive, as opposed to feeling empty or feeling nothing
• A way of releasing tension or anger
• Using physical pain to create distraction from emotional pain
Nursing skills for helping clients manage self-harming behaviour include:
• Adopting an empathetic and nonjudgmental attitude
• Demonstrating support and using active listening
• Encouraging the client to share their thoughts and feelings about self-harm
• Helping the client to identify personal triggers and stressors
• Exploring with the client adaptive ways to cope with uncomfortable feelings
• Gaining the client’s agreement that they will contact a staff member if they experience negative or overwhelming thoughts concerning self-harm
• Demonstrating a sense of calm and safety for the client
• Staying with the client and providing support if they are distressed
• Telling the client that you will spend time with them when they need emotional support
• Encouraging the client to engage in their usual activities and self-care where possible
• Maintaining a safe environment—removing harmful substances or objects from the client and the area
• Selecting a room that is close to the nurses’ station in order to keep the client safe
• Following the policies and procedures of the setting regarding observation and medication (Elder et al 2009; Kneisl et al 2004).
Suicidal behaviour
Self-destructive behaviour may result from any stress a person perceives as overwhelming, and is commonly associated with low self-esteem. When the sense of self-worth is extremely low, self-destructive behaviour reaches its peak and it is at this point that the risk of suicidal behaviour is likely. Suicidal behaviour implies a loss of the ability to see oneself as being of any value or worth at all (Stuart & Laraia 2005). Some of the risk factors for suicide are identified in Table 37.6.
Table 37.6 Suicide risk factors
| Variable | Risk categories |
|---|---|
| Age | Risk generally increases with age but also at particular risk are young men and young Asian females |
| Marital status | Higher risk in single, widowed, separated and divorced people. The death of a loved one is a particular risk factor in the older population |
| Gender | More common in men than in women (more women attempt suicide, more males succeed) |
| Physical health | |
| Psychological health | |
| Social health | |
| History | |
| Previous suicidal attempts |
Adapted from Ryrie 2000 & Muir-Cochrane, Barkway and Nizette 2010
Risk assessment is a crucial intervention in estimating a person’s intent to self-mutilate or end their own life, and a formal risk assessment should be conducted whenever there is any indication of the possibility of either, whether the client is in a general acute-care hospital, a mental healthcare facility, residential care or living in the community. It should be noted that the successful use of an assessment tool involves the ability to establish effective open and honest communication with the client, and expertise in the art of therapeutic communication is perhaps the most important component of the mental health nurse’s contribution to care (see Ch 6).
The first priority in dealing with a person who is at risk of, or exhibits, self-destructive behaviour is to protect the person from harm. All dangerous or potentially dangerous objects that could be used in an act of self-harm must be removed from the individual’s environment. This includes knives and other sharp implements, matches, glass, items of clothing such as belts, scarves or stockings or anything else that may be used by the client to inflict self-harm. Other approaches for dealing with self-harm and suicidal behaviour are outlined in Table 37.7. While it takes time and experience to become an accomplished mental health nurse, and the care and management of at-risk clients requires particular expertise, the principles of care, when necessary and appropriate, may be applied by others in any healthcare setting to protect clients.
Table 37.7 Approaches for dealing with self-harm and suicidal behaviour in the mental healthcare environment
| Action | Rationale |
|---|---|
| Engage in an open exploration of suicidal ideas, including the frequency and intrusiveness of the thoughts, the planning and motivation | Open exploration is an essential component of identifying the level of risk of self-harm. Any statement that alludes to self-harm; for example, a threat or innuendo made by the client that they are thinking about harming themself should be taken seriously |
| Assess the risk factors | A formal risk assessment should be conducted whenever any risk of self-harm is detected. Risk-minimisation strategies appropriate to the level of risk identified should be put in place; for example, close observation, contractual agreement for the client to report to the nurse when thoughts of self-harm are likely to be acted on. Mental healthcare agencies usually have specific guidelines and policies for management of clients at risk of self-harm |
| Be with clients in a calm, accepting and empathic manner | Facilitates open and honest communication and the development of a therapeutic relationship |
| Engage in therapeutic conversation that facilitates the safe expression of distress and the identification of the underlying issues and concerns | Helps the client to identify the factors (stressors) responsible for wanting to commit acts of self-destruction and will inform as to the measures that are appropriate to facilitate the healing of mental anguish |
| Recognise the opportunity for learning, personal growth and positive change as a potential outcome of the client’s present experience | Recognising that positive outcomes are possible stimulates a sense of hope in the nurse, which can be relayed to the client. Hope and realistic optimism facilitate recovery |
| Work collaboratively with at-risk clients, their significant others and other health professionals in assessing needs and planning care | Appropriate interventions may involve different areas of professional expertise; for example, recreational therapist, psychiatrist, dietitian, psychologist. The client’s significant others need to be aware of the strategies required to maintain the client’s safety, and their involvement can be supportive for the client |
| An appropriately qualified person should negotiate a risk-minimisation plan with the client and significant others | Risk-minimisation plans usually involve a contractual agreement, and this needs to be frm and clear. Nurses are advised to work with experienced staff in relation to these before attempting to implement them |
| Be clear about the client’s responsibility for their own safety within the context of the plan | Clients need to understand that, within the contractual arrangement, control of the situation is theirs. This is empowering, but clients also need to feel supported in managing their feelings |
| The care plan must be clear to all staff working in the client’s environment | It is a team responsibility to support and protect the client and facilitate the success of the contractual arrangement |
| Be clear about the availability of support when a person feels unsafe, and ensure the person understands the boundaries that apply | The client needs to be clear about who is available and when they can provide support, and the type of support that is possible. This ensures that the risk of inappropriate dependency on staff is reduced and the client’s sense of responsibility in the situation is reinforced |
| Mobilise social support | Social support is important in maximising the client’s coping abilities. It can also assist the client to increase self-esteem (e.g. by promoting relationships with others). For clients who are at risk but living in the community, arrangements may be made for another person to ‘keep the means’ (e.g. the client’s medication), and for people to visit the client during times of the day when they are likely to be on their own |
| Engage in problem solving with the client | Helps maximise the client’s constructive coping strategies and develop others |
| The nurse must be aware of personal and team responsibilities and accountability in relation to caring for at-risk clients | Client safety depends on staff fulfilling responsibilities. Responsibilities include knowing which clients are demonstrating an increasing risk of self-harm (e.g. increasing alienation), and which are showing signs of improvement (e.g. smiling, interacting with others). The nurse should be aware that signs of improvement can be misleading |
Kelly 2000; Stuart & Laraia 2005; Watkins 2001
Self-mutilation and suicide are complex issues, and a simple and brief overview has been provided here. As people with depression and self-harming tendencies may be encountered in every area of nursing, it is recommended that nurses explore the issues further by accessing psychiatric or mental health nursing textbooks and state government policies. See, for example, Working with the Suicidal Person (Department of Health (Victoria) 2010).
