▪ Any orthosis has primary and secondary effects on the joint(s) to which it is applied as well as on adjacent joints.
▪ Basic principles of mechanics related to the hand and materials mechanics must be considered in the fabrication and application of a mobilization orthosis.
Basic principles of soft tissue mechanics, hand biomechanics, and materials properties are relevant to hand therapy clinical practice and provide a background for understanding the principles of orthotics fabrication.1-6 Dr. Paul Brand pioneered the idea of a biomedical engineer as a valued member of the hand surgery and therapy team. He championed this concept in hand centers in both India and Louisiana. He established the New Life Center in India, and the Rehabilitation Research Laboratory at the U.S. Public Health Service National Hansen’s Disease Hospital, in Carville, Louisiana. Brand and the Rehabilitation Research Laboratory he created have been responsible for many of the therapy techniques used in hand clinics today. Brand is known to some as the father of hand therapy and hand therapy centers.7-12 A dedication to him can be found in the first edition of this textbook.13 His work, “The Forces of Dynamic Splinting: Ten Questions Before Applying a Splint to a Hand,” is revised and updated in this chapter, closely following his original descriptions of techniques14 that continue to be as relevant today as when he first wrote of them.
Fabrication of an orthosis for the hand and upper extremity is a science as well as an art. The science of orthoses has advanced significantly, requiring comprehensive knowledge of biomechanics. By its very presence on the hand, wrist, and/or forearm, an orthosis must do no harm. It is inhibiting the free movement and use of the hand and is justified only if the benefit of the orthosis compensates for the potential harm of restriction.
A mobilization orthosis, commonly referred to as a dynamic splint, is one that achieves its effect through movement and force. It is a form of controlled mobilization. It may use forces generated by the patient’s own muscles or externally imposed by rubber bands or springs. Whenever passive movement is used, there is a danger that an eager surgeon or therapist will use too much force. The unintended result may be that the patient has pain and edema, and a short-term gain in motion is followed by long-term stiffness. Active exercise and work-related movements are controlled by the patient, who usually keeps within the limits of pain, which is protective of overstress of tissues. During active movement, hand reflexes and coordination, which are essential to normal hand function, are maintained or restored. Any orthosis should allow or enhance other movement where needed and restrict only what is necessary. The orthosis should only be used for the duration needed to achieve its goal.
Orthoses are needed when exercise and positioning are not enough to achieve satisfactory results and movement must be assisted, replaced, or restricted. Sometimes an orthosis may be worn only at night to enable full active movement during the day. It may be critical that an orthosis be worn during the day to control active movement when the hand is used, whereas if an orthosis is worn for correction of tissue contractures, it may be needed for 24 hours. We first must realize that the orthosis may have the same bad results as manipulation unless surgeons and therapists utilize stern discipline to ensure that the forces they impose are well controlled. Too little force may do no good; too much may do harm. So, how much is just right?
