Chapter Twenty-four Ears
INTRODUCTION
The ear is the sensory organ for hearing and maintaining equilibrium. In this chapter we review the structure and function of the external and internal ear. As changes in neurological function can affect hearing, you are advised to review the relevant sections in Chapter 22.
STRUCTURE AND FUNCTION
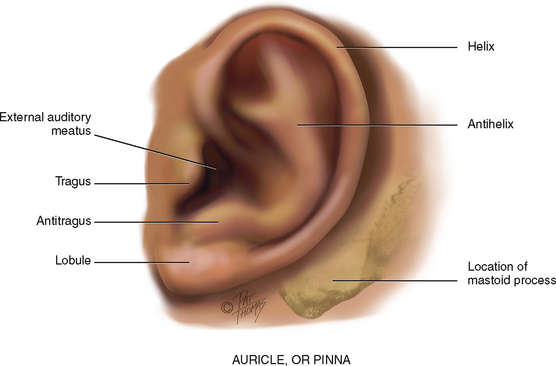
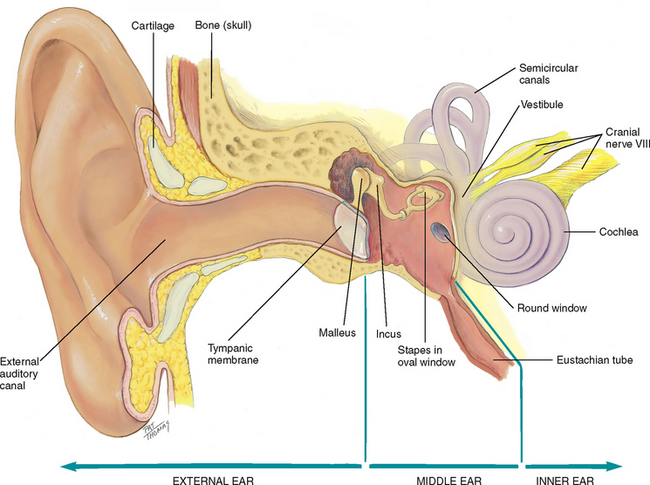
The ear has three parts: the external, middle and inner ear. The external ear is called the auricle or pinna and consists of movable cartilage and skin (Fig 24.1). Note the landmarks of the auricle and use these terms to describe your findings. The mastoid process, the bony prominence behind the lobule, is not part of the ear but is an important landmark.
EXTERNAL EAR
The external ear has a characteristic shape and serves to funnel sound waves into its opening, the external auditory canal (Fig 24.2). The canal is a cul-de-sac 2.5 to 3 cm long in the adult and terminates at the eardrum, or tympanic membrane. The canal is lined with glands that secrete cerumen, a yellow waxy material that lubricates and protects the ear. This secretion also repels water and traps dust and stops small particles from entering and damaging the ear. Cerumen migrates out to the meatus by the movements of chewing and talking. The presence of earwax can press against the eardrum and occlude the auditory canal and impair hearing. Wax can be grey and flaky, or wet cerumen which is honey brown to dark brown and moist. The presence and composition of cerumen are not related to poor hygiene.
The outer one-third of the canal is cartilage; the inner two-thirds consists of bone covered by thin sensitive skin. The canal has a slight S-curve in the adult. The outer third curves up and towards the back of the head, whereas the inner two-thirds angles down and forwards towards the nose.
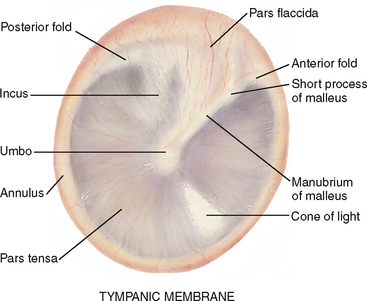
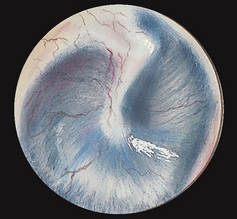
The tympanic membrane (TM), or eardrum, separates the external and middle ear and is tilted obliquely to the ear canal, facing downwards and somewhat forwards. It is a translucent membrane with a pearly grey colour and a prominent cone of light in the anteroinferior quadrant, which is the reflection of the otoscope light (Fig 24.3). The drum is oval and slightly concave, pulled in at its centre by one of the middle ear ossicles, the malleus. The parts of the malleus show through the translucent drum; these are the umbo, the manubrium (handle) and the short process. The small, slack, superior section of the tympanic membrane is called the pars flaccida. The remainder of the drum, which is thicker and more taut, is the pars tensa. The annulus is the outer fibrous rim of the drum.
Lymphatic drainage of the external ear flows to the parotid, mastoid and superficial cervical nodes.
MIDDLE EAR
The middle ear is a tiny air-filled cavity inside the temporal bone (see Fig 24.2). It contains tiny ear bones, or auditory ossicles: the malleus, incus and stapes. Several openings into the middle ear are present. Its opening to the outer ear is covered by the tympanic membrane. The openings to the inner ear are the oval window at the end of the stapes and the round window. Another opening is the eustachian tube, which connects the middle ear with the nasopharynx and allows passage of air. The tube is normally closed, but it opens with swallowing or yawning.
The middle ear has three functions: (1) it conducts sound vibrations from the outer ear to the central hearing apparatus in the inner ear, (2) it protects the inner ear by reducing the amplitude of loud sounds and (3) its eustachian tube allows equalisation of air pressure on each side of the tympanic membrane so that the membrane does not rupture (e.g. during altitude changes in an airplane).
INNER EAR
The inner ear contains the bony labyrinth, which holds the sensory organs for equilibrium and hearing. Within the bony labyrinth, the vestibule and the semicircular canals compose the vestibular apparatus, and the cochlea (Latin for ‘snail shell’) contains the central hearing apparatus. Although the inner ear is not accessible to direct examination, its functions can be assessed.
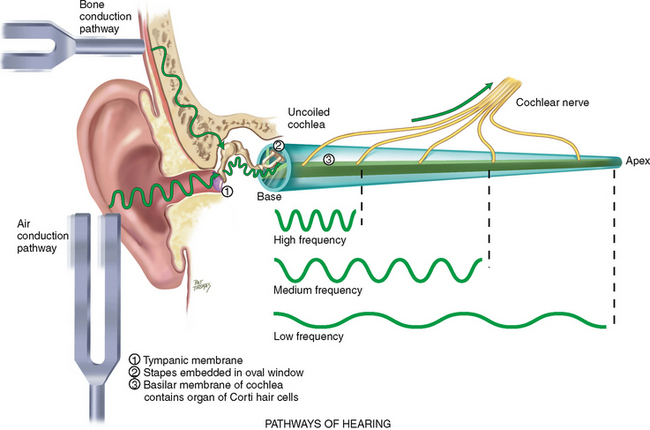
HEARING
Concerning the function of hearing, the auditory system can be divided into three levels: peripheral, brainstem and cerebral cortex. At the peripheral level, the ear transmits sound and converts its vibrations into electrical impulses, which can be analysed by the brain. For example, you hear an alarm bell ringing in the hall. Its sound waves travel instantly to your ears. The amplitude is how loud the alarm is; its frequency is the pitch (in this case, high) or the number of cycles per second. The sound waves produce vibrations on your tympanic membrane. These vibrations are carried by the middle ear ossicles to your oval window. Then the sound waves travel through your cochlea, which is coiled like a snail’s shell, and are dissipated against the round window. Along the way, the basilar membrane vibrates at a point specific to the frequency of the sound. In this case, the alarm’s high frequency stimulates the basilar membrane at its base near the stapes (Fig 24.4). The numerous fibres along the basilar membrane are the receptor hair cells of the organ of Corti, the sensory organ of hearing. As the hair cells bend, they mediate the vibrations into electrical impulses. The electrical impulses are conducted by the auditory portion of cranial nerve VIII to the brainstem.
The function at the brainstem level is binaural interaction, which permits locating the direction of a sound in space as well as identifying the sound. How does this work? Each ear is actually one half of the total sensory organ. The ears are located on each side of a movable head. The cranial nerve VIII from each ear sends signals to both sides of the brainstem. Areas in the brainstem are sensitive to differences in intensity and timing of the messages from the two ears, depending on the way the head is turned.
Finally, the function of the cortex is to interpret the meaning of the sound and begin the appropriate response. All this happens in the split second it takes you to react to the alarm.
