Biomechanical Strategies for Optimal Finishing
Flavio Andres Uribe, Padma Mukherjee, Ravindra Nanda
Orthodontic finishing is described as an “art” composed of individual perceptions and small detailing. Finishing distinguishes a true master of the profession from an average orthodontist. It is a critical step that involves fine-tuning individual tooth positions and intra-arch and inter-arch relationships and optimizes the treatment results.1 This step can be especially challenging to the clinician since the minor changes performed generally are not appreciated by patients.
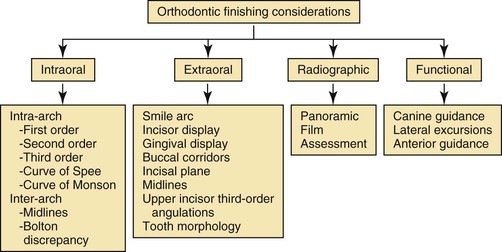
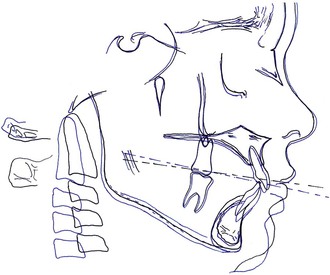
Finishing is the last phase of “active” treatment and thus is heavily dependent on the previous stages of treatment. It is extremely difficult, if not impossible, to achieve an acceptable end result when the treatment objectives have not been met and the mechanics have not been delivered properly. Major tooth movement should have been executed properly so that the minute tooth movements can be achieved with precision in the final finishing phase of treatment. When the treatment mechanics are less than optimal, the finishing stage often includes indiscriminate use of intermaxillary elastics and quick-fix therapies such as interproximal reduction. Although there are definite indications for these procedures, they should not be used routinely to compensate for deficiencies in treatment planning and/or application of mechanics. Overall, the finishing stage of treatment should be evaluated according to four major categories: intraoral, extraoral, radiographic, and functional objectives. In each category specific objectives must be met to obtain a desirable finish (Fig. 27-1).
Intraoral Objectives
Intraoral objectives are arguably the most important of the four major categories.2 The intraoral objectives are classified into two subcategories: intra-arch and inter-arch objectives. The primary objective in both is to achieve ideal occlusion with well-aligned arches. Most of these intraoral objectives are described in the American Board of Orthodontics (ABO) grading criteria.2
Intra-Arch Analysis
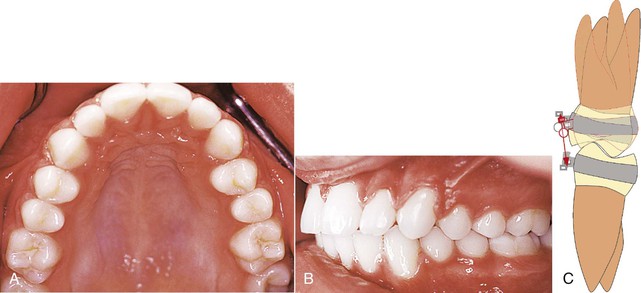
Each tooth must be evaluated with reference to its first-, second-, and third-order position. When evaluating the first order, teeth should have no rotations and have tight interproximal contacts.1 In addition, tooth morphology must be taken into consideration and the cusp tips and fossae should follow the perfect arch form. An occlusal mirror can be very useful to identify minor rotations and buccolingual displacement of teeth outside of the perfect arch form (Fig. 27-2). The upper first molar has special considerations regarding its first-order position. A mesial-out rotation of the mesiobuccal cusp3 is considered to be ideal. It has also been advocated that the buccal surface of the upper first molar should be parallel to the palatal suture (Fig. 27-3).4
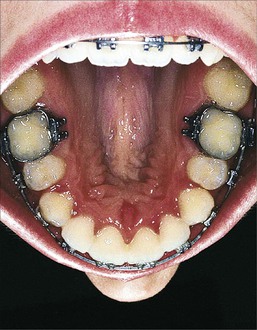
Figure 27-2 Occlusal mirror used as an aid to evaluate intra-arch discrepancies during finishing. This view is used to identify first-order rotations, spacing, and any arch form problems.
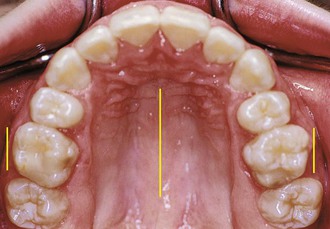
Figure 27-3 Occlusal view of a finished case where the buccal surface of the upper first molar is parallel to the midpalatal raphe.
In the second order, the root parallelism and marginal ridges are evaluated. The marginal ridges should be at the same level, particularly in the buccal segments. Often when marginal ridges between adjacent teeth coincide, root parallelism also will. A panoramic x-ray is an adjunct to evaluate second-order discrepancies. In extraction cases, a small degree of crown tipping most likely will occur and root parallelism will be required. Small adjustments in the second-order angulation of the anterior teeth (i.e., accentuating the distal tip) can help to decrease any excess space in the anterior region (Fig. 27-4).1 The third order is most relevant to the inter-arch objectives (i.e., the occlusal relationship) and to the esthetics of the smile (an extraoral category, discussed below). Regarding the intraoral objectives, a small curve of Monson between the buccal segments allows for proper occlusal function (i.e., adequate intercuspation without balancing interferences). An accentuated curve of Monson usually results in balancing interferences, especially in the second molar area.5 This clinical situation is commonly encountered in adults after the dental correction of buccal crossbites without expansion of the basal bone and palatal suture (Fig. 27-5). Proper third-order angulation of anterior teeth is also important for good occlusion (Fig. 27-6). Furthermore, regarding the extraoral category, third-order angulation is important for good esthetics of the smile (Fig. 27-7).1 Significant emphasis on the upper canine and first premolar third-order inclination has been proposed by some clinicians.6 In general, the buccal surfaces of these teeth should be close to parallel to the midsagittal facial line in an ideal smile.
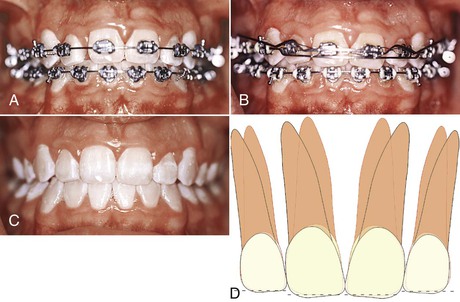
Figure 27-4 A–C, Patient shows no overjet but excess space between the incisors due to a Bolton discrepancy. These spaces can be closed or reduced by accentuating the distal root tip of the incisors, thereby increasing the interproximal contact distance. Incisal adjustments (enamoplasty) were done at the appliance removal visit. D, Diagram showing the distal tip and enamoplasty required.
