
Figure 26-1 An example of excessive scar and contractures limiting hand motion. Note swan-neck deformity on ring finger and proximal interphalangeal joint flexion contractures (perhaps boutonnière deformities) on other digits.
HYPERTROPHIC SCARS AND SCAR CONTRACTION
THERAPEUTIC MANAGEMENT OF COMMON DEFORMITIES OF THE BURNED HAND
▪ When treating the burned hand, therapists spend a great deal of time in limiting, reducing, or preventing the negative effects of hypertrophic scarring and scar contraction on hand structures and function.
▪ The positioning program for the burned hand is designed to minimize edema, prevent tissue destruction, and preserve soft tissues in an elongated state to facilitate functional recovery.
▪ Hypertrophic scars appear red, raised, and rigid to touch. Gentle pressure on the scar during palpation causes transient blanching.
▪ Keloid scars are distinguished from hypertrophic scars in that they have an irregular shape (often bulbous or pendulous), extend beyond the boundary of the wound, and encroach on the surrounding skin.
The hand accounts for only 3% of the total body surface area (TBSA).1-3 Despite this small percentage, an injury to the hand can cause lifelong deformity and disability. Musculoskeletal impairment and loss of the normal appearance can influence the patient’s self-image, occupation, and lifestyle. Skilled therapeutic intervention is imperative in order to preserve motion and joint integrity, prevent scarring, restore cosmesis, and ultimately optimize function of the hand.
Hand burns are the leading cause of impairment following a burn injury.4 They are typically seen as an isolated injury; however, the hands are rarely unaffected in larger burns.4 The American Burn Association classifies a hand burn as a major injury requiring treatment at a burn center.5 Although a burn to the hand is typically not life-threatening, it can, however, be devastating. Loss of hand use results in an impairment rating of 95% for the involved extremity and a 57% loss of the whole person’s function.6 Early wound closure and rehabilitation can facilitate restoration of hand function. This chapter describes the role of the therapist during each phase of healing, emphasizing scar assessment, prevention, and management.
Loss of hand function following burns may be attributed to a variety of factors including loss of sensation due to damage to sensory nerves and nerve endings as well as the loss of motion due to contractures. Contractures may be functionally defined as shortening of soft tissues, including skin, muscle, tendon, ligament, and fascia, which restricts the ability to perform full range of motion (ROM) of a joint. In the burned hand, contracture formation may be a primary or secondary outcome of scar formation and contraction. Primary contractures following a burn are mainly due to the formation of hypertrophic scars and excessive contraction of scars (Fig. 26-1).

Figure 26-1 An example of excessive scar and contractures limiting hand motion. Note swan-neck deformity on ring finger and proximal interphalangeal joint flexion contractures (perhaps boutonnière deformities) on other digits.
During typical wound healing, spatial reduction of the wounded area commences once a matrix of collagen and proteoglycans known as cicatrix is formed. Within 1 week after injury, the cicatrix covers the wound and actively contracts to form scar. Scar conversion is an active process, but may extend further into scar contraction, in which the scar shortens, gathers, and pulls the surrounding unscarred tissue. Scar contractures are dense, adherent to underlying tissues, relatively immobile, and painful with pinpoint pressure. Many physicians and therapists do not distinguish between scar contraction and scar contracture. As a point of clarification, scar contraction is a process in which scar contracture is the ultimate outcome.
Scar contractures tend to occur more in areas where skin is loose or more pliable. Typically, a scar continues to contract until it meets an equal or opposing force. Skin immediately surrounding scar contractures tends to be less pliable as it gets pulled taut by the scar and therefore could result in movement limitations in joints and soft tissues. Over time, the taut surrounding skin loses its extensibility even if it is uninjured.7 A simple “pinch” test could give the therapist an idea of the extent of the scar contracture’s centripetal pull. The pinch test assesses the degree of tautness and extensibility of the surrounding skin and compares it with the contralateral side or comparable skin on an unburned body part (Fig. 26-2). Decrease in skin pliability reduces joint movement, accessory joint play, and, in certain cases, tendon glide. For example, scar contracture on the dorsum of the hand tends to pull the metacarpophalangeal (MCP) joint in hyperextension. Attempts to actively complete a fist position may be difficult since the scar adds resistance and drag against typical MCP joint arthrokinematics. In addition, adhesion of the scar to the extensor digitorum communis may limit distal excursion of its tendon and cause the tendon to be passively insufficient before optimal MCP joint flexion is reached.
Postburn scars become hypertrophic due to excessive proliferation of dermal tissue during the healing process.8 Scar formation is marked by deposition of bundles of disorganized collagen and production of fibrous tissue matrices, creating a meshwork on the site where skin and adjacent tissues were disrupted. Over time, collagen cross-linking increases and subsequent reorganization of fibers occurs in response to mechanical stress on the skin and underlying soft tissues. The collagen fibers that were once bundled and disorganized like hay in a haystack become flatter and more parallel to follow the same orientation as the skin surface. This process of collagen reorganization is evident within 3 to 5 weeks after injury.9 However, in hypertrophic scars, this process of collagen reorganization is significantly protracted and is further complicated by persistent fibroplasia and local chronic inflammatory reaction.9
Through visual inspection, one may find that hypertrophic scars appear red, raised, and rigid to touch. Gentle pressure on the scar during palpation causes transient blanching. As the scar matures, it becomes flatter, paler, and more pliable. With consistent scar management, the process of scar maturation is expected to last at least 6 months following the burn. Certain populations, especially those with higher melanin pigmentation (skin of color), may experience a greater challenge with scar maturation, including keloid scar formation. Keloid scars are distinguished from hypertrophic scars in that they have an irregular shape, are often bulbous or pendulous, extend beyond the boundary of the wound, and encroach on the surrounding skin. Beyond familial tendencies, keloids are proposed to be different histologically, biochemically, and immunologically; however, these differences are not necessarily accepted universally.10,11 Clinical observations and anecdotal evidence suggest that keloids often do not appear to respond as readily as hypertrophic scars to the traditional treatment of pressure application.
The extent of hypertrophic scarring and scar contraction in burns is related to various factors, including the size and depth of the injury.12 In a classic study by Deitch and colleagues,13 which investigated the factors predictive of the development of scar hypertrophy, the most predominant factor appeared to be the time needed to obtain complete closure of the wound. If the burns healed between 14 and 21 days, 33% of the sites became hypertrophic, and if the healing took longer than 21 days, 78% of the sites became hypertrophic. In a related study conducted by Smith and coworkers,14 increases in both the percentage of third-degree burn and in the number of weeks after injury were associated with an increase in serum anticollagen antibody level. Smith proposed that such an increase in the anticollagen antibody may have lead to an increase in collagen accumulation at the burn site.14
Another important predictor in the formation of hypertrophic scars is the anatomic location of the burn. Richards and associates15 postulated that skin tension may be a factor in scar formation and contraction due to the directional variance in skin movement between the volar and dorsal skin surfaces. Myer and McGrouther16 found that skin that typically receives multidirectional tension during various limb movements is more likely to develop hypertrophic scar due to overstimulation of collagen-producing fibroblasts. The mechanism proposed by Myer and McGrouther16 may partly explain why hypertrophic scars develop more often in the hand and larger areas such as the axilla due to the greater degrees of freedom and multidirectional skin tension afforded during joint movements of the hand and shoulder.
Another predictor of scar-induced contracture is the timing and the type of surgical intervention. Sheriden and colleagues17,18 demonstrated that early eschar excision and sheet grafting in 90% of patients with deep thermal burns had function consistent with independent performance of activities of daily living. A full-thickness skin graft (FTSG) can almost completely inhibit wound contraction, whereas the amount of wound contraction seen with a split-thickness skin graft (STSG) is inversely proportional to the thickness of the graft.19
In rehabilitating the burned hand, therapists must spend a great deal of time to limit, reduce, or prevent the negative effects of hypertrophic scarring and scar contraction on hand structures and function. The processes of scar hypertrophy and contraction essentially begin almost as soon as the wound begins healing and are most “active” for the first 4 to 6 months after the injury. However, as time goes by along the continuum of burn recovery, therapists may also need to focus on addressing secondary contractures. Secondary contractures may arise due to substantial reduction in mobility and tension in the soft tissues, which over time decrease their elasticity. Contractures are consistently considered as anticipated sequelae of any traumatic or postsurgical injury of the upper extremity due to immobilization. In the burned hand, immobilization may be a necessity earlier in the recovery process for safety reasons such as in postgrafting procedures. However, in the latter stages of recovery, secondary contractures may evolve due to primary contractures caused by hypertrophic scarring and scar contraction.
Once scar maturation activity abates, the scar is said to be mature. The period of scar maturation for children is 12 to 24 months; for adults this period is 6 to 24 months. While the scar is active, especially early on, hypertrophy and contraction can be minimized or corrected by therapeutic interventions such as ROM exercises, pressure application, and orthotic intervention. Scar maturation can also bring about development of flexible deformity or worse, the formation of fixed deformities. Once the scar maturation is complete, scar management may no longer respond to nonsurgical interventions.
Another motivating factor to the therapist’s management of hypetrophic scars is cosmetic appearance of the hand. Next to facial and genital disfigurement, the cosmetic appearance of the burned and scarred hand is deemed to be most concerning to a patient’s body image and self-esteem.20
The therapist’s role in management of the burned hand is discussed in four phases of burn recovery: (1) the emergent phase, (2) the acute phase, (3) the skin-grafting phase, and (4) the rehabilitation phase. Depending on the particular burn injury and treatment approach, a hand that has sustained a burn can be in more than one stage of recovery at any given time or, because of early grafting, may even “skip” the acute phase.
The emergent phase of burn recovery is generally considered to be the first 24 to 72 hours after injury. In a survey on therapeutic interventions conducted by Whitehead and Serghiou,21 91% of those surveyed reported that initial evaluations are performed within the first 24 to 48 hours after acute admission. At this time, the therapist’s goals are to examine the patient and develop treatment goals and a plan of care. This should include minimizing edema, obtaining optimal positioning of the hand, initiating motion, and maximizing function. Early and timely intervention by the therapist is necessary to help minimize the deforming effects of both the injury and the natural sequelae of healing, as well as to maximize functional recovery.
The medical record is reviewed and the following information should be collected: age, TBSA, cause of burn, procedures (intubation, escharotomy, fasciotomy), social history, and previous medical history.22,23 Additional components of the initial evaluation include: burn wound assessment (e.g., depth, color, texture, moisture, location, joints involved), edema (description of and location), pain (via a visual analog scale), cognition, ROM (active and passive), sensation (particularly light touch), muscle performance, gross and fine motor coordination (e.g., hand dominance, opposition, diadochokinesia, i.e., rapid execution of opposite movements such as quick repetitions of pronation and supination), and activities of daily living (ADLs) or play.22,23 In order to prevent infection, ROM measurements are performed over the patient’s dressings. Special tests are often not performed at this stage due to dressings covering the hand and upper extremity.
In response to the injury and also to fluid resuscitation, the extremity becomes edematous (Fig. 26-3). Fluid translocates to the extravascular space of both burned and unburned tissue in patients who have sustained greater than 25% TBSA burn injuries. For many years, this fluid shift was thought to be caused by an increase in capillary permeability. However, research has shown that although increased capillary permeability is contributory to edema formation, burn-induced edema in the emergent phase is caused primarily by interstitial components generating a strong negative tissue pressure.24,25 Deep partial-thickness and full-thickness burns produce more prolonged and severe edema than do superficial partial-thickness burns,26 but the typical full-thickness injury gives less edema and exudation than does a partial-thickness injury.27,28 Edema develops from 8 to 12 hours after the burn injury, peaks up to 36 hours after the injury, begins to resolve after 1 or 2 days, and usually is completely gone by 7 to 10 days after the injury.24

Figure 26-3 A child with deep partial-thickness and full-thickness hand burns on day of admission to hospital. Note how the edema is contributing to flattening of the palmar arches, metacarpophalangeal joint extension, and interphalangeal joint flexion.
Edema may cause several problems, such as ischemia and fibrosis, particularly in conjunction with inelastic burn tissue. Compromised blood flow to the intrinsics can lead to intrinsic tightness. Edema places the hand in a deforming position restricting motion and interfering with performance of ADLs and other functional activities. The protein-rich components of unresolved edema 42 to 72 hours after the burn injury may become organized around joint capsules, ligaments, and other soft tissue structures and form a scar tissue matrix, leading to contracture and loss of motion.29-31 Chronic edema may result from damage to or destruction of dorsal veins or lymphatic vessels.
As previously described in Chapter 25, burn eschar (destroyed, nonviable tissue) is inelastic. Therefore, when the injury is circumferential, such inelasticity in conjunction with the development of hard, immobile edema produces a tourniquet effect. Intervention is necessary to prevent fibrosis and ischemic necrosis of the intrinsic muscles of the hand,32 nerve damage,33 and gangrene of the digits.34 If circulation is compromised, a surgeon must perform an escharotomy. A fasciotomy may be necessary if the circulation is not restored by an escharotomy (Fig. 26-4).
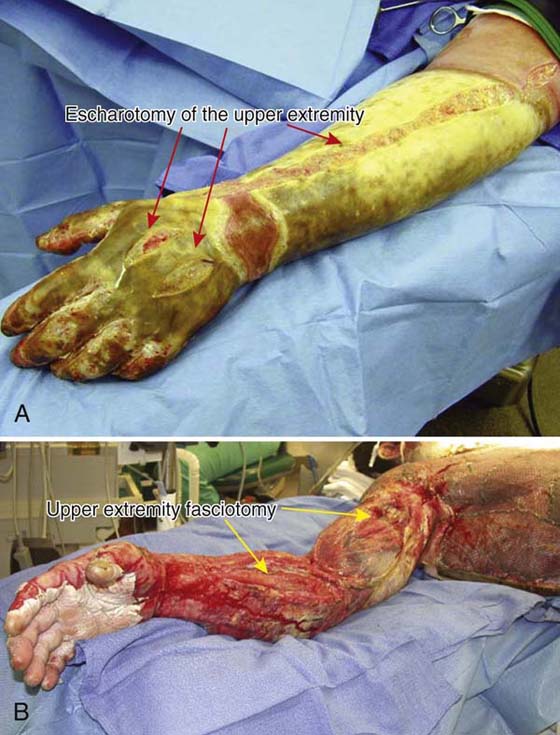
Figure 26-4 A, Escharotomies of the forearm and dorsum of the hand. B, Fasciotomies of the forearm and upper arm.
ROM exercises (active and passive) are permitted in extremities that have undergone an escharotomy. In the case of a fasciotomy it is especially important that the wound is viewed prior to performing ROM to ensure the viability and gliding of the tendons. In some cases, ROM may need to be performed when the dressings are down to ensure gliding of the tendons in the case of exposure. Typically, patients are cleared for full ROM; however, in the case of a fasciotomy ROM may be limited due to the nature of the exposed structures.
Proper positioning is one of the keys to the successful rehabilitation of a burn patient.29 A burn patient’s positioning program is designed to minimize edema, prevent tissue destruction, and maintain soft tissues in an elongated state to facilitate functional recovery.29 Ninety-five percent of surveyed burn centers in 2006 reported that positioning begins within 24 hours of admission as opposed to 54% in 1994.21 Ideally, the upper extremity is positioned at or above heart level with the elbow in extension, forearm is either supinated or in neutral, wrist in neutral, and hand in an intrinsic plus position.29,31,35-37 In the case of a palmar burn, the digits are positioned in, with interphalangeal (IP) joints in extension, and the first webspace in a slight stretch.28 With circumferential hand burns, hand positioning may alternate every 12 hours to account for both a palmar and dorsal burn. A foam wedge is an effective and inexpensive positioning device (Fig. 26-5). It is easy to apply and keep in place, is well accepted by patients and staff, and was found not to cause any adverse reactions such as pain or sensory problems.38 Other upper extremity elevation devices include commercial arm troughs, pillows, blankets, bedside table, and surgical netting (Fig. 26-6).

