
Figure 25-1 Superficial second-degree burn depth that is expected to heal within 10 days with minimal scarring.
▪ Thermal burns to the upper extremity constitute a major injury and source of disability, despite the disproportionately small body surface area involved.
▪ The depth of burn injury predicts the course of treatment and the degree of functional recovery. Correct assessment is essential.
▪ Early excision and grafting of deep burns is preferred.
▪ Burn contraction and surface contour determine therapy planning and plateaus.
▪ The quality of the burn scar, its response to therapy, and the expected functional outcome suggest the timing and extent of the burn scar reconstruction.
Every year in the United States, approximately 700,000 people receive treatment for a burn injury, of whom 40,000 require hospitalization.1,2 Of those burned patients admitted to the hospital, nearly 80% have a burn injury involving the upper extremity.3,4 Flame burns are the predominant cause of burn injury in adults admitted to the hospital. Scald burns from hot liquids are the most common cause of burn injury in children; 45% of children sustaining burns are younger than 5 years. Work-related injuries account for 25% of all burn-related hospital admissions.3
Burns of the hand and upper extremity result in permanent functional and esthetic deformities. The extent of the deformity is directly related to the severity of the initial injury. Thermal burns to the hand constitute a major injury, despite the disproportionately small body surface area involved. Proper evaluation, assessment of burn depth, and coordinated management of the burned upper extremity can improve the level of functional return and shorten the period of time before a return to productivity and work.5,6
Knowledge of the cause of the burn as well as the length of time of exposure play a significant role in assessing the depth of the injury, the recovery time, the plan for treatment, and the anticipated level of functional recovery. A burn wound heals by reepithelialization if the depth of injury is confined to the dermis or epidermis. The concentration of uninjured hair follicles, neural elements, and sweat glands at the depth of the unburned dermis determines the rate of reepithelialization. The greater the remaining concentration of these uninjured adnexal elements in the dermis, the faster the burn wound will heal and the better the quality of the resultant burn scar. Complete loss of the dermis, as occurs in full-thickness burns, requires skin resurfacing. The quality of a healed burn scar heavily influences the degree of functional return. Correct assessment of the depth of injury is the first step in managing the upper extremity burn.
Burn care involves a team management approach. A total patient care plan must be established within the first 24 hours. The physicians are responsible for resuscitation and the management plan. The nursing staff coordinates and implements dressing change protocols and family interaction. Their constant patient contact allows the nurses to provide physicians with the information necessary to make appropriate decisions regarding pain management and times of dressing change, therapy, and rest. Occupational and physical therapists coordinate a plan for orthosis use and exercise and interact with staff. Nutritionists plan the appropriate calorie and protein content and coordinate with nurses and physicians regarding ongoing procedures. The social service department plays a significant role in establishing benefits for the patient and answering insurance coverage and job-related questions. Many others play a role in total patient care. Management strategies are formulated in twice-weekly multidisciplinary conferences. The patient and family are immediately aware of the treatment planned as well as the changing goals for optimum functional improvement. Strict attention to upper extremity function during total patient care is a responsibility of all involved in the treatment of the burn patient.
The initial extent of the total burn injury is assessed using the “rule of nines.”7,8 The total body surface area burned is estimated using this easily reproducible protocol. This information predicts the overall severity of the burn injury and estimates early patient fluid resuscitation. The upper extremity constitutes 9% of the total body surface area; the hand by itself represents 3%.3,9 The depth of burn injury as well as the total surface area and location involved predict the course of treatment and the functional recovery. This assessment also provides early valuable information to the patient and family concerning time of recovery.
A first-degree burn is confined to the epithelial layer of skin, producing erythema and mild discomfort. The injured area is red, and blisters are usually not seen on examination. Full function remains, reduced, however, by the acute pain. Symptoms of pain and swelling are of short duration. Topical application of a moisturizer to the exposed surface of the burned area reduces the pain. Reepithelialization begins within 48 hours. No restrictive scar results.
By definition, second-degree burn injury penetrates into the dermis (Fig. 25-1). These levels of injury are classified into superficial second-degree and deep second-degree burn. The superficial second-degree injury involves the upper level of the dermis and is expected to reepithelialize within 10 to 14 days with topical wound care.10 The appearance of the burn is characterized by blisters, intact or ruptured, a thin eschar, and severe pain. The periphery shows an erythema as the level of burn injury becomes progressively more superficial.

Figure 25-1 Superficial second-degree burn depth that is expected to heal within 10 days with minimal scarring.
The deep second-degree injury extends to the depth of the dermis, injuring a greater concentration of the adnexal hair follicles and sweat glands. This diminishes the ability for reepithelialization and results in delayed healing—taking between 14 and 21 days to completion. The appearance of this injury, in contrast to the superficial second-degree burn, shows the absence of blisters and sometimes a moderate-thickness eschar (Fig. 25-2). Immediate pain is less intense because the superficial nerve endings are injured by the burn at this depth. The quality of the resultant burn scar healing after these depth injuries can be poor, increasing the risk of later hypertrophy and secondary scar contracture.
The specific location of injury also helps guide the management plan. Areas of thin skin, flexion and extension creases, and fine joints of the fingers are severely affected by the persistent inflammation of slowly healing wounds and the resultant restricting scars. When poor-quality healing or hypertrophic scar is anticipated, early resurfacing with better quality skin must be considered.
Full-thickness burn injury, or third-degree burn, destroys the entire dermis, and with it the potential for reepithelialization and healing. The presence of a thick inelastic eschar defines the depth of injury (Fig. 25-3). Initially, the burn surface is not painful. Skin graft resurfacing is indicated because no spontaneous epithelialization is possible. Early grafting reduces the morbidity of anticipated contracture and subsequent reduction of function. The small joints of the hand are extremely sensitive to any degree of skin restriction.
A fourth-degree burn results from prolonged thermal contact and involves the soft tissue and underlying tendon, joint, and bones.4 The injured tissue at this depth is charred. Prolonged hot immersion, extended flame contact, and electrical burn injury may show this depth of tissue destruction. Extensive reconstructive procedures and, more often, amputation result.
Burn depth in the hand is often mixed (Fig. 25-4). Superficial areas of injury heal spontaneously by epithelialization, whereas others require resurfacing to prevent functional loss. The treatment plan must be individualized after careful burn assessment. The management goal is to resurface all burns that are not expected to reepithelialize within 14 to 21 days with suitable quality grafts.11 Burns that will reepithelialize sooner are carefully assessed for improvement daily.

