Upper Quarter Screen
▪ The upper quarter screen is appropriate when the diagnosis is unclear or when there is potential for referred pain from more proximal structures.
▪ The purpose of the upper quarter screen is to determine which anatomic region of the upper quarter is contributing to the patient’s symptoms and to rule out gross sensory or motor neurologic deficits.
▪ The examiner should observe for reproduction of the patient’s chief complaint of pain or symptoms, and, when identified, a more thorough examination of that region is necessary.
▪ The screening examination is performed bilaterally. This is especially true for reflex testing since results in normals can vary widely.
Anatomically, the upper quarter includes the cervical spine, upper thoracic spine, and the upper extremity. Because the source of a patient’s symptoms is often unclear, a screening examination can be helpful in providing an efficient mechanism for determining more precisely which region(s) may be contributing to the symptoms.1 The upper quarter screening examination is designed to achieve two basic purposes: (1) determine which anatomic region of the upper quarter is contributing to the patient’s symptoms and therefore needs to be examined in greater detail, and (2) rule out gross sensory or motor neurologic deficits consistent with a cervical radiculopathy or other source.2,3
A screening examination is often unnecessary when the source of a patient’s symptoms or dysfunction is very clear from the history, such as with postsurgical problems or when some isolated traumatic injury has occurred to the upper extremity. The screening examination is most appropriate when the diagnosis is unclear or when there is a potential for referred pain, typically emanating from more proximal structures.
Referred pain can be simply defined as pain perceived in an area other than its source. A complete discussion of referred pain is beyond the scope of this chapter, but understanding some general characteristics of referred pain can be very helpful clinically. First, deeper, more proximal structures are most likely to refer pain.4,5 Therefore, the majority of the upper quarter screening examination focuses on the cervical spine and shoulder. These areas are known to be potential sources able to refer pain to multiple sites in the upper extremity.6-8 However, it is rare that distal structures in the upper extremity refer pain proximally. Referred pain is also typically described as a poorly localized, dull aching sensation.4,5 Therefore, the patient who rubs the entire lateral aspect of the arm while describing a dull aching pain is more likely to have referred pain than a patient who, for example, complains of a sharp localized pain on the lateral aspect of the elbow.
While performing the examination, the goal is to reproduce the patient’s chief complaint of pain or other symptoms. Occasionally, patients have mild restrictions in cervical range of motion (ROM) or complaints of discomfort or pulling sensations during cervical spine testing. Painless restrictions in motion or symptoms that are not part of the patient’s chief complaint should not be interpreted as positive tests but more likely represent normal variations.
What is included in the screening examination varies greatly; however, a suggested format is given in the form shown as Figure 10-1. As a general rule, the vigor and extent of the examination should be based on the patient’s history. The goal is to gain enough information to proceed intelligently without exacerbating the patient’s symptoms unnecessarily. Therefore, for patients with very severe symptoms the exam should be more limited. Also, tests or motions that are anticipated to most likely provoke symptoms should be saved for the end of the examination whenever possible so as to avoid clouding the remaining tests.
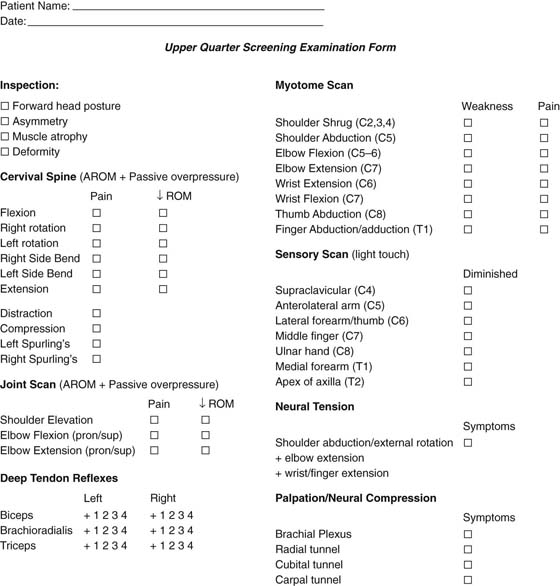
Figure 10-1 Upper quarter screening form. (This figure is available as a PDF at ExpertConsult.com)
The screening examination includes inspection, progressively vigorous cervical spine testing, a brief systematic scan of the peripheral joints, myotome testing for motor weakness, sensory testing for diminished light touch sensation, reflex testing, and special tests related to neural tension and palpation of common entrapment sites.
