Chapter 3 Joint Assessment Principles and Procedures
The doctor of chiropractic views the human being as a dynamic, integrated, and complex living thing who has an innate capacity for self-healing.1 2 3 4 5 6 Chiropractic health care focuses on the evaluation and treatment of neuromusculoskeletal (NMS)-based disorders, but does not disregard the multiple potential causes of ill health and the complex nature of health maintenance.7,8
In keeping with this philosophy and the responsibility as “portal-of-entry” health care providers, chiropractors must maintain broad and thorough diagnostic skills. The Council on Chiropractic Education (CCE) defines the primary care chiropractic physician as an “individual who serves as a point for direct access to health care delivery; the doctor of chiropractic’s responsibilities include (1) patient’s history; (2) completion and/or interpretation of physical examination and specialized diagnostic procedures; (3) assessment of the patient’s general health status and resulting diagnosis; (4) provision of chiropractic care and/or consultation with continuity in the co-management, or referral to other health care providers; and (5) development of sustained health care partnership with patients.”9 Before applying therapy, the chiropractor must first ascertain if there is a clinical basis for treatment. The chiropractic physician who chooses to limit therapeutic alternatives must still possess the skills necessary to determine if patients seeking their care have a health problem responsive to the specific treatments they provide.10 This dictates that chiropractors be trained to screen and evaluate a broad range of complaints if they wish to maintain their primary contact privileges. Diagnostic skills must have sufficient depth to screen all organ systems of the body for those conditions that are and are not amenable to chiropractic treatment. The social expectation and regulatory requirement of a primary contact provider are to provide a suitable health status assessment and initial clinical impression regardless of the patient presentation or the health care professional’s particular discipline, philosophy, or theories.
A core area of focus and expertise for the chiropractic physician is the evaluation of the NMS system. This chapter focuses on the knowledge, principles, and evaluation procedures central to the process of determining whether a patient is a candidate for adjustive therapy.
The manipulable lesion
Manual therapy has been proposed as an effective treatment for a wide variety of conditions, but it is most commonly associated with disorders that have their origins in pathomechanical or pathophysiologic alterations of the locomotor system and its synovial joints. As a result, manual therapy is based on assessment procedures that take into consideration both functional and structural alteration of the NMS system. Haldeman11 has referred to this process as the identification of a manipulable lesion. Spinal manipulation is thought to act on this manipulable or functional joint lesion, but given the historical presumption of this entity, it is somewhat surprising that there is not more information on its pathomechanical properties.12 The lesion is viewed as a set of possible individual maladies responsible for the patient’s symptoms.13,14
The identification of the common functional and structural components of the manipulable lesion is critical to the management of this condition, but it has also contributed to the misconception that all manipulable disorders have the same pathologic basis. The overwhelming majority of disorders effectively treated with chiropractic adjustments do display joint and somatic functional alterations, but many pathologic processes can induce joint dysfunction.
A diagnosis of joint dysfunction syndrome identifies local altered mechanics, but it does not identify the underlying nature of the dysfunction. Although joint derangements may present as independent clinical syndromes, they are more commonly associated with other identifiable disorders and injuries of the NMS system.15 16 17 18 19 20 21 22 23
If chiropractors limit their examination to the identification of structural or functional signs of joint dysfunction, they may minimize the extent of the disorder and the effectiveness of their treatment. For example, both the patient with acute disc herniation and the patient with acute facet syndrome present with clinical signs of joint dysfunction. An evaluation confined to the detection of joint dysfunction might not uncover the underlying pathomechanical and pathophysiologic differences between these two conditions and the distinctions in therapy that might be necessary. Furthermore, other disease states or traumatic events that would contraindicate adjustive therapy may induce spinal malpositions or fixations.
A singular diagnosis of joint dysfunction or subluxation syndrome should be reserved for instances when it is determined to be the sole identifiable lesion; the terms should not be used as a category for all conditions treated with adjustive therapy. When joint dysfunction is perceived as the sole cause of the disorder being considered for treatment, adjustive therapy may be the only treatment necessary. However, when joint dysfunction is secondary to other disorders that are not responsive to adjustive treatments, other effective treatments should be provided or made available to the patient by referral.
Determination of the appropriateness of adjustive therapy should not be based on the presence of a fixation, malposition, or spinal listing alone. The cause of the altered mechanics indicates whether adjustive therapy or some other form of therapy is in order.23
Subluxation
Within the chiropractic profession, the manipulable lesion has been equated primarily with the term joint subluxation. The concept of subluxation is a central defining clinical principle and the source of contentious debate and disagreement within the profession.24 Mootz suggests that the chiropractic profession’s attention to subluxation (pro and con) is found in virtually every dimension of the profession’s existence, be it clinical, scientific, philosophical, or political.25 He identifies four distinct ways that subluxation is used by the profession, each with merits and liabilities. They are25:
Historically, joint subluxation was defined predominantly in structural terms.1,2,23,26 27 28 29 30 The founder of chiropractic, D.D. Palmer, defined joint subluxation as a “partial or incomplete separation, one in which the articulating surfaces remain in partial contact.”31 Central to Palmer’s original subluxation hypothesis was the concept that vertebral subluxations could impinge on the spinal nerve roots (NRs) as they exit through the intervertebral foramina. This was postulated to obstruct the flow of vital nerve impulses from the central nervous system to the periphery and to induce lowered tissue resistance and potential disease in the segmentally innervated tissues.1,2,8,29,31 32 33 34 35 Palmer went so far as to suggest that the primary cause of all disease could be related to subluxations and interruption of normal “tone—nerves too tense or too slack.”1,8
The most impassioned supporter of this concept was D.D. Palmer’s son, B.J. Palmer. Throughout his career, B.J. Palmer ardently promoted a monocausal concept of disease,8,27,28,36,37 specifically stating that chiropractic is “a science with provable knowledge of one cause of one disease being an internal interference of the internal flow of abstract mental impulses or nerve force flow supply, from above down, inside out.”36
Although the profession today emphasizes the important relationship between health and the structure and function of the NMS system,4 5 6 7 32 33 34 3538,39 it does not promote a monocausal concept of subluxation-induced disease.7 8 9 10 37 38 39 40 The monocausal concept runs contrary to much of the profession’s recent literature24,34,35,37 38 39 and to the view held by the overwhelming majority of practicing chiropractors.8 Although a small minority of chiropractors still promotes this extreme view, both the profession’s national associations and the CCE have disavowed it.9,39
Beginning with the published work of Gillet,41 42 43 44 45 46 Illi,47 and Mennell,48,49 and later through the writings of Sandoz23,30,50,51 and Faye,52,53 the importance of the dynamic characteristics of joint subluxation moved to the forefront. As a result, joint integrity was defined not only in structural terms but also in functional terms.23,30,34,35,42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 Within this context, joint subluxation took on a broader definition, and joint malposition became a possible sign of disturbed joint function, not absolute confirmation.
This view provides a more dynamic perspective and suggests that minor joint misalignment does not necessarily predict the presence or absence of joint dysfunction or the direction of possible restricted movement.23,30,50 51 52 53 54 From this perspective, joints do not have to be malpositioned to be dysfunctional. Joint fixation can occur with the joint fixed in a neutral position, or it can have multiple planes of joint restriction.23,30,50,57,58 Consequently, treatment decisions concerning adjustive therapy and adjustive vectors, once based predominantly on the direction of malposition, grew to incorporate an assessment of the functional status of the patient including an assessment of joint mobility.41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 Today, consideration is given to both the static and dynamic components of spinal dysfunction, including presence or absence of joint pain with loading (joint provocation/challenge).23,32,34
Other health care providers within the field of manual medicine also struggle with multiple definitions and explanations for manipulable lesions.59 60 61 62 63Box 3-1 contains a list of terms and definitions commonly used to describe functional or structural disorders of the synovial joints. A common principle behind all of these concepts is that there is a somatic component to disease and that dysfunction of the NMS system can affect a patient’s overall health status as well as the ability to recover from injury and disease.
BOX 3-1 Terms Describing Functional or Structural Disorders of the Synovial Joints
Subluxation
The alteration of the normal dynamic, anatomic, or physiologic relationships of contiguous articular structures56; a motion segment in which alignment, movement integrity, or physiologic function is altered, although the contact between the joint surfaces remains intact60; an aberrant relationship between two adjacent articular structures that may have functional or pathologic sequelae, causing an alteration in the biomechanical or neurophysiologic reflections of these articular structures or body systems that may be directly or indirectly affected by them.10
Subluxation syndrome
An aggregate of signs and symptoms that relate to pathophysiology or dysfunction of spinal and pelvic motion segments or to peripheral joints.60
Subluxation complex
A theoretic model of motion segment dysfunction (subluxation) that incorporates the complex interaction of pathologic changes in nerve, muscle, ligamentous, vascular, and connective tissues.10
Joint dysfunction
Joint mechanics showing area disturbances of function without structural change—subtle joint dysfunctions affecting quality and range of joint motion. Definition embodies disturbances in function that can be represented by decreased motion, increased motion, or aberrant motion.61
Somatic dysfunction
Impaired or altered function of related components of the somatic (body framework) system; skeletal, arthrodial, and myofascial structures; and related vascular, lymphatic, and neural elements.62
Osteopathic lesion
A disturbance in musculoskeletal structure or function, as well as accompanying disturbances of other biologic mechanisms. A term used to describe local stress or trauma and subsequent effects on other biologic systems (e.g., effects mediated through reflex nerve pathways, including autonomic supply of segmentally related organs).63
Joint fixation
The state whereby an articulation has become temporarily immobilized in a position that it may normally occupy during any phase of physiologic movement; the immobilization of an articulation in a position of movement when the joint is at rest or in a position of rest when the joint is in movement.30
Vertebral subluxation complex
Because of continued professional debate and increasing scientific inquiry, a trend toward viewing subluxations as complex clinical phenomena has unfolded.* Rather than a condition definable by one or two characteristics, subluxation is more commonly presented as a complex, multifaceted pathologic entity, known as the vertebral subluxation complex (VSC) (see Box 3-1). The VSC is a conceptual model and should not be confused with the vertebral subluxation syndrome. The vertebral subluxation/dysfunction syndrome defines a clinical disorder identified by its presenting symptoms and physical signs.
Gitelman, and later Faye, were the first to promote this broader model and its theoretic components.51,56,65,66 More recently, Lantz67 and Gatterman60,64 have championed this cause. In 1994, a consensus60 presented broader definitions for the VSC that seems to be growing in recognition and acceptance.
Although the trend toward a broader perspective of subluxation has helped move the profession from a simplistic and reductionistic model of spinal health, it has not necessarily advanced the investigation into its existence and nature. Reaching consensus on subluxation theory and expanding the number of clinical spinal disorders that are supposedly subluxation-related does not provide proof of their presence as the primary “lesion” treated by chiropractors. Faye suggests that the subluxation complex is a conceptualization for organizing the essential information relevant to treatment, allowing a chiropractor to examine a person in both a classic orthoneurologic manner and using a biomechanical approach to arrive at a double diagnosis.68 The first assesses the state of the pathologic tissue changes and also aids in determining the prognosis. The second determines the therapeutic procedures to be used and the treatment schedule.68
Nelson24 states that subluxation theory lacks several necessary properties that would allow it to serve as a vehicle for research. First, a theory should attempt to explain existing phenomena and observations; the VSC theory has not been used to explain any specific clinical phenomena. Lantz67 adds that the VSC does not identify any single event or process as the sole causative element in the complex process of subluxation development. Second, a theory should make predictions; the VSC theory makes none. It does not lead in any particular direction or draw any distinction or specific conclusions. The VSC theory suggests that any number of pathologic conditions affecting tissue are possible, with none being more important than any other.67 Third, a theory should be testable and falsifiable so that a study may provide results or observations that either confirm or refute the theory. The VSC theory is so encompassing, allowing for a wide range of mitigating and changing circumstances, that it is difficult to evaluate. Nelson24 points out that this circular type of argument and reasoning (tautology) validates itself simply by renaming accepted principles as a new theory or principle. A tautology has the virtue of being irrefutable, but the deficiency of being useless. It explains nothing, makes no predications, draws no distinctions, and is untestable.
There is value in reaching consensus on the theoretic pathophysiologic and pathomechanical components of functional disorders of spinal motion segments, but mainly for purposes of dialogue and research. The VSC therefore remains a theoretic model in need of investigation. The VSC theory should not be considered as one grand theory, but rather a series of interlocking and interdependent principles. The principles that form a basis for considering the existence and significance of the subluxation should be consistent with current basic science precepts. They must reflect current practice and educational standards, be clinically meaningful, and present a distinct and unique point of view. Unfortunately, the available research data tell us little about the presumed clinical meaningfulness of the traditional chiropractic lesion. Clinical meaningfulness refers to the practical value of a concept in directing the clinician to successful resolution of the health problem the patient has presented. Unfortunately, no one has systematically addressed the predictive power (if any) of subluxation correction for any specific disease or “condition.” None of the controlled clinical trials of the effects of spinal manipulative therapy has, to date, included a subluxation element.69,70
Keating and colleagues point out that the concept of chiropractic subluxation stands pretty much today as it did at the dawn of the 20th century: It is an interesting notion without validation.71 Although there is a strong intraprofessional commitment to the subluxation construct and there are reimbursement strategies that are legally based on subluxation, there is no scientific “gold standard” for detecting these clinical entities.72 The term chiropractic subluxation continues to have as much or more political than scientific meaning.73
Subluxation is still the most common term chiropractors use to describe the spinal joint disorders they treat.74 However, chiropractors are much more likely to view subluxations as disorders that have either structural or functional components rather than simply malpositioned joints. Furthermore, the VSC has been described using theoretic pathologic components broadly divided into mechanical, inflammatory-vascular, and neurobiologic categories. Although these divisions are modeled after those proposed by previous authors, they do not represent an established professional convention. Instead the categories and topics presented here represent an overview of the theoretic effects of the VSC and are not intended to be an all-inclusive or exhaustive treatise on the subject. While these categories are discussed separately, it must be emphasized that although these characteristics may occur in isolation, they can also occur in varying combinations. Some are emphasized more than others, depending on the mode of onset, rate of repair, and length of treatment time.
