Health Physics
At the completion of this chapter, the student should be able to do the following:
2 List the cardinal principles of radiation protection and discuss the ALARA concept.
3 Explain the meaning of NCRP and the concept of dose limits.
4 Name the recommended dose limits for radiation workers and the public.
5 Discuss the radiosensitivity of the stages of pregnancy.
6 Describe the recommended management procedures for pregnant radiation workers and for the pregnant patient.
IMMEDIATELY AFTER their discovery, x-rays were applied to the healing arts. It was recognized within months, however, that radiation could cause harmful effects.
The first American fatality that resulted from radiation exposure was Thomas Edison’s assistant, Clarence Dally. Since that event, a great deal of effort has been devoted to developing equipment, techniques, and procedures to control radiation levels and reduce unnecessary radiation exposure to radiation workers and the public.
The cardinal principles for radiation protection are simplified rules designed to ensure safety in radiation areas for occupational workers. In 1931, the first dose-limiting recommendations were made. Today, the National Council on Radiation Protection and Measurements (NCRP) continuously reviews the recommended dose limits.
Providing radiation protection for workers and the public is the practice of health physics. Health physicists design equipment, calculate and construct barriers, and develop administrative protocols to maintain radiation exposures as low as reasonably achievable (ALARA). That is the substance of this chapter.
The term health physics was coined during the early days of the Manhattan Project, the secret wartime effort undertaken to develop the atomic bomb. The group of physicists and physicians responsible for the radiation safety of persons involved in the production of atomic bombs were the first health physicists. Thus, the health physicist is a radiation scientist who is concerned with the research, teaching, or operational aspects of radiation safety.
Radiation and Health
At the turn of the Millennium, the year 2000, the National Academy of Sciences identified the 20 greatest scientific and technical accomplishments of the 20th century. Medical imaging was number 14 on this list.
This is important to point out to our patients, many of whom remain wary of radiation. One never reads the word “radiation” in a newspaper or a magazine without the modifier “dangerous,” “deadly,” or “harmful.”
We practice ALARA because of the linear nonthreshold radiation dose-response relationship (LNT) for stochastic effects—cancer, leukemia, and genetic effects. Yet we should also recognize that we actually employ low levels of radiation in diagnostic imaging.
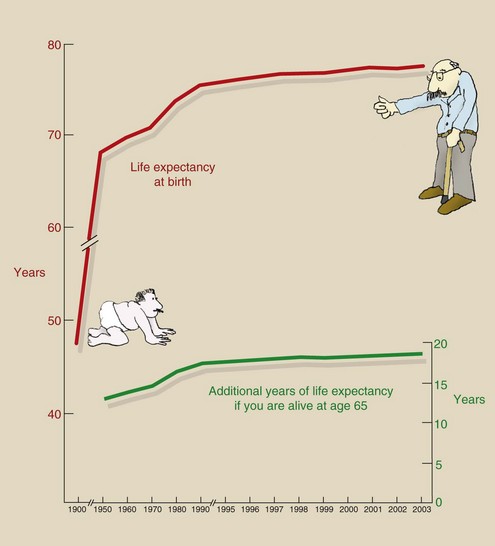
Unquestionably, the application of this radiation has had a major impact on our health and increasing longevity. If you had been born in the United States in 1900, your life expectancy was 47 years. During the first century of diagnostic x-ray imaging, life expectancy has soared. Life expectancy is now 78 years (Figure 35-1).
Nevertheless, because of LNT, we must continue to be aware of patient and occupational radiation dose and must take those steps necessary to implement ALARA.
Cardinal Principles of Radiation Protection
All health physics activity in radiology is designed to minimize the radiation exposure of patients and personnel. Three cardinal principles of radiation protection developed for nuclear activities—time, distance, and shielding—find equally useful application in diagnostic radiology. When these cardinal principles are observed, radiation exposure can be minimized (Box 35-1).