We have to measure and calculate. It is not enough to say, “rubber band traction” or “not too much force” or “be gentle.” In terms of force on the hand, we must use a unit of measure, e.g., grams of force. Then we can begin to compare results.15 Most books and articles about orthoses are concerned with design, not measurement of force. Paul Brand identified 10 basic questions that each therapist considers with each orthosis application after defining the objective of the mobilization orthosis for the specific joint(s) to be mobilized or modified. The 10 questions to ask are:
10. Warned by what signs?14
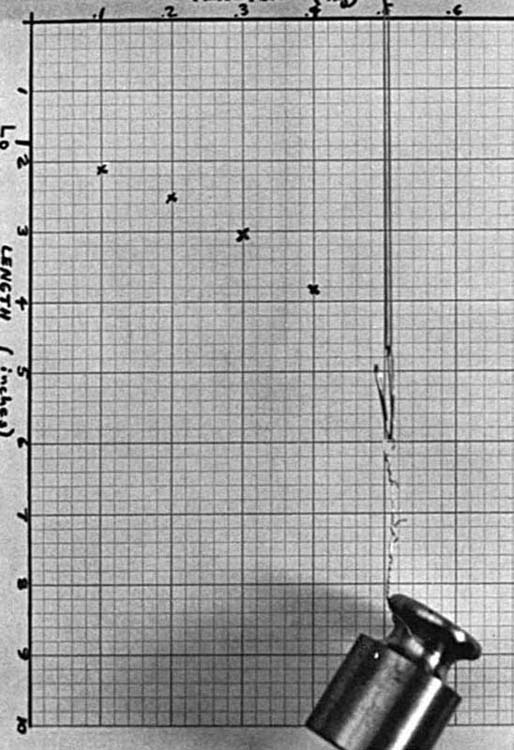
In most dynamic mobilization hand orthoses, the force is provided by rubber bands or steel springs. Some companies have springs that are calibrated for tension, specifically for use with dynamic hand orthoses. Rubber bands must be replaced more frequently, because rubber changes its length-tension curve with age and with constant stretch. Therapists or orthotists should purchase their rubber bands in batches that appear uniform and then test them for tension before use. A simple stress-strain diagram may be quickly prepared for each batch to be used as a guide for future use. A weight or series of weights can be used to extend the band to a measurable distance for comparison of strengths. One is hung from the rubber band, using a paper clip, while the other end is suspended from a rod. The length the rubber band extends with the weight can be measured with a standard ruler or read on a sheet of graph paper divided into different units. For a simplified measurement, one weight (e.g., 300 g) can be used to find similar bands that extend to equal length with the weight applied. By using standard 100-g, 200-g, 300-g, 400-g, and 500-g weights and measuring the lengths of the bands at these weights, one can understand the elastic properties of the rubber bands. The length of the band as it changes with each of those five weights hooked one by one onto the rubber band can be graphed as a curve of its stress versus strain. Figure 123-1 shows the curve for one of our rubber bands. If a dynamic/mobilization orthosis requires a pull of 200 g from an outrigger 6 cm from the finger, a quick glance across our graphs will show which band we should use and how far we should stretch it. If one is using a spring steel wire, this may be calibrated in advance with a similar stress-strain curve to select and match the elastic capacity of springs.
In most dynamic/mobilization orthoses, there will be a range of movement that will result in lengthening and shortening of the rubber band or spring. For example, in Harold Kleinert’s method following primary suture of a severed flexor tendon, he used a rubber band from the fingernail to a wristband.15 The purpose of this is to hold the finger flexed when it is at rest and to allow the patient to extend the finger against the tension of the rubber band by using the extensor muscles. The rubber band should be strong enough to pull the finger back into flexion without the use of the flexor muscle–tendon unit. For such a purpose, use a rubber band that is 5 cm long at rest (no tension) that would have a tension of 200 to 300 g at 15-cm length.
Long, thin bands elongate more than short, thick bands. Rubber bands should be selected that will allow the strength (tension) and elongation (length) needed for the particular orthosis being used. At the time force is applied, we can check the tension of the rubber band with a strain gauge. A Haldex gauge is often used, as it has been found to be accurate and repeatable by rehabilitation research engineers2 (Fig. 123-2). The hand is placed in the orthosis with the rubber band in the position where it will apply traction to the intended finger or joint segment. For determining the actual tension of a band on an orthosis, the length of the rubber band is first measured when it is under tension while in place on the patient. Then the rubber band cuff is slipped off the finger, and the rubber band or spring is again elongated in the same direction and to the same distance. The rubber band can be extended the same distance by pulling it with the arm of the strain gauge at its tip. When the rubber band is extended, any standard ruler can measure length as the force is read on the strain gauge. The force read is the tension being produced by the band or spring through the same range that it will act on the finger. In applying the arm of the strain gauge to the rubber band, care should be taken to keep the arm of the gauge perpendicular to the rubber band being measured, as angulations of the arm to the band can make measurements less precise.
