CHAPTER 28 Digital Technology in Endodontic Practice
Endodontic offices rely on words, numbers, and images to communicate with patients, assess patient status, evaluate treatment options, and determine treatment outcomes. Many dental offices already use computer-based programs to manage patient demographic and financial information; the electronic oral health record23 (EOHR) is the next logical step in the journey to the paperless office.
Although EOHRs are now widely available, integration of this information with an electronic health record (EHR) to create a unified, scalable, searchable, and secure patient database documenting the current health status and lifetime medical history of each patient is still elusive. In a broader sense, the real challenge is to understand dental informatics and the ways the collective efforts of the profession can be applied to improve patients’ health care. Two experts in dental informatics observed that79 “application of computer and information sciences to improve dental practice, research, education, and management” is the holy grail of dental informatics.34,80
The goals of this chapter are (1) to improve the dental care delivery organization’s understanding of dental informatics and (2) to devise a strategic plan to help design office systems that use the latest computer, digital-radiographic, photographic, charting, and management tools to document vital information. Once this strategic guide has been implemented, continual upgrading based on best-recommended practices is important to ensure continued success.
In the early 1990s, the American Dental Association (ADA) initiated the development of technical reports, guidelines, and standards on electronic technologies used in dental practices. A task group was established to promote the concept of a computerized dental clinical workstation and to allow the integration of different software and hardware components into one system to accommodate all a clinician’s information needs. Establishment of interoperability standards for these modules eliminates the need for multiple stand-alone systems in the dental office and provides a seamless information exchange throughout all facets of health care. The American National Standards Institute (ANSI) recognized the ADA as an accredited standards developer in 20004; the ADA is working to ensure that common conventions have worldwide acceptance.43
The U.S. government has already begun using the Government Computer-Based Patient Record (GCPR) in federal health care agencies. The advantages of the EOHR were highlighted in a recent study46 that compared an EHR with manual record keeping. The study’s findings were favorable to the EHR: improved understandability (89.2% versus 69.9%), better legibility (100% versus 64.3%), and the benefits of having at least one diagnosis recorded (48.2% versus 33.2%). Additional findings included improved prescription writing (86.6% versus 66.2%) and improved ability to recall advice given to patients (38.6% versus 26.8%).
Comprehensive Technology Plan
Information technology (IT) systems are changing every day and at an ever-increasing rate. Deciding what equipment to purchase for patient use in the reception area, as well as for clinical, front desk, administrative, and clinician needs, can be daunting. Upgrading older office systems, especially while an office is in operation, complicates this process.
Clinicians should begin by establishing clear goals for the systems they want to implement. Generally, such technology planning can be divided into three areas: (1) the strategic plan, (2) the operational plan, and (3) measurement of success.
Strategic Plan
The strategic plan should be based on a list of goals for the seamless integration of all computer functions in the office. Clinicians should focus on what is necessary to provide the best service to patients and establish clear priorities. The more sophisticated the system, the more customization that can be done to provide exactly what patients and clinicians value most.
Dental practice systems are meant to assist the human user. These systems are work multipliers—that is, the technology replaces human effort, making tasks the clinician and staff members do easier and more error free and in some cases making possible new tasks that otherwise would be too costly in terms of expense or time. The bottom line for these systems is the value provided in terms of labor savings and quality of services compared with the total cost of acquisition and use. If the value the system produces is greater than the cost of buying and using it, the clinician and the practice benefit.
At its most detailed, or granular, level, dental care is delivered differently across the United States. Although many commonalities exist, and best practices generally are agreed upon, the goal of achieving the best outcome for the patient often means tailoring the dental arts and sciences to what works best in the hands of a specific clinician. Clinicians build or modify their practice environments to fit the nature of their practice; the workflow is tailored to allow the clinician to operate at the highest level of excellence in the clinical process.
Clinical and practice management systems are most beneficial when technology helps to make activities in the clinical process more efficient, more economic, and less subject to error. As noted in 1996 in a concept model for the electronic dental record published by the ADA, the fundamental activities in the clinical process are2:
Table 28-1 presents the usual types of computer support available for these activities.
TABLE 28-1 Typical Computer Support for the Clinical Process
| Procedure |
Task |
Typical Automation Support |
| Examination |
Data acquisition |
Automated charting, note taking, digital radiography |
| Diagnosis |
Data analysis |
Clinical decision support, automated real-time consultation |
| Treatment |
Service planning |
Decision support: case planning, automated presentation, documentation of informed selection and consent |
| Care delivery |
Service delivery |
Documentation of services provided; digital radiography of completed services |
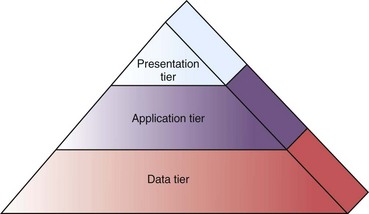
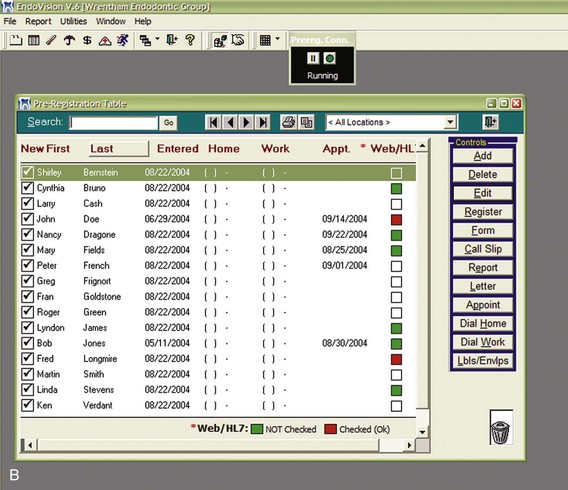
The systems that provide this type of support typically are composed of several layers, or tiers, that correspond to the basic functions provided by computer technology (Fig. 28-1). Each tier provides the dental practice system with a capability, and for best use, each tier must be configured to support the nature of the practice and its workflow. The tiers usually are categorized as follows:
•
Data tier: The form and physical storage of data; in clinical practice, this often is the EHR and a variety of clinical and administrative reference data.
•
Application tier: The internals of the system, which provide logic, calculation, and help with decision-making functions.
•
Presentation tier: The part of the overall computer system that interacts with people and the outside environment, including other computer systems.
At the data tier, the heart of the clinical system is the EHR. ANSI/ADA Specification No. 1000 provides a data blueprint for digital representation of clinical and support data for an individual human patient.4 This standard is the only model-based, data-level specification of clinical data for building an EHR database. In such an EHR data system, not only the individual patient but also family members and significant others are identified. Often this capability is expanded to identify individuals who may provide health care services to the patient. Administrative data such as personal characteristics, employment, and similar information frequently are included in the EHR. The digital structures used to build the dental chart (but not the graphic chart per se) are maintained in the data tier. Also in the data tier, but outside the scope of the EHR, are the reference tables and rules sets for clinical decision support, lists of pharmaceutical items in a formulary database, and code sets for anatomic location, diagnosis, procedures, and so forth. The data tier is the foundation of the practice system.
The application tier is the functional heart of the practice system. All processing of data occurs in this tier, such as clinical decision support whereby the computer acts on rules to alert the clinician to a potential problem with a particular therapeutic agent in the case at hand. The application tier can operate on the data specific to a case, the reference codes, and notations and construct the graphic dental chart for a particular patient. It also operates on any signals from automated diagnostic devices, such as digital periodontal probes, cardiac monitoring devices or root canal depth gauges, converting these into human-understandable measurements that can be displayed to the clinician by the presentation tier.
The presentation tier provides the face of the dental practice system. The application and data tiers usually are neither seen nor heard by the clinician and staff; the presentation tier is by far the most interesting aspect of the computer system because it is the point where the clinician and staff interact with the system. The presentation tier is where the dental chart takes form, where the clinician can watch as its graphic features are recorded, and where the clinician can key in any special notes required. It also is where the clinician receives any patient care advisories, enabling patient safety features such as alerts to prevent adverse events. The presentation tier is where the electronic prescription is sent to a pharmacy. Finally, the presentation tier is the realm of digital radiography, regarded by many as one of the most beneficial aspects of automation in dentistry.19
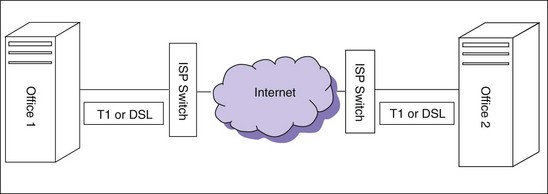
The core of the office IT infrastructure is the central information store (CIS) (Fig. 28-2). The CIS is the “center of the universe” of the IT system, comprising the server and its attendant software and hardware; it also may include data generated in the office or imported from the Internet. The CIS should be located in a secure area and have an always-on connection to the Internet to increase functionality. The establishment of a local area network (LAN) now is considered essential for dealing with the heterogeneous information generated in each physical location and for integrating a wide area network (WAN) to connect several practice locations.
A comprehensive strategic technology plan should address all the information generated and processed in the practice and the ways it will be handled. The clinician must be prepared to manage information from patients and referring clinicians and to document and communicate all pretreatment, treatment, and posttreatment information via LAN, WAN, mail, fax, e-mail, and the web. An ideal system that handles this mix of data and gives all members of the office team what they want integrates the CIS with the reception, clinical, front desk, administrative, and clinician’s office components.
Operational Plan
The newest concept in dental office management is frontdesklessness. The central tenet of this concept is to minimize office interactions that traditionally take place at the front desk and shift them to the operatories (e.g., procedure code and fee posting, prescription writing, and all associated communications). Some programs now available to endodontists allow pending or posting of all relevant data from any computer in the office, including the generation of postoperative forms, instruction sheets, patient treatment reports, and e-mail correspondence. Advantages of this system include improved workflow and accuracy, because significant office revenues can be lost through posting inaccuracies that are never discovered.58
The operational strategy covers the planning and day-to-day practices that ensure a smoothly running IT system. Training and cross-training of staff are essential elements of a complete plan. To begin, at least one staff member must be knowledgeable about basic computer operations, especially word processing. End-user training courses are available online (e.g., globalknowledge.com) and nationwide to teach these basic skills. Books and video self-study materials can augment classroom training. The purchase of most clinical and front desk software systems should include ample opportunity for initial training.
Once initial training has been accomplished, a second training session, preferably on site, is advisable. This second visit, which should be scheduled several months after the initial installation, allows the clinician and the office staff to fine-tune the program by customizing certain preferences and double-checking that all the program’s features are used to full advantage. In addition, to get the most out of the software, staff members should periodically review the program’s training manual to discover features and shortcuts that may have been overlooked.
All computer workstation environments should be designed with ergonomic considerations in mind, such as work surface, keying, seating (Fig. 28-3), acoustics, lighting, and ventilation (Box 28-1).42 Special care should be taken to design each area of the office so that employees, patients, and clinicians are comfortable, and all personal health information (PHI) is protected.
BOX 28-1 HEALTH AND SAFETY FACTORS FOR EMPLOYEES
In the past, worker safety primarily involved preventing accidental injury or death from hazards in the factory or other industrial environment. Because the office now is the most common work setting, attention is turning toward subtler but still serious health problems associated with office work, especially cumulative trauma disorders (CTDs) and vision disorders. The incidence of these disorders is growing.
CTDs of the muscles, tendons, or nerves can be caused by repetitive movements of the body. As the frequency and duration of a repetitive task increase, so does the likelihood that a CTD will develop. Although most CTDs can occur in any part of the body, the term usually refers to disorders of the hands, wrists, arms, or shoulders. Carpal tunnel syndrome is one example of a CTD. Typical symptoms of CTDs include pain, swelling, tingling, numbness, or heat around the affected area during both work and rest. These disorders differ from simple fatigue, which disappears after rest. With a CTD, a person may still experience symptoms after days or even weeks of inactivity.
Ergonomists often note that computers themselves are not really to blame; repetitive, unvarying work is the cause of most CTDs. Individual physiology plays a big part in whether a person develops a CTD. However, experts recognize the importance of workstation design and layout in the prevention of CTDs. For example, a work surface’s height and forearm support and work process issues (e.g., a company’s break policy) affect the incidence of CTDs. For a worker involved in repetitive motion, frequent breaks, even short ones of 30 seconds every 10 minutes, help reduce the probability of a CTD developing. Task variety is also important. Therefore clinicians should design their office duties to allow clerical workers to alternate among different types of work (some of it computer based and some of it not) or to alternate computing tasks that require different motions and muscle groups.
Front Desk, Administrative, and Clinician Computer Workstations: General Specifications
Work Surface
A desktop height of 28.3 inches (71.9 cm), with a keyboard tray below the work surface that places the hands and wrists in a wrist-neutral position, is a good compromise height for front desk and administrative workstations. A bullnose (i.e., curved) edge can be placed on countertops to eliminate sharp corners. CRT monitors should be positioned far enough from the user to reduce extremely low frequency (ELF) radiation exposure.
Keying
Positioning the elbows at 90 degrees and keeping the arms and hands parallel to the floor can help prevent CTDs. With use of Microsoft’s “Natural Keyboard” wrist rests,93 locating mouse and writing platforms in the primary reach zone may also contribute to a more comfortable work environment. Work surface space must allow for efficient organization of documents, papers, and other materials. Peripheral equipment should be easy to reach.
Seating
Seat height should be adjustable to allow for positioning in the range of 16 to  inches (41 to 52 cm) above the floor. The seat should have a “waterfall” or gradually curved contour just behind the user’s knee and the underside of the thigh to prevent excessive pressure in this area. A seat back rest and lumbar support should also be provided.
inches (41 to 52 cm) above the floor. The seat should have a “waterfall” or gradually curved contour just behind the user’s knee and the underside of the thigh to prevent excessive pressure in this area. A seat back rest and lumbar support should also be provided.
Acoustics and Lighting
Ambient or background noise (i.e., white noise) is desirable at a level that does not interfere with task performance (40 to 55 dB). Experts agree that open-plan acoustics are subject to three main problems: sound level, speech intelligibility, and sound paths.44
Lighting sources should be designed and located to minimize glare and provide luminance in the range of 200 to 500 lux in the work area. Task or local lighting may be needed for reading documents. A combination of indirect overhead, natural, and task lighting is preferable. For close-up work, light should be directed sideways onto documents to avoid glare on the monitor; this helps prevent eye fatigue and headaches. Eyestrain is the leading complaint among computer users, according to the American Optometric Association.7 Computer users should take frequent breaks and have their vision checked, and the work space should be designed so as to reduce visual stress.
Modern LCD monitors are designed to operate at their “native” resolution and a 60 to 70 Hz refresh rate to reduce monitor-induced eye strain. Further improvement can be realized by turning on “ClearType,” imbedded in Microsoft Windows XP, Vista, and Windows 7 operating systems. ClearType provides improved font display quality over traditional forms of font smoothing or anti-aliasing. Glare can be reduced by replacing fluorescent lighting diffusers with grids that break up the light pattern. Office color schemes should be neutral and pleasing to the eye.
Ventilation
Proper ventilation requires about two air exchanges per hour. The temperature and humidity level should be kept constant, with temperature range adjustable from 68° F to 75° F (20° C to 24° C).
Management of database security is another important aspect of a good operational plan. The security standards mandated by the Health Insurance Portability and Accountability Act (HIPAA) now apply to all covered entities (see also Chapters 11 and 27). Practices are required to (1) perform a risk analysis to safeguard all electronic protected health information (E-PHI); (2) use technical, administrative, and physical safeguards to protect E-PHI; and (3) institute ongoing risk management. Security standards require that each employee have an individual password to access the electronic medical records system. Even in offices that are not covered entities, prudence dictates that clinicians use software that provides multiple levels of protection to reduce the chance of malicious tampering with data. For example, control over deletion of files should be protected to allow only senior staff members and/or the clinician to make changes. Compliance with the security standards requires a framework for ongoing compliance, including the designation of a security official and continual analysis of security needs as office systems change.
The purchase and continuation of hardware and software maintenance contracts are another area where diligence is important. The clinician should create a system for monitoring the status of the maintenance plans for key elements of the IT system, especially digital radiography and front desk software. Establishing insurance coverage for computer hardware, software, and data also requires special attention. General office insurance policies often limit computer coverage; therefore clinicians should discuss policies with a knowledgeable insurance agent. In addition, staff members should keep a file of purchase invoices, including digital photographs of all equipment, to document purchases for insurance purposes.
Marketing the practice is another way in which an IT system can prove invaluable. Referral and educational materials should be upgraded continually. The production of newsletters, e-newsletters, informational mailings, patient education handouts, and management of sponsored study clubs and meetings can be handled with the help of an up-to-date word processing and practice management system (see Fig. 28-1). Marketing is most effective if it is customized, frequent, and consistent.
Measuring Success
Once various technologic systems have been implemented, clinicians should learn how to measure their progress toward achieving strategic goals. For example, if premedication instructions are included in a “welcome kit” sent to new patients or on an Internet “welcome” page, staff members should see a quantifiable improvement in compliance with these instructions. Enhanced communication with patients and referrers should lead to improved satisfaction and increased engagement. Other ways to measure success with regard to operational strategies include surveying patients and referring doctors on the effectiveness of communication materials. A proactive approach to these procedural issues is the hallmark of a well-managed office.
