Chapter Twenty-two Neurological system
INTRODUCTION
The head and neck are important structures to consider when assessing neurological function. These structures support and protect parts of the nervous system.
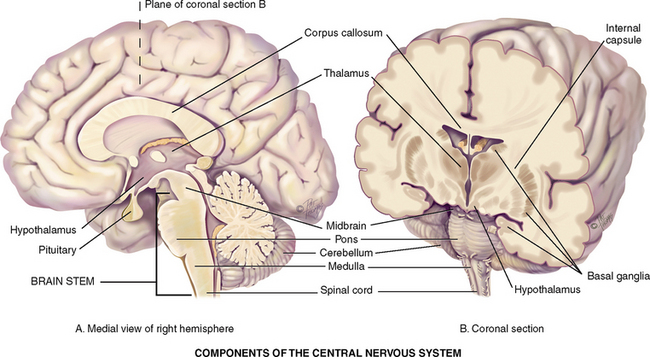
The nervous system can be divided into two parts—central and peripheral. The central nervous system (CNS) includes the brain and spinal cord. The peripheral nervous system (PNS) includes the 12 pairs of cranial nerves, the 31 pairs of spinal nerves and all their branches. The peripheral nervous system carries sensory (afferent) messages to the CNS from sensory receptors, motor (efferent) messages from the CNS out to muscles and glands, as well as autonomic messages that govern the internal organs and blood vessels. You may also need to review the structure and function related to the peripheral vascular system (Ch 11) as often neurological and vascular assessment is conducted concurrently. You will also need to review the structure and function of the visual pathways and visual fields, and visual light reflexes which are described in Chapter 23.
THE HEAD
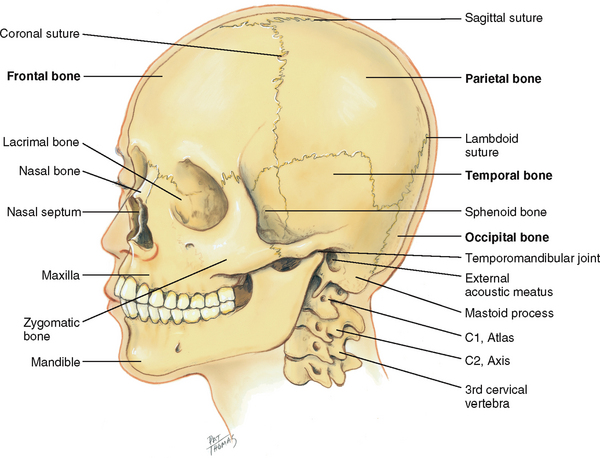
The skull is a rigid bony box that protects the brain and special sense organs, and it includes the bones of the cranium and the face (Fig 22.1). Note the location of these cranial bones: frontal, parietal, occipital and temporal. Use these names to describe any of your findings in the corresponding areas.
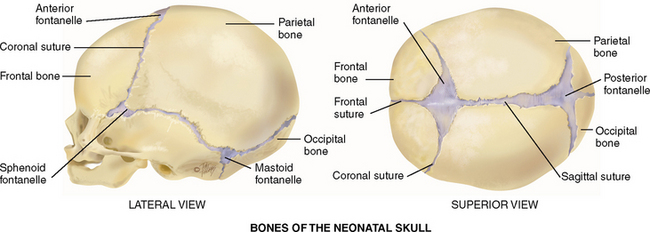
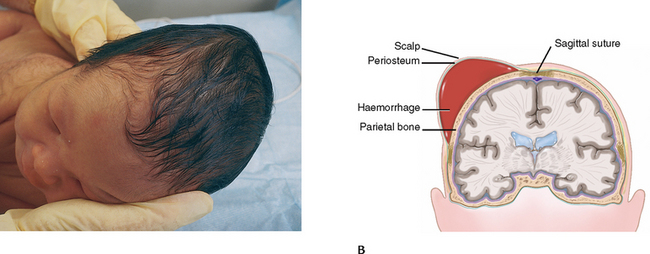
The adjacent cranial bones unite at meshed immovable joints called the sutures. The bones are not firmly joined at birth; this allows for the mobility and change in shape needed for the birth process. The sutures gradually ossify during early childhood. The coronal suture crowns the head from ear to ear at the union of the frontal and parietal bones. The sagittal suture separates the head lengthwise between the two parietal bones. The lambdoid suture separates the parietal bones crosswise from the occipital bone.
The 14 facial bones also articulate at sutures (note the nasal bone, zygomatic bone and maxilla), except for the mandible (the lower jaw). It moves up, down and sideways from the temporomandibular joint, which is anterior to each ear.
The cranium is supported by the cervical vertebra: C1, the ‘atlas’; C2, the ‘axis’; and down to C7. The C7 vertebra has a long spinous process that is palpable when the head is flexed. Feel this useful landmark, the vertebra prominens, on your own neck.
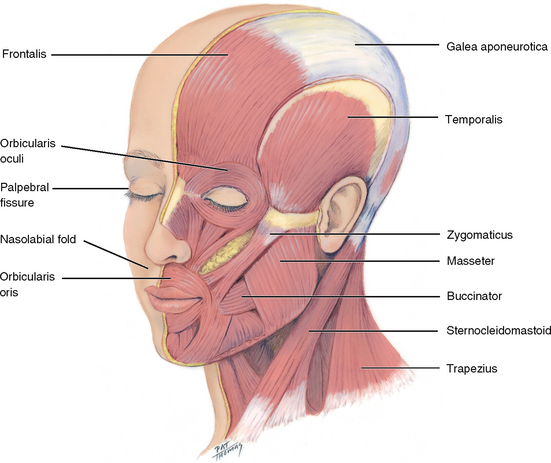
The human face has myriad appearances and a large array of facial expressions that reflect mood. The expressions are formed by the facial muscles (Fig 22.2), which are mediated by cranial nerve VII, the facial nerve. Facial muscle function is symmetrical bilaterally, except for an occasional quirk or wry expression.
Facial structures also are symmetrical; the eyebrows, eyes, ears, nose and mouth appear about the same on both sides. The palpebral fissures—the openings between the eyelids—are equal bilaterally. Also, the nasolabial folds, the creases extending from the nose to each corner of the mouth, should look symmetric. Facial sensations of pain or touch are mediated by the three sensory branches of cranial nerve V, the trigeminal nerve.
THE NECK
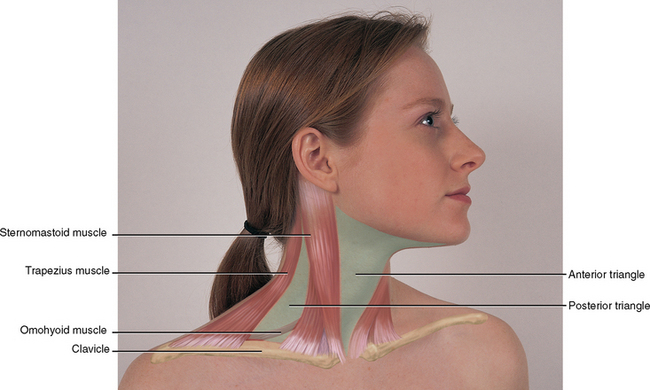
The neck is delimited by the base of the skull and inferior border of the mandible above, and by the manubrium sterni, the clavicle, the first rib and the first thoracic vertebra below. Think of the neck as a conduit for the passage of many structures, which are lying in close proximity: vessels, muscles, nerves, lymphatics and viscera of the respiratory and digestive systems. Blood vessels include the common and internal carotid arteries and their associated veins. The internal carotid branches off the common carotid and runs inwards and upwards to supply the brain; the external carotid supplies the face, salivary glands and superficial temporal area. The carotid artery and internal jugular vein lie beneath the sternomastoid muscle. The external jugular vein runs diagonally across the sternomastoid muscle.
The major neck muscles are the sternocleidomastoid and the trapezius (Fig 22.3); they are innervated by cranial nerve XI, the spinal accessory. The sternocleidomastoid muscle arises from the sternum and the medial part of the clavicle and extends diagonally across the neck to the mastoid process behind the ear. It accomplishes head rotation and head flexion. The two trapezius muscles form a trapezoid shape on the upper back. Each arises from the occipital bone and the vertebrae and extends fanning out to the scapula and clavicle. The trapezius muscles move the shoulders and extend and turn the head.
The sternocleidomastoid muscle divides each side of the neck into two triangles. The anterior triangle lies in front, between the sternomastoid and the midline of the body, with its base up along the lower border of the mandible and its apex down at the suprasternal notch. The posterior triangle is behind the sternocleidomastoid muscle, with the trapezius muscle on the other side and with its base along the clavicle below. It contains the posterior belly of the omohyoid muscle. These triangles are helpful guidelines when describing findings in the neck.
THE CENTRAL NERVOUS SYSTEM
Cerebral cortex.
The cerebral cortex is the cerebrum’s outer layer of nerve cell bodies, which looks like ‘grey matter’ because it lacks myelin. Myelin is the white insulation on the axon that increases the conduction velocity of nerve impulses.
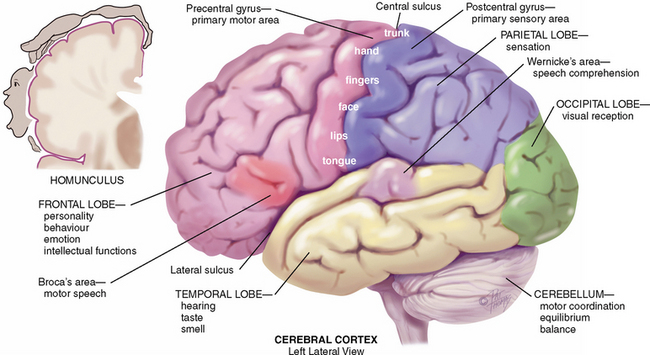
The cerebral cortex is the centre for humans’ highest functions, governing thought, memory, reasoning, sensation and voluntary movement (Fig 22.4). Each half of the cerebrum is a hemisphere; the left hemisphere is dominant in most (95%) people, including those who are left-handed.
Each hemisphere is divided into four lobes: frontal, parietal, temporal and occipital. The lobes have certain areas that mediate specific functions.
• The frontal lobe has areas concerned with reasoning, concentration, personality, behaviour, emotions and intellectual function.
• The precentral gyrus of the frontal lobe is the primary centre involved in voluntary contra lateral movement.
• The parietal lobe’s postcentral gyrus is the primary centre for the interpretation of contra lateral sensation. Additionally in the non-dominant hemisphere it is important in visual/proprioception, and in the dominant hemisphere it is important in calculation.
• The occipital lobe is the primary visual receptor centre, some visual reflexes and involuntary smooth eye movements.
• The temporal lobe behind the ear has the primary auditory reception centre, language function, learning and memory.
• Wernicke’s area in the temporal lobe is associated with language comprehension. When damaged in the person’s dominant hemisphere, receptive or Wernicke’s aphasia results. The person hears sound, but it has no meaning, like hearing a foreign language.
• Broca’s area (inferior part of the dominant frontal lobe) in the frontal lobe mediates motor speech. When injured in the dominant hemisphere the person may experience either expressive or Broca’s aphasia (cannot communicate at all) or expressive dysphasia (difficulty in communicating). The person can understand language and knows what they want to say, but cannot express what they want to say.
Damage to any of these specific cortical areas produces a corresponding loss of (usually contra lateral) function: motor weakness, paralysis, loss of sensation or impaired ability to understand and process language. Damage occurs when the highly specialised neurological cells are deprived of their blood supply, such as when a cerebral artery becomes occluded, or when vascular bleeding or vasospasm occurs.
Basal ganglia.
The basal ganglia are additional bands of grey matter buried deep within the two cerebral hemispheres that form the subcortical associated motor system (the extrapyramidal system) (Fig 22.5). They control automatic associated fine motor movements, for example, the arm swing alternating with the legs during walking. The basal ganglia also control some emotion and learning.
Thalamus.
The thalamus is the main relay station for the nervous system. Sensory pathways of the spinal cord and brainstem form synapses (sites of contact between two neurons) on their way to the cerebral cortex. As such, it is important in consciousness, pain perception and awareness.
Hypothalamus.
The hypothalamus is a major control centre with many vital functions: temperature, heart rate and blood pressure control, water metabolism, appetite, sleep centre, sexual arousal, anterior and posterior pituitary gland regulator and coordinator of autonomic nervous system activity and emotional status.
Cerebellum.
The cerebellum is a coiled structure located under the occipital lobe that is concerned with motor coordination of voluntary movements, equilibrium (i.e. the postural balance of the body) and muscle tone. It does not initiate movement but coordinates and smooths it, for example, the complex and quick coordination of many different muscles needed in playing the piano, swimming or juggling. It is like the ‘automatic pilot’ on an aeroplane in that it adjusts and corrects the voluntary movements, but operates entirely below the conscious level.
Brainstem.
The brainstem is the central core of the brain consisting of mostly nerve fibres. It has three areas:
1. Midbrain—the most anterior part of the brainstem that still has the basic tubular structure of the spinal cord. It merges into the thalamus and hypothalamus. It contains many motor neurons and tracts. Cranial nerves III and IV nuclei are located in the midbrain.
2. Pons—the enlarged area containing ascending and descending fibres tracts. Additionally, cranial nerves V through to VIII have nuclei in the pons.
3. Medulla—the continuation of the spinal cord in the brain that contains all ascending and descending fibre tracts connecting the brain and spinal cord. It has vital autonomic centres (respiration, heart, gastrointestinal function), as well as nuclei for cranial nerves IX through to XII. Pyramidal decussation (crossing of the motor fibres) occurs here (see below).
Spinal cord.
The spinal cord is the long cylindrical structure of nervous tissue with a circumference about as big as that of the little finger. It occupies the upper two-thirds of the vertebral canal from the medulla to lumbar vertebrae L1–L2. It is the main highway for ascending and descending fibre tracts that connect the brain to the spinal nerves, and it mediates reflexes. Its nerve cell bodies, or grey matter, are arranged in a butterfly shape with anterior and posterior ‘horns’.
Pathways of the CNS
Crossed representation is a notable feature of the nerve tracts: the left cerebral cortex receives sensory information from and controls motor function to the right side of the body, while the right cerebral cortex likewise interacts with the left side of the body. Knowledge of where the fibres cross the midline will help you interpret clinical findings.
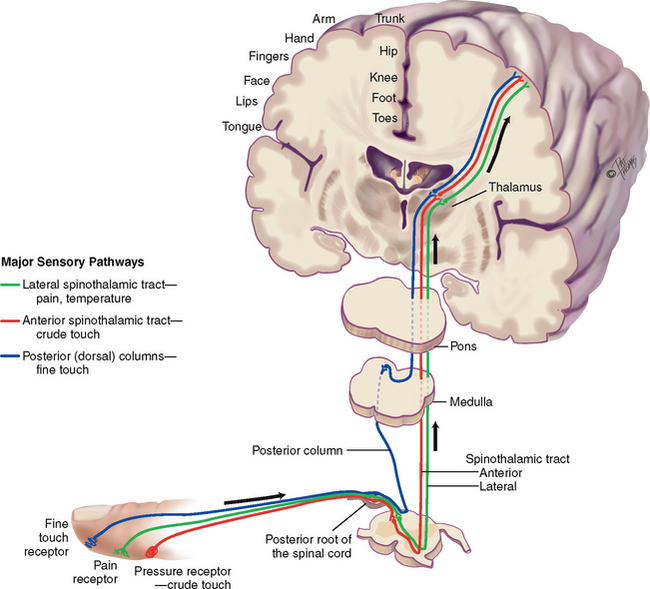
Sensory pathways
Millions of sensory receptors are embroidered into the skin, mucous membranes, muscles, tendons and viscera. They monitor conscious sensation, internal organ functions, body position and reflexes. Sensation travels in the afferent fibres in the peripheral nerve, then through the posterior (dorsal) root, then into the spinal cord. There, it may take one of two routes—the spinothalamic tract or the posterior (dorsal) columns (Fig 22.6).
