Individualized Orthodontic Diagnosis
Flavio Andres Uribe, Taranpreet K. Chandhoke, Ravindra Nanda
The term diagnosis is defined as the identification of a disease by careful investigation of its symptoms and history.1 While not a true disease per se, malocclusions are the “disease” processes of orthodontics and the central focus of orthodontic diagnoses. Malocclusions can have esthetic and functional implications, and an accurate diagnosis is required to best understand their etiology and the treatment options for managing the abnormality. From an esthetic standpoint, there are psychological implications associated with malocclusions related to social acceptance and success.2 From a functional standpoint, mastication, speech, and protection of the structures in the entire stomatognathic system can contribute to or be the result of the malocclusion that is present.
To define the abnormal or pathological characteristics of the malocclusion, there needs to be an appreciation of what is defined as “normal.” This is a particular challenge because what is considered normal falls within a wide range. Variability is found throughout nature, so defining the limits of the normal range can be difficult. While esthetic perceptions vary through history and among individuals, races, and cultures, ideal occlusion and its functional implications are characterized by strict morphological features. Thus the definition of a normal occlusion involves both objective and subjective components.
Extensive research has determined the characteristics of normal functional occlusion. Concepts such as cusp-to-fossa or cusp-to-interproximal space occlusion, lateral and anterior guidance, and mutually protected occlusion are described comprehensively in other textbooks.3 However, the criteria for ideal occlusal function are better defined in comparison to ideal esthetic values. Most of the occlusal concepts accepted today are derived from the assumed premise that good anatomy (i.e., good occlusal interdigitation) is analogous to proper function (Fig. 1-1).
From the esthetic standpoint, orthodontists base their judgment on cephalometric norms obtained many decades ago from population samples with vaguely defined parameters of esthetics. In general, these studies assumed that good occlusion was directly related to good facial esthetics. Although these measurements provide some objective guidelines that can be used to start defining how each patient differs from the norm, there are limitations to these analyses. Furthermore, it is not the absolute numeric amounts and their variation that dictate treatment but the accurate interpretation of these and all data obtained from the clinical examination and other patient records.
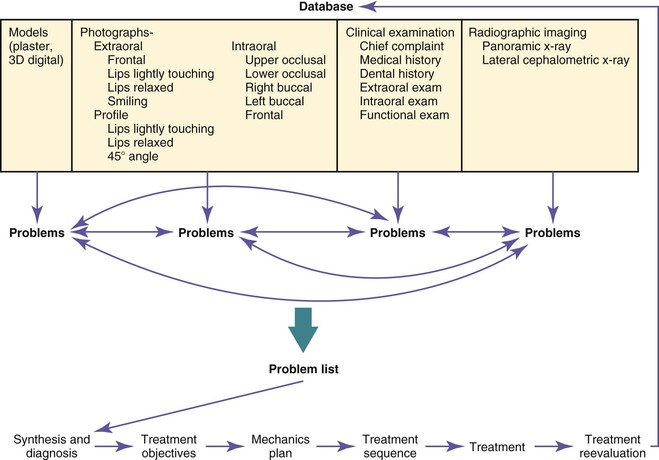
To accurately diagnose a malocclusion, orthodontics has adopted the problem-based approach originally developed in medicine.4 Every factor that potentially contributes to the etiology, might contribute to the abnormality, or might influence treatment should be evaluated. Information is gathered through a medical and dental history, clinical examination, and records that include models, photographs, and radiographic imaging. A problem list is generated from the analysis of the database that contains a network of interrelated factors. The diagnosis is established after a continuous feedback between the problem recognition and the database. Ultimately, the diagnosis should provide some insight into the etiology of the malocclusion (Fig. 1-2).
The diagnosis and problem list is the framework that dictates the treatment objectives for the patient. Once formulated, the treatment plan is designed to address those objectives, from the mechanics to the sequence that will be used.
From the treatment objectives perspective, one or more treatment options can be developed to address each objective. Each treatment option will have advantages and disadvantages for the patient. During the process of obtaining informed consent from the patient, clear descriptions of the advantages, disadvantages, and risks of each treatment plan should be presented and the patient will ultimately determine the final treatment plan. The treatment plan then dictates the mechanics plan designed to achieve the desired goals with the greatest efficiency and fewest side effects.
This chapter discusses some of the objective measures that define the range of normality, both from an occlusal and a dentofacial standpoint. It is important to know that although emphasis is placed on the entire dentofacial complex, there are limits to the amount of correction that can be achieved with orthodontic treatment.
The clinician has to work within certain constraints and understand the limitations of the various treatment options. For example, the soft tissue envelope allows for only a certain amount of correction. If major movements are needed, they may require other treatment options such as surgery or skeletal anchorage, which, although able to achieve a wider range of movements, are limited by the boundaries of the soft tissue envelope. The primary goal should be to achieve the best possible facial balance and functional occlusion.
Finally, while great care is taken in formulating a detailed treatment plan, it is important to realize that the diagnosis and treatment plan are dynamic processes. As the plan is executed, continuous monitoring and effective evaluation of the objectives are needed. Appropriate reassessment, adjustment, and corrective measures to the original plan are crucial if all specific goals and not only the occlusal goals are to be achieved.
As described above, very precise collection of data is needed to achieve a proper diagnosis. The database should include a thorough medical and dental history, a set of models, the necessary radiographs, and a clinical examination accompanied by extraoral and intraoral photographs.
Clinical Examination
Medical and Dental History
“What is the patient's chief complaint?” This question is the basis of the anamnesis. At a minimum, the treatment plan should aim to address this important fundamental component of the patient's initial screening. The clinician is responsible for accurately understanding and addressing the chief complaint. Some patients will have very specific goals for treatment while others will provide more generalized expectations. Clear communication is the key to understanding a patient's objectives. With young patients, it is usually the parents who voice their complaint about the child's teeth. Commonly, the child is lacking in motivation or is too shy to express himself or herself. The parents' concerns should be a major consideration but the child should also be involved through a set of simple questions that will guide the clinician in discovering the child's motivation for treatment, if any.
The medical history gives pertinent information about the physical well-being of the patient. Numerous medical conditions can affect treatment in one way or another (Table 1-1).5 For example, a history of a cardiac malformation or anomaly may be an indication for premedication before certain orthodontic procedures.6 A history of rheumatoid arthritis can have direct implications on the temporomandibular joint (TMJ) and thus on the occlusion. A patient with hemophilia may opt for a nonextraction treatment approach. All of these conditions may affect the delivery of treatment in the various phases: pre-treatment, treatment, and post-treatment.
TABLE 1-1
Medical Conditions to be Considered in Orthodontic Treatment
| Medical Condition | Implications | Action |
| Allergies | Allergic reaction | Determine material causing allergy and substitute a nonallergic material |
| Asthma | Root resorption | Monitor every 6 months for evidence of EARR |
| Coagulation disorders | Bleeding risk | Avoid treatment plans involving extractions if possible |
| Diabetes | Periodontal disease | Monitor adequate control of diabetes. Manage with a periodontist |
| Epilepsy | Gingival hypertrophy (medications) | Monitor excellent plaque control. Manage with a periodontist for possible surgical intervention during treatment |
| Heart valve conditions | Endocarditis | Premedication when fitting bands |
| High blood pressure patient taking calcium channel blockers | Gingival hyperplasia secondary to medications | Monitor oral hygiene. Complement brushing with chlorhexidine |
| HIV | Periodontal disease, opportunistic infections | Consult with physician about patient's general condition. Monitor oral hygiene and periodontal status |
| Leukemia | Mucositis, oral infections | Remove appliances until remission (consult physician) |
| Osteoporosis | Bisphosphonate-related ONJ, delayed tooth movement | Determine formulation of medication and explain potential limited outcomes of treatment to patient |
| Physical or mental handicap | Gingivitis, relapse (muscle hyperactivity or hypoactivity) | Electric toothbrushes may aid in oral hygiene. Consider mechanics plan in which manual dexterity is not needed (noncompliance mechanics) |
| Rheumatoid arthritis | TMJ degeneration | Monitor TMJ. Manage with an oral surgeon if severe arthritic degeneration |
| Transplant patient | Gingival hyperplasia related to immunosuppressant drugs | Monitor oral hygiene. Consider chemical complement to brushing such as chlorhexidine |
| Xerostomia (primary or secondary) | Caries | Monitor for loose appliances. Consider fluoride rinses as an oral hygiene supplement |
EARR, External apical root resorption; HIV, human immunodeficiency virus; ONJ, osteonecrosis of the jaws; TMJ, temporomandibular joint.
Any metabolic disorder, such as diabetes, should be well-controlled before and during treatment, as healing is greatly hindered in uncontrolled types of diabetes.7
Another common medical condition of concern, especially in young patients, is asthma, not only because of the respiratory implications, but also because there is some evidence that patients with asthma who undergo orthodontic treatment have an increased incidence of root resorption.8
The above are some of the more common medical conditions, but it is important that all medical conditions be reviewed and further investigated (e.g., with a phone call to the patient's physician) if needed, as they may affect the treatment directly or indirectly. A more extensive review of these and other common medical disorders related to orthodontics can be found elsewhere.5
Another part of the medical history review specific to female patients is pregnancy. It is usually best to delay treatment until the pregnancy is over. The three basic reasons for postponing treatment are that radiographs usually are not recommended during pregnancy, there is an increased possibility of gingival hyperplasia due to hormonal influence, and in some instances the future mother's nutrition may be compromised as pain is elicited by tooth movement.
Other important information related to the medical history is the list of medications the patient may be taking and the existence of any allergies. Medications such as phenytoin (anticonvulsant), nifedipine (calcium channel blocker), and cyclosporine (immunosuppressive) need special attention, as they have the potential to cause a hyperplastic gingival response.9 Some medications may also influence the progress of orthodontic treatment. Among these are oral bisphosphonates, which are used to treat osteoporosis in perimenopausal women through inhibition of osteoclastic activity, thereby reducing bone resorption. Proper osteoclastic activity is necessary to ensure physiological tooth movement. Local administration of bisphosphonates has been shown to significantly delay tooth movement and space closure in rats.10,11 Studies have shown that patients taking bisphosphonates have increased treatment times, especially in extraction cases, and potentially compromised outcomes due to difficulty in achieving root parallelism and complete space closure.12 There is an increased risk of osteonecrosis of the jaws (ONJ) with bisphosphonates, specifically with an intravenous formulation. However, this risk is significantly lower in patients taking oral bisphosphonates.
Potential allergies to the alloys used in orthodontics should also be identified. Hypersensitivity to nickel has been reported with a prevalence of up to 28%.13 Allergies to other metals used in orthodontics, such as chromium and cobalt alloys, have also been reported.14 It is important to know the nature of the reaction to each allergen. Allergies related to the airway are also a significant finding, as they impair normal nasal breathing thus potentially affecting the growth and development of the jaws.15
The use of tobacco should also be ascertained from the medical history. It is not uncommon to encounter adolescent and adult patients who smoke. Smoking can have an adverse effect on the periodontal condition of patients,16 is a risk factor for periodontal disease, and has been shown to delay wound healing.17 Health providers also have an important duty to dissuade teenagers and adults from tobacco use.
With more adult patients seeking orthodontic treatment, it is critical to determine whether these patients are periodontally stable for fixed treatment. Fixed appliance therapy will likely aggravate an underlying peridontal problem due to poor oral hygiene and activation of bone remodelling.18 The orthodontist should take the necessary steps to minimize deleterious effects and also set realistic expectations for these patients. A full mouth series should be evaluated prior to the start of treatment and a focused clinical exam should be done to determine the periodontal status. Collaboration with a periodontist may be necessary to determine whether the patient is periodontally healthy for orthodontic treatment. If the patient has periodontitis, further periodontal therapy is indicated, which may involve a combination of therapies of scaling and root planing or open flap debridement depending on the severity of the disease.19 It may also be indicated to increase the frequency of prophylaxis and monitoring by a general dentist or periodontist during fixed appliance treatment to ensure that the periodontal status remains stable.
Growth and Development
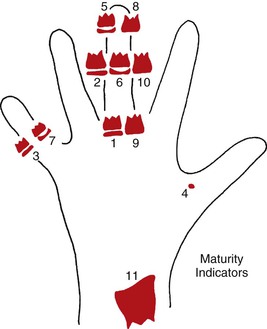
A specific section in the medical and dental interview should be dedicated to growth and development information. Most pediatricians keep a growth record of every child from birth (Fig. 1-3). A growth chart classifies the child under a height and weight percentile for comparison to the established norms for gender and chronological age. More importantly, the growth chart highlights any accelerations or peaks of growth that may have occurred. With this information, the objective is to evaluate the skeletal maturational level of the patient. The underlying rationale for this information is to properly time orthodontic treatment to the period that would be most efficient and effective.20 This implies that treatment will rely not only on tooth movement, but also on modifying growth to achieve a wider range of movement, thereby correcting larger dentofacial discrepancies.
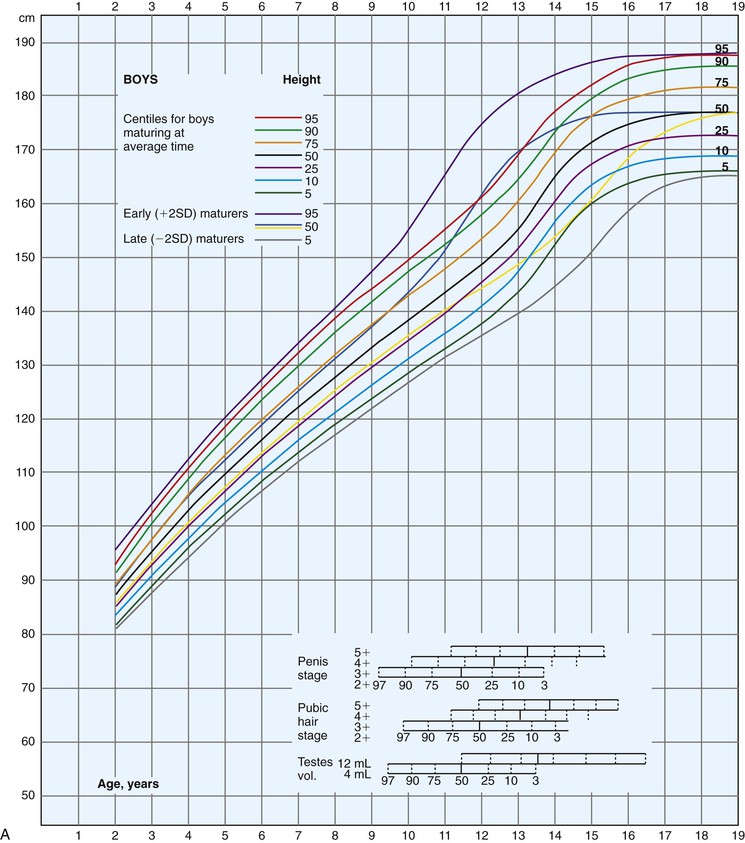
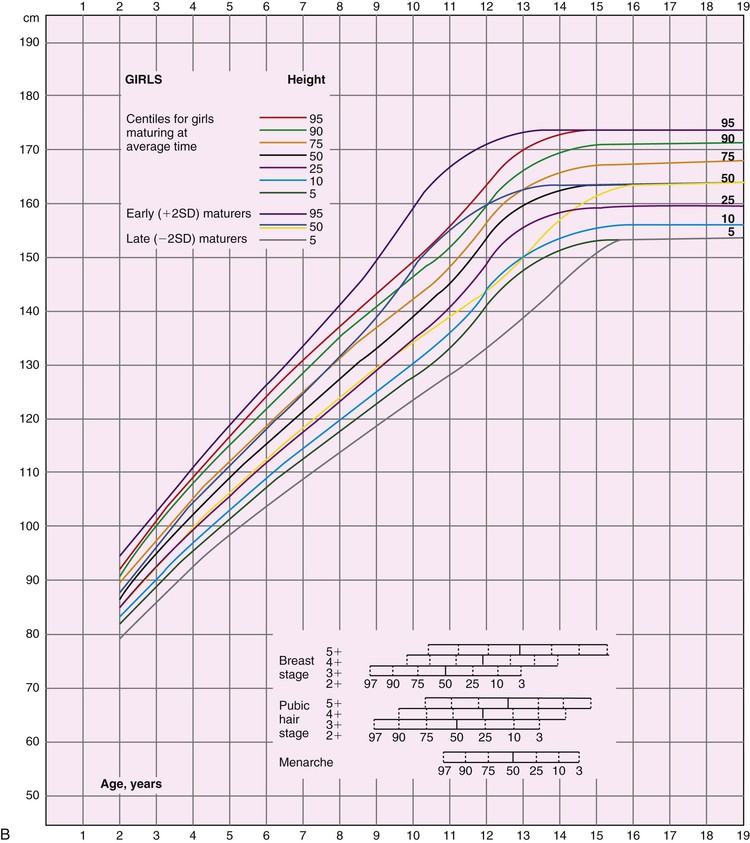
Figure 1-3 Growth curves for (A) boys and (B) girls (height and weight). SD, Standard deviation. (Modified from Tanner JM, Davies PS. Clinical longitudinal standards for height and height velocity for North American children. J Pediatr. 1985;107:317–329.)
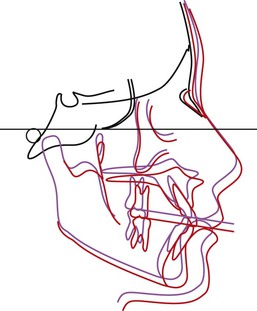
The pubertal growth spurt is associated with a differential maxillomandibular growth that involves a more anterior positioning of the mandible (Fig. 1-4). The timing of this spurt has been of interest to orthodontists. During this period the orthodontist should be able to influence growth of the mandible and the midface by mechanically affecting the environment. Experiments in animal models have shown the possibility of mandibular growth enhancement during this period.21 Unfortunately, there is no clear evidence that this additional mandibular growth enhancement is predictably achievable in humans.22 Although clinical studies have shown impressive results at the occlusal level, the results may be the sum of a combination of small orthopedic and dental movements.23,24 Some of the orthopedic movements involve remodeling within the temporal bone that is difficult to quantify with traditional research methods.25
Chronological age, dental development, and eruption sequence are not good indicators of skeletal maturity. Biological indicators, such as menarche (females), voice change (males), hand-wrist ossification sequence, metacarpal ossification sequence, cervical vertebrae morphology, and statural growth curves, have been used to evaluate general skeletal craniofacial maturity.20,26–28 Studies have shown a close correlation between peak height velocity and maximum acceleration in growth in the maxilla and mandible.21,26,28,29
Currently, there are no methods that can accurately predict the extent of craniofacial growth that a patient will ultimately achieve. This predictive inability becomes a problem in young patients with significant maxillomandibular discrepancies. For these patients a decision between a surgical approach or a growth modification approach is not simple. Moreover, these treatment strategies (surgery and growth modification) differ in timing, objectives, and often the direction of tooth movement. Some studies suggest that weak correlations can be drawn between final craniofacial form of growing children and their parents and other siblings.30,31
Although the absolute amount of growth cannot be predicted accurately, the direction of growth is more predictable. It has been shown that facial patterns are maintained.32,33 Skieller et al. also published findings related to the morphology of the mandible in the prediction of growth patterns.34 Some controversy relates to their findings, as their sample was made up of individuals with extreme patterns of vertical growth. Therefore the applicability of these predictive methods to individuals with less severe aberrations in their growth pattern might be limited.35
Finally, information regarding the timing of active growth cessation is important for young patients needing maxillofacial surgery. Radiographic films can be used to evaluate this feature. Use of cervical maturation indicators and hand-wrist films can provide further information on the stage of the patient's growth and is discussed later in the chapter. The best method to confirm that no further growth will occur in the craniofacial region is to take two sequential lateral head films with a 6- to 12-month interval; the superimposition of these radiographs should reveal no bony changes.36
Factors Influencing Craniofacial Growth
It is well known that many conditions affect the growth and development of the craniofacial complex. Knowing the etiology of the malocclusion is of prime importance for the diagnosis and eventual success of treatment. The etiology of the malocclusion is often multifactorial. In general, the etiologic factors can be categorized into genetic factors, environmental factors, or a combination of the two. Genetic information can be gathered from the interview with the guardian of the child patient or from the adult patient. This information is more important in patients where syndromes or extensive craniofacial deviations are present. Also, as mentioned, the parents' information may give some insight into the craniofacial form at the end of growth. The genetic component is also of further importance as it relates to abnormalities of tooth development and morphology, such as canine impaction, congenitally missing teeth, and abnormalities in tooth shape.37,38
Numerous environmental factors have been attributed to the etiology of malocclusions. The classic example is the habit of thumb-sucking. A long-term applied force (pressure) has been shown to affect skeletal hard tissues. The tissues of the musculature can apply constant low forces and result in adaption of the adjacent bony structures.39 Muscular dysfunction by either hyperactivity or hypoactivity in certain disease processes also may affect the normal growth and development of the jaws.40 If the forces exerted by the muscles are not in equilibrium, the net effect will be reflected in the hard tissues in the form of displacement and eventually conditions leading to malocclusion and maxillomandibular skeletal discrepancy.41,42
Frontal View
Traditionally, orthodontists have paid little attention to facial analysis from the frontal view and instead have focused mostly on anteroposterior changes (i.e., Angle classification). With the surge in three-dimensional (3D) imaging technology more information from the frontal view, especially relating to the soft tissue analysis, will be available in the future.43
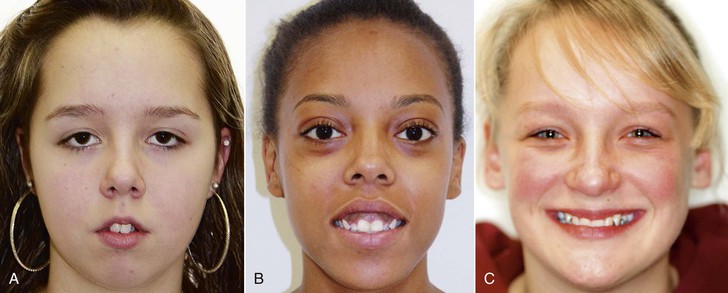
When describing a patient from the frontal view, an overall assessment of the patient's symmetry is made. Attractiveness and pleasing facial esthetics have been linked to certain proportions and symmetry.44,45 Minor asymmetries exist in all patients, even those who are visibly symmetrical, likely due to skeletal and soft tissue compensations during growth (Fig. 1-5).

