Interventional Radiology
At the completion of this chapter, the student should be able to do the following:
1 Describe the measures used to provide radiation protection for patients and personnel during interventional radiology.
2 Describe the reasons why minimally invasive (percutaneous) vascular procedures often are more beneficial than traditional surgical procedures.
3 Discuss the advantages that nonionic (water-soluble) contrast media offer over ionic contrast media.
4 Identify the risks of arteriography.
5 Describe the special equipment found in the interventional radiology suite.
IN PREVIOUS years, myelography and venography were considered special procedures. Recently, the area of therapeutic angiographic intervention has undergone rapid development. We now have suites of x-ray rooms and complex equipment that have been specially designed for interventional radiology (IR).
The following discussion concerns various IR procedures and the special x-ray equipment necessary to perform such procedures.
Isn’t it interesting how advances in technology are accompanied by changes in terminology? We made radiographs with x-rays because that is what Roentgen named them. X is the mathematical symbol for “unknown,” which is how Roentgen viewed his discovery.
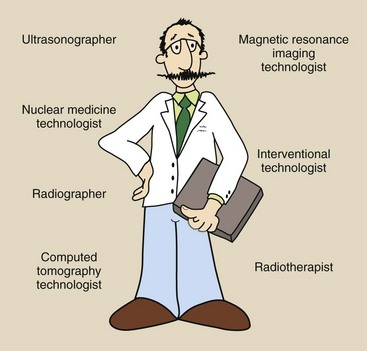
As imaging technology has developed, so has our identity. First, we were called x-ray operators, then technicians, and now radiologic technologists or, more specifically, radiographers. A radiologic technologist can be a radiographer, a nuclear medicine technologist, or another imaging technologist (Figure 27-1).
In the same way that radiologic technology has been more precisely divided into disciplines, so has our imaging task. We used to do special procedures, such as pneumoencephalography, myelography, and neuroangiography. The rapid development of vascular imaging and aggressive therapeutic intervention through vessels has resulted in rooms and equipment designed especially for interventional radiologic procedures. The radiologic technologists involved are interventional radiologic technologists.
Types of Interventional Procedures
Interventional radiology procedures began in the 1930s with angiography; needles and contrast media were used to enter and highlight an artery. In the early 1960s, Mason Jones pioneered transbrachial selective coronary angiography—entering select coronary arteries through an artery of the arm.
Also during the 1960s, transfemoral angiography—entering an artery in the thigh—of selective visceral, heart, and head arteries was developed. Melvin Judkins introduced coronary angiography, and Charles Dotter introduced visceral angiography.
Angiography refers to the opacification of vessels through injection of contrast media. Angioplasty, thrombolysis, embolization, vascular stents, and biopsy are interventional therapeutic procedures that are conducted in and through vessels. Table 27-1 lists the types of imaging and interventional procedures that are likely to be conducted in an IR suite.
TABLE 27-1
Representative Procedures Conducted in an Interventional Radiology Suite
| Imaging Procedures | Interventional Procedures |
| Angiography | Stent placement |
| Aortography | Embolization |
| Arteriography | Intravascular stent |
| Cardiac catheterization | Thrombolysis |
| Myelography | Balloon angioplasty |
| Venography | Atherectomy |
| Electrophysiology |
Basic Principles
In 1953, Sven Ivar Seldinger described a method of arterial access in which a catheter was used. The Seldinger needle is an 18-gauge hollow needle with a stylet. After the Seldinger needle is inserted into the femoral artery and pulsating arterial blood returns, the stylet is removed.
A guidewire then is inserted through the needle into the arterial lumen. With the guidewire in the vessel, the Seldinger needle is removed, and a catheter is threaded onto the guidewire. Under fluoroscopic view, the catheter then is advanced along the guidewire.
In angiography, the common femoral artery is most often used for arterial access. The common femoral artery can be palpated by locating the pulse in the groin below the inguinal ligament, which passes between the symphysis pubis and the anterior superior iliac spine.
Guidewires
After the catheter is in place, the guidewire allows the radiologist to position the catheter within the vascular network.
Guidewires are fabricated of stainless steel and contain an inner core wire that is tapered at the end to a soft, flexible tip. This core wire prevents loss of sections of the wire if it breaks. The trailing end of the guidewire is stiff and allows the guidewire to be pushed and twisted so the catheter can be positioned in the chosen vessel.