Spinothalamic tract.
The spinothalamic tract contains sensory fibres that transmit the sensations of pain, temperature and crude or light touch (i.e. not precisely localised). The fibres enter the dorsal root of the spinal cord and synapse with a second sensory neuron. The second-order neuron fibres cross to the opposite side and ascend up the spinothalamic tract to the thalamus. Fibres carrying pain and temperature sensations ascend the lateral spinothalamic tract, whereas those of crude touch form the anterior spinothalamic tract. At the thalamus, the fibres synapse with a third sensory neuron, which carries the message to the sensory cortex for full interpretation.
Posterior (dorsal) columns.
These fibres conduct the sensations of position, vibration and finely localised touch.
• Position (proprioception)—without looking, you know where your body parts are in space and in relation to each other
• Vibration—feeling vibrating objects
• Finely localised touch (stereognosis)—without looking, you can identify familiar objects by touch.
These fibres enter the dorsal root and proceed immediately up the same side of the spinal cord to the brainstem. At the medulla, they synapse with a second sensory neuron and then cross. They travel to the thalamus, synapse again, and proceed to the sensory cortex, which localises the sensation and makes full discrimination.
The sensory cortex is arranged in a specific pattern forming a corresponding ‘map’ of the body (see the homunculus in Fig 22.4). Pain in the right hand is perceived at its specific spot on the left cortex map. Some organs are absent from the brain map, such as the heart, liver or spleen. You know you have one but you have no ‘felt image’ of it. Pain originating in these organs is referred, because no felt image exists in which to have pain. Pain is felt ‘by proxy’ by another body part that does have a felt image. For example, pain in the heart is referred to the chest, shoulder and left arm, which were its neighbours in fetal development. Pain originating in the spleen is felt on the top of the left shoulder.
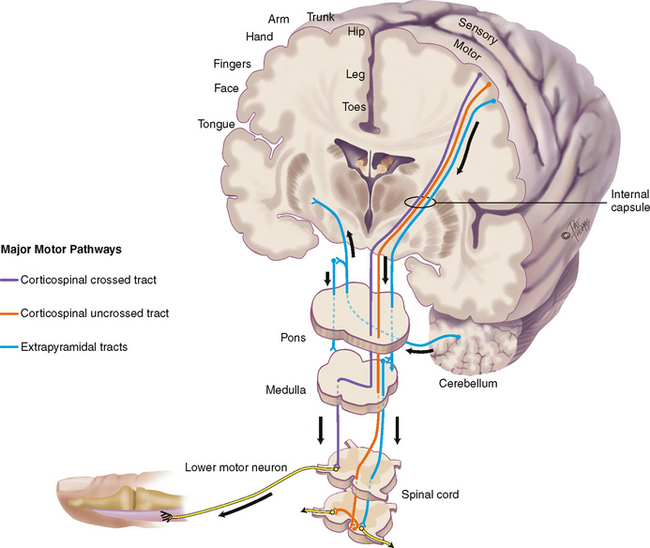
Motor pathways
Corticospinal or pyramidal tract.
(Fig 22.7) The area has been named ‘pyramidal’ because it originates in pyramidal-shaped cells in the motor cortex. Motor nerve fibres originate in the motor cortex and travel to the brainstem, where they cross to the opposite or contralateral side (pyramidal decussation) and then pass down in the lateral column of the spinal cord. At each cord level, they synapse with a lower motor neuron contained in the anterior horn of the spinal cord. Ten per cent of corticospinal fibres do not cross, and these descend in the anterior column of the spinal cord. Corticospinal fibres mediate voluntary movement, particularly very skilled, discrete, purposeful movements, such as writing.
The corticospinal tract is a newer, ‘higher’, motor system which humans have that permits very skilled and purposeful movements. The tract’s origin in the motor cortex is arranged in a specific pattern called somatotopic organisation. It is another body map, this one of a person, or homunculus, hanging ‘upside down’ (see Fig 22.1). Body parts are not equally represented on the map, and the homunculus looks distorted. To use political terms, it is more like an electoral map than a geographic map. That is, body parts whose movements are relatively more important to humans (e.g. the hand) occupy proportionally more space on the brain map.
Extrapyramidal tracts.
The extrapyramidal tracts include all the motor nerve fibres originating in the motor cortex, basal ganglia, brainstem and spinal cord that are outside the pyramidal tract. This is a phylogenetically older, ‘lower’, more primitive motor system. These subcortical motor fibres maintain muscle tone and control body movements, especially gross automatic movements, such as walking.
Cerebellar system.
This complex motor system coordinates movement, maintains equilibrium and helps maintain posture. The cerebellum receives information about the position of muscles and joints, the body’s equilibrium and what kind of motor messages are being sent from the cortex to the muscles. The information is integrated, and the cerebellum uses feedback pathways to exert its control back on the cortex or down to lower motor neurons in the spinal cord. This entire process occurs on a subconscious level.
Upper and lower motor neurons
Upper motor neurons are a complex of all the descending motor fibres that can influence or modify the lower motor neurons. Upper motor neurons are located completely within the CNS. The neurons convey impulses from motor areas of the cerebral cortex to the lower motor neurons in the anterior horn cells of the spinal cord. Examples of upper motor neurons are corticospinal, corticobulbar and extrapyramidal tracts. Examples of upper motor neuron diseases are cerebrovascular accident, cerebral palsy and multiple sclerosis.
Lower motor neurons are located mostly in the peripheral nervous system. The cell body of the lower motor neuron is located in the anterior grey column of the spinal cord, but the nerve fibres extend from here to the muscle. The lower motor neuron is the ‘final common pathway’, because it funnels many neural signals here and it provides the final direct contact with the muscles. Any movement must be translated into action by lower motor neuron fibres. Examples of lower motor neurons are cranial nerves and spinal nerves of the peripheral nervous system. Examples of lower motor neuron diseases are Bell’s palsy in cranial nerve lesions and in spinal cord lesions, poliomyelitis and amyotrophic lateral sclerosis.
THE PERIPHERAL NERVOUS SYSTEM
A nerve is a bundle of fibres outside the CNS. The peripheral nerves carry input to the CNS via their sensory afferent fibres and deliver output from the CNS via the efferent fibres.
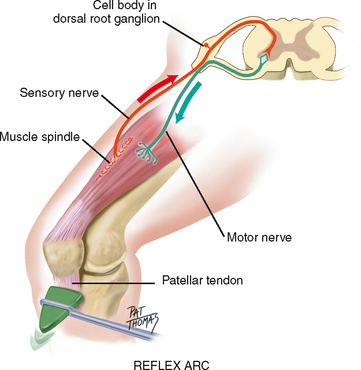
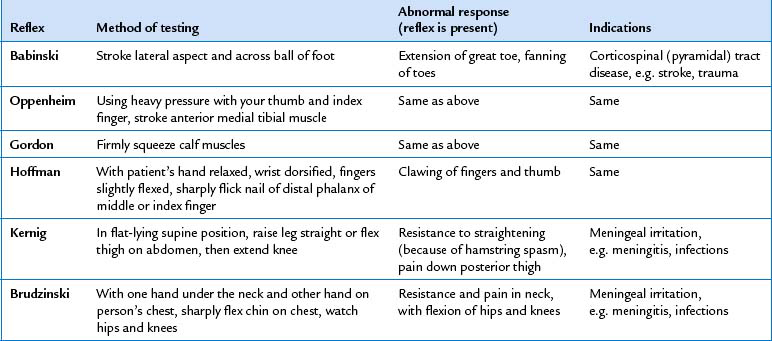
Reflex arc
Reflexes are basic defence mechanisms of the nervous system. They are involuntary, operating below the level of conscious control and permitting a quick reaction to potentially painful or damaging situations. Reflexes also help the body maintain balance and appropriate muscle tone. There are four types of reflexes: (1) deep tendon reflexes (myotatic), for example, patellar or knee jerk; (2) superficial, for example, corneal reflex, abdominal reflex; (3) visceral (organic), for example, pupillary response to light and accommodation; and (4) pathological (abnormal), for example, Babinski’s or extensor plantar reflex.
The fibres that mediate the reflex are carried by a specific spinal nerve. In the simplest reflex, tapping the tendon stretches the muscle spindles in the muscle, which activates the sensory afferent nerve. The sensory afferent fibres carry the message from the receptor and travel through the dorsal root into the spinal cord (Fig 22.8). They synapse directly in the cord with the motor neuron in the anterior horn. Motor efferent fibres leave via the ventral root and travel to the muscle, stimulating a sudden contraction.
The deep tendon (myotatic or stretch) reflex has five components: (1) an intact sensory nerve (afferent); (2) a functional synapse in the cord; (3) an intact motor nerve fibre (efferent); (4) the neuromuscular junction; and (5) a competent muscle.
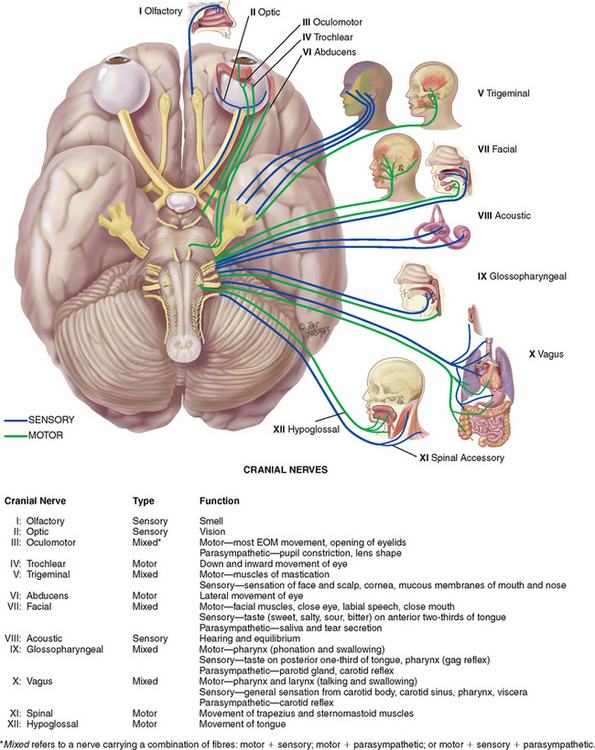
Cranial nerves
Cranial nerves enter and exit the brain rather than the spinal cord (Fig 22.9). Cranial nerves I and II extend from the cerebrum; cranial nerves III–XII extend from the lower diencephalon and brainstem. The 12 pairs of cranial nerves supply primarily the head and neck, except the vagus nerve (Lat. vagus, or wanderer, as in ‘vagabond’) which, apart from supplying some sensory (tympanic membrane, external auditory canal, external ear and pharynx) and motor function (muscles of the palate, pharynx and larynx), also travels to the heart, respiratory muscles, stomach and gallbladder.
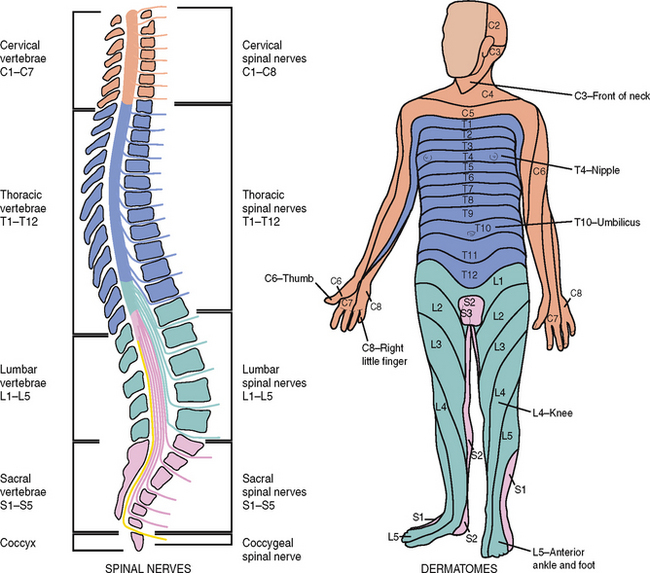
Spinal nerves
The 31 pairs of spinal nerves arise from the length of the spinal cord and supply the rest of the body. They are named for the region of the spine from which they exit: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 1 coccygeal. They are ‘mixed’ nerves because they contain both sensory and motor fibres. The nerves enter and exit the cord through roots—sensory afferent fibres through the posterior or dorsal roots, and motor efferent fibres through the anterior or ventral roots.
The nerves exit the spinal cord in an orderly ladder. Each nerve innervates a particular segment of the body. Dermal segmentation is the cutaneous distribution of the various spinal nerves.
A dermatome is a circumscribed skin area that is supplied mainly from one spinal cord segment through a particular spinal nerve (Fig 22.10). The dermatomes overlap, which is a form of biological insurance. That is, if one nerve is severed, most of the sensations can be transmitted by the one above and the one below. Do not attempt to memorise all dermatome segments; just focus on the following as useful landmarks:
Autonomic nervous system
The peripheral nervous system is composed of cranial nerves and spinal nerves. These nerves carry fibres that can be divided functionally into two parts—somatic and autonomic. The somatic fibres innervate the skeletal (voluntary) muscles; the autonomic fibres innervate smooth (involuntary) muscles, cardiac muscle and glands. The autonomic system mediates unconscious activity. Although a description of the autonomic system is beyond the scope of this book, its overall function is to maintain homeostasis of the body.
DEVELOPMENTAL CONSIDERATIONS
Infants and children
The bones of the neonatal skull are separated by sutures and by fontanelles, the spaces where the sutures intersect (Fig 22.11). These membrane-covered ‘soft spots’ allow for growth of the brain during the first year. They gradually ossify; the triangle-shaped posterior fontanelle is closed by 1 to 2 months, and the diamond-shaped anterior fontanelle closes between 9 months and 2 years.
During the fetal period, head growth predominates. Head size is greater than chest circumference at birth. The head size grows during childhood, reaching 90% of its final size when the child is 6 years old. But during infancy, trunk growth predominates so that head size changes in proportion to body height. Facial bones grow at varying rates, especially nasal and jaw bones. In the toddler the mandible and maxilla are small and the nasal bridge is low, so that the whole face seems small compared with the skull.
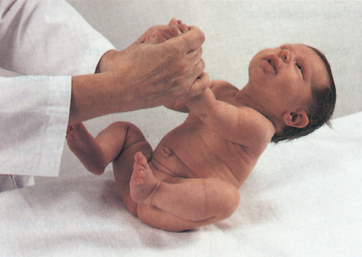
The neurological system is not completely developed at birth. Motor activity in the newborn is under the control of the spinal cord and medulla. Very little cortical control exists and the neurons are not yet myelinated. Movements are directed primarily by primitive reflexes. As the cerebral cortex develops during the first year, it inhibits these reflexes and they disappear at predictable times. Persistence of the primitive reflexes is an indication of CNS dysfunction.
The infant’s sensory and motor development proceeds along with the gradual acquisition of myelin, because myelin is needed to conduct most impulses. The process of myelinisation follows a cephalocaudal and proximodistal order (head, neck, trunk and extremities). This is just the order we observe the infant gaining motor control (lifts head, lifts head and shoulders, rolls over, moves whole arm, uses hands, walks). As the milestones are achieved, each is more complex and coordinated. Milestones occur in an orderly sequence, although the exact age of occurrence may vary.
Sensation is also rudimentary at birth. The newborn needs a strong stimulus and then responds by crying and with whole body movements. As myelinisation develops, the infant is able to localise the stimulus more precisely and to make a more accurate motor response.
Late adulthood (65+ years)
The facial bones and orbits appear more prominent, and the facial skin sags as a result of decreased elasticity, decreased subcutaneous fat and decreased moisture in the skin. The lower face may look smaller if teeth have been lost.
