Continuing professional development and revalidation
Introduction
This chapter is designed to develop an understanding of continuing professional development (CPD) and to consider the importance to pharmacists and pharmacy technicians of individual active engagement in an ongoing programme of CPD.
In the UK and many other countries, CPD is mandatory for pharmacists and pharmacy technicians. It is relevant to all pharmacists and pharmacy technicians, whether experienced or newly qualified and just starting a career, or working full-time or part-time. CPD is part of being a professional with an obligation on all to continue to enhance their own knowledge and skills throughout their career and working life.
CPD is related to, and indeed part of, clinical governance (see Ch. 9). Clinical governance is about both continuous quality improvement and being accountable for quality improvement. As such, CPD is an integral part of clinical governance and it involves all healthcare professionals. Those healthcare professionals working in the UK NHS will find there are specific requirements for clinical governance and CPD, which are mandatory. The Community Pharmacy Contract (England) with the NHS states a clear need for community pharmacists to be undertaking and maintaining CPD records within the clinical governance requirements. In addition to this in the UK, the Standards of conduct, ethics and performance of the GPhC places further obligations on pharmacists. Before any service is offered, whether to prescribers, patients or others, a pharmacist must ensure that whoever is delivering the service has a relevant level of competence, skill or knowledge in that area. CPD allows the pharmacist to provide evidence and demonstrate competence.
What is continuing professional development?
The NHS defines it as ‘a process of lifelong learning for all individuals and teams which meets the needs of patients and delivers the health outcomes and healthcare priorities of the NHS and which enables professionals to expand and fulfill their potential’ (DH 1998). While this definition is accurate, it is somewhat lengthy. An easier option is to consider the three words individually:
 Continuing: this is about lifelong learning, an ongoing (or continuing) process regardless of the age of the pharmacist or the stage of their career
Continuing: this is about lifelong learning, an ongoing (or continuing) process regardless of the age of the pharmacist or the stage of their career
 Professional: this is focused on individual competence in a professional role, i.e. it is to do with the work of the pharmacist
Professional: this is focused on individual competence in a professional role, i.e. it is to do with the work of the pharmacist
 Development: this is about identifying and undertaking learning that improves the personal skills of the pharmacist to enhance patient care and career development, i.e. it changes for the better the work of the pharmacist.
Development: this is about identifying and undertaking learning that improves the personal skills of the pharmacist to enhance patient care and career development, i.e. it changes for the better the work of the pharmacist.
CPD can be defined as the process of reflection, planning, action and evaluation through which pharmacists and pharmacy technicians continuously develop their knowledge, skills, attitudes and behaviours throughout their professional careers.
The UK former pharmacy regulator (Royal Pharmaceutical Society of Great Britain) introduced a framework for CPD for pharmacists in 2002 in response to the requirements of the Health Act 1999.
Today, the concept of CPD is becoming a familiar process for the pharmacy profession. There is a formal (GPhC) requirement for CPD records to be completed and retained for the duration of a person’s registration in order to demonstrate their competence to undertake the role they are working in at the time.
CPD gives a pharmacist and pharmacy technician the opportunity to demonstrate to their employer, the NHS, and to patients, that they are maintaining and building their own professional capability.
Background to CPD
The requirement for formal CPD in the UK arose from increasing pressure on the government to ensure healthcare professions operate in a ‘professional’ manner. Recommendations for ongoing professional development suggested that CPD should not focus solely on clinical skills but should encompass both attitudes and communication skills. CPD is now mandatory for all pharmacists and pharmacy technicians in the UK. This means that pharmacists and pharmacy technicians must keep a record which shows they are ‘actively’ keeping up-to-date with the knowledge they use day-to-day. The records need to reflect the scope of practice in which the individual works. By keeping up-to-date, they are able to demonstrate ongoing competence in their current role(s), and prepare themselves for roles that they wish to pursue in the future.
The GPhC format for recording CPD involves keeping a written record of an activity or event, demonstrating that the individual has learnt from a situation relevant to their professional role. This written record can be kept as a paper-based record or as an electronic record.
Pharmacists and pharmacy technicians gain from taking ownership of their CPD, since CPD is a personal activity: it is specific to each individual. No two individuals will have the same CPD records. CPD is designed to help an individual structure and plan ways to ensure that their skills are constantly being updated and renewed. CPD puts pharmacists and pharmacy technicians in control of their learning.
CPD cycle
CPD is defined as a systematic, ongoing, cyclical process of self-directed learning. It should enable pharmacists and pharmacy technicians to do their job more effectively and involves employers as well as individuals.
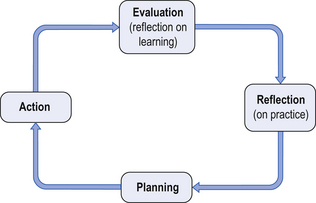
CPD is a four-stage process which helps individuals plan their learning and track, record and reflect on learning and development. The learning may be clinical or related to a skill, attitude or behaviour associated with their role. The four stages are often depicted as a cyclical process. The GPhC recording system is based on the four stages of the CPD cycle.