Conventional guidewires are 145 cm long. Catheters overlaying the guidewire are usually 100 cm long or less. Guidewires are categorized additionally by length to the beginning of the tapered tip, configuration of the tip, stiffness of the guidewire, and coating. They are coated with a hydrophilic material so the catheter slides over the wire more easily. This coating makes guidewires more resistant to thrombus (blood clot) and easier to irrigate while they are in the vascular system.
The J-tip for guidewires is a variation of the tip configuration that was initially designed for use in atherosclerotic vessels filled with plaque. The J-tip deflects off the edges of plaques and helps prevent subintimal dissection of the artery. The coatings on guidewires are materials that are designed to reduce friction; they include Teflon, heparin coatings, and, more recently, hydrophilic polymers. The latter type, called a glide wire, represents a major technologic advance in IR.
Catheters
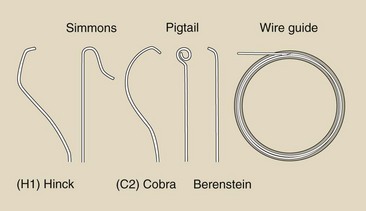
Similar to guidewires, catheters are designed in many different shapes and sizes. Usually, catheter diameter is categorized in French (Fr) sizes, with 3 Fr equaling 1 mm in diameter. Figure 27-2 illustrates four common catheter shapes.
The H1 or headhunter tip designed by Vincent Hinck is used for the femoral approach to the brachiocephalic vessels. The Simmons catheter is highly curved for approach to sharply angled vessels and was also designed for cerebral angiography but was later adopted for visceral angiography. The C2 or Cobra catheter has an angled tip joined to a gentle curve and is used for introduction into celiac, renal, and mesenteric arteries.
Pigtail catheters have side holes for ejecting contrast media into a compact bolus. A catheter with side holes helps reduce a possible whiplash effect. The jet effect is minimized with the curved pigtail, which prevents injury to the vessel.
After the catheter is introduced into the vessel, the guidewire is removed. The catheter then must be flushed immediately to prevent clotting of blood within the catheter. Heparinized saline generally is used to flush catheters.
After catheter placement, a test injection is performed under fluoroscopy before static imaging to check that the catheter tip is not wedged and that it is in the correct vessel. Injection rates of the automatic power injector are gauged by the test flow speed.
Contrast Media
Vessels under investigation in angiography are injected with radiopaque contrast media. Initially, ionic iodine compounds were used for contrast injections; however, nonionic contrast media have largely replaced ionic agents. Because of their low concentration of ions (low osmolality), physiologic problems and adverse reactions are reduced for patients undergoing angiographic injection with nonionic contrast media.
Patient Preparation and Monitoring
Before angiography is performed, the radiologist visits the patient to establish rapport and to explain the procedure and its risks. A history and physical examination are necessary to assess the patient for allergies and other conditions so the radiologist can conclude whether a procedure is indicated and which route is optimal. Orders are written for intravenous hydration and a diet of clear liquids. The patient may be premedicated in the IR suite to reduce anxiety.
During the procedure, monitoring by electrocardiography, automatic blood pressure measurement, and pulse oximetry is mandatory. The code or “crash” cart for life-threatening emergencies must be accessible.
After the procedure has been performed, when the catheter is removed, the femoral puncture site must be manually compressed. The patient then is instructed to remain immobile for several hours after the angiographic procedure has been completed while vital signs are monitored and the puncture site inspected.
Risks of Arteriography
The most common complication associated with catheter angiography is continued bleeding at the puncture site. Of course, the risk of reaction to contrast media is present, and other risk factors are related to kidney failure. Minimization of these risks requires a complete patient medical examination and the taking of surgical and allergy histories before any angiographic procedure can be done. Although uncommon, serious adverse reactions related to blood clot formation or catheter or guidewire penetrating injury can occur.