Figure 25-4 Mixed deep and superficial second-degree burns. The depth of the burn is related in part to the thickness of the skin.
Although the depth of burn is important, additional information concerning the injury permits the treatment team to plan more precisely. The source of the thermal injury is extremely important. A scald injury traditionally produces a burn more homogeneous in depth and appearance. Knowledge of the temperature of the scalding liquid and the length of the contact time helps to better define the depth of injury. Water at 158°F causes full-thickness injury in a child within 1 second.7 Lower temperatures also produce equal-depth burn if the contact time is prolonged. Liquid with fat or grease added retains greater heat, producing a deeper burn in less time (Table 25-1). Fire burns in open air at approximately 500°F. Contact with burning substances or ignition of clothing produces a full-thickness burn injury almost immediately.
Table 25-1 Time Needed for Hot Water Immersion to Produce Third-Degree Burns
Temperature (°F) |
Time |
158° |
1 sec |
150° |
2 sec |
140° |
10 sec |
130° |
30 sec |
127° |
1 min |
120° |
10 min |
The thickness of the skin in the involved area also plays a very significant role. The thickness of the dermis in the injured area determines the speed with which the skin can reepithelialize. The depth of injury relative to the skin thickness also predicts the quality of the healing process. The skin of the dorsum of the finger, the dorsum of the hand, the volar wrist, and the inner arm represents relatively thin dermal areas. A deep second-degree burn at any of these levels is associated with delayed epithelialization and a poor quality restricting burn scar. Scar breakdown, fibrosis, and injury in proximity to joints compromises function because of associated joint contracture and restricted motion. The same source and contact time of the burn injury applied to the palm, however, may be associated with a more rapid epithelialization with no functional long-term restriction owing to the rich concentration of adnexal elements in the dermis of palmar skin. The quality of the skin at the level of injury is another important factor in determining the outcome.
The severity of the burn is determined by the combination of the temperature of the source, time of contact, thickness of the skin, and area of the burn injury. This information, as well as the early appearance on examination, permit decision making for either continuation of conservative management or an early plan for excision and grafting of the wound. The goal of burn management is maximum restoration of function with stable soft tissue coverage in the earliest possible time.12,13
The management of each burn must be individualized. Patient compliance, understanding the type of work the patient performs, and overall burn size are important factors in the management plan. The experience of the surgeon and therapist in evaluating the progressing clinical picture in light of the expected outcome is an extremely important part of the treatment protocol.
Admission to a burn treatment facility is indicated for second-degree burns in excess of 10% to 15% of body surface and for third-degree injuries as small as 3%. Patients requiring resuscitation or those having smaller areas of burn requiring specialized care meet the criteria for hospital admission as well.2 A large number of minor burn injuries are also treated on an outpatient basis in major centers or physicians’ offices. Initial management involves evaluation of the burn wound severity and the selection of a treatment plan. The burn surface is cleaned and all foreign debris is removed. Broken blister epithelium is débrided. When blisters are intact, the treating physician is faced with a decision to either débride the blisters or leave them intact until the next dressing change.14,15 As a matter of protocol, when the blisters are covered by thin epithelium, they are débrided along with the exudate. Blisters in the palm are usually covered by a thicker epithelium. These blisters are incised, the fluid is removed, and the epithelium is used for resurfacing the wound as a biological dressing. This provides effective wound coverage, diminishes pain, and permits epithelialization below. For wounds without epithelial coverage, an impregnated gauze dressing or skin substitute may be used as temporary coverage with dressing changes at 24 to 48 hours.
A more extensive burn injury requiring fluid resuscitation produces local and often generalized edema. An orthosis should be applied immediately to maintain joint position of the wrist in extension and the metacarpophalangeal (MCP) joint at 90 degrees of flexion to protect ligament tension. The interphalangeal (IP) joints are positioned in full extension (Fig. 25-5).12,13 This extended position decreases tension on IP joint capsules, ligaments, and the overlying burned skin. The extended position also provides protection, when indicated, from exposure of the extensor tendon through the severely injured thin skin covering the proximal interphalangeal (PIP) or distal interphalangeal (DIP) joint.


Figure 25-5 A, Universal orthosis used to protect ligaments and fine joint capsules. B, MCP joints at 90 degrees and IP joints in full extension.
Fibrosis and persistent small-joint inflammation is a cause of postburn stiffness and joint deformity. The longer the burn wound remains open, the longer inflammation around the fine joints continues. This inflammation is the source of progressive scar formation and restriction of motion. Intensive hand therapy during the acute period is scheduled at least twice daily, with the nursing staff continuing exercises between dressing changes. Pain, high levels of sedation, and significant swelling may preclude full active or passive joint motion. Continuous passive motion (CPM) devices can be employed in an attempt to maintain overall range until the patient can participate in active exercises.5 Compliance, however, is often altered by pain, and goals are all too often not completely met during the acute period.
Most patients with burns of the upper extremity have additional areas of burn injury. Forty-five percent of nonfatal burns involve the upper extremity.2 The burn patient is assessed for the extent of the total burn injury. Fluid resuscitation and airway patency are first ensured. When the patient’s emergent condition is stabilized, management of the upper extremity becomes a definitive part of the overall burn care. Evaluation of the hand and upper extremity begins with an appreciation for the presence of compartment swelling. Observation of the extremity with dressings removed is essential. Circumferential burns of the hand, fingers, and extremity increase venous pressure and begin acting as a tourniquet. Combined with an increase in soft tissue swelling, compartment pressure may increase above 30 mm Hg, causing tissue necrosis. An initial clinical diagnosis may be sufficient when the pattern of burn involvement is extensive and deep.16 Burn injury, however, may show progressive swelling with slowly increasing pressure and less acute signs of compartment syndrome. Clinical signs of severe distal swelling despite elevation, progressive loss of sensibility, intrinsic negative posturing of the hand, and constant unrelenting pain suggest increased compartment pressures.
Anticipation of increasing pressure suggests the need for compartment measurements performed with a baseline value obtained for comparison over the first 24 hours. Increased pressure values or the expectation of a compartment syndrome as edema continues indicate the need for an emergency escharotomy (Fig. 25-6).17 Complete decompression of all compartments involved in the burn injury is then indicated. The axial escharotomy incisions of the fingers and the upper extremity result in immediate reduction of pressure. Individualized compartment releases in the hand, including the intrinsic muscles, may be necessary to achieve pressure reduction.18 Escharotomy is, however, not a guarantee of tissue survival. The origin of the burn and length of exposure may be too extensive for soft tissue survival of the distal digits (Fig. 25-7). Clinical observation of progressive distal swelling, intracompartment measurements, and pulse oximetry have been used to evaluate these conditions.19

Figure 25-7 Escharotomy had been indicated, but tissue injury resulted in necrosis of the fine soft tissue distally.
The thin dorsal skin of the hand and fingers is often involved in deep burns of the extremities based on initial protective motions such as firm fist making. Immediate management of all burns includes surface lavage of all debris and débridement of nonviable epithelium and blisters. Topical silver sulfidiazine antibacterial cream is applied with soft bulky nonconstricting gauze dressings, contoured to the burned areas of the extremity. Custom-fitted orthoses are fabricated at the bedside to maintain individual functional positions and to protect the small joints.
Management of second-degree burns of the extremity is guided by burn depth and area of involvement. Conservative management with dressing changes, whirlpool, and active and passive range of motion (ROM) exercises provided by a therapist is appropriate for burns that are expected to heal satisfactorily in a defined period of time. Early excision and grafting are advocated for those injuries for which no healing, or poor-quality healing is anticipated.
Several authors have advocated delayed excision of deep second-degree and even third-degree burns of the hand, allowing additional time to see if epithelialization will occur.20 In a selected group of patients with deep second-degree burns, Salisbury and Wright showed that intensive therapy produced functional results similar to those achieved in hands in which the burns were excised and grafted early in their course.11 Patient compliance is essential in these circumstances. In my experience, deep second-degree burns of the hand and fingers that are not expected to epithelialize within 14 days are excised early and immediately skin-grafted. This has resulted in a predictable return to function and less long-term stiffness.
Direct tangential excision or fascial excision is indicated for burns that will not heal by reepithelialization.21,22 Early excision is preferred as soon as possible after the decision to excise is reached and the patient is stable for anesthesia. Tangential excision under tourniquet control removes all injured tissue, leaving only viable dermis and a well-vascularized bed for a skin graft (Fig. 25-8). If the burn injury involves the entire dermis and includes thrombosis of the subdermal vessels, the plane of excision must be deeper at the fascial level. In the hand, all attempts are made to excise above the neurovascular plane of the dorsum. Excision involves surgical judgment to ensure complete resection of nonviable burn tissue. This plane is characterized by white, soft, pliable tissue. Once complete excision is achieved, the tourniquet is deflated and the wound is observed for dermal or subcutaneous bleeding. Questionable areas are reexcised until all nonviable tissue is removed. Hemostasis is obtained, temporary pressure dressings are applied, and the hand and extremity are elevated as preparations are made for skin graft harvest.

