Anatomy and Kinesiology of the Elbow
CRITICAL POINTS
▪ A functional and stable elbow allows for the complex motions of flexion and extension and pronation–supination necessary for daily life.
▪ The functional range of motion of the elbow joint has been determined to be 30 to 130 degrees in the flexion extension arc and 50 degrees each of pronation and supination.
▪ The elbow joint is a trochleoginglymoid joint that has complex motion in flexion–extension and axial rotation difficult to reapproximate with implants or external fixators.
▪ Stability of the elbow is conferred by bony congruity, ligamentous structures, and dynamic action of muscular forces.
▪ A posterior utilitarian approach to the elbow is useful for addressing many conditions. Variations exist to deal with specific problems.
▪ An understanding and appreciation of the complex anatomy of the elbow joint, including the soft tissues and neurovascular structures, is essential to understand and treat pathology about this joint.
The elbow joint functions as a link between the arm and forearm to position the hand in space and allow activities of prehension; it transmits forces and it allows the forearm to act as a lever in lifting and carrying. A functional and stable elbow allows for the complex motions of flexion and extension and pronation–supination necessary for daily life.1 Stability of the elbow is conferred by bony congruity, ligamentous restraints, and dynamic stabilization by muscular forces. Biomechanical aspects of the elbow are considered in the context of motion, function, and stability. An understanding of the anatomic features contributing to these roles is critical and is outlined in this chapter.
It has been determined that although the normal arc of motion of the elbow is 0 to 150 or 160 degrees in the flexion extension arc and 75 to 85 degrees each of pronation and supination, a functional range of motion in which most activities of daily living can be accomplished is 30 to 130 degrees in flexion extension and 50 degrees each of pronation and supination.2 When the elbow is affected by pathologic conditions, the ability to place the hand in space is diminished.
In full extension, 60% of axial loads are transmitted across the radiocapitellar joint while 40% of loads are transmitted across the ulnohumeral joint3 (Fig. 3-1, online). With elbow flexion, the relationship is altered such that loads are equally shared between the ulnohumeral and radiocapitellar articulations.4
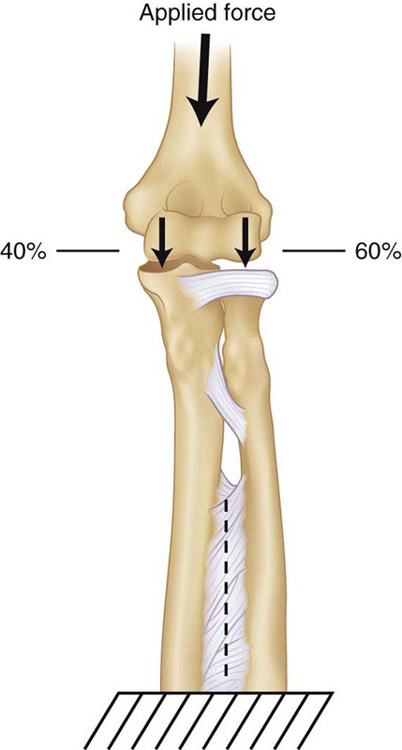
Figure 3-1 It has been estimated that approximately 60% of the axial load is transmitted across the radiohumeral joint when the elbow is in full extension. (Morrey BF, An KN. Stability of the elbow: Osseous constraints. J Shoulder Elbow Surg 2005;14:174S–178S. Used with permission from Elsevier.)
In the flexion–extension arc the elbow does not follow motion of a simple hinge joint; the obliquity of the trochlear groove and ulnar articulation results in a helical pattern of motion1,5 (Fig. 3-2). The varus–valgus laxity over the arc of flexion–extension measures 3 to 4 degrees. The center of rotation in the sagittal plane lies anterior to the midline of the humerus and is colinear with the anterior cortex of the distal humerus. The axis of rotation runs through the center of the articular surface on both the anteroposterior and lateral planes (Fig. 3-3, online). Forearm rotation occurs through an axis oblique to both the longitudinal axis of the radius and the ulna, through an imaginary line between the radial head at the proximal radioulnar joint and the ulnar head at the distal radioulnar joint.1 As described in the analogy by Kapandji, the distal and proximal radioulnar joints function as the hinges of a door. Disruption of either hinge results in loss of complete motion in pronation or supination.1,6
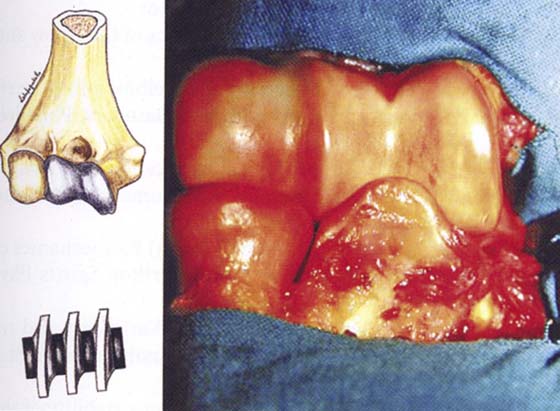
Figure 3-2 The olecranon moves on the articular surface of the trochlea like a screw tapping on it. (Celli A. Chapter 1: Anatomy and biomechanics of the elbow. In: Celli A, Celli L, Morrey BF, eds. Treatment of Elbow Lesions: New Aspects in Diagnosis and Surgical Techniques. Milan, Springer-Verlag Italia, 2008, pp. 1–11. Used with permission from Springer-Verlag.)