In many cases, the question, “How much force?” has more than one answer. If a finger is to be flexed and extended while the patient wears the orthosis, tension in both positions must be measured at the ends of their arc of movement. For example, rubber band traction may measure 250 g when the finger is extended and 50 g when the finger is flexed. To many surgeons and therapists such figures will be meaningless, because they have not used them before and do not know what 100 g feels like. One can check a tension that “feels right” on the hand and then measure how much tension is there by using a spring scale.2,16 If this seems complicated, a little experience can go a long way to create understanding of what tension is optimal and establish the ability to measure the forces of traction.
Every applied force may be presumed to act on the bones or on the musculoskeletal system. However, it has to act through the surface of the body. (Often, the limits on the amount of force we can use are set more by what the skin can tolerate than by what the joint can accept.) Most forces in a hand orthosis are applied through a sling around a finger, and most are comfortable at the time they are applied. However, as time passes they may become uncomfortable or painful because of ischemia from pressure. This is probably the most common cause of patients discarding an orthosis or becoming “uncooperative.”
Both the ischemia and the pain are caused by pressure, not just by force. Pressure is force divided by area. A given force may be safe if the sling is wide enough, and unsafe if it is too narrow. A good general rule is that if a force is to be applied continuously, it should not result in a continual resting pressure of more than 50 g/cm2, about the same as 35 mm Hg, which is within the margin of safety for long-term pressure on soft tissues.8 Note that 35 mm Hg is higher than actual capillary pressure, but capillaries in normal tissue can withstand higher pressures. Thus, a 200-g pull needs a 4-cm2 area of sling. All of the 4-cm2 area should apply equal pressure to the finger. When in doubt, apply a cuff with given traction for a short period of time and observe the results. If the skin tissue underlying the cuff is red and stays red for longer than 15 minutes, then the tissue has been deprived of blood and the pressure is too high. Pressure is relatively unimportant if it is intermittent. Sustained pressure that reduces blood flow to the skin is what causes discomfort or pain, causes tissue damage, and may lead to skin necrosis.
A special danger from pressure occurs when a sling becomes tilted. Perhaps the finger changes its angle because it is responding to the treatment or simply because the whole orthosis is loose. Now the same applied force acts on only the edge of the sling. The actual effective surface of the sling may now be less than a quarter of what it was, so the pressure is multiplied by four. The slings should be checked during phases of finger opening and closing, especially in the resting position.
The problem of a tilting sling is so serious and so common that Brand never used a sling that could tilt. He covered the area of skin that would be under the sling with an equal area of plaster of Paris, forming a shell covering half the circumference of the digit. When that was set, the force could be applied by a nylon thread passed around the middle of the plaster shell and secured by a small strip of plaster added at just the apex of the curve. Now, if the direction of the pull changes, it does not tilt the plaster shell through which it is applied (Fig. 123-3).
Time is important in two respects: the total time the orthosis is on the hand and the time that the actual force is pressing on the tissues. If the force acts only in certain positions or when certain muscles pull against it, it is intermittent and the question of ischemia may not arise. If all is normal for a trial period, the orthosis may be worn for gradually longer periods. If the objective of the orthosis is to lengthen a scar or to stimulate the development of free loose skin where previously tight skin has limited joint motion, then time has another kind of importance. We sometimes speak of “stretching” skin or scar. Stretch is a passive action that results in the elongation of elastic elements in skin, scar, or connective tissue. Every bit of elongation of tissue that is accomplished by stretch will shorten again when the force is relaxed. When a rubber band is pulled, it becomes longer. It is “stretched.” When the pull is relaxed, it returns to its old length. If it is pulled harder, it may break. It is the same with living tissue. The immediate lengthening of tight skin that is produced by pulling will be lost when it is relaxed. If it is pulled too hard, microscopic ruptures in the tissue result in inflammation and later scar formation. The last state may then be worse than the first.
The true lengthening of any living tissue results from the activity of living cells as they constantly take up and absorb old tissues and lay down new tissues. Old collagen is absorbed; new collagen is laid down in new patterns responsive to new needs. Cells in the skin multiply and proliferate in response to need. Our responsibility is not to try shortcuts by “stretching” or breaking the old tissues but to stimulate the living cells to do the work. We do this by keeping the tissues in a physical state that elicits the need. The cells will then sense the need and will make changes to meet that need.
