Chapter 8 The First Year
Advances in imaging permit us to understand the anatomic and physiologic correlates of the physical growth, maturation, acquisition of competence, and psychologic reorganization that characterizes infancy and radically change the infant’s behavior and social relationships. Some activities previously thought to be “primitive” or “reflexive” result from complex systems. Swallowing, rather than a simple reflex, results from a complex highly coordinated process involving multiple levels of neural control distributed among several physiologic systems whose nature and relationships mature throughout the 1st year of life. Substantial learning of the basic tools of language (phonology, word segmentation) occurs during infancy. Speech processing in older individuals requires defined and precise neuronal networks; imaging studies have revealed that the infant brain possesses a structural and functional organization similar to that of adults, leading to the belief that structural neurologic processing of speech may guide infants to discover the properties of his or her native language. Myelination of the cortex begins at 8 mo gestation and is nearly complete by age 2 yr; much of this process occurs during infancy. Given the importance of iron and other nutrients in myelination, adequate stores throughout infancy are critical (Chapter 42). Inadequate dietary intake, insufficient interactions with caregivers, or both may alter experience-dependent processes that are critical to brain structure development and function during infancy. Although some of these processes may be delayed, as the periods of plasticity close during the rapid developmental changes occurring in infancy, more permanent deficits may result.
The infant acquires new competences in all developmental domains. The concept of developmental trajectories recognizes that complex skills build on simpler ones; it is also important to realize how development in each domain affects functioning in all of the others. Physical growth parameters and normal ranges for attainable weight, length, and head circumference are found in the Centers for Disease Control and Prevention growth charts (see Figs. 9-1 and 9-2 on the Nelson Textbook of Pediatrics website at www.expertconsult.com ![]() ). Table 8-1 presents an overview of key milestones by domain; Table 8-2 presents similar information arranged by age. Table 8-3 presents age at time of appearance on x-ray of centers of ossification. Parents often seek information about “normal development” during this period and should be directed to reliable sources, including the American Academy of Pediatrics website (www.AAP.org).
). Table 8-1 presents an overview of key milestones by domain; Table 8-2 presents similar information arranged by age. Table 8-3 presents age at time of appearance on x-ray of centers of ossification. Parents often seek information about “normal development” during this period and should be directed to reliable sources, including the American Academy of Pediatrics website (www.AAP.org).
Table 8-1 DEVELOPMENTAL MILESTONES IN THE FIRST 2 YR OF LIFE
| MILESTONE | AVERAGE AGE OF ATTAINMENT (MO) | DEVELOPMENTAL IMPLICATIONS |
|---|---|---|
| GROSS MOTOR | ||
| Holds head steady while sitting | 2 | Allows more visual interaction |
| Pulls to sit, with no head lag | 3 | Muscle tone |
| Brings hands together in midline | 3 | Self-discovery of hands |
| Asymmetric tonic neck reflex gone | 4 | Can inspect hands in midline |
| Sits without support | 6 | Increasing exploration |
| Rolls back to stomach | 6.5 | Truncal flexion, risk of falls |
| Walks alone | 12 | Exploration, control of proximity to parents |
| Runs | 16 | Supervision more difficult |
| FINE MOTOR | ||
| Grasps rattle | 3.5 | Object use |
| Reaches for objects | 4 | Visuomotor coordination |
| Palmar grasp gone | 4 | Voluntary release |
| Transfers object hand to hand | 5.5 | Comparison of objects |
| Thumb-finger grasp | 8 | Able to explore small objects |
| Turns pages of book | 12 | Increasing autonomy during book time |
| Scribbles | 13 | Visuomotor coordination |
| Builds tower of 2 cubes | 15 | Uses objects in combination |
| Builds tower of 6 cubes | 22 | Requires visual, gross, and fine motor coordination |
| COMMUNICATION AND LANGUAGE | ||
| Smiles in response to face, voice | 1.5 | More active social participant |
| Monosyllabic babble | 6 | Experimentation with sound, tactile sense |
| Inhibits to “no” | 7 | Response to tone (nonverbal) |
| Follows one-step command with gesture | 7 | Nonverbal communication |
| Follows one-step command without gesture | 10 | Verbal receptive language (e.g., “Give it to me”) |
| Says “mama” or “dada” | 10 | Expressive language |
| Points to objects | 10 | Interactive communication |
| Speaks first real word | 12 | Beginning of labeling |