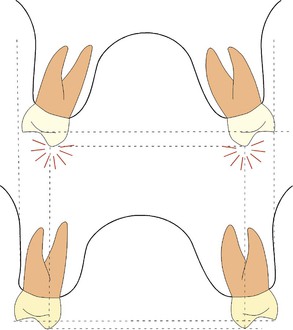
Figure 27-5 Proper third-order angulation needed in the posterior buccal segments may not be achieved in adults after arch width expansion without surgery. Occlusal balancing contacts may result from the dental third-order compensation. The lower diagram shows the difference in skeletal width and vertical cusp position that can be achieved with skeletal expansion.
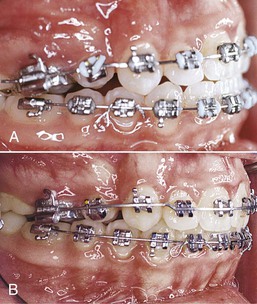
Figure 27-6 A and B, Patient showed an improvement in the occlusion after proper third-order angulation of the anterior teeth was obtained.
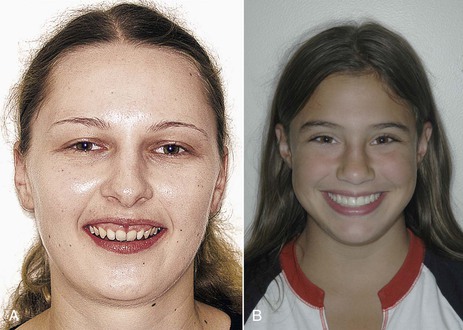
Figure 27-7 Depending on the upper anterior third-order angulation, light is reflected differently in the frontal view. A, Patient with retroclined incisors. Note the light reflected in the periodontal tissues. B, Patient with proper incisor inclination. Note the light reflected in the middle third of the incisors.
The final intra-arch objective is to achieve a gentle curve of Spee from the anterior teeth to the posterior buccal segments.1 The magnitude of this curve will vary depending on the overbite (inter-arch relation) and incisor display (an extraoral objective, discussed below).
Inter-Arch Analysis
The first molars and canines are the most important teeth to evaluate regarding the interocclusal relationship. Traditionally, orthodontists have classified malocclusion in the anteroposterior dimension and thus the static analysis of the occlusion has primarily been based on the first molar relationship. Additionally, the canine is of primary importance if canine-guided functional occlusion is to be achieved. The main objective is to “seat” the canines in a Class I relationship and obtain good coupling with the antagonistic canines. This ideal interocclusal relationship is difficult to achieve when a significant tooth size discrepancy exists between the dental arches (i.e., a Bolton discrepancy).7 The upper lateral incisors and lower second premolars are usually responsible for this inter-arch tooth size discrepancy,8 as abnormal tooth morphology is more common in these teeth. This results in less than ideal occlusion, such as a Class II canine tendency on that side, that becomes apparent during finishing (Fig. 27-8).

Figure 27-8 Bolton discrepancy reflected in the occlusion in the finishing stage. There is a tendency toward a Class II canine relationship due to the small upper laterals.
Two types of occlusion have been considered ideal: cusp-to-fossa and cusp-to–interproximal space relationships. In the natural dentition, a cusp-to–interproximal space relationship is most characteristic.3 The lingual cusps in the upper arch and the buccal cusps in the lower arch are primarily responsible for function. The buccal cusps of the upper premolars and the lingual cusps of the lower premolars should occlude in the interproximal space. In Class II patients, some of the anteroposterior correction can be achieved by overrotation of the buccal cusps of the upper premolars distally to coincide with the lower interproximal spaces.9,10 In the anterior segment, overbite and overjet are the most critical factors in achieving a proper interocclusal relationship. These two occlusal traits determine the disclusion of the posterior teeth during protrusive movements. More than 50% overbite may be excessive, as the contact of the lower incisors on the lingual surface of the upper incisors in these patients would not be on the cingulum (the most suitable portion to receive occlusal forces). Finally, it is important that the lingual surface of the upper incisors be properly inclined to allow the lower incisors to slide anteriorly in an angle that is in synchrony with the articular eminence.11
Arch coordination is also evaluated from the frontal view. This allows proper cusp seating to be visualized. The intercanine and inter-molar widths should be coordinated to prevent excessive buccal overjet or a buccal crossbite tendency. The premolar area is also inspected transversely for proper coordination between the upper and lower arches.
Midlines are also used to evaluate interocclusal relationships. During finishing, minor midline problems should be addressed. Any discrepancy >2-mm should have been addressed during the previous phases of treatment. A discrepancy of 1- to 2-mm or more between the midlines is usually due to a tooth size discrepancy and will probably result in an inadequate occlusal relationship, at least in one of the buccal segments (Class II or Class III on one side) (Fig. 27-9). The midline objectives in the finishing stage are evaluated in the extraoral finishing category as well, particularly in the upper arch.
Extraoral Objectives
The extraoral objectives are based on esthetic concepts, with the majority of these concerning the smile. The key factors within the smile that must be addressed are smile arc, incisor display, gingival display, buccal corridors, incisal plane, midlines, upper incisor third-order inclination, and tooth morphology in the esthetic zone.
Smile Arc
The ideal smile arc is discussed in Chapter 1. In the finishing stage, little can be done to significantly affect the smile arc. Small finishing bends can differentially extrude or intrude the anterior teeth but that is about all that can be accomplished. The dilemma concerning these wire bends is the potential for antagonistic effects on the interocclusal finishing objectives. An example of this is seen when the overbite is perfect and the teeth need to be extruded to achieve an ideal smile arc. A choice between achieving an esthetic objective (ideal smile arc) and an occlusal objective (ideal overbite) is needed. A compromise might be the best decision. In such situations the initial objectives of the individual treatment plan must be reviewed. More importantly, a limit to the amount of compromise for each characteristic should be set (i.e., avoiding finishing with >50% overbite and a flat or reverse smile arc).
Incisor Display
On average, females show 2- to 3-mm of incisor at rest and 1-mm of gingiva when smiling.12 Males show approximately 1-mm less incisor in each of these lip positions. During the diagnosis and treatment planning phases, an appropriate plan for correction of any deviation should be made. By the finishing phase of treatment the vertical incisor objectives should have already been accomplished. Detailing in this area should be limited to proper alignment and leveling of the incisal edges (provided no restorations are needed). Attempting to significantly intrude or extrude the incisors may complicate and prolong treatment.
Open-bite malocclusions with moderate to excessive incisor display present a challenge, as they are difficult to correct. It is not unusual to find an open-bite tendency still present at the finishing phase in this type of malocclusion. If no additional upper incisor display is desired, the overbite correction should be done by extruding the lower anterior teeth. This can be accomplished by accentuating the lower curve of Spee.