Figure 26-5 Foam wedge used for positioning and edema management that is widely accepted by patients and hospital staff.

Figure 26-6 Example of an abduction arm trough from orthotic material for positioning of the upper extremity.
Complications can arise from incorrect positioning of the upper extremity. Elevation beyond heart level may result in decreased arterial supply to the hand.38 Excessive weight-bearing stress to the olecranon of the elbow, especially with a flexed elbow, should be avoided since this may lead to pressure on the ulnar nerve. Helm39 has cautioned therapists to regard neurologic considerations when positioning the burn patient. Helm cited Wadsworth and Williams,40 who demonstrated how the prolonged position of the elbow in acute flexion or forearm pronation may cause compression on the ulnar nerve. This may result in motor weakness of the intrinsic muscles and impaired sensation in the ulnar-nerve distribution in the hand. In addition to proper elevation of the hand to help control edema, exercise and orthotic intervention may also be beneficial in helping control edema and minimizing the adverse effects of edema.
During the emergent phase, a static orthosis is often used to counteract the deforming position of edema, support the hand, and maintain joint alignment.41-46 Edema, pain, and tight eschar immediately after a burn are the leading reasons why a person may demonstrate impaired ROM.41-45 The hand is commonly positioned in an orthosis following a burn.47 Whitehead and Serghiou21 found that 61% of surveyed burn centers in 2006 initiated orthotic intervention within 24 hours of admission as opposed to 54% of responding centers in 1994. Burn depth, ROM limitations, as well as level of arousal (intubated vs. nonintubated) should be taken into account when considering orthotic intervention. The duration of wear time has not been adequately studied and is facility-dependent. Malick47 suggests removing orthoses every 2 hours for cleaning to prevent patient contamination. If the patient is alert, many facilities recommend the orthosis only be worn when asleep.48 In the case of the intubated patient, orthoses are often worn at all times except during burn care and therapy.
To counteract the position of deforming forces and to protect the structures of the hand, an orthosis that positions the hand in wrist slight or neutral extension, MCP joint flexion, IP joint extension, and the thumb away from the palm is recommended. This position is commonly referred to as the “protected,” or “safe,” position of the hand. Placing the wrist in slight extension facilitates MCP joint flexion by action of the extrinsic forearm muscles—the tenodesis effect. Boswick49 described the basic burned hand orthosis as one that positions the wrist in 30 degrees or more of extension, contributing to MCP joint flexion. When the MCP joints are flexed, the flexor tendons are on slack, which, along with the pull of the intrinsic hand musculature, facilitates the positioning of the IP joints in extension. The position of the IP joints in extension prevents adaptive shortening of the volar plate and collateral ligaments and the development of IP joint flexion contractures.
However, as Richard and colleagues50 discovered in a review of the literature, a set of universal, standard dimensions for what exactly constitutes the “basic” burn orthosis, and even what its name is, does not exist. They found more than 40 different descriptions of how to position dorsal hand burns as well as a variety of names for such an orthosis. Although most practitioners agreed that the wrist should be in slight extension and all agreed that the MCP joints should be flexed, a wide range of specific joint angles have been cited. Surprisingly, almost one fourth listed that the proximal interphalangeal (PIP) joints should be flexed, and an assortment of combinations of positions for the thumb were reported.
We recommend that the wrist be positioned in 15 to 20 degrees of extension, the MCP joints flexed 60 to 70 degrees, the IP joints extended fully, and the thumb positioned midway between radial and palmar abduction, with the thumb MCP joint flexed 10 degrees and the IP joint fully extended. In addition to maintaining thumb opposition and abduction, the orthosis must maintain the thenar webspace and properly support the MCP joint of the thumb, which the 10 degrees of thumb MCP joint flexion aids. Failure to properly support the thumb MCP joint could result in a swan-neck deformity.
The burned hand orthosis described previously is not applied to hands when only the palm is burned or to hands that have sustained other specific burns such as those of just the thenar webspace. When applying an orthosis to a palmar hand burn, the wrist should be positioned in neutral or slight extension, the fingers in full extension and abduction, and the thumb in radial abduction and extension. This is typically called a “pan” orthosis (Fig. 26-7). As healing progresses, the orthosis should be molded to maintain the palmar arches. Burns involving only the thenar webspace are positioned in radial abduction, but care must be taken to support the thumb MCP joint. This is typically called a “C-bar” orthosis.
Prefabricated hand orthoses can be applied initially if a therapist is not immediately available to construct custom orthoses. However, such orthoses, when commercially made, may need to have their forearm troughs widened before initial application so that they can accommodate both edema and bulky bandages.43
In the case of an alert adult patient, hand orthoses are usually applied with strapping for easy application. Pediatric hand orthoses and those of an intubated patient are secured with an elastic gauze bandage such as Dermacea. The elastic gauze prevents poor positioning of the orthosis in patients who wear them for longer durations and is more challenging for a child to remove. If orthotic intervention is not chosen at this time, a small roll of gauze can be placed or wrapped in an intubated patient’s hand to help maintain the thenar webspace and the palmar arch. All hand burns are not always routinely positioned in orthoses. Whether to use an orthosis during the emergent phase is determined by the experienced therapist (in accordance with physician orders) based on the depth and extent of the wound and on the ability of the patient to cooperate with exercise, positioning, and ADLs. The therapist should evaluate the patient daily to determine the need for orthotic intervention and to ensure the correct fit.
Although orthotic intervention is commonplace in burn rehabilitation, decisions regarding initiation of an orthosis, duration of wear, and design vary significantly among burn centers. Further research is necessary to determine best practice within each phase of recovery.51
Initiation of ROM, specifically active range of motion (AROM), is vital to preserving function and preventing deformity.51-54 The purpose of active motion during the emergent phase is to preserve ROM, tendon gliding, and muscle function. Active motion, in conjunction with elevation, is also effective in the early management of edema. Simple wiggling of the digits is not as effective as focused efforts on full active motion. The muscle contraction must be forceful enough to serve as a pumping mechanism to help venous blood and lymph return.55 Whitehead and Serghiou21 found that 96% of surveyed burn centers initiated AROM within 24 hours of admission. If tendon involvement is suggested, precautions should be taken. See the following section on Acute Phase for considerations on the management of exposed and ruptured tendons.
The acute phase generally extends from the emergent phase until wound closure. Wound closure is defined here as either the surgical closure of the burn wound, which in the hand usually is accomplished by the application of skin graft(s), or as closure of the burn wound by secondary-intention healing so that any remaining partial-thickness wounds are approximately less than the size of a postage stamp. The reader should note that according to the description and delineation of phases of healing in this chapter, an acute phase technically may not exist for some hand burns. As a result of advances in surgical techniques, some hand burns may be grafted 1 to 2 days after the burn injury. This is particularly true of small TBSA burns of known depth.
The goals of the therapist during the acute phase are to increase or preserve ROM, preserve tendon gliding, maintain muscle activity, inhibit contraction, and promote function. Clark56 reported that collagen synthesis may begin as early as 3 days after injury and remain rapid for up to 6 months. After 6 months, this process slows and continues for 1 to 2 years after the injury. Therefore early intervention is imperative for orientation of the collagen fibers that are being deposited so that deformity caused by scar formation is minimized or prevented.
The therapist should continue with the AROM exercises previously described. During the acute phase, the therapist should be aware that full AROM can be compromised by fibrous (not pitting) edema, inelastic eschar (Fig. 26-8), or tension from newly deposited collagen. The scar band from newly deposited collagen can appear in the open wound as well as in the closed wound, particularly when there is a protracted acute phase. To help judge whether more active motion should be expected from the patient when he or she appears to be at maximum range, gently press the band (e.g., the thenar web in radial abduction) to test the tension. If it is as taut as a stretched rubber band and blanching occurs, the patient is indeed at maximum range. If not, the patient should be encouraged to achieve more motion. This same method can be used during the rehabilitation phase with a scar in a closed wound. ROM, especially in children, may be more accurately assessed while the patient is under anesthesia before surgical procedures or during a dressing change.

Figure 26-8 Contact palmar hand burn. Inelastic eschar may compromise active range of motion of the newly burned hand.
If the patient has limited AROM, passive or active assistive stretching can be performed to increase ROM. Other exercises that are typically incorporated into a hand treatment or home exercise program are tendon glides, opposition, blocking exercises at the digits, and contract–relax exercises. When exercising the burned hand, the therapist should support the joint proximal to the joint being stretched. Pain should be considered to determine the intensity of the exercises.52 To avoid unnecessary pain, support should be provided where eschar is present rather than on granulation tissue. Gentle passive range of motion (PROM) may be the only type of ROM that the therapist is able to administer to young children because they are often not able to cooperate with an AROM exercise program.
Care should be taken while performing PROM. Scar tissue ultimately responds well when passive force is applied in a steady, controlled manner, over a period of time.52 Overly aggressive passive ranging constantly reinjures the fragile new tissue, resulting in an increase of collagen deposition and consequently more scarring.57
Active motion, with emphasis on isotonic contraction, should be encouraged. The patient should be carefully instructed about his or her exercise program and then observed to be sure that the exercises are performed correctly. At this time, spontaneous use of the hand and upper extremity should be strongly encouraged. Functional activities should be incorporated into the treatment plan.
The use of virtual reality (VR) and video gaming has become an increasingly popular treatment intervention. Virtual reality and video gaming are often utilized during painful or anxiety-provoking interventions such as dressing changes and therapy. These interventions offer an escape and often distract patients, allowing them to tolerate more aggressive debridement and ROM and encouraging them to actively move more freely within the game.58
Upon initial wound assessment and as the eschar is debrided, the therapist should look carefully for tendon exposure (Fig. 26-9). Tendon exposure can also appear in the recently healed wound. If tendon involvement is suggested because of the depth of the injury, the therapist should proceed with the same precautions that would be used if tendon involvement were confirmed. Two of the most common sites for tendon exposure are the dorsum of the hand, where the skin is thin, and the extensor tendon over the PIP joint. In a review of 50 patients with hand burns, Hunt and Sato59 found that the more distal the tendon exposure, the less the functional deficit noted, and the worst functional outcomes were from damage to the extensor tendon over the PIP joint. Loss of the central slip of the extensor tendon to the PIP joint can result in a boutonnière deformity (see Fig 26-1).
After tendon exposure has been noted, close monitoring and care by the surgeon, nurse, and therapist is critical to preserve as much tendon integrity and function as possible. Saffle and Schnebly60 stated that exposed tendons rapidly become desiccated and dissolve as a result of the action of surrounding leukocytes and bacteria. To prevent desiccation, the exposed tendon must be kept covered with a protective dressing that will keep it from drying, which will also assist with healing.
Exercise and Orthotic Intervention of the Exposed Tendon: Before Grafting. Choice of the specific orthotic intervention and exercise program depends on the extent and location of the exposure, the apparent integrity of the tendon and surrounding tissue and structures, and the willingness or ability of the patient to comply with the plan of care. These conditions and factors must be assessed daily. Exercises are performed under the supervision of a therapist who has received physician orders.
Some therapists and physicians opt for more aggressive ROM regimens if the tendon appears healthy and the exposure is small. For example, when the extensor digitorum communis (EDC) is exposed over the MCP joint of the index finger, the wrist is positioned in 15 to 30 degrees of extension, the involved MCP joint in 30 to 40 degrees of flexion (to prevent tightening of the collateral ligaments), and the IP joints in full extension.61 When ROM exercises are being performed at the IP joint, the MCP joint and the wrist should be positioned in extension to put the tendon at maximum slack. Conservatively, gentle passive extension of the PIP and distal interphalangeal (DIP) joints and active flexion of the PIP and DIP joints can also be performed. When the central slip of the extensor tendon over the PIP joint is exposed, the PIP joint must be maintained in extension.62 However, gentle, isolated ROM exercises in the available ROM at the DIP joint can be performed. The previously stated advisory should be kept in mind. Exercises are performed to help preserve joint ROM and to ensure tendon gliding and may help maintain oblique and transverse retinacular ligament length.63
A finger orthosis, typically called a finger gutter, has been found to be effective for immobilization of exposed tendons of the PIP joint while still allowing MCP joint flexion.64 Gutter orthoses may be applied before, and worn under, traditional hand burn orthoses, although some adjustment may be necessary to accommodate them. Use of 1/6-inch thermoplastic material in the construction of finger orthoses limits the amount of space they occupy; limiting each orthosis to cover just the volar aspect of the digit reduces bulk and minimizes the finger abduction that can result from using multiple finger-based orthoses. Finger abduction should be avoided because it may cause malalignment and may limit MCP flexion due to tension on collateral ligaments. In addition, the finger orthosis should cover only the proximal and middle phalanges so that active flexion and extension of the MCP and DIP joints can be accomplished. Gutter orthoses may be secured with Coban.
Pullium65 advised the use of a full volar orthosis if damage appears to extend beyond the extensor hood. A more restrictive exercise program is also indicated in such cases. When an exposed tendon is present, ADL tasks should be monitored to prevent accidental rupture. In the case of a dry or ruptured tendon, ROM is avoided at the joint to prevent further damage.
Generally, a hand that is healing without complications does not have to be positioned in an orthosis unless there is a limitation in active motion of the MCP or IP joints of 20 degrees or greater in extension, or MCP or IP joint flexion is less than 70 degrees. If active MCP or IP joint extension is limited by 20 degrees or greater, the therapist can initiate serial extension orthotic fabrication. If MCP joint flexion is less than 70 degrees, the therapist should position the hand as close to the previously described position of 15 to 20 degrees of wrist extension, 60 to 70 degrees of MCP joint flexion, full extension of the IP joints, and the thumb positioned midway between radial and palmar abduction with the thumb MCP joint flexed 10 degrees and the IP joint fully extended.29,41-44,50,66,67 The orthosis can be adjusted as MCP joint flexion increases. When a limitation in motion does exist, the therapist should evaluate and make any necessary changes to other components of the therapy program, such as exercise and participation in ADLs, which might help increase ROM.
In addition to evaluating the wound, the therapist must evaluate the fit of the orthosis and check to see if it is being applied correctly. If an orthosis is applied incorrectly and not secured adequately, it can slip forward, contributing to the deforming forces of thumb adduction, MCP joint hyperextension, IP joint flexion, and breakdown from pressure at the carpometacarpal joint. Changes in bulk of the bandages also affect the fit of the orthosis.
As the patient’s ROM and level of arousal improves, the use of the orthosis during the day can be decreased. If the patient is unwilling or unable to cooperate, the orthosis should be worn continuously and removed only for dressing changes, self-care activities, and therapy. The orthosis should be worn during all hours of sleep. It is not unusual for a patient to lose significant range because the orthosis was not applied during the night.
The therapist should be careful not to overly immobilize the patient. This can result in joint stiffness, contractures, and soft tissue adhesions. Children can tolerate immobilization longer than adults because of the elasticity of their joints and soft tissue, but they still need to be monitored.53,54 In addition to immobilization caused by orthotic intervention, the therapist should note whether the patient is causing the increased joint stiffness by self-immobilization or muscle guarding, which typically results from pain.
Once it is determined that a patient requires skin grafting (see Chapter 25) and surgery is scheduled, it is crucial to obtain full ROM prior to grafting because the patient will need to be immobilized for approximately 2 to 5 days after surgery (Fig. 26-10). However, in some cases of early excision and grafting, some edema is still present or reports of pain may limit full ROM at the time of grafting. For most hand burns, an orthosis that positions the hand in the previously discussed antideformity position (wrist extension, MCP joint flexion, IP joint extension, and the thumb midway between radial and palmar abduction) should be applied by the therapist in the operating room immediately after grafting. This orthosis is worn for approximately 5 days. Adjacent nongrafted areas may be mobilized. As previously discussed in the case of a palmar burn, the wrist and digits are positioned in extension and thumb in radial abduction and extension.