Mechanical components
The mechanical category of the VSC includes derangements or disorders of the somatic structures of the body that lead to altered joint structure and function. Derangement of the articular soft tissues and mechanical joint dysfunction may result from acute injury, repetitive-use injury, faulty posture or coordination, aging, immobilization, static overstress, congenital or developmental defects, or other primary disease states.*
Joint Malposition
Historically, the basis for subluxation was founded on the concept that traumatic events could lead to altered joint position and that this malposition would interfere with neurologic impulses. Both the chiropractic profession (through D.D. Palmer) and the osteopathic profession (through A.T. Still) have stressed joint position as an important quality for normal joint function.1,94
One of the oldest concepts from the literature on manipulation is the interdependence of structure and function. In other words, structure determines function and function determines structure. When there is a change in structure, there will be a change in function. Therefore, if a structural alteration is identified, a functional change should also be perceived. When a spinal joint is either acutely traumatized or undergoes chronic repetitive stresses, it is assumed that asymmetric muscle tension is likely to develop and hold the joint in a position away from its neutral alignment. The central idea is that misaligned positions of skeletal components can result in movement limitations, associated inflammatory changes, and irritation of nociceptors leading to pain. From a historical perspective, the chiropractic profession primarily viewed spinal subluxations as a structural failure that alters body function.95
The concept of static vertebral misalignment is difficult to support, however. Triano cites evidence that there is no “normal position” between vertebrae in the sense of the historic subluxation argument.95 The spine and the component parts are not perfectly symmetric in their development. Spinous processes in particular are quite prone to asymmetric growth. It is also very unlikely that one could palpate a displacement of a few millimeters or degrees based on the location of the spinous processes. Identification of joint malposition is typically through static palpation or radiographic mensuration. Both of these procedures have only fair to poor inter- and intraobserver agreement. Furthermore, there is no evidence that supports a change in alignment following manipulative intervention. Clearly the “bone-out-of-place” concept is not likely to be the sole explanation for subluxation.25,96
Joint Fixation (Hypomobility)
A more biologically plausible model of spinal joint pain incorporates abnormal joint mechanics and postulates that vertebral hypomobility can cause pain and abnormal spinal mechanics because of changes in sensory input from spinal and paraspinal tissues. Work by Henderson and associates provide the first preliminary anatomic evidence that altered spinal mechanics may produce neuroplastic changes in the dorsal horn of the spinal cord.97 98 99 Their preliminary data suggest that chronic vertebral hypomobility (fixation) at L4 through L6 in the rat affects synaptic density and morphology in the superficial dorsal horn of the L2 spinal cord level.99
Soft Tissue Injury and Repair
A commonly proposed source of joint fixation (hypomobility) and dysfunction is periarticular soft tissue injury with its resultant fibrosis and loss of elasticity and strength.15 16 17 18 19 20 21 2254,56,57,75 76 77 Soft tissue injury and fibrosis may result from acute or repetitive trauma to muscular, tendinous, myofascial, or ligamentous tissue. Regardless of the mechanism of injury, an ensuing inflammatory response is triggered57 resulting in extracellular accumulation of exudates and blood. Platelets then release thrombin-converting fibrinogen into fibrin, which organizes into collagenous scar tissue, resulting in a variety of soft tissue and articular adhesions. This process is considered to be nonspecific and often excessive in the case of traumatic NMS injuries.15,79 As a consequence, early conservative management is often directed at limiting the extent of the inflammatory response. Therapies directed at minimizing the extent of associated inflammatory exudates are helpful in reducing pain and muscle spasm and in promoting early pain-free mobilization and flexible repair.79,83 84 8593,100 101 102 103 104 105 106 107 108 109 110 111 112 113 Aggressive early care and mobilization provide the best opportunity for optimal healing and an early return to work for the patient. Bed rest and prolonged inactivity increase the chances of long-term disability and lost work time.103,105,114,115
The exudates that form as a byproduct of injury and inflammation set the stage for the next step in the process of connective tissue repair. They provide the matrix for the development of granulation tissue and scar formation. The formation of granulation tissue is predominantly carried out by the proliferation of fibroblasts and the synthesis and deposit of collagen tissue. The collagen is initially very poorly organized and must add additional collagen cross-linkages and reorganize along planes of stress to improve the tensile strength of the injured area. This process of repair and remodeling may take months and may result in less than optimal restoration and extensibility of the involved tissue. Immobilization slows the process of recovery, leading to loss of strength and flexibility and potential intra-articular fatty adhesions.75,76,83 84 85 86 87 88 89 90 91 92 93 Immobilization also leads to dehydration, causing proteoglycans to approximate and stick together.83,84,88 If injury or immobilization leads to decreased flexibility, therapies such as articular adjustments or joint mobilization should be directed toward the restoration of motion.15,79,82,102
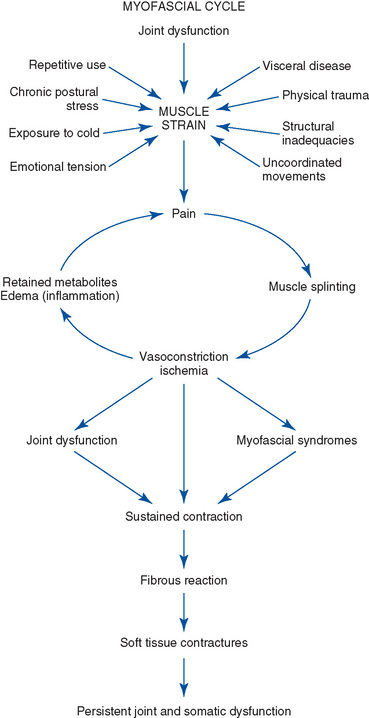
Myofascial Cycle
Painful conditions capable of triggering persistent muscle hypotoncity are additional sources of restricted joint motion (Figure 3-1). Muscle contraction, once initiated, may become a self-perpetuating source of pain and muscle hypotoncity.* Reactive splinting in the joint’s intrinsic muscles may further accentuate this process by blocking passive joint movement and the pain-inhibiting qualities of joint mechanoreceptor stimulation.120 Persistent contractions over time may develop into muscle contractures as a result of adaptational shortening and loss of elasticity from disuse or underuse. Although there is little direct evidence to support the belief that sustained muscle contraction is a feature of intervertebral dysfunction, the concept of protective muscle splinting appears plausible.121 Maladies capable of producing acute muscle contraction are wide ranging; they include trauma, structural inadequacies, visceral disease, emotional distress, and exposure to cold.122,123
Interarticular Derangements
A number of internal joint derangements have also been submitted as probable causes of joint locking and back pain. They include internal derangements of the intervertebral disc (IVD; intradiscal block), derangements of the posterior spinal joints (interarticular, intermeniscoid block),50,51,77,78,130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 and compressive buckling injuries.12,13 They are hypothesized to induce mechanical blockage to movement and unleveling of the motion segment, with resultant tension on the joint capsule, annulus, or both. The joint capsule and posterior annulus are pain-sensitive structures, and tension on these elements may induce additional painful muscle splinting, further accentuating the mechanical blockage and joint restriction. Mechanical joint dysfunction is therefore considered to be a significant and frequent cause of spinal pain and a potential source of spinal degeneration.
Interarticular Block
One source of derangement of the posterior joints is speculated to result from entrapment (Figure 3-2) or extrapment (Figure 3-3) of joint meniscoids or synovial folds.131 132 133 134 135 136 137 138 139 140 141 The intra-articular meniscoids are leaflike fibroadipose folds of synovium that are attached to the inner surface of the joint capsule and project into the joint cavity. These meniscoids have been found to be present in all of the posterior joints of the spine.
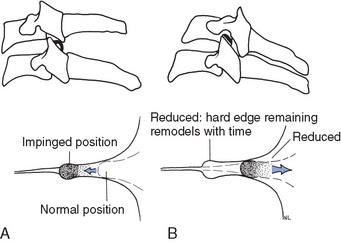
Figure 3-2 Theory of meniscoid entrapment. A, Diagrammatic representation of meniscoid entrapment inducing flexion and extension malpositions, capsular tension, pain, and subsequent restrictions in spinal mobility. B, Manipulation of the joint separates the joint surfaces, allowing the meniscoid to return to a neutral position.
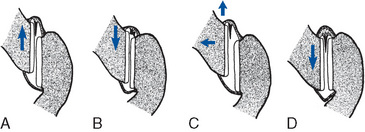
Figure 3-3 Theory of meniscoid extrapment. A, On flexion, the inferior articular process of a zygapophyseal joint moves upward, taking a meniscoid with it. B, On attempted extension, the inferior articular process returns toward its neutral position, but the meniscoid, instead of reentering the joint cavity, buckles against the edge of the articular cartilage, forming a space-occupying lesion under the capsule. C, Manipulation gaps the joint and allowing the meniscoid to return to its neutral resting position (D).
Bogduk and Jull140 have suggested that extrapment of these meniscoids may be one cause of restricted joint motion. They speculate that the meniscoid may occasionally be pulled out of its resting position by the inferior articular process of a zygapophyseal joint as it moves upward during flexion. On attempted extension, the inferior articular process returns toward its neutral position, but the meniscoid, instead of re-entering the joint cavity, impacts against the edge of the articular cartilage and buckles, representing a space-occupying lesion under the capsule. Pain occurs as a result of capsular tension, and extension motion is restricted. The use of a distractive or joint gapping adjustive procedure may function to separate the articular surfaces and release the extrapped meniscoid (see Figure 3-3). 140,147
Maigne78 and others77,116,137,148 149 150 151 152 have proposed a model of interapophysary meniscus entrapment rather than extrapment. In this model the menisci are purportedly drawn into a position between the joint margins during poorly coordinated spinal movements or sustained stressful postures. With resumption of normal postures, pain resulting from impaction of the menisci or traction of the articular capsule induces reactive muscle splinting and joint locking. The development of a painful myofascial cycle is initiated as prolonged muscle contraction leads to muscle fatigue, ischemia, and more pain. If spasm and locking persist, the articular cartilage may mold around the capsular meniscus, causing it to become more rigidly incarcerated within the joint.116 117 118 To interrupt the cycle of pain, muscle cramping, and joint locking, distractive adjustments have also been presented as a viable therapy capable of inducing joint separation, cavitation, and liberation of the entrapped menisci (see Figure 3-2).118 It is important to note that meniscoid derangement is only one hypothetical cause of joint dysfunction. Meniscoid derangement is postulated to be a more likely source of joint dysfunction in circumstances in which trivial trauma leads to acute joint irritation or locking and associated muscle spasm.139
Interdiscal Block
The mechanical derangements of the IVD that may lead to joint dysfunction are postulated to result from pathophysiologic changes associated with aging, degenerative disc disease, and trauma. Farfan153 has proposed a model of progressive disc derangement based on repetitive rotational stress to the motion segment. He postulates that repetitive torsional loads of sufficient number and duration may, over time, lead to a fatigue injury in the outer annular fibers. The process would begin with circumferential distortion and separation in the outer annular fibers, followed by progression to radial fissuring and outward migration of nuclear material. Another view postulates that disc derangement, fissuring, and herniation begin in the innermost annular rings and progresses outward.154
The rate of fatigue and injury depends on the duration and magnitude of the force applied. In the individual with disrupted segmental biomechanics, the process is potentially accelerated as an altered axis of movement leads to increased rotational strain on the IVD. Postmortem dissection studies of degenerated discs have indeed identified radial fissures in the annulus fibrosus. Cyriax155 believes that displaced nuclear material along an incomplete fissure is the source of joint fixation. Nuclear migration along these radial fissures has also been demonstrated by computed tomography (CT) discography and correlated with patient pain.156
Interwoven in the natural history of degenerative disc disease may be episodes of acute mechanical back pain and joint locking. Maigne178 and others23,129 130 131 have postulated that incidents of blockage may occur during efforts of trunk flexion as nuclear fragments become lodged in fissures in the posterior annulus (interdiscal block) (Figure 3-4). Consequently, tension on the posterior annulus and other mobile elements of the involved motion segment are produced, initiating local muscle guarding and joint locking. Cyriax126 proposes that these lesions may induce tension on the dura mater, inducing lower back pain (LBP) and muscle splinting. Once local pain and muscle splinting are initiated, a self-perpetuating cycle of pain, cramping, and joint locking may result.
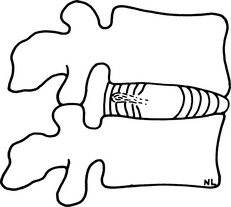
Figure 3-4 Interdiscal block. Illustration of nuclear material migrating into internal annular fissures, producing tension on the posterior annulus.