Figure 25-8 A, Deep second-degree burns on the dorsum of the hand and fingers. B, Tangential excision of burn eschar to punctate bleeding in dermis. C, Application of split-thickness skin graft. D, Supple graft at 3 months with expected hyperpigmentation.
Once hemostasis is complete, the skin graft is applied to the bed. Sheet grafts, piecrusted for drainage, generally measuring approximately 0.012 inches in thickness for the average adult, are preferred for the hand and fingers. Resurfacing a child’s hand requires thinner grafts. Meshed grafts in ratios of 1:1.5, 1:2, or 1:3 may be used to minimize the use of available remaining noninjured skin (see Fig. 25-8). Conservation of donor skin is critical when the patient has sustained injuries over more than 50% of the body’s surface. The interstices of these meshed grafts heal by epithelialization over scar and are subject to somewhat greater contraction than the sheet graft. If the wound is initially thought unsuitable for graft coverage, application of a topical skin substitute or frequent dressing changes are preferable to immediate grafting. Delayed secondary grafting is preferable to incurring a significant risk of graft loss on a less than optimal recipient bed.
The graft is applied to the bed with the hand in the functional position of gentle flexion of the fingers and wrist extension.23 The graft is secured with sutures, staples, or fibrin glue (or a combination).24-26 An interface dressing is used, followed by a bulky soft dressing and an immobilizing orthosis. Vacuum-assisted closure (VAC) is a technique of wound management that seals the wound with a foam dressing and applies negative pressure to the wound bed by tubing threaded through the dressing. The vacuum pressure can be applied continuously to the skin-grafted site. Use of the VAC dressing supports the graft, prevents shear forces, and is associated with a lower need for secondary grafting.27,28 Initially, graft observation and assessment are performed at 24 to 48 hours after the acute excision, depending on the confidence in the hemostasis obtained. If no fluid collections are noted, the next dressing change can be at postoperative day 3 to 5. Hand therapy begins at 4 to 5 days after grafting, when graft adherence is secure.29 Exercises consist of active and gentle passive ROM. Orthoses are designed with an emphasis on wrist extension and MCP joint flexion. Dynamic orthoses may be used when the graft is stable and active ROM is slow to return because of stiffness or lack of compliance. Pain management is an essential part of the therapy plan. (See Chapter 26 for an in-depth discussion of therapy for the burned hand).
Burns of the palm often require a more conservative management plan (Fig. 25-9). The specialized skin of the palm and volar aspect of the fingers has a thick epidermis and a dermis rich in adnexal elements. Burn depth based on palmar skin thickness and a protective flexion response to injury may permit high-quality reepithelialization in a shorter than expected time. More conservative treatment is suggested until the depth of the palmar burn is fully defined. When the palmar burn is full-thickness, resurfacing is indicated to prevent the functional loss brought about by late palmar and digital joint contracture.
Advocates for resurfacing of the palm with either full-thickness or split-thickness skin have based their decisions on long-term wound hypertrophy, recurrence of contractures, and development of burn syndactyly.30 A split-thickness graft offers the best alternative in the acute burn wound. Graft take is often better because of the shorter time to revascularization and the ability to resurface larger areas. No appreciable difference was seen in long-term contracture results in deep palmar burns. Full-thickness grafting can be reserved for later reconstructive procedures when graft take presents less of a risk for loss.31
Once the acute burn wound has healed completely, attention is given to a program of improved motion, stretch, and positioning during scar maturation. Hand therapy includes frequent visits for active and passive motion. Serial orthosis use maintains position; a dynamic orthosis is often used for constant and progressive stretch between exercise periods. Massage, silicone sheeting, and conformer application are part of the management plan during the maturing phase of approximately 12 months. The therapist’s role is to bring all joints of the extremity to their maximum function and aid in soft tissue softening and desensitization. The therapist and treating physician must also identify when functional improvement reaches a plateau.
The quality of the burn scar influences the ease of return of hand and extremity motion. A poor-quality thick scar is associated with stiffness that is more pronounced after sleep or inactivity. Improvement in scar quality as softening occurs over the first 6 to 12 months updates the prognosis for improved or full-joint function. Strict attention to anticipated time of healing of the initial burn wound, scar fibrosis and thickening, proximity of the injury to fine joints, age, and occupation help predict return to function. Early resurfacing of a deep burn injury with a better-quality skin produces a better long-term result. The following case study outcome defines the practical meaning of quality results in burns of the hand.
A 19-year-old man was admitted to the burn center when he sustained burns to the dorsal aspect of both hands and fingers while working on a car engine. The entire dorsal aspect of both hands and fingers were noted to have deep second-degree burns with extensions onto the thenar eminence and distal wrist. Left and right hands were similar in involvement. The palmar surfaces were not burned. There was no suggestion of compartment syndrome or increased pressure. A decision was made to excise the deep burns early with immediate skin graft resurfacing, beginning with the right hand and following 48 hours later with the left.
All fingers and the dorsum of the right hand and wrist underwent an uncomplicated excision and graft procedure. Graft take was complete. Just before scheduling the left hand for a similar procedure, the treating physician made a decision to allow more time for reepithelialization rather than grafting the left hand. The management plan was changed. The left hand had completely epithelialized by the 20th postburn day. The patient showed excellent compliance in therapy and achieved full flexion of all digits of both hands. He returned to his work as an auto mechanic approximately 4 months after his injury.
At 6 months, during routine follow-up examination, this patient provided a superb insight into the quality of burn healing (Fig. 25-10). He noted that the right hand showed no stiffness on awakening, and he had a full ROM of all digits. He was comfortable and had no pain in making a fist. The stability of the hand grafts was excellent, and he described no wound breakdown since the graft had been applied. He had no trouble going about his work, even sustaining frequent superficial injuries against the engine block. The left hand, however, was extremely stiff in the morning, taking up to 20 minutes for him to overcome the stiffness in the small joints and obtain full flexion. The left hand had a constant general aching, and wound breakdown in response to minor trauma was frequent. The appearance of the left hand showed parchment-like burn scar and web syndactyly as opposed to the smooth, well-pigmented graft on the right hand.

Figure 25-10 A, Significant functional difference between the grafted right hand and the left hand after second-degree burn. Note the parchment-like epithelium, hypertrophic scarring, and the loss of pigmentation on the left. B, Note the poor-quality scar and the contracting webs associated with secondary healing on the left compared with skin grafting resurfacing on the right.
The patient was not about to undergo a secondary procedure unless absolutely necessary for unstable scarring or web restriction. The patient achieved full coverage of the burn wound of both hands and, with therapy, achieved full active and passive ROM. The difference in quality of the function of the healed burn wounds is clearly appreciated in this patient interview. Appreciation of expected wound quality is an important part of decision making during the acute period. The notion that if the wound becomes hypertrophic or unstable then one can always return for resurfacing is not valid. The fibrosis, soft tissue shortening, and tendon imbalance that occur cannot be improved satisfactorily after long-standing stiffness and decreased motion (Fig. 25-11). Early aggressive wound management based on a thorough knowledge of wound healing decreases many of the problems seen in the reconstructive period.