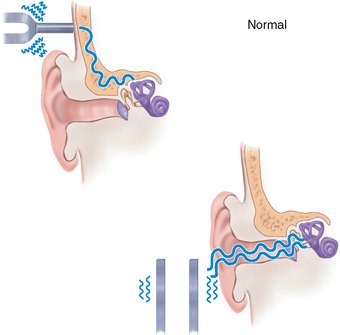
Pathways of hearing.
The normal pathway of hearing is air conduction (AC) described above; it is the most efficient. An alternative route of hearing is by bone conduction (BC). Here, the bones of the skull vibrate. These vibrations are transmitted directly to the inner ear and to cranial nerve VIII.
Hearing loss.
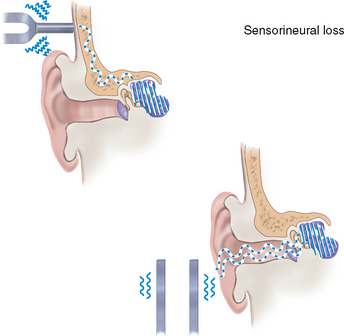
Anything that obstructs the transmission of sound impairs hearing. A conductive hearing loss involves a mechanical dysfunction of the external or middle ear. It is a partial loss because the person is able to hear if the sound amplitude is increased enough to reach normal nerve elements in the inner ear. Conductive hearing loss may be caused by impacted cerumen, foreign bodies, a perforated tympanic membrane, pus or serum in the middle ear and otosclerosis (a decrease in mobility of the ossicles).
Sensorineural (or perceptive) loss signifies pathology of the inner ear, cranial nerve VIII or the auditory areas of the cerebral cortex. A simple increase in amplitude may not enable the person to understand words. Sensorineural hearing loss may be caused by presbycusis, a gradual nerve degeneration that occurs with advancing years of age, and by ototoxic drugs, which affect the hair cells in the cochlea. A mixed loss is a combination of conductive and sensorineural types in the same ear.
Equilibrium.
The labyrinth in the inner ear constantly feeds information to your brain about your body’s position in space. It works like a plumb line to determine verticality or depth. The ear’s plumb lines register the angle of your head in relation to gravity. If the labyrinth ever becomes inflamed, it feeds the wrong information to the brain, creating a staggering gait and a strong, spinning, whirling sensation called vertigo.
DEVELOPMENTAL CONSIDERATIONS
Infants and children
The inner ear starts to develop early in the fifth week of gestation. In early development the ear is posteriorly rotated and low set; later it ascends to its normal placement around eye level. If maternal rubella infection occurs during the first trimester, it can damage the organ of Corti and impair hearing.
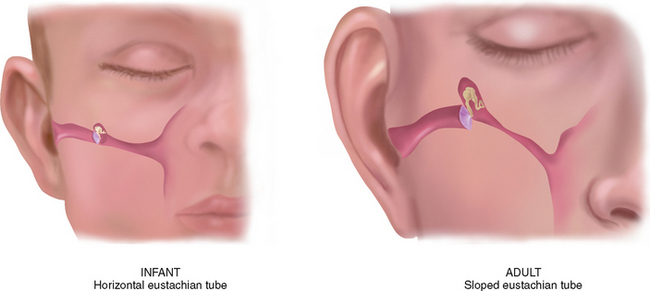
The infant’s eustachian tube is relatively shorter and wider and its position is more horizontal than the adult’s, so it is easier for pathogens from the nasopharynx to migrate through to the middle ear (Fig 24.5). The lumen is surrounded by lymphoid tissue, which increases during childhood; thus, the lumen is easily occluded. These factors place the infant at greater risk for middle ear infections than the adult.
The infant’s and toddler’s external auditory canal is shorter and has a slope opposite to that of the adult’s (see Fig 24.14 below).
Otitis media (OM) is an infection or inflammation of the middle ear and can affect all ages. Infection ascends into the middle ear cavity via the throat and causes swelling of the lining and blockage of the eustachian tube and reduction of airflow (National Institute of Deafness and Other Communication Disorders (NIDCD), 2010). A lack of ventilation resulting from obstruction of the eustachian tube or passage of nasopharyngeal secretions into the middle ear leads to an accumulation of fluid. This fluid may be serous, as in acute otitis media, or purulent, as occurs in suppurative otitis media and causes the tympanic membrane to bulge. Persistent OM and fluid in the middle ear may lead to effusion and hearing loss, placing the child at risk for delayed cognitive development (O’connor et al, 2009).
The incidence of otitis media is also increased in premature infants, in those with Down syndrome and in babies fed by bottle in a supine position. In the supine position the effects of gravity and sucking tend to draw the nasopharyngeal contents directly into the middle ear.
The adult
Otosclerosis is a common cause of conductive hearing loss in early adult years between the ages of 20 and 40 years. It is a gradual hardening that causes the foot plate of the stapes to become fixed in the oval window, impeding the transmission of sound and causing progressive deafness.
Late adulthood (65+ years)
In the person over 65 years, cilia lining the ear canal become coarse and stiff. This may cause decreased hearing because it impedes sound waves travelling towards the tympanic membrane. It also causes cerumen to accumulate and oxidise, which greatly reduces hearing. The cerumen itself is drier because of atrophy of the apocrine glands. Also, a life history of frequent ear infections may result in scarring on the drum.
Impacted cerumen is a common but reversible cause of hearing loss in people over 65 years. After removal of cerumen, most people have significantly improved hearing ability. We can improve the hearing health of people over 65 years by routinely performing otoscopic examinations and by performing ear canal irrigations when impacted cerumen occurs.
A person living in a noise-polluted area (e.g. near an airport or a busy highway) has a greater risk of hearing loss due to damage to the inner ear cells located in the cochlear. But presbycusis is a type of hearing loss that occurs with ageing, even in people living in a quiet environment. It is a gradual sensorineural loss caused by nerve degeneration in the inner ear or auditory nerve. Its onset usually occurs in the fifth decade, then it slowly progresses. The person first notices a high-frequency tone loss; it is harder to hear consonants (high-pitched components of speech) than vowels. This makes words sound garbled. The ability to localise sound is impaired also. This communication dysfunction is accentuated when unfavourable background noise is present (e.g. with music, with dishes clattering or at a large noisy party).
The auditory reaction time increases after age 70 years; that is, there is a delay in receiving and sending nerve impulses associated with hearing in an ageing adult (Brown, 2007).
CULTURAL AND SOCIAL CONSIDERATIONS
Indigenous Australians and New Zealanders remain at risk of more severe otitis media due to overcrowded living conditions and frequent exposure to nonpathogenic bacteria (Morris et al, 2009). As many as 80% of Aboriginal children have otitis media at some time during their school years, although 75% to 80% of all young children experience at least one episode of otitis media in their first 3 years (Morrison, 2010).
Hearing loss.
Hearing loss will become an important issue to be managed in the future by our healthcare system as it can significantly affect a person’s ability to live and work independently. Hearing loss is classified as congenital or acquired, pre-lingual or post-lingual, conductive or sensorineural (Australian Hearing, 2009). Ultimately any problem in the outer, middle, inner hearing pathway or auditory nerve pathway can cause hearing loss. In today’s society the most significant cause of hearing loss is noise-induced hearing loss. Other causes include accidents, the effects of ototoxic drugs or chemicals and normal ageing (Australian Hearing, 2009).
Noise-induced hearing loss results from damage to the hearing cells of the cochlear of the inner ear. The damage, which results from either exposure to very loud noise or long-term exposure to ‘reasonably loud noise’, can often be attributed to prolonged employment in high-noise industries. Any noise louder than 85 decibels (dB) has potential to cause hearing loss. Over half the population aged between 60 and 70 years reports hearing loss, with an increasing incidence over 70 years (70%) and again at 80 years (80%), with men having a higher incidence than women. For younger age groups there is great concern about the use of iPods, MP3 players and other music devices (see ‘Promoting a health lifestyle’ below).
New Zealand is anticipating a hearing loss epidemic (Accident Compensation Corporation, 2010). Expenditure related to hearing loss has doubled in recent years and over 40 million dollars is spent on compensation, assistive devices and medical attention. In Australia this figure has reached $12 billion dollars annually (Australian Hearing, 2009).