The four stages of the cycle are shown in Figure 6.1 and involve:
Reflection on practice
Reflection involves the individual spending time reflecting on current performance and how work is undertaken. The reflection time helps in identifying personal learning and development needs. Reflection involves thinking about how daily tasks are carried out, the areas in which the individual feels their knowledge or skills are weak or reflecting on events that have happened, which indicate a need to improve their knowledge or skills.
Sometimes a particular situation or event will draw the attention of the pharmacist to a weakness in knowledge, ability or systems of work which, if not addressed, could cause further problems. This is called a critical incident (see Ch. 10).
When reflecting, there are several questions which should be addressed:
 What knowledge gaps do I have when undertaking my current role?
What knowledge gaps do I have when undertaking my current role?
 What areas do I need to develop to further progress my career?
What areas do I need to develop to further progress my career?
 What have I done recently which I could improve next time?
What have I done recently which I could improve next time?
 What do I want to be able to do?
What do I want to be able to do?
 What extra skills can I offer my patients that would be of benefit to them?
What extra skills can I offer my patients that would be of benefit to them?
 What skills could I develop that would help deliver my organization goals more effectively?
What skills could I develop that would help deliver my organization goals more effectively?
Other ways of identifying learning needs or knowledge, skill, attitude or behaviour gaps, include the pharmacist or pharmacy technician considering the following activities:
 Asking colleagues for feedback on one’s own practice – how do they think you are doing? What do they think you could do differently?
Asking colleagues for feedback on one’s own practice – how do they think you are doing? What do they think you could do differently?
 Participating in new activities
Participating in new activities
 Formulating a development plan to structure future development
Formulating a development plan to structure future development
 Questions from customers/patients
Questions from customers/patients
 Learning from a past event, sometimes referred to as critical incident analysis
Learning from a past event, sometimes referred to as critical incident analysis
 Professional audit, measuring one’s own standard against current competencies for a similar role.
Professional audit, measuring one’s own standard against current competencies for a similar role.
An identified learning need is easier to address if broken down into bite-size pieces.
Planning
Having identified learning needs, the pharmacist or pharmacy technician needs to plan what can be done to meet these learning needs and how it can be achieved. If several learning needs have been identified, then they should be prioritized.
If more than one learning need has been identified, then more than one CPD cycle needs to be started. When planning actions to meet learning objectives, the following should be considered:
 What level of competence needs to be reached?
What level of competence needs to be reached?
 When does the learning objective need to be met by?
When does the learning objective need to be met by?
 What will be the impact of the learning on customers, colleagues, the organization and the pharmacist?
What will be the impact of the learning on customers, colleagues, the organization and the pharmacist?
 What activities can be undertaken to best meet needs?
What activities can be undertaken to best meet needs?
 What activities lead to the best learning? (This will differ for each individual.)
What activities lead to the best learning? (This will differ for each individual.)
At this stage, there needs to be consideration of what the consequence of not undertaking the learning would be. If the learning need is no longer urgent or important, then it is appropriate not to take it any further.
When considering how to meet learning needs, there are a number of ways that learning can be undertaken. The list below is not exhaustive:
Action
Action is simply carrying out the plan. The time taken to undertake the learning needs to be built into the plan and the timetable adhered to.
Questions to be asked while undertaking the actions are:
As these questions are answered, a record should be made of what has been learnt.
Evaluation (reflection on learning)
Evaluating what learning has been undertaken and how it has been undertaken is important. A series of questions should be considered during the evaluation process:
 Has the activity achieved what the original learning objective was?
Has the activity achieved what the original learning objective was?
 Have any further learning needs been identified?
Have any further learning needs been identified?
 Has an opportunity to apply the learning occurred? If so, was there any feedback?
Has an opportunity to apply the learning occurred? If so, was there any feedback?
In some cases, individuals may find that what has been learned is not what they set out to learn. In this case, there is a need to revisit the original learning need and consider if the requirement to undertake further actions is still necessary for their practice. If the learning need is still valid, then this will lead into a new CPD cycle or alternatively, the individual can go back a couple of steps in the cycle and add in different actions.
Assessing whether the learning undertaken has been effective
A further question that needs to be asked is: ‘Can my practice now be shown to have improved as a result of the learning experience or is further learning required?’ Realistically, true evaluation may not occur for some weeks or months, since an opportunity to apply the learning may not occur sooner.
Scheduled learning vs unscheduled learning
The CPD cycle is a circle – each stage flows into the next. There are three entry points into the cycle: ‘Reflection on practice’, ‘Planning’ and ‘Action’. The exit (end point) is always ‘Evaluation’, when the impact of the learning undertaken is reviewed.
