CHAPTER 8 Calculating in paediatrics
Learning outcomes
In relation to children:
•
Be able to interpret a range of prescriptions for oral and parenteral medicines
•
Be able to interpret a range of labels used for oral and parenteral medicines
•
Understand the use of body weight and body surface area in calculating drug doses
•
Appreciate the importance of precision in calculating drug doses
•
Through practice, gain confidence in calculating accurately the quantity to give based on: (a) ‘prescriptions’ and ‘labels’, (b) information in abbreviated form
Introduction
Children are not small adults, and the delivery of safe and effective drug therapy presents challenges for all those involved in their care. Great progress has been made over the years to help to ensure that children (in the developed world) have access to the medicines best suited to their care. Team working is always the key to achieving good outcomes for patients. Nurses are central to all the processes needed to ensure effective medicines management in paediatric practice. Accurate calculation of drug doses is a prerequisite.
Key aspects
Key aspects in the safe and effective use of medicines in paediatric practice can be summarised as follows.
•
Only give medicines when fully justified, having considered the potential risks/benefits, and any legal implications (e.g. using drugs outwith terms of product licence). Always consider alternatives
•
Children should, whenever possible, be involved in decisions relating to the use and taking of medicines
•
Calculations may be complex especially when using body weight or body surface area to calculate the dose
•
Take care to avoid measuring errors by using the correct equipment (small quantities are often involved)
•
Use the most suitable formulation/presentation (some products may be used in an unorthodox manner)
•
Some medicines used to treat children may not be licensed for the purpose. The Medicines Act does not prohibit this but the prescriber must be aware of the implications
•
Always be aware that patients at extremes of age are more vulnerable to adverse drug reactions than other patients
•
It is essential for paediatric nurses to keep their skills and knowledge up to date (
NMC 2008) particularly in respect of the atypical drugs and doses that may be encountered
Response to medicines
Children and particularly neonates (up to 28 days old) respond to medicines differently from adults. Great care must be exercised in calculating doses, particularly in the neonatal period as a reduced rate of clearance of the drug or metabolites increases the risk of toxicity. Where required, the total daily dose of a medicine can be reduced by either reducing individual doses or increasing the interval between doses. For certain medicines, young children may need a higher dose per kilogram or body surface area (m2) than adults because of their higher metabolic rate. In such cases, the dose should never exceed the usual adult dose.
Renal impairment
A detailed discussion of the issues involved here is beyond the scope of this publication. The following principles should be borne in mind.
•
Glomerular filtration rate (GFR) is low at birth but increases rapidly in the first 6 months and gradually thereafter to reach adult levels by 1–2 years of age (see
Table 8.1)
•
Patients with renal impairment are very intolerant of some drugs
•
The
British National Formulary for Children (
BNFC) (2009) includes guidance on the calculation of creatinine clearance (a proxy for GFR). The MDRD equation (see
p. 185) should not be used for dosage adjustment in children
Table 8.1 Development of renal function
| Age |
GFR (mL/min) approx. |
| < 37 weeks |
<25 |
| Neonate |
15–35 |
| 1–2 weeks |
35–60 |
| 2–4 months |
60–80 |
| 6–12 months |
80–110 |
| 12 months → adult |
85–150 |
Paediatric medicines
•
As with all medicines, always use products that have been prepared and tested under rigorously controlled conditions. This will ensure the integrity and stability of the medicine
•
Special paediatric formulations should be used where available. However, many medicines used in paediatrics have been formulated primarily for adults. Pharmacy may be able to provide specially prepared formulations in a form and strength to meet an individual patient’s needs. This will help to reduce the requirement for complex calculations prior to administration
•
Very often, a liquid oral preparation will be required. It may be important to use a ‘sugar-free’ preparation and avoid products which contain certain excipients
•
Novel preparations such as straws containing a medicine may be useful (see clarithromycin,
BNFC 2009)
Oral route
The oral route is the most common route of administration in children and should be used where available. It is associated with less pain and anxiety, and is more cost effective than a parenteral route. It is also more convenient and less time-consuming, it requires less equipment and the need to undertake calculations may be reduced. Many children can swallow tablets and capsules but a liquid preparation may be preferred. Prescriptions for liquid preparations should include the dose in milligrams, micrograms or nanograms and not just the volume to be given. The choice between liquid and solid oral dose will depend on product availability or personal preferences. Crushing tablets or opening capsules not specifically designed for this purpose renders their use unlicensed (NMC 2008). On some occasions, it may be necessary to use a medicine in an unorthodox way, for example, administering an injectable product orally. Further advice should be sought from the pharmacy. Some products have a high osmolality and must be diluted before administration (e.g. vitamin E suspension).
Other routes of administration
Where the oral route is contraindicated or not available, the rectal route may be used, ensuring compliance with local policies. Otherwise, parenteral therapy will be required, often by the intravenous route. Intramuscular injections should be avoided where possible as children find these distressing.
Parenteral administration is more complex and as a result presents greater risk than non-parenteral drug administration. The process involves selection of the appropriate administration device, calculating and setting the rate of infusion, and monitoring delivery. It is essential that the nurse is trained in and fully conversant with the use of the equipment.
All parenteral drug calculations should be carefully checked by a second member of staff and attention paid to the rate of administration. Where possible, it is good practice to record details of the calculation and the check. Where the contents of a vial are being reconstituted, consideration of the displacement volume is essential. If an injection requires further dilution, the appropriate diluent must be used. It is good practice to attach a label to the syringe (where a syringe driver is being used), the infusion bag or the burette chamber. Details on the label include patient’s name, ward number, name of drug additive and infusion fluid, volume, time of reconstitution, and date of expiry.
Cytotoxic therapy will normally be in accordance with national protocols. Cytotoxic preparations should always be prepared in the pharmacy. Similarly, to ensure controlled aseptic conditions, safety and accuracy, special precautions must be taken at all stages in the preparation and use of intrathecal injections.