Adjustive therapy has been proposed as a viable treatment for interrupting this cycle of acute back pain and joint locking. In addition to the distractive effect on the posterior joints, adjustive therapy is thought to have a potential direct effect on the IVD, either by directing the fragmented nuclear material back toward a more central position or by forcing the nuclear fragment toward a less mechanically and neurologically insulting position (see Figures 4-18 and 4-19). Of course there are spinal joints (atlanto-occipital and atlantoaxial articulations) that do not have IVDs, and they are common sites of dysfunction. This clearly indicates that IVD derangement is not the sole source of spinal joint subluxation or dysfunction.
Compressive Buckling Injury
Triano suggests that a causal factor for a manipulable lesion may be a compressive buckling injury.12,13 Intersegmental buckling is likely the result of some error in neuromuscular control that fails either to provide adequate prestability to the segment or to respond appropriately with muscle activation to a perturbation.157 When a mechanical overload to spinal functional units occurs, either as a single traumatic event or cumulative events, a critical buckling load may be reached. Individual structural elements (disc, facet, ligament, nerve, muscle) may experience concentration of local stresses with reduced functional limits and symptom production specific to the tissue affected. The result is a state of dysfunction that may lead to local inflammatory or biomechanical changes.158,159
Each joint possesses some inherent stability resulting from the stiffness of the ligaments and joint capsule. Further stability and control are provided by the neuromuscular system and faulty motor control may lead to inappropriate levels of muscle force and stiffness at a given spinal segment. This may compromise segmental stability at that level,160 leading to transient intersegmental buckling.161 The segment briefly exceeds its safe physiologic motion, which leads to loading of the surrounding soft tissues (ligaments, IVD, etc.).157 Furthermore, exposure to vibration and previous disc injury may augment the buckling event. The result of intersegmental buckling is asymmetric positioning of the vertebra that is maintained by the intrinsic muscles producing hypomobility of the functional unit.
Clinical Joint Instability and Hypermobility
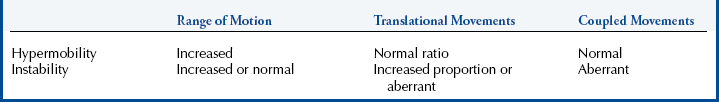
Joint dysfunction resulting from soft tissue injury or degeneration does not necessarily result in joint hypomobility. Disturbances of function of the vertebral column can also result from a loss of joint stability. Joint derangement and dysfunction resulting from a loss of joint stability are commonly referred to as joint hypermobility or clinical joint instability. Both terms are often used interchangeably, and there is no standard for defining these terms. Definitions vary among clinicians and authors and between the clinical and biomechanical literature.162,163
Although numerous definitions abound, all seem to incorporate a loss of stiffness or sensorimotor control affecting the joints’ stabilizing structures.162 163 164 165 The loss of stiffness is clinically relevant if excessive or aberrant movements lead to pain, progressive deformity, or compromised neurologic structures. Movement can be abnormal in quality (abnormal coupling) or in quantity (increased movement).
Attempts have been made to distinguish clinical joint instability from hypermobility (Table 3-1). The differences are a reflection of the structures involved and degree of pathologic change in the joints’ stabilizing structures. Hypermobile joints are assumed to be stable under normal physiologic loads. Hypermobile joints demonstrate increased segmental mobility, but they maintain normal patterns of movement. Hypermobility may be in one plane and not associated with any abnormal translational movements.166,167
In contrast, patients with clinically unstable joints have been postulated to have ineffective neural motor control or more advanced changes in the joints’ stabilizing structures.168 Damage to these structures leads to abnormal patterns of coupled and translational movements and possible multiple planes of aberrant joint movement. Clinical joint instability should not be equated with gross orthopedic instability resulting from fracture or dislocation.
There is little doubt that clinical spinal joint instability exists, but current methods lack the necessary sensitivity and specificity for clearly identifying its contributions to back pain.162 Clinical opinion suggests that the typical presentation is one of recurring episodes of marked back pain, often initiated by trivial events such as bending or twisting. Global movements are often limited and may demonstrate a painful arc with abnormal patterns of deviation or hitching. Symptoms often resolve within several days, only to recur at a later date.165
Physical examination tools are limited but increasing.162,168 Manual palpation of passive posteroanterior glide has been suggested as one physical means of testing for excessive shear and instability. One recent investigation did demonstrate that prone posterior-to-anterior (P-A) passive joint play (JP) evaluation of the spine can accurately identify abnormal segmental translation as compared with a reference standard of flexion extension radiographs.169 This test demonstrated good specificity (89%) but poor sensitivity (29%), with a positive likelihood ratio of 2:52. Both the P-A passive segmental mobility assessment and the prone “instability test” were predictive of which patients with low back pain (LBP) would benefit from a lumbar exercise stabilization program.168 The prone instability test requires the patient to lie in a prone position on an examination table with his or her feet on the floor. The doctor applies segment-passive P-A pressure and, if pain is produced, the patient is asked to raise his or her feet off the floor. If pain is diminished, the test is consider positive and indicative of segmental instability.
Dynamic flexion-extension and lateral bending radiographs are the most commonly used radiographic methods for detecting end-range instability, but they do not provide information about quality of movement during the midrange of segmental motion.162 Methods using transducers or markers placed over bony landmarks have not demonstrated effective results as a consequence of the skin motion artifact. Methods using pins embedded in the spinous processes to measure movement have adequate accuracy, but these methods are invasive and are not practical for clinical use.162
In the absence of gold standard diagnostic tools for detecting spinal joint instability, the chiropractor should pay close attention to the clinical presentation, including history and manual examination, and consider instability in a patient who has recurring episodes of back pain with only temporary relief from manipulation. Suspicion of instability may be reinforced by dynamic x-ray flexion-extension examination, but this procedure may have false-negative results. When instability is still suspected, a conservative treatment trial directed at stabilizing the spine through proprioceptive and specific spinal stabilizing exercises should be applied.168
Mechanical Models of Spinal Dysfunction and Degeneration
The profession places significant emphasis on the mechanical components of joint dysfunction and subluxation. Mechanical joint dysfunction is considered a significant and frequent cause of spinal pain and a potential source of spinal degeneration.*
The spine is viewed as an interdependent organ system inextricably connected with the rest of the locomotor system. Altered mechanics in one component of the motion segment are perceived to have unavoidable mechanical effects on other functional elements of the motion segment and spine. Several models that outline the proposed sequential dysfunctional and degenerative effects that may ensue subsequent to spinal dysfunction have been developed.
Gillet Model
Gillet41 42 43 44 45 4653 considers the process of mechanical joint dysfunction developing through three different phases of joint fixation: muscular, ligamentous, and articular. Muscular fixation is considered to be a product of segmental muscle hypertonicity and contraction; ligamentous fixations, the product of contracture and shortening in the joint capsule and its periarticular ligaments; and articular fixations, the product of fibrous interarticular adhesions between articular surfaces. The end stage of articular adhesions is the potential progression to full bony ankylosis and irreversible fixation.
Muscular fixations are identified by the palpation of taut and tender muscle fibers and restricted joint mobility. The end play (EP) is restricted, but has a rubbery and giving quality. Ligamentous fixations demonstrate restricted joint movement and a hard, abrupt, leathery end feel. Articular fixations demonstrate the same quality of restriction, but in all planes of motion.
Gillet maintains that ligamentous or articular fixations are the most significant. He considers muscular fixations as secondary compensations to marked fixations at other levels. As a result, he presents an approach that stresses the identification and treatment of the patient’s major fixations. Gillet classifies major fixations as those demonstrating the most dramatic blockages to movement. He contends that the major fixations are frequently not the most symptomatic sites, but are the key to inhibiting pain-free spinal function. Although his ideas are intriguing and have had a profound effect on the profession, they have not been experimentally confirmed.
Kirkaldy-Willis’ Model
Kirkaldy-Willis169,170 presents a pattern of spinal degeneration founded on the principle that spinal degeneration often begins with local mechanical derangement in the absence of structural alteration. He postulates that the process is often initiated with the development of individual motion segment dysfunction secondary to alteration in segmental muscle tone and function. Although the disorders that are postulated to initiate dysfunction are extensive, most share as a consequence the potential to induce joint hypomobility.26 Joint hypomobility is speculated to initiate the degenerative cycle through the development of altered segmental biomechanics.*
If mechanical derangement persists, repetitive abnormal loading eventually leads to fatigue and attenuation of the articular soft tissues. Local joint instability develops as a result of capsular laxity and internal disruption of the IVD.26,170,171 Consequently, if the derangement is of sufficient magnitude, osseous structural alteration will result, and degenerative joint disease becomes radiographically visible (Figure 3-5).170
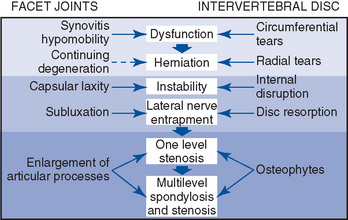
Figure 3-5 The proposed sequence of pathologic changes in the facet joints and disc as a consequence of biomechanical derangement.
(From Kirkaldy-Willis WH, Bernard TN Jr: Managing low back pain, ed 4, New York, 1999, Churchill Livingstone.)
The final effect of this degenerative cycle is the restabilization of the joint through soft tissue fibrosis and bony exostosis.26,170 As a consequence, the incidence of spinal pain may decrease during the later stages of stabilization. However, bony entrapment of the NRs or stenosis of the spinal canal are of increasing frequency, which may lead to an increased frequency of leg pain and neurologic deficits.170,171
The presented models of motion segment degeneration and the compensational adaptations initiated are not necessarily limited to the involved joint. Not only is it possible for joint hypomobility, instability, and degenerative joint disease all to occur at the same motion segment, but it is also possible for compensatory dysfunction and degenerative changes to develop at other spinal levels or other joints within the locomotor system.26,34,46,51 52 5375
Certainly not all joint dysfunction fits this pattern of progression. A large percentage of dysfunction is self-limiting or so minor that an individual adapts and compensates to the change with limited structural or functional alteration. If dysfunction persists, the processes of local and distant joint degeneration may ensue. A point of emphasis and concern for the chiropractic profession is therefore to detect persistent mechanical dysfunction at an early stage of alteration and strive to eliminate it before it develops into irreversible or permanent disorders.
Neurobiologic components
Theory of Intervertebral Encroachment and Nerve Root Compression
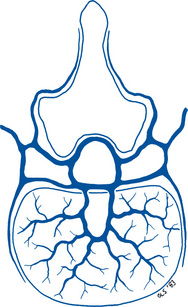
Historically, the profession has emphasized spinal NR compression as the significant neurologic disorder accompanying vertebral subluxations.1 2 3 27 28 29 30 31 32 33 34 35 36 37 38 Spinal subluxations were hypothesized to induce NR compression as a result of direct anatomic compression of neural elements (non–impulse-based model) within the intervertebral foramen (IVF) (Figure 3-6). The resulting NR dysfunction was subsequently hypothesized to induce dysfunction of the somatic or visceral tissues they supplied. Marked or prolonged compression was hypothesized to induce loss of function. More moderate compression was hypothesized to lead to increased neural activity and increased pain, paresthesias, and hypertonic muscles.2,3,27 28 29 30 31 32 33 34 35 36 37 38
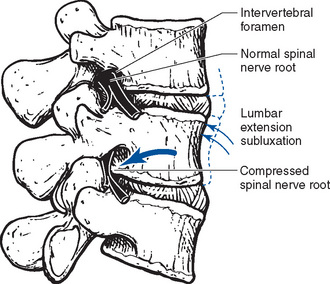
Figure 3-6 Diagram illustrating lumbar extension subluxation and theory of subluxation-induced compression of spinal nerve roots as they exit the intervertebral foramen.
The initial model of direct bony compression of NRs has produced considerable skepticism outside the profession and less than universal endorsement within the profession.35,38,172 In 1973, Crelin172 challenged the anatomic plausibility of subluxation-induced NR compression. He conducted cadaveric lumbar dissections, measuring the lateral borders of the IVF, and concluded that the bony borders of the lateral IVF provided for a minimum of 4 mm of space around each exiting NR. In addition, the NRs gain a dural covering at their point of entry to the IVF, further reducing their vulnerability to compression.173,174 He concluded that in the absence of degenerative joint or disc disease, it was unlikely that joint subluxation could produce enough narrowing of the IVF to produce direct anatomic compression of spinal NRs.
In 1994, Giles175 revisited Crelin’s criticism of the chiropractic model of subluxation-induced NR compression. Lumbar cadaveric dissections were again performed, but this time they included dissections at the level of the interpedicular zone, not just at the lateral borders of the IVF as Crelin had performed. Measurements made at the interpedicular zone demonstrate an average of 0.4 to 0.8 mm of space around each NR and the dorsal root (DR) ganglion (Figure 3-7). These margins are only a small percentage (10% to 20%) of the space originally described by Crelin and theoretically small enough to be affected by joint dysfunction and subluxation. Moreover, his methodology and conclusions did not account for structural variants such as the transforaminal ligaments or the presence of functional alterations such as edema.176
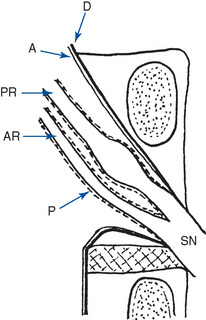
Figure 3-7 Diagram showing the interpedicular zone in a lumbar motion segment. Contained within the zone are dura mater (D), arachnoid mater (A), the anterior root (AR), pia mater (P), the posterior root (PR), ganglion, and the spinal nerve (SN). Note the proximity of the neural structures to the cephalad pedicle.