Figure 1-5 Cone beam computed tomography (CBCT) images from normal, Class I adolescent patients. Minor skeletal asymmetries are evident in these patients when examined in 3D.
Ideal facial proportions have been described since ancient times by Roman and Greek artists. Horizontal as well as vertical lines are used as reference planes to evaluate these proportions. The horizontal planes, such as the interpupillary, interauricular, alar base, and occlusal planes, should be parallel to each other and special attention should be paid to the presence of cants (Fig. 1-6). The proportions between these horizontal planes can also be evaluated on the profile view. From the frontal view the vertical reference lines are more important since it is only from this view that the transverse dimension can be evaluated (Fig. 1-7).

Figure 1-6 Maxillary cant evidenced at smile. More gingival display is appreciated in the upper right buccal segment than in the left buccal segment.
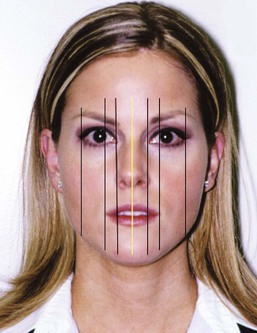
Figure 1-7 Vertical reference lines used to evaluate symmetry. The face is divided into six portions in the transverse analysis. The yellow line is an estimate of the facial midline.
Midline
The frontal view is also helpful in the evaluation of the relationship between the facial and dental midlines. It is important to note that analysis of the facial midline can be difficult, especially in patients with deviated nasal septums (Fig. 1-8, A). Thus the commonly used technique of placing a piece of dental floss vertically through the facial midline to relate it to the dental midline can be deceiving. A better method is to assess the relationship between the Cupid's bow and the dental midline (Fig. 1-8, B).46 Hence the dental midline can be related to an adjacent well-defined midsagittal anatomic structure. A more detailed analysis of the dental midline is included below since many other factors must be considered.
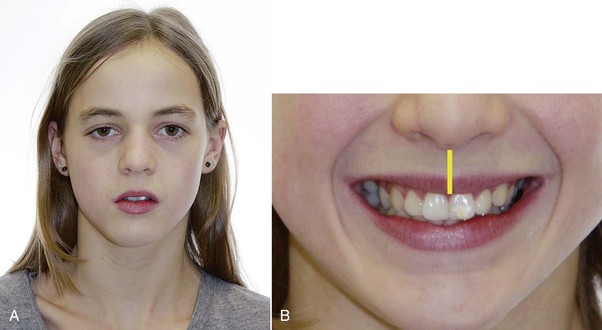
Figure 1-8 A, Patient exhibiting facial asymmetry, including a deviating chin and vertical discrepancy in the eyes. B, Same patient showing a coincident dental midline in relation to the philtrum.
Finally, the chin is evaluated for any deviation in relation to the facial midline (Fig. 1-9, A). A view taken from above the patient (coronal) enhances the ability to detect any deviations (Fig. 1-9, B). Similarly, observing the patient from the lower (ventral) aspect of the mandible can complement this analysis (Fig. 1-9, C). This part of the clinical examination is very important, as a large chin deviation is an indication for further analysis, perhaps with additional radiographic imaging.
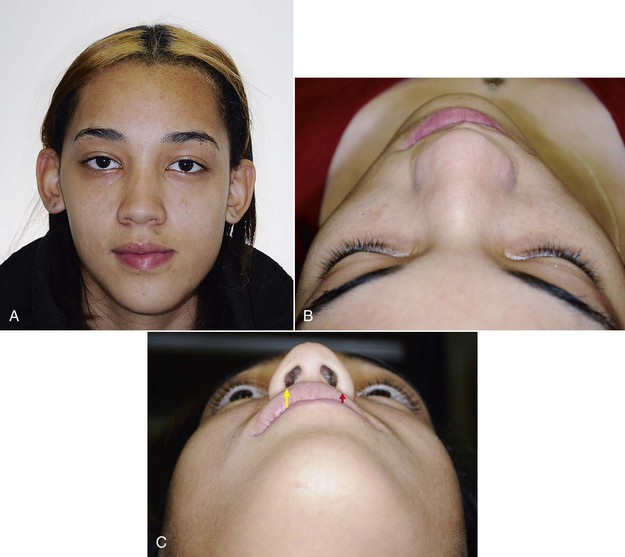
Figure 1-9 A, Patient with asymmetrical mandible. B, Coronal view to evaluate mandibular asymmetry during the clinical examination. C, Ventral view complements the assessment for mandibular asymmetry. In this patient the ventral view provides better information about the asymmetry. Arrows show the asymmetry between the left and right sides in the lip region.
Lips
A good analysis of the patient's lips is done at rest position or with the upper and lower lips lightly touching (Fig. 1-10, A). Indications of any muscle strain on lip closure should be noted (Fig. 1-10, B). Upper and lower lip lengths can be assessed in the frontal and profile views. Upper lip length when noted alone is not as important per se as its relationship to the upper incisors at rest and when smiling. The proper relationship between the upper lip and the amount of upper teeth exposure is a key factor in modern esthetic smile construction (Fig. 1-11). Full display of the upper incisor crown upon smiling has been linked to youthful smiles.47 A differential diagnosis between a short or long lip and a maxillary vertical excess or deficiency is valuable in patients with an inadequate upper incisor display (Fig. 1-12).

