Clinical reasoning
From the Maitland Concept and beyond
Clinical reasoning and evidence-based practice
Critical thinking and clinical reasoning
Importance of skilled clinical reasoning to expert practice
Clinical reasoning and the bio-psychosocial model of health and disability
Clinical reasoning as a hypothesis-oriented and collaborative process
Clinical reasoning and knowledge
Clinical reasoning and cognition/metacognition
Skilled questioning important to critical thinking and learning
Skilled questioning important to clinical practice
Facilitating application of bio-psychosocial practice: clinical reasoning strategies and hypothesis categories
Complexity of clinical reasoning
Improving clinical reasoning: learning through clinical reasoning
Introduction
Geoff Maitland always insisted on a systematic and comprehensive patient examination that in his words ‘enables you to live the patient’s symptoms over 24 hours’. All patient information regarding their problem, its effects on their life and the associated physical impairments found on physical examination had to be analysed with the aim of ‘making features fit’. Patient treatments were never recipes or protocols, rather specific treatments were based on thorough analysis of the subjective (i.e. patient interview) and physical findings combined with knowledge of research, clinical patterns, treatment strategies that had been successful for similar presentations and systematic reassessment of all interventions. While Geoff did not refer to this process of information gathering, analysis, decision making, intervention and reassessment as clinical reasoning, it clearly was a structured and logical approach in line with contemporary clinical reasoning theory. Consistent with the aim of contemporary evidence-based practice, his ‘Brick Wall’ concept emphasized consideration of both research and experienced-based evidence with the research providing a general guide and the patient's unique presentation determining how that research was applied and ultimately the specific interventions to trial. The open-minded yet critically reflective bio-psychosocial philosophy of practice that Geoff promoted is evident in the following quote:
The Maitland concept requires open-mindedness, mental agility and mental discipline linked with a logical and methodical process of assessing cause and effect. The central theme demands a positive personal commitment (empathy) to understand what the person (patient) is enduring. The key issues of ‘the concept’ that require explanation are personal commitment, mode of thinking, techniques, examination and assessment.
(Maitland 1987, p. 136)
In this chapter the clinical reasoning implicit in ‘The Maitland Concept’ is made explicit. The importance of skilled clinical reasoning to expert practice and to evidence-based practice is noted. The components of critical thinking inherent in skilled clinical reasoning are highlighted. The role clinical reasoning plays in assisting application of bio-psychosocial models of health and disability, such as the World Health Organization International Classification of Functioning, Disability and Health (ICF) (WHO 2001), is discussed along with frameworks for directing and organizing the different foci of thinking and categories of decision making needed to understand both the person and their problem(s) and to guide a collaborative approach to management. Lastly, common errors of reasoning are considered and the value of skilled reflective reasoning to learning and to the continual evolution of physiotherapy practice is stressed.
Clinical reasoning defined
Clinical reasoning is a reflective process of inquiry and analysis carried out by a health professional in collaboration with the patient with the aim of understanding the patient, their context and their clinical problem(s) in order to guide evidence-based practice.
More simply it is the thinking and decision making associated with clinical practice that enables therapists to take the best-judged action for individual patients. In this sense, clinical reasoning is the means to ‘wise’ action (Cervero 1988, Harris 1993).
Clinical reasoning and evidence-based practice
Evidence-based practice (EBP), defined as ‘the integration of best research evidence with clinical expertise and patient values’ (Sackett et al. 2000, p. 1), is critical to minimize misconceptions in clinical theory and practice and to understand how best to work with patients in their health management. Clinical practice is subject to unrecognized bias, taken-for-granted assumptions and errors of reasoning that necessitate audits of practice as encouraged by the evidence-based movement. In fact, Thomas Kuhn, a science historian, highlights how the majority of misconceptions through the history of science, including such things as the function of the heart as the organ of thought, can almost universally be attributed to a lack of critical appraisal of contemporary theory (Kuhn 1970). However, EBP was never intended to be prescriptive. Our current body of research is either incomplete or incomplete in its reporting to adequately guide therapists in their recognition and management of the multitude of patient problems we face (Jones et al. 2006). Common limitations with physiotherapy effectiveness studies include high drop-out rates or loss to follow-up, lack of blinding (patient, therapist, measurer), lack of random and concealed allocation to treatment arms, lack of adequate identification of population subgroups, artificial isolation of treatment interventions in determining their effect and lack of evidence of sustainable outcomes. As such, practicing clinicians face the daunting challenge of maintaining best practice based on best evidence when the evidence is still largely not available or is incomplete. Even when primary research studies (or systematic reviews) testing therapeutic interventions for the condition of interest are available, numerous issues must be considered for the clinician to have confidence in the applicability of the findings including whether their patient matches the population studied (often made difficult by lack of homogeneity of subjects and insufficient consideration of psychosocial variables) and whether the intervention tested can be replicated. Very few studies provide sufficient detail and justification of the assessments and treatments (e.g. what precisely was done including details of positions, dosage, sequence and progression; who treated the patients including level of procedural competence; what was the therapeutic environment including associated explanations, instructions, verbal cues and advice) to enable clinicians to replicate the assessments and management (educatively, behaviourally and humanistically) with confidence. Application of evidence to practice requires skilled clinical reasoning. Skilled clinical reasoning is underpinned by skilled critical thinking.
Critical thinking and clinical reasoning
While generic thinking skills are themselves insufficient for expertise in clinical practice (Boshuizen and Schmidt 2008, Elstein et al. 1978), skilled clinical reasoning incorporates the fundamentals of critical thinking. Critical thinking is a field of study on its own (e.g. see Baron & Sternberg 1987, Brookfield 1987, de Bono 1994, Forneris 2004, Mezirow 1990, 1991, 2000, Nickerson et al. 1985, Schön 1983, 1987). Paul and Elder (2007) provide a clear and simple overview of critical thinking which they propose has three dimensions: the analytic, the evaluative and the creative. Critical thinking generally involves analyzing and assessing information, issues, situations, problems, perspectives and thinking processes. It enables the judging of information regarding its accuracy, precision, completeness and relevance to facilitate understanding and identification of solutions. It enables creation of new insights and knowledge. While everyone is already capable of thinking, and as Nickerson (1985, p. 28) points out, ‘All of us compare, classify, order, estimate, extrapolate, interpolate, form hypotheses, weigh evidence, draw conclusions, devise arguments, judge relevance, use analogies and engage in numerous activities that are typically classified as thinking’, this is not to say that we do these things well in all circumstances, or that we couldn't learn to do them better. Steven Brookfield (1987, p. ix), a prominent researcher and writer in the field of adult learning and critical thinking, summarizes the value of critical thinking and reasoning as follows:
• When we become critical thinkers we develop an awareness of the assumptions under which we, and others, think and act
• We learn to pay attention to the context in which our ideas and actions are generated
• We become sceptical of quick fix solutions, of single answers to problems, and of claims of universal truth
• We also become open to alternative ways of looking at and behaving in the world
• Critical thinking influences all aspects of our lives. For example, in our personal relationships we can learn to see our own actions through the eyes of others
• At our workplace we seek democracy and take initiative in forming new directions
• We become aware of the potential for distortion and bias in media depictions
• We value political freedom, we practice democracy, we encourage a tolerance of diversity, and we hold in check the demagogic tendencies of politicians.
In addition to Brookfield's list, critical thinking and reasoning are also important to:
• Avoid misdirection in beliefs
• Discover alternative understandings and solutions and generate new ideas
• Optimize health care outcomes
• Analyze arguments of others thereby making you less susceptible to manipulation by others
• Enrich your life aesthetically by becoming more observant.
For some therapists who already possess good critical thinking skills, developing skilled clinical reasoning mostly requires acquiring the necessary research and practice knowledge with which to apply those skills. However, others either lack those fundamental critical thinking skills or they fail to use them, instead falling into the trap of uncritically following routines and protocols. Even skilled therapists are vulnerable to habits of practice and over allegiance to particular approaches or paradigms of practice. It can be difficult to critically examine your own perspective when you consider as Brookfield (2008, p. 68) notes:
No matter how much we may think we have an accurate sense of our practice, we are stymied by the fact that we are using our own interpretive filters to become aware of our own interpretive filters! … To some extent we are all prisoners trapped within the perceptual frameworks that determine how we view our experiences. A self-confirming cycle often develops whereby our uncritically accepted assumptions shape clinical actions which then serve only to confirm the truth of those assumptions. It is very difficult to stand outside ourselves and see how some of our most deeply held values and beliefs lead us into distorted and constrained ways of thinking and practicing.
Suggestions for improving critical thinking in general through ‘Socratic questions’ along with skilled clinical questioning to optimize the quality of patient information obtained are discussed later in the chapter.
Importance of skilled clinical reasoning to expert practice
Research into expertise in a number of fields (e.g. physics, mathematics, medicine, chess) has identified the following generic characteristics (Glaser & Chi 1988):
• Experts excel in their own domains
• Experts possess large repertoire of well-developed profession specific patterns they recognize
• Experts solve problems fast with less error
• Experts see problems at a deeper level, spending more time analyzing problems qualitatively (i.e. more aware of contextual cues in the presentation)
• Experts have strong self-monitoring skills
• Experts possess the affective dispositions necessary to learn from their experiences including:
Clinical expertise, of which clinical reasoning is a component, can be viewed as a continuum along multiple dimensions including clinical outcomes and personal attributes such as knowledge, technical skills, communication and interpersonal skills, cognitive/metacognitive proficiency, professional judgment and empathy (Higgs & Jones 2000). Health professions' research into clinical expertise (e.g. Beeston & Simons 1996, Benner 1984, Elstein et al. 1978, Edwards et al. 2004a, Embrey et al. 1996, Jensen et al. 2007, Jensen et al. 2008, Mattingly & Fleming 1994, May & Dennis 1991, Patel & Groen 1986, Payton 1985, Thomas-Edding 1987) has identified the following characteristics and expectations of expert clinicians:
• Experts value participation of others (patients, family, other health professionals)
• Experts value different forms of knowledge in their reasoning (research and experienced based)
• Experts' theory, practice, reasoning and intuition are intertwined through practical experience
• Experts are patient-centred, collaborative with superior practice based knowledge. For example patients are viewed as active participants in therapy
• Primary goal of care is empowerment of patients through collaboration between patient and therapist
• Expert has a strong moral commitment to beneficence or doing what is in the patient's best interest
• Expert is willing to serve as a patient advocate or moral agent in helping them become successful
• Experts have good communication skills
• Experts use collaborative problem-solving to help patients learn how to resolve their problems on their own, fostering self-efficacy and empowering them to take responsibility
• Experts share their expertise to assist others; and
• Experts communicate their reasoning well at an appropriate level depending on who they are speaking to.
Many of the generic and health professions' specific characteristics of expertise above are also associated with skilled clinical reasoning. Physiotherapy specific research investigating expert practice (e.g. Edwards et al. 2004a, Embrey et al. 1996, Jensen et al. 1990, Jensen et al. 1992, Resnik & Jensen 2003) has contributed significantly to our evolving understanding of clinical reasoning, much of which is reported in the text Expertise in physical therapy practice (Jensen et al. 2007). Key dimensions of skilled clinical reasoning emanating from this research include:
• Clinical reasoning is situated within a bio-psychosocial model of health
• Clinical reasoning is complex, non-linear and cyclical in nature involving both inductive and deductive reasoning
• Clinical reasoning is patient-centred involving a collaborative exchange to achieve a mutual understanding of the problem and to negotiate an agreed-upon plan for addressing that problem
• Clinical reasoning requires different foci of thinking, or ‘reasoning strategies’ within which expert physiotherapists make judgments
• Clinical reasoning plays a critical role in reflective learning from practice experiences and in the development of clinical expertise.
Clinical reasoning and the bio-psychosocial model of health and disability
Contemporary understanding of health and disability recognizes disability is not simply the cumulative effects of physical impairments, rather disability is also socially constructed (e.g. Borrell-Carrió et al. 2004, Imrie 2004, Johnson 1993, Werner 1998). This broader view of disability is consistent with the holistic bio-psychosocial philosophy of practice as depicted in the World Health Organization ICF framework (World Health Organization 2001) (Fig. 2.1). The bio-psychosocial model initially put forward by Engel:
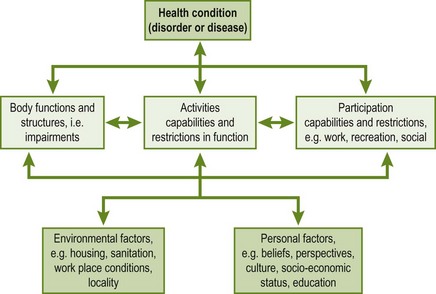
Figure 2.1 Adaptation of World Health Organization International Classification of Functioning, Disability and Heath Framework (World Health Organization 2001, p. 18).
…dispenses with the scientifically archaic principles of dualism and reductionism and replaces the simple cause-and-effect explanations of linear causality with reciprocal causal models.
(Engel 1978, p. 175)
However, despite overwhelming evidence for the bio-psychosocial philosophy of practice, many therapists still practice in a predominantly biomedical mode. Some argue it's not their role (i.e. ‘I'm a physiotherapist not a psychologist'); some agree it is important but see psychosocial factors as only relevant to chronic pain; some have a dualistic conception of bio-psychosocial rather than understanding it as a genuine integration of mind and body (Borrell-Carrió et al. 2004, Duncan 2000, Engel 1978, Pincus 2004); some claim to be bio-psychosocial but their actual practice does not reflect this approach (Argyris & Schön 1978, Jorgensen 2000, Mattingly & Fleming 1994); and some do practice bio-psychosocially but due to a lack of formal training they tend to be informal and superficial with an over focus on behavioural over cognitive and social factors (Sharp 2001, Sim & Smith 2004).
The ICF framework depicted in Figure 2.1 portrays the patient's clinical presentation through the boxes across the middle of the diagram incorporating impairments of body functions and structures, restrictions and capabilities in functional activities and restrictions and capabilities in their ability to participate in life situations (e.g. work, family, sport, leisure). This clinical presentation of impairments, activity and participation restrictions (i.e. the patient's ‘disability’) is represented as an outcome of interactions between the biomedical health condition (i.e. disorder, disease, illness) and contextual environmental and personal factors. Environmental factors include architectural characteristics, social attitudes, legal and social structures, climate, terrain, etc. Personal factors include gender, age and psychological features such as thoughts/beliefs, feelings, coping styles, health and illness behaviours, social circumstances, education, past and current experiences. Environmental and personal factors can positively or negatively influence the clinical presentation. Bidirectional arrows are used between the different factors to reflect the reciprocal relationship between components. Understanding a patient's clinical presentation therefore necessitates attention to their physical health, environmental and personal factors. While physiotherapists are generally well prepared to assess and manage the physical dimensions of the patient's health condition, formal education and experience assessing, analyzing and managing environmental and personal factors is often less developed and less structured. The ICF framework provides an excellent overarching profile of the scope of areas in which physiotherapists must be competent to holistically understand and manage their patients with a growing body of physiotherapy literature now available relating the ICF to categorization of clinical problems and to clinical reasoning (e.g. Childs et al. 2008, Cibulka et al. 2009, Edwards & Jones 2007a, Escorpizo et al. 2010, Jette 2006, Logerstedt et al. 2010, McPoil et al. 2008, Steiner et al. 2002). The scope of clinical reasoning required to practice within this bio-psychosocial framework is discussed next.
Clinical reasoning as a hypothesis-oriented and collaborative process
Understanding the clinical reasoning underlying a physiotherapist's assessment and management of a patient requires consideration of the thinking process of the therapist, the thinking process of the patient and the shared decision making between therapist and patient. Figure 2.2 presents a bio-psychosocial framework of clinical reasoning as a collaborative process between physiotherapist and patient (Edwards & Jones 1996). The left-hand side of Figure 2.2 depicts the therapist's thinking while the right represents the patient's. The arrows linking the two sides reflect the collaborative nature of the process.
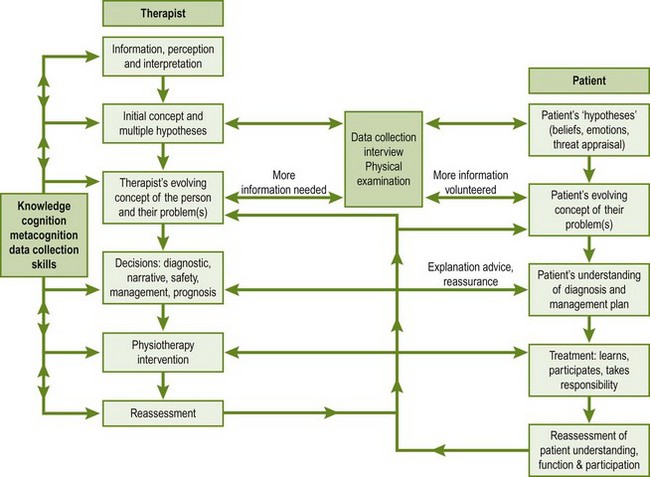
Figure 2.2 Collaborative reasoning model (Edwards & Jones 1996, Jones & Rivett 2004).
The physiotherapist's thinking
The therapist's reasoning is an ongoing hypothesis-oriented process of perception, interpretation and synthesis of information. Information about or from the patient must first be perceived as relevant and then interpreted. Both perception and interpretation are directly related to the therapist's knowledge base (e.g. novices often miss relevant information, struggle to identify and give weight to the most relevant information, and may interpret information incorrectly or superficially). Once identified and interpreted, information must then be synthesized with other information obtained. This is a higher order thinking skill, again directly related to the clinician's organization of knowledge. It is useful to conceptualize the working interpretations made throughout the patient examination and ongoing management as hypotheses as this discourages premature conclusions. Instead, further information obtained is interpreted and considered against existing hypotheses (i.e. tested) as either supporting or not-supporting. This process of hypothesis generation involves a combination of specific data interpretations or inductions (generalizing from the specific) and the synthesis of multiple clues or deductions (instancing from generalizations) that, taken together, has been characterized as hypothetico-deductive or ‘backward reasoning’ (Arocha et al. 1993, Patel & Groen 1991). In this sense clinical reasoning is a cyclic process of information perception and interpretation (i.e. hypothesis generation) followed by further information collection, interpretation and synthesis (i.e. hypothesis testing, modification and additional hypothesis generation). The reassessments following treatment interventions represent another example of hypothesis testing as reflected in the arrow in Figure 2.2 which runs from reassessment back up to the therapist's evolving understanding of the problem and person. It is important for student physiotherapists to learn to think on their feet. While examination routines are helpful to ensure a thorough and systematic assessment of the neuro-musculoskeletal system, examination by rote (i.e. simply following a protocol without reasoning) is inefficient and likely to lead to recipe treatments that are not tailored to the individual patient and so are less effective.
The hypothetico-deductive reasoning process portrayed in the left side of Figure 2.2 underpins the diagnostic process used in medicine and physiotherapy. While experts with extensive experience and superior knowledge are often able to use pattern recognition (discussed later) to circumvent extensive generation and testing of competing hypotheses when confronting familiar presentations (Elstein & Schwarz 2002, Kaufman et al. 2008, Patel & Groen 1986, Patel et al. 1986), the process of differential diagnosis still exists as typically the two or three most likely patterns are considered. However, where medical diagnosis normally has a disease or pathology focus, physiotherapy physical diagnostic reasoning tends to incorporate a broader analysis of the patient's functional capabilities and physical impairments along with their established or hypothesized pathology as they relate to the presenting activity and participation restrictions (APTA 2003, Jensen et al. 2007, Jones & Rivett 2004).
The patient's thinking
Understanding the patient as a person rather than simply their biomedical physical problems requires understanding their perspectives or their thoughts, feelings, self-efficacy and coping strategies as reflected in the boxes on the right side of Figure 2.2. Patients' beliefs and feelings which are counterproductive to their management and recovery can contribute to their lack of involvement in the management process, poor self-efficacy and ultimately a poor outcome. Patients acquire their own ideas and associated feelings regarding their health problems from their personal experiences including advice from medical practitioners, family and friends. While typically not thought of as such, these can be equated to their ‘hypotheses’ regarding what is going on with their body, how serious it is and what can and should be done about it. A brief summary of research findings demonstrating the potential influences of patients' perspectives on their clinical presentation, expectations and willingness to self-manage follows.
Patients' perspectives of their problem have been shown to impact on their levels of pain tolerance, attempts to adjust or cope, their mood and pain related disability and eventual outcome (Craig 2006, Flor & Turk 2006, Gottlieb et al. 2001, Jensen et al. 2003, King et al. 2002, Williams & Keefe 1991, Wilson et al. 1993). Levels of anxiety have been shown to influence pain severity, complications following surgery and days of hospitalization (DeGroot et al. 1997, Pavlin et al. 1998, Salkovskis 1996). Anxiety is most common when symptoms are unexplained, the future is uncertain and the patient is concerned about the perception of others. A reciprocal relationship exists so that negative thoughts elicit negative moods and negative feelings in turn adversely influence patients' appraisals of their problem. Reduction in pain-related anxiety has been demonstrated to predict improvement in functioning, affective distress, pain and activity levels (McCracken & Gross 1998). Patients' preoccupation with negative thoughts and self-statements about their circumstances and future prospects (i.e. ‘catastrophizing’) is a risk factor for pain-related fear and long-term disability (Pincus 2004, Vlaeyen & Linton 2000). Greater worry about pain is also associated with hypervigilance, or over-attention and misinterpretation of body sensations. Negative, unhelpful thoughts tend to relate to the meaning patients attribute to their problem or pain. Patients with low self-efficacy (i.e. low perception and confidence in ability to cope and make a change) tend to be convinced their own efforts will not be successful and tend to use less constructive coping strategies. This perceived helplessness has been related to pain level and disability (Gatchel et al. 2007).
Assessment, management and reassessment of patients' thoughts and feelings contribute to both the patient's and the therapist's evolving understanding of the significance these factors have to the clinical presentation. When unhelpful thoughts and feelings are successfully addressed patients gain a deeper understanding of their problem that includes recognition of the extent to which their incorrect and often excessively negative perspectives have been contributing to it. This new more constructive understanding enhances their self-efficacy and self-management. Assessing a patient's perspectives requires an understanding of what makes up a health perspective.