| Speaks 4-6 words | 15 | Acquisition of object and personal names |
| Speaks 10-15 words | 18 | Acquisition of object and personal names |
| Speaks 2-word sentences (e.g., “Mommy shoe”) | 19 | Beginning grammaticization, corresponds with 50 word vocabulary |
| COGNITIVE | ||
| Stares momentarily at spot where object disappeared | 2 | Lack of object permanence (out of sight, out of mind [e.g., yarn ball dropped]) |
| Stares at own hand | 4 | Self-discovery, cause and effect |
| Bangs 2 cubes | 8 | Active comparison of objects |
| Uncovers toy (after seeing it hidden) | 8 | Object permanence |
| Egocentric symbolic play (e.g., pretends to drink from cup) | 12 | Beginning symbolic thought |
| Uses stick to reach toy | 17 | Able to link actions to solve problems |
| Pretend play with doll (e.g., gives doll bottle) | 17 | Symbolic thought |
Table 8-2 EMERGING PATTERNS OF BEHAVIOR DURING THE 1ST YEAR OF LIFE*
| NEONATAL PERIOD (1ST 4 WK) | |
| Prone: | Lies in flexed attitude; turns head from side to side; head sags on ventral suspension |
| Supine: | Generally flexed and a little stiff |
| Visual: | May fixate face on light in line of vision; “doll’s-eye” movement of eyes on turning of the body |
| Reflex: | Moro response active; stepping and placing reflexes; grasp reflex active |
| Social: | Visual preference for human face |
| AT 1 MO | |
| Prone: | Legs more extended; holds chin up; turns head; head lifted momentarily to plane of body on ventral suspension |
| Supine: | Tonic neck posture predominates; supple and relaxed; head lags when pulled to sitting position |
| Visual: | Watches person; follows moving object |
| Social: | Body movements in cadence with voice of other in social contact; beginning to smile |
| AT 2 MO | |
| Prone: | Raises head slightly farther; head sustained in plane of body on ventral suspension |
| Supine: | Tonic neck posture predominates; head lags when pulled to sitting position |
| Visual: | Follows moving object 180 degrees |
| Social: | Smiles on social contact; listens to voice and coos |
| AT 3 MO | |
| Prone: | Lifts head and chest with arms extended; head above plane of body on ventral suspension |
| Supine: | Tonic neck posture predominates; reaches toward and misses objects; waves at toy |
| Sitting: | Head lag partially compensated when pulled to sitting position; early head control with bobbing motion; back rounded |
| Reflex: | Typical Moro response has not persisted; makes defensive movements or selective withdrawal reactions |
| Social: | Sustained social contact; listens to music; says “aah, ngah” |
| AT 4 MO | |
| Prone: | Lifts head and chest, with head in approximately vertical axis; legs extended |
| Supine: | Symmetric posture predominates, hands in midline; reaches and grasps objects and brings them to mouth |
| Sitting: | No head lag when pulled to sitting position; head steady, tipped forward; enjoys sitting with full truncal support |
| Standing: | When held erect, pushes with feet |
| Adaptive: | Sees pellet, but makes no move to reach for it |
| Social: | Laughs out loud; may show displeasure if social contact is broken; excited at sight of food |
| AT 7 MO | |
| Prone: | Rolls over; pivots; crawls or creep-crawls (Knobloch) |
| Supine: | Lifts head; rolls over; squirms |
| Sitting: | Sits briefly, with support of pelvis; leans forward on hands; back rounded |
| Standing: | May support most of weight; bounces actively |
| Adaptive: | Reaches out for and grasps large object; transfers objects from hand to hand; grasp uses radial palm; rakes at pellet |
| Language: | Forms polysyllabic vowel sounds |
| Social: | Prefers mother; babbles; enjoys mirror; responds to changes in emotional content of social contact |
| AT 10 MO | |
| Sitting: | Sits up alone and indefinitely without support, with back straight |
| Standing: | Pulls to standing position; “cruises” or walks holding on to furniture |
| Motor: | Creeps or crawls |
| Adaptive: | Grasps objects with thumb and forefinger; pokes at things with forefinger; picks up pellet with assisted pincer movement; uncovers hidden toy; attempts to retrieve dropped object; releases object grasped by other person |
| Language: | Repetitive consonant sounds (“mama,” “dada”) |
| Social: | Responds to sound of name; plays peek-a-boo or pat-a-cake; waves bye-bye |
| AT 1 YR | |
| Motor: | Walks with one hand held (48 wk); rises independently, takes several steps (Knobloch) |
| Adaptive: | Picks up pellet with unassisted pincer movement of forefinger and thumb; releases object to other person on request or gesture |
| Language: | Says a few words besides “mama,” “dada” |
| Social: | Plays simple ball game; makes postural adjustment to dressing |
* Data are derived from those of Gesell (as revised by Knobloch), Shirley, Provence, Wolf, Bailey, and others.