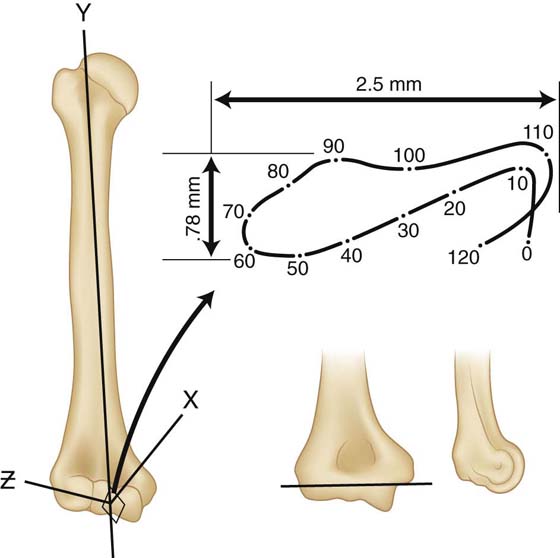
Figure 3-3 Very small locus of instant center of rotation for the elbow joint demonstrates that the axis may be replicated by a single line drawn from inferior aspect of the medial epicondyle through the center of the lateral epicondyle, which is in the center of the lateral projected curvature of the trochlea and capitellum. (Morrey BF, Chao EY. Passive motion of the elbow joint. J Bone Joint Surg Am 1976;58:501–508. Used with permission from Elsevier [Churchill Livingstone].)
Palpable bony landmarks about the elbow include the medial and lateral epicondyles, the radial head, and the olecranon7 (Figs. 3-4 and 3-5).
The prominent medial and lateral epicondyles serve as the attachment point for the medial collateral ligament (MCL), the flexor pronator group and lateral collateral ligament complex (LCL), and the common extensor tendon origin. The distal humerus articulates with the proximal ulna via the trochlea, a spool-shaped surface. The center of the medullary canal is offset laterally to the center of the trochlea. The olecranon, together with the coronoid process, forms the semilunar or greater sigmoid notch of the ulna (Fig. 3-6). This articulates with the trochlea of the humerus and confers stability and facilitates motion in the anteroposterior plane.7 The lateral ridge of the trochlea is less prominent than the medial side, resulting in a 6- to 8-degree valgus orientation and creating the valgus carrying angle of the arm.8 Laterally, the capitellum articulates with the proximal radius. The radius also articulates with the lesser sigmoid notch of the ulna. Together, the hinge motion at the trochlea–proximal ulnar articulation and the rotational motion at the radiocapitellar joint provide the complex motion at the elbow in flexion–extension and forearm rotation.
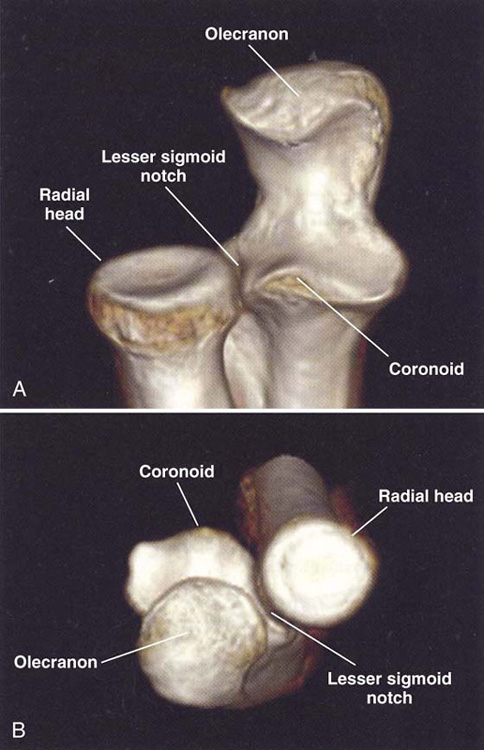
Figure 3-6 A, B, The proximal ulna and radius aspects with the bone landmarks (CT 3D reconstruction). (Celli A. Chapter 1: Anatomy and biomechanics of the elbow. In: Celli A, Celli L, Morrey BF, eds. Treatment of Elbow Lesions: New Aspects in Diagnosis and Surgical Techniques. Milan, Springer-Verlag Italia, 2008, pp. 1–11. Used with permission from Springer-Verlag.)
Anatomically, a transverse “bare area” devoid of cartilage is found at the midpoint between the coronoid and the tip of the olecranon. The unwary surgeon may inadvertently discard structurally significant portions of the olecranon if this is not considered when reconstructing a fracture.9 The anterior portion of the sigmoid notch is represented by the coronoid, which has increasingly been recognized as an important contributor to stability of the elbow (Fig. 3-7, online). Posteriorly, the olecranon tip is the attachment site of the triceps. McKeever and Buck determined in the laboratory that one may excise up to 80% of the olecranon without sacrificing stability if the coronoid and anterior soft tissues are intact.10,11 In addition, An and colleagues12 noted increasing instability of the elbow with olecranon excision in a linear fashion, with laboratory data suggesting that loss of up to 50% of the olecranon may be associated with no instability. If anterior damage is present, instability results if too much proximal ulna is excised. Significant coronoid loss, such as occurs with untreated coronoid fractures, will lead to instability.13,14 The clinical importance is that severely comminuted olecranon fractures in the absence of anterior injury may be treated with partial excision, particularly in elderly or low-demand patients. However, if significant anterior damage is present, reconstruction is essential9 (Fig. 3-8).

Figure 3-7 3-D CT scan view of an anteromedial coronoid fracture. Arrow demonstrates fracture fragment. (Steinmann SP. Coronoid fractures. In: Tumble TE BJ, ed. Wrist and Elbow Reconstruction & Arthroscopy: A Master Skills Publication. Rosemont: American Society for Surgery of the Hand, 2008. Used with permission from American Society for Surgery of the Hand.)