Gingival Display
The amount and characteristics of the gingival display (symmetry and height relationships of adjacent teeth) are important aspects to consider in a smile. Generally, males do not show any marginal gingiva when smiling. Females, on the other hand, display approximately 1-mm of gingiva on smiling.13 Symmetry in the gingiva and proper gingival height relationships in the upper arch are important considerations during initial bracket positioning and final finishing repositions (Fig. 27-10).
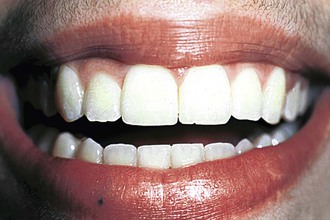
Figure 27-10 Finished treatment in a young female patient who displays the upper gingiva on smiling. An asymmetry in the gingival heights of the lateral incisors is evident.
During finishing, gingival display and symmetry can be altered within a narrow range of approximately 1-mm by selective intrusion or extrusion of any of the anterior teeth. Most frequently, the incisal edges will reflect gingival height asymmetries provided that incisal wear is not present (Fig. 27-11). The overbite will be the limiting factor of the magnitude of the finishing bends. However, if wear is present, the gingival height relationship will determine the finishing movements of the anterior teeth in the vertical dimension, instead of it being determined by the level of the incisal edges (Fig. 27-12).14 The final incisal edge position, if there is significant incisal wear, is determined by proper tooth proportions, gingival heights, relationship to the upper lip, crown/root ratio, and overbite (Fig. 27-13).
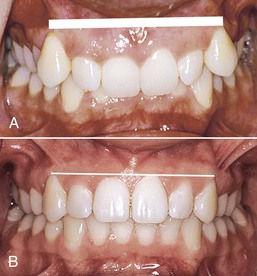
Figure 27-11 A, Incisal edges reflect the discrepancies in the gingival heights provided that no incisal wear is present. B, Correction of the incisal edges generally results in adequate gingival heights.
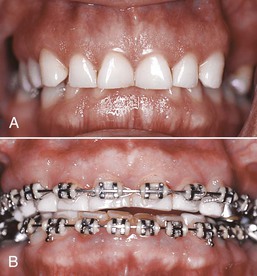
Figure 27-12 A, Inadequate gingival height in the upper anterior region with excessive overbite and worn incisors. B, Intrusion mechanics of the four upper anterior teeth to obtain proper gingival heights. Restoration of the incisors is needed to achieve adequate proportions and overbite.
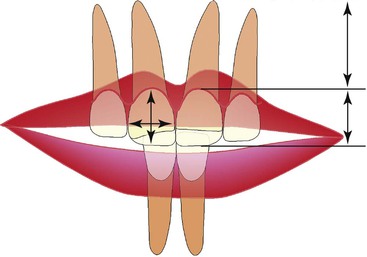
Figure 27-13 Factors involved in the final incisal edge position. The interrelationship of gingival height, tooth proportions, lip to tooth relationship, crown/root ratio, and overbite determines the position of the upper incisor in space.
Periodontal procedures should be considered as an adjunct to the esthetic objectives after finishing in patients with an excessive gingival display or asymmetrical gingival heights. The periodontal procedures that can be considered are gingivectomy or crown lengthening (depending on the alveolar bone level) (Fig. 27-14). These procedures may also be combined with prosthetic alternatives in patients with worn incisal edges or abnormally shaped incisors (i.e., peg laterals).

Figure 27-14 Asymmetrical gingival heights. A, Upper right lateral incisor has a more coronal gingival height. The upper right central incisor also has a slight coronal relationship of the gingival margin compared with its contralateral tooth. B, Gingivectomy performed on the upper right central and lateral incisors. C, Postsurgery.
A common unesthetic result after gingivectomies or crown lengthening (performed exclusively in the anterior segment) is seen in the transition area from the canine to the premolars. Ideally, there should be a 1-mm step down in gingival height between these teeth. When gingivectomies are not carried to the premolars, excess gingiva remains more pronounced in the corners of the smile (Fig. 27-15).15

Figure 27-15 Excess gingival show on the upper buccal segments. Gingival heights are adequate from canine to canine. A smoother transition from the canine to the first premolar can be obtained through periodontal surgical procedures.
In the literature little attention has been given to the gingival heights of the lower teeth. Symmetry and gingival height of the lower incisors in relation to the canines are important factors, especially in individuals over 30 years of age, as the lower gingival margin is more visible.12 It is not uncommon to find a discrepancy in gingival heights between the lower incisors and the canines, particularly in deep bite patients (Fig. 27-16). In young patients, the gingival margin usually follows the incisal edges of the lower anterior teeth. This problem is corrected as the canines and central incisors are leveled during the initial phases of orthodontic treatment. In the adult, wear facets can complicate the determination of where proper gingival heights should be located. As the incisors supraerupt, a good incisal edge relationship with the canines will exist but a significant discrepancy in the gingival height will develop. To correct this discrepancy a decision must be made from the following choices: gingivectomy/crown lengthening to match gingival heights with no restorations, gingivectomy/crown lengthening and restorations (composites or veneers or crowns), intrusion of the four anterior teeth to level the gingival heights (no surgery), and restorations (composites, veneers, or crowns). A very important additional factor in deciding among these alternatives is the crown/root ratio. Any osseous resective periodontal procedure (crown lengthening) increases this ratio; therefore a good assessment of the eventual remaining root structure is required (Fig. 27-17).

Figure 27-16 Discrepancy between the gingival heights of the lower incisors and the canines. Supraeruption of the lower incisors is evident at the incisal edges and is reflected on the overbite.
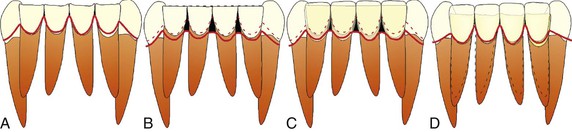
Figure 27-17 A, Significant attrition with supraeruption of the lower incisors. Different treatment modalities include the following. B, Gingivectomy/crown lengthening to match the gingival heights. As the gingival margin is brought down, a more tapered crown morphology is observed. Black triangles may result with this alternative. C, Gingivectomy/crown lengthening with additional restorations (crowns or veneers). The crown morphology is restored to normal tooth proportions and the crown/root ratio is increased. D, Orthodontic intrusion plus restorative procedures. The crown/root ratio is more favorable.
Buccal Corridors
The esthetic objective of widening the narrow buccal corridors, if indicated (see Chapter 1), should have been achieved long before the finishing stage. Any type of arch expansion during the finishing stage is difficult to achieve and unstable in the long-term.
Incisal Plane
In the frontal view, a cant in the upper incisor segment is sometimes found during finishing procedures. This cant may be limited to the incisor segment or involve the entire maxillary arch. The incisal cant can be the result of incorrect bracket positioning, asymmetrical mechanics, or a true maxillary skeletal cant that was undetected during diagnosis due to dental compensations. Therefore a differential diagnosis between a dental and a skeletal incisal cant is important.