The best way to lengthen tissues is to keep them constantly in a state of mild tension. Brand termed the technique he described for contracted joints “the inevitability of gradualness” (see Chapter 125). Tissue remodeling requires less tension than most of us use, but it needs to be maintained longer than most of us do. A good test is blanching of the skin. If we pull so hard that the skin is blanched, that may be too much. However, the tension should be maintained for many hours every day, or even for all day. For proximal interphalangeal (PIP) joint contractures, Brand used cylindrical plaster casts reapplied every day to create a mild state of tissue tension and hold the joint in its optimal position until it could be extended further (reset the end of its elastic limits). Theoretically, a good mobilization orthosis that keeps fairly constant tension could work as well as serial plaster casting and involves fewer visits to the therapist, but it is hard to achieve constant tension in an orthosis that allows movement. For tissue remodeling it is ideal to maintain a constant position of tension almost 24 hours a day.
In dealing with stiff joints we have to determine the limiting structures or tissues. If it is decided that the tissues surrounding the joint are tight and inflexible, the patient probably should not be in an orthosis, except for pain or inflammation. The patient should be exercising freely and using the hand. However, if the tissues are free on one side and tight on the other, a corrective orthosis may be of value. Even so, it is good to determine the target tissue.
On the flexor side of a PIP joint, for example, tight skin or connective tissue will probably remodel and lengthen with constant tension. An adherent tendon or volar plate, however, may not respond. A good general test is to pull the finger gently toward extension. If it comes to a slow stop and the skin blanches a little on further attempted movement, this suggests that the skin may be short; the prognosis for improvement with an orthosis is good. If the joint moves freely to a certain point and then stops dead, the prognosis for conservative treatment is poor and an orthosis may be a waste of time.
When one has determined which structure or layer around the joint is in need of lengthening, it is possible to visualize the problem in terms of levers around the axis of the joint. The axis of movement of most joints of the hand is at about the midpoint of the head of the proximal bone. Thus, if the palmar skin of the PIP joint is tight, it may be about 1 cm from the axis of the joint in an adult male. If a sling is placed 3 cm down the finger and hooked to a force of 250 g to pull the finger straight, the leverage will be 3:1, and the skin will experience a tension of 750 g (Fig. 123-4A). If the skin is bowstringing across the joint, it will be farther from the joint axis and will have a longer lever arm. It will be more difficult to provide an effective tension to it without producing pressure effects under the sling. We use the term mechanical advantage to express the ratio between the length of the lever through which force is applied and the length of the lever arm through which the force is delivered. In the case of hand orthoses, this is commonly a number between 2:1 and 5:1. The length of the finger or hand is used to apply the force, and half the thickness of the finger or hand delivers the force. When muscles are moving the fingers from inside the hand, they have very small mechanical advantages because they use levers related to finger thickness to apply their force and have to move levers related to finger length to deliver the force. Thus their ratios are inverted and are commonly 1:5. This is why active exercises are safer than passive movements: They use small leverages and are less likely to do violence to the tissues. It is good to think about this when doing passive movement. After a therapist starts to think in terms of leverages and mechanical advantages, he or she is much less likely to make the mistake of overstressing or understressing the key tissues he or she is trying to modify.