Trend analysis is another key method of evaluating the success of office programs. The ability to better track referral patterns and follow up on collections, treatment efficiency, outcomes, and uncompleted treatments is one of the benefits of a well-designed software program. For example, generating reports that analyze fading referrals can be an important measure of referral satisfaction. Once these data are evaluated, an action plan and global strategy can be devised to address issues that need attention.
Tracking Bits and Bytes through the “Patient Loop”
The patient loop begins when a patient is informed that he or she needs an endodontic procedure and ends with the postoperative check-up visit (Box 28-2). This process begins the patient’s journey through different operational steps that result in the successful management of endodontic treatment and completion of the EOHR.
BOX 28-2 THE VIRTUAL OFFICE: READY NOW
The new paradigm for exceptional patient care calls for sophisticated communication and customization that can be accomplished most efficiently in the integrated digital office. The following steps outline the process, or patient loop, from introduction of endodontic treatment to the last follow-up visit.
1.
The process begins when patients need an endodontic or implant procedure. The endodontic office should make the following options available:
•
A website for patient education, contact information, referral materials, and patient registration forms
•
A
referral kit for referring doctors that contains a brochure, a map to the office, customized referral forms, past newsletters, introductory information on the office website, and business reply envelopes
•
Informational meetings with referring clinicians to enhance communication and discuss expectations
2.
When patients call for an appointment, the office should be ready to do the following:
•
Preregister patients using the practice management software
•
Refer patients to the office website, where they can read a welcome letter and complete the patient registration forms using a HIPAA compliant security protocol
•
Mail, fax, or e-mail a
welcome kit with a welcome letter, brochure, explanation of the procedure, map, biography of the treating endodontist, and statement of the fee policy
3.
When patients arrive for their first visit, they can also fill out the personal information sheets on a reception area computer kiosk connected to the network, or they can watch educational material while waiting. Any film-based radiographs can be scanned into the patient database. The patient’s status can be indicated in the endodontic time and patient tracking module so that every member of the dental team knows the status of all patients from their presentation visit until they are discharged.
4.
When patients are seated in the operatory, an assistant can perform indicated radiographic studies and capture a visible light (VL) image of any teeth or area in question, using an intraoral camera. The assistant then can enter the chief complaint, history of the current illness, list of medications, and medical history into the digital chart and check for drug interactions on the chairside computer workstation. The clinician performs pulp tests and records the endodontic findings in the charting module, followed by an oral and written consent and vital signs check. Treatment then can be started, and each step of the procedure can be recorded by mouse and keyboard input or voice command. If desired, subsequent appointments can be made for patients while they are still in the operatory, treatment reports can be generated, and their insurance information can be sent to the office financial coordinator or directly to the insurance company.
5.
Patients are discharged at the front desk departure station, with all pertinent information already entered into the computer. This is an opportunity for patients to receive customized information about their treatment, next appointment, follow-up care, and any medications prescribed or dispensed.
6.
Patient treatment reports and other correspondence can be created by the front desk or assisting staff; reviewed by the clinician at a computer terminal; forwarded to the print queue; and sent by mail, fax, or e-mail.
7.
When patients return for follow-up visits, digital radiographs can be exposed, and comparisons of immediate postoperative and check-up radiographs can be made side by side on the same screen to assess healing. Reports can then be generated.
Central Information Store
Creation and management of the EOHR and all its components is the job of the CIS. A CIS requires a single, robust central computer, called a server, that links all the computers in the practice. When computer systems are connected in this way, they most often are referred to as a client/server network. The server is designed to administer the network efficiently, taking care of management functions such as backup, file sharing, print processing, and web and e-mail tasks.
A server-based system has four primary benefits:
1.
It saves time and effort because all information can be stored for instant access by any team member. As files are updated, all the new information is available instantly.
2.
Security is better because all data are centrally stored and (normally) automatically backed up.
3.
Each user can be better monitored, because each workstation can be uniquely identified at every transaction.
4.
Remote access to the entire database is possible, so records can be reviewed from outside the office and more easily maintained.
The Microsoft Windows Server System allows the creation of a single point of contact with the Internet, which improves security as well as security settings that allow for appropriate remote access levels for employees or vendors.
Software
Servers have evolved into microprocessor-based machines dedicated to running certain software applications. Two basic types of software can be purchased to run on a server:
•
Network operating system (NOS). Most LANs and WANs in endodontic practices use a Microsoft NOS, which is based on the Microsoft Windows Server System. These sophisticated, stable systems are ubiquitous, and many servers come configured with base installations of the software.
•
Database engine. One of the most robust and commonly used database management technologies is the structured query language (SQL), an ANSI standard computer language that uses SQL statements for obtaining and manipulating data. SQL is a technology, not a product, and many vendors offer versions of SQL (e.g., SQL Anywhere, SQL Base, and DB2).
Hardware
Two basic hardware recommendations can be made to ensure a reliable network that can handle both digital imaging and practice management databases:
•
Redundant arrays of inexpensive disks (RAID Level 5). To reduce the chance of hardware failure and subsequent data loss, RAID 5 uses an array of multiple hard disk drives that behave like a single storage disk but have increased capacity and improved fault tolerance and performance.
•
Serial computer systems interface (SAS). More advanced than the IDE/ATA interface, SAS
82 is really a system-level bus with intelligent controllers that allow hard drives and other peripherals to operate with unmatched performance, expandability, and compatibility. Newer serial ATA (SATA) drives and IDE RAID are not considered as reliable as SAS and should not be used for critical hardware.
49Data Security
All data in the office are subject to security threats. Network attacks can interrupt office operations and cause loss of patient data, leading to legal liability. Whether a disgruntled employee decides to delete information, a disk with an infected Word file is brought from home and uploaded on an office computer, or an Internet connection allows unauthorized access, client and server tiers of the network are vulnerable to attack. Scalable security approaches are emerging to address these new challenges in three basic data security categories: integrated security, data backup, and archiving.
Integrated Security
Symantec (Mountain View, CA) and McAfee (Santa Clare, CA) are two leading vendors of enterprise-wide security suites that address malicious code attacks, denial of service attacks, unauthorized network entry, and blended threats.90 Single-source enterprise protection can automatically update the office server and each client every day via the Internet. This includes:
1.
Protection against viruses, worms, and Trojans
2.
Software firewall protection to prevent unauthorized access to the network
3.
Content filtering to eliminate unwanted materials
4.
Connection security for any virtual private networks (VPNs). VPNs are constructed by using public wires (i.e., the Internet) to connect nodes and provide encryption and other security mechanisms.
Data Backup
Data backup is the process of transferring data from the office server to a separate storage medium such as a tape drive or another hard drive. Because data are only as good as the last backup, it is imperative that a consistent backup and recovery protocol be followed. Data loss can be attributed to hard drive failure, data corruption, or physical damage to the server because of fire, flood, or theft. Although many backup strategies exist, even solo clinicians using periapical, panoramic and CBCT digital radiography modalities, and visible light imaging can generate 500 gigabytes of data per year. This means that backing up with CDs and DVDs is not a practical solution. Removable hard drive storage is also not recommended as a primary backup method because it does not allow regression to a previous configuration if an application failure is not evident for several days. Instead, a recommended scheme is a nightly tape backup with a 20-business-day rotation (1 business month) using a different tape for each of 20 days, replacing all tapes at manufacturer’s suggested intervals or at least yearly.12
All backups should be full backups, rather than incremental or differential backups, to improve efficiency if reinstallation is required. Use of backup-to-disk functions and universal service bus (USB) hard drives can also be useful if multiple point-in-time backups are necessary. A full backup before any software upgrade must always be performed. Backup media should be tested periodically and backup logs examined to make sure the system can be properly restored. Other backup schemes that automatically upload encrypted data to a dedicated Web vendor nightly, ideally SAS 70 Type II certified, and store the data at a minimum of two geo-separate remote sites are available and can also provide a high level of security.
Archiving
An archive is a permanent data backup that usually is stored off site. All computer data are subject to loss, and merely making a daily backup of the data does not provide sufficient protection if the data are corrupted because of a previously unknown virus, worm, or Trojan. Removing one tape from the normal backup tape rotation on a monthly basis and placing it in fireproof off-site storage usually ensures that a valid data set is available if a catastrophic event causes data corruption or loss. Another advantage is that this tape can be archived at a local medical records storage facility and logged in and out to ensure that the tape is not altered if required during litigation.
Equipment Protection
The server should be located in a secure area of the office, preferably a computer “closet” with locked access (HIPAA-covered entities are required to provide physical security of E-PHI). Designing lockable front and rear access to the server system or rack, if applicable, enhances access to the CIS when maintenance of upgrades are performed. Although rack-mount systems offer better space efficiency, there is a cost premium for this kind of equipment. All server installations must have adequate cooling, another factor that must be considered when planning the practice’s air conditioning and heating systems.
Privacy
Security considerations are recommended for ensuring that data are reliable and safe and for meeting the requirements of Title II of HIPAA. The server and all software, including the wired and wireless LAN and WAN if any, should be protected by a system of individual passwords that allow different levels of security. Server log-in, remote access to the server via the Internet, program security, and especially the practice management system and digital imaging software must be password protected from unauthorized deletions and changes. The server password should be difficult to decipher (e.g., #eio9$kej**) to reduce the chance that the password will be decoded if the server is stolen from the office.
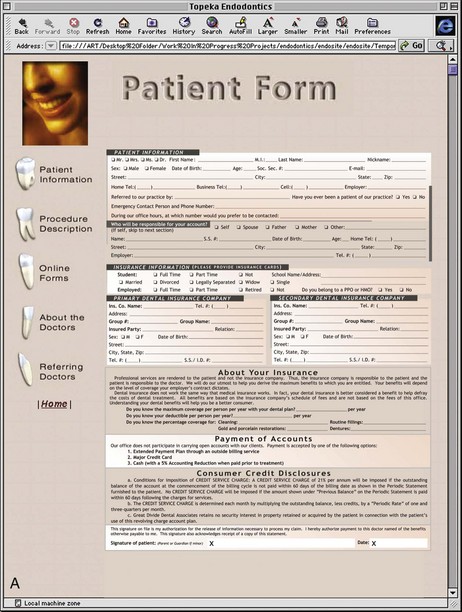
Reception Area
Placement of a computer kiosk in the reception area with Internet-only access can be a convenience for patients who want to complete their registration materials online (Fig. 28-4). A computer installation in the reception area is often overlooked, but this is an ideal place to market the practice, educate patients, and introduce the “high-tech” office. The clinician should plan the location of the kiosk to follow HIPAA guidelines for ensuring patient privacy.
Operationally, this computer can run an Internet kiosk program that prevents users from manipulating the operating system or tampering with the office LAN. The system can serve the following three purposes:
1.
The computer can provide new patients with a link to the practice’s website, allowing patient registration forms to be completed and sent via the Internet to the office for upload into the office’s practice management software, if applicable. This software should use secure file transfer protocol (SFTP) technology to ensure that E-PHI is sent with high-level encryption to maintain privacy.
2.
The computer can also be used by patients as a convenience to allow free Internet access if an appointment is delayed.
3.
The computer kiosk or a stand-alone computer system can be used to run a PowerPoint or Web-enabled patient education module to help familiarize the patient with services offered by the office and to provide information about the practice and office team members.
Front Desk
In a small office, the computer setup at the front desk is used primarily to process patient accounting and insurance, manage scheduling, and in some cases generate patient treatment reports. Another strategy, especially in multiple clinician practices, is to have separate computer workstations for patient intake and checkout. The addition of Internet functionality is another area where the intake computer can prove valuable.
Production of a customized “welcome letter” sent directly to the patient by mail, e-mail, or fax can help introduce patients to the practice, better inform patients about the office, and set expectations about treatment and billing practices. More offices are now creating websites that offer patient education modules and enhanced functionality; this allows tight integration of the Web materials and office software, as follows:
1.
Patients can complete Web forms that transmit demographic data and E-PHI via a HIPAA-compliant protocol directly to the intake computer.
2.
TruForm (PBHS, Santa Rosa, CA, and Henry Schein, Inc., Melville, NY) allows a patient to access the office website, complete the registration forms, and transmit them to the office by means of a remote host computer. The data can then populate the preregistration fields in the practice management software automatically.
3.
More flexibility can be added with new software program modules that permit greater frontdesklessness. WebConnect, an integrated product by PBHS, allows patients to log on to the practice website, view and change future appointments, review financial information, pay bills online, and communicate automatically by e-mail.
Larger offices, especially in multiple-clinician practices with two or more front desk personnel, may benefit from configuring the front desk with a separate departure area and computer. This computer can be linked to a shared multidrawer laser printer so that both front desk computer stations print to a central printer, with each unit able to print specific documents or envelopes on demand.
Software
Practice management software for an endodontist has some of the same features as software for the generalist. Specialty markets, especially endodontics, have several key requirements. Considerations for hardware and networking, as well as product features (e.g., scheduling, referral tracking, preregistration, advanced reporting, and analysis), have poor analogs in general practice management software and require the selection of a product written specifically for the endodontic specialist.
Another important factor in the selection of software has to do with the recent consolidation trends in the dental software industry.57 Careful investigation of software companies should include a look at the parent companies in an attempt to determine which ones will survive. When purchasing software, the clinician also should give careful consideration to the basic language and robustness of the program’s database engine.
Great software, like a great building, is constructed on a solid foundation. Although there are many techniques for building software, some are superior.
The 2000s saw the delivery of incredible power to the desktop. A client/server model now exists that eclipses all others. Put simply, it features a powerful database engine run on a central computer (i.e., a dedicated server) that controls access to data requested by client workstations. The standard in databases for this model is SQL,102 which delivers data faster than any other database system and does so with far greater efficiency, safety, and simplicity. Unlike other systems that move data back and forth between the network server and client workstations, client/server systems produce less network traffic and greater performance. This is because in an SQL system, virtually all data manipulation is done at the server. This also reduces the chance of the data becoming corrupt, because data never leave the server, and the SQL engine actively controls access to the data.
In previous models, each client workstation read data from the server, manipulated it, and then wrote it back. Because no client was aware of the activity of any other client, and the network operated more or less like multiple independent systems, two or more workstations writing data to the server at the same moment was commonplace. In addition, older models looked at data one row at a time, whereas SQL engines grab chunks of data in response to queries issued by the client and send these result sets in their entirety to the client. The resulting performance increases in terms of speed are significant, especially with remote offices. Therefore a true 32-bit client/server product with an SQL database is recommended as a minimum requirement.
Hardware
A well-designed front desk workstation includes a computer equipped with a dual monitor card and two large-screen liquid crystal display (LCD) monitors, label printer, and high-speed Internet connection.
Operatory
The core function of an endodontic office is to provide the best clinical care for patients, yet only about 25% of dental offices today use a chairside computer workstation.81 The chairside clinical workstation (Fig. 28-5) is the natural place to begin the most important gathering of data.
Software
The EOHR begins with thorough documentation of care at an individual site (e.g., a practice or hospital) and eventually becomes part of an individual patient’s cradle-to-grave EHR. Electronic charting does everything paper systems do and much more. Numerous systems are available specifically for endodontists.
Electronic charting serves three purposes: (1) accurately and legibly recording diagnostic and treatment data for individual patients,46 (2) automating many aspects of record taking, and (3) indicating trends by allowing analysis of patient records based on user-defined queries.
An electronic charting system can include the following:
1.
Integration with the general practice management software
2.
Extensive trend analysis and reporting
3.
Voice integration (i.e., the ability of the computer to understand natural speech and record findings)
4.
Comprehensive, easy-to-use interface with pick-lists and drop-down boxes that automate entries, many of which are customizable. (Note that any fields that allow customization may not be easily data-mined for groups of users at a later time.)
5.
Macroautomation (i.e., the ability of the program to automate common functions by playing back a series of recorded actions)
6.
Scanner integration, which allows the user to scan in supporting documents, radiographs, and other paper records
An EOHR for endodontic visits should have the following information, arranged in a logical sequence:
1.
General demographic and medical information (integrated with online pharmacologic and medical databases to allow quick lookup of medications and diseases on the Internet in real time)
2.
Chief complaint and history of present illness
a.
Chief complaint (which contains a notes field for recording, in the patient’s words, what prompted the trip to the office)
b.
History of present illness (notes field for recording the history of the current illness in the patient’s words)
3.
Clinical examination (describes findings by tooth numbers)
4.
Radiographic examination (includes radiographic analysis, which is essential to measurement of treatment outcomes)
5.
Etiology (list of causative factors)
6.
Diagnosis and treatment plan
7.
Treatment notes, which are based on user-defined criteria and include the following information:
a.
Patient’s vital signs, (blood pressure, pulse, respiration and temperature)
d.
Type of injection, gauge and length of needle, type and amount of anesthetic
f.
Number and names of canals
g.
Trial length, actual length, reference point, measurement methodology, and final instrument size
h.
Instrumentation technique, irrigants
i.
Obturation material and technique, including sealer
j.
Detailed record of restorative treatment
k.
Prescribed medications (may include over-the-counter drugs)
l.
Temporization method, post-and-core procedures and materials
m.
Recommended posttreatment instructions
8.
Postoperative report generator
a.
