Palpation
Palpation is the application of variable manual pressures, through the surface of the body, to determine tenderness, shape, size, consistency, position, and inherent motility of the tissues beneath.61 It can also serve as an important doctor-patient communication tool, helping patients understand the significance of their problems because they can feel the provoked pain and resistance as they are palpated.240 Furthermore, palpation is the oldest examination technique used by chiropractors to detect subluxation/dysfunction.74,234 235 236 237
Like observational skills, palpation skills are learned tasks that take hours of devotion and practice. Good palpation skills are the result of both physical abilities and mental concentration. The skillful palpator is one who has developed an improved ability to tactually discriminate and mentally focus.
Palpatory procedures are commonly divided into static and motion components. Static palpation, which is often further subdivided into bony and soft tissue palpation, is performed with the patient in a stationary position. Motion palpation is performed during active or passive joint movement and also involves the evaluation of accessory joint movements. Motion palpation procedures have been an integral part of chiropractic since its inception, but not until the work and cultivation of Gillet41 42 43 44 45 and Faye52,53 have formalized techniques been widely disseminated.
Reliability of Palpation Procedures
Clinical evaluation of palpation procedures has increased significantly in the last several decades. The majority of tests have been conducted on reliability. Reliability testing for the various manual palpation procedures has demonstrated mixed results. Interexaminer palpation for bony alignment and muscle tension has demonstrated poor results, but palpation for bony and soft tissue tenderness has established good to excellent interexaminer reliability.245,255,377 378 379 380 Palpation for bony and soft tissue tenderness is frequently cited as one of the most valuable clinical cues for identifying dysfunction and targeting spinal manipulation. Research by Schneider and coworkers386 confirmed the reliability of pain provocation. They tested the reliability of spinal palpation for segmental mobility testing and pain provocation in 39 patients with a history of LBP. The resulting kappa values showed generally good reliability for the springing palpation that relied on patient self-reports of pain but poor reliability for assessment of mobility.386
Joint motion palpation, particularly passive EP assessment, is recognized as an essential skill by manual medicine disciplines387 and is used extensively by chiropractors, physical therapists, osteopaths, and medical manipulators in clinical practice as an indicator for spinal manipulation and mobilization. However, despite a few noteworthy exceptions that identified good interexaminer and intraexaminer reliability,384,385,388 389 390 391 the majority of studies evaluating spinal and sacroiliac joint (SIJ) mobility tests have identified poor interexaminer reliability and good intraexaminer reliability.* Some studies have shown weak or clinically insignificant reliability of motion palpation for certain groups of young, asymptomatic subjects.407 408 409 410 Most other studies have obtained poor to mixed results,247,378,391 with a few demonstrating an acceptable level of reliability for motion palpation testing.392,398 A summary of reliability studies conducted by Haneline and Cooperstein for motion palpation, pain provocation, landmark location, and alignment is presented in Appendix 2.
Good intraexaminer reliability in the face of poor interexaminer reliability should be viewed with caution. Good intraexaminer reliability does allow the examiner to evaluate how a test responds to treatment and may be helpful in directing individual patient treatments, but the ability to show internal consistency has limited value if different examiners cannot agree on their findings.371
The poor interexaminer reliability demonstrated in the majority of studies evaluating motion palpation is likely the product of several factors. One may be the very small qualitative and quantitative changes it attempts to measure. The line between normal and abnormal segmental joint movement has not been clearly established.411 In this environment, each examiner develops his or her own standard of what constitutes pathologic movement. Each examiner must develop his or her own “feel” for what is abnormal, with no common basis for comparison. The wide range of techniques taught and individual modifications and idiosyncrasies that each practitioner develops further complicate reliability. Interexaminer reliability is also likely negatively affected by the inability of examiners to precisely or repeatedly identify spinal bony landmarks and segmental joint level of palpation.391,412 Interexaminer reliability for motion palpation may demonstrate poor results not because examiners are inaccurate at sensing movement changes but because they are mislabeling and disagreeing on the joints that each is palpating. Furthermore, there is growing evidence that the biomechanical effects of spinal manipulation may not be as joint-specific as previously thought,413,414 and if the biomechanical effects are more widespread, we may be focusing on the wrong clinical question. A more appropriate clinical research topic might be the reliability of motion palpation assessment within a spinal region or two or three spinal motion segments.
The question of whether a multidimensional diagnostic approach to the physical examination of mechanical spine pain might lead to more reliable outcomes has had limited investigation. A study designed to assess the intraexaminer and interexaminer reliability of such an approach demonstrated moderate levels of intraexaminer reliability for the decision to manipulate a certain spinal segmental level and fair interexaminer agreement pooled across all spinal joints. However, the conclusion of the study was that the common diagnostic methods, including visual postural analysis, pain description by the patient, plain static erect x-ray film of the lumbar spine, leg length discrepancy, neurologic tests, motion palpation, static palpation, and orthopedic tests used on patients with chronic mechanical LBP are not reproducible. They further suggest that the implementation of these examination techniques alone cannot provide reliable information concerning where to direct a manipulative procedure in patients with chronic mechanical LBP.291
Based on available information, it seems reasonable to conclude the following: Palpation for bony and soft tissue pain and movement-induced joint pain (joint provocation or challenge) are reliable spinal manual examination procedures. Intraexaminer reliability for spinal motion palpation is mixed and interexaminer reliability for spinal motion palpation is generally poor. It is difficult to evaluate the interexaminer reliability of motion palpation because of inherent difficulties related to the standardization of the procedure, the inherent problems with identifying a specific segmental level of palpation, and the subtlety of functional spinal joint lesions. The following list provides a more detailed summary of the present status of spinal palpation reliability:
If intercollege standards for identification of abnormal spinal segmental motion can be developed, and agreement reached on the degree of joint specificity that is needed, spinal motion palpation may have the potential to develop improved interexaminer reliability. Insight into how this may be educationally accomplished is illustrated by an experiment conducted by Harvey and Byfield.415 They constructed a mechanical spinal model that was covered with leather to simulate skin and equipped with devices for artificially fixating segmental motion. Good interexaminer agreement was demonstrated by 8 graduate chiropractors and 19 final-year chiropractic students when given a choice between movement and the absence of movement. If mechanical models can economically be designed to simulate varying degrees of reduced movement, rather than complete absence of movement, they might have a valuable role to play in teaching and improving palpation reliability.
Validity of Palpation Procedures
Although the reliability of spinal motion palpation procedures has been extensively evaluated, there is a limited body of literature on the validity of motion palpation. A summary of validity studies is in Appendix 3. One of the early promising validity studies on spinal joint assessment was conducted by Jull, Bogduk, and Marsland.290 They investigated the accuracy of manual examination procedures in locating painful cervical joints confirmed by diagnostic nerve blocks. Using a combination of pain response and accessory and physiologic joint movements, a group of therapists identified the appropriate individuals and levels of abnormal painful cervical joints with 100% sensitivity and specificity. In another study,416 physiotherapists were able to identify 24 of 26 painful vertebral levels that correlated to a single level of unilateral multifidus muscle wasting confirmed by ultrasound examination. The examination consisted of segmental motion palpation methods with an evaluation for pain reproduction and abnormal resistance to movement.
Although these results are quite dramatic, the results are somewhat suspect. The procedures used during injections did not control for placebo effects and possible false-positive responses. The possibility of false-positive responses bring into question the accuracy of using uncontrolled injections as a gold-standard comparison.417 Furthermore, both studies included evaluations of mobility and pain. This makes it impossible to discern which procedure or combination of procedures is responsible for identifying the painful joint. Some have suggested that it is the provocation of pain and the patient’s verbal pain cues that are responsible for identifying symptomatic spinal joint dysfunction.394,418
In a subsequent single-blind study, Jull, Treleaven, and Versace419 were able to demonstrate that “cervical symptomatic joint dysfunction could be identified without reference to specific vertebral reports of pain by the subject.” The study did not rely solely on the evaluation of abnormal motion, but also allowed the examiner to determine the level of symptomatic joint dysfunction by the presence of “tissue stiffness and associated muscle reactivity or increased resistance through range of motion.” The authors concluded that “mechanical variables in segmental tissue stiffness, which are related to symptoms, can be detected.”419
King and associates258 replicated the study of Jull and colleagues257 with placebo-controlled facet blocks to determine the sensitivity, specificity, and likelihood ratio of manual examination for the diagnosis of cervical zygapophyseal joint pain. Manual joint motion examination demonstrated high sensitivity for cervical zygapophyseal palpated joint pain at the segmental levels that were commonly symptomatic, but its specificity was poor. Likelihood ratios were barely greater than 1:0, indicating that manual palpation for joint pain lacked validity. However, the study did have some significant methodologic limitations that affect its value. The manual examinations were not conducted by chiropractors and were performed by only one examiner with limited manual examination training. The reference standards (facet blocks) were applied only to subjects with positive manual examination findings and not those who had negative findings.
Humphreys and coworkers421 studied the validity of motion palpation using the presence of a congenital block vertebra as a gold standard. Twenty fourth-year chiropractic students had to identify the hypomobile segments in three subjects with a congenital block vertebra. They found a sensitivity of 74% and a specificity of 98% for the general detection of all blocks and a kappa value of 0.67, which is considered good. Assuming that block vertebra are a fair representation of marked spinal joint hypomobility, they concluded that their substantial demonstrated agreement lends support to the validity of motion palpation in detecting major spinal fixations in the cervical spine.
A study evaluating the prevalence of positive motion-palpation findings (so-called fixations and spontaneous pain response) in relation to self-reported LBP status was performed to determine the sensitivity and specificity of the motion-palpation technique on the sacroiliac and lumbar joints.421 No logical pattern of fixations and spontaneous pain reactions were found in relation to the LBP status of the patients. The sensitivity was low for fixations and pain, but the specificity was significantly higher for pain in the mid-lumbar area. However, there was no strong association found between fixations and the examiners’ interpretation of a pain reaction in response to motion palpation, leading to the conclusion that motion palpation does not appear to be a good method to differentiate persons with or without LBP.421 However, it was concluded that it was possible to dissociate the findings of fixations and those of pain reactions.421
The identification of hypomobility with prone P-A mobility testing has demonstrated validity in identifying patients who are more likely to benefit from manipulative therapy.260,261 This procedure was combined with pain of less than 16 days’ duration, no radiating pain below the knee and low fear avoidance belief scores as criteria to select patients for a short trial of manipulative therapy. Subsequent evaluations have indicated that the other criteria may be more predictive of outcome and that the P-A mobility testing may not add significant value.