(Modified from Giles LGF: J Manipulative Physiol Ther 17:4, 1994.)
The spinal nerve rootlets at this level lack the epineural covering of the NRs as they exit the IVF and are more susceptible to pressure, inflammation, and ischemia. The DR ganglia (DRG), which lie within this space, are especially susceptible to compressive forces,177 and chronically injured dorsal NRs respond more vigorously to mechanical deformation.178
Furthermore, it is not necessary for spinal NRs to be directly compressed by bony structures to develop pathologic dysfunction. There are other structures within the IVF (e.g., arteries, veins, recurrent meningeal nerve, lymphatics, fat, areolar connective tissue) that occupy space, making it possible that other kinds of mechanical stresses may affect the nerve tissue.25 Sustained misalignment or inflammation of the spinal motion segment may stretch or compress the local vascular structures, leading to disruption of neural blood supply and neuroischemia.35,179 It has also been demonstrated that mechanical pressures and tensions applied to the spinal segments may create myriad subclinical neurophysiologic alterations ranging from changes in intraneural protein composition to altered nerve conduction characteristics.180 181 182 183
The density of sodium ion channels in the soma and initial segment of DRG cells is relatively high, suggesting these regions may be unusually excitable.184 These properties may render neural tissue within the IVF vulnerable to effects of mechanical compression and the chemical environment produced by changes in the IVD or facet joints.185 Substantial evidence demonstrates that the DRs and DRG are more susceptible to the effects of mechanical compression than are the axons of peripheral nerves because impaired or altered function is produced at substantially lower pressures.185,186 Whether spinal manipulation can alter neural function by mechanically changing compressional pressures or reducing the concentration of metabolites in the IVF is unknown.187
Compression studies investigating how herniated IVDs affect NR function have been performed. The mechanism by which a herniated disc could directly compress the DRs or DRG is well understood and straightforward.187 However, a herniated IVD could also affect NR function through indirect effects mediated by the release of neuroactive chemicals.188 This explains the common observation that in the absence of compression, herniated discs can produce neurologic findings. Recent studies demonstrate that the application of nucleus pulposus to a lumbar NR causes mechanical hyperalgesia in the distal limb and causes swelling in and decreased blood flow to the DRG.189,190 In addition, phospholipase A2, an inflammatory mediator associated with disc herniation188,191 is neurotoxic in high doses to afferent nerves.192 In moderate doses it increases mechanical sensitivity of the DRs, producing long-lasting discharge, and it increases the discharge of previously silent DRG cells.192,193
The intervertebral canal and each of its motion segments have a vascular supply composed of spinal arteries and veins. The spinal arteries provide oxygenated blood to the spinal cord and dorsal and ventral NRs. Blood vessels are softer and more susceptible to the effects of stretch and compression than are the nerves they supply, making localized neuroischemia, without direct compression, a possible result of spinal joint dysfunction.
If joint malposition does contribute to dysfunction of the spinal NRs, it is more likely to occur by narrowing the more vulnerable interpedicular zone. Furthermore, joint subluxation has a greater potential to affect NR function if it is secondary to other disorders that have already led to narrowing of the lateral recess, such as disc herniation or other space-occupying lesions, degenerative disc and joint disease, and joint instability.
Although recent anatomic investigations have provided a plausible mechanism by which joint subluxation may contribute to NR dysfunction, it still remains a tenuous theory. The clinical literature has established that encroachment of neural structures within the IVF may produce NR dysfunction, but it has not established whether spinal subluxations alone (i.e., without other neurocompressive sources) can cause encroachment and altered neural activity. Furthermore, it must be appreciated that a subluxation occurs within the normal ROM for the segment. The IVFs of each segment change size and shape with movements. Extension combined with rotation and lateral flexion to the same side maximally decreases the opening of the IVF, yet no NR compression occurs. Therefore, something in addition to a sustained malposition has to occur to produce clinical signs of NR compression, such as inflammation, disc deformation, or vascular changes.
In conclusion, it appears that the early “foot-on-the-hose” model of joint subluxation and NR compression is not biologically plausible. Joint subluxations alone are extremely unlikely to “pinch” the spinal NRs at the margins of the IVF.
Theory of Altered Somatic and Visceral Reflexes
Somatosomatic and Somatovisceral Reflexes
In the absence of evidence to confirm the NR compression hypothesis, the profession has assembled an alternative model of subluxation syndrome–induced neurologic alterations (impulse-based model). The impulse-based paradigm of neurodysfunction has been developed from the work of Homewood and Korr.32 33 34 35 32 33 34 35 37 38 39194,
A somatoautonomic reflex is elicited when stimulation of somatic tissue (the musculoskeletal system and the dermis of the skin) is manifested as an alteration in autonomic nervous system function. A spinal visceral reflex is a type of somatoautonomic reflex in which stimulation of the spinal column alters visceral function.195
This hypothesis envisions vertebral joint dysfunctions as lesions capable of inducing chronically altered nociceptive and proprioceptive input. This persistent afferent input, driven by mechanical alteration, pain, and potential local inflammation, triggers a segmental cord response, which in turn induces the development of pathologic somatosomatic or somatovisceral reflexes. The persistent altered afferent input is then theorized to produce sensitization of local spinal neuron pools and the establishment of abnormal somatosomatic or somatovisceral reflexes. The reflexes, once established, become the potential driving source of altered somatic or visceral function. If these reflexes persist, they are hypothesized to induce altered function in segmentally supplied somatic or visceral structures.32 33 34 35 37 38 3956,196 197 198
Thus joint subluxation/dysfunction syndrome (JSDS) may initiate secondary dysfunction in tissues with shared segmental innervation. Indeed, clinical investigations have demonstrated that altered muscle tone, deep tendon reflexes, and altered sympathetic activity may accompany joint derangement and dysfunction.199 200 201 202 203 Many of these findings had been previously assumed to be associated with NR dysfunction only. The segmental muscle hypertoncity that may be associated with joint dysfunction illustrates a clinical example of a somatosomatic reflex; cervical disequilibrium secondary to cervical joint dysfunction illustrates an example of a somatovisceral disorder (Figure 3-8).201
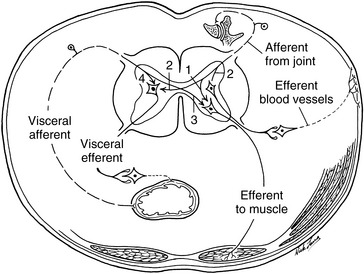
Figure 3-8 Afferent pathways from the somatic and visceral structures can produce somatosomatic (1), somatovisceral (2), viscerosomatic (3), and viscerovisceral reflex phenomena (4).
The proposed joint subluxation- or dysfunction-induced neurologic phenomena may be clinically manifested by the presence of referred pain, hypertonicity, hyperesthesia, or altered sympathetic activity, such as altered temperature regulation and skin conductance.199 200 201 202 203 Manual therapy, including soft tissue techniques and other forms of adjustive therapy, would have the potential for arresting both the local and distant somatic and visceral effects by terminating the altered neurogenic reflexes that are associated with somatic or joint dysfunction.
Viscerosomatic (Autonomic) Reflexes
Persistent pathologic conditions in visceral structures also have the theoretic potential to induce reflexive dysfunction in other somatic or visceral structures. Visceral disease or dysfunction may activate the autonomic nervous system through connections with the lateral horn cells in the cord to produce vasomotor, trophic, visceral, or metabolic changes (see Figure 3-8). Numerous conditions have been linked to hyperactivity of the sympathetic nervous system; these include various types of cardiovascular, gastrointestinal, and genitourinary disorders, and certain musculoskeletal disorders such as complex regional pain syndrome.
It has been suggested that the body wall manifestations of visceral disease are an integral part of the disease process, rather than just physical signs and symptoms,204 although the definitive causal factors and the characteristic response of the individual are still unknown. Early signs of most disease states are manifested as symptoms and signs that are part of a common reaction pattern to injury or stress. Pain in the somatic tissues is a frequent presenting symptom in acute conditions related to visceral dysfunction. Palpatory cues of transient muscle hypertonicity and irritation or subcutaneous edema may be accompaniments of ill-defined subclinical states.205 Moreover, subtle changes in tissue texture, joint position, and joint mobility identified by discerning palpatory skills may at times be latent manifestations of the somatic component of visceral disease.
In a study performed on cardiac patients in an intensive care unit,206 autonomic spinal reference changes were noted for the involved viscera (Box 3-2). In studies by Kelso,207 it was noted that as the visceral condition progresses, the somatic stress pattern subsides, and a typical visceral reflex pattern is seen. Therefore, the chronic phase of reflex activity is characterized by trophic changes in the skin and subcutaneous tissues, as well as local muscle contraction. This may result in a joint misalignment and decreased segmental mobility. However, it is not known whether the continuation of reflex somatic dysfunction is related to the initial effect of the visceral disease or whether it is a result of long-term segmental facilitation.
BOX 3-2 Autonomic Changes in Soft Tissues Identified in Patients with Viscera Problems
Vasomotor reaction—increase in skin temperature
Sudomotor reaction—increase in skin moisture
Increase in muscle tone and contraction
In a blind study of 25 patients, Beal208 was able to differentiate patients with cardiac disease from those with gastrointestinal disease with a reported accuracy of 76% using a compression test to examine for soft tissue texture changes and resistance to segmental motion. Similarly, Beal and Dvorak209 examined 50 patients in a physician-blind format and were able to identify characteristics specific for patients with cardiovascular, pulmonary, gastrointestinal, or musculoskeletal diseases.
In summation, it is apparent that spinal dysfunction has the potential to both produce and be the product of visceral or somatic dysfunction or disease. The literature supports the existence of somatovisceral and viscerosomatic reflexes,210 211 212 but there is little or no evidence to support the notion that the VSC can cause prolonged aberrant discharge of these reflexes. Also unsupported in the literature is the notion that the prolonged activation of these reflexes can induce pathologic change and visceral disease. Nor does the literature support the position that spinal manipulative therapy can alter the prolonged reflex discharge to an extent that induces a reversal of the pathologic degeneration of the affected tissues.213,214 Although there have been investigations using animal models on the effects of mechanical stimulation of the spine on blood pressure, heart rate, and renal sympathetic nerve activity,215,220 unfortunately there is almost no physiologic research concerning responses in humans to either spinal pain or innocuous mechanical stimulation. Furthermore, most of the data obtained were elicited with noxious stimulation. There is still little support for the contention that painless spinal dysfunction can affect organ function, which is not surprising, considering that all the basic physiologic work cited was performed on anesthetized animals. The evidence does suggest that muscle spindles in cervical paraspinal muscles may in fact be capable of eliciting somatoautonomic reflexes.221
The complex interrelationship of the NMS system demands that chiropractors and other manual therapists be open to the numerous potential sources of their patients’ complaints. Spinal pain and dysfunction may be secondary to a disorder that is not amenable to manual therapy. In circumstances in which JSDSs are secondary to active visceral or somatic disease, manipulative treatment alone would be inappropriate.
Inflammatory and vascular components
Joint injury, chronic mechanical joint derangement, or joint immobilization may initiate the inflammatory and vascular components of the VSC.34,54,56,75 These components include vascular congestion, ischemia, and inflammation.
Vascular Congestion
It is unclear at this time what role, if any, spinal segmental function or dysfunction plays in local vascular congestion. Speculation has centered on the potential for motion segment dysfunction or associated inflammation to impede blood flow through segmental venous structures. Venous pressure is very low and depends on gravity in the spinal veins, making them quite susceptible to compression and venous congestion. Lantz suggests that immobilization may lead to localized venous stasis, creating a negative pressure and lack of proper venous drainage that may lead to inflammation.222
A segmental vein drains each motion segment and related spinal canal. Each segmental vein receives venous blood from an extensive internal venous plexus (Batson), which in turn receives blood from a basivertebral vein that drains each individual vertebra (Figure 3-9). The intraspinal venous plexus is located within the epidural space and basically consists of two paired columns that are united via a transverse communication vein. A lack of venous drainage in these structures is speculated to lead to increased capillary pressure, diminished arterial blood flow, and the production of local ischemia, inflammation, and potential associated joint stiffness.223 In addition, a tear in a fragile vein may occur, possibly as a result of repetitive increases in intra-abdominal pressure, producing a hematoma that serves as a space-occupying lesion. Because the veins course vertically at the posterolateral aspect of each disc bilaterally, they can produce the same clinical picture as a disc herniation as they expand. The only differentiating test is magnetic resonance imaging (MRI), using T2-weighted images to visualize more water content in the blood-filled hematoma.
Inflammatory Reactions
Inflammatory reactions are largely mediated by the vascular system and accompanied by cellular and humoral components that act as an intrinsic source of pain and vasodilation.224 The inflammatory reaction initiated by musculoskeletal injury or dysfunction is identical to that initiated by a foreign object or infection. Although it is a normal protective response, it may accentuate the pain response, slow the recovery time, and perpetuate joint dysfunction. Pain accompanying inflammation may initiate local reflex muscle contraction, which, over time, may lead to local ischemia and potentially more pain and muscle splinting. The result, as described previously, is a self-perpetuating cycle of pain and continued muscle spasm.* If the muscle contraction persists, it may eventually develop into a muscle contracture as the myofascial structures become shortened and infiltrated with fibrotic tissue.170,225 The resulting soft tissue derangements and contractions that develop must be dealt with therapeutically, or they will serve as a source of continued pain and recurring joint subluxation and dysfunction.