Minimize Time
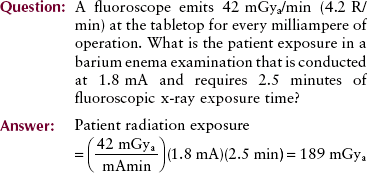
The dose to an individual is directly related to the duration of radiation exposure. If the time during which one is exposed to radiation is doubled, the exposure will be doubled, as follows:
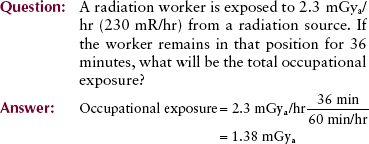
During radiography, the time of exposure is kept to a minimum to reduce motion blur. During fluoroscopy, the time of exposure also should be kept to a minimum to reduce patient and personnel radiation exposure. This is an area of radiation protection that is not directly controlled by the radiologic technologist.
Radiologists are trained to depress the fluoroscopic foot switch in an alternating fashion, sequencing on-off rather than continuous on during the course of the examination. A repeated up-and-down motion on the fluoroscopic foot switch permits a high-quality examination to be performed with considerably reduced exposure to the patient. The use of pulse-progressive fluoroscopy can reduce patient dose considerably.
The 5-minute reset timer on all fluoroscopes reminds the radiologist that a considerable amount of fluoroscopic time has elapsed. The timer records the amount of x-ray beam on time. Most fluoroscopic examinations take less than 5 minutes.
Only during difficult interventional radiology procedures should it be necessary to exceed 5 minutes of exposure time. A particular hazard lies in the use of mobile image intensifiers in surgical suites where some physicians are less radiation conscious.
Maximize Distance
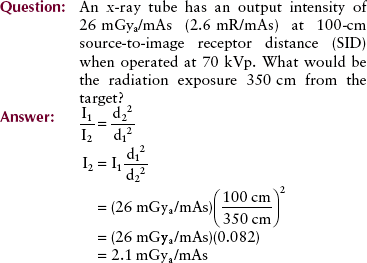
As the distance between the source of radiation and the person increases, radiation exposure decreases rapidly. This decrease in exposure is calculated using the inverse square law, which was discussed in Chapter 3.
Most radiation sources are point sources. The x-ray tube target, for example, is a point source of radiation. The scattered radiation generated in a patient appears, however, to come not from a point source but rather from an extended area source. As a rule of thumb, even an extended source can be considered a point source at sufficient distance.
Earlier, when the square law was used to calculate exposure in radiographic technique, the following formula may have been used:
In this case, the exposure from the source (the x-ray tube) was varied so that the optical density of the film (OD) would remain constant.
When the inverse square law is used in calculations for radiation protection, it is usual to calculate the dose received at a point with the radiation from the tube as the constant.
Thus the above formula becomes
Note that the “distance” part of the equation is reversed.
In radiography, the distance from radiation source to patient usually is fixed by the type of examination, and the radiologic technologist is positioned behind a protective barrier.
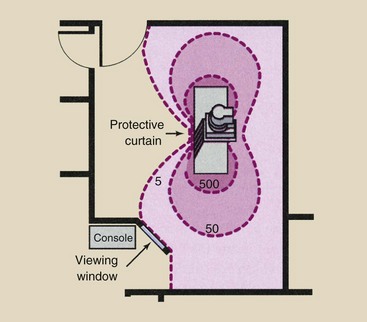
During fluoroscopy, the radiologic technologist can exercise good radiation protection procedures. Figure 35-2 shows approximate radiation exposure levels at waist height during a fluoroscopic examination. The lines on the plot plan, called isoexposure lines, represent positions of equal radiation exposure in the fluoroscopy room. At the normal position for a radiologist or a radiologic technologist, the exposure rate is approximately 3 mGya/hr (300 mR/hr).
During portions of the fluoroscopic examination, when it is not necessary for the radiologic technologist to remain close to the patient, the technologist should step back. Two steps back, the exposure rate is only approximately 50 µGya/hr (5 mR/hr). This reduction in exposure does not follow the inverse square law because during fluoroscopy, the patient is an extended source of radiation because of scattered x-rays generated within the body.