Another validity study using dynamic x-ray as a reference standard compared lower cervical lateral glide motion palpation to lateral flexion radiographs in patients presenting with mechanical neck pain.422 The lateral gliding test for the cervical spine was as good as the radiologic assessment for the diagnosis of intervertebral joint dysfunction in the lower cervical spine in this small group of patients. These results indicate that the lateral gliding test for the cervical spine is as accurate as lateral flexion radiographs in identifying restricted intervertebral mobility in the lower cervical spine.422 However, lateral flexion radiographs have not been validated as a reliable and valid tool for identifying cervical dysfunction.
The clinical value of diagnostic procedures can also be assessed relative to their ability to change in response to treatment. Investigations into the responsiveness of motion palpation to adjustive treatments are limited to one randomized, controlled study conducted on thoracic rotational adjustments.291 Patients were evaluated for thoracic rotational EP restrictions and randomly assigned to treatment and control groups. When re-examined by the blinded evaluators, those patients receiving treatments did show significant postmanipulative reductions in EP restrictions. Segmental EP palpation was thus found to have “utility as a postmanipulative evaluative test for patients who are symptomatic or mildly symptomatic in the thoracic spine.”293 This provides encouraging evidence that chiropractors may be able to manually palpate postmanipulative segmental EP restriction changes in human subjects.
The question also arises as to whether or not reliability and validity of motion palpation may be demonstrating less than optimal results because chiropractors are asking the wrong questions and not structuring the experiments accordingly. The majority of procedures evaluated to date have been based on the premise that a precise level of spinal dysfunction needs to be ascertained before effective treatment can be rendered. Hass and Panzer271 question if this is an accurate assumption. They wonder if specific localization “might not be necessary for correction of the ‘true’ underlying manipulable subluxation syndrome.” They pose the possibility that identification of regional dysfunction might be sufficient for effective treatment of dysfunction.
As discussed previously, if identification of regional dysfunction were sufficient to establish effective treatment, it would likely be more reliable than procedures used to identify a specific level of dysfunction.271 Although this may be a valid point, Hass and Panzer271 correctly point out that it needs to be examined. It would be premature to abandon the specificity model without an established alternative “biomechanical model or clinical evidence to suggest how big the zone of agreement might be or how it might vary in different regions.”271
To address this issue, Hass and associates423 conducted a preliminary investigation to evaluate the efficacy of a specific diagnostic indicator (segmental EP) to see if it improved spinal manipulative outcome. The study evaluated patients with neck pain who were randomized to receive cervical spine manipulation at restricted levels identified by motion palpation versus manipulation at levels randomly generated by a computer. The results show that both groups had similar, and in some cases dramatic, improvements in symptoms directly after receiving one HVLA cervical adjustment. The results of this study indicate that cervical EP-directed manipulation does not improve same-day outcomes in pain or stiffness. The outcome lends support to the hypothesis that spinal manipulation may have a more generalized, nonspecific mechanism of action in relieving symptoms. It also implies that the mechanical effects associated with manipulation may lack spatial specificity and specificity of adjustive contacts and adjustive vector may not be as important as generally thought.
Although the evidence from this study indicates that using EP to identify the level of dysfunction does not improve the measured outcome, it would be inappropriate to draw conclusions from this study alone. It is the only study to clinically investigate this topic and it has a number of limitations that significantly affect its clinical implications. First, it measures the effects of only one adjustment on immediate and same-day pain and stiffness reduction. It is likely that manipulation has a dose-dependent therapeutic effect,424 and this trial does not come close to approximating the typical course of adjustive treatments. Adjustive treatments for a cervical mechanical pain syndrome average 6 to 12 treatments over the course of a few weeks. EP assessment also may not be a valid indicator for same-day postmanipulative pain and yet valid in directing therapy that has an effect on other clinical outcomes such as pain and function over time. The immediate pain and stiffness relief noted by both groups may also be attributable to placebo or nonspecific effects associated with assessment and treatment, concealing differences between groups that might have developed over time.
Despite the controversy surrounding motion palpation techniques and a call to abandon motion palpation techniques,425 the majority of chiropractors and other manipulating professions continue to use these procedures and consider them to be reliable and valuable methods.74,283,292,387 Although chiropractors may not be as informed and questioning of motion palpation procedures as they should be, it is clear that the evaluation of motion palpation procedures is incomplete. Although evidence is building that spinal intersegmental ROM palpation has poor interexaminer reliability, evidence does imply that it may have clinical value in context with other manual examination procedures, especially when incorporated with pain provocation. The results concerning the segmental motion palpation tools are mixed and, in a number of cases, are inconclusive. It is premature to discard a safe, low-cost, and potentially useful procedure. There is not enough evidence to draw firm conclusions on the validity of a number of manual examination procedures at this time. Further research into various palpatory regimens is necessary to evaluate and differentiate clinically relevant and useful palpation procedures. Within this context, it is important to remain informed and not rely excessively on any one procedure, but to use a combination of diagnostic procedures and allow the weight of evidence to build a clinical impression of the patient’s problem.
It is also important to stress that all clinical procedures have imperfect diagnostic reliability and validity. Saal426 reviewed the literature on invasive spinal diagnostic tests (imaging studies, facet joint diagnostic blockade, anesthetic blocks, lumbar discography, NR blockade, sciatic nerve block, posterior ramus block, and subcutaneous injection) and concluded that there are inherent limitations in the accuracy of the diagnostic tests they evaluated. Although the reliability of all palpatory procedures is not at the same level as the reading of a thermometer or the taking of blood pressure (sphygmomanometry), it is comparable to cardiac auscultation.427 The agreement between observers and the phonocardiographic gold standard in the correct identification of S4 and S3 heart sounds was poor and the lack of agreement did not appear to be a function of the experience of the observers. The overall interobserver agreement for the detection of either S4 or S3 was little better than chance alone.427 Yet cardiac auscultation continues to be taught and used because of the low-risk clinical information it yields. The key is for each clinician to understand the strengths and limitations of the procedures they may use. Clinical decisions concerning the application and interpretation of diagnostic and therapeutic procedures should be based on the best available evidence. For each procedure it is important to understand its comparative advantages, limitations, and costs. When available, knowing a diagnostic test’s specificity, sensitivity, predictive value, and likelihood ratios can only lead to better risk-benefit assessments.
Sacroiliac Articulation
A separate and focused discussion of the SIJ is warranted based on the many specialized manual examination procedures that have been developed to evaluate its function.428 Dysfunction of the SIJ is defined as a state of relative hypomobility associated with possible altered positional relationships between the sacrum and the ilium.429,430 Motion palpation and pain provocation tests have been used in various forms and advocated by a number of professions employing manual therapies in the assessment and treatment of SIJ dysfunction.431 432 433 434 435 However, the results of the reliability studies for mobility tests and pain provocation tests of the SIJ have been mixed. Laslett and Williams436 reported in 1994 that pain-provocation SIJ tests are reliable if performed in a highly standardized manner, using sufficient force to stress the SIJ. The results of a review of SIJ tests by van der Wurff and associates437 could not demonstrate reliable outcomes and concluded that there is no evidence on which to base acceptance of mobility tests of the SIJ into daily clinical practice. Hungerford and coworkers438 demonstrated that an altered pattern of intrapelvic motion could be reliably palpated and recognized during the Stork test (a modified interpretation of the Gillet test), and that the practitioner could distinguish between no relative movement and anterior rotation of the innominate during a load-bearing task.438
Tests designed to provoke a patient’s pain appear to have more support for use in identifying patients who may have SIJ region dysfunction than do tests presumed to measure SIJ alignment or movement.439 Provocation SIJ tests are more frequently positive in back pain patients than the accepted prevalence of SIJ pain.440 This indicates that individual tests may be confounded by a number of false-positive responses. Laslett and colleagues441 tested provocation tests and found that any two of four positive tests (distraction, compression, thigh thrust, or sacral thrust) or three or more of the full set (distraction, compression, thigh thrust, sacral thrust, and Gaenslen sign) were the best predictors of reducing or abolishing a patient’s pain by intra-articular SIJ anesthetic injection. They further concluded that when all of the SIJ provocation tests are negative, painful SIJ pathologic conditions may be ruled out, suggesting that provocation SIJ tests have significant diagnostic utility.
Arab and coworkers442 evaluated intraexaminer and interexaminer reliability of individual motion tests and pain provocation tests for the SIJ and found both to have fair to substantial reliability. They also looked at “clusters” of motion palpation or provocation tests and found moderate to excellent reliability. Intraexaminer and interexaminer reliability of composites of motion palpation and provocation tests were also considered substantial to excellent. They therefore concluded that composites of motion palpation and provocation tests together have reliability sufficiently high for use in clinical assessment of the SIJ.442
Manipulative treatment methods for the SIJ are based explicitly or implicitly on the presumption that some biomechanical dysfunction causes the SIJ or its associated soft tissues to become painful. This hypothesis may be questioned because the means for identifying dysfunction are based on an evidential base with disputed or conflicting results concerning reliability and validity of SIJ dysfunction tests.443
Bony palpation
The major goal of bony palpation is to locate bony landmarks and assess bony contour for any joint malpositions, anomalies, or tenderness. Typically, the palmar surfaces of the fingers or thumbs are used because they are richly endowed with sensory receptors. Light pressure is used for superficial structures, gently increasing pressure for deeper landmarks.
During spinal palpation, the pelvis, lumbar, and thoracic regions are customarily evaluated while the patient is in the prone position and the patient’s cervical spine is evaluated in the sitting or supine position. The spinous processes in the entire spine—the articular pillars in the cervical spine, the transverse processes in the thoracic spine, and the mammillary processes in the lumbar spine—are palpated for tenderness and compared for contour and alignment (Figure 3-18). The cervical articular pillars and thoracic transverse process are both palpated through overlying muscular layers, and tenderness in these structures must be differentiated from tenderness in overlying soft tissues. The lumbar mammillary processes are not directly palpable in most individuals. They are located by a sense of deep resistance palpated through the overlying muscular layer. Individual motion segments are often located relative to these bony landmarks, and it is important to appreciate the anatomic relationship of the transverse processes to the corresponding spinous processes (Figure 3-19).
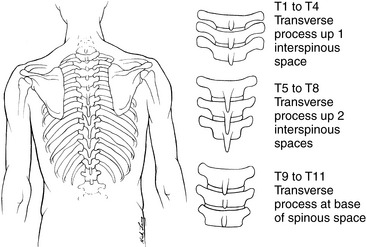
Figure 3-19 The structural relationship between thoracic spinous processes and transverse processes.