The client who experiences hyperactivity
Hyperactivity can be a manifestation of a variety of mental health disorders, caused by the misuse of certain substances such as cocaine and amphetamines (Chitty 2004), but is particularly associated with bipolar disorders. Bipolar disorders are a group of mood disorders that manifest with periods of depression and mania. The hyperactivity associated with mania is quite different to the normal exuberant activity engaged in by most people at various times. Hypomania is a clinical syndrome similar to, but not as severe as, mania which is sometimes termed hypermania (Stuart & Laraia 2005). Previously people who experienced the mood cycles associated with bipolar disorders were said to have a manic–depressive illness.
Mania is characterised by excitability, optimism, marked hyperactivity, talkativeness and a decreased need for sleep. The symptoms vary in intensity. In the milder form, people can appear to have excess energy, they may present as the ‘life and soul of the party’, be able to work long hours and be very productive in work and leisure activities. If the symptoms increase to the most severe level, people may experience serious impairment in judgment that allows them to behave in ways not usually in keeping with their personalities. For example, a normally shy and quiet woman may become loud, dress in bright and gaudy clothing and become overtly sexually provocative; a normally sensible and frugal young man may run up huge and unmanageable debts on his credit card, drive his car at outrageously dangerous speeds and yell obscenities out of the car window as he narrowly misses other vehicles and pedestrians. Such dangerous and life-threatening behaviours may be of no concern to the affected person if they have psychotic symptoms, because delusional thoughts may make them believe that they are indestructible; for example, the young man above may believe that he is immortal because he is a new god come to save the world. Common symptoms associated with mania are summarised in Table 37.8. People who are experiencing the severe form of mania may need to be admitted to an inpatient unit for their own protection and for the protection of others.
Table 37.8 Common symptoms associated with mania
Stuart & Laraia 2001; Videbeck 2001
Treatment includes firm limit-setting, seclusion (only when essential), cognitive therapy, counselling and chemical restraint (medication). Lithium is one drug that is effective in treating the symptoms of acute mania and in reducing or preventing recurrence of the mood swings associated with bipolar disorders. However, lithium and other drugs often cause unwanted side effects and levels in the blood require strict monitoring to prevent lithium toxicity. In addition, some of the feelings of elation and mania are enjoyed, so clients are understandably not always willing to take the medications that stop the feelings so drastically and they may seek alternative ways of controlling the illness. Nursing interventions vary according to the level of hyperactivity and include:
• Maintaining client safety and the safety of others
• Maintaining the client’s biological normality (e.g. meeting rest, nutrition, fluid and elimination needs)
• Facilitating activities of daily living (e.g. meeting hygiene needs)
• Helping the client to regain and maintain self-control
• Preserving the client’s dignity when behaviour is out of character and when it will be a source of embarrassment or humiliation when functioning more normally
• Reducing the amount of stimulation to which the client is subjected
• Providing a structured daily program that allows opportunities to expend energy in set activities (e.g. physical activity such as using an exercise bike or walking may help to drain excess energy).
The overall goals of care are to help the client establish constructive coping mechanisms and increase the client’s satisfaction gained from interaction with the world (Stuart & Laraia 2005). To do this the mental health nurse must establish and maintain a trusting relationship with the client. Attempting to do this can be challenging and frustrating for the nurse, partly because particular unusual speech patterns are common in people experiencing episodes of mania that impact on the ability to communicate effectively, particularly when clients are in the acute phase of mania. The speech patterns associated with mania are listed in Clinical Interest Box 37.12.
CLINICAL INTEREST BOX 37.12 Examples of speech patterns associated with mania
(Shives 2005; Stuart & Laraia 2001; Videbeck 2001)
| Pressured speech | Rapid and accelerated speech that continues without pauses between words or sentences. The flow of rapid talking continues without regard to others who may be attempting to answer, intervene or add something |
| Clang associations | The stringing together of words that rhyme without regard to their meaning |
| Circumstantiality | Use of long irrelevant descriptions when trying to describe a person, situation or event. The account may include vast amounts of irrelevant and unrelated information and may include lots of repetition |
| Loose associations | Lack of a logical relationship between thoughts and ideas that renders spoken communication vague, unfocused (waffy) and diffuse (long-winded) |
| Flight of ideas | A nearly continuous flow of accelerated speech characterised by abrupt verbal skipping from topic to topic, usually based on chance associations between words |
| Tangentiality | Constantly diverging in mid-conversation to different and unrelated topics. When describing a situation, frequently losing the train of thought, and not completing descriptions of anything |
Some of the factors that present challenges to nurses in developing therapeutic relationships are that the client may:
• Find it difficult to be still, and need to be in perpetual motion
• Find it difficult to listen to others and constantly interrupt
• Appear unaware of verbal and non-verbal cues indicating that others wish to speak
• Continue with a constant stream of speech that is sometimes unintelligible
• Have confused thinking, with thoughts racing one after the other (this makes it difficult for the client to make connections between concepts and so when speaking they may jump rapidly from one subject to another)
• Have diminished awareness of personal space boundaries and tend to invade the ‘intimate zone’ of others (see Ch 6 for information about personal zones)
• Have little understanding of how overpowering, excessive and confrontational their interactions can feel to others
• Test the rules and limits set for the therapeutic environment
• Be insistent on having their own way and may attempt to manipulate people, including the nurse, in order to achieve this
• Frequently insult staff or others, use foul or sexually explicit language, taunt and annoy others
• Be seductive towards the nurse (among others) (Elder et al 2009; Fortinash & Holoday Worret 2007; Varcarolis et al 2010).
Management includes setting clear limits on behaviour while being supportive but firm. Setting limits involves reinforcing that it is the behaviour and not the person that is rejected. For example, it is preferable to say, ‘That sort of language is not accepted in this unit’, rather than, ‘You are so crude speaking like that’.
The nurse at all times needs to remain calm, speak clearly and explain what is required simply and firmly but in a caring manner. All staff must be aware of the limits and rules set for the client’s behaviour, which must be constantly reinforced to assist the client to regain control of their behaviour. It must be remembered that behaviours that appear manipulative, fault finding or exploitative of others’ vulnerabilities are the outward expression of inner turmoil, distress and often serious emotional need. Such behaviour is the client’s way of trying to gain a sense of control at a time when they have no control of most aspects of their life; not even their own thoughts or feelings (Varcarolis et al 2010). Table 37.9 provides some approaches for dealing with hyperactivity associated with the manic phases of bipolar disorders, but the principles apply to clients experiencing excessive or uncontrolled hyperactivity from any cause.