Calculating a paediatric dose
Many medicine doses for children are determined by body weight. To determine the dose for an individual child, use the current body weight in kilograms. Care must be exercised in calculating by body weight in the obese child as higher doses than necessary may result. It is advisable in these cases to calculate from an ideal body weight related to height and age. Using aminophylline as an example:
| Normal dose |
5 mg/kg over 20 minutes |
| 5-year-old Height 108 cm |
Ideal body weight 18 kg |
| 5-year-old Height 108 cm |
Obese child weighs 21 kg |
| Using child’s ideal body weight |
Dose 5 x 18 = 90 mg |
| Using child’s actual weight |
Dose 5 x 21 = 105 mg |
It is clear that there is a significant difference between the two doses. In practice, it would be a matter for the prescriber to decide on the actual dose to prescribe.
Occasionally, doses are standardised by body surface area in square metres (m2). Paediatric doses calculated from body surface area generally reflect more accurately the patient’s needs than doses based on body weight. When a child is being treated for a chronic condition, the dose of the medicine should be reviewed at regular intervals to take account of changing age and weight.
Oral (enteral) syringes
A syringe exclusively for oral use is supplied when oral liquid medicines are prescribed in doses less than 5 mL (see also p. 60). Oral syringes are available in 1 mL, 3 mL and 5 mL, and supplied with a protective cap and adaptor, and a guidance leaflet. After shaking the medicine bottle, the bottle adaptor is inserted into the open neck of the bottle. The required dose is then drawn up into the oral syringe. The tip of the oral syringe is cautiously put into the child’s mouth and the plunger gently squeezed to run a small amount into the child’s mouth. The child is allowed to swallow before pushing the plunger again. The child is then given a drink to wash down the medicine and the syringe washed in warm soapy water, rinsed and dried. Alternatively, a graduated pipette may be used (see also p. 60).
Examples: Demonstration and practice
The demonstration examples that follow are provided as in the rest of the book so that the steps in each can be followed and understood.
The practice examples provide the opportunity to gain competence in doing calculations and thus increase confidence. Each practice example raises a question for the reader to consider. Answers are on pp. 196–197.
Whether or not a calculation is needed, care must be taken to measure the precise dose.
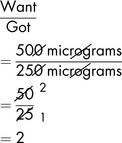
LEVEL 0 Demonstration
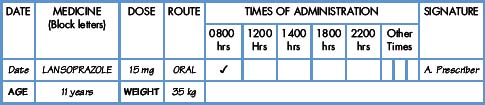
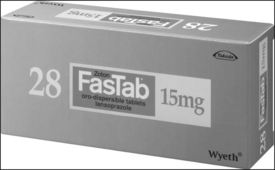
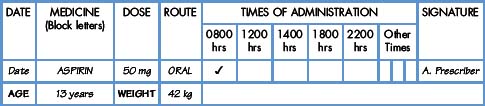
Demonstration 8.1
Commentary
•
Lansoprazole is a proton pump inhibitor used to treat gastro-oesophageal reflux disease
•
No calculation is required here since the prescribed dose corresponds to the strength on the label
The patient will be given:
One tablet (dispersed in small amount of water)
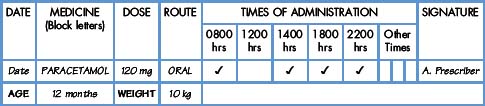
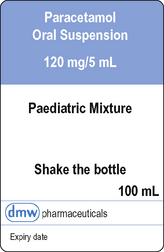
Demonstration 8.2
Commentary
•
Paracetamol is an analgesic and antipyretic
•
No calculation is required, but the dose should be carefully measured and administered using an oral syringe
•
The prescribed dose is the
same as the amount contained in 5 mL
The patient will be given:
5 mL of oral suspension
Level I Demonstration
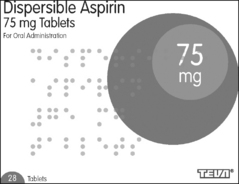
Demonstration 8.3
Commentary
•
Aspirin is an antiplatelet drug which has limited use in children owing to its association with Reye’s syndrome.
•
A solution requires to be prepared from the soluble tablets
•
One tablet is to be dissolved in 7.5 mL of water for injections
•
The prescribed dose is
less than the amount contained in one tablet
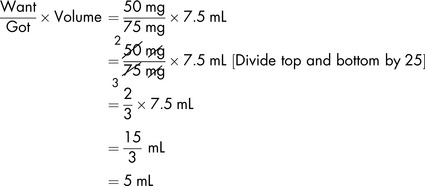
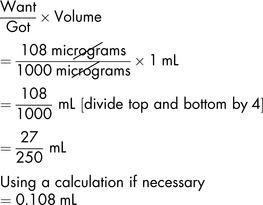
Workings
75 mg is dissolved in 7.5 mL of water
Applying the formula,
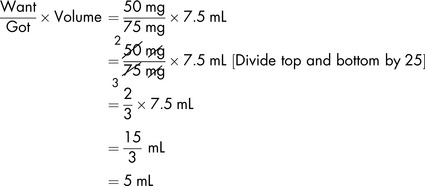
The patient will be given:
5 mL of prepared solution
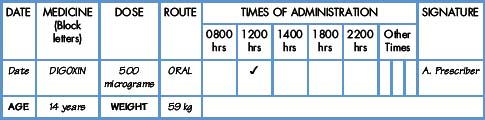
Demonstration 8.4
Commentary
•
Digoxin is a cardiac glycoside used to treat supraventricular tachycardia
•
The prescribed dose is
more than the amount contained in one tablet
Workings
Applying the formula,
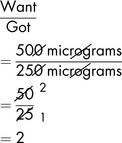
The patient will be given:
2 tablets
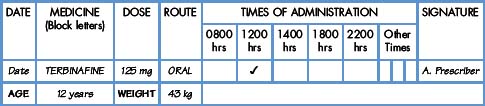
Level I Exercises
Exercise 8.1
Commentary
•
Terbinafine is an antifungal drug
What should the patient be given?
Level I Further exercises
8.2
The child is nine years old. The prescription states promethazine hydrochloride 37.5 mg orally once a day. The available tablets are 25 mg each. What should the patient be given?
8.3
Diltiazem hydrochloride is available as 60 mg modified-release tablets. The child is 14 years old and has been prescribed 30 mg 3 times daily. This product is not licensed for use in children. How would you deal with this prescription?
8.4
What should you give to an eight-year-old who has been prescribed 7.5 mg of cinnarizine every 8 hours. The strength of the tablets is 15 mg.