Tenderness over articular landmarks is an important potential sign of JSDSs. Of all the diagnostic signs of JSDS, palpation for tenderness appears to be the most reliable.244 255 256382,444 445 446 However, joint dysfunction is not always synonymous with joint pain. Dysfunction may or may not directly cause joint pain. Although JSDS is commonly associated with pain, chronic dysfunctions may be nonpainful, but potentially create a region of altered mobility that can predispose to joint strain and pain elsewhere.
Misaligned articular structures may implicate the presence of joint subluxation/dysfunction, but apparent joint malpositions may result from anomaly or compensation without dysfunction. Spinal landmarks, especially the spinous processes, are prone to congenital or developmental malformation. Disrelationship between adjacent spinous processes can be falsely positive and cannot be relied on to represent true misalignment. Furthermore, the spine functions as a kinetic chain, and disease or dysfunction at one level may force adaptational alterations in neutral alignment at adjacent levels. These sites of compensational change may palpate as being malpositioned (out of ideal neutral alignment), yet have normal pain-free function. Static bony palpation does not ascertain joint mobility or the full extensibility of the articular soft tissues and cannot distinguish normal compensation from joint subluxation/dysfunction.
In the spine, the spinous process and interspinal spaces are commonly palpated for tenderness to screen for a possible level of segmental pathology or dysfunction. The relationship between spinous and interspinous tenderness and dysfunction is speculated to result from reflex sensitivity in tissues with shared segmental innervation (allodynia) or from mechanical deformation in structures attaching at these bony sites.
Remember that bony tenderness may result from many different pathologic processes such as bone infection, neoplasia, osteoporosis, and fractures. In addition, the spinous process may be tender whether the joint is hypomobile, hypermobile, or unstable. For the previously outlined reasons, suspected malpositions or bony tenderness must be associated with other clinical signs before an impression of joint subluxation/dysfunction is formed.
Soft tissue palpation
One of the commonly stated diagnostic characteristics of the manipulable spinal lesion is altered segmental tissue tone and texture. The major function of soft tissue palpation is to determine the contour, consistency, quality, and presence or absence of pain in the dermal, subdermal, and deeper “functional” tissue layers. The dermal layer incorporates the skin; the subdermal layer incorporates subcutaneous adipose, fasciae, nerves, and blood vessels. The functional layer consists of the muscles, tendons, tendon sheaths, bursae, ligaments, fasciae, blood vessels, and nerves.
Palpation of the dermal layer is directed toward the assessment of temperature, moisture, motility, consistency, and tissue sensitivity (e.g., hyperesthesia and tenderness). Palpation techniques involve light, gentle exploration of the skin with the palmar surfaces of the fingers or thumbs. When manually assessing temperature of superficial tissues, the dorsum of the hands is typically used (Figure 3-20). Motility and sensitivity of the dermal layer may also be assessed by the technique of skin rolling (see Figure 3-20).
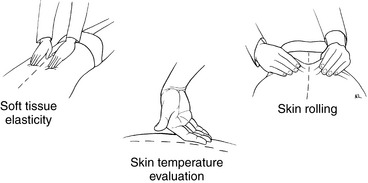
Figure 3-20 Assessment techniques for evaluating alterations in temperature, tenderness, tone, and texture of the superficial layer of the soft tissues.
The subcutaneous and deeper functional layers are explored for internal arrangement, contour, consistency, flexibility, and response to pressure. The deeper soft tissues are usually investigated with the fingertips or thumbs (Figure 3-21). Palpation of paraspinal soft tissues is customarily performed immediately after bony palpation. The cervical spine is customarily examined with the patient in the supine or sitting position and the lumbopelvic and thoracic regions in the prone position.
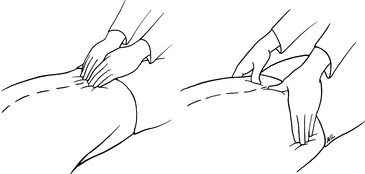
Figure 3-21 Assessment techniques for evaluating tone and texture in the deep paraspinal soft tissues using fingertips.
The palpatory investigation of the functional layer is the decisive element in the soft tissue investigation for signs of joint dysfunction. Suppleness and flexibility of muscle and connective tissues are important and necessary for proper functioning of the joint systems of the body. Muscular and myofascial dysfunction are considered to be common factors in the pathogenesis of somatic and joint pain syndromes.118,447 Segmental tissue texture changes may include abnormal hardness, bogginess, or ropiness of the underlying paraspinal muscles.448 The reliability and accuracy of palpation to detect muscle dysfunction are not well established in the scientific literature.121,449
The presence of soft tissue pain and asymmetric tone is regarded as an important indicator of joint dysfunction.419 Grieve449 suggests that it may be the objective findings of muscle abnormality (palpable nodules, bands, or stringiness) and the presence of muscle tenderness that represent external evidence of changes in peripheral tissues related to joint problems. Furthermore, muscle pain is sometimes acute and surprisingly quite unknown to the asymptomatic patient until made manifest by careful localized palpation. Nilsson382 found acceptable reliability of palpation for cervical erector spinae muscle tenderness using a grading pain scale of 0 to 3 that incorporated both verbal and nonverbal responses from the patient. Christensen and colleagues450 also reported good interexaminer reliability for thoracic paraspinal tenderness. The interexaminer agreement for the detection of tissue texture changes within muscle tissue appears to be less reliable than the detection of tenderness.121
In health, normal neuromuscular coordination is accepted as unremarkable; only in dysfunction does the underlying complexity of movement become apparent and the disturbance of reciprocal muscle action become manifest.449 Moreover, abnormal soft tissues patterns and presentations may persist after joint function has been restored. Although chronic muscle imbalance has a role in initiating and perpetuating joint problems and somatic pain, it may be secondary to stresses imposed by ligamentous failure, denervation, or reflex inhibition from pain. Adjustments of the joint without attention to the supporting and controlling effects of the soft tissues will likely result in recurrence of joint dysfunction.
Soft tissue asymmetries may also result from congenital or developmental variations or be the product of nonmanipulable disorders. Accordingly, any noted soft tissue abnormalities must be assessed within the context of a broader examination to be clinically significant. Instructions and tips on the use of static bony and soft tissue palpation are included in Boxes 3-7 and 3-8.
BOX 3-7 How to Use Palpation Tools
Motion palpation
Motion palpation is a procedure in which the hands are used to assess mobility of joints. It is a skill that depends not only on psychomotor training but also on an understanding of the local functional anatomy, biomechanics, and pathomechanics. Each individual extremity joint and spinal region has its unique patterns and ROMs that must be learned if the chiropractic student is to master the art of motion palpation.
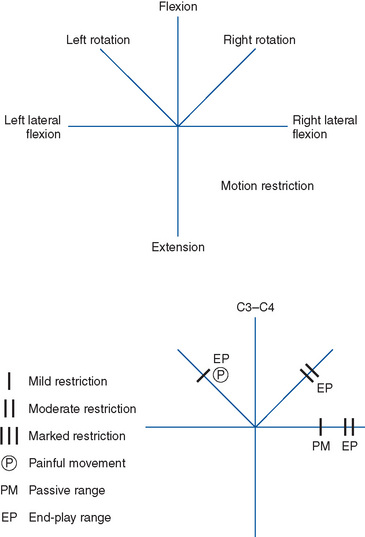
Motion palpation covers a collection of manual examination procedures that are customarily divided into techniques designed to assess active, passive, and accessory joint movements. Active movements are internally driven and are the result of voluntary muscle contraction. During active movement assessment, the doctor may help guide the patient through a given motion, but the patient provides the muscular effort necessary to induce joint movement. The range of active joint movement is determined by the joint’s articular design and the inherent tension and resilience in its associated muscular, myofascial, and ligamentous structures. Greenman337 has labeled the end point of active joint movement as the physiologic barrier. (Figure 3-22).
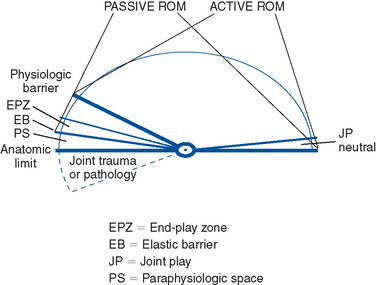
Figure 3-22 Joint motion starting from a neutral position. The first motion evaluated from a neutral starting position is joint play (JP). JP is a component of active and passive joint motion. It is induced by the examiner and represents the give and flexibility of the joint capsule. Active range of motion (ROM) represents the movement that is actively produced by the patient. Passive ROM represents the motion produced by the examiner. It is usually slightly greater in range because the patient’s muscles are not active but relaxed. Toward the end of passive movement the end-play zone (EPZ) is encountered. The EPZ represents the increased resistance that is felt as the joint’s elastic limits are reached. The elastic barrier represents the end point of the joint’s elastic limits and the point at which additional movement is only possible after joint surface separation. Joint surface separation at this point usually occurs only after joint cavitation. After cavitation, the paraphysiologic space (PS) extends the passive ROM. At the end of the PS, the joint’s anatomic limits are encountered. If the joint is carried beyond its anatomic limit, injury results.
In contrast, passive joint movements are involuntary movements. With the patient in a relaxed position, the examiner carries the joint through its arc of available motion. The range for passive joint movement is somewhat greater than the range for active joint movement because of decreased muscle activity (see Figure 3-22). The range of passive joint movement also depends on articular design and flexibility of related articular soft tissues.
As the limits of passive joint movement are approached, additional resistance is encountered as the joint’s elastic limits are challenged. Movement into this space, the EP zone (EPZ) (see Figure 3-22), may be induced by forced muscular effort by the patient or by additional overpressure (EP) applied by the examiner. If the forces applied at this point are removed, the joint springs back from its elastic limits. Movements into this region are valuable in assessing the elastic properties of the joint capsule and its periarticular soft tissues.
Movement beyond the EPZ is possible, but usually only after the fluid tension between synovial surfaces has been overcome. This process is typically associated with an articular crack (cavitation). Sandoz50 has labeled this as the zone of paraphysiologic movement and identified its boundaries as the elastic and anatomic barriers (see Figure 3-22). In circumstances in which the joint capsule is especially flexible, joint separation may occur without cavitation. The loose capsule allows for separation without fluid tension build-up between articular surfaces.51
The labeling of the postcavitation increase in joint movement as paraphysiologic can be misleading. Although the paraphysiologic space (PS) aptly identifies an area of increased movement, it is still within the joint’s elastic range and anatomic limits. Movement into this space does not induce joint injury. However, if the outer boundaries (anatomic limits) of the PS are breached, then plastic deformation and joint injury may occur50 (Figure 3-23).