Moderate or greater hearing loss is detected in 9–12 children per 10 000 live births in Australia. Twenty three in 1000 children will require hearing aids for hearing impairment that has resulted from either an accident or illness (Australian Hearing, 2009). Otitis media is a common middle ear infection which is associated with temporary or fluctuating hearing loss. As mentioned earlier in this chapter, the incidence of otitis media is significantly higher amongst the Indigenous Australian and New Zealand children. This problem is compounded in New Zealand because hearing disorders are often detected quite late (Hear-it, 2010). Hearing loss in children is also associated with life-long negative consequences of language development, socialisation, education (including numeracy and literacy), social and emotional wellbeing and self esteem, training and employment opportunities, mental health and self harm and domestic violence (Commonwealth of Australia, 2010). People of all ages with hearing loss are at risk of feeling isolated and frustrated.
Australian and New Zealand governments have initiated a number of strategies to manage hearing loss including; the development of agencies such as ‘Australian Hearing’ to provide quality hearing to all people with hearing loss; conducting inquiries into hearing health; conducting research; providing national codes of practice and initiating screening programs for all children (Australian Hearing, 2009; Hear-it, 2010).
SUBJECTIVE DATA
Determining what the person feels or experiences in both recent and past times contributes subjective data to the assessment of ear pain, infection, discharge, hearing loss, vertigo, the environmental circumstances and how they care for their ears. Asking specific questions may be useful to elicit subjective data and for determining relevance of the assessment to nursing practice. As you read this section be thinking critically about each assessment and its clinical significance. Clearly you will have to adjust your assessment techniques if the person is hearing impaired.
| Assessment guidelines | Clinical significance and clinical alerts |
|---|---|
Otalgia–ear pain–may be directly due to ear disease or may be referred pain from a problem in teeth or oropharynx. Pain that occurs when the person puts pressure on the ear or pulls the earlobe may indicate the presence of an inner ear infection. The character of the pain may indicate the severity of the ear problem. People with severe or persistent earache should be referred to a medical practitioner. |
|
| • Presence of any accompanying cold symptoms or sore throat? Have there been any problems with sinuses or teeth? | Virus/bacteria from upper respiratory infection may migrate up eustachian tube to involve middle ear. |
| • Past or recent trauma of the ear area; for example, have you ever been hit on the ear or on the side of the head, or had any sports injury? Ever had any trauma from a foreign body? | Trauma may rupture the tympanic membrane. |
| • What have you tried to relieve the earache/pain? | Assess affect of coping strategies. |
| A history of chronic ear problems suggests possible sequelae. | |
| Discharge (otorrhoea) suggests in fected canal or a perforated eardrum. For example: | |
| • Colour—Does it look like pus, or is it bloody? | |
| • Odour—Is there any odour/smell to the discharge? | Cholesteatoma–dirty yellow/grey discharge, foul odour. |
| • Is there any relationship between the discharge and the ear pain? | Typically with perforation–ear pain occurs first, stops with a popping sensation then drainage occurs. |
| Presbycusis is gradual onset over years, whereas a trauma hearing loss is often sudden. Refer any sudden loss in one or both ears not associated with upper respiratory tract infection (URTI). | |
| • Onset—Did the loss come on slowly or all at once? | |
| • Character—Has all your hearing decreased, or just on hearing certain sounds? | |
| • In what situations do you notice the loss: conversations, using the telephone, listening to TV, at a party? | Loss is apparent when competition from background noise is present, as at a party. |
| • Do people seem to shout at you? | Recruitment–a marked loss when sound is at low intensity, but sound actually becomes painful when repeated in a loud voice. |
| • Do ordinary sounds seem hollow, as if you are hearing in a barrel or under water? | Character of hearing loss when cerumen expands and becomes impacted, as after swimming or showering. |
| • Have you recently travelled by aeroplane? | |
| • Is there any family history of hearing loss? | |
| • Have you tried to treat the hearing loss with a hearing aid or other device? Have you tried anything to help with your hearing? | |
| • Assess the person’s coping strategies. How does the loss affect your daily life? Any job problem? Feel embarrassed? Frustrated? How do your family friends react? | Hearing loss can cause social isolation and can lessen pleasure of leisure activities. |
| Note during history taking, the following clues from normal conversation indicate possible hearing loss: | |
| 1 Person lip reading or watching your face and lips closely rather than your eyes | |
| 2 Frowning or straining forwards to hear | |
| 3 Posturing of head to catch sounds with better ear | |
| 4 Misunderstanding your questions or frequently asking you to repeat | |
| 5 Irritability or showing startle reflex when you raise your voice (recruitment) | |
| 6 Speech sounds garbled, possibly with vowel sounds distorted | |
| 7 Inappropriately loud voice | |
| 8 Flat, monotonous tone of voice. | |
| Old trauma to hearing initially goes unnoticed but results in further decibel loss in later years. | |
| • Are you near other noises such as heavy machinery or a loud persistent noise or loud music? | |
| • Assess the person’s coping strategies. Have you taken any steps to protect your ears, such as headphones or ear plugs? | |
| Tinnitus originates within the person; it accompanies some hearing or ear disorders. | |
| • Have you ever felt ringing, crackling or buzzing in your ears? | |
| • When did this occur? | |
| • Does this seem louder at night? | Tinnitus seems louder with no competition from environment noise. |
| • Are you taking any medications? | Many medications have ototoxic sequelae: aspirin, aminoglycosides (streptomycin, gentamicin, kanamycin, neomycin), ethacrynic acid, frusemide, indomethacin, naproxen, quinine, vancomycin. |
| True rotational spinning occurs with dysfunction of labyrinth. Objective vertigo–feels like room spins. Subjective vertigo–person feels as if they are spinning. | |
| • Ever felt vertigo, that is, the room spinning around or yourself spinning? (Vertigo is a true twirling motion.) | |
| • Ever felt dizzy, like you are not quite steady, like falling or losing your balance? Giddy, lightheaded? | |
| Assess potential trauma from invasive instruments. Cotton-tipped applicators can impact cerumen, causing hearing loss. | |
| Prescribe frequency of hearing assessment according to person’s age or risk factors. | |
| Additional history for infants and children | |
| A first episode that occurs within 3 months of life increases risk of recurrent otitis media (OM). Recurrent OM is three episodes in past 6 months but more likely in the presence of OM with effusions (Morris and Leach, 2009) | |
| • Are the infections increasing in frequency in severity or staying the same? | |
| • Does anyone in the home smoke cigarettes or a pipe? | Passive and gestational smoke is a risk factor for OM (NIDCD, 2010). |
| • Does your child receive child care outside your home? In a daycare centre or someone else’s home? How many children in the group care? | Attendance at group daycare and bottle feeding (as opposed to breastfeeding) are also risk factors for otitis media. |
2. Does the child seem to be hearing well? • Have you noticed that the infant startles with loud noise? Did the infant babble around 6 months? Do they talk? At what age did talking start? Was the speech intelligible?
• Ever had the child’s hearing tested? If there was a hearing loss, did it follow any diseases in the child, or in the mother during pregnancy?
(Note: It is important to identify any problem early, because a child with hearing loss is at risk for delayed speech and social development and learning deficit.) |
Children at risk for hearing deficit include those exposed to maternal rubella, syphilis, cytomegalovirus or toxoplas-mosis or to maternal ototoxic drugs in utero; premature infants; low birth weight infants; trauma or hypoxia at birth; and infants with congenital liver or kidney disease. In children the incidence of meningitis, measles, mumps, otitis media and any illness with persistent high fever may increase risk of hearing deficit. |
| These children are at increased risk for trauma. |
OBJECTIVE DATA
Undertaking an ear examination enables the nurse to thoroughly evaluate the condition of the ears. The focus of the examination includes screening for hearing loss and assessing for other ear problems such as ear pain, discharge, lumps or the presence of other objects. A nurse will be able to detect problems in the ear canal, tympanic membrane or middle ear. Signs of infection, excessive cerumen or foreign objects will clearly be seen.
Collecting objective data is an important part of any ear assessment. The objective ear assessment is used for: screening infants and children for hearing loss, investigating symptoms such as ear pain, pressure and fullness, checking for excessive cerumen or other objects in the ear canal and locating the site of an ear infection. Objective data collection also enables a nurse to monitor the effectiveness of a treatment plan for an ear problem.