Protocols for when to initiate motion and how much motion is permitted following grafting vary from facility to facility. Some prefer immobilization of the hand for up to 5 days, whereas others may initiate some or full motion much earlier.68 Specific reintroduction of motion depends on the appearance of the graft and on the ability of the patient to cooperate. Motion should not be performed on hands when grafts appear wet or discolored, or when bleeding is excessive. Assuming graft integrity and patient cooperation, gentle AROM in isolated ranges can be performed on the second postoperative day. By the third or fourth day, gentle full AROM may be permitted. Also by the fourth day, the orthosis may be removed during the day and worn at night only. In the case of a FTSG, ROM is typically initiated between 5 and 7 days after surgery, depending on how well the graft takes to the palm (Fig. 26-11).

Figure 26-11 In the case of a full-thickness skin graft, range of motion is typically initiated between 5 to 7 days postoperatively, depending on how well the graft takes to the palm.
Cultured epithelial autografts (CEA) are more fragile than traditional STSGs, often lacking long-term durability.69,70 Ensuring graft adherence and survivability of CEA frequently requires adjustments in the therapy program. Resumption of motion often is delayed until 7 to 10 days postoperatively or longer after CEA application rather than the typical 4- to 5-day immobilization period common with standard STSGs. The implementation of orthoses or pressure garments also may be delayed or limited because of their potential stress and shearing forces.
As previously described in Chapter 25, Integra is an artificial skin comprising two layers, both of which are essentially temporary. One significant benefit of Integra is that scar formation is minimal.71 One of its shortcomings, however, is that the final dermis does not contain hair follicles and sweat glands; however, Burk,72 a pioneer in the development of artificial skin, reported that sensory function returns to the same level and on the same time course as it does following normal split-thickness autografting.
Initiation of ROM and removal of orthoses following Integra placement depend on the surgeon’s preferences. Integra Life Sciences Corporation states that the site of placement should be immobilized for 5 days, with ROM beginning on the fifth day.73 No other therapeutic guidelines are outlined. Some facilities only allow partial ROM until final coverage, but others progress to full ROM prior to final coverage. It is important that the therapist views the Integra prior to and during the initiation and progression of ROM. If the ROM program is too aggressive, it causes the Integra to tear or lift off of the wound bed.
The rehabilitation phase generally extends from the time of graft adherence or wound closure until scar maturation. The primary goals of therapy at this time are to protect the new spontaneously healed wound or the fragile graft, preserve joint mobility, increase strength and function, and inhibit the development of scar contraction and hypertrophy.
In addition to the typical hand therapy clinical examination, evaluation of the burned hand during the rehabilitation phase should include evaluation of the scar. If the patient has suffered anoxia or an electrical injury, assessment of other burn-related aspects, such as muscle tone and cognition, should be included. Several dexterity measures are available; however, there has been minimal testing within the burn population. Anecdotally, evidence has suggested the use of objective measures such as the Jebsen’s Hand Function Test, Minnesota Rate of Manipulation Test, Purdue Peg Board, and Grooved Peg Board test.74 More functional-based nontimed assessments, such as the Manual Ability Measure, are emerging, which incorporate a self-rating by the patient and clinician. Upper-extremity-specific outcome measures that are self-reports and not clinician-driven include the Michigan Hand Outcomes Questionnaire (MHQ) and the Disability of Arm, Shoulder, and Hand Questionnaire (DASH). Both measures assess beyond the impairment level. In the case of a pediatric patient, developmental assessments or screenings should be administered, particularly those that assess fine motor skills.
Scar is evaluated to provide both an objective and a subjective description, to assess the need for and efficacy of treatment, and to estimate maturation. Several methods and tools for evaluating scar have been presented:
1. Oximeter to measure transcutaneous oxygen tension as an index of maturity75
2. Laser Doppler flowmeter to measure microcirculation in grafts and healed wounds to assess such variables as likelihood of hypertrophic scar formation and scar maturity27,76,77
3. Tonometer to measure scar pliability, firmness, and tension (data that can be used to quantify the course of cicatrization and evaluate the effectiveness of therapy)78-81
4. Elastometer to measure elastic properties of scar to objectively document scar response to treatment or scar maturity82
5. Quasistatic extensometer to measure extensibility of hypertrophic scar83
6. Dermal torque meter to measure viscoelastic properties of scar and grafts to assess various components of pliability84
7. Ultrasound (US) to measure scar thickness to monitor the progress of hypertrophic scar79,80,85
8. Objective measurements from positive molds of the scar86
9. Shear velocity device to measure propagation of an auditory shear wave through the skin surface to assess biomechanical alterations (e.g., stiffness) of scar87
10. Scales with visual and other components88-93
Although all of these tools are useful in measuring aspects of scar and the scarring process, no instrument or method has been accepted or used universally.51 Many are costly, time-consuming, and impractical within the clinic setting.93
In 1990, the Vancouver Scar Scale (VSS) was developed by the Occupational Therapy Department at Vancouver General Hospital, Vancouver, British Columbia, Canada (Fig. 26-12). This instrument is currently the most widely utilized scar assessment tool among burn therapists.89 The VSS rates four characteristics of burn scar: pigmentation, vascularity, pliability, and scar height89 (Fig. 26-13). The originators of the VSS believe such characteristics relate to the healing and maturation of wounds, cosmetic appearance, and function of the healed skin.89 Several authors and clinicians have made or proposed modifications to the VSS, including Nedelec and coworkers,91 whose proposed changes relate to improving the scale’s construct validity. Forbes-Duchart and associates93 modified the scale to include two color scales for Caucasians and Aboriginal clients and to adopt the Plexiglas tool developed by Baryza and Baryza.92 At the conclusion of their study, they further suggest omitting the pigment section and reclassifying the color scales as “light,” “medium,” and “dark.” It is recommended that the VSS be performed following autografting and at every reevaluation thereafter.
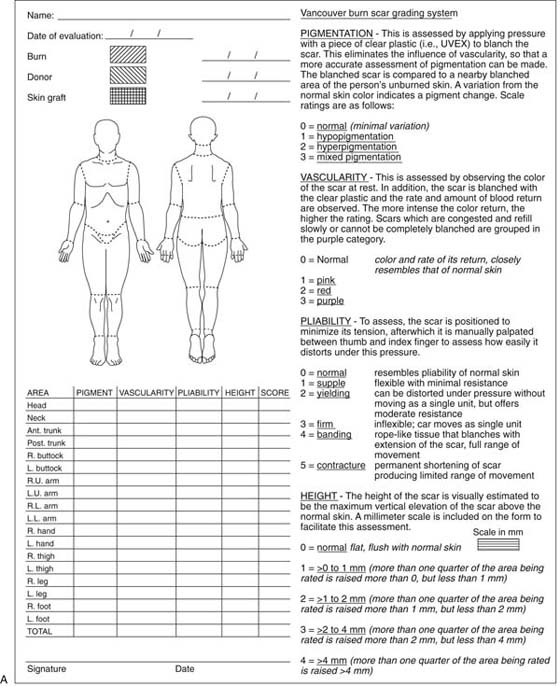
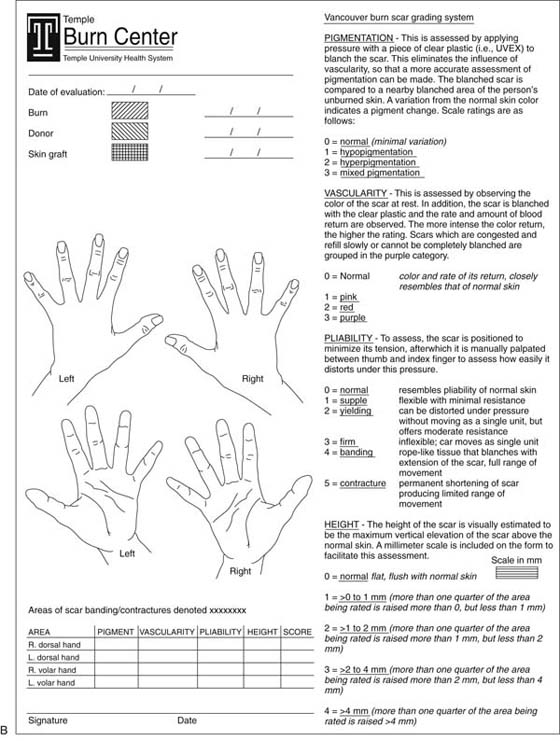
Figure 26-12 A, Vancouver Scar Scale (VSS). B, VSS, the occupational therapy department at Temple University Hospital, Philadelphia.

Figure 26-13 The Vancouver Scar Scale rates four characteristics of burn scar: pigmentation (A), vascularity (B), pliability (C), and scar height (D).
Although not objective, photographs are helpful in cataloging change in a scar. They should be taken in a standardized fashion (i.e., distance from subject, angle, lens) at regular intervals and can be used with a visual assessment scale).85 Because donor sites occasionally develop hypertrophic scar, the therapist should evaluate the donor site or sites in addition to evaluating healed burned and grafted sites.
Currently no published studies have evaluated the relationship between a patient’s subjective scar evaluations and that of the therapist’s objective measurement. Nor are there any studies that relate these two findings to function and return to life roles.
The continued presence of edema during the rehabilitation phase can be addressed by several means. If some wounds still remain open, edema management may be initiated to the digits via self-adherent wraps such as 3M Coban or Co-Wrap.94-96 However, care must be taken to protect fragile new tissue or recently adherent grafts, and circulation should be monitored during the period they are worn. If reduction in edema is a treatment goal, objective measurements (circumferential measurements at joint or phalanx) should be taken before and after intervention to determine and monitor the intervention’s effectiveness. Once the hand is completely healed, wrapping the entire hand can be initiated, or commercially available interim compression gloves, such as an Isotoner Therapeutic Glove, can be utilized.95 Due to the fragile nature of newly healed tissue and grafts, it is recommended that compression initially remain on for only a few hours.
Massage has been reported to be effective in increasing and preserving mobility (by freeing restrictive fibrous bands) and in increasing circulation.97 However, in one study of 15 pediatric patients who received 10 minutes daily of massage over a 3-month period,98 no differences were found in the vascularity, pliability, and height of the scars, as measured by a modified VSS, although there were reports of decreased itching in some patients. Massage may be helpful in alleviating the commonly reported itching sensation that is partly caused by excessively dry and cracked skin resulting from damage to the sweat glands99 and from increased evaporative water loss from scar tissue.100 Massage appears to have other therapeutic benefits as well. Field and colleagues101 compared burn patients who received massage therapy with a control group who did not. The group who received massage therapy had reduced itching, pain, anxiety, depressed mood, and showed long-term improvements on these measures from the first to the last day of the 5-week study.
In a pilot study conducted by Morien and coworkers102 eight pediatric burn survivors received massage over a grafted area once a day for 3 to 5 days. Each massage session lasted 20 to 25 minutes. Therapeutic massage on scar tissue consisted of 5 minutes of lengthening using long light strokes (effleurage); 5 minutes of stretching and rolling strokes, which consisted of lifting and rolling the tissue between hands, fingers, or thumbs (petrissage); and, depending on the pain tolerance of the child, 2 to 5 minutes of small cross-fiber movements (friction) to loosen the scar tissue from the underlying tissue. The last 5 minutes of the massage session consisted of general lengthening and rolling. Overall the massage was found to increase ROM in children with burn scars; however, no change in mood was noted. The authors account for this by the fact that the study was conducted during a burn camp, so the kids were excited about the week ahead.102
Only gentle massage should be performed on newly spontaneously healed or recently adherent grafts because the skin is fragile and friction can result in skin breakdown and blister formation. New or fragile skin may appear translucent and wet, be sensitive to touch, or appear as though it will break open with slight pressure. As the skin becomes thicker and stronger, greater pressure can be exerted by massaging in a rotary motion along the scar. Creams that are not water-based, such as BIOTONE dual-purpose massage creme, are recommended because they are good lubricants and are not rapidly absorbed into the skin. One should not massage over small open areas because this could result in delayed wound healing at those sites. The skin should be massaged at least twice a day and up to six times a day for 5 to 10 minutes.67,96 After the massage, the excess cream should be removed and pressure garments reapplied. An electrical or battery-operated massager may be utilized and may be helpful for carryover of the home exercise program. Heat attachments may be used; however, skin checks should be performed regularly67 (Fig. 26-14).

Figure 26-14 An electrical or battery-operated massager may be helpful for carryover of the home exercise and desensitization program.
When evaluating ROM in the recently healed burned hand, the therapist should look at the total ROM across several joints and evaluate individual joint motion. A patient with a dorsal hand burn may have full passive flexion of the MCP and PIP joints individually yet still be unable to make a full fist actively. Contracting scar, leading to loss of skin mobility, also can cause loss of active motion in an adjacent, unburned area. For example, the patient with a burn to the dorsum of the hand may be able to actively make a fist with the wrist extended but, because of scar contraction, may not be able to do so with the wrist at neutral or in slight flexion.
The exercise program, performed a minimum of three times a day, should consist of exercises to achieve full active and passive wrist motion and full total active motion (TAM) and total passive motion (TPM) of the digits in flexion and extension. Isolated tendon gliding exercises for the flexor digitorum profundus and flexor digitorum superficialis, as well as intrinsic muscle exercises, should be included. PROM should be performed if there is individual joint or tendon tightness. Joint ROM can be facilitated by mild traction.103 Webspaces should be stretched both actively and passively.103 The thumb should be exercised in all planes of motion. It is particularly important to maintain thumb opposition and to maintain the thumb webspace in both radial and palmar abduction. Spontaneous use of the hand should be strongly encouraged to help the patient overcome the fear of potential skin breakdown or pain with use.
Resistive exercises and activities that challenge finger dexterity should be increased in pace with the patient’s tolerance (Fig. 26-15). Cronan and colleagues104 reported that because muscle tissue is one of the most mutable tissues in the body; a burn injury can affect the musculoskeletal system as well as the skin. In a study of burn patients returning to work, Cronan and colleagues104 demonstrated that those patients given isokinetic exercise in addition to isometric and isotonic exercises were found to produce a better test outcome than those receiving isometric and isotonic exercise training only. Citing other work105 that shows that slow-twitch and fast-twitch muscle fibers are present in an equal ratio, Cronan and colleagues104 stated that therapy must involve training of both types of fibers. They explained that fatigue results from improper training of slow-twitch fibers and that joint pain after increased activity or inability to perform certain work loads for extended periods may be caused by improper training of fast-twitch fibers. Training involved the use of isokinetic exercise equipment. Cronan and colleagues104 stated that light submaximal contraction selectively recruits slow-twitch fibers, moderate submaximal contraction adds fast-twitch fibers, and maximal contraction leads to an “all-or-none” recruitment of both fiber types.
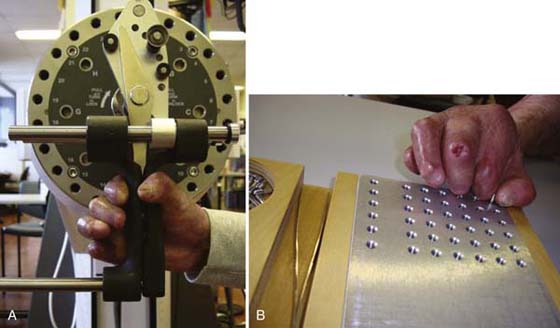
Figure 26-15 Resistive exercises (A) and activities that challenge finger dexterity (B) should be increased in pace with the patient’s tolerance.
The unburned hand also may need to be included in the therapy program. In a study of hand function after major burns, Covey and coworkers104 found that the unburned hand also can show impairments in strength, TAM, and coordination at the time of hospital discharge. By 3 months after discharge, all study participants had normal TAM, and most had achieved normal grip strength and coordination; however, some required as long as 12 months after discharge to regain normal strength and coordination.