Inspection includes observation from the side as well as anterior and posterior views. Any asymmetry should be noted as well as gross postural abnormalities. Careful attention should be given to normal soft tissue contours to observe for muscle wasting in key areas such as the supra- and infraspinous fossa (rotator cuff atrophy), and the upper trapezius and deltoid musculature (Fig. 10-2A). Anteriorly, the supraclavicular area should be inspected for any swelling (loss of normal concavity), which could represent swelling associated with brachial plexus injury as well as the potential for an upper lung tumor (Fig. 10-2B). Asymmetrical shoulder heights are somewhat common, with the dominant side being lower than the nondominant side. However, an elevated shoulder girdle could represent protective guarding associated with a cervical spine or neural tension problem, and a low shoulder may provoke neural tension problems.
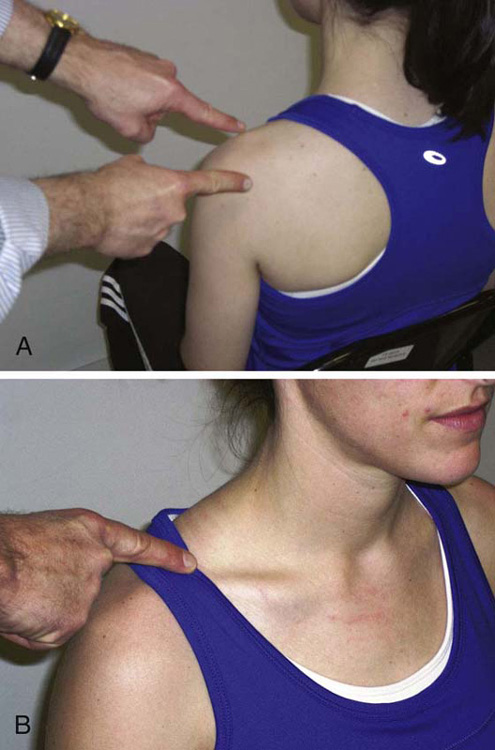
Figure 10-2 A, Normal soft tissue contours for the upper trapezius, supraspinatus, and infraspinatus muscles. B, Normal concavity in supraclavicular area.
The cervical spine is probably the most common source of referred pain to the upper extremity. If the problem is from direct compression of a nerve root or spinal nerve (cervical radiculopathy), the symptoms will include either sensory disturbances or motor weakness.3,10 More commonly, the cervical somatic tissues (ligaments, facet joints, disk, muscle) can refer pain to the upper extremity without direct neural compression.4,5,9,11-13 In either case, the goal of the examination is to reproduce the chief complaint symptoms with ROM tests or special tests. ROM testing is done in each direction, first actively, then with passive overpressure applied at the end range if the active motion was pain-free (Fig. 10-3). Generally, cervical extension is the most provocative motion and should be performed last. If standard motions do not provoke symptoms, special tests can be performed. These include cervical distraction, the Spurling test, shoulder abduction test, and the upper limb tension test (Figs. 10-4 to 10-7). For cervical distraction (see Fig. 10-4A, B), patients must be relaxed, which is best accomplished by having them supine and applying traction by pulling on the occiput and mandible.3 A positive test is diminished symptoms during distraction. Distraction may also be accomplished with the patient seated while leaning back slightly on the chair or directly on the examiner.14,15 Spurling’s maneuver16 as originally described involves passive sidebending with overpressure and axial loading (see Fig. 10-5); although, several authors have described the test to include ipsilateral rotation and extension. A positive test requires reproduction of the patient’s chief complaint symptoms, because many patients feel some local neck discomfort during the maneuver that is not part of their symptom complex. The basis for this test is that this position maximally narrows the intervertebral foramina on the side being tested.17 The shoulder abduction test is performed by the patient resting the hand on top of the head for approximately 30 seconds, and a positive test is when the chief complaint symptoms are reduced or eliminated (see Fig. 10-6). The upper limb tension test has many variations, but all utilize a combination of extremity movements performed sequentially to produce tension in the neural tissues.18 Specific tests for adverse neural tension within the upper quarter are discussed more completely in Chapter 118. A simple screening maneuver for the upper quarter is the combined active motions of full shoulder abduction in the frontal plane plus elbow, wrist, and finger extension. Generally, the elbow, wrist, and fingers are extended first, and shoulder abduction is the final motion. If the chief complaint symptoms are reproduced, or shoulder abduction is appreciably reduced when combined with elbow, wrist, and finger extension, the possibility of adverse neural tension must be more fully evaluated. Wainner and colleagues3 studied the upper limb tension test (ULTT, part A), which was performed passively with the patient supine in a sequential fashion as follows: (1) scapular depression, (2) shoulder abduction, (3) forearm supination with wrist and finger extension, (4) shoulder lateral rotation, (5) elbow extension, and (6) contralateral and ipsilateral cervical sidebending. The patient is questioned regarding reproduction of chief complaint symptoms during the entire procedure. The criteria for a positive response were any of the following: (1) reproduction of the chief complaint symptom, (2) greater than a 10-degree difference between sides with elbow extension, (3) chief complaint symptoms increased with contralateral sidebending and decreased with ipsilateral sidebending.