With persistent inflammation and pain, plastic changes may occur in the peripheral and central nervous systems that lower pain thresholds, giving rise to allodynia (pain in response to a normally innocuous stimulus), hyperalgesia (heightened pain intensity in response to a normally painful stimulus), and sensitization of the central nervous system. Afferent nerve fibers that are quiescent in normal joints may become active and start to send nociceptive information to the central nervous system, which can also become sensitized to perceive what is typically nonpainful stimuli as painful.226 227 228
In addition, chronic joint inflammation may lead to synovial tissue hyperplasia and thickening as a result of persistent irritation and secretion of synovial fluid.229,230 Synovial tags may develop as a hyperplastic reaction to chronic inflammation, and they in turn may become further impediments to joint movement.225,231 Eventually, fibrous invasion of the synovial connective tissue layer may induce an attendant loss of vascularity and subsequent loss of synovial fluid secretion.148
Some degree of joint or soft tissue inflammation should be suspected when the patient’s pain is constant. Clinical signs include muscle splinting, soft tissue swelling, and temperature alteration. Inflammation associated with spinal joint injuries or dysfunction is unlikely to produce palpable swelling at the surface. Some have suggested, however, that joint dysfunction may be associated with a local sympathetic reflex alteration capable of inducing a slight boggy feeling in overlying segmental tissues.
Joint subluxation/dysfunction syndrome
A Joint Subluxation/Dysfunction Syndrome (JSDS) diagnosis is a clinical diagnosis defined by an aggregate of signs and symptoms that are assumed to identity dysfunction of spinal, pelvic, or peripheral joints.232,233 It is a functional (biomechanical) diagnosis, not a structural (pathoanatomic) diagnosis. When applied to the spine, it implies that the spinal motion segments and their associated soft tissues are the source of the patient’s symptoms. Unlike traditional structural diagnoses like disc derangement, sprain or strain, and spinal stenosis, the diagnosis of JSDS does not attempt to identify specific tissue pain generators within the spinal motion segment. This diagnosis typically includes local axial spine pain reproduced or accentuated by static or dynamic palpation. It may be associated with sclerogenic referred pain into the proximal extremity. The diagnosis of JSDS usually denotes to chiropractic physicians that the condition may be amenable to manual therapy; high velocity–low amplitude (HVLA) adjustive therapy is most commonly applied treatment.
Joint dysfunction may occur in isolation, but is commonly associated with other identifiable functional and pathoanatomic disorders and conditions. The individual chiropractor and the profession as a whole should make every attempt to incorporate these diagnoses in assessment and patient management.
Spinal listings
As the chiropractic profession has evolved, it has developed various abbreviated descriptions for designating abnormal joint position or movement. The result is a profession laden with redundant nomenclatures (listing systems) that describe spinal subluxations and fixations. As new descriptive terms are introduced, old ones are not replaced. It is not uncommon for each technique to have its own unique listing system. Unique listing methods may be efficient for those performing the associated technique, but many are not commonly understood.
As part of the process to include chiropractic in Medicare, there was an attempt to standardize listing systems at the 1977 American Chiropractic Association (ACA) conference in Houston. Although the parties did succeed in developing a common nomenclature for Medicare claims based on standard kinesiologic terms, it unfortunately did not form a basis for larger professional consensus. There is still significant variation among chiropractors and on national board examinations as to the preferred listing systems.
To their students’ continual frustration, colleges are left in a position of teaching repetitive and often contradictory methods of describing joint malpositions and fixations. Presently, the common systems used to describe abnormal position are Medicare, Palmer-Gonstead, and National–Diversified systems. In an attempt to reduce the confusion and redundancy, this book emphasizes standard kinesiologic terms and the Medicare listing system. When deviations in position are described, the term malposition is used, and when limitations to movement are described, the term restriction is used.
Spinal joint listing systems should be incorporated only in conjunction with a diagnosis of spinal JSDS. They describe characteristics of subluxation and dysfunction syndromes, but they are not expected to be stand-alone diagnostic terms. Spinal listings should be viewed only as a short-hand method of recording which joint changes were subjected to manipulation (Figure 3-10).
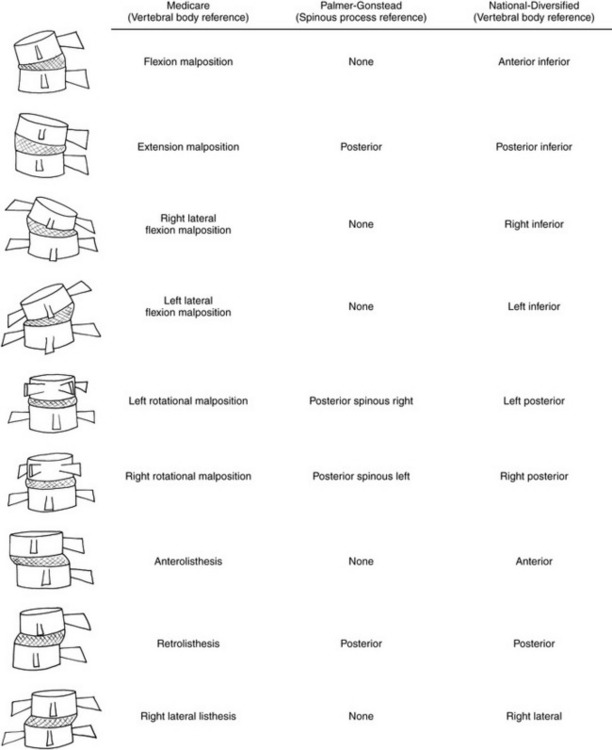
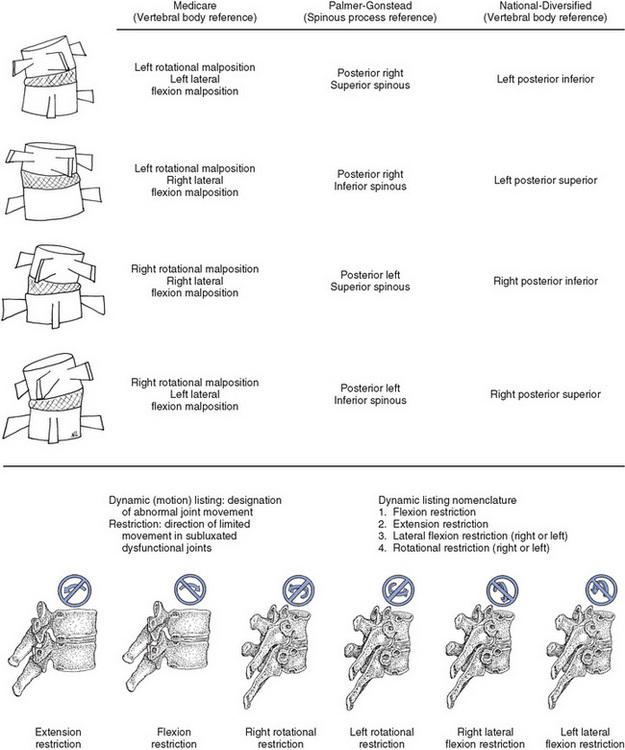
Figure 3-10 Comparative chart of static listing systems.
(Modified from ACA Council on Technic: J Am Chiropr Assoc 25[10]:46, 1988.)
All motion segment malpositions are described with the position of the upper vertebra compared with the lower vertebra. For example, a flexion malposition describes a vertebra that has deviated into a position of flexion relative to the vertebra below, and a flexion restriction describes a limitation or loss of joint flexion between the two vertebrae.
Trunk and neck movements are described in kinesiologic terms. They are based on vertebral body movement, not spinous process movement. Left rotation of the trunk is defined by left posterior vertebral body rotation, not by right rotation of the spinous process.
Clinical evaluation of joint subluxation/dysfunction syndrome
Before adjustive treatments are applied, the chiropractor must evaluate the patient’s complaint and determine if the patient is suffering from a condition (manipulable lesion) that is amenable to chiropractic care. As mentioned previously, therapeutic decisions on where and how to apply adjustive therapy are based primarily on the evaluation of the NMS system and a determination that injury, derangement, or disease has led to altered function.
Although the diagnosis of joint dysfunction identifies a painful clinical syndrome that may respond to manual therapy, the nature of the dysfunction must be evaluated before therapy is administered. The mere presence of joint subluxation or dysfunction does not determine the need for adjustive therapy. Joint dysfunction may result from diseases or disorders that contraindicate treatment or result from disorders that do not respond to adjustive treatments. The ability to thoroughly evaluate and triage disorders of the NMS system and distinguish those conditions that are appropriate for chiropractic care is critical. Differentiating mechanical from nonmechanical conditions, assessing the source of the presenting complaint, and understanding the potential pathomechanics and pathophysiology of the disorders being considered for chiropractic care are crucial elements for successful treatment. Therefore, before instituting treatment, the clinician must perform a thorough case history, physical examination, and any other appropriate imaging or laboratory procedures to rule out any disorders that contraindicate adjustive treatments. The evaluation should assess whether the dysfunction is associated with joint hypermobility or hypomobility and the site, side, and potential directions of immobility, aberrant movement, or hypermobility.
Examination procedures and diagnostic criteria
Uncomplicated JSDS is a clinical diagnosis identified by a collection of presenting symptoms and physical findings. It is not independently detectable by laboratory procedures, and a single gold standard for detecting primary joint subluxation or dysfunction does not currently exist. Often it is suspected after the possibilities of other conditions with a similar presentation have been eliminated. A favorable patient response to manipulation or mobilization (decreased pain or improved function) and reduction or normalization of abnormal physical findings indicates the original working diagnosis and application of manual therapy was a clinically sensible and effective approach.
History
JSDS is commonly symptomatic but the diagnosis does not depend on the patient being symptomatic. However, in asymptomatic JSDS, one would expect the physical findings supporting the diagnosis to be pronounced. In the spine, patients with JSDS commonly complain of pain located in the midline to paraspinal region with or without pain referral into the extremities. Although the somatic referred pain does not usually extend below the knee or upper arm, pain may radiate as far as the foot or hand. However, the location, quality, and referral patterns of the patient’s pain complaints are not unique to this diagnosis. These symptoms overlap with a number of other axial spine complaints and do not differentiate JSDS from other mechanical spine disorders. The patient’s history is also crucial in identifying possible red flags and differentiating nonspecific mechanical back pain from nonmusculoskeletal or nonmechanical NMS disorders. It is also helpful in implicating neurologic involvement and identifying mechanisms of possible injury and load sensitivities pertinent to JSDS.
Physical Examination
With the exception of radiographic evaluation, the majority of the commonly used examination procedures devoted to assessing joint structural and functional integrity are physical examination procedures. They include standard orthopedic, neurologic, and physical examination procedures and a wide array of unique “system technique” diagnostic procedures. Observation and palpation are the most commonly used physical examination procedures and include postural and gait evaluation, soft tissue and bony palpation, global ROM, and segmental ROM testing or what is also referred to as passive intervertebral motion tests.55,74,234 235 236 237 238 239 Manual palpation is the primary evaluative tool, necessitating many hours of practice and concentration to develop adequate skill. The application of joint manipulation relies heavily on the clinician’s ability to locate and identify landmarks, painful musculoskeletal tissue, painful joint movements, contracted muscles, restrictions of motion, and hard EP resistance.240
Specialized laboratory procedures, such as thermography and electromyography (EMG), are presently not in common clinical use for detection of JSDS. Further research is necessary before their role in clinical practice can be fully ascertained. The classic physical signs indicative of JSDS are provocation of pain, abnormalities in alignment, abnormal resistance to joint movement, and altered tissue texture. Bergmann,241 modifying the acronym PARTS from Bourdillon and Day,242 identifies the five diagnostic categories commonly applied by chiropractors for the identification of joint dysfunction: pain and tenderness; asymmetry; ROM abnormality; tone, texture, and temperature abnormality; and special tests. Various investigators have suggested that detection of the spinal manipulative lesion should not rely on a single assessment method.
During spinal evaluation, the physical examination should focus on identifying the source of the patient’s complaints and differentiating segmental from nonsegmental sources. The examination findings supportive of a spinal JSDS diagnosis can be divided into primary and secondary categories and are listed in Box 3-3. It is recommended that the physical assessment of JSDS focus on reproducing the patient’s joint pain with palpation and joint provocation and challenge procedures. Although a number of manual examination findings have historically purported to confirm this disorder, bony and paraspinal soft tissue tenderness or pain reproduced with JP or EP are the most reliable and potentially valid diagnostic tools.243 244 245 246
BOX 3-3 Physical Examination Findings Supportive of Spinal Joint Subluxation/Dysfunction Syndrome Diagnosis
Primary findings
Joint motion is traditionally assessed in its open packed position with joint play (JP) procedures, through its segmental range of motion, and with end play (EP) at the end range of motion. All three components of joint motion are evaluated for quantity, quality, and pain response. Clinical studies indicate that JP and EP are more reliable for pain response than range of motion assessment.