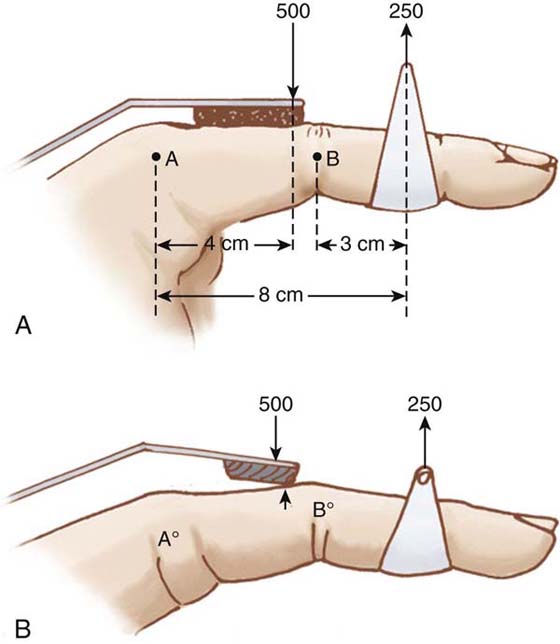
Figure 123-4 A, Diagram of finger subjected to force of 250 g through sling 3 cm from axis, B, of the interphalangeal joint. Proximal segment of the finger is held in flexion by a felt pad, which is 4 cm from axis, A, of MCP joint. This pad receives thrust of 500 g to balance force on the sling; 500 g × 4 cm = 250 g × 8 cm. B, Same finger but because the proximal part of hand was not supported, the whole finger has tilted. Now only the edge of the felt pad presses on the finger, creating high pressure.
“To every action there is an equal and opposite reaction.” Newton knew about this 300 years ago, but we forget it every day. We make a sling to spread the pressure on a finger where we pull, but we forget that the pull on the finger results in a push on the hand. In the reaction, as well as in the primary action, the damage is done most often by pressure rather than by force. Pressure is force divided by area. Our areas are too small, so our pressures are big. Consider a simple and common example. A finger has a PIP joint that is stiff in flexion and a metacarpophalangeal (MCP) joint that is freely mobile. An orthosis is applied to provide traction in a dorsal direction to result in tension on the palmar side of the PIP joint. Using our previous figures, the dorsal pull is 250 g at 3 cm from the axis of the PIP joint, resulting in a 750-g tension on the volar skin.
How much force will be needed as a reaction or stabilizing force to hold the proximal phalanx steady so that the distal force can act only on the PIP joint? If no other force is applied, the finger would hyperextend at the MCP joint, where it is not stiff, and the PIP joint would not benefit. So, how much? Most assume that the reaction force should be the same as the action force; that is, in this example it would be 250 g. If you pull North with 250 g, you can balance it by pushing South with 250 g, right? Wrong. Think about leverages and moments. The PIP joint is stiff and will not move much. The movable joint is the MCP joint. The 250-g force is applied 3 cm distal to the PIP joint, which means it is about 8 cm distal to the MCP joint. Thus, its moment for extending the PIP joint is 750 g-cm, but for the MCP joint it is 250 × 8 g-cm = 2000 g-cm. Now to oppose that moment at the MCP joint, 2000 g-cm are needed in the opposite direction. If the restraint on the dorsal surface is placed 4 cm distal to the MCP joint, 500 g of force will be exerted on the restraining pad to balance the moment of 2000 g-cm: 500 × 4 = 250 × 8. Therefore, it takes double the force on the proximal phalanx to balance the force farther down the finger (see Fig. 123-4A).
Orthosis makers commonly use a flat bar across the proximal phalanges to balance a sling around the finger. A sling spreads the force around the fingers; a flat bar presses only on the dorsum. Furthermore, the volar side of the finger is soft and compliant, whereas the dorsal side is bone and skin. This is why both the pain of an orthosis and the damage from an orthosis are more common from the dorsal reaction bar than from the pull on the volar side.
Recognizing how common dorsal problems are, most therapists take care to use a broad plate and have it padded. However, the breadth of the plate is of no significance if the finger does not remain in total contact with it. The elastic pull on the finger, failing to straighten the PIP joint, may use the reaction bar as a fulcrum and tilt the finger upward and the MCP joint downward. This results in the finger pressing only on the edge of the plate. This results in the force becoming concentrated on a narrow edge: Small area = high pressure = pain, pressure sores, or both (Fig. 123-4B).
The way to prevent this is to think ahead and think in numbers, leverages, moments, and axes. Also, a snug total-contact fit that is molded to the curve of the dorsum of the fingers should be used for the proximal support of the hand, so that the proximal phalanx cannot move in relation to the hand or the orthosis (Fig. 123-5).