Changes in the objective data have significant implications. Infants and children with ear problems have been known to be irritable, display signs of stress and anxiety and be socially isolated. Social isolation is also a common consequence for adolescents, adults and older adults. As the adult ages changes in ear function can result in a safety risk due to dizziness or hearing loss.
| Preparation | Equipment needed |
|---|---|
| Position the adult sitting up straight with their head at your eye level. Occasionally the ear canal is partially filled with cerumen, which obstructs your view of the tympanic membrane. In this case the person should be referred to a medical practitioner for further assessment. | Otoscope with bright light (fresh batteries give off white–not yellow–light) |
| Procedures and normal findings | Abnormal findings and clinical alerts |
|---|---|
| INSPECT AND PALPATE THE EXTERNAL EAR | |
| Size and shape | |
| The ears are of equal size bilaterally with no swelling or thickening. Ears of unusual size and shape may be a normal familial trait with no clinical significance. | |
| Skin condition | |
| The skin colour is consistent with the person’s facial skin colour. The skin is intact, with no lumps or lesions. On some people you may note Darwin’s tubercle, a small painless nodule at the helix. This is a congenital variation and is not significant (see Table 24.2). | Reddened, excessively warm skin indicates inflammation (see Table 24.1). Crusts and scaling occur with otitis externa, eczema, contact dermatitis, seborrhoea. Enlarged tender lymph nodes in the region indicate inflammation of the pinna or mastoid process. Red-blue discolouration indicates frostbite. Tophi, sebaceous cyst, chondroderma-titis, keloid, carcinoma (see Table 24.2). |
| Tenderness | |
| Move the pinna and push on the tragus. They should feel firm and movement should produce no pain. Palpating the mastoid process should also produce no pain. | |
| The external auditory meatus | |
| Note the size of the opening to direct your choice of speculum for the otoscope. No swelling, redness or discharge should be present. | |
| Some cerumen is usually present. The colour varies from grey-yellow to light brown and black, and the texture varies from moist and waxy to dry and desiccated. A large amount of cerumen obscures visualisation of the canal and drum. | |
| INSPECT WITH THE OTOSCOPE | |
| As you inspect the external ear, note the size of the auditory meatus. Then choose the largest speculum that will fit comfortably in the ear canal and attach it to the otoscope. Tilt the person’s head slightly away from you towards the opposite shoulder. This method brings the obliquely sloping eardrum into better view. | |
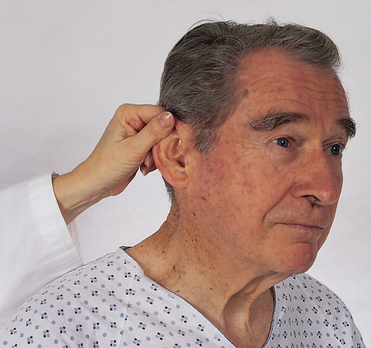
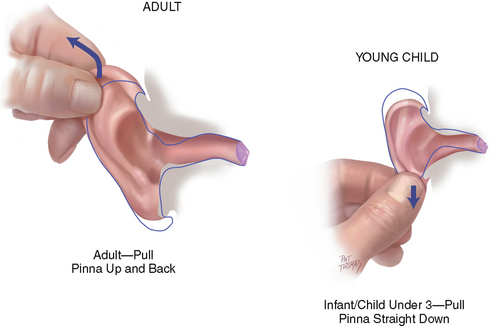
| Pull the pinna up and back on a pre-adolescent child or adult; this helps straighten the S-shape of the canal (Fig 24.6). Hold the pinna gently but firmly. Do not release traction on the ear until you have finished the examination and the otoscope is removed. | Pulling on the pinna may cause and increase pain if the person has otitis media. |
| Hold the otoscope ‘upside down’ along your fingers and have the dorsa (back) of your hand along the person’s cheek braced to steady the otoscope (Fig 24.7). This position feels awkward to you only at first. It soon will feel natural and you will find it useful to prevent forceful insertion. Also, your stabilising hand acts as a protecting lever if the person suddenly moves their head. | |
| Insert the speculum slowly and carefully along the axis of the canal. Watch the insertion; then put your eye up to the otoscope. Avoid touching the inner ‘bony’ section of the canal wall, which is covered by a thin epithelial layer and is sensitive to pain. Sometimes you cannot see anything but canal wall. If so, try to reposition the person’s head, apply more traction on the pinna, and re-angle the otoscope to look forwards towards the person’s nose. | |
| Once it is in place, you may need to rotate the otoscope slightly to visualise all the eardrum; do this gently. Lastly, perform the otoscopic examination before you test hearing; ear canals with impacted cerumen give the erroneous impression of pathological hearing loss. | |
| The external canal | |
| Note any redness and swelling, lesions, foreign bodies or discharge. If any discharge is present, note the colour and odour. (Also, clean any discharge from the speculum before examining the other ear to avoid contamination with possibly infectious material.) For a person with a hearing aid, note any irritation on the canal wall from poorly fitting hearing aid ear moulds. | Redness and swelling occur with otitis externa; canal may be completely closed with swelling. This condition clearly will induce temporary unilateral hearing loss and has implications for communication. Purulent otorrhoea suggests otitis externa or otitis media if the drum has ruptured. Frank blood or clear, watery drainage (cerebrospinal fluid (CSF)) after trauma suggests basal skull fracture and warrants immediate referral. Foreign body, polyp, furuncle, exostosis (see Table 24.3). |
| The tympanic membrane | |
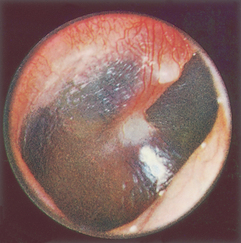
| Colour and characteristics. Systematically explore its landmarks (Fig 24.8). The normal eardrum is shiny and translucent, with a pearl-grey colour. The cone-shaped light reflex is prominent in the anteroinferior quadrant (at 5 o’clock in the right drum and 7 o’clock in the left drum). This is the reflection of your otoscope light. Sections of the malleus are visible through the translucent drum: the umbo, manubrium and short process. (Infrequently, you also may see the incus behind the drum; it shows as a whitish haze in the upper posterior area.) At the periphery the annulus looks whiter and denser. | Yellow-amber drum colour occurs with otitis media with effusion (serous). Red colour occurs with acute otitis media. Absent or distorted landmarks. Air/fluid level or air bubbles behind drum indicate otitis media with effusion (see Tables 24.4 and 24.5). |
| Position. The eardrum is flat, slightly pulled in at the centre, and flutters when the person performs the Valsalva manoeuvre or holds the nose and swallows (insufflation). You may elicit these manoeuvres to assess drum mobility. Avoid them with an ageing person because they may disrupt equilibrium. Also avoid middle ear insufflation in a person with upper respiratory infection because it could propel infectious matter into the middle ear. | Retracted drum resulting from vacuum in middle ear with obstructed eustachian tube. Bulging drum from increased pressure in otitis media. Drum hypomobility is an early sign of otitis media (see Table 24.5). |
| Integrity of membrane. Inspect the eardrum and the entire circumference of the annulus for perforations. The normal tympanic membrane is intact. Some adults may show scarring, which is a dense white patch on the drum. This is a sequela of repeated ear infections. | Perforation shows as a dark oval area or as a larger opening on the drum. |
| Vesicles on drum (see Table 24.5). | |
| TEST HEARING ACUITY | |
| Whispered voice test | |
| Test one ear at a time while masking hearing in the other ear to prevent sound transmission around the head. This is done by placing one finger on the tragus and rapidly pushing it in and out of the auditory meatus. Shield your lips so the person cannot compensate for a hearing loss (consciously or unconsciously) by lip reading or using the ‘good’ ear. With your head 30 to 60 cm from the person’s ear, exhale and whisper slowly some two-syllable words, such as Tuesday, armchair, football and fourteen. Normally, the person repeats each word correctly after you say it. | The person is unable to hear whispered words. A whisper is a high-frequency sound and is used to detect high-tone loss. |
| DEVELOPMENTAL CONSIDERATIONS | |
| Infants and young children | |
| Simple hearing test. The room should be silent and the baby contented. Make a loud sudden noise (hand clap or squeeze toy) out of the baby’s peripheral range of vision of about 30 cm. You may need to repeat this a few times, but you should note these responses: | |
| Absence of alerting behaviour may indicate congenital deafness. | |
| 6 to 8 months—infant turns head to localise sound, responds to own name | Failure to localise sound. |
| No intelligible speech by 2 years of age. | |
1. The child is inattentive in casual conversation. 2. The child reacts more to movement and facial expression than to sound. 3. The child’s facial expression is strained or puzzled. 4. The child frequently asks to have statements repeated. 5. The child confuses words that sound alike. 6. The child has an accompanying speech problem: speech is monotonous or garbled; the child mispronounces or omits sounds. 7. The child appears shy and withdrawn and ‘lives in a world of their own’. 8. The child frequently complains of earaches. 9. The child hears better at times when the environment is more conducive to hearing. |
|
| The adult over 65 years | |
An older person may have pendulous earlobes with linear wrinkling because of loss of elasticity of the pinna. Coarse, wiry hairs may be present at the opening of the ear canal. During otoscopy the eardrum normally may be whiter in colour and more opaque, duller than in the early or middle adult. It may also look thickened. A high-tone frequency hearing loss is apparent for those affected with pres-bycusis, the hearing loss that occurs with ageing. This condition is revealed in difficulty hearing whispered words in the voice test and in difficulty hearing consonants during conversational speech. The late adult feels that ‘people are mumbling’ and feels isolated in family or friendship groups. |
FURTHER OBJECTIVE ASSESSMENT FOR ADVANCED PRACTICE
The assessments that are described in the following sections require advanced skill and scope of practice. Nurses working in specialist ear hospitals and clinics and some community nurses need to develop these skills.
