Sexually Transmitted and Other Infections
• Describe prevention of sexually transmitted infections in women, including risk reduction measures.
• Differentiate signs, symptoms, diagnosis, and management of nonpregnant and pregnant women with sexually transmitted bacterial infections.
• Examine the care of nonpregnant and pregnant women with selected sexually transmitted viral infections (human immunodeficiency virus [HIV]; hepatitis A, B, and C; human papillomavirus).
• Compare and contrast signs, symptoms, and management of selected vaginal infections in nonpregnant and pregnant women.
• Discuss the effect of group B streptococci (GBS) on pregnancy and management of pregnant clients with GBS.
• Identify the effects of TORCH infections on pregnancy and the fetus.
• Describe the health consequences (e.g., ectopic pregnancy, infertility) for women who are infected with reproductive tract infections.
• Review principles of infection control for HIV and blood-borne pathogens.
Reproductive tract infection is a term that encompasses both sexually transmitted infections and other common genital tract infections (Marrazzo, Guest, & Cates, 2007). Sexually transmitted diseases (STDs), or sexually transmitted infections (STIs), include more than 25 organisms that cause infections or infectious disease syndromes primarily transmitted by close, intimate contact (Box 7-1). These terms, used interchangeably in this text, have replaced the older designation, venereal disease, which described primarily gonorrhea and syphilis. Caused by a wide spectrum of bacteria, viruses, protozoa, and ectoparasites (organisms that live on the outside of the body, such as a louse), STIs are a direct cause of tremendous human suffering, place heavy demands on health care services, and cost society hundreds of millions of dollars to treat. Despite the U.S. Surgeon General’s targeting STIs as a priority for prevention and control efforts, STIs are among the most common health problems in the United States, especially for young people. The Centers for Disease Control and Prevention (CDC) estimate that more than 19 million Americans are infected with STIs every year; almost half of these are between the ages of 15 and 24 (CDC, 2009b). The most common STDs or STIs in women are chlamydia, gonorrhea, human papillomavirus, herpes simplex virus type 2, syphilis, and HIV infection; these are discussed in this chapter. Common vaginal infections are also discussed. Neonatal effects of STIs are discussed in Chapter 35.
Prevention
Preventing infection (primary prevention) is the most effective way of reducing the adverse consequences of STIs for women and for society. With the advent of serious and potentially lethal STIs that are not readily cured or are incurable, primary prevention becomes critical. Prompt diagnosis and treatment of current infections (secondary prevention) also can prevent personal complications and transmission to others.
Preventing the spread of STIs requires that women at risk for transmitting or acquiring infections change their behavior. A critical first step is for the nurse to include questions about a woman’s sexual history, risky sexual behaviors, and drug-related risky behaviors as a part of her assessment (Box 7-2). Techniques that are effective in providing prevention counseling include using open-ended questions, using understandable language, and reassuring the woman that treatment will be provided regardless of consideration such as ability to pay, language spoken, or lifestyle (Marrazzo et al., 2007; Ravin, 2007). Prevention messages should include descriptions of specific actions to be taken to avoid acquiring or transmitting STIs (e.g., refraining from sexual activity when STI-related symptoms are present) and should be individualized for each woman, giving attention to her specific risk factors.
To be motivated to take preventive actions, a woman must believe that acquiring a disease will be serious for her and that she is at risk for infection. However, most individuals tend to underestimate their personal risk of infection in a given situation; thus many women may not perceive themselves as being at risk for contracting an STI. Telling them that they should carry condoms may not be well received. Although levels of awareness of STIs are generally high, widespread misconceptions or specific gaps in knowledge also exist. Therefore nurses have a responsibility to ensure that their clients have accurate, complete knowledge about transmission and symptoms of STIs and behaviors that place them at risk for contracting an infection.
Primary preventive measures are individual activities aimed at deterring infection. Risk-free options include complete abstinence from sexual activities that transmit semen, blood, or other body fluids or that allow skin-to-skin contact (Marrazzo et al., 2007). Alternatively, involvement in a mutually monogamous relationship with an uninfected partner also eliminates risk of contracting STIs. When neither of these options is realistic for a woman, however, the nurse must focus on other, more feasible measures.
Risk Reduction Measures
An essential component of primary prevention is counseling women regarding risk reduction practices, including knowledge of her partner, reduction of the number of partners, low risk sex, avoiding the exchange of body fluids, and vaccination (CDC, Workowski, & Berman, 2006).
No aspect of prevention is more important than knowing one’s partner. Reducing the number of partners and avoiding partners who have had many sexual partners decreases a woman’s chance of contracting an STI. Deciding not to have sexual contact with casual acquaintances also may be helpful. Discussing each new partner’s previous sexual history and exposure to STIs are augment other efforts to reduce risk; however, sexual partners may not always be truthful about their sexual history. Women must be cautioned that practicing risk reduction measures is always advisable, even when partners insist otherwise. Critically important is whether male partners resist or accept wearing condoms. This is crucial when women are not sure about their partners’ history. Women should be cautioned against making decisions about a partner’s sexual and other behaviors based on appearances and unfounded assumptions such as the following (Marrazzo et al., 2007):
• Single people have many partners and risky practices.
• Older people have few partners and infrequent sexual encounters.
• Sexually experienced people know how to use risk reduction measures.
• Married people are heterosexual, low risk, and monogamous.
Sexually active persons also may benefit from carefully examining a partner for lesions, sores, ulcerations, rashes, redness, discharge, swelling, and odor before initiating sexual activity. Teach women about low risk sexual practices and which sexual practices to avoid (Table 7-1).
TABLE 7-1
| SAFEST | LOW BUT POTENTIAL RISK | HIGH RISK (UNSAFE) |
| Abstinence Self-masturbation Monogamous (both partners and no high risk activities) and tested negative for HIV and other STIs Hugging, massage, touching (assuming no break in skin) Dry kissing Mutual masturbation without contact with semen or vaginal secretions and no broken skin Drug abstinence Sexual fantasy Erotic conversation, books, movies Erotic bathing, showering Eroticizing feet, fingers, buttocks, abdomen, ears |
Wet kissing∗ Vaginal intercourse with condom; anal intercourse with condom Monogamous (both partners and no high risk activities) but not tested for HIV or other STIs Oral sex with woman wearing female condom Oral sex with man wearing condom Mutual masturbation without contact with semen or vaginal secretions; healthy intact skin or use of latex or plastic barrier Urine contact with intact skin |
Unprotected anal intercourse; unprotected vaginal intercourse Oral-anal contact Multiple sexual partners, no HIV or STI testing Any sex (fisting, rough vaginal or anal intercourse, rape) that causes tissue damage or bleeding Oral sex on man or woman without a latex or plastic barrier Sharing sex toys, douche equipment Sharing needles Blood contact, including menstrual blood |
HIV, Human immunodeficiency virus; STI, sexually transmitted infection.
Sources: Centers for Disease Control and Prevention, Workowski, K., & Berman, S. (2006). Sexually transmitted diseases treatment guidelines, 2006. MMMR Morbidity and Mortality Weekly Report, 55(RR-11), 1-94; Marrazzo, J., Guest, F., & Cates, W. (2007). Reproductive tract infections, including HIV and sexually transmitted infections. In R. Hatcher, J. Trussell, A. Nelson, W. Cates, F. Guest, & D. Kowal (Eds.), Contraceptive technology (19th ed.). New York: Ardent Media.
The physical barrier promoted for the prevention of sexual transmission of HIV and other STIs is the condom (male and female). Nurses can help motivate clients to use condoms by initiating a discussion of the subject with them. This gives women permission to discuss any concerns, misconceptions, or hesitations they may have about using condoms. Information to be discussed includes the importance of using latex or plastic male condoms rather than natural skin condoms for STI protection. The nurse should remind women to use a condom with every sexual encounter, to use each one only once, to use a condom with a current expiration date, and to handle it carefully to avoid damaging it with fingernails, teeth, or other sharp objects. Condoms should be stored away from high heat. Although it is not ideal, women may choose to safely carry condoms in wallets, shoes, or inside a bra. Women can be taught the differences among condoms: price ranges, sizes, and where they can be purchased. Explicit instructions for how to apply a male condom are included in Box 8-3.
The female condom—a lubricated polyurethane sheath with a ring on each end, one end that is inserted into the vagina and the other end covering the labia (see Figure 8-7, A)—has been shown in laboratory studies to be an effective mechanical barrier to viruses, including HIV. Although no clinical studies have been completed to evaluate the efficacy of female condoms in protecting against STIs, laboratory studies have demonstrated that polyurethane can block smaller viruses such as the herpesvirus and HIV (Murphy, Morgan, & Likis, 2006). Further, studies suggest that the female condom is at least as effective as male condoms in preventing transmission of STIs. The CDC, Workowski, and Berman (2006) state that when used correctly and consistently, the female condom may substantially reduce STI risk and recommends its use when a male condom cannot be used properly. What is important and should be stressed by nurses is the consistent use of condoms for every act of sexual intimacy when there is the possibility of transmission of disease.
Despite concern about the potential for cervicovaginal epithelial disruption with nonoxynol-9 (N-9)–based spermicides, interest in vaginally applied chemical barriers that provide dual contraceptive and protection against bacterial STIs remains. Evidence has shown that vaginal spermicides do not protect against certain STIs, although more than 60 potential microbicides are in development and 18 are in clinical trials (Murphy et al., 2006). Condoms lubricated with N-9 are not recommended (American College of Obstetricians and Gynecologists [ACOG], 2008; CDC et al., 2006).
A key issue in condom use as a preventive strategy is to stress to women that in sexual encounters men must comply with a woman’s suggestion or request that they use a condom. Moreover, condom use must be renegotiated with every sexual contact, and women must address the issue of control of sexual decision making every time they request a male partner to use a condom. Women may fear that their partner would be offended if a condom were introduced. Some women may fear rejection and abandonment, conflict, potential violence, or loss of economic support if they suggest the use of condoms to prevent STI transmission. For many individuals, condoms are symbols of extrarelationship activity. Introduction of a condom into a long-term relationship in which one has not been used previously threatens the trust assumed in most long-term relationships.
Nurses must suggest strategies to enhance a woman’s condom negotiation and communication skills. It can be suggested that she talk with her partner about condom use at a time removed from sexual activity, which may make it easier to bring up the subject. Role playing possible partner reactions with a woman and her alternative responses can be helpful. Asking a woman who appears particularly uncomfortable to rehearse how she might approach the topic is useful, particularly when a woman fears her partner may be resistant. The nurse might suggest the woman begin by saying, “I need to talk with you about something that is important to both of us. It’s hard for me, and I feel embarrassed, but I think we need to talk about reducing risk during sex.” If women are able to sort out their feelings and fears before talking with their partners, they may feel more comfortable and in control of the situation. Women can be reassured that it is natural to be uncomfortable and that the hardest part is getting started. Nurses should help their clients clarify what they will and will not do sexually because it will be easier to discuss their concerns with their partners if they have thought about what to say. Women can be reminded that their partner may need time to think about what they have said and that they must pay attention to their partner’s response.
Many women do not anticipate or prepare for sexual activity in advance; embarrassment or discomfort in purchasing condoms may prevent some women from using them. Cultural barriers also may impede the use of condoms; for example, Hispanic gender roles make it difficult for Hispanic women to suggest using condoms to a partner. In general, suggesting condom use implies that a woman is sexually active, that she is “available” for sex, and that she is “seeking” sex; these are messages that many women are uncomfortable conveying, given the prevailing mores of our country. In a society that commonly views a woman who carries a condom as overprepared, possibly oversexed, and willing to have sex with any man, expecting her to insist on the use of condoms in a sexual encounter is somewhat optimistic at best and unrealistic at worst.
Finally, women should be counseled to watch out for situations that make it hard to talk about and to practice safer sex. These include romantic times when condoms are not available and when alcohol or drugs make it impossible to make wise decisions about safer sex.