From Knobloch H, Stevens F, Malone AF: Manual of developmental diagnosis, Hagerstown, MD, 1980, Harper & Row.
Table 8-3 TIME OF APPEARANCE IN X-RAYS OF CENTERS OF OSSIFICATION IN INFANCY AND CHILDHOOD
| BOYS—AGE AT APPEARANCE* | BONES AND EPIPHYSEAL CENTERS | GIRLS—AGE AT APPEARANCE* |
|---|---|---|
| HUMERUS, HEAD | ||
| 3 wk | 3 wk | |
| CARPAL BONES | ||
| 2 mo ± 2 mo | Capitate | 2 mo ± 2 mo |
| 3 mo ± 2 mo | Hamate | 2 mo ± 2 mo |
| 30 mo ± 16 mo | Triangular† | 21 mo ± 14 mo |
| 42 mo ± 19 mo | Lunate† | 34 mo ± 13 mo |
| 67 mo ± 19 mo | Trapezium† | 47 mo ± 14 mo |
| 69 mo ± 15 mo | Trapezoid† | 49 mo ± 12 mo |
| 66 mo ± 15 mo | Scaphoid† | 51 mo ± 12 mo |
| No standards available | Pisiform† | No standards available |
| METACARPAL BONES | ||
| 18 mo ± 5 mo | II | 12 mo ± 3 mo |
| 20 mo ± 5 mo | III | 13 mo ± 3 mo |
| 23 mo ± 6 mo | IV | 15 mo ± 4 mo |
| 26 mo ± 7 mo | V | 16 mo ± 5 mo |
| 32 mo ± 9 mo | I | 18 mo ± 5 mo |
| FINGERS (EPIPHYSES) | ||
| 16 mo ± 4 mo | Proximal phalanx, 3rd finger | 10 mo ± 3 mo |
| 16 mo ± 4 mo | Proximal phalanx, 2nd finger | 11 mo ± 3 mo |
| 17 mo ± 5 mo | Proximal phalanx, 4th finger | 11 mo ± 3 mo |
| 19 mo ± 7 mo | Distal phalanx, 1st finger | 12 mo ± 4 mo |
| 21 mo ± 5 mo | Proximal phalanx, 5th finger | 14 mo ± 4 mo |
| 24 mo ± 6 mo | Middle phalanx, 3rd finger | 15 mo ± 5 mo |
| 24 mo ± 6 mo | Middle phalanx, 4th finger | 15 mo ± 5 mo |
| 26 mo ± 6 mo | Middle phalanx, 2nd finger | 16 mo ± 5 mo |
| 28 mo ± 6 mo | Distal phalanx, 3rd finger | 18 mo ± 4 mo |
| 28 mo ± 6 mo | Distal phalanx, 4th finger | 18 mo ± 5 mo |
| 32 mo ± 7 mo | Proximal phalanx, 1st finger | 20 mo ± 5 mo |
| 37 mo ± 9 mo | Distal phalanx, 5th finger | 23 mo ± 6 mo |
| 37 mo ± 8 mo | Distal phalanx, 2nd finger | 23 mo ± 6 mo |
| 39 mo ± 10 mo | Middle phalanx, 5th finger | 22 mo ± 7 mo |
| 152 mo ± 18 mo | Sesamoid (adductor pollicis) | 121 mo ± 13 mo |
| HIP AND KNEE | ||
| Usually present at birth | Femur, distal | Usually present at birth |
| Usually present at birth | Tibia, proximal | Usually present at birth |
| 4 mo ± 2 mo | Femur, head | 4 mo ± 2 mo |
| 46 mo ± 11 mo | Patella | 29 mo ± 7 mo |
| FOOT AND ANKLE‡ | ||
Values represent mean ± standard deviation, when applicable.