Patients who have an incisal cant due to a skeletally canted maxilla generally present with uneven heights between the labial commissure and the occlusal surfaces of the premolars (Fig. 27-18). This can also be identified by an uneven gingival display between the left and right sides when smiling. Care must be taken when developing a differential diagnosis between a true maxillary cant (skeletal etiology) and an asymmetrical smile (soft tissue etiology). A true maxillary cant is difficult to correct and, when the discrepancy is excessive, a maxillary Le Fort I osteotomy may be the best treatment. Other alternatives may involve periodontic and prosthodontic options to camouflage the cant (see Fig. 27-18, B).
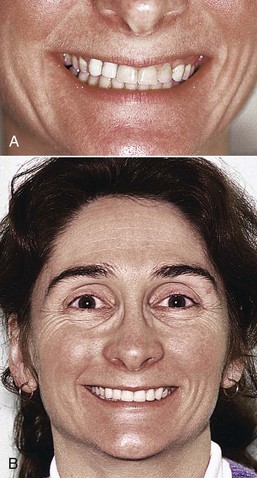
Figure 27-18 A, Occlusal cant of the maxilla evidenced on the left side. Gingiva is displayed only on the left side in relation to the labial commissure. B, Cant was camouflaged by prosthodontic work. Crowns were elongated on the right side and shortened on the left. Interproximal contacts were made more parallel to the facial midline.
In patients where the cant involves only the anterior teeth, corrections in the finishing stage are difficult but possible. An option is to place an intrusive force on the area that needs to be intruded (Fig. 27-19).16,17 If the rotation of the anterior segment needs to be around the center of resistance, two cantilevers (with equal and opposite forces that produce a couple) may be placed to achieve intrusion of one side and extrusion of the opposite side (Fig. 27-20, A). A second method to achieve rotation around the center of resistance is to place a cantilever in an auxiliary tube of the anterior segment (Fig. 27-20, B).
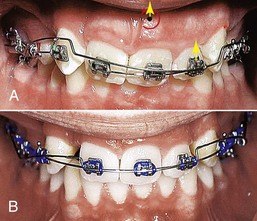
Figure 27-19 Asymmetrical intrusion arch placed to correct the incisal cant. A, A 0.017-inch × 0.025-inch nickel-titanium (Ni-Ti) intrusion arch is tied to the distal aspect of the upper left lateral incisor. A continuous 0.017-inch × 0.025-inch stainless steel segment from the upper right central incisor to the upper left lateral incisor is tied into the brackets of these teeth. The force system produces an intrusive force (yellow arrows) and a moment at the center of resistance (red curved arrow) of the anterior segment. B, Correction seen 1 month later. The cant was corrected and the midline discrepancy had improved.
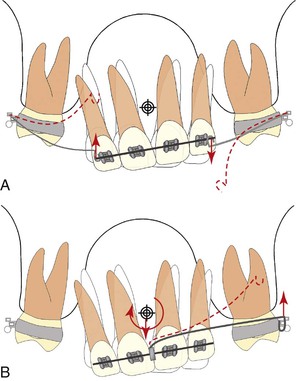
Figure 27-20 A, Moment produced by two cantilevers with the same amount of force in opposite directions. B, Moment produced by a cantilever with the single couple tied to an auxiliary tube in the anterior segment. A transpalatal arch is used in both situations as a solid anchor unit to minimize the side effects.
Midlines
A discrepancy between the upper and lower dental midlines is generally most noticeable at the end of treatment. Coincidentally, it is also at this time that this problem is most difficult to correct. To achieve coincident midlines during finishing, the range of correction for each arch is approximately 1-mm to each side. Tipping is the major type of tooth movement that can be used to correct midlines at the finishing stage. It is important to stress that a slight discrepancy between the upper midline is esthetically acceptable18–20 and generally does not have any functional implications.
On occasion there is a relationship between an incisal cant and a midline discrepancy. By correcting the incisal cant the midline problem may be improved (see Fig. 27-19), although in some instances the midline discrepancy might be accentuated. It is important to consider all smile characteristics together; correction of one characteristic should maintain, if not improve, the others.
The techniques used to correct midline problems during the finishing phase mainly rely on the use of anterior cross elastics. In some instances a combination of Class II elastics on one side and Class III elastics on the other side can be used. This method seems easy but can result in serious side effects if used indiscriminately. The orthodontist must watch for the side effects that may occur in the vertical and transverse planes with this method of long-term elastic use. In the vertical direction, canting of the occlusal plane as a result of the vertical component of the anterior cross elastic force may occur (Fig. 27-21). In the transverse plane, rotation of the dental arches around the y axis with the use of Class II or Class III elastics may result in a crossbite tendency on one buccal segment and a Brodie bite tendency on the other (Fig. 27-22).21
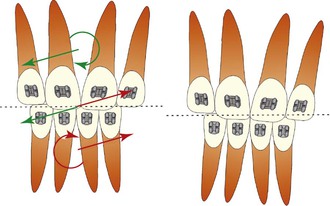
Figure 27-21 Vertical effects produced by an anterior cross elastic. The vertical component of the elastic force to correct midline discrepancy may produce canting of the incisal plane.
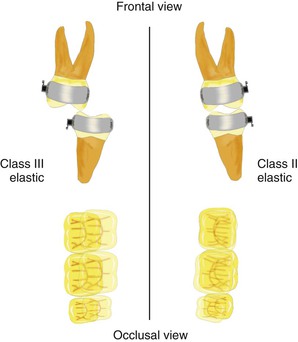
Figure 27-22 Class II and Class III elastics produce rotation around the y axis. Brodie bite tendency is seen on the Class III elastic side and a crossbite tendency is seen on the Class II elastic side.
A final method to correct the dental midline in the finishing stage is the use of a cantilever with the active force along the x axis. The upper anteriors are treated as a segment and a force is applied at the bracket level of this segment. The anchor unit (posterior segment) is made up of the molars and premolars. A palatal arch is used to offset the rotational moment and lingual force on the anchor unit where the cantilever (couple side) is inserted (Fig. 27-23).
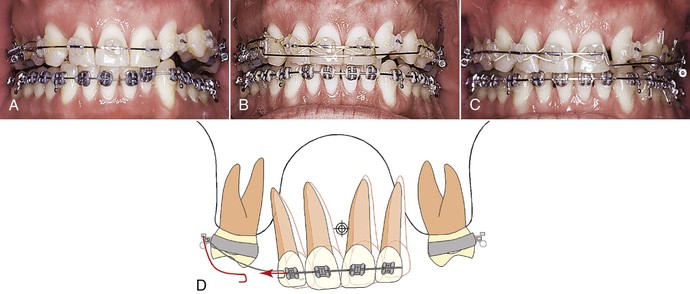
Figure 27-23 Method for correction of small midline deviations. A, Upper incisors tipped to the left with a midline deviation of approximately 2-mm. B, Force system in place (see D for detailed illustration.). A transpalatal arch offsets the moment on the posterior segment (mesial in). A continuous base arch bypassing the incisors aids in preventing their extrusion as they tip. The cantilever can be tied directly to the anterior segment. An elastic was placed for patient comfort. C, Force from the cantilever tips the teeth in the direction of the midline correction. D, Force system.