Vaccination is an effective method for the prevention of some STIs such as hepatitis B and human papillomavirus (HPV). Hepatitis B vaccine is recommended for women at high risk for STIs (CDC, 2008b, 2008c). A vaccine is available for HPV types 6, 11, 16, and 18 for girls and women. It is recommended for girls 11 and 12, but can be given to girls as early as 9 years of age; catch-up vaccinations for girls and young women ages 13 to 26 may also be given (CDC, 2010b).
Sexually Transmitted Bacterial Infections
Chlamydia trachomatis is the most commonly reported STI in American women. In 2008 there were 1.2 million cases reported and estimates of more than 2 million cases unreported (CDC, 2009b). These infections are often silent and highly destructive; their sequelae and complications can be very serious. In women, chlamydial infections are difficult to diagnose; the symptoms, if present, are nonspecific, and the organism is expensive to culture.
Early identification of C. trachomatis is important because untreated infection often leads to acute salpingitis or pelvic inflammatory disease. Pelvic inflammatory disease is the most serious complication of chlamydial infections, and past chlamydial infections are associated with an increased risk of ectopic pregnancy and tubal factor infertility. Furthermore, chlamydial infection of the cervix causes inflammation, resulting in microscopic cervical ulcerations, and thus may increase the risk of acquiring HIV infection. More than half of infants born to mothers with chlamydia will develop conjunctivitis or pneumonia after perinatal exposure to the mother’s infected cervix. C. trachomatis is the most common infectious cause of ophthalmia neonatorum. Neonatal ocular prophylaxis with silver nitrate solution or antibiotic ointment does not prevent perinatal transmission from mother to infant, nor does it adequately treat chlamydial infection (see Chapter 35). Sexually active women ages 15 to 19 have the highest rates of infection (CDC, 2009b). Women older than 30 years have the lowest rate of infection. Risky behaviors, including multiple partners and nonuse of barrier methods of birth control, increase a woman’s risk of chlamydial infection. Lower socioeconomic status may be a risk factor, especially with respect to treatment-seeking behaviors.
Screening and Diagnosis
In addition to obtaining information regarding the presence of risk factors, the nurse should inquire about the presence of any symptoms. The CDC, Workowski, and Berman (2006) and U.S. Preventive Services Task Force (USPSTF, 2007a) strongly recommend screening of asymptomatic women at high risk in whom infection would otherwise go undetected (see www.cdc.org, and www.ahrq.gov). CDC guidelines recommend yearly screening of all sexually active adolescents, women between ages 20 and 25 years, and women older than 25 years who are at high risk (e.g., those with new or multiple partners). In addition, whenever possible, all women with two or more of the risk factors for chlamydia should be cultured. All pregnant women should have cervical cultures for chlamydia at the first prenatal visit. Screening late in the third trimester (36 weeks) may be carried out if the woman was positive previously, or if she is younger than 25 years, has a new sex partner, or has multiple sex partners.
Although chlamydial infections are usually asymptomatic, some women may experience spotting or postcoital bleeding, mucoid or purulent cervical discharge, or dysuria. Bleeding results from inflammation and erosion of the cervical columnar epithelium. Women taking oral contraceptives may have breakthrough bleeding.
Laboratory diagnosis of chlamydia is by culture (expensive and labor intensive), deoxyribonucleic acid (DNA) probe (relatively less expensive but less sensitive), enzyme immunoassay (also relatively less expensive but less sensitive), and nucleic acid amplification tests (expensive but has relatively higher sensitivity) (CDC et al., 2006). Special culture media and proper handling of specimens are important, so the nurse should always know what is required in his or her individual practice site. Chlamydial culture testing is not always available, primarily because of expense.
Management
The CDC recommendations for treatment of urethral, cervical, and rectal chlamydial infections, which are summarized in Table 7-2, are doxycycline and azithromycin (CDC et al., 2006). Azithromycin is often prescribed when compliance may be a problem, because only one dose is needed; however, expense is a concern with this medication. If the woman is pregnant, erythromycin or amoxicillin is used. Women who have a chlamydial infection and also are infected with HIV should be treated with the same regimen as those who are not infected with HIV.
TABLE 7-2
SEXUALLY TRANSMITTED INFECTIONS AND DRUG THERAPIES FOR WOMEN∗
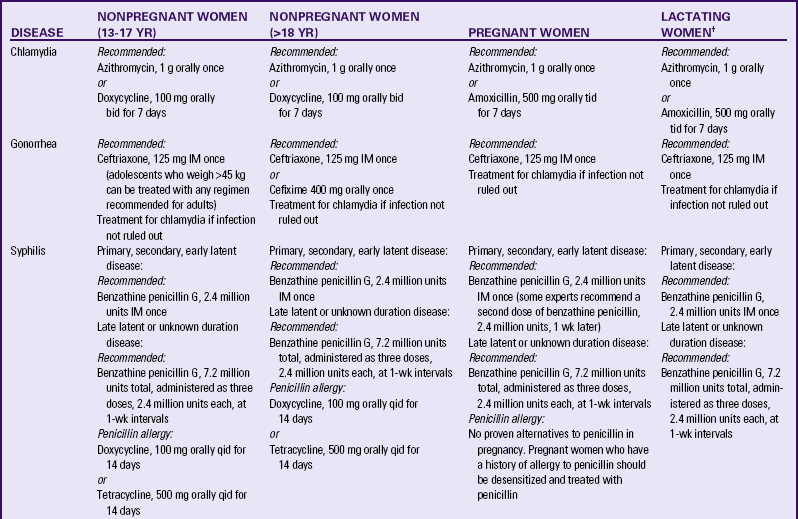
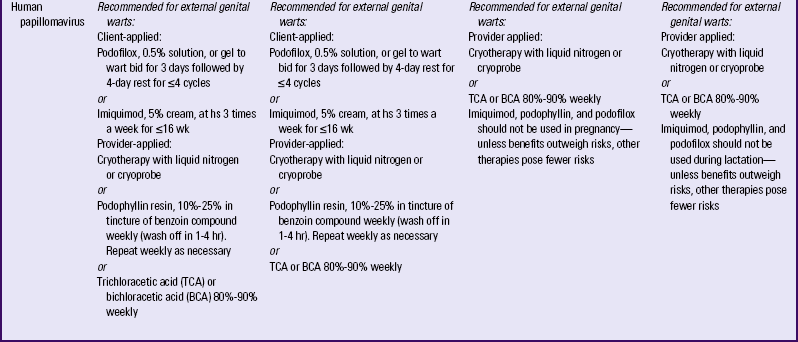
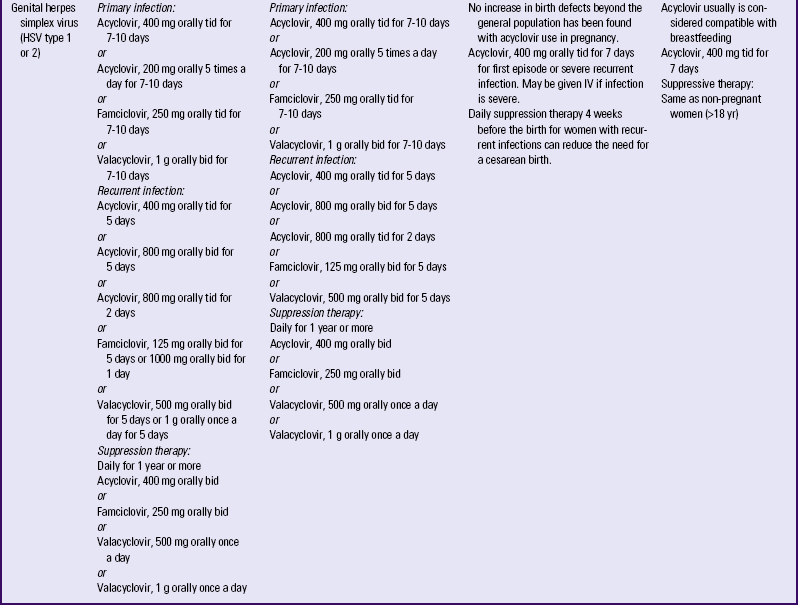
bid, Twice daily; hs, bedtime; IM, intramuscularly; IV, intravenous; qid, four times daily; tid, three times daily.
∗List is not inclusive of all drugs that may be used as alternatives.
†These medications are usually compatible with breastfeeding.
Sources: American Academy of Pediatrics Committee on Drugs. (2002). The transfer of drugs and other chemicals into human milk. Pediatrics, 108(3), 776-789; Centers for Disease Control and Prevention, Workowski, K., & Berman, S. (2006). Sexually transmitted diseases treatment guidelines 2006. MMWR Morbidity and Mortality Weekly Report, 55(RR-11), 1-94; Centers for Disease Control and Prevention (CDC). (2007). Updated recommended treatment regimens for gonococcal infections and associated conditions, United States, April, 2007. Available at www.cdc.gov/std/treatment/2006/updated-regimens.htm. Accessed June 2, 2010.
Because chlamydia is often asymptomatic, the woman should be cautioned to take all medication prescribed. All exposed sexual partners should be treated. Women, especially pregnant women, should be encouraged to be retested 3 to 4 months after treatment, especially if their partners did not seek treatment (CDC, 2007).
Gonorrhea
Gonorrhea is probably the oldest communicable disease in the United States and second to chlamydia in reported cases. The CDC estimates about 700,000 cases of gonorrhea a year will occur in the United States (CDC, 2009b). The incidence of drug-resistant cases of gonorrhea, in particular, penicillinase-producing Neisseria gonorrhoeae (PPNG), is increasing dramatically in the United States.
Gonorrhea is caused by the aerobic, gram-negative diplococcus, N. gonorrhoeae. Gonorrhea is almost exclusively transmitted by sexual contact. The principal means of communication is genital-to-genital contact; however, it also is spread by oral-to-genital and anal-to-genital contact. There also is evidence that infection may spread in females from vagina to rectum. Age is probably the most important risk factor associated with gonorrhea. In the United States the highest reported rates of infection are among sexually active teenagers, young adults, and African-Americans. In 2008, 70% of cases of gonorrhea were reported by African-Americans, and mostly in young girls ages 15 to 19 (CDC, 2009b).
Women are often asymptomatic, with one third of infections in adolescent women going unnoticed. When symptoms are present they are often less specific than are the symptoms in men. Women may have a purulent endocervical discharge, but discharge is usually minimal or absent. Menstrual irregularities may be the presenting symptom, or women may complain of pain—chronic or acute severe pelvic or lower abdominal pain or longer, more painful menses. Infrequently, dysuria, vague abdominal pain, or low backache prompts a woman to seek care. Gonococcal rectal infection may occur in women after anal intercourse, with 10% to 30% of urogenital infections accompanied by rectal infection. Individuals with rectal gonorrhea may be completely asymptomatic or, conversely, have severe symptoms with profuse purulent anal discharge, rectal pain, and blood in the stool. Rectal itching, fullness, pressure, and pain also are common symptoms, as is diarrhea. A diffuse vaginitis with vulvitis is the most common form of gonococcal infection in prepubertal girls. There may be few signs of infection, or vaginal discharge, dysuria, and swollen, reddened labia may be present.
Gonococcal infections in pregnancy can affect both mother and fetus. In women with cervical gonorrhea, salpingitis may develop in the first trimester. Perinatal complications of gonococcal infection include premature rupture of membranes, preterm birth, chorioamnionitis, neonatal sepsis, intrauterine growth restriction, and maternal postpartum sepsis. Amniotic infection syndrome manifested by placental, fetal, and umbilical cord inflammation after premature rupture of the membranes may result from gonorrheal infections during pregnancy. Ophthalmia neonatorum, the most common manifestation of neonatal gonococcal infections, is highly contagious and, if untreated, may lead to blindness of the newborn (see Chapter 35).
Screening and Diagnosis
Because gonococcal infections in women often are asymptomatic, the CDC recommends screening all women at risk for gonorrhea (CDC et al., 2006). All pregnant women should be screened at the first prenatal visit, and infected women and those identified with risky behaviors rescreened at 36 weeks of gestation. Gonococcal infection cannot be diagnosed reliably by clinical signs and symptoms alone. Individuals may have “classic” symptoms, vague symptoms that may be attributed to a number of conditions, or no symptoms at all. Cultures with selective media are considered the gold standard for diagnosis of gonorrhea. Cultures should be obtained from the endocervix, the rectum, and when indicated, the pharynx. Thayer-Martin cultures are recommended to diagnose gonorrhea in women. Any woman suspected of having gonorrhea should have a chlamydial culture and serologic test for syphilis if one has not been done in the past 2 months, because coinfection is common.