Figure 25-11 Extensive fibrosis and hypertrophic scarring has resulted from prolonged secondary healing of this second-degree burn. The resultant stiffness will be permanent.
Basic principles in planning burn scar reconstruction involve a serious appreciation of forces of contraction.32 Understanding how the contracture developed increases the possibility that a reconstructive procedure will be successful, avoiding an early recurrence and its associated functional restriction. These principles assume that the burn scar is well healed and fully mature and that all therapy has reached the maximum level of improvement.
Montandon and colleagues write that a scar or skin graft continues to contract until it meets an opposite and opposing force.33-35 Scar and graft contraction progresses over the first 3 months of maturation. The surface over which a contracting burn scar lies also influences the contraction process. Scar over concave surfaces meets less resistance than that over convex surfaces, allowing greater migration of the scar and webbing. Examples of this include axillary contractures, distal migration of the dorsal finger webs, and flexion contractures on the antecubital surface of the elbow (Fig. 25-12). The quality of the scar, its response to therapy, and the expected functional result based on the contour of the area in question help determine the timing and extent of the burn scar reconstruction.

Figure 25-12 Burn scar deformities on concave surfaces of the flexor portions of the wrist and digits result in decreased forces opposing contracture.
A burn scar is always synonymous with a skin deficit. In planning a reconstructive procedure, the deficit of soft tissue after scar release is always larger than expected. A diagram of the original burn-injury surface helps to anticipate the reconstruction defect. A generous overcorrection with skin graft alone does not ensure a successful reconstruction because the forces of contraction are governed by the surface characteristics of the area. Adding more skin grafts to the release of a severe axillary contracture does not guarantee that restriction of the arm abduction will not recur. External orthosis application and the early return of abduction motion adds resistance to the contractile forces. The graft will simply continue to contract until it meets the precise opposing force, also determined by surface characteristics.
The resting posture of the hand normally maintains the fingers and wrist in slight flexion. Moderate to deep burn injury across the volar wrist, the palm, and the palmar surface of the digits can easily produce a flexion contracture if the details of proper treatment are neglected (Fig. 25-13). Palmar burns that heal by epithelialization or even those that require skin graft coverage have a common tendency to contract, producing flexion deformities. ROM and stretch exercises as well as sequential orthosis use during the period of scar maturation counter the forces of contraction and result in well-balanced motion. Failure to satisfactorily improve this flexion deformity as the burn scar matures prompts consideration for early scar contracture release, skin graft or flap application, and renewed hand therapy to restore ROM.
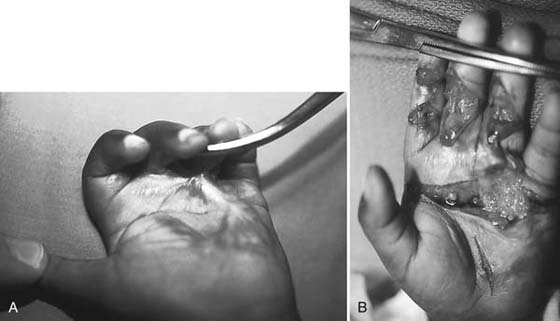
Figure 25-13 A, Palmar contractures result in significant soft tissue deficit. Burn contractures in the palm almost always necessitate the addition of skin. B, Note the significant tissue deficit resulting from simple release of burn scar contractures.
Flexion contraction that progresses despite extension orthosis use results in secondary joint contractures as the burn scar matures and contracts. Progressive pain with orthosis use and the inability to obtain full extension of the digits reduce the amount of passive stretch that can be tolerated. The contracture becomes permanent and reduces motion and function. Surgical reconstruction is indicated before further joint contraction is appreciated. Radiographic examination is obtained prior to reconstruction to verify the alignment of the joint surfaces. Kurtzman and Stern classified PIP joint contractures based on their degree of skin deficit and joint narrowing.36,37 More severe and long-standing flexion contractures may require volar joint release in addition to resurfacing of the volar skin deficit. Arthrodesis must be considered in those fingers in which secondary joint destruction precludes full extension, despite adequate soft tissue release.
Complete soft tissue release perpendicular to the direction of maximum contracture is indicated. A transverse incision from midaxial to midaxial point is necessary to release all tissue tension.38 Passive stretch of the contracted joint after soft tissue release defines existing tension. Complete excision of contracted scar is usually not indicated because residual hypertrophic burn scar will mature and soften when the tension forces are released. Resurfacing of the deficit is often achieved using full-thickness skin graft.39 When contracture release involves exposure of tendon, a local flap, if available, is the procedure of choice.40-43 Soft bulky dressings and extension orthotic positioning continue during the postgrafting period. Once adequate release of a contracture in children was established, longitudinal growth did not necessarily produce a recurrence of the contracture. Active extension exercises increase the resistive forces against the graft contraction, diminishing the rate of recurrence.
Maturing dorsal hand burns are characterized by restricted motion and pain. Rehabilitation begins in the acute period with early motion and excision of the burn for deep second-degree or full-thickness burns. The relatively thin dorsal skin of the hand and digits contracts when thermally injured, making digital flexion difficult and producing extension deformities. Achieving maximum flexion at the MCP joints increases resistive force over the dorsum of the hand and is the best prevention against extension contractures. Active ROM, passive stretch into flexion, and dynamic flexion orthotic positioning all attempt to achieve a flexion posture of the fingers during wound healing and maturation.5 This progressive flexion increases the force over the dorsum of the hand and is strong enough to prevent contractures. Failure to achieve progressive improvements in flexion results in hyperextension deformities of the MCP joints and secondary flexion deformities at the PIP joints (Fig. 25-14). This deformity occurs more easily in the ring and small fingers because of the higher degree of metacarpal flexion in these fingers at the carpal–hamate articulation.44,45 As these metacarpals are pulled into increasing extension, the resistance against continued MCP hyperextension continues to decrease. If uncorrected, the outcome produces fixed MCP joint hyperextension and PIP flexion deformities. This pattern differs from the stable second and third carpal metacarpal (CMC) joints—the fixed unit of the hand. Similar hyperextension deformities at these joints are seen only in the most severe burn contractures.
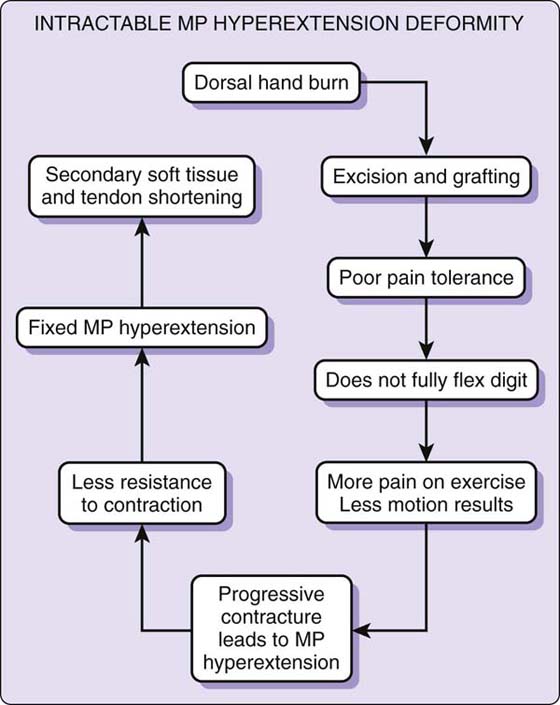
Figure 25-14 Metacarpophalangeal hyperextension deformities may be prevented by early initiation of hand therapy. Range of motion and passive stretch exercises diminish contractions before secondary soft tissue shortening.
The ability to overcome hyperextension stiffness across the dorsum of the hand and fingers demands persistence, compliance with therapy, and tolerance of pain. Some patients, despite analgesia and encouragement, cannot or will not achieve sufficiently improved digital flexion at the MCP level necessary to overcome the increasing forces of contraction. As the dorsal graft or reepithelializing burn scar continues to contract until it meets an equal and opposing resistive force, the MCP joint extension contraction steadily increases toward fixed deformity contracture (Fig. 25-15). The fourth and fifth metacarpals descend progressively into palmar flexion, creating a more concave dorsal surface at the MCP joint level. Resistance to graft contraction is therefore further reduced. This accentuated hyperextension is more prominent on the ring and small fingers. If this cycle is not broken, fixed MCP joint hyperextension results, followed by secondary flexion deformities at the PIP joints. The PIP joint deformity in these cases originates from MCP joint hyperextension and not from direct injury to the central slip over the PIP joint. Because these PIP joint flexion changes are secondary, this deformity is termed pseudoboutonnière deformity, as opposed to a true boutonnière deformity resulting from primary deep tendon injury at the PIP joint level.44