Figure 3-8 A, This 69-year-old man with poorly controlled type I diabetes fell sustaining this type IIA olecranon fracture. B, He was subsequently treated to excise fracture fragments, and the triceps was sutured down to the remaining distal fragment. C, At 4 years’ follow-up, the patient had no complaints, no instability, and range of motion was pronation–supination 80–80, full flexion and a 25-degree extension lag. Radiographs were satisfactory. (Adams JE, Steinmann SP. Fractures of the olecranon. In: Celli A, Celli L, Morrey BF, eds. Treatment of Elbow Lesions: New Aspects in Diagnosis and Surgical Techniques. Milan: Springer-Verlag Italia, 2008, pp. 71–81. Used with permission from Springer-Verlag.)
The articular surface of the radial head is oriented at a 15-degree angle to the neck away from the radial tuberosity7 (Fig. 3-9). The radial head has been called a secondary stabilizer of the elbow. In the setting of a ligamentously intact elbow, fracture or removal of the radial head renders the joint unstable. However, in the setting of MCL deficiency, the radial head becomes crucial to stability against valgus forces15 (Fig. 3-10, online). The portion of the radial head that articulates with the capitellum is an eccentric dish-shaped structure with a variable offset from the neck,16 both of which factors have implications for fracture fixation or prosthetic replacement. Likewise, the portion of the radial head that articulates with the proximal ulna has clinically important features. The cartilage of the radial head encompasses an arc of about 280 degrees about the rim of the radius.

Figure 3-9 Proximal radius has a 15-degree angulation away from the radial tuberosity. (Morrey BF. Anatomy and surgical approaches. In: Morrey BF, ed. Reconstructive Surgery of the Joints, Vol. 1, 2nd ed. New York: Churchill Livingstone, 1996, pp. 461–487. Used with permission from Elsevier [Churchill Livingstone].)
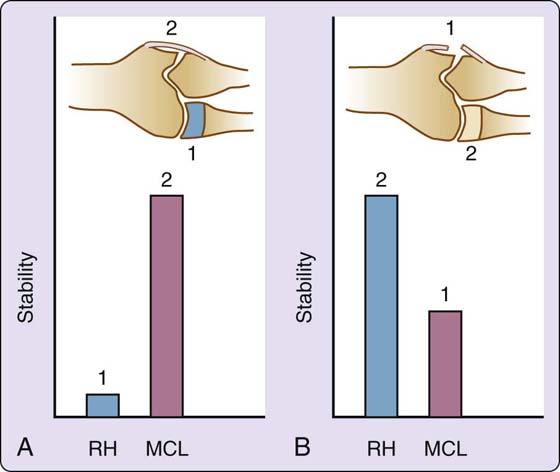
Figure 3-10 A, Removing the radial head (RH) and placing the elbow in valgus when the medial collateral ligament (MCL) is intact results in relatively little displacement of the forearm. When the MCL is then removed, marked instability is demonstrated. B, When the sequence is altered and the MCL is released, however, some valgus instability is noted. After this, removal of the RH results in subluxation of the elbow. This defines the RH as an important secondary stabilizer of the elbow to resist valgus stress. (Morrey BF, An KN. Stability of the elbow: Osseous constraints. J Shoulder Elbow Surg 2005;14:174S–178S. Used with permission from Elsevier.)
Ligamentous structures that contribute to the stability of the elbow joint include the collateral ligaments and the capsule both anteriorly and posteriorly.17 Dynamic stability is conferred by the actions of the muscles crossing the joint.
Medially, the medial collateral ligament consists of the anterior oblique ligament (AOL), the posterior oblique ligament (POL), and the transverse ligament7,17 (Fig. 3-11). The AOL of the MCL is the most important stabilizer to valgus stresses and should be preserved or reconstructed.15,17-20 The AOL has two bands: an anterior band that is tight from 0 to 60 degrees and a posterior band that is tight from 60 to 120 degrees.19 The AOL and POL arise from the central portion of the anterior inferior medial epicondyle21 and insert near the sublime tubercle (AOL) and in a fan-shaped insertion along the semilunar notch (POL).22 The transverse segment of the MCL appears to have little functional significance.23
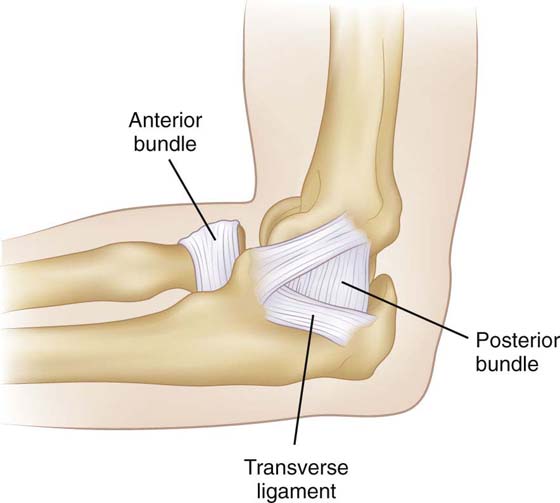
Figure 3-11 Medial aspect of the joint. The anterior and posterior bundles of the medial collateral ligament are consistently present and identifiable. (Morrey BF. Anatomy and surgical approaches. In Morrey BF, ed. Reconstructive Surgery of the Joints, Vol. 1, 2nd ed. New York: Churchill Livingstone, 1996, pp. 461–487. With permission from Elsevier [Churchill Livingstone].)