Management
Management of gonorrhea is straightforward, and the cure is usually rapid with appropriate antibiotic therapy (see Table 7-1). Single-dose efficacy is a major consideration in selecting an antibiotic regimen for women with gonorrhea. Another important consideration is the high percentage (45%) of women with coexisting chlamydial infections. The treatment of choice for uncomplicated urethral, endocervical, and rectal infections in pregnant and nonpregnant women is cefixime or ceftriaxone. The CDC recommends concomitant treatment for chlamydia (CDC, 2007). All women with both gonorrhea and syphilis should be treated for syphilis according to CDC guidelines (see discussion of syphilis in this chapter).
Gonorrhea is a highly communicable disease. Recent (past 30 days) sexual partners should be examined, cultured, and treated with appropriate regimens. Most treatment failures result from reinfection. The client must be informed of this, as well as of the consequences of reinfection in terms of chronicity, complications, and potential infertility. Women are counseled to use condoms. All clients with gonorrhea should be offered confidential counseling and testing for HIV infection.
Syphilis
Syphilis, one of the earliest described STIs, is caused by Treponema pallidum, a motile spirochete. Transmission is thought to be by entry in the subcutaneous tissue through microscopic abrasions that can occur during sexual intercourse. The disease also can be transmitted through kissing, biting, or oral-genital sex. Transplacental transmission may occur at any time during pregnancy; the degree of risk is related to the quantity of spirochetes in the maternal bloodstream.
Rates of syphilis in the United States among women, especially African-Americans have continued to rise since 2004.
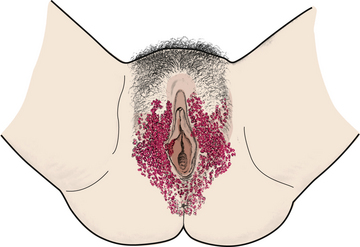
Syphilis is a complex disease that can lead to serious systemic disease and even death when untreated. Infection manifests itself in distinct stages with different symptoms and clinical manifestations. Primary syphilis is characterized by a primary lesion, the chancre, that appears 5 to 90 days after infection. This lesion often begins as a painless papule at the site of inoculation and then erodes to form a nontender, shallow, indurated, clean ulcer several millimeters to centimeters in size (Fig. 7-1, A). Secondary syphilis occurs 6 weeks to 6 months after the appearance of the chancre and is characterized by a widespread, symmetric maculopapular rash on the palms and soles and generalized lymphadenopathy. The infected individual also may experience fever, headache, and malaise. Condylomata lata (broad, painless, pink-gray, wartlike infectious lesions) may develop on the vulva, the perineum, or the anus (see Fig. 7-1, B). If the woman is untreated, she enters a latent phase that is asymptomatic for the majority of individuals. Latent infections are those that lack clinical manifestations but are detected by serologic testing. If the infection was acquired in the preceding year, the infection is termed an early latent infection. If it is left untreated, tertiary syphilis will develop in about one third of these women. Neurologic, cardiovascular, musculoskeletal, or multiorgan system complications can develop in the third stage.
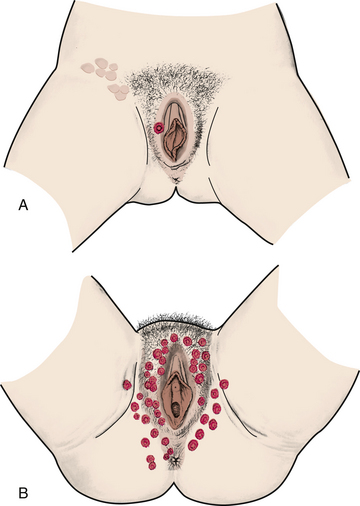
FIG. 7-1 Syphilis. A, Primary stage: chancre with inguinal adenopathy. B, Secondary stage: condylomata lata.
Screening and Diagnosis
All women who are diagnosed with another STI or with HIV should be screened for syphilis. All pregnant women should be screened for syphilis at the first prenatal visit and again in early third trimester and at the time of giving birth if high risk (CDC et al., 2006; USPSTF, 2009b). Diagnosis is dependent on microscopic examination of primary and secondary lesion tissue and serology during latency and late infection. A test for antibodies may not be reactive in the presence of active infection because it takes time for the body’s immune system to develop antibodies to any antigens. Up to one third of people in early primary syphilis may have nonreactive serologic tests. Two types of serologic tests are used: nontreponemal and treponemal. Nontreponemal antibody tests such as the Venereal Disease Research Laboratories (VDRL) or rapid plasma reagin (RPR) are used as screening tests. False-positive results are not unusual, particularly when conditions such as acute infection, autoimmune disorders, malignancy, pregnancy, and drug addiction exist and after immunization or vaccination. The treponemal tests, fluorescent treponemal antibody absorbed (FTA-ABS), and microhemagglutination assays for antibody to T. pallidum (MHA-TP), are used to confirm positive results. Test results in clients with early primary or incubating syphilis may be negative. Seroconversion usually takes place 6 to 8 weeks after exposure, so testing should be repeated in 1 to 2 months when a suggestive genital lesion exists. Tests for concomitant STIs (e.g., chlamydia and gonorrhea) should be done (e.g., wet preps and cultures) and HIV testing offered if indicated.
Management
Penicillin is the preferred drug for treating clients with syphilis (see Table 7-2). It is the only proven therapy that has been widely used for clients with neurosyphilis, congenital syphilis, or syphilis during pregnancy. Intramuscular benzathine penicillin G is used to treat primary, secondary, and early latent syphilis. Although doxycycline, tetracycline, and erythromycin are alternative treatments for penicillin-allergic clients, both tetracycline and doxycycline are contraindicated in pregnancy, and erythromycin is unlikely to cure a fetal infection. Therefore, pregnant women should, if necessary, receive skin testing and be treated with penicillin or be desensitized (CDC, et al., 2006). Specific protocols are recommended by the CDC.
Monthly follow-up is mandatory so that repeated treatment may be given if needed. The nurse should emphasize the necessity of long-term serologic testing even in the absence of symptoms. The woman should be advised to practice sexual abstinence until treatment is completed, all evidence of primary and secondary syphilis is gone, and serologic evidence of a cure is demonstrated. Women should be told to notify all partners who may have been exposed. They should be informed that the disease is reportable. Preventive measures should be discussed.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an infectious process that most commonly involves the uterine (fallopian) tubes (salpingitis), uterus (endometritis), and more rarely, the ovaries and peritoneal surfaces. Multiple organisms have been found to cause PID, and most cases are associated with more than one organism. In the past, the most common causative agent was thought to be N. gonorrhoeae; however, C. trachomatis is now estimated to cause half of all cases of PID. In addition to gonorrhea and chlamydia, a wide variety of anaerobic and aerobic bacteria are recognized to cause PID. PID encompasses a wide variety of pathologic processes; the infection can either be acute, subacute, or chronic and can have a wide range of symptoms.
Most PID results from ascending spread of microorganisms from the vagina and endocervix to the upper genital tract. This spread most frequently happens at the end of or just after menses following reception of an infectious agent. During the menstrual period, several factors facilitate the development of an infection: the cervical os is slightly open, the cervical mucus barrier is absent, and menstrual blood is an excellent medium for growth. PID also may develop after a miscarriage or an induced abortion, pelvic surgery, or childbirth.
Risk factors for acquiring PID are those associated with the risk of contracting an STI, including young age (most cases of acute PID are in women younger than age 25), nulliparity, multiple partners, high rate of new partners, and a history of STIs and PID. Women who use intrauterine devices (IUDs) may be at increased risk for PID up to 3 weeks after insertion (Eckert & Lentz, 2007b).
Women who have had PID are at increased risk for ectopic pregnancy, infertility, and chronic pelvic pain. After a single episode of PID, a woman’s risk for ectopic pregnancy increases sevenfold compared with the risk for women who have never had PID. Other problems associated with PID include dyspareunia (painful intercourse), pyosalpinx (pus in the uterine tubes), tuboovarian abscess, and pelvic adhesions.
The symptoms of PID vary, depending on whether the infection is acute, subacute, or chronic; however, pain is common to all types of infection. It may be dull, cramping, and intermittent (subacute) or severe, persistent, and incapacitating (acute). Women may also report one or more of the following: fever, chills, nausea and vomiting, increased vaginal discharge, symptoms of a urinary tract infection, and irregular bleeding. Abdominal pain is usually present (Eckert & Lentz, 2007b).
Screening and Diagnosis
PID is difficult to diagnose because of the accompanying wide variety of symptoms. The CDC recommends treatment for PID in all sexually active young women and others at risk for STIs if the following criteria are present and no other cause or causes of the illness are found: lower abdominal tenderness, bilateral adnexal tenderness, and cervical motion tenderness. Other criteria for diagnosing PID include an oral temperature of 38.3° C or above, abnormal cervical or vaginal discharge, elevated erythrocyte sedimentation rate, elevated C-reactive protein, and laboratory documentation of cervical infection with N. gonorrhoeae or C. trachomatis (CDC et al., 2006).
Management
Perhaps the most important nursing intervention is prevention. Primary prevention includes education in preventing the acquisition of STIs, and secondary prevention involves preventing a lower genital tract infection from ascending to the upper genital tract. Instructing women in self-protective behaviors such as practicing risk reduction measures and using barrier methods is critical. Also important is the detection of asymptomatic gonorrheal and chlamydial infections through routine screening of women with risky behaviors or specific risk factors such as age.
Although treatment regimens vary with the infecting organism, a broad-spectrum antibiotic is generally used (Table 7-3). Treatment for mild to moderately severe PID may be oral, or a combination of oral and parenteral, and regimens can be administered in inpatient or outpatient settings (CDC, 2007). The woman with acute PID should be on bed rest in a semi-Fowler position. Comfort measures include analgesics for pain and all other nursing measures applicable to a woman confined to bed. The woman should have as few pelvic examinations as possible during the acute phase of the disease. During the recovery phase the woman should restrict her activity and make every effort to get adequate rest and a nutritionally sound diet. Follow-up laboratory work after treatment should include endocervical cultures for a test of cure.
TABLE 7-3
TREATMENT OF PELVIC INFLAMMATORY DISEASE
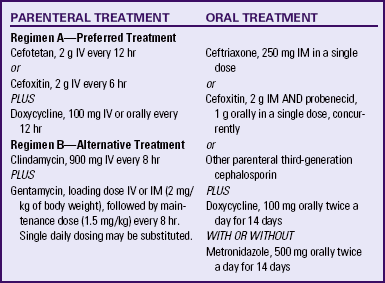
bid, Twice daily; IM, intramuscularly; IV, intravenously.
Sources: Centers for Disease Control and Prevention, Workowski, K., & Berman, S. (2006). Sexually transmitted diseases treatment guidelines 2006. MMWR Morbidity and Mortality Weekly Report, 55(RR-11), 1-94; Centers for Disease Control and Prevention (CDC). (2007a). Updated recommended treatment regimens for gonococcal infections and associated conditions, United States, April, 2007. Available at www.cdc.gov/std/treatment/2006/updated-regimens.htm. Accessed June 2, 2010.
Health education is central to effective management of PID. Explain to women the nature of their disease, and encourage them to comply with all therapy and prevention recommendations, emphasizing the necessity of taking all medication, even if symptoms disappear. Counsel women to refrain from sexual intercourse until their treatment is completed. Provide contraceptive counseling. Suggest that the woman select a barrier method such as condoms or a diaphragm. A woman with a history of PID should not choose an IUD as her contraceptive method (Mishell, 2007).
The potential or actual loss of reproductive capabilities can be devastating and can adversely affect a woman’s self-concept. Because PID is so closely tied to sexuality, body image, and self-concept, the woman diagnosed with it will need supportive care. Referral to a support group or for counseling may be appropriate.