Upper Incisor Third-Order Inclination
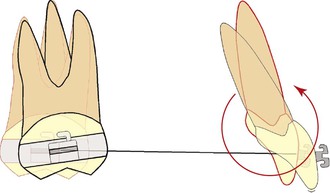
Esthetic considerations of the upper incisal inclination are important not only from the profile view, but also from the frontal view. A common occurrence in the final stages of treatment, particularly in extraction cases, is excessive lingual crown torque. Although this is easily visualized in the lateral view, it can also be appreciated in the frontal view.22 Third-order tooth corrections are difficult and time-consuming movements.
Extensive bone remodeling needs to occur as root correction is pursued and side effects such as upper molar mesial migration become common. Perhaps the best way to approach this objective is by maintaining a proper moment/force ratio during the retraction phase in extraction cases.23 Some of the alternative mechanics in the finishing phase include auxiliary torquing springs (Fig. 27-24). Care must be taken to prevent the incisors from flaring if only root correction is needed. This can be achieved by cinching the archwires or lacing together the entire arch. The clinician must also be aware of the rowboat effect that is generated with root correction (Fig. 27-25).24 Simultaneous use of Class II elastics is recommended to prevent this effect. Additionally, a mild bowing of the anterior segment with the torquing spring is expected due to the intrusive lateral forces on the posterior segment.

Figure 27-24 A, Upright upper incisors with anterior crossbite tendency. The torquing spring produces an anterior moment and an extrusive force needed in the anterior segment. The upper arch is laced together to prevent anterior spacing. B, Correction seen after 1 month. C, Final correction achieved in approximately 3 months.
Tooth Morphology
Tooth morphology in the anterior or esthetic zone is of primary importance. The upper lateral incisors most often exhibit abnormal morphology in this zone. It is less common to find abnormally shaped central incisors. Preliminary planning regarding the space distribution for restoring teeth with abnormal morphology should be accomplished during the diagnosis and treatment planning phase. Involving a restorative dentist and a periodontist during the treatment planning phase is a good practice. In the finishing phase, communication within the team is crucial and will help to determine any precise finishing orthodontic tooth movements needed. Many of the restorative procedures should be done in conjunction with periodontal procedures to achieve the best tooth proportions.
Tooth proportions are influenced by the position of the gingival margin as well as the width and height of the tooth. These factors can be affected by the restorative dentist in conjunction with the periodontist. The shape of the incisor and the restorative option (composite buildup, veneers, or crowns) will determine the position of the abnormally shaped lateral incisor within the dental arch.15
It is of primary importance in achieving excellent esthetic results that good communication is maintained with the restorative dentist. Slight contouring of the incisal edges of the upper anterior teeth, especially the canines, has been recommended at the end of treatment for most patients.25 The incisal edges of the anterior teeth with a small incisal edge fracture can also be contoured after previous extrusion. The gingival height relationship to the adjacent tooth may be altered with the extrusion of the incisor; thus an additional gingivectomy or crown lengthening procedure may be indicated if the patient displays gingiva on smiling. In patients with congenitally missing lateral incisors that have been treated by canine substitution, the alteration of canine morphology to mimic a lateral incisor is usually done in the early stages of treatment, with small detailing left for the finishing stages (Fig. 27-26). The premolars that substitute for canines also need to be contoured on the lingual cusps to avoid balancing interferences. One important consideration often overlooked in the esthetics of canine substitution is the emergence profile of the canine. To replicate the anatomy of the lateral incisor, significant lingual root torque is necessary in the canine. This small detail enhances the possibility of mimicking the lateral incisor and allows the restorative dentist to achieve a better esthetic result (Fig. 27-27).

Figure 27-27 A, Patient with canine substitution showing good esthetic results. B, Note the reduced canine prominence and the similar emergence profile of a maxillary lateral incisor.
The final situation in which abnormalities in tooth morphology are considered during finishing is the pronounced lingual fossae of the upper incisors. This abnormal crown morphology is found most frequently in Asian and African populations.26 In these patients the mesial and distal ridges adjacent to the fossa are pronounced and prevent a good intercuspation in the buccal segments. It is recommended that the height of these ridges should be reduced to achieve better posterior occlusion.
Radiographic Objectives
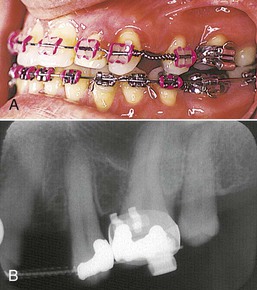
Just before starting the finishing stage of treatment, it is always recommended that a panoramic radiograph be taken to evaluate root angulation and root parallelism. Problems in second-order angulation of the upper lateral incisors, lower premolars, and teeth adjacent to the extraction sites are commonly found (Fig. 27-28). Clinically, marginal ridge discrepancies are also a good method to detect possible root angulation discrepancies. However, the panoramic radiograph provides better evidence of root position, angulation, and parallelism.

Figure 27-28 Finished four-premolar-extraction (upper first premolars and lower second premolars) patient with poor root alignment of the lower first premolars and upper laterals.
Root angulation problems observed in the finishing panoramic radiograph might also be related to abnormal tooth morphology and/or bracketing errors. This is especially evident in the buccal segments, where it is difficult to gain access for bracket placement and premolars with abnormal crown morphology are common.
Root parallelism is important for three reasons. First, the occlusal load of the forces will be transmitted properly across the longitudinal axis of the tooth. Second, in patients where only the crown has been tipped and the root is not in its proper position, there is a greater potential for relapse.27 Finally, there is a potential for periodontal problems due to root proximity. However, the rationale for this last statement is not well supported by the literature; no deleterious effects on the periodontium have been found in finished orthodontic cases with root proximity.28
The finishing panoramic radiograph is also helpful in evaluating root resorption. If external apical root resorption is observed, the orthodontist may want to decrease the length of time spent on the finishing stage. Although monitoring for root resorption has been recommended during the first 6 months of treatment,29,30 usually it is noticed on the finishing panoramic radiograph.
Finally, two other important pieces of information can be obtained from a panoramic radiograph: evidence of any deterioration in periodontal health and the eruption angle of the third molars. If the eruption of the second molars is delayed or the orthodontic treatment is being finished before complete eruption of the second molars, it is important to evaluate their position and the eruption pattern (Fig. 27-29).

Figure 27-29 Panoramic x-ray should be taken before appliance removal to evaluate root apices, root parallelism, and status of unerupted teeth. This panoramic x-ray reveals an abnormally erupting second molar, which was noticed only after appliance removal.