Health perspectives (pain, illness, self)
Research into patient's health and disability perspectives highlights important components that make up a patient's understanding/beliefs and concerns about their problem. The experience of pain is integrally associated with personal perceptions and social influences such that patients' pain perceptions, experiences and coping combine into a pain or disability experience lived as a whole (Kleinman et al. 1992, Sim & Smith 2004). As such, the various elements can never truly be isolated. However, greater understanding of the components of the pain experience and their interrelationships is important to guiding what information the physiotherapist listens for and seeks out (either through questionnaire or interview) when attempting to understand the person and any psychosocially related factors that may be contributing to their presentation. Research in medical anthropology, medical sociology and cognitive psychology has all contributed to the understanding of illness representations or schemas (e.g. Bishop 1991, Pincus & Morley 2001, Skelton & Croyle 1991, Sim & Smith 2004, Turk & Rudy 1992). Leventhal et al. (1980) put forward the notion that patients' mental representations of health threats determine how they respond to those threats. Illness schemata are defined as individuals' ‘implicit theories of illness’ that they use in order to interpret and respond to health threats. These illness (or pain) schemas are like imprints, or patterns of interconnected features, learned (consciously or unconsciously) through social and personal experiences. Skelton and Croyle (1991, p. 4) report on illness cognition research that demonstrates illness schemas comprise the following elements:
1. Concrete symptoms and a label (e.g. a common cold vs pneumonia) that facilitate identification of the health problem
2. Beliefs about the immediate and long-term consequences of the problem, and
3. Its temporal course, and attributions concerning the cause of the problem and the means by which a cure may be affected.
Research has also identified a number of dimensions that people use in evaluating their health problem including their perception of its seriousness, social desirability, personal responsibility, controllability and changeability (Bishop 1991). Therefore it is not only the person's existing beliefs and assumptions that make up their illness schema and contribute to determining their coping but also their appraisal of the threat their medical condition poses. This highlights the importance of assessing, and if necessary addressing through education, the patient's threat appraisal (Jones & Edwards 2006, Moseley 2004).
A person's understanding, expectations and concerns about different types of pain (e.g. needle injection pain, toothache pain, back pain, etc.) would make up their pain schema which Pincus and Morley (2001) suggest comprises beliefs regarding the immediate sensory-intensity, spatial and temporal features of pain along with the initial affective responses and self-protective behaviours that ensue. The pain schema would also likely include a similar appraisal as the illness schema regarding its seriousness and controllability/changeability.
Lastly, Pincus and Morley (2001) discuss a ‘self’ schema as a complex multifaceted construct that relates to who you are with reference to who you used to be (prior to your perceived change in self) and who you would like to be in the future. It includes an evaluative dimension that contributes to an individual's sense of self-worth. Pain and disability have the potential to disrupt aspects of the self, such that repeated failures to function ‘normally’ and the negative emotions that result can lead to changes in a person's self-image (Osborn & Smith 1998, Sim & Smith 2004, Steen & Haugli 2000).
Pincus and Morley (2001) also propose that these different schemas can be enmeshed so that a pain schema for example may enmesh with an illness schema and elicit interpretations of the pain as a marker or part of a larger illness or health problem. Similarly, perceptions of the threat a pain condition or illness may create can be enmeshed with the patient's self-worth as with the chronic back pain patient whose pain has not been adequately explained by the medical system who develops perceptions (real or imagined) that his family, employer and/or co-workers don't believe him, causing him to feel he is not a good work-mate, spouse, parent, etc.
The value of this concept of different pain, illness and self schemas to patients' presentations is not for physiotherapists to attempt to classify a patient's schemas or their theoretical schema enmeshment, instead the value is to our clinical reasoning and the scope of patient perspectives we listen for and seek out when attempting to assess psychosocial factors. Patients are clearly not homogeneous when you consider the different pathologies that can cause pain and disability, the continuum of any particular pathology (minor to extensive), the physical impairments that can predispose to the problem or be created by the problem, and the different perspectives (understandings, beliefs, fears, coping mechanisms, self-image, etc.) that exists in varying combinations. This is important to our clinical reasoning as it highlights theory we must understand (e.g. pain and disability associations with psychosocial factors), skills we must acquire in order to assess (e.g. questioning about psychosocial factors, questionnaires to use) and manage (e.g. education and cognitive-behavioural strategies, referral pathways) this dimension of our patients' presentations. Understanding patients' perspectives is also important as their understanding, attributions, feelings, etc., will influence other perspectives. For example, expectations of management such as the perspective ‘my disc is out’ causing the expectation that nothing can be done or perhaps physical/passive treatment is required; expectations regarding personal responsibility and self-management, such as the perspective/belief that ‘the problem is my degenerative spine’, without appreciating the physical (e.g. relative flexibility, motor control, fitness), lifestyle and environmental factors that may have predisposed the degenerative spine to become symptomatic and require a significant contribution of self-management; and expectations regarding the future as with the perspective ‘my back-knee-shoulder, etc. is stuffed and I will never be able to work-exercise-etc. again’. Understanding patients' problems diagnostically and understanding patients' perspectives require considerable bio-psychosocial research and practice knowledge.
The level of education physiotherapists receive in psychosocial assessment and management varies considerably. Jones and Edwards (2006) have suggested the following categories of information are screened when assessing patients' perspectives (i.e. psychosocial status):
• What are patient's perspectives of their experience?
 their understanding of their pain/condition?
their understanding of their pain/condition?
 their management expectations and goals?
their management expectations and goals?
 their threat appraisal with regard to its seriousness, social desirability, personal responsibility, controllability and changeability?
their threat appraisal with regard to its seriousness, social desirability, personal responsibility, controllability and changeability?
 their level of stress and distress?
their level of stress and distress?
 stress: over-attention to sensory information and fear-avoidance or more extensive over-attention to overall health with catastrophizing cognitions and overt symptoms of stress?
stress: over-attention to sensory information and fear-avoidance or more extensive over-attention to overall health with catastrophizing cognitions and overt symptoms of stress?
 distress: natural, harmless feelings of frustration to more significant and higher levels of distress (e.g. depression) affecting their ‘self’?
distress: natural, harmless feelings of frustration to more significant and higher levels of distress (e.g. depression) affecting their ‘self’?
• How does patient think they are perceived by others and how does this affect how they feel about themselves?
 attention seeking or response to society's expectations? Some will feel they need to justify their pain as real and not just in their head
attention seeking or response to society's expectations? Some will feel they need to justify their pain as real and not just in their head
• How does the patient compare themself with others?
• Does patient avoid activities/withdraw from others due to pain/disability/social stigma?
• What is the patient's ‘motivation’ for change? For example:
As a measure of their ‘motivation’ the patient can then be asked: ‘On a scale of 0 to 100, how ready are you to make these changes? How important are these changes to you? How confident/ able are you to make these changes?’
There is now also a wide range of questionnaires available for screening patients' psychosocial related issues (see Table 2.1 for an example). While these questionnaires provide a helpful resource, on their own they are insufficient to guide the physiotherapist's management. They provide useful insight to a patient's thoughts, beliefs and feelings but they generally do not provide the basis of those thoughts and feelings. As such, physiotherapists need to review the completed questionnaire with the patient to explore further the patient's answers. That is, questionnaires such as these should not be seen as a replacement for the interview questions suggested above, rather they should be used as an adjunct and an objective means of documenting and scoring patients' psychosocial status.
Table 2.1
Examples of psychosocial screening questionnaires
| Questionnaire | Purpose | Source |
| Fear-avoidance Beliefs Questionnaire | To measure patients' beliefs about how physical activity and work affect their low back pain. It can help identify patients for whom psychosocial interventions may be beneficial | Waddell et al. (1993) |
| Tampa Scale of Kinesiophobia | To measure patients' fear of movement/re-injury in persistent pain. The Tampa Scale Kinesiophobia-11 (TSK-11) uses 11 out of the 17 items from the original version of the Tampa Scale of Kinesiophobia | Woby et al. (2005) |
| Örebro Musculoskeletal Pain Screening Questionnaire | To identify how likely it is that workers with soft tissue injury will develop long-term problems (screening for yellow flags). This screening questionnaire, when completed 4–12 weeks after musculoskeletal injury, predicts long-term disability and failure to return to work | Linton and Hallden (1998) |
| Centre for Epidemiologic Studies-Depression Scale | To measure anxiety, depression and depressed mood symptoms | Radloff (1977) |
| Kessler Physiological Distress Scale | To measure non-specific psychological distress (primarily intended as a measure of mood, anxiety and depression) | Kessler et al. (2002) |
| Chronic Disease Self-efficacy Scales | To measure patients' beliefs that they can manage their chronic condition (e.g. symptom control, role function, emotional functioning and communicating with physicians). | Lorig et al. (1996) |
| Self-Efficacy for Managing Chronic Disease 6 Item Scale | To measure patients' symptom control, role function, emotional functioning and communicating with physicians | Lorig et al. (2001) |
| Perceived Health Confidence Scale | To measure patients' views of their competence in taking care of their health. It is a domain-specific measure of the degree to which an individual feels capable of effectively managing their health outcomes. | Smiths, Wallston and Smith (1995) |
| Perceived Stress Scale | To measure patients' perception of stress. It is a measure of the degree to which situations in one's life are appraised as stressful. The scale also includes a number of direct queries about current levels of experienced stress | Cohen, Kamarck and Mermelstein (1983) |
| Pain Self-efficacy Questionnaire | To measure chronic pain patients' self-rated confidence in performing activities despite the presence of pain | Nicholas (2007) |
| Modified Somatic Perceptions Questionnaire | To measure clinically significant psychological distress in patients with persistent back pain (a measure of heightened somatic and autonomic awareness related to anxiety and depression) | Main (1983) |
| PHQ9 and PHQ2 | PHQ-9: To assist diagnosis and guide management of depression. PHQ-2: To identify patients who may have depression and require referral for further diagnostic assessment. |
Arroll et al. (2010) |
It is beyond the scope of this chapter to extend this discussion to the physical and cognitive-behavioural management strategies needed to address patient perspectives judged as contributing to their disability and/or presenting as obstacles to their recovery. However, there is now very helpful physiotherapy literature providing suggestions on assessment and management strategies specifically targeting patients' unhelpful thoughts, feelings and behaviours (e.g. Harding 1998, Johnson & Moores 2006, Keefe, Scipio & Perri 2006, Kendall & Watson 2000, Main & Watson 2002, Main et al. 2008, Muncey 2002, Strong & Unruh 2002).
Clinical reasoning as collaboration between therapist and patient
Thinking of clinical reasoning through examination and management as a therapeutic alliance where collaboration, rather than simply compliance, is sought is important to encourage students and therapists to involve their patients in the decision making process (Edwards et al. 2004b, Higgs & Hunt 1999, Jensen et al. 2002, Payton et al. 1998, Trede & Higgs 2008). While obviously the patient has come to the physiotherapist seeking their expertise, treatment and advice, patients who have been given an opportunity to share in the decision making have been shown to take greater responsibility for their own management, are more satisfied with their health care (reducing risk of formal complaints) and have a greater likelihood of achieving better outcomes (Arnetz et al. 2004, Edwards et al. 2004b, Trede & Higgs 2008). Despite acknowledging the importance of being collaborative with their patients many physiotherapists do not respond to patients' life and treatment priorities or work with patients in collaboratively setting goals (Edwards et al. 2004b). Patient learning (i.e. altered understanding and improved health behaviour), improved self-efficacy and shared responsibility in management are primary outcomes sought in a collaborative reasoning approach.
Therapist learning also occurs through collaboration. That is, when patients are given the opportunity to tell their story rather than simply answer questions, reflective therapists, who attend to individual patient presentations noting features that appear to be linked (such as increased stress affecting one patient's symptoms but not another's), will learn the variety of ways in which patients' health, cognition, behaviour, movement and pain can interact. Specific strategies for involving patients in their health care, including when differences in opinion exist, are addressed by Edwards et al. (2004b) and Trede and Higgs (2008).
The box on the far left-hand side of Figure 2.2 highlights important variables influencing the therapist's clinical reasoning including their knowledge base, their cognitive, metacognitive (including critical thinking), and their data collection skills.
Clinical reasoning and knowledge
The importance of knowledge to physiotherapists' clinical reasoning is highlighted in Jensen's expertise research where expert physiotherapists were seen to possess a broad, multidimensional knowledge base acquired through professional education and reflective practice where both patients and other health professionals were valued as sources for learning (Jensen et al. 2007). All forms of knowledge are important including physiotherapists' broader worldview, their philosophy of practice and their medical and physiotherapy specific knowledge (Cusick 2001, Higgs and Hunt 1999, Hooper 1997, Jensen et al. 2007, Unsworth 2004). However, it is not simply how much an individual knows, rather it is their organization of knowledge that is most important (Chi et al. 1988, Ericsson & Smith 1991, Hayes & Adams 2000, Rumelhart & Ortony 1977). Glaser (1984, p. 99) states that ‘effective thinking is the result of conditionalized knowledge – the knowledge that becomes associated with the conditions and constraints of its use’. In other words, for knowledge to be accessible in a clinical setting it must be organized or linked to its clinical significance. While not addressed here, this has important implications to physiotherapy educators to ensure that the basic sciences underpinning physiotherapy practice are taught in a manner that facilitates this clinical link (e.g. Problem based/experiential learning) and that practical and clinical subjects also strategically link their content to the relevant basic sciences (e.g. biomechanics, pain science, etc.).
Knowledge emerges from what we believe or hold to be true (Higgs et al. 2008). Physiotherapists utilize a combination of propositional knowledge (‘knowing that’) generated formally through research and scholarship and non-propositional knowledge (‘knowing how’) generated primarily through practice experience. Higgs and Titchen (1995) divide non-propositional knowledge further into professional craft knowledge and personal knowledge. Craft knowledge comprises professional knowledge such as procedural and communication knowledge and skills, based on academic propositional knowledge that has been refined and contextualized through clinical experience. Personal knowledge includes that knowledge acquired through personal life experiences (including community and cultural) that contribute to shaping a person's beliefs, values and attitudes, or what Mezirow (1990, 1991) has called their ‘meaning perspective’ (also synonymous with Maitland's ‘Frame of reference’). As already discussed, a person's perspectives (therapist and patient) significantly influence their interpersonal interactions and their expectations. Therapists who are alert to both community and their own attitudes (i.e. personal knowledge) regarding for example different population subgroups (e.g. ethnic, workers compensation, substance abuse) are better able to safeguard against their own assumptions, biases/prejudices leading to premature or incorrect judgments.
Understanding and successfully managing patients' problems requires a rich organization of all three types of knowledge. Propositional knowledge provides us with theory and research substantiation on which to base our practice while non-propositional professional craft knowledge provides us with the means to use that theory and research evidence in the clinic.
The importance of craft knowledge cannot be overstated. Maitland placed enormous emphasis on clinical skills (subjective questioning and examination/treatment procedures). While these were initially taught as propositional knowledge of subjective and physical examination routines and correct execution of examination and treatment techniques, they were then refined through clinical supervision to be tailored to patients' particular presentations with continual clarification of patient answers and adjustment of examination and treatment procedures. It was not uncommon for Maitland to demonstrate on a patient a treatment procedure he had never used in exactly the way it was being demonstrated, as he had adapted the procedure to the patient's particular presentation. That nicely illustrates the use of craft knowledge and the importance of using propositional knowledge as a guide, not a prescription, for how to practise.
Clinical reasoning and cognition/metacognition
In addition to the therapist's organization of knowledge, their cognitive skills (e.g. data synthesis/analysis and purposeful inquiry strategies) and their metacognitive skills (self-awareness and critical reflection) are key factors influencing their clinical reasoning proficiency. Cognition in clinical reasoning commences with the perception of what is relevant. Closely related to knowledge, perception includes recognizing potentially relevant cues available from medical records/reports and patient information (verbal and non-verbal) obtained directly through interview and from the physical examination. A student's reasoning may be limited simply due to their inability to recognize important information.
Physiotherapists' decisions regarding physical assessment (e.g. extent of assessment that can be safely carried out and which assessments to prioritize at the first appointment), physical diagnosis, influence of environmental and psychosocial factors, treatment and prognosis relate to their ability to synthesize and analyze the mass of information obtained about a patient's presentation and the weighting they have given (consciously or unconsciously) to the various findings. Synthesis (e.g. for consistency of information) and analysis (i.e. for meaning and recognition of patterns) are higher order forms of cognition. A challenging aspect of analysis is that one cue can alter the interpretation of another. For example, patients with significant central sensitization in their clinical presentation may have provocative physical examination tests that on their own would implicate pathology/impairment of a particular structure/tissue. However, when the pain provoked is considered in light of an apparent dominant central pain state it may actually be a false positive, painful due to the sensitization rather than actual local pathology (Meyer et al. 2006, Nijs et al. 2010, Wolf 2011).
Metacognition is a form of self-awareness that incorporates monitoring of yourself (e.g. your performance, your thinking, your knowledge) as though you are outside yourself observing and critiquing your practice. There is an integral link between cognition, metacognition and knowledge acquisition or learning from clinical practice experience (Eraut 1994, Higgs et al. 2004, Higgs et al. 2004, Schön 1987). For example, following protocol assessments without reasoning requires little cognition beyond remembering a routine that was memorized. In contrast, questions and physical assessments used with a specific purpose in mind provide a more complete picture of the patient's presentation while enabling working hypotheses to be ‘tested’ and clinical patterns recognized. While hopefully all therapists think, not all therapists think about their thinking. It is this self-awareness and self-critique that prompts the metacognitive therapist to reconsider their hypotheses, plans and management.
This self-awareness is not limited to formal hypotheses considered and treatments selected as metacognitive awareness of performance is also important. This for example underpins the experienced therapist's immediate recognition that a particular phrasing of a question or explanation was not clear. Similarly metacognitive awareness of the effectiveness of a physical procedure enables immediate recognition that the procedure needs to be adjusted or perhaps should be abandoned as for example when cues such an increase in muscle tone or the patient's expression signal the procedure was not achieving its desired effect.
Lastly metacognition is important to recognizing limitations in knowledge. The student or therapist who lacks awareness of their own knowledge limitations will learn less. Experts not only know a lot in their area of practice, they also know what they don't know. That is, the expert is typically very quick to recognize a limitation in their knowledge (e.g. a patient's medication they are unfamiliar with, a medical condition, a peripheral nerve sensory and motor distribution) and act on it by consulting a colleague or appropriate resource. In short metacognition and critical reflection are important means to continued professional career-long learning.
Motivation to acquire knowledge through entry level physiotherapy education emanates from internal interests enhanced by formal assessment requirements to pass a subject/program. Knowledge acquisition in clinical practice is driven largely by personal desire to understand more and achieve better outcomes. Inherent in the learning through formal academia and through clinical practice is the critical thinking and reasoning ability to ask skilled questions of yourself (i.e. critical reflection) and of others (educators, colleagues, patients). What follows is a brief discussion of skilled questioning important to critical thinking in general (e.g. self-reflection and discussions/debates with students, classmates, work colleagues and educators) and skilled questioning specific to clinical practice.
Skilled questioning important to critical thinking and learning
Thinking is driven by questions in that questions define or clarify issues being discussed. An open and questioning mind is a prerequisite to skilled critical thinking and reasoning which in turn cultivates deep learning. The art of asking questions and pursuing answers originated by Socrates (Athens, c. 469–399 BC), called ‘Socratic questioning’, is based on the notion that thinking (e.g. interpretations, opinions, analyses, conclusions) has a logic or structure that underpins it that typically is not evident in the initial expression (Paul & Elder 2007). The purpose of Socratic questioning is to clarify and understand the logic of someone's thought (including your own through critical reflection). Paul and Elder (2006, pp. 54–55) note that:
All thinking has assumptions; makes claims or creates meaning; has implications; focuses on some things and throws others into the background; uses some concepts or ideas and not others; is defined by purposes, issues, or problems; uses or explains some facts and not others; is relatively clear or unclear; is relatively deep or superficial; is relatively critical or uncritical; is relatively elaborated or underdeveloped; is relatively mono-logical or multi-logical.
Through disciplined questioning complex ideas and concepts can be explored, truth can be sought, unrecognized issues and problems can be revealed, assumptions can be made apparent, what is known and not known can be made evident and the logical implications of thought can be highlighted. From an educator's perspective Paul and Elder (2006, p. 55) highlight the value of successful Socratic questioning discussions to:
…take student thought from the unclear to the clear, from the unreasoned to the reasoned, from the implicit to the explicit, from the unexamined to the examined, from the inconsistent to the consistent, from the unarticulated to the articulated.
Edited examples of different types of Socratic questions related to critical thinking in general (but also relevant to critical thinking in the clinic) as suggested by Paul and Elder (2006, pp. 5–7, 20–23) are highlighted in Box 2.1.
Skilled questioning important to clinical practice
The accuracy and effectiveness of our clinical judgments is influenced by the quality of information (e.g. patient interview and physical examination) on which those judgments are based. The manner in which an examination and therapy is provided with respect to patient rapport and the level of therapist interest, empathy and confidence conveyed influences patients' information volunteered, motivation for change, willingness to participate in self-management and their outcome in general (Klaber et al. 1997). While the specific questions and sequence of questions asked will vary according to education and personal experience, the aim should be the same, that is to understand the patient's problem and their individual pain/disability experience in order to inform effective, collaborative management.
Many of the generic critical thinking questions outlined above are equally relevant to skilled patient questioning. Maitland offered excellent examples of questioning strategies to optimize the quality of information obtained (Maitland 1986). Perhaps the one he emphasized most was to never assume and therefore to always clarify the patient's meaning. There are numerous examples of where this is helpful including the following:
Clarification for precision
There are many situations where the patient makes a general statement that requires clarification to understand precisely their meaning. Examples include such things as constancy of symptoms (where clarification of ‘constant’ reveals daily symptoms but not every moment of the day); area of symptoms (where for example patient's perception of their ‘shoulder’ is clarified to actually be their supraspinous fossa); and aggravating factors (where for example ‘walking’ requires clarification regarding what aspect of the walking is a problem – time, speed, distance, surface, phase of gait, etc.?).
Clarification for accuracy
Patient responses are often generalizations where the lack of accuracy can lead to misinterpretations. Examples here include reassessments of previous treatment sessions (where the patient reports no benefit but clarification reveals symptoms significantly improved for a period of time before returning); and patient reports of what others have said or the attitude/support of others (e.g. doctors, employers, family) that reflect the patient's perspective but not always reality.
Clarification for relevance
While it is important to always give patients a voice and an opportunity to tell their story, it is also necessary to control the interview for time management. This requires considerable communication skills to establish the relevance of a particular tangent the patient seems to be taking and diplomacy to bring them back on track while still conveying interest.
Clarification for completeness
Completeness (thoroughness) of examination and reassessments is necessary to ensure nothing important is missed. This relates to another clinical reasoning tactic referred to as ‘screening questions’.
Screening questions
Patients will typically volunteer the information they feel is important and related to their main problem. However, they will often not appreciate the potential importance of other information they may feel is unrelated. Without thorough screening, information may be missed and as a result reasoning compromised. Important areas to use screening questions for completeness include mapping out the patient's symptoms, establishing their behaviour of symptoms and medical screening for precautions and contraindications to examination and treatment.