Figure 25-15 Intractable hyperextension deformities at the metacarpophalangeal joints with secondary proximal interphalangeal flexion deformities.
Reconstruction of MCP joint extension contractures begins as hand therapy reaches a plateau. The dorsal soft tissue contracture is released transversely, including the MCP joint capsules when indicated, and the deficit covered with a split-thickness skin graft.46 Postoperative orthosis application following the graft application and the use of dynamic flexion orthoses after the graft has taken (5–7 days) help maximize improvement of the contracture deformity. However, these results depend on the overall suppleness of the released MCP joint and the continued ability to overcome capsular and soft tissue contraction.
Long-standing extension contractures over the dorsum of the hand, if unresolved, produce fixed hyperextension MCP joint deformities (Fig. 25-16). Simple release of the overlying contracted skin may not reduce the entire soft tissue tension present at the capsule level and surrounding the extensor tendons. Forced passive stretch of the MCP joint may achieve the desired degree of flexion. K-wire pin fixation can hold the MCP joint at near 90 degrees if the surgeon anticipates significant residual tension as may remain in the longitudinal contraction of the extensor tendons over the dorsum. This unresolved extrinsic extensor tightness favors recurrence of the hyperextension deformity, frequently within weeks of the contracture release. In this instance, a relative discrepancy persists between skeletal length and available soft tissue.

Figure 25-16 True boutonnière deformities following burn injury are the result of exposure or attenuation of the central slip and capsule over the proximal interphalangeal joint.
Fixed MCP joint extension contractures caused by soft tissue shortening following burn injury can only be resolved by lengthening the foreshortened composite soft tissue or shortening the skeleton length, returning this soft tissue to skeletal ratio to 1 : 1. Available techniques for these intractable deforming contractures include metacarpal shortening, MCP joint replacement, arthrodesis (skeletal length shortening), and extensor tendon lengthening with dorsal flap reconstruction (composite soft tissue elongation). An advanced technique using a tissue expander placed below the extensor tendons stretches these tendons as well as the overlying soft tissue and skin graft, creating a composite soft tissue stretch, returning the skeletal/soft tissue length ratio to normal. Slow, progressive inflation of the expander is not associated with an increased risk of morbidity and complication, even in burn-scarred soft tissue. On removal of the expander, release of the dorsal MCP joint capsule permits passive flexion to 90 degrees with no restriction from the now stretched extensor tendon. A dynamic orthosis protocol permits the extensor tendon to rebalance itself against normal MCP joint flexion exerted by the patient. The strength of this unrestricted digital flexion is now sufficient to bring about a lasting resolution to the extension contracture. The overlying skin and soft tissue remain stable and do not recontract once the force of flexion is unrestricted.47
Deep burns occurring over the PIP joints may produce secondary extension contractures or may result in true boutonnière deformities, depending on the depth of involvement (see Fig. 25-16). The dorsal skin is extremely thin, and exposure or injury to the underlying extensor tendon is not uncommon in patients sustaining deep flame burn injuries. Extension orthosis use protects the tendon from exposure in the acute period depending on the original depth of injury. Early graft resurfacing provides quality tissue if the underlying tendon was not injured.
Injury to the central slip of the extensor tendon overlying the PIP joint progressively results in a true boutonnière deformity. If the quality of the overlying skin remains poor, arthrodesis of the PIP joint into an optimum position of function shortens the skeleton length relative to the available, often unstable, soft tissue. Multiple procedures for soft tissue reconstruction of a postburn boutonnière deformity have been described.48-50 When the overlying skin quality is good, results of tendon reconstruction are fair at best. Stiffness and tendon imbalance persist. Late complications are related to overlying poor-quality skin breakdown and unresolved joint stiffness. Arthrodesis of the PIP joint is a reproducible procedure that improves function of the hand and, by shortening, establishes decreased soft tissue tension and stable wound coverage.
Contracture of the first web space of the hand results in reduction of thumb abduction and opposition (Fig. 25-17).51 Once contraction progresses, static and dynamic orthoses become less effective because their force is dissipated by the radial deviation of the MCP joint of the thumb. Secondary contracture and stiffness of the first dorsal interosseous muscle fascia and the metacarpal trapezial joint can result in a more severe restriction of function.52,53
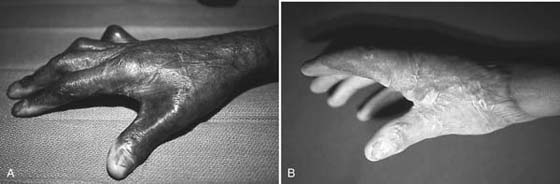
Figure 25-17 A, Mild to moderate postburn contracture of the first dorsal thumb index web space. B, Progressive loss of thumb abduction is appreciated with more severe contracture.
The classification of the thumb index web contracture can be based on the severity of injury.54 A simple web-band contracture, often resulting from a palmar burn, restricts only abduction. With minimal or no burn on the dorsal skin, a lengthening Z-plasty is usually sufficient. When dorsal and palmar surfaces show burn scarring, the anticipated deficit exceeds the soft tissue gain provided by a Z-plasty local flap (Fig. 25-18). A three-dimensional reconstruction may be indicated to lengthen the scar and regain depth of the web. A double Z/V-Y advancement is suitable coverage for the moderate contracture deficit. A tighter web contracture is characterized by a greater skin deficit, exceeding the lengthening possibility with local flap tissue alone. Release of the contracture and resurfacing with full- or split-thickness skin grafts permits maximum functional return in those cases.55-61
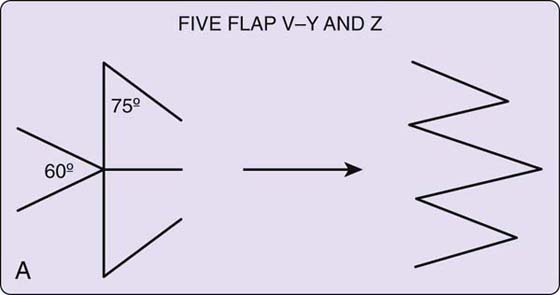