The ageing process causes a general atrophy with a steady loss of neurons in the brain and spinal cord. The loss of neurons causes a decrease in weight and volume of the brain (Raz et al, 2005). Neuron loss leads many people over 65 to show signs that, in the younger adult, would be considered abnormal, such as general loss of muscle bulk, loss of muscle tone in the face, in the neck and around the spine, decreased muscle strength, impaired fine coordination and agility, loss of vibratory sense at the ankle, decreased or absent Achilles reflex, loss of position sense at the big toe, pupillary miosis, irregular pupil shape and decreased pupillary reflexes.
The velocity of nerve conduction decreases between 5% and 10% with ageing, making the reaction time slower in some older persons. An increased delay at the synapse also occurs, so the impulse takes longer to travel. As a result, touch and pain sensation, taste and smell may be diminished.
The motor system may show a general slowing down of movement. Muscle strength and agility decrease. A generalised decrease occurs in muscle bulk, which is most apparent in the dorsal hand muscles. Muscle tremors may occur in the hands, head and jaw, along with possible repetitive facial grimacing (dyskinesias).
Ageing has a progressive decrease in cerebral blood flow and oxygen consumption. In some people this causes dizziness and a loss of balance with position change. These people need to be taught to get up slowly. Otherwise they have an increased risk for falls and resulting injuries. Additionally, older people may forget they fell, which makes it hard to diagnose the cause of the injury.
When they are in good health, ageing people walk about as well as they did during their middle and younger years, except more slowly and more deliberately. Some survey the ground for obstacles or uneven terrain. Some show a hesitation and a slightly wayward path.
CULTURAL AND SOCIAL CONSIDERATIONS
There are between 40 000 and 48 000 acute presentations and 9000 deaths related to stroke in Australia each year; this accounts for approximately 7% of all deaths (Begg et al, 2007) and in New Zealand, stroke accounts for about 9% of all deaths per year (New Zealand Ministry of Health, 1999). In 2003, it was estimated that over 346 700 Australians experienced a stroke at some time during their lives, with 146 400 suffering some form of disability as a direct result (Australian Institute of Health and Welfare (AIHW), 2006).
In Australia, Aboriginal and Torres Strait Islander people are more than twice as likely to suffer a stroke than the general population (AIHW and National Heart Foundation of Australia, 2004) This may also be related to modifiable determinants of health, which can compound these risks.
SUBJECTIVE DATA
Assessment of the neurological system is an important assessment area for nurses in a variety of healthcare settings. The extent of the questioning and examination will depend on the person’s main health concern. Subjective assessment of the neurological system investigates a variety of symptoms such as headache, dizziness, seizures, tremors, weakness, incoordination, numbness or tingling, dysphagia and dysphasia. Symptoms such as these can impact the individual’s safety and capacity to perform their activities of daily living. There may also be effects on the nutritional state of the person, their relationships and capacity to work. In addition, significant past history and environmental/occupational hazards are also explored. Neurological subjective assessment is performed in conjunction with assessment of the individual’s mental state, vision, hearing, ability to smell, taste, touch and position sense.
| Assessment guidelines | Clinical significance and clinical alerts |
|---|---|
1 Headache. Have you experienced any unusually frequent or severe headaches? • When did this start? How often does this occur? Gradual, over hours, or a day? Or, suddenly, over minutes, or less than 1 hour?
|
Clinical alert: if a person reports any sudden onset of headache of increasing severity they should be referred to a medical practitioner for further assessment. Tension headaches tend to be occipital, frontal or with band-like tightness; migraines (vascular) tend to be supraorbital, retro-orbital or frontotemporal; cluster headaches (vascular) produce pain around the eye, temple, forehead, cheek. Unilateral or bilateral (e.g. with cluster headaches pain is always unilateral and always on the same side of the head). Character is typically vice-like with tension headache, throbbing with migraine or temporal arteritis. |
Quantity is often severe with migraine, or excruciating with cluster headache. Migraines occur about two per month, each lasting 1 to 3 days; one to two cluster headaches occur per day, each lasting ½ to 2 hours for 1 or 2 months; then complete remission may last for months or years. Alcohol ingestion and daytime napping typically precipitate cluster headaches, whereas alcohol, letdown after stress, menstruation and eating chocolate or cheese precipitate migraines. |
|
| • Associated factors. Any relation to other symptoms: any nausea and vomiting? (Note which came first, headache or nausea.) Any vision changes, pain with bright lights, neck pain or stiffness, fever, weakness, moodiness, stomach problems? | Nausea, vomiting and visual disturbances are associated with migraines; eye reddening and tearing, eyelid drooping, rhinorrhoea and nasal congestion are associated with cluster headaches; anxiety and stress are associated with tension headaches; neck rigidity and fever are associated with meningitis or encephalitis. |
| • Do you have any other illness? | Hypertension, fever, hypothyroidism and vasculitis produce headaches. |
| • What makes it worse: movement, coughing, straining, exercise? | |
| Migraines are associated with family history of migraine | |
| • Effort to treat. What seems to help: going to sleep, medications, positions, rubbing the area? | With migraines, people lie down to feel better, whereas with cluster headaches they need to move—even to pace the floor—to feel better. |
| • Coping strategies. How have these headaches affected your self-care, or your ability to function at work, home and socially? | |
| 2 Neck pain. Any neck pain? | |
| Acute onset of stiffness with headache and fever occurs with meningeal inflammation. | |
| • Coping strategies. Able to do your work, to sleep? | Pain creates a vicious circle. Tension increases pain and disability, which produces more anxiety. |
| Refer to Chapter 10 for further discussion of pain assessment | |
In some circumstances you might be obtaining this information from another person if the patient is unable to respond or remember. Clinical alert: any change in conscious state should be referred to a medical practitioner. The presence of nausea, vomiting, drowsiness or confusion can indicate rising intracranial pressure and the person should be urgently referred to a medical practitioner for further assessment. |
|
| 6 Seizures. Have you ever had any seizures (sometimes referred to as convulsions or fits)? When did they start? How often do they occur? | Seizures occur with epilepsy, a paroxysmal disease characterised by altered or loss of consciousness, involuntary muscle movements and sensory disturbances. However, an isolated seizure does not mean the patient has epilepsy. |
• Motor activity: Where in your body do the seizures begin? Do the seizures travel through your body? On one side or both? Does your muscle tone seem tense or limp?
|
Aura is a subjective sensation that precedes a seizure; it could be auditory, visual or motor. |
| 8 Weakness. Do you experience any weakness or problem moving any part of the body? Is this generalised or local? Does weakness occur with any particular movement? (e.g. with proximal or large muscle weakness, it is hard to get up out of a chair or reach for an object; with distal or small muscle weakness, it is hard to open a jar, write, use scissors or walk without tripping.) | |
| 9 Lack of coordination. Do you experience any problem with coordination? Any problem with balance when walking? Do you lean to one side? Any falling? Which way? Do your legs seem to give way? Any clumsy movement? | Dysmetria is the inability to control range of motion of muscles. |
| 10 Numbness or tingling. Do you have any numbness or tingling in any part of the body? Does it feel like pins and needles? When did this start? Where do you feel it? Does it occur with activity? | |
| 11 Difficulty swallowing (dysphagia). Have you experienced a problem with swallowing? Does this occur with solids or liquids? Have you experienced excessive saliva, drooling? | Dysphagia is difficulty with swallowing. See Chapter 16 for further discussion of swallow assessment. Clinical alert: difficulty with swallowing can pose serious risk to a person’s airway and requires further detailed assessment. |
| 12 Difficulty speaking. Do you experience any problem speaking: for example, with forming words or with saying what you intended to say? When did you first notice this? How long did it last? | Dysarthria is difficulty forming words; dysphasia is difficulty with language comprehension or expression (see Table 22.3). |
| 13 Significant past history. Stroke, head injury, spinal cord injury, meningitis or encephalitis, degenerative neurological disease, congenital defect, mood-altering drug use or alcoholism? | |
| 14 Environmental/occupational hazards. Are you exposed to any environmental/occupational hazards: for example, insecticides, organic solvents, lead? | |
| Additional history for infants and children | |
| 3 Reflexes: What have you noticed about the baby’s behaviour? Do the baby’s sucking and swallowing seem coordinated? When you touch the cheek, does the baby turn their head towards the touch? Does the baby startle with a loud noise or shake of crib? Does the baby grasp your finger? | |
| 4 Does the child seem to have any problem with balance? Have you noted any unexplained falling, clumsy or unsteady gait, progressive muscular weakness, problem with going up or down stairs, problem with getting up from lying position? | |
| 5 Has this child had any seizures? Please describe. Did the seizure occur with a high fever? Did any loss of consciousness occur—how long? How many seizures occurred with this same illness (if occurred with high fever)? | Seizures may occur with high fever in infants and toddlers. Or seizures may be sign of neurological disease. |
| 6 Did this child’s motor or developmental milestones seem to come at about the right age? Does this child seem to be growing and maturing normally to you? How does this child’s development compare to siblings or to age mates? | |
| Chronically elevated lead levels may cause a developmental delay, a loss of a newly acquired skill or no clinical signs may be present. | |
| Additional history for the adult over 65 years | |
1 Do you experience any problem with dizziness? Does this occur when you first sit or stand up, when you move your head, when you get up and walk just after eating? Does this occur with any of your medications? |
Diminished cerebral blood flow and diminished vestibular response may produce staggering with position change, which increases risk of falls. |
| 2 Have you noticed any decrease in memory, change in mental function? Have you felt any confusion? Did this seem to come on suddenly or gradually? | Micturition syncope is a temporary loss of consciousness while urinating and is thought to be caused by a sudden positional drop in blood pressure. |
| 3 Have you ever noticed any tremor? Is this in your hands or face? Is this worse with: anxiety, activity, rest? Does the tremor seem to be relieved with: alcohol, activity, rest? Does the tremor interfere with daily or social activities? | Senile tremor is relieved by alcohol, although this is not a recommended treatment. Assess if the person is abusing alcohol in effort to relieve tremor. |
| 4 Have you ever had any sudden vision change, fleeting blindness? Did this occur along with weakness? Did you have any loss of consciousness? | Clinical alert: these symptoms can be characteristic of decreased blood flow to the brain and require more detailed medical investigation. |
OBJECTIVE DATA
There are three main types of objective neurological examinations—ongoing neurological observations, a screening examination and a complete examination.
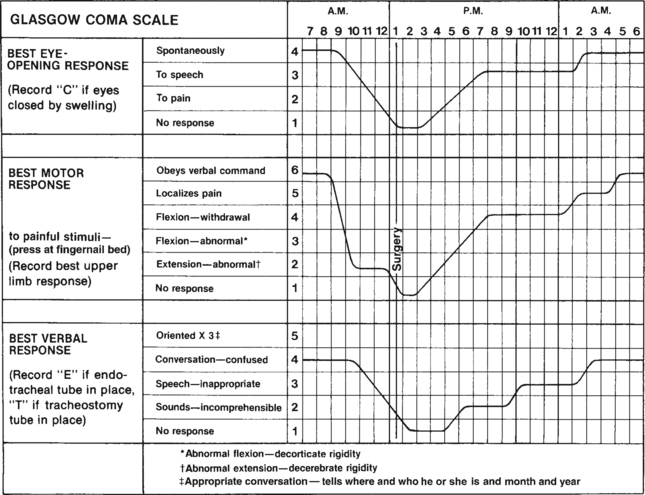
The most common objective neurological assessment performed by nurses is ongoing neurological observations. This type of assessment is conducted on persons with demonstrated neurological deficits who require periodic or ongoing assessments. Most hospitals have specific charts to guide you in this assessment and for ease in recording the data. The assessment data is presented in graphic form and usually includes the Glasgow Coma Scale (see Fig 22.12), pupillary response and vital signs.
You would perform a screening neurological examination (items identified in following sections) on seemingly well persons who have no significant subjective findings from the history.
You would perform a complete neurological examination on persons who have neurological symptoms (e.g. headache, weakness, loss of coordination) or who have shown signs of neurological dysfunction. The screening and complete neurological examination sequence is described in the advanced practice section below.