Sexually Transmitted Viral Infections
Human papillomavirus (HPV) infections, also known as condylomata acuminata, or genital warts, is the most common viral STI seen in ambulatory health care settings. An estimated 20 million Americans are infected with HPV, and about 6.2 million new infections occur every year (CDC, 2009b). HPV, a double-stranded DNA virus, has more than 30 serotypes that can be sexually transmitted, 5 of which are known to cause genital wart formation, and 8 of which are currently thought to have oncogenic potential (CDC et al., 2006). HPV is the primary cause of cervical neoplasia (American Cancer Society [ACS], 2010).
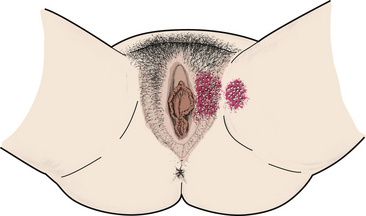
HPV lesions in women are most commonly seen in the posterior part of the introitus; however, lesions also are found on the buttocks, the vulva, the vagina, the anus, and the cervix (Fig. 7-2). Typically the lesions are small—2 to 3 mm in diameter and 10 to 15 mm in height—soft, papillary swellings occurring singly or in clusters on the genital and anorectal region. Infections of long duration may appear as a cauliflower-like mass. In moist areas such as the vaginal introitus, the lesions may appear to have multiple, fine, fingerlike projections. Vaginal lesions are often multiple. Flat-topped papules, 1 to 4 mm in diameter, are seen most often on the cervix and often are visualized only under magnification. Warts are usually flesh colored or slightly darker on Caucasian women, black on African-American women, and brownish on Asian women. The lesions are often painless but may be uncomfortable, particularly when very large, inflamed, or ulcerated. Chronic vaginal discharge, pruritus, or dyspareunia can occur.
HPV infections are thought to be more frequent in pregnant than in nonpregnant women, with an increase in incidence from the first trimester to the third. Furthermore, a significant proportion of preexisting HPV lesions enlarge greatly during pregnancy, a proliferation presumably resulting from the relative state of immunosuppression present during pregnancy. Lesions may become so large during pregnancy that they affect urination, defecation, mobility, and fetal descent, although birth by cesarean is rarely necessary (Duff, 2007). HPV infection may be acquired by the neonate during birth; the frequency of such transmission is unknown. The preventive value of cesarean birth is unknown, and it is not recommended solely to prevent transmission of HPV infection to newborns (Duff).
Screening and Diagnosis
A woman with HPV lesions may complain of symptoms such as a profuse, irritating vaginal discharge, itching, dyspareunia, or postcoital bleeding. She also may report “bumps” on her vulva or labia. History of a known exposure is important; however, because of the potentially long latency period and the possibility of subclinical infections in men, the lack of a history of known exposure cannot be used to exclude a diagnosis of HPV infection.
Physical inspection of the vulva, the perineum, the anus, the vagina, and the cervix is essential whenever HPV lesions are suspected or seen in one area. Because speculum examination of the vagina may block some lesions, it is important to rotate the speculum blades until all areas are visualized. When lesions are visible, the characteristic appearance previously described is considered diagnostic. However, in many instances, cervical lesions are not visible, and some vaginal or vulvar lesions also may be unobservable to the naked eye. Because of the potential spread of vulvar or vaginal lesions to the anus, gloves should be changed between vaginal and rectal examinations.
Viral screening and typing for HPV are available but not standard practice. History, evaluation of signs and symptoms, Papanicolaou (Pap) test, and physical examination are used in making a diagnosis. The HPV-DNA test can be used in women older than the age of 30 in combination with the Pap test to screen for types of HPV that are likely to cause cancer or in women with abnormal Pap test results (ACS, 2010). The only definitive diagnostic test for presence of HPV is histologic evaluation of a biopsy specimen.
HPV lesions must be differentiated from molluscum contagiosum and condylomata lata. Molluscum contagiosum lesions are half-domed, smooth, flesh-colored to pearly white papules with depressed centers. Condylomata lata are a form of secondary syphilis and generally flatter and wider than genital warts. A serologic test for syphilis would confirm the diagnosis of secondary syphilis.
Management
Untreated warts may resolve on their own in young women since their immune systems may be strong enough to fight the HPV infection. Treatment of genital warts, if needed, is often difficult. No therapy has been shown to eradicate HPV. The goal of treatment therefore is removal of warts and relief of signs and symptoms. The woman often must make multiple office visits; frequently, many different treatment modalities will be used.
Treatment of genital warts should be guided by preference of the woman, available resources, and experience of the health care provider. None of the treatments is superior to all other treatments, and no one treatment is ideal for all warts (CDC et al., 2006). Available treatments are outlined in Table 7-2. Imiquimod, podophyllin, and podofilox should not be used during pregnancy. Because the lesions can proliferate and become friable during pregnancy, many experts recommend their removal by using cryotherapy or various surgical techniques during pregnancy (CDC et al.).
Women with discomfort associated with genital warts may find that bathing with an oatmeal solution and drying the area with a cool hair dryer will provide some relief. Keeping the area clean and dry will also decrease growth of the warts. Cotton underwear and loose-fitting clothes that decrease friction and irritation also may decrease discomfort. Women should be advised to maintain a healthy lifestyle to aid the immune system; women can be counseled regarding diet, rest, stress reduction, and exercise.
Client counseling is essential. Women must understand how the virus is transmitted, that no immunity is conferred with infection, and that reacquisition of the infection is likely with repeated contact. Women should know that their partners should be checked even if they are asymptomatic. Because HPV is highly contagious, the majority of women’s partners will be infected and should be treated. All sexually active women with multiple partners or a history of HPV should be encouraged to use latex condoms for intercourse to decrease acquisition or transmission of condylomata.
Instructions for all medications and treatments must be detailed. Women should be informed before treatment of the possibility of posttreatment pain associated with specific therapies. The importance of thorough treatment of concurrent vaginitis or STI should be emphasized. The link between cervical cancer and HPV infections and the need for close follow-up should be discussed. Annual health examinations are recommended to assess disease recurrence and screening for cervical cancer. Women should be counseled to have regular Pap screening, as recommended for women without genital warts (CDC et al., 2006).
Prevention
Preventive strategies that have been suggested include abstinence from all sexual activity, staying in a long-term monogamous relationship, and prophylactic vaccination (CDC, 2009a, 2010b). Two vaccines, Cervarix and Gardisil, are available and other vaccines continue to be investigated. The vaccines are most effective if given before the woman has her first sexual contact (CDC, 2009a). Practitioners should stay current with results of these clinical trials and make recommendations about vaccination based on the outcomes of the research.
Genital Herpes Simplex Virus
Unknown until the middle of the 20th century, genital herpes simplex virus (HSV) infection is now widespread in the United States. Genital HSV is more common in women: approximately 1 in 5 women ages 14 to 49 are infected (CDC, 2010a). HSV infection results in painful recurrent genital ulcers and is caused by two different antigen subtypes of herpes simplex virus: herpes simplex virus 1 (HSV-1) and herpes simplex virus 2 (HSV-2). HSV-2 is usually transmitted sexually, and HSV-1, nonsexually. Although HSV-1 is more commonly associated with gingivostomatitis and oral labial ulcers (fever blisters; cold sores) and HSV-2 with genital lesions, neither type is exclusively associated with the respective sites.
Although HSV infection is not a reportable disease, it is estimated that about 50 million people in the United States are infected with genital herpes (CDC et al., 2006). Women between the ages of 15 and 34 are most likely to become infected, especially if they have multiple sex partners. Many persons infected with HSV-2 are asymptomatic and therefore undiagnosed. They can transmit the infection unaware that they are infected.
An initial HSV genital infection is characterized by multiple painful lesions, fever, chills, malaise, and severe dysuria and may last 2 to 3 weeks. Women generally have a more severe clinical course than men. Women with primary genital herpes have many lesions that progress from macules to papules, then forming vesicles, pustules, and ulcers that crust and heal without scarring (Fig. 7-3). These ulcers are extremely tender, and primary infections may be bilateral. Women also may have itching, inguinal tenderness, and lymphadenopathy. Severe vulvar edema may develop, and women may have difficulty sitting. HSV cervicitis also is common with initial HSV-2 infections. The cervix may appear normal or be friable, reddened, ulcerated, or necrotic. A heavy, watery-to-purulent vaginal discharge is common. Extragenital lesions may be present because of autoinoculation. Urinary retention and dysuria may occur secondary to autonomic involvement of the sacral nerve root.
Women with recurrent episodes of HSV infections commonly have only local symptoms that are usually less severe than those associated with the initial infection. Systemic symptoms are usually absent, although the characteristic prodromal genital tingling is common. Recurrent lesions are unilateral, are less severe, and usually last 5 to 7 days. Lesions begin as vesicles and progress rapidly to ulcers. Few women with recurrent disease have cervicitis.
During pregnancy, maternal infection with HSV-2 can have adverse effects on both the mother and fetus. Viremia occurs during the primary infection, and congenital infection is possible, though rare. Primary infections during the first trimester have been associated with increased miscarriage rates. The most severe complication of HSV infection is neonatal herpes, a potentially fatal or severely disabling disease occurring in 1 in 2000 to 1 in 10,000 live births. Most mothers of infants who contract neonatal herpes lack histories of clinically evident genital herpes. Risk of neonatal infection is highest among women with primary herpes infection who are near term and is low among women with recurrent herpes (CDC et al., 2006).
Screening and Diagnosis
A history provides much information when making a diagnosis of herpes. A history of exposure to an infected person is important, although infection from an asymptomatic individual is possible. A history of having viral symptoms such as malaise, headache, fever, or myalgia is suggestive. Local symptoms such as vulvar pain, dysuria, itching or burning at the site of infection, and painful genital lesions that heal spontaneously also are highly suggestive of HSV infections. The nurse should ask about a history of a primary infection, prodromal symptoms, vaginal discharge, and dyspareunia. Pregnant women should be asked whether they or their partner(s) have had genital lesions.
During the physical examination, the nurse should assess for inguinal and generalized lymphadenopathy and elevated temperature. The entire vulvar, perineal, vaginal, and cervical areas should be carefully inspected for vesicles or ulcerated or crusted areas. A speculum examination may be very difficult for the woman because of the extreme tenderness often associated with herpes infections. Any suggestive or recurrent lesions found during pregnancy should be cultured to verify HSV. Although a diagnosis of herpes infection may be suspected from the history and physical, it is confirmed by laboratory studies. A viral culture is obtained by swabbing exudate during the vesicular stage of the disease.
Management
Genital herpes is a chronic and recurring disease for which there is no known cure. Management is directed toward specific treatment during primary and recurrent infections, prevention, self-help measures, and psychologic support.
Systemic antiviral medications partially control the symptoms and signs of HSV infections when used for the primary or recurrent episodes or when used as daily suppressive therapy. However, these medications do not eradicate the infection nor do they alter subsequent risk or frequency of recurrences after the medication is stopped. Three antiviral medications provide clinical benefit: acyclovir, valacyclovir, and famciclovir. Treatment recommendations are given in Table 7-2. The safety of acyclovir, valacyclovir, and famciclovir therapy during pregnancy has not been established; however, acyclovir may be used to reduce the symptoms of HSV if the benefits to the woman outweigh the potential harm to the fetus (CDC et al., 2006). Continued investigation of HSV therapy with these medications in pregnancy is needed.
Cleaning lesions twice a day with saline will help prevent secondary infection. Bacterial infection must be treated with appropriate antibiotics. Measures that may increase comfort for women when lesions are active include warm sitz baths with baking soda; keeping lesions dry by blowing the area dry with a hair dryer set on cool or patting dry with a soft towel; wearing cotton underwear and loose clothing; using drying aids such as hydrogen peroxide, Burow’s solution, or oatmeal baths; applying cool, wet, black tea bags to lesions; and applying compresses with an infusion of cloves or peppermint oil and clove oil to lesions.![]()
Oral analgesics such as aspirin or ibuprofen may be used to relieve pain and systemic symptoms associated with initial infections. Because the mucous membranes affected by herpes are extremely sensitive, any topical agents should be used with caution. Nonantiviral ointments, especially those containing cortisone, should be avoided. A thin layer of lidocaine ointment or an antiseptic spray may be applied to decrease discomfort, especially if walking is painful.