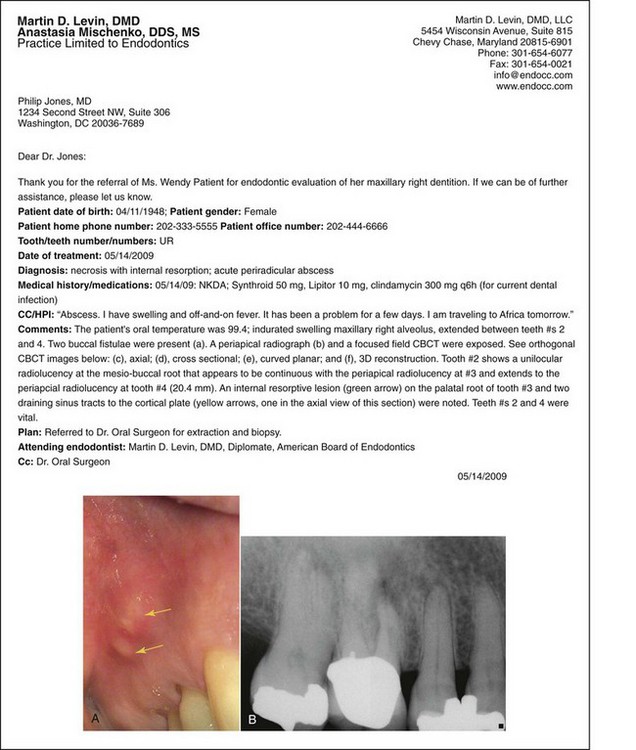
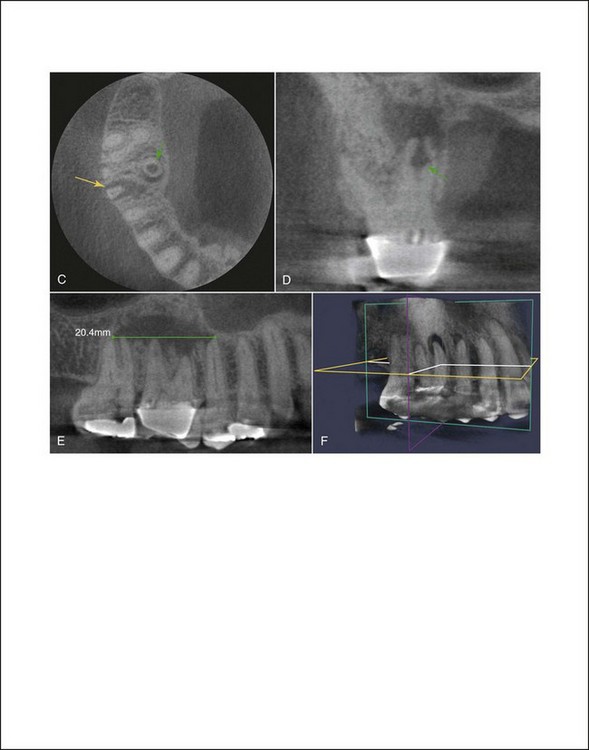
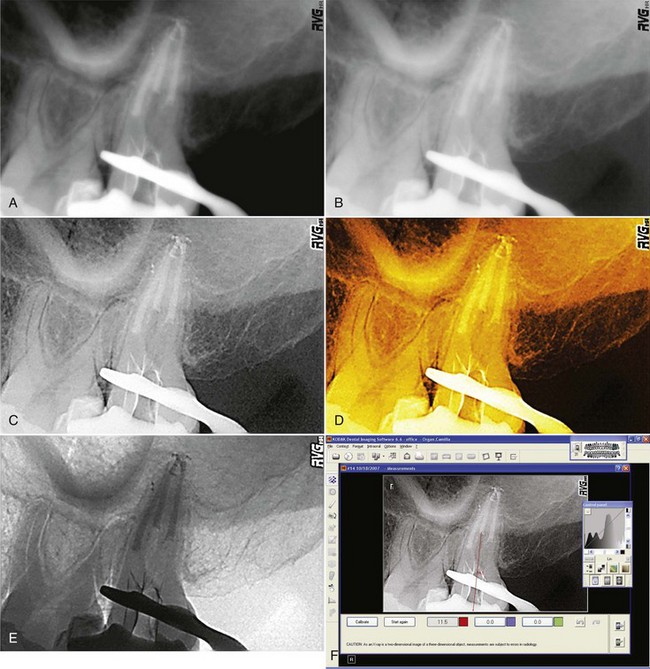
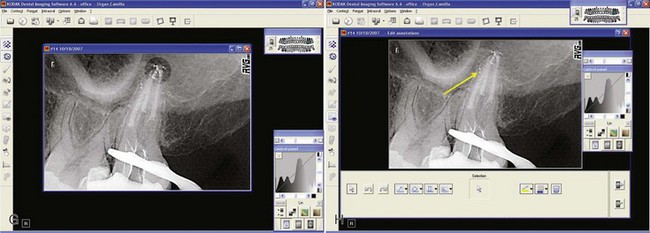
Patient treatment reports can be created automatically and sent to referring clinicians by hard copy or e-mail (using a HIPAA-compliant protocol) (
Fig. 28-6)
b.
Documentation of oral and written instructions and a reevaluation plan
In keeping with the concept of frontdesklessness introduced earlier, to reduce congestion at the front desk, a customized screen can allow the dental team to post the treatment information in the operatory to generate billing, prescription, customized instruction sheets, and patient treatment reports with a few mouse clicks or the touch of an input pen. The information then can be posted at the front desk or in the operatory, and instructions, prescriptions, and reports can be directed to the appropriate printer for hard copy production or e-mail distribution to any referrers or co-therapists.
Reference software is another area where the Internet-connected concept can prove invaluable. With each chairside computer workstation connected to the Internet, the clinician can subscribe to an online pharmacologic reference that gives specific information about pharmaceuticals as they pertain to dental treatment. One example of such a service is Lexi-Comp Online (Lexi-Comp, Hudson, OH), a site that offers information on medications that are indexed alphabetically and by disease, with specific reference to dental considerations and dental vasoconstrictor precautions.
Hardware
The computer chairside workstation is the “center of the universe” for the endodontic clinician. The central processing unit (CPU) should be placed in a location that allows easy access to connections so that upgrades can be made without major disruption. This computer should be equipped with a dual monitor card to allow two or more monitors to operate simultaneously, as follows: (1) a monitor to display the current schedule, visible only to the clinician and staff; (2) a second output that is then further split by an amplified video splitter to two monitors in “clone” configuration, allowing the clinician and staff to have identical screen views and input tools (Fig. 28-7). This HIPAA-compliant arrangement conceals the schedule and other patients’ E-PHI from the view of patients in the dental chair.
In endodontics, clinical input systems represent a very broad category that can be divided into two groups: input devices and charting software. Input devices can be subclassified further into radiographic and photographic or VL imaging equipment.
Imaging
Microscopic Imaging
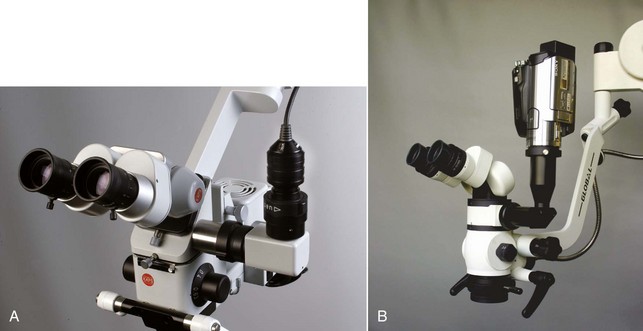
Microscopic imaging has evolved over the past several years to include many choices for high-resolution image capture.
♦
Medical-grade, single-frame digital cameras are available from several manufacturers that can produce superior images and allow capture directly to the chairside clinical workstation via the USB
95 or the FireWire (IEEE 1394) port or a memory card. Many cameras let the clinician preview an image on the camera’s integral display so that images can be quickly retaken if not satisfactory. The cameras attach to the microscope by means of a beam splitter and camera adapter. Professional-grade digital photography has replaced the 35-mm film format for medical and scientific use. It allows an instant picture with image resolution that approximates that of film-based photography.
♦
Solid-state analog video cameras also can be purchased for microscopic videography (
Fig. 28-8). These cameras produce an analog output (either a
composite signal or an
S-Video signal). Composite signals with images of 280 lines of resolution usually are less expensive than S-Video models, but the images have inadequate resolution (
Box 28-3). Cameras capable of S-Video output can produce images in the range of 480 lines and are preferred for microscopic imaging. They can be connected either to video capture cards for incorporation into imaging databases or to a video splitter to provide several S-Video outputs. One output can be connected to the chairside computer workstation, a second to an LCD flat screen monitor with S-Video inputs, and a third to a videocassette recorder. This arrangement allows legacy systems to operate in a multiscreen mode, but it has been supplanted for the most part by a mostly digital imaging chain. Even more sophisticated cameras with three charged-coupled devices (CCDs) and
component outputs are available for the highest-level resolution, but they are not necessary for routine clinical documentation.
♦
A hybrid system that uses the newest consumer-grade video/still cameras with solid state memory allows nonlinear editing, a 16 × 9 recording ratio for widescreen playback, and instant viewing or copying. Many of these cameras can be connected directly to the computer by means of a USB or FireWire and can take credible still images in addition to 30 fps (frames per second) video.
BOX 28-3 Short Primer on Video Signals
Visible light (VL) imaging is one of the most powerful documentation tools available to the clinician for recording the patient’s dental condition. Most operating microscopes can accommodate a wide range of analog and digital VL imaging equipment. Although analog cameras are still popular for microscopic documentation, digital technology is increasingly competitive, especially as the consumer video market converts to digital equipment.
Video cameras generate red, green, and blue (RGB) signals to create video images. If the RGB signals were sent as three separate signals, huge storage and bandwidth capacities would be required. Instead, it is possible to take advantage of the human visual system to reduce storage requirements. This is done by transforming the RGB signals into new video signals that can be band limited with minimal loss of perceived picture quality. In Europe, the dominant television standards are PAL and SECAM. The United States uses three common National Television Standards Committee (NTSC) analog signal formats:
•
Composite video (single 75-ohm cable terminated at each end with RCA connectors). With composite video, the red, blue, and green signals are mixed together. This architecture is present on almost all contemporary home video equipment; when modulated with audio onto a radio frequency (RF) carrier, it is used by over-the-air digital broadcast stations or on coaxial wire by cable TV systems. These systems have the lowest-quality signals.
•
S-Video, or super-video (looks like a single cable but internally has two 75-ohm coax or twisted pair cables terminating at each end in a four-pin DIN connector). S-Video involves the transmission of video signals over a cable through division of the video information into two separate signals, one for color (i.e., chrominance) and the other for brightness (i.e., luminance). Professionals refer to this as
Y/C video, rather than S-Video, because the former is more descriptive of the signal format. These systems produce midrange quality signals.
•
Component video (analog component video uses three 75-ohm coax cables that terminate at each end in RCA connectors, usually color coded and bundled together). Component video reduces artifacts and color errors by minimizing the number of video-signal format conversions between the source and the display device; it transmits its video signal by dividing the Y, R-Y, and B-Y signals separately. These component video signals produce the highest quality signals.
In professional and industrial video equipment, impedance-matched 75-ohm BNC connectors are used for all these signal formats. Also, each of these analog signal formats can be stored, processed, and transported in the digital domain in professional applications. Digital home satellite systems receive MPEG compressed digital component signals and provide component, S-video, HDMI outputs. The digital versatile disk (DVD) format, and the newer “Blu-Ray” format, also based on MPEG technology, is available with analog component video and HDMI interfaces for the highest possible picture quality.
Computer monitors, on the other hand, are designed for RGB signals. Most digital video devices (e.g., digital cameras and game machines) produce video in the RGB format, so the images look best when shown on a computer monitor. When seen on a television, however, these images look better in S-video format than in composite format. To use S-video, the sending and receiving devices and the interconnect cable must be S-video compatible. The newest connections between computers and monitors is the DisplayPort interface standard, which supports both RGB and component encoding formats. DisplayPort connections are interoperable (capable of supporting analog and digital interfaces), can drive display panels directly, eliminating scaling and control circuits that allow cheaper and thinner displays.
Intraoral Cameras
Intraoral cameras that can photograph a single tooth, a group of teeth, or a patient’s full face are available in digital format, using a USB interface with plug-and-play setup. These cameras are very useful for recording the condition of soft and hard tissues for documentation and for patient education and “co-diagnosis” (allowing the patient to visualize problem areas and participate in the evaluation). When VL images from the intraoral cameras are transmitted directly to a clinical chairside workstation, they can be stored along with radiographic images in the patient’s imaging database for easy retrieval. This type of camera can be a valuable adjunct to the microscope-mounted camera because of its lower overall cost. Another advantage of intraoral cameras is the ease with which they can be positioned (Fig. 28-9), especially by dental auxiliaries; a microscope, on the other hand, can be somewhat difficult to position and use with mirrors. Intraoral cameras are available with barrier sheaths to prevent cross-contamination.
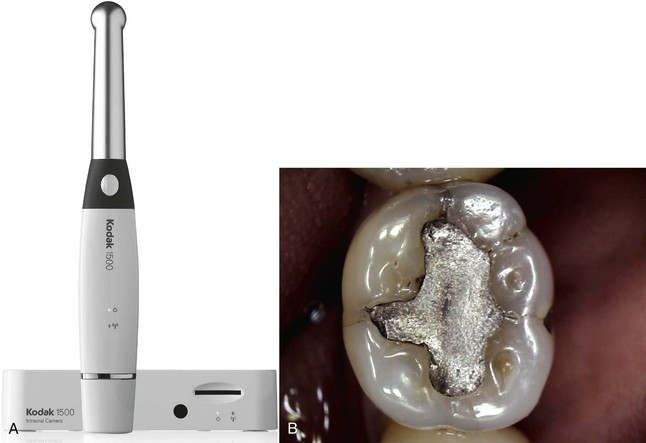
A new intraoral camera (Fig. 28-10, A) is now available for endodontic offices and features a unique liquid lens technology that instantaneously focuses like the human eye. It features a CMOS sensor that captures still images (1024 × 768) and video (640 × 480) with the highest resolution currently available, and supports a focus range from 1 mm to infinity (Fig. 28-10, B). The video output includes the following options: USB 2.0, TV-NTSC, TV-PAL, S-Video, and VGA. Using eight light-emitting diodes (LEDs) to provide illumination, the system automatically adjusts to lighting conditions to optimize illumination and contrast levels. The intraoral camera provides the advantages of auto-focus of still images and video, elimination of undesired light reflection by using a unique polarization filter, and automatic adjustment to lighting conditions.
This camera can substitute for microscope-mounted VL imaging hardware. Unlike older wireless technologies, this camera uses “Wi-Fi” connectivity, which enables reliable wireless performance and easy integration with and without a computer. The small docking and charging station allows the camera to be used anywhere in the practice, encouraging camera sharing across multiple operatories.
Fiberoptic Imaging
The introduction of fiberoptic and rod-lens endoscopes specifically for use in the oral cavity has taken endodontic imaging into the root canal and periapical space.9,10 Both the fiberoptic and the rod-lens endoscope works in conjunction with a camera, light source, and monitor. The clinician views the treatment field on the monitor, which allows the entire treatment team to see the site. A documentation device can be added to the endoscope’s visual system to record the endodontic procedure.
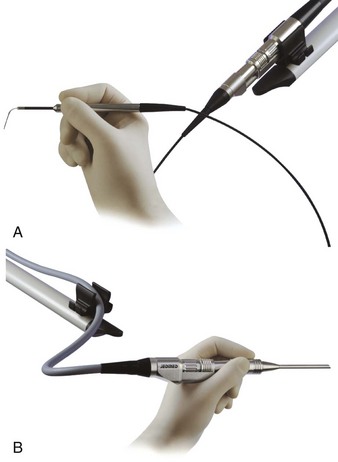
The fiberoptic endoscope is used for intracanal visualization (Fig. 28-11, A). The device is composed of 10K flexible fibers that transmit light to a treatment field and images back to the camera. The fiberoptic scope’s lens has a diameter of 0.8 mm with 0 degrees of angulation.
Two types of rod-lens endoscopes are used for endodontic procedures (Fig. 28-11, B). The model that is 4 cm long and has a lens 4 mm in diameter with 30 degrees of angulation can be used for both conventional and surgical endodontic visualization. Another model, which is 3 cm long and has a lens diameter of 2.7 mm with 70 degrees of angulation, is used primarily for endodontic surgical procedures.
Digital Photography
Intraoral and perioral digital imaging provide valuable documentation tools for clinicians. Many clinicians routinely take images of their patients for identification purposes with consumer-grade digital cameras. However, a dedicated model with specific features is recommended for documenting the patient’s intraoral and perioral condition for patient education purposes, consultation with colleagues, teaching, and other professional uses.
The following criteria should be considered when purchasing a digital camera:
1.
High resolution is important to ensure good image clarity. Although the size of the camera’s image sensor and monitor quality are constantly improving, cameras that can produce an image of at least 1600 × 1200 pixels are recommended.
2.
The camera should have macro capability (i.e., should be adjustable from about 2 inches [5 cm] to infinity) to ensure that oral and full-face images are distortion free and in focus.
3.
Lighting is an important consideration in the selection of a digital camera. For this reason, either a flash diffuser or a ring flash is advised to ensure consistent illumination, make sure color values are accurate, and prevent shadows and highlights that are too bright (
Fig. 28-12).
The advantages of a digital camera include savings on the cost of film and processing, absolute archiveability, instantaneous evaluation of the image, and the ability to catalog and search the image database. In addition, the clinician can print multiple, identical, inexpensive high-quality copies in just a few minutes. The standard methods of image transfer in the industry are direct wiring via the USB or FireWire port and use of small memory cards. Any TWAIN-compliant94 (standard software protocol and applications programming interface that regulates communication between software applications and imaging devices) digital radiography or image organizational software allows the clinician to store these images directly in the patient database.