Figure 25-18 A, Design of interdigitating flaps to lengthen the scar contracture and deepen the web space. These flaps are most successful in contractures showing little skin deficit. B, Restoration of web contour and depth.
Very severe contractures involve contraction of the first dorsal interosseous muscle and fascia and even the joint capsule of the metacarpal trapezial joint. The thumb is slowly pulled into the plane of the palm with severe restriction in all directions of motion. The release of the skin deficit contractures, muscle fascia, and, if needed, the CMC joint capsule, permits the return of the thumb to a functional position. Flap coverage is then necessary (radial forearm, free flap, groin, random) to reliably resurface the large defect and possible basal joint exposure.62,63
Maintenance of joint position after contracture releases ensures good graft or flap contact to the underlying bed. The immobilization of the area is maintained for 5 to 10 days until complete graft take or flap stability permits motion without risk of shear. Positioning of the thumb index web space has been described using pin fixation or an external fixator in the more severe cases.
Burn syndactyly is anticipated on any concave web surface where scar or graft has been pulled distally by contraction (Fig. 25-19). This distal migration continues until the scar has reached its maximum tension against resistance. Acute burn injuries of the dorsal hand and fingers often produce burn syndactyly in the web spaces as scar contraction matures. In deep dermal burns that are allowed to reepithelialize over time, burn syndactyly reconstruction is expected as part of the reconstructive plan at some point in the future. In deep hand burns that are excised and grafted, injury extending into the web and dorsally onto the digits ensures web syndactyly during the healing and maturing period. The details of early skin grafting should include the application of deep darts from the dorsal to volar aspect of the web in an attempt to break the anticipated straight-line contraction of the graft interface with healthy soft tissue. Application of a dart elongates the graft surface. This technique may not be sufficient to counterbalance the distal pull of the contracting graft that advances the soft dorsal skin distally toward the digit, creating a prominent dorsal hood.

Figure 25-19 Burn scar syndactyly showing distal migration of the dorsal burn scar, distorting the web spaces.
Pressure garments with conformers inserted into the web create extrinsic pressure in an attempt to restrict the distally migrating contraction (Fig. 25-20). This pressure is maintained until the wound is mature. Any residual burn syndactyly can be reconstructed at that time.64 A neglected burn, allowed to heal mostly by secondary intention, may produce a tight web between digits with severe functional restriction.

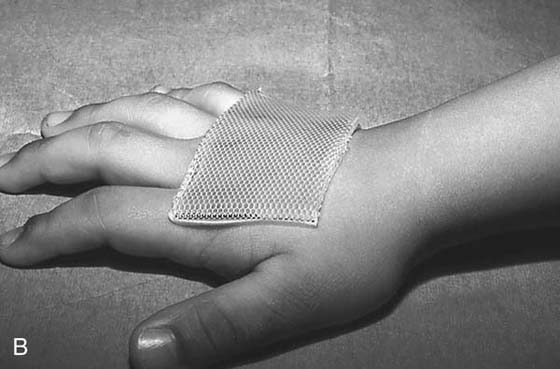
Figure 25-20 A, Compression gloves or gauntlets provide pressure on the dorsal hand burns. Web space conformers (beneath the glove) or silicone (B) sheeting also plays a role in softening contracting and hypertrophic scars.
Many techniques of reconstruction have been described, varying according to the location and extent of the skin deficit. A simple midline split with placement of the skin graft simply re-creates the original contraction pattern; recurrences are therefore common. Local flap rotations may be sufficient for the minimal syndactyly web. The basic principle of skin deficit must not be underestimated. The use of a dorsal flap physically separating portions of the skin graft usually re-creates the dorsal web slope and offers significant protection against recurrence (Fig. 25-21A). The composite tissues in the dorsal flap show minimal contraction. Placing the skin graft against the lateral and medial aspect of the digits, separated by the dorsal flap, protects the finger from future distal scar migration and recurrent contraction. Pressure garments and conformers are continued until complete scar maturation is complete (approximately 12 months).
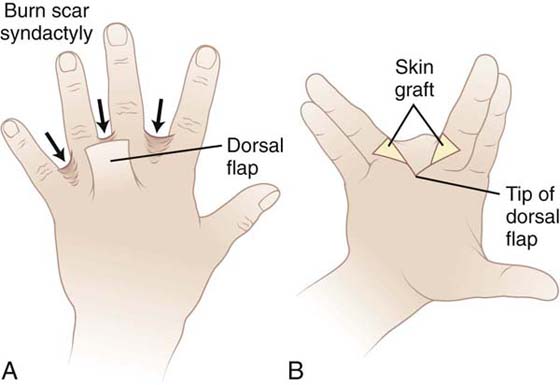
Figure 25-21 A, Burn scar syndactyly using reliable dorsal flap. B, Mandatory skin deficit requires full-thickness skin grafts.
Burn scar contracture over the middle and distal phalanges often results in extension contractures of the DIP joint and deformities about the nail and eponychial area.65 Once the contracture is present, active exercise and passive stretch are not completely successful in restoring full flexion. Pain is often a symptom of the sensitive DIP joint being pulled into hyperextension. Release of the contracture centered over the DIP area is preferred with either graft or flap coverage.66,67 The deformity of the eponychial fold from longitudinal contraction causes proximal migration of the nail fold (Fig. 25-22). Restoring the curvature of the nail cuticle from extrinsic contracture requires release across the DIP area, perpendicular to the line of contraction. Improvement of motion and a restored nail fold often result. Direct burn injury may, however, result in destruction of the nail matrix, which cannot be restored by simple resolution of the contracture. Techniques at postburn reconstruction of the entire nail and nail matrix have produced fair results.68,69

Figure 25-22 Release of proximal nail fold contracture at the interphalangeal joint level. Addition of full-thickness skin graft decreases tension and restores paronychial contour.
Kurtzman and Stern classified elbow flexion contractures into extra-articular and intra-articular contractures.36 The extra-articular contractures involve the skin, possibly tendon structures, and the underlying joint capsule (Fig. 25-23). Scar contraction at the level of the capsule is not fully appreciated until all of the overlying structures are first released. The complete antecubital release is approached by a horizontal midaxial-to-midaxial incision.70 With maximum elbow extension achieved and a stable soft tissue base present, a split-thickness skin graft can be applied. Extension positioning is maintained with an orthosis until full graft take is appreciated. Passive stretch and use of a dynamic orthosis can apply even greater force to improve extension after the graft is stable.71 If the elbow joint is exposed during the course of deep multilevel contracture release, local or regional composite flap reconstruction is required.72 Release to within 30 degrees of full extension permits most activities of daily living.36