Figure 1-10 A, Patient showing incompetent lips at rest. B, Upon lip contact the mentalis strain is noted.
Buccal Corridors and Smile Line
Other important relationships that can be evaluated only in the frontal view are the buccal corridors and the curvature of the smile line (relationship to lower lips). The buccal corridors and smile line concepts have been discussed extensively in the prosthetic literature.48 The ideal esthetic parameter in smile design in the transverse dimension has been related to wide dental arches and narrow buccal corridors (Fig. 1-13). Some authors have described upper first molar display on a full smile as a feature of an attractive smile.49 Although this does seem to be an attribute of beautiful smiles, its validity and applicability is doubtful. Anatomic structures limit the amount of transverse expansion needed to reduce the unattractive wide buccal corridors. The long-term periodontal health of teeth with expansion is not well understood. Computed tomography (CT) scans have shown that indiscriminate expansion of the maxillary arch results in buccal root dehiscences as these extend beyond the cortical plates.50 Another important reason to avoid indiscriminate expansion relates to long-term stability.51 Skeletal tissues (bones and teeth) are usually in equilibrium with the surrounding musculature; long-term stability might be compromised when teeth invade the neighboring muscle confinements.41,42

Figure 1-13 Esthetically pleasing smile. Patient exhibits the upper first molars with narrow buccal corridors and wide dental arches.
Another concept that has been related to esthetic smiles is the parallelism of the curve of the upper anterior teeth to the lower lip curvature on smiling (Fig. 1-14). Although this does seem to be an ideal objective, it should be noted that there are different types of smiles and the lower lip posture varies accordingly.52 Moreover, this smile arc is a result of the occlusal plane inclination and second-order crown angulations in the upper anterior teeth.53 Thus there are some limitations to achieving this ideal smile arc in every patient. A reasonable objective is to prevent a flat or reverse smile line (Fig. 1-15, A) and to obtain some degree of curvature that resembles the one found in the lower lip (Fig. 1-15, B).
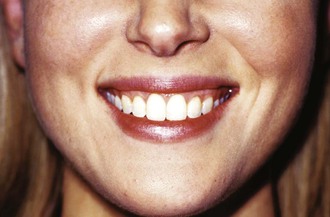
Figure 1-14 Ideal parallelism between the incisal edges of the upper anterior teeth and the lower lip. The contact between the incisors and the lip is very slight.

Figure 1-15 A, Reverse relationship between the upper incisors and the lower lips, which is frequently found in patients with a finger habit. B, Correction of the reverse relationship after treatment. A better esthetic relationship to the lower lip was achieved.
Symmetry has always been linked to beauty. Not surprisingly, it has also been ascribed as one of the characteristics of a beautiful smile. This symmetry can be related to the size and shape of the teeth on both sides of each arch (see Fig. 1-11, A). Also, it is related to the relationship of the intraoral tissues to the lips on both the right and left sides. Therefore the same amount of gingival display should be seen upon smiling, on both sides of the arch. Reasons for any asymmetry include a cant in the maxillary skeletal base, different amounts of tooth eruption on the right and left sides, or asymmetrical smiles. It is estimated that 8.7% of normal adults have asymmetrical smiles (Fig. 1-16).54

Figure 1-16 Asymmetrical smile with more tooth structure display on the right side. A reverse smile curve is also evident.
The last feature related to symmetry in the smile is the dental midline. The ideal relationship of the dental midline to the facial midline was mentioned above. The upper dental midline has been considered more important than the lower dental midline in esthetic smile design. It has been shown that a discrepancy of <2 mm (to the right or left) between the upper dental midline and the facial midline is not readily perceived (Fig. 1-17, A).55,56 However, any type of unparallel relationship between the interproximal contacts of the incisors related to the facial midline (incisal cant) is more easily perceived (Fig. 1-17, B).57 Two further characteristics of an attractive smile are the gingival heights of the anterior teeth and the tooth shade. The gingival heights of the six upper anterior teeth are similar. The central incisors and the canines are at the same level, while the lateral incisors' free gingival level is approximately 0.5 mm incisal to the level of the canines and central incisors (Fig. 1-18). Moreover, the gingival heights of the premolars and molars should be approximately 1 and 1.5 mm less than the canines, respectively (Fig. 1-19).58 The significance of tooth shade in the esthetic smile has been reviewed extensively in the prosthodontic literature.49 Light shades have always been considered one of the most important characteristics of an esthetic smile. Therefore procedures such as tooth bleaching may be considered after orthodontic appliance removal. Tooth shade also becomes an important factor in patients where canine substitution for missing upper laterals is considered. Differences in the tone between the canines (dark yellow) and incisors may be an indication to opt to restore the laterals prosthetically instead of closing the edentulous space (canine substitution).
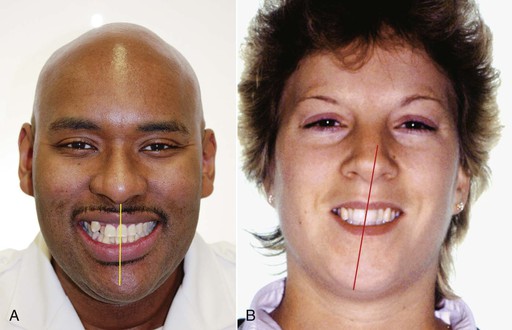
Figure 1-17 A, Patient with upper midline deviated approximately 2 mm to the right of the facial midline. B, Patient with upper midline deviated approximately 1 mm from the facial midline. The inclination of the line described by the interproximal contact area accentuates the midline discrepancy.

Figure 1-18 Proper gingival heights. The upper central incisors and canines have the same gingival height; the lateral incisors' gingiva is 1 mm below the canines and central incisors.
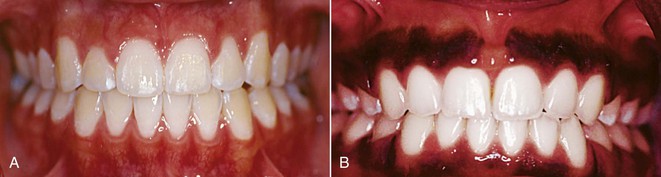
Figure 1-19 A, Gingival heights from the canines to the molars decrease gradually. B, Abrupt change in gingival heights between the canine and the second premolar. This situation is commonly seen in upper first premolar extraction.
The last notable factor in the ideal smile is tooth shape. Incisors are the predominant teeth in the smile, especially the upper central incisor. The ideal proportion of this tooth is found when the width approximates 75% to 80% of the height (Fig. 1-20).59 Similarly, lateral incisor size is often small in the mesiodistal dimension and should be considered in determining final occlusion and overall treatment outcome. Tooth shape is discussed further later in the chapter.
Profile View
Orthodontists spend more time evaluating patients from the profile view. Most of the literature is based on analysis from lateral cephalometric films. The classification of malocclusions is also based on the anteroposterior dimension (i.e., Angle classification). Even though the vertical dimension can be analyzed from this view, interest in this dimension has lagged. Later chapters describe the importance of the vertical dimension in the treatment of various malocclusions by an application of sound biomechanical principles.
Anteroposterior Dimension
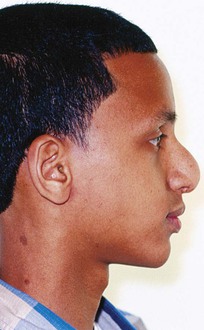
The anteroposterior dimension is the backbone of most contemporary orthodontic analyses. In this dimension the soft tissue convexity is initially assessed by observing the spatial relationship between the forehead, maxilla, and mandible. These are separate but interrelated anatomic structures with independent timings in development. Each structure provides feedback to the others to maintain a normal facial growth pattern.60 Normally these three structures maintain a slight convexity that is reduced during puberty as a result of differential jaw growth.33 During the pubertal growth spurt the mandible has a greater anterior displacement compared to the maxilla. It is important to note that at the end of growth there are also gender differences in the convexity of the profiles. On average the female profile is more convex due to a smaller chin projection.61
Once the magnitude of the facial profile convexity is assessed, the next step is to evaluate which of the three structures is contributing to the abnormality. With an increased angle of convexity or concavity, the question to be answered is which structure is causing the deformity (mandible or maxilla). It has been reported that the majority of skeletal convexities exhibit a deficient mandible.62 On the other hand, studies show that approximately half of skeletal concavities present with a deficient maxilla.63
To evaluate maxillary and mandibular position during the clinical examination, an adequate reference plane must be determined. During the clinical examination the easiest assessment can be done using the natural head position. This can be achieved when the extraoral photographs are taken. More detailed analysis of the soft tissue spatial relationships in the anteroposterior dimensions is obtained from the lateral cephalograms.
Nose
Although the nose is outside the limits of what can be affected by orthodontic treatment, it is important for facial balance. More importantly, the apparent nose projection can be affected by the anteroposterior position of the lips. During the clinical examination, the length and height of the nose are evaluated. Any morphological variations in shape are noted (Fig. 1-21).
Lips
Lip response to orthodontic treatment is one of the most discussed topics in modern orthodontics. With the increased interest in esthetics, patients and practitioners are interested in not only the dental and skeletal changes, but also the response of the surrounding soft tissues to treatment. As teeth move, there is a direct effect on lip support. Although this is a subject of perpetual research, no good predictor of the precise lip response to orthodontic movement has been identified.64 The only predictable variable is the direction of lip response. It has been established that if any lip changes occur, these will be in the direction of the upper anterior tooth movement.65,66
During clinical examination an overall assessment of the lips at rest is necessary. Special attention should be given to lip posture and tonicity. The influence of lip pressure in the etiology of certain types of malocclusions has been discussed in the literature.67 To evaluate lip posture, the anteroposterior and vertical relationship of the lips (rest position) to the incisors is examined (Fig. 1-22).68 In the anteroposterior dimension, a gap between the labial surface of the anterior teeth and the oral mucosa may be absent or present. In the vertical dimension, the lip line may be high (middle of the incisor root) or low. If the lips and the incisors contact each other, the exact location (incisal, middle, or apical third) of this junction is noted. The vertical and anteroposterior relationship of the lips to the incisors can aid in the prediction of upper lip movement in response to lingual incisor movement and the long-term stability of the incisors to labial movement as well.69
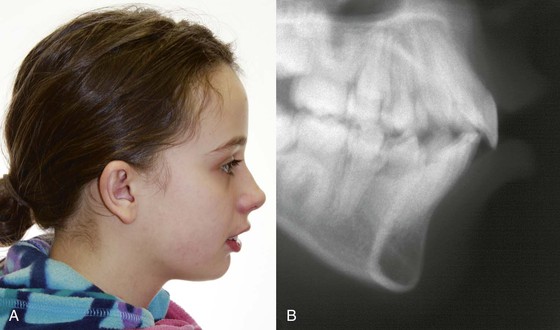
Figure 1-22 A, Patient with no contact between the crown of the upper incisors and the upper lip. The upper lip is not supported by the crowns of the upper central incisors. The effect on the upper lip after lingual tipping of the incisors would depend on the amount of movement of the coronal portion of the root. B, Lateral cephalometric film showing the vertical and anteroposterior relationship of the lip to the incisors. Intimate contact is noticed with the alveolar process of the anterior teeth in the maxilla.
The relationship between the upper and lower lips is another important feature that must be evaluated. When the lips are at rest, the normal interlabial gap ranges from 1- to 3-mm. As the patient closes their lips, any strain on the perioral musculature, such as mentalis strain, may be indicative of an excessive interlabial gap. Another very important dimension to note is the amount of incisor display with the lips maintained at this rest position.
An excessive display of tooth or gum tissue may be the result of a single factor or a combination of factors, such as vertical maxillary excess, short upper lip, or supra-erupted upper incisors. From the profile view, a general indication of a short upper lip is evident when an obtuse angle is found between a line drawn from the commissure of the mouth to the labrale superioris and the horizontal reference plane (Fig. 1-23). In general, the lower lip is almost parallel to the horizontal plane; therefore these patients will present with an excessive interlabial gap.
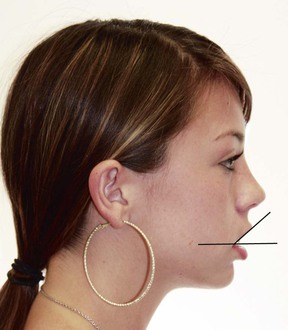
Figure 1-23 Large interlabial gap. There is a large angle between the horizontal plane and a line from the angle of the mouth to the labrale superioris.
Another important feature is lip thickness. It is well-known that lip thickness varies between different races.70–72 Moreover, the response to orthodontic tooth movement may be different between thin and thick lips. Some evidence suggests that thicker lips respond less and more variably to tooth movement than thinner lips (Fig. 1-24).73

Figure 1-24 A, Patient with very thick lips. The response to incisor movement may be limited by the tissue mass. B, Patient with very thin lips that may be more susceptible to lip changes with tooth movement.
The ideal anteroposterior position of the lips has been estimated by many studies using different reference lines. The definition of protrusive or retrusive lips varies with age, gender, and race. To define lip protrusion, different reference planes have been used. One of the most common reference planes used in clinical orthodontics is the E-line defined by Ricketts formed by a line passing from the tip of the nose to soft tissue pogonion (Pg').74 The limitation of this reference line is that it is influenced by the anteroposterior position of the chin and nose. Any large deviation in the chin or nose position relative to the norm will give a false impression of lip position. To control for the nose variability, Burstone proposed the Sn–Pg' line extending from subnasale (Sn) to Pg' (Fig. 1-25).75,76 Others have used different angles using the chin and lips as reference points and not incorporating the nose (Z angle, Steiner's S-line, and Holdaway angle).77–79

Figure 1-25 Relationship of the lips to two commonly used reference lines: E-line (influenced by the nose, red) and Sn–Pg' line (yellow).
The nasolabial angle is another important measurement related to lip protrusion. Although this angle is also influenced by the angulation of the nose (upturn or downturn of the nasal tip), it gives an indication of the upper lip inclination (Fig. 1-26).