Tissues texture changes are represented by a loss of paraspinal tissue symmetry at the segmental level or between adjacent segments. These changes are characterized by palpable alterations in muscle resting tone (hypo or hypertonicity or spasm) and textural changes characterized by a palpable sense of tissue induration or fibrosis often described as a hardening or thickening of tissue.
Secondary findings
Note: Because of individual variation and the high prevalence of asymmetry many manual therapists do not consider this an indicator of joint dysfunction
It has been suggested that tests should be considered in groupings leading to a multidimensional approach.247 248 249 250 251 A 2006 literature review by Stochkendahl and associates concluded that a “global assessment” (i.e., segmental static and motion tenderness, palpatory altered joint motion, and palpable tissue changes) demonstrates reproducible intraexaminer reliability (0.44 kappa). However, there was not enough evidence to calculate pooled results for interexaminer reliability. The significance of a multidimensional approach is further illustrated by the Health Care Financing Administration requirement that the manipulable lesion be supported by physical examination.252 From the initial coverage of chiropractic care in the Medicare program in 1974–1999, Medicare required x-rays to demonstrate subluxation of the spine and therefore the clinical necessity for chiropractic care. Beginning in 2000, Medicare allowed physical examination findings (the pain and tenderness, asymmetry or misalignment, ROM abnormality, and tissue or tone changes [PARTs] multidimensional approach) for the demonstration of subluxation in place of x-rays: To demonstrate a subluxation based on physical examination, two of the four criteria mentioned under “physical examination” are required, one of which must be asymmetry/misalignment or ROM abnormality.252
Pain and Tenderness
The perception of pain and tenderness is evaluated in terms of location, quality, and intensity. Most primary musculoskeletal disorders manifest by a painful response. The patient’s description of the pain and its location is obtained. Furthermore, the location and intensity of tenderness produced by palpation of osseous and soft tissue are noted. Pain and tenderness findings are identified through observation, percussion, palpation, and provocative orthopedic testing. The patient’s description and location of pain is obtained verbally, physically, or by a pain drawing. The location and intensity of tenderness produced by palpation of osseous and soft tissues is identified and noted. Changes in pain intensity can be objectified using visual analog scales, algometers, and pain questionnaires. The production of palpatory pain over osseous and soft tissues has been found to have good levels of interexaminer and intraexaminer reliability.244,246,253 254 255 256 The validity of motion palpation or pain reproduction with palpation to identify painful spinal joints or direct effective treatment is limited. The results have been mixed but encouraging in a few studies.257 258 259 260 261 262 Although assessment of segmental motion has generally scored poorly in terms of reliability, in several studies lumbar P-A mobility assessment did succeed in achieving acceptable predictor scores (likelihood ratios) for classifying and directing various types of therapies (e.g., manual therapy vs exercise).263,264 In these studies P-A mobility testing was only one of several presentations or physical findings used to categorize patients, and P-A mobility testing may not be a materially contributing factor in predicting outcome.
Asymmetry
Asymmetric qualities are noted on a sectional or segmental level. This includes observation of posture and gait, as well as palpation for misalignment of vertebral segments and extremity joint structures. Asymmetry is identified through observation (posture and gait analysis), static palpation for misalignment of vertebral segments, and evaluation of static plain-film radiographs for malposition of vertebral segments. The complex structure of the human body, and especially its frame, is never completely or perfectly symmetric. Therefore, focal changes in symmetry may or may not be clinically significant. They must be judged by the degree of deviation and placed within the context of the overall clinical presentation and examination.
Range-of-Motion Abnormality
Changes in active, passive, and accessory joint motions on a segmental and sectional basis are noted. These changes may be reflected by increased, decreased, or aberrant motion. It is thought that a decrease in motion is a common component of joint dysfunction. Global ROM changes are measured with inclinometers or goniometers. Segmental ROM abnormalities are identified through the procedures of motion palpation and stress x-ray examination.
Tone, Texture, and Temperature Abnormality
Changes in the characteristics of contiguous and associated soft tissues, including skin, fascia, muscle, and ligaments, are noted. Tissue tone, texture, and temperature (vasomotor skin response) changes are identified through observation, palpation, instrumentation, and tests for length and strength.
Special Tests
The category of special tests includes two major subsets. One group incorporates testing procedures that are specific to chiropractic technique systems, such as specific leg length tests (e.g., Derifield) and muscle tests (e.g., arm fossa test). The other group encompasses laboratory procedures such as x-ray examination, EMG, and thermography.
System technique assessment procedures are typically manual examination procedures. They are commonly the products of individual innovation. They are distinguished from other physical examination procedures by their unique use and association with brand-name techniques. Most of these procedures have not been subjected to testing, and their reliability and validity have not been evaluated.
Many of the laboratory procedures that are promoted as potential detectors of JSDS have substantiated value in evaluating disorders of the NMS system. However, most have not been subjected to in-depth evaluation relative to their ability to detect segmental joint dysfunction. In addition, visceral relationships are considered (e.g., evaluation of the upper thoracic spine in cases of asthma) in localizing the spinal segment or segments that might be dysfunctional.
Clinical usefulness of joint assessment procedures
Although the effectiveness and appropriateness of chiropractic adjustive therapy for treating mechanical neck and back pain has been demonstrated (see Chapter 4), the clinical value and usefulness of many of the diagnostic procedures used to detect JSDS have not been thoroughly or properly evaluated.236,244,253,256,265 266 267 268 269 270 271 272 The clinical usefulness of a diagnostic procedure is measured by its ability to provide accurate information that leads to appropriate and effective management of health care problems. These attributes can be evaluated by assessing a given procedure’s reliability, validity, responsiveness, and utility.
Chiropractic is not alone in its need to advance the critical appraisal of its diagnostic and therapeutic procedures.273 274 275 276 277 Other health disciplines also suffer from significant variations in the use of diagnostic tests, and many lack experimental evaluation and confirmation.278 The prudent practitioner should remain skeptical of unsubstantiated and biologically unfeasible claims, but supportive of and open-minded toward investigation of untested procedures. Untested procedures are not necessarily invalid procedures. It is just as wrong to reject a therapeutic procedure because it is untested as it is to accept the same procedure in the absence of supporting evidence.
It is likely, however, that examination procedures that depend on human evaluation will always carry the potential for some error. Furthermore, quantifying a manual art is difficult because of the lack of a standard for comparison.240 The chiropractic doctor must be aware of these limits, yet constructively use the physical evaluation to help gain the patient’s confidence and compliance. Physical examination procedures placed within proper clinical perspective still provide a significant cost-effective contribution to the formation of a clinical impression. Within this context, it is important not to rely excessively on any one procedure, but rather to use a combination of diagnostic procedures and allow the weight of evidence to build a clinical impression of the patient’s problem.
Reliability
“Reliability is the reproducibility or consistency of measurement or diagnosis. It is the extent to which a test can produce the same result on repeated evaluation of an unchanged characteristic.”271 Reliability estimates the contribution a given test makes to the clinical decision-making process beyond what would be expected by chance. Reliability measures include evaluation for interexaminer and intraexaminer consistency, and test-retest evaluation to determine if measurements are reproducible and consistent over time. Fortunately, the profession has witnessed a significantly increased interest in evaluating its diagnostic procedures. It is now possible to make some generalizations about the reliability of common chiropractic diagnostic procedures.
In 1991, Haas265 reviewed the literature on the reliability of chiropractic joint assessment procedures and concluded that many of the studies had questionable design and statistical analyses. These same conclusions have been echoed repeatedly since then.243,244,256,279 280 281 282 283 284 In addition, most of the studies evaluated the reliability of only one procedure at a time. This leaves the question of combined reliability in need of further evaluation; the procedures may demonstrate higher reliability when used in conjunction with each other.244,245,253,285,286 Furthermore, combining different assessment methods in a multitest regimen more closely parallels actual clinical practice.262,286 There are a number of retrievable studies investigating the utility of multidimensional evaluation procedures.256,286 287 288 289 290 291 Only one primary study showed any reliability approaching acceptable levels, and that varied from marginal to good.256 A systematic review conducted in 2006 implied that multitest regimens did appear to demonstrate acceptable intraexaminer reliability.244 Based on the available research, it has to be concluded that there is insufficient evidence to determine the level of interexaminer reliability of a multidimensional manual examination procedure for detecting manipulable lesions. Certainly further research is warranted to better investigate a multidimensional approach.
Validity
Reliability testing is critical, but it is only one element in the process of assessing the clinical value of diagnostic procedures and it must not be confused with validity. The accuracy, or validity, of a procedure, or the degree to which the test actually evaluates what is intended, is of paramount importance.271 Valid health care procedures are those that are useful in helping heath care providers make accurate and effective heath care decisions.
Although reliability testing for chiropractic joint assessment procedures has expanded significantly in the last several decades, validity testing remains in its infancy. Most chiropractors and manual therapists accept the face validity of common joint assessment292 procedures, but most procedures have not been subjected to rigorous experimental evaluation. Face validity is a measure of a diagnostic procedure’s plausibility (biologic reasonableness) to evaluate a known phenomenon.
Experimental evaluation of diagnostic procedures is necessary to establish their true merit in accurately identifying a given disorder. Experimental evaluation of validity can be broken down into construct-based and criterion-based validity assessments. Construct validity attempts to measure the accuracy of a procedure when a reference standard is not available. Construct validity measures “the ability of a test to perform up to the standards predicted from a theoretical model or construct.”293
Hass and colleagues293 illustrate an example of construct validity evaluation in their assessment of joint motion palpation. Motion palpation theory assumes that EP restriction is a palpable indication for thrust manipulation and that immediate postmanipulative restoration of motion should be palpable in some cases. Therefore, the construct validity of motion palpation for the assessment of EP and manipulable subluxation and dysfunction could be assessed by testing the examiner’s ability to identify EP restrictions and discern if improvement in EP restriction occurs after thrust manipulation.
Criterion-based validity testing allows the evaluation of a diagnostic procedure as it compares with a known gold and coworkers standard procedure.294 The glucose tolerance test is an established criterion for substantiating blood glucose levels. This test could therefore be used as the standard for comparing new tests. There is no established gold standard test for identifying JSDSs.
Responsiveness
The responsiveness of a diagnostic procedure measures its ability to respond to changes in the condition or phenomenon it is assessing. For a testing procedure to be effective in this category, it must demonstrate the ability to change with the entity being evaluated. If a given testing procedure is responsive, it has the ability to reflect improvement or worsening in the condition or function it is measuring. Responsive tests are valuable in measuring the effects of treatment and therefore are effective outcome measures.
Utility
Test utility represents the practical usefulness of a diagnostic test. Clinical utility measures the health benefits provided by a given procedure. It represents the value the procedure has in directing effective patient care. A new diagnostic test demonstrates good clinical utility if it leads to fewer adverse reactions, improved patient care, improved patient outcome, or equal outcome at lower costs. A new radiographic procedure that provides the same information as a palpatory procedure has poor utility and no diagnostic value because it provides the same information at a greater cost and risk to the patient.
Outcome assessment procedures
The limited understanding of the nature, cause, pathophysiologic condition, and diagnostic criteria for identifying JSDSs has stimulated a search for alternative and more valid outcome measures by which to measure the effectiveness of chiropractic care. Escalating health care costs and the need to document the appropriateness and effectiveness of care further illustrate the need for the profession to develop and use valid outcome measures.295 Instead of relying solely on procedures traditionally used to identify JSDS, chiropractors should also use procedures that measure the effect their treatment is having on the patient’s symptoms and function. In this context, the name and nature of the disorder become less of a focus, and more attention is paid to how the patient is functioning and responding to treatment.55,296,297
The disorders commonly treated by chiropractors are painful or have a significant effect on the patient’s ability to function. Therefore, the degree of the patient’s pain and his or her ability to perform physical maneuvers and activities of daily living are important outcome measures of the efficiency and effectiveness of chiropractic treatment. A number of the procedures presented can be used in this context. However, many are more useful in guiding decisions on where and how to adjust patients than they are as outcome measures. Each examination procedure presented includes a brief discussion on the procedure’s clinical usefulness and appropriateness for use as outcome measures.
Symptoms of joint subluxation/dysfunction syndrome
Pain is a common and clinically important sign of JSDS, but JSDS cannot be excluded or confirmed by the presence or absence of pain alone. Pain is considered a subjective finding and some contend that subjective findings such as pain reproduction have less significance than findings that are “objective.” However, many so-called objective tests rely on the patient’s report of pain. For example, the straight-leg raising test is considered an objective test, yet it is the patient’s report of leg pain that constitutes a positive test. This is no different than applying pressure over osseous or soft tissue structures and having the patient report the presence or absence of pain. The use of provocative tests to localize a painful area is therefore a useful means for identifying musculoskeletal problems, including JSDS. These manual physical maneuvers are designed to reproduce the patient’s symptoms or verify the location of pain, thereby giving support for the local presence of a dysfunctional process. Typically, these tests stretch, compress, or distract specific anatomic structures with the patient reporting pain characteristics. When patients experience pain caused by one of these mechanical tests, there is likely to be a local mechanical component contributing to the condition.
Joint dysfunction is typically, but not necessarily, symptomatic. The nature and cause of joint pain and dysfunction cannot be determined from the pain pattern alone. Joint pain does not discriminate between joint hypomobility, hypermobility, and clinical instability. Furthermore, not all structures of the synovial joint are sensitive to pain. Some are very poorly innervated, and some are not innervated at all. The articular cartilage, nondisrupted nucleus pulposus, and cartilaginous end plates are devoid of nociceptive innervation.231 Thus pathologic change within certain articular structures may be insidious and well advanced before it becomes symptomatic.