Table 37.9 Approaches for dealing with hyperactivity associated with bipolar disorders (manic phase)
| Action | Rationale |
|---|---|
| Use a frm and calm approach | This helps promote a therapeutic relationship and is reassuring for the client and provides structure and control for a client who is out of control |
| Use short concise explanations or statements | A short concentration span and confused thinking make it difficult for the client to absorb complex information |
| Remain neutral, avoid power struggles and value judgments | Avoids provoking hostility or combativeness. Client can use inconsistencies and value judgments as justifcation for arguing and escalating mania |
| Maintain a consistent approach; for example, provide a consistent and structured environment and keep expectations the same | This provides the framework that assists the client to regain a feeling of control. Clear and consistent limits and expectations minimise the potential for clients to manipulate staff or annoy others |
| Firmly redirect energy into appropriate and constructive channels, provide an outlet for physical energy in a non-stimulating environment; for example, use of a punching bag in a quiet area | Helps in establishing constructive mechanisms for coping with excess energy. Can help release pent-up hostility and relieve muscle tension |
| Decrease environmental stimuli whenever possible; for example, avoid loud music, noises, bright lights and people | Limits distractions that can provoke agitation and escalate mania |
| Provide structured solitary activities—tasks that take minimal concentration are best. Avoid groups and stimulating activities | Solitary activities are best until distractibility is settled and the client is able to comfortably tolerate being part of a group |
| Spend one-on-one time with the client, especially when psychotic or anxious | Provides reassurance and gives the message that the client is a worthwhile person. As mania and hyperactivity settle, provides time for exploration of issues |
| It is important that the client’s physical wellbeing is maintained during the time they are not concerned with it themselves | |
| Provide the client and the family with explanations and written information about the illness and the treatment plan (it is particularly important that the client and family understand the information concerning medication) | Information is important to promote compliance with treatment regimens and minimise the risk of recurrence of symptoms |
| Ensure client and family or significant others understand how to access the supportive services in the community | Knowing about community supports includes information about accessing help in a crisis, which can be reassuring. Information about support groups and activities aimed at prevention are helpful in promoting coping mechanisms and recovery |
Adapted from Varcarolis et al 2010
Bipolar disorders and any disorder in which hyperactivity is a serious problem can be potentially devastating for clients and their families. It is an important part of the mental health nurse’s role to ensure that everyone affected understands about the illness causing the behaviour, is aware of what can and cannot be done to control the illness and what services and supports are available to help them to cope.
Clients experiencing confusion or disorientation
A person may become confused or disoriented for a variety of reasons, including as a result of delirium, dementia or from the toxic effects of alcohol and some prescribed and non-prescribed drugs. The effect in each case is a significant marked change in cognitive abilities from the client’s previous level of functioning. Cognitive functioning includes the mental processes of memory, reasoning, judgment, orientation, problem solving, decision making, the acquisition of knowledge and the ability to use and comprehend language. Some causes of cognitive dysfunction are reversible, others are not. Delirium, for example, is a syndrome that involves a disturbance to a person’s state of consciousness, which is accompanied by changes in cognition, almost always due to an identifiable cause that can in most cases be rectified. Dementia, on the other hand, is a progressive, irreversible and disabling condition in which changes in cognitive function are caused by gradually increasing, permanent damage to the brain. The focus here is on caring for those with progressive dementia.
Dementia is one of the most common causes of confusion and disorientation, with over 280 000 people in Australia currently identified as having the illness. It is a disorder normally associated with older clients but, although the risk of dementia does increase with age, more than 16 000 of those identified as having dementia are under age 65 (Alzheimer’s Australia 2011). Alzheimer’s dementia (AD) is the most common form of the illness, but all types of dementia share similar symptoms and require similar interventions. The symptoms depend on the sequence in which areas of the brain are damaged by the disease process, so the progression of symptoms varies in different people. Symptoms change and increase in severity over the duration of the illness, which in the case of AD can be 3–20 years, the average span being 7 to 10 years (Alzheimer’s Australia nd). Symptoms include:
• Increasing loss of language and communication skills
• Progressive decline in ability to perform routine tasks despite having intact physical functioning (in the early stages of dementia this may mean difficulty with coordination when preparing a meal or when shopping and handling money, or when driving a car. Later this extends to include difficulty with tasks such as dressing, eating and bathing)
• Impaired judgment, abstract thinking
• Difficulty in concentrating and learning new information or skills
• Changes in behaviour (e.g. wandering, incessant walking, constant repetition of words, confabulation)
• Changes in personality and mood (up to two-thirds of people with AD have symptoms of depression, and about 20% exhibit aggression)
• Hallucinations and delusions (hallucinations are experienced by about 16% of people with AD, delusions by about 30% and they are often paranoid in nature)
• Loss of bladder and bowel continence (usually later stage) (Access Economics 2003).
Caring for the client with dementia
Care interventions for clients with dementia are dependent on the client’s abilities, and the focus of care should be on what the client can still do rather on abilities lost. General care interventions are listed in Table 37.10 and in Clinical Interest Box 37.13.
Table 37.10 Information for nurses and for clients with dementia and their family carers
Adapted from Fortinash & Holoday Worret 2007
CLINICAL INTEREST BOX 37.13 Interventions appropriate for clients experiencing confusion or disorientation
Appropriate care for the confused or disorientated client includes:
• A safe, consistent, pleasant and familiar environment
• Freedom from physical/emotional/spiritual pain
• A calm, relaxed, caring and non-challenging atmosphere
• Staff who have appropriate expertise and are compassionate
• Skilled communicators (expertise in communicating with cognitively impaired clients)
• Frequent contact and interaction with staff/family
• Contact with pets if desired (especially the client’s own pets)
• A structured individualised routine (as close to the client’s familiar routine at home as is possible)
• The presence of the client’s own familiar belongings (e.g. personal objects)
• Therapeutic activities/programs to promote cognitive stimulation (e.g. reminiscence therapy, music therapy)
• Nutritious diet/adequate hydration, including pleasurable snacks
• Adequate periods of rest and sleep
• High standard of hygiene/personal grooming
• Effective use of well-maintained visual/hearing/sensory aids
(adapted from Fortinash & Holoday Worret 2003)
Reality orientation is a form of rehabilitation used to orientate confused or cognitively impaired clients by promoting or maintaining their awareness of person, time and place. It is recognised as unrealistic to expect to orientate people in the later stages of dementia to present time reality, but some of the principles of reality orientation are appropriate and helpful (Ebersole & Hess 2001). Helpful aspects include:
• Calling the client by their preferred name every time they are approached
• Stating your name each time you start an interaction with the client
• Maintaining a normal day–night cycle; for example, opening curtains and blinds during the day and closing them at night and encouraging the client to dress in their own clothes during the day, rather than in nightwear
• Leaving the furniture and the client’s belongings in the same place, as rearranging objects in the environment adds to confusion
• Encouraging the client to wear their spectacles and/or hearing aids, as not wearing them adds to sensory confusion
• Maintaining a routine and a sense of order in daily activities
• Ensuring that the environment is designed to minimise confusion; for example, using distinctive colours or pictures on bathroom or toilet doors to help the confused person identify these areas, and ensuring adequate lighting in all areas to minimise the effect of shadows that might confuse perceptions of what is seen
• Using a notice board to display information about the date and place that is consistently maintained to give residents an opportunity to remain orientated to dates, times and important events.