Radiographic Imaging
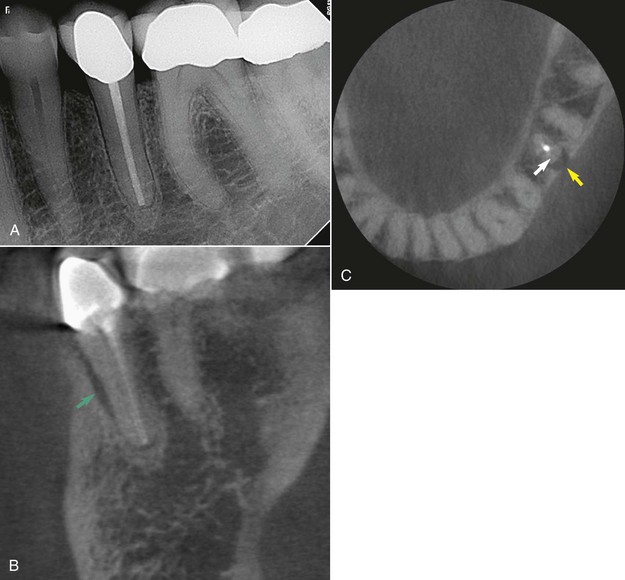
The value of digital radiography in dental and medical diagnosis is well known, especially during operative procedures where time to image is important. Key advantages of digital radiography are: reduction in radiation dose to the patient; patient education; image optimization and computer-aided feature extraction;96a workflow improvement; the avoidance of shipping, darkroom, or chemical processing errors; environmental waste reduction; improved electronic communications68; image archiving; and projecting a technologically advanced practice image.21,68 Solid-state digital imaging using CCD or complementary metal oxide semiconductor (CMOS) detectors has become an increasingly popular technology for intraoral and extraoral dental radiography. Three methods of producing digital images are available: direct solid-state detectors (e.g., CCD/CMOS detectors35,77), indirect photostimulable phosphor plates,97 and indirect secondary capture of conventional film by scanning.27 The most useful technology for endodontic practice is the direct model, because digital detectors can produce an image in seconds, often at a lower radiation dose than film.13
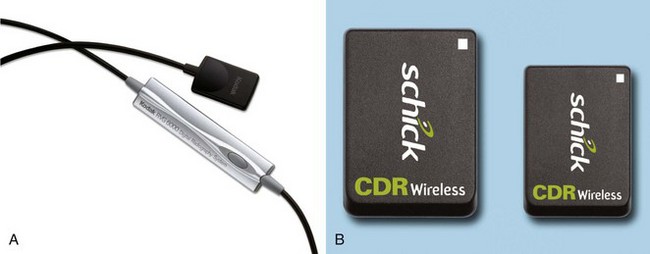
A CMOS detector is literally a camera on a chip (Fig. 28-13, A). Because it has a full digital interface, the analog signals from the scintillator are translated to digital signals by the chip. Simply stated, CCD systems require many supporting components (e.g., timing generators, shuttering and signal-processing chips), whereas CMOS detectors integrate all these functions in a single chip. Any computer with a USB port can accept this detector, and a separate processing board is not needed. Several manufacturers produce CMOS detectors of x-radiation, integrate the radiographic image, and initiate the readout of the pixel data.
Taking this technology a step farther, Schick Technologies (Long Island City, NY) manufactures a wireless sensor, the CDR Wireless (see Fig. 28-13, B). This device sends a radio frequency signal to a nearby remote receiver on the 2.4 GHz band that produces an image with the same quality as the wired version. Unlike the CCD, the CMOS chip requires very little electrical energy; therefore no external power supply is needed to support USB utilization, and wireless applications are feasible.
Storage phosphor plate technology allows indirect production of radiographic images using a semiflexible, phosphor-coated plate. With the DenOptix system (Gendex, Des Plaines, IL), plates are loaded into a sheath, exposed, mounted in a carousel, and then placed in the scanner. As many as eight intraoral images are ready for viewing in about 1 minute if the lowest-resolution scan is used. The plates are available in periapical, panoramic, and cephalometric sizes, and they support a wide range of exposure settings. The advantages of this system are that very thin plates are equivalent to film in size, and placement characteristics are very similar to those of film because there is no wire on the plate. The main disadvantages are longer processing times (compared with only seconds for CCD/CMOS sensors), light sensitivity during transfer to the scanner, and the additional handling steps of erasing and sheathing the individual plates between uses. For individual intraoral images, the Air Techniques Scan-X processor (Air Techniques, Hicksville, NY) can process the initial image in less than 20 seconds and subsequent images in about 4 seconds. New intraoral plates have a surface protective layer but can still degrade as a result of scratching during use.
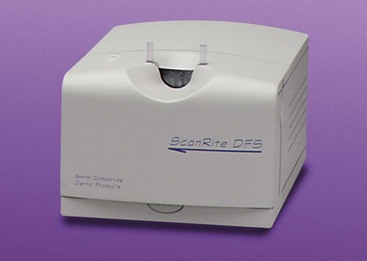
For the truly paperless office, a film scanner (Box 28-4) is necessary because it allows input of historical, film-based radiographic images. Both dedicated film scanners and flatbed scanners are available for digitizing radiographs. The ScanRite dedicated film scanner (ScanRite Systems, Fremont, CA) provides a single image in about 10 seconds (Fig. 28-14). This high-resolution image can be enhanced and imported into any TWAIN-compliant software through the USB port on the computer.
BOX 28-4 Dental Film Scanning
A scanner can be used as a complement or an alternative to a sensor-based or phosphor plate–based digital radiography system. Scanned film images can be saved in digital radiography system software, patient management software, or third-party imaging software (such as that included in the Windows XP and Vista operating software).
Complementary System
To complement a sensor- or phosphor-based digital radiography system, both the scanner and the system software must be TWAIN compliant. This allows images to be scanned directly into the electronic oral health record (EOHR). Some system software even names the file automatically to simplify the process.
Alternative System
Scanners can be used as an alternative to a sensor- or phosphor-based digital radiography system because the investment cost is lower, and the image quality can be excellent. If the office is networked or is wired for monitors in the operatories, the image can be scanned at any location and shown on any computer linked to the network. Two major classes of scanners are of interest to the dental clinician: (1) the relatively inexpensive flatbed scanner and (2) the more expensive dedicated film scanner.
Flatbed Scanners
Certain models of flatbed scanners offer a transparency adapter to allow scanning of radiographic film. Flatbed scanners typically are best used for documents, photographs, panoramic films, and cephalometric films. Flatbed scanners usually are slow to preview and slow to scan, and their image quality and resolution are inferior to those of dedicated film scanners.
Film Scanners
Dedicated film scanners typically are best used for film-based images. The ScanRite (see Fig. 28-14) is a fast, high-quality film scanner specifically designed to input periapical and bite-wing films, mounted 35-mm color slides, and 35-mm color film. The primary considerations in choosing a dental film scanner are resolution, levels of gray scanned, speed, software, and convenience. Scanner resolution typically is quantified as dots per inch (dpi). Higher resolutions result in better clarity when images are enlarged. Optical resolution describes the capability of the hardware. Interpolated resolution is the ability of the scanner software to place additional dots among the data scanned. Image quality can be adversely affected by “noise” during image processing of either a scanned or direct digital image.
The levels of gray or number of colors scanned is important because each scanned dot is assigned a “color.” The more grays or colors scanned, the better the image quality. With fewer grays or colors, images are “blotchy.” This can be demonstrated by adjusting the computer monitor settings to a low color palette or depth while viewing a digital image.
The scanning speed depends on many factors. Better scanners have a built-in buffer memory so that the data do not have to be sent in multiple “bursts” to the computer. Better scanners scan in one pass without stopping. Scanning speed also depends on the resolution selected, the physical size of the original, whether color or grayscale is used, the speed of the microprocessor, and the amount of random access memory (RAM) in the computer.
The better scanners include software with the capability to change the color, select film calibrations, sharpen the image, rotate the image, scale the output, match the output (i.e., gamma level) to other software applications, invert colors or grayscale levels, and save settings for various types of originals. Most scanner software allows an image to be previewed before it is saved to disk; however, this small preview image makes it difficult to make image enhancements accurately. Dedicated film scanners save time by automatically optimizing the brightness, contrast, and color for each scanned image.
Consumer-level flatbed scanners can be used to scan film-based images, but these require transparency adapters. Flatbed scanners also can be used to scan paper documents and append them to the patient’s digital chart. Nevertheless, a dedicated single-purpose scanner with a document feeder is recommended for paper documents.
The value of instant digital imaging in the modern dental office is well known, especially for endodontic and implant procedures. Many researchers have concluded that digital x-ray sensors equal analog film for diagnostic tasks, with the added benefits of immediate image production, image feature enhancement and the increased security of offsite archiving.24 Conventional film provides a finer grade of detail through continuous shades of grayscale images, rather than the discrete pixels of individual gray levels used by digital systems. Advances in digital imaging continue, such as improved resolution, enhanced digital subtraction radiography,72 and active surfaces approaching those of film, and in the not-too-distant future, digital image quality may surpass that of film.
To produce the highest quality digital radiographic image, consideration must be given to the entire “imaging chain” (i.e., the x-ray generator, subject, sensor, computer interface, and monitor). The quality of a digital image depends on each step of the process, and the weakest link degrades the final result. The following sections discuss basic considerations for a better understanding of digital imaging.
Image Quality
One of the most critical and most misunderstood issues concerning digital representation of image data is clinical performance. Computer screen selection, ambient lighting,52 and image compression all affect the image; however, for the purchasing decision, the most compelling issue should be the image quality of dental structures as perceived by the clinician.
Clinical performance depends on numerous interrelated factors and can be expressed as detective quantum efficiency (DQE), the measure of noise and contrast expressed as a function of object detail. Noise is an inevitable product of the digital imaging chain and is reflected in the signal-to-noise ratio (SNR). Systems with a high SNR produce the best image quality. Compensating for poor SNR is possible—to a point—with increased radiation, but this increasing dose negates one of the key advantages of digital systems. Moreover, excessive dosage can lead to detector saturation and reduced image contrast. Contrast performance is the ability of the system to display the actual contrast of an object, and the ability to make window and level adjustments is potentially one of the true benefits of digital radiography over film. Digital detectors generally have a wide dynamic range, with thousands of shades of gray; therefore they might depict areas that might be overexposed or underexposed on film. Window and level adjustments are needed to display all the subtle contrast variations in a digital image, just as a bright light might be used to evaluate an overly dense analog film’s radiographic detail.
The ideal is to produce a high DQE by combining low noise and high contrast so that small low-contrast objects can be detected. Another potentially significant advantage of a high DQE is that digital systems can produce better small, low-contrast object detection than film with the same radiation dose. In the future, improving the DQE (high DQE results in low-noise images with high object detectability) coupled with advanced image processing algorithms and other postprocessing improvements will lead to enhanced visualization.31,40 According to one expert,28 “DQE is useful when it comes to accurate measurement for endodontic purposes”; however, the DQE is largely theoretical because few dental studies have actually used it.
Simple comparisons of limiting spatial resolution (LSR), the spatial frequency at which the observer can no longer detect a high-contrast test pattern under laboratory conditions, and digital detectors are problematic because there is a point of diminishing returns. The amount of signal captured per pixel is reduced as pixel size becomes smaller, although the amount of noise remains relatively constant for each system. Increasing the number of pixels can result in a lower SNR at each pixel, which limits small object detection. Even though sensors may have LSRs as high as 20 to 22 line pairs per millimeter (lp/mm) when measured using high-contrast lead grids, the smallest object that can be detected is usually larger in clinical circumstances. In addition, noise and contrast combined with limitations of human vision’s poor response to high spatial frequencies limit small object visibility. Nevertheless, the latter problem is somewhat obviated by the ability to zoom-enlarge digital image details. Unfortunately, as low-contrast details such as lateral root canals become even thinner in dimension, there might not be sufficient contrast to detect them, regardless of the system’s spatial resolution. There is no free ride. A low DQE, even with a high LSR resulting from high noise and low contrast, may remain a limiting factor.
Furthermore, the quality of many film-based images may be compromised by operational problems such as chemical and film freshness, developing inconsistencies, light leaks, and shipment handling. Gross and moderate caries can be detected with both conventional film and digital imaging systems with a great degree of surety. Studies50,101 showed relative equality between digital and film-based radiographs for caries detection. Another study91 compared the accuracy of caries detection in film-based, storage phosphor, and CCD sensors. They found that the diagnostic accuracy of film was comparable to that of digital systems. The study also noted that the dentist’s ability to evaluate the radiographs accurately was the most significant variable in radiographic diagnosis. Unfortunately, the presence of caries is always more extensive than depicted by either digital or film systems. Incipient caries and some periapical lesions continue to present a challenge for both film and digital-based systems.
Caries detection on interproximal surfaces has been further refined with the development of smart software that uses a software algorithm approved by the U.S. Food and Drug Administration (FDA), originally developed for the defense industry. This predictive software, the Logicon Caries Detector (PracticeWorks, LLC, Atlanta, GA), produces three types of diagnostic aids to improve caries detection by up to 20%.38
In the detection of periapical bone lesions created in cortical and trabecular bone, some have stated that no difference was seen among E-speed film, CCD, and CMOS sensors.74 Furthermore, the study noted that “cortical bone lesions were detected with significantly higher accuracy once the junction of the cortical plate was involved or perforated.”6 However, caution must be exercised when evaluations are made using artificially created lesions.
Digital detectors produce images with a dynamic range of 8 to 16 bits. A typical 12-bit system records 4096 shades of gray. Because most computer monitors can display only 8 bits, or 256 shades of gray, some of the data are lost in the transformation. If these data are processed linearly instead of by sophisticated algorithms, some useful data are discarded.26 These types of algorithms are commonly used in most modern digital systems to maintain the clinical usefulness of the images produced.
Radiation
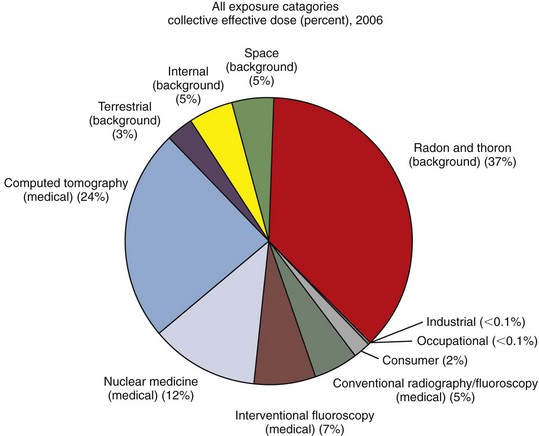
Silver-halide film records the interaction of x-ray photons with electrons in the film emulsion.30 The photons are either attenuated (absorbed or scattered) or transmitted (along with some scatter) and reach the film emulsion to create a latent image. This image is then chemically processed to reveal the viewable radiograph. Film images are characterized by continuous shades of gray between the extremes of black and white.76 However, film requires a relatively high dose of x-radiation to achieve the same result as a direct digital detector. According to van der Stelt,96 “the primary principles of radiation protection in diagnostic radiology are justification (the patient will experience more benefit than harm from the exposure) and the ‘as low as reasonably achievable’ (ALARA) principle.” Despite the fact that radiation exposure can be reduced by using thyroid shields, the highest-speed films, and rectangular collimation, studies consistently demonstrate that radiation hygiene is not practiced by dentists to its fullest benefit. In 2006, medical x-rays, especially medical CT and nuclear medicine imaging, constituted nearly half of the total radiation exposure of the U.S. population from all sources (Fig. 28-15). New guidelines issued in 2003 by the National Council on Radiation Protection (NCRP) in its Report No. 145 supersedes the previous report published in 1970.68b
If the states adopt the newest NCRP recommendations (Box 28-5), as is commonly done, most dental offices would not be in compliance. Two terms used in the report have been specifically defined. The terms shall or shall not indicate that adherence to the recommendation would be in compliance to the standards of radiation safety. The terms should or should not indicate prudent practice and acknowledge that exceptions may be made in certain circumstances. In addition, there are also nine new recommendations for image processing of conventional film in the NCRP report. A strong argument can be made for clinicians to switch to a direct digital radiography system to avoid all the drastic changes necessary to assure compliance with the new recommendations.
BOX 28-5 National Council on Radiation Protection Recommendations
From the National Council on Radiation Protection and Measurements: Radiation protection in dentistry, Report #145, Bethesda, MD, 2003, NCRP. Available at <ncrponline.org/Publications/145press.html>. Accessed July 17, 2009.
1.
Dentists must examine their patients prior to ordering or prescribing x-ray images (this is not a new guideline).
2.
The use of leaded aprons on patients shall not be required if all other recommendations in this report are rigorously followed (read full report #145).
3.
Thyroid shielding shall be used for children and should be provided for adults, when it will not interfere with the examination (e.g., panoramic imaging).
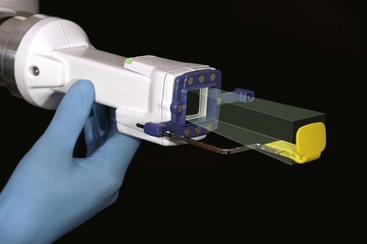
4.
Rectangular collimation of the beam, which has been recommended for years, shall be routinely used for periapical radiographs. Each dimension of the beam, measured in the plane of the image receptor, should not exceed the dimension of the image receptor by more than 2% of the source-to-image receptor distance. Similar collimation should be used, when feasible, for bitewing radiographs.