† Except for the capitate and hamate bones, the variability of carpal centers is too great to make them very useful clinically.
‡ Standards for the foot are available, but normal variation is wide, including some familial variants, so this area is of little clinical use.
The norms present a composite of published data from the Fels Research Institute, Yellow Springs, OH (Pyle SI, Sontag L: AJR Am J Roentgenol 49:102, 1943), and unpublished data from the Brush Foundation, Case Western Reserve University, Cleveland, OH, and the Harvard School of Public Health, Boston, MA. Compiled by Lieb, Buehl, and Pyle.
Age 0-2 Months
Myelination begins prenatally at 30 wk gestation. In the full term infant, it is present by the time of birth in the dorsal brainstem, cerebellar peduncles, and posterior limb of the internal capsule. The cerebellar white matter acquires myelin by 1 mo of age and is well myelinated by 3 mo of age. The subcortical white matter of the parietal, posterior frontal, temporal, and calcarine cortex is partially myelinated by 3 mo of age. In this period, the infant experiences tremendous growth. Physiologic changes allow the establishment of effective feeding routines and a predictable sleep-wake cycle. The social interactions that occur as parents and infants accomplish these tasks lay the foundation for cognitive and emotional development.
Physical Development
A newborn’s weight may initially decrease 10% below birthweight in the 1st wk as a result of excretion of excess extravascular fluid and limited nutritional intake. Nutrition improves as colostrum is replaced by higher-fat breast milk, as infants learn to latch on and suck more efficiently, and as mothers become more comfortable with feeding techniques. Infants regain or exceed birthweight by 2 wk of age and should grow at approximately 30 g (1 oz)/day during the 1st mo (see Table 13-1). This is the period of fastest postnatal growth. Limb movements consist largely of uncontrolled writhing, with apparently purposeless opening and closing of the hands. Smiling occurs involuntarily. Eye gaze, head turning, and sucking are under better control and thus can be used to demonstrate infant perception and cognition. An infant’s preferential turning toward the mother’s voice is evidence of recognition memory.
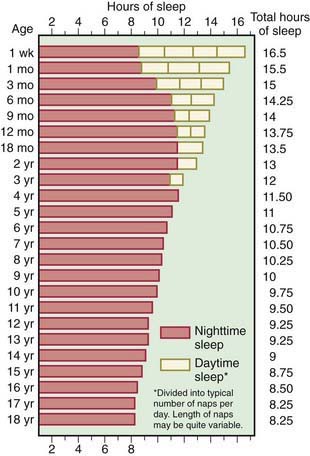
Six behavioral states have been described (Chapter 7). Initially, sleep and wakefulness are evenly distributed throughout the 24-hr day (Fig. 8-1). Neurologic maturation accounts for the consolidation of sleep into blocks of 5 or 6 hr at night, with brief awake, feeding periods. Learning also occurs; infants whose parents are consistently more interactive and stimulating during the day learn to concentrate their sleeping during the night.
Cognitive Development
Infants can differentiate among patterns, colors, and consonants. They can recognize facial expressions (smiles) as similar, even when they appear on different faces. They also can match abstract properties of stimuli, such as contour, intensity, or temporal pattern, across sensory modalities. Infants at 2 mo of age can discriminate rhythmic patterns in native vs non-native language. Infants appear to seek stimuli actively, as though satisfying an innate need to make sense of the world. These phenomena point to the integration of sensory inputs in the central nervous system. Caretaking activities provide visual, tactile, olfactory, and auditory stimuli; all of these support the development of cognition. Infants habituate to the familiar, attending less to repeated stimuli and increasing their attention to novel stimuli.