8.5
The patient is prescribed methylphenidate hydrochloride modified-release 54 mg once daily. The strength of the available tablets is 27 mg. How many tablets should you give?
8.6
A 30 kg 10-year-old girl with an acute exacerbation of asthma is prescribed 30 mg of oral prednisolone once daily for 3 days. How many 5 mg prednisolone tablets will she require each day?
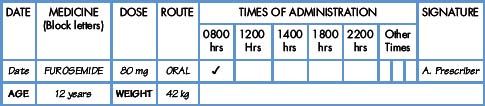
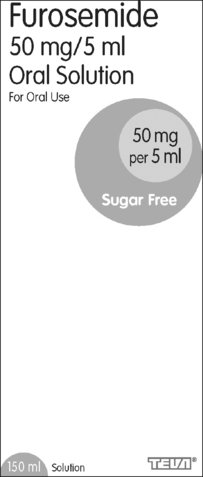
Level II Demonstration
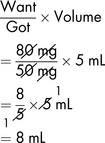
Demonstration 8.5
Commentary
•
Furosemide is a loop diuretic
•
The prescribed dose is
more than the amount contained in 5 mL
Workings
Applying the formula,
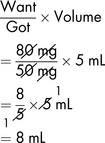
The patient will be given:
8 mL oral solution
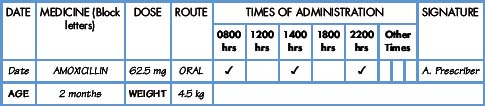
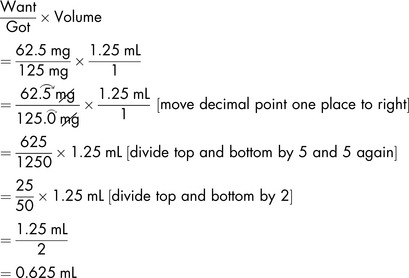
Demonstration 8.6
The medicine
Amoxicillin (Amoxil) belongs to the penicillin group. For paediatric use, it is available as a suspension (when reconstituted) containing 125 mg in 1.25 mL.
Commentary
•
Amoxicillin is a broad-spectrum antibiotic used for community-acquired infection and middle ear infections
•
The prescribed amount is
less than the amount contained in 1.25 mL
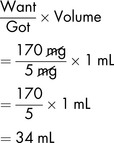
Workings
Applying the formula,
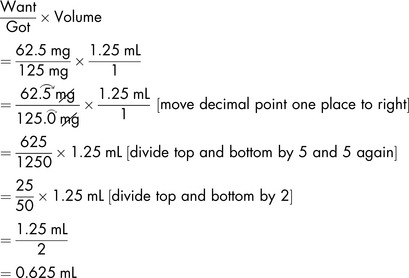
The patient will be given:
0.625 mL of suspension
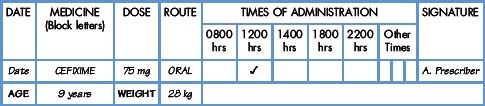
Level II Exercises
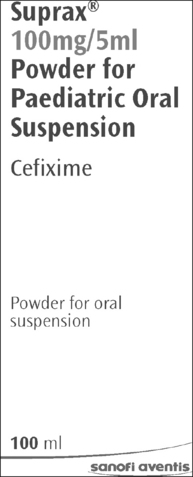
Exercise 8.7
Commentary
•
Cefixime is a cephalosporin licensed only for acute infections
What should the patient be given?
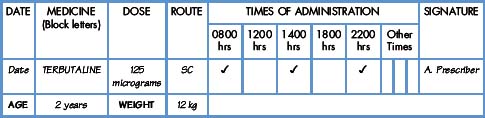
Exercise 8.8
Commentary
•
Terbutaline is a short-acting beta
2-adrenoceptor agonist used in the treatment of asthma
•
0.5 mg = 500 micrograms
What should the patient be given?
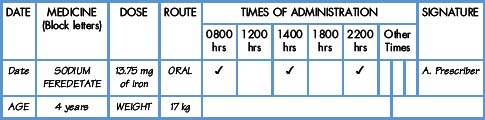
Exercise 8.9
Medicine label (27.5 mg of iron in 5 mL elixir)
Commentary
•
This medicine is used to treat iron-deficiency anaemia
What should the patient be given?
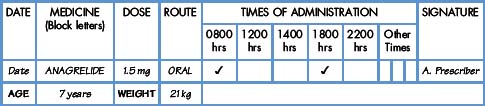
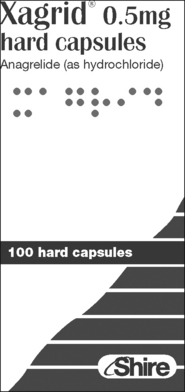
Exercise 8.10
Commentary
•
Anagrelide is used in platelet disorders where the patient is not responding to other therapy
•
Anagrelide is not licensed for use in children
What should the patient be given?
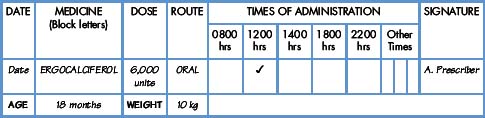
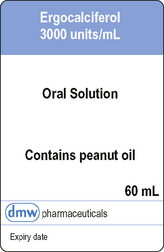
Exercise 8.11
Commentary
Ergocalciferol (vitamin D2) is used to treat vitamin D deficiency
What should the patient be given?
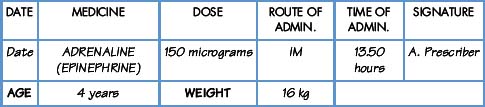
Exercise 8.12
Commentary
•
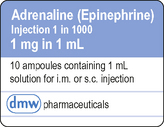
Adrenaline is used to treat anaphylactic shock and angioedema
•
A suitable syringe will be needed for such a small volume
What should the patient be given?
Level II Further exercises
8.13
A 25 kg 8-year-old boy is prescribed phenytoin 100 mg twice daily. How many mL of 30 mg/5 mL suspension will be required for each dose?
8.14
How many grams of glucose are contained in a 500 mL bag of infusion of glucose 5%?
8.15
An oral solution of ranitidine contains 75 mg/5 ml. What volume is required for a 14-year-old prescribed 150 mg twice daily?