| Preparation | Equipment needed |
|---|---|
| People who have recent head trauma, neurological surgery, stroke or a neurological deficit due to a systemic disease process must be monitored closely for any improvement or deterioration in neurological status and for any indication of increasing intracranial pressure. Signs of increasing intracranial pressure signal impending cerebral disaster and potential death and require early and prompt intervention. |
| Procedures and normal findings | Abnormal findings and clinical alerts |
| ONGOING NEUROLOGICAL OBSERVATIONS | |
You need to consider whether you also need to conduct a mental status assessment as part of the ongoing neurological observations (neuro obs) (see Ch 21 for details). Level of consciousness. A change in the level of consciousness is the single most important factor in this examination. It is the earliest and most sensitive index of change in neurological status. Note the ease of arousal and the state of awareness, or orientation. Assess orientation by asking questions about: • Person—own name, occupation, names of workers around the person, their occupations |
A change in consciousness may be subtle. Note any decreasing level of consciousness, disorientation, memory loss, uncooperative behaviour or even complacency in a previously combative person. |
Vary the questions during repeat assessments so that the person is not merely memorising answers. Note the quality and the content of the verbal response; articulation, fluency, manner of thinking; and any deficit in language comprehension or production (see Ch 6). If the person cannot speak, you will have to ask questions that require a nod or shake of the head, ‘Are we in a hospital?’ ‘Are you at home?’ ‘Are we in… (city)?’ |
If the person can not speak fluent English or if English is not their first language you may need to get the assistance of a qualified interpreter to ensure accuracy in the assessment. |
| Refer to Table 22.2 | |
| 1 Name called | |
| 2 Light touch on person’s arm | |
| 3 Vigorous shake of shoulder | |
| 4 Pain applied (pressure to nail bed, pinch trapezius muscle, rub your knuckles on the person’s sternum). | Be careful not to inflict trauma/bruising on the person. If the person is not responding there is no point in repeatedly continuing to inflict pain. Note your findings and report any changed findings. |
| Record the stimulus used as well as the person’s response to it. | |
| Motor function. Check the voluntary movement of each extremity by giving the person specific commands. (This procedure also tests level of consciousness by noting the person’s ability to follow commands.) | |
Ask the person to lift the eyebrows, frown and bare teeth. Note symmetric facial movements and bilateral nasolabial folds (cranial nerve VII). You can check upper arm strength by checking hand grasps. Ask the person to squeeze your fingers. Offer your two fingers, one on top of the other, so that a strong hand grasp does not hurt your knuckles (Fig 22.13). Do not place fingers in the palm of the person’s hand as some people with diffuse brain damage, especially frontal lobe injury, have a grasp that is a reflex only. |
Asymmetrical movement, inability to follow instructions, no movement. Unequal grasp. |
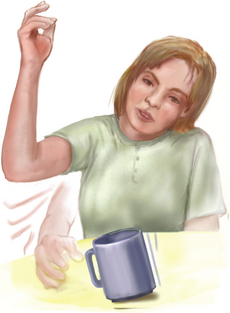
| Alternatively, ask the person to lift each hand or to hold up one finger. You can also check upper extremity strength by palmar drift. Ask the person to extend both arms forwards or halfway up, palms up, eyes closed and hold for 10 to 20 seconds (Fig 22.14). Normally, the arms stay steady with no downward drift. | |
| Check lower extremities by asking the person to do straight leg raises. Ask the person to lift one leg at a time straight up off the bed (Fig 22.15). Full strength allows the leg to be lifted 90 degrees. If multiple trauma, pain or equipment exclude this motion, ask the person to push one foot at a time against your hand’s resistance, ‘like putting your foot on the accelerator pedal of your car’ (Fig 22.16). | |
| For the person with decreased level of consciousness, note if movement occurs spontaneously and as a result of noxious stimuli such as pain or suctioning. An attempt to push away your hand after such stimuli is called localising and is characterised as purposeful movement. | Any abnormal posturing, decorticate rigidity or decerebrate rigidity indicates diffuse brain injury (see Table 22.11). |
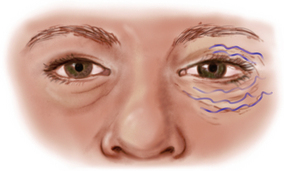
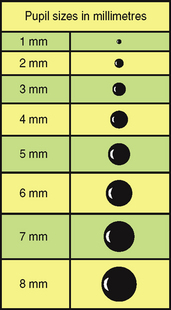
Pupillary response. Note the size, shape and symmetry of both pupils. Shine a fine light beam (from a penlight torch) into each pupil and note the direct and consensual light reflex. Both pupils should constrict briskly. (Allow for the effects of any medication that could affect pupil size and reactivity.) |
Increasing intracranial pressure causes a sudden, unilateral, dilated and nonreactive pupil. Cranial nerve III runs parallel to the brain stem. When increasing intra cranial pressure pushes the brain stem down (uncal herniation), it puts pressure on cranial nerve III, causing pupil dilatation. Clinical alert: report this finding immediately to medical officer. You should continue to perform ongoing neurological observations. |
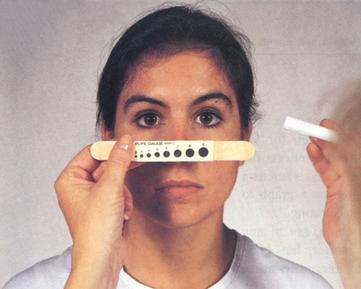
| In the acute care setting, gauge the pupil size in millimetres, both before and after the light reflex. Normally, the resting size is 3, 4 or 5 mm and decreases equally in response to light (Fig 22.17). This indicates that both pupils measure 3 mm in the resting state and that both constrict to 1 mm in response to light. A graduated scale printed on a handheld vision screener or taped onto a tongue blade facilitates your measurement (Fig 23.18). | Recording the pupil size in millimetres is more accurate when many nurses and physicians care for the same person or when small changes may be significant signs of increasing intracranial pressure. Clinical documentation: Record the normal response to all these manoeuvres as PERRL, or Pupils Equal, Round, React to Light. |
| To test the pupillary light reflex, darken the room and ask the person to gaze into the distance. (This dilates the pupils.) Advance a light in from the side and note the response. Normally you will see (1) constriction of the same-sided pupil (a direct light reflex) and (2) simultaneous constriction of the other pupil (a consensual light reflex). | Unequal, slowed response. |
| Vital signs. Measure the temperature, pulse, respiration and blood pressure as often as the person’s condition warrants. Although they are vital to the overall assessment of the critically ill person, pulse and blood pressure are notoriously unreliable parameters of CNS deficit. Any changes are late consequences of rising intracranial pressure. Vital signs should always be performed after neurological assessment as the act of performing these activities elicits a painful response to eye opening rather than to name. | The Cushing reflex shows signs of increasing intracranial pressure: blood pressure–sudden elevation with widening pulse pressure; pulse–decreased rate, slow and bounding. This requires urgent medical referral. |
| USING THE GLASGOW COMA SCALE | |
| Since the terms describing levels of consciousness are ambiguous, the Glasgow Coma Scale (GCS) was developed as an accurate and reliable quantitative tool (see Fig 22.12). The GCS is a standardised, objective assessment that defines the level of consciousness by giving it a numeric value. | Where possible have one nurse conduct the assessments over a shift time frame. This will increase the reliability of the data over time. Before handing over to the next shift nurse take the time to conduct the test together to increase the reliability of the data between the two nurses. |
The scale is divided into three areas: verbal response, eye opening and motor response. Each area is rated separately, and a number is given for the person’s best response. The three numbers are added; the total score reflects the brain’s functional level. A fully alert, normal person has a score of 15, whereas a score of 7 or less reflects coma. Serial assessments can be plotted on a graph to illustrate visually whether the person is stable, improving or deteriorating. The GCS assesses the functional state of the brain as a whole, not of any particular site in the brain. The scale is easy to learn and master, has good interrater reliability (Juarez and Lyons, 1995) and enhances interprofessional communication by providing a common language. |
Clinical alert: Any downward trend in the GCS score should be urgently reported to a medical practitioner. |
Best eye opening response: Note the person’s ability to open their eyes spontaneously. If the person is not opening their eyes spontaneously ask them to open their eyes (record if they open their eyes to speech). If they do not open their eyes to speech apply painful stimuli as described above (start with light touch and increase as necessary). If they do not open their eyes to painful stimuli record no response. Best motor response: Check the voluntary movement of each extremity by giving the person specific commands. (This procedure also tests level of consciousness by noting the person’s ability to follow commands.) Follow the instructions detailed above. Best verbal response: Check the person’s orientation to person, place, time (follow the instructions detailed above). Assess clarity and appropriateness of words/speech or note if there is no verbal response. If the person is unable to speak due to an endotracheal tube or tracheostomy tube, record this on the chart. |
FURTHER OBJECTIVE ASSESSMENT FOR ADVANCED PRACTICE
The assessments described in the following sections require advanced skill and scope of practice. Nurses working in specialist settings need to develop these skills.
TABLE 22.6 Abnormalities in muscle movement
| Preparation | Equipment needed |
|---|---|
| Procedures and normal findings | Abnormal findings and clinical alerts |
| INSPECT HEAD, FACE AND NECK | |
| Inspect and palpate the skull | |
| Size and shape | |
| Note the general size and shape. Normocephalic is the term that denotes a round symmetrical skull that is appropriately related to body size. Be aware that ‘normal’ includes a wide range of sizes. | Deformities: microcephaly, abnormally small head; macrocephaly, abnormally large head (hydrocephaly, acromegaly, Paget’s disease). |
| To assess shape, place your fingers in the person’s hair and palpate the scalp. The skull normally feels symmetrical and smooth. The cranial bones that have normal protrusions are the forehead, the lateral edge of each parietal bone, the occipital bone and the mastoid process behind each ear. There is no tenderness to palpation. | Note lumps, depressions or abnormal protrusions. |
| Temporal area | |
| Palpate the temporal artery above the zygomatic (cheek) bone between the eye and top of the ear. | The artery looks more tortuous and feels hardened and tender with temporal arteritis. |
| The temporomandibular joint is just below the temporal artery and anterior to the tragus. Palpate the joint as the person opens the mouth and note normally smooth movement with no limitation or tenderness. | Crepitation, limited range of motion or tenderness. |
| Inspect the face | |
| Facial structures | |
| Inspect the face, noting the facial expression and its appropriateness to behaviour or reported mood. Anxiety is common in the hospitalised or ill person. | |
| Although the shape of facial structures may vary somewhat among races, they should always be symmetrical. Note symmetry of eyebrows, palpebral fissures, nasolabial folds and sides of the mouth. | Marked asymmetry with central brain lesion (e.g. cerebrovascular accident) or with peripheral cranial nerve VII damage (Bell’s palsy). See Table 22.14 |
| Note any abnormal facial structures (coarse facial features, exophthalmos, changes in skin colour or pigmentation) or any abnormal swelling. Also note any involuntary movements (tics) in the facial muscles. Normally none occur. | |
| Inspect and palpate the neck | |
| Symmetry | |
| Head position is centred in the midline, and the accessory neck muscles should be symmetrical. The head should be held erect and still. | |
| Range of motion (ROM) | |
| Note any limitation of movement during active motion. Ask the person to touch the chin to the chest, turn the head to the right and left, try to touch each ear to the shoulder (without elevating shoulders) and to extend the head backwards. When the neck is supple, motion is smooth and controlled. | |
| Test muscle strength and the status of cranial nerve XI by trying to resist the person’s movements with your hands as the person shrugs the shoulders and turns the head to each side. | |
As the person moves the head, note enlargement of the salivary glands and lymph glands. Normally no enlargement is present. Note a swollen parotid gland when the head is extended; look for swelling below the angle of the jaw. Also, note thyroid gland enlargement. Normally none is present. Also note any obvious pulsations. The carotid artery runs medial to the sternomastoid muscle, and it creates a brisk localised pulsation just below the angle of the jaw. Normally, there are no other pulsations while the person is in the sitting position (see Ch 12). |
Thyroid enlargement may be a unilateral lump, or it may be diffuse and look like a doughnut lying across the lower neck (see Table 16.7). |
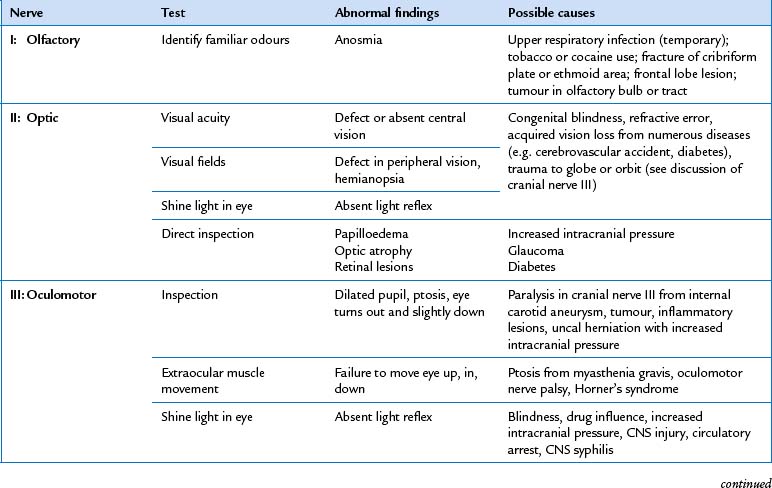
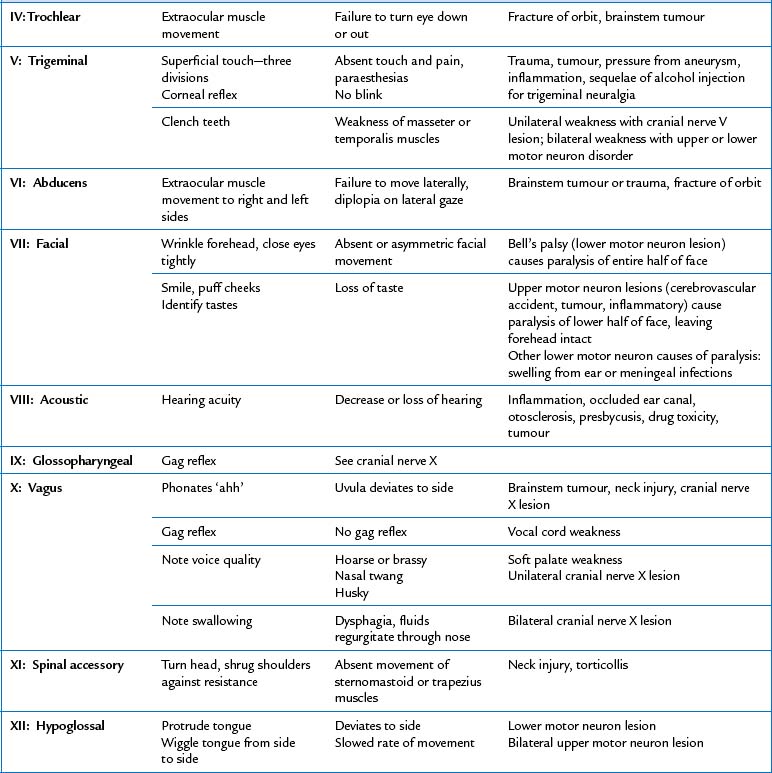
| TEST CRANIAL NERVES | |
| Cranial nerve I–olfactory nerve | |
| Do not test routinely. Test the sense of smell in those who report loss of smell, those with head trauma and those with abnormal mental status, and when the presence of an intracranial lesion is suspected. First, assess patency by occluding one nostril at a time and asking the person to sniff. Then, with the person’s eyes closed, occlude one nostril and present an aromatic substance. Use familiar, conveniently obtainable and non-noxious smells, such as coffee, toothpaste, orange, vanilla, soap or peppermint. Alcohol wipes smell familiar and are easy to find but are irritating. | |
| Normally, a person can identify an odour on each side of the nose. Smell is normally decreased bilaterally with ageing. Any asymmetry in the sense of smell is important. | Unilateral loss of smell in the absence of nasal disease is neurogenic anosmia (see Table 22.4). |
| Cranial nerve II–optic nerve | |
| Test visual acuity and test visual fields by confrontation (see Ch 23). | Visual field loss (see Table 23.5). |
| Using the ophthalmoscope, examine the ocular fundus to determine the colour, size and shape of the optic disc (see Ch 23). | Papilloedema with increased intracranial pressure; optic atrophy (see Table 23.9). |
| Cranial nerves III, IV and VI–oculomotor, trochlear and abducens nerves | |
| Palpebral fissures are usually equal in width or nearly so (see Fig 23.1). | Ptosis (drooping) occurs with myasthenia gravis, dysfunction of cranial nerve III or Horner’s syndrome (see Table 23.2). |
| Check pupils for size, regularity, equality, direct and consensual light reaction and accommodation (see above and Ch 23). | |
Assess extraocular movements by the cardinal positions of gaze (see Ch 23). Nystagmus is a back-and-forth oscillation of the eyes. End-point nystagmus, a few beats of horizontal nystagmus at extreme lateral gaze, occurs normally. Assess any other nystagmus carefully, noting: • Presence of abnormal movement in one or both eyes. • Pendular movement (oscillations move equally left to right) or jerk (a quick phase in one direction, then a slow phase in the other). Classify the jerk nystagmus in the direction of the quick phase. • Amplitude. Judge whether the degree of movement is fine, medium or coarse. • Frequency. Is it constant, or does it fade after a few beats? • Plane of movement: Horizontal, vertical, rotary or a combination? |
Strabismus (deviated gaze) or limited movement (see Table 23.1). Nystagmus occurs with disease of the vestibular system, cerebellum or brainstem. Nystagmus leads to low vision: symptoms include: blurred vision and a reduction in depth perception which may put the person at risk of injury, falls or an inability to manage their activities of daily living. |
| Cranial nerve V–trigeminal nerve | |
| Motor function. Assess the muscles of mastication by palpating the temporal and masseter muscles as the person clenches the teeth (Fig 22.19). Muscles should feel equally strong on both sides. Next, try to separate the jaws by pushing down on the chin; normally you cannot. | |
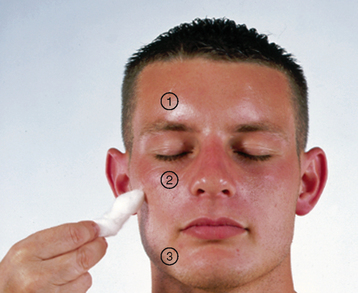
| Sensory function. With the person’s eyes closed, test light touch sensation by touching a cotton wisp to these designated areas on person’s face: forehead, cheeks and chin (Fig 22.20). Ask the person to say ‘Now’, whenever the touch is felt. This tests all three divisions of the nerve: (1) ophthalmic, (2) maxillary and (3) mandibular. | Decreased or unequal sensation. |
| Corneal reflex. Remove any contact lenses. With the person looking forwards, bring a wisp of cotton in from the side (to minimise defensive blinking) and lightly touch the cornea, not the conjunctiva (Fig 22.21). Normally, the person will blink bilaterally. The corneal reflex may be decreased or absent in those who have worn contact lenses. This procedure tests the sensory afferent in cranial nerve V and the motor efferent in cranial nerve VII (muscles that close the eye). Omit this test, unless the person has abnormal facial sensation or abnormalities of facial movement. | |