The lateral ligament complex includes the radial collateral ligament, the lateral ulnar collateral ligament (LUCL), the annular ligament, and the accessory LCL (Fig. 3-12). The LUCL serves as the major lateral ligamentous stabilizer. It arises from the inferior aspect of the lateral epicondyle and inserts on the supinator crest. It has near isometry during the flexion extension arc.7 The radial collateral ligament also arises from the lateral epicondyle and inserts on the radial head along the annular ligament. The annular ligament arises and inserts on the anterior and posterior margins of the lesser sigmoid notch. It functions to stabilize the radial head in contact with the ulna. Because of the eccentric dish-shaped nature of the radial head, the anterior leaf of the ligament becomes tight in supination and the posterior portion becomes tight in pronation.23,24
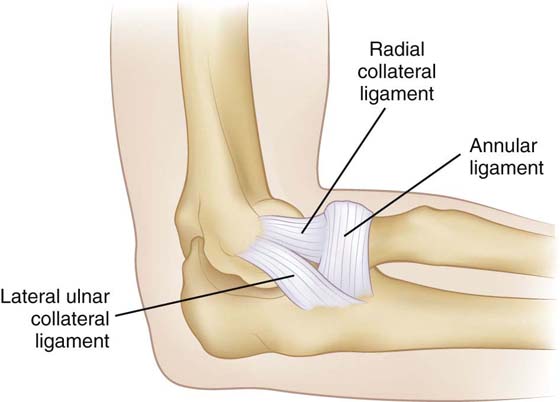
Figure 3-12 Lateral ligament complex is composed of the radial collateral ligament, the annular ligament, and the less well-recognized ulnar collateral ligament. (Morrey BF. Anatomy and surgical approaches. In Morrey BF, ed. Reconstructive Surgery of the Joints, Vol. 1, 2nd ed. New York: Churchill Livingstone, 1996, pp. 461–487. With permission from Elsevier [Churchill Livingstone].)
The joint capsule has been regarded as a passive stabilizer of the elbow; however, conflicting opinions exist regarding this point. Morrey and An suggest that it functions as a stabilizer to varus–valgus stresses and against distraction loading in extension but not flexion.22 The maximal capacity of the joint exists at 70 to 80 degrees of flexion and is 25 to 30 mL.25 This may be significantly decreased when the capsule becomes contracted by post-traumatic changes or arthritic conditions. Clinically, this may make joint entry more difficult and dangerous during arthroscopy.23,25
The biceps serves as a flexor and supinator of the elbow and forearm. The brachialis originates from the distal half of the humeral shaft and inserts along the tuberosity of the ulna; it acts as a strong flexor of the elbow.25
The common extensor group and the mobile wad of Henry arise from the lateral epicondyle and humerus. The mobile wad of Henry, which comprises the brachioradialis, the extensor carpi radialis brevis (ECRB), and extensor carpi radialis longus (ECRL), forms the radial-sided contour of the forearm and lateral border of the antecubital fossa (Fig. 3-13). The brachioradialis has a lengthy origin along the distal third of the humerus; it then has a broad insertion along the distal radial radius shaft and styloid. It is a strong flexor of the elbow. The ECRL and ECRB arise from the lateral epicondyle and insert on the base of the second and third metacarpals, respectively. These two muscles extend the wrist. The ECRB is covered by the ECRL proximally, which must be elevated to expose the diseased origin of the ECRB in open lateral epicondylitis procedures. Dorsally lie the extensor digitorum communis (EDC), extensor indicis (EI), the extensor digiti quinti (EDQ or EDM), the humeral and ulnar attachments of the extensor carpi ulnaris (ECU), and the anconeus (Fig. 3-14, online).

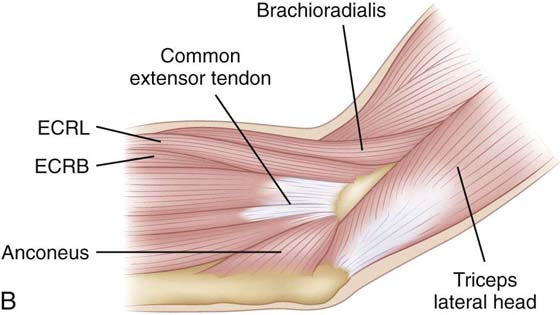
Figure 3-13 A, Lateral elbow demonstrating extensor carpi radialis longus (forceps) and common extensor origin. B, Drawing of common extensor origin, lateral elbow. ECRB, extensor carpi radialis brevis; ECRL, extensor carpi radialis longus. (Murray PM. Elbow anatomy. In: Trumble TE, Budoff J, eds. Wrist and Elbow Reconstruction & Arthroscopy: A Master Skills Publication. Rosemont: American Society for Surgery of the Hand, 2006. Used with permission from American Society for Surgery of the Hand.)
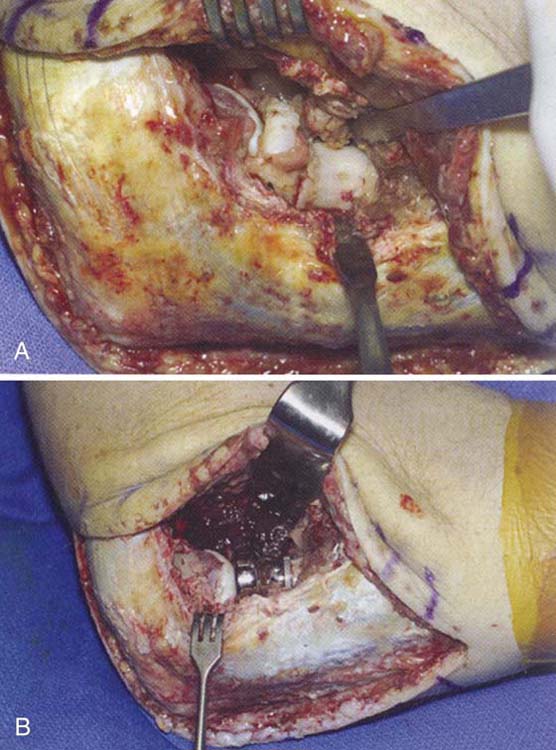
Figure 3-14 For exposures of the radial head for fracture fixation, an extensor splitting approach is preferred rather than the Kocher approach, as the lateral ulnar collateral ligament (LUCL) is at risk of injury during the latter approach. Care is taken to limit the extent of resection and protect the LUCL. A, Type III fracture. Severe comminution noted at surgery. Surgical approach involved posterior skin incision with split of the extensor digitorum communis tendon origin to gain exposure. B, Radial head prosthesis. Note metallic head centered on capitellum. (Hartman MW, Steinmann SP. The radial head fractures. In: Celli A CL, Morrey BF, eds. Treatment of Elbow Lesions: New Aspects in Diagnosis and Surgical Techniques. Milan: Springer-Verlag, Italia, 2008. Used with permission from Springer-Verlag.)