8.16
A three-year-old weighing 15 kg is prescribed atenolol 15 mg daily to be given in two divided doses. How many mL of atenolol sugar-free syrup 25 mg/5 mL will be given for each dose?
8.17
A two-year-old 12 kg boy is prescribed 120 mg rifampicin twice daily as prophylaxis as his brother has meningococcal meningitis. How many millilitres of 100 mg/5 mL syrup will be required for each dose?
8.18
A child of 12 years is prescribed lymecycline 1.224 g daily. The medicine is available as capsules 408 mg. How many should the child be given each day?
8.19
A child of five years is prescribed ibuprofen 150 mg three times daily. What volume of ibuprofen oral suspension 100 mg in 5 mL is given?
8.20
A 30 kg child is prescribed 300 mg of azithromycin daily for 3 days. What volume of oral suspension 200 mg/5 mL is given for each dose?
8.21
A child is prescribed clonazepam orally, initially 250 micrograms at night for 4 nights. Scored clonazepam 500 microgram tablets are available. What is the child given? The child finds difficulty in taking tablets. Injection solution (1 mg/mL) can be given orally. What volume of injection solution will be given orally?
8.22
15 g of mannitol is to be given by IV infusion. What volume of mannitol 20% is required?
8.23
An ampoule of furosemide contains 20 mg/2 mL. A child is prescribed 10 mg. What volume of injection is drawn up?
8.24
What volume of a 40 mg/mL injection of gentamicin is required to provide a dose of 28 mg?
8.25
On reconstitution, a vial of benzylpenicillin injection contains 600 mg in 5 mL. What volume is measured to give 240 mg?
8.26
The patient is 7 years old and is prescribed 4 mg of pholcodine linctus, strong, 4 times daily. The linctus is available as 10 mg/5 mL. How much should the patient be given?
8.27
What volume should be given to a child of 18 months prescribed 5 mg of dicycloverine hydrochloride? The available product is 10 mg/5 mL syrup.
8.28
Phenylephrine has been prescribed for a child of 12 years in a dose of 4 mg by SC injection. The injection is available as 10 mg/mL. How much should be given?
8.29
A 4-year-old child is prescribed 2 mg of metoclopramide as a premedication 5–10 minutes before a procedure. What volume of paediatric liquid 1 mg/mL will be required?
8.30
A child is prescribed 150 micrograms of atropine. What is the volume to be administered from an injection containing 300 micrograms/mL?
8.31
The child is 6 months old and weighs 8 kg. Betamethasone sodium phosphate has been prescribed at a dose of 1 mg to be given by slow IV injection. Each ampoule is 4 mg/mL. What volume of injection would you give?
8.32
Trifluoperazine 500 micrograms syrup is prescribed for a 5-year-old 18 kg child who has severe nausea and vomiting which is unresponsive to other anti-emetics. The syrup is supplied as 1 mg/5 mL. How much would you give?
8.33
Levocetirizine hydrochloride 1.25 mg oral is prescribed for a 3-year-old weighing 15 kg. 2.5 mg/5 mL oral solution is available. What volume would you give?
8.34
Furosemide 2 mg is prescribed by IV injection. 10 mg/1 mL ampoules are available. How much would you give the patient?
8.35
The child is 4 years old and weighs 16 kg. Erythromycin 62.5 mg oral is prescribed. 125 mg/5 mL oral suspension is available. What volume would you give?
8.36
A 14-year-old boy weighing 50 kg is prescribed sevelamer 1.6 g by mouth. 800 mg tablets are available. How many tablets should be given? Although this product is not licensed for use in children under 18 years, the prescriber will take into account any ethical/legal issues that arise.
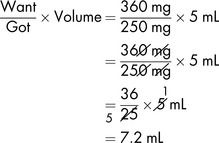
Level III Demonstration
Demonstration 8.7
Commentary
•
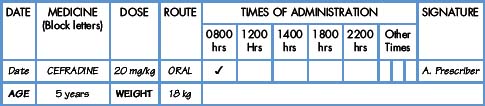
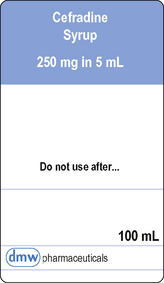
Cefradine is a cephalosporin used to treat infections due to sensitive Gram-positive and Gram-negative bacteria
Workings
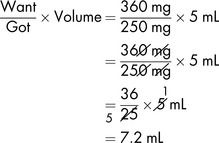
The patient will be given:
7.2 mL syrup
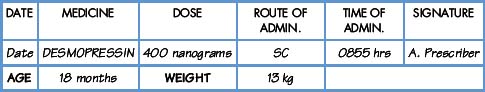
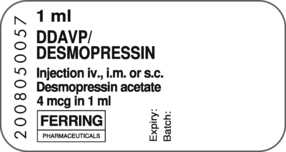
Demonstration 8.8
Commentary
•
Desmopressin injection is an antidiuretic hormone and in this dose is used in the diagnosis of diabetes insipidus
•
The prescription and the label are in different units
•
Working with nanograms calls for the utmost care
•
The sample label bears a security number
•
The prescribed dose is
less than the amount contained in 1 mL
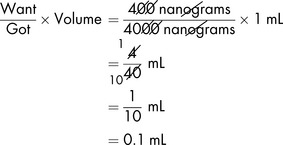
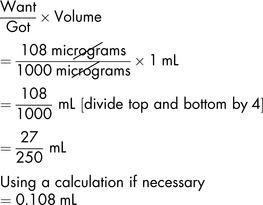
Workings
First, convert 4 micrograms to nanograms:
Applying the formula,
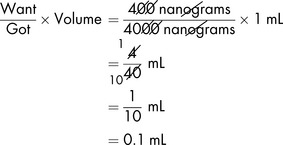
The patient will be given:
0.1 mL SC injection
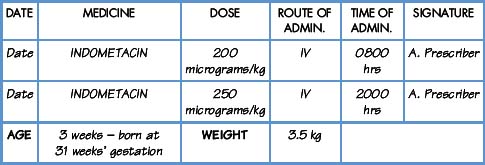
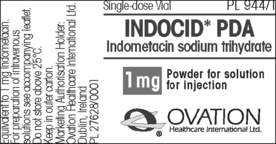
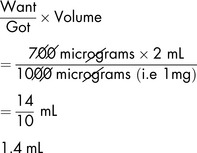
Demonstration 8.9
Commentary
•
Indometacin is used to close patent ductus arteriosus (PDA) in premature babies
•
The product literature states that 2 mL of water for injections should be used to reconstitute the 1 mg vial
Workings
| First dose |
Second dose |
| Multiply prescribed dose by patient’s weight, |
Multiply prescribed dose by patient’s weight, |
| 200 micrograms × 3.5 |
250 micrograms × 3.5 |
| = 700 micrograms |
= 875 micrograms |
| Applying the formula, |
Applying the formula, |
|
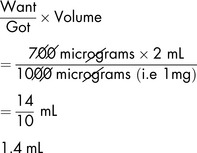
|

|
The patient will be given:
First dose: 1.4 mL IV injection Second dose: 1.75 mL IV injection
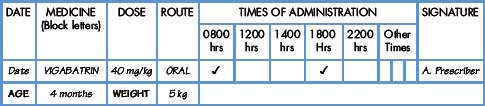
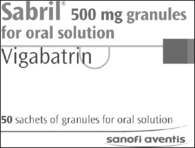
Demonstration 8.10
Commentary
•
Vigabatrin is used as adjunctive treatment of partial seizures not satisfactorily controlled with other antiepileptics
Workings
The dose is 40 mg/kg. The child weighs 5 kg. The required dose is therefore
Dissolve the contents of a sachet in water and make up to 10 mL. Therefore, 500 mg of vigabatrin are contained in 10 mL of solution.