While the patient will obviously describe their main complaint they may not feel other symptoms and problems in other body areas are relevant. Clearing other body areas, as emphasized by Maitland, ensures the main complaint is considered in the context of the patient's broader health presentation. For example, when clarified a recent peripheral joint pain may turn out to be part of a broader systemic disorder, only recognized when further screening reveals involvement of other joints. Similarly, patients will report their main symptom(s) but may not consider other symptoms as relevant or may not even recognize other feelings as symptoms until questioned. Examples of common neuromusculoskeletal symptoms that should be screened for include:
• Neuropathic symptoms (numbness, paraesthesias, etc.)
• Vascular and autonomic symptoms (swelling, skin colour, skin dryness/perspiration)
• Clicks, clunks, giving way, locking
• Vertebrobasilar insufficiency (VBI)/ cervical arterial dysfunction (CAD) symptoms (related to cervical problems), spinal cord symptoms (related to spinal problems), cauda equina symptoms (related to lumbar problems).
As with mapping out the patient's symptoms, when questioning in order to determine aggravating factors, patients will often only mention what they remember or consider most significant. However, if the therapist is reasoning through the examination they should, based on the patient's area of symptoms, consider different structures that may be involved and with that knowledge direct further questions to ‘test’ those hypotheses. For example, a posterior buttock pain may be emanating from the hip, the sacroiliac joint, the buttock muscles/soft tissues, a neural source (e.g. sciatic or nerve root), or be referred from the lumbar spine. While no aggravating activity will affect a single joint or structure in isolation, questions about other potential aggravating factors that tend to affect one area more than another can assist the evolving picture. For example, if the buttock pain is worsened by crossing the legs and/or squatting, the hip and/or sacroiliac joint-associated tissues are incriminated. This can then be considered against other aggravating factors explicitly screened for which relate to spinal movements and neurodynamics; it may also highlight movements and structures that must be examined and differentiated. The third main area where it is important to screen for completeness, medical screening for precautions, and contraindications to examination and treatment will be discussed later within the section on Hypothesis Categories.
Effects of therapist's questioning/manner on the patient
While the patient interview is largely about gaining information to understand the patient and their problem, the nature and manner (i.e. tone, non-verbal behaviours) of the therapist's questions and responses to patient answers will influence the interest the patient perceives the therapist has in them, the confidence they have in the therapist and the success of the therapeutic relationship in general (Klaber et al. 1997). Maitland emphasized the importance of establishing patient rapport through the interest and belief conveyed in what they say and through the thoroughness of examination you demonstrate. Our questions and responses (verbal and non-verbal) are interpreted by patients as conveying our thoughts. Many patients report negative experiences with medical and other health professionals who they felt didn't listen or believe them. Without good rapport the patient is less likely to collaborate in providing the necessary information or participate in the management jeopardizing the eventual outcome.
Skilled questioning should be open but specific. The therapist should seek understanding of the person and their problem(s), be efficient while giving the patient a voice, and constantly clarify responses for precision, accuracy, relevance and completeness. The therapeutic relationship, reasoning and outcome are all enhanced when the therapist's listening and responding conveys interest, acknowledgement/empathy, respect, and collaboration while reserving judgment. While patients may need to be challenged at some stage regarding their beliefs, attitudes and health behaviours, argumentation should be avoided and where possible opportunities should be sought to support patient self-efficacy. Patients are unlikely to make the necessary lifestyle changes unless they believe they have the capacity to do so. Brief summaries of your understanding of the patient's story, including your assessment of their perspectives, are important to validate the patient's meaning. While physical impairments such as range of movement and strength are quantitative measures that can be judged against established normative data, patient perspectives represent qualitative data that does not lend itself to absolute interpretations of normality (i.e. adaptive versus maladaptive/unhelpful perspectives) and hence require validation with the patient (Edwards et al. 2004b, Stewart et al. 2011).
Facilitating application of bio-psychosocial practice: clinical reasoning strategies and hypothesis categories
Being able to practice within a bio-psychosocial framework requires different sets of knowledge and clinical skills to be able to understand both the biomedical problem (disease, disorder, illness) and the environmental and personal factors that may predispose or contribute to the problem. As such a distinction can be made between understanding and managing the physical problem to effect change versus understanding and interacting with the person to effect change. To assist physiotherapists' application of bio-psychosocial practice, we have promoted the evolution of our understanding and recommended use of two frameworks for guiding the focus of decision making required (clinical reasoning strategies) and the types of decisions required (hypothesis categories) (American Physical Therapy Association 2003, Christensen et al. 2011, Edwards et al. 2004a, Jones 1987, 1992, 1995, 1997a, 1997b, Jones et al. 2002, Jones and Rivett 2004, Jones et al. 2008).
Clinical reasoning strategies
While clinical reasoning is often equated with diagnostic decision making, in reality that represents only a small portion of the reasoning that actually occurs in clinical practice. In a qualitative research study of clinical reasoning in physiotherapy, Edwards and colleagues (Edwards 2000, Edwards et al. 2004a) identified patterns in the focus of expert physiotherapists' clinical reasoning in three different fields of physiotherapy (musculoskeletal, neurological and domiciliary care). Individual expert therapists in all three fields employed a range of ‘clinical reasoning strategies’, despite the differing emphases of their examinations and management. The clinical reasoning strategies identified were each associated with a range of diverse clinical actions. While this was the first physiotherapy study to elucidate expert physiotherapists use of this full range of strategies, they have been identified previously either by research, by theoretical proposition or by an exposition of the relevant skills in the literature of medicine, nursing, occupational therapy and physiotherapy under the following names: diagnostic or procedural reasoning (Elstein et al. 1978, Fleming 1991); interactive reasoning (Fleming 1991); conditional or predictive reasoning (Fleming 1991, Hagedorn 1996); narrative reasoning (Benner et al. 1992, Mattingly 1991); ethical reasoning (Barnitt & Partridge 1997, Gordon et al. 1994, Neuhaus 1988); teaching as reasoning (Sluijs 1991); and collaborative decision making (Beeston and Simons 1996, Jensen et al. 2007, Mattingly & Fleming 1994). The clinical reasoning strategies identified by Edwards and colleagues (Edwards 2000, Edwards et al. 2004a) can be grouped broadly under a classification of ‘Diagnosis’ and ‘Management’ as follows:
Diagnosis
1. Diagnostic reasoning is the formation of a diagnosis related to functional limitation(s) and associated physical impairments with consideration of pain mechanisms, tissue pathology and the broad scope of potential contributing factors.
2. Narrative reasoning involves understanding patients' pain, illness and/or disability experiences, or their ‘story’. This incorporates their understanding of their problem and the effect it is having on their life, their expectations regarding management, their feelings and ability to cope and the effects these personal perspectives have on their clinical presentation, particularly whether they are facilitating or obstructing their recovery.
Management
3. Reasoning about procedure is the decision making behind the selection, implementation and progression of treatment procedures.
4. Interactive reasoning is the purposeful establishment and ongoing management of therapist-patient rapport.
5. Collaborative reasoning is the nurturing of a therapeutic alliance towards the interpretation of examination findings, the setting of goals and priorities and the implementation and progression of treatment.
6. Reasoning about teaching is the planning, execution and evaluation of individualized and context sensitive teaching, including education for conceptual understanding and education for physical performance (e.g. exercise, posture, sport technique correction).
7. Predictive reasoning is the therapist's judgment regarding prognosis and their interaction with the patient to envision future scenarios with collaborative exploration of the different paths identified and the implications each holds.
8. Ethical reasoning involves the recognition and resolution of ethical dilemmas which impinge upon the patient's ability to make decisions concerning their health and upon the conduct of treatment and its desired goals.
The reasoning and judgments made within these different reasoning strategies span a continuum from biomedically focused diagnostic reasoning to psychosocially focused ‘narrative’ reasoning. The diagnostic reasoning focus and the associated procedural management of physical impairments are aligned more with the experimental quantitative research paradigm with its underlying assumptions that reality, truth and/or knowledge are best understood in an objective, measurable, generalizable and predictable framework (Edwards et al. 2004a, Jones et al. 2008). In contrast patients' pain and disability experiences (i.e. their perspectives) are less amenable to objective measurement against normative standards. As such narrative reasoning is more aligned with the interpretive qualitative research paradigm with its underlying assumptions that truth, reality and/or knowledge are context dependent, socially constructed with multiple realities. The ‘normality’ versus ‘abnormality’ language of diagnostic reasoning is too absolute and therefore less appropriate to understanding patient's pain and disability experiences through narrative reasoning (Mattingly 1991, Stewart et al. 2011) and to understanding the effects patients thoughts and feelings can have on biological phenomena such as movement (Edwards et al. 2006).
When examining and treating a patient the therapist's thinking and actions should incorporate a combination of both diagnostic and narrative oriented assessments, interventions (e.g. procedural and educative) and re-assessments. Edwards (Edwards 2000, Edwards et al. 2004a, Edwards & Jones 2007b) demonstrated that these occur dialectically, meaning the therapist will move back and forth in attending (assessing and responding) to these different dimensions of the patient's presentation as dictated by the immediate circumstances. For example, the therapist may be performing a procedure to a physical impairment that elicits a patient response relevant to understanding their perspective, necessitating a fluidity of reasoning and action that explores the patient meaning and possibly even its relationship to the procedure being performed. That is, diagnostic and narrative reasoning are not carried out separately, rather they are intertwined with the key being the therapist's knowledge and ability to listen for and question patient perspectives both in a structured manner and as opportunities arise. While physical/biomedical and psychosocial factors represent different dimensions of a patient's presentation, in reality they are closely related such that each can influence the other (Borrell-Carrió et al. 2004, Duncan 2000, Engel 1978, Leventhal 1993, Pincus 2004). Further, it is not possible to fully understand a patient's pain and disability experience without a comprehensive physical examination that reveals the extent of physical impairment and disability they have to cope with. Similarly, understanding patient's perspectives provides the therapist with valuable insight that will assist their interpretation of movement and pain responses that may not fit typical patterns of pathology and nociception.
Hypothesis categories
While the clinical reasoning strategies provide a framework to assist students and practising therapists recognize the different focus of thinking required, it is also helpful to recognize the different types of clinical decisions required in the application of these different reasoning strategies. It is not necessary or even appropriate to stipulate a definitive list of decisions all physiotherapists in all areas of physiotherapy practice must consider, as this would only stifle the independent and creative thinking important to the evolution of our profession. However, a minimum list of categories of decisions that can/should be considered is helpful to those learning clinical reasoning as it provides them with initial guidance to understand the purpose of their questions and physical assessments, encourages holistic reasoning and breadth of thought, and creates a framework in which to organize their clinical knowledge as it relates to decisions that must be made (i.e. diagnosing, understanding patients' perspectives, determining therapeutic interventions, establishing rapport/therapeutic alliance, collaborating, teaching, prognosis and managing ethical dilemmas). Any group (profession, area of practice, physiotherapy educators, and physiotherapy departments/practices) can critically reflect on the categories of decisions important for optimal bio-psychosocial practice and patient care. What follows is a list of ‘hypothesis categories’ initially proposed by Jones (1987) that has continued to evolve through professional discussion to this current format (see Box 2.2). Some evidence is available to support these categories by demonstrating that physiotherapists generate and test diagnostic and management hypotheses throughout their encounters with patients (Doody & McAteer 2002, Rivett & Higgs 1997). Anecdotal evidence from experienced physiotherapists and clinical educators also has supported the relevance and use of these particular hypothesis categories across all areas of physiotherapy practice with some variation in emphasis between therapists working in neurological, paediatric, cardiopulmonary care settings compared to outpatient musculoskeletal and sports physiotherapy. Nevertheless, these particular hypothesis categories are not being recommended for uncritical use by all therapists and whatever categories of decisions are adopted should continually be reviewed to ensure they reflect contemporary health care and physiotherapy practice.
Activity capability/restriction
Patients' activity capabilities and restrictions directly relate to the ICF framework of health and disability presented in Figure 2.1 and refer to the patient's functional abilities and restrictions (e.g. walking, lifting, sitting, etc.) that are volunteered and for which they are further screened. To gain a complete picture it is important the therapist identifies those activities the patient is capable of alongside those that are restricted.
Participation capability/restriction
Patients' participation capabilities and restrictions refer to the patient's abilities and restrictions to participate in life situations (e.g. work, recreation/sport, family, etc.). Again, determining participation capabilities, including modified participation (e.g. modified work duties) is important as this will contribute to other decisions such as prognosis and management. It is particularly important to pay attention to the proportionality of activity and participation restrictions and the physical pathology/impairments identified through examination. When activity and participation restrictions are out of proportion to identified pathology and physical impairments then it is likely the patient's perspectives on their experience (i.e. psychosocial factors) will be negatively contributing to their disability.
Patient perspectives on their experience
Patient perspectives on their experience relates to the patient's psychosocial status which the therapist tries to understand through their narrative reasoning (as discussed earlier in this chapter under ‘The patient’s thinking’). It incorporates such things as the patient's understanding of their problem (including attributions about the cause and beliefs about pain), their goals and expectations for management, the stressors in their life and any relationship these have with their clinical presentation, as well as the effects the problem and any stressors appear to have on their thoughts, feelings, motivations, their coping and self-efficacy.
Pathobiological mechanisms
The pathobiological mechanisms category incorporates hypotheses about pathology or tissue mechanisms and hypotheses about pain mechanisms. While neither of these can be validated on the basis of a clinical examination alone, biomedical knowledge of pathology and pain combined with clinical and research supported knowledge of typical clinical patterns enables therapists to hypothesize with reasonable confidence about the likely pathology and dominant pain mechanism, both of which have implications to other categories of decisions including precautions/contraindications, management and prognosis.
Pathology within the neuromusculoskeletal system can be considered at both the process and structure levels. For example, in some presentations the process (e.g. inflammatory, degenerative, ischaemic, infection, etc.) or syndrome (e.g. stenosis, impingement, instability) underpinning a person's pain and disability can be identified even when the exact structures or tissues cannot be confirmed. In other presentations the pathology can be confirmed through a combination of clinical and medical investigations (e.g. spondylolisthesis, muscle tears/tendinopathy, disc disease, etc.). Since pathology can be asymptomatic and clinical presentations within a symptomatic pathology will vary according to the extent of pathology and influence of both physical and psychological factors, skilled clinical reasoning necessitates that the therapist avoid simply administering prescribed pathology focused treatments. Rather, therapists must consider the safety and management implications of a hypothesized pathology and then strike a balance between treating the associated physical impairments and unhelpful patient perspectives while also utilizing research evidence and theory supporting pathology directed treatments (e.g. tendinopathy – Cook & Purdam 2009; intervertebral disc – Adams et al. 2010, exercise for tissue repair – Khan & Scott 2009; Van Wingerden 1995, etc.).
Pain mechanisms refer to the different input, processing and output mechanisms underlying the patients' activity/participation restrictions, unhelpful perspectives and physical impairments. These are explained more comprehensively elsewhere (e.g. Butler 2000, Fields et al. 2006, Gifford 1998a, 1998b, 1998c, Gifford et al. 2006, Meyer et al. 2006) but briefly the input mechanisms include the sensory and circulatory systems that inform the brain about the internal and external environment. Two input pain mechanisms relevant to physiotherapists are nociceptive mechanisms and peripheral neuropathic mechanisms (Butler 2000, Galea 2002, Gifford 1998a, Gifford 1998d, Meyer et al. 2006, Wright 2002). Technically all pain perception is an output from our central nervous system as nociceptive activity following a noxious stimuli will always be subjected to central modulation and it is this modulation that ultimately determines whether pain is perceived or not. However, clinically it is useful to recognize patterns of pain perception associated with nociceptive activity triggered by a peripheral stimulus such as tissue injury or overload. That is, nociceptive pain involving chemical and mechanical activation of nociceptors in somatic or visceral tissues such as joints, muscles, bone, meninges, peripheral nerve sheaths and the various viscera has a recognizable clinical pattern (Butler 2000, Smart et al. 2012a, Wolf 2011). While clinical patterns for different pain mechanisms are not fully validated, broadly nociceptive pain includes local symptoms plus or minus referral to areas of common segmental innervation (Bielefeldt & Gebhart 2006, Bogduk 1993, Schaible 2006, Smart et al. 2012a, Vicenzino et al. 2002) (chronic nociceptive pain may only present with referred symptoms), a predictable stimulus-response relationship with aggravating and easing factors (Butler 2000, Nijs, Van Houdenhove & Oostendorp 2010, Smart et al. 2012a), a history of either trauma or specific predisposing factors (e.g. overload, new activity, etc.), physical impairments that are proportional to the symptoms, activity and participation restrictions and a predictable response to treatment.
Peripheral neuropathic pain refers to symptoms with contributions from neural tissue outside the dorsal horn or cervicotrigeminal nucleus as occurs with spinal nerve root or peripheral nerve irritation/compression. Peripheral neuropathic pain can be less clear in its presentation (Butler 2000, Devor 2006, Gifford 1998d). Common features include: the type of symptoms (e.g. numbness, pins and needles, weakness, burning, itching, etc.); quality of symptoms (severe, shooting if acute); area of symptoms (distribution according to nerve although nerve root pain is typically not in classic dermatomes while paraesthesias are more dermatomal; Smart et al. 2012b); symptoms often worse at night; symptoms aggravated by movements and positions that compress or stretch the involved nerve (Smart et al. 2012b) or by situations that elicit stress or anxiety (possibly reflecting a component of central sensitization); symptoms eased by movements and positions that unload the nerve; physical impairments in neural conduction (i.e. positive neurological findings), neural mechansensitivity (i.e. positive neurodynamic and neural palpation findings) and in interfacing tissues that can compress or irritate neural tissue (e.g. structures forming borders of intervertebral foramina, adjacent muscles and fascia).
Central processing refers to the neural modulation of both input and output that occurs throughout the central nervous system/neuromatrix (e.g. Fields et al. 2006, Gatchel et al. 2007, Melzack 2005, Moseley 2003, Nijs et al. 2010, Wolf 2011) in response to internal and external sensory inputs including physical (e.g. overloaded tissues), cognitive and emotional input (e.g. thoughts, fears, anxiety, frustrations, self-efficacy, etc.). While the central nervous system is always processing input and generating output, maladaptive central processing is known to underpin some pain states causing increased responsiveness to a range of stimuli including emotional stressors, mechanical pressure, chemical substances, light, sound, cold and heat (Nijs et al. 2010). The increased sensitivity (or decreased load tolerance) can co-exist with somatic or visceral noxious stimulus nociception but can also be evoked or maintained without a peripheral noxious stimulus. Symptom provocation therefore occurs out of proportion to existing pathology and can even exist when overt pathology no longer exists. Wolf (2011) reports evidence that central sensitization has been demonstrated in a wide range of conditions commonly treated by physiotherapists including rheumatoid arthritis, osteoarthritis, temporomandibular disorders, fibromyalgia, chronic musculoskeletal disorders, headache, neuropathic pain, complex regional pain syndrome, post-surgical pain and visceral pain hypersensitivity syndromes. With central sensitization normally non-noxious stimuli and loads become provocative often creating false positive findings in the physical examination (i.e. physical testing is provocative despite the lack of overt pathology) leading to ineffective management when pain mechanisms are not understood (Butler 2000, Gifford 1998c).
Currently diagnostic criteria and biomarkers for central sensitization are lacking (Wolf 2011). However, contemporary thinking extrapolated from a broad range of research supports the observation that maladaptive central symptoms no longer follow the predictable pattern of pain with nociceptive and peripheral neuropathic contributions (Butler 2000, Nijs et al. 2010, Smart et al. 2012c, Wolf 2011). Instead, activity and participation restrictions and symptoms are typically out of proportion to the physical impairments and the symptom behaviour is less predictable with spontaneous pains, latent pains, inconsistent stimulus-response relationships to aggravating and easing factors and more pronounced associations with psychosocial stressors. Pain may be disproportionate to the nature and extent of injury or pathology with strong association to psychosocial factors and diffuse, non-anatomical areas of pain or tenderness to palpation (Smart et al. 2012c). Traditional nociceptively oriented therapies may produce short-term gains but are themselves ineffective in making lasting changes.
Melzack (2005) describes the neuroscience of patients' thoughts, feelings and pain as neurosignatures of a widely distributed neural network involving diverse areas of the brain he calls the ‘body-self neuromatrix’. Since these neurosignatures are related in part to our own subjective experiences or perceptions (e.g. pain and what it means, interpretation of what others' think, etc.) they are like our own ‘virtual reality’ of our experienced existence (Revonsuo 1995, 2006). That is our conscious experience is a construction of our brain. In this sense the chronic pain patient with significant central sensitization is trapped in their own representations/neurosignatures of their internal and external world. This is what cognitive-behavioural therapy attempts to change by firstly identifying unhelpful perspectives and then by assisting the patient to construct more adaptive perspectives, feelings and behaviours through a combination of providing convincing alternative understandings and through behavioural strategies that facilitate controlled reactivation (e.g. graded exposure, pacing, relaxation, flare-up management; e.g. Donaghy et al. 2008, Gatchel et al. 2007, Harding & Williams 1995, Keefe et al. 2006, Linton & Nordin 2006, Main et al. 2008, Muncey 2002, Strong & Unruh 2002, Turk & Flor 2006). There is now a convincing body of literature supporting the efficacy of neuroscience based pain education and cognitive-behavioural interventions for chronic low back pain patients and for preventing progression from acute to chronic pain. For example, Moseley (2004) demonstrated that individualized pain education to moderately disabled chronic low back pain patients successfully changed patients' pain cognitions (i.e. understanding) and physical performance (e.g. straight leg raise and forward bending). Vlaeyen et al. (2002) demonstrated an exposure in vivo (individually tailored practice tasks developed on the basis of graded hierarchy of fear-eliciting situations) intervention resulted in reductions in chronic low back pain patients' pain-related fear, pain catastrophizing, pain disability, pain vigilance while increasing their physical activity levels. Linton and Nordin (2006) reported on a 5-year follow-up of a randomized clinical trial investigating the efficacy of a cognitive-behavioural intervention for prevention of chronic back pain. The effects of six (2-hour) cognitive-behavioural sessions promoting patients' individualized problem solving, risk analysis, activity scheduling and other coping strategies were compared with an information comparison group who received standardized pamphlets emphasizing self-help, remaining active and ergonomic, ‘back school’ based information. The cognitive-behavioural group improvements demonstrated at an initial 1-year follow-up (Linton & Andersson 2000) were maintained at this 5-year follow-up including significantly less pain, greater activity levels, better quality of life, better general health and significantly fewer days off work due to illness.
Lastly the output mechanisms refer to the effects of central nervous system/neuromatrix modulation that produce, for example, our cognitions, emotions, learning, sleep and language as well as our motor, autonomic, endocrine and immune system functions, all of which can be adversely affected in some acute, and particularly chronic, pain conditions. In fact pain itself is an output in that it is a perception of our brain in response to the internal and external influences discussed above. While it is beyond the scope of this chapter to cover the neurophysiology and clinical presentations of these different systems, the reader is referred to a variety of resources that provide clinically relevant overviews with reference to the underlying basic science research (Butler 2000, Gifford 1998c, Jänig & Levine 2006, Mackinnon 1999, Martin 1997, Sapolsky 1998).