At the ulnar side of the elbow, the flexor pronator group arises from the medial epicondyle and includes the flexor carpi ulnaris (FCU), the palmaris longus, the flexor carpi radialis (FCR), flexor digitorum profundus (FDP) and superficialis (FDS), and the pronator teres (Fig. 3-15, online). The pronator teres usually has two heads through which the median nerve passes: one from the medial epicondyle and a second from the coronoid. This can be a site of median nerve entrapment. The pronator inserts on the radius and acts as a strong pronator of the forearm and a weak flexor of the elbow. The FCR is a wrist flexor, and the palmaris longus is functionally insignificant but is useful as a graft donor for reconstructive procedures. The supinator originates from the lateral epicondyle, the LCL, and the proximal anterior ulna along the supinator crest. The muscle runs obliquely to finally wrap around the radius and end in a broad insertion along the proximal radius. Like the biceps, it serves as a supinator of the forearm.25
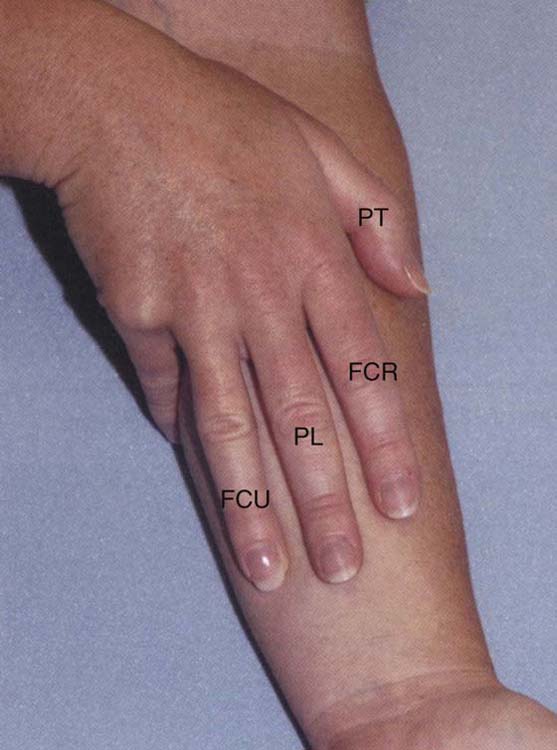
Figure 3-15 The medial epicondyle is the origin of the flexor pronator muscles of the forearm. PT, pronator teres; FCU, flexor carpi ulnaris. (Murray PM. Elbow anatomy. In: Trumble TE Budoff J, eds. Wrist and Elbow Reconstruction & Arthroscopy: A Master Skills Publication. Rosemont: American Society for Surgery of the Hand, 2006. Used with permission from American Society for Surgery of the Hand.)
The triceps posteriorly acts to extend the elbow. It arises from the posterior aspect of the humerus (lateral and medial heads) and from the scapula (long head).
Multiple neurovascular structures are at risk of injury with procedures or pathology about the elbow joint. An understanding of anatomy is crucial to avoiding iatrogenic injury and for anticipating possible problems as well as exploiting internervous planes during surgical approaches.26
The brachial artery traverses between the brachialis and biceps muscles in its course down the arm and lies lateral to the median nerve in the antecubital fossa. Typically, the radial artery arises at the level of the radial head, travels between the brachioradialis and the pronator teres, and sends a recurrent branch (radial recurrent branch) proximally. This anastamoses with the radial collateral and middle collateral arteries (from the profunda brachii) to form the radial-sided network of collateral circulation. The ulnar artery is the larger of the two branches and gives rise to the common interosseous artery and then posterior and anterior interosseous arteries. The ulnar artery, like the radial artery, gives off recurrent branches (the posterior and anterior recurrent arteries) that then anastamose with the superior and inferior ulnar collateral arteries arising from the brachial artery proximal to the elbow.7 The basilic vein and cephalic vein drain the distal extremity and cross the elbow in a variable course.
Proximal to the elbow joint, the median nerve travels anteromedial to the humerus and lateral to the brachial artery. At the elbow joint, it crosses anterior to the artery to lie medial to the artery and the biceps tendon in the antecubital fossa (Fig. 3-16). No muscular branches arise from the median nerve in the arm.27 At the antecubital fossa, the nerve is covered by the lacertus fibrosis as it crosses over the elbow joint. It then dips beneath the two heads of the pronator teres. The first motor branches from the median nerve arise laterally and are to the pronator teres and flexor carpi radialis. The nerve passes through the forearm along the dorsal surface of the FDS, which it supplies.7,27
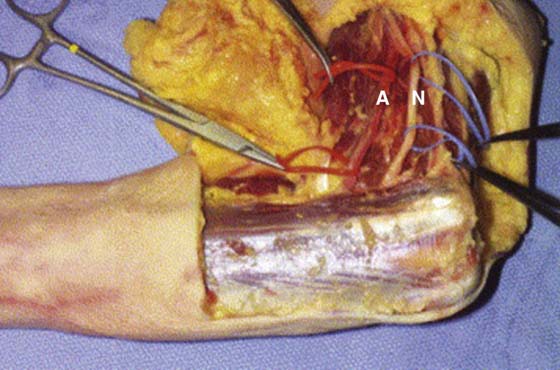
Figure 3-16 The relationship of the median nerve (N) and brachial artery (A) proximal to the elbow joint. (Adams JE, Steinmann SP. Nerve injuries about the elbow. J Hand Surg Am 2006;31A:303–313. Used with permission from Elsevier.)