Counseling and education are critical components of the nursing care of women with herpes infections. Information regarding the etiology, signs and symptoms, transmission, and treatment should be provided. The nurse should explain that each woman is unique in her response to herpes and emphasize the variability of symptoms. Women should be helped to understand when viral shedding and thus transmission to a partner is most likely, and that they should refrain from sexual contact from the onset of prodromal symptoms until complete healing of lesions. Some authorities recommend consistent use of condoms for all persons with genital herpes. Condoms may not prevent transmission, particularly male-to-female transmission; however, this does not mean that the partners should avoid all intimacy. Women can be encouraged to maintain close contact with their partners while avoiding contact with lesions. Women should be taught how to look for herpetic lesions with a mirror and good light source and a wet cloth or finger covered with a finger cot to rub lightly over the labia. The nurse should ensure that women understand that when lesions are active, sharing intimate articles (e.g., washcloths, wet towel) that come into contact with the lesions should be avoided. Plain soap and water is all that is needed to clean hands that have come into contact with herpetic lesions.
Stress, menstruation, trauma, febrile illnesses, chronic illnesses, and ultraviolet light have all been found to trigger genital herpes. Women may wish to keep a diary to identify stressors that seem to be associated with recurrent herpes attacks so that they can then avoid these stressors when possible. The role of exercise in reducing stress can be discussed. Referral for stress-reduction therapy, yoga, or meditation classes may be indicated. Avoiding excessive heat and sun and hot baths and using a lubricant during sexual intercourse to reduce friction also may be helpful. Women in their childbearing years should be counseled regarding the risk of herpes infection during pregnancy. They should be instructed to use condoms if there is any risk of contracting an STI from a sexual partner. If they become pregnant while taking acyclovir, the risk of birth defects does not appear to be higher than for the general population; however continued use should be based on whether the benefits for the woman outweigh the possible risks to the fetus. Acyclovir does enter breast milk but the amount of medication ingested during breastfeeding is very low and is usually not a health concern (Weiner & Buhimschi, 2009).
Because neonatal HSV infection is such a devastating disease, prevention is critical. Current recommendations include carefully examining and questioning all women about symptoms at onset of labor (CDC et al., 2006). If visible lesions are not present at onset of labor, vaginal birth is acceptable. Cesarean birth within 4 hours after labor begins or membranes rupture is recommended if visible lesions are present. Infants who are born through an infected vagina should be carefully observed and cultured (see Chapter 35).
The emotional effect of contracting an incurable STI such as herpes is considerable. At diagnosis, many emotions may surface—helplessness, anger, denial, guilt, anxiety, shame, or inadequacy. Women need the opportunity to discuss their feelings and help in learning to live with the disease. Herpes can affect a woman’s sexuality, her sexual practices, and her current and future relationships. She may need help in raising the issue with her partner or with future partners.
Viral Hepatitis
Five different viruses (hepatitis viruses A, B, C, D, and E) account for almost all cases of viral hepatitis in humans. Hepatitis viruses A, B, and C are discussed. Hepatitis D and E viruses, common among users of intravenous drugs and recipients of multiple blood transfusions, are not included in this discussion.
Hepatitis A
Hepatitis A virus (HAV) infection is acquired primarily through a fecal-oral route by ingestion of contaminated food, particularly milk, shellfish, or polluted water, or person-to-person contact. Women living in the western United States, Native Americans, Alaska Natives, and children and employees in daycare centers are at high risk. Hepatitis A, like other enteric infections, can be transmitted during sexual activity.
HAV infection is characterized by flulike symptoms with malaise, fatigue, anorexia, nausea, pruritus, fever, and right upper quadrant pain. Serologic testing to detect the immunoglobulin M (IgM) antibody is done to confirm acute infections. The IgM antibody is detectable 5 to 10 days after exposure and can remain positive for up to 6 months. Because HAV infection is self-limited and does not result in chronic infection or chronic liver disease, treatment is usually supportive. Women who become dehydrated from nausea and vomiting or who have fulminating hepatitis A may need to be hospitalized. Medications and other ingested substances that might cause liver damage or that are metabolized in the liver (e.g., acetaminophen, ethyl alcohol) should be avoided. A well-balanced diet is recommended. Hepatitis A vaccine is recommended for women at high risk for being exposed to HAV infection. The safety of the vaccine has not been established in pregnancy; therefore, immune globulin (gamma-globulin) or immune-specific globulin is indicated for a pregnant woman exposed to HAV. All household contacts of the woman also should receive gamma globulin (CDC et al., 2006).
Hepatitis B
Hepatitis B virus (HBV) is the virus most threatening to the fetus and neonate. It is caused by a large DNA virus and is associated with three antigens and their antibodies: hepatitis B surface antigen (HBsAg), HBV antigen (HBeAg), HBV core antigen (HBcAg), antibody to HBsAg (anti-HBs), antibody to HBeAg (anti-HBe), and antibody to HBcAg (anti-HBc). Screening for active or chronic disease or disease immunity is based on testing for these antigens and their antibodies.
Populations at risk include women of Asian, Pacific Island (Polynesian, Micronesian, Melanesian), or Alaskan-Inuit descent and women born in Haiti or sub-Saharan Africa. Women who have a history of acute or chronic liver disease, who work or receive treatment in a dialysis unit, or who have household or sexual contact with a hemodialysis client are at greater risk. Women who work or live in institutions for the mentally challenged are considered to be at risk, as are women with a history of multiple blood transfusions. Health care workers and public safety workers exposed to blood in the workplace are at risk. Behaviors such as having multiple sexual partners and a history of intravenous drug use increase the risk of contracting HBV infections.
HBsAg has been found in blood, saliva, sweat, tears, vaginal secretions, and semen. Drug abusers who share needles are at risk, as are health care workers who are exposed to blood and needlesticks. Perinatal transmission most often occurs in infants of mothers who have acute hepatitis infection late in the third trimester or during the intrapartum or postpartum period from exposure to HBsAg-positive vaginal secretions, blood, amniotic fluid, saliva, and breast milk. HBV has also been transmitted by artificial insemination. Although HBV can be transmitted via blood transfusion, the incidence of such infections has decreased significantly since testing of blood for HBsAg became routine.
HBV infection is a disease of the liver and is often a silent infection. In an adult the course of the infection can be fulminating, and the outcome, fatal. Symptoms of HBV infection are similar to those of hepatitis A: arthralgias, arthritis, lassitude, anorexia, nausea, vomiting, headache, fever, and mild abdominal pain. Later the woman may have clay-colored stools, dark urine, increased abdominal pain, and jaundice. Between 5% and 10% of individuals with HBV have persistence of HBsAg and become chronic hepatitis B carriers.
Screening and Diagnosis: All women at high risk for contracting HBV should be screened on a regular basis. However, screening only individuals at high risk may not identify up to 50% of HBsAg-positive women. Screening for the presence of HBsAg is recommended on allw pregnant women at the first prenatal visit, regardless of whether they have been tested previously; screening should be done on admission for labor and birth for women at high risk for infection during pregnancy or if prenatal test results are not available (CDC, 2008b; USPSTF, 2009a).
The HBsAg screening test is usually performed, given that a rise in HBsAg occurs at the onset of clinical symptoms and usually indicates an active infection. If HBsAg persists in the blood, the woman is identified as a carrier. If the HBsAg test result is positive, further laboratory studies may be ordered: anti-HBe, anti-HBc, serum glutamic-oxaloacetic transaminase (SGOT), alkaline phosphatase, and liver panel.
Management: There is no specific treatment for hepatitis B. Recovery is usually spontaneous in 3 to 16 weeks. Pregnancies complicated by acute viral hepatitis are managed on an outpatient basis. Women should be advised to increase rest periods, eat a high-protein, low-fat diet; and increase their fluid intake. They should avoid medications metabolized in the liver, and alcohol. Pregnant women with a definite exposure to HBV should be given hepatitis B immune globulin and should begin the hepatitis B vaccine series within 14 days of the most recent contact to prevent infection (CDC et al., 2006). Vaccination during pregnancy is not thought to pose risks to the fetus.
All nonimmune women at high or moderate risk of hepatitis should be informed of the availability of hepatitis B vaccine. Vaccination is recommended for all individuals who have had multiple sex partners within the past 6 months (CDC et al., 2006). In addition, intravenous drug users, residents of correctional or long-term care facilities, persons seeking care for an STI, prostitutes, women whose partners are intravenous drug users or bisexual, and women whose occupation exposes them to high risk should be vaccinated. The vaccine is given in a series of three (four if rapid protection is needed) doses over a 6-month period, with the first two doses given at least 1 month apart. The vaccine is given in the deltoid muscle (CDC et al.).
Client education includes explaining the meaning of hepatitis B infection, including transmission, state of infectivity, and sequelae. The nurse also should explain the need for immunoprophylaxis for household members and sexual contacts. To decrease transmission of the virus, women with hepatitis B or who test positive for HBV should be advised to maintain a high level of personal hygiene (e.g., wash hands after using the toilet; carefully dispose of tampons, pads, and bandages in plastic bags; do not share razor blades, toothbrushes, needles, or manicure implements; have male partner use a condom if unvaccinated and without hepatitis; avoid sharing saliva through kissing, or sharing of silverware or dishes; and wipe up blood spills immediately with soap and water). They should inform all health care providers of their carrier state. Postpartum women should be reassured that breastfeeding is not contraindicated if their infants received prophylaxis at birth and are currently on the immunization schedule.
Hepatitis C
Hepatitis C virus (HCV) infection has become an important health problem as increasing numbers of persons acquire the disease. Hepatitis C is responsible for nearly 50% of the cases of chronic viral hepatitis. Risk factors include having STIs such as hepatitis B and HIV, multiple sexual partners, history of blood transmissions, and history of intravenous drug use. HCV is readily transmitted through exposure to blood and much less efficiently via semen, saliva, or urine.
Most clients with hepatitis C are asymptomatic or have general influenza-like symptoms similar to those of hepatitis A. HCV infection is confirmed by the presence of anti-C antibody during laboratory testing. Interferon-alfa alone or with ribavirin for 6 to 12 months is the main therapy for chronic HCV-related liver disease, although effectiveness of this treatment varies. Currently, no vaccine is available for hepatitis C. Transmission of HCV through breastfeeding has not been reported.
Human Immunodeficiency Virus
Approximately 37,000 new HIV infections occur in the United States each year. An estimated 26% of these new infections occur in women. African-American women are estimated to have 64% of these infections, Caucasian women are estimated to have 19%, Hispanic women, 15%, and Native American women less than 1% (CDC, 2008d).
Severe depression of the cellular immune system associated with HIV infection characterizes acquired immunodeficiency syndrome (AIDS). Although behaviors that place women at risk have been well documented, you should assess all women for the possibility of HIV exposure. The most commonly reported opportunistic diseases are Pneumocystis (jiroveci) pneumonia (PCP), Candida esophagitis, and wasting syndrome. Other viral infections such as HSV and cytomegalovirus infections seem to be more prevalent in women than men (CDC et al., 2006). PID is often more severe in HIV-infected women than in the general population, and rates of HPV and cervical dysplasia are sometimes higher in non–HIV-infected women (Eckert & Lentz, 2007a). The clinical course of HPV infection in women with HIV infection is accelerated while recurrence is more frequent in non–HIV-infected women.
Once HIV enters the body, seroconversion to HIV positivity usually occurs within 6 to 12 weeks. Although HIV seroconversion may be totally asymptomatic, it usually is accompanied by a viremic, influenza-like response. Symptoms include fever, headache, night sweats, malaise, generalized lymphadenopathy, myalgias, nausea, diarrhea, weight loss, sore throat, and rash.
Laboratory studies may reveal leukopenia, thrombocytopenia, anemia, and an elevated erythrocyte sedimentation rate. HIV has a strong affinity for surface-marker proteins on T lymphocytes. This affinity leads to significant T-cell destruction. Both clinical and epidemiologic studies have shown that declining CD4 levels are strongly associated with increased incidence of AIDS-related diseases and death in many different groups of HIV-infected persons.