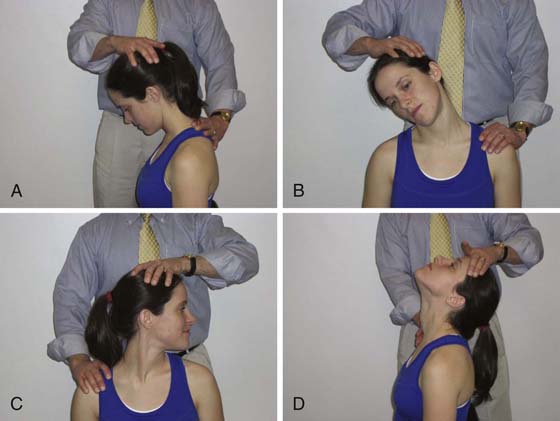
Figure 10-3 Cervical range-of-motion testing. The patient first moves to the end range actively. If no symptoms are elicited, passive overpressure is added. A, Flexion. B, Sidebending. C, Rotation. D, Extension.
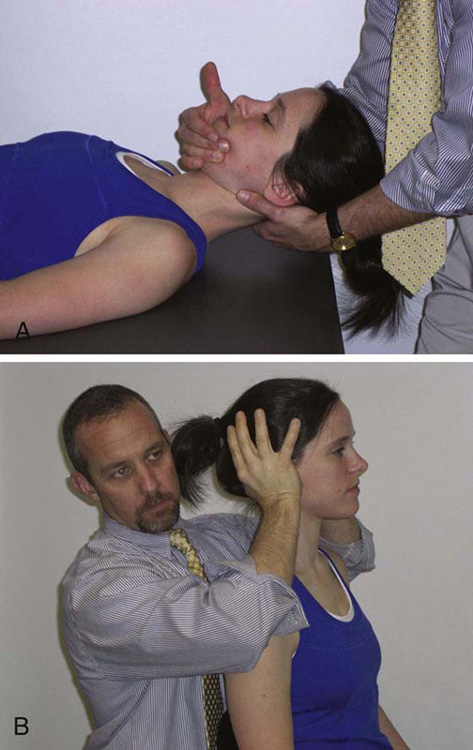
Figure 10-4 Cervical distraction. A, The supine position is best for relaxation and application of force but may not be efficient during a screening examination. B, In seating, the force is applied superiorly via the occiput. The patient must be completely relaxed which is best achieved by asking her or him to lean back on the chair or against the examiner.
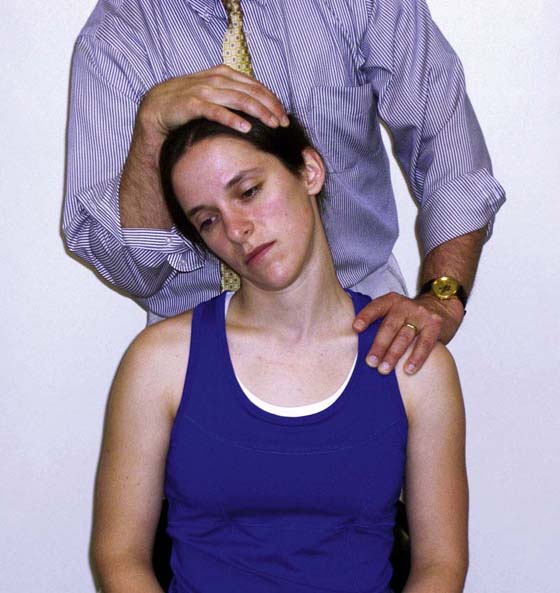
Figure 10-5 Spurling’s maneuver is performed by combining cervical sidebending and axial compression to the cervical spine.