The anterior interosseous nerve (AIN) arises from the median nerve 2 to 6 cm distal to the medial epicondyle.28 This purely motor nerve travels down the forearm on the interosseous membrane.27,29 The AIN may be injured in association with a (typically pediatric) supracondylar fracture as a result of contusion, traction, or both, particularly in the setting of irreducible, highly displaced or comminuted fractures.28
The ulnar nerve travels subcutaneously along the medial aspect of the arm between the coracobrachialis laterally and the long and medial heads of the triceps posteriorly (Fig. 3-17). Near the insertion of the coracobrachialis, the ulnar nerve passes through the medial intermuscular septum and the arcade of Struthers to enter the posterior compartment of the arm. The nerve then travels along the medial head of the triceps toward the medial epicondyle. It passes posterior to this structure, superficial to the joint capsule and the MCL, and through the cubital tunnel30 (Fig. 3-18). The posterior branch of the medial antebrachial cutaneous nerve passes over the ulnar nerve at a point between 6 cm proximal to 4 cm distal to the medial epicondyle.30,31
The ulnar nerve passes between the humeral and ulnar heads of the FCU as it enters the forearm. The first muscular branch is usually to the FCU, and multiple branches may arise anywhere from 4 cm proximal to 10 cm distal to the medial epicondyle. The muscular branch to the FDP usually arises 4 to 5 cm distal to the medial epicondyle.30
Because of its close proximity to the MCL of the elbow and its tethered location under the medial epicondyle, the ulnar nerve is often affected by pathology about the elbow joint. In addition to cubital tunnel syndrome, the nerve may be stretched during elbow dislocations, or injured as a result of fractures or during surgical procedures. In addition, the late sequelae of trauma, including deformities such as cubital varus or valgus or heterotopic ossification, may be problematic.30 Trauma may promote adhesions and scarring, which can cause compression at classic locations of ulnar nerve entrapment, including the cubital tunnel, the arcade of Struthers, the medial intermuscular septum, or between the two heads of the FCU.29,30 Typically, decompression and/or transposition is recommended when procedures such as total elbow arthroplasty or open reduction of significant distal humerus fractures is performed. Likewise, with contracture releases, the nerve is particularly vulnerable to stretch postoperatively if a large restoration of motion occurs; in this case the ulnar nerve may need to be assessed.32
The radial nerve exits the triangular space and travels along the posterior aspect of the humerus.27,33 Distally, the nerve emerges from the spiral groove about 10 cm and 15 cm proximal to the lateral epicondyle and elbow joint, respectively34,35 (Fig. 3-19). Above the spiral groove, a muscular branch to the medial head of the triceps is given off. This continues distally to supply the anconeus muscle. Surgical approaches can exploit this relationship to reflect the anconeus on a proximally based pedicle preserving its neurovascular supply.7 Prior to piercing the lateral intermuscular septum to travel in the anterior aspect of the arm, two cutaneous branches are given off: the inferior lateral brachial cutaneous branch and the posterior antebrachial cutaneous nerve.36 The radial nerve then pierces the lateral intermuscular septum and travels down the lateral column of the humerus over the lateral edge of the brachialis muscle.33-37
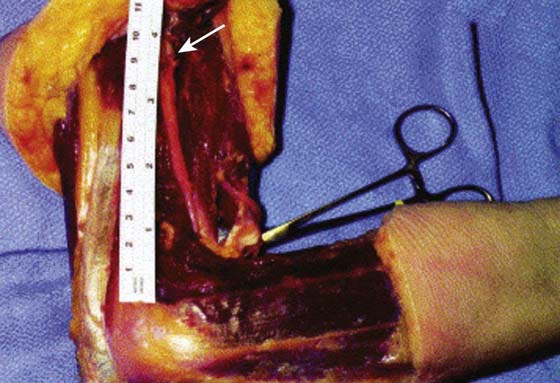
Figure 3-19 The radial nerve (arrow) as it pierces the intermuscular septum 9 to 10 cm proximal to the elbow joint. (Adams JE, Steinmann SP. Nerve injuries about the elbow. J Hand Surg Am 2006;31A:303–313. Used with permission from Elsevier.)
Muscular branches to the brachialis and ECRL are given off proximal to the elbow joint.36,37 The nerve travels deep to the brachioradialis, ECRB, and ECRL muscles and passes directly over the annular ligament.36 At the radiocapitellar joint level, the radial nerve bifurcates into a deep branch, which becomes the posterior interosseous nerve (PIN), and a superficial branch, which continues as the superficial radial nerve.37-39 Innervation to the ECRB arises at the level of the bifurcation of the nerve and is variable.36 The superficial branch of the radial nerve initially lies deep to the brachioradialis and superficial to the ECRL but distally emerges from the lateral edge of the brachioradialis to provide cutaneous sensation to the dorsoradial aspect of the hand.36,38
The PIN dips into the arcade of Frohse—a tunnel formed by fibrous bands of the brachialis and brachioradialis muscle, ECRB, and the superficial head of the supinator36,39 (Fig. 3-20). The floor of the tunnel is formed by the anterior capsule of the elbow and the deep head of the supinator. The PIN then wraps about the lateral aspect of the radius, giving off branches to the supinator muscle.36 At the distal border of the supinator, the PIN splits into two major branches: a short or recurrent branch, which supplies the ECU, EDC, EDM; and the long or descending branch, which innervates the abductor pollicis longus (APL), extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and EI, and supplies sensation to the dorsal aspect of the wrist.36,38,39
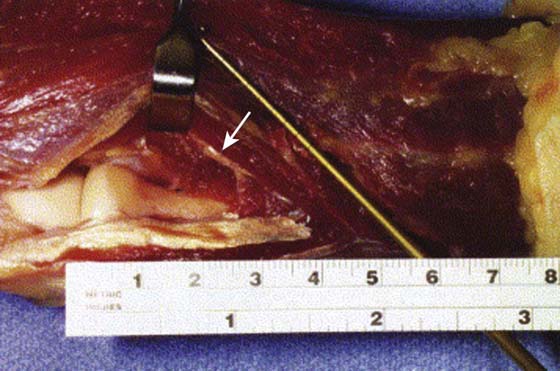
Figure 3-20 The posterior interosseous nerve (arrow) entering the supinator muscle distal to the radial head. (Adams JE, Steinmann SP. Nerve injuries about the elbow. J Hand Surg Am 2006;31A:303–313. Used with permission from Elsevier.)