Interventional Radiology Suite
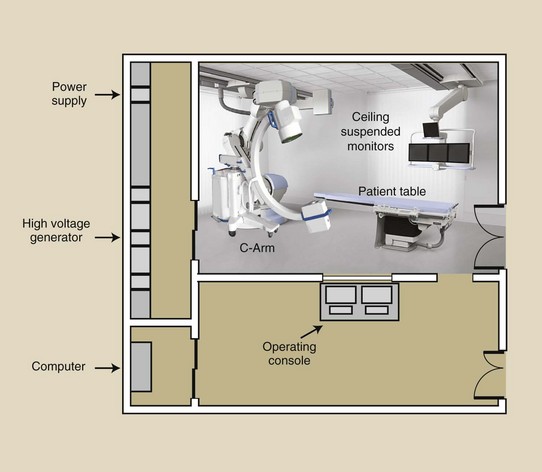
Different from radiography and fluoroscopy, IR requires a suite of rooms (Figure 27-3). The procedure room itself should not be less than 20 ft along any wall and not less than 500 ft2. This size is necessary to accommodate the quantity of equipment required and the large number of people involved in most procedures.
The procedure room usually has at least three means of access. Patient access should be available through a door wide enough to accommodate a bed. Access to the procedure room from the control room with the operating console does not usually require a door. An open passageway is adequate. Such doors interfere with movement of personnel.
The procedure room should be finished with consideration for maintaining a clean and sterile environment. The floor, walls, and all counter cabinet surfaces must be smooth and easily cleaned.
The control room should be large, perhaps 100 ft2. Ideally, this room should communicate directly with the viewing areas. It also should have positive air pressure and filtered incoming air.
Personnel
A radiographer can specialize in many different fields. A radiographer who specializes in IR requires additional skills. The American Registry of Radiologic Technologists offers an examination in cardiovascular and interventional radiography. After the examination is passed, the radiographer may add (CI) or (VI) after the RT (R).
Two or three radiographers may be present in the IR suite, as well as the interventional radiologist and a radiology nurse, who carefully monitors the patient. During procedures that require the patient to be highly medicated, an anesthesiologist also may be present.
Equipment
The x-ray apparatus for an IR suite is generally more massive, flexible, and expensive than that required for conventional radiographic and fluoroscopic imaging. Advanced radiographic and fluoroscopic equipment is required (Figure 27-4). Generally, two ceiling track–mounted radiographic x-ray tubes are required along with a digital fluoroscope mounted on a C- or an L-arm.
X-ray Tube
The x-ray tube used for IR procedures has a small target angle, a large-diameter massive anode disc, and cathodes designed for magnification and serial radiography. Table 27-2 describes the specifications for such an x-ray tube.
TABLE 27-2
Specifications for a Typical Interventional Radiology X-ray Tube
| Feature | Size | Why |
| Focal spot | 1.0 mm/0.3 mm | Large for heat load; small for magnification radiography |
| Disc size | 15-cm diameter; 5 cm thick | To accommodate heat load |
| Power rating | 80 kW | For rapid sequence, serial radiography |
| Anode heat capacity | 1 MHU | To accommodate heat load |
A small focal spot of not greater than 0.3 mm is necessary for the spatial resolution requirements of small-vessel magnification radiography. Neuroangiography can be performed in contrast-filled vessels as small as 1 mm with typical selection of geometric factors and careful patient positioning.
When a source-to-image receptor distance (SID) of 100 cm and an object-to-image receptor distance (OID) of 40 cm are used, the radiographer can take advantage of the air gap to improve image contrast. A 0.3-mm focal spot results in a focal-spot blur of 0.2 mm.
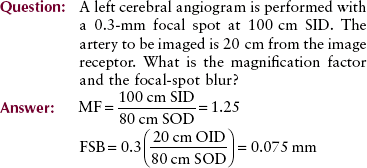
Spatial resolution for this procedure can be approximated by multiplying the focal-spot blur by 2. Figure 27-5 shows geometry that results in 0.2-mm focal-spot blur images of a 1.0-mm vessel. A 0.5-mm vessel will be too blurred to be seen. Any vessel larger than 1.0 mm will be imaged.
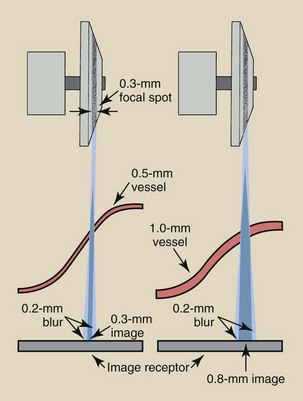
FIGURE 27-5 For a given geometry such as this one, which produces a 0.2-mm focal-spot blur, the vessels must be twice the size of the focal-spot blur.