A few studies have provided data regarding the ability of these special clinical tests to detect cervical radiculopathy.2,3,15,19-21 In these studies, cervical radiculopathy was generally confirmed using needle electromyography or imaging findings as an appropriate gold standard. However, positive electromyographic or imaging findings would not necessarily be expected with referred pain from the cervical somatic tissues (i.e., disks, ligaments, facet joints, muscles), which could occur with or without direct irritation of a cervical nerve root (radiculopathy). Therefore, these studies are relevant only to screening for cervical radiculopathy and not for any referred pain emanating from the cervical spine. The findings of these studies are summarized in Table 10-1. Of particular relevance to a screening examination are the sensitivity and specificity of these tests. For screening purposes, tests with high sensitivity are most valuable because a highly sensitive test is least likely to miss a positive case (i.e., a low rate of false negatives) and is therefore useful for “ruling out.” In contrast, tests with high specificity are useful for “ruling in” a specific condition, which is not the goal of a screening examination. Based on the available data, the ULTT is the most valuable screening test because of its high sensitivity. Although other tests may be useful in diagnosing radiculopathy, they are less useful as screening tests because of their generally low sensitivity. However, given generally acceptable specificity, when they are positive, patients should be examined in greater detail for a probable cervical spine-related problem.
Table 10-1 Sensitivity and Specificity of Special Tests to Detect Cervical Radiculopathy*
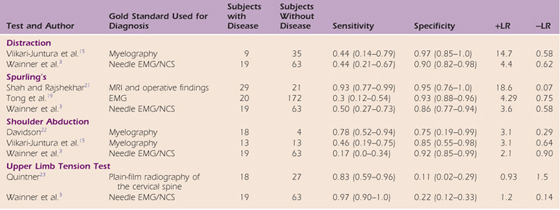
EMG/NCS: electromyography/nerve conduction study.
* Downloadable form available at ExpertConsult.com.
Having tested the cervical spine, the joint scan is designed to quickly ascertain whether the shoulder or elbow joints may be a source of symptoms. The idea here is to take the glenohumeral and elbow joints through full passive motion and then apply overpressure. If no symptoms are produced, this is reasonable evidence that these joints are not the source of symptoms. For glenohumeral testing, the scapula must be blocked from gliding or rotating superiorly, so the stress is focused on the glenohumeral joint (Fig. 10-8). Full elbow flexion and extension are combined with pronation and supination.

Figure 10-8 Passive stress to the glenohumeral joint is accomplished by blocking upward scapular motion with one hand while passively elevating the arm.
During the myotome scan (Fig. 10-9), muscles that correspond to particular spinal segments are tested for the presence of weakness, as listed in the form in Figure 10-1. The patient should be instructed to “hold, don’t let me move you” while the examiner slowly increases the applied force in a controlled fashion. Because the primary goal here is to detect weakness associated with neurologic compromise, strength should be judged normal or diminished relative to the uninvolved side. If both sides are symptomatic, the examiner must use judgment based on past experience. The results of manual muscle testing must be interpreted cautiously because the reliability of these tests is generally poor to moderate.3 If the strength of the muscle is questionable, some type of instrument should be used to document muscle performance more precisely. Resistance that is initially strong but then is easily broken because of pain does not represent neurologic compromise but more likely some irritation of the muscle–tendon unit itself. Painless weakness is most suggestive of neurologic compromise or a complete tear within the muscle-tendon unit.

Figure 10-9 Myotome scan. A, Shoulder shrug (C2–4). B, Shoulder abduction (C5). C, Elbow flexion (C5–6). D, Elbow extension (C7). E, Wrist extension (C6). F, Wrist flexion (C7). G, Thumb abduction (C8). H, Finger abduction. I, Finger adduction (T1).
During the sensory scan (Fig. 10-10), dermatomes that correspond to particular spinal segments are tested for the presence of diminished sensitivity to light touch as listed in the form. A cotton ball or a brush of the examiner’s fingertip may be used bilaterally while the patient is asked “Do these feel the same or different?” If the patient responds “different,” the examiner asks “more or less?” The examiner should be careful not to lead the patient by saying something like “Does this feel less here?”
If the history suggests the possibility of peripheral nerve entrapment, the more common sites of entrapment may be palpated in an effort to reproduce the symptoms (Fig. 10-11). These sites include the brachial plexus in the supraclavicular fossa, the posterior interosseous nerve in the radial tunnel as it pierces the supinator muscle, the ulnar nerve in the cubital tunnel, and the median nerve in the carpal tunnel.

Figure 10-11 Palpation of common entrapment points. A, Brachial plexus. B, Radial tunnel. C, Cubital tunnel. D, Carpal tunnel.