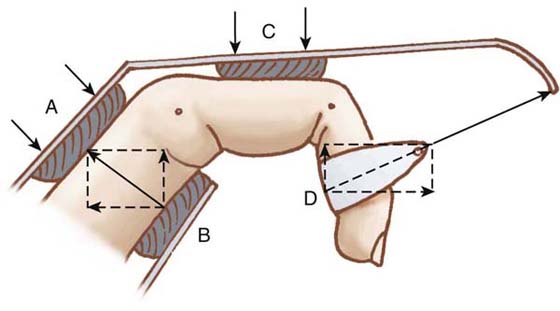
Figure 123-5 Vector diagram to show how both horizontal and vertical forces must be balanced. Whereas in Figure 123-4A the sling was pulling dorsally, here it pulls obliquely because the interphalangeal joint is flexed. Vector diagram of force of sling, D, shows that the horizontal vector is double the dorsal vector. Thus, felt pad C, which balances dorsal force, will not take much force. However, felt pad in palm, B, must be capable of considerable horizontal restraint. It also has dorsal vector, which keeps hand snug against pad C and prevents the tilting shown in Figure 123-4B. Pad A has no force to exert or absorb. It is there to stabilize against pad B and prevent unexpected shifts of position of hand as a whole.
It has already been stated that before an orthosis is recommended, there must be a definition of its specific objective. A typical statement of objective for PIP joint contractures might read “to overcome the flexion contracture of the PIP joints of the index and middle fingers and to restore full passive range of motion.” A plaster orthosis may be judged useful as long as 10 degrees of improvement are being recorded per week. Thermoplastic orthoses do not conform as well as plaster, and for small joints they are best used as retainer orthoses instead of for tissue remodeling.17
The introduction of specific objective criteria that are time-related should ensure that orthoses are discontinued as soon as their job is done or as soon as they have stopped contributing to total improvement. The criteria may be related to muscle strength, re-education, or some other factor. Some way should be found to link the criteria to a scale of numbers that may be periodically checked. Graphs of recorded range of motion improvement inform both the therapist and the patient of the progress achieved and of the value of the objective that has been chosen.
It is good to pause at the beginning and ask oneself what possible harm could come to this hand from use of this orthosis. One example is when too much force is used to mobilize a stiff joint. The result is inflammation of the periarticular tissues followed by swelling and subsequent increased stiffness. Another example is in rheumatoid arthritis when a mobilization/dynamic orthosis applies force distally on the fingers to extend stiff MCP joints (Fig. 123-6).
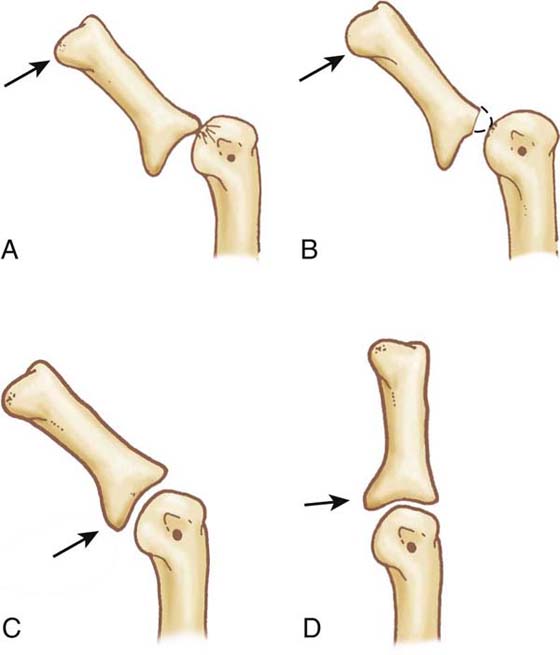
Figure 123-6 In rheumatoid arthritis, if a phalanx begins to sublux into flexion on the metacarpal head and lies in chronic flexion, it is tempting to use passive external force to extend the joint. If the force is applied distally (A) it results in tilting, which in turn results in high stress on the dorsal lip, which becomes absorbed (B). If the external force is applied at the base of the phalanx (C) it tends to restore joint congruence and correct the subluxation (D). (Modified from Brand PW, Hollister A. Clinical Mechanics of the Hand. St Louis: Mosby, 1993.)