In addition to weakness that can occur as the result of any hospitalization, many metabolic disorders, including altered protein kinetics with muscle weakness, result from burn injury. Investigators106 compared muscle dysfunction in burn-injured rats in the absence of apparent immobilization with muscle dysfunction after immobilization alone. Their findings suggest that muscle dysfunction after immobilization alone occurs primarily as the result of loss of muscle mass, whereas muscle dysfunction after burn injury on days 1 to 7 is a result of a decline in specific tension, and at day 14 is the result of a decline in specific tension and muscle mass. Research on rats with 40% TBSA scald burns showed that although the muscles directly beneath the burned skin were not damaged by the burn, they demonstrated dramatic apoptotic (cell death initiated by the cell itself) changes.107 Apoptosis also was confirmed at muscle sites distant from the injury. These changes peaked at postburn days 3 and 7, indicating to the investigators the need for early and continuous intervention.
Use of compression therapy dates back to the 16th century. Rayer utilized pressure in the treatment of keloids in 1835 and Unna in 1881 for burned scars.108 Its use gained popularity in the 1970s when alterations in burn scar tissue were noted with the use of vascular support garments and orthoses.109,110 Since that time burn therapists have generally accepted and utilized pressure garments (PG) as the first line of defense against scarring, despite the lack of evidence supporting its clinical effectiveness.
A large body of dermatologic, histologic, clinical, and anecdotal or case study evidence supports the effectiveness of PGs; however, the working mechanism has not been fully proven.111 Studies112,113 on tissue gases in normal dermis and in hypertrophic scars have found that pressure of approximately 25 mm Hg is believed to decrease the blood flow to rapidly metabolizing collagenous tissue. The authors of these studies noted that hypoxia does not appear to result in cell death but does indirectly affect the metabolic pathway (e.g., collagen formation) of scar growth or maturation. Another viewpoint is that pressure only causes dehydration of the scar (by indirectly affecting mast cells) and that the temporary diminished size of the scar noted after application of pressure is caused by the close approximation of collagen cross-linking.114,115
In 2009, Anzarut and associates116 performed the first meta-analysis of the effectiveness of PG therapy for the prevention of scarring after a burn injury. The review included 316 patients from six randomized controlled trials. After reviewing scar assessments, they were unable to find a difference between scars that received PG and those that did not; however, there was a trend toward decreased scar height. Although the findings of this study do not fully support the use of PGs, the investigators conclude that the review had several limitations due to small number of studies. Despite lack of objective data, the therapist can take advantage of the positive effects seen clinically.
PG compliance varies and can be as low as 40% in some instances. A majority of the problems are physical, such as sweating, overheating, itching, pain, and difficulty performing various movements. A lack of communication between the therapist and patient and a patient’s perceived lack of information may also lead to noncompliance.117,118 Patients often complain about the quality of the garments, noting rapid wear and tear and the high cost to replace.117,118
Initiation of Pressure. Pressure is applied when a graft is adherent or wounds are almost closed (open wounds are smaller than a quarter). The purpose of pressure at this time is not just to inhibit scar contraction and hypertrophy but also to inhibit vascular and lymphatic pooling and to avert hypersensitive, fragile skin.119
Interim Pressure Bandages and Gloves. Interim pressure bandages or gloves may be used until the patient can tolerate commercially custom-made gloves. The choice of type of interim pressure bandage or glove depends on how much pressure the patient can tolerate, which typically increases over time. A progression of interim pressure bandages and gloves commonly is used until the patient receives commercially custom-made gloves. The therapist should postpone application of interim pressure bandages or gloves if the skin appears too fragile.
Early forms of pressure include self-adherent elastic wraps such as Coban or commercially made compression or edema gloves such as an Isotoner Therapeutic Glove. Several companies make self-adherent elastic wraps. They are available in several colors and widths and can be easily applied to a digit, hand, or over a dressing. A Coban glove may be a better option for a child who is noncompliant with an interim glove (Fig. 26-16). The Cincinnati Shriners Burns Institute guidelines96 are as follows:
1. Wrap each finger, beginning at the nail bed and wrapping in a spiral fashion proximally to the webspace.
2. The fingertip should be left exposed so that capillary refill can be monitored.
3. Then wrap the hand in a spiral fashion, starting at the knuckles and ending 1 inch past the wrist. When wrapping, the self-adherent wrap should be stretched up to 25% of its elasticity.
4. A small layer of moisturizer can be applied over the wrap to eliminate any tackiness.67,96
5. The glove should be removed daily for skin inspection and washing.
Several of the custom PG companies also manufacture interim gloves. They are typically softer and provide less pressure than the custom gloves. Sizes for adult interim gloves typically range from extra small to large. To fit a pediatric glove, a therapist must measure the circumference of the hand at the distal palmar crease (Fig. 26-17). Any of these pressure bandages and gloves can be worn over small open wounds. A light, nonadherent dressing should be placed over the open area prior to application of pressure.
Commercially Made Custom-Fitted Pressure Gloves. Commercially made custom-fitted gloves can be ordered from several companies, such as Barton-Carey Medical Products (Jellico, Tennessee); Bio-Concepts, Inc. (Phoenix, Arizona); Torbot Group, Inc. (Toledo, Ohio); Gottfried Medical, Inc. (Toledo, Ohio); Empathy Inc.; and Medical Z Inc. (San Antonio, Texas). Depending on the company, several types of materials, colors, adaptations, and individual custom designs are available. The therapist should select according to the requirements of the individual patient, and these may change over time depending on factors such as stage of scar maturation, the need for inserts, and the patient’s daily activity regimen.
Glove Materials and Options. A therapist may select from several materials. Depending on the manufacturer, gloves may be constructed from one of several different materials (or from a combination of two or more), with each material having its own properties of smoothness and stretch. Gloves may be made from softer material for patients who have more fragile skin or who cannot tolerate regular material. For durability, gloves for children should be made from regular material, unless the child is younger than 1 year of age. Then a softer material may be considered, particularly if the skin is fragile over the MCP joints and amputation sites.
Gloves can be ordered with zippers, Velcro closures, or without either.30,96 These closures can be placed almost anywhere on the dorsal, volar, or ulnar aspect of the glove. There are pros and cons with the use of closures. If skin tear is a concern, zippers are ordered in the first set of gloves to decrease friction on new, fragile skin. Patients and family members may also prefer zippers because they make it easier to put on or take off gloves, especially in the case of a child. If the therapist anticipates that the patient will need an insert, the glove should include a zipper to ensure proper placement of the insert and to provide ease of application.
The addition of a zipper or Velcro closures should be carefully considered as it decreases or disrupts pressure across the burn scar. The closures take the place of elastic material, are nonmobile, and can ripple, thereby causing disruption of pressure on and around their location. This may be particularly true in a pediatric glove where the zipper may make up a proportionally large part of the glove. In some cases the zipper leaves may leave an indentation on the skin and cause breakdown. If an insert is not anticipated and a skin tear is not a concern, the glove should be ordered without a zipper or Velcro closure.
Other modifications to the glove include slanted inserts at the webspaces. It is standard to request a glove with inserts if a client has self-healed skin or grafted areas surrounding the webspaces. On request, the glove manufacturer may also sew a dart almost anywhere in a glove to help provide pull in a particular direction. For example, a dart sewn in the area of the thenar eminence may help pull the thumb into opposition. In addition, when gloves have open fingertips, it is easier to ensure that the glove webspaces are flush with the webspaces of the hand than when the tips are closed. It also allows for improved dexterity. However, if the scar extends to the DIP and beyond, the fingertips should be enclosed. Additional glove options include extending the length of the glove past the wrist to include to the forearm or ordering a gauntlet if the digits are not involved.30,96
Grip Enhancements. Often the PG fabric makes it difficult to perform ADLs, work, and play due to a lack of friction and sensation at the palmar surface of the gloved hand.120-122 Recent addition of grip enhancements to the palmar surface of the glove have increased dexterity. O’Brien and colleagues121 developed the New York-Presbyterian Dexterity Glove (NYPDG) in conjunction with Torbot Group, Inc. (Toledo, Ohio). They added Silon to the volar surface of the digits and MCPs (Fig. 26-18). Medical Z, Inc. (San Antonio, Texas), also offers grip enhancements on their gloves. Dewey and coworkers120 performed a case series analysis of five different silicone and rubber grip enhancements developed and manufactured by Medical Z, Inc. The enhancements included rectangular rubber tabs, honeycomb pattern silicone, wavelike pattern silicone, line pattern silicone beads, and line pattern silicone beads embedded into the fabric. The researchers concluded that the wavy silicone pattern embedded into the fabric provide the best combination of grip and durability.120 The following companies currently manufacture gloves with grip enhancements: Barton-Carey Medical Products, Inc. (Jellico, Tennessee); Bioconcepts, Inc. (Phoenix, Arizona); Gottfried Medical, Inc. (Toledo, Ohio); Medical Z, Inc. (San Antonio, Texas); and Torbot, Inc. (Toledo, Ohio).120

Figure 26-18 New York-Presbyterian Dexterity Glove (NYPDG) with grip enhancements to the palmar surface of the glove for increased dexterity.
Wear and Care of Gloves. Commercially made custom-fitted pressure gloves are worn 23 hours per day until scar maturation, at which time the scar is no longer active (i.e., hypertrophying and contracting) and permanent removal of the glove will not lead to relapse.123-125 While the scar is active, the glove is removed only for bathing. The glove and added inserts can inhibit full AROM and at times may need to also be removed for exercise. Because of a developing child’s need to use his or her hand for both sensory and motor input, a child’s glove may need to be removed for specified periods throughout the day. Two sets of gloves are recommended due to the continuous wearing schedule, so that one can be worn while the other is being laundered.
The burn glove should fit snugly but not too tightly. A glove is too loose if the material can be pinched up from the skin. Custom-made pressure garments can lose their elasticity (and therefore their pressure) due to the frequent, rapid, and complex movements of the hand. Although seeming to fit adequately, new sets may be necessary approximately every 2 to 3 months to ensure that adequate pressure is being provided.
Many factors contribute to the breakdown of elasticity. Some of these factors are normal wear and tear (“normal” can vary widely according to occupation or daily activity), the use of petroleum-based lotions and ointments, and laundering. Some glove manufacturers recommend washing your glove in the delicate cycle; however, this has been observed to lead to quicker wear and tear. It is recommended that gloves be hand-washed with a mild soap and warm water and laid out to dry. Avoid “ringing out” of the glove as this further stretches the material. Even without daily wear and tear, gloves may need to be adjusted or new measurements taken to accommodate for edema and weight changes, contractures, or normal growth in a child.
Dynamics of Pressure and the Use of Inserts. The amount of pressure the gloves are designed to apply varies according to the individual manufacturer. In addition, some manufacturers design gloves to provide a uniform pressure, whereas other manufacturers design gloves to apply a gradient pressure (i.e., pressure that decreases distally to proximally). Although the gloves are designed to apply a specific amount of pressure over a specific body part, the actual pressure being applied may be below what is considered therapeutic or vary depending on the position of the hand.126 In addition, despite the fact that pressure garments are custom-made and appear to fit well, there still may be problems with hard, thickening, or contracting scar. If this is so, pressure in those areas may be insufficient.
To be effective, pressure must be conforming. The palm of the hand is a concave surface. The best-made custom-fitted glove always bridges across this area while fitting snugly over convex areas. When a glove is applied to a hand with a burn on the palmar surface, an insert must be used to achieve adequate pressure. Many materials can be used as inserts. Some examples are Rolyan Silicone Elastomer, Rolyan 50/50 Mix Elastomer Putty, Rolyan Polycushion, OTOFORM-K/c Elastomer, Rolyan Prosthetic Foam, or Rolyan Ezemix Elastomer Putty. When Rolyan Polycushion or any sponge with an adhesive side is used as an insert, the paper backing is removed from the adhesive side and a stockinette or similar fabric is placed on the adhesive side. The sponge side is placed against the patient’s skin. The glove manufacturer can sew a pocket in the palmar, dorsal, or other specified part of the glove to secure an insert. However, a pocket may interfere with the conformity of the insert to the surface of the skin, and therefore care should be taken in this regard.
Most hand burns involve the dorsal rather than the palmar surface. Although the dorsum is a convex surface, inserts still may be necessary. Interdigital webspaces are concave surfaces that can hypertrophy even when a glove is worn. These areas are a problem not only because they are concave but because there is essentially little opposing force for the webspaces. One can compensate for this by using a dynamic webspacer or by adding conforming pressure with the use of inserts (Fig. 26-19). Webspacers can be constructed from many materials. Some examples are Rolyan Polycushion, Neo-Plush Sheet, 1/16-inch Aquaplast, Beta-pile, Otoform-K/c Elastomer, and Rolyan Silicone Elastomer and Oleeva FOAM.
When a custom-made glove is used, pressure is usually greater over harder surfaces of the body than over softer ones. Therefore, inserts may be needed over softer surfaces. Where inserts are used, the skin must be checked routinely for maceration or breakdown. Inserts, especially more rigid or bulky ones, also can limit motion or function. For these reasons, even though constant pressure is preferred, it may be possible to use inserts only part of the day. Softer or less restricting inserts can be used during the day and more rigid inserts used at night.
Inserts can also be fabricated specifically to be worn in an orthosis. Ideally, the insert is fabricated on a perforated material, and then the patient’s hand is placed over the insert as it is setting. The insert conforms and somewhat seeps into the perforations and is therefore less likely to slide. Orthoses also can be made of 1/16-inch Aquaplast. Both types of orthoses can be adjusted or reconstructed regularly as scar or ROM changes. Because this type of pressure inhibits hand use, these types of orthoses may be desirable for only a brief period or may be used solely at night, while a glove and an insert are worn during the day. The orthosis is attached with an elastic gauze wrap or with Coban. A sponge or gauze roll insert over the dorsum of the hand can be wrapped in to inhibit curling of the fingers and provide excellent conforming pressure and traction.
Silicone Gel Sheets. Silocone gel sheets (SGS), which are soft, semiocclusive, and flexible sheets, have been utilized in the United States with increasing popularity since the 1980s.127 Some brands have a tacky or adhesive surface that helps the sheet to better stay in place. SGS are indicated in a scar that remains raised and with decreased pliability despite PGs. The scar may or may not affect ROM. It is contraindicated in patients with open wounds and known allergies to silicone. The addition of an SGS increases pressure against the scar and adds to the risk for breakdown if worn for 24 hours upon initiation. Therefore, it is recommended that patients begin with 4 hours the first day and gradually increase the wearing time over the next 5 days. If a patient complains of a rash or increased itchiness, the SGS should be removed and therapist notified as the patient may be having an allergic reaction. In this case silicone-free Silon and Silipos products can be tried. The SGS should be washed daily with warm water and a mild soap and laid out to dry. If an SGS is indicated over a joint, patients may often only wear it at times of rest even if they could benefit from longer use. If the joint is frequently flexing and extending it may cause the silicone to roll up under the pressure garments.
Controlled studies report topical SGS to be effective in both the prevention and the treatment of hypertrophic scars and of keloids, and in increasing ROM that has been limited by burn scar contracture.80,127-138 In a study that included subjective assessments and objective measurements, Ahn and coworkers134,135 showed that SGS placed on hypertrophic scar for a minimum of just 12 hours daily and worn for a duration of only 2 months were effective in increasing scar elasticity and in flattening established hypertrophic burn scars. They were also effective in preventatively limiting large-scar volume of surgical scars. Although SGS were effective in studies in inhibiting the development of hypertrophy of all surgical scars, not all established hypertrophic scars responded to treatment by SGS.80,135 They were beneficial in treating longstanding hypertrophic scars, some as old as 3 years.134 Wessling and colleagues,133 in a controlled investigation involving patients with limited ROM resulting from bilateral elbow burn scar contractures, demonstrated that SGS and exercise achieved greater gains in AROM than did the use of exercise alone; they also found that these gains were not the result of a placebo effect.