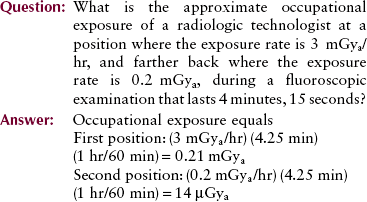
Better yet, after two steps back to take advantage of “maximize distance,” take one step to the side and get behind the radiologist! This move results in additional shielding.
Use Shielding
Positioning shielding between the radiation source and exposed persons greatly reduces the level of radiation exposure. Shielding used in diagnostic radiology usually consists of lead, although conventional building materials also are used.
The amount that a protective barrier reduces radiation intensity can be estimated if the half-value layer (HVL) or the tenth-value layer (TVL) of the barrier material is known. The HVL is defined and discussed in Chapter 12. The TVL is similarly defined as follows:
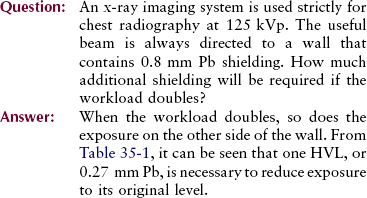
Table 35-1 shows approximate HVLs and TVLs for lead and concrete for diagnostic x-ray beams between 40 and 150 kVp.
TABLE 35-1
Approximate Half-Value and Tenth-Value Layers of Lead and Concrete at Various Tube Potentials
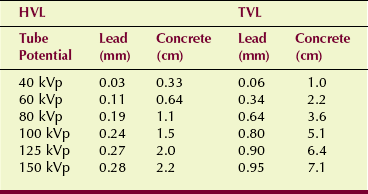
Another example of the application of shielding in radiology is the use of protective apparel. Protective aprons usually contain 0.5 mm Pb. This is approximately equivalent to 2 HVLs, which should reduce occupational exposure to 25%. Actual measurements show that such protective aprons reduce exposure to approximately 10% because scattered x-rays are incident on the apron at an oblique angle.
Usually, application of the cardinal principles of radiation protection involves consideration of all three. The typical problem involves a known radiation level at a given distance from the source. The level of exposure at any other distance, behind any shielding, for any length of time can be calculated. The order in which these calculations are made makes no difference.
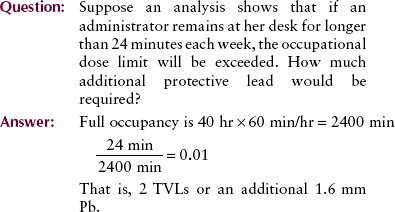
Figure 35-3 illustrates the use of these cardinal principles of radiation protection during a typical clinical situation.
Effective Dose
It is relatively easy to measure patient radiation exposure and dose during medical x-ray imaging. However, x-ray imaging involves partial-body exposure. Radiographic images are collimated to the tissue of importance; therefore, the total body is not exposed.
Radiation risk coefficients are based on total body radiation exposure, as for the atomic bomb survivors of Hiroshima and Nagasaki. When only part of the body is exposed, as in medical x-ray imaging, the risk of a stochastic radiation response is not proportional to the tissue dose but rather to the effective dose (E).
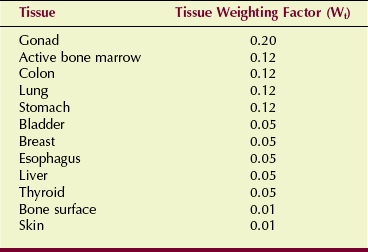
The equivalent whole-body dose is the weighted average of the radiation dose to various organs and tissues. The National Committee on Radiation Protection (NCRP) has identified various tissues and organs and the relative radiosensitivity of each (Table 35-2).
Effective dose is the weighted average dose to each of the tissues in Table 35-2.