| Cranial nerve VII–facial nerve | |
| Motor function. Note mobility and facial symmetry as the person responds to these requests: smile (Fig 22.22), frown, close eyes tightly (against your attempt to open them), lift eyebrows, show teeth and puff cheeks (Fig 22.23). Then, press the person’s puffed cheeks in, and note that the air should escape equally from both sides. | Muscle weakness is shown by flattening of the nasolabial fold, drooping of one side of the face, lower eyelid sagging and escape of air from only one cheek that is pressed in. Loss of movement and asymmetry of movement occur with both central nervous system lesions (e.g. stroke that affects the lower face on one side) and peripheral nervous system lesions (e.g. Bell’s palsy that affects the upper and lower face on one side). Clinical alert: facial nerve weakness can result in difficulty in chewing food and control of saliva in the mouth. |
| Sensory function. Do not test routinely. Test only when you suspect facial nerve injury. When indicated, test sense of taste by applying to the tongue a cotton applicator covered with a solution of sugar, salt or lemon juice (sour). Ask the person to identify the taste. | |
| Cranial nerve VIII–acoustic (vestibulocochlear) nerve | |
| Test hearing acuity by assessing the person’s ability to hear normal conversation: by the whispered voice test, and by Weber and Rinne tuning fork tests (see Ch 24). | |
| Cranial nerves IX and X–glossopharyngeal and vagus nerves | |
| Motor function. Depress the tongue with a tongue blade, and note pharyngeal movement as the person says ‘ahhh’ or yawns; the uvula and soft palate should rise in the midline, and the tonsillar pillars should move medially. | |
If motor function abnormalities are detected or the person reports swallowing difficulties, touch the posterior pharyngeal wall with a tongue blade and note the gag reflex. Also note that the voice sounds smooth and not strained. Sensory function. Cranial nerve IX does mediate taste on the posterior one-third of the tongue, but technically this sensation is too difficult to test. |
|
| Cranial nerve XI–spinal accessory nerve | |
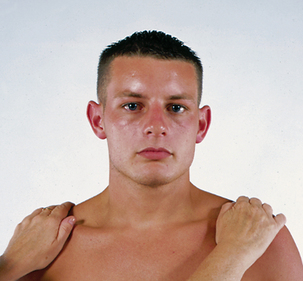
| Examine the sternomastoid and trapezius muscles for equal size. Check equal strength by asking the person to rotate the head forcibly against resistance applied to the side of the chin (Fig 22.24). Then ask the person to shrug the shoulders against resistance (Fig 22.25). These movements should feel equally strong on both sides. | |
| Cranial nerve XII–hypoglossal nerve | |
| Inspect the tongue. No wasting or tremors should be present. Note the forward thrust in the midline as the person protrudes the tongue. Also ask the person to say ‘light, tight, dynamite’, and note that lingual speech (sounds of letters l, t, d, n) is clear and distinct. | |
| INSPECT AND PALPATE THE MOTOR SYSTEM | |
| Clinical alert: abnormalities in muscle strength, coordination and balance can impact on the person’s ability to manage activities of daily living and pose an injury risk such as falling. | |
| Muscles | |
| Size. As you proceed through the examination, inspect all muscle groups for size. Compare the right side with the left. Muscle groups should be within the normal size limits for age and should be symmetrical bilaterally. When muscles in the extremities look asymmetrical, measure each in centimetres and record the difference. A difference of 1 cm or less is not significant. Note that it is difficult to assess muscle mass in very obese people. | |
| Strength. (See Ch 15.) Test the power of homologous muscles simultaneously. Test muscle groups of the extremities, neck and trunk. | Paresis or weakness is diminished strength; paralysis or plegia is absence of strength. |
| Tone. Tone is the normal degree of tension (contraction) in voluntarily relaxed muscles. It shows as a mild resistance to passive stretch. To test muscle tone, move the extremities through a passive range of motion. First, persuade the person to relax completely, to ‘go loose like a rag doll’. Move each extremity smoothly through a full range of motion. Support the arm at the elbow and the leg at the knee (Fig 22.26). Normally, you will note a mild, even resistance to movement. | Flaccidity–decreased resistance, hypotonic. Spasticity and rigidity–types of increased resistance (see Table 22.5). |
| Involuntary movements. Normally, no involuntary movements occur. If they are present, note their location, frequency, rate and amplitude. Note if the movements can be controlled at will. | Tic, tremor, fasciculation, myoclonus, chorea and athetosis (see Table 22.6). |
| Cerebellar function | |
| Balance tests | |
| Gait. Observe as the person walks 5 to 10 metres, turns and returns to the starting point. Normally, the person moves with a sense of freedom. The gait is smooth, rhythmic and effortless; the opposing arm swing is coordinated; the turns are smooth. The step length is about 40 centimetres from heel to heel. | Stiff, immobile posture. Staggering or reeling. Wide base of support. Lack of arm swing or rigid arms. Unequal rhythm of steps. Slapping of foot. Scraping of toe of shoe. Ataxia–uncoordinated or unsteady gait (see Table 22.7). |
| Ask the person to walk a straight line in a heel-to-toe fashion (tandem walking) (Fig 22.27). This decreases the base of support and will accentuate any problem with coordination. Normally, the person can walk straight and stay balanced. | |
You may also test for balance by asking the person to walk on their toes, then on their heels for a few steps. The Romberg test. Ask the person to stand up with feet together and arms at the sides. Once in a stable position, ask the person to close the eyes and to hold the position (Fig 22.28). Wait about 20 seconds. Normally, a person can maintain posture and balance even with the visual orienting information blocked, although slight swaying may occur. Stand close to catch the person in case they fall. |
Muscle weakness in the legs prevents this. Sways, falls, widens base of feet to avoid falling. Positive Romberg sign is loss of balance that occurs when closing the eyes. You eliminate the advantage of orientation with the eyes, which had compensated for sensory loss. A positive Romberg sign occurs with cerebellar ataxia (multiple sclerosis, alcohol intoxication), loss of proprioception and loss of vestibular function. |
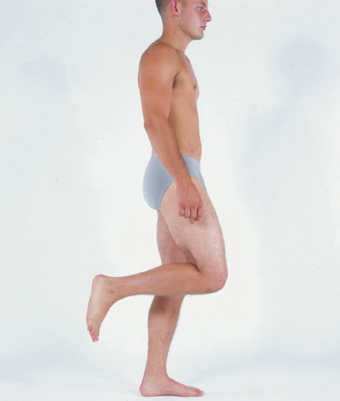
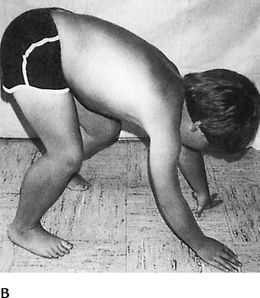
| Ask the person to perform a shallow knee bend or to hop in place, first on one leg, then the other (Fig 22.29). This demonstrates normal position sense, muscle strength and cerebellar function. Note that some individuals cannot hop because of ageing or obesity. | Unable to perform knee bend because of weakness in quadriceps muscle or hip extensors. |
| Coordination and skilled movements | |
| Rapid alternating movements (RAM). Ask the person to pat the knees with both hands, lift up, turn hands over and pat the knees with the backs of the hands (Fig 22.30). Then ask the person to do this faster. Normally, this is done with equal turning and a quick rhythmic pace. | |
| Alternatively, ask the person to touch the thumb to each finger on the same hand, starting with the index finger, then reverse direction (Fig 22.31). Normally, this can be done quickly and accurately. | Lack of coordination. |
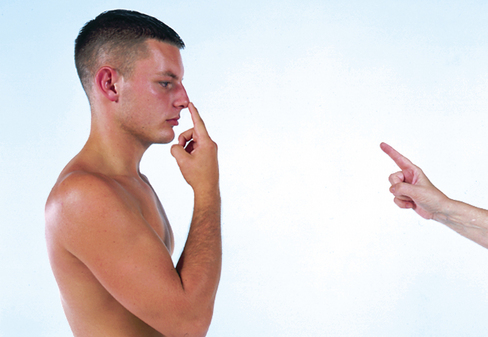
| Finger-to-finger test. With the person’s eyes open, ask them to use the index finger to touch your finger, then their own nose (Fig 22.32). After a few times move your finger to a different spot. The person’s movement should be smooth and accurate. | |
| Finger-to-nose test. Ask the person to close the eyes and to stretch out the arms. Ask the person to touch the tip of their nose with each index finger, alternating hands and increasing speed. Normally this is done with accurate and smooth movement. | Misses nose. Worsening of coordination when the eyes are closed occurs with cerebellar disease or alcohol intoxication. |
| Heel-to-shin test. Test lower extremity coordination by asking the person, who is in a supine position, to place the heel on the opposite knee, and run it down the shin from the knee to the ankle (Fig 22.33). Normally, the person moves the heel in a straight line down the shin. | Lack of coordination, heel falls off shin, occurs with cerebellar disease. |
| ASSESS THE SENSORY SYSTEM | |
Ask the person to identify various sensory stimuli in order to test the intactness of the peripheral nerve fibres, the sensory tracts and higher cortical discrimination. Ensure validity of sensory system testing by making sure the person is alert, cooperative and comfortable and has an adequate attention span. Otherwise, you may get misleading and invalid results. Testing of the sensory system can be fatiguing. If the person is tired you may need to repeat the examination later or to break it into parts. You do not need to test the entire skin surface for every sensation. Routine screening procedures include testing superficial pain, light touch and vibration in a few distal locations and testing stereognosis (see below). This will suffice for all who have not demonstrated any neurological symptoms or signs. Complete testing of the sensory system is warranted in those with neurological symptoms (e.g. localised pain, numbness and tingling) or when you discover abnormalities (e.g. motor deficit). Then, test all sensory modalities and cover most dermatomes of the body (see Fig 22.10). |
Clinical alert: abnormalities in sensory perception can pose an injury risk such as burns and pressure injury. |
Compare sensations on symmetrical parts of the body. When you find a definite decrease in sensation, map it out by systematic testing in that area. Proceed from the point of decreased sensation towards the sensitive area. By asking the person to tell you where the sensation changes, you can map the exact borders of the deficient area. Draw your results on a diagram. Avoid asking leading questions, ‘Can you feel this pinprick?’ This creates an expectation of how the person should feel the sensation, which is called suggestion. Instead, use unbiased directions such as ‘What can you feel?’ The person’s eyes should be closed during each of the tests. Take time to explain what will be happening and exactly how you expect the person to respond. |
Note if the topographic pattern of sensory loss is distal, i.e. over the hands and feet in a ‘glove and stocking’ distribution, or if it is over a specific dermatome. |
| Spinothalamic tract | |
Pain. Pain is tested by the person’s ability to perceive a pinprick. Break a tongue blade lengthwise, forming a sharp point at the fractured end and a dull spot at the rounded end. Lightly apply the sharp point or the dull end to the person’s body in a random, unpredictable order (Fig 22.34). Ask the person to say ‘sharp’ or ‘dull’, depending on the sensation felt. (Note that the sharp edge is used to test for pain; the dull edge is used as a general test of the person’s responses.) Let at least 2 seconds elapse between each stimulus to avoid summation. With summation, frequent consecutive stimuli are perceived as one strong stimulus. Discard tongue blade. |
|
| Temperature. Test temperature sensation only when pain sensation is abnormal; otherwise, you may omit it because the fibres’ tracts are much the same. Fill two test tubes, one with hot water and one with cold water, and apply the bottom ends to the person’s skin in a random order. Ask the person to say which temperature is felt. Alternatively, you could place the flat side of the tuning fork on the skin; its metal always feels cool. | |
| Light touch. Apply a wisp of cotton to the skin. Stretch a cotton ball to make a long end and brush it over the skin in a random order of sites and at irregular intervals (Fig 22.35). This prevents the person from responding just from repetition. Include the arms, forearms, hands, chest, thighs and legs. Ask the person to say ‘now’ or ‘yes’ when touch is felt. Compare symmetrical points. | |
| Posterior column tract | |
| Vibration. Test the person’s ability to feel vibrations of a tuning fork over bony prominences. Use a low-pitch tuning fork (128 Hz or 256 Hz) because its vibration has a slower decay. Strike the tuning fork on the heel of your hand, and hold the base on a bony surface of the fingers and great toe (Fig 22.36). Ask the person to indicate when the vibration starts and stops. If the person feels the normal vibration or buzzing sensation on these distal areas, you may assume proximal spots are normal and proceed no further. If no vibrations are felt, move proximally and test ulnar processes and ankles, patellae and iliac crests. Compare the right side with the left side. If you find a deficit, note whether it is gradual or abrupt. | Unable to feel vibration. Loss of vibration sense occurs with peripheral neuropathy, e.g. diabetes and alcoholism. Often, this is the first sensation lost. Peripheral neuropathy is worse at the feet and gradually improves as you move up the leg, as opposed to a specific nerve lesion, which has a clear zone of deficit for its dermatome. |
| Position (kinaesthesia). Test the person’s ability to perceive passive movements of the extremities. Move a finger or the big toe up and down, and ask the person to tell you which way it is moved (Fig 22.37). The test is done with the eyes closed, but to be sure it is understood, have the person watch a few trials first. Vary the order of movement up or down. Hold the digit by the sides, since upwards or downwards pressure on the skin may provide a clue as to how it has been moved. Normally, a person can detect movement of a few millimetres. | Loss of position sense. |
Tactile discrimination (fine touch). The following tests also measure the discrimination ability of the sensory cortex. As a prerequisite, the person needs a normal or near-normal sense of touch and position sense. Stereognosis. Test the person’s ability to recognise objects by feeling their forms, sizes and weights. With the eyes closed, place a familiar object (paper clip, key, coin, cotton ball or pencil) in the person’s hand and ask the person to identify it (Fig 22.38). Normally, a person will explore it with the fingers and correctly name it. Test a different object in each hand; testing the left hand assesses right parietal lobe functioning. |
|
| Graphaesthesia. Graphaesthesia is the ability to ‘read’ a number by having it traced on the skin. With the person’s eyes closed, use a blunt instrument to trace a single digit number or a letter on the palm (Fig 22.39). Ask the person to tell you what it is. Graphaesthesia is a good measure of sensory loss if the person cannot make the hand movements needed for stereognosis, as occurs in arthritis. | Inability to distinguish number occurs with lesions of the sensory cortex. |
| Two-point discrimination. Test the person’s ability to distinguish the separation of two simultaneous pin points on the skin. Apply the two points of an opened paper clip lightly to the skin in ever-closing distances. Note the distance at which the person no longer perceives two separate points. The level of perception varies considerably with the region tested; it is most sensitive in the fingertips (2 to 8 mm) and least sensitive on the upper arms, thighs and back (40 to 75 mm). | An increase in the distance it normally takes to identify two separate points occurs with sensory cortex lesions. |
| Extinction. Simultaneously touch both sides of the body at the same point. Ask the person to state how many sensations are felt and where they are. Normally, both sensations are felt. | The ability to recognise only one of the stimuli occurs with sensory cortex lesion; the stimulus is extinguished on the side opposite the cortex lesion. |
| Point location. Touch the skin, and withdraw the stimulus promptly. Tell the person, ‘Put your finger where I touched you’. You can perform this test simultaneously with light touch sensation. | With a sensory cortex lesion, the person cannot localise the sensation accurately, even though light touch sensation may be retained |
| TEST THE REFLEXES | |
| Stretch, or deep tendon reflexes (DTRs) | |
| Measurement of the stretch reflexes reveals the intactness of the reflex arc at specific spinal levels as well as the normal override on the reflex of the higher cortical levels. | |
| For an adequate response, the limb should be relaxed and the muscle partially stretched. Stimulate the reflex by directing a short, snappy blow of the reflex hammer onto the muscle’s insertion tendon. Use a relaxed hold on the hammer. | |
As with the percussion technique, the action takes place at the wrist. Strike a brief, well-aimed blow, and bounce up promptly; do not let the hammer rest on the tendon. Use the pointed end of the reflex hammer when aiming at a smaller target such as your thumb on the tendon site; use the flat end when the target is wider or to diffuse the impact and prevent pain. Use just enough force to get a response. Compare right and left sides—the responses should be equal. The reflex response is graded on a 4-point scale: |
|