Clients who have temporary confusion or who are in the early stages of dementia and are seeking to maintain orientation to time and place may benefit from the following interventions:
• Telling the person the date and time each morning and repeating the information as appropriate during the day
• Having the day and date displayed in large bold letters on a board and having the person change it accordingly each day
• Reminding the person of holidays, birthdays and other special events
• Providing cues to reinforce verbal information; for example, clocks with clear and large numbers, large calendars
• Discussing current affairs; for example, items in the newspaper or on television news.
A key to providing quality care is to find a way to connect with clients who have dementia. This is different to simply communicating, which can be one sided, with the nurse talking and the client largely passive. Connecting involves the nurse or other carer having to develop skills and spend time and effort establishing connection. The use of validation therapy, reminiscence and remotivation therapy promotes connection and these therapies are highly appropriate for use with clients who have dementia (Varcarolis et al 2010). (How to communicate effectively with clients who have dementia and the use of appropriate therapies such as validation and reminiscence therapy are outlined in Ch 6.) Recreational, occupational and complementary therapies can also be therapeutic in promoting cognitive, sensory and physical stimulation and can provide opportunities for staff to connect with clients.
Managing challenging behaviours in confused clients
Many of the behaviours that people with dementia exhibit are a direct result of the illness and so need to be considered as ‘normal’ symptoms of the illness, rather than abnormal behaviours. Behaviours that fall into this category include aimless wandering, becoming lost, muddled actions and conversations, disturbances in sleep–wake cycles and, especially with some particular types of dementia (e.g. Pick’s disease), loss of emotional control and aggressive reactions (Sherman 1999). Other behaviours, such as unusual outbursts of physical or verbal aggression, dressing or disrobing publicly or refusing to bathe, eat or attend activities previously enjoyed, can be due to a range of influences that can exacerbate the normal effects of the illness. The reason for the behaviour—the core of the problem—may be related to a variety of issues including:
• A change in the environment (e.g. too noisy, too busy, causing feelings of being overwhelmed)
• The person’s physical condition (e.g. too hot or cold, clothing uncomfortable, pain or discomfort)
• Hallucinations or delusions (may create fear and anxiety)
• Provocation by another resident
• The way a particular staff member interacts with the person (e.g. being loud or bustling or rushing the person).
Whatever the client’s behaviour, it is important for the nurse to respond quietly, calmly, confidently and kindly. This kind of response is often enough to modify the behaviour. The use of psychotropic medications for managing challenging behaviour is best avoided because these agents tend to have little effect on problem behaviour associated with dementia, particularly of the Alzheimer’s type, and they may cause serious side effects more difficult to deal with than the behaviour itself (Shives 2008). When behaviour is not acceptable the nurse should firmly let the person know that this is the case, and behaviour that is appropriate should be praised.
Care by staff who fully understand the effects of the dementia illness and have appropriate expertise in communicating with confused people is important to the client’s sense of wellbeing, and it is clearly evident that disruptive behaviour is less likely in residential care settings when the principles of dementia care management are followed (Shives 2008). The appropriate interventions for clients with challenging behaviour are outlined in Clinical Interest Box 37.14.
CLINICAL INTEREST BOX 37.14 Nursing responsibilities for managing challenging behaviour
• Maintain a calm environment and respond to the situation calmly
• Remain neutral, do not attribute blame, never ‘tell off’ in a patronising manner or punish in any way
• Avoid the use of restraints, including chemical restraints; in particular physical restraints tend to increase agitation and confusion
• Observe and keep a record of when the behaviour occurs, the type of behaviour, the client’s mood and where and with whom the behaviour occurs: this helps to identify triggers for the behaviour that in many cases suggest how the cause can be eliminated
• Is there a physical or emotional trigger for the behaviour? Is the client or resident unwell, in pain, overtired, overstimulated, bored, anxious, embarrassed or feeling ignored, misunderstood or patronised?
• Is the client or resident reacting to an unpleasant incident or is the behaviour associated with:
• Consider all the facts together. Ask:
• Use a team approach to problem solving
• It may take time and several different ideas may need to be implemented before certain problem behaviours are resolved. If one nurse finds a successful intervention, this should be documented appropriately and shared with all team members
Redirection
Redirection involves distracting the client from the situation causing the behaviour. For example, the nurse may distract the client who is upset and shouting at another resident without obvious cause by saying, ‘I don’t know what’s wrong but I think we should get away from here—let’s go for a walk outside’. The client who is jumping up from the meal table and upsetting other clients by saying ‘this food is bad, it tastes like poison’ may be directed if the nurse responds, ‘I don’t think things are right, come with me, you can leave that food, let’s go and find something else to eat’ or ‘You’d better leave that, let’s get something else to eat later on—can you come and help me water the plants outside and then we’ll eat later?’
Triggers
The following example is an illustration of how identifying a trigger can help to reduce challenging behaviour and how different strategies may need to be tried until a successful way of stopping the behaviour is found.
Mrs Lamb, 72, who has dementia and is living in a residential care facility, was generally happily confused but on some days would be very agitated, pace about, bang on tables and sometimes swear and shout out abuse such as ‘get away, you cow’ at the top of her voice. On these days she would often start crying for no apparent reason and the staff found it difficult to console her or to establish what was upsetting her. On the last two occasions of being so upset, she became physically aggressive and even succeeded in biting one of the nurses.
After keeping a detailed record of when and where the behaviour occurred it was realised that it was on certain days of the week that corresponded with when a particular nurse was on duty. This was a surprise, as the nurse was respected for her compassion and skill in dementia care nursing, but it was soon confirmed that the challenging behaviour was definitely triggered by the nurse’s presence. It was only after consulting with Mrs Lamb’s sister that the cause became clear. The nurse bore a close resemblance to a next-door neighbour who had reversed her car over and killed Mrs Lamb’s much adored Labrador dog over 40 years previously.
The problem was discussed at a team meeting. It was decided that the nurse should not be responsible for Mrs Lamb’s personal care and that she should attempt to reinforce her own identity with Mrs Lamb. When the nurse next came on duty she wore her hair differently and made a point over the next few weeks of consistently introducing herself and showing Mrs Lamb her name badge. She managed to tell Mrs Lamb about herself; she even used photographs of her family, her home and her holidays to assist the process of trying to reinforce her real identity. This seemed to be effective on most occasions, although Mrs Lamb sometimes continued to respond with agitation and aggression towards the nurse she believed had killed her pet dog.