Diliberti and colleagues40 demonstrated in a cadaveric study the effect of pronation on the PIN. With full supination of the forearm, the PIN crossed the radial shaft at an average of 33 mm (range, 22–47 mm) from the radiocapitellar joint, whereas pronation caused the PIN to become more parallel to the long axis of the radius, and full pronation increased the distance to 52 mm (range, 38–68 mm).40 The PIN is “tethered” by the supinator muscle and therefore is rotated with the radius during rotation.41 Thus, during dorsal surgical approaches to the proximal radius, the forearm should be positioned in pronation to minimize risk of injury to the PIN.41,42 Additional principles that may be helpful in avoiding PIN injury include releasing the supinator close to its ulnar attachment rather than over the radius and using the bicipital tuberosity as a landmark to the region that may be safely exposed during surgery.42
Several cutaneous nerves are important to mention about the elbow. Inadvertent injury can cause a bothersome numb patch or a painful neuroma. The lateral antebrachial cutaneous nerve is the terminal sensory branch of the musculocutaneous nerve and pierces the brachial fascia approximately 3 cm proximal to the lateral epicondyle.27,43 It then passes 4.5 cm medial to the lateral epicondyle. Anterior and posterior branches supply cutaneous sensation to the anterolateral and posterolateral surfaces of the forearm, respectively.43 It is at risk during exposures of the distal humerus and should be identified in the interval between the brachialis and the biceps muscles and preserved.27
The medial antebrachial cutaneous nerve travels down the arm medial to the brachial artery.31 It pierces the deep fascia in the mid or distal arm to become subcutaneous and has a variable relationship with the basilic vein.31,44 At an average of 14.5 cm proximal to the medial epicondyle (range, 1–31 cm), the medial antebrachial cutaneous nerve gives off its anterior and posterior branches. The anterior branch crosses over the elbow joint between the medial epicondyle and biceps tendon.31 The posterior branch gives off two to three additional branches, which have a variable course, crossing over the elbow usually proximal to the medial epicondyle, but between 6 cm proximal to 6 cm distal to it.31,43 Injury of the medial antebrachial cutaneous branch of the median nerve or its branches may occur during cubital tunnel release. A more posterior incision, full-thickness flaps, and careful dissection and preservation of branches can lessen the risk of a bothersome hypoesthetic patch over the olecranon or symptomatic neuromas.31,43,44
An understanding of the complex anatomy and biomechanics of the elbow joint including the soft tissues and neurovascular structures is essential in treating pathology about this joint. Stability of the elbow is conferred by bony congruity, ligamentous structures, and dynamic action of muscular forces. Mobility of the elbow is critical for the accomplishment of a variety of activities of daily living. The functional ROM of the elbow has been determined to be 30 to 130 degrees in the flexion and extension arc and 50 degrees each of pronation and supination. The intimate relationship of the many neurovascular structures about the elbow make them vulnerable in elbow injuries, and they require protection during surgery.
1. An KN, Morrey BF. Chapter 4: Biomechanics of the elbow. In: Morrey BF, ed. The Elbow and Its Disorders. 2nd edition Philadelphia: WB Saunders; 1993:53–72.
2. Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981; 63: 872–877.
3. Halls AA, Travill A. Transmission of pressures across the elbow joint. Anat Rec. 1964; 150: 243–247.
4. Morrey BF, An KN. Stability of the elbow: osseous constraints. J Shoulder Elbow Surg. 2005; 14: 174S–178S.
5. Morrey BF, Chao EY. Passive motion of the elbow joint. J Bone Joint Surg Am. 1976; 58: 501–508.
6. Kapandji A. [The radio-ulnar unit. Its functional importance in fractures of both bones of the forearm]. Chir Main. 1998; 17: 348–361.
7. Morrey BF. Anatomy and surgical approaches. 2nd editionMorrey BF, ed. Reconstructive Surgery of the Joints. Vol. 1. New York: Churchill Livingstone; 1996:461–487.
8. Bryce CD, Armstrong AD. Anatomy and biomechanics of the elbow. Orthop Clin North Am. 2008; 39: 141–154.
9. Adams JE, Steinmann SP. The fractures of the olecranon. In: Celli A, Celli L, Morrey BF, eds. Treatment of Elbow Lesions: New Aspects in Diagnosis and Surgical Techniques. Milan: Springer-Verlag Italia; 2008:71–81.
10. Fern ED, Brown JN. Olecranon advancement osteotomy in the management of severely comminuted olecranon fractures. Injury. 1993; 24: 267–269.
11. McKeever FM, Buck RM. Fracture of the olecranon process of the ulna: treatment by excision of fragment and repair of triceps tendon. JAMA. 1947; 135: 1–5.