Figure 1-26 Obtuse nasolabial angle. The upturned nasal tip and retrusive lip contribute to the obtuse angle.
Although numerically the soft tissue analysis can be better analyzed in a lateral cephalometric film, a general overview is achieved during the clinical examination. Using a combination of all these reference planes allows for a proper interpretation of the lip position.
Another important structure that is analyzed in the lateral view is chin projection. In adult patients, the ratio of the chin-to-throat depth length compared to the lower facial height is 1.2 : 1.80 It seems that not only the length of this line but also the angulation to the true horizontal plane are important features in well-balanced faces. Normally, a parallel relation or slightly negative angle (throat point above the menton) is found in esthetically pleasing faces (Fig. 1-27, A). A deficient chin shows a reduction in the chin-to-throat depth length (Fig. 1-27, B).
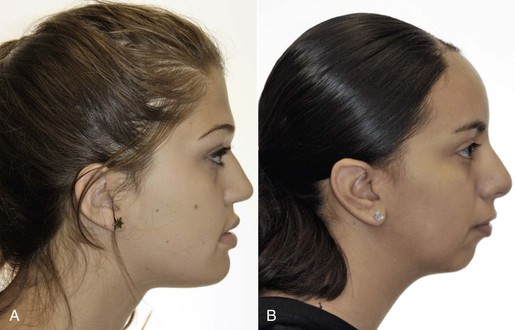
Figure 1-27 A, Parallel relationship of the chin–throat line to the horizontal plane. An adequate ratio between the lower facial height and throat depth is 1.2 : 1. B, Inadequate ratio between the lower facial height and throat depth (no throat depth) gives an unesthetic inclination of the chin–throat line.
Vertical Dimension
As stated above, the vertical dimension can be analyzed in both the frontal and the profile views. Both of these views can be related through the vertical dimension to provide a composite 3D analysis. The face can be divided into three equal thirds: upper, middle, and lower facial heights. The true upper facial height is seldom used, as it is measured from the trichion to the glabella. More commonly, the middle facial height is referred to as the upper facial height. The normal upper to lower facial height ratio is 1 : 1 (glabella [G] to subnasale [Sn] and Sn to soft tissue menton [Me']) (Fig. 1-28, A).

Figure 1-28 A, Facial heights divided into three equal thirds: trichion–glabella, glabella–subnasale, subnasale–menton. B, Lower facial height is further divided into unequal thirds: subnasale–stomion (one-third), stomiom–menton (two-thirds).
The lower facial third is very important since the effects of orthodontic treatment are most profound in this third. It is further subdivided into two proportional heights. One third of the lower facial height normally corresponds to Sn to St and two thirds from St to Me' (Fig. 1-28, B).
The vertical analysis is not limited to the anterior part of the face but also includes the posterior. The ratio between these two determines, to a degree, the steepness of the mandibular plane. The normal ratio of the lower facial height to the posterior facial height is 0.69.81 An overall assessment of this relationship can be determined from the mandibular plane. Palpating and placing a flat object along the lower border of the mandible can give a general idea of the steepness of this plane.
In the vertical dimension from the profile view the face is generally categorized as convergent (short face) or divergent (long face). A short face is characterized by a flat mandibular plane angle with a similar posterior and anterior facial height, lip redundancy with a deep mentolabial sulcus, and short lower facial height (Fig. 1-29, A). At the other end of the spectrum, a long face is characterized by an increased anterior facial height relative to the posterior facial height, steep mandibular plane angle, possible lip incompetence with large interlabial gap, and shallow mentolabial sulcus (Fig. 1-29, B).

Figure 1-29 A, Short face (brachycephalic or euryprosopic). B, Long face (dolichocephalic or leptoprosopic).
Most of the clinical analysis is static in nature; therefore during the examination it is important to pay close attention to the animation of the facial soft tissues. During this time an analysis of more natural lip function, including different smile heights, symmetry of the smile, and the amount of upper and lower incisor display during conversation, is more important than forced unnatural snapshots of animated features.
Photographs
Extraoral Photographs
Although the clinical examination provides an excellent opportunity for patient evaluation, it is important to document specific information (images, intraoral impressions). This information can be used later for data analysis (radiographs, photographs, and models), medicolegal reasons, and treatment progress and outcome evaluations.
Different photographic images from the profile and frontal views are recommended. Initially pictures of the patient with relaxed lips and lips lightly touching each other are taken from the frontal and profile views (Fig. 1-30, A–D). Frontal and profile view pictures are taken in the natural head position.
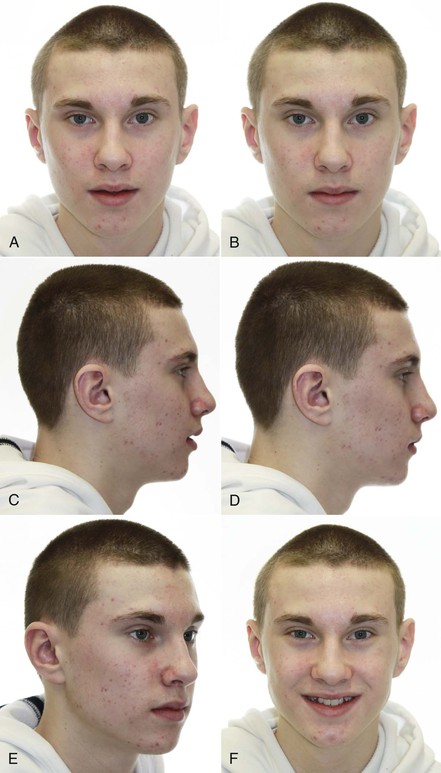
Figure 1-30 Extraoral photographs for the records. Frontal view (A) with lips at rest and (B) with lips lightly touching each other. Profile view (C) with lips at rest and (D) with lips lightly touching each other. E, Forty-five degree–angle photograph. Assessment of the cheek projection and mandibular plane angle is obtained from this view. F, Frontal view smiling photograph.
A 45 degree–angle image between the profile and frontal views provides information related to the amount of malar prominence and lower jaw shape (mandibular plane angle and gonial angle). This view usually confirms the findings of the analysis from the frontal and profile views (Fig. 1-30, E).
Finally, a frontal view photograph depicting a full smile should be taken. It is somewhat difficult to capture a natural, unposed smile. Usually this photograph does not reflect the full extent of the smile. Thus special attention is needed during the clinical examination to record important data such as the amount of tooth and gum display, the relationship of the upper teeth to the lower lip, and the width of buccal corridors (Fig. 1-30, F). During data analysis this information can be correlated to the still images. As an alternative, a video image of the different animated facial features has recently been suggested as part of the clinical record.82
Intraoral Photographs
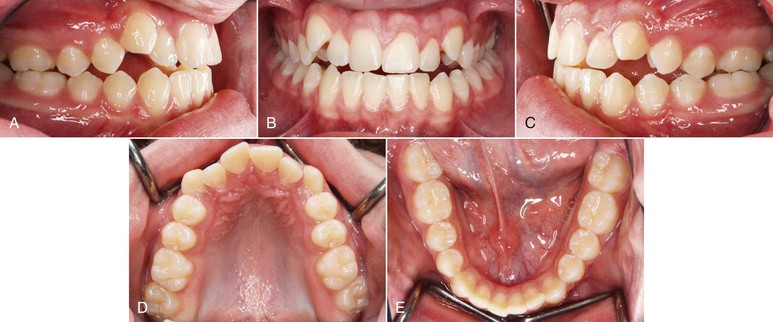
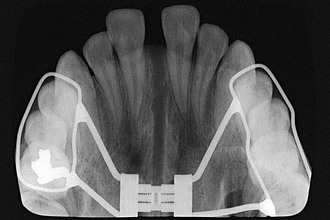
A total of five views of the dentition and the occlusion are taken. These pictures include two buccal photos (left and right), two occlusal photos (upper and lower arch), and one frontal intraoral view. These photographs should be taken in maximum intercuspation (Fig. 1-31). Additionally, intraoral centric relation photographs are taken if a significant centric relation–centric occlusion (CR–CO) shift is present (mandibular shift).
Intraoral Examination
The intraoral examination for an orthodontic patient starts as does any other dental examination. First, an overall inspection of the oral mucosa in search of any pathological lesions is performed. Upon analyzing the soft tissue, special attention should be given to the gingival tissues. Periodontal status evaluation is of prime importance, especially in the adult, as discussed earlier in the chapter. It is not uncommon to find active periodontal disease in adults around the molar areas. A random probing should be done around the first and second molars and on some anterior teeth for every adult patient.
The quality of the attached gingiva is examined next. The thickness (gingivo-occlusal) and width of the attached gingiva are very important. Many times these are overlooked and recession may occur as the teeth are displaced labially out of their alveolar housing. It should be noted that recession also may be present before starting treatment (Fig. 1-32).

Figure 1-32 A, Preoperative photograph of the lower incisor gingival attachment. Incipient recession with a thin band of attached gingiva is seen. B, Postoperative photograph shows no attached gingiva in the lower right central incisor and slight progression of gingival recession. Grafting of this area is indicated.
Continuing with the intraoral soft tissue analysis, the labial frenum attachment is evaluated. A high insertion into the attached gingiva might contribute to a persisting diastema (Fig. 1-33).83 Moreover, high frenum attachments have also been linked to recession of the labial surface of the lower incisors.84

Figure 1-33 A, Thick band of labial frenum possibly contributing to the diastema. B, Diastema closure post-treatment with frenectomy complete. C, A bonded lingual retainer was placed between the incisors.
Oral Hygiene
Good oral hygiene is very important during orthodontic treatment and should be stressed from the start of treatment. It is well-established that orthodontic appliances hinder oral hygiene. Therefore careful evaluation of oral hygiene at the initial examination is needed and treatment should be delayed until good plaque control is achieved by the patient.
Tongue
Initially, the mucosa of the tongue should be screened for any signs of pathological lesions. A general evaluation of the shape and size of the tongue is performed and the tongue's relation to the lower dental arch should be noted. Evidence of indentations on the lateral borders of the tongue accompanied by generalized spacing between the teeth may suggest macroglossia.
The tongue is a powerful muscle that applies constant pressure to the lingual surfaces of the teeth, counteracting the lip pressure on the buccal surfaces.37 Functional evaluation of the tongue during speech and swallowing could give some insight as to etiology of the malocclusion.
Finally, the lingual frenum is evaluated. Ankyloglossia or tongue-tie is found in some patients and may be a reason for impeded speech.85
Dentition
Before starting the dental examination, a thorough dental history should be taken. First, the patient is asked if he or she is under regular dental care. Although an affirmative answer does not mean that there is no active disease, it can be assumed that the patient or guardian has an interest in maintaining good oral health. A patient's oral hygiene habits (brushing frequency, use of floss, etc.) should be noted.
History of previous orthodontic treatment is also important. It might provide some insight into a patient's expectations, as well as relapse tendencies and sequelae (e.g., root resorption, decalcified lesions) after treatment. Additionally, the information can enable anticipation of complications that may have occurred with previous orthodontic therapy.
Within the dental history, the patient is questioned about previous trauma to the jaws or teeth. A history of trauma to the jaws may explain asymmetries, abnormal growth, or in some cases, TMJ symptoms. A history of trauma and the nature of the trauma (avulsion, luxation, fractures, etc.) to the teeth should be noted. Certain types of dentoalveolar trauma have been related to external root resorption and ankylosis.86 Orthodontic movement can be a precipitating factor to this resorption in severely traumatized teeth (Fig. 1-34).87