Not knowing what else to do as Mrs Lamb one day yelled at her ‘get out, dangerous bitch’ the nurse quickly said, ‘I’m so sorry, I was so careless, I never meant to hurt your dog. I am so sorry, please forgive me.’ With this, Mrs Lamb acknowledged the apology with a firm quick nod of the head, walked to her chair and with a sigh sat down. This seemed to settle what for Mrs Lamb may have been unfinished business. The nurse continued to use this approach whenever Mrs Lamb was agitated and eventually the agitation and aggressive response to the nurse stopped.
It should be noted that, while many of these principles apply to caring for clients who are confused or disorientated from causes other than progressive dementia, the approach for reversible confusion or temporary disorientation may include strategies to assist the person with progressive dementia to remain orientated to reality.
Dementia is one of the most complex and disabling illnesses. It presents huge challenges to nurses and to the many family carers who tend loved ones with dementia at home. Table 37.10 provides a summary of some of the information that nurses need to know and some of the information that nurses need to teach to family carers.
Dementia care, while not always acknowledged as such, is a specialty area of nursing, requiring a high level of integrated skills. It is predominantly a disorder of the elderly, who often have multiple other concurrent health issues that the nurse must be knowledgeable about. Dementia clients are often not able to explain their feelings or their needs; the nurse therefore needs high-level observation and communication skills to provide quality care. The nurse also needs to be able to support the family carers of people with dementia, who are often devastated by what has happened to their loved ones.
Though this section has briefly highlighted some of the many issues relating to dementia care it is recommended that nurses undertake specialist courses to enhance their knowledge and skills in this area. Organisations such as Alzheimer’s Australia provide up-to-date information relevant to people with dementia, their families and health professionals. All caring needs to be undertaken with an understanding of the legal and ethical issues that relate to mental health nursing. The next section adds some specific points to the general legal and ethical principles impacting on mental health nursing.
LEGAL AND ETHICAL ASPECTS OF MENTAL HEALTH NURSING
The provision of healthcare for individuals suffering from mental health disorders is governed by government mental health Acts. Each Australian state and territory has its own Act, as does New Zealand, and these Acts are periodically revised. The nurse who is involved in mental health nursing has a responsibility to be aware of the relevant current Acts in the geographical area of their employment. Information about legal issues may also be accessed from government departments responsible for the health of the community such as the Department of Health (Victoria) or its equivalent in other states and territories.
Mental health Acts provide guidelines and directions regarding the provision of mental healthcare, for example, criteria for determining criteria for admission to hospital, and regulations and requirements regarding the periodic review of individuals suffering from mental illness. The information here is based on the law as it relates to mental health clients in the state of Victoria but the principles apply to laws across Australia and New Zealand.
Legal issues relating to informal and formal admission
Treatment in a mental healthcare facility or by a community mental healthcare team may take the form of informal or formal admission. Informal (voluntary) admission is when an individual chooses to receive treatment. Treatment may be at personal request or based on the advice of family or a health professional, and the client is able to withdraw from treatment or leave the healthcare facility whenever they choose.
Formal (involuntary) admission is when the request for admission comes from a source other than the mentally ill person, who is deemed incompetent to make an informed decision. An individual may be referred for admission if they pose a danger to themself or others or if they require treatment but are too confused or disorganised to seek voluntary admission. A medical officer completes a recommendation for admission form after examining the person. The admitting psychiatrist at the treatment centre then examines the person and decides whether or not to act on the recommendation by admitting the individual as a formal (involuntary) client, which means that the client may be given treatment deemed necessary whether or not they consent to the treatment.
In a crisis situation it may be a team of professionals based in the community, such as a crisis assessment and treatment team (CATT) that is called to assist. The team can request formal (involuntary) admission for a client but a medical officer must examine the client and sign the recommendation form as soon as possible. There are five criteria, all of which must be met to justify a person being admitted involuntarily. These are that:
1. The person must be mentally ill (mental illness is described in the Victorian Mental Health Act 1986 as a medical condition that is characterised by a significant disturbance of thought, mood, perception or memory)
2. The person must need immediate treatment
3. The person must present a health or safety risk to themself or others
4. The person refuses or is unable to consent voluntarily to treatment
5. There is no less restrictive way of providing needed treatment.
As soon as a client no longer meets all five criteria they must be discharged from their involuntary status, or what is termed formal detention. There are strict guidelines governing who should review formal clients and how often they should be reviewed. Two psychiatrists must independently review formal clients on, or within 24 hours of, admission. All clients should be provided with a statement of rights on admission and given details of whom they can contact for support. Clients have a right to appeal against involuntary admission. The Mental Health Review Board reviews clients who appeal, but in any case automatically reviews formal clients on a regular basis.
Treatment orders and issues of consent
Mental health clients who are admitted involuntarily to a mental health service are sometimes treated under a community treatment order (CTO) or a restricted community treatment order (RCTO) while living in the community. The CTO may require that the person lives in a particular place to facilitate treatment; the RCTO may stipulate which psychiatrist will provide treatment, where and how often treatment will be applied and how long the order will last. It may also stipulate other specific conditions under which the client may remain in the community while receiving treatment. All formal clients, whether treated in the community or in a hospital, are legally obliged to accept recommended treatment, and treatment can be enforced against the client’s will if necessary. Even though this is the case it is in everyone’s best interest for formal and informal clients alike to be given all relevant information connected with any treatment, and informed consent should be gained whenever possible. The right of formal and informal clients to seek a second opinion must be respected.
The mental health Acts in each state and territory have clear guidelines concerning issues such as informed consent to treatment, the way treatments may be implemented (e.g. electroconvulsive therapy) and the use of restraint, including the use of seclusion as a therapeutic measure. It is an offence to restrain or seclude someone if it is not conducted within the requirements of the mental health Act applicable to where the practice occurs, and the mental health service can be prosecuted and fined if an offence is committed. All consumers admitted to hospital under the Victorian Mental Health Act 1986 (section 19A(1)) must have a treatment plan, the purpose of which is to provide a clear statement about the treatment and services to be provided to the consumer and to establish mutual expectations. The authorised psychiatrist must prepare, review on a regular basis and revise as required a treatment plan for each consumer.
Legal issues and electroconvulsive therapy
Electroconvulsive therapy (ECT) is a prescribed treatment and as such it is regulated under the different mental health Acts and regulations in each state. The use of ECT is indicated when the client has an increased risk of suicide, not responded to psychotropic medication or had an adverse reaction to medication. It is also indicated when the client has had a previous history of a good response to ECT (Henderson 2011).