All other essential characteristics of an interventional x-ray tube are based on required tube loading. The size and construction of the anode disc determine the anode heat capacity, which in turn influences the power rating. An x-ray tube with a minimum 80 kW rating and 1 MHU heat capacity is required.
High-Voltage Generator
High-frequency generators are increasingly popular in all x-ray examinations, including IR procedures. However, some IR procedures require higher power than may be available with high-frequency generators. High-voltage generators with three-phase, 12-pulse power capable of at least 100 kW with low ripple are needed for such high power requirements.
Patient Couch
Whereas most general fluoroscopy imaging systems have a tilt table, IR imaging systems do not. General fluoroscopy often requires head-down and head-up tilting of the patient for manipulation of contrast media. Imaging techniques such as myelography require a tilt couch; therefore, such procedures are common in general fluoroscopy.
Other imaging and interventional procedures do not require a tilt couch, but a stationary patient couch with a floating or movable tabletop is used instead (Figure 27-6). Controls for couch positioning are located on the side of the table and are duplicated on a floor switch. The floor switch is necessary to accommodate patient positioning while a sterile field is maintained.
FIGURE 27-6 Typical interventional radiology patient couch with a floating, rotating, and tilting top. (Courtesy Odelft Corporation.)
The patient couch may have computer-controlled stepping capability. This feature is necessary to allow imaging from the abdomen to the feet after a single injection of contrast medium. An additional requirement of this stepping feature is the ability to preselect the time and position of the patient couch to coincide with the image receptor.
Image Receptor
Several different types of digital image receptors can be used in IR procedures. The digital image receptor begins with a television camera pickup tube or a charge-coupled device (CCD).
Charge-coupled devices are photosensitive silicon chips that are rapidly replacing the television camera tube in the fluoroscopic chain. CCDs resemble computer chips and can be used anywhere that light is to be converted to a digital video image. CCDs are discussed in Chapter 26.
Flat panel image receptors, also described in Chapter 26, are now the image receptor of choice for IR. Imaging system advances for IR have been driven largely out of concerns for patient radiation dose, covered more completely in Chapter 39.
Summary
Angiography refers to the many ways of imaging contrast-filled vessels. In 1953, Sven Ivan Seldinger described a method of arterial access that uses an 18-gauge hollow needle with a stylet. Using a guidewire and a catheter, radiologists can access the vascular network without surgery. The common femoral artery is used most often for arterial access in angiography.
Catheter tip designs vary widely, and each is used for specific arteries. The contrast media used are generally nonionic; this reduces the incidence of physiologic problems and adverse reactions in patients undergoing angiographic procedures. During the procedure, the patient’s vital signs must be monitored carefully. The most common risk to patients is continued bleeding at the puncture site.
The typical interventional radiologic x-ray tube is designed for magnification, high spatial resolution, and massive heat loads. The patient couch is a floating tabletop with a stepping capability that automatically allows imaging from abdomen to feet after a single injection of contrast media.
Digital imaging is used for interventional procedures with power injection of contrast media and imaging synchronized to optimize visualization of the vessel of interest.
1. Define or otherwise identify the following:
2. Describe cardiac catheterization.
3. What is the Seldinger method for arterial access?
4. What artery is used most often for arterial access in angiography?
5. Why is a guidewire used for arterial access of catheters?
6. List four types of catheters and the vessels for which they are designed.
7. Name two reasons why the radiologist visits the patient before an interventional radiologic procedure is performed.
8. What is the most common problem that patients encounter after an interventional radiologic procedure?
9. What are thrombolysis and embolization?
10. What is the required heating capacity of the interventional x-ray tube?
11. Name the titles and describe the duties of the team of personnel who work in the IR suite.
12. List the focal-spot requirements for the interventional x-ray tube. For what procedure is the small focal spot used?
13. What does it mean when the patient couch has a stepping capability?
14. Name the frame rates for a cine camera.
15. List three “special procedures.”
16. What is transbrachial selective coronary angiography?
17. Why are some catheters fenestrated (pierced with holes)?
18. How does osmolarity affect the action of a contrast agent?
19. What is the recommended minimum size for an IR suite?
20. What initials may an ARRT with a specialty in IR place as a title postscript?
The answers to the Challenge Questions can be found by logging on to our website at http://evolve.elsevier.com.