Reflex testing (Fig. 10-12) may be helpful in determining if there is neurologic compromise; however, hyporeflexia is rather common, so care must be taken to compare reflexes bilaterally.1,10 Hyporeflexia represents lower motor neuron compromise, which may be at the nerve root, spinal nerve, or at a more distal level. If hyper-reflexia is observed, upper motor neuron compromise is suggested, such as might occur with spinal stenosis in the cervical region.
The upper quarter screening examination is designed to provide a quick (5–10 minute) method of (1) determining the region(s) that should be examined in greater detail and (2) ruling out serious neurologic deficits. The screen is most useful in patients whose history suggests the possibility of cervical spine involvement, referred pain, or those for whom the source of symptoms is unclear.
1. Magee DJ. Orthopedic Physical Assessment. Philadelphia: Saunders; 2002.
2. Rubinstein SM, Pool JJ, van Tulder MW, et al. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007; 16: 307–319.
3. Wainner RS, Fritz JM, Irrgang JJ, et al. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003; 28: 52–62.
4. Feinstein B, Langton J, Jameson R, Schiller F. Experiments on pain referred from deep tissues. J Bone Joint Surg (Br). 1954; 36: 981–997.
5. Kellgren JH. On the distribution of pain arising from deep somatic structures with charts of segmental pain areas. Clin Sci. 1939; 4: 35–46.
6. Bogduk N. The anatomical basis for spinal pain syndromes. J Manipulative Physiol Ther. 1995; 18: 603–605.
7. Bogduk N, Aprill C. On the nature of neck pain, discography and cervical zygapophysial joint blocks. Pain. 1993; 54: 213–217.
8. Simons DG, Travell JG, Simons LS. Travell & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore: Williams & Wilkins; 1999.
9. Bogduk N. The anatomy and pathophysiology of neck pain. Phys Med Rehabil Clin North Am. 2003; 14: 455–472. v
10. Lestini WF, Wiesel SW. The pathogenesis of cervical spondylosis. Clin Orthop Relat Res. 1989; 239: 69–93.
11. Kellgren J. Observations on referred pain arising from muscle. Clin Sci. 1938; 3: 175–190.
12. Cooper G, Bailey B, Bogduk N. Cervical zygapophysial joint pain maps. Pain Med. 2007; 8: 344–353. (Malden, Mass).
13. Mimori K, Muneta T, Komori H, et al. Relation between the painful shoulder and the cervical spine with narrow canal in patients without obvious radiculopathy. J Shoulder Elbow Surg. 1999; 8: 303–306.
14. Bertilson BC, Grunnesjo M, Strender LE. Reliability of clinical tests in the assessment of patients with neck/shoulder problems—impact of history. Spine. 2003; 28: 2222–2231.
15. Viikari-Juntura E, Porras M, Laasonen EM. Validity of clinical tests in the diagnosis of root compression in cervical disc disease. Spine. 1989; 14: 253–257.
16. Spurling RG, Scoville WB. Lateral rupture of the cervical intervertebral disc: a common cause of shoulder and arm pain. Surg Gynecol Obstet. 1944; 78: 350–358.
17. Yoo JU, Zou D, Edwards WT, et al. Effect of cervical spine motion on the neuroforaminal dimensions of human cervical spine. Spine. 1992; 17: 1131–1136.
18. Elvey RL. Physical evaluation of the peripheral nervous system in disorders of pain and dysfunction. J Hand Ther. 1997; 10: 122–129.
19. Tong HC, Haig AJ, Yamakawa K. The Spurling test and cervical radiculopathy. Spine. 2002; 27: 156–159.
20. Wainner RS, Fritz JM, Irrgang JJ, et al. Development of a clinical prediction rule for the diagnosis of carpal tunnel syndrome. Arch Phys Med Rehabil. 2005; 86: 609–618.
21. Shah KC, Rajshekhar V. Reliability of diagnosis of soft cervical disc prolapse using Spurling’s test. Br J Neurosurg. 2004; 18: 480–483.
22. Davidson RI, Dunn EJ, Metzmaker JN. The shoulder abduction test in the diagnosis of radicular pain in cervical extradural compressive monoradiculopathies. Spine. 1981; 6: 441–446.
23. Quintner JL. A study of upper limb pain and parasthesiae following neck injury in motor vehicle accidents: assessment of the brachial plexus tension test of Elvey. Br J Rheumatol. 1989; 28: 528–533.

To view a companion video on this topic, please access ExpertConsult.com.