Applying the formula,

The patient should be given:
4 mL of prepared solution using an oral syringe
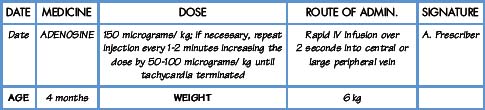
Demonstration 8.11
Commentary
•
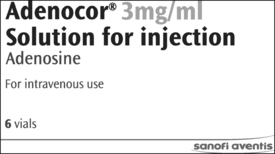
Adenosine is an anti-arrhythmic drug used for terminating supraventricular tachycardias
•
Injection solution may be diluted with sodium chloride 0.9% if required
•
Injection is followed by rapid sodium chloride 0.9% flush
Calculate the volume to be administered for the first three doses, increasing the second and third by 75 micrograms/kg.
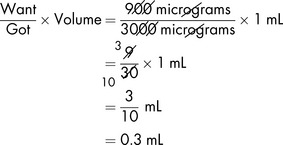
Workings
First dose
Applying the formula,
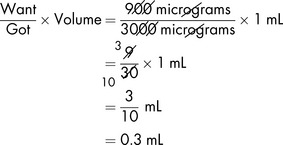
First dose the patient will be given:
0.3 mL of adenosine injection 3 mg/mL
Second dose
Applying the formula,
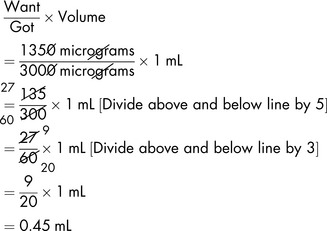
Second dose the patient will be given:
0.45 mL of adenosine injection 3 mg/mL
[Another way to work out (or verify) the second dose is to say the first dose is 150 micrograms/kg, which gives a required volume of injection of 0.3 mL. The second dose is 150 + 75 = 225 micrograms/kg. The dose (150 micrograms) has been increased by 50% (75 micrograms), i.e. 0.3 mL increased by 50% (0.15 mL) is 0.45 mL.]
Third dose
We know from previous calculations that to increase the dose for this child by 75 micrograms/kg requires an additional 0.15 mL of injection of adenosine 3 mg/mL. The second dose is 0.45 mL. Therefore the third dose will be 0.45 mL + 0.15 mL = 0.6 mL.
Third dose the patient will be given:
0.6 mL of adenosine injection 3 mg/mL
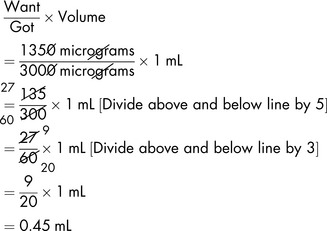
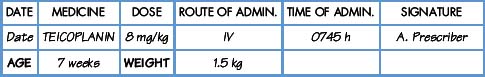
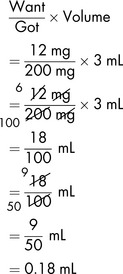
Demonstration 8.12
Commentary
•
Teicoplanin is an antibiotic active against aerobic and anaerobic Gram-positive bacteria including multiresistant
Staphylococci•
Diluent for reconstruction is supplied with the vial of powder and displacement volume has been allowed for
Workings
Dose to be administered is 8 mg/kg
Baby’s weight is 1.5 kg
Dose to be administered is 8 x 1.5 mg = 12 mg
The powder is reconstituted with the diluent supplied giving 200 mg in 3 mL
200 mg of teicoplanin is contained in 3 mL
Applying the formula,
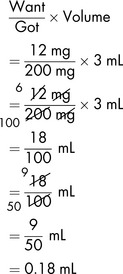
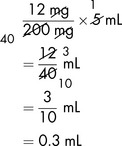
To make measuring the dose easier, the 200 mg in 3 mL of solution could be further diluted to 5 mL, i.e. if 200 mg were contained in 5 mL, then 12 mg (the prescribed dose) would be contained in:
The patient will be given:
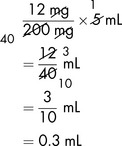
0.3 mL by IV injection
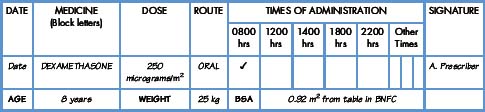
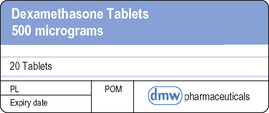
Demonstration 8.13
Commentary
•
Dexamethasone is a glucocorticoid used to treat inflammatory and allergic disorders
•
Disperse in water so that the final volume is 5 mL
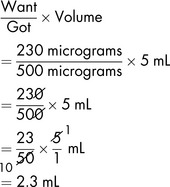
Workings
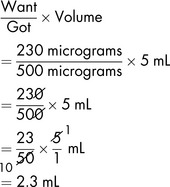
Applying the formula,
The patient will be given:
2.3 mL solution (In practice, it would be better to use the ready-prepared oral solution)
Level III Exercises
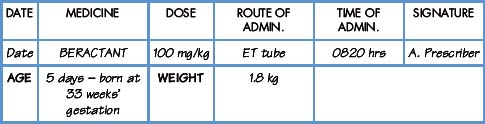
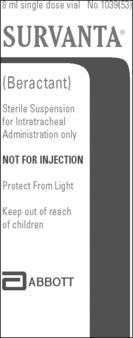
Exercise 8.37
Medicine label (25 mg/mL)
Commentary
•
Beractant is used to treat respiratory distress syndrome
•
It is administered by a special route, i.e. endotracheal tube
What should the patient be given?