5.
Image receptors of speeds slower than ANSI speed Group E films shall not be used for intraoral radiography. Faster receptors should be evaluated and adopted if found acceptable. For extraoral radiography high-speed (400 or greater) rare earth screen-film systems or digital-imaging systems of equivalent or greater speed shall be used.
6.
Dental radiographic films shall be developed according to the film manufacturer’s instructions using the time-temperature method. In practical application, this means that sight development (reading wet x-ray films at the time of the procedure) shall not be used.
7.
Radiographic techniques for digital imaging shall be adjusted for the minimum patient dose required to produce a signal-to-noise ratio sufficient to provide image quality to meet the purpose of the examination.
8.
Clinicians designing new offices or remodeling existing locations will need shield protection to be provided by a qualified expert.
Digital intraoral imaging generally requires less radiation than film-based systems, a key public health benefit. According to the ADA Council on Scientific Affairs, digital imaging reduces radiation exposure by 50% to 90%.5 Film scanning provides no reduction in radiation, because a conventional film image must first be produced.
Although digital radiography promises to reduce radiation for each image exposure, the real radiation a patient receives in relation to the diagnostic information gained remains controversial. In studies by Versteeg et al. and Sommers, technique errors for digital detectors were higher than film-based systems.87,98 The most common difficulty, according to focus-group studies, was found to be sensor positioning. These findings dramatically point out the need for careful and ongoing training of dental technicians in the art of taking radiographs with digital sensors—a critical step in taking full advantage of the benefits of reduced radiation for each image exposed.
Placement errors aside, most CCD and CMOS-APS detectors have a similar range or exposure latitude to counteract under- or overexposure. Direct digital detectors take about 100 times more exposure to produce a black image than a light gray image, or a 100:1 ratio. In comparison, film has about a 1000:1 ratio, and PSPs have a range of 10,000:1.99 Although the benefit of PSPs’ wider range of exposure latitude may “save” an occasional overexposed image, PSPs can lead to inadvertent excessive radiation exposure, because overexposure will less likely produce poor image quality as a warning.11 Strict adherence to preset exposure settings will continue to require diligence to reduce radiation exposure. Additional reduction in radiation to special-needs patients (e.g., patients with developmental disabilities or are severely mentally handicapped) may also be realized because of the advantages of digital detectors.29
Common dental projections rarely if ever deliver a measurable absorbed dose to an embryo or fetus, but any radiologic procedure on a pregnant patient should be conducted so as to minimize the radiation dose to the pelvic region.47 This procedure should be conducted only if x-ray exposure is required for adequate diagnosis and treatment. If dental care is to be delayed until after delivery, exposure should also be delayed. Also, usual and customary radiographic selection criteria should be applied for patients who are trying to get pregnant, breastfeeding, or have received radiation therapy to the head and neck for medical purposes (the radiation dose from dental radiography is insignificant when compared to therapeutic dosing).39,64
Even though restriction of an intraoral dental x-ray beam is mandated by federal law to be a circle no greater than 7 cm, rectangular collimation has proven to significantly reduce radiation dose to the patient. The ADA Council on Scientific Affairs states that the “tissue area exposed to the primary x-ray beam should not exceed the minimum coverage consistent with meeting diagnostic requirements and clinical feasibility. For periapical and bitewing radiography, rectangular collimation should be used whenever possible because a round field beam used with a rectangular image receptor produces…unnecessary radiation exposure to the patient.”5 In a recent study by Seltzer et al.83 comparing a new rectangular collimation system, Tru-Align (Interactive Diagnostic Imaging Inc, Atlanta, GA), with conventional round collimation, the rectangular collimator (Fig. 28-16) reduced skin surface–area dose by a factor of almost 5. The Tru-Align system, deemed easy to use, generally gave perfect alignment with only occasional cone-cuts.
Personnel monitoring is required in all states to assure compliance with established ionizing radiation limits. According to the Maryland Department of the Environment guidelines,88 monthly badges are required for the first 6 months of employment to document that radiation will not exceed 10% of the legal radiation limit set by the state. Ionizing radiation dose limits for Maryland of 5000 millirem for workers, 500 millirem in 9 months for pregnant women,47 and 100 millirem for the general public are mandated by state regulation. All dosimetry badge reports must be maintained at the office for review as proof of minimal radiation exposure. Variations of these requirements are found in each state, so familiarity with the controlling laws is mandatory.
Quality Assurance
Clinicians should ensure that their practices take all necessary steps to produce consistently high-quality radiographs with minimal ionizing radiation exposure to patients and staff. Dental office quality assurance involves periodic evaluation of the entire imaging chain, including the x-ray generator, film procurement and storage, developer,30 darkroom, view boxes, and protective aprons. Administration of quality assurance requires assigning responsibility, training, evaluating results of testing, and taking corrective action.53 Ohio, for example, requires each registrant to maintain a site-specific written quality assurance program with published requirements for how often x-ray generators need to be tested and calibrated and so on.73
Patient Education
Most people of college age and older are visual learners, and presentations that include both visual and auditory modalities are superior to visual or auditory modalities alone.32 Consider the educational value for the patient able to view a large, high-resolution radiograph in conjunction with the clinician’s diagnostic explanation (Fig. 28-17). Once the patient understands their dental condition (e.g., caries, periradicular pathosis), treatment acceptance becomes more assured, and the patient experience is enhanced.
Workflow Improvement: A Work Multiplier
Digital radiography is a work multiplier; it replaces human effort, making tasks the practitioner and staff members perform easier and more error free. In some cases, it makes new tasks possible.19 DDR images take less time to expose, duplicate, retake, and transmit, all with less radiation and environmental impact. With solid-state systems, any operative procedure, such as endodontic therapy and implant placement, can be performed in less time. The diagnostic yield of digital imaging systems will improve as enhancements are made to image acquisition, but also to our understanding of human vision and cognition. Image processing can improve diagnostic outcomes by defining diagnostic issues and designing tools to achieve specific goals.68a Also, visual information such as digital radiography and visible light images (i.e., intraoral photography, microscopy) is easier to access than film-based images and improves office operations by increasing efficiency. PSP plates take at least 8 seconds to process after the detector is transported to the developing site and unwrapped, whereas CCD/CMOS-APS detectors are virtually instant, with “paint times” usually just a few seconds. Some workflow advantages are shown in the following comparisons.73a
Optimization
All digital radiographic systems allow for some image optimization (Fig. 28-18, A). Postexposure image processing routines differ among manufacturers. Some produce a raw image for which automatic enhancement routines can be turned on and off, whereas others produce images that are filtered automatically. Most software features the ability to change contrast and brightness to view images that are underexposed or overexposed, as well as to equalize density, magnify (see Fig. 28-18, B), create an inverse image (see Fig. 28-18, E), and allow for image rotation and mirror imaging. Another enhancement, pseudocoloring, ascribes false colors based on the brightness of pixels and can help with patient visualization of images.54 A number of systems also have algorithms that can sharpen and enhance caries imaging, and the future promises even more improvements.70
Filtering tools are available in all commercially available software, but comparison is difficult because proprietary names do not reveal the underlying algorithms. Investigators55 studied the functionality of 13 software programs and suggested more standardization of filtering tools to improve exchange, enhancement, processing, and analysis. They further suggested that public-domain image processing and analysis software, similar to software adopted for medicine by the National Institutes of Health (NIH), may provide the basis for more standardization.70
Measurement
The three types of measurement generally available with digital imaging software are (1) linear measurement, the distance between two points in millimeters (see Fig. 28-18, F); (2) angle measurement, the angle between two lines; and (3) area measurement, the area of the image or a segment of the image.
Because magnification and distortion error play a significant role in all two-dimensional radiographic measurement accuracy, both film and digital systems are subject to parallax error. However, a study22 that compared endodontic file length images of human teeth taken with a custom jig suggested that “measurement error was significantly less for the digital images than the film-based images.” This was true even though, as the authors pointed out, the measurement differences may not be clinically significant. Sophisticated calibration algorithms are under development, and accurate measurement of parallel images should be more feasible in the future.13
Security
Although film-based images can easily be produced in duplicate, each subsequent rendition of the image is reduced in quality. Digital images, on the other hand, can be reproduced in unlimited number because the images can be stored and produced without any loss of detail. Furthermore, digital images can be stored on and off site and on many types of media, which helps prevent permanent loss from theft, fire, or other causes.
Paradoxically, the ease with which digital images can be reproduced and stored allows for alteration of radiographs without a trace.25,100 Of course, this has always been possible with duplicated analog film images, but the issue has not been commonly addressed. The ease of producing an altered image is controversial, but most digital vendors on the market have safeguards that greatly minimize the possibility of this occurring. In addition, standards such as Digital Imaging and Communications in Medicine (DICOM; discussed later in the chapter) help protect image integrity through the use of digital signatures in the form of tagged attributes attached to each image.25 Archiving radiographic images in a secure site in DICOM format using removable media such as DVD and tape is one of the current solutions to this problem. These types of magnetic and optical media can be stored off site by a third party archivist for extra protection.
These data are also vulnerable when sent via the Internet to a discussion site. Two common technologies, Secure Socket Layer (SSL)1 and digital certificates (VeriSign, Mountain View, CA), can provide at least 128-bit encryption and virtually eliminate the chance of alteration or fraud. SSL connections to Internet servers can be recognized by the prefix https:// in the address line. In any event, such material should be carefully secured to fulfill HIPAA requirements regarding privacy.
Another important security consideration is the database engine used to store the files on the server. Among the most robust systems are SQL-based models, which allow for client-server configuration with industry-standard software protocols. Images that are stored and retrieved cannot be deleted, nor can patient identification be changed, without opening a separate administration utility, which can be password protected on the server.
Image Storage and Compression
All computer-based images are voracious consumers of hard drive space, and various manufacturers have used a number of techniques to reduce image size. For example, Schick Technologies allows acquisition of each image with the advanced compression technology of the JPEG4 codec. Clinicians can also compress selected groups of images between certain dates with up to four different compression schemes, allowing for lossless (no visible change in image clarity with approximately 50% to 75% reduction in file size) to lossy (significant reduction in file size with some degradation of image resolution) compression. Lossy compression is not recommended for dental grayscale images.
Markers
Occasionally, radiographs and VL images need a tag so the clinician can return to them later to assemble teaching or patient education materials. Most software today allows markers to be placed so that a computer search can call up the images efficiently. These customized tags can be useful in organizing cases that require special follow-up to evaluate postoperative healing. In addition, readily available software enables the clinician to create notes and diagrammatic annotation of important features of an image (see Fig. 28-18, D, F, and G).
Computer Interface
Many digital sensors connect to the chairside computer workstation via the USB port. As of 2004, only Schick Technologies had produced a wireless sensor that transmits the image data by radio frequency to a nearby receiver and thence to the USB port, eliminating any sensor wire. The direct USB connection eliminates any computer interface board, which simplifies installation and maintenance. Laptop configurations add flexibility if the clinician wants to move the equipment between different operatories and office locations or use it for off-site procedures at hospitals and nursing homes. Laptop configurations also benefit from the elimination of special cards for sensor connection. System backup strategies are particularly important for laptops because of the increased risk of theft or of being dropped.
X-Ray Generator
According to Miles, the image chain is only as good as its weakest link, and digital systems work best with a modern x-ray generator.66 Images from digital detectors are optimized if taken with an x-ray generator that has (1) an extremely accurate timer, especially for short exposures,51 (2) low mA and kV settings, and (3) a direct current (DC) circuit. Farman,28 however, contends that the x-ray generator has not been shown to have a significant effect on digital radiographic quality.
Focused Field Cone-Beam Computerized Tomography in Endodontics
Endodontics is an image-guided specialty, and until recently, endodontic radiographic diagnosis relied on two-dimensional radiographic assessment. The introduction of cone-beam computerized tomography (CBCT), and especially recent refinements such as very small field of view (FOV) or focused-field devices, is revolutionizing the visualization of the dentition and the maxillofacial complex (see online Chapter 29).
The shortcomings of panoramic radiography have been well understood for many years. They are flat, two dimensional, superoinferior or posteroanterior images that suffer from superimposition of all structures imaged and distortion and magnification errors. Therefore, measurements of objects on panoramic images are inaccurate. CBCT images, on the other hand, capture anatomic entities in three dimensions (3D) and can be viewed by digital selection of the region of interest (ROI) with great accuracy. In recent research published by Stratemann et al.,89 linear measurements of skulls comparing calipers and CBCT imaging revealed only a 1% relative error.
According to one source,41 “these machines are smaller than medical CTs, less expensive to purchase and operate, produce a fraction of the radiation dose, and possess an open architecture that, generally, eliminates patient complaints of claustrophobia.” Unlike periapical radiography, CBCT scans enable the visualization of the “true extent of lesions and their spatial relationship to important anatomic landmarks.”15 Comparing periapical radiographs (PAs) of 156 maxillary posterior roots with small field CBCT images prior to surgery, investigators61 found that these CBCT images showed 34% more lesions than were visible with PAs alone (Fig. 28-19). Numerous papers have demonstrated that CBCT imaging is superior to PA radiography in detection of periradicular lesions. Researchers37,67 created artificial osseous defects and conclusively demonstrated the improved detection rate of bony defects with CBCT imaging. Other researchers59 reported that in 70% of cases that were evaluated with both PA and CBCT, CBCTs provided clinically relevant information not visible on PA radiography. Other researchers have reported that CBCT, which can be used to measure the grayscale values of lesions, may provide a better, more accurate, and faster method to differentially diagnose a solid from a fluid-filled lesion or cavity. This may allow the clinician to decide whether or not periradicular surgery is necessary without waiting for a long recall period to see if healing has occurred.84
Newly introduced hybrid units like the Kodak 9000 3D extraoral imaging system (PracticeWorks, LLC, Atlanta, GA) have two digital detectors, one for digital panoramic imaging and one for focused-field digital volumetric tomography (Fig. 28-20). Aside from panoramic radiographs, this unit produces 3D images of an area measuring just 37 mm × 50 mm (approximately a quadrant), with less radiation than a standard CBCT and improved readability because of its new higher-resolution detector. Unique to the Kodak 9000 3D system is the highest-resolution sensor available at this time, with a voxel (volume pixel, representing a quantity of 3D data similar to a pixel representation in 2D data) size of just 0.076 mm. While not necessary for use in every case, when appropriate, this technology will improve visualization and ultimately lead to better care. This is because imaging the maxillary posterior region poses unique challenges, where roots of teeth overlap and anatomic structures such as the zygomatic buttress and maxillary sinus are present.
Medical CTs necessitate a significant radiation dose to patients, with a typical scan of the maxilla and mandible of 2.00 millisieverts (mSv), or as much as 345 panoramic images. On the other hand, large FOV CBCTs will image the same area at 0.068 to 1.073 mSv or 3 to 44 panoramic equivalents.63 The focused-field FOV CBCT will further reduce radiation exposure to 0.005 to 0.038 mSv62 because of its limited coverage and low mA technique factors (Table 28-2).
TABLE 28-2 Effective Doses From Various Dental X-Ray Procedures
| Radiation Source* |
Millisieverts (mSv) |
Time Period for Equivalent Effective Dose From Natural Background Radiation(United States is 3 mSv/year) |
| CBCT (focused FOV) |
0.005-0.038 |
1-5 days |
| CBCT (large FOV) |
0.068-1.073 |
9-131 days |
| Panoramic† |
0.010-0.026 |
1.2-3.2 days |
| Cephalometric |
0.026 |
3.2 days |
| Full-mouth intraoral (18 F speed films)‡ |
0.150 |
18.3 days |
| Bitewings (4 F speed films)‡ |
0.038 |
4.6 days |
| Intraoral periapical radiograph |
0.005 |
0.61 days |
| Maxillomandibular CT |
2.000 |
243 days |
| Maxillary CT |
1.400 |
170 days |
| Mandibular CT |
1.320 |
160 days |
| CT abdomen |
10.000 |
3.3 years |
| Chest (PA film) |
0.020 |
2.4 days |
| Average galactic radiation in Denver, CO (per year) |
0.510 |
62 days |
CBCT, Cone-beam computed tomography; CT, computed tomography; FOV, field of view; PA, posteroanterior.
Effective doses from various dental x-ray procedures adapted from the Health Physics Society: <http://hps.org/publicinformation/ate/faqs/dentalpatientissuesq&a.html>. Accessed July 17, 2009; American Dental Association: <http://www.ada.org/public/topics/xrays_faq.asp>. Accessed July 17, 2009; and White SC, Pharoah MJ: Oral radiology: principles and interpretation, ed 6, St Louis, 2009, Mosby.
Integration of third-party digital radiography and VL imaging products is very important to the modern endodontic practice, especially if the goal is to create a paperless environment. Several open platform applications specific to dentistry are available that allow the clinician to acquire, store, annotate, manipulate, and output many types of images. Comprehensive packages such as ViperSoft (Integra Medical, American Fork, UT), TigerView (Televere Systems, Los Gatos, CA), and Kodak Dental Imaging Software (PracticeWorks, LLC) work with analog and digital still and video cameras, scanners, and digital radiography programs. Once an image has been acquired, these sophisticated software programs allow the clinician to label and annotate the image, transmit it by e-mail, and even simulate the repair and restoration of teeth (i.e., cosmetic imaging). As operatory-based computers become the norm, dental imaging systems are becoming mainstream, allowing secure network e-mail transfer of images in several industry standard formats (i.e., DICOM, TIFF, BMP, JPEG, and TGA). Before purchasing any software, including imaging software, the clinician should confirm that it is HIPAA compliant (transaction types, standards, and code sets) and DICOM conformant to the requirements set forth in DICOM Supplement 92 (2004).18
Imaging software can be an invaluable aid for cataloging images for easy retrieval, case presentation to other dentists and patients, analysis, and magnification of images for improved diagnosis. Sophisticated practice management software should integrate smoothly with these systems, extending the functionality of the office software and creating a complete EOHR.