12. An KN, Morrey BF, Chao EY. The effect of partial removal of proximal ulna on elbow constraint. Clin Orthop Relat Res. 1986.270–279.
13. Regan W, Morrey BF. Classification and treatment of coronoid process fractures. Orthopedics. 1992; 15: 845–848.
14. Closkey RF, Goode JR, Kirschenbaum D, Cody RP. The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. J Bone Joint Surg Am. 2000; 82A: 1749–1753.
15. Morrey BF, Tanaka S, An KN. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res. 1991.187–195.
16. King GJ, Zarzour ZD, Patterson SD, Johnson JA. An anthropometric study of the radial head: implications in the design of a prosthesis. J Arthroplasty. 2001; 16: 112–116.
17. Safran MR, Baillargeon D. Soft-tissue stabilizers of the elbow. J Shoulder Elbow Surg. 2005; 14: 179S–185S.
18. Hotchkiss RN, Weiland AJ. Valgus stability of the elbow. J Orthop Res. 1987; 5: 372–377.
19. Regan WD, Korinek SL, Morrey BF, An KN. Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res. 1991.170–179.
20. Callaway GH, Field LD, Deng XH, et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997; 79A: 1223–1231.
21. O’Driscoll SW, Jaloszynski R, Morrey BF, An KN. Origin of the medial ulnar collateral ligament. J Hand Surg Am. 1992; 17A: 164–168.
22. Morrey BF, An KN. Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res. 1985.84–90.
23. Celli A. Chapter 1: Anatomy and biomechanics of the elbow. In: Celli A, Celli L, Morrey BF, eds. Treatment of Elbow Lesions: New Aspects in Diagnosis and Surgical Techniques. Milan, Italy: Springer-Verlag Italia; 2008:1–11.
24. Olsen BS, Sojbjerg JO, Dalstra M, Sneppen O. Kinematics of the lateral ligamentous constraints of the elbow joint. J Shoulder Elbow Surg. 1996; 5: 333–341.
25. Morrey BF. Chapter 3: Anatomy of the elbow joint. In: Morrey BF, ed. The Elbow and Its Disorders. 2nd edition Philadelphia: WB Saunders; 1993:16–52.
26. Adams JE, Steinmann SP. Nerve injuries about the elbow. J Hand Surg Am. 2006; 31A: 303–313.
27. Hoppenfeld S, deBoer P. Surgical Exposures in Orthopaedics: The Anatomic Approach. 2nd ed New York: JB Lippincott; 1984.
28. Cramer KE, Green NE, Devito DP. Incidence of anterior interosseous nerve palsy in supracondylar humerus fractures in children. J Ped Orthop. 1993; 13: 502–505.
29. Ristic S, Strauch RJ, Rosenwasser MP. The assessment and treatment of nerve dysfunction after trauma around the elbow. Clin Orthop Relat Res. 2000.138–153.
30. Khoo D, Carmichael SW, Spinner RJ. Ulnar nerve anatomy and compression. Orthop Clin North Am. 1996; 27: 317–338.
31. Masear VR, Meyer RD, Pichora DR. Surgical anatomy of the medial antebrachial cutaneous nerve. J Hand Surg Am. 1989; 14A: 267–271.
32. Adams JE, Wolff LH 3rd, Merten SM, Steinmann SP. Osteoarthritis of the elbow: results of arthroscopic osteophyte resection and capsulectomy. J Shoulder Elbow Surg. 2008; 17: 126–131.
33. Gerwin M, Hotchkiss RN, Weiland AJ. Alternative operative exposures of the posterior aspect of the humeral diaphysis with reference to the radial nerve. J Bone Joint Surg Am. 1996; 78A: 1690–1695.
34. Nelson AJ, Izzi JA, Green A, et al. Traumatic nerve injuries about the elbow. Orthop Clin North Am. 1999; 30: 91–94.
35. Uhl RL, Larosa JM, Sibeni T, Martino LJ. Posterior approaches to the humerus: when should you worry about the radial nerve? J Orthop Trauma. 1996; 10: 338–340.
36. Kleinert JM, Mehta S. Radial nerve entrapment. Orthop Clin North Am. 1996; 27: 305–315.
37. Tornetta P 3rd, Hochwald N, Bono C, Grossman M. Anatomy of the posterior interosseous nerve in relation to fixation of the radial head. Clin Orthop Relat Res. 1997; 345: 215–218.
38. Hirachi K, Kato H, Minami A, et al. Clinical features and management of traumatic posterior interosseous nerve palsy. J Hand Surg Br. 1998; 23B: 413–417.
39. Thomas SJ, Yakin DE, Parry BR, Lubahn JD. The anatomical relationship between the posterior interosseous nerve and the supinator muscle.[see comment]. J Hand Surg Am. 2000; 25A: 936–941.
40. Diliberti T, Botte MJ, Abrams RA. Anatomical considerations regarding the posterior interosseous nerve during posterolateral approaches to the proximal part of the radius. [see comment]. J Bone Joint Surg Am. 2000; 82A. 809–713
41. Strauch RJ, Rosenwasser MP, Glazer PA. Surgical exposure of the dorsal proximal third of the radius: how vulnerable is the posterior interosseous nerve? J Shoulder Elbow Surg. 1996; 5: 342–346.
42. Witt JD, Kamineni S. The posterior interosseous nerve and the posterolateral approach to the proximal radius. J Bone Joint Surg Br. 1998; 80B: 240–242.
43. Patterson SD, Bain GI, Mehta JA. Surgical approaches to the elbow. Clin Orthop Rel Res. 2000.19–33.
44. Race CM, Saldana MJ. Anatomic course of the medial cutaneous nerves of the arm. J Hand Surg Am. 1991; 16: 48–52.