Occupational Radiation Dose Management
At the completion of this chapter, the student should be able to do the following:
1 Discuss the units and concepts of occupational radiation exposure
2 Discuss ways to reduce occupational radiation exposure
3 Explain occupational radiation monitors and where they should be positioned
RADIATION DOSE is measured in units of Gyt (rads). Radiation exposure is measured in Gya (roentgens). When the exposure is to radiologic technologists and radiologists, the proper unit is the (rem).
The Sv is the unit of effective dose; it is used for radiation protection purposes. Although exposure, dose, and effective dose have precise and different meanings, they often are used interchangeably in radiology because they have approximately the same numeric value following whole-body exposure.
When properly used, exposure (Gya, R) refers to radiation intensity in air. Dose (Gyt, rad) measures the radiation energy absorbed as a result of radiation exposure; it is used to identify irradiation of patients. Effective dose (Sv, rem) identifies the biologic effectiveness of the radiation energy absorbed. This unit is applied to occupationally exposed persons and to population exposure, and the SI unit the sievert (Sv) is preferred because all regulations are expressed in sievert.
Occupational Radiation Exposure
Although the recommended dose limit for radiologic personnel is 0.5 Sv/yr (5000 mrem/yr), experience has shown that considerably lower exposures than this are routine. The occupational radiation exposure of radiologic personnel engaged in general x-ray activity normally should not exceed 1 mSv/yr (100 mrem/yr).
Radiologists usually receive slightly higher exposures than radiologic technologists. This is because the radiologist receives most of his or her exposure during fluoroscopy and is usually closer to the radiation source—the patient—during such procedures. Table 38-1 reports the results of an analysis of the annual occupational radiation exposure of radiologic personnel. Clearly, the radiation exposures are low.
TABLE 38-1
Occupational Radiation Exposure of Radiologic Personnel
| Exposure Category | Value |
| Average whole-body dose | 0.7 mSv/yr |
| Those receiving less than the minimum detectable dose | 53% |
| Those receiving <1 mSv/yr | 88% |
| Those receiving >50 mSv/yr | 0.05% |
Fluoroscopy
Unquestionably, the highest occupational exposure of diagnostic x-ray personnel occurs during fluoroscopy and mobile radiography. During radiographic exposure, the radiologist is rarely present and the radiologic technologist is behind the console protective barrier.
When fixed protective barriers are not available, such as during mobile examination, the mobile x-ray imaging system is equipped with an exposure cord long enough to allow the technologist to leave the immediate examination area. The radiologic technologist should wear a protective apron for each such mobile examination.
During fluoroscopy, both radiologist and radiologic technologist are exposed to relatively high levels of radiation. Personnel exposure, however, is related directly to the x-ray beam-on time. With care, personnel exposures can be kept as low as reasonably achievable (ALARA).
| Question: | A barium enema examination requires 2.5 minutes of fluoroscopic x-ray beam time. If the radiographer is exposed to 2.5 Gya/hr, what will be his or her occupational radiation exposure? |
| Answer: | Exposure = Exposure rate × Time = 2.5 Gya/hr × 2.5 minutes = 2.5 Gya/hr × 0.0417 hour = 0.1 mGya |
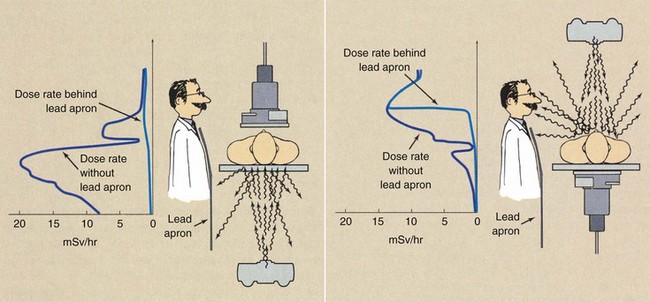
Remote fluoroscopy results in low personnel exposures because personnel are not in the x-ray examination room with the patient. With some fluoroscopes, the x-ray tube is over the table and the image receptor under the table. This geometry offers some advantage in terms of image quality, but personnel exposures are higher because secondary radiation (scatter and leakage) levels are higher.
This condition should be kept in mind during mobile and C-arm fluoroscopy. It is best to position the x-ray tube under the patient during C-arm fluoroscopy (Figure 38-1).
Interventional Radiology
Personnel engaged in interventional radiology procedures often receive higher exposures than do those in general radiologic practice because of longer fluoroscopic x-ray beam-on time. The frequent absence of a protective curtain on the image-intensifier tower and the use of cineradiography also contribute to higher personnel exposure.
Extremity exposure during interventional radiology procedures may be significant. Even with protective gloves, exposure of the forearm can approach the recommended dose limit of 500 mSv/yr (50 rem/yr) if care is not taken. Without protective gloves, excessive hand exposures are possible.
Mammography
Personnel exposures associated with mammography are low because the low kVp of operation results in less scatter radiation. Usually, a long exposure cord and a conventional wall or window wall are sufficient to provide adequate protection.
Rarely does a room that is used strictly for mammography require protective lead shielding. Dedicated mammography x-ray units have personnel protective barriers made of lead glass, lead acrylic, and even plate glass as an integral component. Usually, such barriers are totally adequate.
Computed Tomography
Personnel exposures in computed tomography (CT) facilities are low. Because the CT x-ray beam is finely collimated and only secondary radiation is present in the examination room, radiation levels are low compared with those experienced in fluoroscopy. Figure 38-2 shows the isoexposure profiles for the horizontal and vertical planes of a multislice helical CT imaging system. These data are given as mGya/360 degrees rotation, and they show that personnel can be permitted to remain in the room during imaging. However, protective apparel should always be worn in such situations.