Emotional Development
The infant is dependent on the environment to meet his or her needs. The consistent availability of a trusted adult to meet the infant’s urgent needs creates the conditions for secure attachment. Basic trust vs mistrust, the first of Erikson’s psychosocial stages (Chapter 6), depends on attachment and reciprocal maternal bonding. Crying occurs in response to stimuli that may be obvious (a soiled diaper), but are often obscure. Infants who are consistently picked up and held in response to distress cry less at 1 yr and show less aggressive behavior at 2 yr. Cross-cultural studies show that in societies in which infants are carried close to the mother, babies cry less than in societies in which babies are only periodically carried. Crying normally peaks at about 6 wk of age, when healthy infants may cry up to 3 hr/day, then decreases to 1 hr or less by 3 mo.
The emotional significance of any experience depends on both the individual child’s temperament and the parent’s responses (see Table 6-1); differing feeding schedules produce differing reactions. Hunger generates increasing tension; as the urgency peaks, the infant cries, the parent offers the breast or bottle and the tension dissipates. Infants fed “on demand” consistently experience this link between their distress, the arrival of the parent, and relief from hunger. Most infants fed on a fixed schedule quickly adapt their hunger cycle to the schedule. Those who cannot because they are temperamentally prone to irregular biologic rhythms experience periods of unrelieved hunger as well as unwanted feedings when they already feel full. Similarly, infants who are fed at the parents’ convenience, with neither attention to the infant’s hunger cues nor a fixed schedule may not consistently experience feeding as the pleasurable reduction of tension. These infants often show increased irritability and physiologic instability (spitting, diarrhea, poor weight gain) as well as later behavioral problems.
Implications for Parents and Pediatricians
Success or failure in establishing feeding and sleep cycles determines parents’ feelings of efficacy. When things go well, the parents’ anxiety and ambivalence, as well as the exhaustion of the early weeks, decrease. Infant issues (colic) or familial conflict will prevent this from occurring. With physical recovery from delivery and endocrinologic normalization, the mild postpartum depression that affects many mothers passes. If the mother continues to feel sad, overwhelmed, and anxious, the possibility of moderate to severe postpartum depression, found in 10% of postpartum women, needs to be considered. Major depression that arises during pregnancy or in the postpartum period threatens the mother-child relationship and is a risk factor for later cognitive and behavioral problems. The pediatrician may be the first professional to encounter the depressed mother and should be instrumental in assisting her in seeking treatment (Chapter 7).
Age 2-6 Months
At about 2 mo, the emergence of voluntary (social) smiles and increasing eye contact mark a change in the parent-child relationship, heightening the parents’ sense of being loved reciprocally. During the next months, an infant’s range of motor and social control and cognitive engagement increases dramatically. Mutual regulation takes the form of complex social interchanges, resulting in strong mutual attachment and enjoyment. Parents are less fatigued.
Physical Development
Between 3 and 4 mo of age, the rate of growth slows to approximately 20 g/day (see Table 13-1; see Figs. 9-1 and 9-2 on the Nelson Textbook of Pediatrics website ![]() at www.expertconsult.com). By 4 mo, birthweight is doubled. Early reflexes that limited voluntary movement recede. Disappearance of the asymmetric tonic neck reflex means that infants can begin to examine objects in the midline and manipulate them with both hands (Chapter 584). Waning of the early grasp reflex allows infants both to hold objects and to let them go voluntarily. A novel object may elicit purposeful, although inefficient, reaching. The quality of spontaneous movements also changes, from larger writhing to smaller, circular movements that have been described as “fidgety.” Abnormal or absent fidgety movements may constitute a risk factor for later neurologic abnormalities.
at www.expertconsult.com). By 4 mo, birthweight is doubled. Early reflexes that limited voluntary movement recede. Disappearance of the asymmetric tonic neck reflex means that infants can begin to examine objects in the midline and manipulate them with both hands (Chapter 584). Waning of the early grasp reflex allows infants both to hold objects and to let them go voluntarily. A novel object may elicit purposeful, although inefficient, reaching. The quality of spontaneous movements also changes, from larger writhing to smaller, circular movements that have been described as “fidgety.” Abnormal or absent fidgety movements may constitute a risk factor for later neurologic abnormalities.