TABLE 24.1 Abnormalities of the external ear
 |
| Frostbite |
 |
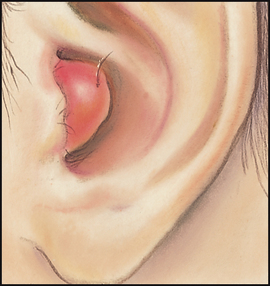
| Otitis externa (swimmer’s ear) |
| An infection of the outer ear, with severe painful movement of the pinna and tragus, redness and swelling of pinna and canal, scanty purulent discharge, scaling, itching, fever and enlarged tender regional lymph nodes. Hearing is normal or slightly diminished. More common in hot humid weather. Swimming causes canal to become waterlogged and swell; skinfolds are set up for infection. Prevent by using rubbing alcohol or 2% acetic acid eardrops after every swim. |
 |
| Branchial remnant and ear deformity |
| A facial remnant or leftover of the embryological branchial arch usually appears as a skin tag, in this case one containing cartilage. They occur most often in the preauricular area, in front of the tragus. When bilateral, there is increased risk of renal anomalies. |
| Cerebrospinal fluid otorrhoea (not illustrated) |
| Skull fracture of temporal bone causes cerebrospinal fluid to leak from ear canal and pool in concha when the person is supine. Cerebrospinal fluid feels oily and tests positive for glucose—often clinicians use glucose oxidase paper or dextrose sticks to test for CSF. However, this form of testing is not definitive and has been shown to be unreliable because lacrimal gland secretions and nasal mucus have reducing substances that potentially cause a positive reaction with glucose concentrations as low as 0.28 mmol/L. Another test used by healthcare professionals includes the ‘halo test’. In this test a drop of the leaking fluid is placed onto a white tissue or towel. If CSF is present, the blood will coalesce in the middle and a yellowish ring will form around it after a few minutes. This test, too, can provide a false positive (Baker, 2008). |
TABLE 24.2 Lumps and lesions on the external ear
 |
| Darwin’s tubercle |
| Small painless nodule at the helix. It is a congenital variation and is not significant. Do not mistake it for a tophus. |
 |
| Sebaceous cyst |
| Location is commonly behind lobule, in the postauricular fold. A nodule with central black punctum indicates blocked sebaceous gland. It is filled with waxy sebaceous material and is painful if it becomes infected. Often are multiple. |
 |
| Tophi |
 |
| Chondrodermatitis nodularis helicus |
| Painful nodules develop on the rim of the helix (where there is no cushioning subcutaneous tissue) as a result of repetitive mechanical pressure or environmental trauma (sunlight). They are small, indurated, dull red, poorly defined and very painful. |
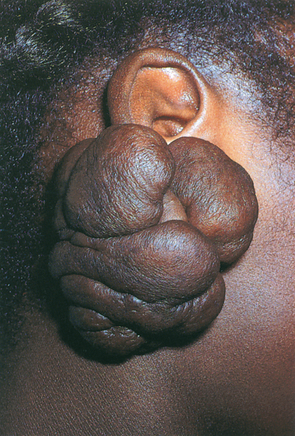 |
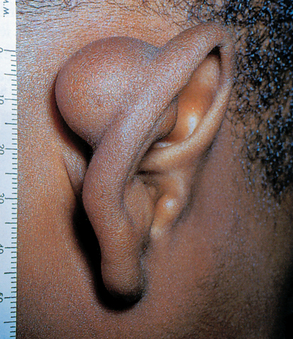
| Keloid |
| Overgrowth of scar tissue, which invades original site of trauma. It is more common in dark-skinned people. In the ear it is most common at lobule at the site of a pierced ear. Overgrowth shown here is unusually large. |
 |
| Carcinoma |
| Ulcerated crusted nodule with indurated base that fails to heal. Bleeds intermittently. Must refer for biopsy. Usually occurs on the superior rim of the pinna, which has the most sun exposure. May occur also in ear canal and show chronic discharge that is either serosanguineous or bloody. |
| Preparation | Equipment needed |
|---|---|
| Position the adult sitting up straight with their head at your eye level. | Tuning forks–frequencies from 256 to 1024 Hz are available. The high pitch tuning forks are appropriate for hearing testing, e.g. 512 Hz |
| Procedures and normal findings | Abnormal findings and clinical alerts |
|---|---|
| TEST HEARING ACUITY | |
| Your screening for a hearing deficit begins during the history; how well does the person hear conversational speech? An audiometer gives a precise quantitative measure of hearing by assessing the person’s ability to hear sounds of varying frequency. Because this equipment is usually not available in the clinical setting, you may use alternative screening measures. These are ‘crude’ tests. They are nonquantitative; they are useful to document the presence of hearing loss but do not measure the degree of loss. Refer any abnormal findings for more accurate measures with pure tone audiometry. | |
| Tuning fork tests | |
| Tuning fork tests measure hearing by air conduction (AC) or by bone conduction (BC), in which the sound vibrates through the cranial bones to the inner ear. The AC route through the ear canal and middle ear is usually the more sensitive route. The high pitch tuning fork is more discriminative for hearing testing. To activate the tuning fork, hold it by the stem and strike the tines softly on the back of your hand (Fig 24.9). A hard strike makes the tone too loud, and it takes a long time to fade out. | |
| The Weber test is valuable when a person reports hearing better with one ear than the other. Place a vibrating tuning fork in the midline of the person’s skull and ask whether the tone sounds the same in both ears or better in one (Fig 24.10). The person should hear the tone by bone conduction through the skull, and it should sound equally loud in both ears. | Sound lateralises to one ear with a conductive or a sensorineural loss (see Table 24.6). |
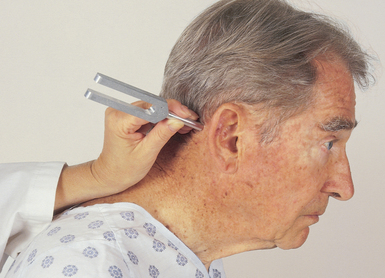
| The Rinne test compares air conduction and bone conduction sound (Fig 24.11). Place the stem of the vibrating tuning fork on the person’s mastoid process and ask them to signal when the sound goes away. Quickly invert the fork so the vibrating end is near the ear canal; the person should still hear a sound (Fig 24.12). Normally the sound is heard twice as long by air conduction (next to ear canal) as by bone conduction (through the mastoid process). A normal response is a positive Rinne test, or ‘AC > BC’. Repeat with the other ear. | Ratio of AC to BC is altered with hearing loss (see Table 24.6). Sound is heard longer by bone conduction with a conductive loss. |
| THE VESTIBULAR APPARATUS | |
| The Romberg test assesses the ability of the vestibular apparatus in the inner ear to help maintain standing balance. Because the Romberg test also assesses intactness of the cerebellum and proprioception, it is discussed in Chapter 22 (see Fig 22.23). | |
| Infants and young children | |
| Otoscopic examination. In addition to its place in the complete examination, eardrum assessment is mandatory for any infant or child requiring care for illness or fever. For the infant or young child, the timing of the otoscopic examination is best towards the end of the complete examination. Many young children protest vigorously during this procedure no matter how well you prepare, and it is difficult to re-establish cooperation afterwards. Save the otoscopic examination until last. Then the parent can hold and comfort the child. | |