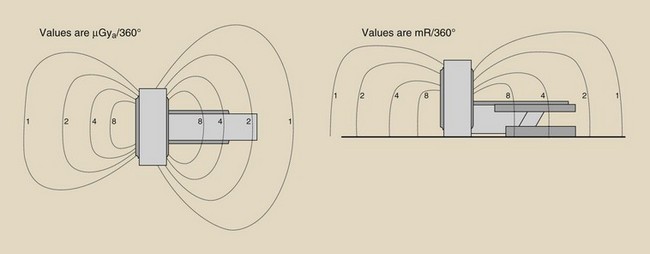
FIGURE 38-2 Isoexposure profiles (in mR/360 degrees) in horizontal and vertical planes for multislice spiral computed tomography.
| Question: | It is necessary for a radiologic technologist to remain in the CT room at midtable position during a 20-rotation examination. What would be the occupational exposure if no protective apron were worn? |
| Answer: | From Figure 38-2, we may assume an exposure of 1 µGya/scan. Occupational exposure = 1 µGya/scan × 2 = 2 µGya Of course, with a protective apron the trunk of the body would receive essentially zero exposure. |
Surgery
Nursing personnel and others working in the operating room and in intensive care units are sometimes exposed to radiation from mobile x-ray imaging systems and C-arm fluoroscopes. Although these personnel are often anxious about such exposures, many studies have shown that their occupational exposure is near zero and certainly is no cause for concern. It usually is not necessary to provide occupational radiation monitors for such personnel.
Mobile Radiology
Occupational radiation monitors are not necessary during mobile radiography, except as used with the radiologic technologist and anyone who is required to immobilize or hold patients. Personnel who regularly operate or are in the immediate vicinity of a C-arm fluoroscope should wear an occupational radiation monitor, in addition to protective apparel. During C-arm fluoroscopy, the x-ray beam may be on for a relatively long time, and the beam can be pointed in virtually any direction.
It should never be necessary for radiologic personnel to exceed 50 mSv/yr (5000 mrem/yr). In smaller hospitals, emergency centers, and private clinics, occupational exposures rarely exceed 5 mSv/yr (500 mrem/yr). As Table 38-1 reported, average exposures in most facilities are less than 1 mSv/yr (100 mrem/yr).
Radiation Dose Limits
A continuing effort of health physicists has been the description and identification of occupational dose limits. For many years, a maximum permissible dose (MPD) was specified. The MPD was the dose of radiation that would be expected to produce no significant radiation effects.
At radiation doses below the MPD, no responses should occur. At the level of the MPD, the risk is not zero, but it is small—lower than the risk associated with other occupations and reasonable in light of the benefits derived. The concept of MPD is now obsolete and has been replaced by dose limits (DLs).
Whole-Body Dose Limits
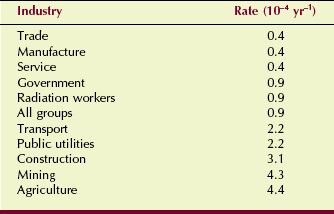
To establish DLs, the National Council on Radiation Protection and Measurements (NCRP) assessed risk on the basis of data from reports of the National Academy of Sciences (Biologic Effects of Ionizing Radiation [BEIR] Committee) and the National Safety Council (Table 38-2). State and federal government agencies routinely adopt these recommended dose limits as law. Current DLs are prescribed for various organs as well as for the whole body, and for various working conditions. If one received the DL each year, the lifetime risk would not exceed 10−4 yr−1.
The value 10−4 yr−1represents the approximate risk of death for those working in safe industries. The DLs recommended by the NCRP ensure that radiation workers have the same risk as those in safe industries.
| Question: | Suppose all 300,000 American radiologic technologists receive the DL (50 mSv) this year. How many would be expected to die prematurely |
| Answer: | (300,000) (10−4) = 30 But of course, they actually receive approximately 0.5m Sv/year; therefore, the expected mortality is as follows: 30 (0.5)/(50) = 0.3; less then 1!Particular care is taken to ensure that no radiation worker receives a radiation dose in excess of the DL. The DL is specified only for occupational exposure. It should not be confused with medical x-ray exposure received as a patient. Although patient dose should be kept low, there is no patient DL. |
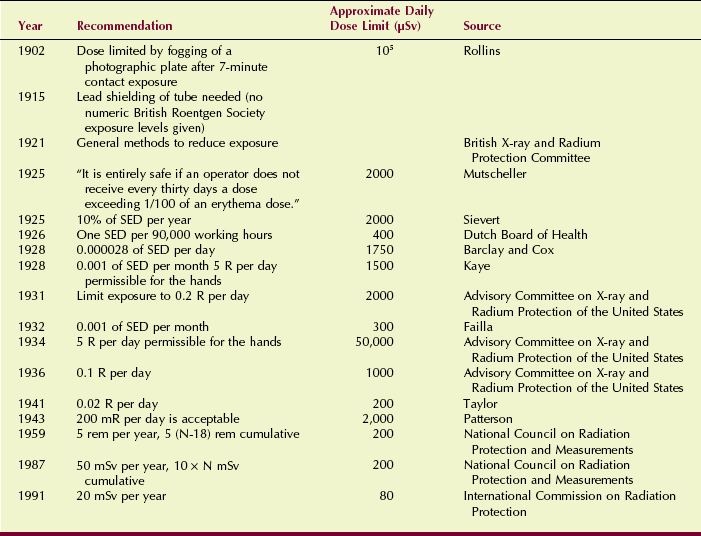
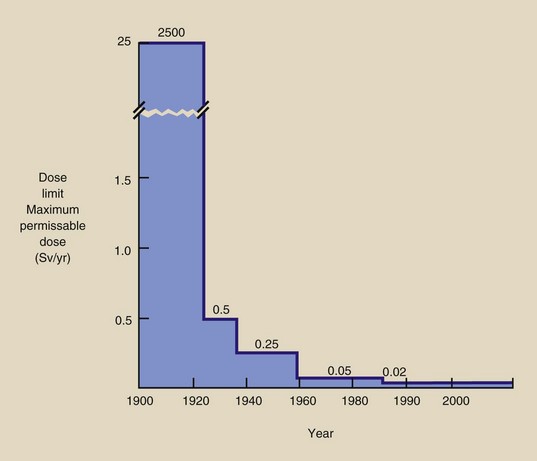
The first DL—500 mSv/wk (50,000 mrem/wk)—was recommended in 1902. The current DL is 1 mSv/wk (100 mrem/wk). Through the years, a downward revision of the DL has occurred. The history of these continuing recommendations is given in Table 38-3 and is shown graphically in Figure 38-3.