At present, contemporary thinking holds that if a patient presents with a ‘normal’ adaptive pain mechanism, wherein symptoms are the result of pathology or abnormal load to specific structures/tissues, it is appropriate to identify and treat relevant physical impairments while also addressing physical, environmental and psychosocial contributing factors. However, when ‘abnormal’ maladaptive central pain mechanisms are hypothesized to be present, management requires attention to stressors (physical and non-physical) thought to be sensitizing the nervous system and use of cognitive-behavioural strategies to promote increased activities, participation and general fitness. Making these judgments is not simple as often clinical features of several pain mechanisms will be present along with clear physical impairments that may or may not prove relevant. This is where skilled clinical reasoning to recognize the overlapping patterns combined with short-term treatments and re-assessments to identified relevant physical impairments will assist in establishing how much an apparent central sensitization is being driven by the symptomatic physical impairments or other co-existing cognitions, emotions and life stressors. In some cases physical impairments and disability will underpin the stress, frustrations, etc. that a patient is experiencing with resolution of the pain and the negative psyche following thorough assessment and skilled physical and environmental management. Here it is important to recognize that symptomatic physical pathology/impairment is also a source of stress that can affect neuromodulation and the neuromatrix (Melzack 2001) in order to avoid the erroneous assumption that all stress is necessary psychosocial in origin, requiring hands off therapy. In other cases sensitization is driven by both physical and cognitive/affective factors necessitating management of both. In contrast, extreme central sensitization driven primarily by psychosocial factors requires cognitive-behavioural management (Donaghy et al. 2008, Harding & Williams 1995, Muncy 2002, Strong & Unruh 2002, Turk & Flor 2006) and is unlikely to be helped by tissue-based approaches.
Physical impairments and associated structures/tissue sources
Clinical decisions identifying and judging the relevance of the patient's physical impairments combined with hypotheses regarding structures involved and potential sources of any symptoms provoked are based on findings obtained throughout the subjective and physical examination combined with re-assessments following targeted interventions to different impairments. The physical impairments are the specific regional neuromusculoskeletal abnormalities found through physical examination including impairments in posture, active and passive movement, soft tissue, neurodynamics and motor control/strength/etc. Physical impairments may be symptomatic and directly associated with the source of the patient's symptoms or asymptomatic but still contributing by altering stress/load elsewhere causing other structures to be symptomatic. Asymptomatic physical impairments must be analysed with regard to the structures responsible (e.g. restricted passive hip extension due to hip joint hypomobility, hip flexor tightness/tone or both) and whether the impairment is truly contributing to other structures being symptomatic. Again, this requires specific treatments, re-assessments and skilled reasoning to determine. Symptomatic physical impairments also have to be analysed as to the structures (and pathology) implicated and for their particular clinical presentation with respect to pain (e.g. minor to severe, non-irritable to irritable), mobility (e.g. stiff to hypermobile), dynamic control (e.g. weakness/inadequate stabilization to over-activity), and the relationship of pain provocation to passive movement (i.e. Maitland's passive movement diagram), all of which represent non-propositional craft knowledge that assists selection and progression of treatment. While clinical examination generally cannot confirm the actual source of a patient's symptoms, clues from the area and behaviour of symptoms, history, physical examination and treatments/re-assessments, combined with knowledge of common clinical patterns, will enable the therapist to hypothesize with confidence the likely structures at fault and possibly their pathology.
As an example of generating hypotheses regarding possible sources of the patient's symptoms based on the area of symptoms, consider the body chart in Table 2.2 depicting a common area of shoulder pain and the potential sources of that pain that should be considered.
Table 2.2
Body chart depicting an example of symptom location and the potential sources that should be considered for that symptom area
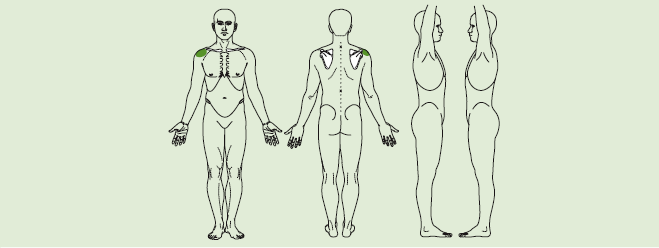
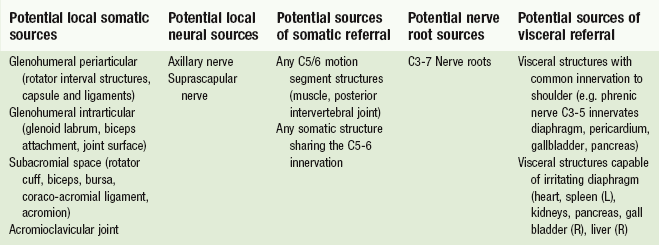
Considering potential structures involved within the suggested columns assist a though generation of hypotheses that can then be tested with further questioning through the behaviour of symptoms (aggravating and easing factors), history, medical screening and physical examination–treatment– re-assessment. As alluded to earlier, hypotheses about specific sources of the patient's symptoms must be made with consideration of the dominant pain mechanisms hypothesized. Symptomatic local tissue impairment is likely an accurate reflection of structures involved in nociceptive dominant patterns where maladaptive central processing can create false positives causing ‘healthy’ structures/tissues to be symptomatic.
Contributing factors
Hypotheses regarding potential contributing factors represent the predisposing or associated factors involved in the development or maintenance of the patient's problem. These include environmental, psychosocial, behavioural, physical/biomechanical and hereditary factors.
The potential physical contributing factors that can create excessive strain causing another structure to be symptomatic are quite varied. Examples here include hip extension stiffness causing increased lumbar spine strain during walking and weakness of the scapular upward rotators causing increase subacromial strain during shoulder elevation. Just as physical impairments commonly exist without becoming symptomatic (i.e. sources of pain), physical impairments can also cause increased strain without those tissues becoming symptomatic. While these impairments still represent risk factors for musculoskeletal symptoms later (analogous to dietary risk factors for heart disease), establishing their relevance in a patient's current pain presentation requires systematic intervention to alter the impairment and reassessment of the effect. Often this can be established relatively quickly with procedures that immediately address the impairment (e.g. manual assistance or taping of the scapula) or brief trial treatments to assess their benefit.
Even with the same pathology different patients can have different physical, environmental and psychosocial contributing factors necessitating quite different management. For example, three patients can present with similar subacromial bursitis pathology causing subacromial pain but quite different predisposing contributing factors necessitating quite different management. Patient 1, for example, may present with a tight posterior glenohumeral joint capsule causing increased anterosuperior humeral head translation during overhead activities that result in bursal irritation. Patient 2 has good posterior capsule mobility, as reflected in their good range of humeral internal rotation and horizontal flexion, but this patient has poor control/strength of their scapular force couples which are required to upwardly rotate the scapula, resulting in inadequate rotation, a narrowed subacromial outlet during overhead activities and bursal irritation. Patient 3 also has a motor control/strength problem but not of the scapula, instead the rotator cuff force couples responsible for maintaining humeral head depression during elevation are ineffective resulting in increased superior translation and, again, bursal irritation. Knowledge of common contributing factors to different clinical problems combined with skilled reasoning to establish their relevance is essential. While treatment directed to the hypothesized source of the patient's symptoms is often effective in relieving symptoms, contributing factors must be addressed in order to minimize reoccurrence.
The scenario above of one pathology (subacromial bursitis) having three different clinical presentations requiring three different approaches to management is one example of the philosophical principle contained within the ‘Brick wall’ concept put forward by Maitland (Maitland 1986; also see Chapter 1). While research evidence provides some guidance to management of different pathologies/problems, variation in clinical presentations necessitates that the therapist's management decisions are based on consideration of the patient's unique clinical presentation combined with contemporary knowledge from the current body of research evidence.
Precautions and contraindications to physical examination and treatment
Patient safety is paramount and there are a range of decisions within this hypothesis category that therapists must consider including: whether a physical examination should be carried out at all (versus immediate referral for further medical consultation/investigation) and if so the extent of examination that can be safely performed that will minimize the risk of aggravating the patient's symptoms; whether specific safety tests are indicated (e.g. vertebra-basilar insufficiency testing, neurological, blood pressure/heart rate, instability tests); whether any treatment should be undertaken (versus referral for further consultation/investigation); and the appropriate dose/strength of any physical interventions planned. A number of factors will contribute to determining the extent of physical examination and treatment that is safe to perform, including the following:
• Dominant pain mechanism (peripheral neuropathic and maladaptive central processing typically require more caution)
• Patient's perspectives (anxious, fearful, angry patients, particularly with negative past medical/physiotherapy experiences require more caution)
• Severity and irritability of symptoms (Maitland 1986)
• Nature of the pathology (e.g. rheumatoid arthritis or osteoporosis require caution due to weakened tissues)
• Progression of the presentation (e.g. worsening problems require more caution)
• Presence of other medical conditions that may masquerade as a musculoskeletal problem or co-exist and require consideration and monitoring so that musculoskeletal interventions do not compromise the patient's other health problems (e.g. cardiac and respiratory conditions).
Medical screening for other health problems requires knowledge of the body systems and common features of medical conditions, particularly those that overlap with neuromusculoskeletal problems. This form of screening is not for the purpose of assigning a medical diagnosis; rather medical screening by physiotherapists is for the purpose of identifying patients who may have medical conditions that require further investigation and medical consultation. It is particularly important to first contact practitioners who see patients that have not previously been evaluated by a medical practitioner but is it also important to physiotherapists practising under referral as non-musculoskeletal conditions may have been missed or developed since the patient last saw their doctor. Physiotherapists should be familiar with recognized ‘red flags’ which are signs and symptoms that may indicate the presence of more serious pathology and systemic or viscerogenic pathology/disease which should elicit consideration of referral for further consultation/investigation. There are different lists of ‘red flags’ available in the literature but two excellent resources written for physiotherapists are Boissonnault (2011) and Goodman and Snyder (2013). As an example of important medical screening to guide clinical reasoning regarding precautions and contraindications to physical examination and treatment, Goodman and Snyder (2013) provide the lists of ‘Guidelines for medical referral’ and ‘Precautions and contraindications to therapy’:
Readers are referred to Goodman and Snyder (2013) for additional lists of ‘red flags’ and ‘Guidelines for immediate medical attention’.
Physiotherapists need to develop a through yet efficient system of medical screening. The texts by Boissonnault (2011) and Goodman and Snyder (2013) provide a comprehensive Review of Systems that assist therapists to recognize combinations of symptoms and signs that may reflect non-musculoskeletal conditions requiring further medical consultation. Both texts also provide examples of information to include in a medical screening questionnaire which is an excellent way to thoroughly and efficiently screen a patient's medical health. Having completed the questionnaire the physiotherapist must then review the patient's responses and clarify conditions or symptoms/signs ticked to establish their history, medical management and relationship with the patient's current problem.
Management and treatment
Management in this context refers to the overall health management of the patient, including consultation and referral to other health professionals, health promotion interventions (e.g. fitness assessment and management) and patient advocacy as required (e.g. with insurers or employers). Treatment refers to the specific therapeutic interventions (physical and educational) carried out during an appointment and the underlying reasoning required to determine which impairments to address, which to address first, the strategy/procedure and dosage to use, the outcome measures to reassess and the self-management appropriate for optimizing change (in understanding, impairment, activity and participation).
Most important to skilled reasoning is that there are no recipes! Health care in general and physiotherapy care in particular are not an exact science. While clinical trials and theory extrapolated from basic science provide helpful guides to management for different problems, these should not be taken as prescriptions. Instead, therapists must judge how their patient matches the population in the research reported and then tailor their management to the individual patient's unique lifestyle, goals, activity and participation restrictions, perspectives, pathobiological mechanisms and physical impairments. Since research supported management efficacy is still lacking for most clinical problems, skilled reasoning is the therapist's best tool to minimize the risk of mismanagement and over servicing.
The bio-psychosocial model highlights the need for management to be holistic (i.e. addressing physical, environmental, psychosocial as required) with systematic and thorough re-assessments to determine inter-relationships between different physical impairments (e.g. presence of a neurodynamic impairment secondary to a soft tissue interface impairment) and between physical impairments and cognitive/affective factors (e.g. education to improve understanding leading to a decrease in patient fear and concurrent improvement in movement impairments). Management of contributing factors is essential to minimize risk of reoccurrence and patient understanding and active involvement is critical to promoting self-efficacy, self-management and long-term success.
As discussed earlier, much of the reasoning and practice knowledge associated with selection, delivery and progression of treatment falls within the area of professional craft knowledge. Since such knowledge typically lacks direct research validation therapists must be diligent in their personal reflection and critique to minimize the trap of falling into habits of practice. As discussed later, a good strategy to avoid this is to subject your reasoning and practice to critical appraisal from your peers through patient reviews and case study discussions.
Prognosis
Prognosis refers to the therapist's judgment regarding their ability to help their patient and an estimate of how long this will take. Broadly a patient's prognosis is determined by the nature and extent of patient's problem(s) and their ability and willingness to make the necessary changes (e.g. lifestyle, psychosocial contributing factors, physical contributing factors) to facilitate recovery or improved quality of life within a permanent disability. Clues will be available throughout the subjective and physical examination and the ongoing management including the:
• Patient's perspectives and expectations
• Extent of activity/participation restrictions
• Nature of problem (e.g. systemic disorder such as rheumatoid arthritis versus local ligamentous such as ankle sprain)
• Extent of ‘pathology’ and physical impairments
• Social, occupational and economic status
• Dominant pain mechanisms present
• Irritability of the disorder
While prognostic decisions also are not an exact science (Jeffreys 1991) it is helpful to consider a patient's prognosis by reflecting on the positives and negatives from the list above.
The decisions required in clinical practice will determine the information sought (e.g. safety information considered important necessitates safety oriented questions and physical tests). However, the hypothesis category framework is not intended to direct the order in which information is obtained or the precise inquiries and physical tests utilized to obtain that information. For example, musculoskeletal physiotherapists will typically follow a systematic subjective and physical examination as depicted in Table 2.3.
Table 2.3
Typical components of the subjective and physical examinations used by musculoskeletal physiotherapists
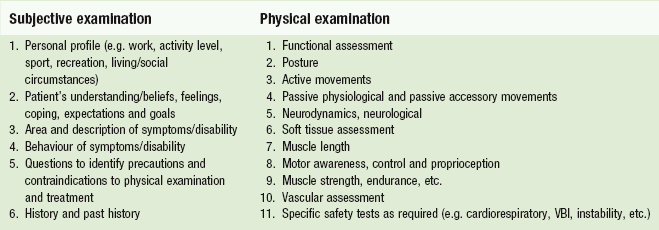
Clinical reasoning within the hypothesis category framework involves consideration of the different categories of decisions as information unfolds. While it is not possible or desirable to stipulate what hypothesis categories a therapist should be considering at any given point in time (e.g. it is not realistic or cognitively efficient to consider every hypothesis category after every new piece of information is obtained), equally the therapist should not simply be obtaining information without thinking. Mostly during the examination the therapist will be trying to understand the patient and their problem(s) in order to plan their management including judging how much physical examination can be safely performed and which physical examination procedures are most important to prioritize at the first appointment. For this focus the therapist would need to consider the patient's activity and participation capabilities and restrictions, the patient's perspectives, the pathobiological mechanisms, the structures/sources and contributing factors implicated from the subjective examination (hence requiring priority in examination), the precautions to physical examination and treatment, physical impairments found on physical testing and the structures/sources implicated, and management clues (emanating from both the subjective and physical examination). It is the therapist's ability to think on their feet through the examination and ongoing management that leads to their qualification of patient responses and the variations in examination routines. That is, all tests are not performed on every patient.
Interpreting information across different hypothesis categories
Patient information will inform several hypothesis categories at the same time. Just as the therapist may be asking a pathology/impairment oriented question but receive a patient answer that sheds light on their perspectives (i.e. psychosocial status), a question directed at understanding their activity capability and restrictions will often provide clues to other hypothesis categories at the same time. Consider for example a 72-year-old patient's response to a question regarding what aggravates their back and bilateral leg pains?
Walking. I'm afraid to even try anymore. Even short 5–10 minute walks make the back and legs worse and then I have to sit down to ease it off. Sitting is good but I can't sit all day! I can't even help out around the house anymore or get over to see the grandchildren. I'm really worried it might be something serious.
This one answer provides the following hypothesis categories information:
• Activity restriction: walking
• Activity capability: sitting
• Participation restrictions: helping around house and seeing grandchildren
• Patient perspectives: afraid to try walking, worried it may be serious
• Pathobiological: clues to nociceptive, neuropathic, vascular claudication, stenosis (neuropathic claudication)
• Physical impairments/sources: back and leg symptoms related; lumbar joints and nerve roots implicated
• Precautions: age, easily aggravated, bilateral leg pain, patient's fears/worry
• Prognosis: (−) age, disability, extent of symptoms, neuropathic, perspectives; (+) easing factor.
In the end the therapist gains clues to the different hypothesis categories throughout the whole examination and ongoing management that must be interpreted, weighed for significance and analyzed with other supporting and negating information. The knowledge that underpins the different clinical decisions comes from a broad range of both propositional and craft knowledge. Learning theory suggests that for knowledge to be clinically accessible it needs to be acquired within the conditions and constraints for which it will be used (Glaser 1984, Greeno 1998, Lave & Wenger 1991). This is typically achieved in physiotherapy education through the use of experiential/problem based teaching strategies. With the same aim, the hypothesis categories provide a bio-psychosocially oriented organizing framework to link academic knowledge to the clinical reasoning through the patient examination–treatment–re-assessment process facilitating the learning of clinical patterns.
Pattern recognition
Pattern recognition is characteristic of all mature thought (Nickerson et al. 1985). Experts across a wide range of professions have been shown to possess a large repertoire of profession specific patterns that enable them to more quickly recognize familiar problems and associated solutions (Chi et al. 1988, Higgs & Jones 2008, Jensen et al. 2007, Schön 1983). Pattern recognition relates to memory storage where knowledge has been shown to be stored in chunks or patterns that facilitate more efficient communication and thinking (Anderson 1990, Ericsson & Smith 1991, Hayes & Adams 2000, Newell & Simon 1972, Rumelhart & Ortony 1977). These patterns form categories or prototypes of frequently experienced situations (e.g. symptoms, signs, predisposing factors) that individuals use to recognize and interpret other situations, a process referred to in the medical literature as ‘forward reasoning’ (Elstein & Schwarz 2002, Patel & Groen 1986, Boshuizen & Schmidt 2008, Higgs & Jones 2008). Clinical patterns can be either generic prototypes, as found in textbooks, or they may be memories of particular patient presentations (Brooks et al. 1991, Schmidt et al. 1990) where the clinical pattern becomes meaningful through its instantiation with a real patient (Boshuizen & Schmidt 2008).
The information contained in a clinical pattern is quite varied. Boshuizen and Schmidt (2008) review the research on the development of expertise in medicine and suggest that medical clinical patterns, called ‘illness scripts’ (originally proposed by Feltovich & Barrows, 1984), typically include the ‘enabling conditions’, that is the conditions or constraints under which a disease occurs (e.g. personal, social, medical, hereditary, environmental); the ‘fault’, that is the pathophysiological process taking place; and the ‘consequences of the fault’, that is the signs and symptoms. Illness scripts are consistent with the clinical patterns physiotherapists learn and look for within their diagnostic reasoning, although the pathophysiological process will not always be confirmed.
Clinical patterns also exist when interpreting patients' perspectives through narrative reasoning and should incorporate at a deeper level: not simply the patient's perspective but also the basis of the perspective and its relationship with the behaviour and history of their symptoms/disability. Similarly clinical patterns exist within the hypothesis categories of precautions/contraindications (i.e. recognizing typical clinical features that signal the need for caution ± referral) and prognosis (i.e. recognizing typical features that support a positive or negative outcome and whether change is likely to be quick or slow).
Forward reasoning or pattern recognition enables efficiency in examination with familiar presentations. Pattern recognition is required to generate hypotheses while hypothesis testing (i.e. backward reasoning) provides the means by which those patterns are refined, proved reliable and new patterns such as recognition of common features in a particular subgroup of patients are learned (Barrows & Feltovich 1987). Where experts are able to function largely via pattern recognition with familiar problems, novices who lack sufficient knowledge and experience to recognize clinical patterns will rely on the slower hypothesis testing approach to work through a problem. However, when confronted with a complex, unfamiliar problem, the expert, like the novice, will rely more on the hypothesis-oriented method of clinical reasoning (Barrows & Feltovich 1987, Patel & Groen 1991).
The advantage of pattern recognition is its efficiency and ability to reduce cognitive load. The disadvantage of pattern recognition is the risk of missing or misinterpreting important features or differential diagnoses. If clinical patterns become the focus of your attention where you examine patients only to determine which pattern their problem fits into, then the accuracy of your reasoning will depend on whether their presentation fits a clinical pattern you know. That is, when patterns become the focus of your attention it can be difficult to see outside the patterns you know resulting in over-emphasis on those features that most closely match a pattern you recognize. This will be discussed further later under common errors in clinical reasoning.
Complexity of clinical reasoning
The similarity of the clinical reasoning process to common logic where both involve information collection, perception/interpretation/analysis, hypothesis generation/modification makes it easy to understand. However, in reality clinical reasoning is complex, challenging to execute and subject to error. The complexity of clinical reasoning relates to a number of factors including: the complexity of many patients' problems, particularly when the physical (biomedical) is considered alongside the environmental and personal (psychosocial) factors; the subjective nature of much of the information that must be interpreted (e.g. patient reports, therapist observations and feel); the lack of absolute or research validated interpretations for much of the patient information obtained (i.e. patient reports and therapists' physical tests used); and the necessity for therapists to reason across different categories of clinical judgments at the same time, while obtaining information, qualifying responses and working through a systematic examination–treatment–re-assessment process that is tailored to the patient's unique presentation.
Christensen reviews the literature of complexity theory as it relates to health care and physiotherapy and relates this to the complexity inherent in many patient presentations (Christensen 2009, Christensen et al. 2008a). She utilizes a model of organizational management approaches to problem solving originally proposed by Stacey (1996) and adapted by Zimmerman et al. (2001, p. 141) to illustrate the continuum of patient presentations from the simple to the complex (see Fig. 2.3). Clinical decisions made in conditions of high certainty tend to be associated with more linear cause and effect relationships as opposed to decisions where cause and effect are less clear and consequently decisions less certain. Here, the greater the clinician's knowledge (research and experience-based) the greater their certainty. The agreement axis relates to the extent of consensus within a group, team or organization (e.g. physiotherapy and medical professions). Decisions made in conditions of high certainty and high agreement are characterized as falling into the simple zone where the problem and its management are clear and supported by evidence. In contrast, decisions made in conditions of little certainty and high levels of disagreement fall within the zone of anarchy often leading to either poor decisions or avoidance of decisions all together. The largest zone between simple and anarchy is the zone of complexity where much of physiotherapy practice and reasoning occurs. Again this can be related to the complexity of clinical presentations combined with the lack of sufficient evidence and/or agreement regarding diagnosis (pathology and impairment) and management. Most patient problems are multifactorial, often with more than one source of pain or impairment and typically with their own unique mix of environmental, psychosocial, cultural and physical contributing factors requiring a mixture of management interventions. As such, while clinical reasoning is relatively easy to understand, skilled reasoning is difficult to do.