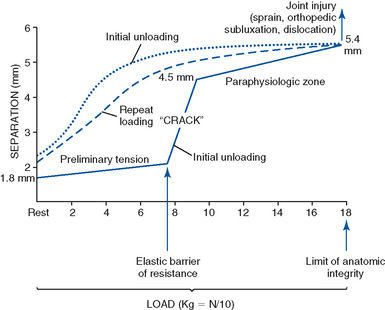
Figure 3-23 Increased movement that occurs after joint cavitation. The solid line represents the initial loading of the joint and the increased joint separation and movement that occurs only with cavitation. The broken line illustrates that repeated loading of the joint will induce the same amount of joint separation without joint cavitation.
Restrictions of joint motion may occur at any point within the joint’s ROM. They may be minor or major in nature and encountered within the joint’s active or passive range. Restrictive barriers encountered within the joint’s active ROM are primarily a result of myofascial shortening.337 This may be a product of muscle splinting, hypertrophy, aging, or contracture. Restrictive barriers to movement at the end range of passive motion are more indicative of shortening in the joint capsule and periarticular soft tissues.
During the performance of motion palpation, the examiner characteristically uses one hand to palpate joint movement (palpation hand) while the other hand (indifferent hand) produces or guides movement. The palpation hand establishes bony or soft tissue contacts over the joint as attention is directed to the assessment of joint range, pattern, and quality of movement (Figure 3-24). When assessing joint motion, the palpator is evaluating the quality and quantity of movement from the starting or zero point to the end range of passive movement. In spinal evaluation, the landmarks commonly used are the spinous processes, articular pillars, transverse process, rib angles, and mammillary processes. During spinal palpation the examiner can attempt to assess the ROM of a single spinal motion segment or take broader contacts to assess a spinal region and several joints at a time.
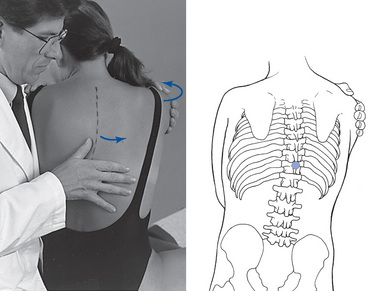
 Figure 3-24 Assessment of segmental range of motion (e.g., midthoracic left axial rotation). The small circle located on the skeletal drawing represents the location of the thumb contact traversing the left side of the T10 and T11 spinous processes.
Figure 3-24 Assessment of segmental range of motion (e.g., midthoracic left axial rotation). The small circle located on the skeletal drawing represents the location of the thumb contact traversing the left side of the T10 and T11 spinous processes.
Accessory Joint Motion
Accessory joint movements are necessary for normal function. They are small, involuntary movements made possible by the give within the articular soft tissues of each synovial joint. Joint surfaces do not form true geometric shapes with matching articular surfaces. As a result, movement occurs around a shifting axis, and the joint capsule must allow sufficient play and separation between articular surfaces to avoid abnormal joint friction.
Accessory joint movements are evaluated by the procedures of JP and EP.48,53 EP evaluation is the qualitative assessment of resistance at the end point of passive joint movement, and JP is the assessment of resistance from a neutral or loose-packed joint position.61 Both motions depend on the flexibility (play) of the articular soft tissue and are not distinguished by some authors.48,53 Rather, EP is considered to be JP delivered at the end range of joint motion.
Joint Play
JP assessment is the qualitative evaluation of the joint’s resistance to movement when it is in a neutral or loose-packed position. The loose-packed position allows for the greatest possible play between the joint surfaces and the best opportunity to isolate the joint capsule from the periarticular muscles (see Figure 3-22). JP assessment therefore is helpful in the isolation and differentiation of articular-based pain and dysfunction from nonarticular soft tissue disorders. It has also been proposed as an evaluative procedure for the clinical assessment of joint instability; it has demonstrated some validity in detecting excessive translational movements that may result from derangement of the joint’s stabilizing structures.167,169
JP is assessed by placing the tested joint in its loose-packed position, establishing palpating contacts over the joint, and inducing gentle shallow springing movements (Figure 3-25). This is most commonly done in the spine by placing the patient in a prone position and applying a P-A force. The true loose-packed position may not be achievable in the acutely injured or pathologic joint, and attempts to force a loose-packed position should be avoided. In such circumstances, the chiropractor should attempt to find the loosest possible pain-free position. JP movements are small in magnitude and vary by spinal region or extremity joint. It is therefore essential that the examiner, through practice, develop an appreciation for the regional and specific qualitative differences. As mentioned previously, this procedure has demonstrated good reliability for reproduction of pain (joint provocation and challenge) but poor reliability of determining hypomobility.246
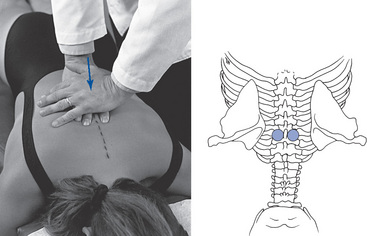
 Figure 3-25 Assessment of joint play movement: posteroanterior glide, midthoracic segment. Circles indicate location of fingers over joints to be assessed.
Figure 3-25 Assessment of joint play movement: posteroanterior glide, midthoracic segment. Circles indicate location of fingers over joints to be assessed.
JP procedures include methods in which the palpatory contacts are established over the joints to be assessed. Methods that involve contacts on both sides of the spinous process can be applied with opposing springing movements in attempts to specifically isolate a particular level of pain or dysfunction (Figure 3-26). During the performance of JP, the chiropractor should check for the presence or absence of pain, the degree of encountered resistance, and the quality of movement. JP should not induce pain; some resistance to movement should be encountered, but the joint should yield to pressure and spring back, producing short-range movements. Production of pain or increased resistance to JP movements suggests that the joint and its articular soft tissue may be the source of the patient’s local spine complaint.
End Play
During EP assessment, the chiropractor is concerned with the symptomatic and qualitative assessment of motion through the EPZ (Figure 3-27). The EPZ is characterized by a sense of increasing resistance as it is approached (first stop) and a second firmer resistance (second stop) as its limits are approached (see Figure 3-27). In a healthy joint, it should be pain-free.
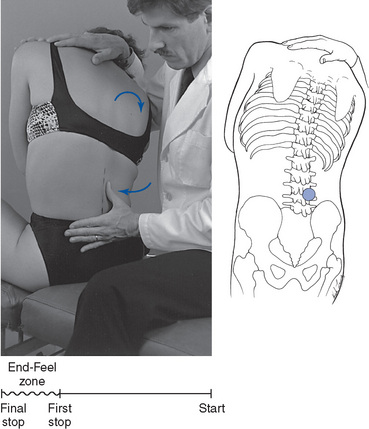
 Figure 3-27 Assessment of lateral flexion end play motion. The circle between L3 and L4 on the skeletal drawing represents the location of the thumb contact against the lateral surface of the spinous process.
Figure 3-27 Assessment of lateral flexion end play motion. The circle between L3 and L4 on the skeletal drawing represents the location of the thumb contact against the lateral surface of the spinous process.
EP is assessed by applying additional overpressure to the specified joint at the end range of passive movement. During spinal EP assessment, a gentle springing force is typically induced through the palpation and indifferent hand contacts (see Figure 3-27). To execute end feel, the chiropractor should evaluate the point at which resistance is encountered, the quality of that resistance, and whether there is any associated tenderness.
EP evaluation is an important element in the assessment of joint function. In spinal joints, it has been reasoned that EP may be more informative than procedures designed to assess the ROM of individual spinal joints. This is based on the premise that qualitative changes in movement may be more reliably evaluated than quantitative changes, especially in the spine where the joints are deep and less accessible to palpation and the segmental ROM is normally small.252 A recent qualitative literature review evaluated this question and did not confirm a significant advantage for EP over segmental ROM. The authors did note an advantage to EP over segmental ROM, but it did not rise to the level of being statistically significant.391
However, the number of quality studies is very limited and further evaluation of EP reliability and validity as compared with segmental ROM is needed before conclusive statements are made.391
Each spinal region or extremity joint has characteristic EP qualities that are determined by the local bony and soft tissue anatomy (physiologic end feel). For example, elbow extension has a hard, bony end feel produced by the bony impact of the olecranon on the humerus, and elbow flexion has a soft springy end feel produced by the impact, or compression, of soft tissues on the arm and forearm. What may be a normal EP at one joint may be a pathologic EP at another. A hard, bony EP to elbow flexion might indicate a fracture or an intra-articular blockage, and a soft, springing EP to elbow extension might indicate joint effusion. Physiologic and pathologic EPs have been tabulated for the spine and extremity joints and are outlined in Box 3-9.
BOX 3-9 Normal and Abnormal End Feels
Capsular
Loss of normal EP elasticity is thought to be indicative of disorders within the joint, its capsule, or periarticular soft tissue. Abnormal EP resistance or increased pain is considered a significant finding in the determination of JSDSs and directing adjustive vector. Adjustive therapy is commonly applied in the direction of encountered resistance in an attempt to restore normal mobility.
Cyriax22 has suggested that EP assessment is particularly valuable in isolating the integrity of the joint capsule. He has proposed that injuries or disorders that lead to contractures of the joint capsule will lead to predictable patterns of JP or EP restrictions in multiple ranges. Each joint purportedly has its own characteristic capsular pattern of restricted movement that indicates capsular involvement (Table 3-4). Injuries or contractures in only one aspect of the capsule do not necessarily follow this typical pattern and may affect movement in only one direction.
| Joint | Pattern* |
|---|---|
| Spine | Ipsilateral rotation and contralateral lateral flexion |
| Hip | Internal rotation-abduction, flexion-extension, adduction-external rotation |
| Knee | Flexion (great)-extension (slight) |
| Ankle | Dorsiflexion-plantar flexion |
| Metatarsophalangeal joint | Flexion-extension |
| Interphalangeal joint | Flexion-extension |
| Shoulder | External rotation-abduction–internal rotation-flexion |
| Elbow | Flexion-extension (pronation and supination, full range) |
| Distal radioulnar joint | Pronation-supination |
| Radioulnar carpal joint | Flexion-extension |
| Midcarpal joint | Extension-flexion |
| Thumb carpometacarpal joint | Abduction-extension |
| Metacarpophalangeal joint | Flexion-extension |
* Patterns are in order of decreasing stiffness, except the spine, in which either is possible.
Loss of normal EP resistance (empty end feel) is also clinically significant because it is a potential manifestation of joint hypermobility or instability. Injuries or disorders that lead to elongation of the joint’s stabilizing structures may lead to a loss of normal end-range resistance. Although an empty EP is indicative of possible clinical joint instability, segmental muscle splinting in the symptomatic patient may mask its presence.