4+ Very brisk, hyperactive with clonus, indicative of disease 3+ Brisker than average, may indicate disease This is a subjective scale and requires some clinical practice. Even then the scale is not completely reliable because no standard exists to say how brisk a reflex should be to warrant a grade of 3+. Also, a wide range of normal exists in reflex responses. Healthy people may have diminished reflexes or they may have brisk ones. Your best plan is to interpret the deep tendon reflexes only within the context of the rest of the neurological exam. Sometimes the reflex response fails to appear. Try further encouragement of relaxation, varying the person’s position or increasing the strength of the blow. Reinforcement is another technique to relax the muscles and enhance the response (Fig 22.40). Ask the person to perform an isometric exercise in a muscle group somewhat away from the one being tested. For example, to enhance a patellar reflex, ask the person to lock the fingers together and ‘pull’. Then strike the tendon. To enhance a biceps response, ask the person to clench the teeth or to grasp the thigh with the opposite hand. |
Clonus is a set of rapid, rhythmic contractions of the same muscle. Hyperreflexia is the exaggerated reflex seen when the monosynaptic reflex arc is released from the usually inhibiting influence of higher cortical levels. This occurs with upper motor neuron lesions, e.g. a stroke. Hyporeflexia, which is the absence of a reflex, is a lower motor neuron problem. It occurs with interruption of sensory affer-ents or destruction of motor efferents and anterior horn cells, e.g. spinal cord injury. |
| Biceps reflex (C5 to C6). Support the person’s forearm on yours; this position relaxes, as well as partially flexes, the person’s arm. Place your thumb on the biceps tendon and strike a blow on your thumb. You can feel as well as see the normal response, which is contraction of the biceps muscle and flexion of the forearm (Fig 22.41). | |
| Triceps reflex (C7 to C8). Tell the person to let the arm ‘just go dead’ as you suspend it by holding the upper arm. Strike the triceps tendon directly just above the elbow (Fig 22.42). The normal response is extension of the forearm. Alternatively, hold the person’s wrist across the chest to flex the arm at the elbow, and tap the tendon. | |
| Brachioradialis reflex (C5 to C6). Hold the person’s thumbs to suspend the forearms in relaxation. Strike the forearm directly, about 2 to 3 cm above the radial styloid process (Fig 22.43). The normal response is flexion and supination of the forearm. | |
| Quadriceps reflex (‘knee jerk’) (L2 to L4). Let the lower legs dangle freely to flex the knee and stretch the tendons. Strike the tendon directly just below the patella (Fig 22.44). Extension of the lower leg is the expected response. You will also palpate contraction of the quadriceps. | |
| For the person in the supine position, use your own arm as a lever to support the weight of one leg against the other leg. This manoeuvre also flexes the knee. | |
| Achilles reflex (‘ankle jerk’) (L5 to S2). Position the person with the knee flexed and the hip externally rotated. Hold the foot in dorsiflexion, and strike the Achilles tendon directly (Fig 22.45). Feel the normal response as the foot plantar flexes against your hand. | |
| For the person in the supine position, flex one knee and support that lower leg against the other leg so that it falls ‘open’. Dorsiflex the foot and tap the tendon (Fig 22.46). | |
| Clonus. Test for clonus, particularly when the reflexes are hyperactive. Support the lower leg in one hand. With your other hand, move the foot up and down a few times to relax the muscle. Then stretch the muscle by briskly dorsi flexing the foot. Hold the stretch (Fig 22.47). With a normal response, you feel no further movement. When clonus is present, you will feel and see rapid rhythmic contractions of the calf muscle and movement of the foot. | Clonus is repeated reflex muscular movements. A hyperactive reflex with sustained clonus (lasting as long as the stretch is held) occurs with upper motor neuron disease. |
| Superficial (cutaneous) reflexes | |
| Here, the sensory receptors are in the skin rather than in the muscles. The motor response is a localised muscle contraction. | |
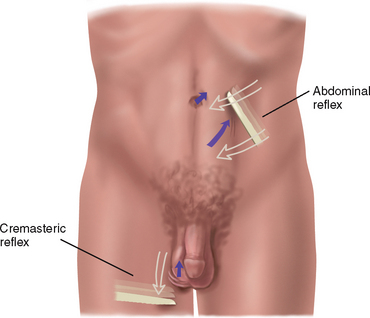
| Abdominal reflexes—upper (T8 to T10), lower (T10 to T12). Have the person assume a supine position, with the knees slightly bent. Use the handle end of the reflex hammer, a wood applicator tip or the end of a split tongue blade to stroke the skin. Move from the side of the abdomen towards the midline at both the upper and the lower abdominal levels (Fig 22.48). The normal response is ipsilateral contraction of the abdominal muscle with an observed deviation of the umbilicus towards the stroke. When the abdominal wall is very obese, pull the skin to the opposite side and feel it contract towards the stimulus. | Superficial reflexes are absent with diseases of the pyramidal tract, e.g. they are absent on the contralateral side with stroke. |
| Cremasteric reflex (L1 to L2). This is not routinely done. On the male, lightly stroke the inner aspect of the thigh with the reflex hammer or tongue blade (see Fig 22.48). Note elevation of the ipsilateral testicle. | Absent in both upper motor neuron and lower motor neuron lesions. |
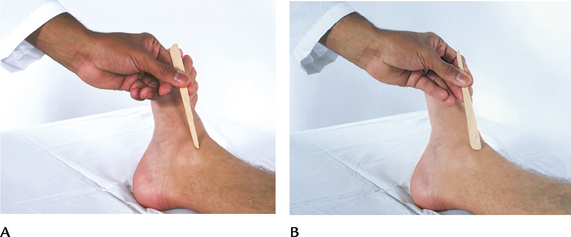
| Plantar reflex (L4 to S2). Position the thigh in slight external rotation. With the reflex hammer, draw a light stroke up the lateral side of the sole of the foot and inwards across the ball of the foot, like an upside-down J (Fig 22.49, A). The normal response is plantar flexion of the toes and inversion and flexion of the forefoot. | Except in infancy, the abnormal response is dorsiflexion of the big toe and fanning of all toes, which is a positive Babinski sign, also called ‘upgoing toes’ (Fig 22.49, ß). This occurs with upper motor neuron disease of the corticospinal (or pyramidal) tract. |
| DEVELOPMENTAL CONSIDERATIONS | |
| Skull | |
| Measure an infant’s head size with measuring tape at each visit up to age 2 years, then yearly up to age 6 years. (Measurement of head circumference is presented in detail in Ch 9.) | Note an abnormal increase in head size or failure to grow. |
| The newborn’s head measures about 32 to 38 cm (average around 34 cm), and is 2 cm larger than chest circumference. At age 2 years, both measurements are the same. During childhood the chest circumference grows to exceed head circumference by 5 to 7 cm. | |
| Observe the infant’s head from all angles, not just the front. The contour should be symmetrical. Some racial variation occurs in normal head shapes; Nordic children tend to have long heads and Asian children have broad heads. | Frontal bulges, or ‘bossing’, occur with prematurity or rickets. |
| Two common variations in the newborn cause the shape of the skull to look markedly asymmetrical: A caput succedaneum is oedematous swelling and ecchymosis of the presenting part of the head caused by birth trauma (Fig 22.50). It feels soft, and it may extend across suture lines. It gradually resolves during the first few days of life and needs no treatment. | |
| A cephalhaematoma is a subperiosteal haemorrhage, which is also a result of birth trauma (Fig 22.51). It is soft, fluctuant and well defined over one cranial bone because the periosteum (i.e. the covering over each bone) holds the bleeding in place. It appears several hours after birth and gradually increases in size. No discolouration is present but it looks bizarre, so parents need reassurance that it will be reabsorbed during the first few weeks of life without treatment. Rarely, a large haematoma may persist to 3 months. | An infant with cephalhaematoma is at greater risk for jaundice as the red blood cells within the haematoma are broken down and reabsorbed. |
As you palpate the newborn’s head, the suture lines feel like ridges. By 5 to 6 months, they are smooth and not palpable. A newborn’s head may feel asymmetrical and the involved ridges more prominent due to moulding of the cranial bones during engagement and passage through the birth canal. Moulding is overriding of the cranial bones; usually, the parietal bone overrides the frontal or occipital bone. Reassure parents that this lasts only a few days or a week. Babies delivered by caesarean section are noted for their evenly round heads. Also, some asymmetry may occur if an infant continually sleeps in one position; this is a flattening of the dependent cranial bone, usually the occiput. |
|
| Gently palpate the skull and fontanels while the infant is calm and somewhat in a sitting position (crying, lying down or vomiting may cause the anterior fontanel to look full and bulging). The skull should feel smooth and fused except at the fontanels. The fontanels feel firm, slightly concave and well defined against the edges of the cranial bones. You may see slight arterial pulsations in the anterior fontanel. | |
| The posterior fontanel may not be palpable at birth. If it is, it measures 1 cm and closes by 1 to 2 months. The anterior fontanel may be small at birth and enlarge to 2.5 cm by 2.5 cm. A large diameter of 4 to 5 cm occasionally may be normal under 6 months. A small fontanel is usually normal. The anterior fontanel closes between 9 months and 2 years. Early closure may be insignificant if head growth proceeds normally. | |
| Note the infant’s head posture and head control. The infant can turn the head side to side by 2 weeks and shows the tonic neck reflex when supine and the head is turned to one side (extension of same arm and leg, flexion of opposite arm and leg). The tonic neck reflex disappears between 3 and 4 months, then the head is maintained in the midline. Head control is achieved by 4 months, when the baby can hold the head erect and steady when pulled to a vertical position. | |
| Face | |
| Check facial features for symmetry, appearance and presence of swelling. Note symmetry of wrinkling when the infant cries or smiles (e.g. both sides of the lips rise and both sides of forehead wrinkle). Children love to comply when you ask them to ‘make a face’. Normally, no swelling is evident. Parotid gland enlargement is seen best when the child sits and looks up at the ceiling; the swelling appears below the angle of the jaw. | Unilateral immobility indicates nerve damage (central or peripheral) (e.g. note angle of mouth droop on paralysed side). Some facies are characteristic of congenital abnormalities or chronic allergy. See Table 16.8 |
| Neck | |
| An infant’s neck looks short; it lengthens during the first 3 to 4 years. You can see the neck better by supporting the infant’s shoulders and tilting the head back a little. This positioning also enhances palpation of the trachea, which is buried deep in the neck. Feel for the row of cartilaginous rings in the midline or just slightly to the right of midline. | A short neck or webbing (loose fan-like folds) may indicate congenital abnormality (e.g. Down or Turner syndrome) or it may occur alone. |
| Assess muscle development with gentle passive ROM. Cradle the infant’s head with your hands and turn it side to side and test forward flexion, extension and rotation. Note any resistance to movement, especially flexion. Ask a child to actively move through the ROM, as you would an adult. | |
| The neurological system shows dramatic growth and development during the first year of life. Assessment includes noting that milestones you normally would expect for each month have indeed been achieved, and that the early, more primitive reflexes cease at the appropriate developmental stage. | |
| At birth, the newborn is very alert, with the eyes open and demonstrates strong, urgent sucking. The normal cry is loud, lusty and even angry. The next 2 or 3 days may be spent mostly sleeping as the baby recovers from the birth process. After that, the pattern of sleep and waking activity is highly variable; | |
| Lethargy, hyporeactivity, hyperirrita-bility and parent’s report of significant change in behaviour all warrant referral. | |
| By 2 months of age, the baby smiles responsively and recognises the parent’s face. Babbling occurs at 4 months, and nonspecifically after 9 months.one or two words (mama, dada) are used | |
Observe spontaneous motor activity for smoothness and symmetry. Smoothness of movement suggests proper cerebellar function, as does the coordination involved in sucking and swallowing. To screen gross and. ne motor coordination, use the Denver II test with its age-speci.c developmental milestones. You also can assess movement by testing the re.exes listed in the following section. Note their smoothness of response and symmetry. Also, note whether their presence or absence is appropriate for the infant’s age. |
Delay in motor activity occurs with brain damage, mental retardation, peripheral neuromuscular damage, prolonged illness and parental neglect. |
| Assess muscle tone by. rst observing resting posture. The newborn favours a. exed position; extremities are symmetrically folded inwards, the hips are slightly abducted and the. sts are tightly. exed (Fig 22.52). Infants born by breech delivery, however, do not have. exion in the lower extremities. | Frog position–hips abducted and almost flat against the table, externally rotated (only normal after breech delivery). Opisthotonos—head arched back, stiffness of neck and extension of arms and legs; occurs with meningeal or brainstem irritation and kernicterus (see Table 22.3). Extension of limbs may occur with intracranial haemorrhage. Any type of continual asymmetry, e.g. asymmetry of upper limbs occurs with brachial plexus palsy. |
| After 2 months of age, flexion gives way to gradual extension, beginning with the head and continuing in a cephalocaudal direction. Now is the time to check for spasticity; none should be present. Test for spasticity by flexing the infant’s knees onto the abdomen and then quickly releasing them. They will unfold but not too quickly. Also, gently push the head forward—the baby should comply. | Spasticity is an early sign of cerebral palsy. After releasing flexed knees, legs will quickly extend and adduct, even to a ‘scissoring’ motion when spasticity is present. Also, the baby often resists head flexion and extends back against your hand when spasticity is present. |
| The fists are normally held in tight flexion for the first 3 months. Then the fists open for part of the time. A purposeful reach for an object with both hands occurs around 4 months of age, a transfer of an object from hand to hand at 7 months of age, a grasp using fingers and opposing thumb at 9 months of age and a purposeful release at 10 months of age. Babies are normally ambidextrous for the first 18 months. | Note persistent one-hand preference in baby younger than 18 months of age, which may indicate a motor deficit on the opposite side. |
| Head control is an important milestone in motor development. You can incorporate the following two movements into every infant assessment to check the muscle tone necessary for head control. | |
| First, with the baby supine, pull to a sit holding the wrists and note head control (Fig 22.53). The newborn will hold the head almost in the same plane as the body, and it will balance briefly when the baby reaches a sitting position, then flop forward. (Even a premature infant shows some head flexion.) At 4 months of age, the head stays in line with the body and does not flop. | |
| Second, lift up the baby in a prone position, with one hand supporting the chest (Fig 22.54). The term newborn holds the head at an angle of 45 degrees or less from horizontal, the back is straight or slightly arched and the elbows and knees are partly flexed. | |
| At 3 months of age, the baby raises the head and arches the back, as in a swan dive. This is the Landau reflex, which persists until 1½ years of age. | |
| Assess muscle strength by noting the strength of sucking and of spontaneous motor activity. Normally, no tremors are present, and no continual overshooting of the mark occurs when reaching. | |
| The sensory system | |
| You will perform very little sensory testing with infants and toddlers. The newborn normally has hypoaesthesia and requires a strong stimulus to elicit a response. The baby responds to pain by crying and a general reflex withdrawal of all limbs. By 7 to 9 months of age, the infant can localise the stimulus and shows more specific signs of withdrawal. Other sensory modalities are not tested. | |
| Reflexes | |
| Infantile automatisms are reflexes that have a predictable timetable of appearance and departure. The reflexes most commonly tested are listed in the following section. For the screening examination, you can just check the rooting, grasp, tonic neck and Moro reflexes. | |
| Rooting reflex. Brush the infant’s cheek near the mouth. Note whether the infant turns the head towards that side and opens the mouth. Appears at birth and disappears at 3 to 4 months. | |
| Sucking reflex. Touch the lips and offer your gloved little finger to suck. Note strong sucking reflex. The reflex is present at birth and disappears at 10 to 12 months. | |
| Palmar grasp. Place the baby’s head midline to ensure symmetrical response. Offer your finger from the baby’s ulnar side, away from the thumb. Note tight grasp of all the baby’s fingers (Fig 22.55). Sucking enhances grasp. Often you can pull baby to a sit from grasp. The reflex is present at birth, is strongest at 1 to 2 months and disappears at 3 to 4 months. | |
| Plantar grasp. Touch your thumb at the ball of the baby’s foot. Note that the toes curl down tightly (Fig 22.56). The re.ex is present at birth and disappears at 8 to 10 months. | |
Babinski’s reflex. Stroke your. nger up the lateral edge and across the ball of the infant’s foot. Note fanning of toes (positive Babinski’s re.ex) (Fig 22.57). The re.ex is present at birth and disappears (changes to the adult response) by 24 months of age (variable). |