Figure 1-34 Radiograph of a patient with a history of severe trauma to the upper central incisor taken after orthodontic treatment. Note the calcification of the pulp chamber in the lateral incisor and the severe resorption of the root of the central incisor.
Finally, any history of deleterious habits, such as thumb- or digit-sucking or a tongue posturing habit, might explain, in part, the etiology of the malocclusion. With regard to a habit, it is important to find out if this is an active or past habit. In the case of an active habit, the frequency and time during the day when the habit is performed are noted.
The dental examination starts by counting the number of teeth. The specific aim is to inspect for any supernumerary or missing teeth. Primary teeth should be distinguished from permanent teeth and any tooth transpositions should be noted. The panoramic film is a useful aid for corroborating the clinical examination findings.
The size and shape of the teeth are critical for achieving an optimal esthetic outcome. Attention to morphological variation is especially important in the anterior segment. It is not unusual to find peg laterals, conical-shaped teeth, or other dental anomalies in this esthetic zone. Peg laterals are unsightly teeth that usually generate a Bolton tooth size discrepancy (Fig. 1-35). Subtle discrepancies in tooth size and shape are often noticed at the end of treatment when the occlusal and esthetic goals are not met. Therefore a careful evaluation of tooth size is needed from the beginning of treatment. Different restorative alternatives will dictate the specific distribution of spaces and positioning of the teeth to facilitate and enhance the restorative result.88
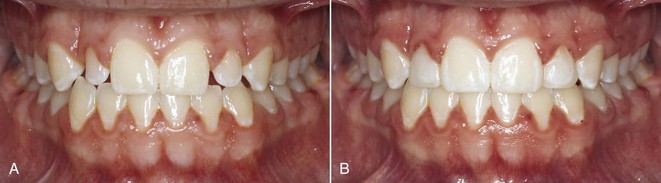
Figure 1-35 A, Morphology of the peg laterals creates wide unesthetic incisal embrasures. B, Restoration of these teeth is generally recommended in the last stages of treatment if composites are the selected restorative material.
Open gingival embrasures, also known as “black triangles,” are a common unesthetic finding in adults. These black spaces are closely related to tooth shape (Fig. 1-36) and are often a result of the papilla not filling the interproximal space. It has been shown that if the interproximal contact of two adjacent teeth is 5-mm or less from the crestal bone, a papilla will be present almost 100% of the time.89 Thus triangular shaped teeth will have a low incisal contact that increases the distance to the crestal bone, resulting in a black triangle. At the initial examination the clinician should be aware that crowding between the upper incisors can displace the contact gingivally; therefore as proper alignment is achieved in the initial phases of treatment, the contact may be displaced incisally, resulting in a black triangle (Fig. 1-37). The black triangle frequently found with the extraction of a lower incisor is often related to the bone recession that occurs after a tooth extraction (Fig. 1-38). Interproximal contact in the incisal third following lower incisor extraction also has been associated with these open gingival embrasures.90

Figure 1-36 A, “Black triangle” as a result of the shape of the incisors. Contact between the incisors was too low. B, Good proportions between maximum height and width present in the incisal edge. Composite material was added to the mesial surfaces to alter the mesiodistal width in the middle and gingival thirds of the crowns.

Figure 1-37 Abnormal morphology of the central and lateral incisors. The triangular shape can lead to “black triangles” interproximally once aligned.
Incisor crowns with a wider middle than incisal third also may result in excessive incisal embrasures (Fig. 1-39). Other abnormalities in tooth shape, such as irregularities in the borders of the incisors, may be related to a worn dentition or trauma to the incisors.

Figure 1-39 Abnormal morphology of the central incisors. The mesiodistal width is larger in the middle third compared to the incisal third, resulting in large incisal embrasures.
Tooth shape is related not only to the clinical crown but also to the root morphology and crown-to-root angulation. This is an important consideration in the straight-wire technique, as it is based on the coronal angulation to the occlusal plane in the three planes of space.91 An acute angle between the root and the crown with a prescribed bracket may position the root outside the cortical bone in the third order or displace the root against the tooth adjacent to it in the second order (Fig. 1-40).
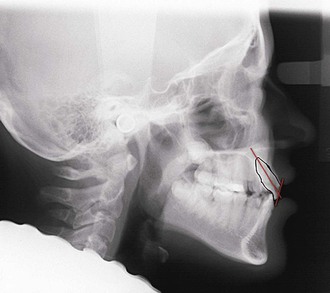
Figure 1-40 Acute crown–root angulation. Caution should be used during root correction of the incisors, as the lingual root portion may approximate the cortical plate of the palate.
Tooth shade is the final factor to be evaluated. It has been shown that patients prefer lighter shades. More importantly, any white or brown spots should be noted in the initial examination, to distinguish them from spots that can be caused by poor bacterial plaque control with fixed appliances.
The two most common dental diseases are caries and periodontal disease. Periodontal disease is more common in the adult population. Thus molars in all adult patients should be probed on all surfaces. Any additional probing will depend on the degree of periodontal involvement of the posterior teeth or will be based on the radiographic evidence obtained.
The deleterious effects of traumatic forces to teeth with periodontal disease have been well-reported (Fig. 1-41). Orthodontic forces have been shown to produce a similar breakdown effect on the tooth supporting structures in the presence of active periodontal disease. Therefore, as discussed earlier, prior to orthodontic treatment the clinician should ensure that no active disease is present and that suitable oral health conditions exist in the oral cavity.
Caries, the other common dental disease, is more prevalent in adolescents than in adults. Nevertheless, all patients should be screened for caries before and throughout orthodontic treatment. Any lesions present should be permanently restored and any pulpal involvement addressed before initiating treatment. It has been reported that infection within the confinement of the root canal can cause root resorption in response to an orthodontic force.87 In addition, teeth with previous root canal treatment should be inspected for a good-quality seal and no signs of periapical pathology. Referring the patient to a general or pediatric dentist for cleaning and checkup before appliance placement is also recommended.
It is common for adults to present with missing teeth and heavily restored dentitions (i.e., crowns, bridges, and extensive amalgam or composite buildups). These patients should be checked for ill-fitting bridges and crowns. A good analysis of the tooth structure supporting the bridges should be done in collaboration with the restorative dentist. A multidisciplinary approach is needed in these cases to carefully plan the orthodontic movement that will facilitate ideal subsequent crown and bridge work. Furthermore, it should be anticipated that appliance insertion in heavily restored dentition is complicated. Banding and bonding procedures in these patients are difficult due to irregular tooth shapes and variable surface characteristics of the restorative materials. Hence appliance breakage during treatment is more common.
For the majority of patients, orthodontics is an elective procedure. Periodontal disease and caries affect many individuals seeking orthodontic treatment. Both dental diseases should be under control before orthodontic treatment is started. It should be stressed again that close communication with the general dentist is of key importance.
Tooth Eruption
As mentioned, there is great variation in the timing of eruption of different teeth among individuals. Delayed eruption of teeth is not a problem per se. However, an abnormal eruption sequence has been considered one of the factors involved in the etiology of malocclusion.92 Other eruption disturbances, such as retained primary teeth, ankylosed teeth, and ectopic eruption, are important etiologic factors in malocclusion (Fig. 1-42). It has been reported that there is a correlation between the abnormal eruption sequence and direction, abnormal shape of teeth, and congenitally missing teeth.37
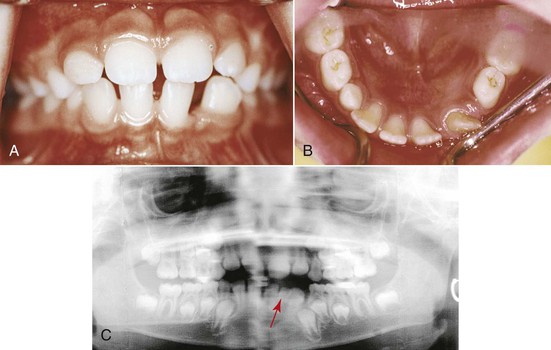
Figure 1-42 Ectopic eruption of lower left lateral incisor. A, Distal eruption of the lower lateral incisor exfoliated left primary canine instead of the lower lateral primary incisor. B, Space for the left permanent canine is greatly reduced. C, Panoramic radiograph shows that the primary left lateral incisor is still present (arrow) mesial to the lower left permanent lateral incisor. Eruption of the lower left permanent canine is hampered.
Dental Arches
During the intra-arch analysis, a general appreciation of the arch shape and an overall view of crowding or spacing are achieved. Intra-arch evaluation of the tooth relationships also includes marginal ridge discrepancies. Severe marginal ridge discrepancies between adjacent teeth may be indicative of ankylosis. This condition is most often found between the permanent first molars and the lower second primary molars (Fig. 1-43).