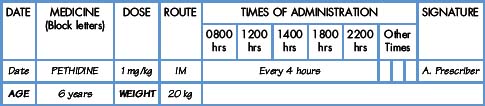
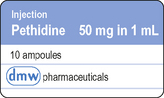
Exercise 8.38
Commentary
•
Pethidine is an opioid analgesic used for moderate to severe pain
•
This is a Controlled Drug
•
These ampoules would normally contain a declared overage of 0.1 mL
What should the patient be given?
Level III Further exercises
8.39
Domperidone 200 micrograms/kg is prescribed orally for a 3-year-old child weighing 16 kg. Suspension is available as 5 mg/5 mL. How much would you give?
8.40
A 3-year-old weighing 15 kg is prescribed 4 mg/kg of ranitidine twice daily. What volume of ranitidine oral solution 75 mg/5 mL will be given for each dose?
8.41
Atenolol syrup 25 mg/5 mL is prescribed once daily at a dose of 1 mg/kg for a 5-year-old weighing 18 kg. How many mL of syrup will be given daily?
8.42
An 8-year-old child (25 kg) is prescribed trimethoprim 4 mg/kg twice daily. What volume of trimethoprim suspension 50 mg/5 mL is given for each dose?
8.43
A 7-year-old child weighing 23 kg is prescribed midazolam at 500 micrograms/kg to be taken orally as a premedication 30–60 minutes before the procedure. How many mL of midazolam oral liquid 2.5 mg/mL are to be taken?
8.44
Carbamazepine is prescribed three times daily to an 11-year-old boy weighing 35 kg with epilepsy. The dose is 5 mg/kg. What volume of carbamazepine sugar-free liquid 100 mg/5 mL is given for each dose?
8.45
A 10-year-old weighing 30 kg is prescribed diazepam 200 micrograms/kg as a premedication. What volume of diazepam 2 mg/5 mL is required?
8.46
A 5-year-old weighing 18 kg is prescribed lorazepam 50 micrograms/kg by intravenous injection over 3–5 minutes. Lorazepam injection 4 mg/mL is available and the
BNF for Children (2008) advises diluting this with an equal volume of sodium chloride 0.9%. What volume of the diluted injection should be administered?
8.47
A child of one year weighing 10 kg is prescribed furosemide 2 mg/kg by slow IV injection. The label states 10 mg/mL. What volume should you give?
8.48
A neonate weighing 1.8 kg is prescribed flucloxacillin 25 mg/kg twice daily. What volume of a 125 mg/5 mL oral solution will be given?
8.49
Digoxin is prescribed orally at a dose of 6 micrograms/kg daily in two divided doses for an 8-year-old weighing 25 kg. What volume of elixir 50 micrograms/mL is given for each dose?
8.50
Alfacalcidol 40 nanograms/kg once daily is prescribed for a child of 12 months with a body weight of 10 kg. The oral (drops) preparation available contains 2 micrograms/1 mL. What volume would you give?
8.51
Alpha tocopheryl acetate is available as an oral suspension 100 mg/mL. A dose of 10 mg/kg once daily is prescribed for a neonate weighing 3.5 kg. What volume would you give?
8.52
Diclofenac sodium 1 mg/kg is prescribed orally for a child weighing 10 kg. The tablets are 50 mg and are dispersible. Add 10 mL water and work out what volume to give.
8.53
A 6-year-old child weighing 20 kg is prescribed pethidine 1 mg/kg every 4 hours by IM injection The ampoules are 50 mg in 1 mL. How much pethidine injection (mL) and pethidine (mg) will the child have had in 36 hours?
8.54
Vancomycin 125 mg has been prescribed orally. The formulation is a powder (500 mg vial) which requires to be reconstituted by adding 3.8 mL diluent to the vial to make a total volume of 4 mL taking account of the displacement volume of 500 mg of vancomycin. What volume should the patient be given?
8.55
The child is 10 years old and weighs 30 kg. The prescription states ‘chlorothiazide 10 mg/kg oral’. The medicine label states ‘chlorothiazide oral suspension 250 mg/5 mL’. What should the child be given?
8.56
Doxorubicin hydrochloride is prescribed at a dose of 30 mg/m
2 for a patient with a body surface area of 0.47 m
2. What volume of an injection 2 mg/mL is required?
Level IV Demonstration
Demonstration 8.14
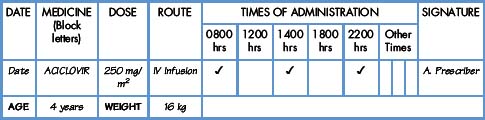
The medicine
Aciclovir (Zovirax) vials containing 250 mg powder for reconstitution are available
Commentary
•
Aciclovir is used to treat infections caused by herpes viruses
•
In the case of aciclovir powder for reconstitution, the displacement volume is negligible and you do not require to take account of this
Workings
The vial contains 250 mg powder for reconstitution.
The BNF for Children (2008) advises that for intravenous infusion, reconstitute the vial with 10 mL of water for injections or sodium chloride 0.9% (gives 25 mg/mL) then dilute to a concentration of 5 mg/mL with sodium chloride 0.9%.
25 mg/mL is contained in 10 mL.