The Cochrane Collaboration reviewed the use of SGS in the prevention and treatment of hypertrophic scarring and keloid scars.8 They reviewed 15 trials, involving 615 patients. From this literature they concluded that evidence for the effects of SGS are obscured by the poor quality of the research. There appeared to be few abnormal scars in people at high risk associated with use of SGS; however, they report that these findings are highly susceptible to bias.
There are many SGS options. The therapist needs to consider the flexibility of the insert, application site, the width, and if an adhesive backing is required.96 Oleeva Fabric works well over the dorsal hand because of its fabric backing. It decreases friction and allows the glove to slide over the insert more easily. Topigel and Oleeva Clear are also two types of thinner, adhesive SGS that can be utilized over the dorsum of the hand and dorsal or volar wrist.
Orthotic fabrication is used initially during the rehabilitation phase to preserve ROM by opposing the force of contracting scar, usually during periods of patient inactivity. Traction also is used to correct scar contractures. Static and static progressive orthoses are typically used, but in some cases dynamic orthoses may be helpful30 (Fig. 26-20).
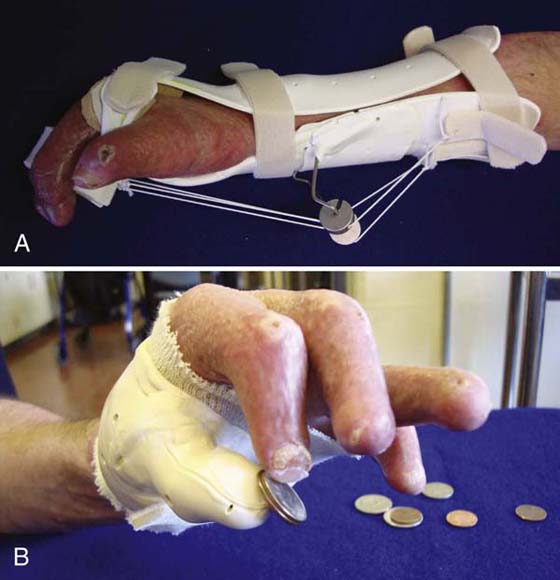
Figure 26-20 A, Static progressive orthosis to increase metacarpophalangeal joint flexion. B, Static orthosis to increase prehensile function.
Recently, Bio Med Sciences, Inc., developed an orthosis material called Silon-LTS that combines both thermoplast and silicone. This material works well in areas, such as the palm and webspaces, in which it is typically difficult to apply steady, even pressure. When wearing an orthosis made of this material, it is recommended that the patient remove the glove in order to get the scar management effects of the top, conforming silicone layer.
A great resource for burn orthoses is An Atlas and Compendium of Burn Splints.139 The editors compiled a single comprehensive resource of burn orthoses. Sections 4 through 9 are dedicated to the upper extremity. Materials needed, fabrication instructions, advantages, disadvantages, indications, precautions, and supporting references are listed with each orthosis.
Casting to provide positioning or serial casting to correct scar contractures or to increase ROM can be used at almost any time throughout the acute and rehabilitation phases. Casting may delay or eliminate the need for surgical correction of contractures, including finger deformities, MCP joint hyperextension contractures, thumb–index webspace contractures, and other soft tissue contractures, that may occur after burn injuries.140 Casting theory is based on Brand’s work of using plaster to promote elongation of tissue and collagen realignment through application of continuous force in a desired corrective position.141 Serial casting also can result in flatter, softer, and more supple tissue.142 In addition, casts can provide protection for wounds or exposed tendons. Casts have advantages over orthotic fabrication in that they cannot be removed by the patient and they do not slip,143 and, depending on the specific cast, they can provide a higher degree of conformity. They are particularly useful when traditional methods of therapy have been ineffective142 or when multiple joints are involved.
Casts may be applied over dressings or inserts. They can be circular, univalve, or bivalve, and made of either plaster or synthetic material. 3M Soft Cast and Delta-Cast Soft are synthetic casts that appear particularly suited for children because they are light, semirigid, and easy to apply. Both can be removed via scissors or unraveling by a therapist or parent. Such removal may be less frightening to the child than removal by a cast saw. Specialist plaster bandages also may be removed without a cast saw by soaking the cast in warm water and unrolling it.
With the goal of increasing finger flexion of all involved joints, Harris and associates144 serial casted 15 grafted, burned hands that had limited ROM. Most of the casts were removed and reapplied in 1 day, and most of the second casts were worn for more than 1 day but for fewer than 6 days. A mean increase in total ROM of 51.1% was achieved. The greatest increase in motion was found at the MCP joint, and the greatest gains were obtained with the second cast.
Rivers142 recommends casting as a way to increase motion in the burned hand when the hand is stiff in both flexion and extension. In such cases, serial casting is performed alternating flexion with extension casts. Casts may be particularly effective in maintaining MCP joint flexion in toddlers while allowing active flexion of the digits,145 and serial casting may be effective in correcting scar contractures even in the small digits of children.
The choice of specific casting procedure varies according to the individual patient’s status and needs. The therapist should consider the type of cast material used and ensure that the water temperature is cool and that the cast-application environment is well ventilated and has a moderate temperature and humidity. Patients with uncontrolled edema, circulatory problems, or neuropathies are not good candidates for casting. If a cast is to be applied over a wound, the wound must be clean and free of infection. Any necessary topical agents and nonadherent dressings are placed on the wound prior to casting. In some cases, it may be beneficial to measure the size of the open wound before casting and following removal. The use of nonbulky dressings reduces the potential for cast migration and resultant skin shear. If an insert is being used, it is secured in an area requiring particular conforming pressure; it should be placed over intact skin only. An insert should not be initiated the day of casting. It is important to ensure that a patient is tolerating the insert well prior to casting to eliminate the possibility of an allergic reaction. Next, a stockinette, terrycloth liner, or cast padding is then donned. Cast padding such as Rolyan Padding or Polycushion should be applied over bony prominences and can be utilized along the line of cut. A strip of felt can also be taped to protect the patient from the vibration of the cast saw during cast removal.11 If the goal of casting is to increase ROM, the tissue usually is placed on maximum or near-maximum stretch. However, serial casting that is executed with low increments in ROM and with low force applied over burn scar reduces the risks of edema, skin breakdown, tissue rupture, and increased scar formation. If the cast padding is too bulky or if the cast is applied too loosely, the maximum benefits of casting may not be achieved. However, if the cast is applied too tightly, the excessive pressure can result in skin breakdown, vascular compromise, and peripheral neuropathies. The practitioner also should be alert to wrinkles in the padding, which can cause skin breakdown because of the increased skin fragility in burn patients. The hand position is checked and adjusted as necessary. The desired position is held until the cast is dry or hard, but care should be taken to avoid indentations from the therapist’s fingers.133 Depending on the specific patient, the cast is changed between twice per day142 and a week.133 On average a cast is left on for 2 to 4 days.
Another method of casting utilizes Delta-Cast conformable (polyester cast) tape. Two to four layers of cast material are placed in a parallel fashion over the area of concern (e.g., just proximal to dorsal PIPs to midforearm to promote MCP flexion). The roll is then wrapped in a spiral fashion up and down the length of cast (e.g., PIPs to two thirds up forearm). One of the advantages of the Delta-Cast material is that it can later be removed and used as an orthosis. It also sets quickly, can be washed in the dishwasher, dried with a hair dryer, and worn during swimming. The gains achieved through casting must always be maintained through orthotic fabrication, pressure, exercise, and other indicated treatments.
Besides the physical agents already discussed, many other methods may be beneficial in scar management of the burned hand. More studies and documentation concerning the use and effectiveness of many of these modalities with the burned hand are needed.
Paraffin. The use of paraffin in treating burn scar contractures has been described by Head and Helm,146 who state that paraffin, when combined with sustained stretch, can increase collagen extensibility, make the skin more pliable, decrease joint discomfort, and increase joint ROM. The paraffin is mixed with mineral oil (12 pounds of paraffin to 1 quart of mineral oil), and the temperature is lowered to 115°F.147 Patients with limited finger flexion can be flexion wrapped with a self-adherent tape such as Coban or they should make a tight fist around a cone or cylinder before dipping the hand into the paraffin. Often patients cannot tolerate the heat of the paraffin bath, in which case the paraffin should be painted on with a paintbrush or piece of gauze.148 After the paraffin has been applied, the hand is covered with plastic wrap, and the position of finger flexion is maintained with an elastic wrap.
Gross and Stafford147 described a modified method for paraffin application. Pieces of coarse mesh gauze are dipped in paraffin and applied on the scar area. A layer of plastic wrap and a towel are then applied. With the wax in place, gentle long stretch and active exercises are performed.
Paraffin should not be used on patients with fragile skin or decreased sensation. Many burn patients appear to have increased sensitivity to heat or may be fearful of hot liquids.
Continuous Passive Motion. Therapists may use continuous passive motion (CPM) machines in the treatment of hand burns to help maintain or restore ROM.149-151 The machines can be applied over dressings. CPM machines do not replace the therapist; they are an adjunct to therapy. In addition, hand CPMs do not take all of the finger joints through the full ROM. Studies on the use of CPM with patients with hand burns that required excision and grafting found no difference between CPM and non-CPM groups in the degree of and length of time to regain TAM and TPM, in the rate of edema reduction, in reported pain, and in loss of graft attributable to motion.149,150 The authors of one study149 concluded that those who would most benefit from CPM included patients with extensive burns covering multiple joint areas; patients who have decreased cognitive function and who require passive motion over a protracted period; and patients who demonstrate little active motion because of pain, edema, and anxiety.
Functional Electrical Stimulation. A pilot study reported by Apfel and colleagues152 investigated the use of functional electrical stimulation (FES) with three patients with three severely burned hands that had not responded to traditional ROM and exercise techniques. The FES was applied to the flexor digitorum superficialis in hands with an intrinsic-plus imbalance. Objective measurement showed late improvement in hand function after the use of FES. However, FES appears to be used rarely in burn care.
Ultrasound. Ultrasound (US) has been used in the treatment of scars to increase ROM, reduce pain, and decrease scar formation.151 In 1954, Bierman153 reported increases in ROM and reduction of pain after US treatments of scars. Except for one patient who had sustained a burn 2 months before initiation of US treatments, the age of the scars was not specified. However, in 1993, Ward and coworkers154 reported no difference in ROM or in perceived pain between a control group that received placebo US followed by passive stretching and an experimental group that received US followed by passive stretching. As pointed out by Nussbaum,155 this study also omits detail, such as time from initial injury and breakdown of results for different burn sites, that might be relevant to a discussion of the study’s findings. In 1970, Wright and Haase156 examined biopsies and photographs of keloids of six individuals before and after a period of 24 US treatments and found no difference between treated and untreated scars. Because all of their specimens revealed a great deal of hyalinized connective tissue, Wright and Haase156 concluded that US was unsuccessful in the treatment of keloids in the later stages, when a great deal of hyalinized tissue had developed, and that the favorable reports of US in the literature represented keloids or hypertrophic scars that had been treated in the fibroblastic or fibrous stage.
The aforementioned US studies state or imply that the pain being treated by US was scar pain, and the results of the studies were conflicting. Despite such incongruities in the effectiveness of US in treating scar pain, Head63,146 pointed out that US is useful in the treatment of painful joints in burn patients.
Iontophoresis. In two separate case studies when used with exercises and manual treatment, iontophoresis with iodine (Iodex) and with methyl salicylate ointment (because of its sclerolytic effect), can be an effective agent for reducing post-traumatic scar adhesions.157,158 We have used saline with 0.9% to 3.0% concentration as a means of hydrating the tough and adherent burn scars before mobilization with encouraging results. When applying iontophoresis to a scar, we recommend lower intensities and longer delivery time because tissue resistance and permeability of scars is greater than in unburned skin. To maximize tissue diffusion, the buffered pad should be left on the patient’s skin for a few hours. We find this method to be safe since the fluid composition of the human body is primarily made up of saline. However, we have yet to demonstrate the efficacy of our methods through empirical means (Fig. 26-21).
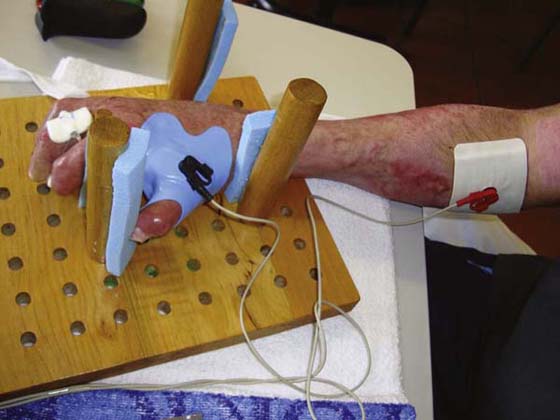
Figure 26-21 Iontophoresis with iodine (Iodex) and with methyl salicylate ointment may be an effective agent for reducing post-traumatic scar adhesions.
One agent, tranilast, appears to be the only known medication in the literature that has been examined extensively in the treatment of scars. Tranilast, an antiallergenic agent, has been shown to inhibit collagen synthesis in the treatment of keloid and hypertrophic scars when delivered via iontophoresis.159,160 This agent appears to be widely used in Japan where it was developed; however, we are not aware of any comparable studies conducted in the United States.
As noted previously, scar hypertrophy and contraction are major forces during the healing of the thermally injured hand that can contribute to decreased function, deformity, and disability. Besides the obvious effect scar hypertrophy and contraction can have on the appearance of the hand, without intervention they can have a devastating effect on the structures and function of the hand (Fig. 26-22).

Figure 26-22 Extreme example of deformity that can result from scarring and other deforming forces in the deeply burned hand.
The location of the scar contracture is of greater relevance than its size when it comes to the effect on function. A 1-cm scar contracture on the dorsal surface of the PIP joint can produce far more devastating effects than the same sized scar on the palm. In a retrospective review of 659 adult patients with hand burns who were treated over a 10-year period, 90% of hands with injuries not involving the extensor mechanism, any joint capsule, or bone eventually regained normal function.18 In a parallel study with children, Sheriden and colleagues found that only 20% of children with hand burns involving the underlying tendons and bones resulted in normal hand function, although 70% were able to perform basic ADLs.17 Scar size and its effect on function is also relative to its proportion to the body. For instance, a 1-cm scar on the palm of an adult may cause little loss of motion. That same 1-cm contracture in a small child’s hand may cause a more significant loss of motion.
In a retrospective study of 985 patients with burns, nearly 1 out of 4 demonstrated a hand contracture.161 From this subset group of 226 patients, an average of 10 joint contractures was found per patient, for a total of 2320 hand joint contractures. This number is not surprising, given the proximity of the joints of the hand and how they functionally interrelate during prehensile movements. Given the complexity of the hand and the extent of the functional effect of postburn contractures, therapists should get a sense of the gravity and complexity of the rehabilitative process.
Boutonnière deformity of the finger is a common problem in the burned hand (see Chapter 25 for pathophysiology). Given the complexity of the development of a boutonnière deformity, there is no simple solution to management. With nonoperative or preoperative rehabilitative management, patients with boutonnière or pseudoboutonnière deformity could benefit from a finger gutter orthosis that maintains the PIP joint in extension but allows some degree of DIP flexion. The extension at the PIP helps preserve the length of the volar plate, whereas the allowance for active DIP flexion facilitates dorsal displacement of the lateral bands by passive tension. In addition to maintenance of the PIP in extension, finger abduction and adduction exercises could promote proximal migration of the extensor mechanism with concomitant dorsal displacement of the lateral bands. To minimize PIP and DIP stiffness due to collateral ligament tightness or oblique retinacular ligament shortening, patients must be instructed to perform ROM exercises with the next proximal joint (i.e., MCP and PIP joints, respectively) in neutral extension.