Figure 1-43 Thirteen-year-old patient with the lower right second primary molar submerged below the occlusal plane. This clinical finding is highly suggestive of ankylosis of this primary tooth.
A more thorough evaluation of the intra-arch and inter-arch relationships can be achieved with the model analysis. Crowding, spacing, and problems with the angulations and orientation of teeth in the three dimensions of space can be analyzed more precisely in study models. Moreover, these models provide the unique possibility of analyzing the occlusion from the lingual aspect.
Extraoral Examination
Functional Analysis
One of the reasons that patients seek or are referred for orthodontic care is to achieve proper occlusal function. Therefore the orthodontist must have a good understanding of the critical concepts in occlusion and how they relate to other structures such as the TMJ.
Much has been discussed about which type of occlusion provides the best function.93 In general, it is accepted that ideal occlusal function relates to a mutually protected occlusion.93,94 This means that the posterior teeth protect the anterior teeth in maximum intercuspation by receiving the majority of the occlusal load and the anterior teeth protect the posterior teeth in the excursive movements. In lateral excursions, most clinicians agree that canine guidance is the ideal occlusal scheme. Yet group function on lateral movements can also be an acceptable occlusal scheme. Overall, balancing occlusal contacts is considered deleterious for occlusal function.
A good analysis of the different excursive movements is necessary in the initial clinical examination. The different excursive movements to be analyzed are anterior protrusive, lateral, and lateral protrusive movements. As mentioned above, any contacts between the posterior teeth during the anterior protrusive movement should be noted. In the lateral movements, attention should be given to any posterior contacts on the working side but most importantly on the balancing side. No anterior contacts should be present in lateral excursions. During all of these excursive movements, close attention should be paid to wear facets and how these relate interocclusally in the different end movements.
Temporomandibular Disorders
Temporomandibular disorders (TMD) encompass certain conditions in and around the TMJ. These disorders have been subdivided into internal derangements (within the articulation) and myofascial pain dysfunction (masticatory and cervical muscles).95 Internal derangements are classified according to the relationship of the articular disc to the condyle during jaw opening. Four distinct stages of condyle–disc relationships have been found that denote progressive degeneration. The first stage starts with initial incoordination between the condyle and the disc during opening. The second and third stages are characterized by anterior displacement of the disc, which is not recaptured in the third stage. The fourth stage involves damage to the retrodiscal tissue.
The four major characteristics of myofascial pain dysfunction (MPD) are pain of unilateral origin, limited jaw opening, masticatory muscle tenderness, and no radiographic or clinical evidence of joint degeneration.96 Each patient should be examined for the presence of any of these symptoms. The masticatory muscles and the temporomandibular articulation are palpated in search of any areas or trigger points that elicit pain.
In general, the TMJ examination should focus on evaluating jaw movements and areas of pain in and around the joint upon palpation or function. Mandibular movements should be painless and within a normal range (approximately 50-mm on maximum opening and 10-mm in lateral excursions).94,97 The path followed during the opening movements of the mandible should be evaluated from the frontal view. This gives an indication of interferences, adhesions, or disc recapturing in the articulation. Although articular noises, such as clicking, popping, and crepitation, are important diagnostic findings, if any of these is the sole finding, it does not imply a diagnosis of TMD.95
In general, diagnosis and treatment of TMD is complex, as many other factors such as stress may be involved. In patients with a history of TMJ problems, a more advanced TMJ examination that may include the Helkimo index should be done.98 Clinical examinations should be complemented with a very thorough medical and dental history that may include a psycho-stress analysis.99
CR–CO
A major area of controversy in orthodontics and dentistry overall is the relevance and importance of the centric relation.100–103 Orthodontists should attempt to record the centric relation and detect whether any major shifts to the centric occlusion are present. It is normal to find a shift of approximately 1.5-mm in most individuals. The correlation between these small shifts and temporomandibular adverse effects is marginal but major shifts of 3- to 4-mm have been correlated with increased TMD.104
Some clinicians have recommended mounting every case in an articulator in order to treat an occlusion where CR–CO coincides. There is no evidence to support the need to mount every patient's models, less so if the potential source of error is considered in registering and transferring centric relation from the patient to an articulator.105
Radiographic Records
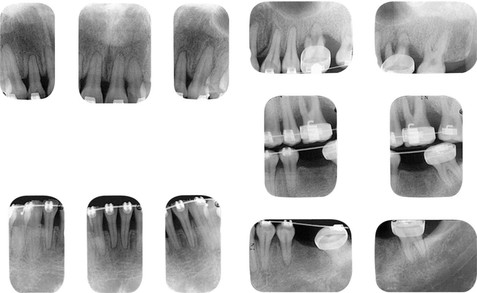
Several radiographic images can be used as diagnostic aids for orthodontic therapy. The most commonly used images are the panoramic and lateral cephalometric radiographic films.
Before concentrating on any measurement analysis, a careful screening of each radiograph for any signs of pathology is indicated. Pathological images often pass undetected by clinicians, as attention usually centers on the orthodontic analysis instead of the anatomic structures. Interestingly, it was found that 6% of orthodontic patients show some kind of anomalous or pathological finding in orthodontic diagnostic radiographs (Fig. 1-44).106,107
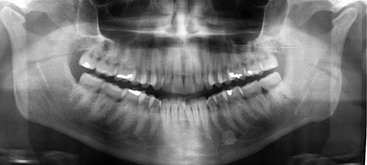
Figure 1-44 Condylar shape on panoramic radiograph is indicative of osteoarthritic changes. Note also the radiopaque structure between the root apices of the lower left premolars (compatible with idiopathic osteosclerosis).
Panoramic Radiograph
The panoramic radiograph provides a good general overview of the craniofacial anatomy, especially of the mandible, despite distortion of the image in some areas. Anatomy of the condyles should be examined carefully. Any asymmetry in length or width of the condyles, as well as in the shape of the articular surface, is noted. Ramus length and width symmetry should also be evaluated. Conditions such as hemimandibular hypoplasia or hyperplasia can be also detected in this radiograph.108 The most important information available in this radiograph are the presence or absence of teeth, any variation in development or eruption timings, impaction of teeth, and variation in tooth anatomy.109 The panoramic radiograph also provides general information on certain areas of interest that can be inspected closely with more specific imaging.
The panoramic radiograph is also good for screening periodontal disease and caries. If an area looks suspicious for any of these diseases, a periapical or bitewing radiograph should be taken.
With the advent of dental implants and their use in anchorage, the panoramic radiograph is also an important tool for inspection of the quality and quantity (height and width) of bone for possible implant sites.110 It is also useful for evaluating the proximity of implant sites to vital structures such as the mandibular canal and the maxillary sinuses.
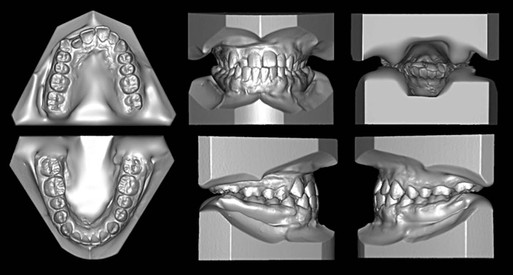
Lateral Cephalometric Radiograph
The lateral cephalogram is one of the oldest and still most often used radiographic images in orthodontics. Its limitation, as with any radiograph, is that it displays only a 2D (vertical and anteroposterior) image of 3D structures. Most orthodontic research and growth and development data are based on information obtained from this radiograph. It has been used for evaluation of the hard tissue anatomy in the craniofacial structures, evaluation of growth, treatment planning, and treatment results.
Traditionally, angles and linear measurements have been used to evaluate the different anatomic structures in the craniofacial complex.79,111 These measurements are compared to population means and the deviation from these norms is usually determined to be the problem. More recently, the development of numerous software programs enables an orthodontist to easily adopt his or her own relevant measurements from a plethora of cephalometric analyses. It should be emphasized that cephalometric analyses are only a diagnostic tool and are not diagnostic in themselves. Independent measures are meaningless if not interpreted properly; every deviation from the norm should be analyzed along with other measurements and within the whole context of the patient.
In the spatial analysis of an anatomic structure and its relation to others, three factors are important. The first is the size of the structure that can be measured, either in terms of height or width, and is usually defined by two points that determine a line. Second, the shape of the structure is usually defined by planes and angles and usually requires three or more points. Finally, the position of the structure is usually defined by angles and linear measurements to other reference structures.
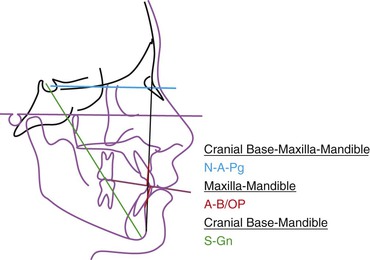
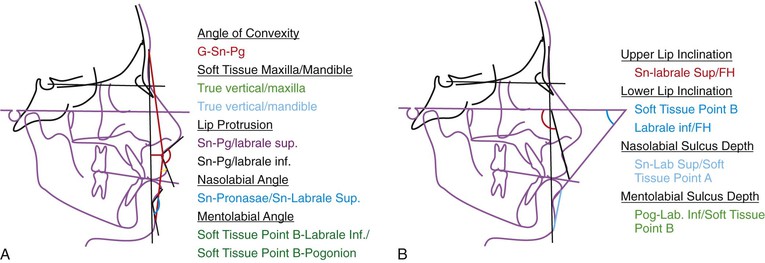
The cephalometric analysis for orthognathic surgery (COGS) developed at the University of Connecticut has been divided into five major craniofacial components in an attempt to define their size, shape, and position.75 These components are cranial base, maxilla, mandible, dentition, and soft tissue.
Before describing the specific spatial cephalometric analysis of these five components, a reference line or plane must be defined. This plane is important, as it will determine the orientation of the cranium in space. Many of the angular and linear measurements that analyze facial morphology relate back to this plane.
The Frankfurt horizontal (FH) plane was defined by anthropologists in the nineteenth century and was adopted in cephalometry as the horizontal reference line. Although still used, there are inherent problems with this reference line as both porion and orbitale are difficult landmarks to locate. It is especially difficult to visualize porion since it is a bilateral landmark and is often not well-defined on lateral head films. On the other hand, the sella-nasion (SN) line is composed of two easily visualized landmarks. At the University of Connecticut we have recommended an FH line located on average 7 degrees below the SN line.112 This constructed FH reference line is more reproducible and thus allows better evaluation of treatment progress and outcome.
For an accurate interpretation of the different structures in space, a reference line that was based on a physiological posture instead of cranial anatomic landmarks has also been recommended. Studies have shown that variation in cranial base inclination may result in an unreliable impression of facial relationships.113 A reference line that was made up of extracranial instead of intracranial points was recommended as being more reliable. This horizontal line should be parallel to the floor and represents the average head posture. The importance of this plane is that it not only reflects the normal position of the head in space, but also is a reproducible position not affected by intracranial landmarks. When a radiograph is taken in this natural head position (registered when a patient looks at a mirror in front of him or her at eye level), true vertical and horizontal reference lines can be traced.
Cranial Base
The cranial base, particularly the anterior portion, is an important structure in the cephalometric analysis. Since growth of the anterior cranial base is nearly completed early in life, it can be used as a reference for the other structures. The anterior cranial base is also used to superimpose successive cephalograms in order to evaluate the overall changes related to growth and treatment. By knowing the length of the cranial base, size correlations to the other structures (maxilla and mandible) can be estimated (Fig. 1-45).
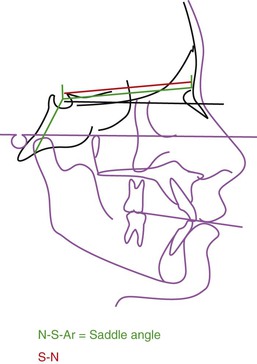
Figure 1-45 Measurements commonly used to evaluate the size and shape of the cranial base (first component in the cephalometric analysis).
The saddle angle formed by nasion (N) to sella (S) to articulare (Ar) (referred to as N–S–Ar) (see Fig. 1-45) and its influence on the craniofacial morphology has been evaluated in various studies. Its contribution to Class II and III malocclusions is somewhat controversial. It was proposed that an obtuse angle related to the former and an acute angle related to the latter114 but recent studies have not found a strong correlation between the two.115
Maxilla
The second component of the cephalometric analysis is the maxilla. Initially, a general idea of its size is obtained by measuring the posterior border to the anterior border. This measurement is specifically defined as the distance from the anterior nasal spine to the posterior nasal spine (ANS–PNS). Thereafter the anteroposterior position is assessed. The distance from A point, which is related to a vertical reference line passing through N, provides good information relative to the position of the maxilla. It is important to remember that A point is affected by dentoalveolar movement. Another measurement used to assess the anteroposterior position of the maxilla is the perpendicular distance from PNS to a vertical line passing through pterygomaxillary fissure point (PTM) (Fig. 1-46).
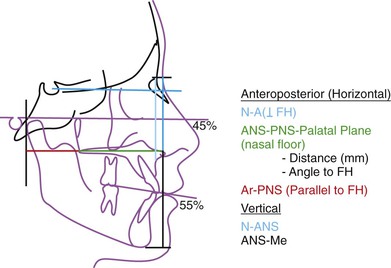
Figure 1-46 Commonly used measurements to evaluate size and position of the maxilla (second component). ANS, Anterior nasal spine; FH, Frankfurt horizontal; PNS, posterior nasal spine.
To assess the vertical position of the maxilla, the distance from the ANS to the N is measured. This is known as the upper facial height and its absolute measurement is not as important as the relationship to the lower facial height (ANS–Me): 45% for the upper to 55% for the lower facial height (see Fig. 1-44).112 Another important measurement indicating the vertical position or inclination of the maxilla is the angulation of the palatal plane (PNS–ANS) in relation to the horizontal line (see Fig. 1-44). Usually in skeletal open-bite patients this plane is tipped up anteriorly instead of being close to parallel, as is found in normal individuals.116
Mandible
The third major component of the cephalometric analysis is the mandibular position. Many cephalometric measurements relate to this craniofacial structure. All mandibular anatomic structures, except for the condyles, are well-visualized in the lateral cephalograms. For this reason, mandibular length and angular measurements are often taken from the constructed point, articulare (Ar). This point may be confounding, as mandibular positional or postural changes can give contradictory measurements.