Joint Challenge (Provocation)
The assessment of pain during the application of JP and EP is often referred to as joint challenging or joint provocation. It is commonly used to isolate joint pain and to determine which segmental tissues placed under tension may be sensitive to mechanical deformation and responsible for the patient’s pain. It often involves methods that attempt to isolate a given joint by applying counterpressure across the joint.
In the spine, the counter-opposing pressures are commonly applied against the spinous processes. During this procedure, the vertebrae are stressed in different directions from their neutral positions, and directions of increased and decreased pain are noted (see Figure 3-26). Pain during movement is theorized to result from increased tension on injured or inflamed articular tissue. The absence of pain during movement indicates that tissues tractioned (challenged) in the direction of movement are not injured.
Provocation of joint pain during movement assessment in combination with tests for mobility have demonstrated promising results.389,416,453 Recent studies have indicated that P-A springing of the spine has good interexaminer reliability for the reproduction of pain, but mixed reliability for hypomobility. Some have suggested that the provocation of pain during joint movement assessments is the element responsible for reliably and accurately identifying symptomatic joint dysfunction.394,418 Others have suggested that pain provocation is an important tool, but they are concerned that reliance on this procedure would lead to an increased incidence of false-positive results.419 Spinal pain is often poorly localized and commonly associated with sites of referred pain. The site of maximal tenderness is not always the source of the pathology or JSDSs. Chiropractic theory implies that joint restrictions (fixations) are not necessarily symptomatic. Marked reduction in movement at one spinal level may induce increased compensatory hypermobility at other joints that may be more symptomatic than the restricted joints.
In addition, this procedure has been proposed as a method for determining the alignment of joint subluxations and direction of appropriate adjustment. The assumption is that pain is increased when subluxated vertebrae are pushed in directions that increase the misalignment (into lesion) and that pain is decreased in the direction that reduces the misalignment (out of lesion). For example, pressure exerted toward the right against the left side of a right-rotated T4 spinous process (left rotating the joint) purportedly would increase the misalignment and induce pain (see Figure 3-26). Pressure exerted toward the left, against the right side of the T4 spinous process would decrease the misalignment and not elicit discomfort. This approach has value in the evaluation and treatment of the acutely injured patient when the clinician is trying to determine how to induce joint distraction or reduce a traumatic subluxation without causing more tissue damage. However, whether this principle applies equally in all cases of joint subluxation/dysfunction is questionable.
If the rule of pain-free manipulation were applied in the case of post-traumatic joint dysfunction resulting from periarticular soft tissue contractures, would it accurately determine the appropriate direction of adjustment? Manual therapy applied in this scenario would logically be directed to stretch the shortened and contracted tissue. Tensile stretch applied to contracted and inelastic tissue commonly induces some discomfort. Applying the rule of pain-free manipulation in this scenario would lead to an adjustment in the direction opposite the restriction. In this circumstance, the adjustment should be made in the direction of encountered joint restrictions, even if it is associated with some tenderness. Without attention to patient history and directions of encountered abnormal resistance, proper adjustive care may be missed.
From this discussion, the following generalizations about adjustive treatment for established joint dysfunction can be made:
The procedures of segmental motion palpation have focused on the detection of joint pain and mobility, and although restricted joint and accessory joint motion may be indicative of joint dysfunction and sufficient evidence for joint manipulation, clinicians must guard against perceiving it as a diagnostic panacea. Isolation of a painful joint does not determine the cause of the pain or possible disease. Motion palpation cannot be used in all clinical situations (e.g., acute joint pain or injury), and certain disease states capable of producing joint restrictions may produce pathophysiologic change that contraindicates adjustive therapy.
As mentioned previously, segmental motion palpation is also subject to error and therefore should not be applied in isolation. However, Phillips and Twomey454 did find that motion palpation was highly sensitive and specific for detecting a symptomatic lumbar segment when they incorporated a subjective pain response from the patient. Nonetheless, the determination of joint dysfunction should be made in conjunction with other clinical findings. No one evaluative tool should be the sole source for therapeutic decisions. Goals, principles, and tips for conducting motion palpation are outlined in Boxes 3-10, 3-11, and 3-12.
BOX 3-11 Principles of Motion Palpation
BOX 3-12 Motion Palpation Tips
Percussion
Percussion plays a secondary role in the assessment of joint dysfunction. The area of greatest application is probably the spine, where a positive response may help localize a painful motion segment. Spinal percussion may be applied by the hypothenar of the clinician’s hand or with a reflex hammer (Figure 3-28). In both circumstances, the clinician should apply a gentle percussive force sequentially to the spinous processes. A marked or persistent pain response to percussion may indicate an underlying fracture or a nonmechanical pathologic condition, whereas a mild pain response may indicate local irritation and dysfunction. When the response indicates a potentially serious disease, additional radiographic or laboratory procedures are necessary to differentiate a manipulable lesion from a nonmanipulable one.
Muscle testing
Motor changes are characteristic of many neuromuscular conditions, making tests for muscle length and strength an integral part of the examination process. The testing of muscle structure and function requires knowledge of joint motion, origin and insertion of muscles, agonistic and antagonistic actions, and the ability to palpate the muscle or its tendinous attachments for tone and texture changes.
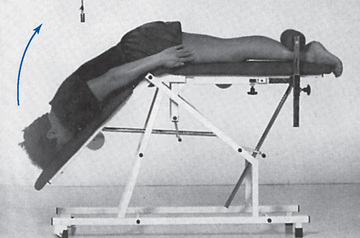
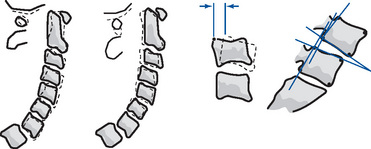
Muscle strength testing incorporates tests for strength and endurance. Endurance can be evaluated by the patient’s ability to perform repeated movements or maintain static postures. Normative values for repetitive squatting, sit-ups, prone arch-ups, and sustained prone back extension have been established and are valid measures for measuring spinal fitness and treatment outcomes (Figure 3-29). Strength testing can be evaluated manually or with the aid of specialized equipment, such as computer-aided dynamometry (e.g., Biodex, Cybex, Med-X, and Promotron).
Manual muscle testing procedures have been extensively described for isolating specific muscle function.455 Manual resisted muscle tests are performed to assess the strength and sensitivity of muscle and its tendinous attachments (Figure 3-30). Any noted muscle weakness should be recorded and graded on a five-point system (Box 3-13). Muscle testing procedures are numerous, and descriptions of individual procedures are beyond the scope of this text. The reader is encouraged to refer to any number of excellent texts for detailed descriptions on how to perform individual muscle tests. Pain with muscle contraction may indicate a muscle injury, a joint injury, or a combined muscle and joint injury. Pain with isometric contraction generally indicates a muscle injury rather than a capsular injury.22 Isometric muscle contraction, however, may still produce some degree of joint compression and capsular tension. To differentiate a purely muscular injury from a capsular injury, passive joint movement and compression must be performed and their results compared with the response elicited during isometric muscle contraction.19,22

Figure 3-30 Resisted muscle tests evaluate strength and sensitivity at the tendinous attachments (e.g., left psoas muscle test.)
A capsular injury produces pain with passive and active movements as the capsule is elongated. A purely muscular injury produces pain with muscle contraction and muscle elongation, but passive shortening of myofascial tissue should not be painful.
The small segmental muscles of the back are not independently accessible to palpation or specific muscle tests. Injuries to the deep segmental muscle of the back cannot be easily differentiated from other injury or dysfunction of the spinal joints. Therefore, muscle testing in the back is used primarily to differentiate injuries to the large, nonsegmental back muscles from dysfunction or injury to the spinal joints and their associated soft tissues.
Within the chiropractic profession, manual muscle testing has also been used to evaluate spinal joint function and the health and function of other organ systems of the body. Central to the use of these procedures is the premise that changes in muscle strength can be affected by functional and pathologic changes in other tissues of the body.456 Muscle testing in this capacity is controversial and typically is used by professionals who use procedures associated with the technique of applied kinesiology.
The applied kinesiology technique proposes the use of manual muscle tests coupled with the use of applied vertebral pressures to determine the level and direction of spinal subluxation. This procedure is commonly referred to as the vertebral challenge.456
The vertebral challenge involves digital pressure applied by the examiner against spinal bony landmarks as the examiner simultaneously evaluates the strength of a selected muscle. The tested muscle is evaluated for its ability to resist torque and maintain a locked position. If the muscle gives way under pressure, the test is considered positive and the level of spinal contact is considered a site of dysfunction.
During testing, the contacted vertebra is pushed (challenged) in different directions. If the muscle gets weak, the assumption is that the segment is being directed more into a subluxated position. If the muscle remains strong or gets stronger, the assumption is that the vertebra is being pushed out of its subluxated position. It is believed that all muscles of the body are temporarily inhibited by stimulation of subluxated segments. Therefore, any muscle of the body can be selected as the “indicator muscle” during the use of this procedure.
This procedure is often performed as a rebound challenge. This procedure is based on the premise that subluxation syndromes are associated with hyperactivity in segmental muscles. The rebound challenge is performed by the application and quick release of spinal pressure.456 During testing the contacted vertebra is pushed (challenged) in different directions. The rebound phase is represented by the quick release of applied pressure.
If this method is used in a direction that stretches hyperactive muscle, it is assumed the hyperactive muscle will contract against a quick stretch and pull the vertebra farther into its malpositioned state during the rebound phase. If the vertebra is pulled farther in the direction of malposition, a weak muscle response is predicted. Therefore, a weak muscle response during the rebound phase indicates that a segment should be adjusted in the direction of the applied testing force.
The vertebral challenge and rebound vertebral challenge have not been extensively evaluated. The few studies that have been conducted have demonstrated poor intraexaminer and interexaminer reliability and no responsiveness to adjustive treatments.457,458
Provocative (orthopedic) tests
Provocative testing covers a wide range of manual testing procedures, many of which have already been discussed. Provocative procedures are tests that are conducted to reproduce a specific sign or accentuate pain. The major purpose of testing is to locate the anatomic site responsible for producing the patient’s pain. Provocative orthopedic tests represent a separate category of named procedures designed to use movements or positions to localize the source and nature of the patient’s disorder. The procedures are commonly labeled with the name of the original innovator (e.g., Kemp test) or carry a descriptive label (e.g., straight leg raise test).