When the central slip of the extensor tendon to the PIP joint has ruptured, the PIP joint is immobilized in extension for 6 weeks and active flexion exercises of the DIP joint are performed. DIP joint flexion with the PIP joint held in extension requires lengthening of the oblique retinacular ligaments and helps to prevent the DIP joint hyperextension component of the boutonnière deformity. After 4 weeks, the orthosis may be removed for AROM exercises to the PIP joint. PIP joint flexion should be done with care to avoid stressing the healing central slip and the development of an extension lag at the PIP joint. Flexion can be performed in a limited arc at first, and the ratio of exercises can be done in favor of PIP joint extension over flexion. By the sixth week, the orthosis is worn only at night, and PROM may be initiated as long as there is no significant extensor lag. Use of the orthosis may be discontinued after 8 weeks if no significant extensor lag is present.
Multiple surgical techniques are suggested in the literature,162-164 but with little consensus from the literature, there appear to be two general prevailing principles in the surgical repair of postburn boutonnière deformities: (1) maintenance of the lateral bands dorsal to the PIP axis of rotation with the ability to extend the PIP and DIP simultaneously, and (2) restoration of the continuity of the central slip in the extensor mechanism (see Chapter 25 for further discussion).
Contractures at the PIP joint after a burn may develop in various ways. One such pathomechanical sequence is PIP contractures due to boutonnière deformity, pseudoboutonnière deformity, or scar banding of the palmar surface of the finger. Other potential means of PIP joint contracture development include inadequate positioning that renders the PIP joints in partial flexion and prolonged dorsal hand edema in which extra fluid deposit produces tautness on the dorsal skin, flattening of the hand, and compression of the extensor tendons.
Rehabilitative management of the PIP joint contractures requires a multidimensional approach. Stern and MacMillan proposed a three-level classification of PIP joint contractures after a burn.165 Type I refers to PIP joint contractures that are due to scar alone (Fig. 26-23). Type II refers to PIP joint contractures due to involvement of articular structures, including the collateral ligaments and the volar plate. Type III occurs when the stiffness is most remarkable or the joint has arthrodesed. By highlighting various types of contractures, Stern and MacMillan have also presented different mechanisms in which PIP joint contractures may evolve.165 Thus, it is necessary to determine the exact pathomechanics of the contracture for treatment to be most effective. To illustrate, if the PIP joint contracture is due to scar banding (type I), it is logical to manage the scar and the contracture together. A “two-bird-with-one-stone” solution is the use of a finger gutter orthosis that extends to the DIP joint distally and MCP joint proximally. Not only is the orthosis more mechanically advantageous than a three-point orthosis as it spreads the force application and lengthens the moment arm of the corrective forces, the broad surface area creates a wide pressure application over the volar PIP joint scar. Although an infrequent occurrence in hand burns, singular PIP joint contractures may also be treated with dynamic or static progressive orthoses with a hand-based dorsal outrigger device. Whether the therapist opts for a static or dynamic/static progressive orthosis, the aim of orthotic fabrication must be to provide low-load passive stretching of the PIP joint volar structures (Fig. 26-24).

Figure 26-23 Example of a type I proximal interphalangeal joint contracture due to scar contraction.

Figure 26-24 The aim of orthotic fabrication must be to provide low-load passive stretching of the proximal interphalangeal volar structures.
Other interventions for PIP joint contractures include joint mobilization with sustained distraction through end ranges and serial casting for contractures that do not respond to conventional orthoses and traditional thermal agents. In 15 patients (total of 34 joints), Bennett and colleagues140 demonstrated that with unresponsive burn contractures, an average of 54% gain in joint ROM can be achieved through systematic application of serial casting.
The various configurations of carpals and metacarpals along with strong ligamentous support create three important arches of the hand: (1) the very stable proximal transverse arch; (2) the very mobile distal transverse arch; and (3) the variable longitudinal arch. All three arches are a necessary foundation to the various prehensile and grip patterns of the hand. In addition, the longitudinal arch has varying degrees of mobility and stability. The ulnar column, which is formed by the fourth and fifth metacarpals and the triquetrohamate articulation, offers carpometacarpal mobility necessary for power grip, and cylindrical and spherical grasps. Meanwhile, the radial column, which is formed by the second and third metacarpals and the lunocapitate and scaphocapitotrapezoid articulations, offers proximal stability for more prehensile precision patterns, such as tip and tripod pinch. Flattening of the hand can disrupt the anatomechanical configuration necessary for efficient and coordinated hand function.
As suggested earlier, flattening of the hand may be a direct outcome of dorsal hand edema. In our observation, scar contractures from dorsal hand and wrist burns are by far more common factors in producing flattening of the hand. In very few cases, postsurgical complications of partial-thickness grafts with excessive pulling of the dorsal skin may contribute to flattening of the hand.
Flattening of the hand may be treated with function-based activities that encourage use of the hand in various configurations. It may be necessary to add extra inserts within the compressive glove to the dorsum of the hand to increase the pressure on the scar. As a proactive measure during the early stages of recovery, therapists must continually evaluate the effect of the resting hand or pan orthosis on the arches of the hand. Preservation of the arches of the hand is just as important as maintaining the required joint angles of the wrist and digits. An effective orthosis is one that does both.
The opposite of flattening is cupping of the hand, in which the distal transverse arch of the palm becomes exaggerated or less mobile. This phenomenon is typically seen in patients with palmar burns and heavy scar bands. With hand use mainly consisting of frequent pressure contact on the palm such as during in-hand manipulation tasks or gross grip, many scars mature faster and become more pliable. Although cupping of the hand can be disabling, the extent of its effect on functional is comparably less than in persons whose burned hand has flattened.
Contractures in the webspaces of the fingers or the thumb are commonly observed in deep partial- or full-thickness burns that are located in the hand dorsally or circumferentially30 (Fig. 26-25). Two ways in which contractures at the webspaces typically form are syndactylism and scar banding. Syndactyly forms when scar or grafted skin advances over the webspace, creating a “hooding” over what normally is a down-sloping webspace between the fingers or between finger and thumb.166 Webspace contractures may occur on palmar, dorsal, or both surfaces and frequently require reconstructive surgery (see Chapter 25 for further discussion). On the other hand, scar bands develop across or along the lines of tension on the skin or on the borders of grafts.30 When either scar band or hood forms in the webspaces, abduction and opposition of the fingers (especially the ulnar rays) become limited. Consequently, patients have functional limitations in tasks that require spherical grasp, such as grabbing an apple and any other movements that requires cupping of the hand. In addition, scar bands over or across the webspace or hooding over the webspace may create “pockets” that pose additional functional challenges, especially for hand hygiene.

Figure 26-25 Contractures in the webspaces of the fingers are commonly observed in deep partial- or full-thickness burns that are located in the hand dorsally or circumferentially. (Howell JW. Management of the burned hand. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practice. Philadelphia: FA Davis; 1994:531–575.)
Since syndactylism and webspace contractures are mainly driven by scarring, specific considerations must be taken when it comes to the use of pressure gloves. Pressure inserts that are custom-made to individual webspaces have been demonstrated to be effective in reducing scar advancement, increasing digital ROM, and even restoring the anatomic slope and dorsal slant of the webspace.167,168
One highly disabling complication of scar banding is when it involves the thumb. Salisbury estimates that the thumb accounts for 50% of hand function. Practically, most prehensile movements requisite to normal ADLs involve the thumb.169
Compressive garments and pressure inserts to manage scar banding of the thumb may not be sufficient. As previously discussed in the pathogenesis of hypertrophic scars, multidirectional tension that is produced on the healing skin during thumb movements is proposed as the primary stimulus for scar band development. Thus, the thumb web needs a more rigid implement, such as an L-bar or radial/palmar abduction orthosis (Fig. 26-26) to provide prolonged and progressive pressure over the scar, stretch over the contracture, and limitation of multidirectional tension on the skin of the thumb web. A thin moldable insert such as Otoform K/c Elastomer may be placed underneath the orthosis to give added pressure over the scar band. If functionality is preferred, a wide C-bar orthosis that offers MCP and IP mobility of the thumb and composite flexion of the index finger may be provided during times when the patient is more active; alternating the C-bar with the L-bar orthosis during resting times can promote more prolonged pressure on the scar.

Figure 26-26 The C-bar or radial/palmar abduction orthosis to provide prolonged and progressive pressure over the scar of the thumb webspace.
Of the four fingers, excluding the thumb, the fifth is the most mobile. As a result, the fifth finger is most vulnerable to the formation of burn boutonnière.170 At times, the deformity may include torque malrotation and abduction of the fifth finger at the MCP joint due to scar bands. Unlike other digits of the hand, the origin of fifth digit boutonnière and associated deformation is typically nontraumatic, meaning there is no exposure, disruption, or rupture of the central slip at the PIP joint. If early attention is not given to the positioning of the fifth digit, severe scar contracture extending to the extensor mechanism and articular structures may ensue. To prevent MCP joint hyperextension and subsequent PIP joint flexion especially in the early stages of rehabilitation, we use separate strapping or a thermoplastic bar in the resting hand or pan orthosis for the fifth finger.
Other than its hypermobility, one additional explanation for the fifth finger’s tendency to deform is that people often do not fully include the fourth and fifth fingers in ADLs; instead they mainly use two-point, three-point, or lateral prehension to accomplish many tasks. This may be especially true of individuals who have sustained a burn to the hand because many of the deforming forces tend to flatten the palmar arches and extend or hyperextend the MCP joint; they therefore position the fifth finger in a manner such that the disinclination to use it and the difficulty to include it when performing ADLs is greater. It is therefore important to encourage and prompt patients to maximize volar surface contact on objects with the fifth finger during certain manipulation tasks such as holding a bottle or turning a doorknob.
Return to work, whether to the same or a different job, should be considered early in the course of treatment. Ideally, this goal requires a collaborative effort among the patient and his or her family, employer, medical professionals, workers’ compensation personnel, and insurer. When possible, referral to a work program is preferable for vocational assessment, work hardening, and work adaptation. Zeller and coworkers171 reported that 91% of burn patients returned to work after completing a work-hardening program versus 60% of patients with other diagnoses. The high success rate was attributed to early referral to the program and to the focus on rehabilitation in the burn center.
Helm and associates,172 in a study of time elapsed until return to work in patients with hand burns, examined the variables of (1) percentage of TBSA burned, (2) which hand was burned (dominant vs. nondominant), (3) whether grafting was required, (4) patient age, and (5) occupational category. The best indicator of time elapsed until return to work was percentage of TBSA burned. The second-highest predictor was found to be distributed equally between the categories of those patients requiring grafting and those patients with both hands burned.
In a continuation of the previous study, including additional variables and patients with and without hand burns, Helm and Walker173 again found that percentage of TBSA burned was the best predictor of time elapsed until return to work. Although patients with hand burns had smaller TBSA burns than the general burn population, they required a significantly longer time until they returned to work.
In a study of return to work of patients who had been employed before the burn injury, Saffle and colleagues174 found that the length of hospitalization, number of surgeries, TBSA and full-thickness burn size, and patients’ subjective assessment of their functional ability (including hand function), as well as their subjective assessment of scarring and appearance, correlated with time off from work. Also more likely to return to work than expected were patients who were covered by health insurance, whereas patients covered by Medicaid and those involved in injury-related lawsuits were less likely to return to work. The authors of the study noted that objectively assessed functional status may not be the only or primary indicator affecting return to work, rather an individual’s attitude and ability regarding return to work may be profoundly affected by personal, psychological, legal, and societal influences. Other investigators who studied the influence of various factors that might affect return to work in persons who had sustained severe burns (not specifically hand burns) found that burn severity and other acute factors (e.g., receiving grafts) were not the strongest factors predicting whether an individual returned to work; rather, the strongest positive predictors were being employed before the injury, receiving workers’ compensation, not blaming oneself, and being white.175
Back-to-work status after a burn injury depends on the preinjury employment status, the extent of the burn injury, the resulting physical limitations, and the patient’s motivation for returning to work. With transitional modified or light-duty job placement, environmental considerations, and job adaptations, most patients can successfully return to work. A detailed determination of the job requirements and description of the work environment are required before allowing the patient to return to work. No open wounds should be present, and skin fragility must be taken into account when considering job demands. Light-duty transitional jobs with environmental restrictions may need to be negotiated as a step toward reintegrating the patient back into work.
Although school reentry programs and anecdotal information on return to school have been described, actual studies are sparse. Just as with return to work, return to school should be considered early in the course of treatment. Some hospitals have school programs or tutors, and some school districts provide a teacher to help the child continue school work during hospitalization. Tutors are provided as necessary when the child is an outpatient. Successful return to school is the result of a cooperative effort between the child and his or her family, medical professionals, school professionals, and classmates.
School reentry programs that involve visits to the school by medical professionals or the use of videos or puppet programs have the goal of facilitating the child’s physical, social, and emotional return to school. School guidance counselors can assist in coordinating such programs with the parent and member of the burn center (often the play therapist or community outreach coordinator). Information is provided to the child’s classmates about his or her appearance and scars, what happened to the child, and the purpose of pressure garments and orthoses. The inappropriateness of teasing, the noncommunicability of scars, and fears are discussed. Highlighted is the fact that, although the child may not look the same, he or she is still the same on the inside and can still participate in and accomplish most, if not all, activities, or soon will be able to. The information presented to classmates is graded according to age. Specific instructions concerning orthoses, pressure garments, any wounds and dressings, skin care and sun precautions, and itching are provided to teachers, the school nurse, and other school personnel. The presence of bandaged open wounds does not preclude a student from returning to school. Contact with and coordination of services with a school occupational or physical therapist is indicated in some cases. The student may be restricted from recess or physical education activities, at least initially, because of skin fragility. Just as with return to work, sun and heat precautions should be taken.
Evaluation of the effectiveness of burn treatment protocols is encouraging. The assessments of functional return of the thermally injured hand have shown promising results. As to be expected, individuals who have sustained the deepest burns requiring grafts appear to demonstrate the greatest dysfunction in ROM, grip strength, and coordination. One year or more may be required for normal function to return.
A prospective longitudinal study by Roberts and coworkers176 investigated the relationship of strength recovery to living skills in the burn-injured child. All subjects had functional ROM. At 6 weeks after hospital discharge, all subjects tested normal for tip-to-tip pinch strength. At 6 months, 75% of the children achieved normative values for grip, lateral pinch, and tripod pinch strength. Subjects in the 14- to 19-year-old age group reached norms at 6 weeks after hospital discharge, and those in the 9- to 11-year-old age group reached norms at 6 months. The investigators speculated that this difference in recovery rate was secondary to the older age group having higher expected responsibilities and greater capabilities in skilled performance. However, because of the limited number of subjects, the investigators could not determine from the study whether limitations in hand prehension hindered independent performance of age-appropriate ADLs.
An investigation of physical and psychological rehabilitation outcomes of pediatric patients who had sustained 80% or more TBSA, 70% or more full-thickness injuries, found that 80% were independent in basic ADL skills and that 86% of children ages 10 years and older were independent in advanced ADL skills.126 Patients with amputated fingers were significantly more dependent in ADL skills than those without amputations. However, finger amputation alone was not the best predictor of functional independence. One or more finger amputations had to be paired with a major burn, one or more amputations of either limb, joint fusion, or brain anoxia. Encouragingly, psychosocial adjustment was normal.