In the early years of radiology, the DL consisted of a single value that was considered the safe working level for whole-body exposure. It was based primarily on the known acute response to radiation exposure and presumed that a threshold dose existed.
Today, the DL is specified not only for whole-body exposure but also for partial-body exposure, organ exposure, and exposure of the general population, again excluding medical exposure as a patient and exposure from natural sources (Table 38-4). The DLs included in Table 38-4 were published first by the NCRP in 1987 and were refined in 1993. They replaced the previous MPDs, which had been in effect since 1959. These DLs have been adopted by state and federal regulatory agencies and are now the law of the United States. Note that International System (SI) units are preferred.
TABLE 38-4
Dose Limits Recommended by the National Council on Radiation Protection and Measurements
The basic annual DL is 50 mSv/yr (5000 mrem/yr). The DL for the lens of the eye is 150 mSv/yr (15 rem/yr), and that for other organs is 500 mSv/yr (50 rem/yr).
The cumulative whole-body DL is 10 mSv (1000 mrem) times age in years. The DL during pregnancy is 5 mSv (500 mrem), but once pregnancy has been declared, monthly exposure shall not exceed 0.5 mSv (50 mrem).
In practice, at least in diagnostic radiology, it is seldom necessary to exceed even 1/10 the appropriate DL. However, because the basis for the DL assumes a linear, nonthreshold dose-response relationship, all unnecessary radiation exposure should be avoided.
Occupational exposure is described as dose equivalent in units of millisievert (millirem). DLs are specified as effective dose (E). This scheme has been adopted to afford enhanced precision in radiation protection practices.
The effective dose (E) concept accounts for different types of radiation because of their varying relative biologic effectiveness. Effective dose also considers the relative radiosensitivity of various tissues and organs.
These are particularly important considerations when a protective apron is worn. Wearing a protective apron reduces radiation dose to many tissues and organs to near zero. Therefore, effective dose is much less than that recorded by a collar-positioned radiation monitor.
Adoption of this scheme is progressing. For our purposes, effective dose (E) is the quantity of importance. It is expressed in mSv (mrem) and forms the basis for our DLs.
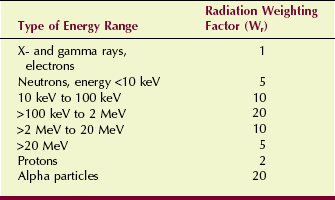
As can be seen in Table 38-5, the radiation weighting factor (Wr) is equal to 1 for the types of radiation used in medicine. The value of Wr for other types of radiation depends on the linear energy transfer (LET) of that radiation.
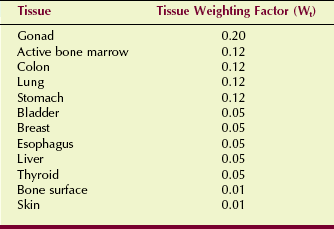
The tissue weighting factor (Wt) accounts for the relative radiosensitivity of various tissues and organs. Tissues with a higher value of Wt are more radiosensitive. These are shown in Table 38-6.
Practical implementation of these DLs and weighting factors does not change our previous approach. The DL is sufficiently high that it rarely, if ever, is exceeded in diagnostic radiology.
With a collar-positioned radiation monitor, a change in procedure is necessary to estimate effective dose (E). Because essentially all of our radiation exposure occurs during fluoroscopy and the trunk is shielded by a lead apron, the response of the monitor overestimates the effective dose (E).
A conversion factor of 0.3 should be applied to the collar monitor–reported value to estimate effective dose (E). If a protective apron is not worn (e.g., by a radiographer who does no fluoroscopy), then the monitor response may be considered the effective dose.
Dose Limits for Tissues and Organs
The whole-body DL of 50 mSv/yr (5000 mrem/yr) is an effective dose, which takes into account the weighted average to various tissues and organs. In addition, the NCRP has identified several specific tissues and organs with specific recommended dose limits.
Skin
Some organs of the body have a higher DL than the whole-body DL. The DL for the skin is 500 mSv/yr (50 rem/yr).
This limit is not normally of concern in diagnostic radiology because it applies to nonpenetrating radiation such as alpha and beta radiation and very soft x-rays. Radiologic technologists exclusively engaged in mammography or nuclear medicine are highly unlikely to sustain radiation exposure to the skin in excess of 10 mSv/yr (1000 mrem/yr).
Extremities
Radiologists often have their hands near the primary fluoroscopic radiation beam; therefore, extremity exposure may be of concern. The DL for the extremities is the same as that for the skin—500 mSv/yr (50 rem/yr).
These radiation levels are quite high and under normal circumstances should not even be approached. For certain occupational groups, such as interventional radiologists and nuclear medicine technologists, extremity personnel monitors should be provided. Such devices are worn on the wrist or the finger.
Public Exposure
Individuals in the general population are limited to 1 mSv/yr (100 mrem/yr). For hospital workers who are not radiology employees but who may regularly visit x-ray rooms, the DL is 1 mSv/yr (100 mrem/yr).
This value of 1 mSv/yr is the DL that medical physicists use when computing the thickness of protective barriers. If a barrier separates an x-ray examining room from an area occupied by the general public, the shielding is designed so that the annual exposure of an individual in the adjacent area cannot exceed 1 mSv/yr (100 mrem/yr).