ECT involves the client being given a light general anaesthetic and muscle relaxant medication. A regulated electrical current is passed through the brain until a seizure occurs (a therapeutic fit). This is sometimes referred to as shock treatment. A course of ECT involves a series of treatments. Informed consent must be gained whenever possible for any form of treatment, but there are some issues specific to ECT. The client can only consent to one course of ECT at a time. One course must not exceed any more than six treatments. No more than 7 days can pass between two treatments without the client’s consent being sought again. The client’s consent must be sought for each new course of treatment. ECT can be performed without consent on involuntary clients but only if set criteria are met. The criteria are that:
• The ECT has clinical merit and is appropriate
• The benefits, discomforts and risks have been considered in the decision to perform ECT
• Other beneficial alternatives have been given due consideration
• Without ECT the client’s physical or mental status will decline significantly
• All reasonable measures have been taken to contact the client’s guardian or primary carer who can provide consent on behalf of the client (Mental Health Legal Centre Inc 2010).
Further information about ECT and the law can be located in mental health nursing texts, mental health Acts and at mental health legal centres. References and websites for accessing legal information are provided at the end of this chapter.
ETHICAL ISSUES AND DILEMMAS
Ethical issues and dilemmas abound in the area of mental health nursing. It is sometimes a challenge to balance the client’s right to autonomy, the rights of others and the legal concepts relevant to nursing care. Some of the areas that may give rise to ethical concerns include:
• Informed consent/refusal of treatment
• Seclusion and other forms of restraint
• Client confidentiality versus the need to prepare/warn/protect other parties
• Client autonomy (self-reliance and choice issues) as opposed to paternalism
Within these areas are situations that may give rise to the nurse experiencing conflicting or troublesome feelings. For example, enforcing medication or treatment that is refused, or needing to restrain a client by enforced seclusion, may give rise to feelings of guilt, concern or distaste. Or the nurse may be torn between a client’s right to confidentiality and the importance of informing a family carer about a client’s diagnosis, such as HIV (human immunodeficiency virus) infection, or of the risk of violence if the client has voiced threats when they do not want their diagnosis, feelings or voiced intentions revealed.
It can also be discomforting and confusing trying to balance establishing and maintaining a trusting and helping relationship while maintaining the appropriate professional boundary with certain clients, and this can cause ethical dilemmas, particularly for nurses new to psychiatric nursing (Elder et al 2009). Nurses must practise within professional codes of practice and the law, and consistently remain aware of the ethical principles of beneficence (do good), non-maleficence (do no harm), autonomy (client self-determination) and those of justice, fairness and equity when caring for clients. Whenever ethical concerns arise where the decisions about what to do are not clear, nurses should raise the issues and discuss them openly with colleagues. Stuart (2001b) recommends that nurses should take certain steps and consider the answers to particular questions when faced with ethical dilemmas. These suggestions are listed in Table 37.11. Nurses considering a career in mental health nursing are advised to access further information concerning ethical issues in mental healthcare.
Table 37.11 Steps and questions in ethical decision making
| Steps | Relevant questions |
|---|---|
| Gathering background information | |
| Identifying ethical components | |
| Clarification of agents | |
| Exploration of options | |
| Application of principles | |
| Resolution into action |
Stuart 2001b:208
Summary
Many enrolled nurses (ENs) may wish to follow a career in the specialty area of mental health nursing, and those who remain in other fields may be required to assist in the care of individuals experiencing mental illness; for example, when they are being cared for in general hospitals or in residential care facilities.
There is no clear dividing line between mental health and mental illness; rather, mental wellbeing is represented on a continuum and no one is entirely mentally unhealthy or fully mentally healthy at all times. The ability to remain mentally healthy depends on a wide range of interrelating factors, including those that are physiological, psychological and sociocultural. There are many theoretical models to explain the development of mental illness, on which mental health nurses base their clinical practice. These include the biological (medical) model, psychological/psychodynamic, social/interpersonal, cognitive-behavioural and stress vulnerability/adaptation models.
Mental illness can be diagnosed and formally classified according to the presenting symptoms. A diagnosis can guide treatment but also places a label on the person that can be a source of stigma, which can be one of the most difficult aspects of mental illness for clients to cope with. It is a primary role of the mental health nurse to educate the public about mental illness to reduce stigmatising attitudes, which are in part based on historical factors.
Mental health nurses, who work as members of a multidisciplinary team, develop nursing diagnoses and focus care on the feelings of clients and the behavioural manifestations of mental distress that they display. The development of a trusting, helping relationship is essential to being able to work therapeutically with mentally unwell clients and in promoting the healing process. Assisting clients to develop constructive coping mechanisms is an important component of the therapeutic relationship, as is supporting effective rehabilitation of clients living in the community, where currently most mental healthcare takes place.
This chapter has not provided detailed information about mental illness but it has provided a brief overview of some issues and suggestions appropriate to the care of clients who are anxious, depressed, aggressive, self-destructive, hyperactive or confused. The nurse interested in working in the wonderfully challenging area of mental health nursing is advised to access more information about manifestations of mental anguish, models of care and the legal and ethical issues that relate to this dynamic field of nursing.
1. Jim, aged 85, was recently admitted to the inpatient aged persons unit. He had been found wandering, confused and disorientated, by his young neighbour late one evening. His daughter was notified and took him to see his doctor. Following assessment by his doctor who thought he might have delirium he was referred to the aged persons cognitive assessment team. Admission to the inpatient unit was suggested for further assessment and observations.
2. Jane is a 19-year-old unemployed woman who was brought into the emergency department by her mother after taking an overdose of drugs from the family medicine cabinet. Her mother had found her unconscious in her bedroom. Following treatment in the emergency department she was transferred to the inpatient psychiatric unit. She has recently separated from her boyfriend and her father has left to live interstate with a new partner.
1. Explain what is meant by mental health.
3. Identify four (4) attributes that can be considered indicators of mental health.
4. Identify four (4) groups of people that are at particular risk of developing a mental illness and explain why.
5. Identify four (4) early warning signs of mental illness in children, in pre-adolescents and in adults.
6. Explain the primary characteristics of thought disorders, mood disorders and behavioural disorders and give an example of each.
7. How can nurses reduce stigma about mental illness?
8. Define the terms hallucination, delusion and confabulation.
9. Define the four following terms and indicate when they are experienced: akathisia, anhedonia, anxiety, apathy.
10. Identify five (5) ways of assisting a client experiencing a panic attack.
11. Outline four (4) strategies for promoting effective communication with clients who have depression.
12. Identify ten (10) interventions necessary to provide quality care for people with dementia in an aged-care residential facility. Consider the environment, the staff and nursing care activities.
13. What are the five (5) criteria required to be met if a client is to be admitted as an involuntary client to a mental healthcare facility?