Named provocative orthopedic procedures are not commonly cited because many procedures are not applicable to the identification of spinal subluxation/dysfunction syndromes. They are helpful in identifying the anatomic location of painful complaints and discriminating between mechanical, nonmechanical, and NR pain. They have demonstrated less value in discriminating between conditions.197 Orthopedic tests are also helpful in identifying possible contraindications to adjustive therapy and monitoring patients’ response to treatment.459 Evans provides an excellent description of spine and extremity provocative orthopedic tests, including how they are performed and interpreted.459
Radiographic analysis
Radiographic assessment and determination of joint subluxation have been an integral part of chiropractic evaluation since the early 1900s.335,460,461 Ever since Sausser first made a full-spine exposure, the chiropractic profession has desired and sought out methods for marking x-ray films to identify manipulable lesions. The history of chiropractic marking procedures dates back to 1910462 when it was first introduced in the Palmer School curriculum.
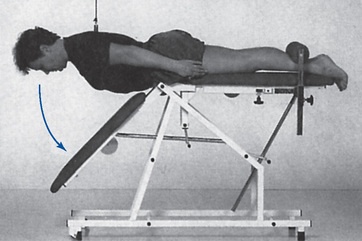
The early use of diagnostic x-ray examinations in the chiropractic profession centered on the assessment of biomechanical relationships and the measurement and description (listing) of spinal joint malpositions. To that end, the profession and many of its individual technique innovators have developed specific radiographic measurement techniques (spinography) designed to quantify and classify spinal malpositions and subluxations (Figure 3-31).32,128,461,463 464 465 466 467
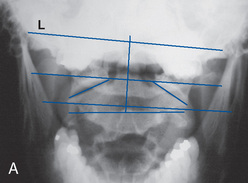
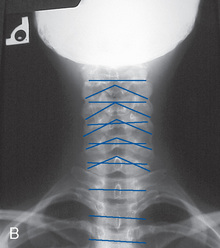
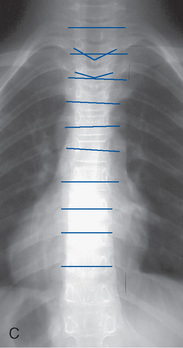
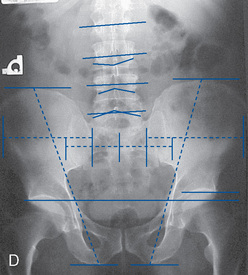
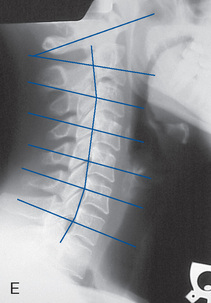
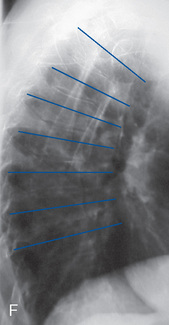

Figure 3-31 Static spinographic measures. A, Anteroposterior open mouth. B, Anteroposterior lower cervical. C, Anteroposterior thoracic and D, anteroposterior lumbar and pelvis. E, Lateral cervical neutral. F, Lateral thoracic and G, lateral lumbosacral.
Although many “systems” to detect static subluxations on x-ray films have emerged over the years, these procedures remain controversial. Criticism and failure of the static x-ray marking systems come from trying to use quantitative measures on landmarks that vary and that are subject to geometric distortion.468 Moreover, the spine and its functional units are living, moving, and dynamic structures that depend on complex relationships among bones, ligaments, and muscles. Plain-film x-ray examination does not evaluate movement of the spine, nor does it directly assess the soft tissues.
Although the limitations of radiographic marking systems are well established469 (Box 3-14), static alignment abnormalities can have some significance when taken in context with other clinical, historical, and laboratory findings. In recent years, more emphasis has been placed on the dynamic concepts of the subluxation complex, in some cases totally disregarding static biomechanical relationships. Sandoz470 feels that this shift of emphasis is counterproductive. He suggests considering the mechanical, static, and dynamic concepts in harmony with the neurologic and reflex elements of spinal subluxation/dysfunction.
Over the years, the role of x-ray examination has been modified according to scientific and technical developments, as well as to philosophic tenets and beliefs. Sherman462 summarized the clinical rationale for the use of x-ray examination in chiropractic (Box 3-15). Evidence-based diagnostic imaging practice guidelines have been developed.471 472 473 474 They are intended to assist primary care providers, interns, and residents in determining the appropriate use of diagnostic imaging for specific clinical presentations. In all cases, the guidelines are intended to be used in conjunction with sound clinical judgment and experience. The goal of these guidelines is to avoid unnecessary radiographs, increase examination precision, and decrease health care cost without compromising the quality of care.471 Ammendolia and co workers475 surveyed chiropractic colleges around the world to evaluate whether imaging guidelines were being taught and adhered to. The results of this study suggest that instruction provided at most chiropractic schools appears to adhere to evidence-based guidelines for LBP with respect to the use of routine radiography, full-spine radiography, and oblique views, but there appears to be some disparity between instruction and existing evidence for the use of radiography in acute LBP.475
Spinal X-ray Examinations
Historically, the use of spinal radiography examinations in chiropractic centered on the detection and quantification of the intervertebral misalignment.476 Proponents of radiographic evaluation for the detection of spinal subluxations claim that x-ray examinations are the best method for accurately determining the level and direction of vertebral malposition.460 They contend that chiropractors who do not use radiography to evaluate spinal subluxations are at a disadvantage in determining and delivering indicated and safe adjustments. In the 1970s, this view produced a policy requiring chiropractors to demonstrate radiographically the presence of spinal subluxations to treat and receive reimbursement for Medicare patients. This policy has been recently modified and was rescinded in 2000 in favor of the PART multidimensional index for joint dysfunction.
Preadjustive x-ray examinations are also rationalized as necessary because the treatment incorporates the use of force. It is reasoned that the integrity and mechanical characteristics of the spine should first be screened radiographically before adjustments are made.476 This position is controversial and unsubstantiated. Screening x-ray examinations taken without clear clinical guidelines have not correlated with improved diagnosis or patient outcome.477,478 Furthermore, thrusting forms of manipulation have been used safely for centuries without the aid of x-ray examinations.
Spinal x-ray examinations are usually taken with the patient in an upright, weight-bearing position and should consist of two views, typically an anteroposterior and lateral projection. Traditionally, the alignment of the upper vertebrae is compared with that of the lower vertebrae, and any malpositions are recorded.32,128,460
Full-spine radiographs are used primarily for biomechanical evaluation, including the assessment of individual motion segment alignment. Full-spine evaluations provide an integrated view of spinal biomechanics and are the method of choice in the evaluation of spinal scoliosis. Full-spine radiographs, however, compromise bony detail and should not be used as a routine procedure for the assessment of suspected local pathologic conditions.469,479,480
“The clinical justification for the full-spine radiograph must insure that the benefit to the patient is greater than the radiation hazard. The film must be of such quality that the presence or absence of pathology can be determined.”481 When indicated, consideration should be given to full-spine posteroanterior projections to improve visualization of the lumbar IVD spaces and to minimize exposure to the ovaries and breasts.31,461
Although the majority of the profession uses some form of radiographic measurement and assessment of spinal subluxation, there is considerable controversy as to whether radiographic evaluation should play a significant role in the diagnosis of spinal subluxation syndromes.* Claims of accuracy in detecting minor joint malpositions may not be supportable against the technical limitations of radiography.† Inherent radiographic magnification and distortion, patient positional errors, and the exactness of the marking procedures are common concerns.
The lack of a consensus on the definition, pathophysiology, and pathomechanics of spinal subluxations further complicates the debate and analysis of x-ray marking procedures. Therefore, the clinical significance of these measurements is controversial and suspect. Radiographic measures should not be the primary criteria used to perform chiropractic care.489 However, if there were a clinical indication for taking a radiograph, it would be imprudent not to evaluate the x-ray examinations for biomechanical relationships and look for correlations to other clinical findings.
The process of critically evaluating radiographic marking procedures has only begun in the last several decades.335,478,490 491 492 493 494 495 The process is in its infancy, and a limited number of studies have been conducted. A significant number of procedures have yet to be evaluated. Although it is difficult to draw firm conclusions, it is possible to briefly summarize the present state of affairs.
First, many of the radiographic marking procedures used to evaluate segmental spinal alignment can be reliably performed.* However, most of the reliability studies do not include a full evaluation of all the steps involved in performing and determining segmental alignment. Many of the studies did not include patient positioning. Consequently, at this time it is difficult to conclude whether x-ray marking procedures are or are not reliable for identifying spinal motion segment subluxations.469
Although recent attempts have been made to address issues of spinographic reliability, very little has been done to investigate the validity of radiographic measurement in diagnosing and treating spinal dysfunction.338,470,476 477 478496,497,
Spinal displacement analysis has not demonstrated the ability to identify an established clinical entity nor demonstrated its value as an independent outcome measure. The validity and clinical usefulness of static marking procedures for identifying treatable motion segment misalignment have not been demonstrated.488
A retrospective case analysis performed in 1990 identified only one postmanipulation segmental spinographic change, that being a reduction in retrolisthesis. There was no identified change in cervical lordosis, sacral base angle, lumbar lordosis, scapular angle, or Cobb angle.489 Yi-Kai and coworkers504 investigated the relationship between radiographic signs of subluxation in the cervical spine and their clinical diagnostic value. They concluded that there was little evidence to support the contention that signs of subluxation in the cervical vertebrae are diagnostically significant in identifying individuals with cervical pain. In addition, static marking procedures have not been found to discriminate between those with back pain and those without back pain.338,505
Harrison et al483 reviewed the literature on the reliability and clinical value of spinal displacement analysis in plain-film x-ray examinations, concluding that x-ray line drawing is a reliable and effective outcome measure. The conclusion is based on their assertion that there is an ideal normal spinal configuration based on a mathematical model and that radiographic marking procedures can identify real spinal displacements. However, the vast majority of cited reliability studies were on curve measurements, not spinal segment position.
Haas and colleagues469 challenged Harrison and colleagues conclusions483 by questioning the biologic plausibility of an ideal spine model and the authors’ failure “to present any credible evidence for the validity, clinical utility and appropriateness for using these procedures.” Haas and colleagues469 conclude that there is currently no justification for the routine use of radiographic spinal displacement analysis in clinical practice.
Functional X-ray Examination
The potential limitations of static radiographs in determining joint dysfunction has led to increased use of functional x-ray studies.51,506 507 508 509 510 The principal attraction of functional x-ray examinations is the ability to assess joint mobility and identify disturbances in function that might not be represented by static films. Functional x-ray studies involve the evaluation of regional and segmental spinal movements by comparing range and pattern of movement at each segmental level. A series of three views are typically taken for each plane of movement evaluated: an end-range view in each direction and a neutral view. These views are then used to measure and evaluate restricted or aberrant segmental movements.