Positive Babinski’s reflex after 2 or 2½ years of age occurs with pyramidal tract disease. |
| Tonic neck reflex. With the baby supine, relaxed or sleeping, turn the head to one side with the chin over shoulder. Note ipsilateral extension of the arm and leg and. exion of the opposite arm and leg; this is the ‘fencing’ position. If you turn the infant’s head to the opposite side, positions will reverse (Fig 22.58). The reflex appears by 2 to 3 months, decreases at 3 to 4 months and disappears by 4 to 6 months. | Persistence later in infancy occurs with brain damage. |
| Moro reflex. Startle the infant by jarring the crib, making a loud noise or supporting the head and back in a semi-sitting position and quickly lowering the infant to 30 degrees. The baby looks as if they are hugging a tree. That is, symmetrical abduction and extension of the arms and legs, fanning fingers and curling of the index finger and thumb to C position occur. The infant then brings in both arms and legs (Fig 22.59). The reflex is present at birth, and disappears at 1 to 4 months. | Absence of the Moro reflex in the newborn or persistence after 5 months of age indicates severe CNS injury. Absence of movement in just one arm occurs with fracture of the humerus or clavicle and with brachial nerve palsy. Absence in one leg occurs with a lower spinal cord problem or a dislocated hip. A hyperactive Moro reflex occurs with tetany or CNS infection. |
| Placing reflex. Hold the infant upright under the arms, close to a table. Let the dorsal ‘top’ of foot touch the underside of table. Note flexing of hip and knee, followed by extension at the hip, to place foot on table. Reflex appears at 4 days after birth. | |
| Stepping reflex. Hold the infant upright under the arms, with the feet on a flat surface. Note regular alternating steps. The reflex disappears before voluntary walking. | Extensor thrust, or ‘scissoring’; crossing of lower extremities. |
| Special procedures | |
| Palpation. Craniotabes is a softening of the skull’s outer layer. With a newborn, pressure along the suture of the parietal and occipital bones above the ear produces a snapping sensation because of the pliable skull bone. It is like indenting a ping-pong ball and feeling it snap back. Do not attempt this unless craniotabes is suspected because of other abnormal findings, and even then avoid excessive pressure. Craniotabes may be normal, especially with pre mature infants. | Craniotabes may occur with rickets, hydrocephaly or congenital syphilis. |
| Percussion. With an infant, you may directly percuss with your plexor finger against the head surface. This yields a resonant or ‘cracked pot’ sound, which is normal before closure of the fontanels. | The sound occurs with hydrocephalus from separation of cranial sutures (Macewen’s sign). |
| Auscultation. Bruits are common in the skull in children under 4 or 5 years of age or in children with anaemia. They are systolic or continuous and are heard over the temporal area. | After 5 years of age, bruits indicate increased intracranial pressure, aneurysm or arteriovenous shunt. |
| Transillumination. Use this procedure if you suspect an abnormal head size or an intracranial lesion. In a completely darkened room, hold a rubber-collared flashlight firmly against the infant’s skull. You need a tight fit against the head Explore all regions of the head: frontal, both sides, occiput (Fig 22.60). A small ring of light around the flashlight is normal (less than 2 cm in the frontal area, less than 1 cm in the occipital area). But you should not see a larger halo around the rubber collar. | Presence of a halo of light through the skull indicates a loss or thinning of cerebral cortex. If the cortex is absent, the entire cranium lights up (Fig 22.61). |
Use the same sequence of neurological assessment as with the adult, with the omissions or modifications mentioned in the following section. Assess the child’s general behaviour during play activities, reaction to parent and cooperation with parent and with you. Complete details are described in Chapter 21. Smell and taste are almost never tested, but if you need to test the child’s sense of smell (cranial nerve I), use a scent familiar to the child such as peanut butter or orange peel. When testing visual fields (cranial nerve II) and cardinal positions of gaze (cranial nerves III, I V, VI), you often need to gently immobilise the head, or the child will track with the whole head. Make a game out of asking the child to imitate your funny ‘faces’ (cranial nerve VII); thus, the child has fun and you win a friend. |
|
Much of the motor assessment can be derived from watching the child undress and dress and manipulate buttons. This indicates muscle strength symmetry, joint range of motion and fine motor skills. Use the Denver II to screen gross and fine motor skills that are appropriate for the child’s specific age Be familiar with developmental milestones described in Chapter 2 for each age Note the child’s gait during both walking and running. Allow for the normal wide-based gate of the toddler and the normal knock-kneed walk of the preschooler. Normally, the child can balance on one foot for about 5 seconds by 4 years of age, can balance for 8 to 10 seconds at 5 years of age and can hop at 4 years. Children enjoy performing these tests (Fig 22.62). |
Muscle hypertrophy or atrophy occurs with muscular dystrophy. Causes of motor delay are listed earlier in the infant section. Weakness climbing up or down stairs occurs with muscular dystrophy. Broad-based gait beyond toddlerhood, scissor gait (see Table 22.7). Failure to hop after 5 years of age indicates incoordination of gross motor skill. |
| Observe the child as they rise from a supine position on the floor to a sitting position, and then to a stand. Note the muscles of the neck, abdomen, arms and legs. Normally, the child curls up in the midline to sit up, then pushes off with both hands against the floor to stand (Fig 22.63, A). | Weak pelvic muscles are a sign of muscular dystrophy; from the supine position, the child will roll to one side, bend forward to all four extremities, plant hands on legs and literally ‘climb’ up themself. This is Gower’s sign (Fig 22.63, ß). |
| Assess fine coordination by using the finger-to-nose test if you can be sure the young child understands your directions. Demonstrate the procedure first, then ask the child to do the test with the eyes open, then with the eyes closed. Fine coordination is not fully developed until the child has reached 4 or 6 years of age. Consider it normal if a younger child can bring the finger to within 2 to 5 cm of the nose. | Failure of the finger-to-nose test with the eyes open indicates gross incoordination; failure of the test with the eyes closed indicates minor incoordination or lack of position sense. |
| Testing sensation is very unreliable in toddlers and preschoolers. You may test light touch by asking the child to close the eyes and then to point to the spot where you touch or tickle. Testing of vibration, position, stereognosis, graph aesthesia or two-point discrimination usually is not done on a child younger than 6 years of age. Also, do not test for perception of superficial pain. In children older than 6 years of age, you may perform sensory testing as with adults. Use a fractured tongue blade if you need to test superficial pain. | |
| The deep tendon reflexes are usually not tested in children younger than 5 years of age due to lack of cooperation in relaxation. When you need to test DTRs in a young child, use your finger to percuss the tendon. Use a reflex hammer only with an older child. Coax the child to relax, or distract and percuss discreetly when the child is not paying attention. The knee jerk is present at birth, then the ankle jerk and brachial reflex appear and the triceps reflex is present at 6 months. | Hyperactivity of DTRs occurs with upper motor neuron lesion, hypocalcae-mia and hyperthyroidism and with muscle spasm associated with early poliomyelitis. Decreased or absent reflexes occur with a lower motor neuron lesion, muscular dystrophy and flaccidity or flaccid paralysis. Clonus may occur with fatigue, but it usually indicates hyperreflexia. |
| Any decrease in muscle bulk is most apparent in the hand, as seen by guttering between the metacarpals. These dorsal hand muscles often look wasted, even with no apparent arthropathy. The grip strength remains relatively good. | Hand muscle atrophy is worsened with disuse and degenerative arthropathy. |
| Senile tremors occasionally occur. These benign tremors include an intention tremor of the hands, head nodding (as if saying yes or no) and tongue protrusion. Dyskinesias are the repetitive stereotyped movements in the jaw, lips or tongue that may accompany senile tremors. No associated rigidity is present. | Distinguish senile tremors from tremors of parkinsonism. The latter includes rigidity and slowness and weakness of voluntary movement. |
| Absence of a rhythmic reciprocal gait pattern is seen in parkinsonism and hemiparesis (see Table 22.7). | |
After 65 years of age, loss of the sensation of vibration at the ankle malleolus is common and is usually accompanied by loss of the ankle jerk. Position sense in the big toe may be lost, although this is less common than vibration loss. Tactile sensation may be impaired. The ageing person may need stronger stimuli for light touch and especially for pain. The deep tendon reflexes are less brisk. Those in the upper extremities are usually present, but the ankle jerks are commonly lost. Knee jerks may be lost, but this occurs less often. The plantar reflex may be absent or difficult to interpret. Often, you will not see a definite normal flexor response. However, you still should consider a definite extensor response to be abnormal. The superficial abdominal reflexes may be absent, probably because of stretching of the musculature through pregnancy or obesity. |
Note any difference in sensation between right and left sides, which may indicate a neurological deficit. |
TABLE 22.1 Testing cranial nerve function of infants
| Cranial nerve | Response |
|---|---|
| II, III, IV, VI | |
| V | Rooting reflex, sucking reflex |
| VII | Facial movements (e.g. wrinkling forehead and nasolabial folds) symmetric when crying or smiling |
| VIII | |
| IX, X | |
| XII | Pinch nose, infant’s mouth will open and tongue rise in midline |
TABLE 22.2 Levels of consciousness
Adapted from Strub RL, Black FW: Mental status examination in neurology, 4th edn. Philadelphia, 2000, Davis, with permission.
TABLE 22.9 Common patterns of motor system dysfunction
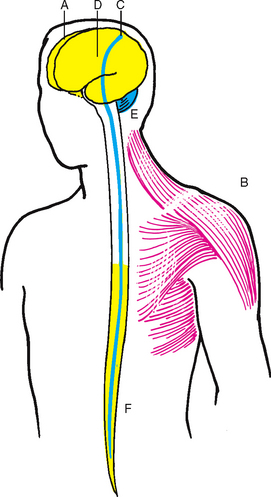 |
A–Cerebral palsy. Mixed group of paralytic neuromotor disorders of infancy and childhood; due to damage to cerebral cortex caused by a developmental defect, intrauterine meningitis or encephalitis, birth trauma, anoxia or kernicterus. B–Muscular dystrophy. Chronic, progressive wasting of skeletal musculature, which produces weakness, contractures and, in severe cases, respiratory dysfunction and death. Onset of symptoms occurs in childhood. Many types exist; the most severe is Duchenne’s dystrophy, characterised by the waddling gait described in Table 22.7 C–Hemiplegia. Damage to corticospinal tract, e.g. stroke. Upper motor neuron damage occurs above the pyramidal decussation crossover, so motor impairment is on contralateral (opposite) side. Initially flaccid when the lesion is acute; later, the muscles become spastic and abnormal reflexes appear. Characteristic posture: arm–shoulder adducted, elbow flexed, wrist pronated, leg extended; face–weakness only in lower muscles. Hyperreflexia and possible clonus occur on the involved side; loss of corneal, abdominal and cremasteric reflexes; positive Babinski’s and Hoffman’s reflexes. D–Parkinsonism. Defect of extrapyramidal tracts, in the region of the basal ganglia, with loss of the neurotransmitter dopamine. Classic triad of symptoms: tremor, rigidity, akinesia. Also slower monotonous speech and diminutive writing. Body tends to stay immobile; facial expression is flat, staring, expressionless; excessive salivation occurs; reduced eye blinking (see Table 22.14). Posture is stooped; equilibrium is impaired; loses balance easily; gait is described in Table 22.7 Parkinsonian tremor; cogwheel rigidity on passive range of motion. E–Cerebellar. A lesion in one hemisphere produces motor abnormalities on the ipsilateral side. Characterised by ataxia, lurching forward of affected side while walking, rapid alternating movements are slow and arrhythmic, finger-to-nose test reveals ataxia and tremor with overshoot or undershoot, and eyes display coarse nystagmus. F–Paraplegia. Lower motor neuron damage caused by spinal cord injury. A severe injury or complete transection initially produces ‘spinal shock’, which is defined as no movement or reflex activity below the level of the lesion. Gradually, deep tendon reflexes reappear and become increased, flexor spasms of legs occur; and finally, extensor spasms of legs occur; these spasms lead to prevailing extensor tone. |
Promoting a healthy lifestyle Stroke prevention
Symptoms, non-modifiable and well-documented modifiable risk factors for stroke
According to the National Stroke Foundation (2010) stroke is a leading cause of long-term disability and the second leading cause of death after heart disease. A stroke occurs when the blood flow is interrupted to a part of the brain. The most common type is an ischaemic stroke, occurring when a blood clot blocks a blood vessel in the brain. Less common is a haemorrhagic stroke, which occurs when a blood vessel in the brain ruptures and causes bleeding. The symptoms and after-effects of a stroke depend on which area of the brain is affected and to what extent. This can make a stroke difficult to diagnose. However, early recognition of symptoms and prompt treatment are essential.
The most common symptoms of stroke include:
1. Sudden weakness or numbness in the face, arms or legs, especially when it is on one side of the body
2. Sudden confusion, trouble speaking or understanding speech
3. Sudden changes in vision, such as blurry vision or partial or complete loss of vision in one or both eyes
4. Sudden trouble walking, dizziness and/or loss of balance or coordination
Less common symptoms of stroke include:
Stroke symptoms usually do not hurt, which is why many people ignore them or delay seeking medical attention. Sometimes, people can have a ‘mini-stroke’ or transient ischaemic attack (TIA). In these cases, the stroke symptoms last only temporarily and then disappear, often within an hour. Because the symptoms ‘go away’, people too often do not report them or seek medical attention. However, a TIA is a warning sign that should not be ignored. When people experience chest pain, they seek medical attention, to rule out a heart attack. Having a TIA should also prompt people to seek medical attention to rule out the possibility of a future stroke.
Stroke can strike anyone without any warning. Preventing a stroke is still the best medicine. People need to be aware of their stroke risk and take steps to change the risk factors they can control.
The National Stroke Foundation Australia (2010) recommends the FAST test as an easy way to recognise and remember the signs of stroke. Using this test involves the following:
• Face—Check their face. Has their mouth drooped?
• Arms—Can they lift both arms?
• Speech—Is their speech slurred? Do they understand you?
• Time—Time is critical. If you see any of these signs call 000 now!
Well-documented modifiable risk factors for stroke include:
1. History of cardiovascular disease
8. Asymptomatic carotid stenosis
10. Postmenopausal hormone therapy
Non-modifiable risk factors for stroke, although non-modifiable, may help to identify those who, in conjunction with well-documented modifiable risks, are at highest risk of stroke and who may benefit from more rigorous treatment of modifiable risk factors.
Non-modifiable risk factors for stroke include:
2. Gender—strokes are generally more prevalent in men than in women. However, exceptions are in 35 to 44 year olds and ≥85 years of age—groups in which women have slightly greater age-specific stroke incidence than do men
4. Ethnicity—Aboriginal and Torres Strait Islander people have higher stroke incidence and mortality rates than European Australians. Incidence rates are also relatively higher among some Asian groups
5. Genetic factors disorders (e.g. Marfan syndrome, Fabry disease, cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy (CADASIL).
(Pink and Allbon, 2008; Hankey, 2007; National Stroke Foundation Australia, 2007, 2010; AIHW and National Heart Foundation of Australia, 2004).
DOCUMENTATION AND CRITICAL THINKING
FOCUSED ASSESSMENT: CLINICAL CASE STUDY
JT is a 61-year-old male who works as a carpenter with a large building firm and who is admitted to the Rehabilitation Unit with a diagnosis of right hemiplegia and aphasia following stroke 4 weeks ago.
Subjective
Because of JT’s speech dysfunction, history provided by wife.
Prior to the stroke he reported severe headache, then sudden onset of collapse and loss of consciousness while at work. Did not strike head as fell. Transported by ambulance to hospital. On examination his right arm and leg were flaccid, and he was unconscious. Admitted to stroke unit. Regained consciousness day 3 after admission, unable to move right side, unable to speak clearly or write.