Sterilization Area
The computer in the sterilization area can be used to create, print, or transmit patient treatment reports, to order supplies, for general communication duties, and as a backup for the front desk system. One advantage of creating the report in the clinical area is that the staff member who assisted with treatment can individualize the report as necessary. Once a template has been created and the software populates the preset fields, radiographs and VL images can be inserted and then sent to an approval queue to be inspected by the clinician in the private office, or an assigned staff member can print or e-mail it. Some practice management software programs are designed to create these reports at the chairside computer workstation and send them directly to predesignated printers and specific paper trays. Report generation at the chairside promises to further streamline the patient treatment report process.
Administrative Area
The generation of marketing materials; bookkeeping, payroll, and banking functions; bulk scanning; and special projects can be assigned to the administrative computer. Although small offices often use the front desk computer for these tasks, the increased utility of a separate computer for special projects cannot be overemphasized.
Clinician’s Office
The clinician’s office should be equipped with a workstation that allows entry into all the programs on the network. Ample connections for uploading camera images and digital video sequences, for Internet access, and for a smart phone are also recommended. The smart phone modules available from some vendors allow the clinician to take home a synchronized database of patient and referring clinician information, the appointment schedule, and images (Fig. 28-21). This facilitates after-hours emergency communication and allows notations made to the patient’s chart to be synchronized with the office database the next time the smart phone is connected to the LAN.
Real-time video conferencing and collaboration can also be handled from the clinician’s office computer. Addition of an Internet camera with audio capability is all that is needed to communicate with a colleague via the Web.
Computer Industry Standards
Graphics and Imaging
For most clinicians, graphics and imaging is a confusing area. Windows has many graphics standards; it has been difficult to sort out which ones to use, but this is beginning to change. Although some dental imaging software stores graphics data in nonstandard ways, most products support computer industry norms. It is less important that clinicians understand the peculiarities of the different graphics storage categories than which ones to look for in a program. The importance of standards here is simply that if the graphics are stored in a standard manner, clinicians will be able to manipulate an image and drop it directly into the dental software. Some of the common image formats are:
•
Bitmap (BMP): This is the Microsoft standard for Windows. It is used and understood by almost all imaging software and is the format of most pictures delivered with a Windows computer. Its strengths are universal distribution and very high quality. Its chief weakness is that the files it creates are not compressed and take up more space.
•
Joint photographic experts group (JPEG or JPG): This is probably the most popular standard for PCs and the Internet. It has good quality and supports compressed formats (allowing for smaller files). When JPEGs are resaved, they are recompressed; therefore, care must be taken to limit the number of times the image is saved, or it must be saved in a different format (e.g., TIFF). JPEG 2000, the new image coding system, uses wavelet technology that allows improved compression and smaller-sized files.
92•
Tagged image file format (TIFF or TIF): This is also a very popular standard because the images are highly flexible and can be used with many different image processing applications.
6 The images are usually very high quality and typically support minimal compression.
•
Graphic interchange format (GIF): This is a very compressed format that is most popular on the Internet and online services, but it is not helpful in storing digital images.
Open Database Connectivity
One of the classic problems in the computer industry is that each vendor stores and manipulates its data differently. As a result, data can be read only if tools created by the same company are used. To correct this problem, Microsoft introduced open database connectivity (ODBC). With ODBC in place, software programs connecting to databases first connect to ODBC (another software product, called a driver), and ODBC connects to the database. This makes ODBC (and other derivative standards, such as JDBC and OLE DB36) a translator between software programs and databases. The advantage of ODBC is that software developers can plug into different databases without changing their program codes. In addition, ODBC-compliant databases are accessible from many programs.
ODBC is helpful to clinicians because it allows them to read and analyze the database from spreadsheet programs, report writers, graphics programs, and other database programs. In today’s open-standards world, it is unwise to purchase any product that is not ODBC compliant.
Digital Imaging and Communications in Medicine
DICOM is a set of international standards established in 1985 by the American College of Radiology (ACR) and the National Electrical Manufacturers Association17,69 (NEMA) to address the issue of vendor-independent data formats and data transfers for digital medical images.75 The ADA has promoted the interoperability of dental images through the efforts of its Working Group 12.1.26
DICOM serves as a standard for the transferal of radiologic images and other medical information between computers, allowing digital communication between systems from various manufacturers and across different platforms (e.g., Apple or Windows).19 The DICOM standard provides for several hundred attribute fields in the record header, which contains information about the image (e.g., pixel density, dimensions, and number of bits per pixel), as well as relevant patient data and medical information. Although earlier versions did not specify the exact order and definition of the header fields, each vendor is required to publish a DICOM conformance statement, which gives the location of pertinent data. The DICOM standard also supports a form of SSL (see section on security) for the transmission of digital output. The big hurdle is to support medical and dental consultations between two or more locations with different imaging software. With DICOM in place, dental clinicians can change vendors and maintain database continuity. Most software vendors are striving to achieve full DICOM compliance, and some have achieved at least partial compliance.
Based on the DICOM model, the ADA Standards Committee on Dental Informatics has identified four basic goals for electronic standards in dentistry: (1) interoperability, (2) electronic health record design, (3) clinical workstation architecture, and (4) electronic dissemination of dental information.3 The dental profession must continue to promote DICOM compatibility so that proprietary software and file types do not hinder communication and risk making data obsolete.
Systematized Nomenclature of Dentistry
Systematized nomenclature of dentistry (SNODENT) is an ADA-sponsored, comprehensive set of standardized terms for defining dental disease in an electronic environment. SNODENT is part of a larger code set called systematized nomenclature of medicine (SNOMED),86 which was developed by the College of American Pathologists. The codes allow dentists to document a wide range of conditions and risk factors using standard terms to aid communication among dental and medical clinicians. In addition, SNODENT allows dentists and researchers to better assess the long-term benefits of certain treatment protocols by standardizing the measurement of outcomes and the documentation of evidence-based care.65
Internet
The Internet offers current and prospective patients and referrers an opportunity to learn about the office at their convenience. The Web has consistently proved itself a cost-effective communication and marketing tool in dentistry (Fig. 28-22). The right content mix, one that is unique and well targeted to the needs of prospective and current patients, can improve both the image of the practice and patient satisfaction.
Getting started on a website can be a daunting task, because the possibilities are virtually limitless. The following steps can help the beginner get started:
1.
The best way to begin is to visit other medical and dental providers’ websites. The clinician should learn how to navigate the sites and should determine the elements that are required and which high-end graphic effects might prove effective. Simple is better, but patients want to see an esthetically pleasing site, and they want to learn something on each visit.
2.
The clinician should then decide on a set of goals for the site; for example, should the site generate referrals via Internet search engines or serve as a resource for patients and referrers?
3.
A design for the site should then be created. It should project the practice’s image or brand and should fulfill patients and referring clinicians’ needs. All design elements should be consistent with other marketing materials to further the practice’s brand identity.
4.
The next step is to outline the proposed site and create a storyboard that includes navigation possibilities for the audience. Each page is designed on a separate piece of paper, and these ideas are tested with friends and selected prospective users.
5.
A uniform resource locator (URL) must be chosen so that the site address can be easily remembered and entered in a browser with minimal effort and confusion. Again, the URL should tie in to the practice’s desired image.
6.
The blanks on the web pages are then filled in with copy, photographs, and an appealing style that projects the practice’s vision. Copyright laws apply to most material on the Internet; therefore written permission must be obtained before using protected material.
7.
The website must be kept fresh. To draw repeat visitors, it must be updated continually, and all links must be relevant and functional. Some dental Internet vendors allow the clinician to edit the site on an as-needed basis 24 hours a day, 7 days a week, by adding a small applet that allows password-protected entry.
An endodontic office website can contain searchable educational material for study clubs and referrers. Websites can be transformed into a communications center, a scientific reference library, and clinical and business information resource. This can provide fast, convenient access to resources such as MEDLINE, online continuing education courses, product catalogs, practice management information, and pharmacology references.
Many vendors currently provide service for site construction and hosting that include creative patient education modules, maps with customized directions, clinician biographies, and animated procedure descriptions. Some sites also include referral forms that automate attachment of digital radiographs and promote interactive discussions about treatment.
New patients can benefit by submitting forms directly to the practice’s management software via an always-on Internet connection. Clinicians can customize referral forms to provide data fields that require inclusion of certain information for submission, so that patients can provide more complete registration information.
Important Software Features
Financial Security
Although fraud in dental offices is not often discussed, even conservative statistics indicate that it is a significant problem. No absolute solution exists; therefore vigilance is the key. However, the clinician should do at least three things56:
1.
Become educated. Clinicians should find out how people embezzle from a dental office. Sometimes this means taking a course or two, hiring a fraud expert to review office systems, or both.
2.
Pay attention to the business. Too many dental professionals abdicate the function of their front office to trusted “office managers.” This dynamic, in which the owner of the business ignores the business, is ill conceived and invites fraud.
3.
Select software with a security log. The practice should use an office computer system that carefully tracks all deletions, edits, and other potentially suspicious behavior automatically and prevents anyone except the clinician from viewing the security log. In addition, each user is logged on and off the system, so that the software knows when a particular person was on the system; what station the person was using; and which transactions they created, edited, or removed. Most security experts recommend that each financial transaction (i.e., routing slips) be sequentially numbered without the possibility of modification or deletion.
Referral Tracking
Sophisticated referral tracking and trend analysis are crucial to the success of a specialized practice. These capabilities are lacking in software created for the general dentist. Software designed using SQL tracks financial and other statistics associated with referrers in the practice at the moment transactions are posted. Thus the statistics are always current and accurate. Key features of referral tracking include:
1.
Real-time statistics. The software should give the clinician up-to-the-second statistics (without the need to run reports) in several key areas:
•
Production/collections ratio (the collections percentage)
2.
Real-time ranking of all referrers relative to all others in any of the previously mentioned categories.
3.
Sophisticated, flexible reports based on production, collections, procedures, and other factors that can be filtered and sorted.
4.
Generation of correspondence, labels, and envelopes to one referrer or a selection of referrers based on queries.
5.
Availability of referrer data from the patient screen, the schedule, and other key areas so that the clinician can make quick decisions and see the juxtaposition of referrer and other system information.
6.
Charts and graphs on referrer and patient activity associated with referrers.
7.
Tracking of multiple-referrer categories:
•
Referral source (i.e., general dentist, patient, phone book, website, etc.)
•
General dentist (track multiple office locations and group name identity of referring doctor)
•
Dental specialists (i.e., periodontist, oral surgeon, orthodontist, etc.)
8.
Collection of the previously mentioned data by multiple facilities of the referrer. In other words, if the referral source has multiple facilities, the clinician should be able to track statistics for each of those facilities and summarize a consolidated set of numbers for all facilities.
9.
Collection of the previously mentioned data by practice. If the practice uses several referral sources, this feature allows the clinician to assess statistical data by practice.
Preregistration
Using a specialized system, some software can preregister a patient (i.e., the process of recording information for patients referred but not yet seen by the clinician) at almost any level of detail. The major features associated with preregistration are:
1.
The ability to record all pertinent data about a referred patient—including insurance, referral source, and medical conditions—before an appointment is made. Ample notes fields are available for recording comments from both the patient and other clinicians. A direct link to e-mail and home and work phone icons facilitates quick communication. A “welcome letter” and information about the patient’s first appointment can be produced automatically and sent out with a brochure.
2.
An integrated link to the schedule allows the clinician to easily drag and drop the preregistration record into the appointment book, complete with all the relevant information from preregistration.
3.
Automatic correspondence can be sent to the patient after creation of the preregistration record.
4.
An integrated link to the registration module means that the system can automatically create both the patient record and the insurance records without reentering the data. Sophisticated algorithms continually update insurance data based on previous cases submitted.
Reference
Infrastructure and Connectivity
Single Locations: Local Area Networking
LANs allow the sharing of data and network-attached devices to improve workflow efficiency. The simplest form of LAN is the peer-to-peer model. Connected by a hub and simple wiring, two or more computers can network to share resources and data. The drawbacks of this type of system are the limited number of workstations that can be adequately supported and the necessity to restart the entire system if a program fault occurs. Peer-to-peer systems are not recommended. A much more robust solution requires a dedicated server connected with cabling to each workstation via a central hub. The utility of a network cannot be underestimated. For example, a central repository of digital radiographs allows clinical chairside workstations in each operatory to call up all patient images so that a patient does not have to be in the same operatory for each subsequent visit. A server-based LAN has several additional advantages. It provides greater reliability and faster overall speed; it allows individual stations to be rebooted without restarting the entire system; it secludes the server in a safe location; and it supports a large number of workstations at one or multiple sites. Addition of enterprise-level virus, Trojan, and worm protection is another benefit of the server. With this feature, the server can go online daily to automatically download the latest virus definitions from the manufacturer and allow client machines to self-update as preset by the clinician.
Multiple Locations: Wide Area Networking
The efficiency of the client/server model also allows practices with multiple facilities to set up high-speed communications between those locations, keeping the database on a single server. Maintaining a single database at one location means that updates to patient and billing data are instantly visible practice-wide, reducing errors and consequent liability. But maintaining a single database also requires high-speed access to that data from all practice and remote (e.g., laptop) locations.
The features, power, and complexity of today’s software solutions have forever retired dial-up modem banks as a remote-access option. High-speed access is no longer an option, but a requirement. Interconnected offices have access to various options when it comes to high-speed wide-area connectivity. Typically, there is a trade-off between speed, cost, and reliability. For example, a T1 circuit, which is available in “point-to-point” format or as a conduit to the Ethernet, has moderate speed, is generally highly reliable, and is reasonably expensive. Lower-cost options such as DSL or broadband (cable, FIOS), often targeted more at consumers, offer higher speed but often with less reliability than their more-expensive counterparts. Keep in mind that offices in remote or rural locations will have fewer connectivity options than offices in cosmopolitan, higher-tech areas.
Virtual Private Networks
As part of an office’s connectivity package, Internet access is now effectively a requirement. Leveraging the Internet as a communication medium makes data security concerns imperative. This is easily accomplished by implementing firewalls at each internet-connected office location and deploying industry-standard, affordable Virtual Private Networks (VPNs)48 between these locations (see Fig. 28-23).
VPNs use the Internet as their long-distance backbone, leveraging TCIP/IP 60 internet protocols to effect communication. Essentially, the process looks like this:
1.
Each office obtains local internet service, connecting it to an Internet service provider (ISP). A VPN is configured at each office’s firewall to encrypt data going to other offices.
2.
The ISP passes the signal through the Internet, occasionally through another ISP, to the second office. VPNs are private because the signal that passes through the very public Internet is encrypted to prevent others from intercepting and reading the traffic. VPN solutions are often packages with Internet routers or firewalls.
Citrix and Windows Terminal Server
Just a few years ago, all networking was wide area, combining mainframe-like servers at one location with remote dumb terminals at other locations using the UNIX platform. The difference between these systems and the current technology is that the old networks are just receiving and transmitting stations and are capable only of displaying text. The advantage of these systems is that they are highly efficient. Because only one central computer is involved, no data moves through the network; only screens and key clicks move between server and terminal. These systems require only low-speed, inexpensive data lines. In addition, UNIX is and always was designed to run high-performance WANs. Even today, almost all Internet servers run on a UNIX platform.
By comparison, Windows-based networks are highly inefficient. Because everything in Windows is an image, all workstations are computers; real data move across the network, and higher-performance communications lines are required to carry the signals. Citrix (Citrix Systems, Ft. Lauderdale, FL), has provided the closest approximation (in the Windows world) of the mainframe model of computing. Citrix software (e.g., Xen Server, Xen App, Xen Desktop) offers leading solutions to maintain all data and programs on a single server. In other words, the client workstations (PCs in most cases) are not running any software; they are simply sending and receiving Windows screens and transmitting keyboard and mouse activity. Because a much smaller amount of data is moving around the network, Citrix systems can perform well with much lower-speed communication lines. Microsoft’s Windows server platforms (e.g., Windows 2003 Server, Windows 2008 Server) also offer remote “terminal servers” capability.
No matter which WAN model the clinician chooses, the client/server system is recommended because only a very small amount of real data travels on the network. This is vastly different from other dental software systems, which transmit data to the workstation for change and then transmit the data back for storage. In these non–client/server systems, the server is simply a passive storage system. Client/server systems feature a dynamic, active server that controls access. This can be likened to a busy intersection. A client/server system has “traffic lights” and “police officers” (i.e., the SQL database engine) which control access. No such controls exist in a non–client/server system. Each car (i.e., workstation) entering the intersection makes its own decisions as to when to stop and when to go. As a result, “collisions” and “accidents” (i.e., corrupted data) are more common.