References and Recommended Reading
Access Economics. The Dementia Epidemic: Economic Impact and Positive Solutions for Australia. Prepared for Alzheimer’s Australia by Access Economics, Canberra. Online. Available: www.alzheimers.org.au, 2003.
Alzheimer’s Australia. (nd) Alzheimer’s Disease. Available: www.fightdementia.org.au/understanding-dementia/alzheimers-disease.aspx.
Alzheimer’s Australia. Key Facts and Statistics for Media. Available: www.fightdementia.org.au/media/key-facts-and-statistics-for-media.aspx, 2011.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th edn. Washington DC: APA, 1994.
American Psychiatric Association. Diagnosis: the DSM-IV Definition of Mental Illness. Online. Available: www.psych.utah.edu/2002_fall_3250_01/Notes/9_12_Diagnosis.pdf, 2002.
American Psychiatric Association. Healthy Minds, Healthy Lives. What are the Warning Signs of Mental Illness? Online. Available: www.healthyminds.org/warningsigns.cfm, 2008.
Antai-Otong D. Psychiatric Nursing: Biological and Behavioural Concepts. Clifton Park, NY: Thomson Delmar Learning, 2003.
Antai-Otong D. Psychiatric Nursing: Biological and Behavioural Concepts, 2nd edn. Clifton Park, NY: Thomson Delmar Learning, 2007.
Anthony WA. A recovery-oriented service system: setting some system level standards. Psychiatric Rehabilitation Journal. 2000;24(2):159–168.
Ashton P, Keady J. Mental disorders of older people. In: Newell R, Gournay K. Mental Health Nursing: an Evidence-Based Approach. Edinburgh: Churchill Livingstone, 2000.
Australian Bureau of Statistics (ABS) and Australian Institute of Health and Welfare (AIHW) (2011) The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples. ABS Cat No 4704.0. AIHW Cat No IHW–42. ABS, Canberra
Australian Health Ministers Advisory Council. National Standards for Mental Health Services. Canberra: Australian Government Publishing Service, 1996.
Australian Health Ministers. National Mental Health Policy. Canberra: Australian Government Publishing Service, 1992.
Australian Health Ministers. Second National Mental Health Plan: 1998–2003. Canberra: Australian Government Publishing Service, 1998.
Australian Health Ministers. National Mental Health Plan 2003–2008. Canberra: Australian Government, 2003.
Australian Institute of Health and Welfare (AIHW). Mental Health Services in Australia 1999–2000. Canberra: AIHW, 2002.
Barkway P. Theories of mental health and illness. In: Elder R, Evans K, Nizette D. Psychiatric and Mental Health Nursing. Sydney: Elsevier, 2009.
Beck CK, Rawlins RP, Williams SR. Mental Health–Psychiatric Nursing, 2nd edn. St Louis: Mosby, 1988.
Brown R. Australian Indigenous mental health. Australian and New Zealand Journal of Mental Health Nursing. 2001;10(1):33–41.
Chitty K. Clients with mood disorders. In: Kneisl CR, Wilson HS, Trigoboff E. Contemporary Psychiatric-Mental Health Nursing. NJ: Prentice Hall, 2004.
Deegan PE. Recovery: the lived experience of rehabilitation. Psychosocial Rehabilitation Journal. 1988;11(4):11–19.
Department of Health (Victoria). Working with the Suicidal Person: Clinical guidelines for emergency departments and mental health services. Melbourne: State Government of Victoria, 2010.
Ebersole PR, Hess PA. Geriatric Nursing & Healthy Aging. Mosby: St Louis, 2001.
Edward KL, Munro I, Robins A, et al. Mental Health Nursing: Dimensions of Praxis. Melbourne: Oxford University Press, 2011.
Egan G. The Skilled Helper: a Problem Management Approach to Helping. Pacific Grove: Brooks Cole, 1994.
Elder R, Evans K, Nizette D. Psychiatric Mental Health Nursing. Sydney: Elsevier, 2009.
Erikson E, Erikson J. The Life Cycle Completed. New York: WW Norton, 1997.
Feil N. The Validation Breakthrough: Simple Techniques for Communicating with People with Alzheimer’s Type Dementia, 2nd edn. Sydney: MacLennan & Petty, 2002.
Fenichel M. Concepts in practice: on therapy—a dialogue with Aaron T Beck and Albert Ellis. Reported highlights from the American Psychological Association 108th Convention, Washington DC, August 4–8. Online. Available: www.fenichel.com/Beck-Ellis.shtml, 2000.
Fontaine KL, Mood disorders. Fontaine KL, Fletcher JS. Mental Health Nursing, 5th edn., Menlo Park: Addison Wesley, 2003.
Fontaine KL, Fletcher JS. Mental Health Nursing, 5th edn. Menlo Park: Addison Wesley, 2003.
Fortinash KM, Holoday Worret. Psychiatric Nursing Care Plans, 4th edn. St Louis: Mosby, 2003.
Fortinash KM, Holoday Worret PA. Psychiatric Nursing Care Plans, 5th edn. St Louis: Mosby, 2007.
Gibb R, Macpherson G, A common language of classification and understanding. Thompson T, Mathias P. Lyttle’s Mental Health and Disorder, 3rd edn., Edinburgh: Baillière Tindall, 2000. (2000)
Goldberg RJ. Practical Guide to the Care of the Psychiatric Patient, 3rd edn. St Louis: Mosby, 2007.
Griffiths R, Emrys E, Finney Lamb C. Operation safe haven: the needs of nurses caring for refugees. International Journal of Nursing Practice. 2003;9(3):183–191.
Grigg M, Judd F, Ryan L, et al. Rural and remote psychiatry: identifying marginal housing for people with a mental illness living in rural and regional areas. Australasian Psychiatry. 2004;12(1):36–42.
Happell B, Roper C. The role of a mental health consumer in the education of postgraduate psychiatric nursing students: the students’ evaluation. Journal of Psychiatric Mental Health Nursing. 2003;10(3):343–350.
Healy D. Psychiatric Drugs Explained, 3rd edn. Edinburgh: Churchill Livingstone, 2002.
Henderson S. Mood and Anxiety Disorders. In: Edward KL, Munro I, Robins A, et al. Mental Health Nursing: Dimensions of Praxis. Melbourne: Oxford University Press, 2011.
Horsfall J, Cleary M, Jordan R. Towards Ethical Mental Health Nursing Practice. South Australia: Australian and New Zealand College of Mental Health Nurses Inc, Greenacres, 1999.
Jewell K, Posner N. A consumer focus. In: Clinton M, Nelson S. Mental Health and Nursing Practice. Sydney: Prentice Hall, 1996.