If the adjacent area is occupied by radiation workers, the shielding must be sufficient to maintain an annual exposure level less than 10 mSv/yr (1000 mrem/yr). This approach to shielding derives from the 10 mSv × N cumulative DL.
Radiation exposure of the general public or of individuals in this population is measured rarely because this process is not necessary. Most radiology personnel do not receive even this level of exposure.
Educational Considerations
Several special situations are associated with whole-body occupational DL. Students younger than 18 years of age may not receive more than 1 mSv/yr (100 mrem/yr) during the course of their educational activities. This is included in and is not added to the 1 mSv (100 mrem) permitted each year as a nonoccupational exposure.
Consequently, student radiologic technologists younger than 18 years of age may be engaged in x-ray imaging, but their exposure must be monitored and must remain below 1 mSv/yr (100 mrem/yr). Because of this, it is general practice not to accept underage persons into schools of radiologic technology unless their 18th birthday is within sight.
In keeping with ALARA, even more changes in DL are on the way. The International Commission on Radiological Protection (ICRP) has issued several recommendations, including an annual whole-body DL of 20 mSv (2000 mrem). Such a reduction is currently under consideration in the United States.
Reduction of Occupational Radiation Exposure
The radiologic technologist can do much to minimize occupational radiation exposure. Most exposure control procedures do not require sophisticated equipment or especially rigorous training, but simply a conscientious attitude regarding the performance of assigned duties. Most equipment characteristics, technique changes, and administrative procedures designed to minimize patient dose also reduce occupational exposure.
In diagnostic radiology, at least 95% of the radiologic technologist’s occupational radiation exposure comes from fluoroscopy and mobile radiography. Attention to the cardinal principles of radiation protection (time, distance, and shielding) and ALARA are the most important aspects of occupational radiation control.
During fluoroscopy, the radiologist should minimize x-ray beam-on time. This can be done through careful technique, which includes intermittent activation of fluoroscopic views rather than one long period of x-ray beam-on time. It is a common radiation protection practice to maintain a log of fluoroscopy time by recording x-ray beam-on time with the 5-minute reset timer.
During fluoroscopy, the radiologic technologist should step back from the table when his or her immediate presence and assistance are not required. The radiologic technologist also should take maximum advantage of all protective shielding, including apron, curtain, and Bucky slot cover, as well as the radiologist.
The radiologic technologist should wear a protective apron during all mobile examinations and should maintain maximum distance from the source. The primary beam should never be pointed at the radiologic technologist or other nearby personnel.
During radiography, the radiologic technologist is positioned behind a control booth barrier. Such barriers usually are considered secondary barriers because they intercept only leakage and scatter radiation. Consequently, leaded glass and leaded gypsum board are often unnecessary for such barriers.
Other work assignments in diagnostic imaging, such as scheduling, darkroom duties, and filing, result in essentially no occupational radiation exposure.
Occupational Radiation Monitoring
The level of occupational exposure to radiologists and radiologic technologists depends on the type and frequency of activity in which they are engaged. Determining the quantity of radiation they receive requires a program of occupational radiation monitoring. Occupational radiation monitoring refers to procedures instituted to estimate the amount of radiation received by individuals who work in a radiation environment.
Most clinical diagnostic imaging personnel must be monitored; however, it usually is not necessary to monitor diagnostic radiology secretaries and file clerks. Furthermore, it usually is not necessary to monitor operating room personnel, except perhaps those routinely involved in cystoscopy and C-arm fluoroscopy.
The occupational radiation monitor simply measures the quantity of radiation to which the monitor was exposed; therefore, it is simply an indicator of exposure to the wearer. Basically, three types of personnel monitors are used in diagnostic radiology: film badges, thermoluminescence dosimeters (TLDs), and optically stimulated luminescence dosimeters (OSLs).
Regardless of the type of monitor used, it is essential that it be obtained from a certified laboratory. In-house processing of radiation monitors should not be attempted. Figure 38-4 presents a view of two typical occupational radiation monitors.
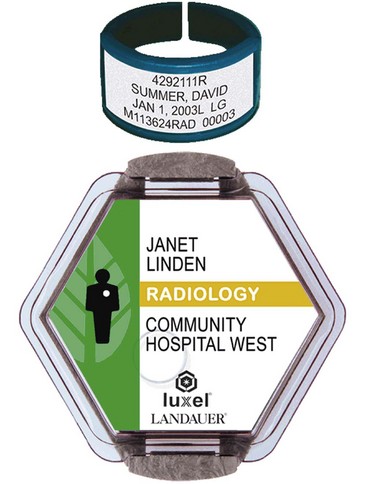
FIGURE 38-4 Some representative radiation monitors. In many, metal filters are incorporated to help identify the type of radiation and its energy. (Courtesy Landauer, Inc.)
Film Badges
Film badges came into general use during the 1940s and have been used widely in diagnostic radiology ever since. Film badges are specially designed devices in which a film similar to dental radiographic film is sandwiched between metal filters inside a plastic holder.
The film incorporated into a film badge is special radiation dosimetry film that is particularly sensitive to x-rays. The optical density on the exposed and processed film is related to the exposure received by the film badge.
Carefully controlled calibration, processing, and analyzing conditions are necessary for the film badge to measure accurately occupational radiation exposure. Usually, exposures less than 10 mR (100 µGya) are not measured by film badge monitors, and the film badge vendor will report only that a minimum exposure (M) was received. When higher exposures are received, they can be reported accurately.
The metal filters, along with the window in the plastic film holder, allow estimation of the x-ray energy. The usual filters are made of aluminum and copper.
When the radiation exposure is a result of penetrating x-rays, the image of the filters on the processed film is faint, and there may be no image at all of the window in the plastic holder. If the badge is exposed to soft x-rays, the filters are well imaged and the optical densities under the filters allow estimation of x-ray energy.