Periapical radiographs are usually indicated only in the finishing stage to obtain a more detailed view of any significant findings observed in the panoramic radiograph, such as extensive root resorption, root parallelism between adjacent teeth to an implant site, or evidence of periodontal bone loss.
Functional Objectives
A proper functional occlusion is the goal in every orthodontic treatment. However, as mentioned in Chapter 1, the definition of an ideal functional occlusion is not completely clear. In general, a mutually protected occlusion is considered the ideal goal.
To achieve this ideal occlusion during the finishing stage, it is important to have the maximum amount of normal occlusal contacts during maximum intercuspation. Although a coinciding centric relation with centric occlusion is the goal proposed by some clinicians, a small discrepancy between these two occlusal relationships is acceptable (long centric).11
With lateral movements of the jaw, a canine disclusion is the standard, although group function is acceptable. More importantly, no balancing contacts should be present. Canine disclusion is also a major protective factor in patients who receive any type of anterior esthetic restorations (veneers, composites, or porcelain crowns). Finally, the anterior teeth should disclude the posterior teeth during protrusive movements. All of these movements should be evaluated during the finishing stage and proper adjustments in crown angulations (relative to tip and torque) should be achieved. Small adjustments can be made after appliance removal (e.g., occlusal adjustments with rotary instruments); however, these should be minimal, as there is a limit to the amount of tooth structure that can be removed.
Overcorrection
Rotational Correction
During finishing, the concept of overcorrection can be applied to the alignment (first-order corrections) and to certain malocclusions.10,31–33 It is believed by some that overcorrection of rotated teeth, especially in the anteroinferior segment of teeth, may be necessary for stability. Since the amount of, and to a certain extent the direction of, rotational relapse is unpredictable,34 this practice may not be indicated.
Vertical Correction
Overcorrection in some malocclusions, such as open-bite and deep bite cases, may be beneficial. This process ideally should begin during initial bracket placement but even during the finishing stage the clinician can fine-tune the process. Brackets on the anterior teeth could be placed 0.5-mm more gingival in cases with an open-bite tendency and 0.5-mm more incisal in deep bite cases.
Unique Finishing Situations
Lower Incisor Extraction
Lower incisor extraction treatment introduces a Bolton (tooth size) discrepancy that complicates orthodontic finishing. If no tooth size discrepancies are present (i.e., excessive tooth mass in the lower arch), the patient will generally finish with either a Class I canine relationship with excessive overjet or an ideal overjet and a Class III canine tendency relationship (Fig. 27-30).

Figure 27-30 A–C, Patient with a lower incisor extraction finished with an ideal overjet but a Class III tendency on the right side and poor interdigitation. Gingival contours are not ideal, especially in the area of incisor extraction.
Another problem frequently observed with incisor extractions is that the patient ends up with black interproximal triangles in the lower incisor segment (Fig. 27-31). To solve this problem, slight interproximal enamel reduction and/or root reapproximation on the lower teeth is done to move the contact more gingivally and to decrease the size of these black triangles. To some degree this procedure will accentuate the overjet because more tooth structure is removed from the lower anterior incisors, thus increasing the inter-arch tooth size discrepancy. Finally, major efforts should be made to coordinate the arches as the lower incisor extraction space is closed. Lower incisor extraction also results in a decrease in the intercanine distance35 and thereby an excessive canine overjet could occur (see Figs. 27-30, B, and 27-31).
Finishing with Primary Teeth
Finishing can be challenging when a patient is missing permanent teeth (most commonly second premolars) and has overretained or ankylosed primary molars. Some advocate extraction of the primary molar and closure of the space while others believe that the primary molar should be kept for as long as possible and then be restored with an implant or bridge on its eventual loss.36 The extent of finishing and detailing would depend on the initial treatment objectives of the individual case and any planned compromises in the buccal segment occlusion should be discussed with the patient and/or parent.
Bypassing Debilitated Teeth during Finishing
In certain clinical situations, after taking a finishing panoramic radiograph there may be evidence of localized root resorption. Two options are available: minimize the time spent on the finishing stage or bypass the affected tooth in order to avoid any force that will perpetuate the root resorption. Figure 27-32 illustrates the latter option during finishing. Sound biomechanical principles should be used to achieve the desired tooth movement with minimum side effects (the ideal objective during finishing).
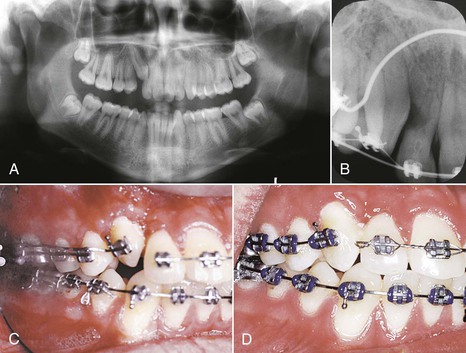
Figure 27-32 A and B, Patient with extensive root resorption on the upper right lateral tooth. C, This tooth was bypassed using segmental mechanics to position the canine in the arch. A 0.017-inch × 0.025-inch stainless steel segment was placed from the upper right first molar to the first premolar. A transpalatal arch (not seen) connected this segment to the other side of the arch. A 0.017-inch × 0.025-inch CNA beta-titanium segment was tied from the molar to the canine. The resultant geometry of the two-couple force system produced a distal crown tip and intrusive force on the canine in the second order. The intrusive force was counteracted by a vertical elastic. D, Canine correction in 4 weeks. Finishing detailing for the canine was done by sectioning the wire without engaging the upper right lateral incisor.
Canine Substitution of Missing Lateral Incisors
When canines replace lateral incisors, it is difficult to adjust their morphology to resemble that of lateral incisors. Ideally, the majority of the canine contouring should have been accomplished in the early phases of treatment. During finishing, only minor contouring should be done in consultation with the restorative dentist.
One of the most challenging esthetic concerns for the restorative dentist in these situations is the gingival heights. In a patient with normal gingival architecture, the premolar that is replacing the canine usually has a gingival height that is 1- to 1.5-mm occlusal than that of the canine, and the canine's gingival height is usually at the same level of the central incisor. To achieve proper gingival heights, the canine substituting the lateral incisor morphology should be extruded slightly (approximately 0.5- to 1.0-mm) and for the premolar replacing the canine, the only option is a periodontal resective procedure.
However, this periodontal procedure must be done with caution, as the anatomic crown height of the premolar is much smaller than that of the canine and such a procedure may end up exposing the cementum on the facial aspect of the premolar.
Another challenge with canine substitution concerns lingual cusp contouring of the upper first premolar. This cusp should be reduced mainly for functional reasons to avoid balancing interferences during disocclusion. Care should be taken not to remove excessive amounts of tooth structure, in order to avoid postoperative sensitivity.