Often, there is already some degree of volar subluxation of these joints and a tight volar plate. Distal force will then angulate the finger backward at the MCP joint without true gliding of the joint surfaces. This results in intense pressure on the dorsal lip of the proximal articular surface of the phalanx, which presses into the head of the metacarpal because this is now the fulcrum of this abnormal movement. Finally, the lip wears away, and complete subluxation ensues. This common problem can be prevented only if the therapist and the patient understand how the joint works and are warned never to try to extend a subluxed joint by external force unless the force is applied close to the joint at the base of the finger, where it will stimulate gliding at the joint, not just angulation.
Prevention of stiffness to other joints when an orthosis is used for selected joints consists in the institution of regular range-of-motion exercises to all joints that might be affected.
All members of the team need to be alerted to the signs that might indicate the beginning of actual harm. A graphic record of hand volume and joint temperatures for problem hands is recommended by Brand in the same manner we chart blood pressure and body temperature. To objectively measure edema and help monitor and direct treatment, Brand, Helen Ramsammey, OTR, and his engineers designed, developed, and provided the specifications for the volumeter as we know it today. Eccles, Engler, and Sweat similarly described the water displacement method as an accurate form of measurement.18,19 This method measures increase in fluid volume by a corresponding amount of water displacement.3,7,20-23 The hand volumeter provides a quick record of changes in hand volume (Fig. 123-7).10 Volume increases when patients keep their hands in dependent positions or when the hand becomes inflamed from excessive use of force.
Brand also conceived and investigated ways to use temperature to monitor tissue reaction. He examined cellular changes in skin and soft tissue resulting from various types of pressure.14 As early as the 1970s he used thermographic infrared photography for maps that would change color from cool to warm for each degree change in temperature, and this technology remains invaluable to today’s investigator. He envisioned that once the principles were understood, therapists could use a simple skin thermometer to keep a record of temperature differentials between a given joint and a contralateral normal joint. In 2000, the Paul W. Brand Rehabilitation Research Laboratory was transferred with the hospital to a new location in Baton Rouge, Louisiana, where engineers, therapists, and surgeons continue to work. The current rehabilitation research team has recently compared commercially available infrared digital skin thermometers in a study and found many less expensive instruments to be accurate to needed specifications24 (Fig. 123-8). It is rising temperatures (particularly in the presence of edema) that suggest and document inflammation from too much tissue stress, while no increase in redness and temperature suggests there is no irritation. Lower temperature with swelling suggests inactivity. Low temperatures may also be associated with sympathetic dystrophy. A careful inspection of the surface of the hand and palpation of the hand by the therapist’s fingers (temperature-sensitive dorsal aspect of the fingers) will frequently determine the presence of redness, swelling, or hot spots.
It is very important to consider the patient’s response to treatment and that the patient is part of the rehabilitation team. The patient has been educated and alerted to the potential benefits and problems of any treatment method.25 This is an integral part of the therapist–patient relationship that has to be established if mobilization orthoses are to be successful. The patient’s brain adds up and analyzes a stream of information from skin, joint, and muscle and integrates it with an awareness of personal priorities. The subconscious mind, more flexible and better programmed than any computer, comes up with an evaluation of your orthosis that should be taken seriously by any physician, therapist, or orthosis maker. We may be specialists treating a single limb using scientific instruments, and in designing orthoses, but we must be guided by the whole individual—body, mind, and spirit—who has to decide the extent to which he or she is prepared to place the whole person at the service of one of the digits and restrict his or her whole freedom and activity to improve a single joint. The art of a therapist is to remain poised, flexible, and responsive to the input of science and technology on one hand and to the human values and needs of a patient on the other. This balance is constantly different with each patient, and that should keep the therapist alert and challenged throughout his or her professional career.
1. Bell Krotoski JA, Breger-Stanton DE. Biomechanics and evaluation of the hand. In: Hunter JM, Mackin EJ, Callahan AD, eds., et al. Rehabilitation of the Hand and Upper Extremity. 5th ed St Louis: Mosby; 1995:240–261.