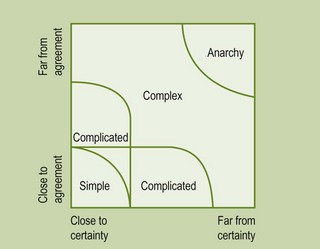
Figure 2.3 Adaptation of Stacey agreement and certainty matrix, with kind permission of Brenda Zimmerman (Zimmerman et al. 2001, p. 141).
Errors of clinical reasoning
Errors in clinical reasoning are frequently linked to errors in cognition (Kempainen et al. 2003, Rivett & Jones 2004, Scott 2000). Examples of these include overemphasis on findings which support an existing hypothesis, misinterpretation of non-contributory information as confirming an existing hypothesis, rejection of findings which do not support a favoured hypothesis, and incorrect interpretation related to limitations in knowledge and inappropriately applied inductive and deductive logic. Errors such as these are commonly associated with habits of thinking and over-focus on pattern recognition resulting in bias for a favourite hypothesis. The challenge here for students and therapists is to learn and use clinical pattern knowledge while not relying solely on it. Clinical pattern knowledge, particularly in musculoskeletal physiotherapy, is typically unproven due to lack of research and variability in clinical presentations for different problems and pathologies. Therefore therapists must obtain a comprehensive understanding of the patient's presentation that enables them to consider what ‘diagnostic’ pattern(s) (pathology and impairment based) are implicated so that any research supported management is considered while at the same time not limiting themselves to classification according to textbook patterns or treatment according to set protocols. While many musculoskeletal problems will fit into clear clinical patterns (e.g. muscle strains, ligament sprains) many problems also do not fit, either because there is more than one symptomatic pathology/impairment or simply because there are considerable variations in physical, environmental and personal (i.e. psychosocial) factors that contribute to patients' clinical presentations. Thorough examination and a systematic process of treatment and re-assessment will often enable therapists to gradually determine the key factors responsible for the patient's pain and disability eventually allowing identification of the most likely clinical pattern. However, even when a specific clinical syndrome cannot be established, as long as appropriate medical screening has been conducted for potential systemic or visceral problems, treatment of presenting symptoms and impairments with emphasis on restoring function will usually be effective.
Associated with over-focusing on clinical patterns is reaching a premature conclusion regarding the patient's presentation. Initial impressions will sometimes bias interpretations of other information. This error typically occurs when the therapist is biased by a dominant cue and does not adequately consider or rule out (through further questioning and physical assessment) alternative explanations/hypotheses. A good example here is of the patient who arrives with a medical diagnosis. While that is clearly important to consider, it does not obviate the need for thorough examination as the diagnosis may be wrong or there may be other problems not detected by the referring doctor. Even with a correct diagnosis (structures involved ± pathology) the therapist must still establish how that diagnosis manifests with respect to specific symptoms and impairments and the stage of the disorder (e.g. acute/inflammatory versus subacute/mechanical versus chronic). By thinking of these early impressions as ‘working hypotheses’, and ensuring competing diagnostic and narrative hypotheses are entertained, premature conclusions can be avoided.
While efficiency is important, many errors stem from a general lack of thoroughness in information obtained and hypotheses generated and tested. The use of ‘screening questions’ (related to other types of symptoms, other aggravating/easing factors, and medical screening for safety) will minimize the risk of missing relevant information. Thoroughness of the physical examination for musculoskeletal problems requires good knowledge of the potential sources (i.e. tissue or structure) of the patient's symptoms and knowledge of structures or mechanisms (e.g. motor control, biomechanics, ergonomics) that may be contributing directly or indirectly to increased load (i.e. strain) on the symptomatic area.
Errors in reasoning can also be precipitated by lack of skilled questioning, as discussed earlier. Here the most common example is making assumptions without explicitly clarifying the patient's meaning (e.g. patient's ‘shoulder pain’ actually occurring in the supraspinous fossa; back pain aggravated by walking down hills rather than just any walking; patient's fear of aggravating their pain being an adaptive concern causing avoidance of overdoing activities and not a more maladaptive total avoidance). This last example touches on an error within the narrative reasoning focus. Other common narrative reasoning related errors include the following:
• Therapist views biomedical and psychosocial as separate, assuming that their role as a physiotherapist is to manage only the biomedical, with the psychosocial exclusively the responsibility of psychologists and counsellors
• Therapist does not attempt to understand biomedical diagnosis in the context of patient's personal circumstances
• Therapist does not screen psychosocial factors or their psychosocial assessment is too superficial, leading to judgments based on insufficient assessment. Common examples here include:
 patient does not volunteer personal problems so therapist assumes none exist
patient does not volunteer personal problems so therapist assumes none exist
 therapist relies on psychosocial screening questionnaires without giving the patient an opportunity to qualify their responses, including the basis of those responses
therapist relies on psychosocial screening questionnaires without giving the patient an opportunity to qualify their responses, including the basis of those responses
 therapist does not explore effects of problem on patient's self, understanding/beliefs, symptoms, expectations and future prospects
therapist does not explore effects of problem on patient's self, understanding/beliefs, symptoms, expectations and future prospects
 patient alludes to stress at work/home but therapist does not clarify or establish history and relationship of stress to clinical presentation
patient alludes to stress at work/home but therapist does not clarify or establish history and relationship of stress to clinical presentation
 therapist does not clarify if patient is coping with their problem or what coping strategies they use or have tried
therapist does not clarify if patient is coping with their problem or what coping strategies they use or have tried
 therapist approaches narrative reasoning judgements in same way as diagnostic reasoning judgements, assuming patient perspectives can be understood/measured as maladaptive by a standard normative interpretation (such as range of movement).
therapist approaches narrative reasoning judgements in same way as diagnostic reasoning judgements, assuming patient perspectives can be understood/measured as maladaptive by a standard normative interpretation (such as range of movement).
Reasoning errors related to management are often the result of reasoning errors made through the examination (e.g. lack of thoroughness, not considering competing hypotheses, poor questioning and manual skills resulting in inaccurate information, etc.). Also common is inadequate re-assessment of appropriate management outcomes (e.g. pain, physical impairments, function, quality of life, disability measures) to determine the value of any intervention but also to establish the significance and relationship between different impairments. For example, systematic re-assessment of several impairments (active and passive movement, soft tissue, neurodynamics, motor control) following spinal mobilization for pain and stiffness may reveal improvement in neurodynamics and motor control supporting their relationship to the spinal stiffness. While most therapists recognize the importance of re-assessment of function and physical impairments, re-assessment of patient understanding following explanation/education is less appreciated and practiced.
Lastly a lack of self-awareness (i.e. metacognition) is a reasoning error that limits the therapist's ability to recognize other errors and limits their learning from reflections on their experiences.
Improving clinical reasoning: learning through clinical reasoning
Physiotherapists must be competent in the examination, reasoning and management of a wide range of patient problems, many of which are complex and multifactorial. In addition they must be capable of effectively managing unfamiliar, ambiguous presentations outside their current knowledge and skill base. So how can therapists and students improve their critical thinking and reasoning to minimize errors of reasoning and assist their management of the diverse variety of familiar to difficult and unfamiliar presentations they encounter? Christensen et al. (2008a, p. 102) review the ‘capability’ literature and offer the following definition of capability as it relates to clinical reasoning:
Capability in clinical reasoning involves integration and effective application of thinking and learning skills to make sense of, learn collaboratively from and generate knowledge within familiar and unfamiliar clinical experiences.
Acquisition of clinical reasoning capability should be facilitated throughout the physiotherapy professional entry education. This does not always occur with some schools having no overt academic content covering clinical reasoning theory and/or no explicit framework or strategies for ensuring clinical educators facilitate application of clinical reasoning to practice consistent with contemporary theory (Christensen 2009, Christensen et al. 2008b). Students in those programs tend to develop their clinical reasoning capability through self-directed learning with the individual views/knowledge of their clinical educators often having a significant influence (positive and negative).
Christensen (2009) provides a comprehensive report of students' development of clinical reasoning capability across four physiotherapy programs in the USA. It is beyond the scope of this chapter to cover this topic in detail. Instead, key findings and implications of her research are briefly mentioned here and interested readers can refer to the references (Christensen 2009, Christensen et al. 2008a, 2008b) for further details. Christensen discusses four dimensions of clinical reasoning capability in the context of her research including reflective thinking, critical thinking, dialectical thinking and complexity thinking, each of which have been briefly addressed in this chapter. She discusses the role of professional socialization in shaping students' approach to clinical reasoning and proposes educators incorporate learning activities that assist students to see their own clinical reasoning as a reflection of their professional identity as a physiotherapist where the profession's espoused philosophy of practice, professional values, ethics and behavioural expectations are apparent in their practice and their reasoning. She discusses the need to strengthen connections between academic classroom learning of clinical reasoning and clinical application/learning of clinical reasoning. She proposes that this can be enhanced through classroom clinical reasoning focused learning activities that utilize existing models and frameworks within the literature to give form to clinical reasoning concepts and their clinical application (an educational process called reification, Wenger 1998) in order to assist students' understanding of clinical reasoning. Examples of frameworks that can be used in classroom theoretical discussions and case studies include models of clinical reasoning (e.g. Fig. 2.2), models of health and disability (e.g. Fig. 2.1) and the clinical reasoning strategies and hypothesis categories presented in this chapter. Lastly she emphasizes the importance of students having supervised clinical experiences that include overt attention to their developing clinical reasoning from clinical educators who are themselves familiar with clinical reasoning theory, skilled in their own clinical reasoning and skilled in facilitating students' clinical reasoning.
Maitland advocated open-mindedness (e.g. not being limited by current knowledge), analytical thinking (e.g. making features fit by attending to all aspects of the patient's story including features that do not immediately make sense) and use of advanced inquiry skills (i.e. questioning and physical assessments) to maximize the quality of information obtained. Inherent in Maitland's approach and unanimously promoted throughout the critical thinking, clinical reasoning, and education literature in general is continual reflection to note, critique, discuss and revise our research and experience based knowledge and actions (e.g. Brookfield 1987, Clouder 2000, Cranton 1994, Forneris 2004, Higgs& Jones 2008, Mezirow 2000, Rodgers 2002, Schön 1983, 1987). Reflection in clinical reasoning is the basis for experiential learning from practice (Christensen et al. 2008b; Eraut 1994; Schön 1987). In addition to the obvious reflection on a patient's problem, students and therapists should also reflect on their own thinking and the factors that limit it (e.g. knowledge).
Brookfield (2008) discusses critical appraisal as a process of recognizing and researching the assumptions that underpin clinical practice. EBP necessitates critical appraisal of available evidence with formal appraisal tools available according to the type of research. Critical appraisal applied to clinical reasoning requires reflection on existing knowledge, the basis of that knowledge and the assumptions underpinning or associated with that knowledge. This sort of critical reflection should improve clinical reasoning itself while also fostering learning through clinical reasoning.
Assumptions are taken-for-granted beliefs acquired through life and through formal education that are often tacit and hence typically not considered or challenged. Uncritically accepted assumptions often emerge from professional philosophies or approaches to practice or from personal experiences that have shaped one's views. Without scrutiny such assumptions place us at risk of thinking (in everyday life) and reasoning (in practice) on the basis of inaccurate and biased ‘knowledge’ (i.e. views/opinions) making us vulnerable to misinterpretations, inaccurate judgments and ultimately less effective health care.
Brookfield (2008) categorizes assumptions as paradigmatic, prescriptive and causal. Paradigmatic assumptions are the broad structuring assumptions we use to order the world into fundamental categories. They are typically the most difficult assumptions to recognize and change as they are supported by our personal experiences. A classic example of a paradigmatic assumption in medicine and physiotherapy is the traditional biomedical paradigm that equates pathology with symptom presentation and disability. The more contemporary bio-psychosocial model requires a broader consideration of environmental and personal or psychosocial factors alongside pathology in the assessment, analysis and management of patients' health problems.
Prescriptive assumptions relate to what we think should happen in a particular situation. Clinically related examples, including assumptions about clinical syndromes (e.g. chronic pain, shoulder impingement) or assumptions about patients themselves (e.g. different ethnic groups, workers compensation cases) can lead to inaccurate generalizations regarding their presentation, their attitude/motivation and the appropriate management. It is these sorts of prescriptive assumptions that commonly underpin failure to recognize the uniqueness of patients' individual clinical presentations and uncritical application of research findings and protocols of treatment. Prescriptive assumptions are inevitably related to our paradigmatic assumptions. For example, if you are biomedically (as opposed to bio-psychosocially) biased you are more likely to treat patients with a particular pathology or clinical syndrome the same rather than modifying your treatment to the patient's individual presentation.
Causal assumptions are assumptions about how different parts of the world (or human body) work (or do not work as with health) and what is required to create change (e.g. promote improved health). Physiotherapy and medicine in general are replete with causal assumptions typically based on unproven clinical management extrapolations from basic research or bias from personal experience not supported by adequate follow-up or critical comparison to other approaches.
What follows are some specific suggestions for facilitating students' and practising therapists' clinical reasoning drawn from research and personal experiences of educators across the health professions (Christensen et al. 2002, Higgs & Jones 2008, Rivett & Jones 2004, Scott 2000, Watts 1995). It is important that learning activities are well planned to target specific aspects of clinical reasoning (e.g. hypothesis generation, hypothesis testing, diagnostic versus narrative reasoning, etc.) while linking core biomedical and psychosocial theory to examination and management principles applied to simulated and real patient presentations. Students should have opportunity to reflect on their existing knowledge/understandings and to question new information covered (concepts, principles, clinical patterns, management strategies) in order to promote construction of new knowledge/understandings that are acquired through critical consideration (as opposed to rote memory) in the context of clinical scenarios. There is a wealth of educational and clinical reasoning specific literature available to guide educators' development of learning activities. While it is beyond the scope of this chapter to review that literature, publications by Shepard and Jensen (2002), Higgs (1990, 1992, 1993, 2008), Higgs and Edwards (1999), Higgs and Hunt (1999), Higgs et al. (2008) and Rivett and Jones (2008) are helpful resources.
Understanding clinical reasoning theory
Just as students are expected to learn basic and applied science theory from presentations and review of literature, they should also be presented with contemporary theory and research of clinical reasoning. Ideally they should read selected clinical reasoning literature with activities or assignments that require them to demonstrate their understanding and application of that theory to practice. Reading literature from medicine, physiotherapy and the other allied health professions (e.g. Higgs et al. 2008) provides students with a comprehensive overview that will assist construction of their own understanding while at the same time giving them insight to the reasoning of their colleagues in other health professions.
Facilitated clinical reasoning through case studies and real patients
Real or hypothetical clinical problems can be used in clinical reasoning learning activities presented as paper-based, computer-based, filmed or through the use of simulated patients (trained actors). The text Clinical reasoning for manual therapists (Jones & Rivett 2004) provides theory chapters on clinical reasoning, learning theory and improving clinical reasoning as well as 23 case study contributions from recognized musculoskeletal clinical experts around the world. Through their cases the experts are questioned about their evolving reasoning, with the case providing valuable resources for educators and practicing therapists to use in clinical reasoning learning activities. A recent monograph entitled Clinical reasoning and evidence-based practice, available as an independent study course through the American Physical Therapy Association (Christensen et al. 2011) also provides a good overview of clinical reasoning theory linked to three patient cases. Newer books also now commonly include case studies and associated clinical reasoning (e.g. see Lee 2011, Vicenzino et al. 2011). When using case studies drawn from published resources or your own clinical experiences it is important that the cases are selected with an appropriate level of complexity for the student group with strategically planned discussions around aspects of clinical reasoning, basic science and physiotherapy examination, clinical pattern and management theory all linked to EBP (including experience and research-based evidence). Clinical reasoning activities with real patients are essential for students to develop their clinical reasoning capability within the variability of clinical presentations (problems and people), variability of practice environments and variability of time constraints inherent in real life practice. It is often useful to bridge the learning between case studies/simulated patients and students' reasoning through real patients they examine and treat with opportunities for students to observe patient demonstrations (and discuss associated reasoning) by their educators.
Whether using case studies, simulated or real patients it is essential that educators access students' thoughts in order to understand the reasoning and knowledge on which they base their reasoning. Students' reflections on their reasoning can be encouraged before, during and after the patient case/encounter. While stopping part way through an examination or treatment of a real patient is time consuming, it is also invaluable in exploring the student's immediate perceptions, interpretations and synthesis of patient information. The educator clearly must provide feedback and share their own interpretations but at the same time allow students the opportunity to explore (within reason and without risk to patient safety) their own reasoning even if it proves to be less efficient/effective than that of the educator. A balance is required to shape the student's knowledge, skills and reasoning without necessarily forcing them to only think and do the same as you. Peer coaching involving demonstration, observation, collaborative practice, feedback and reasoning discussions between students has also been demonstrated to be effective in facilitating student reasoning (Ladyshewsky & Jones 2008).
Self-reflection worksheets and clinical pattern diaries
Often educator / student ratios and time constraints prohibit one-on-one discussion with all students on every case. Here, use of self-reflection worksheets completed by students following their patient encounter is effective in accessing students' reasoning and promoting their self-awareness. Two examples of clinical reasoning self-reflection forms (long and short versions) are provided in Appendix 2.1. These have evolved to their present form from Maitland's original ‘planning sheet’ and readers are invited to use or modify them according to your own teaching and learning needs. Students commonly find the forced reflection these forms require is itself illuminating in highlighting information they failed to obtain or areas of knowledge and reasoning where they need further work. This, combined with feedback from the clinical educator, makes them a useful teaching, self-reflection and assessment tool.
Requiring students to compile a diary of clinical patterns facilitates their knowledge organization around common clinical patterns for use in their clinical reasoning. While there are a variety of ways clinical patterns can be presented, two examples of templates for constructing a clinical pattern used in the Master of Musculoskeletal and Sports Physiotherapy program, University of South Australia (single pattern versus comparative pattern) are available in Appendix 2.2. The content for constructing the patterns will come from the literature, ideally with acknowledgment of the level of supporting evidence used. Importantly for these patterns to become meaningful, educators should encourage students to include summaries of real patients they have seen who fit a particular pattern as this instantiation promotes deeper learning and highlights that clinical presentations typically do not match textbook patterns perfectly, enabling students to learn common variations and recognition of overlap between different patterns.
Mind maps
Mind maps (Buzan 2009) (also called concept and cognitive maps, although some differences exist) are another teaching and assessment strategy useful for facilitating metacognition, knowledge organization and clinical reasoning. A mind map is a pictorial representation of a person's knowledge and organization of knowledge on a specified topic. As such, it externalizes for the learner and the assessor the breadth and depth of the learner's understanding with potential to reveal preconceptions, assumptions, misunderstandings and biases. Cahill and Fonteyn (2008) review the literature on mind mapping and attribute its theoretical basis to the learning theory espoused by Ausubel (1963) who is credited with identifying the importance of relationships between concepts to a person's understanding and thinking. Meaningful (i.e. deep as opposed to superficial or rote) learning occurs when new learning is related to existing concepts or knowledge structures resulting in some change in understanding. This may be revision of a previous concept and/or new insight to relationships with other concepts previously not appreciated. Buzan and Buzan (1996) draw parallels between the mind map and the associative nature of brain pathways and argue for the importance of learning associations to improving understanding and memory. A growing body of education research is now available supporting the efficacy of mind mapping for promoting meaningful learning (see Cahill & Fonteyn 2008).
There are different processes for creating mind maps described in the literature. In natural science education students are often given a group of related concepts accompanied by a lecture after which the students are asked to create a mind map depicting their understanding of the concepts and any relationships between concepts. Arrows are generally used to illustrate relationships and words may be written along the arrows to qualify the nature of the particular relationship (e.g. ‘leads to’, ‘causes’, etc.). Cahill and Fonteyn (2008) describe how they had student nurses complete mind maps representing their ‘thinking about a patient case’ including patient problems, assessments, interpretations and management. At the University of South Australia, Master of Musculoskeletal and Sports Physiotherapy programme we have used mind maps as both a teaching and assessment tool. We start by having the students brainstorm on a sheet of paper everything they know about a specified topic prior to reading or receiving a lecture on the topic (e.g. inflammation, subacromial impingement). The students are then asked to number the items they brainstormed by grouping related items (i.e. giving every item that they feel should be categorized together the same number, for example for a common clinical presentation such as ‘groin pain’ all symptoms might be given a ‘1’, signs a ‘2’, possible pathologies a ‘3’ and so on). After completing the categorization of items the students then transfer those category headings and items within categories to another paper. Lastly students are asked to illustrate the relationships between categories (or concepts) by their placement on the paper (e.g. predisposing factors may be above pathology and signs and symptoms) and by arrows between categories with words along the arrows to qualify the relationship. The process of constructing a mind map itself is often illuminating to the student highlighting gaps in their knowledge. When time allows for students to complete maps prior to another learning activity (reading, lecture, demonstration) the pre-mind map promotes self-awareness (i.e. metacognition) of what they know and do not know about the nominated topic. This alone is valuable as students are then more likely to engage in the learning activity with greater interest and interaction as they listen for and ask about the gaps in their knowledge. Ideally a post-mind map is completed after the learning activity which enables the student to review new information and revise previous understandings. The second map will almost always have greater breadth and depth of information and relationships represented reflecting the learning and knowledge reorganization that has occurred. We have used this formatively to facilitate deeper learning and we have used it as a summative assessment for a whole course on ‘Ethics and communication’ where students are required to complete pre-course and post-course mind maps illustrating their understanding of the constructs and relationships between clinical reasoning and ethical reasoning (Jones et al. 2013). In this case students also wrote a brief essay explaining their second map which provided further insight to their understanding and learning through the course.
Lateral/creative thinking
Logical (also called vertical) thinking is essential to inductively recognize clinical patterns and to deductively substantiate those patterns through hypothesis oriented questioning and physical assessment (i.e. differential diagnosis). While this hypothetico-deductive process is clearly important to diagnostic reasoning and to advances in knowledge through quantitative research, lateral thinking is also important to the generation of new insights and discoveries that enable the individual therapist and the profession to advance their knowledge and practice. In fact, Kuhn (1970), in his text The structure of scientific revolutions, points out that many of the major breakthroughs in science did not occur due to carefully controlled scientific research, rather they often emerged from accidents or the lone insight of an individual. As long as a student's or therapist's clinical reasoning is logical and safe, lateral thinking should be encouraged. If we only encourage logical thinking and practice within the realm of what is ‘known’ or substantiated by research evidence we limit the variability and creativity of thinking that is important to the generation of new ideas.