Although the use of dynamic x-ray examinations overcomes concerns about the inability to functionally assess the spine with static x-ray examinations, there remains considerable controversy as to their contribution in predicting back pain or differentiating those individuals with back pain from those without. Methods for measuring and classifying segmental motion abnormalities in the lumbar spine and cervical spine are in common use.51,164,506 507 508 511 512 513 Taylor478 suggests that functional radiography should be used to establish the presence of the following:
Flexion-Extension Radiographs
Those investigating the relationship between spinal pathologic conditions and segmental movement have demonstrated supportive evidence for the use of flexion-extension studies in the detection of spinal instability.167,478,506,514 Flexion-extension studies are used to identify excessive angular or translational movements between spinal segments (Figure 3-32).478,515,516 The amount of translation or angular movement necessary to define instability is not definitively established. Most references classify any flexion-to-extension translation greater than 3 to 5 mm as indicative of instability.478 Dvorak and colleagues517 suggest that applying global overpressure at the end ROM during a functional x-ray examination may aid in identifying translational movement characteristics of instability.
Clinical validity studies have been done for flexion-extension radiographs of the lumbar and cervical spine.518,519 The conclusions were that the functional studies did show a tendency for the presence of hypomobility in patients with clinical problems, but they were not sufficient to aid in differentiating the underlying pathologic conditions.
In the cervical spine, flexion-extension studies are used most commonly to ascertain if a traumatic injury has resulted in instability. Translational movements of more than 3 mm are considered a significant finding for instability of the cervical spine. In the cervical spine, an overlay method may be used for templating flexion and extension (see Figure 3-32).
Lateral-Flexion Radiographs
Lateral-flexion (side-bending) radiographs are used predominantly in the evaluation of the lumbar spine. Interpretation of the films incorporates the use of lines and angles that are drawn on the films for the purpose of quantifying and gauging comparative quality of joint motion.
The total range of regional lateral flexion is determined by extending a line from the superior end plate of the uppermost vertebra and the inferior end plate (or sacral base) of the lowest vertebra in the concavity of the curve. Perpendicular lines are constructed from each of these with the angle formed at their intersection, establishing the limit of lateral flexion (Figure 3-33).
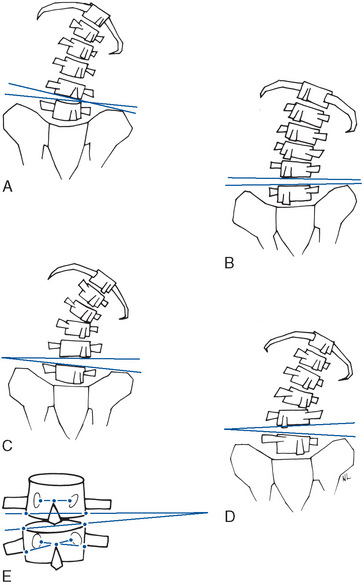
Figure 3-33 Evaluation of functional lateral bending radiographs in the lumbar spine demonstrating movement patterns. A, Type I, lateral bending with contralateral rotation. B, Type II, lateral bending with ipsilateral rotation. C, Type III, contralateral bending with contralateral rotation. D, Type IV, contralateral bending with ipsilateral rotation. E, Segmental measurement methods for determining rotation in millimeters and lateral flexion in degrees.
(A–D from Grice A, Cassidy D: J Manipulative Physiol Ther 2:18, 1979; E from Haas M, Nyiendo J, Peterson C: J Manipulative Physiol Ther 13[4]:179, 1990.)
The films can then be marked for segmental rotation and lateral flexion. The body-lamina junction is used for rotation and the end plate angulation for lateral disc wedging. Aberrant lateral flexion can be assessed by using superior end plate lines and evaluating if they converge toward the side of lateral bending (see Figure 3-33).
Early investigation into the value of functional radiography did identify its merit in the diagnosis of sciatica,520 although abnormal lumbar motion was also noted in asymptomatic patients. Vernon509 concluded that there was a higher prevalence of abnormal lateral bending patterns in symptomatic subjects, but Phillips et al329 and Haas and colleagues332,333 failed to demonstrate a relationship between abnormal spinal motion and patients suffering from LBP.
Although these procedures have demonstrated limited predictive value in differentiating individuals with back pain from those without, their value in managing patients with back pain has not been fully assessed. Using side-bending stress x-ray studies to help ascertain abnormalities of intersegmental motion in individuals with back pain in theory, may affect clinical decision-making in a manner that improves patient outcome. In this context, evaluation would be qualitative and quantitative. The detection of hypomobility, paradoxical motion (reversal of an unexpected motion or aberrant motion), or excessive motion would have precedence over exact measurements.
Identifying levels and directions of decreased movement might affect decisions on where and how to make adjustments in ways that improve patient outcome. This may be particularly applicable in individuals with persistent pain or patients who have not been responsive to treatment. The answers to these questions await further research.
Videofluoroscopy
Videofluoroscopy (VF) of the spine is another radiographic procedure that has been proposed as a potential tool for the assessment of segmental spinal motion. Before the development of VF, cineradiography (CR) was the main radiographic method used to evaluate spinal motion. Fielding521 first described its use for the cervical spine, and Illi was the first to use CR in the chiropractic profession to study spinal segmental and sectional motion. He was followed by Rich and Goodrich in the 1960s. Howe57,522 performed numerous studies, and this procedure became an experimental procedure at a number of institutions. The major drawback to CR was that it involved taking 16-mm movies during which substantial radiation exposure (often exceeding 10 or 20 radiation absorbed doses) was applied to the spine.
VF development has led to improvements in image intensifiers and digital recording technology that has resulted in far fewer radiation doses and increased interest in recent years.523,524 VF has the capabilities to measure the full arc of motion and therefore provides information on the quality of motion in addition to the ROM. This allows the clinician to see aberrations in the mid-ROM, as well as at the extremes. Advocates of VF suggest that these studies provide objective evidence of biomechanical abnormalities not seen with other studies. This technology has made significant advances, and the new techniques of digital VF (DVF) have dropped the radiation exposure rates considerably below those of the conventional x-ray examination.525,526 When appropriate equipment and calibration are used, the procedure has demonstrated promising interobserver and intraobserver reliability, with measurement accuracy between 1 and 2 degrees.525 526 527
Although DVF holds significant promise in the assessment of spinal mechanics, it is presently in the investigational stage, without established clinical protocols for use. It should be stressed that spinal VF is a special test with several limitations and disadvantages (Box 3-16). Much research is necessary to precisely define the role of VF in chiropractic.
In clinical practice, VF should be considered an experimental procedure, and its use should be reserved for complex cases that fail to respond, that respond poorly to a trial of conservative management, or in which suspected ligamentous damage leading to instability has occurred. Growing concern about the inappropriate use of VF has led to the formation of protocols for the use of VF in chiropractic by the American Chiropractic College of Radiology, a branch of the ACA. These protocols should be followed when contemplating the use of VF.528
Clinical Use of X-ray Examination
The clinical utility of static and functional radiographs might be improved if these procedures were placed in a proper clinical perspective and considered a component of evaluation and not a pathognomonic indicator of JSDSs. With further refinement, they may eventually parallel a role provided by specialized imaging techniques in the structural detection of IVD derangement.
For example, the presence of IVD derangement on a CT scan or an MRI indicates the presence of anatomic derangement of the IVD, but it does not confirm that the disc derangement is of clinical significance. The incidence of radiographically detected disc derangement in asymptomatic patients is significant (24% to 37%), suggesting that there is a poor correlation between mechanical disc derangement and morbidity.529 Within this context, it becomes apparent that the imaging findings must be matched to the clinical presentation and physical findings before a final impression is established. The role of x-ray examination in the evaluation of spinal subluxation/dysfunction syndromes (JSDS) should play a similar purpose. Radiographic findings alone cannot identify whether a given joint subluxation/dysfunction is clinically relevant and worthy of treatment. They must be placed within the context of the physical examination and patient complaints.
This discussion on the use and application of radiography has been directed toward its relationship to the detection of joint subluxation/dysfunction. This is not meant to imply that chiropractors use x-ray examinations to detect joint subluxation/dysfunction only. They are commonly used to investigate fractures, pathologic conditions, and biomechanical integrity.
A rational for the use of plain-film imaging in the chiropractic office is (1) to assist in the establishment of a working diagnosis when clinically indicated, (2) to rule out the presence of pathologic conditions that contraindicate manipulative therapy, (3) to identify any anomalies or structural changes that may influence how an adjustment will be made, and (4) to determine static and functional biomechanical relationships that may have clinical relevance to the patient’s symptoms or health.
No one tool should be used to make clinical decisions, and x-ray interpretation should not be an exception. The fundamental principles in the use of radiology that are of prime importance and that should be considered before x-ray examinations are ordered are identified in Box 3-17.
Instrumentation
In the absence of a “gold standard” for the assessment of characteristics associated with joint subluxation/dysfunction syndrome (JSDS), the chiropractic profession has sought an instrument that would objectively measure and quantify its presence.
However, even if such an instrument existed, it would likely be limited to the identification of only a single clinical characteristic or finding. This finding may be associated with joint subluxation/dysfunction or with other clinical entities. Therefore, no single tool should be relied on to make the diagnosis or assessment of subluxation/dysfunction syndrome.
The following tools represent means to identify specific characteristics potentially associated with joint subluxation/dysfunction. Although most have fair to good reliability, their validity has not been adequately determined or tested. Moreover, some proponents of specific instruments have made inappropriate claims about the value of the information gleaned from the instruments.
Algometry
Algometry is the measurement of pain. Algometers are force gauges that are used to quantify the amount of pressure necessary to elicit a painful response (Figure 3-34). Algometers are used at both bony and soft tissue sites. Algometric measurements represent the point of maximal pressure the patient can tolerate (pressure tolerance [PTo]) or the point at which pressure induces pain (pressure pain threshold [PPT]).
PPT is alternatively referred to as the first verbal report of pain. PTo is alternatively referred to as the pain reaction point (PRP), the point at which the patient reports that it “hurts a lot.” PPT measurements are more commonly used because they are less intrusive.
To evaluate the patient’s PPT, the examiner places the rubber-tipped stylus of the algometer over the site to be evaluated and applies steady, gentle pressure at a rate of approximately 1 kg/sec. Pressure is applied until the patient feels pain and responds by saying “now.” At this point the stylus is removed, and tender sites and their pressure values are recorded.