| Test hearing acuity. Use the developmental milestones mentioned in the previous section to assess hearing in an infant. Also, attend to the parents’ concern over the infant’s inability to hear; their assessment is usually well founded. | |
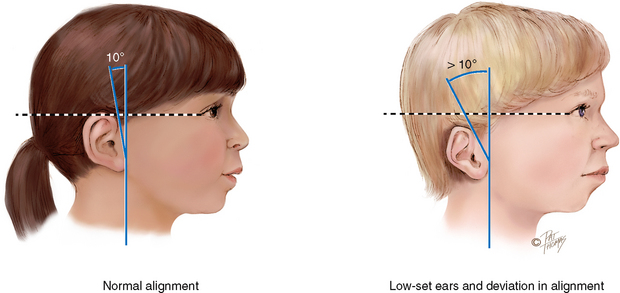
| Examination of the external ear is similar to that described for the adult, with the addition of examination of position and alignment on head. Note the ear position. The top of the pinna should match an imaginary line extending from the corner of the eye to the occiput. Also, the ear should be positioned within 10 degrees of vertical (Fig 24.13). | Low-set ears or deviation in alignment may indicate mental retardation or a genitourinary malformation. |
| To help prepare the child, let the child hold your funny-looking ‘torch’. You may wish to have the child look in the parent’s ear as you hold the otoscope (Fig 24.14). | |
| Positioning of the child is important. You need a clear view of the canal. Avoid harsh restraint, but you must protect the eardrum from injury in case of sudden head movement. Enlist the aid of a cooperative parent. Prop an infant upright against the parent’s chest or shoulder, with the parent’s arm around the upper part of the head (Fig 24.15). A toddler can be held in the parent’s lap or may lie on the examining table with their arms secured (Fig 24.16). In each case, the child’s head is stabilised to avoid movement against the otoscope. | |
| Remember to pull the pinna straight down on an infant or a child under 3 years old. This method will match the slope of the ear canal (Fig 24.17). | |
At birth the patency of the ear canal is determined, but the otoscopic examination is not performed because the canal is filled with amniotic fluid and vernix caseosa. After a few days the tympanic membrane (TM) is examined. During the first few days, the TM often looks thickened and opaque. It may look ‘injected’ and have a mild redness from increased vascularity. The eardrum also looks injected in infants after crying. The position of the eardrum is more horizontal in the neonate, making it more difficult to see completely and harder to differentiate from the canal wall. By 1 month of age, the drum is in the oblique (more vertical) position as in the older child, and examination is a bit easier. |
|
| When examining an infant or young child, a pneumatic bulb attachment for the otoscope enables you to direct a light puff of air towards the drum to assess vibratility (Fig 24.18). For a secure seal, choose the largest speculum that will fit in the ear canal without causing pain. A rubber tip on the end of the speculum gives a better seal. Give a small pump to the bulb (positive pressure), then release the bulb (negative pressure). Normally the tympanic membrane moves inwards with a slight puff and outwards with a slight release. | An abnormal response is no movement. Drum hypomobility indicates effusion or a high vacuum in the middle ear. For the newborn’s first 6 weeks, drum immobility is the best indicator of middle ear infection. |
| Normally the tympanic membrane is intact. In a child being treated for chronic otitis media, you may note the presence of a tympanostomy tube in the central part of the eardrum. This is inserted surgically to equalise pressure and drain secretions. Finally, although the condition is not normal, it is not uncommon to note a foreign body in a child’s canal, such as a small stone or a bead. | Chronic otitis media relieved by tympanostomy tubes (see Table 24.5). Foreign body (see Table 24.3). |
TABLE 24.3 Abnormalities in the ear canal
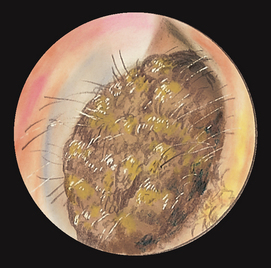 |
| Excessive cerumen |
| Excessive cerumen is produced or is impacted because of narrow tortuous canal or poor cleaning method. May show as round ball partially obscuring drum or totally occluding canal. Even when canal is 90% to 95% blocked, hearing stays normal. But when last 5% to 10% is totally occluded (when cerumen expands after swimming or showering), person has ear fullness and sudden hearing loss. |
 |
| Otitis externa |
| Severe swelling of canal, inflammation, tenderness. Here canal lumen is narrowed to one-quarter normal size. (See complete description in Table 24.1.) |
 |
| Osteoma |
| Single, stony hard, rounded nodule that obscures the drum; nontender; overlying skin appears normal. Attached to inner third, the bony part, of canal. Benign, but refer for removal. |
 |
| Foreign body |
| Usually it is children who place a foreign body in the ear (here, a stone completely occludes the canal), which is later noted on routine examination. Common objects are beans, corn, breakfast cereals, jewellery beads, small stones, sponge rubber. Cotton is most common in adults and becomes impacted from cotton-tipped applicators. A trapped live insect is uncommon but makes the person especially frantic. |
 |
| Exostosis |
| More common than osteoma. Small, bony hard, rounded nodules of hypertrophic bone, covered with normal epithelium. They arise near the drum but usually do not obstruct the view of the drum. They are usually multiple and bilateral. They may occur more frequently in cold-water swimmers. The condition needs no treatment, although it may cause accumulation of cerumen, which blocks the canal. |
 |
| Furuncle |
| Exquisitely painful, reddened, infected hair follicle. Here, it occurs on the tragus but also may be on cartilaginous part of ear canal. Regional lymphadenopathy often accompanies a furuncle. |
 |
| Polyp |
| Arises in canal from granulomatous or mucosal tissue; redder than surrounding skin and bleeds easily; bathed in foul purulent discharge; indicates chronic ear disease. Benign, but refer for excision. |
TABLE 24.4 Abnormal findings seen on otoscopy
| Appearance of eardrum | Indicates | Suggested condition |
|---|---|---|
| Yellow-amber colour | Serum or pus | Serous otitis media or chronic otitis media |
| Prominent landmarks | Retraction of drum | Negative pressure in middle ear from an obstructed eustachian tube |
| Air/fluid level or air bubbles | Serous fluid | Serous otitis media |
| Absent or distorted light reflex | Bulging of eardrum | Acute otitis media |
| Bright red colour | Infection in middle ear | Acute purulent otitis media |
| Blue or dark red colour | Blood behind drum | Trauma, skull fracture |
| Dark oval areas | Perforation | Drum rupture |
| White dense areas | Scarring | Sequelae of infections |
| Diminished or absent landmarks | Thickened drum | Chronic otitis media |
| Black or white dots on drum or canal | Colony of growth | Fungal infection |
From Sherman JL, Fields SK: Guide to patient evaluation, 5th edn. New York, 1988, Medical Examination Publishing. Reprinted by permission of Elsevier Inc.