Logical and its associated scientific thinking typically discourage individual intuition (i.e. gut feelings). However, in reality both the frontal cortex (cognition) and limbic system (emotions) are involved in most decisions to varying degrees. Research investigating the effects of over analyzing (too much logic) versus insufficient analysis (relying too much on emotions/gut feelings) suggests both can lead to poor decisions (Lehrer 2009). That decision-making research was primarily conducted in the realm of day to day decisions (e.g. which wine or food product you prefer, which house to buy, on field sports decisions, etc.) rather than clinical decision making. However, given the reality that health and disability are not an absolute science where judgments are black and white, correct or incorrect, intuition and emotions will also be involved in clinical reasoning. It is easy to imagine the errors of clinical reasoning that might occur with relying completely on gut feelings but could being too analytical and resistant to intuition also lead to clinical judgment errors? This has not been investigated but at the very least personal intuition should be reflected on and even pursued (i.e. line of questioning, physical assessment, treatment intervention) as it may lead to a fruitful outcome (e.g. useful information, positive response to intervention) that would not have been discovered if obvious logical avenues are the only things pursued. That is, new ideas and new approaches can emerge from intuition as well as logic.
Teaching lateral thinking centres on helping students recognize their current thinking processes (e.g. interpretations of patient information, diagnostic and management decisions) and encouraging them to think more widely, outside what may seem obvious and logical to them (de Bono 1970, 1994). Lateral thinking is relative to each individual's perspectives. That is, what is logical to one person is not necessarily logical to another. De Bono characterizes vertical thinking as logical, sequential, predictable thinking where the thinker aims to systematically make sense of all information. In contrast lateral thinking involves restructuring and escape from old patterns, looking at things in different ways and avoidance of premature conclusions. The logical thinker attends only to what is obviously relevant where the lateral thinker recognizes that sometimes seemingly irrelevant information assists in viewing the problem from a different perspective. As a practical example of encouraging lateral thinking a student could be encouraged to conduct a review of patient progress and their reasoning (i.e. Maitland's ‘retrospective assessment’) where the student is explicitly asked to identify their dominant interpretation of the patient's diagnosis (e.g. pathology vs impairment, physical vs psychosocial, etc.) and the dominant approach they have been taking in their management to date (e.g. passive or dynamic bias, bias to treating source versus contributing factors, bias to physical impairments vs psychosocial factors, etc.). It is difficult to think laterally/creatively if you cannot first recognize how you have been thinking or approaching the problem thus far. Once recognized, the student can then be encouraged to think more laterally about alternative interpretations of the patient's presentation and alternative management approaches. Maitland's way of emphasizing this process was to physically turn around in a circle, take a deep breath and start again. If students and therapists always follow the same interpretations and always manage problems the same way they never learn the place for alternative interpretations or that other approaches may be equally or even more effective.
We are all imposters
Every student and therapist will have experienced the uncomfortable situation of having to treat a patient who is not responding to treatment and whose presentation is not fully understood. Confirmation of pathology is often not possible from medical investigations or clinical assessment. Symptoms and physical impairments also commonly exist without overt pathology and many physical impairments exist without symptoms making it challenging to be clear which factors in the patient's life and clinical presentation are genuinely contributing to their symptoms and disability. Fortunately treatment of impairments is often effective in more straightforward nociceptive dominant presentations even when pathology is unclear. But as discussed earlier, many patient presentations are complex and multifactorial. Physical impairments are present alongside psychosocial issues and it is not always clear how much each is driving or contributing to the patient's disability. Systematic treatment addressing the different components hypothesized as being potentially relevant is not always effective causing some to conclude the problem is centrally mediated and the patient lacks understanding, acceptance, motivation and/or self-efficacy to actively participate in the rehabilitation recommended and to make the necessary lifestyle changes. While these factors may well underpin a patient's failed management they are difficult to assess/measure (Stewart et al. 2011) and challenging to manage. When a patient is not responding to treatment the therapist will inevitably go through a period of inner torment as they question whether they lack adequate knowledge of the latest research or missed something in the presentation. Many therapists in this situation are hesitant to acknowledge their lack of understanding to the patient. They may similarly hesitate to request assistance from a colleague in fear that their examination and management will be judged incompetent. In short, they feel like an imposter who does not know enough, isn't skilled enough and are afraid they will be found out (Brookfield 2008). I chose to finish on this note as I see it as an unspoken reality that restricts some students' and therapists' learning and makes their practice less enjoyable. So what is the solution to minimize the struggle against ‘impostership’? Brookfield (2008) discusses this phenomenon and suggests the answer is to go public. That is, to acknowledge to both patient and colleagues when you are not clear and would like a second opinion. Earlier I indicated that expert clinicians not only know a lot, they also know what they don't know. The student has the impression that the expert solves all patient problems and never needs assistance. All experienced clinicians will know how false that assumption is. The expert has become an expert precisely because they recognize their limitations and they act on them, often consulting other colleagues. When teachers and senior therapists acknowledge their difficult cases, their ‘failures’, it can be enormously reassuring to those less experienced making them more comfortable to ask for help. A second opinion may uncover missed information important to management or errors in reasoning but may also support the management trialled in which case other referral pathways should be considered. Creating an environment in the classroom or clinic where students/therapists feel comfortable discussing theory, research and clinical principles they don't understand is important. This can be facilitated through clinical discussion groups where patient cases are presented. Here it is important to not focus only on everyone's success, rather cases should be included that were not understood or where, in hindsight, errors were recognized. Health, disability and physiotherapy assessment and management are not exact sciences. Skilled clinical reasoning is important to work through the myriad of factors in a patient's presentation and critical reflection (metacognition) is important to recognizing limitations in knowledge, communication, procedural skills, and reasoning. When reflection leads to action (e.g. change in practice, request for assistance) the result is life-long learning.
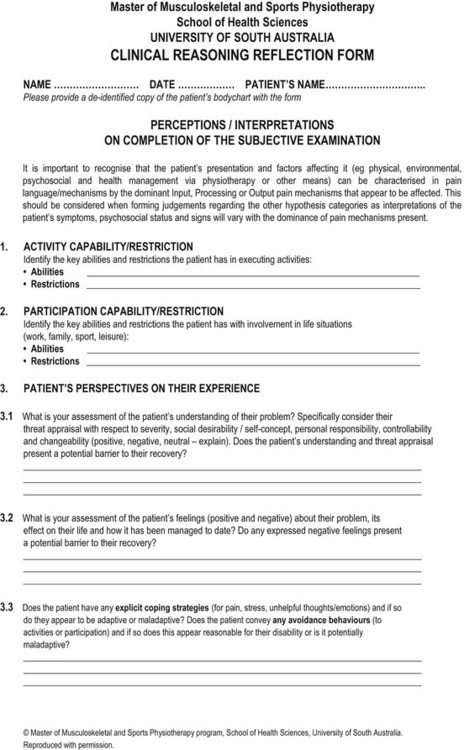
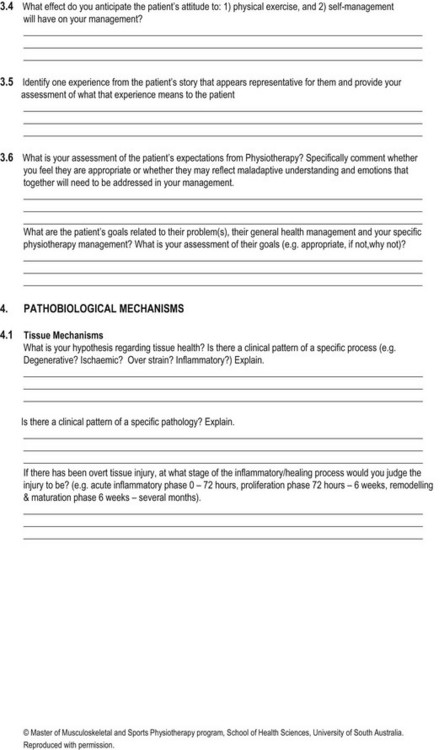
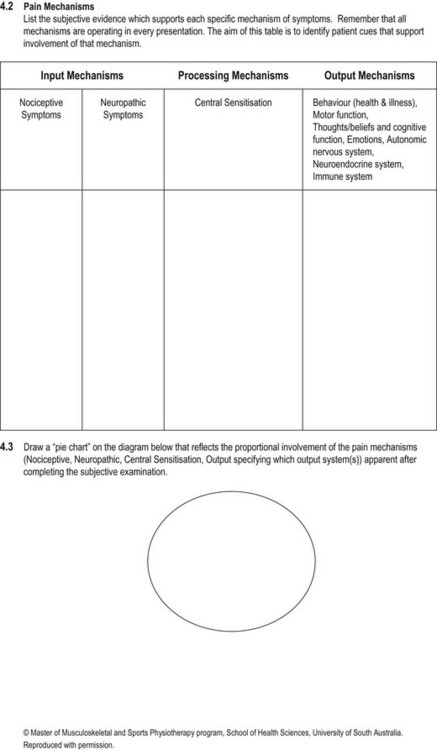
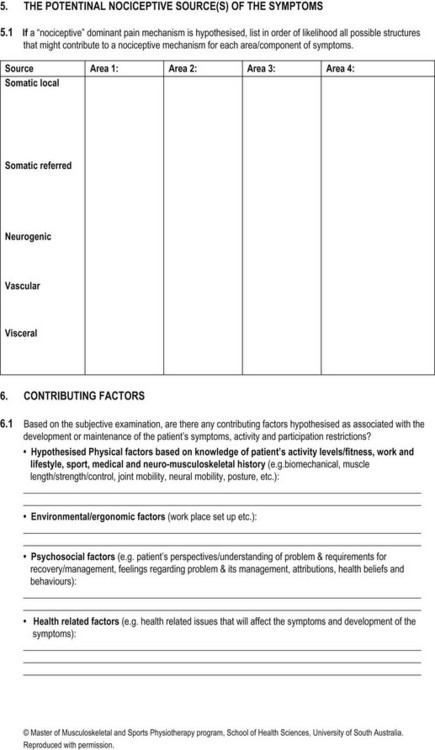
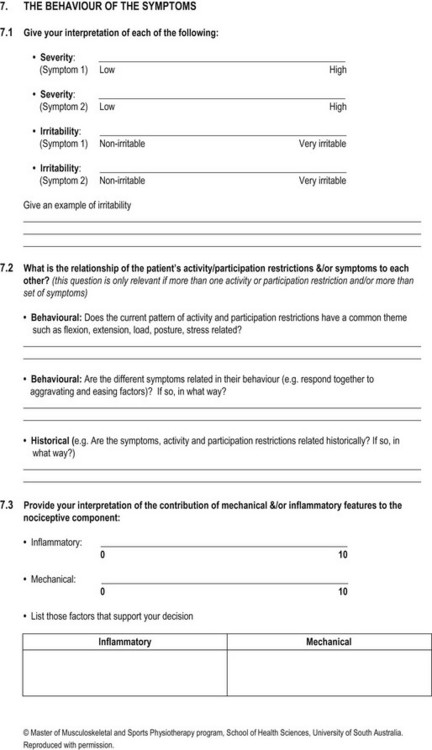
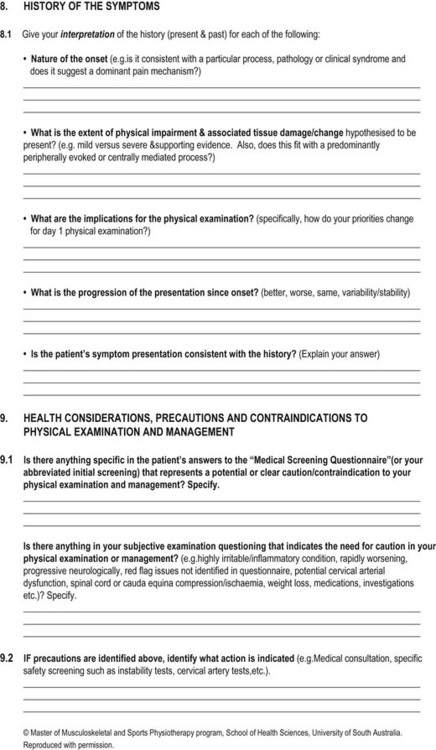
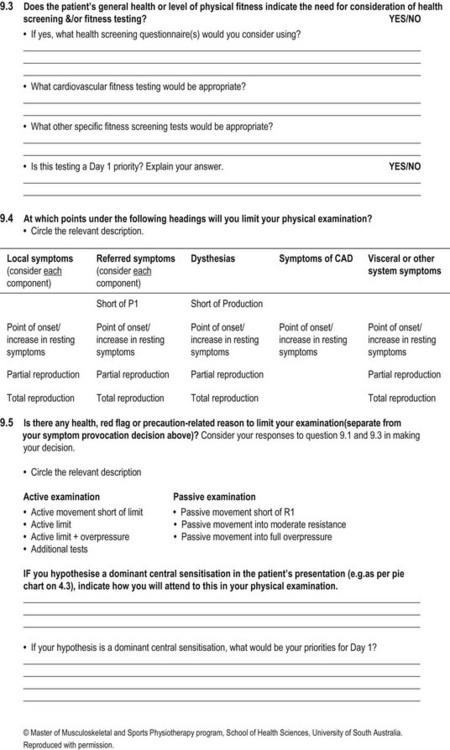
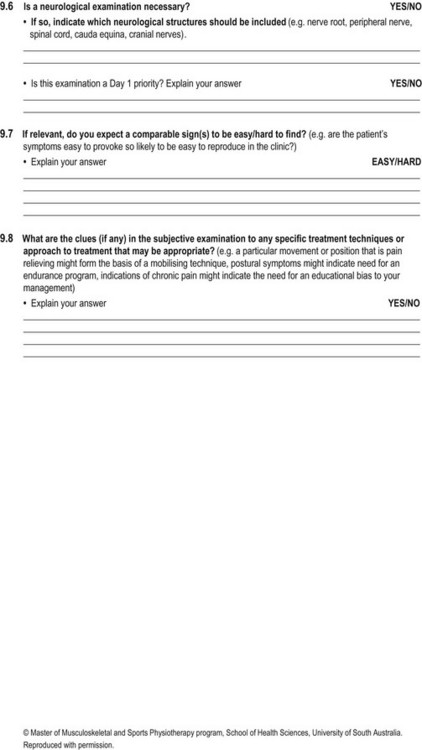
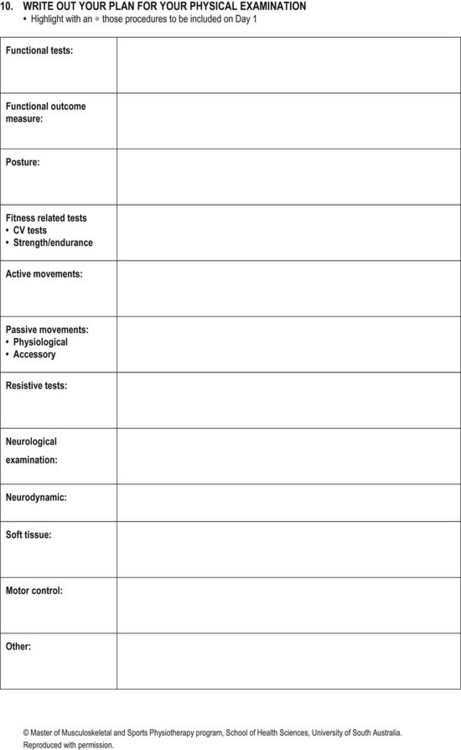
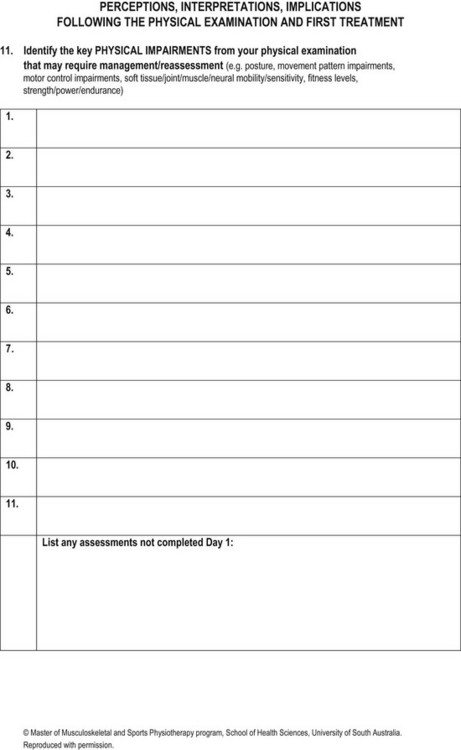
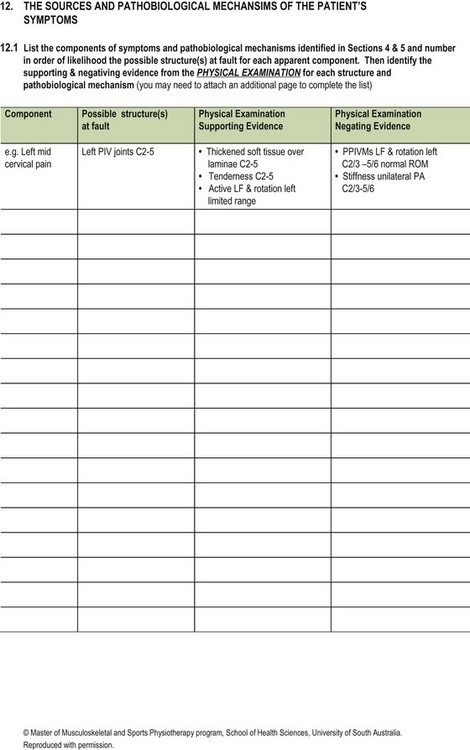
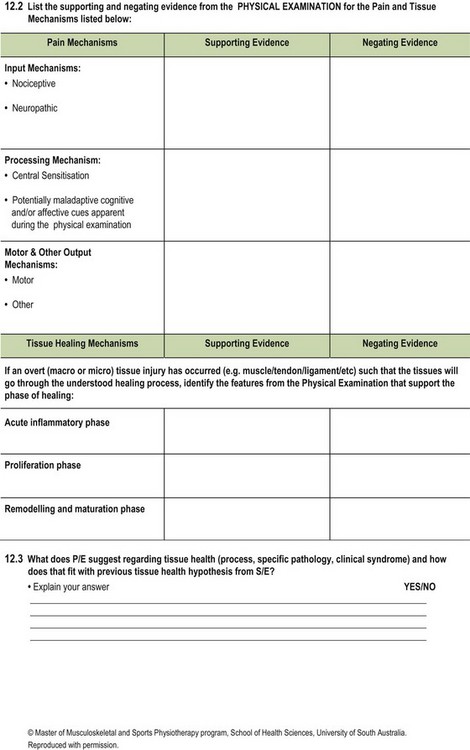
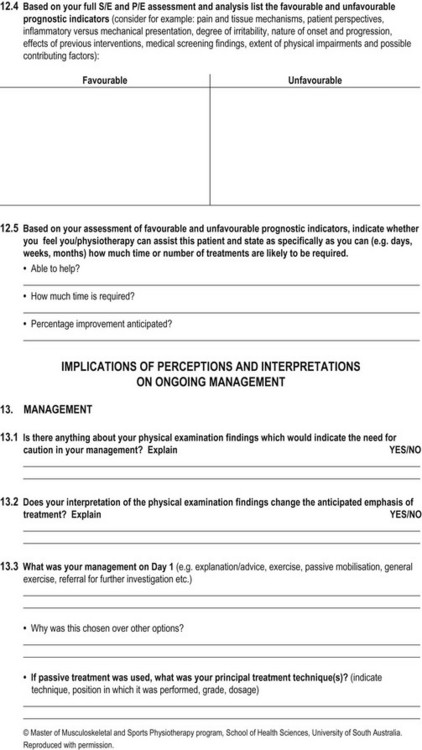
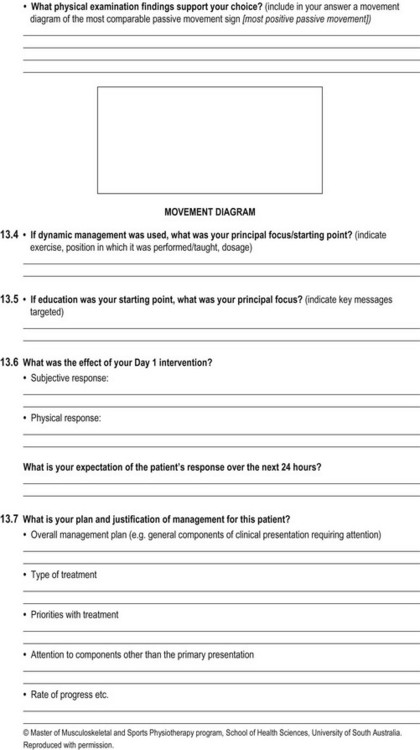
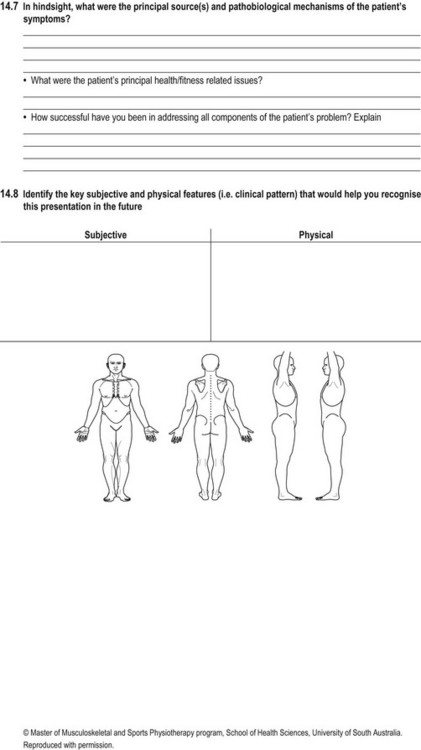
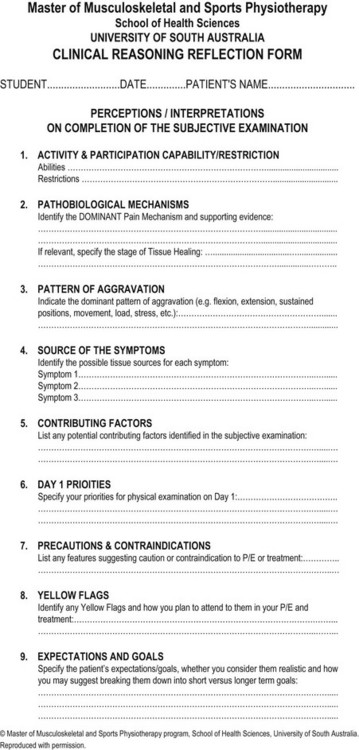
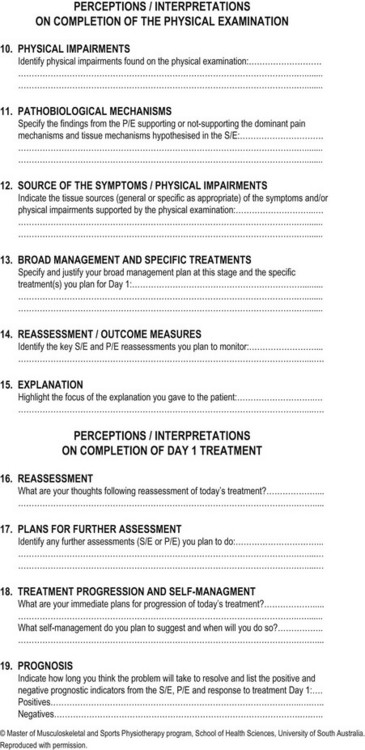
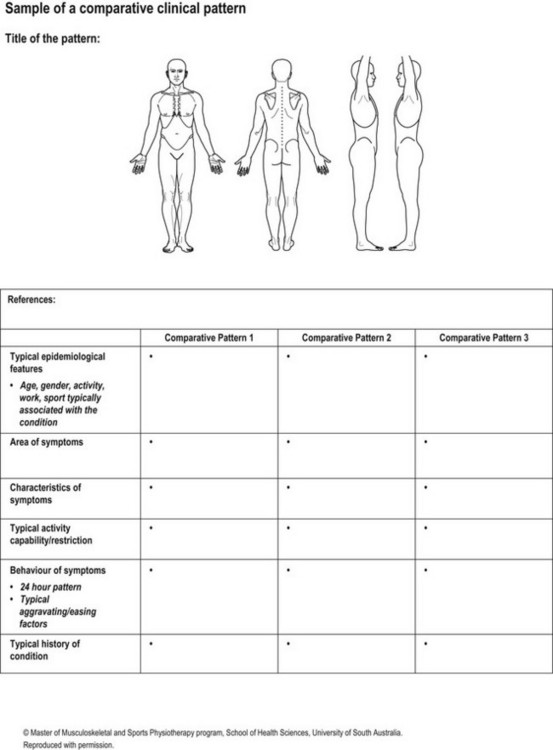
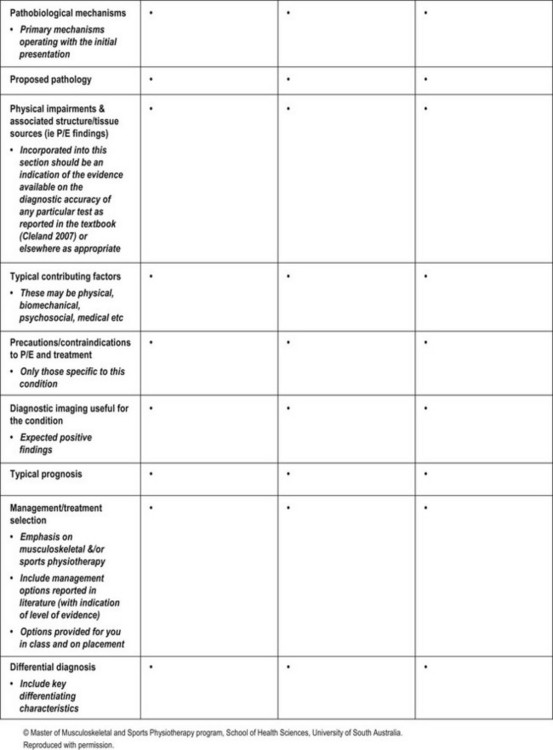
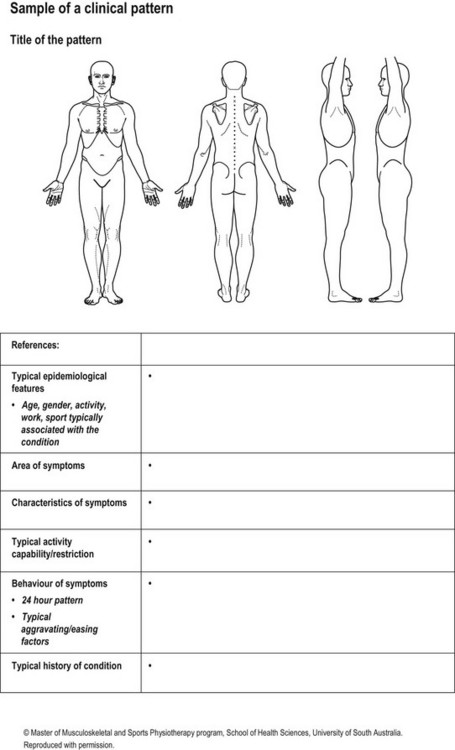
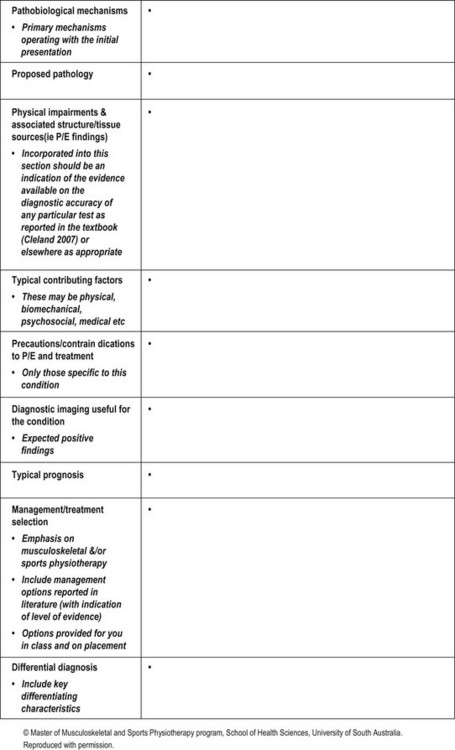
References
Adams, MA, Stefanakis, M, Dolan, P. Healing of a painful intervertebral disc should not be confused with reversing disc degeneration: implications for physical therapies of discogenic back pain. Clin Biomechan. 2010;25:961–971.