Often, the filters to the front of the film badge differ in shape from the filters to the back of the film badge. Radiation that had entered through the back of the film badge normally would indicate that the person wearing the badge received considerably higher exposure than indicated, because the x-rays would have penetrated through the body before interacting with the film badge.
Several advantages of film badge occupational radiation monitors continue to make them popular. They are inexpensive, easy to handle, easy to process, and reasonably accurate, and they have been in use for several decades.
Film badge monitors also have disadvantages. They cannot be reused, and because they incorporate film as the sensing device, they cannot be worn for longer than 1 month because of possible fogging caused by temperature and humidity.
Film badge monitors should never be left in an enclosed car or other area where excessive temperatures may occur. The fogging produced by elevated temperature and humidity results in a falsely high evaluation of radiation exposure.
Thermoluminescence Dosimeters
The sensitive material of the TLD monitor (Figure 38-5) is lithium fluoride (LiF) in crystalline form, either as a powder or more often as a small chip approximately 3 mm square and 1 mm thick. When exposed to x-rays, the TLD absorbs energy and stores it in the form of excited electrons in the crystalline lattice.

FIGURE 38-5 Thermoluminescence dosimeters are available as chips, discs, rods, and powder. These are used for area and environmental radiation monitoring, and especially for occupational radiation monitoring. (Courtesy Bicron.)
When heated, these excited electrons fall back to their normal state with the emission of visible light. The intensity of visible light is measured with a photomultiplier tube or photodiode and is proportional to the radiation dose received by the crystal. This sequence was described in Chapter 35.
The TLD occupational radiation monitor offers several advantages over film. It is more sensitive and more accurate than a film badge monitor. Properly calibrated TLD monitors can measure exposure as low as 50 µGya (5 mR). The TLD monitor does not suffer from loss of information after it is exposed to excessive heat or humidity.
The primary disadvantage of TLD personnel monitoring is cost. The price of a typical TLD monitoring service is perhaps twice that of film badge monitoring. If the frequency of monitoring is quarterly, however, the cost is about the same.
Optically Stimulated Luminescence
OSL dosimeters (Figure 38-6) are worn and handled just as film badges and TLDs are, and they are approximately the same size. OSL dosimeters have one advantage over TLDs. They are more sensitive, measuring as low as 10 µGya (1 mR).
Where to Wear the Occupational Radiation Monitor
Much discussion and research in health physics have gone into providing precise recommendations about where a radiologic technologist should wear the occupational radiation monitor. Official publications of the NCRP offer suggestions that have been adopted as regulations in most states.
Many radiologic technologists wear their personnel monitors in front at waist or chest level because it is convenient to clip the badge over a belt or a shirt pocket. If the technologist is not involved in fluoroscopic procedures, these locations are acceptable.
The recommended dose limit of 50 mSv/yr (5000 mrem/yr) refers to the effective dose (E). It has been shown that during fluoroscopy, when a protective apron is worn, exposure to the collar region is approximately 20 times greater than that to the trunk of the body beneath the protective apron. So, if the occupational radiation monitor is worn beneath the protective apron, it will record a falsely low exposure and will not indicate what could be excessive exposure to unprotected body parts.
In some clinical situations, for example, during pregnancy and with extremity monitoring, it may be advisable to wear more than one radiation monitor. The abdomen should be monitored during pregnancy. The extremities should be monitored during interventional procedures when the radiologist’s hands are in close proximity to the useful beam. Nuclear medicine technologists should wear extremity monitors when handling millicurie quantities of radioactive material.
Occupational Radiation Monitoring Report
State and federal regulations require that results of the occupational radiation monitoring program be recorded in a precise fashion and maintained for review. Annual, quarterly, monthly, or weekly monitoring periods are acceptable.
The occupational radiation monitoring report must contain a number of specific items of information (Figure 38-7). These various items are identified in the headers of the columns.
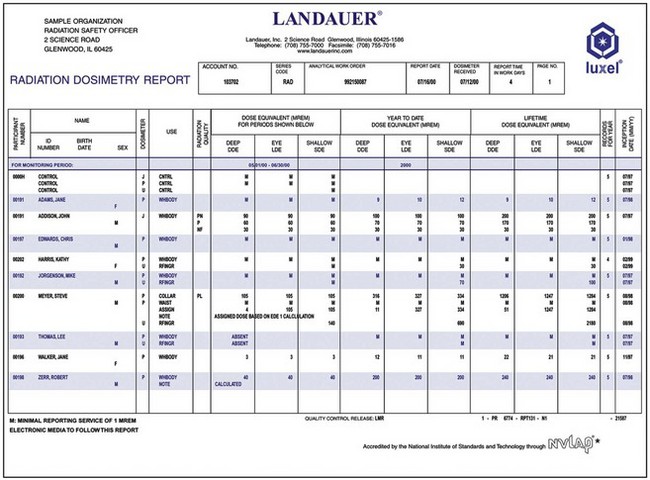
FIGURE 38-7 Occupational radiation monitoring report must include the items of information shown here. (Courtesy Landauer, Inc.)
Exposure data that must be included on the form include current exposure and cumulative annual exposure. Separate radiation monitors, such as extremity monitors or fetal monitors, are identified separately from the whole-body monitor.
Occasionally, if occupational exposure involves low energy radiation, the dose to the skin might be greater than the dose of penetrating radiation. In such cases, the skin dose is separately identified. Areas on the report are provided for neutron radiation exposure to accommodate nuclear reactor and particle accelerator workers.
When a radiologic technologist changes employment, the total radiation exposure history must be transferred to the records of the new employer. Consequently, when one leaves a job, one should automatically receive a report of the total radiation exposure history at that facility. Such a report should be given automatically; if it is not, it must be requested.