Research has been performed to assess sensibility of grafted skin. Investigators, particularly in the past, have not always agreed. Several variables may contribute to the presence of sensory deficits and final sensory outcome. Such variables include the depth of injury, the type (or depth) of excision, the type of graft used, and age (but probably only if the individual is a young child). It also has been suggested that larger grafts or flaps may limit the number of axons available for reinnervation.176 Another explanation given for the diminished sensation is that increased scar formation impedes axon regeneration in skin grafts, and it may take up to 1 or 2 years to achieve final sensory return.178
The skin’s function, both to help regulate body temperature by sweating and to act as a water barrier to inhibit evaporative water loss, may be altered in the spontaneously healed or grafted burn wound. STSGs do not contain sweat glands,179 although sweat glands may be present in the interstices of meshed grafts.99 The loss of sweating may contribute to heat intolerance, especially in larger BSA burns.99 One report of poorly recognized sequelae of thermal hand injuries showed that those patients who had skin-grafted hands had more complaints of heat intolerance and altered perspiration than those whose hands were not grafted.180 In the study by Apfel and colleagues181 of enzymatically debrided and grafted partial-thickness hand burns, no sweating was seen initially in the grafted areas. However, by the second half of the year, more sweating was noted than in areas next to the graft. Apfel and colleagues181 stated that the presence of sweating was because of the preservation of the original dermal sweat glands and indicated one of the benefits of enzymatic (vs. surgical) excision and early autografting of the hand with deep dermal burns. A study by Cadwallader and Helm99 showed a decrease in the number of functioning sweat glands in hypertrophic scar tissue. However, interestingly, an increase in the activity of sweat glands was noted in burned areas as compared with control, unburned areas.
Studies of evaporative water loss from healed burn wounds revealed that grafted wounds had significantly lower rates of water loss than did normal skin.100,182 Partial-thickness wounds that healed with hypertrophic scarring had higher rates of evaporative water loss than did partial-thickness wounds that healed without hypertrophic scarring and grafted wounds with and without hypertrophic scarring.100 Such water loss results in extreme dryness of the skin and perhaps is another cause of patients’ common complaints of itching.100
A burn injury is sudden and can be quite frightening and overwhelming. Often, its psychological effects are not felt until after discharge from the hospital. Patients and their families must be instructed early and encouraged regularly about the extensive time involved and the commitment to often unforgiving treatment regimens required for good results. Goals regarding function should be set high and should be set in conjunction with the patient. If the therapist expects less, the patient also will expect less.
Many patients and their family members benefit from one-to-one counseling and support groups following a burn injury. Burn facilities frequently offer monthly parent and burn survivor support groups. Online support groups and chat rooms can also be found. The Phoenix Society (2153 Wealthy Street SE, #215, East Grand Rapids, MI 49506, 800-888-BURN), a nonprofit burn support organization, offers many programs such as school reentry, peer support, annual World Burn Congress, online resource center, and scholarships for burn survivor students.
Rehabilitation of the burned hand begins immediately following injury. Early therapy by a skilled clinician is essential to maximizing the functional outcome and cosmesis of the hand. Therapists must have a good understanding of the anatomy and kinesiology of the hand and phases of wound healing, specifically scar maturation, in order to adequately treat a burn injury. Further research is necessary to identify best practices for the treatment of burned hands.
1. American Burn Association. Appendix B to hospital resources document: Guidelines for service standards and severity classifications in the treatment of burn injury. Bull Am Coll Surg. 1984;69:24–28.
2. Lund CC, Browder NC. The estimation of areas of burns. Surg Gynecol Obstet. 1944;79:352–358.
3. Rossiter ND, Chapman P, Haywood IA. How big is a hand? Burns. 1996;22:230–231.
4. Anzarut A, Chen M, Shankowsky H, Tredget EE. Quality-of-life and outcome predictors following massive burn injury. Plast Reconst Surg. 2005;116:791–797.
5. Committee on Trauma, American College of Surgeons. American Burn Association (ABA) Criteria for Patient Transfer to Burn Unit. In: Guidelines for the Operations of Burn Units: Resources for Optimal Care of the Injured Patients. Chicago: American Burn Association; 1999:55–62.
6. Engrav LH, Dutcher KA, Nakamura DY. Rating burn impairment. Clin Plast Surg. 1992;19:569–598.
7. Pliskin NH, Meyer GJ, Dolske MC, et al. Neuropsychiatric aspects of electrical injury. Ann NY Acad Sci. 1994;720:219–223.
8. O’Brien L, Pandit A. Silicon gel sheeting for preventing and treating hypertrophic and keloid scars (Review). Cochrane Database Syst Rev. 2006;2:CD003826.
9. Linares HA. Pathophysiology of the burn scar. In: Herndon DN, ed. Total Burn Care. London: WB Saunders; 1996:383–397.
10. Rockwell WB, Cohen IK, Ehrlich HP. Keloids and hypertrophic scars: a comprehensive review. Plast Reconstr Surg. 1989;84:827–837.
11. Polo M, Ko F, Busillo F, Cruse CW, et al. The 1997 Moyer award: cytokine production in patients with hypertrophic burn scars. J Burn Care Rehabil. 1997;18:477–482.
12. Widgerow AD, Chait LA, Stals R, Stals B. New innovations in scar management. Aeth Plast Surg. 2000;24:227–234.
13. Deitch EA, Wheelahan TM, Rose MP, et al. Hypertrophic burn scars: analysis of variables. J Trauma. 1983;23:895–898.
14. Smith CJ, Smith JC, Finn MC. The possible role of mast cells (allergy) in the production of keloid and hypertrophic scarring. J Burn Care Rehabil. 1997;8:126–131.
15. Richard R, DerSarkisian D, Miller SF, et al. Directional variance in skin movement. J Burn Care Rehabil. 1999;20:259–264.
16. Meyer M, McGrouther DA. A study relating wound tension to scar morphology in the pre-sternal scar using Langers technique. Br J Plast Surg. 1991;44:291–294.
17. Sheridan RL, Baryza MJ, Pessina MA, et al. Acute hand burns in children: management and long-term outcome based on a 10-year experience with 698 injured hands. Ann Surg. 1999;229:558–564.
18. Sheridan RL, Hurley J, Smith MA, et al. The acutely burned hand: management and outcome based on a ten-year experience with 1047 acute hand burns. J Trauma. 1995;38:406–411.
19. Current Concepts and Approaches to Wound Healing: Wound Healing and Rehabilitation. Baltimore: American Burn Association Course; 1991.
20. Blakeney PE, Fauerbach JA, Meyer WJ III, Thomas CR. Pyschosocial recovery and reintegration of patients with burn injuries. In: Herndon D, ed. Total Burn Care. London: WB Sanders; 2002:629–640.
21. Whitehead C, Serghiou M. A 12-year comparison of common therapeutic interventions in the burn unit. J Burn Care Res. 2009;30:281–287.
22. Richard RL, Staley MJ. Burn patient evaluation and treatment planning. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practice. Philadelphia: F.A. Davis; 1994:242–321.
23. Barillo DJ, Harvey KD, Hobbs CL, et al. Prospective outcome analysis for the surgical and rehabilitative management of burns to the hands. Plast Reconst Surg. 1997;100:1442–1451.
24. Lund T. The 1999 Everett Idris Evans memorial lecture: edema following thermal injury—an update. J Burn Care Rehabil. 1999;20:445–452.
25. Lund T, Onarheim H, Wiig H, et al. Mechanisms behind increased dermal inhibition pressure in acute burn edema. Am J Physiol. 1989;256:H940–H948.
26. Witte CL, Witte MH, DuMont AE. Significance of protein in edema fluid. Lymphology. 1971;4:29–31.
27. Leung KS, Sher A, Clark JA, et al. Microcirculation in hypertrophic scars after burn injury. J Burn Care Rehabil. 1989;10:436–444.
28. Demling RH, Mazess RB, Witt RM, et al. The study of burn wound edema using dichromatic absorptiometry. J Trauma. 1978;18:124–128.
29. Apfel LM, Irwin CP, Staley MJ, et al. Approaches to positioning the burn patient. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practice. Philadelphia: FA Davis; 1994:221–241.
30. Howell JW. Management of the burned hand. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practice. Philadelphia: FA Davis; 1994:531–575.
31. Howell JW. Management of the burned hand for the nonspecialized clinician. Phys Ther. 1989;69:1077–1090.
32. Puddicombe BE, Nardone MA. Rehabilitation of the burned hand. Hand Clin. 1990;6:281–292.
33. Brown HC. Current concepts of burn pathology and mechanisms of deformity in the burned hand. Orthop Clin North Am. 1973;4:987–989.
34. Waldbillig A. The adequacy of escharotomy in the pediatric burn patient. Proc Am Burn Assoc. 1989;21:196.
35. Hildebrant W, Herrmann J, Stegemann J. Vascular adjustment and fluid reabsorption in the human forearm during elevation. Eur J App Physiol. 1993;66:397–400.
36. Villeco J, Mackin E, Hunter J. Edema: therapist’s management. In: Hunter J, Mackin E, Callahan A, eds. Rehabilitation of the Hand. 5th ed St. Louis: Mosby; 2002:899–913.
37. Tilley W, McMahon S, Shukalak B. Rehabilitation of the burned upper extremity. Hand Clin. 2000;16:303–318.
38. Rivers L, Solem LD, Ahrenholz DH. Improved management of post-burn edema in the upper extremity using a foam elevation wedge. Proceedings of the American Burn Association Meeting, Baltimore, MD, 1991.
39. Helm P. Neuromuscular considerations. In: Fisher SV, Helm PA, eds. Comprehensive Rehabilitation of Burns. Baltimore: Williams & Wilkins; 1984:235–241.
40. Wadsworth TG, Williams JR. Cubital tunnel external compression syndrome. Br Med J. 1973;1:662–666.
41. Daugherty MB, Carr-Collins JA. Splinting technique for the burn patient. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practice. Philadelphia: F.A. Davis; 1994:242–321.
42. Richard R, Staley M, Miller S, Warden G. To splint or not to splint—past philosophy and present practice: part I. J Burn Care Rehabil. 1996;17:444–453.
43. Richard R, Staley M, Miller S, Warden G. To splint or not to splint—past philosophy and present practice: Part II. J Burn Care Rehabil. 1997;18:64–71.
44. Richard R, Staley M, Miller S, Warden G. To splint or not to splint—past philosophy and current practice: Part III. J Burn Care Rehabil. 1997;18:251–255.
45. Leman CJ. Splints and accessories following burn reconstruction. Clin Plast Surg. 1992;19:721–731.
46. Helm PA, Kevorkian CG, Lushbaugh M, et al. Burn injury: rehabilitation management in 1982. Arch Phys Med Rehabil. 1982;63:6–16.
47. Malick MH. Management of the severely burned patient. Br J Occ Ther. 1975;38:76–80.
48. Richard R, Ward RS. Splinting strategies and controversies. J Burn Care Rehabil. 2005;26:392–396.
49. Boswick JA. Rehabilitation of the hand. Clin Orthop Relat Res. 1974;104:162–174.
50. Richard R, Staley M, Daugherty MB, et al. The wide variety of designs for dorsal hand burn splints. J Burn Care Rehabil. 1994;15:275–280.
51. Richard R, Baryza MJ, Carr JA, et al. Burn rehabilitation and research: proceedings of a consensus summit. J Burn Care Rehabil. 2009;30:543–573.
52. Humphrey C, Richard RL, Staley MJ. Soft tissue management and exercise. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practices. Philadelphia: FA Davis; 1994:324–360.
53. Feldman ME, Evans J. Early management of the burned hand. O SJ J Craniofac Surg. 2008;19:942–950.
54. Birchenough SA, Gampper TJ, Morgan RF. Special considerations in the management of pediatric upper extremity and hand burns. J Craniofac Surg. 2008;19:933–941.
55. Beasley RW. Secondary repair of burned hands. Clin Plast Surg. 1981;8:141–162.
56. Clark R. Cutaneous tissue repair: basic biologic considerations. Int J Am Acad Dermatol. 1985;13:701–725.
57. Hunt TK. Spontaneous healing of burns. In: Fundamentals of Wound Management in Surgery: Selected Issues. South Plainfield, NJ: Chirurgecom; 1977.
58. Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. Clin J Pain. 2000;16:244–250.
59. Hunt TK, Sato R. Early excision of full-thickness hand and digit burns: factors affecting morbidity. J Trauma. 1982;22:414–419.
60. Saffle JR, Schnebly WA. Burn wound care. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practice. Philadelphia: FA Davis; 1994:119–176.
61. Hatler BD, Harris L. Outpatient Management of Large and Small Burns: Occupational Therapy Aspects, Wound Care and Rehabilitation Post-graduate Course, American Burn Association Conference.
62. Dutcher K, Johnson C. Neuromuscular and musculoskeletal complications. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practices. Philadelphia: FA Davis; 1994:576–602.
63. Head M. Outpatient Management of Large and Small Burns: Physical Therapy Aspects, Wound Care And Rehabilitation Post-graduate Course, American Burn Association Meeting, Orlando, 1994.
64. Mlakar JM, Dougherty WR. Reconstruction of the burned hand. In: Herndon D, ed. Total Burn Care. Philadelphia: W.B. Saunders; 2002:628–655.
65. Pullium GF. Splinting and positioning. In: Fisher SV, Helm PA, eds. Comprehensive Rehabilitation of Burns. Baltimore: Williams & Wilkins; 1984:64–95.
66. Richard R, Jonhson R, Miller S. A compendium of customized burn splint designs. J Burn Care Rehabil. 2003;24:S142–S147.
67. Serghiou MA, Burke Evans E, Ott S, et al. Comprehensive rehabilitation of the burn patient. In: Herndon D, ed. Total Burn Care. Philadelphia: WB Saunders; 2002:563–592.
68. Anzarut A, Olson J, Singh P, et al. The effectiveness of pressure garment therapy for the prevention of abnormal scarring after burn injury: a meta-analysis. J Plast Reconstr Aesth Surg. 2009;62:77–84.
69. Compton CC. Skin regenerated from cultured epithelial autografts on full-thickness burns from 6 days to 5 years after grafting. Lab Invest. 1989;60:600–612.
70. Garner WL. Epidermal regulation of dermal fibroblast activity. Plast Reconstr Surg. 1998;102:135–139.
71. Sheridan RL, Tompkins RG. Alternative wound coverings. In: Herndon D, ed. Total Burn Care. Philadelphia: WB Saunders; 2002:212–218.
72. Burk JF. Observations on the development and clinical use of artificial skin: an attempt to employ regeneration rather than scar formation in wound healing. Jpn J Surg. 1987;17:431–438.
73. Integratm Dermal Regeneration Template. Available at www.integra-ls.com/home/search.aspx?qry=burns.
74. Kowalske K. Outcome assessment after hand burns. Hand Clin. 2009;25:557–561.
75. Berry RB, Tan OT, Cooke ED, et al. Transcutaneous oxygen tension as an index of maturity in hypertrophic scars treated by compression. Br J Plast Surg. 1985;38:163–173.
76. Hosada G, Holloway G, Heimbach D. Laser Doppler flowmetry for early detection of hypertrophic scar (abstract). American Burn Association Meeting, Chicago, 1986.
77. Kelley SF, Ehrlich HP. Characteristics of blood flow patterns in hypertrophic scar (abstract). American Burn Association Meeting, New Orleans, 1989.
78. Esposito G, Ziccardi P, Scioli M, et al. The use of a modified tonometer in burn scar therapy. J Burn Care Rehabil. 1990;11:86–90.
79. Fong SS, Hung LK, Cheng JC. The cutometer and ultrasonography in the assessment of postburn hypertrophic scar: a preliminary study. Burns Suppl. 1997;I:S12–S18.
80. Katz BE. Silastic gel sheeting is found to be effective in scar therapy. Cosmetic Dermatol. 1992;June(5):32–34.
81. Spann K, Mileski WJ, Atiles L, et al. The 1996 Clinical Research Award: use of a pneumatonometer in burn scar assessment. J Burn Care Rehabil. 1996;17:515–517.
82. Bartell TH, Monafo WW, Mustoe TA. A new instrument for serial measurements of elasticity in hypertrophic scar. J Burn Care Rehabil. 1988;9:657–660.
83. Clark JA, Cheng C, Leung KS. Mechanical properties of normal skin and hypertropic scars. Burns. 1996;22:447–450.
84. Boyce ST, Supp AP, Wickett RR, et al. Assessment with the dermal torque meter of skin pliability after treatment of burns with cultured skin. J Burn Care Rehabil. 2000;21:55–63.