Johnstone MJ. Stigma, social justice and the rights of the mentally ill: challenging the status quo. Australian and New Zealand Journal of Mental Health Nursing. 2001;10(4):200–210.
Kelly S. Suicide and self-harm. In: Newell R, Gournay K. Mental Health Nursing: an Evidence-Based Approach. Edinburgh: Churchill Livingstone, 2000. (2000)
Keltner N, Bostrom C, McGuinness T. Psychiatric Nursing. St Louis: Mosby, 2011.
Keltner NL, Schwecke LH, Bostrom CE, et al. Psychiatric Nursing, 4th edn., St Louis: Mosby, 2003.
Kennedy W, Mitzeliotis C. Schizophrenia and other psychotic disorders. In: O’Brien P, Kennedy W, Ballard K. Psychiatric Nursing: an Integration of Theory and Practice. New York: McGraw-Hill, 1999.
Kneisl CR, Wilson HS, Trigoboff E. Contemporary Psychiatric Mental Health Nursing. New Jersey: Prentice Hall, Upper Saddle River, 2004.
Lovejoy M. Recovery from schizophrenia: a personal odyssey. Hospital & Community Psychiatry. 1984;35(8):809–812.
Markowitz FE. Sociological models of recovery. In: Ralph RO, Corrigan PW. Recovery in Mental Illness: Broadening our Understanding of Wellness. Washington DC: American Psychological Association, 2007.
Mayo Foundation for Medical Education and Research. Mental Illness: an Overview with a Mayo Clinic Psychiatrist. Online. Available: www.mayoclinic.com/invoke.cfm?id=HQ01079, 2002.
Mental Health Foundation. Knowing Our Own Minds. A Survey of How People in Emotional Distress Take Control of their Lives. London: Mental Health Foundation, 1997.
Mental Health Legal Centre Inc. Patients’ Rights: a Self-help Guide to the Mental Health Act, 8th edn. Melbourne: MHL Centre, 2010. Online. Available: www.communitylaw.org.au/mhlc/cb_pages/patient_rights_booklet.php
Moller M, Fontaine KL. Common clinical problems. In: Fontaine KL & Fletcher JS (1999) Mental Health Nursing, 4th edn. Menlo Park: Addison Wesley, 1999.
Muir-Cochrane E, Barkway P, Nizette D. Mosby’s Pocketbook of Mental Health. Australia: Mosby, 2010.
National Institute of Mental Health (2000) Depression in Children and Adolescents: a Fact Sheet for Physicians. NIH Publication No 00-4544, September
National Mental Health Association (USA). Mental Illness in the Family: Recognizing the Warning Signs and How to Cope. NMHA MHIC Fact sheet. Online. Available: http://www.nmha.org/go/information/get-info/mi-and-the-family/recognizing-warning-signs-and-how-to-cope, 2012.
Peplau HE. Interpersonal Relations in Nursing: a Conceptual Framework of Reference for Psychodynamic Nursing. New York: Springer Publishing Co, 1991.
Peplau HE, A working definition of anxiety. Varcarolis EM, Carson VB, Shoemaker NC. Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 5th edn., Philadelphia: WB Saunders, 2006. (2006)
Riley E, Kneisl CR, Suicide and self-destructive behaviour. Wilson HS, Kneisl CR. Psychiatric Nursing, 5th edn., Menlo Park: Addison Wesley, 1996.
Rogers C. On Becoming a Person. Boston: Houghton Mifflin, 1961.
Ryrie I. Assessing risk. In: Gamble C, Brennan G. Working with Serious Mental Illness. A Manual for Clinical Practice. Edinburgh: Baillière Tindall, 2000.
Schwecke LH, Anxiety, coping and crisis. Keltner NL, Schwecke LH, Bostrom CE. Psychiatric Nursing, 4th edn., St Louis: Mosby, 2003.
Sherman B. Dementia with Dignity: a Handbook for Carers, 2nd edn. Sydney: McGraw-Hill, 1999.
Shives LR. Basic Concepts of Psychiatric Mental Health Nursing, 6th edn. Philadelphia: Lippincott, Williams & Wilkins, 2005.
Shives LR. Basic Concepts of Psychiatric Mental Health Nursing, 7th edn. Philadelphia: Lippincott Williams & Wilkins, 2008.
Smith P. So You Think You Are Going Crazy? New Zealand: Dunmore Press, 1993.
Stuart G, Psychophysiological responses and somatoform and sleep disorders. Stuart G, Laraia T. Principles and Practice of Psychiatric Nursing, 7th edn., St Louis: Mosby, 2001.
Stuart G, Actualizing the psychiatric nursing role: professional performance standards. Stuart G, Laraia T. Principles and Practice of Psychiatric Nursing, 7th edn., St Louis: Mosby, 2001. (2001)
Stuart G, Laraia T. Principles and Practice of Psychiatric Nursing, 8th edn. St Louis: Mosby, 2005.
Touhy TA, Jett KF. Ebersole and Hess’ Gerontological Nursing & Healthy Aging, 3rd edn. St Louis: Mosby, 2009.
Umstead-Raschmann C. Age Specific Considerations: the Elder Client. Online. Available: www.ihs.gov/MedicalPrograms/nursinged/files/handouts/elder.doc.html, 1995.
Varcarolis EM, Carson VB, Shoemaker NC. Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 5th edn. Philadelphia: WB Saunders, 2006.
Varcarolis E, Halter M. Foundations of Psychiatric Mental Health Nursing; A Clinical Approach, 6th edn. Saunders: St Louis, 2010.
Videbeck SL. Psychiatric Mental Health Nursing, 3rd edn. Philadelphia: Lippincott Williams & Wilkins, 2001.
Videbeck SL. Psychatric Mental Health Nursing, 5th edn. Philadelphia: Lippincott Williams & Wilkins, 2010.
Watkins P. Mental Health Nursing: The Art of Compassionate Care. Oxford: Butterworth–Heinemann, 2001.
Weir D, Oei T. Life stressors. In: Clinton M, Nelson S. Mental Health Nursing and Nursing Practice. Sydney: Prentice Hall, 1996. (1996)
Wilson HS, Kneisl CR. Psychiatric Nursing, 5th edn. Menlo Park: Addison Wesley, 1996.
AllPsych Online, www.allpsych.com/biographies.
Alzheimer’s Australia, www.alzheimers.org.au.
Australian and New Zealand College of Mental Health Nurses, www.anzcmhn.org.
British Psychological Society, www.bps.org.uk/.
Mental Health Legal Centre Inc (Vic), www.communitylaw.org.au/mentalhealth/.
Victorian Government Department of Human Services, www.health.vic.gov.au/mentalhealth Victorian Government Health Information: www.health.vic.gov.au/mentalhealth.
Victorian Mental Health Act 1986. www.health.vic.gov.au/mentalhealth/mh-act/index.htm.