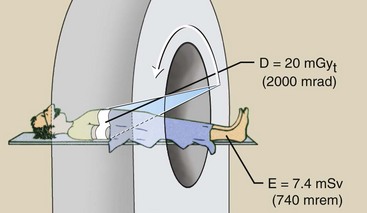
Patient Effective Dose
Consider, for example, the relationship between patient dose and effective dose in computed tomography (CT) (Figure 35-4). CT examination of the pelvis results in a rather uniform dose of 20 mGy (2000 mrad) to the tissues of the pelvis. Other tissues are not irradiated.
The exercise shown in Box 35-2 illustrates the manner in which one arrives at patient effective dose. This exercise shows that the effective dose for pelvic CT is 7.4 m Sv.
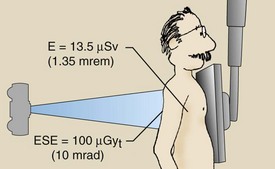
Another example, as shown in Figure 35-5, postero-anterior chest radiography, should help explain this concept. Entrance skin dose for this examination is approximately 100 µGya. If one assumes an average tissue dose of half the entrance skin dose, 50 µGya, the effective dose is 0.014 m Sv or 14 µGya, as computed in Box 35-3.
Radiologic Technologist Effective Dose
We receive essentially all of our occupational radiation exposure during fluoroscopy. During radiography and mammography, the radiographer is positioned behind a protective barrier, resulting in zero occupational radiation exposure.
During fluoroscopy, we position our occupational radiation monitor at the collar, as shown in Figure 35-6, to estimate dose to the tissues of the head and neck. The tissues of the trunk of the body receive essentially zero dose; the protective apron does what it is designed to do.
Figure 35-6 Effective dose for occupational radiation exposure is based on the occupational radiation monitor.
So the estimation of effective occupational dose is shown in Box 35-4 for an occupation monitor response of 1 mSv. The result of this exercise is an occupational effective dose of 100 µ Sv.
Assuming an effective dose of 10% of the occupational monitor dose is conservative. In actual fact, it is something less than 10%.
We will return to the concept of effective dose in Chapters 36 and 37. Be reminded that it is effective dose that should be used for radiation risk estimation.
Radiologic Terrorism
Emergency response to a radiologic incident conducted by terrorists, an exceptionally rare event, must be dealt with quickly and competently in order to save life and limit property and environmental damage. Emergency responders are those individuals who must make the first decisions and take the first steps in the early stages of such an event.
The first emergency responders are likely to be police, fire, or emergency medical personnel. In the setting of a health care facility, radiologic technologists may likely be the first emergency responders.
The first task of emergency responders is to prevent injury and death and to attend to the medical needs of victims. Such immediate responses include limiting acute, high-intensity radiation exposure and limiting low-intensity radiation exposure that could result in late stochastic effects. This is an ALARA exercise and will involve the application of the cardinal principles of radiation protection: Reduce time of exposure, increase distance from the source, and impose shielding between the source and the victim.
Radiologic Device
The malevolent use of radiologic material by terrorists can be described as one of three devices: a radiation exposure device (RED), a radiologic dispersal device (RDD), and an improvised nuclear device (IND). Dealing with the effect of such devices requires specific response techniques for each.
An RED is a sealed source of radioactive material that directly exposes people. An RED will not disperse radioactive material; therefore, decontamination of an RED is not required.
An RDD is a bomb that when exploded disperses radioactive contamination over a wide area. Although the contamination can be particularly troublesome, it is not usually life threatening. The RDD may not be explosive, but rather, radioactive material. It may be dispersed by hand in the form of powder, mist, or gas into a water supply or ventilation system.
An IND contains nuclear material that can produce a nuclear explosion. An IND is indeed a nuclear weapon; therefore, it is unlikely to be the form of attack used by a terrorist. However, should an IND be employed, the death and devastation would be extreme.