To assess mandibular size, measurements such as condylion (Co) to gnathion (Gn) (Co–Gn), Co–Me, and Ar–Me are used (Fig. 1-47, A). These can further be divided into ramus height and corpus length: articulare (Ar) to gonion (Go) (Ar–Go) and gonion to menton (Go–Me), respectively (see Fig. 1-47, A). The anteroposterior position of the mandible is measured anteriorly by relating the distance of B point and the pogonion to a true vertical line (perpendicular to FH) passing through N (see Fig. 1-47, A). The difference between these two measurements gives an indication of the length of the hard tissue chin. Posteriorly, the anteroposterior position of the mandible can be evaluated from the angle formed by the ramus and the true horizontal (see Fig. 1-47, A). The shape of the mandible is defined by the gonial angle (Ar–Go–Me) (see Fig. 1-47, A).
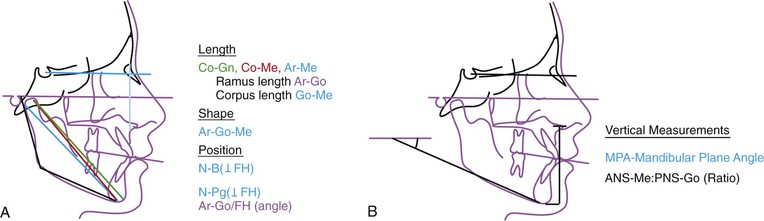
Figure 1-47 Measurements commonly used to evaluate size, shape, and position of the mandible (third component). A, Anteroposterior and (B) vertical images. ANS, Anterior nasal spine; FH, Frankfurt horizontal; PNS, posterior nasal spine.
The vertical anterior measurement of the mandible is calculated by quantifying the distance from ANS to Me (lower facial height). A ratio of the lower facial height to the posterior facial height (PNS–Go) can give an indication of the vertical pattern of the face (Fig. 1-47, B). These measurements can be correlated to the mandibular plane angle (true horizontal Go–Me, see Fig. 1-47, B). Traditionally, these angular measurements have been used to describe vertical growth (high angle versus low angle) and facial patterns (long face versus short face).
Before starting the fourth major component (dental) of the cephalometric analysis, a set of measurements that relate the maxilla and mandible to each other and the cranial base needs to be mentioned. These measurements are A–B relative to the true horizontal and the occlusal plane and the angle of convexity (N–A–Pg) (Fig. 1-48). Lastly, the S–Gn line is an isolated measurement that correlates directly with direction (angle with respect to the true horizontal) and magnitude (absolute length) of mandibular growth and indirectly with the growth of the whole facial complex (see Fig. 1-48).
Dental Measurements
The spatial relationship of the teeth is described in terms of their horizontal and vertical position within the bones. One of the reference planes for the dental measurements is the occlusal plane, which on average has a downward inclination anteriorly of approximately 12 degrees related to the true horizontal or constructed FH plane.
Different types of occlusal planes have been described. Downs originally described the occlusal plane as a constructed line that bisects the upper and lower molars and the anterior teeth.111 This plane does not take into consideration the axial inclinations of the posterior teeth. The inherent problem with this plane can be seen in patients who have no incisor overlap, such as in the case of an anterior open-bite.
A better method for defining this plane is the anatomic or functional occlusal plane. This occlusal plane follows the occlusal contacts of the posterior teeth and is extended anteriorly. It can be determined easily, as the longitudinal axis of the posterior teeth is almost perpendicular to this occlusal plane.
In the analysis of the dentition, the inclination of the upper incisors is evaluated in relation to the maxillary palatal plane and the true horizontal plane (Fig. 1-49). In the lower arch, the ideal relationship of the incisors to the mandibular plane has been considered to be an angle close to 90 degrees (see Fig. 1-49). The interincisal angle should confirm the findings of the upper and lower incisor inclination to the palatal and mandibular plane respectively (see Fig. 1-49).
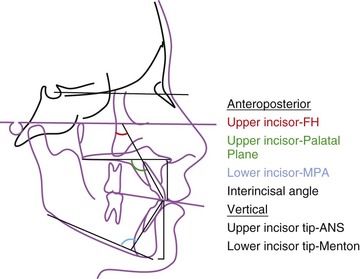
Figure 1-49 Measurements commonly used in the fourth component of the cephalometric analysis (dentition). ANS, Anterior nasal spine; FH, Frankfurt horizontal; MPA, mandibular plane angle.
Vertically, a measurement from ANS to 1 (ANS–upper incisor tip) determines the amount of eruption of the upper incisor. In the lower arch, the vertical height of the lower incisor is assessed by the measurement of Me to –1 (menton–lower incisor tip, see Fig. 1-49).
Soft Tissue
Some of the reference lines used for cephalometric soft tissue analysis were introduced above in the description of the clinical examination. It is important to stress that these lines are only guidelines based on averages and that esthetics is highly subjective.
The soft tissue analysis should start by determining the general convexity of the profile (G–Sn–Pg; Fig. 1-50, A). Thereafter, the anteroposterior position of the maxilla and the mandible can be analyzed separately by drawing a line perpendicular to the horizontal reference line passing through the glabella, soft tissue nasion, subnasale, or any other anterior soft tissue landmark (depending on the analysis) and measuring the distance to the maxilla and the mandible (see Fig. 1-50, A). On average the mandible lies within this line (when a true vertical is drawn through the glabella) and the maxilla is 2- to 3-mm in front. It is important to determine the upper lip, lower lip, and soft tissue chin thickness since these elements might be compensating for a skeletal disharmony.
The next step in the soft tissue analysis is evaluation of the lips. In general, measurements of lip protrusion are made using Sn–Pg as the reference line (see Fig. 1-50, A). Other angles used to evaluate lip protrusion are the nasolabial angle for the upper lip and the mentolabial angle for the lower lip (see Fig. 1-50, A). To eliminate the influence of the nose when measuring upper lip inclination, an angle is measured between the true horizontal and a line is traced from Sn to the labrale superioris (Fig. 1-50, B). A similar measurement to evaluate lower lip inclination has been used by connecting a line from the depth of the mentolabial sulcus to the labrale inferioris and measuring the angle to FH (see Fig 1-50, B).
Growth Assessment
To complement the lip analysis, the curl of both lips is evaluated. This is an important esthetic feature. The depth of the upper lip and the mentolabial sulcus is measured by drawing a line from the upper lip to Sn and the lower lip to Pg, respectively (see Fig. 1-50, B). Excessive depth in these measurements may indicate lip redundancy. Finally, a measurement of the chin to throat depth is important, especially in prospective surgery patients.
In general, when soft tissues are assessed, the tongue, soft tissue palate, and airway structures are often overlooked. It is important to evaluate the airway patency as well as the position of the hyoid bone. It has been reported that patients with obstructive sleep apnea have a low position of the hyoid bone.117
All cephalometric measurements and their deviations from the norms are only guides to describe the problems. An explanation for each deviation from the norm is examined in conjunction with the other measurements to obtain a cephalometric summary. Attention should be paid to contradictory measurements and an explanation for these should be sought. Cephalometric analysis is a tool and as such it is only one of the components in the database that needs to be complemented with the clinical examination, models, and other imaging.
Traditionally, hand-wrist radiographs have been used to evaluate skeletal maturity. The stage of ossification of the wrist and phalanges in the hand correlates to skeletal maturity (Fig. 1-51). However, efforts to correlate skeletal maturation to the cervical vertebrae have diminished the need for a hand-wrist radiograph. It has been shown that the peak of pubertal growth can be estimated adequately from a lateral cephalometric film.118 Visual assessment of the lower border concavities and progressive elongation of the odontoid process (C2) and C3 and C4 vertebrae on the lateral cephalogram form the basis of this staging method. Based on this assessment, the patient can be placed in one of six cervical stage categories (CS1–CS6) and an estimation can be made on the growth stage of the patient relative to the peak in mandibular growth.119
Occlusal Radiograph
The occlusal radiograph has been used to locate supernumerary or impacted teeth. In conjunction with a panoramic radiograph, the occlusal x-ray has been reported to give a good indication of the location of the impacted or supernumerary tooth.109 This radiograph is also indicated to evaluate the amount of suture distraction with rapid palatal expansion (Fig. 1-52).
Posteroanterior-Cephalometric Radiograph
The posteroanterior-cephalometric radiograph (posteroanterior cephalogram) is indicated in patients in whom a significant clinical asymmetry is noticed (Fig. 1-53). It can be used for both skeletal and dental base asymmetry detection. Mandibular ramus heights as well as corpus lengths can be evaluated. A large discrepancy between the lower borders of the mandible observed in a lateral cephalometric radiograph is highly indicative of a skeletal asymmetry that can be better evaluated with a posteroanterior cephalogram.
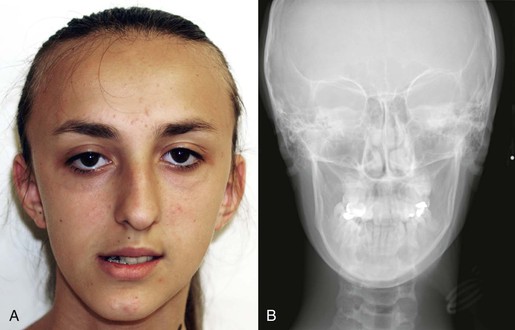
Figure 1-53 Significant mandibular asymmetry evident (A) in the clinical examination with the patient in centric occlusion and (B) on the posteroanterior cephalic radiograph in centric occlusion.
This radiograph is also a good tool for evaluation of dental midline discrepancies. A method to obtain a differential diagnosis between an apical base midline problem and a dental midline problem has been described elsewhere.120 In the transverse dimension, width measurements in the craniofacial region can be compared to recently published normative data obtained from a growth study.121
Submento-Vertical Radiograph
The submento-vertical radiograph is excellent for evaluating mandibular asymmetry. An analysis of this radiographic image was developed for the evaluation of condylar position as well as mandibular symmetry of the corpus and ramus.122 Symmetry of the zygomaxillary complex can also be evaluated on this radiograph. The findings obtained from this x-ray can be correlated to those found on the posteroanterior cephalogram for a 3D analysis of a skeletal asymmetry.
Cone Beam Computed Tomography
Cone beam computed tomography (CBCT) has gained popularity in recent years for imaging the craniofacial complex. CBCT delivers a significantly lower dose of radiation compared to conventional CT methods and has distinct advantages over 2D images, including providing 1 : 1 orthogonal representations of structures. CBCT images can be used in lieu of other 2D images, such as panoramic radiographic projection and lateral cephalogram, with the software capable of generating these images from the 3D data. Caution should be exercised to minimize radiation doses to patients. Studies have shown great variability in the amount of radiation exposure between different CBCT machines and the control of the field of view and intensity can help to minimize these levels.123–125 CBCT is a valuable tool for 3D surgical planning, which is discussed in Chapter 2. In addition, in cases with impacted teeth, CBCT images can provide a number of advantages over periapical and occlusal films for localization of these teeth, since they provide images free of distortion and overlapping structures.124,126
Diagnostic Models
One of the major advantages of models is the ability to inspect the malocclusion from the lingual aspect. Models also provide a more accurate and accessible way to evaluate arch shape, occlusion, and the 3D position of each tooth in space (first, second, and third order) and how it relates to the other teeth. Also, arch symmetry can be analyzed from the deviation of the teeth from the midsagittal suture.
Models also can be used for space analysis in the mixed dentition and as a template from which an occlusogram can be constructed. While traditionally stone models have been used, new technologies have further advanced the capabilities of digital 3D models. These models can be acquired through surface scanning of stone models or through the use of direct intraoral scanners, eliminating the need for an alginate impression (Fig. 1-54). A variety of software programs exist that are able to manipulate these models in all three dimensions and do a variety of analyses, including measuring Bolton discrepancies, space analysis, and doing occlusograms.127
Summary
A synopsis of the most important components needed for the orthodontic diagnosis has been given. A detailed analysis of the clinical examination, radiographs, patient records, and additional imaging has been described. A good treatment outcome is heavily dependent on good data collection and analysis of the database. Ultimately, the diagnosis should answer the question “why?” so that later we can determine where we are going (objectives), how we are going to get there (treatment plan), and what techniques are going to be used (mechanics plan).
References
1. Soanes C, Stevenson A. Concise Oxford English Dictionary. 11th ed. Oxford University Press: Oxford, England; 2009.
2. Tobiasen JM. Social judgments of facial deformity. Cleft Palate J. 1987;24:323–327.
3. Ash M, Ramfjord SR. Occlusion. 4th ed. WB Saunders: Philadelphia, PA; 1995.
4. Barrows HS. Practice-Based Learning. Southern Illinois University School of Medicine: Springfield, IL; 1994.
5. Burden D, Mullally B, Sandler J. Orthodontic treatment of patients with medical disorders. Eur J Orthod. 2001;23:363–372.
6. Epstein JB. Infective endocarditis: dental implications and new guidelines for antibiotic prophylaxis. American Heart Association. J Can Dent Assoc. 1998;64:281–286.
7. Devlin H, Garland H, Sloan P. Healing of tooth extraction sockets in experimental diabetes mellitus. J Oral Maxillofac Surg. 1996;54:1087–1091.
8. McNab S, Battistulla D, Taverne A, Symons AL. External apical root resorption of posterior teeth in asthmatics after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1999;116:545–551.
9. Meraw SJ, Sheridan PJ. Medically induced gingival hyperplasia. Mayo Clin Proc. 1998;73:1196–1199.
10. Karras JC, Miller JR, Hodges JS, Beyer JP, Larson BE. Effect of alendronate on orthodontic tooth movement in rats. Am J Orthod Dentofacial Orthop. 2009;136(6):843–847.
11. Ortega AJ, Campbell PM, Hinton R, Naidu A, Buschang PH. Local application of zoledronate for maximum anchorage during space closure. Am J Orthod Dentofacial Orthop. 2012;142(6):780–791.
12. Lotwala RB, Greenlee GM, Ott SM, Hall SH, Huang GJ. Bisphosphonates as a risk factor for adverse orthodontic outcomes: a retrospective cohort study. Am J Orthod Dentofacial Orthop. 2012;142(5):625–634.
13. Janson GR, Dainesi EA, Consolaro A, Woodside DG, de Freitas MR. Nickel hypersensitivity reaction before, during, and after orthodontic therapy. Am J Orthod Dentofacial Orthop. 1998;113(6):655–660.