Spinal or extremity joint pain is often poorly localized, and sites of pain and pathologic conditions may not necessarily correspond. Disorders of the musculoskeletal system are often associated with areas of referred pain and hypalgesia.298,299
Referred pain is sclerogenic, ill-defined, deep, and achy. It is referred from the deep somatic tissues of the involved joint to the corresponding sclerotome. The anatomic sites of referred pain correspond to tissues that share the same segmental innervation (Figure 3-11).
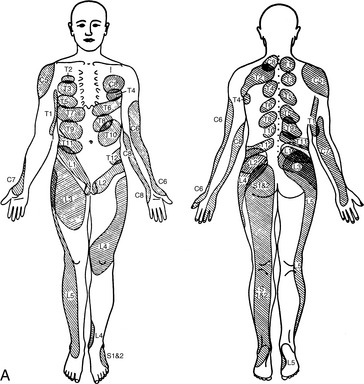
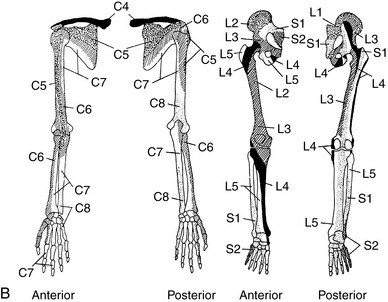
Figure 3-11 Segmental areas of pain of deep somatic origin. A, Interspinous ligament injection—Kellgren. B, Sclerotomal pain patterns.
(A from Lewis T: Pain, New York, 1942, Macmillan. B from Grieve GP: Common vertebral joint problems, ed 2, Edinburgh, 1988, Churchill Livingstone.)
Sites of referred pain may be more painful to palpation and of greater intensity than the site of injury. The common phenomenon of interscapular pain with cervical joint derangement or disc herniation illustrates this point. The body is also more adept at discriminating sensations on the surface than pain originating in deep somatic structures and joints.298,299 Ordinarily, the closer the affected tissue is to surface of the body, the better the pain coincides to the site of injury.
Joint pain of mechanical origin characteristically has pain-free intervals, whereas joint pain associated with inflammation is more constant. Joint movement and the activities of daily living often aggravate mechanical joint pain. Although it is often alleviated by deceased activity, total immobilization may accentuate the pain response. Pain diagrams, visual and verbal analog scales (Figure 3-12), and functional capacity questionnaires are very helpful measures in the examination and quantification of painful complaints.300 301 302 303 304 305 306
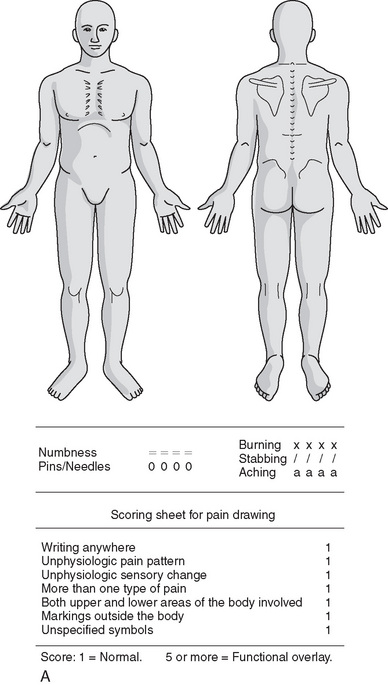
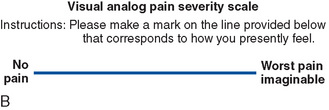
Figure 3-12 Tools to localize and record pain intensity. A, Pain diagram. B, Visual analog scale.
(A adapted from Mooney V, Robertson J: Clin Orthop 115:149, 1976.)
Because the character, location, quality, and intensity of pain can vary greatly from individual to individual and from disorder to disorder, it is essential to subject all painful joint disorders to a thorough physical examination and to rule out contraindications before considering adjustive therapy.
Patient observation
The examination of any regional complaint begins with superficial observation and investigation for any signs of trauma or inflammation. These signs include abrasions, lacerations, scars, discoloration, bruises, erythema, pallor, swelling, or misalignment. Acute injury, congenital or developmental defects, and many systemic diseases of the NMS are often represented by abnormalities observed in posture or gait.
The human body uses an ingenious three-dimensional framework of bones, joints, muscles, and ligaments for posture and movement.307 Therefore, the observational evaluation of NMS function routinely incorporates an assessment of patient symmetry, posture, and locomotion. The examination is based on the premise that there is a postural ideal that can be used as a comparative standard and that deviations in posture, gait, or movement may identify NMS disease or dysfunction or predispose an individual to NMS disease or dysfunction. Poor posture can be viewed as a faulty relationship of bones, ligaments, and muscles that produces an increased stress on the supporting structures leading to decreased efficiency for maintaining the body’s balance over its base of support. Ample evidence supports the association of painful disorders of the NMS with restrictions to joint motion and abnormalities in posture.308 309 310 311 312 313 314 315 316 317 318 319 320 321
Evidence also suggests that deviations from “ideal posture” may predispose an individual to NMS dysfunction and possible joint degeneration.199,322 323 324 325 326 However, the degree of deviation necessary to affect a patient’s health has not been established. Individual biologic variation and adaptability certainly play a role in limiting the development and morbidity of joint dysfunction and degenerative joint disease. Those that would set a narrow standard for posture and ROM ignore the research evidence that suggests a range of normal individual variation.23,316,324,327 328 329 330 331 332 333 334 335
Gait Evaluation
Gait evaluation is conducted formally during the physical examination, but it begins as the patient walks into the examination room. Locomotion involves integrated activity of numerous components of the motor system and therefore becomes an efficient method for screening NMS function.
The objectives of gait analysis are to identify deviations, to obtain information that may assist in determining the cause of the deviations, and to provide a basis for the use of therapeutic procedures or supportive devices to improve the walking pattern.336 There are two basic phases of the normal pattern of gait: one involves a weight-bearing period (stance phase) and the other, a non–weight-bearing period (swing period) (Figure 3-13). Disease or dysfunction may affect one phase and not the other, necessitating careful evaluation of both components.
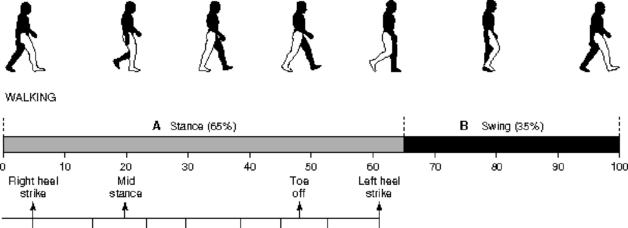
Figure 3-13 The phases of gait. A, Stance phase. B, Swing phase.
(Modified from Adelaar RS: Am J Sports Med 14:497, 1986.)
Evaluation begins with a general impression of locomotion. Is it guarded or painful? Is the patient protective of any part or unwilling to put equal weight on each leg?
The movements of the upper and lower extremities are noted. Length of stride, degree of pronation or supination, tilt of pelvis, adaptational movements of the shoulder girdle, and pendulousness of the arms are assessed. Specific components of gait evaluation are listed in Box 3-4, and disorders that may alter gait are listed in Box 3-5.
BOX 3-4 Components of Gait Evaluation
Apparent abnormal findings or deviations from the expected pattern identified with gait analysis must be supported or validated by other test procedures, including muscle tests for strength, length, tone, and texture, as well as tests for joint function.
Postural Evaluation
Like all physical examination skills, postural evaluation must be learned and practiced. Reliable and accurate assessment is founded on attention to proper technique. The room must be appropriately lit to clearly illuminate the body parts being examined and to prevent shadows from projecting false contours. The doctor should be oriented to the patient so that the dominant eye is located in the midline between the landmarks being compared.337 If observing the patient while he or she is supine or prone, the doctor stands on the side of eye dominance (Box 3-6).
When combining observation and palpation of asymmetry, it is important that the doctor’s hands and eyes are on the same reference plane. For example, when evaluating the relative heights of the iliac crests, the doctor places a hand on each crest and positions the dominant eye in the midline on the same plane as his or her hands.
The assessment of symmetry, locomotion, and posture is critical in the evaluation of NMS dysfunction. They are objective signs supportive of NMS disease or injury310 and effective outcome measures for monitoring patient progress. Regional asymmetry should trigger further evaluation of that area, but asymmetry alone does not confirm or rule out the presence of segmental subluxation and dysfunction syndromes.
Postural asymmetry is a challenge to homeostatic regulation and does indicate potential areas of muscular imbalance, bony asymmetry, and mechanical stress. Its relationship to initiating, predisposing, or perpetuating segmental dysfunction should not be overlooked. In a rush to find the specific level of spinal JSDS, chiropractors often overlook significant postural decompensations that may predispose the patient to pain and dysfunction. The patient with extremity or spinal complaints may not respond to local therapy until gait and postural stresses are removed.
Spinal Postural Evaluation
Although deviations in spinal posture do not identify the presence or absence of a specific level of spinal dysfunction, deviations do provide evidence of underlying postural syndromes or the presence of painful NMS conditions. Spinal postural assessment has demonstrated satisfactory reliability309,338 339 340 and validity as a screening procedure for distinguishing symptomatic myofascial back pain subjects from normal subjects.310 In this capacity, it may function as a useful outcome measure to document changes in painful antalgic postures associated with NMS disease and dysfunction.
During standing postural assessment, the patient is instructed to assume a relaxed stance, looking straight ahead, with feet approximately 4 to 6 inches apart and arms hanging loose at the sides. The patient should be in a gown or undergarments, and should not be wearing shoes. If the patient has orthotics or corrective footwear, posture is assessed with the patient’s shoes both off and on. The evaluation is conducted from the posterior and anterior to determine distribution of weight and symmetry of landmarks in the coronal plane and from the side to evaluate posture and landmarks relative to the center of gravity line. In addition, the upper and lower extremities are surveyed for deformity, pronation or supination, and internal or external rotation.
The examination should include a determination of the carriage of the center of gravity and symmetry of key bony and soft tissue landmarks. Any curvatures, scoliosis, or rib humps should be measured and recorded. The flexibility (Adams test) of the curve should also be determined and noted.
The evaluation of spinal posture may be aided by the use of a plumb line (Figure 3-14) and devices such as the posturometer, scoliometer, and bilateral weight scales. The plumb line assessment from the posterior should find the gravity line, splitting the body into equal left and right halves. The plumb line should pass from the external occipital protuberance through the center of the spinal column to the center of the sacrum and points equidistant from the knees and ankles. The lateral plumb line assessment has the gravity line splitting the body into equal front and back portions. The plumb line should pass from the external auditory meatus down through the shoulder joint to the greater trochanter of the femur, continuing down to just anterior to the midline of the knee and slightly anterior to the lateral malleolus.
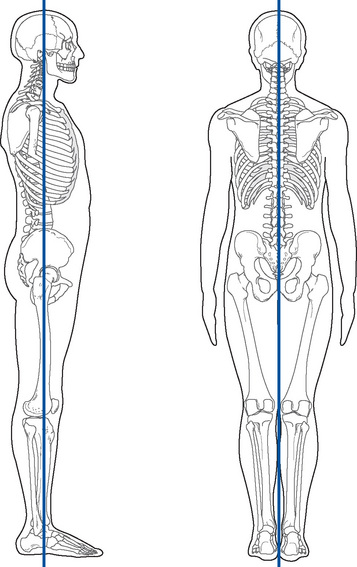
Figure 3-14 Anteroposterior and lateral plumb line evaluation of spinal posture.
In a patient with suspected scoliosis, an assessment for potential leg length inequality and a screen for anatomic or functional leg length discrepancy should be included. Suspected anatomic discrepancy should be measured and radiographically confirmed if clinically significant. Postural distortions with possible muscle imbalance causes are identified in Table 3-2.
TABLE 3-2 Common Postural Findings With Possible Muscular Imbalances
| A-P or P-A Postural | Examination |
|---|---|
| Head tilt | Neck extensors and/or scalenes |
| Head rotation/tilt | SCM |
| Shoulder tilt | Trapezius (upper, lower) latissimus |
| Scapular winging | Serratus anterior |
| Scapular heights | Rhomboids |
| Arm rotation | Subscapularis, teres minor, infraspinatus |
| Pelvic unleveling | TFL, adductors, psoas, quadratus lumborum, gluteals |
| Genu valgus/varus | TFL, sartorius, gracilis |
| Leg rotation | Hamstrings, tibialis anterior, peroneus, piriformis, psoas |
| Lateral Postural | Examination |
|---|---|
| Forward head carriage | Neck extensors, longus coli, scalenes |
| Thoracic kyphosis | Trapezius (middle and lower) |
| Lumbar lordosis | Psoas |
| Pelvic tilt | Quadriceps, hamstrings, sartorius, gracilis, abdominals, gluteus maximus |
| Forward lean | Gastrocnemius, soleus |
| Knee hyperextension | Quadriceps, popliteus, gastrocnemius, soleus |
A-P, Anterior-to-posterior; P-A, posterior-to-anterior; SCM, sternocleidomastoid; TFL, tensor fascia lata.