Increasing control of truncal flexion makes intentional rolling possible. Once infants can hold their heads steady while sitting, they can gaze across at things rather than merely looking up at them, and can begin taking food from a spoon. At the same time, maturation of the visual system allows greater depth perception.
In this period, infants achieve stable state regulation and regular sleep-wake cycles. Total sleep requirements are approximately 14-16 hr/24 hr, with about 9-10 hr concentrated at night and 2 naps/day. About 70% of infants sleep for a 6-8 hr stretch by age 6 mo (see Fig. 8-1). By 4-6 mo, the sleep electroencephalogram shows a mature pattern, with demarcation of rapid eye movement (REM) and 4 stages of non-REM sleep. The sleep cycle remains shorter than in adults (50-60 min vs approximately 90 min). As a result, infants arouse to light sleep or wake frequently during the night, setting the stage for behavioral sleep problems (Chapter 17).
Cognitive Development
The overall effect of these developments is a qualitative change. At 4 mo of age, infants are described as “hatching” socially, becoming interested in a wider world. During feeding, infants no longer focus exclusively on the mother, but become distracted. In the mother’s arms, the infant may literally turn around, preferring to face outward.
Infants at this age also explore their own bodies, staring intently at their hands, vocalizing, blowing bubbles, and touching their ears, cheeks, and genitals. These explorations represent an early stage in the understanding of cause and effect as infants learn that voluntary muscle movements generate predictable tactile and visual sensations. They also have a role in the emergence of a sense of self, separate from the mother. This is the first stage of personality development. Infants come to associate certain sensations through frequent repetition. The proprioceptive feeling of holding up the hand and wiggling the fingers always accompanies the sight of the fingers moving. Such self sensations are consistently linked and reproducible at will. In contrast, sensations that are associated with “other” occur with less regularity and in varying combinations. The sound, smell, and feel of the mother sometimes appear promptly in response to crying, but sometimes do not. The satisfaction that the mother or another loving adult provides continues the process of attachment.
Emotional Development and Communication
Babies interact with increasing sophistication and range. The primary emotions of anger, joy, interest, fear, disgust, and surprise appear in appropriate contexts as distinct facial expressions. When face-to-face, the infant and a trusted adult can match affective expressions (smiling or surprise) about 30% of the time. Initiating games (facial imitation, singing, hand games) increases social development. Such face-to-face behavior reveals the infant’s ability to share emotional states, the first step in the development of communication. Infants of depressed parents show a different pattern, spending less time in coordinated movement with their parents and making fewer efforts to re-engage. Rather than anger, they show sadness and a loss of energy when the parents continue to be unavailable.
Implications for Parents and Pediatricians
Motor and sensory maturation makes infants at 3-6 mo exciting and interactive. Some parents experience their 4 mo old child’s outward turning as a rejection, secretly fearing that their infants no longer love them. For most parents, this is a happy period. Most parents excitedly report that they can hold conversations with their infants, taking turns vocalizing and listening. Pediatricians share in the enjoyment, as the baby coos, makes eye contact, and moves rhythmically. If this visit does not feel joyful and relaxed, causes such as social stress, family dysfunction, parental mental illness, or problems in the infant-parent relationship should be considered. Parents can be reassured that responding to an infant’s emotional needs cannot spoil him or her. Giving vaccines and drawing blood while the child is seated on the parent’s lap or nursing at the breast increases pain tolerance.
Age 6-12 Months
With achievement of the sitting position, increased mobility, and new skills to explore the world around them, 6-12 mo old infants show advances in cognitive understanding and communication, and there are new tensions around the themes of attachment and separation. Infants develop will and intentions, characteristics that most parents welcome, but still find challenging to manage.