Figure 25-23 A, Extra-articular contracture of the elbow precluding full extension. Fibrosis of soft tissue and joint capsule is appreciated. B, Axillary burn scar can create a contracture on the concave surface, resulting in functional restriction to motion. C, Longstanding contracture with hypertrophy.
Heterotopic ossification occurs in less than 2% of all burns of the upper extremity.36,73 X-ray examination before contracture release will document its presence. Resection after maturation of the bone formation is possible with difficulty. Indications for surgery include failure of improvement of elbow motion, inability to reach the mouth or perineum, and a total ROM of less than 50 degrees. Injury to articular cartilage or nerve compression about the elbow is not uncommon. Surgical correction usually at about 18 months postinjury has resulted in an improved ROM and absence of recurrence.74
Contractures of the anterior axillary or posterior axillary fold result in restricted abduction, flexion, and extension of the shoulder. Restriction and progressive loss of motion, refractory to therapy, indicate early release.75 In some cases the central portion of the axilla is spared from burn injury and contraction. The concave surfaces of the anterior and posterior folds allow progressive contraction because full abduction is often limited by pain. Release of the contracted axillary fold perpendicular to its axis and use of split-thickness skin grafting extending into the axilla and beyond the folds allow for early active abduction and stretch, once the graft is secure. Release often must be carried on to the lateral chest wall to include the pectoralis fascia if that portion participates in the contracture.
When the soft tissue of the axilla is also contracted, successful long-term release is difficult. Resurfacing the axilla after complete release requires an abduction orthosis until active stretch is possible. The large surface area of graft in this case is associated with recurring contracture on both the anterior and posterior surfaces. Secondary release once the skin graft is mature and abduction has been maximized is not uncommon. Lateral chest wall flaps or distant muscle flaps may reduce the rate of recurrent contracture significantly in the more severe cases.76
The use of tissue expansion in burn reconstruction can replace the deficient soft tissue with donor skin and subcutaneous tissue of similar color, thickness, and texture.47 Resection of unstable or unsightly scars is possible by advancement of the expanded, better-quality, sensate skin. An attempt is always made to hide the resultant scars in concealed sites when possible (Fig. 25-24). Longitudinal defects lend themselves better to expansion reconstruction than do wide horizontally oriented burn scars on the upper extremity. The broad lateral-based flaps have a more reliable base circulation. Excessive tension in the expanded flap after advancement necessitates a staged reconstruction of the burn scar. It is prudent not to resect the entire scar until the expanded flap is completely advanced and its tension assessed.77
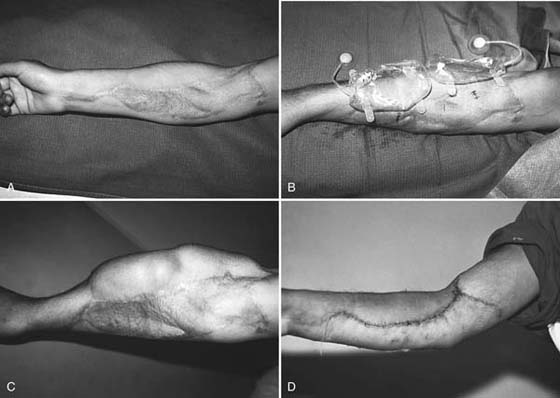
Figure 25-24 Tissue expansion for unsightly or unstable scarring (A). Multiple expander insertion (B) and progressive expansion (C). Subsequent resection of burn scar and advancement of healthy composite flaps (D).
Management of the burned upper extremity begins with attention to detail during the acute phase. Appreciation of burn depth, potential for contraction, and loss of function indicate an aggressive approach of burn excision and resurfacing. Therapy plays a significant role in preventing early burn deformity and in maximizing functional return following closure and resurfacing of the burn wound. Once this management has reached a maximum improvement, a decision concerning additional reconstructive procedures must be weighed against the potential benefit of functional gain. Burn scar is synonymous with skin deficit, and the concave and convex surface contours play a significant role in planning the reconstructive procedure. Attention to these details prevents secondary contracture where possible. Maximum functional return of the upper extremity with quality skin coverage is the goal for each thermally injured patient.
1. American Burn Association. Resources. 2009.
2. Hartford C, Kealey GP. Care of outpatient burns. In: Herndon DN, ed. Total Burn Care. Philadelphia: Saunders; 2007:67.
3. Pruitt B, Wolf SE, Mason AD. Epidemiological, demographic, and outcome characteristics of burn injury. In: Herndon DN, ed. Total Burn Care. 3rd ed Philadelphia: Saunders; 2007:14.
4. Tredget EE. Management of the acutely burned upper extremity. Hand Clin. 2000;16:187–203.
5. Barillo DJ, Harvey KD, Hobbs CL, et al. Prospective outcome analysis of a protocol for the surgical and rehabilitative management of burns to the hands. Plast Reconstr Surg. 1997;100:1442–1451.
6. Sheridan RL, Hurley J, Smith MA, et al. The acutely burned hand: management and outcome based on a ten-year experience with 1047 acute hand burns. J Trauma. 1995;38:406–411.
7. Boswick JJ. The Art and Science of Burn Care. Rockville, Maryland: Aspen; 1987.
8. Lee J, Herndon DN. The pediatric burned patient. In: Herndon DN, ed. Total Burn Care. 3rd ed Philadelphia: Saunders; 2007:487.
9. Rossiter ND, Chapman P, Haywood IA. How big is a hand? Burns. 1996;22:230–231.
10. Zawacki BE. The natural history of reversible burn injury. Surg Gynecol Obstet. 1974;139:867–872.
11. Salisbury RE, Wright P. Evaluation of early excision of dorsal burns of the hand. Plast Reconstr Surg. 1982;69:670–675.
12. Boswick JA Jr. Management of the burned hand. Orthop Clin North Am. 1970;1:311–319.
13. Boswick JA Jr. Rehabilitation after burn injury. Ann Acad Med Singapore. 1983;12:443–448.
14. Heggers JP, Ko F, Robson MC, et al. Evaluation of burn blister fluid. Plast Reconstr Surg. 1980;65:798–804.
15. Robson MC, Heggers JP. Evaluation of hand frostbite blister fluid as a clue to pathogenesis. J Hand Surg Am. 1981;6:43–47.
16. Wong L, Spence RJ. Escharotomy and fasciotomy of the burned upper extremity. Hand Clin. 2000;16:165–174. vii
17. Salisbury RE, Taylor JW, Levine NS. Evaluation of digital escharotomy in burned hands. Plast Reconstr Surg. 1976;58:440–443.
18. Salisbury RE, McKeel DW, Mason AD Jr. Ischemic necrosis of the intrinsic muscles of the hand after thermal injuries. J Bone Joint Surg Am. 1974;56:1701–1707.
19. Bardakjian VB, Kenney JG, Edgerton MT, et al. Pulse oximetry for vascular monitoring in burned upper extremities. J Burn Care Rehabil. 1988;9:63–65.
20. Krizek TJ, Flagg SV, Wolfort FG, et al. Delayed primary excision and skin grafting of the burned hand. Plast Reconstr Surg. 1973;51:524–529.
21. Beasley RW. Principles and techniques of resurfacing operations for hand surgery. Surg Clin North Am. 1967;47:389–413.
22. Janzekovic Z. A new concept in the early excision and immediate grafting of burns. J Trauma. 1970;10:1103–1108.
23. Burm JS, Chung CH, Oh SJ. Fist position for skin grafting on the dorsal hand: I. Analysis of length of the dorsal hand surgery in hand positions. Plast Reconstr Surg. 1999;104:1350–1355.