When an occupational radiation monitoring program is established, the supplier of the monitor should be informed of the type of radiation facility involved. This information influences the method of calibration of monitors and control monitors.
The control monitor should never be stored in or adjacent to a radiation area. It should be kept in a distant room or office. After processing, the response of the control monitor is subtracted from each individual monitor. In this way, the report for each individual monitor represents only occupational radiation exposure.
All monitors should be returned to the supplier together and in a timely fashion, so they can be processed together. Lost or inadvertently exposed monitors must be evaluated, and an estimate of true exposure should be made by the medical physicist.
Protective Apparel
The operating console usually is positioned behind fixed protective barriers during diagnostic radiographic procedures. During fluoroscopy or mobile radiography, radiologic personnel are in the examination room and near the x-ray source.
Protective gloves and aprons are available in many sizes and shapes. These usually are constructed of lead-impregnated vinyl. Some protective garments are impregnated with tin or other metals because other metals have some advantages over lead as a shielding material in the diagnostic x-ray energy range.
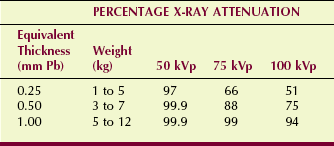
Normal thicknesses for protective apparel are 0.25, 0.5, and 1 mm of lead equivalent. The garments themselves are much thicker than these dimensions, but they provide shielding equivalent to these thicknesses of lead (Table 38-7). Protection of at least 0.25 mm Pb is required; 0.5 mm Pb is normal.
Maximum exposure reduction is obtained with the 1 mm lead equivalent garment, but an apron of this material can weigh as much as 12 kg (25 lb). The wearer could be exhausted by the end of the fluoroscopy schedule just from having to carry the protective apron. X-ray attenuation at 75 kVp for 0.25 mm lead equivalent and 1 mm lead equivalent is 66% and 99%, respectively.
Protective aprons for interventional radiology should be of the wrap-around type. During these procedures, a lot of personnel movement can occur, and some personnel, such as anesthesiologists, may even have their backs to the radiation source.
When not in use, protective apparel must be stored on properly designed racks. If they are continually folded or heaped in the corner, cracks can develop. At least once a year, aprons and gloves should be fluoroscoped to ensure that no such cracks appear. If fluoroscopy is not available, high-kVp radiography (e.g., 120 kVp/10 mAs) may be used.
Position
During fluoroscopy, all personnel should remain as far from the patient as possible, keeping the front of the apron facing the radiation source at all times. After loading spot films, the radiologic technologist should take a step or two backward from the table when his or her presence is not required. The radiologist should use the dead man foot switch sparingly. Naturally, when x-ray beam-on time is high, the radiation exposure to patient and personnel will be proportionately high.
Patient Holding
Many patients referred for x-ray examination, including infants, the elderly, and the incapacitated, are not physically able to support themselves. Mechanical immobilization devices should be available for such patients. Otherwise, a relative or a friend who accompanies the patient should be asked to help. As a last resort, other hospital employees such as nurses and orderlies may be used occasionally to hold patients.
When it is necessary to have another person hold the patient, protective apparel must be provided to that person. An apron and gloves are necessary, and the holder should be positioned and instructed carefully, so that he or she is not exposed to the useful beam. Because the holder is often the mother of a child patient, be sure to ask whether she could be pregnant.
Pregnant Technologist/Radiologist
When a radiologic technologist becomes pregnant, she should notify her supervisor. The pregnancy then is declared, and the DL becomes 0.5 mSv/mo (50 mrem/mo). The supervisor then should review her previous radiation exposure history because this facilitates decisions regarding what protective actions are necessary.
The DL for the fetus is 5 mSv (500 mrem) for the period of pregnancy—a dose level that most radiologic technologists will not reach regardless of pregnancy. Although some may receive doses that exceed 5 mSv/yr (500 mrem/yr), most receive less than 1 mSv/yr (100 mrem/yr).
This usually is indicated with the personnel monitoring device positioned at the collar above the protective apron. Exposure at the waist under the protective apron normally does not exceed 10% of these values; therefore, under normal conditions, specific protective action is not necessary.
Most lead protective aprons are 0.5 mm lead equivalent. These provide approximately 90% attenuation at 75 kVp, which is sufficient. One millimeter lead equivalent protective aprons are available, but such thickness is not necessary, particularly in view of the additional weight of the apron. Back problems during pregnancy constitute a greater hazard than radiation exposure.
The length of the apron need not extend below the knees, but wrap-around aprons are preferred during pregnancy. If necessary, a special effort should be made to provide an apron of proper size because of its weight.
An additional radiation monitor should be positioned under the protective apron at waist level. The exposure reported on this second monitor should be maintained on a separate record and identified as exposure to the fetus.
Do not allow the monitors to be switched and the record confused. Try color-coding—red for the collar badge (red neck!) and yellow for the waist badge (yellow belly!). Additional or thicker lead aprons normally are not necessary (Figure 38-8).
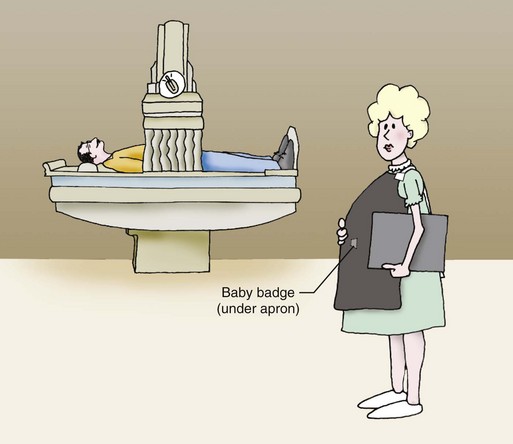
FIGURE 38-8 When the fluoroscopist is pregnant, a second “baby monitor” should be positioned under the protective apron.