Transmission of the virus from mother to child can occur throughout the perinatal period. Exposure may occur to the fetus through the maternal circulation as early as the first trimester of pregnancy, to the infant during labor and birth by inoculation or ingestion of maternal blood and other infected fluids, or to the infant through breast milk (Marrazzo et al., 2007).
Screening and Diagnosis
Screening, teaching, and counseling regarding HIV risk factors, indications for being tested, and testing are major roles for nurses caring for women today. A number of behaviors place women at risk for HIV infection, including intravenous drug use, high risk sexual partners, multiple sex partners, and a previous history of multiple STIs. HIV infection is usually diagnosed by using HIV-1 and HIV-2 antibody tests. Antibody testing is first done with a sensitive screening test such as the enzyme immunoassay (EIA). Reactive screening tests must be confirmed by an additional test, such as the Western blot or an immunofluorescence assay. If a positive antibody test is confirmed by a supplemental test, it means that a woman is infected with HIV and is capable of infecting others. HIV antibodies are detectable in at least 95% of individuals within 3 months after infection. Although a negative antibody test usually indicates that a person is not infected, antibody tests cannot exclude recent infection. Because HIV antibody crosses the placenta, definite diagnosis of HIV in children younger than 18 months is based on laboratory evidence of HIV in blood or tissues by culture, nucleic acid, or antigen detection (CDC et al., 2006).
The U.S. Food and Drug Administration (FDA) (2008) has approved six rapid HIV antibody screening tests. These tests use a blood sample obtained by fingerstick or venipuncture, an oral fluid sample, or a urine sample to provide test results within 20 minutes, with sensitivity and specificity rates of more than 99%. If the results are reactive, further testing is necessary (CDC, Divisions of HIV/AIDS Prevention, 2008). Quicker results mean that clients do not have to make extra visits for follow-up standard tests, and the oral test provides an option for clients who do not want to have a blood test.
The CDC, Workowski, and Berman (2006) and the USPSTF (2007b) recommend offering HIV testing to all women whose behavior places them at risk for HIV infection. It may be useful to allow women to self-select for HIV testing. On entry to the health care system, a woman can be handed written information about the risk factors for the AIDS virus and asked to inform the nurse if she believes she is at risk. She should be told that she does not have to say why she may be at risk, only that she thinks she might be.
Counseling for HIV Testing: Counseling before and after HIV testing is standard nursing practice today. It is a nursing responsibility to assess a woman’s understanding of the information such a test would provide and to be sure the woman thoroughly understands the emotional, legal, and medical implications of a positive or negative test before she is ready to take an HIV test.
Given the strong social stigma attached to HIV infection, nurses must consider the issue of confidentiality and documentation before providing counseling and offering HIV testing to clients.
Unless rapid testing is done, there is generally a 1- to 3-week waiting period after testing for HIV, which can be a very anxious time for the woman. It is helpful if the nurse informs her that this time period between blood drawing and test results is routine. Test results, whatever they are, always must be communicated in person, and women need to be informed in advance that such is the procedure. Whenever possible, the person who provided the pretest counseling also should tell the woman her test results. Some women, when informed of negative results, may escalate their risk behaviors because of an equating of negativity with immunity. Others may believe that negative means “bad” and positive means “good.” Women’s reactions to a negative test should be explored, such as by asking, “How do you feel?” HIV-negative result counseling sessions are another opportunity to provide education. Emphasis can be placed on ways in which a woman can remain HIV free. She should be reminded that if she has been exposed to HIV in the past 6 months, she should be retested, and that if she continues high risk behaviors, she should have ongoing testing.
In posttest counseling to an HIV-positive woman, privacy with no interruptions is essential. Adequate time for the counseling sessions also should be provided. The nurse should make sure that the woman understands what a positive test means and review the reliability of the test results. Risk reduction practices should be reemphasized. Referral for appropriate medical evaluation and follow-up should be made, and the need or desire for psychosocial or psychiatric referrals should be assessed.
The importance of early medical evaluation so that a baseline assessment can be made and prophylactic medication begun should be stressed. If possible, the nurse should make a referral or appointment for the woman at the posttest counseling session.
Management
During the initial contact with an HIV-infected woman, the nurse should establish what the woman knows about HIV infection and that she is being cared for by a medical practitioner or facility with expertise in caring for persons with HIV infections, including AIDS. Psychologic referral also may be indicated. Resources such as counseling for financial assistance, legal advocacy, suicide prevention, and death and dying may be appropriate. All women who are drug users should be referred to a substance-abuse program. A major focus of counseling is prevention of transmission of HIV to partners.
Nurses counseling seropositive women wishing contraceptive information can recommend oral contraceptives and latex condoms or tubal sterilization or vasectomy and latex condoms. For women who are HIV infected, the diaphragm is classified as having more risks than advantages; the IUD appears safe for selected women (World Health Organization [WHO], 2004). Suggest female condoms or abstinence to women whose male partners refuse to use condoms.
No cure is available for HIV infections at this time. Rare and unusual diseases are characteristic of HIV infections. Opportunistic infections and concurrent diseases are managed vigorously with treatment specific to the infection or disease. Routine gynecologic care for HIV-positive women should include a pelvic examination every 6 months. Thorough Pap screening is essential because of the greatly increased incidence of abnormal findings on examination (CDC et al., 2006). In addition, HIV-positive women should be screened for syphilis, gonorrhea, chlamydia, and other vaginal infections and treated if infections are present. General prevention strategies are an important part of care (e.g., smoking cessation, sound nutrition) as is antiretroviral therapy. Discussion of the medical care of HIV-positive women or women with AIDS is beyond the scope of this chapter because of the rapidly changing recommendations. The reader is referred to the CDC (www.cdc.gov), AIDS hotline (800-342-2437), and Internet websites such as HIV/AIDS Treatment Information Service (www.hivatis.org) for the current information and recommendations.
HIV and Pregnancy
HIV counseling and testing should be offered to all women at their initial entry into prenatal care as part of routine prenatal testing unless the woman opts out of the screening (Branson, Handsfield, Lampe, Janssen, Taylor, Lyss, et al., 2006; USPSTF, 2007b.) Universal testing is recommended versus selective testing for maternal HIV because it results in a greater number of
women being screened and treated and can reduce the likelihood of perinatal transmission and maintain the health of the woman (American Academy of Pediatrics Committee on Pediatric AIDS, 2008). The CDC also recommends retesting in the third trimester for women known to be at high risk for HIV and rapid HIV testing in labor for women with unknown HIV status (Branson et al.).
Perinatal transmission of HIV has decreased significantly in the past decade because of the administration of antiretroviral prophylaxis (e.g., zidovudine) to pregnant women in the prenatal and the perinatal periods. Treatment of HIV-infected women with the triple-drug antiviral therapy or highly active antiretroviral therapy (HAART) during pregnancy has been reported to decrease the mother-to-child transmission to 1% to 2% (Volmink, Siegfried, van der Merwe, & Brocklehurst, 2007). All HIV-infected women should be treated with a combination of antiretroviral drugs (e.g., HAART) during pregnancy, regardless of their CD4 cell counts (Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, 2010). Data are insufficient to support or refute the teratogenic risk of antiretroviral medications given for prophylaxis in the first 10 weeks or pregnancy. Current research does not support major teratogenic effects for most of the antiretroviral agents (Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, 2010). Pregnant women already receiving antiretroviral treatment should continue their regimen, except the use of efavirenz should be avoided. Women who are HIV-infected and need treatment for their own health should start the therapy as soon as possible, even in the first trimester. Women who are taking the therapy as prophylaxis usually start therapy after the first trimester (Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, 2010).
Antiviral therapy is administered orally and is continued throughout pregnancy. The major side effect of this therapy is bone marrow suppression. Periodic hematocrit, white blood cell count, and platelet count assessments should be performed (Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, 2010). Women who are HIV positive should also be vaccinated against hepatitis B, pneumococcal infection, Haemophilus influenzae type B, and viral influenza. To support any pregnant woman’s immune system, appropriate counseling is provided about optimal nutrition, sleep, rest, exercise, and stress reduction. Use of condoms is encouraged to minimize further exposure to HIV if her partner is the source.
In the intrapartum period, antiretroviral therapy and cesarean birth are recommended to prevent vertical transmission of HIV (Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, 2010). The Panel recommends a scheduled cesarean birth at 38 weeks of gestation for women with a viral load of more than 1000 copies/ml. A vaginal birth may be an option for HIV-infected women who have a viral load of less than 1000 copies/ml at 36 weeks, if a woman has ruptured membranes and labor is progressing rapidly, or if she declines a cesarean birth. Intravenous zidovudine is recommended for all HIV-infected pregnant women during the intrapartum period. The drug is administered 3 hours before a scheduled cesarean birth and is continued until the baby is born. It should be given during labor if the woman is having a vaginal birth (Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, 2010). Fetal scalp electrode and scalp pH sampling should be avoided because these procedures may result in inoculation of the virus into the fetus. Similarly, the use of forceps or vacuum extractor should be avoided when possible. Infants should receive oral zidovudine for 6 weeks after birth. Avoidance of breastfeeding is recommended in the United States and most developed countries (American Academy of Pediatrics Committee on Pediatric AIDS, 2008).
Women who have HIV but who are without symptoms may have an unremarkable postpartum course. Immunosuppressed women with symptoms may be at increased risk for postpartum urinary tract infections (UTIs), vaginitis, postpartum endometritis, and poor wound healing. Good perineal hygiene should be stressed. Women who are HIV positive but who were not on antiretroviral drugs before pregnancy should be tested in the postpartum period to determine whether therapy that was initiated in pregnancy should be continued (Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, 2010). After the initial bath the newborn can be with the mother. In planning for discharge, comprehensive care and support services will need to be arranged. After discharge the woman and her infant are referred to physicians who are experienced in the treatment of HIV and AIDS and associated conditions for intensive monitoring and follow-up (Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, 2010).
Vaginal Infections
Vaginal discharge and itching of the vulva and vagina are among the most frequent reasons a woman seeks help from a health care provider. More women complain of vaginal discharge than of any other gynecologic symptom. Vaginal discharge resulting from infection must be distinguished from normal secretions. Women who have adequate endogenous or exogenous estrogen will have vaginal secretions. Normal vaginal secretions, or leukorrhea, are clear to cloudy in appearance and may turn yellow after drying; the discharge is slightly slimy, is nonirritating, and has a mild, inoffensive odor. Normal vaginal secretions are acidic, with a pH range of 4 to 5. Normal vaginal secretions contain lactobacilli and epithelial cells. The amount of leukorrhea differs with phases of the menstrual cycle, with greater amounts occurring at ovulation and just before menses. Leukorrhea also is increased during pregnancy.
The most common vaginal infections are bacterial vaginosis (BV), candidiasis, and trichomoniasis. Vulvovaginitis, or inflammation of the vulva and vagina, may be caused by vaginal infection or copious amounts of leukorrhea, which can cause maceration of tissues. Chemical irritants, allergens, and foreign bodies that produce inflammatory reactions can also cause vulvovaginitis.
Bacterial Vaginosis
Bacterial vaginosis (BV), formerly called nonspecific vaginitis, Haemophilus vaginitis, or Gardnerella, is the most common type of vaginitis today (Eckert & Lentz, 2007a). BV is associated with preterm labor and birth. The exact etiology of BV is unknown. It is a syndrome in which normal H2O2-producing lactobacilli are replaced with high concentrations of anaerobic bacteria (Gardnerella and Mobiluncus). With the proliferation of anaerobes, the level of vaginal amines is increased, and the normal acidic pH of the vagina is altered. Epithelial cells slough, and numerous bacteria attach to their surfaces (clue cells). When the amines are volatilized, the characteristic odor of BV occurs.
Many women with BV complain of the characteristic “fishy odor.” The odor may be noticed by the woman or her partner after heterosexual intercourse because semen releases the vaginal amines. When present, the BV discharge is usually profuse, thin, and white or gray, or milky in appearance. Some women also may experience mild irritation or pruritus.