24. Buckley RC, Breazeale EE, Edmond JA, et al. A simple preparation of autologous fibrin glue for skin-graft fixation. Plast Reconstr Surg. 1999;103:202–206.
25. Kubo T, Hosokawa K, Haramoto U, et al. A simple technique for fibrin glue application in skin grafting. Plast Reconstr Surg. 2000;105:1906–1907.
26. McGill V, Kowal-Vern A, Lee M, et al. Use of fibrin sealant in thermal injury. J Burn Care Rehabil. 1997;18:429–434.
27. Adamkova M, Tymonova J, Zamecnikova I, et al. First experience with the use of vacuum assisted closure in the treatment of skin defects at the burn center. Acta Chir Plast. 2005;47:24–27.
28. Scherer LA, Shiver S, Chang M, et al. The vacuum assisted closure device: a method of securing skin grafts and improving graft survival. Arch Surg. 2002;137:930–933. discussion 933-934
29. Richard RL, Miller SF, Finley RK Jr, et al. Comparison of the effect of passive exercise v static wrapping on finger range of motion in the burned hand. J Burn Care Rehabil. 1987;8:576–578.
30. Pensler JM, Steward R, Lewis SR, et al. Reconstruction of the burned palm: full-thickness versus split-thickness skin grafts—long-term follow-up. Plast Reconstr Surg. 1988;81:46–49.
31. Simpson RL. Skin grafts for the burned palm in children. Plast Reconstr Surg. 1988;82:728.
32. Parks DH, Evans EB, Larson DL. Prevention and correction of deformity after severe burns. Surg Clin North Am. 1978;58:1279–1289.
33. Montandon D, D’Andiran G, Gabbiani G. The mechanism of wound contraction and epithelialization: clinical and experimental studies. Clin Plast Surg. 1977;4:325–346.
34. Peacock E, Van Winkle W. Surgery and Biology of Wound Repair. Philadelphia: WB Saunders; 1970.
35. Peacock EE Jr, Madden JW, Trier WC. Some studies on the treatment of burned hands. Ann Surg. 1970;171:903–914.
36. Kurtzman LC, Stern PJ. Upper extremity burn contractures. Hand Clin. 1990;6:261–279.
37. Kurtzman LC, Stern PJ, Yakuboff KP. Reconstruction of the burned thumb. Hand Clin. 1992;8:107–119.
38. Salisbury RE, Pruitt BA. Burns of the Upper Extremity. Philadelphia WB: Saunders; 1976.
39. Park S, Hata Y, Ito O, et al. Full-thickness skin graft from the ulnar aspect of the wrist to cover defects on the hand and digits. Ann Plast Surg. 1999;42:129–131.
40. Groenevelt F, Schoorl R. Cross-finger flaps from scarred skin in burned hands. Br J Plast Surg. 1985;38:187–189.
41. McLean NR, Clarke JA. Resurfacing of the severely burned hand with a radial forearm flap. Burns Incl Therm Inj. 1985;11:371–373.
42. Pribaz JJ, Pelham FR. Use of previously burned skin in local fasciocutaneous flaps for upper extremity reconstruction. Ann Plast Surg. 1994;33:272–280.
43. Schoofs M, Bienfait B, Calteux N, et al. The forearm fascia flap. Ann Chir Main. 1983;2:197–201.
44. Simpson R. Post burn pseudoboutonnière deformity. In: Kasdan M, Amadio PC, Bowers WH, eds. Technical Tips for Hand Surgery. St. Louis: Mosby; 1994.
45. Simpson RL, Flaherty ME. The burned small finger. Clin Plast Surg. 1992;19:673–682.
46. Graham TJ, Stern PJ, True MS. Classification and treatment of postburn metacarpophalangeal joint extension contractures in children. J Hand Surg Am. 1990;15:450–456.
47. Simpson RL. The use of tissue expansion in reconstructive upper extremity surgery. Tubiana R, ed. The Hand.Vol. 5. Philadelphia: WB Saunders; 1999.
48. Grishkevich VM. Surgical treatment of postburn boutonnière deformity. Plast Reconstr Surg. 1996;97:126–132.
49. Groenevelt F, Schoorl R. Reconstructive surgery of the post-burn boutonnière deformity. J Hand Surg Br. 1986;11:23–30.
50. Larson DL, Wofford BH, Evans EB, et al. Repair of the boutonnière deformity of the burned hand. J Trauma. 1970;10:481–487.
51. Kessler I. Etiology and management of adduction contracture of the thumb. Bull Hosp Joint Dis Orthop Inst. 1984;44:260–275.
52. Mehrotra ON. Restoration of grasp and pinch in a burnt hand by pollicization of an island flap taken from the same finger. Aust N Z J Surg. 1977;47:806–810.
53. Meyer RD, Gould JS, Nicholson B. Revision of the first web space: techniques and results. South Med J. 1981;74:1204–1208.
54. Stern PJ, Neale HW, Carter W, et al. Classification and management of burned thumb contractures in children. Burns Incl Therm Inj. 1985;11:168–174.
55. Bhattacharya S, Bhatnagar SK, Pandey SD, et al. Management of burn contractures of the first web space of the hand. Burns. 1992;18:54–57.
56. Dmitriyev GI, Petrov SV. Surgery for adduction contracture of the thumb after burn. Acta Chir Plast. 1989;31:236–242.
57. Hallock GG. The radial forearm flap in burn reconstruction. J Burn Care Rehabil. 1986;7:318–322.
58. Housinger TA, Ivers B, Warden GD. Release of the first web space with the “goalpost” procedure in pediatric burns. J Burn Care Rehabil. 1993;14:353–355.
59. Jin YT, Guan WX, Shi TM, et al. Reversed island forearm fascial flap in hand surgery. Ann Plast Surg. 1985;15:340–347.
60. Scheker LR, Lister GD, Wolff TW. The lateral arm free flap in releasing severe contracture of the first web space. J Hand Surg Br. 1988;13:146–150.
61. Sharpe C. Tissue cover for the thumb web: a review. Arch Surg. 1972;104:21–25.
62. Araico J, Valdes JL, Ortiz JM. An internal wire splint for adduction contracture of the thumb. Plast Reconstr Surg. 1971;48:339–342.
63. Harnar T, Engrav L, Heimbach D, et al. Experience with skeletal immobilization after excision and grafting of severely burned hands. J Trauma. 1985;25:299–302.
64. Gorham K, Hammond J. An improved web-space pressure technique to prevent burn syndactyly. J Burn Care Rehabil. 1991;12:157–159.
65. Alsbjorn BF, Basse P. Surgical relocation of retracted eponychion. Acta Chir Plast. 1991;33:110–113.
66. Achauer BM, Welk RA. One-stage reconstruction of the postburn nailfold contracture. Plast Reconstr Surg. 1990;85:937–940. discussion 941
67. Hayes CW. One-stage nail fold reconstruction. Hand. 1974;6:74–75.
68. Ngim RC, Soin K. Postburn nailfold retraction: a reconstructive technique. J Hand Surg Br. 1986;11:385–387.
69. Spauwen PH, Brown IF, Sauer EW, et al. Management of fingernail deformities after thermal injury. Scand J Plast Reconstr Surg Hand Surg. 1987;21:253–255.
70. Breen TF, Gelberman RH, Ackerman GN. Elbow flexion contractures: treatment by anterior release and continuous passive motion. J Hand Surg Br. 1988;13:286–287.
71. Weiss AP, Sachar K. Soft tissue contractures about the elbow. Hand Clin. 1994;10:439–451.
72. Salinas Velasco VM, Garcia-Morato V, Fregenal Garcia FJ. Burn of the elbow: the role of the radial forearm island flap. Burns. 1992;18:71–73.
73. Elledge ES, Smith AA, McManus WF, et al. Heterotopic bone formation in burned patients. J Trauma. 1988;28:684–687.
74. Gaur A, Sinclair M, Caruso E, et al. Heterotopic ossification around the elbow following burns in children: results after excision. J Bone Joint Surg Am. 2003;85:1538–1543.
75. Greenhalgh DG, Gaboury T, Warden GD. The early release of axillary contractures in pediatric patients with burns. J Burn Care Rehabil. 1993;14:39–42.
76. Achauer BM, Spenler CW, Gold ME. Reconstruction of axillary burn contractures with the latissimus dorsi fasciocutaneous flap. J Trauma. 1988;28:211–213.
77. Borenstein A, Yaffe B, Seidman DS, et al. Tissue expansion in reconstruction of postburn contracture of the first web space of the hand. Ann Plast Surg. 1991;26:463–465.