Experience with the use of an additional monitor shows consistently that exposures to the fetus are zero. Suppose, for instance, that a pregnant radiologic technologist wearing a single radiation monitor at collar level receives 1 mSv (100 mrem) during the 9-month period. The dose at waist level under a protective apron would be less than 10% of the collar dose, or 0.1 mSv (10 mrem). This is the dose to the monitor; the dose to the fetus is near zero.
Attenuation by maternal tissues overlying the fetus reduces the dose to the fetus to approximately 30% of the abdominal skin dose, or 30 µSv (3 mrem). Consequently, when normal protective measures are taken, it is nearly impossible for a radiologic technologist even to approach the fetal DL of 5 mSv (500 mrem).
Management Principles
It should be clear that the probability of a harmful effect after any occupational radiation exposure in diagnostic imaging is highly unlikely. A biologic response is expected very rarely and has not been observed in radiologic personnel for the past 50 years or so.
Nevertheless, it is essential for the director of radiology to incorporate three steps into the radiation protection program: new employee training, periodic in-service training, and counseling during pregnancy.
New Employee Training
The initial step in any administrative protocol involving pregnant employees involves orientation and training. During these orientation discussions, all female employees should be instructed as to their responsibility regarding pregnancy and radiation.
Each radiologic technologist should be provided with a copy of the facility radiation protection manual and other appropriate materials. This material might include a one-page summary of doses, responses, and proper radiation control working habits (Table 38-8).
TABLE 38-8
Pregnancy in Diagnostic Radiology
| Human Response to Low-Level Exposure | |
| Life-span shortening | 1 day/mGyt |
| Cataracts | None below 2 Gyt |
| Leukemia | 1 cases/106/mGyt/yr |
| Cancer | 0.2 cases/104/mGyt |
| Genetic effects | Doubling dose = 0.5 Gyt |
| Death from all causes | 0.2 deaths/104/mGyt |
| Effects of Irradiation In Utero | |
| 0 to 14 days | Spontaneous abortion: 25% natural incident; 0.1% increase/100 mGyt |
| 2 to 10 weeks | Congenital abnormalities: 5% natural incidence; 1% increase/100 mGyt |
| 2nd to 3rd trimester | Cell depletion: no effect at <0.5 Gyt |
| Latent malignancy: 4 : 10,000 natural incidence; 0.6 : 10,000/mGyt | |
| 0 to 9 months | Genetic effects: 10% natural incidence; 5 × 10−8 mutations/mGyt |
| Protective Measures for the Pregnant Radiologic Technologist | |
| Two occupational radiation monitors | |
| Dose limit: 5 mSv/9 mo, 0.5 mSv/mo |
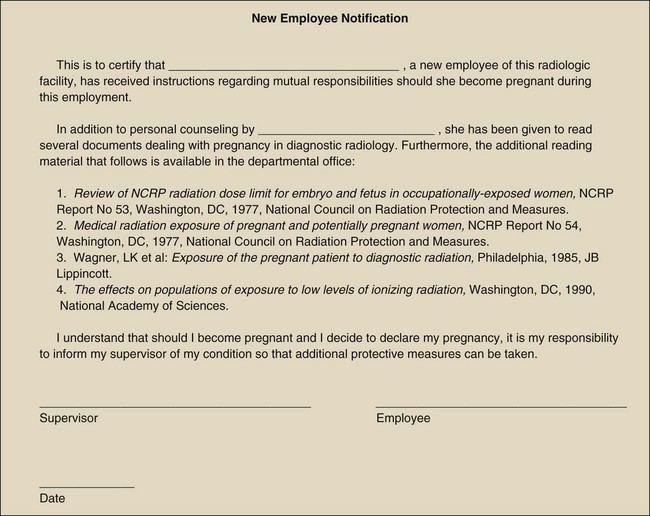
The new employee then should read and sign a form (Figure 38-9) to indicate that she has been instructed in this area of radiation protection. An important point to be made by signing this document is that the employee will notify her supervisor voluntarily when she is pregnant or suspects she is pregnant.
In-Service Training
Every well-run radiology service maintains a regular schedule of in-service training. Usually, this training is conducted at monthly intervals, but sometimes it occurs more often. At least twice each year, such training should be devoted to radiation protection, and a portion of these sessions should be directed at the potentially pregnant employee.
The material to be covered in such sessions is outlined in Table 38-8. Although it is good to review doses and responses, it is probably more appropriate to emphasize radiation control procedures. These, of course, affect the radiation safety of all radiologic technologists—not only pregnant technologists.
A review of personnel monitoring records is particularly important. A helpful procedure is to post the most recent radiation monitoring report for all to see. The year-end report should be initialed by each radiologic technologist, and the director of radiology should ensure that technologists understand the nature and magnitude of their annual exposure.
Through such training, radiologic personnel will realize that their occupational exposure is minimal—usually at less than 10% of the DL.
Counseling During Pregnancy
The director of radiology takes the next action when the radiologic technologist declares her pregnancy. First, the director should counsel the employee after reviewing her radiation exposure history and considering any future modifications to her schedule that may be appropriate.
In all likelihood, a review of the employee’s previous radiation exposure history will show a low exposure profile. Those who wear the radiation monitor positioned at the collar, as recommended, and who are heavily involved in fluoroscopy, may receive an exposure greater than 5 mSv/yr (500 mrem/yr). Such employees, however, are protected by lead aprons, so that exposure to the trunk of the body normally would not exceed 500 µSv (50 mrem/yr).
During this review of occupational radiation exposure, it is appropriate to emphasize that the DL during pregnancy is 5 mSv (500 mrem) and 0.5 mSv/mo (50 mrem/mo). Furthermore, it should be shown that this DL refers to the fetus and not to the radiologic technologist. The level of 5 mSv (500 mrem) to the fetus during gestation is considered an absolutely safe radiation exposure level.
In view of this discussion, the director of radiology should point out to the radiologic technologist that an alteration in her work schedule normally is not required.