Now—some improvement in right motor function. Bowel control achieved with use of commode same time each day (after breakfast). Bladder control improved. Some occasional incontinence, usually when cannot tell people he needs to urinate.
Objective
Mental status: Dressed in tracksuit, sitting in wheelchair, appears alert with appropriate eye contact, listening intently to history. Speech is slow, requires great effort, able to give one-word answers that are appropriate in content but voice lacks normal tone. Seems to understand all language spoken. Follows requests appropriately, within limits of motor weakness.
Sensory: Pinprick and light touch present but diminished on right arm and leg. Position sense impaired on right side.
Motor: Right hand grip weak, right arm drifts, right leg weak, unable to support weight. Spasticity in right arm and leg muscles, limited range of motion on passive motion. Unable to stand up and walk unassisted.
ABNORMAL FINDINGS FOR ADVANCED PRACTICE
| Condition | Disorder of | Description |
|---|---|---|
| Dysphonia | Voice | Difficulty or discomfort in talking, with abnormal pitch or volume, due to laryngeal disease. Voice sounds hoarse or whispered, but articulation and language are intact. |
| Dysarthria | Articulation | Distorted speech sounds; speech may sound unintelligible; basic language (word choice, grammar, comprehension) intact. |
| Aphasia | Language comprehension and production secondary to brain damage | True language disturbance, defect in word choice and grammar or defect in comprehension; defect is in higher integrative language processing. |
| Types of aphasia | ||
| An earlier dichotomy classified aphasias as expressive (difficulty producing language) or receptive (difficulty understanding language). Since all people with aphasia have some difficulty with expression, beginning examiners tend to classify them all as expressive. The following system is more descriptive. | ||
| Condition | Description | |
| Global aphasia | The most common and severe form. Spontaneous speech is absent or reduced to a few stereotyped words or sounds. Comprehension is absent or reduced to only the person’s own name and a few select words. Repetition, reading and writing are severely impaired. Prognosis for language recovery is poor. Caused by a large lesion that damages most of combined anterior and posterior language areas. | |
| Broca’s aphasia | Expressive aphasia. The person can understand language but cannot express themself using language. This is characterised by nonfluent, dysarthric and effortful speech. The speech is mostly nouns and verbs (high-content words) with few grammatic fillers, termed ‘agrammatic’ or ‘telegraphic’ speech. Repetition and reading aloud are severely impaired. Auditory and reading comprehensions are surprisingly intact. Lesion is in anterior language area called the motor speech cortex or Broca’s area. | |
| Wernicke’s aphasia | Receptive aphasia. The linguistic opposite of Broca’s aphasia. The person can hear sounds and words but cannot relate them to previous experiences. Speech is fluent, effortless and well articulated but has many paraphasias (word substitutions that are malformed or wrong) and neologisms (made-up words) and often lacks substantive words. Speech can be totally incomprehensible. Often, there is a great urge to speak. Repetition, reading and writing also are impaired. Lesion is in posterior language area called the Association auditory cortex or Wernicke’s area. | |
(For a discussion of other types of aphasia (e.g. conduction, anomic, transcortical), please consult a neurology text.)
TABLE 22.5 Abnormalities in muscle tone
| Condition | Description | Associated with |
|---|---|---|
| Flaccidity | Decreased muscle tone or hypotonia; muscle feels limp, soft and flabby; muscle is weak and easily fatigued | Lower motor neuron injury anywhere from the anterior horn cell in the spinal cord to the peripheral nerve (peripheral neuritis, poliomyelitis, Guillain-Barré syndrome). Early cerebrovascular accident and spinal cord injury are flaccid at first. |
| Spasticity | Increased tone or hypertonia; increased resistance to passive lengthening; then may suddenly give way (clasp-knife phenomenon) | Upper motor neuron injury to corticospinal motor tract, e.g. paralysis with cerebrovascular accident (chronic stage) |
| Rigidity | Constant state of resistance (lead-pipe rigidity); resists passive movement in any direction; dystonia | Injury to extrapyramidal motor tracts, e.g. basal ganglia with parkinsonism |
| Cogwheel rigidity | Type of rigidity in which the increased tone is released by degrees during passive range of motion so it feels like small regular jerks | Parkinsonism |
| Type | Characteristic appearance | Possible causes |
|---|---|---|
Spastic hemiparesis  |
Arm is immobile against the body, with flexion of the shoulder, elbow, wrist, fingers and adduction of shoulder. The leg is stiff and extended and circumducts with each step (drags toe in a semicircle) | Upper motor neuron lesion of the corticospinal tract, e.g. cerebrovascular accident, trauma |
Cerebellar ataxia  |
Staggering, wide-based gait; difficulty with turns; uncoordinated movement with positive Romberg sign | Alcohol or barbiturate effect on cerebellum; cerebellar tumour; multiple sclerosis |
Parkinsonian (festinating)  |
Posture is stooped; trunk is pitched forwards; elbows, hips and knees are flexed. Steps are short and shuffling. Hesitation to begin walking, and difficult to stop suddenly. The person holds the body rigid. Walks and turns body as one fixed unit. Difficulty with any change in direction | Parkinsonism |
Scissors  |
Knees cross or are in contact, like holding an orange between the thighs. The person uses short steps, and walking requires effort | Paraparesis of legs, multiple sclerosis |
Steppage or footdrop  |
Slapping quality–looks as if walking up stairs and finds no stair there. Lifts knee and foot high and slaps it down hard and flat to compensate for footdrop | Weakness of peroneal and anterior tibial muscles; due to lower motor neuron lesion at the spinal cord, e.g. poliomyelitis, Charcot-Marie-Tooth disease (an inherited peripheral neuropathy) |
Waddling  |
Weak hip muscles–when the person takes a step, the opposite hip drops, which allows compensatory lateral movement of pelvis. Often, the person also has marked lumbar lordosis and a protruding abdomen | Hip girdle muscle weakness due to muscular dystrophy, dislocation of hips |
Short leg  |
Leg length discrepancy >2.5 cm. Vertical telescoping of affected side, which dips as the person walks. Appearance of gait varies depending on amount of accompanying muscle dysfunction | Congenital dislocated hip; acquired shortening due to disease, trauma |
TABLE 22.8 Characteristics of upper and lower motor neuron lesions
| Upper motor neuron lesion | Lower motor neuron lesion | |
|---|---|---|
| Weakness/paralysis | In muscles corresponding to distribution of damage in pyramidal tract lesion; usually in hand grip, arm extensors, leg flexors | In specific muscles served by damaged spinal segment, ventral root or peripheral nerve |
| Location | Descending motor pathways that originate in the motor areas of cerebral cortex and carry impulses to the anterior horn cells of the spinal cord | Nerve cells that originate in the anterior horn of spinal cord or in brain stem, and carry impulses by the spinal nerves or cranial nerves to the muscles, the ‘final common pathway’ |
| Example | Stroke or cerebrovascular accident | Poliomyelitis, herniated intervertebral disc |
| Muscle tone | Increased tone; spasticity | Loss of tone, flaccidity |
| Bulk | May have some atrophy from disuse; otherwise normal | Atrophy (wasting), may be marked |
| Abnormal movements | None | Fasciculations |
| Reflexes | Hyperreflexia, ankle clonus; diminished or absent superficial abdominal reflexes; positive Babinski’s sign | Hyporeflexia or areflexia; no Babinski’s sign, no pathological reflexes |
| Possible nursing diagnoses | Risk for contractures; impaired physical mobility | Impaired physical mobility |
TABLE 22.10 Common patterns of sensory loss
| Type | Characteristics | Possible causes |
|---|---|---|
Peripheral neuropathy  |
Loss of sensation involves all modalities. Loss is most severe distally (feet and hands); response improves as stimulus is moved proximally (glove-and-stocking anaesthesia). Anaesthesia zone gradually merges into a hypoaesthesia zone, then gradually becomes normal. | Diabetes, chronic alcoholism, nutritional deficiency |
Individual nerves or roots  |
Decrease or loss of all sensory modalities. Area of sensory loss corresponds to distribution of the involved nerve. | Trauma, vascular occlusion |
Spinal cord hemisection (Brown-Séquard syndrome)  |
Loss of pain and temperature, contralateral side, starting one to two segments below the level of the lesion. Loss of vibration and position discrimination on the ipsilateral side, below the level of the lesion. | Meningioma, neurofibroma, cervical spondylosis, multiple sclerosis |
Complete transection of the spinal cord  |
Complete loss of all sensory modalities below the level of the lesion. Condition is associated with motor paralysis and loss of sphincter control. | Spinal cord trauma, demyelinating disorders, tumour |
Thalamus  |
Loss of all sensory modalities on the face, arm and leg on the side contralateral to the lesion. | Vascular occlusion |
Cortex  |
Since pain, vibration and crude touch are mediated by thalamus, little loss of these sensory functions occurs with a cortex lesion. Loss of discrimination occurs on the contralateral side. Loss of graphaesthesia, stereognosis, recognition of shapes and weights, finger finding. | Cerebral cortex, parietal lobe lesion, e.g. stroke |
 |
| Decorticate rigidity |
| Upper extremities–flexion of arm, wrist, and fingers; adduction of arm, i.e. tight against thorax. Lower extremities–extension, internal rotation, plantar flexion. This indicates hemispheric lesion of cerebral cortex. |
 |
| Decerebrate rigidity |
| Upper extremities stiffly extended, adducted, internal rotation, palms pronated. Lower extremities stiffly extended, plantar flexion; teeth clenched; hyperextended back. More ominous than decorticate rigidity; indicates lesion in brainstem at midbrain or upper pons. |
 |
| Flaccid quadriplegia |
| Complete loss of muscle tone and paralysis of all four extremities, indicating completely nonfunctional brainstem. |
 |
| Opisthotonos |
| Prolonged arching of the back, with head and heels bent backwards. This indicates meningeal irritation. |
Images © Pat Thomas, 2006.
TABLE 22.13 Frontal release signs
Snout 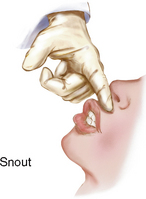 |
|
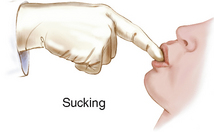 |
|
Shuaing |
|
TABLE 22.14 Abnormal facial appearances with chronic illnesses
 |
| Parkinson’s syndrome |
| A deficiency of the neurotransmitter dopamine and degeneration of the basal ganglia in the brain. The immobility of features produces a face that is flat and expressionless, ‘mask-like’, with elevated eyebrows, staring gaze, oily skin and drooling. |
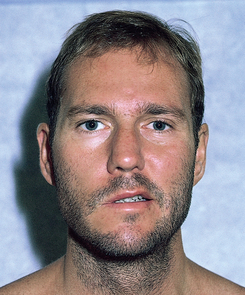 |
| Bell’s palsy (right side) |
| A lower motor neuron lesion (peripheral), producing cranial nerve VII paralysis, which is almost always unilateral. It has a rapid onset and its cause is currently thought to be the herpes simplex virus (HSV). Note complete paralysis of half of the face; the person cannot wrinkle forehead, raise eyebrows, close eye, whistle or show teeth on the right side. Usually presents with smooth forehead, wide palpebral fissure, flat nasolabial fold, drooling and pain behind the ear. |
 |
| An upper motor neuron lesion (central). A ‘stroke’ is an acute neurological de.cit caused by an obstruction of a cerebral vessel, as in atherosclerosis, or a rupture in a cerebral vessel. Note paralysis of lower facial muscles, but also note that the upper half of the face is not affected because of the intact nerve from the unaffected hemisphere. The person is still able to wrinkle the forehead and close the eyes. |
Australian Institute of Health and Welfare (AIHW) and National Heart Foundation of Australia. Heart, stroke and vascular diseases Australian facts 2004. Canberra: AIHW and National Heart Foundation of Australia, 2004.
Australian Institute of Health and Welfare: Australia’s health 2006. Cat. no. AUS 73. Canberra, 2006, AIHW.
——: Australia’s health 2008. Cat. no. AUS 99. Canberra, 2008, AIHW.
Begg S, Vos T, Barker B, et al. The burden of disease and injury in Australia 2003. Canberra: AIHW, 2007.
Beghi E. Epilepsy. Current Opinion in Neurology. 2007;20:169–174.
Bossen AL, Specht JKP, McKenzie SE. Needs of people with early-stage Alzheimer’s disease: reviewing the evidence. Journal of Gerontological Nursing. 2009;35:8–15.
Cordonnier C, Leys D. Stroke: the bare essentials. Practical Neurology. 2008;8:263–272.
Dickson DW, Braak H, Duda JE, et al. Neuropathological assessment of Parkinson’s disease: refining the diagnostic criteria. Lancet Neurology. 2009;8:1150–1157.
Hankey GJ. Clinical update: management of stroke. Lancet. 2007;369:1330–1332.
Iadecola C, Park L, Capone C. Threats to the mind: aging, amyloid, and hypertension. Stroke. 2009;40:S40–S44.
Jaffee MS, Meyer KS. A brief overview of traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD) within the Department of Defense. Clinical Neuropsychologist. 2009;23:1291–1298.
Jevon P. Neurological assessment part 1—assessing level of consciousness. Nursing Times. 2008;104:26–27.
Jevon P. Neurological assessment part 2—pupillary assessment. Nursing Times. 2008;104:26–27.
Jevon P. Neurological assessment part 3—Glasgow Coma Scale. Nursing Times. 2008;104:28–29.
Jevon P. Neurological assessment part 4—Glasgow Coma Scale 2. Nursing Times. 2008;104:24–25.
Juarez VJ, Lyons M. Interrater reliability of the Glasgow Coma Scale. J Neurosci Nurs. 1995;27(5):283–286.
Loring DW, Meador KJ. No kidding: high risk of cognitive difficulty in new-onset pediatric epilepsy. Neurology. 2009;73:496–497.
National Stroke Foundation, 2010: Facts, figures and stats. Available at http://www.strokefoundation.com.au/facts-figures-and-stats.
National Stroke Foundation. Clinical guidelines for acute stroke management. Melbourne: National Stroke Foundation, 2007.
Nelson PT, Braak H, Markesbery WR. Neuropathology and cognitive impairment in Alzheimer disease: a complex but coherent relationship. Journal of Neuropathology & Experimental Neurology. 2009;68:1–14.
New Zealand Ministry of Health. Our health, our future: Hauora pakari, koiora roa. Wellington: Ministry of Health, 1999.
Philip S, Udomphorn Y, Kirkham FJ, et al. Cerebrovascular pathophysiology in pediatric traumatic brain injury. Journal of Trauma—Injury, Infection, & Critical Care. 2009;67:S128–S134.
Pink B, Allbon P. The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples. Canberra: Australian Bureau of Statistics and AIHW, 2008.
Ranjan T, Abrey LE. Current management of metastatic brain disease. Neurotherapeutics. 2009;6:598–603.
Raz N, Lindenberger U, Rodrigue KM, et al. Regional brain changes in aging healthy adults: general trends, individual differences and modifiers. Cereb Cortex. 2005;15:1676–1689.
Rodriguez-Oroz MC, Jahanshahi M, Krack P, et al. Initial clinical manifestations of Parkinson’s disease: features and pathophysiological mechanisms. Lancet Neurology. 2009;8:1128–1139.
Salloway S, Correia S. Alzheimer disease: time to improve its diagnosis and treatment. Cleveland Clinic Journal of Medicine. 2009;76:49–58.
Scanlon A, Sheets Cook S. Febrile seizures, genetic (generalized) epilepsy with febrile seizures plus, and Dravet’s syndrome. Journal for Specialists in Pediatric Nursing. 2010;15(2):154–159.
Senes S. How we manage stroke in Australia. Canberra: AIHW, 2006.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84.
Wasiak R, Young AE, Dunn KM, et al. Back pain recurrence: an evaluation of existing indicators and direction for future research. Spine. 2009;34:970–977.