Physical Development
Growth slows more (see Table 13-1; see Figs. 9-1 and 9-2 on the Nelson Textbook of ![]() Pediatrics website at www.expertconsult.com). By the 1st birthday, birthweight has tripled, length has increased by 50%, and head circumference has increased by 10 cm. The ability to sit unsupported (6-7 mo) and to pivot while sitting (around 9-10 mo) provides increasing opportunities to manipulate several objects at a time and to experiment with novel combinations of objects. These explorations are aided by the emergence of a thumb-finger grasp (8-9 mo) and a neat pincer grasp by 12 mo. Many infants begin crawling and pulling to stand around 8 mo, followed by cruising. Some walk by 1 yr. Motor achievements correlate with increasing myelinization and cerebellar growth. These gross motor skills expand infants’ exploratory range and create new physical dangers as well as opportunities for learning. Tooth eruption occurs, usually starting with the mandibular central incisors. Tooth development reflects skeletal maturation and bone age, although there is wide individual variation (see Table 8-3 and Chapter 299).
Pediatrics website at www.expertconsult.com). By the 1st birthday, birthweight has tripled, length has increased by 50%, and head circumference has increased by 10 cm. The ability to sit unsupported (6-7 mo) and to pivot while sitting (around 9-10 mo) provides increasing opportunities to manipulate several objects at a time and to experiment with novel combinations of objects. These explorations are aided by the emergence of a thumb-finger grasp (8-9 mo) and a neat pincer grasp by 12 mo. Many infants begin crawling and pulling to stand around 8 mo, followed by cruising. Some walk by 1 yr. Motor achievements correlate with increasing myelinization and cerebellar growth. These gross motor skills expand infants’ exploratory range and create new physical dangers as well as opportunities for learning. Tooth eruption occurs, usually starting with the mandibular central incisors. Tooth development reflects skeletal maturation and bone age, although there is wide individual variation (see Table 8-3 and Chapter 299).
Cognitive Development
The 6 mo old infant has discovered his hands and will soon learn to manipulate objects. At first, everything goes into the mouth. In time, novel objects are picked up, inspected, passed from hand to hand, banged, dropped, and then mouthed. Each action represents a nonverbal idea about what things are for (in Piagetian terms, a schema; Chapter 6). The complexity of an infant’s play, how many different schemata are brought to bear, is a useful index of cognitive development at this age. The pleasure, persistence, and energy with which infants tackle these challenges suggest the existence of an intrinsic drive or mastery motivation. Mastery behavior occurs when infants feel secure; those with less secure attachments show limited experimentation and less competence.
A major milestone is the achievement at about 9 mo of object permanence (constancy), the understanding that objects continue to exist, even when not seen. At 4-7 mo of age, infants look down for a yarn ball that has been dropped but quickly give up if it is not seen. With object constancy, infants persist in searching. They will find objects hidden under a cloth or behind the examiner’s back. Peek-a-boo brings unlimited pleasure as the child magically brings back the other player. Events seem to occur as a result of the child’s own activities.
Emotional Development
The advent of object permanence corresponds with qualitative changes in social and communicative development. Infants look back and forth between an approaching stranger and a parent, and may cling or cry anxiously, demonstrating stranger anxiety. Separations often become more difficult. Infants who have been sleeping through the night for months begin to awaken regularly and cry, as though remembering that the parents are in the next room.
A new demand for autonomy also emerges. Poor weight gain at this age often reflects a struggle between an infant’s emerging independence and parent’s control of the feeding situation. Use of the 2-spoon method of feeding (1 for the child and 1 for the parent), finger foods, and a high chair with a tray table can avert potential problems. Tantrums make their first appearance as the drives for autonomy and mastery come in conflict with parental controls and the infants’ still-limited abilities.
Communication
Infants at 7 mo of age are adept at nonverbal communication, expressing a range of emotions and responding to vocal tone and facial expressions. Around 9 mo of age, infants become aware that emotions can be shared between people; they show parents toys as a way of sharing their happy feelings. Between 8 and 10 mo of age, babbling takes on a new complexity, with many syllables (“ba-da-ma”) and inflections that mimic the native language. Infants now lose the ability to distinguish between vocal sounds that are undifferentiated in their native language. Social interaction (attentive adults taking turns vocalizing with the infant) profoundly influences the acquisition and production of new sounds. The first true word (i.e., a sound used consistently to refer to a specific object or person) appears in concert with an infant’s discovery of object permanence. Picture books now provide an ideal context for verbal language acquisition. With a familiar book as a shared focus of attention, a parent and child engage in repeated cycles of pointing and labeling, with elaboration and feedback by the parent.