The identification of postural imbalances can be helpful in diagnosing disorders or in guiding clinical treatments. In some cases it may be central to the identification of the underlying disorder, such as idiopathic scoliosis, and in others it can help guide treatment decisions, such as exercise prescription in patients with postural imbalances and LBP. Subsequent evaluations are used to monitor progress and make decisions about treatment changes. The significance and usefulness of these evaluations depend on repeatability sufficient to ensure that ensuing changes are attributable to the prescribed treatment program and not to any naturally occurring variability in posture. This may not be attainable in all clinical situations; Dunk and coworkers341 demonstrated that the ability to return to the same starting posture exhibited poor to moderate repeatability. This brings into question the benefit and validity of using small deviations from ideal spinal posture in clinical decision making. Therefore, users of postural analysis tools should interpret small to modest postural deviations from a vertical reference with caution, because there are many inherent factors that can contribute to the variability of these measured postures.341 Studies have also demonstrated that visual assessments for an increase or decrease in cervical or lumbar lordosis are not reliable or accurate.342,343
Leg Length Evaluation
The evaluation of leg length inequality incorporates consideration for both anatomic and functional discrepancies. Anatomic inequality results primarily from osseous asymmetry. Functional leg length inequality implies that the legs are anatomically of equal length but appear unequal as a result of a disorder in the NMS system. Anatomic asymmetry is viewed as a potential source of derangement and dysfunction that is potentially treatable with heel or sole lifts. Functional asymmetry is viewed primarily as a consequence of dysfunction.
Leg length evaluation has a long history of affiliation with chiropractic, and functional leg length inequality is considered an important sign of spinal or pelvic subluxation/dysfunction syndromes.344 Spinal joint dysfunction is hypothesized to potentially affect leg length by inducing reflex alterations in spinal muscle balance and unleveling of the pelvis and legs.344 345 346
Disturbances in sacroiliac function and pelvic alignment are theorized to induce torsion between the innominates and affect leg length by creating positional changes in the femoral heads or imbalances in hip flexor and extensor muscle tone.344 A significant percentage of practicing chiropractors and a number of system technique methods emphasize the role of leg length evaluation in detecting spinal subluxations/dysfunction and directing decisions on where, when, and how to adjust patients.345 346 347 Leg alignment change in response to provocative springing (vertebral challenge) is used by some chiropractic techniques to determine the level of spinal dysfunction and direction of therapeutic adjustive thrust.346
Leg length equality can be assessed by physical means or by radiographic evaluation. Evaluation of inequality by physical means includes procedures that assess leg length through direct tape measurement, by visual inspection, or indirectly through combined visual and palpatory assessment of symmetry. Physical measures are appropriately used to screen for leg length inequality, estimate the amount of any noted discrepancy, and participate in differentiating anatomic leg length inequality from functional leg length inequality. Physical assessment procedures cannot determine exact differences in anatomic length.
X-ray evaluation is necessary when precise determination of leg length is required. Radiographic procedures should not be used to screen for possible leg length inequality. X-ray evaluation of leg length should be considered only after suspicion of a significant anatomic leg discrepancy is identified and corrective heel or shoe lifts are being contemplated. Radiographic procedures include both standing and supine methods. Radiographic evaluations are recognized as reliable and valid procedures for determining anatomic leg length discrepancies.345
Standing methods are used to assess the comparative height of the femoral heads and include full spine, lumbar, and femoral head views. Femoral head views afford the most accurate evaluation of femoral head height because they eliminate the false appearance of inequality that can result from rotation of the patient’s pelvis during patient positioning. When precise comparison of length is desired, supine methods are usually used. Of these, the scanogram is the method most commonly used.
The most common physical assessment method used in chiropractic practice combines visual assessment and palpation of symmetric bony landmarks. Evaluation is performed with the patient in a prone or supine position, with his or her shoes on or off, and the doctor standing at the end of the table. The doctor evaluates equality by contacting and comparing the inferior poles of the medial malleoli, the soles of the shoe, or the patient’s heels (Figure 3-15). It is advisable to remove the shoes if significant shoe wear is present or if the doctor suspects that the patient’s heel and shoe cannot remain in firm contact. When using the soles of the shoe or the patient’s heels as the comparative landmark, it is important for the doctor to neutralize the ankles to prevent eversion or inversion from creating a false appearance of inequality.

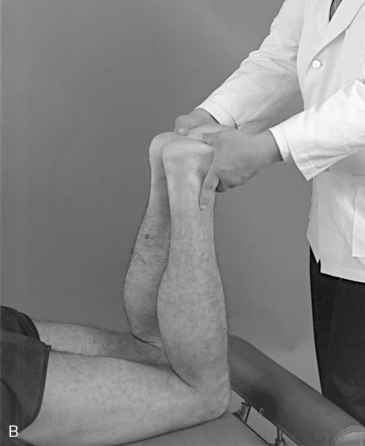
Figure 3-15 Prone evaluation of leg length. A, Evaluation for symmetry of leg length by comparing the patient’s heels or inferior poles of the malleoli. B, Evaluation of tibial length by comparing heel symmetry in a flexed-knee position.
If leg length inequality is noted in the prone position, the doctor bends the patient’s legs to 90 degrees and again observes for inequality. If the inequality remains anatomic, shortening of one tibia is considered. If the heels approach or reach equal height, some degree of functional leg length inequality is suspected. Various interpretations of this process (leg checks) have been developed and are in common use. The Derifield pelvic leg check is foremost in this regard and is commonly affiliated with the Activator and Thompson technique systems.348,349 The specifics of this test are presented in Chapter 5 in the section covering pelvic evaluation procedures.
Despite the common use of physical procedures to detect leg length inequality, significant questions concerning the clinical significance and reliability, validity, and responsiveness of these methods remain.265,344,345,347,350 Procedures using tape measurement, iliac crest comparative height checks, or visual leg checks to assess comparative leg length have demonstrated mixed results.345 These procedures have demonstrated both poor and good interexaminer reliability.346,347,351 352 353 354 355 356 357 A significant number of the studies using visual leg checks have been criticized for poor experimental design or statistical analysis.265,344,345 Leg length inequality testing has also failed to respond as predicted to thoracic rotary vertebral challenge and thoracic adjustment.346,358 Schneider and associates346 performed an interexaminer reliability evaluation of the prone leg length analysis procedure and found good reliability in determining the side of the short leg in the prone position with knees extended, but found poor reliability when determining the precise amount of that leg length difference. In addition, they found that the head rotation test for assessing changes in leg length was unreliable in this sample of patients, nor did there appear to be any correlation between the side of pain noted by the patient and the side of the short leg. It was interesting to note that all 45 patients in this sample were found by both clinicians to have a short leg.346 The weakest element in the leg check procedure is the second position, with the knees bent to 90 degrees, in which overall agreement is poor, reaching only as high as “fair” 25% of the time.345,356
The validity of visual leg checks for anatomic accuracy or subluxation and dysfunction detection has yet to be evaluated clinically. Cooperstein and colleagues did determine that visual leg checks were accurate in measuring artificially induced leg length inequality,357 but no studies have been done to measure their relationship to level of spinal dysfunction or treatment outcomes. Because of the lack of validity testing, it is difficult to form any definitive conclusions as to the clinical utility of these procedures.345
Range-of-motion assessment
Measurement of joint mobility is a critical element in the evaluation of NMS function, and qualitative and quantitative evaluation of joint motion is a fundamental component of the examination of the NMS system. Significant limitation and asymmetry of movement is considered to be evidence of NMS impairment,359 and improvement in regional mobility may be a valuable outcome measure for assessing effectiveness of treatment.
Disorders capable of altering individual joint and regional spinal movements are extensive. They include joint subluxation/dysfunction, dislocation, effusion, joint mice, myofibrosis, periarticular fibrosis, muscle hypertrophy, degenerative joint disease, muscle guarding, and fracture. Other nontraumatic disease states with pathologic effects on somatic structures or the nervous system also produce abnormalities in movement.
Although regional ROM assessment has demonstrated the ability to differentiate individuals with low back disorders from those without,310,360 spinal abnormalities in GROM are more valuable in identifying and monitoring NMS dysfunction than confirming a specific level of joint subluxation/dysfunction. Regional abnormalities in range of spinal motion are potential signs of dysfunction, but they do not confirm the presence of segmental joint dysfunction. GROM may be falsely positive in situations in which spinal injuries or disease affects the nonsegmental somatic tissues and spares the vertebral joints. In these circumstances, altered regional movements are present, but the loss of mobility is uniform, and the individual spinal motion segments demonstrate normal JP and EP (feel). Conversely, normal regional ROM may be falsely negative in circumstances in which individual spinal joint restrictions are concealed by compensatory hypermobility at adjacent joints.
Evaluation of repeated regional spinal movements in conjunction with the patient’s description of pain and limitations to movement have been promoted as effective tools for diagnostically classifying back pain patients.361,362 The information gained about the patient’s symptomatic and mechanical responses to loading allows the clinician to determine which specific movements, positions, and activities to either pursue or avoid in the treatment plan.
The McKenzie method of evaluation and treatment is the most widely practiced procedure using repeat movements to classify back pain patients. It is common for chiropractors to use McKenzie diagnostic procedures, but is more commonly used by physical therapists. Donelson, Aprill, and Grant362 demonstrated that the procedures were capable of reliably differentiating discogenic from nondiscogenic pain and a competent from an incompetent annulus. In comparison with MRI, it also demonstrated superior ability in distinguishing painful from nonpainful discs.362 In a later commentary article, Delany and Hubka363 re-evaluated the data from the original study and concluded that the study demonstrated “informative but not definitive” ability to detect discogenic pain. They concluded that “high sensitivity but low to moderate specificity was demonstrated.”
Early reliability testing of McKenzie procedures demonstrated mixed results.364,365 However, recent studies have concluded that the McKenzie method demonstrates good reliability for classifying patients into syndrome categories based on repeated movements and the principle of centralization of pain.366 367 368
Measurement Procedures
Methods for assessing mobility are commonly used and include both visual and instrument-based procedures. They range from goniometric and inclinometric measurements to the more technical approaches of computerized digitation.308,369 Visual observation and the fingertip-to-floor method of recording motion have demonstrated mixed reliability370 and are considered to be invalid tests because they cannot effectively differentiate lumbar mobility from hip or thoracic movement. The modified Schober method of measuring lumbar mobility has shown consistent reliability, but it has limited use because it measures only lumbar flexion.370 371 372
The use of inclinometers for spinal ROM and inclinometers or goniometers for extremity ROM is becoming a minimal standard.359 For the spine, the one- or two-inclinometer method as described by Mayer and associates308 is a reliable, inexpensive, and efficient technique. With the exception of one study,373 evaluation of motion with hand-held inclinometric measuring devices has demonstrated consistent reproducibility within and between examiners.308,370,371,372 373 374 375 376 It can be used in the measurement of all spinal movements, including trunk rotation, when the spine is in a flexed position (Figures 3-16 and 3-17). However, the range of trunk rotation is significantly limited when it is placed in a flexed position. In the spine, quantitative measures of joint mobility rely primarily on regional ROM measures as a result of joint inaccessibility and limited ROM. Methods for estimating the quality and quantity of individual spinal motion through manual palpation have been developed and are covered regionally in Chapter 5.




Figure 3-16 Measurement of lumbar range of motion using dual inclinometers. A, neutral starting position for evaluating flexion and extension; B, measurement of extension; C, measurement of flexion; D, measurement of left lateral flexion. (Evans, RC: Illustrated orthopedic physical assessment, ed 3, Mosby, Elsevier, St. Louis, Mo 2009.)

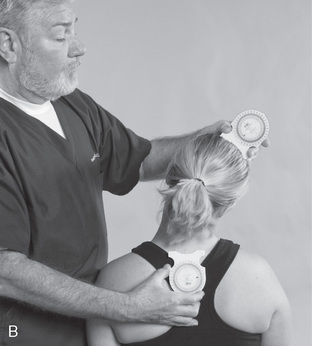


Figure 3-17 Measurement of cervical ranges of motion using dual inclinometers. A, measurement of extension; B, measurement of right lateral flexion; C, neutral starting position for measuring rotation; D, measurement of right rotation. (Evans RC: Illustrated orthopedic physical assessment, ed 3, Mosby, Elsevier, St. Louis, Mo 2009.)
Evaluation of spinal and extremity mobility must take into consideration the normal variations that exist between individuals and gender. Alterations in mobility may be a product of occupation, recreation, or aging, and may not be associated with dysfunction or pain. This increases the importance of making a bilateral comparison of joint and spinal mobility.
Spinal and extremity joint motion are measured in degrees relative to the zero or starting position. In a patient demonstrating 50 degrees of cervical extension and 55 degrees of cervical flexion, the motion is recorded as “EXT/FL 50-0-55.” All physiologic movements, on both sides of the zero position (0 degrees), should be measured and recorded. Table 3-3 outlines the common format for recording spinal and extremity ROM.
TABLE 3-3 Assessment of Spinal and Extremity Motion
| Spinal Motion | ||
|---|---|---|
| Extension | 0 | Flexion |
| Right lateral bending | 0 | Left lateral bending |
| Right rotation | 0 | Left rotation |
| Extremity Motion | ||
|---|---|---|
| Extension | 0 | Flexion |
| Abduction | 0 | Adduction |
| External rotation | 0 | Internal rotation |
| Supination | 0 | Pronation |
| Radial deviation | 0 | Ulnar deviation |
| Inversion | 0 | Eversion |