85. Hambleton J, Shakespeare PG, Pratt BJ. The progress of hypertrophic scars monitored by ultrasound measurements of thickness. Burns. 1992;18:301–307.
86. Sawada Y. A method of recording and objective assessment of hypertrophic burn scars. Burns. 1994;20:76–78.
87. McHugh AA, Fowlkes BJ, Maevsky EI, et al. Biomechanical alterations in normal skin and hypertrophic scar after thermal injury. J Burn Care Rehabil. 1997;18:104–108.
88. Crowe JM, Simpson K, Johnson W, et al. Reliability of photographic analysis in determining change in scar appearance. J Burn Care Rehabil. 1998;19:183–186.
89. Sullivan T, Smith J, Kermode J, et al. Rating the burn scar. J Burn Care Rehabil. 1990;11:256–260.
90. Yeong EK, Mann R, Engrav LH, et al. Improved burn scar assessment through the use of a new scar-rating scale. J Burn Care Rehabil. 1997;18:353–355.
91. Nedelec B, Shankowsky HA, Tredget EE. Rating and resolving hypertrophic scar: a comparison of the Vancouver Scar Scale and Scar Volume. J Burn Care Rehabil. 2000;21:205–212.
92. Baryza MJ, Baryza GA. The Vancouver Scar Scale: an administration tool and its interrater reliability. J Burn Care Rehabil. 1995;16:535–538.
93. Forbes-Duchart L, Marshall S, Strock A, et al. Determination of inter-rater reliability in pediatric burn scar assessment using a modified version of the Vancouver Scar Scale. J Burn Care Rehabil. 2007;28:460–467.
94. Lowell M, Pirc P, Ward S, et al. Effect of 3M Coban Self-Adherent Wraps on edema and function of the burned hand: a case study. J Burn Care Rehabil. 2003;24:253–258.
95. Nadel E. Rehabilitation of the burned hand. Top Acute Care Trauma Rehabil. 1987;1:50–61.
96. Staley MJ, Richard RL. Scar management. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practice. Philadelphia: F.A. Davis; 1994:381–415.
97. Cyriax JH. Clinical application of massage. In: Licht S, ed. Massage, Manipulation, and Traction. New Haven: Elizabeth Licht Publisher; 1960.
98. Patino O, Novick C, Merlo A, et al. Massage in hypertrophic scars. J Burn Care Rehabil. 1999;20:268–271.
99. Cadwallader C, Helm P. Sweat gland distribution in healed severe burns: quantitative topical distribution and qualitative function (abstract). American Burn Association Meeting, San Francisco, 1984.
100. Carnes R, Sollecito W, Salisbury R. Evaporative water loss from healed burn wounds. J Burn Care Rehabil. 1981;2:2379–2380.
101. Field T, Peck M 2nd, Hernandez-Reif M, et al. Postburn itching, pain, and psychological symptoms are reduced with massage therapy. J Burn Care Rehabil. 2000;21:189–193.
102. Morien A, Garrison D, Smith NK. Range of motion improves after massage in children with burns: a pilot study. J Bodyw Mov Ther. 2008;12:67–71.
103. Head MD. Wound and skin care. In: Fisher SV, Helm PA, eds. Comprehensive Rehabilitation of Burns. Baltimore: Williams & Wilkins; 1984:173.
104. Cronan T, Hammond J, Ward CG. The value of isokinetic exercise and testing in burn rehabilitation and determination of back-to-work status. J Burn Care Rehabil. 1990;11:224–227.
105. Johnson MA, Polgor J, Weightman D. Data on the distribution of fiber types in 36 human muscles: an autopsy study. J Neurol Sci. 1977;18:111–129.
106. Ibebunjo C, Martyn JAC. Muscle dysfunction after burn and immobilization: a comparison. J Burn Care Rehabil. 1998.36.
107. Yasuhara S, Kanakubo E, Perez ME, et al. The 1999 Moyer Award: burn injury induces skeletal muscle apoptosis and activation of caspase pathways in rats. J Burn Care Rehabil. 1999;20:462–467.
108. Huang TT, Blackwell SJ, Lewis SR. Ten years of experience in managing patients with burn contractures of axilla, elbow, wrist, and knee joints. Plast Reconstr Surg. 1978;61:71–76.
109. Larson D, Abston S, Evans EB. Splints and traction. In: Polk H, Stone HH, eds. Contemporary Burn Management. Boston: Little, Brown; 1971:488–489.
110. Reid WH. Hypertrophic scarring and pressure therapy. Burns. 1987;13:29–32.
111. Atiyeh BS. Nonsurgical management of hypertrophic scars: evidence-based therapies, standard practices, and emerging methods. Aesth Plast Surg. 2007;31:468–492.
112. Kirscher CW, Shetlar CW. Microvasculature in hypertrophic scars and the effects of pressure. J Trauma. 1979;19:757–764.
113. Sloan DF, Brown RD, Wells CH, et al. Tissue gases in human hypertrophic burn scars. Plast Reconstr Surg. 1978;61:431–436.
114. Jensen LL, Parshley PF. Postburn contractures: histology and effects of pressure treatment. J Burn Care Rehabil. 1984;5:119–123.
115. Peacock EE Jr. Wound Repair. Philadelphia: WB Saunders; 1984.
116. Anzarut A, Olson J, Singh P, et al. The effectiveness of pressure garment therapy for the prevention of abnormal scarring after burn injury: a meta-analysis. J Plast Reconstr Aesthet Surg. 2009;62:77–84.
117. Ripper S, Renneber B, Landmann C, et al. Adherence to pressure garment therapy in adult burn patients. Burns. 2009;35:657–664.
118. Stewart R, Bhagwanjee A, Mbakaza Y, et al. Pressure garment adherence in adult patients with burn injuries: an analysis of patient and clinician perceptions. Am J Occup Ther. 2000;54:598–606.
119. Bruster J, Pullium G. Gradient pressure. Am J Occup Ther. 1983;37:485–488.
120. Dewey DW, Richard RL, Hedman TL, et al. A review of compression glove modifications to enhance functional grip: a case series. J Burn Care Rehabil. 2008;28:888–891.
121. O’Brien KA, Weinstock-Zlotnick G, Sanchez J, et al. Comparison of positive pressure gloves on hand use in uninjured persons. J Burn Care and Rehabil. 2005;26:363–368.
122. Rock KM, Mikat RP, Foster C. The effects of gloves on grip strength and three-point pinch. J Hand Ther. 2001;14:286–290.
123. Stella M, Castagnoli C, Gangemi EN. Postburn scars: an update. Int J Lower Ext Wounds. 2008;7:176–181.
124. Berman B, Perez OA, Konda S, et al. A review of the biologic effects, clinical efficacy, and safety of silicone elastomer sheeting for hypertrophic and keloid scar treatment and management. Dermatol Surg. 2007;33:1291–1303.
125. Berman B, Viera M, Sadegh A, et al. Prevention and management of hypertrophic scars and keloids after burns in children. J Craniofas Surg. 2008;19:989–1006.
126. Meyers-Paal R, Blakeney P, Robert R, et al. Physical and psychologic rehabilitation outcomes for pediatric patients who suffer 80% or more TBSA, 70% or more third-degree burns. J Burn Care Rehabil. 2000;21:43–49.
127. Feldman A, Thomson J, MacMillan B. The molded silicone shoe in the prevention of contractures involving the burn-injured foot. Burns. 1974;1:83–95.
128. Carney SA, Cason CG, Gowar JP, et al. Cica-Care gel sheeting in the management of hypertrophic scarring. Burns. 1994;20:163–167.
129. Malik MH, Carr JA. Flexible elastomer molds in burn scar control. Am J Occup Ther. 1980;34:603–608.
130. Perkins K, Davey BR, Wallis K. Current materials and techniques used in a burn scar management programme. Burns. 1987;13:406–410.
131. de Oliveira GV, Nunes TA, Magna LA, et al. Silicone versus nonsilicone gel dressings: a controlled trial. Dermatol Surg. 2001;27:721–726.
132. Baum TM, Busuito MJ. Use of a glycerin-based gel sheeting in scar management. J Prevent Heal. 1998;11:40–43.
133. Wessling N, et al. Evidence that a silicone wound dressing increases range of motion in limbs after contractures (abstract). American Burn Association Meeting, Orlando, 1985.
134. Ahn ST, Monafo WW, Mustoe TA. Topical silicone gel for the prevention and treatment of hypertrophic scar. Arch Surg. 1991;126:499–504.
135. Ahn ST, Monafo WW, Mustoe TA. Topical silicone gel sheet: a new treatment for hypertrophic scars. Surgery. 1991;126:499–504.
136. Mustoe TA, Cooter RD, Gold MH, et al. International clinical recommendations on scar management. Plast Reconstr Surg. 2002;110(2):560–571.
137. Mustoe TA. Evolution of silicone therapy and mechanism of action in scar management. Aest Plast Surg. 2008;32:82–92.
138. Musgrave MA, Umraw N, Fish JS, et al. The effect of silicone gel sheets on perfusion of hypertrophic burn scars. J Burn Care Rehabil. 2002;23:208–214.
139. Richard R, Chapman T, Dougherty M, et al. An Atlas and Compendium of Burn Splints. 2005.
140. Bennett GB, Heim P, Purdue GF, et al. Serial casting: a method for treating burn contractures. J Burn Care Rehabil. 1989;10:543–545.
141. Tribuzi SM. Serial plaster splinting. In: Hunter JM, ed., et al. Rehabilitation of the Hand. St Louis: Mosby; 1990:1828–1838.
142. Rivers EA. Management of hypertrophic scarring. In: Fisher SV, Helm PA, eds. Comprehensive Rehabilitation of Burns. Baltimore: Williams & Wilkins; 1984.
143. Ridgway CL, Daugherty MB, Warden GD. Serial casting as a technique to correct burn scar contractures. A case report. J Burn Care Rehabil. 1991;12:67–72.
144. Harris L, et al. Serial casting and its efficacy in the treatment of the burned hand (abstract). American Burn Association Meeting, Cincinnati, 1993.
145. Flesch P. Casting the young and the restless (abstract). American Burn Association Meeting, Orlando, 1985.
146. Head M, Helm P. Paraffin and sustained stretching in the treatment of burn contractures. Burns. 1977;4:136–139.
147. Gross J, Stafford S. Modified method for application of paraffin wax for treatment of burn scar. J Burn Care Rehabil. 1984;5:394.
148. Johnson CL. Physical therapists as scar modifiers. Phys Ther. 1984;64:1383–1387.
149. Covey MH, Dutcher K, Marvin JA, Heimbach DM. Efficacy of continuous passive motion (CPM) devices with hand burns. J Burn Care Rehabil. 1988;9:397–400.
150. Harris L, Way-Nee S, Tredget E. Continuous passive motion in the burned hand (abstract). American Burn Association Meeting, Orlando, 1994.
151. Ward SR. Use of physical agents in burn care. In: Richard RL, Staley MJ, eds. Burn Care and Rehabilitation Principles and Practice. Philadelphia: F.A. Davis; 1994:419–446.
152. Apfel L, Wachtel TL, Frank DH, et al. Functional electrical stimulation in intrinsic/extrinsic imbalanced burned hands. J Burn Care Rehabil. 1987;8:97–102.
153. Bierman W. Ultrasound in the treatment of scars. Arch Phys Med Rehabil. 1954;35:209–214.
154. Ward RS, Hayes-Lundy C, Reddy R, et al. Evaluation of topical therapeutic ultrasound to improve response to physical therapy and lessen scar contracture following burn injury. J Burn Care Rehabil. 1994;15:74–79.
155. Nussbaum E. The influence of ultrasound on healing tissues. J Hand Therapy. 1998;11:140–147.
156. Wright ET, Hasse KH. Keloids and ultrasound. Arch Phys Med Rehabil. 1971;52:280–281.
157. Langley PL. Iontophoresis to aid in releasing tendon adhesions: suggestions from the field. Phys Ther. 1984;64(9):1395.
158. Tannenbaum M. Iodine iontophoresis in reducing scar tissue. Phys Ther. 1980;60:792–794.
159. Shigeki S, Murakami T, Yata N, Ikuta Y. Treatment of keloid and hypertrophic scars by iontopheretic transdermal delivery of tranilast. Scand J Plast Reconstr Surg Hand Surg. 1997;31:151–158.
160. Yamada H, Tajima S, Nishikawa T, et al. Tranilast, a selective inhibitor of collagen synthesis in human skin fibroblasts. J Biochem. 1994;116(4):892–897.
161. Schneider JC, Holavanahalli R, Helm P, et al. Contractures in burn injury part II: investigating joints of the hand. J Burn Care Rehabil. 2008;29:606–613.
162. Grishkevich VM. Surgical treatment of postburn boutonniere deformity. Plast Reconst Surg. 1996;97:126–132.
163. Schwarz R. Management of postburn contractures of the upper extremity. J Burn Care Rehabil. 2007;28:212–219.
164. Rico AA, Holguin PH, Vecilla LR, et al. Tendon reconstruction for postburn boutonniere deformity. J Hand Surg. 1992;17A:862–867.
165. Stern PJ, MacMillan BG. Reconstruction of the burned thumb by metacarpal lengthening. Burns. 1983;10:123–130.
166. Torres-Gray D, Greene S. Rehabilitation of the burned hand. Techni Hand Upper Extremity Surg. 1998;2:284–292.
167. Chen MA, Davidson TM. Scar management: prevention and treatment strategies. Facial Plast Surg. 2005;13:242–247.
168. Hwang YF, Chen CL, Chen-Sea MJ. Effectiveness of web space inserts for post burn dorsal slant. J Burn Care Res. 2008;29(5):768–772.
169. Salisbury RE. Reconstruction of the burned hand. Clin Plast Surg. 2000;27:65–69.
170. Simpson RL, Flaherty ME. The burned small finger. Burn Rehabil Reconst. 1992;19:673–682.
171. Zeller J, Sturm G, Cruse CW. Patients with burns are successful in work hardening programs. J Burn Care Rehabil. 1993;14:189–196.
172. Helm P, Walker SC, Peyton SA. Return to work following hand burns. Arch Phys Med Rehabil. 1986;67:297–298.
173. Helm P, Walker SC. Return to work after burn injury. J Burn Care Rehabil. 1992;13:53–57.
174. Saffle JR, Tuohig GM, Sullivan JJ, et al. Return to work as a measure of outcome in adults hospitalized for acute burn treatment. J Burn Care Rehabil. 1996;17:353–361.
175. Wrigley M, Trotman BK, Dimick A, Fine PR. Factors relating to the return to work after burn injury. J Burn Care Rehabil. 1995;16:445–450.
176. Roberts L, et al. Relating hand strength recovery to living skills acquisition in the burn injured child (abstract). American Burn Association Meeting, Salt Lake City, 1992.
177. Mannerfelt L. Evaluation of functional sensation of skin grafts in the hand area. Br J Plast Surg. 1967;15:136–154.
178. Ponten B. Grafted skin: observation on innervation and other qualities. Acta Chir Scand. 1960;257(Suppl):1–78.
179. Dimick AR. Pathophysiology. In: Fisher SV, Helm PA, eds. Comprehensive Rehabilitation of Burns. Baltimore: Williams & Wilkins; 1984:15–27.
180. Fisher S, Ahrenholz DH, Solem LD. Poorly recognized sequelae of thermal hand injuries (abstract). American Burn Association Meeting, San Francisco, 1984.
181. Apfel L, Sunmstegard TA, Wachtel TL, et al. Functional hand assessment after enzymatic debridement and early autografting. J Burn Care Rehabil. 1984;5:438–445.
182. Lamke LO, Liljedahl SO. Evaporative water loss from burns, grafts, and donor sites. Scand Plast Reconstr Surg. 1971;5:17–22.