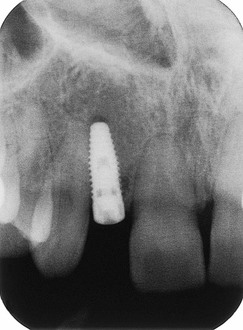
Edentulous Site for an Implant
One of the most common mistakes made when an edentulous space is prepared to receive an implant is to leave inadequate space. The minimum space that should be opened for an implant is approximately 6-mm. This measurement derives from the 3.5-mm mesiodistal width of the fixture and the 1-mm mesial and distal space to the fixture for a papilla in the interproximal space.37
The restorative dentist encounters not only a space problem at the coronal level, but also a root angulation problem of the teeth adjacent to the implant site at the apical level. Since the space is usually achieved by a push coil mechanism at the coronal level, the roots of the teeth tip into the implant space (Fig. 27-33). During finishing, adequate moments for root correction should be placed in these adjacent teeth to achieve the minimum 6-mm distance throughout the entire implant site. It is important to note that new developments in implant fixture shape (anatomically shaped implants) allow more leeway in this respect (Fig. 27-34). The key to success in such a multidisciplinary case scenario is coordination between the orthodontist, oral surgeon, and prosthodontist.
Interproximal Reduction during Finishing
Interproximal tooth reduction generally has been advocated where tooth size discrepancies exist and in some instances it has been recommended during finishing. This procedure is used to achieve a better occlusal relationship in the finishing stages.25 Since the amount of interproximal enamel reduction is limited, it should be noted that tooth size discrepancies should be evaluated during the diagnosis phase to avoid last-minute quick-fix solutions in the finishing stage and to prevent long-term tooth sensitivity. Thus a slight interproximal reduction of certain teeth with abnormal morphology contributing to the discrepancy, usually between the upper lateral incisors and the lower second premolars,8 can be done selectively instead of reducing teeth indiscriminately as a result of inappropriate diagnosis and treatment planning.
Finishing with Class II Mechanics
Usually, in Class II mechanics using elastics or inter-arch Class II appliances, correction of the malocclusion is achieved by rotating the occlusal plane in a clockwise direction. As a result, the maxillary incisors finish with a retroclined angulation (Fig. 27-35). To address this problem, torque needs to be applied to the anterior teeth. This can be accomplished using a bracket prescription with an excessive amount of torque for the anteriors (i.e., 17 degrees or more) or by applying buccal crown torque to the archwire (via individual bends or adding a gentle curve of Spee). Another method involves using a torquing spring that adds a moment to the teeth that will correct the root angulation (see Fig. 27-24).
Finishing Sequence
Figure 27-1 provides a schematic outline and checklist that clinicians can use to address finishing in orthodontics. Third-order objectives during finishing should be addressed first since these usually take the most time to correct. The buccolingual inclination of the upper anterior segment is important in the finishing stage for occlusal and esthetic reasons. Proper incisor inclination is a key factor in achieving good buccal occlusion and an esthetic smile.
The major factors involved in achieving this proper anterosuperior incisor inclination are the bracket and wire coupling. Therefore, depending on the existing buccolingual inclination of the tooth and the relation of the bracket to the occlusal plane, a specific archwire with a medium-to-low load deflection rate (such as a 0.017-inch × 0.025-inch beta-titanium CNA archwire; Ortho Organizers Inc., San Marcos, CA.) can be selected. For example, if a patient has a lingual inclination of the crowns of the upper incisors, a counterclockwise moment given by the coupling between the wire and the bracket is needed to achieve a proper buccolingual inclination. Another option is to increase the dimension of the rectangular wire in a preadjusted bracket system (e.g., 0.021-inch × 0.025-inch in a 0.022-inch slot size bracket) while trying to maintain a medium load deflection (achieving the desired moment) or adding bends to the existing archwire to create the couple. Other options include selecting the proper prescription for patients in whom loss of third-order control in the incisors is anticipated or changing from a 0.022-inch slot to a 0.018-inch slot in the anterior segment. Torque is affected significantly by archwire dimension and edge shape as well as by bracket slot dimension.38
In the straight-wire appliance, proper third-order angulation can be achieved through rectangular archwires engaged into prescription brackets that can then express the torque of the appliance. For additional third-order correction on specific teeth, a 0.019-inch × 0.025-inch beta-titanium CNA (Ortho Organizers Inc.) is recommended. Third-order bends are placed in this archwire, which provides an adequate load-deflection rate39 to achieve proper buccolingual inclination.
After the third-order objectives are met, second-order movements are addressed. Adjustments in this plane take a significant amount of time because they also involve root correction. To achieve second-order objectives, either with a 0.016-inch × 0.022-inch beta-titanium CNA (Ortho Organizers Inc.) or a 0.016-inch steel round archwire can be used, provided that all third-order objectives have been met. This allows marginal ridge discrepancies and root parallelism problems to be corrected.
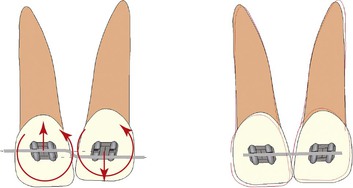
The final step in finishing is the correction of first-order problems. Usually these problems are obvious clinically and can be corrected quickly. In many instances only small correction bends in the archwire are needed. Correction can also be achieved with auxiliary plastic rotation wedges on the brackets or by making small bends in either the 0.016-inch × 0.022-inch beta-titanium CNA (Ortho Organizers Inc.) or the 0.016-inch steel archwire.
All of the finishing bends placed in an archwire will result in either a V-bend or a step bend.40 Care must be taken, as all of these bends will have vertical side effects and rotational tendencies on the adjacent teeth (Fig. 27-36).
Inter-arch objectives are the last to be addressed in the finishing stage. In many instances the intra-arch adjustments mentioned above will result in a good occlusion. To achieve good final intercuspation of the buccal segments, vertical elastics may be worn for a short period of time, usually 2 to 3 weeks.
It is important to note that although some orthodontists expect settling of the occlusion to occur during retention, the amount of settling is unpredictable41 and in some patients it may not occur. Care must also be taken with the elastics in the finishing stages. Prolonged wear of vertical elastics with light or no archwires may result in deformation of the arch form and/or lingual inclination of the teeth (Fig. 27-37) as a result of the elastic force applied buccally to the center of resistance (see Fig. 27-37, C).
Summary
The literature addressing the topic of orthodontic finishing is scarce. Most of the approaches and theories on finishing are anecdotal and subjective in nature. This supports the idea that orthodontic finishing is predominantly an art rather than a science. The common consensus on guidelines to evaluate finishing are described by the ABO standards. The evaluation is based on intraoral criteria and does not incorporate esthetic or functional objectives. This chapter provides an overview of the most important aspects of finishing using sound biomechanical principles. The goals for each of the four categories (intraoral objectives, extraoral objectives, radiographic objectives, and functional objectives) are described. The key to good orthodontics relies heavily on the diagnosis, treatment planning, and application of good mechanics. The key to excellence in orthodontics lies in the ability to identify and correct the small details needed for a perfect smile with an ideal occlusion.