Normative PPT values for muscle and bone have been established, and repeated measures have demonstrated good reliability.530 531 532 533 534 535 536 Algometry is presented as an effective tool for evaluating painful musculoskeletal complaints.537 It has demonstrated reliable measurement of pain in temporomandibular joint dysfunction,536,538 myofascial trigger point syndromes,534 muscle tension headache,539 and the ability to differentiate patients with inflammatory arthritis from healthy controls.540 Algometry is responsive to treatment, effectively documenting increased PTos in disorders treated with adjustive therapy.541,542 Algometry has been used most commonly in research settings, but its ease of use, low-tech application, and affordability make it appropriate for use in clinical practice.
Thermography
Medical thermography is the technique of measuring and recording heat emission from the body. The body radiates heat in a symmetric pattern, with only minor variation in temperature from side to side. In a healthy individual, temperature radiation is regionally symmetric to within 0.5 to 1 degree centigrade.543,544
The most common devices used to assess human heat emission are electronic infrared and liquid crystal appliances. Significant asymmetry in heat emission has been postulated as objective evidence of a variety of underlying disorders and painful complaints. In manual medicine, thermography is most frequently discussed as a noninvasive means to detect functional changes that may be associated with disorders of the NMS system.
Christiansen,545 in a review of the literature, found thermography compared favorably with other diagnostic tests (e.g., myelography, EMG, and CT) for accuracy and sensitivity in determining the level of radiculopathy while demonstrating high correlation with these more invasive tests.546 A hand-held device that uses either infrared contact thermistors or thermocouples may be used. This device is used to detect regional variations in midline spinal temperature or variations in segmental paraspinal temperature. The temperature differential is usually displayed on a calibrated galvanometer or plotted on a strip graph.
The thermocouple device is constructed to make physical contact with the surface of the body and measure differences in segmental paraspinal temperature (Figure 3-35). Deflection of the needle will be to the relatively warmer side. Alteration in segmental temperature is speculated to represent objective evidence of spinal subluxation/dysfunction syndromes. It is postulated that spinal subluxation/dysfunction may produce a local inflammatory reaction or reflex alteration in sympathetic tone, which in turn alters the segmental temperature symmetry of the body.547 548 549 550 551
Although some techniques advocate using hand-held heat detection instruments for spinal subluxation/dysfunction detection, very little research has been conducted on the reliability or validity of these devices. Normative values for hand-held devices have not been established, and reliability studies are very limited. To date, no studies have been conducted to evaluate their validity in determining spinal dysfunction.552 Further research is needed to confirm or refute the theories, indications, and limitations of these devices.553
Galvanic Skin Resistance
Galvanic skin resistance (GSR) is the measure of the skin’s electrical conductivity. Galvanic skin instruments measure the resistance of the skin to a small electrical current. It has been suggested that spinal dysfunction may alter skin conduction by inducing sympathetically mediated changes in sweat gland secretion (somatovisceral reflex).554 Conductivity of the skin is significantly affected by its moisture content and sweat gland activity.555
Spinal dysfunction is hypothesized to alter conduction by either increasing or decreasing sweat gland activity. Spinal dysfunction that leads to increased peripheral autonomic activity and sweat gland secretion could increase segmental conductance. Spinal dysfunction that leads to inhibitory autonomic activity could result in a decrease in skin conductance. The presence of pain has also been shown to induce a segmental decrease in GSR.556,557
Ease of access to the skin makes GSR an uncomplicated tool for measuring autonomic effects that may be associated with spinal dysfunction. GSR has been used in experimental settings on a very limited basis. Its clinical value remains to be evaluated, and it is seldom, if ever, used in the day-to-day clinical evaluation of joint dysfunction.
Surface Electromyography
A method purported to assess a specific characteristic of spinal dysfunction is paraspinal EMG scanning. Paraspinal muscle dysfunction is considered a clinical manifestation of joint subluxation/dysfunction syndrome, and surface EMG is presented as a method that can provide an objective quantitative evaluation of changes in paraspinal muscle function.
EMG is a technique for recording electrical potentials associated with muscular activity. This is considered important to clinicians because it represents the outflow of motor neurons in the spinal cord to the muscle as a result of voluntary or reflex activation.558 Either needle electrodes or surface electrodes can be used to study paraspinal or peripheral muscle function. However, needle electrode and surface electrode EMGs are not interchangeable procedures.559 Needle electrode techniques are indicated for the evaluation of specific muscles, innervation potentials, and myopathies. Surface electrode techniques are indicated for kinesiologic studies of the global function of groups of muscles.
The muscle activity that is recorded by the various paraspinal scanning machines are relative values, relating to resting and contractile muscle states. Muscle unit action potentials are amplified by the EMG machine. The responses are filtered and rectified by the instrument. These rectified responses are bidirectional waves of depolarization and repolarization along cell membranes. They are integrated over time, and analog signals are converted to digital signals.
Surface electrode EMG with attached electrodes has been shown to exhibit very good to excellent test-retest reliability.560 561 562 563 564 565 In a comprehensive review article comparing the properties of fixed-surface electrode EMG and intramuscular EMG, Turker558 identified that both procedures have indicated uses. Surface electrode EMG was found to be more prone to electrical artifacts, mechanical artifacts, and contamination from the activity of other muscles than intramuscular EMG. However, it is possible to make useful recordings with the surface electrode from large superficial muscles if appropriate precautions are observed.
In a comparison study using needle electrode and fixed-surface electrode EMG, evaluated muscles were electrically silent, during standing and full flexion. The use of fixed-surface electrodes provided recordings that were similar, although slightly dampened, to those obtained with intramuscular wire electrodes.566 The surface measurements were found to accurately document the function of back muscles, permitting the use of fixed-surface electrode EMG in outpatient care. Furthermore, fixed-surface EMG has been shown to provide a very valuable set of data used diagnostically with pain-related disorders.567
Scanning-surface EMG should not be confused with surface EMG that uses fixed-surface electrodes. Electromyographic muscle scanning measures 2-second samples of integrated muscle action potentials from individual neck and back muscles using a hand-held scanner with post-style surface electrodes separated by a fixed distance. This scanning technique is used to expeditiously assess muscle activity in the diagnosis of musculoskeletal disorders.564,568 The signal recorded by the apparatus is a transient signal. There are a number of potential technical problems with this equipment, including low signal or noise ratios; movement signal artifacts (because the surface electrodes are not fixed to the skin); and other sources of signal artifacts, such as those from the heart and great vessels. Surface-scanning paraspinal EMG gives a rough estimation of transient muscle activity. It cannot give information about specific muscles because the recording electrodes are placed over the skin and not into a muscle.
Thompson and colleagues564 report that their study supports hand-held post-style electrodes as providing a satisfactorily stable means of monitoring the surface EMG signal. However, they also identify that the 2-second integration period may be inadequate, favoring instead a 10-second integration, especially in research and treatment outcome studies. When attention is directed to scan preparation, hand-held EMG sensors produce dependable results. The reliability of the surface EMG scanning procedure was investigated using a large clinical sample; the results indicated that with adequate attention to scan preparation, EMG sensors held in place by hand with light pressure produced dependable results. The pattern of reliability was seen to be slightly higher in the lower back on patients in the standing position.569
Questions regarding surface electrode EMG’s validity and usefulness exist, yet its use is often embraced by many without reserve.570 Lehman conducted three experimental studies to evaluate surface electrode EMG for asymmetry and repeatability in populations with LBP and populations without LBP. He concluded that EMG signals during quiet stance show excellent repeatability but segmental differences in asymmetry between problematic and nonproblematic segments were not evident. This suggests that the diagnostic validity of EMG evaluations during simple quiet-stance tasks is highly suspect. Ritvanen et al571 also found no positive nor statistically significant association between back pain and EMG parameters.
Surface-electrode EMG has the potential to assist the doctor in evaluating the patient’s response to treatments.559 Myerowitz,572 using hand-held scanning electrodes, evaluated the relationship between post-treatment paraspinal surface EMG improvement and improvements in spinal pain or related musculoskeletal symptoms. He treated 42 symptomatic patients with pain and abnormal scanning surface EMG findings. All 42 patients had post-treatment improvement on scanning-surface EMG readings, and 41 patients (97.6%) reported post-treatment reduction in the pain symptoms. This study raises the possibility of using hand-held scanning surface EMG to correlate EMG activity to symptomatic improvement in common conditions of spinal pain and related musculoskeletal symptoms.
Although scanning-surface EMG has generated some enthusiasm in the profession, the use of scanning surface paraspinal EMG for the detection of spinal subluxation syndromes must be questioned.573 The profession, in attempting to document intersegmental dysfunction, has jumped too quickly onto an unproven application.574 Aside from the potential hardware problems presented, chiropractors must question the need for the routine use of an examination procedure that tells the doctor there is some local muscle tone alterations. Chiropractic doctors have sufficient training and palpation skills to assess contracted muscles, and the cost generated by this technology may not be warranted.
Scanning-surface EMG may have potential value as an outcome measure, but its validity in detecting joint subluxation syndromes has not been substantiated. The important clinical questions remain unanswered. Instruments, including scanning-surface EMG, must be evaluated within a clinical context. The interpretation of information derived from these instruments and how it affects clinical decisions and treatment is the determining factor in establishing its validity and clinical utility.575
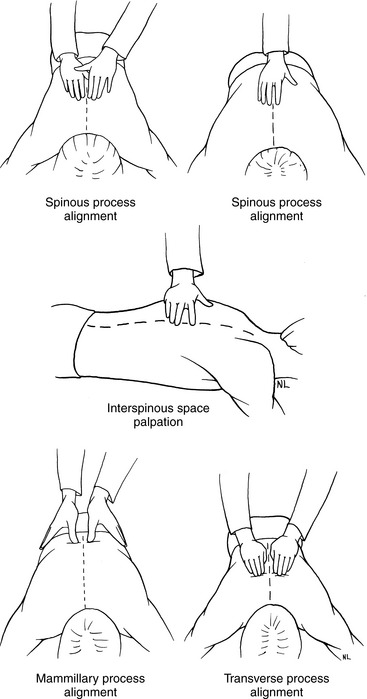
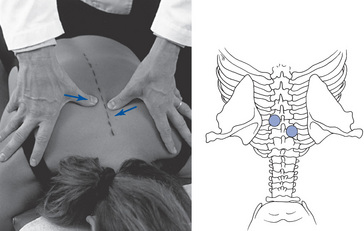
 Figure 3-26
Figure 3-26