2. Bell Krotoski JA, Fess EE. Biomechanics of the hand. J Hand Ther. 1995;8:63–67.
3. Brand PW, Hollister A. Clinical Mechanics of the Hand. 3th ed St Louis: Mosby; 1999.
4. Brand PW, Thompson DE, Micks JE. The Biomechanics of the Interphalangeal Joint; The Proximal Interphalangeal Joint. London: Churchill Livingstone; 1987.
5. Buford WL, Thompson DE. A system for three-dimensional interactive simulation of hand biomechanics. IEEE Trans Biomed Eng. 1987;34:444–453.
6. Jacobs MA, Austin NM. Splinting the Hand and Upper Extremity: Principles and Process. Philadelphia: Lippincott Williams & Wilkins; 2002.
7. Beach RB. Measurement of extremity volume by water displacement. Phys Ther. 1977;37(3):286–287.
8. Brand PW. Rehabilitation of the hand in leprosy. Cramer L, Chase R, eds. Symposium on the Hand.vol. 3. St Louis: CV Mosby; 1971.
9. Brand PW. Rehabilitation of the hand with motor and sensory impairment. Orthop Clin North Am. 1973;4:1135–1139.
10. Brand PW. Surgical treatment of primary deformities of the hand. In: McDowell F, Enna CD, eds. Surgical Rehabilitation in Leprosy and in Other Peripheral Nerve Disorders. Baltimore: Williams & Wilkins; 1974:174–184.
11. Fess EE, Gettle KS, Philips CA, Janson JR. Hand and Upper Extremity Splinting: Principles and Methods. 3rd ed St. Louis: Mosby; 2004.
12. Flowers KR. A proposed decision hierarchy for splinting the stiff joint, with an emphasis on force application parameters. J Hand Ther. 2002;15(2):158–162.
13. Hunter JM, Mackin EJ. Dedication; Edema and bandaging. In: Hunter JM, Schneider LH, Mackin EJ, Bell JA, eds. Rehabilitation of the Hand. 1978:113.
14. Brand PW. The forces of dynamic splinting: ten questions before applying a splint to a hand. In: Hunter JM, Mackin EJ, Callahan AD, eds., et al. Rehabilitation of the Hand and Upper Extremity. 5th ed. St Louis: Mosby; 2002:1811–1817.
15. Mildenberger LA, Amadio PC, An KN. Dynamic splinting: a systematic approach to the selection of elastic traction. Arch Phys Med Rehabil. 1986;67(4):241–244.
16. Breger-Lee DE, Buford WL. Update in splinting materials and methods: frontiers in hand rehabilitation. Hand Clin. 1991;7:3.
17. Breger-Lee DE, Buford WL. Properties of thermoplastic splinting materials. J Hand Ther. 1992;5:4.
18. Eccles MV. Hand volumetrics. Br J Phys Med. 1956;19:5–8.
19. Engler HS, Sweat RD. Volumetric arm measurements: technique and results. Am Surg. 1962;28(7):465–468.
20. Hunter JM, Mackin EJ. Management of edema. In: Hunter JM, Schneider LH, Mackin EJ, Callahand A, eds. Rehabilitation of the Hand: Surgery and Therapy. 3rd ed St. Louis: Mosby; 1990:187–194.
21. Stern EB. Volumetric comparison of seated and standing test postures. Am J Occup Ther. 1992;45(9):801–805.
22. Waylett-Rendall J, Seibly D. A study of the accuracy of a commercially available volumeter. J Hand Ther. 1991;4:10–13.
23. Dodds RL, Nielsen KA, Shirley AG, et al. Test-retest reliability of the commercial volumeter. 22. 2004. Work
24. Foto JG, Brasseaux D, Birke JA. Essential features of a handheld infrared thermometer used to guide the treatment of neuropathic feet. J Am Podiatr Med Assoc. 2007;97(5):360–365.
25. Breger-Lee DE, Bell Krotoski J, Brandsma JW. Torque range of motion in the hand clinic. J Hand Ther. 1990;3:7–13.