References
1. Andrews LF. The six keys to normal occlusion. Am J Orthod. 1972;62:296–309.
2. Casko JS, Vaden JL, Kokich VG, et al. Objective grading system for dental casts and panoramic radiographs. American Board of Orthodontics. Am J Orthod Dentofacial Orthop. 1998;114(5):589–599.
3. Bennett JC, McLaughlin RP. First molars. Bennett JC, McLaughlin RP. Orthodontic Management of the Dentition with Preadjusted Appliance. Mosby: St. Louis, MO; 2002:281–310.
4. McNamara JA Jr. Transpalatal arches. McNamara JA Jr, Brudon WL. Orthodontics and Dentofacial Orthopedics. Needham Press: Ann Arbor, MI; 2001:199–209.
5. McNamara JA Jr. The transverse dimension. McNamara JA Jr, Brudon WL. Orthodontics and Dentofacial Orthopedics. Needham Press: Ann Arbor, MI; 2001:97–110.
6. Zachrisson BU. Making the premolar extraction smile full and radiant. World J Orthod. 2002;3:260–265.
7. Bolton WA. The clinical application of a toothsize analysis. Am J Orthod. 1962;48:504–529.
8. Smith SS, Buschang PH, Watanabe E. Interarch tooth size relationships of 3 populations: “does Bolton's analysis apply? Am J Orthod Dentofacial Orthop. 2000;117:169–714.
9. Swartz M. Comprehensive fixed appliance therapy. McNamara JA Jr, Brudon WL. Orthodontics and Dentofacial Orthopedics. Needham Press: Ann Arbor, MI; 2001:149–168.
10. JCO interviews Dr, Bjorn U. Zachrisson on excellence in finishing, part 1. J Clin Orthod. 1986;20(7):460–482.
11. Ash MM, Ramfjord S. Occlusion. 4th ed. WB Saunders: Philadelphia, PA; 1995.
12. Vig RG, Brundo GC. The kinetics of anterior tooth display. J Prosthet Dent. 1978;39:502–504.
13. Tjan AH, Miller GD. Some esthetic factors in a smile. [The JG] J Prosthet Dent. 1984;51(1):24–28.
14. Kokich VG, Spear FM. Guidelines for managing the orthodontic-restorative patient. Semin Orthod. 1997;3(1):3–20.
15. Poling R. A method of finishing the occlusion. Am J Orthod Dentofacial Orthop. 1999;115:476–487.
16. van Steenbergen E, Nanda R. Biomechanics of orthodontic correction of dental asymmetries. Am J Orthod Dentofacial Orthop. 1995;107:618–624.
17. Nanda R, Margolis MJ. Treatment strategies for midline discrepancies. Semin Orthod. 1996;2(2):84–89.
18. Johnston CD, Burden DJ, Stevenson MR. The influence of dental to facial midline discrepancies on dental attractiveness ratings. Eur J Orthod. 1999;21(5):517–522.
19. Kokich VO, Kiyak HA, Shapiro PA. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 1999;11:311–324.
20. Beyer JW, Lindauer SJ. Evaluation of dental midline position. Semin Orthod. 1998;4:146–152.
21. Burstone CJ. Diagnosis and treatment planning of patients with asymmetries. Semin Orthod. 1998;4:153–164.
22. Peluso C, Kuhlberg A. The axial inclination of central incisors and its effects on the perception of the facial profile. Paper presented at: Annual American Dental Association Meeting; October 2002; Memphis, TN.
23. Uribe F, Nanda R. Treatment of Class II, Division 2 malocclusion in adults: biomechanic considerations. J Clin Orthod. 2003;37:599–606.
24. Shroff B. Root correction during orthodontic therapy. Semin Orthod. 2001;7:50–58.
25. McNamara JA, Nolan PJ, West KS. Finishing and retention. McNamara JA Jr, Brudon WL. Orthodontics and Dentofacial Orthopedics. Needham Press: Ann Arbor, MI; 2001:453–474.
26. Kharat DU, Saini TS, Mokeem S. Shovel-shaped incisors and associated invagination in some Asian and African populations. J Dent. 1990;18:216–220.
27. Hatasaka HH. A radiographic study of roots in extraction sites. Angle Orthod. 1976;46:64–68.
28. Artun J, Kokich VG, Osterberg SK. Long-term effect of root proximity on periodontal health after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1987;91:125–130.
29. Levander E, Bajka R, Malmgren O. Early radiographic diagnosis of apical root resorption during orthodontic treatment: a study of maxillary incisors. Eur J Orthod. 1998;20:57–63.
30. O’Hea CM. A prospective investigation of maxillary central incisor root resorption incident to orthodontic therapy [Masters thesis]. Department of Orthodontics, University of Connecticut: Farmington, CT; 1999.
31. Joondeph D. Retention and relapse. Graber TM, Vanarsdall RL. Orthodontics: Current Principles and Techniques. 3rd ed. Mosby: St. Louis, MO; 2000:985–1012.
32. Proffit WR. The third stage of comprehensive treatment: finishing. Proffit WR. Contemporary Orthodontics. 3rd ed. Mosby: St. Louis, MO; 2000:578–596.
33. McLaughlin R, Bennett J. Finishing with the preadjusted orthodontic appliance. Semin Orthod. 2003;9:165–183.
34. Little RM, Riedel RA, Artun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop. 1988;93:423–428.
35. Faerovig E, Zachrisson BU. Effects of mandibular incisor extraction on anterior occlusion in adults with Class III malocclusion and reduced overbite. Am J Orthod Dentofacial Orthop. 1999;115:113–124.
36. Kokich VO Jr. Congenitally missing teeth: orthodontic management in the adolescent patient. Am J Orthod Dentofacial Orthop. 2002;121:594–595.
37. Spear FM, Mathews DM, Kokich VG. Interdisciplinary management of single-tooth implants. Semin Orthod. 1997;3:45–72.
38. Archambault A, Lacoursiere R, Badawi H, Major PW, Carey J, Flores-Mir C. Torque expression in stainless steel orthodontic brackets: a systematic review. Angle Orthod. 2010;80(1):201–210.
39. Johnson E. Relative stiffness of beta titanium archwires. Angle Orthod. 2003;73:259–269.
40. Burstone CJ, Koenig HA. Creative wire bending: the force system from step and V bends. Am J Orthod Dentofacial Orthop. 1988;93(1):59–67.
41. Parkinson CE, Buschang PH, Behrents RG, Throckmorton GS, English JD. A new method of evaluating posterior occlusion and its relation to posttreatment occlusal changes. Am J Orthod Dentofacial Orthop. 2001;120:503–512.