American Physical Therapy Association. Guide to physical therapist practice, Revised ed 2. Alexandria: American Physical Therapy Association; 2003.
Anderson, JR. Cognitive psychology and its implications, ed 3. New York: Freeman; 1990.
Argyris, C, Schön, D. Organizational learning: a theory in action perspective. Reading: Addison-Wesley; 1978.
Arnetz, JE, Almin, I, Bergström, K, et al. Active patient involvement in the establishment of physical therapy goals: Effects on treatment outcome and quality of care. Adv Physiother. 2004;6:50–69.
Arocha, JF, Patel, VL, Patel, YC. Hypothesis generation and the coordination of theory and evidence in novice diagnostic reasoning. Med Decis Making. 1993;13:198–211.
Arroll, B, Goodyear-Smith, F, Crengle, S, et al. Validation of PHQ-2 and PHQ-9 to Screen for Major Depression in the Primary Care Population. Ann Fam Med. 2010;8:348–353.
Ausubel, DP. The psychology of meaningful verbal learning. New York: Grune and Stratton; 1963.
Barnitt, R, Partridge, C. Ethical reasoning in physical therapy and occupational therapy. Physiother Res Int. 1997;2:178–192.
Baron, JB, Sternberg, RJ. Teaching thinking skills: Theory and practice. New York: WH Freeman and Company; 1987.
Barrows, H, Feltovich, P. The clinical reasoning process. Med Educ. 1987;21:86–91.
Beeston, S, Simons, H. ‘Physiotherapy practice: Practitioners’ perspectives. Physiother Theory Pract. 1996;12:231–242.
Benner, P. From novice to expert: Excellence and power in clinical nursing practice. Menlo Park: Addison-Wesley; 1984.
Benner, P, Tanner, C, Chesla, C. From beginner to expert: Gaining a differentiated clinical world in critical care nursing. Adv Nurs Sci. 1992;14(3):13–28.
Bielefeldt, K, Gebhart, GF. Visceral pain: basic mechanisms. In: McMahon SB, Koltzenburg M, eds. Wall and Melzack's textbook of pain. ed 5. Edinburgh: Elsevier; 2006:721–736.
Bishop, GD. Understanding the understanding of illness: lay disease representations. In: Skelton JA, Croyle RT, eds. Mental Representation in Health and Illness. New York: Springer-Verlag; 1991:32–59.
Bogduk, N. The anatomy and physiology of nociception. In: Crosbie J, McConnell J, eds. Physiotherapy foundations for practice – key issues in musculoskeletal physiotherapy. Oxford: Butterworth-Heinemann; 1993:48–87.
Borrell-Carrió, F, Suchman, AL, Epstein, RM. The bio-psychosocial model 25 years later: Principles, practice, and scientific inquiry. Ann Fam Med. 2004;2(6):576–582.
Boshuizen, HPA, Schmidt, HG. The development of clinical reasoning expertise. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical reasoning in the health professions. ed 3. Amsterdam: Butterworth Heinemann Elsevier; 2008:113–121.
Boissonnault, WG. Primary care for the physical therapist. Examination and triage, ed 2. St Louis: Elsevier; 2011.
Brooker, C. Mosby's 2013 Dictionary of Medicine, nursing and health professions, ed 9. Edinburgh: Elsevier; 2013.
Brookfield, SD. Developing critical thinkers. Challenging adults to expore alternative ways of thinking and acting. San Francisco: Jossey-Bass; 1987.
Brookfield, S. Clinical reasoning and generic thinking skills. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical reasoning in the health professions. ed 3. Amsterdam: Butterworth Heinemann Elsevier; 2008:65–75.
Brooks, L, Norman, GR, Allen, S. Role of specific similarity in a medical diagnostic task. J Exp Psychol Learn Mem Cogn. 1991;120:278–287.
Butler, DS. The sensitive nervous system. Adelaide: Noigroup Publications; 2000.
Buzan, T. The mind map book. Harlow: Pearson Education Limited; 2009.
Buzan, T, Buzan, B. The mind map book. New York: Plume/Penguin; 1996.
Cahill, M, Fonteyn, M. Using mind mapping to improve students’ metacognition. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical Reasoning in the Health Professions. ed 3. Amsterdam: Butterworth-Heinemann Elsevier; 2008:485–491.
Cervero, RM. Effective continuing education for professionals. San Francisco: Jossey-Bass; 1988.
Chi TH, Glaser R, Farr MJ, eds. The Nature of Expertise. Hillsdale: Lawrence Erlbaum Associates, 1988.
Childs, JD, Cleland, JA, Elliott, JM, et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38(9):A1–A34.
Christensen N: ‘Development of clinical reasoning capability in student physical therapists’, Unpublished PhD thesis, 2009, University of South Australia.
Christensen, N, Jones, M, Carr, J. Clinical reasoning in orthopaedic manual therapy. In Grant R, ed.: Physical therapy of the cervical and thoracic spine, ed 3, Edinburgh: Churchill Livingstone, 2002.
Christensen, N, Jones, MA, Higgs, J, Edwards, I. Dimensions of clinical reasoning capability. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical Reasoning in the Health Professions. ed 3. Amsterdam: Butterworth-Heinemann Elsevier; 2008:101–110.
Christensen, N, Jones, MA, Edwards, I, Higgs, J. Helping physiotherapy students develop clinical reasoning capability. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical Reasoning in the Health Professions. ed 3. Amsterdam: Butterworth-Heinemann Elsevier; 2008:389–396.
Christensen, N, Jones, M, Edwards, I. Clinical Reasoning and Evidence-based Practice. Independent Study Course 21.2.2: Current Concepts of Orthopaedic Physical Therapy, ed 3. La Crosse: Orthopaedic Section, APTA, Inc; 2011.
Cibulka, MT, White, DM, Woehrle, J, et al. Hip pain and mobility deficits – hip osteoarthritis: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2009;39(4):A1–A25.
Clouder, L. Reflective practice in physiotherapy education: A critical conversation. Stud Higher Ed. 2000;25(2):211–223.
Cohen, S, Kamarck, T, Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. 1983;24:386–396.
Cook, JL, Purdam, CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009;43:409–416.
Craig, KD. Emotions and psychobiology. In: McMahon S, Koltzenburg M, eds. Wall and Melzack's textbook of pain. ed 5. Elsevier; 2006:231–240.
Cranton, P. Understanding and promoting transformative learning: A guide for educators of adults. San Francisco: Jossey-Bass; 1994.
Cusick, A. Personal frames of reference in professional practice. In: Higgs J, Titchen A, eds. Practice knowledge and expertise in the health professions. Oxford: Butterworth Heinemann; 2001:91–95.
de Bono, E. Lateral thinking. Creativity step by step. New York: Harper and Row; 1970.
de Bono, E. De Bono's thinking course. New York: MICA Management Resources; 1994.
DeGroot, KI, Boeke, S, van den Berge, HJ, et al. Assessing short- and long-term recovery from lumbar surgery with pre-operative biographical, medical and psychological variables. Br J Health Psychol. 1997;2:229–243.
Devor, M. Response of nerves to injury in relation to neuropathic pain. In: McMahon SB, Koltzenburg M, eds. Wall and Melzack's Textbook of pain. ed 5. Edinburgh: Elsevier Churchill Livingstone; 2006:905–927.
Donaghy, M, Nicol, M, Davidson, K. Cognitive-behavioural interventions in physical and occupational therapy. Edinburgh: Butterworth-Heinemann Elsevier; 2008.
Doody, C, McAteer, M. Clinical reasoning of expert and novice physiotherapists in an outpatient orthopaedic setting. Physiotherapy. 2002;88(5):258–268.
Duncan, G. Mind-body dualism and the bio-psychosocial model of pain: what did Descartes really say? J Med Philos. 2000;25:485–513.
Edwards, IC, Clinical reasoning in three different fields of physiotherapy – a qualitative case study approach. Vols. I and II. Unpublished thesis submitted in partial fulfilment of the Doctor of Philosophy in Health Sciences, University of South Australia, Adelaide, Australia, The Australian Digitized Theses Program, 2001. http://www.library.unisa.edu.au/adt-root/public/adt-SUSA-20030603-090552/index.html, 2000
Edwards, IC, Jones, MA, Collaborative reasoning. Unpublished paper submitted in partial fulfillment of the Graduate Diploma in Orthopaedics. Adelaide, Australia:University of South Australia; 1996.
Edwards, I, Jones, MA. The role of clinical reasoning in understanding and applying the International Classification of Functioning, Disability and Health (ICF). Kinesitherapie. 2007;71:e1–e9.
Edwards, I, Jones, M. Clinical reasoning and expertise. In: Jensen GM, Gwyer J, Hack LM, Shepard KF, eds. Expertise in physical therapy practice. ed 2. Boston: Elsevier; 2007:192–213.
Edwards, I, Jones, M, Carr, J, Braunack-Mayer, A, Jensen, G. Clinical reasoning strategies in physical therapy. Phys Ther. 2004;84(4):312–335.
Edwards, I, Jones, M, Higgs, J, Trede, F, Jensen, G. What is collaborative reasoning? Adv Physiother. 2004;6:70–83.
Edwards, I, Jones, MA, Hillier, S. The interpretation of experience and its relationship to body movement: a clinical reasoning perspective. Man Ther. 2006;11:2–10.
Elstein, AS, Schwarz, A. Clinical problem solving and diagnostic decision making: Selective review of the cognitive literature. Br Med J. 2002;324:729–732.
Elstein, AS, Shulman, L, Sprafka, S. Medical problem solving: An analysis of clinical reasoning. Cambridge: Harvard University Press; 1978.
Embrey, DG, Guthrie, MK, White, OR, Dietz, J. Clinical decision making by experienced and inexperienced pediatric physical therapists for children with diplegic cerebral palsy. Phys Ther. 1996;76(1):20–33.
Engel, G. The bio-psychosocial model and the education of health professionals. Ann NY Acad Sci. 1978;310:535–544.
Eraut, M. Developing professional knowledge and competence. London: Routledge Falmer; 1994.
Ericsson A, Smith J, eds. Toward a general theory of expertise: Prospects and limits. New York: Cambridge University Press, 1991.
Escorpizo, R, Stucki, G, Cieza, A, et al. Creating an interface between the International Classification of Functioning, Disability and Health and physical therapist practice. Phys Ther. 2010;90(7):1053–1067.
Feltovich, PJ, Barrows, HS. Issues of generality in medical problem solving. In: Schmidt HG, de Volder ML, eds. Tutorials in problem-based learning: A new direction in teaching the health professions. Assen: Van Gorcum; 1984:128–141.
Fields, HL, Basbaum, AI, Heinricher, MM. Central nervous system mechanisms of pain modulation. In: McMahon SB, Koltzenburg M, eds. Wall and Melzack's textbook of pain. ed 5. Edinburgh: Elsevier Churchill Livingstone; 2006:125–142.
Fleming, MH. The therapist with the three-track mind. Am J Occup Ther. 1991;45:1007–1014.
Flor, H, Turk, DC. Cognitive and learning aspects. In: McMahon SB, Koltzenburg M, eds. Wall and Melzack's Textbook of pain. ed 5. Edinburgh: Elsevier Churchill Livingstone; 2006:241–258.
Forneris, SG. Exploring the attributes of critical thinking: A conceptual basis. IJNES. 1(1), 2004.
Galea, MP. Neuroanatomy of the nociceptive system. In: Strong J, Unrush AM, Wright A, Baxter GD, eds. Pain: a textbook for therapists. Edinburgh: Churchill Livingstone; 2002:13–41.
Gatchel, RJ, Bo, Peng, Y, Peters, ML, Fuchs, PN, Turk, DC. The bio-psychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624.
Gifford, L. Tissue and input related mechanisms. In: Gifford L, ed. Topical issues in pain: Whiplash – science and management. Fear-avoidance beliefs and behaviour. Falmouth: CNS Press; 1998:57–65.
Gifford, L. Central mechanisms. In: Gifford L, ed. Topical issues in pain: Whiplash – science and management. Fear-avoidance beliefs and behaviour. Falmouth: CNS Press; 1998:67–80.
Gifford, L. Output mechanisms. In: Gifford L, ed. Topical issues in pain: Whiplash – science and management. Fear-avoidance beliefs and behaviour. Falmouth: CNS Press; 1998:81–91.
Gifford, L. Acute low cervical nerve root conditions: symptoms, symptom behaviour and physical screening. In Touch. 1998;85(Winter):4–19.
Gifford, L, Thacker, M, Jones, MA. Physiotherapy and pain. In: McMahon SB, Koltzenburg M, eds. Wall and Melzack's Textbook of pain. ed 5. Edinburgh: Elsevier Churchill Livingstone; 2006:603–617.
Glaser, R. Education and thinking: the role of knowledge. Am Psychol. 1984;39:93–104.
Glaser, R, Chi, MTH. Overview. In: Chi MTH, Glaser R, Farr MJ, eds. The nature of expertise. Hillsdale: Lawrence Erlbaum, 1988.
Gottlieb, A, Golander, H, Bar-Tal, Y. The influence of social support and perceived control on handicap and quality of life after stroke. Aging Clin Exp Res. 2001;13:11–15.
Goodman, CC, Snyder, TEK. Differential diagnosis for physical therapists. Screening for referral, ed 5. St Louis: Elsevier; 2013.
Gordon, M, Murphy, CP, Candee, D, Hiltunen, E. Clinical judgement: an integrated model. Adv Nurs Sci. 1994;16:55–70.
Greeno, JG. The situativity of knowing, learning, and research. Am Psychol. 1998;53(1):5–26.
Hagedorn, R. Clinical decision-making in familiar cases: a model of the process and implications for practice. Br J Occup Ther. 1996;59:217–222.
Harding, V. Application of the cognitive-behavioural approach. In: Pitt-Brooke J, Reid H, Lockwood J, Kerr K, eds. Rehabilitation of movement: Theoretical bases of clinical practice. London: WB Saunders; 1998:539–583.
Harding, V, de C Williams, A. Extending physiotherapy skills using a psychological approach: Cognitive-behavioural management of chronic pain. Physiotherapy. 1995;81(11):681–688.
Harris, IB. New expectations for professional competene. In: Curry L, Wergin J, eds. Educating professionals: Responding to new expectations for competence and accountability. San Francisco: Jossey-Bass; 1993:17–52.
Hayes, B, Adams, R. Parallels between clinical reasoning and categorization. In: Higgs J, Jones MA, eds. Clinical reasoning in the health professions. ed 2. Oxford: Butterworth Heinemann; 2000:45–53.
Higgs, J. Fostering the acquisition of clinical reasoning skills. NZ J Physio. 1990;18:13–17.
Higgs, J. Developing clinical reasoning competencies. Physiotherapy. 1992;78(8):575–581.
Higgs, J. A programme for developing clinical reasoning skills in graduate physiotherapists. Med Teach. 1993;15(2):195–205.
Higgs, J. Educational theory and principles related to learning clinical reasoning. In: Jones MA, Rivett DA, eds. Clinical reasoning for manual therapists. Edinburgh: Butterworth Heinemann; 2008:379–402.
Higgs, J, Titchen, A. The nature, generation and verification of knowledge. Physiotherapy. 1995;81(9):521–530.
Higgs J, Edwards H, eds. Educating beginning practitioners. Oxford: Butterworth Heinemann, 1999.
Higgs, J, Hunt, A. Rethinking the beginning practitioner: introducing the ‘Interactional Professional. In: Higgs J, Edwards H, eds. Educating beginning practitioners. Oxford: Butterworth-Heinemann; 1999:10–18.
Higgs, J, Jones, MA. Clinical reasoning in the health professions. In: Higgs J, Jones MA, eds. Clinical reasoning in the health professions. ed 2. Oxford: Butterworth Heinemann; 2000:3–14.
Higgs, J, Jones, MA. Clinical decision making and multiple problem spaces. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical reasoning in the health professions. ed 3. Amsterdam: Butterworth Heinemann Elsevier; 2008:3–18.
Higgs, J, Andresen, L, Fish, D. Practice knowledge – its nature, sources and contexts. In: Higgs J, Richardson B, Dahlgren MA, eds. Developing practice knowledge for health professionals. Edinburgh: Butterworth Heinemann; 2004:51–69.
Higgs, J, Jones, M, Edwards, I, Beeston, S. Clinical reasoning and practice knowledge. In: Higgs J, Richardson B, Dahlgren MA, eds. Developing practice knowledge for health professionals. Edinburgh: Butterworth Heinemann; 2004:181–199.
Higgs, J, Jones, MA, Titchen, A. Knowledge, reasoning and evidence for practice. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical reasoning in the health professions. ed 3. Amsterdam: Butterworth Heinemann Elsevier; 2008:151–161.
Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical reasoning in the health professions, ed 3, Amsterdam: Butterworth Heinemann Elsevier, 2008.
Hooper, B. The relationship between pretheoretical assumptions and clinical reasoning. Am J Occup Ther. 1997;51(5):328–337.
Imrie, R. Demystifying disability: a review of the International Classification of Functioning, Disability and Health. Sociol Health Illn. 2004;26(3):287–305.
Jänig, W, Levine, JD. Autonomic-endocrine-immune interactions in acute and chronic pain. In: McMahon SB, Koltzenburg M, eds. Wall and Melzack's textbook of pain. ed 5. Edinburgh: Elsevier Churchill Livingstone; 2006:205–218.
Jeffreys, E. Prognosis in musculoskeletal injury. A handbook for doctors and lawyers. Oxford: Butterworth-Heinemann; 1991.
Jensen, GM, Shepard, KF, Hack, LM. The novice versus the experienced clinician: Insights into the work of the physical therapist. Phys Ther. 1990;70(5):314–323.
Jensen, GM, Shepard, KF, Gwyer, J, Hack, LM. Attribute dimensions that distinguish master and novice physical therapy clinicians in orthopedic settings. Phys Ther. 1992;72(10):711–722.
Jensen, GM, Lorish, CD, Shepard, KF. Understanding and influencing patient receptivity to change: The patient-practitioner collaborative model. In: Shepard KF, Jensen GM, eds. Handbook of teaching for physical therapists. ed 2. Boston: Butterworth-Heinemann; 2002:323–350.
Jensen, MP, Nielson, WR, Turner, JA, et al. Readiness to self-manage pain is associated with coping and with psychological and physical functioning among patients with chronic pain. Pain. 2003;104:529–537.
Jensen, GM, Gwyer, J, Hack, LM, Shepard, KF. Expertise in physical therapy practice, ed 2. St Louis: Saunders Elsevier; 2007.
Jensen, GM, Resnik, L, Haddad, A. Expertise and clinical reasoning. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical Reasoning in the Health Professions. ed 3. Amsterdam: Butterworth-Heinemann Elsevier; 2008:123–135.
Jette, AM. Toward a common language for function, disability, and health. Phys Ther. 2006;86(5):726–734.
Johnson, R. ‘Attitudes just don't hang in the air …’ disabled people's perceptions of physiotherapists. Physiotherapy. 1993;79:619–626.
Johnson, R, Moores, L. Pain management: integrating physiotherapy and clinical psychology. In: Gifford L, ed. Topical issues in pain 5, Treatment, Communication, Return to Work, Cognitive Behavioural, Pathophysiology. Falmouth: CNS Press; 2006:311–319.
Jones, MA. The clinical reasoning process in manipulative therapy. In: Dalziel BA, Snowsill JC, eds. Proceedings of the fifth biennial conference of the manipulative therapists association of Australia. Melbourne: Manipulative Therapists Association of Australia; 1987:62–69.
Jones, MA. Clinical reasoning in manual therapy. Phys Ther. 1992;72(12):875–884.
Jones, MA. Clinical reasoning and pain. Man Ther. 1995;1:17–24.
Jones, MA. Clinical reasoning: The foundation of clinical practice. Part 1. AJP. 1997;43(3):167–170.
Jones, MA. Clinical reasoning: The foundation of clinical practice. Part 2. AJP. 1997;43(3):213–217.
Jones, MA, Edwards, I. Learning to facilitate change in cognition and behaviour. In: Gifford L, ed. Topical issues in pain 5. Falmouth: CNS Press; 2006:273–310.
Jones, MA, Rivett, DA. Introduction to clinical reasoning. In: Jones MA, Rivett DADA, eds. Clinical reasoning for manual therapists. Edinburgh: Butterworth Heinemann; 2004:3–24.
Jones, MA, Edwards, I, Gifford, L. Conceptual models for implementing bio-psychosocial theory in clinical practice. Man Ther. 2002;7:2–9.
Jones, MA, Grimmer, K, Edwards, I, et al, Challenges in applying best evidence to physiotherapy. Internet J All Health Sci Prac. 2006;4(3). http://ijahsp.nova.edu/articles/vol4num3/jones.htm
Jones, MA, Jensen, G, Edwards, I. Clinical reasoning in physiotherapy. In: Higgs J, Jones MA, Loftus SS, Christensen N, eds. Clinical reasoning in the health professions. ed 3. Amsterdam: Butterworth Heinemann Elsevier; 2008:245–256.
Jones, M, van Kessel, G, Swisher, L, et al. Cognitive maps and the structure of observed learning outcome assessment of physiotherapy students’ ethical reasoning knowledge. Assess Eval High Educ. 2013.
Jorgensen, P. Concepts of body and health in physiotherapy: the meaning of the social/cultural aspects of life. Physiother Theory Pract. 2000;16(2):105–115.
Kaufman, DR, Yoskowitz, NA, Patel, VL. Clinical reasoning and biomedical knowledge: implications for teaching. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical Reasoning in the Health Professions. ed 3. Amsterdam: Butterworth-Heinemann Elsevier; 2008:137–149.
Keefe, F, Scipio, C, Perri, L. Psychosocial approaches to managing pain: current status and future directions. In: Gifford L, ed. Topical issues in pain 5: Treatment, communication, return to work, cognitive behavioural, pathophysiology. Falmouth: CNS Press; 2006:241–256.
Kempainen, RR, Migeon, MB, Wolf, FM. Understanding our mistakes: a primer on errors in clinical reasoning. Med Teach. 2003;25(2):177–181.
Kendall, N, Watson, P. Identifying psychosocial yellow flags and modifying management. In: Gifford L, ed. Topical Issues of Pain 2, Bio-psychosocial assessment and management, Relationships and pain. Falmouth: CNS Press; 2000:131–139.
Kessler, RC, Andrews, G, Colpe, LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976.
Khan, KM, Scott, A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. Br J Sports Med. 2009;43:247–251.
King, G, Tucker, MA, Baldwin, P, et al. A life needs model of pediatric service delivery: services to support community participation and quality of life for children and youth with disabilities. Phys Occup Ther Pediatr. 2002;22(2):53–77.
Klaber Moffett, JA, Richardson, PH. The influence of the physiotherapist-patient relationship on pain and disability. Physiother Theory Pract. 1997;13:89–96.
Kleinman, A, Brodwin, PE, Good, BJ, Good, MJD. Pain as human experience, an introduction. In: Good MJD, Brodwin PE, Good BJ, Kleinman A, eds. Pain as human experience: An anthropological perspective. Berkeley: University of California Press; 1992:1–28.
Kuhn, TS. The Structure of Scientific Revolutions, ed 2. Chicago: University of Chicago Press; 1970.
Ladyshewsky, R, Jones, MA. Peer coaching to generate clinical reasoning skills. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical Reasoning in the Health Professions. ed 3. Amsterdam: Butterworth-Heinemann Elsevier; 2008:433–440.
Lave, J, Wenger, E. Situated learning: Legitimate peripheral participation. Cambridge: Cambridge University Press; 1991.
Lee, D. The pelvic girdle. An integration of clinical expertise and research. Edinburgh: Churchill Livingstone Elsevier; 2011.
Lehrer, J. How we decide. Boston: Mariner Books; 2009.
Leventhal, H. The pain system: a multilevel model for the study of motivation and emotion. Motiv Emot. 1993;17:139–146.
Leventhal, H, Meyer, D, Nerenz, D, The common sense representation of illness danger, Contributions to Medical Pscychology. Rachman, S, eds. Contributions to Medical Pscychology. New York:Pergamon Press; 1980;vol 2:7–30.
Linton, SJ, Andersson, T. Can chronic disability be prevented? A randomized trial of a cognitive-behavior intervention and two forms of information for patients with spinal pain. Spine. 2000;25:2825–2831.
Linton, SJ, Hallden, K. Can we screen for problematic back pain? A screening questionnaire for predicting outcome in acute and subacute back pain. Clin J Pain. 1998;14(3):209–215.
Linton, SJ, Nordin, E. A 5-year follow-up evaluation of the health and economic consequences of an early cognitive behavioural intervention for back pain: A randomised controlled trial. Spine. 2006;31(8):853–858.
Logerstedt, D, Snyder-Mackler, L, Ritter, R, et al. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40(4):A1–A37.
Lorig, K, Stewart, A, Ritter, P, et al. Outcome Measures for Health Education and other Health Care Interventions. Thousand Oaks: Sage Publications; 1996.
Lorig, KR, Sobel, DS, Ritter, PL, et al. Effect of a self-management program for patients with chronic disease. Eff Clin Pract. 2001;4:256–262.
McCracken, LM, Gross, RT. The role of pain-related anxiety reduction in the outcome of multidisciplinary treatment for low back pain: Preliminary results. J Occup Rehabil. 1998;8:179–189.
McPoil, T, Martin, R, Cornwall, M, et al. Heel pain–plantar fasciitis: clinical practice guidelines linked to the International Classification of Function, Disability, and Health from the Orthopedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38(4):A1–A18.
Mackinnon, LT. Advances in exercise immunology. Champaign: Human Kinetics; 1999.
Main, CJ. The Modified Somatic Perception Questionnaire (MSPQ). J Psychosom Res. 1983;27(6):503–514.
Main, C, Watson, P. The distressed and angry low back pain patient. In: Gifford L, ed. Topical Issues in Pain 3. Falmouth: CNS Press; 2002:175–192.
Main, C, Sullivan, M, Watson, P. Pain management: Practical applications of the bio-psychosocial perspective in clinical and occupational settings. Edinburgh: Churchill Livingstone; 2008.
Maitland, GD. Vertebral Manipulation, ed 5. London: Butterworth-Heinemann; 1986.
Maitland, GD. The Maitland concept: assessment, examination, and treatment by passive movement. In: Twomey LT, Taylor JR, eds. Clinics in physical therapy. Physical therapy for the low back. New York: Churchill Livingstone; 1987:135–155.
Martin, P. The sickening mind: brain, behaviour, immunity and disease. London: Harper Collins; 1997.
Mattingly, C. The narrative nature of clinical reasoning. Am J Occup Ther. 1991;45:998–1005.
Mattingly, C, Fleming, MH. Clinical reasoning: forms of inquiry in a therapeutic practice. Philadelphia: F.A. Davis; 1994.
May, BJ, Dennis, JK. Expert decision making in physical therapy-a survey of practitioners. Phys Ther. 1991;71(3):190–206.
Melzack, R. Pain and the neuromatrix in the brain. J Dent Educ. 2001;65(12):1378–1382.
Melzack, R. Evolution of the neuromatrix theory of pain. Pain Pract. 2005;5:85–94.
Meyer, RA, Ringkamp, M, Campbell, JN, Raja, SN. Peripheral mechanisms of cutaneous nociception. In: McMahon SB, Koltzenburg M, eds. Wall and Melzack's textbook of pain. ed 5. Elsevier; 2006:3–34.
Mezirow, J. Fostering critical reflection in adulthood: A guide to transformative and emancipatory learning. San Francisco: Jossey-Bass; 1990.
Mezirow, J. Transformative dimensions of adult learning. San Francisco: Jossey-Bass; 1991.
Mezirow, J. Learning to think like an adult: Core concepts of transformation theory. In: Mezirow J, ed. Learning as transformation: Critical perspectives on a theory in progress. San Francisco: Jossey-Bass; 2000:3–33.
Moseley, GL. A pain neuromatrix approach to patients with chronic pain. Man Ther. 2003;8:1–11.
Moseley, GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain. 2004;8:39–45.
Muncey, H. Explaining pain to patients. In: Gifford L, ed. Topical issues in Pain 4 – Placebo and nocebo, pain management, muscles and pain. Falmouth: CNS Press; 2002:157–166.
Neuhaus, BE. Ethical considerations in clinical reasoning: the impact of technology and cost containment. Am J Occup Ther. 1988;42:288–294.
Newell, A, Simon, HA. Human problem solving. Englewood Cliffs: Prentice-Hall; 1972.
Nicholas, MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. 2007;11:153–163.
Nickerson, RS, Perkins, DN, Smith, EE. The teaching of thinking. Hillsdale: Lawrence Erlbaum Associates; 1985.
Nijs, J, Van Houdenhove, B, Oostendorp, RAB. Recognition of central sensitization in patients with musculoskeletal pain: Application of pain neurophysiology in manual therapy practice. Man Ther. 2010;15:135–141.
Osborn, M, Smith, JA. The personal experience of chronic benign lower back pain: An interpretative phenomenological analysis. Br J Health Psychol. 1998;3:65–83.
Patel, VL, Groen, G. Knowledge-based solution strategies in medical reasoning. Cogn Sci. 1986;10:91–116.
Patel, VL, Groen, GJ. The general and specific nature of medical expertise: A critical look. In: Ericsson A, Smith JJ, eds. Toward a general theory of expertise: prospects and limits. New York: Cambridge University Press; 1991:93–125.
Patel, VL, Groen, G, Frederiksen, C. Differences between medical students and doctors in memory for clinical cases. Med Educ. 1986;20:3–9.
Paul, R, Elder, L. The thinker's guide to: the art of Socratic questioning. Dillon Beach: Foundation for Critical Thinking; 2006.
Paul, R, Elder, L. A guide for educators to: Critical thinking competency standards. Dillon Beach: Foundation for Critical Thinking; 2007.
Pavlin, DJ, Rapp, SE, Pollisar, N. Factors affecting discharge time in adult outpatients. Anesth Analg. 1998;87:816–826.
Payton, OD. Clinical reasoning process in physical therapy. Phys Ther. 1985;65(6):924–928.
Payton, OD, Nelson, CE, Hobbs, MSC. Physical therapy patients’ perceptions of their relationships with health care professionals. Physiother Theory Pract. 1998;14:211–221.
Pincus, T. The psychology of pain. In: French SS, Sim J, eds. Physiotherapy a Psychosocial Approach. Edinburgh: Elsevier; 2004:95–115.
Pincus, T, Morley, S. Cognitive-processing bias in chronic pain: a review and integration. Psychol Bull. 2001;127:599–617.
Radloff, LS. The CES-D scale: a self depression scale for research in the general population. Appl Psychol Measures. 1977;1:385–401.
Resnik, L, Jensen, GM. Using clinical outcomes to explore the theory of expert practice in physical therapy. Phys Ther. 2003;83(12):1090–1106.
Revonsuo, A. Consciousness, dreams and virtual realities. Phil Psychol. 1995;8(1):35–54.
Revonsuo, A. Inner presence. Consciousness as a biological phenomenon. Cambridge: The MIT Press; 2006.
Rivett, DA, Higgs, J. Hypothesis generation in the clinical reasoning behavior of manual therapists. J Phys Ther Educ. 1997;11(1):40–45.
Rivett, DA, Jones, MA. Improving clinical reasoning in manual therapy. In: Jones MA, Rivett DA, eds. Clinical reasoning for manual therapists. Edinburgh: Butterworth Heinemann; 2004:3–24.
Rivett, DA, Jones, MA. Using case reports to teach clinical reasoning. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical reasoning in the health professions. ed 3. Amsterdam: Butterworth Heinemann Elsevier; 2008:477–484.
Rodgers, C. Defining reflection: Another look at John Dewey and reflective thinking. Teach Coll Rec. 2002;104(4):842–866.
Rumelhart, DE, Ortony, E. The representation of knowledge in memory. In: Anderson RC, Spiro RJ, Montague WE, eds. Schooling and the Acquisition of Knowledge. Hillsdale: Lawrence Erlbaum; 1977:99–135.
Sackett, D, Straus, S, Richardson, W, et al. Evidence-based medicine: How to practice and teach EBM, ed 2. Edinburgh: Churchill Livingstone; 2000.
Salkovskis, P. The cognitive approach to anxiety: threat beliefs, safety seeking behaviour, and the special case of health anxiety and obsessions. In: Salkovskis P, ed. Frontiers of Cognitive Therapy. London: The Guilford Press; 1996:48–74.
Sapolsky, RM. Why zebras don't get ulcers. An updated guide to stress, stress-related diseases, and coping. New York: Freeman; 1998.
Schaible, H-G. Basic mechanisms of deep somatic pain. In: McMahon SB, Koltzenburg M, eds. Wall and Melzack's textbook of pain. ed 5. Elsevier; 2006:621–633.
Schön, DA. The reflective practitioner. New York: Basic Books; 1983.
Schön, DA. Educating the reflective practitioner: Toward a new design for teaching and learning in the professions. San Francisco: Jossey-Bass; 1987.
Schmidt, H, Norman, G, Boshuizen, H. A cognitive perspective on medical expertise: Theory and implications. Acad Med. 1990;65(10):611–620.
Scott, I. Teaching clinical reasoning: a case-based approach. In: Higgs J, Jones MA, eds. Clinical reasoning in the health professions. ed 2. Oxford: Butterworth Heinemann; 2000:290–297.
Sharp, TJ. The “safety seeking behaviours” construct and its application to chronic pain. Behav Cogn Psychother. 2001;29:241–244.
Shepard, KF, Jensen, GM. Handbook of teaching for physical therapists, ed 2. Oxford: Butterworth-Heinemann; 2002.
Sim, J, Smith, MV. The sociology of pain. In: French S, Sim J, eds. Physiotherapy a Psychosocial Approach. Edinburgh: Elsevier; 2004:117–139.
Skelton, JA, Croyle, RT. Mental representation, health, and illness: an Introduction. In: Skelton JA, Croyle RT, eds. Mental Representation in Health and Illness. New York: Springer-Verlag; 1991:1–9.
Sluijs, EM. Patient education in physiotherapy: towards a planned approach. Physiotherapy. 1991;77:503–508.
Smart, KM, Blake, C, Staines, A, et al. Mechanisms-based clasificaitons of musculoskeletal pain: Part 3 of 3: Symptoms and signs of nociceptive pain in patients with low back (+/− leg) pain. Man Ther. 2012;17(4):352–357.
Smart, KM, Blake, C, Staines, A, et al. Mechanisms-based classifications of musculoskeletal pain: Part 2 of 3: Symptoms and signs of peripheral neuropathic pain in patients with low back (+/− leg) pain. Man Ther. 2012;17(4):345–351.
Smart, KM, Blake, C, Staines, A, et al. Mechanisms-based classifications of musculoskeletal pain: Part 1 of 3: Symptoms and signs of central sensitisation in patients with low back (+/− leg) pain. Man Ther. 2012;17(4):336–344.
Smiths, MS, Wallston, KA, Smith, CA. Development and validation of the perceived health competence scale. Health Educ Res. 1995;10(1):51–64.
Stacey, RD. Strategic management and organizational dynamics. London: Pitman Publishing; 1996.
Steen, E, Haugli, L. Generalised chronic musculoskeletal pain as a rational reaction to a life situation? Theor Med. 2000;21:581–599.
Steiner, WA, Ryser, L, Huber, E, et al. Use of the ICF model as a clinical problem-solving tool in physical therapy and rehabilitation medicine. Phys Ther. 2002;82(11):1098–1107.
Stewart, J, Kempenaar, L, Lauchalan, D. Rethinking yellow flags. Man Ther. 2011;16:196–198.
Strong, J, Unruh, AM. Psychologically based pain management strategies. In: Strong J, Unruh AM, Wright A, Baxter GDGD, eds. Pain. A textbook for therapists. Edinburgh: Churchill Livingstone; 2002:169–185.
Thomas-Edding D: ‘Clinical problem solving in physical therapy and its implications for curriculum development’, Paper presented at the Tenth International Congress of the World Confederation of Physical Therapy, Sydney, Australia, 1987, May 17–22.
Trede, F, Higgs, J. Collaborative decision making. In: Higgs J, Jones MA, Loftus S, Christensen N, eds. Clinical reasoning in the health professions. ed 3. Amsterdam: Butterworth Heinemann Elsevier; 2008:31–41.
Turk, DC, Flor, H. The cognitive-behavioural approach to pain management. In: McMahon SB, Koltzenburg M, eds. Wall and Melzack's textbook of pain. ed 5. Edinburgh: Elsevier Churchill Livingstone; 2006:339–348.
Turk, DC, Rudy, TE. Cognitive factors and persistent pain: a glimpse into Pandora's box. Cognit Ther Res. 1992;16:99–122.
Unsworth, CA. Clinical reasoning: how do pragmatic reasoning, worldview and client-centredness fit? Br J Occup Ther. 2004;67(1):10–19.
Van Wingerden, BAM. Connective tissue in rehabilitation. Vaduz: Scipro Verlag; 1995.
Vicenzino, B, Souvlis, T, Wright, A. Musculoskeletal pain. In: Strong J, Unrush AM, Wright A, Baxter GD, eds. Pain: A textbook for therapists. Edinburgh: Churchill Livingstone; 2002:327–349.
Vicenzino, B, Hing, W, Rivett, D, Hall, T. Mobilisation with Movement, The art and the science. Edinburgh: Churchill Livingstone; 2011.
Vlaeyen, JWS, Linton, SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–332.
Vlaeyen, JWS, de Jong, J, Geilen, M, et al. The treatment of fear of movement/(Re)injury in chronic low back pain: Further evidence on the effectiveness of exposure in vivo. Clin J Pain. 2002;18:251–261.
Waddell, G, Newton, M, Henderson, I, et al. A fear-avoidance belief's questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168.
Watts, NT. Teaching the components of clinical decision analysis in the classroom and clinic. In: Higgs J, Jones M, eds. Clinical reasoning in the health professions. Oxford: Butterworth-Heinemann; 1995:204–212.
Wenger, E. Communities of practice: Learning, meaning, and identity. Cambridge: Cambridge University Press; 1998.
Werner, D. Disabled persons as leaders in the problem solving process. In: Nothing about us without us: Developing innovative technologies for, by and with disabled persons. Palo Alto: Health Wrights; 1998.
Woby, SR, Roach, NK, Urmston, M, Watson, PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117(1–2):137–144.
World Health Organization. International classification of functioning, disability and health. Geneva: World Health Organization; 2001.
Williams, DA, Keefe, FJ. Pain beliefs and the use of cognitive-behavioral coping strategies. Pain. 1991;46:185–190.
Wilson, P, Henry, J, Nicholas, M. Cognitive methods in the management of chronic pain and tinnitus. Aust Psychol. 1993;28:172–180.
Wolf, CJ. Central sensitization: Implication for diagnosis and treatment of pain. Pain. 2011;152:s2–215.
Wright, A. Neurophysiology of pain and pain modulation. In: Strong J, Unrush AM, Wright A, Baxter GD, eds. Pain: A textbook for therapists. Edinburgh: Churchill Livingstone; 2002:43–64.
Zimmerman, BJ, Lindberg, C, Plsek, PE. Edgeware: Insights from complexity science for health care leaders, ed 2. Irving: VHA Inc; 2001.