TABLE 24.5 Abnormalities of the tympanic membrane
 |
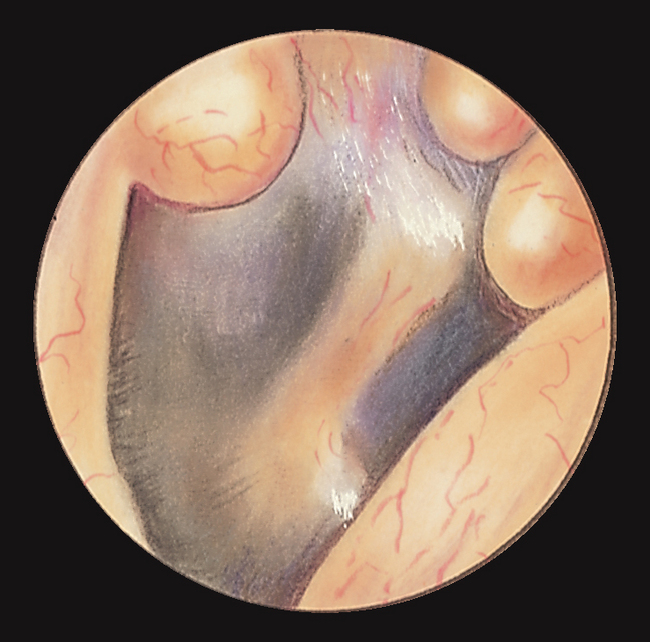
| Retracted drum |
| Landmarks look more prominent and well defined. Malleus handle looks shorter and more horizontal than normal. Short process is very prominent. Light reflex is absent or distorted. The drum is dull and lustreless and does not move. These signs indicate negative pressure and middle ear vacuum from obstructed eustachian tube and serous otitis media. |
 |
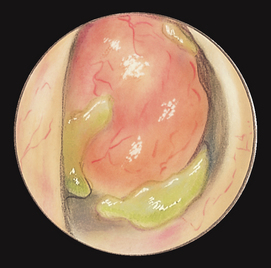
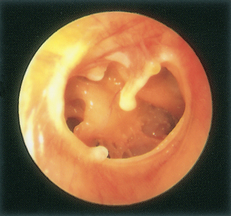
| Otitis media with effusion (OME) |
| An amber-yellow drum suggests serum in middle ear that transudates to relieve negative pressure from the blocked eustachian tube. You may note an air/fluid level with fine black dividing line or air bubbles visible behind drum. Symptoms are feeling of fullness, transient hearing loss, popping sound with swallowing. Also called serous otitis media, glue ear. |
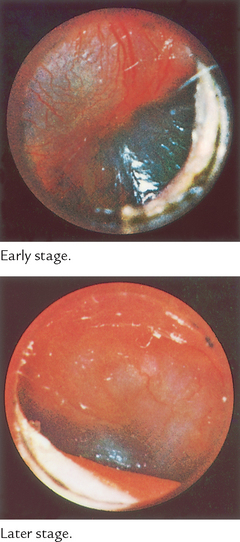 |
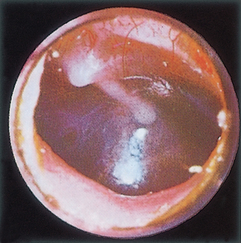
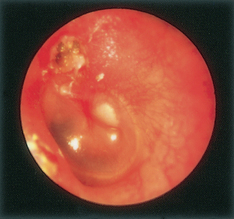
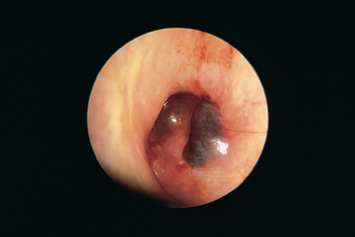
| Acute (purulent) otitis media |
| This results when the middle ear fluid is infected. An absent light reflex from increasing middle ear pressure is an early sign. Redness and bulging are first noted in superior part of drum (pars flaccida), along with earache and fever. Then fiery red bulging of entire drum occurs; deep throbbing pain; fever; transient hearing loss. Pneumatic otoscopy reveals drum hypomobility. |
 |
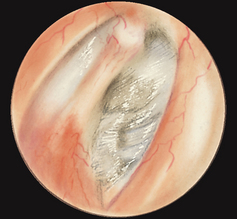
| Perforation |
| If the acute otitis media is not treated, the drum may rupture from increased pressure. Perforations also occur from trauma (e.g. a slap on the ear). Usually the perforation appears as a round or oval darkened area on the drum, but in this photo the perforation is very large. Central perforations occur in the pars tensa. Marginal perforations occur at the annulus. Marginal perforations are called attic perforations when they occur in superior part of the drum, the pars flaccida. |
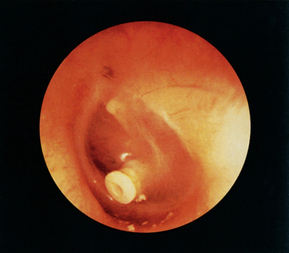 |
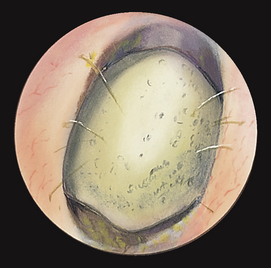
| Insertion of tubes (grommets) |
| Polyethylene tubes are inserted surgically into the eardrum to relieve middle ear pressure and promote drainage of chronic or recurrent middle ear infections. Number of acute infections tends to decrease because of improved aeration. Tubes extrude spontaneously in 12 to 18 months. In Australia and New Zealand these tubes are called ventilation tubes or grommets. |
| Reprinted from Fireman P: Atlas of allergies, 2nd edn, p. 182, 1995, by permission of the publisher, Mosby. |
 |
| Cholesteatoma |
| An overgrowth of epidermal tissue in the middle ear or temporal bone may result over the years after a marginal TM perforation. It has a pearly white, cheesy appearance. Growth of cholesteatoma can erode bone and produce hearing loss. Early signs include otorrhoea, unilateral conductive hearing loss, tinnitus. |
 |
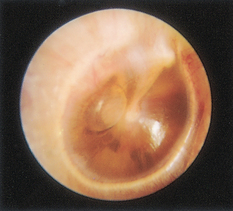
| Scarred drum |
| Dense white patches on the eardrum are sequelae of repeated ear infections. They do not necessarily affect hearing. |
 |
| Blue drum (haemotympanum) |
| This indicates blood in the middle ear, as in trauma resulting in skull fracture. |
 |
| Bullous myringitis |
| Small vesicles containing blood on the drum; accompany mycoplasma pneumonia and virus infections. May have blood-tinged discharge and severe otalgia. |
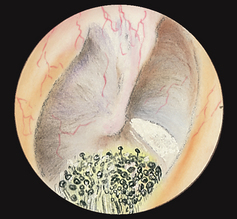 |
| Fungal infection (otomycosis) |
| Colony of black or white dots on drum or canal wall suggests a yeast or fungal infection. |
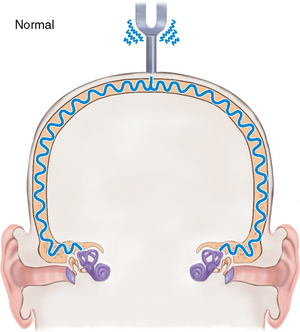 |
| Normal–Sound is equally loud in both ears; sound does not lateralise. |
 |
| Normal–Sound is heard twice as long by air conduction (AC) as by bone conduction (BC); a ‘positive’ Rinne, or AC > BC. |
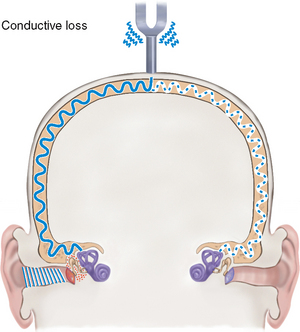 |
| Conductive loss–Sound lateralises to ‘poorer’ ear from background room noise, which masks hearing in normal ear. ‘Poorer’ ear (the one with conductive loss) is not distracted by background noise, thus has a better chance to hear bone-conducted sound. Examples: transient conductive loss with serous or purulent otitis media. |
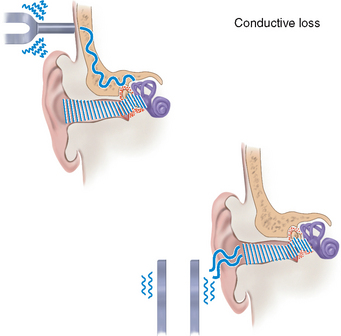 |
| Conductive loss–Person hears as long by bone conduction (AC = BC) or even longer (AC < BC), a ‘negative’ finding on the Rinne test. |
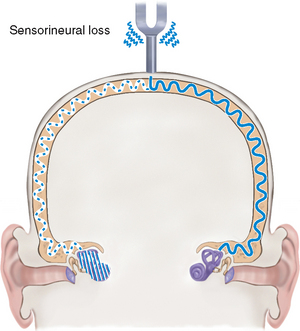 |
| Sensorineural loss–Sound lateralises to ‘better’ ear or unaffected ear. Poor ear (the one with nerve loss) is unable to perceive the sound. |
 |
| Sensorineural loss–Normal ratio of AC > BC is intact but is reduced overall. That is, person hears poorly both ways. |
Promoting a healthy lifestyle
Use of digital music players/earbuds and hearing loss
‘Don’t lose the music’. Today, there is growing concern about the potential for hearing loss in young people using personal digital music devices (MP3 or iPod player) and earbud headphones. Seven out of ten people under 30 years of age now experience symptoms of permanent hearing loss (National Foundation for the Deaf (NFD), 2007). Unlike earphones, which are placed over the ear, earbuds are placed directly in the ear canal, resulting in the sound being placed closer to the eardrum. Further, because the sound is digital, there is virtually no distortion, no matter how loud the volume. And probably most significantly, because digital music players can hold thousands of songs and play for hours without recharging, users tend to listen continuously for hours at a time. Hearing loss occurs slowly and often goes unnoticed until it is quite extensive, so early prevention is the key.