For radiologic technologists involved in radiation oncology, nuclear medicine, or ultrasonography, similar consultation and level of modification as previously discussed are appropriate. In radiation oncology, the pregnant technologist may continue her normal workload but should be advised not to participate in brachytherapy applications.
In nuclear medicine, the pregnant technologist should handle only small quantities of radioactive material. She should not elute radioisotope generators or inject millicurie quantities of radioactive material.
Ultrasound technologists normally are not classified as radiation workers. A sizable number of ultrasound patients, however, are nuclear medicine patients and therefore become a potential source of exposure to the ultrasonographer. This situation presents a remote risk because the quantity of radioactivity used is so low. It may be advisable for the ultrasonographer to be provided with a radiation monitor during pregnancy.
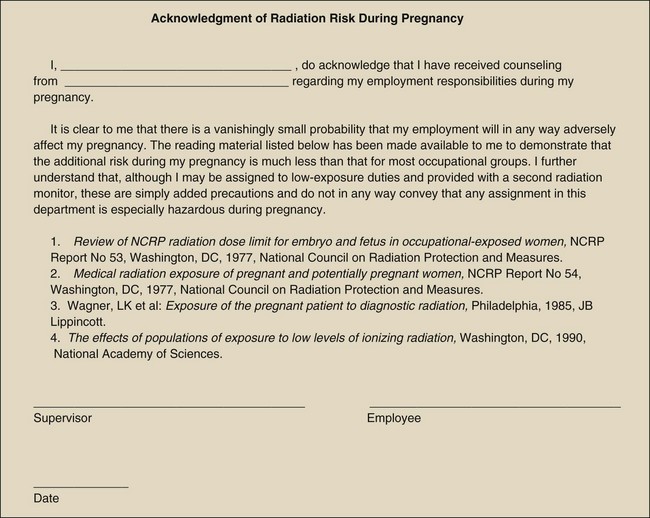
Finally, the pregnant technologist should be required to read and sign a form (Figure 38-10) that attests to the fact that she has been given proper attention to the subject, and that she understands that the level of risk associated with her employment is much less than that experienced by nearly all occupational groups.
Summary
DLs are prescribed by the NCRP for various organs, the whole body, and various working conditions, so that the lifetime risk of each year’s occupational exposure does not exceed 10−4 per year.
The NCRP recommends a cumulative whole-body DL of 10 mSv times age in years. The DL during pregnancy is 5 mSv. In diagnostic imaging, however, it is seldom necessary to exceed 1/10 the appropriate DL.
Occupational radiation exposure is measured in millisieverts (millirems), and the description of such exposure is effective dose (E). Effective dose accounts for type of radiation and the relative radiosensitivity of tissues and organs.
Although the dose limit for occupational workers is 50 mSv/yr, most radiologic personnel receive less than 0.5 mSv/yr. Radiologists may receive a higher dose if engaged in a heavy fluoroscopy schedule.
Because 95% of occupational exposure comes from fluoroscopy and mobile radiography, the radiologic technologist should follow these guidelines for reducing occupational exposure:
• During mobile radiography, wear an apron, maintain maximum distance from the source, and never direct the primary beam toward oneself or others.
• During fluoroscopy, step back from the table if not needed, and use shielding, including an apron, a curtain, a Bucky slot cover, and the radiologist.
• During radiography, stand behind the control booth and never direct the primary beam toward the control booth barrier.
Personnel monitoring is required when there is any likelihood that an individual will receive more than 1/10 the dose limit. The various available personnel radiation monitors include (1) film badges, (2) TLDs, and (3) OSL dosimeters. The OSL is very sensitive and accurate and may be worn for up to 1 year. For general use, the radiographer should wear the personnel monitor at waist or chest level; however, during fluoroscopy, the monitor is worn on the collar outside the protective apron.
Radiographers and occupational workers should never be used to hold patients during an exposure.
The radiobiology of pregnancy requires particular attention to the pregnant radiologic technologist and the pregnant patient. The pregnant radiologic technologist should be provided with a second radiation monitoring device to be worn under the protective apron at waist level.
1. Define or otherwise identify the following:
2. What is the dose limit for diagnostic imaging personnel?
3. During what two examinations can occupational radiation exposure be high?
4. What does the value 10−4 yr−1 mean with regard to the NCRP recommended dose limits?
5. How do some radiation occupational groups such as nuclear medicine technologists monitor their extremity doses?
6. What is the whole-body occupational DL for radiography students younger than 18 years of age?
7. State the management protocol for the pregnant radiologic technologist.
8. What information regarding radiation protection should be covered in regularly scheduled in-service training classes?
9. What exposure will a radiologic technologist receive while wearing a protective apron equivalent to 2 HVLs and exposed for 10 minutes at 4 m from a source with intensity of 1 mGya/hr at 1 m?
10. The collar-positioned monitor of a fluoroscopist records 0.9 mSv during a month. This represents approximately what effective dose (E)?
11. What is the required length of the exposure cord on the mobile radiographic unit?
12. When must occupational radiation monitoring be provided?
13. Describe the design of occupational radiation monitors. How are they to be worn, and where on the body are they placed?
14. List the exposure data that must be included in the personnel monitoring report.
15. What is an appropriate thickness for protective apparel?
16. What procedure is used for holding patients during an x-ray examination?
17. Describe the features of optically stimulated dosimetry that make it particularly effective for occupational radiation monitoring.
18. What is the DL for the lens of the eye and the requirement for protective eyewear?
19. What is the approximate protective value of an occupational radiation monitor?
20. Describe an appropriate radiation protection program for nursing and surgical personnel.
The answers to the Challenge Questions can be found by logging on to our website at http://evolve.elsevier.com.
 of that established for the radiation worker.
of that established for the radiation worker. of the recommended dose limit.
of the recommended dose limit.