Implications for Parents and Pediatricians
With the developmental reorganization that occurs around 9 mo of age, previously resolved issues of feeding and sleeping re-emerge. Pediatricians can prepare parents at the 6 mo visit so that these problems can be understood as the result of developmental progress and not regression. Parents should be encouraged to plan ahead for necessary, and inevitable, separations (e.g., baby sitter, daycare). Routine preparations may make these separations easier. Introduction of a transitional object may allow the infant to self-comfort in the parents’ absence. The object cannot have any potential for asphyxiation or strangulation.
Infants’ wariness of strangers often makes the 9 mo examination difficult, particularly if the infant is temperamentally prone to react negatively to unfamiliar situations. Initially, the pediatrician should avoid direct eye contact with the child. Time spent talking with the parent and introducing the child to a small, washable toy will be rewarded with more cooperation. The examination can be continued on the parent’s lap when feasible.
Barlow SM. Central pattern generation involved in oral and respiratory control for feeding in the term infant. Curr Opin Otolaryngol Head Neck Surg. 2009;17(3):187-193.
Brazelton TB. Touchpoints: the essential reference. Reading, MA: Addison-Wesley; 1992.
Carlson EA, Sampson MC, Sroufe LA. Implications of attachment theory and research for developmental-behavioral pediatrics. J Dev Behav Pediatr. 2003:364-379.
Carberry AE, Colditz PB, Lingwood BE. Body composition from birth to 4.5 months in infants born to non-obese women. Pediatr Res. 2010;68(1):84-88.
Centers for Disease Control. Use of World Health Organization and CDC growth charts for children aged 0–59 months in the United States. MMWR. 2010;59(No. RR-9):1-15.
Dehaene-Lambertz G, Hertz-Pannier L, Dubois J. Nature and nurture in language acquisition: anatomical and functional brain-imaging studies in infants. Trends Neurosci. 2006;29(7):367-373.
Dorea JG. Breastfeeding is an essential complement to vaccination. Acta Paediatr. 2009;98:1244-1250.
Fernald LCH, Gertler PJ, Neufeld LM. 10-year effect of oportunidades, Mexico’s conditional cash transfer programme, on child growth, cognition, language and behavior: a longitudinal follow-up study. Lancet. 2009;374:1997-2005.
Hunziker UA, Barr RG. Increased carrying reduces infant crying: a randomized controlled trial. Pediatrics. 1986;77:641-648.
Jusczyk PW. Chunking language input to find patterns. In: Rakison DH, Oakes LM, editors. Early category and concept development: making sense of the blooming, buzzing confusion. New York: Oxford University Press, 2003.
Kelly Y, Sacker A, Schoon I, et al. Ethic differences in achievement of developmental milestones by 9 months of age: the millennium cohort study. Dev Med Child Neurol. 2006;48:825-830.
Kuhl PK. Human speech and birdsong: communication and the social brain. Proc Natl Acad Sci U S A. 2003;100:9645-9646.
Lozoff B, Beard J, Connor J, et al. Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr Rev. 2006;64(5 Pt 2):S34-S43.
McLearn KT, Minkovitz CS, Strobino DM, et al. The timing of maternal depressive symptoms and mothers’ parenting practices with young children: implications for pediatric practice. Pediatrics. 2006;118:e174-e182.
Mindell JA, Owens JA. A clinical guide to pediatric sleep: diagnosis and management of sleep problems. Philadelphia: Lippincott Williams & Wilkins; 2003.
Rollins JD, Collins JS, Holden KR. United States head circumferance growth reference charts: birth to 21 years. J Pediatr. 2010;156:907-913.
Stern D. The interpersonal world of the infant. New York: Basic Books; 1985.
Williams N, Mughal S, Blair M. ‘Is my child developing normally?’: a critical review of web-based resources for parents. Dev Med Child Neurol. 2008;50(12):893-897.
Wright CM, Williams AF, Elliman D, et al. Using the new UK-WHO growth charts. BMJ. 2010;340:c1140.