One method to decide how much noise is too much is the concept of a ‘noise dose’ which refers to the relationship between the level of noise and the time of exposure. To maintain a safe level of hearing you need to halve the time of exposure for every increase of 3 dB of noise level above 85 dB. The risk of hearing loss also increases as sound is played louder and for longer duration (Melbourne Audiology Centre, 2010). Many experts suggest that digital music players be designed either to prevent playing of music above 85 dB or to be limited to a maximum volume of 100 dB. In the meantime you need to counsel users to turn down the volume or take regular breaks from long-term listening (NFD, 2007).
Other ways to avoid hearing loss include using larger headphones that rest over the ear opening or noise-cancelling headphones that eliminate background noise so that listeners do not have to increase the volume so high. It is often difficult to explain this to people who abound with youthful optimism and tend not to worry about future damage. However, listening with earbuds boosts sound signals.
An increase of 10 dB increases the impact of the sound tenfold. Sound at 70 dB transmits 1000 times as much energy as sound at 40 dB. Normal conversation takes place at about 60 dB, whereas a chainsaw typically records at 100 dB and a rock concert at 110 dB (Better Hearing Australia, 2010).
Although we know not to look into the sun because its intense rays will do damage to our eyes, we do not seem to realise that blasting our ears with increased sound intensity is going to do damage, too; hence the irony when adolescents and adults don sunglasses and earbuds.
Better Hearing Australia, 2010: Noise and hearing loss. Available at www.betterhearingsydney.org.au/content/view/46/53/
Melbourne Audiology Centre, 2010: Noise induced hearing loss. Available at www.melbourneaudiologycentre.com.au/noiseinduce.html
National Foundation for the Deaf Inc, 2007: Music lovers face hearing loss time bomb (media release). Available at www.nfd.org.nz/
DOCUMENTATION AND CRITICAL THINKING
FOCUSED ASSESSMENT: CLINICAL CASE STUDY 1
Matthew W is a 4-year old child who was brought into the local health clinic by his mother after he had been crying for most of the night and was difficult to settle. The only sleep the child had was when he was held upright against his mother’s chest, but he slept for short periods only. The child feels warm to touch.
History: Matthew is the second child born to Mr and Mrs W. He was born at term. The pregnancy, labour and delivery were all uncomplicated. Matthew is up to date with all childhood immunisations and has no significant medical history to speak of.
Social history: Matthew and his parents live in a small two-bedroom house approximately 40 kilometres north of the central business district. He shares a bedroom with his older sister who is aged 6 years. Matthew’s father works at the local council undertaking park and garden maintenance and Matthew’s mother works as a receptionist in a community centre. The children are cared for by their maternal grandmother. The grandmother also cares for two other grandchildren every day. Both parents and Matthew’s grandmother smoke up to ten cigarettes each per day.
Subjective
Yesterday Matthew’s grandmother put him to bed for his afternoon nap. He did not sleep very long before he awoke crying and clearly tugging at his right ear. He would have a small drink but refused to eat solid food. His mother measured his temperature later in the day when she had taken him home. Matthew’s temperature was measured at 38°C tympanically. Matthew has been fussing and crying most of the night. His mother has not tried to give him any medication.
Objective
Vital signs: T 38.4°C (tympanic), P 100, R 20.
General: Alert, developmentally appropriate for age.
Skin: Warm and dry, no rashes or lesions.
Eyes: No exudate, conjunctivae clear, sclerae white.
Ears: Right tympanic membrane dull red and bulging, no light reflex. Left tympanic membrane has a normal appearance.
Mouth/throat: Oral mucosa pink, no lesions or exudate, tonsils 1+.
Neck: Supple, no lymphadenopathy.
Heart: Regular rate and rhythm.
Lungs: Breath sounds clear and equal bilaterally, unlaboured.
FOCUSED ASSESSMENT: CLINICAL CASE STUDY 2
Sam W, an 18-year-old university student, is a state and national swimmer who presents to his student health centre with tenderness and inflammation of the left outer ear and itchy ears for the last 2 weeks.
Objective
Vital signs: T 37°C oral, P 88, BP 120/70.
Ears: R ear, canal, TM normal. L ear—red and swollen pinna with purulent discharge. Painful movement of the tragus.
Neck: R anterior cervical node enlarged, firm, movable, tender. All others not palpable.
Access Economics, 2006: Listen hear! The economic impact and cost of hearing loss in Australia. Available at http://www.access economics.com.au/publicationsreports/reports.php.
Accident Compensation Corporation (ACC). 2010: Hearing loss epidemic anticipated in young New Zealand generation. Available at www.hear-it.org/page.dsp?page=5656.
Australian Hearing. Hearing loss in Australia. In Australian Hearing Annual Report. Available at http://www.hearing.com.au/dev/digitalAssets/9643_1256687692174_9619_1256610992838_AH-AR-2009-part1.pdf.
Baker J, Nursing management: acute intracranial problems. Brown D, Edwards H. Lewis’s medical–surgical nursing, 2nd edn., Marrickville: Mosby Elsevier, 2008.
Better Health Channel. 2010: Ear problems in children (fact sheet). Available at http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Ear_problems_in_children?open.
Better Hearing Australia, 2010: Noise and hearing loss. Available at www.betterhearingsydney.org.au/content/view/46/53/.
Brown S. Health and illness in older adults. Frenchs Forest: Pearson Education Australia, 2007.
Coates H, Morris P, Leach A, et al. Otitis media in Aboriginal children: tackling a major health problem. Medical Journal of Australia. 2002;177:177–178.
Commonwealth of Australia. The Senate Community Affairs References Committee: Hear us: inquiry into hearing health in Australia. Canberra: Commonwealth of Australia, Senate Printing Unit, 2010.
Daniel E. Noise and hearing loss: a review. Journal of School Health. 2007;77(5):225–231.
Del Mar C. Childhood otitis media i. general practitioner view. Available at http://www.australianprescriber.com/magazine/17/4/82/4/#, 2004.
Hear-it, 2010: New Zealand. Hearing problems picked up too late. Available at http://www.hear-it.org/page.dsp?page=3374.
Melbourne Audiology Centre. Noise induced hearing loss. Available at www.melbourneaudiologycentre.com.au/noiseinduce.html, 2010.
Morris P, Leach A. Managing otitis media: an evidence based approach. Australian Prescriber. 2009;32:155–159.
Morris P, Richmond P, Lehmann D, et al. New horizons: otitis media research in Australia. Medical Journal of Australia. 2009;191:S73–S77.
Morrison R. Otitis media (middle ear infection). Available at www.drmorrisonsays.com.au/child-otitis-media.html, 2010.
National Foundation for the Deaf Inc (NFD). 2007: Music lovers face hearing loss time bomb (media release). Available at www.nfd.org.nz/.
National Institute on Deafness and Other Communication Disorders (NIDCD). 2010: Ear infections in children. Available at www.nidcd.nih.gov/health/hearing/otitism.asp.
National Occupational Health and Safety Commission. National code of practice for noise management and protection of hearing at work, 3rd edn. Canberra: Australian Government, 2004.
O’Connor T, Perry C, Lannigan F. Complications of otitis media in indigenous and non-indigenous children. Medical Journal of Australia. 2009;191(9):S60–S64.
Pullar K. 2010: Under-diagnosed hearing loss in elderly. Available at www.hear-it.org/page.dsp?page=2690.
Sydney Children’s Hospital. Aboriginal otitis media (middle ear infection) (Fact sheet). Available at http://www.sch.edu.au/health/factsheets/joint/?otitis_media.htm, 2010.
Thorne P, Ameratunga S, Stewart J, et al. Epidemiology of noise-induced hearing loss in New Zealand. New Zealand Medical Journal. 2008;121:1280–1287.