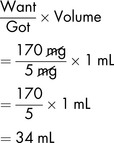
Applying the formula,
The body surface area of a 16 kg child is 0.68 m2 (from BNFC tables). The dose to be administered is therefore:
Applying the formula,
The patient will be given:
34 mL of aciclovir 5 mg/mL in sodium chloride 0.9%
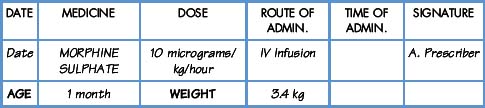
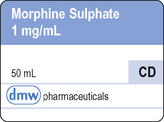
Demonstration 8.15
Commentary
•
Morphine compounds, used to relieve moderate to severe pain
•
Opioid analgesics should be avoided in children with acute respiratory depression.
What volume of IV infusion of morphine sulphate 1 mg/mL requires to be diluted to 50 mL to give an infusion rate of 1 mL per hour?
Workings
Dose of morphine sulphate is 10 micrograms/kg/hour
The weight of the child is 3.4 kg. Therefore 3.4 x 10 micrograms is the dose to be administered in one hour, i.e. 34 micrograms.
At a 1 mL per hour infusion rate, 1 mL must contain 34 micrograms.
Therefore 50 mL of infusion must contain
In the IV infusion of morphine sulphate, there is 1 mg in 1 mL. Therefore the volume of this to be diluted to 50 mL prior to administration is:
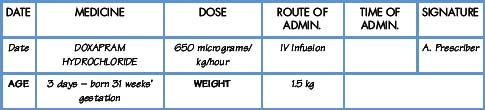
Demonstration 8.16a
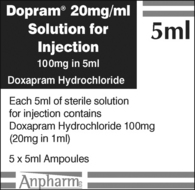
The medicine
Doxapram (Dopram) must be given by continuous IV infusion and is available as an infusion containing 2 mg/mL in 5% glucose solution
Commentary
•
Doxapram hydrochloride is used to treat preterm neonates and infants who have troublesome apnoea
Workings
The infusion rate is:
The baby is then changed to oral administration (8.16b)
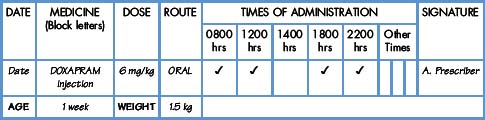
Demonstration 8.16b
Commentary
•
In some circumstances, parenteral products may be given orally (technical advice should be sought)
•
Doxapram injection can be used as an oral medicine diluted as necessary
Workings
Dose to be given orally is 6 mg/kg four times daily
Baby weighs 1.5 kg
Therefore 6 x 1.5 mg = 9 mg to be given orally
20 mg of doxapram hydrochloride is contained in 1 mL
Applying the formula,
The patient will be given:
0.45 mL orally four times daily (diluted appropriately with 5% glucose solution (BNFC))
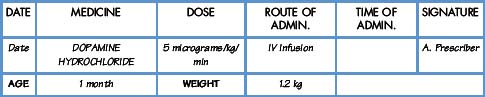
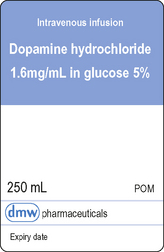
Demonstration 8.17
Commentary
•
Dopamine increases contractibility of cardiac muscle with little effect on heart rate
•
In neonatal intensive care, dilute 30 mg/kg body-weight to a final volume of 50 mL with infusion fluid (BNFC 2008)
(a)
What volume of available infusion requires to be diluted to 50 mL?
(b)
What is the rate of the infusion per hour?
Workings
(a)
Weight of neonate is 1.2 kg.
Therefore 30 x 1.2 mg requires to be diluted to 50 mL, i.e. 36 mg requires to be diluted to 50 mL.
The available infusion fluid contains dopamine hydrochloride 1.6 mg/mL in 5% glucose.
1.6 mg of dopamine hydrochloride is contained in 1 mL. Therefore 36 mg of dopamine hydrochloride is contained in:
Applying the formula,
22.5 mL of dopamine 1.6 mg/mL in glucose 5% is diluted to 50 mL with intravenous glucose 5%. Now 36 mg of dopamine hydrochloride is contained in 50 mL of glucose 5%.
(b)
The neonate’s weight is 1.2 kg
∴ 5 x 1.2 micrograms is to be administered per minute, therefore 6 x 60 micrograms is to be administered per hour, i.e. 360 micrograms per hour.
36 mg, i.e. 36 000 micrograms (1000 micrograms in 1 mg) is contained in 50 mL of infusion.
∴ 360 micrograms is contained in
Rate of infusion is 0.5 mL per hour
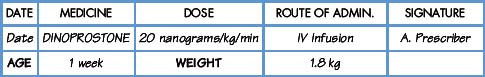
Demonstration 8.18
Commentary
•
Dinoprostone is a potent vasodilator for maintaining the patency of ductus arteriosus whilst awaiting surgery
•
Care is required in undertaking this calculation as milligrams, micrograms and nanograms are involved. Remember, there are 1000 micrograms in 1 milligram and 1000 nanograms in 1 microgram
•
Small volumes, e.g. 0.1 mL are difficult to measure accurately. To get over this, a dilution can be made, e.g. 1 part diluted to 10 parts, which enables a larger volume (10 times in this case) to be measured
What volume of dinoprostone 1 mg/mL is required to make up an infusion solution of 50 mL to be run at 1 mL per hour?
Workings
Dose is 20 nanograms/kg/min
Baby weighs 1.8 kg
∴ dose required is
At a dose rate of 1 mL/h, 2160 nanograms will be contained in 1 mL.
Therefore, a 50 mL infusion to deliver 2160 nanograms in 1 mL will contain 50 x 2160 nanograms, i.e.
The available injection of dinoprostone contains 1 mg in 1 mL of injection, i.e. 1000 micrograms of dinoprostone in 1 mL of injection.
Therefore 108 micrograms are contained in:
Applying the formula,
This volume is difficult to measure accurately.
To enable an accurate dose to be measured, dilute the 1 mg/mL dinoprostone injection to 10 mL with glucose 5% or sodium chloride 0.9%. This dilutes the injection 10 times. Therefore instead of measuring 0.108 mL (round up to 0.11 mL), you need to measure 10 x 0.11 mL of the diluted injection, i.e. 1.1 mL.