Fat- and Thin-Client Computing and the Internet
Software written for PCs and Windows often is referred to as a fat-client model. This unattractive label signifies that software written for the PC must be installed and run separately from each client computer; only the database is centralized. Each fat-client must be a powerful PC with the software individually installed. Because data must travel to and from the client, the bandwidth of the communications channel must be significant. Bandwidth is a term used to specify the speed of a communications channel. For example, a high-speed cable connection offers wide bandwidth because it can transmit 5 megabits of data per second; a T1 connection transmits at 1.544 megabits per second. A 56k modem connection is narrow bandwidth because it can only transmit at speeds up to 56 kilobits per second. A cellular broadband connection may offer 768 kilobits per second. Specialists in communications often refer to bandwidth as “the size of the pipe,” with fat pipes being higher speed than small pipes.
Another disadvantage of the fat-client model is the cost of maintaining it. Imagine for a moment that you worked in a large law office with 200 desktop computers, all running the same software. If the company making the law office’s software released an update, the practice would have to install the update separately on each workstation. In addition, each of those 200 workstations would have to be powerful PCs, which produces its own maintenance headaches.
The thin-client model85 is much simpler. This is not a new model; UNIX networks have always been thin, and most mainframe networks are thin. In fact, the fat-client model is a product of the PC age. The Internet, the ultimate thin-client network, has become so pervasive that thin-client computing has again become the preferred model. Within the next few years, developers of software for endodontists probably will reengineer their software and hardware to run on the Internet as a thin-client solution, with imaging, charting, and patient demographic data stored and archived remotely, and running on a simple Internet browser (e.g., Internet Explorer or Firefox).
The Internet represents a great deal more than just a different place to run office software. Remarkable innovations available now to clinicians include (to name just a few):
•
Automated preregistration over the Internet. Several vendors provide online patient registration forms (
Fig. 28-24, A), which can securely transfer information over the Internet directly into an endodontic software database (see
Fig. 28-24, B).
•
Multiprovider networks. Multiprovider networks allow clinicians to send patient records and images to colleagues in a secure area on the Internet.
•
Online scheduling. Patients can have limited use of the schedule online, 24 hours a day, 7 days a week. For example, patients can enter their name and appointment date, and the website will allow cancellation of the appointment and selection of preferences for a new appointment (i.e., specific days of the week and time of day).
•
Online payments. Patients can pay their bills online.
•
Data backup. With this feature, which is offered by numerous vendors, data can be automatically transferred at night to geo-separate servers at different locations.
•
Online ordering. Clinicians can order most supplies over the Internet.
•
Data analysis. In the future, clinicians may provide anonymous data to data banks that will analyze the information and report statistics regarding their practices.
Early PCs and mainframe computers were isolated and therefore limited islands of information storage. Later, networked systems with some sharing of data allowed exchanges within each business entity only. Today, using software protocols such as HTTP and HTML, the Internet has revolutionized interconnectivity between millions of computer networks, allowing cross-platform connectivity. Software is now the chief driver of distributed computing, characterized by technologic advances such as extensible markup language (XML), a system of small applications that can be connected for specific functions to enhance Web services. With XML, information now can travel to and from different systems regardless of hardware and location. The integration across many platforms provides numerous benefits, including better connections among offices, patients, referrers, and vendors. Finding ways to allow patients, referrers, and vendors to conduct exchanges that remain private and secure, however, has been a continuing challenge. Microsoft.NET is the software technology for connecting disparate systems and the watchword for the next generation of software platforms. That said, the IT plan for endodontic offices should include provision for each computer workstation to be connected to the Internet to improve functionality.
Power, Cabling, and Wireless
Power
All computers, especially the server, should be protected from voltage sags, interruptions, and surges in power and should allow for an orderly shut-down and saving of all open files if a power aberration occurs. Although many uninterruptible power supply (UPS) topologies are available for small business applications, the line interactive UPS is especially well suited for servers. In this scheme, the battery to AC power inverter is always on, and the battery is charged when input AC power is normal, and the inverter is operated in reverse. This design provides power filtering and reduced power transients compared with the standby UPS topology recommended for workstations8 (Table 28-3). Because the primary cause of hard drive failure is power spikes and sags, dedicated and properly specified UPS equipment is highly recommended.
The computer and monitor must be plugged into only the surge/battery backup–protected sockets. Laser printers should not be plugged into the battery positions, just the surge suppression sockets, because they draw too much current. Any system that receives telephone service also should be protected from “back door” lightning strikes that can destroy the office’s system and data.
Cabling and Wireless
Wall jacks for power and Ethernet,71 a LAN technology that transmits information between computers at speeds of 1000 Mbps (million bits per second), should be placed near the computer workstations. A double duplex power outlet should be installed at each location, along with a combination wall plate containing an Ethernet and a telephone jack. Internal wiring for the Ethernet should be run with copper unshielded twisted-pair (UTP) Cat 6 wire terminated in RJ 45 blocks. Cabling used inside walls is different from that used in patch cords. Wall cabling is much more susceptible to breakage and therefore should be terminated in a fixed block mounted on the wall (i.e., a wall jack) and not run out of the wall directly to the CPU. The Cat 6 can operate at a bandwidth of 1000 MHz and carry voice and data at rates of up to 1 Gbps.
Wireless networks are becoming more common, but they can be somewhat problematic because of sometimes inconsistent reception. Some wireless capability is necessary if tablet or slate PCs are part of the practice’s computer hardware. Wireless networks must be carefully configured so that security features effectively shield against hacking. Before installation, the clinician should fully understand the advantages and disadvantages of a wireless LAN.
Central Processing Unit
Two kinds of CPUs are commonly used in dental offices: the standard desktop, or minitower, and the laptop. CPUs designed for businesses, such as Dell’s OptiPlex line (Dell, Austin, TX), are network-optimized for improved manageability and reliability. These units also support multiple monitor configurations, which increases available “desktop” space for displaying multiple application windows to improve productivity.
Desktop CPUs can be used in almost any area or for almost any task, and the clinician should choose one of the fastest processors available. It should have enough random access memory (RAM) to allow several programs to be run at once and should include at least two internal expansion slots and one drive bay for additional peripherals. As a general rule, a faster processor adds to a machine’s useful life, and upgrading the system’s RAM to at least one level more than required to run the computer’s operating system (OS) is advisable. Increasing RAM to at least 4 GB (gigabytes) improves speed for today’s graphic-intensive software. Savings are often available on RAM, and it is well worth the additional investment.
Software applications, the OS, and the data created by the office are stored on the hard drive. As hard drive capacity increases and the price per megabyte declines, it becomes easier to choose a large hard drive that is adequate for most purposes. Because data are stored on the server in the CIS, the office generally does not need to buy individual workstation CPUs with ultralarge-capacity hard drives.
Monitors
The monitor’s size and image quality are critical to image resolution. Clinicians should invest in the highest quality unit they can afford. In all likelihood, the monitor will last well past any single CPU. LCDs are free from geometric image distortions, flicker, and screen brightness variations, which may reduce the incidence of Computer Vision syndrome (eyestrain, headaches, etc.).
LCD screens require little in the way of maintenance. The clinician should make sure that all equipment in clinical areas is protected from cross-contamination with disposable barrier techniques, if applicable, and that manufacturer’s recommendations are followed regarding ventilation, electrical and shock hazards (all clinical equipment should be powered through hospital-grade electrical connections), and cleaning. Many vendors make cleaning solutions, wipes, and cloths specifically for LCD computer screens.
LCD Screens
The gold standard for administrative, front desk, and imaging applications in the operatory are LCD20 screens with high-resolution characteristics. All flat screens are not created equal. The following tips can aid the clinician in selecting a screen:
1.
The screen should have the Video Electronics Standards Association’s (VESA) mounting hole pattern on the back so that it can be attached to an industry-standard mounting arm. This mounting hole pattern is square and measures 3 × 3 inches (75 × 75 mm) or 4 × 4 inches (100 × 100 mm).
2.
LCD monitors are measured by the size of the viewable area. A flat panel screen of 20 to 24 inches is recommended. Most screens list horizontal and vertical viewing angles of at least 140 degrees. The ideal horizontal and vertical viewing angle is 160 degrees or more.
3.
LCD is a transmissive technology. A fixed-intensity fluorescent or light-emitting diode (LED) backlight is filtered by the liquid crystals arranged between two finely grooved surfaces. These new LEDs produce greater dynamic contrast, are thinner, consume 40% less power, have a wider color gamut, but cost more than fluorescents at this time. Organic light-emitting diodes (OLED), another new monitor technology, are composed of a film of organic compounds, are the thinnest technology, and do not require a backlight to function, providing deep black levels. The screen purchased should have a 3-year warranty on the backlight. Most LCD fluorescent screens last for about 60,000 hours (6.8 years) of continuous use.
4.
An LCD panel can display only one resolution at full screen size, because each pixel is hard wired (e.g., a 1280 × 1024 panel has 1,310,720 hard-wired pixels in its native mode). A minimum dot pitch of 0.26 mm is recommended. If an LCD panel has a native resolution of 1280 × 1024 pixels, it can display at a resolution of 640 × 480 by using less of the screen area. Most LCD screens can rescale a lower-resolution image using rathiomatic expansion, which works adequately for photographs but not very well for text or images with fine detail. Objects become jagged, and artifacts fill the extra pixels. When resampling is done for scaling the image up, antialiasing fills the extra pixels, resulting in better results. For the clinician, the bottom line is to choose a screen with a clear understanding of the native resolution and plan to use it as specified.
5.
Only LCD monitors that support digital (binary pulse) signal inputs (i.e., DVI) should be purchased for general office use. Because LCD screens process information digitally, fluttering and ghosting can result if digital information from the computer must be sent to the video card, converted to analog, sent on to the LCD screen, and then converted back into a digital signal. Currently, LCD units that include both analog video and digital inputs such as high definition multimedia interface (HDMI), digital visual interface–digital (DVI-D) with high definition content protection (HDCP), DisplayPort, video graphics array (VGA), component video, S-video, and composite video are recommended for certain applications.
6.
The refresh rate (i.e., how quickly the screen paints the image) is an important indicator of how well the screen will depict moving images. A refresh rate of 6 msec is a minimum standard.
7.
Special attention should be paid to contrast ratios, to ensure that the screen depicts a large range of light and dark tones. A contrast ratio of at least 80,000:1 should help paint an image with excellent appearance quality.
8.
Integral stereo speakers are a nice feature on any monitor. Although most speakers do not take up much room, built-in speakers reduce clutter and make the computer system easier to move.
Printers
Dental offices strive to run compliant, cost-effective operations that minimize cost and maximize productivity. Printers are available in a dizzying array of formats and output types; therefore careful selection for each use is recommended. Although increasingly popular multifunction products (MFP) promise “significant advances in the areas of document distribution and management, security, wired and wireless connectivity, and color,”45 most dental offices use single-function machines. Because most MFP devices use proprietary software drivers, the prospective buyer must make sure that the machines are compatible with all the software used in the office. Selection of the right printers is crucial to the usefulness of the entire computer system.
Monochrome and Color Laser Printers
The front desk, administrative, and clinician’s office computers should be linked to a monochrome or color laser printer for printing of patient instructions, insurance materials, receipts, and general word processing tasks. Clinicians who follow the frontdesklessness concept should consider a multidrawer printer model so that stationery, plain paper, and envelopes are all preloaded. For example, EndoVision software (Henry Schein, Inc., Melville, NY) allows the clinician to use a “rapid post” module to select tasks that can be directed to multiple individual and networked printers and specific drawers.
Label Printers
Sterilization area and front desk computers benefit from dedicated label printers for printing chart labels and mailing labels for general mailing duties. Although the use of industry-standard window envelopes can greatly reduce the need for envelope printing, label printers are often a useful adjunct, especially for larger items.
Inkjet Printers
Production of patient treatment reports and radiographs are the primary functions of the inkjet printer. A high-quality printer with individual archival inks that use a variety of paper formats can produce stunning reports that can improve communication with co-therapists. Epson’s (Epson America Inc, Long Beach, CA) new pigment-based inks with resin-coated 0.1-µm particle size and long-lasting permanence ratings are the gold standard for professional image printing.
Document Scanners
Scanning of documents improves dental processes by increasing security and efficiency and reducing storage space. Scanners can transmit documents in a variety of formats, so careful attention should be given to compatibility with dental management software. Documents should be scanned into a patient’s individual file so that all the documents for that particular patient are easily accessible. Accounting and other miscellaneous office documents can be scanned into a file on the server or client workstation for easy retrieval. Recommended scanners include native support for Adobe portable document format (PDF). The PDF file format has become the document exchange standard because of its wide industry acceptance. PDF files can be read independently from other application software and can be viewed as thumbnails in Microsoft Office application software; each document can be password protected.
Portable Document Format
Unlike TIFF and JPEG image formats, PDF encapsulates other compression formats so that documents become application independent. These files have embedded metadata, or data within the image, that can authenticate the document. As an open specification, PDF also maintains documents in a consistent format, which makes it the best choice for long-term archiving and for preserving the original appearance.
Security
PDF files improve security through digital signatures and document encryption features that improve HIPAA compliance and address general business security demands. All PDF files can be password protected to limit access to only those authorized to view the contents.
Versatility
PDF files can be viewed on every major computing platform, including Microsoft Windows, Mac OS, and UNIX.
Searchable Images
PDF creates image files that can be searched and indexed by optical character recognition (OCR). Processing a document with OCR produces a searchable bitmap that is hidden behind the image while preserving the look of the original image.
Input Devices
With pointing devices and keyboards, location and ease of use should be considered along with infection control. In the operatory, clinicians should choose wireless keyboards and optical mice that can be protected by barriers to eliminate cross-contamination. Logitech manufactures a wide range of wireless input devices, including Bluetooth models with wireless hub/battery charger, keyboard, and rechargeable mouse that allows a range of up to 30 feet (9 m) using the 2.4 GHz ISM band. Care must be taken with the addition of any radio frequency (RF) wireless devices to guard against interference with other wireless equipment, such as the wireless radiographic sensors, tablet and slate computers, and wireless telephones.
Graphic tablets are also useful adjuncts that allow annotation of drawings in the patient’s chart. Graphic tablets can be purchased in several sizes and usually require a USB interface. The pen, or stylus, can be wired or wireless, although batteries add to the weight of the pen. Another solution to graphic input, albeit a more expensive one, is a wireless tablet PC, which has all of the functionality of a PC with wireless RF capability and true tablet functionality. These devices can operate as a laptop and, with “digital ink” technology, can input hand-written notes and graphics into any enabled application.
Consulting and Support
IT systems require thorough planning and careful implementation to ensure trouble-free installation. Clinicians should begin planning with local vendors in close cooperation with the practice management vendor. Because technology changes constantly, clinicians need someone who can update the system’s hardware and software, upload “patches” and “firmware updates,” and generally be available for help with equipment purchase decisions. These vendors usually work on an hourly basis and may offer blocks of time per month or per quarter at discounted rates and guaranteed response times.
Pharmacology Reference Software
Many programs are available that can serve as clinical pharmacology references. As mentioned previously, Lexi-Comp Online is a Web-enabled or installable product that features extensive indexing, cross-referencing, and linking of drugs for optimum quick search functions. For example, the clinician simply types in the name of the drug, and the program calls up every reference to it in the compendium. The search can be done by alphabetic listings, a main index of drug classifications, product identification (by description of the drug), adverse reactions, disease description, drug interactions, and other parameters. This product contains clinically oriented monographs on all drugs used in the United States and allows for quick, accurate identification of drug interactions and contraindications. The program also promotes a quick search of dental and dental vasoconstrictor implications for each drug listed.
Patient Education Software
Patient education is an important part of modern dental practice. One study14 found a positive statistical correlation between patient education and their endodontic treatment experience. To this end, several vendors have created informational software programs for the Web and local computer use. The patient can access these programs on the Internet, at a computer kiosk in the reception area, or at the clinical chairside workstation.
Health Insurance Portability and Accountability Act
Confusion about transmission of protected health information by electronic means has created the myth that clinicians cannot communicate by e-mail or the Internet. The U.S. Department of Health and Human Services has stated16:
The Privacy Rule allows covered health care providers to share protected health information for treatment purposes without patient authorization, as long as they use reasonable safeguards when doing so. These treatment communications may occur orally or in writing, by phone, fax, e-mail, or otherwise.
Summary
Creation of the EOHR is the next logical step in the journey to the paperless office. Integration of this information with an EHR to create a unified patient database that documents the current health status and lifetime medical history for each patient is the pot of gold at the end of the rainbow. As the functionality of digital systems improves, every dental care delivery organization should consider incorporating at least some of these advances. However, technology is not a substitute for treatment excellence, and clinicians must continue to strive to provide quality treatment for patients regardless of the equipment they use.
Acknowledgments
Mr. Brendan Sheehan, Mr. Guy Wassertzug, Mr. Joshua R. Walty, Dr. Robert Lapp, Dr. Allan Farman, Dr. Bruce Lieberthal, Mr. Jay Levine, Dr. David Gain, Mr. David Taylor, Dr. John Goyette, Dr. Mark Diehl, and Mr. Paul Bralower for their invaluable help with IT systems, digital imaging, and dental informatics. Also, Mr. Bruce Dale and Mrs. Katherine Levin Sheehan for their exceptional photographic skills and Mrs. Deborah Lebbin and Mrs. Susan Levin for their editorial help.
Disclaimer
Dr. Levin receives honoraria or equipment or has a financial relationship with the following vendors mentioned in the text: Atlantic Design, LLC; PracticeWorks, LLC; and Henry Schein, Inc.
References
1. A holistic approach to security intelligence: VerisSign i-defense threat intelligence services. http://www.verisign.com/static/037640.pdf, 2009. Accessed Aug 4
2. American Dental Association. Computer-based oral health record: concept model. Benchmark model 1.0 ed. Chicago, IL: American Dental Association; 1996.