Radiation Protection Guidance
Protection against exposure to external radiation, exposure from photon and particle radiation, and internal radioactive contamination transferred from surface radioactive contamination must be considered. This is accomplished by establishing boundaries for known levels of radiation exposure and radioactive contamination.
With the use of radiation monitoring instruments, an inner boundary is established at an exposure rate of 100 mGya/hr (10 R/hr). Inside of this boundary, one should assume that levels of radioactive contamination are high, until it is proved otherwise.
An outer boundary should be established when exposure exceeds 100 µGya/hr (10 mR/hr) or when radioactive contamination is detectable.
Radiation Detection and Measurement Equipment
Radiation detection equipment with specific capacity should be readily available to the first responder. It is recommended that such equipment be stored in the nuclear medicine laboratory and identified to all technologists and radiologists who might be pressed into emergency response.
Radiation detection apparatus should be capable of measuring radiation exposure levels to 500 m Gya/hr (50 R/hr). Further, it is recommended that such instruments should emit unambiguous alarms at 100 µGya/hr (10 mR/hr), 100 mGya/hr (10 R/hr), and 500 mGya/hr (50 R/hr). (Such a specially designed instrument is shown in Figure 35-7.) An additional instrument should be available that can be used to clearly detect the presence of alpha and beta radioactive contamination.

Figure 35-7 Radiation detection instrument designed especially for radiologic terrorism. (Courtesy Ian Hamilton, Ludlum Instruments.)
Emergency responders should have available standard protective coveralls and shoe covers to protect against radioactive contamination of the responder. Protective respiratory devices may be needed in the case of aerosol radioactive contamination. Decontamination of victims may be necessary, and an area should be cordoned off for such activity, so that a contaminated-to-clean step-off pad is provided.
The Radiation Safety Officer of a hospital should assign an individual to be responsible for establishing the emergency response equipment store and for seeing that adequate continuing education is provided for those who might be called upon to perform as emergency responders.
Summary
Health physics is concerned with the research, teaching, and operational aspects of radiation control. The three cardinal principles developed for radiation workers are as follows: Minimize time of radiation exposure, maximize distance from the radiation source, and use shielding to reduce radiation exposure. ALARA (as low as reasonably achievable) defines the principal concept of radiation protection.
Effective dose is that which should be used to estimate radiation risk to the patient or the radiologic technologist. Assuming that effective dose is 10% of a collar-positioned monitor is conservative and results in overestimation of stochastic response.
Radiologic terrorism is possible with three principal devices: a radiation exposure device, a radiologic dispersal device, and an improvised nuclear device.
1. Define or otherwise identify the following:
2. Write the equation for the radiation dose as a function of time of exposure.
3. What is the function of the 5-minute reset timer on a fluoroscopy imaging system?
4. A fluoroscope emits 35 µGya/mA-minute at the tabletop for every mA of operation. What is the approximate patient entrance skin dose (ESD) after a 3.2-minute fluoroscopic examination of 1.5 mA?
5. What are the three cardinal principles of radiation protection?
6. The output intensity of a radiographic unit is 42 µGya/mAs. What is the total output after a 200-ms exposure at 300 mA?
7. At the exposure rate in #6, what is the approximate patient skin dose after a 3.2-minute fluoroscopic examination of 1.5 mA?
8. How can the three cardinal principles of radiation protection be best applied in diagnostic radiology?
9. What exposure will a radiologic technologist receive when exposed for 10 minutes at 4 m from a source with intensity of 1 mGya/hr at 1 m while wearing a protective apron equivalent to 2 HVLs?
10. What wartime effort coined the term health physicist?
11. The collar-positioned monitor of a fluoroscopist records 0.9 mSv over the course of a month. This represents approximately what effective dose (E)?
12. Describe the change in longevity that occurred during the 20th century and the impact of radiation on that change.
13. How many half-value layers are included in a tenth-value layer?
14. What should first responders do in the event of a radiologic emergency?
The answers to the Challenge Questions can be found by logging on to our website at http://evolve.elsevier.com.