14. Grimaudo NJ. Biocompatibility of nickel and cobalt dental alloys. Gen Dent. 2001;49(5):498–503.
15. Smith RM, Gonzalez C. The relationship between nasal obstruction and craniofacial growth. Pediatr Clin North Am. 1989;36(6):1423–1434.
16. Bergstrom J, Preber H. Tobacco use as a risk factor. J Periodontol. 1994;65(suppl 5):545–550.
17. Scabbia A, et al. Cigarette smoking negatively affects healing response following flap debridement surgery. J Periodontol. 2001;72(1):43–49.
18. Sanders NL. Evidence-based care in orthodontics and periodontics: a review of the literature. J Am Dent Assoc. 1999;130(4):521–527.
19. Reichert C, et al. Interfaces between orthodontic and periodontal treatment: their current status. J Orofac Orthop. 2011;72(3):165–186.
20. Franchi L, Baccetti T, McNamara JA Jr. Mandibular growth as related to cervical vertebral maturation and body height. Am J Orthod Dentofacial Orthop. 2000;118(3):335–340.
21. Oudet C, Petrovic A, Stutzmann J. Time-dependent effects of a “functional”-type orthopedic appliance on the rat mandible growth. Chronobiol Int. 1984;1(1):51–57.
22. Chen JY, Will LA, Niederman R. Analysis of efficacy of functional appliances on mandibular growth. Am J Orthod Dentofacial Orthop. 2002;122(5):470–476.
23. Woodside DG. Do functional appliances have an orthopedic effect? Am J Orthod Dentofacial Orthop. 1998;113(1):11–14.
24. Baccetti T, et al. Treatment timing for twin-block therapy. Am J Orthod Dentofacial Orthop. 2000;118(2):159–170.
25. Voudouris JC, et al. Condyle-fossa modifications and muscle interactions during herbst treatment, part 1. New technological methods. Am J Orthod Dentofacial Orthop. 2003;123(6):604–613.
26. Fishman LS. Radiographic evaluation of skeletal maturation: a clinically oriented method based on hand-wrist films. Angle Orthod. 1982;52(2):88–112.
27. Hagg U, Taranger J. Menarche and voice change as indicators of the pubertal growth spurt. Acta Odontol Scand. 1980;38(3):179–186.
28. Hagg U, Taranger J. Skeletal stages of the hand and wrist as indicators of the pubertal growth spurt. Acta Odontol Scand. 1980;38(3):187–200.
29. Silveira AM, et al. Facial growth during adolescence in early, average and late maturers. Angle Orthod. 1992;62(3):185–190.
30. Saunders SR, Popovich F, Thompson GW. A family study of craniofacial dimensions in the Burlington Growth Centre sample. Am J Orthod. 1980;78(4):394–403.
31. Suzuki A, Takahama Y. Parental data used to predict growth of craniofacial form. Am J Orthod Dentofacial Orthop. 1991;99(2):107–121.
32. Bishara SE. Facial and dental changes in adolescents and their clinical implications. Angle Orthod. 2000;70(6):471–483.
33. Nanda RS. The rate of growth of different facial components. Am J Orthod. 1955;41:658–673.
34. Skieller V, Bjork A, Linde-Hansen T. Prediction of mandibular growth rotation evaluated from a longitudinal implant sample. Am J Orthod. 1984;86(5):359–370.
35. Leslie LR, et al. Prediction of mandibular growth rotation: assessment of the Skieller, Bjork, and Linde-Hansen method. Am J Orthod Dentofacial Orthop. 1998;114(6):659–667.
36. Kokich VG. Managing complex orthodontic problems: the use of implants for anchorage. Semin Orthod. 1996;2(2):153–160.
37. Baccetti T. A controlled study of associated dental anomalies. Angle Orthod. 1998;68(3):267–274.
38. Peck S, Peck L, Kataja M. Concomitant occurrence of canine malposition and tooth agenesis: evidence of orofacial genetic fields. Am J Orthod Dentofacial Orthop. 2002;122(6):657–660.
39. Katz JL. The structure and biomechanics of bone. Symp Soc Exp Biol. 1980;34:137–168.
40. Kiliaridis S. Masticatory muscle influence on craniofacial growth. Acta Odontol Scand. 1995;53(3):196–202.
41. Proffit WR. Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthod. 1978;48(3):175–186.
42. Weinstein S, et al. On an equilibrium theory of tooth position. Angle Orthod. 1963;33:1–26.
43. Mah J, Bumann A. Technology to create the three-dimensional patient record. Semin Orthod. 2001;7:251–257.
44. Scheib JE, Gangestad SW, Thornhill R. Facial attractiveness, symmetry and cues of good genes. Proc R Soc Lond B Biol Sci. 1999;266(1431):1913–1917.
45. Thornhill R, Gangestad SW. Facial attractiveness. Trends Cogn Sci. 1999;3(12):452–460.
46. Arnett GW, Bergman RT. Facial keys to orthodontic diagnosis and treatment planning: part I. Am J Orthod Dentofacial Orthop. 1993;103(4):299–312.
47. Vig RG, Brundo GC. The kinetics of anterior tooth display. J Prosthet Dent. 1978;39(5):502–504.
48. Frush JO, Fisher RD. The dysesthetic interpretation in the dentogenic concept. J Prosthet Dent. 1958;8:55–58.
49. Dunn WJ, Murchison DF, Broome JC. Esthetics: patients’ perceptions of dental attractiveness. J Prosthodont. 1996;5(3):166–171.
50. Fuhrmann RAW. Three-dimensional evaluation of periodontal remodeling during orthodontic treatment. Semin Orthod. 2002;8:23–28.
51. Schiffman PH, Tuncay OC. Maxillary expansion: a meta analysis. Clin Orthod Res. 2001;4(2):86–96.
52. Sarver DM, Ackerman JL. Evaluation of facial soft tissues. Proffit WR. Contemporary Treatment of Facial Deformity. Mosby: St. Louis, MO; 2003:92–126.
53. Burstone C. 2003. Personal communication.
54. Benson KJ, Laskin DM. Upper lip asymmetry in adults during smiling. J Oral Maxillofac Surg. 2001;59(4):396–398.
55. Beyer JW, Lindauer SJ. Evaluation of dental midline position. Semin Orthod. 1998;4(3):146–152.
56. Cardash HS, Ormanier Z, Laufer BZ. Observable deviation of the facial and anterior tooth midlines. J Prosthet Dent. 2003;89(3):282–285.
57. Kokich VO Jr, Kiyak HA, Shapiro PA. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 1999;11(6):311–324.
58. Caudill R, Chiche GJ. Establishing an esthetic gingival appearance. Chiche G. Esthetics of Anterior Fixed Prosthodontics. Quintessence Publishing Co Inc: Chicago, IL; 1994:177–198.
59. Chiche G, Pinault A. Replacement of deficient crowns. Chiche G. Esthetics of Anterior Fixed Prosthodontics. Quintessence Publishing Co Inc: Chicago, IL; 1994:53–73.
60. Petrovic A, Stutzmann J. [Growth hormone: mode of action on different varieties of cartilage (author's transl)]. Pathol Biol (Paris). 1980;28(1):43–58.
61. Nanda RS, et al. Growth changes in the soft tissue facial profile. Angle Orthod. 1990;60(3):177–190.
62. McNamara JA Jr. Components of class II malocclusion in children 8–10 years of age. Angle Orthod. 1981;51(3):177–202.
63. Guyer EC, et al. Components of class III malocclusion in juveniles and adolescents. Angle Orthod. 1986;56(1):7–30.
64. Lai J, Ghosh J, Nanda R. Effects of orthodontic therapy on the facial profile in long and short vertical facial patterns. Am J Orthod Dentofacial Orthop. 2000;118(5):505–513.
65. Kocadereli IL. Changes in soft tissue profile after orthodontic treatment with and without extractions. Am J Orthod Dentofacial Orthop. 2002;122(1):67–72.
66. Rains M, Nanda R. Soft-tissue changes associated with maxillary incisor retraction. Am J Orthod. 1982;81(6):481–488.
67. Thuer U, Ingervall B. Pressure from the lips on the teeth and malocclusion. Am J Orthod Dentofacial Orthop. 1986;90(3):234–242.
68. Lapatki BG, et al. The importance of the level of the lip line and resting lip pressure in class II, division 2 malocclusion. J Dent Res. 2002;81(5):323–328.
69. Burstone C. Arch form and dimension: anteroposterior positioning of the incisors. Burstone C. Problem Solving in Orthodontics: Goal-Oriented Treatment Strategies. Quintessence Publishing Co, Inc: Chicago, IL; 2000:98–120.
70. Flynn TR, Ambrogio RI, Zeichner SJ. Cephalometric norms for orthognathic surgery in black American adults. J Oral Maxillofac Surg. 1989;47(1):30–39.
71. Lew KK, et al. Soft-tissue cephalometric norms in Chinese adults with esthetic facial profiles. J Oral Maxillofac Surg. 1992;50(11):1184–1189.
72. Rhine JS, Campbell HR. Thickness of facial tissues in American blacks. J Forensic Sci. 1980;25(4):847–858.
73. Oliver BM. The influence of lip thickness and strain on upper lip response to incisor retraction. Am J Orthod. 1982;82(2):141–149.
74. Ricketts R. Planning treatment on the basis of the facial pattern and an estimate of its growth. Angle Orthod. 1957;27:14–37.
75. Burstone C. The integumental profile. Am J Orthod. 1958;44:1–25.
76. Burstone CJ. Lip posture and its significance in treatment planning. Am J Orthod. 1967;53(4):262–284.
77. Holdaway R. A soft tissue cephalometric analysis and its use in orthodontic treatment planning: part I. Am J Orthod. 1983;84:1–28.
78. Merrifield L. The profile line as an aid in critically evaluating facial esthetics. Am J Orthod. 1966;52:804–822.
79. Steiner C. The use of cephalometrics as an aid to planning and assessing orthodontic treatment. Am J Orthod. 1960;46:721–735.
80. Legan H, Burstone CJ. Soft tissue cephalometric analysis for orthognathic surgery. J Oral Surg. 1980;38:744–751.
81. Horn A. Facial height index. Am J Orthod. 1992;102(2):180.
82. Sarver DM, Ackerman MB. Dynamic smile visualization and quantification: part 1. Evolution of the concept and dynamic records for smile capture. Am J Orthod Dentofacial Orthop. 2003;124(1):4–12.
83. Edwards J. The diastema, the frenum, the frenectomy: a clinical study. Am J Orthod. 1977;71:489–508.
84. Kopczyk R, Saxe SR. Clinical signs of gingival inadequacy: the tension test. J Dent Child. 1974;41:352–355.
85. Fletcher SG, Meldrum JR. Lingual function and relative length of the lingual frenulum. J Speech Hear Res. 1968;11(2):382–390.
86. Andreasen J, Andreasen FM. Textbook and Color Atlas of Traumatic Injuries to the Teeth. Munksgaard: Copenhagen, Denmark; 1994.
87. Hamilton RS, Gutmann JL. Endodontic-orthodontic relationships: a review of integrated treatment planning challenges. Int Endod J. 1999;32(5):343–360.
88. Kokich VG, Spear FM. Guidelines for managing the orthodontic-restorative patient. Semin Orthod. 1997;3(1):3–20.
89. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995–996.
90. Uribe F, Holliday B, Nanda R. Incidence of open gingival embrasures after mandibular incisor extractions: a clinical photographic evaluation. Am J Orthod Dentofacial Orthop. 2011;139(1):49–54.
91. Andrews L. Straight Wire: The Concept and Appliance. K-W Publications: San Diego, CA; 1989.
92. Dale J, Dale HC. Interceptive guidance of occlusion with emphasis on diagnosis. Graber T. Orthodontics Current Principles and Techniques. Mosby: St. Louis, MO; 2000:375–469.
93. Clark JR, Evans RD. Functional occlusion: I. A review. J Orthod. 2001;28(1):76–81.
94. Ash M, Ramfjord SP. Occlusion. WB Saunders: Philadelphia, PA; 1994.
95. Laskin DM. The clinical diagnosis of temporomandibular disorders in the orthodontic patient. Semin Orthod. 1995;1(4):197–206.
96. Greene C, Lerman MD, et al. The TMJ pain-dysfunction syndrome: heterogenicity of the patient population. J Am Dent Assoc. 1969;79:1168–1172.
97. Cox S, Walker DM. Establishing a normal range for mouth opening: its use for oral submucous fibrosis. Br J Oral Maxillofac Surg. 1997;35(1):40–42.
98. Helkimo M. Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state. Sven Tandlak Tidskr. 1974;67:101–121.
99. Fricton JR. Management of masticatory myofascial pain. Semin Orthod. 1995;1(4):229–243.
100. Chhatwani B. More comments on Rinchuse Counterpoint. Am J Orthod Dentofacial Orthop. 1995;108(6):13A.
101. Hew SK. Comment on the Roth/Rinchuse responses. Am J Orthod Dentofacial Orthop. 1996;109(6):15A–16A.
102. Rinchuse DJ. A three-dimensional comparison of condylar change between centric relation and centric occlusion using the mandibular position indicator. Am J Orthod Dentofacial Orthop. 1995;107(3):319–328.
103. Roth RH. Occlusion and condylar position. Am J Orthod Dentofacial Orthop. 1995;107(3):315–318.
104. McNamara JA Jr, Seligman DA, Okeson JP. Occlusion, orthodontic treatment, and temporomandibular disorders: a review. J Orofac Pain. 1995;9(1):73–90.
105. Clark JR, Hutchinson I, Sandy JR. Functional occlusion: II. The role of articulators in orthodontics. J Orthod. 2001;28(2):173–177.
106. Kuhlberg A, Norton LA. Finding pathology on cephalometric radiographs. Athanasious EA. Orthodontic Cephalometry. Mosby-Wolfe: London, England; 1995:175–180.
107. Kuhlberg AJ, Norton LA. Pathologic findings in orthodontic radiographic images. Am J Orthod Dentofacial Orthop. 2003;123(2):182–184.
108. Obwegeser HL, Makek MS. Hemimandibular hyperplasia–hemimandibular elongation. J Maxillofac Surg. 1986;14(4):183–208.
109. Jacobs SG. Radiographic localization of unerupted teeth: further findings about the vertical tube shift method and other localization techniques. Am J Orthod Dentofacial Orthop. 2000;118(4):439–447.
110. Tyndall D, Brooks S. Selection criteria for dental implant site imaging: A position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(5):630–637.
111. Downs W. Variations in facial relationships: their significance in treatment and prognosis. Am J Orthod. 1948;34:812.
112. Burstone CJ, et al. Cephalometrics for orthognathic surgery. J Oral Surg. 1978;36(4):269–277.
113. Moorrees C. Natural head position: the key to cephalometry. Jacobsen A. Radiographic Cephalometry. Quintessence Publishing Co, Inc: Chicago, IL; 1995:175–184.
114. Bjork A. Cranial base development. Am J Orthod. 1955;41:198–225.
115. Dhopatkar A, Bhatia S, Rock P. An investigation into the relationship between the cranial base angle and malocclusion. Angle Orthod. 2002;72(5):456–463.
116. Cangialosi TJ. Skeletal morphologic features of anterior open bite. Am J Orthod. 1984;85(1):28–36.
117. Tangugsorn V, et al. Obstructive sleep apnea: a principal component analysis. Int J Adult Orthodon Orthognath Surg. 1999;14(3):215–228.
118. Baccetti T, Franchi L, McNamara JA Jr. An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 2002;72(4):316–323.
119. Baccetti T, Franchi L, McNamara JA Jr. The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11(3):119–129.
120. Torres M. Treatment objectives and treatment planning. Dent Clin North Am. 1981;25(1):27–41.
121. Basyouni AA, Nanda SK. An atlas of the transverse dimensions of the face. [Craniofacial Growth Series. Vol. 37] McNamara JA Jr. Center for Human Growth and Development, and Department of Orthodontics and Pediatric Dentistry, School of Dentistry, University of Michigan: Ann Arbor, MI; 2001.
122. Forsberg CT, Burstone CJ, Hanley KJ. Diagnosis and treatment planning of skeletal asymmetry with the submental-vertical radiograph. Am J Orthod. 1984;85(3):224–237.
123. Ludlow JB, et al. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35(4):219–226.
124. Guerrero ME, et al. The diagnostic efficacy of cone beam CT for impacted teeth and associated features: a systematic review. J Oral Rehabil. 2011;38(3):208–216.
125. Nervina JM. Cone beam computed tomography use in orthodontics. Aust Dent J. 2012;57(suppl 1):95–102.
126. Kapila S, Conley RS, Harrell WE Jr. The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac Radiol. 2011;40(1):24–34.
127. Tomassetti JJ, et al. A comparison of 3 computerized Bolton tooth-size analyses with a commonly used method. Angle Orthod. 2001;71(5):351–357.