Screening and Diagnosis
A focused history may help distinguish BV from other vaginal infections if the woman is symptomatic. Reports of fishy odor and increased thin vaginal discharge are most significant, and a report of increased odor after intercourse is also suggestive of BV.
Microscopic examination of vaginal secretions is always performed (Table 7-4). Both normal saline and 10% potassium hydroxide (KOH) smears are made. The presence of clue cells (vaginal epithelial cells coated with bacteria) on wet saline smear is highly diagnostic because the phenomenon is specific to BV. Test vaginal secretions for pH and amine odor. Nitrazine paper is sensitive enough to detect a pH of 4.5 or greater. The fishy odor of BV will be released when KOH is added to vaginal secretions on the lip of the withdrawn speculum.
TABLE 7-4
WET SMEAR TESTS FOR VAGINAL INFECTIONS
| INFECTION | TEST | POSITIVE FINDINGS |
| Trichomoniasis | Saline wet smear (vaginal secretions mixed with normal saline on a glass slide) | Presence of many white blood cell protozoa |
| Candidiasis | Potassium hydroxide (KOH) prep (vaginal secretions mixed with KOH on a glass slide) | Presence of hyphae and pseudohyphae (buds and branches of yeast cells) |
| Bacterial vaginosis | Normal saline smear | Presence of clue cells (vaginal epithelial cells coated with bacteria) |
| Whiff test (vaginal secretions mixed with KOH) | Release of fishy odor |
Management
Treatment of bacterial vaginosis with oral metronidazole (Flagyl) is most effective (CDC et al., 2006). Table 7-5 outlines treatment guidelines. Side effects of metronidazole are numerous, including sharp, unpleasant metallic taste in the mouth; furry tongue; central nervous system reactions; and urinary tract disturbances. When oral metronidazole is taken, the woman is advised not to drink alcoholic beverages, or she will experience the severe side effects of abdominal distress, nausea, vomiting, and headache. Gastrointestinal symptoms are common whether alcohol is consumed or not. Treatment of sexual partners is not routinely recommended (CDC et al.).
TABLE 7-5
VAGINAL INFECTIONS AND DRUG THERAPIES FOR WOMEN
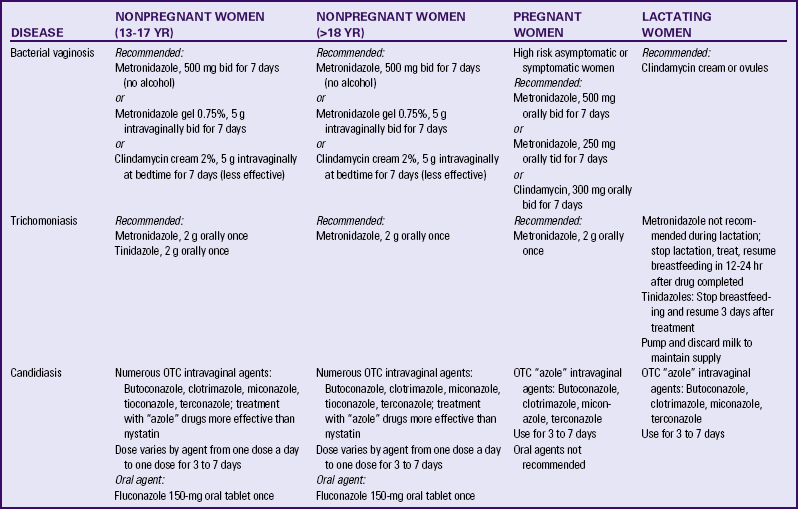
bid, Twice daily; OTC, over-the-counter; tid, three times daily.
Source: Centers for Disease Control and Prevention, Workowski, K., & Berman, S. (2006). Sexually transmitted diseases treatment guidelines 2006. Morbidity and Mortality Weekly Report, 55(RR-11), 1-94.
Metronidazole crosses the placenta but does not pose a major teratogenic risk if used for short durations. Metronidazole is excreted into breast milk; however, limited studies have demonstrated that the risk of adverse effects on the infant is remote (Weiner & Buhimschi, 2009).
Candidiasis
Vulvovaginal candidiasis (VVC), or yeast infection, is the second most common type of vaginal infection in the United States. Although vaginal candidiasis infections are common in healthy women, those seen in women with HIV infection are often more severe and persistent. Genital candidiasis lesions may be painful coalescing ulcerations necessitating continuous prophylactic therapy.
The most common organism is Candida albicans; estimates indicate that more than 90% of the yeast infections in women are caused by this organism. However, in the past 10 years, the incidence of non–C. albicans infections has risen steadily. Women with chronic or recurrent infections often are infected with these organisms (Eckert & Lentz, 2007a).
Numerous factors have been identified as predisposing a woman to yeast infections, including antibiotic therapy, particularly broad-spectrum antibiotics such as ampicillin, tetracycline, cephalosporins, and metronidazole; diabetes, especially when uncontrolled; pregnancy; obesity; diets high in refined sugars or artificial sweeteners; use of corticosteroids and exogenous hormones; and immunosuppressed states. Clinical observations and research have suggested that tight-fitting clothing and underwear or pantyhose made of nonabsorbent materials create an environment in which a vaginal fungus can grow.
The most common symptom of yeast infections is vulvar and possibly vaginal pruritus. The itching can be mild or intense, interfere with rest and activities, and may occur during or after intercourse. Some women report a feeling of dryness. Others may experience painful urination as the urine flows over the vulva, which usually occurs in women who have excoriations resulting from scratching. Most often the discharge has a thick, white, lumpy, and cottage cheese–like consistency. The discharge may be found in patches on the vaginal walls, cervix, and labia. Commonly, the vulva is red and swollen, as are the labial folds, vagina, and cervix. Although there is not a characteristic odor with yeast infections, sometimes a yeasty or musty smell can be detected.
Screening and Diagnosis
In addition to a complete history of the woman’s symptoms, their onset, and course, the history is a valuable screening tool for identifying predisposing risk factors. Physical examination should include a thorough inspection of the vulva and vagina. A speculum examination is always done. Commonly health care practitioners will obtain saline and KOH wet smears and check vaginal pH (see Table 7-4). Vaginal pH is normal with a yeast infection; if the pH is greater than 4.5, trichomoniasis or BV should be suspected. The characteristic pseudohyphae (bud or branching of a fungus) may be seen on a wet smear done with normal saline; however, they may be confused with other cells and artifacts (CDC et al., 2006).
Management
A sizable number of antifungal preparations are available for the treatment of C. albicans infection. Intravaginal agents include miconazole, clotrimazole, butoconazole, tioconazole, terconazole, and nystatin; fluconazole is an effective oral agent (CDC et al., 2006). Many of these vaginal medications (e.g., Monistat, Gyne-Lotrimin) are available over the counter (OTC). Exogenous lactobacillus (in the form of dairy products [yogurt] or powder, tablet, capsule, or suppository supplements) and garlic have been suggested for prevention and treatment of vulvovaginal candidiasis, but research is inconclusive, and no recommendations have been developed for use in practice (Eckert & Lentz, 2007a). ![]() The first time a woman suspects that she may have a yeast infection, she should see a health care provider for confirmation of the diagnosis and treatment recommendation. If she experiences another infection, she may wish to purchase an OTC preparation and self-treat; if she chooses to do so, she should always be counseled regarding seeking care for numerous recurrent or chronic yeast infections. If vaginal discharge is extremely thick and copious, vaginal debridement with a cotton swab followed by application of vaginal medication is useful.
The first time a woman suspects that she may have a yeast infection, she should see a health care provider for confirmation of the diagnosis and treatment recommendation. If she experiences another infection, she may wish to purchase an OTC preparation and self-treat; if she chooses to do so, she should always be counseled regarding seeking care for numerous recurrent or chronic yeast infections. If vaginal discharge is extremely thick and copious, vaginal debridement with a cotton swab followed by application of vaginal medication is useful.
Women who have extensive irritation, swelling, and discomfort of the labia and vulva may find sitz baths helpful in decreasing inflammation and increasing comfort. Adding colloidal oatmeal powder to the bath may also increase the woman’s comfort. Not wearing underpants to bed may help decrease symptoms and prevent recurrences. Completing the full course of treatment prescribed is essential to removing the pathogen. Instruct women to continue the medication even during menstruation. Explain that they should avoid using tampons during menses because the tampon will readily absorb the medication. If possible, women should avoid intercourse during treatment; if abstinence is not feasible, the woman’s partner should use a condom to prevent the introduction of more organisms (see Teaching for Self-Management box: Prevention of Genital Tract Infections).
Trichomoniasis
Trichomonas vaginalis is almost always an STI and is also a common cause of vaginal infection (5% to 50% of all vaginitis) and discharge (Eckert & Lentz, 2007a).
Trichomoniasis is caused by T. vaginalis, an anaerobic one-celled protozoan with characteristic flagellae. Although trichomoniasis may be asymptomatic, commonly women have characteristically yellowish to greenish, frothy, mucopurulent, copious, malodorous discharge. Inflammation of the vulva, the vagina, or both may be present, and the woman may complain of irritation and pruritus. Dysuria and dyspareunia are often present. Typically the discharge worsens during and after menstruation. Often the cervix and the vaginal walls will demonstrate the characteristic “strawberry spots” or tiny petechiae, and the cervix may bleed on contact. In severe infections, the vaginal walls, the cervix, and occasionally the vulva may be acutely inflamed.
Screening and Diagnosis
In addition to obtaining a history of current symptoms, a careful sexual history should be obtained. Any history of similar symptoms in the past and treatment used should be noted. The nurse should determine whether the woman’s partner(s) was treated and if she has had subsequent relations with new partners.
A speculum examination is always done, even though it may be very uncomfortable for the woman; relaxation techniques and breathing exercises may help the woman with the procedure. Any of the classic signs may be present on physical examination. The typical one-celled flagellate trichomonads are easily distinguished on a normal saline wet prep. Trichomoniasis also may be identified on Pap tests. Because trichomoniasis is an STI, once diagnosis is confirmed, appropriate laboratory studies for other STIs should be carried out.
Management
The recommended treatment is metronidazole or tinidazole (CDC et al., 2006) (see Table 7-5). Although the male partner is usually asymptomatic, it is recommended that he receive treatment also because he often harbors the trichomonads in the urethra or prostate. It is important that nurses discuss the importance of partner treatment with their clients because if they are not treated, it is likely that the infection will recur.
Women with trichomoniasis need to understand the sexual transmission of this disease. The woman must know that the organism may be present without symptoms being present, perhaps for several months, and that it is not possible to determine when she became infected. Women should be informed of the necessity for treating all sexual partners and helped with ways to raise the issue with their partner(s).
Group B Streptococci
Group B streptococci (GBS) may be considered a part of the normal vaginal flora in a woman who is not pregnant, and it is present in 20% to 30% of healthy pregnant women. GBS infection has been associated with poor pregnancy outcomes. Furthermore, GBS infections are an important factor in neonatal morbidity and mortality, usually resulting from vertical transmission from the birth canal of the infected mother to the infant during birth (Cunningham, Leveno, Bloom, Hauth, Rouse, & Sprong, 2010).
Risk factors for neonatal GBS infection include positive prenatal culture for GBS in the current pregnancy; preterm birth of less than 37 weeks of gestation; premature rupture of membranes for a duration of 18 hours or more; intrapartum maternal fever higher than 38° C; and a positive history for early-onset neonatal GBS (Cunningham et al., 2010).
To decrease the risk of neonatal GBS infection, it is recommended that all women be screened at 36 to 37 weeks of gestation for GBS using a rectovaginal culture, and that intravenous antibiotic prophylaxis (IAP) be offered during labor to all who test positive. If a culture is not available at onset of labor or if a risk factor is present, IAP is also offered. IAP is not recommended before a cesarean birth if labor or rupture of membranes has not occurred. The recommended treatment is penicillin G, 5 million units intravenous (IV) loading dose, and then 2.5 million units IV every 4 hours during labor. Ampicillin, 2 g IV loading dose, followed by 1 g IV every 4 hours, is an alternative therapy (CDC, 2008a).