3. American Dental Association moves forward on electronic standards. ADA News. 30(15), Aug, 1999.
4. American National Standards Institute and American Dental Association. Specification 1000: standard clinical data architecture for the structure and content of an electronic health record. New York: American National Standards Institute; 2001.
5. ADA Council on Scientific Affairs. An update on radiographic practices: information and recommendations. J Am Dent Assoc. 2001;132:234-238.
6. Adobe Systems, Inc. TIFF, Revision 6 partners.adobe.com/public/developer/en/tiff/TIFF6.pdf, 2009. Accessed Jul 26
7. American Optometric Association. The relationship of computer vision syndrome to musculoskeletal disorders. www.aoa.org/x5378.xml, 2009. Accessed Jul 26
8. APC Corp. White paper: the different types of UPS systems. m.softchoice.com/files/pdf/brands/apc/The%20Different%20Types%20of%20UPS%20Systems.pdf, 2009. Accessed July 26
9. Bahcall J, Barrs J. Fiber optic endoscope usage for intracanal visualization. J Endod. 2001;27:128.
10. Bahcall J, Barrs J. Orascopic visualization technique for conventional and surgical endodontics. Int Endod J. 2003;36:441.
11. Berkhout WE, Beuger DA, Sanderink GC, van der Stelt PF. The dynamic range of digital radiographic systems: dose reduction or risk of overexposure? Dentomaxillofac Radiol. 2004;33:1-5.
12. Black M, Castillo D. Backup exec 9 for Windows servers. Sudbury, MA: Jones and Bartlett Publishers; 2004.
13. Burger CL, Mork TO, Hutter JW, Nicoll B. Direct digital radiography versus conventional radiography for estimation of canal length in curved canals. J Endod. 1999;25:260.
14. Chandler L, Silversin J. What do patients think of you? Building relationships. Chicago: American Association of Endodontists; 1994. (videotape)
15. Cotti E, Vargui P, Dettori C, Mallarini G. Computerized tomography in the management and follow up of extensive periapical lesions. Endod Dent Traumatol. 1999;15:186-189.
16. Department of Health and Human Services. Does the HIPAA Privacy Rule permit a doctor, laboratory, or other health care provider to share patient health information for treatment purposes by fax, e-mail, or over the phone? www.hhs.gov/hipaafaq/providers/smaller/482.html, 2009. Accessed Jul 26
17. DICOM. Digital imaging and communications in medicine (DICOM) Part 1: introduction and overview. ftp://medical.nema.org/medical/dicom/2008/08_01pu.pdf, 2009. Accessed Jul 26
18. Digital imaging and communication in medicine (DICOM), Supplement 92: media application profile for digital radiographic images in dentistry. ftp://medical.nema.org/medical/dicom/final/sup92_ft.pdf, 2009. Accessed Jul 26
19. Diehl M: Personal communication, August 22, 2004.
20. Displaysearch: LCD monitor review: Dell 1900FP. displaysearch.com. Accessed Jul 26, 2009
21. Deleted in pages.
22. Eikenberg S, Vandre R. Comparison of digital dental x-ray systems with self-developing film and manual processing for endodontic file length comparison. J Endod. 1999;26:65.
23. Eisner J, Chasteen J, Schleyer T, et al. The computer-based oral health record. Chicago: American Fund for Dental Health; 1993.
24. Farman AG, Levato CM, Gane D, Scarfe WC. How going digital will affect the dental office. J Am Dent Assoc. 2008;139(Suppl):14S-19S.
25. Farman AG, Lapp RE. Image file interoperability for data protection, communication and trans-system connectivity. Orthop Craniofac Res Suppl. 2003;1:151.
26. Farman AG. A primer on digital x-ray imaging for dentistry. SADJ. 2003;58:78.
27. Farman AG. Fundamentals of image acquisition and processing in the digital era. Orthod Craniofac Res. 2003;1(6 suppl):17.
28. Farman AG: Personal communication, August 20, 2004.
29. Farman AG, Horsley B, Warr E, et al. Outcomes of digital x-ray mini-panel examinations for patients having mental retardation and developmental disability. Dentomaxillofac Radiol. 2003;32:15-20.
30. Farman TT, Farman AG. Evaluation of a new F speed dental x-ray film. The effect of processing solutions and a comparison with D and E speed films. Dentomaxillofac Radiol. 2000;1:41.
31. Farman TT, Vandre RH, Pajak JC, Miller SR, Lempicki A, Farman AG. Effects of scintillator on the detective quantum efficiency (DQE) of a digital imaging system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:219-223.
32. Fleder RM, Silverman LK. Learning and teaching styles in engineering education. Eng Educ. 1988;78:674-681.
33. Foroughi K, Mastromihalis N, Goren A, Bruder G, Button T, Moore W, et al. Comparison of radiation exposure rates necessary to produce computerized images and conventional radiographs. J Endod. 1999;25:305. (abstract)
34. Forrey AW, Heid DW, Chasteen JE, et al. TEPR95 Proceedings. Newton, MA: Medical Record Institute; 1995.
35. Fossum E. CMOS evolution: the digital camera-on-a-chip gets active. Adv Imaging. 1997;12:13.
36. Fronckowiak JW. OLE and ADO. Indianapolis, IN: Sams Publishing; 1991.
37. Fuhrmann R, Bucker A, Diedrich P. Radiological assessment of artificial bone defects in the floor of the maxillary sinus. Dentomaxillofac Radiol. 1997;26:112-116.
38. Gakenheimer DC. The efficacy of a computerized caries detector in intraoral digital radiography. J Am Dent Assoc. 2002;133:883.
39. Gibs SJ. ADA Council on Dental Materials, Instruments and Equipment: Biological effects of radiation from dental radiographs. J Am Dent Assoc. 1982;105:275-281.
40. Granfors P, Aufrichtig R: DQE(f) of an amorphous silicon flat panel x-ray detector: detector parameter influences and measurement methodology. Proceedings of the International Society of Optical Engineering (SPIE) 2000, Conference on the Physics of Medical Imaging 3977: February 13–15, 2000, San Diego, CA, (abstract).
41. Guttenberg SA. Oral and maxillofacial pathology in three dimensions. Dent Clin North Am. 2008;52:843-873.
42. Hedge A. Ergonomics considerations of LCD versus CRT Displays. ergo.human.cornell.edu/Pub/LCD_vs_CRT_AH.pdf, 2009. Accessed Jul 26
43. Heid DW, Chasteen J, Forrey AW. The electronic oral health record. J Contemp Dent Pract. 2003;3:43.
44. Herman Miller, Inc. White paper: It’s a matter of balance. http://www.hermanmiller.com/MarketFacingTech/hmc/research_summaries/pdfs/wp_Matter_of_Balance.pdf, 2009. Accessed Jul 26
45. Hewlett-Packard Development Co. White paper: assessing the imaging and printing environment. www.homeofthesmartpeople.com/Assessing-Your-Print-Environment.pdf, 2009. Accessed Jul 26
46. Hippisley-Cox J, Pringle M, Cater R, Wynn A, Hammersley V, Coupland C, et al. The electronic patient record in primary care—regression or progression? A cross sectional study Nottingham University, Nottingham, GB. Br Med J. 2003;326:1439-1443.
47. Hujoel PP, Bollen AM, Noonan CJ, del Aguila MA. Antepartum dental radiography and infant low birth weight. JAMA. 2004;291:1987.
48. IBM. White paper: IBM WebSphere Everyplace. ftp://ftp.software.ibm.com/software/pervasive/info/products/wes.pdf, 2009. Accessed Jul 26
49. Jones D. The Definitive Guide to Windows Application and Server Backup 2.0. nexus.realtimepublishers.com/dgwasb.php, 2009. Accessed Jul 26
50. Kang BC, Farman AG, Scarfe WC, Goldsmith LJ. Observer differentiation of enamel mechanical defects vs natural proximal dental caries with computed dental radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:459.
51. Kitagawa H, Farman AG. Effect of beam energy and filtration on the signal-to-noise ratio of the Dexis intraoral x-ray detector. Dentomaxillofac Radiol. 2004;33:21.
52. Kump KS, Omernick J: Assessment of image quality among multiple output devices using digital x-ray radiographs (abstract #832). Presented at the Radiological Society of North America (RSNA) 2000 Conference, Chicago, IL, November 26-December 1, 2000.
53. Langland OE, Langlais RP, Preece JW. Principles of dental imaging, ed 2. Philadelphia: Lippincott Williams & Wilkins; 2002.
54. Lehmann TM, Kaser A, Repges R. A simple parametric equation for pseudocoloring grey scale images keeping their original brightness progression. Image Vis Comput. 1997;15:251.
55. Lehmann TM, Troeltsch E, Spitzer K. Image processing and enhancement provided by commercial dental software programs. Dentomaxillofac Radiol. 2002;31:264.
56. Lewis DP. Employee embezzlement and fraud in the dental office. Hudson, OH: Lexi-Comp; 2000.
57. Levato C. Advancing the state of the art. Dent Pract Finance. 7(8), 1999.
58. Lieberthal, B: Personal communication, July 13, 2005.
59. Lofthag-Hansen S, Huumonen S, Grondahl HG, Grondahl K. Limited cone-beam CT and intraoral radiograpahy for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2003;103:114-119.
60. Loshin P. TCP/IP, ed 2. San Diego: AP Professional; 1997.
61. Low KMT, Dula K, Burgin W, von Arx T. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J Endod. 2008;34:557-562.
62. Ludlow JB. Dosimetry of Kodak 9000 3D, personal communication 7-16-2008.
63. Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64 row CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:930-938.
64. Matteson SR, Joseph LP, Bottomley W, et al. The report of the panel to develop radiographic selection criteria for dental patients. Gen Dent. 1991;39:264-270.
65. McKee L. SNODENT to provide inclusive means of transmitting dental information. ADA News. 1999;30:1.
66. Miles D. The “Electronic imaging chain” [and] its effect on your digital radiographic images. learndigital.net/articles/2003/electronic_imaging.htm, 2009. Accessed Jan 26
67. Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261-1266.
68. Mistak EJ, Loushine RJ, Primack PD, West LA, Runyan DA. Interpretation of periapical lesions comparing conventional, direct, and telephonically transmitted radiographic images. J Endod. 1998;24:262.
68a. Mol A. Image processing tools for dental application. Dent Clin North Am. 2000;44:299-318.
68b. National Council on Radiation Protection and Measurements (NCRP) Radiation protection in dentistry, Report #145, Bethesda, MD http://www.ncrponline.org/publications/145press.html, 2003
69. National Electric Manufacturers Association (NEMA). PS 3.1–2004 digital imaging and communications in medicine (DICOM) Part 1: introduction and overview. nema.org/standards, 2009. Accessed Jan 26
70. National Institutes of Health http://rsb.info.nih.gov/nih-image/manual/intro.htm/#ove, 2010 Accessed Jan 26
71. Nemzow M. Fast ethernet: implementation and migration solutions. New York: McGraw-Hill; 1997.
72. Nummikoski PV, Martinez TS, Mattesib SR, McDavid WD, Dove SB. Digital subtraction radiography in artificial recurrent caries detection. Dentomaxillofac Radiol. 1992;21:59.
73. Ohio Department of Health. Regulatory guide for dental x-ray equipment. odh.ohio.gov/ASSETS/38BC87DB0C2E42CEBB4508EB21FC5D07/DentalRegulatoryGuide2004-08.pdf, 2009. Accessed Jul 26
73a. Parks ET, Williamson GF. Digital radiography: an overview. J Contemp Dent Prac. 2002;3:23-29.
74. Paurazas SB, Geist JR, Hoen MP, Pink FE, Steiman HR. Comparison of diagnostic accuracy of digital imaging and E-speed film in the detection of periapical bone lesions. J Endod. 1999;25:285. (abstract)
75. Radiological Society of North America (RSNA). DICOM: the value and importance of an imaging standard. www.rsna.org/Technology/DICOM/index.cfm, 2009. Accessed Jan 26
76. Razmus TF, Williamson GF. Current oral and maxillofacial imaging. Philadelphia: Saunders; 1996.
77. Sanderink GC, Miles DA. Intraoral detectors: CCD, CMOS, TFT, and other devices. Dent Clin North Am. 2000;44:249.
78. Schick D. Alteration of computer dental radiography images. J Endod. 1999;25:475. (letter to the editor)
79. Schleyer T, Spallek H. Dental informatics: a cornerstone of dental practice. J Am Dent Assoc. 2001;132:605.
80. Schleyer T TEPR95 Proceedings 1995 Medical Records Institute Newton, MA
81. Schleyer T. Why integration is key for dental office technology. J Am Dent Assoc. 2004;135:4S.
82. SCSI Trade Association (STA). White paper: explaining hard drive differences. www.scsita.org/aboutscsi/sas/318524.pdf, 2009. Accessed Jul 26
83. Seltzer J, Colosi DC, Bonvento M, et al: Evaluation of the Tru-Align PID using optically stimulated luminescence dosimetry, American Academy of Oral and Maxillofacial Radiology (AAOMR) 59th Annual Session Program; Oct. 28-Nov. 1, Pittsburgh, PA, 2008.
84. Simon JH, Enciso R, Malfaz JM, Roges R, Bailey-Perry M, Patel A. Differential diagnosis of large periapical lesions using cone-beam computed tomography measurements and biopsy. J Endod. 2006;32:833-837.
85. Sinclair JT, Merkow M. Thin clients. New York: Academic Press; 2000.
86. SNOMED clinical terms www.nlm.nih.gov/research/umls/Snomed/snomed_main.html, 2009 Accessed Jul 26
87. Somers TM, Mauriello SM, Ludlow JB, et al. Pre-clinical performance comparing film and CCD-based systems. J Dent Hyg. 2002;76:26-33.
88. State of Maryland. Regulatory guidelines for dental radiation machines. May 2002 www.mde.state.md.us/assets/document/air/dental_rad.pdf, 2009. Accessed Feb 15
89. Stratemann SA, Huang JC, Maki K, Miller AJ, Hatcher DC. Comparison of cone beam computed tomography imaging with physical measures. Dentomaxillofac Radiol. 2008;37:80-93.
90. Symantec. White paper: integrated security: creating the secure enterprise, Symantec enterprise security. security.hoffmanmarcom.com/docs/integrated_security.pdf, 2009. Accessed Jan 26
91. Syriopoulos K, Sanderink GC, Velders XL, van der Stelt PF. Radiographic detection of approximal caries: a comparison of dental films and digital imaging systems. Dentomaxillofac Radiol. 2000;29:312.
92. Taubman DS, Marcellin MW. JPEG 2000: image compression fundamentals, standards and practice. Kluwer International Series in Engineering and Computer Science. 2001:642. Secs
93. Technology and Health. Compaq to put warnings on keyboards about risk of repetitive-stress injuries. Wall Street Journal. February 1995:B6.
94. The TWAIN Working Group. Accessed Jul 26, at http://twain.org, 2009.
95. USB Implementers Forum. An introduction to hi-speed USB. White paper: at http://www.usb.org/developers/usb20/developers/whitepapers/usb_20g.pdf, 2009. Accessed Jan 26
96. van der Stelt. Filmless imaging: The uses of digital radiography in dental practice. J Am Dent Assoc. 2005;136:1379-1387.
96a. van der Stelt PF. Principles of digital imaging. Dent Clin North Am. 2000;44:237-248.
97. Vandre RH, Webber RL. Future trends in dental radiology. Oral Surg Oral Med Oral Pathol. 1995;80:471.
98. Versteeg CH, Sanderink GC, van Ginkel FC, van der Stelt PF. An evaluation of periapical radiography with a charge-coupled device. Dentomaxillofac Radiol. 1998;27:97-101.
99. Versteeg CH, Sanderink GC, van der Stelt PF. Efficacy of digital intra-oral radiography in clinical dentistry. J Dent. 1997;25:215-224.
100. Visser H, Kruger W. Can dentists recognize manipulated digital radiographs? Dentomaxillofac Radiol. 1997;26:67.
101. Wenzel A. Digital radiography and caries diagnosis. Dentomaxillofac Radiol. 1998;27:3.
102. Worden DJ. Sybase developers handbook. San Diego: Academic Press; 2001.
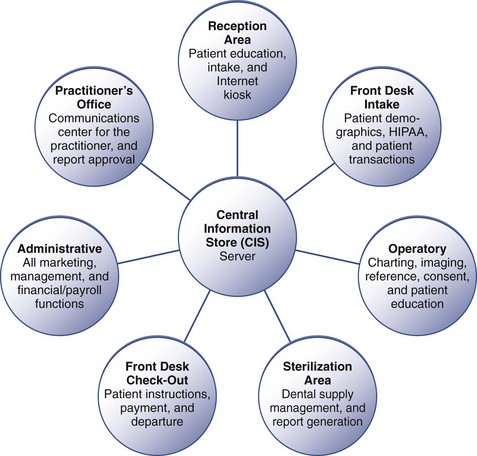

 inches (41 to 52 cm) above the floor. The seat should have a “waterfall” or gradually curved contour just behind the user’s knee and the underside of the thigh to prevent excessive pressure in this area. A seat back rest and lumbar support should also be provided.
inches (41 to 52 cm) above the floor. The seat should have a “waterfall” or gradually curved contour just behind the user’s knee and the underside of the thigh to prevent excessive pressure in this area. A seat back rest and lumbar support should also be provided.