Scheduled learning is another term given to CPD which enters the process at ‘Reflection on practice’. This is when someone or something leads the individual to identify a learning need or knowledge gap and plan ways that they can meet this need or gap. This can be as simple as someone asking a question that the individual does not know the answer to.
Unscheduled learning is learning that starts from ‘Action’. This is learning that happens unexpectedly through someone or something. It is learning that was not planned and has not happened consciously.
All entry points into the CPD cycle are valid. Ordinarily, an individual would have a mixture of cycles, some starting at ‘Reflection’ or ‘Planning’, which indicates thinking about practice and planning appropriate actions, and some entries starting at ‘Action’, which indicates the individual is receptive to new ideas and concepts as they arise. The GPhC requires at least one-third of cycles to start at ‘Reflection’.
Recording CPD
The CPD four-stage cyclical process should be documented to demonstrate learning is being undertaken, which meets the needs of the individuals and the organizations in which they work. The GPhC has issued guidance stating the requirement to record CPD in a specially designed format. It is advised that an individual focuses on the quality of the process and recording rather than the quantity, with a minimum of nine records requiring to be documented per year which reflect the context and scope of the practice.
Generally, the aim is to record at least one CPD entry each month. The time taken to undertake a CPD cycle may be hours, days, weeks, months or, for some learning needs, years. The length of time taken to record a CPD cycle is about 30 minutes. This time includes the recording and the thinking during the process. Pharmacists and pharmacy technicians have to submit their CPD records periodically for review to the GPhC. The method of review involves evaluating the records against a set of evaluation criteria.
In summary, CPD describes any activity that helps a pharmacist or pharmacy technician do their job better. What CPD does is to focus that learning on the needs of the individuals and the organizations which employ them.
Revalidation
While CPD has become embedded in the continued registration of pharmacists and pharmacy technicians in the UK and other countries, it does not necessarily show competence or the fitness of the individual to practice. Concerns have been expressed over the years that healthcare professionals in general are only assessed once in their career and that is at the point of registration. This situation was considered unsatisfactory and the UK government proposed that all statutorily regulated healthcare professions should have in place arrangements for the ‘revalidation’ of their professional registration. Revalidation would require demonstration by healthcare professionals of their continued competence to practice in order to maintain their registration.
The Non-Medical Revalidation group in 2008 published 12 principles on which revalidation should be based. These are: consistency, professional standards, remediation, patient and public involvement, CPD, quality-assured, equality, integration, UK wide, demonstrate benefit, information and incrementally introduced.
The RPS in 2009 proposed that in order to be successful, any future revalidation process should be effective and cost-effective; be standards-based; be proportional; be evidenced-based; be quality-assured; involve stakeholders; be equal and diverse; be remedial; be consistent and be implemented incrementally. These proposals incorporate and are based on the above 12 principles.
The GPhC has agreed a draft definition of revalidation which is: the process by which assurance of continuing FtP of registrants is provided and in a way which is aimed primarily at supporting and enhancing professional practice.
Any revalidation process introduced by any of the health professions will need to be supportive of the professionals involved and basis of revalidation will not be a one-off assessment which if ‘failed’ will mean immediate de-registration of the individual. The process will need to incorporate several sources of information about the individual, which may include annual appraisals, CPD activity, commentaries on complaints or errors, and multi-source feedback, including patient and colleague surveys. The details about these sources of information will need to take full account of the structure of the pharmacy workforce. For example, some industrial pharmacists may have little or no patient contact and so patient surveys would be inappropriate. Similarly who will conduct appraisals? Will it be a line manager who may not be a pharmacist or a fellow pharmacist or a more senior pharmacist working for another organization? What about a community pharmacist, who works alone or locum pharmacists? These are challenges which will need to be addressed if revalidation is seen to be an appropriate and fair process.
Conclusion
It is important for all pharmacists to be engaged in regular CPD regarding updating their knowledge of practice, regulation and legislative changes within their field of work.
Key Points
 CPD is a feature of most professions
CPD is a feature of most professions
 CPD is part of clinical governance
CPD is part of clinical governance
 The CPD cycle involves reflection, planning, action, evaluation
The CPD cycle involves reflection, planning, action, evaluation
 Entry into the cycle can be at any of the first three stages; exit is always at evaluation, but may lead into further cycles
Entry into the cycle can be at any of the first three stages; exit is always at evaluation, but may lead into further cycles
 The UK pharmacy regulator requires pharmacists to record a minimum of nine CPD records each year which reflect the scope of practice of the pharmacist
The UK pharmacy regulator requires pharmacists to record a minimum of nine CPD records each year which reflect the scope of practice of the pharmacist
 Revalidation has been defined by the regulator and in the future will be introduced for registrants
Revalidation has been defined by the regulator and in the future will be introduced for registrants