Demonstration 8.19
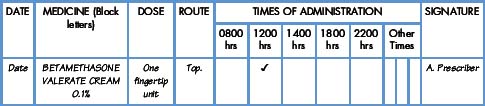
The medicine
Betamethasone (Betnovate) is available in a variety of formulations. The cream contains 0.1% w/w betamethasone valerate.
Commentary
•
Betamethasone valerate cream is a potent corticosteroid used to treat a variety of skin conditions
•
Excessive use of the cream could cause side-effects due to absorption of the drug
•
The patient has used 30 g in 10 days
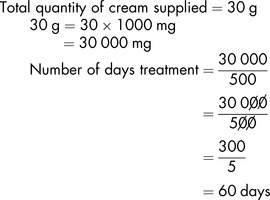
Workings
(a)
How much of the active ingredient has been applied?
Answer: 30 mg of active ingredient has been applied
(b)
If a fingertip unit is approximately equivalent to 500 mg of cream, how long should the 30 g tube have lasted the patient?
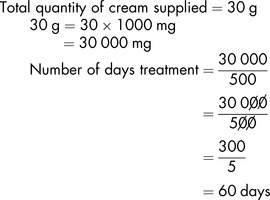
Answer: The tube should have lasted 60 days
Level IV: Exercises
Exercise 8.57
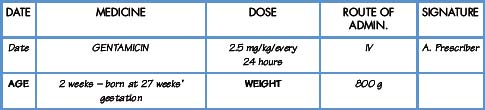
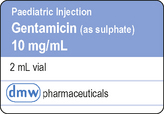
Commentary
•
Gentamicin is an antibiotic active against some Gram-positive and many Gram-negative organisms
What volume of gentamicin paediatric injection should the patient be given?
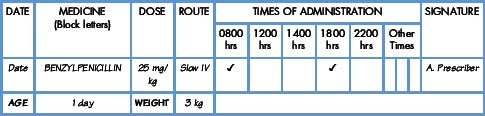
Exercise 8.58
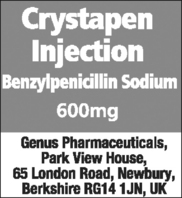
Medicine label (vial of powder for reconstitution)
Commentary
•
Benzylpenicillin is bactericidal and is used to treat a range of infections
(a)
What volume of diluent is used to reconstitute 600 mg in 5 mL if the displacement volume is 0.4 mL?
(b)
What is the dose to be administered twice daily?
(c)
What volume would you inject?
Level IV Further exercises
8.59
A baby is administered an IV infusion of morphine containing 2 mg in 50 mL. The infusion rate is 0.8 mL per hour. (a) What volume of the morphine solution is given over 6 hours? (b) What quantity (micrograms) of morphine is administered over 6 hours?
8.60
A syringe contains 78 mg of dopamine in 50 mL of glucose 5%. This is to be administered to a baby weighing 1.3 kg at a rate of 0.5 mL per hour. What is the dose in micrograms/kg/minute?
8.61
A syringe contains 8.75 mg of morphine sulphate in 50 mL of glucose 5%. The baby’s weight is 3.7 kg and the dose is 9.5 micrograms/kg/hour. What is the required rate of infusion in mL per hour?
8.62
An 11-year-old weighing 35 kg is prescribed imatinib orally, 340 mg/m
2 daily in two divided doses. 100 mg tablets are available. How many tablets are given as a single dose? (The body surface area using the Boyd equation is 1.2 m
2.)
8.63
A 10-year-old weighing 30 kg is prescribed aminophylline 800 micrograms/kg/hour by intravenous infusion 1 mg/mL in glucose 5%. What is the infusion rate per hour to provide this dose?
8.64
A low-dose test of tetracosactide is prescribed at 300 nanograms/m
2 as a single dose to be administered intravenously. Injection of tetracosactide available is 250 micrograms/mL. This can be diluted in sodium chloride 0.9% to 250 nanograms/mL. The child has a body surface area of 0.28 m
2. (a) How is the dilution prepared? (b) What volume is administered?
8.65
A 1-week-old infant, weighing 900 g, is prescribed 50 mg of cefotaxime per kilogram by intravenous infusion every 12 hours. The injection is available as 500 mg in a powder for reconstitution. Account should be taken of displacement volume – 500 mg vial – displacement volume is 0.2 mL when powder reconstituted to 2 mL. For intermittent intravenous infusion dilute in glucose 5% or sodium chloride 0.9%.
(a)
What dose is administered every 12 hours?
(b)
What volume is added to 500 mg vial to make up to 2 mL taking account of displacement volume?
(c)
If the injection is diluted to 5 mL, what volume of injection provides the required dose?
8.66
Alprostadil is available as an intravenous solution of 500 micrograms/mL. It is to be diluted to a volume of 50 mL before use in glucose 5% (avoid contact of solution with walls of plastic container). The dose is 300 micrograms per kilogram body weight (the baby is 1.5 kg).
(a)
What volume of the solution (500 micrograms/mL) is required to prepare the infusion?
b)
How many nanograms/kg/minute will be provided at an infusion rate of 0.1 mL/hour?
8.67
Foscarnet (an antiviral active against cytomegalovirus) 60 mg/kg is to be given every 8 hours by IV infusion. Foscarnet sodium hexahydrate 24 mg in 1 mL (250 mL container) is available. The patien’ weight is 15 kg.
(a)
What is the dose (mg) to be given every 8 hours?
(b)
What is the volume (mL) containing the required dose?
8.68
Daunorubicin is prescribed for a patient with a body surface area of 0.68 m
2 at a dose of 45 mg/m
2. (a) What volume of an injection of 5 mg/mL is required? (b) What volume of 0.9% sodium chloride should be added to adjust the strength to 1 mg/mL prior to adding to the IV infusion?
References
BMA (British Medical Association) and RPSGB (Royal Pharmaceutical Society of Great Britain). British National Formulary for Children (BNFC). London: BMJ Group and RPS Publishing, 2008.
NMC. Standards for medicines management. London: Nursing and Midwifery Council, 2008.
Further reading
Conroy S., Sweis D., Planner C., et al. Interventions to reduce dosing errors in children: a systematic review of the literature. Drug Saf.. 2007;30(12):1111-1125.
.
Sentinel Event Alert. Preventing paediatric medication errors. 2008;(Issue 39):1-11.