Effects of Sexually Transmitted Infections on Pregnancy and the Fetus
Sexually transmitted infections in pregnancy are responsible for significant morbidity and mortality. Some consequences of maternal infection, such as infertility and sterility, last a lifetime. Congenitally acquired infection may affect a child’s length and quality of life. Table 7-6 describes the effects of several common STIs on pregnancy and the fetus. It is difficult to predict these effects with certainty. Factors such as coinfection with other STIs and, when in pregnancy, the infection was acquired and treated can affect outcomes.
TABLE 7-6
PREGNANCY AND FETAL EFFECTS OF COMMON SEXUALLY TRANSMITTED INFECTIONS
| INFECTION | MATERNAL EFFECTS | FETAL EFFECTS |
| Chlamydia | Premature rupture of membranes Preterm labor Postpartum endometritis |
Low birth weight |
| Gonorrhea | Miscarriage Preterm labor Premature rupture of membranes Amniotic infection syndrome Chorioamnionitis Postpartum endometritis Postpartum sepsis |
Preterm birth IUGR |
| Group B streptococci | Urinary tract infection Chorioamnionitis Postpartum endometritis Sepsis Meningitis (rare) |
Preterm birth |
| Herpes simplex virus | Intrauterine infection (rare) | Congenital infection (rare) |
| Human papillomavirus (HPV) | Dystocia from large lesionsExcessive bleeding from lesions after birth trauma | None known |
| Syphilis | Miscarriage Preterm labor |
IUGR Preterm birth Stillbirth Congenital infection |
IUGR, Intrauterine growth restriction.
Source: Gilbert, E. (2011). Manual of high risk pregnancy & delivery (5th ed.). St. Louis: Mosby; Duff, P., Sweet, R., & Edwards, R. (2009). Maternal and fetal infections. In R. Creasy, R. Resnik, J. Iams, C. Lockwood, & T. Moore (Eds.), Creasy and Resnik’s maternal-fetal medicine: Principles and practice (6th ed.). Philadelphia: Saunders.
TORCH Infections
Toxoplasmosis, other infections (e.g., hepatitis), rubella virus, cytomegalovirus (CMV), and herpes simplex virus, known collectively as TORCH infections, form a group of organisms capable of crossing the placenta. TORCH infections can affect a pregnant woman and her fetus. Generally, all TORCH infections produce influenza-like symptoms in the mother, but fetal and neonatal effects are more serious. TORCH infections and their maternal and fetal effects are shown in Table 7-7. Neonatal effects are discussed in Chapter 35. The following discussion focuses on infections not previously discussed.
TABLE 7-7
TORCH INFECTION: MATERNAL AND FETAL
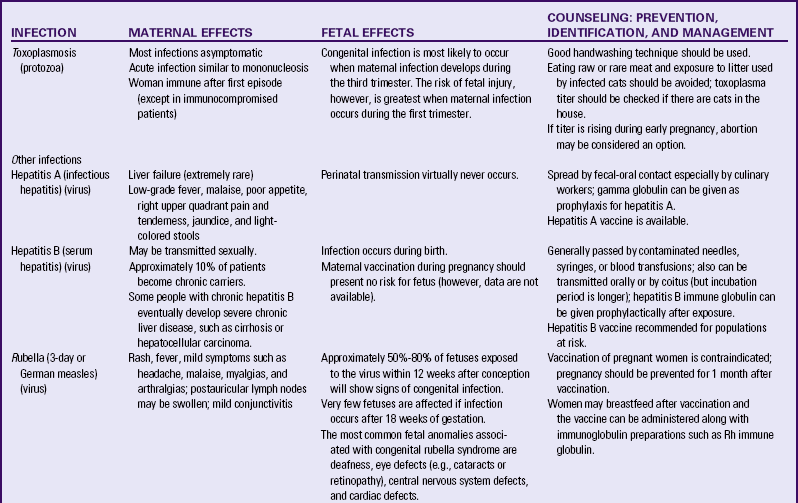
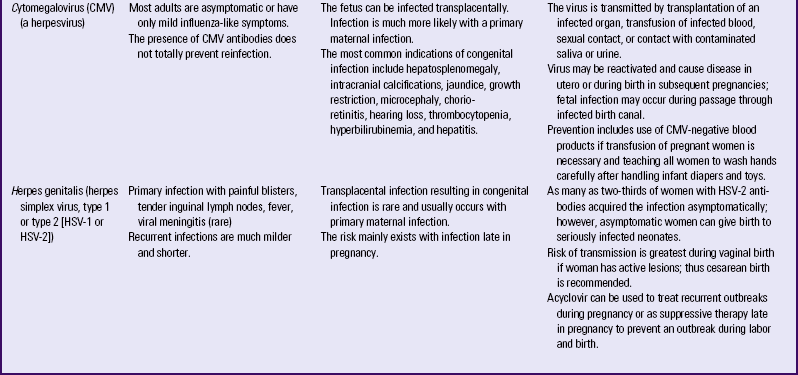
Source: Duff, P., Sweet, R., & Edwards, R. (2009). Maternal and fetal infections. In R. Creasy, R. Resnik, J. Iams, C. Lockwood, & T. Moore (Eds.), Creasy and Resnik’s maternal-fetal medicine: Principles and practice (6th ed.). Philadelphia: Saunders.
Toxoplasmosis
Toxoplasmosis is a protozoal infection associated with the consumption of infested raw or undercooked meat and with poor handwashing after handling infected cat litter. Pregnant women with HIV antibodies are at higher risk because toxoplasmosis is a common accompanying opportunistic infection. The presence of toxoplasmosis can be determined through blood studies, although laboratory diagnosis is difficult. Women at risk for infection should have toxoplasmosis titers evaluated. Acute infection in pregnancy produces influenza-like symptoms and lymphadenopathy in some women but no symptoms in others. Miscarriage may occur.
The treatment of choice for toxoplasmosis is spiramycin, sulfadine, or a combination of pyrimethamine and sulfadiazine. Treatment of the pregnant woman may reduce the risk of congenital toxoplasmosis (Cunningham et al., 2010).
Other Infections
The primary infection included in the category of other infections is hepatitis, which was discussed previously. Infections other than hepatitis also may be identified as “other” TORCH infections. These include GBS, varicella, and HIV.
Rubella
Rubella, also called German measles or 3-day measles, is a viral infection transmitted by droplets (such as from an infected person’s sneeze). Rash, muscle aches, joint pain, and mild lymphedema are usually seen in the infected mother. Consequences for the fetus are much more serious and include miscarriage, congenital anomalies (referred to as congenital rubella syndrome), and death. Vaccination of pregnant women is contraindicated because a rubella infection may develop after the live vaccine is administered. Rubella vaccine is given to women who are not immune as part of preconception counseling or in the postpartum period prior to discharge, with instructions to use contraception for at least 1 month after vaccination (ACOG, 2002).
Cytomegalovirus
Maternal infection with CMV may begin as a mononucleosis-like syndrome. In most adults the onset of CMV infection is uncertain and asymptomatic; however, the disease may become a chronic persistent infection. Approximately 60% of the adult population has antibodies to CMV. This virus is primarily transmitted by close contact but also has been isolated from semen, cervical and vaginal secretions, breast milk, placental tissue, urine, feces, and banked blood. Maternal CMV infection may be diagnosed by presence of CMV in urine or in serum, because many women have evidence of CMV infection. Women who show CMV infection in pregnancy (by positive viral titers) usually have chronic or recurrent infections (Yudkin & Gonik, 2006).
Women at risk for infection include those who work in or have children in daycare centers and women with compromised immune systems.
In the United States, 1% to 2% of infants have congenital CMV infection. Fetal infection can cause microcephaly; eye, ear, and dental defects; and mental retardation. No treatment is available during pregnancy.
Care Management
Women may delay seeking care for STIs and other infections because they fear social stigma, have little accessibility to health care services, are asymptomatic, or are unaware that they have an infection. A comprehensive assessment focuses on lifestyle issues that are often personal or sensitive. A culturally sensitive, nonjudgmental approach is essential to facilitate accurate data collection (see Nursing Process box: Woman with a Sexually Transmitted Infection).
The woman with an STI will need encouragement to seek care at the earliest stage of symptoms. Counseling women about STIs is essential for (1) preventing new infections or reinfection; (2) increasing compliance with treatment and follow-up; (3) providing support during treatment; and (4) assisting women in discussions with their partner(s). Women must be made aware of the serious potential consequences of STIs and the behaviors that increase or decrease the likelihood of infection.
The nurse must make sure that the woman understands what infection she has, how it is transmitted, and why it must be treated (see Teaching for Self-Management box: Sexually Transmitted Infections).
Addressing the psychosocial component of STIs is essential. A woman may be afraid or embarrassed to tell her partner or to ask her partner to seek treatment. She may be embarrassed to admit her sexual practices, or she may be concerned about confidentiality. The nurse may need to help the woman deal with the effect of a diagnosis of an STI on a committed relationship, because the woman is now faced with the necessity of dealing with “uncertain monogamy.”
In many instances sexual partners should be treated; thus the infected woman is asked to identify and notify all partners who might have been exposed. Often she will find this difficult to do. Empathizing with the woman’s feelings and suggesting specific ways of talking with partners will help decrease anxiety and assist in efforts to control infection. For example, the nurse
might suggest that the woman say, “I care about you and I’m concerned about you. That’s why I’m calling to tell you that I have a sexually transmitted infection. My clinician will be happy to talk with you if you would like.” Offering literature and role-playing situations with the client also may be of assistance. It is often helpful to remind the woman that although this is an embarrassing situation, most persons would rather know than not know that they have been exposed. Health professionals who take time to counsel their clients on how to talk with their partner(s) can improve compliance and case findings.
Interrupting the transmission of infection is crucial to STI control. For treatable and vaccine-preventable STIs, further transmission and reinfection can be prevented with referral of sex partners. Many STIs are reportable; all states require that the five traditional STIs—gonorrhea, syphilis, chancroid, lymphogranuloma venereum, and granuloma inguinale—be reported to public health officials. Many other states require that other STIs such as chlamydial infections, genital herpes, and genital warts be reported. In addition, all states require that AIDS cases be reported; 35 states require that HIV infection be reported.
Infection Control
Infection-control measures are essential to protect care providers and to prevent health personnel–related infection of clients, regardless of the infectious agent. The risk for occupational transmission varies with the disease. Even when the risk is low, as with HIV, the existence of any risk warrants reasonable precautions. Precautions against airborne disease transmission are available in all health care agencies. Standard Precautions (precautions to use in care of all persons for infection control) and additional precautions for labor and birth settings are listed in Box 7-3.
KEY POINTS
• Reproductive tract infections include STIs and common genital tract infections.
• Risk-reduction sexual practices are key STI-prevention strategies.
• HIV is transmitted through body fluids, primarily blood, semen, and vaginal secretions.
• Prevention of mother-to-newborn HIV transmission is most effective when the woman receives antiretroviral drugs during pregnancy and labor and birth, and the infant receives the drugs after birth.
• HPV is the most common viral STI.
• Syphilis has reemerged as a common STI, affecting African-American women more than any other ethnic or racial group.
• Chlamydia is the most common STI in women in the United States and the most common cause of PID.
• Viral hepatitis has several forms of transmission; HBV infections carry the greatest risk.
• Young, sexually active women who do not practice risk-reducing sexual behaviors and have multiple partners are at greatest risk for STIs and HIV.
• STIs are responsible for substantial mortality and morbidity, great personal suffering, and heavy economic burden in the United States.
• STIs and vaginitis are biologic events for which all individuals have a right to expect objective, compassionate, and effective health care.
• Pregnancy confers no immunity against infection, and both mother and fetus must be considered when the pregnant woman contracts an infection.
• Because history and examination cannot reliably identify everyone with HIV or other blood-borne pathogens, blood and body-fluid precautions should be used consistently for everyone all the time.
![]() Audio Chapter Summaries Access an audio summary of the Key Points on
Audio Chapter Summaries Access an audio summary of the Key Points on ![]()