CHAPTER 4 Calculating oral and other non-parenteral doses
Introduction
Following discussion of the equipment required, fully worked-up examples of calculations of oral and other non-parenteral drugs are provided, at the different levels of complexity described in Chapter 3.
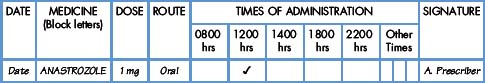
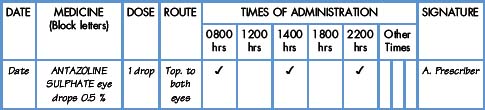
A demonstration of each level of calculation is given. A standard format is used which includes the given information, namely the prescription and the label; a brief commentary to provide guidance; the workings involved; and finally, what the patient will be given.
In order to make best use of space, the prescription forms used in the examples that follow are necessarily incomplete. For example, the patient’s personal details are not included. All the information needed to complete the calculations is shown. The full format of a prescription sheet is shown in Fig. 1.1.
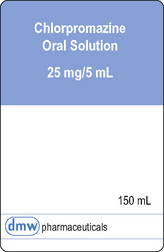
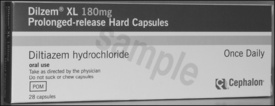
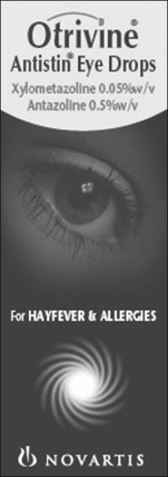
Where it has not been possible to reproduce manufacturers’ labels, facsimile labels have been created.
Each level of demonstration is followed by several examples to practise. These take two forms, the same format as the demonstration and an abridged tabular format. In each case, the ‘answer’ required is the quantity and form of the medicine you would give to the patient (for a single dose) thus ensuring accuracy of dosage. All answers are given on pp. 194–195.
Equipment needed for measuring the dose of liquid medicines
Having calculated (or determined) the correct dose, it is essential to use the right equipment/technique to ensure that the dose is delivered in the best way. There is little point in calculating the dose correctly if some of the dose is lost (or the formulation destroyed) during the administration procedure.
The following items of equipment may be required depending on the medicine being administered.
Glass and suitable liquid. In a number of cases, it may be necessary to provide the patient with a drink to ‘help the medicine go down’. The choice and amount of liquid to use will depend on the patient’s circumstances. If at all possible, the patient’s choice should be taken into account. Some patients may need special help with their medicines; not all patients find medicine-taking easy. For reasons of security, a patient may be asked to follow a dose of an oral liquid (e.g. methadone) with a drink of water to be sure it has been swallowed.
Whenever possible, the patient’s preferences should be recognised and, if possible allowed for. In some cases, e.g. mesna, the BNF recommends that the dose (when using the contents of an ampoule) be dissolved in orange juice or cola.
Tablet crusher. In a very limited number of cases, it is necessary to crush a tablet before administration, e.g. calcium with vitamin D tablets. In general, tablets should not be crushed since this will damage the formulation or special coating. The stability of the formulation may be compromised if the product is changed in some way before administration.
The medical and legal consequences of changing the formulation of a product may be significant. For example, the needs of the patient with dysphagia should always be considered sympathetically (Wright et al 2006). In such cases, whenever possible, a specially formulated liquid oral medicine should be used. In any event, the advice of the pharmacist should be sought especially if it is necessary to administer a medicine via an enteral feeding tube (White and Bradnam 2006). There are also legal implications if tablets are crushed or capsules opened where covert medication is considered to be in the patient’s best interests (Mental Welfare Commission for Scotland 2007).
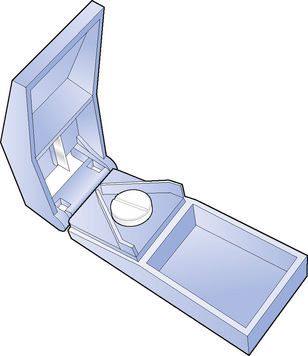
Tablet splitter (Fig. 4.1). Some tablets must be divided to get the correct dose. Only divide scored tablets. The use of a tablet splitter is highly desirable to ensure an accurate dose is used.
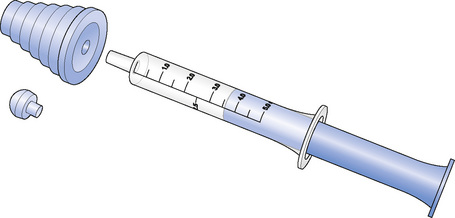
Measures. For liquid medicines, it is important to use the equipment with the appropriate graduations to ensure accuracy of dose delivery.
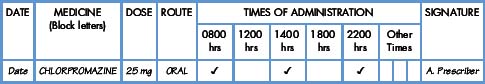
Protective gloves. If handling a medicine (especially a liquid medicine) with known irritant properties, e.g. chlorpromazine or in cases of known hypersensitivity, disposable gloves should be worn. Special care must be taken when administering cytotoxic drugs or drugs which may have adverse effects on women of child-bearing potential (e.g. finasteride).
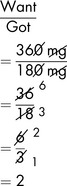
How to calculate the quantity to give of an oral medicine
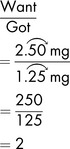
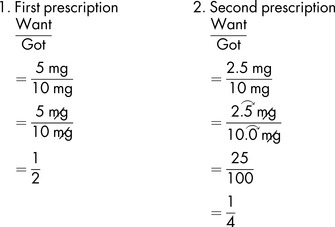
Level 0: Demonstration
Level I: Demonstration
Level I: Exercises
In the following exercises, calculate what you should give the patient.
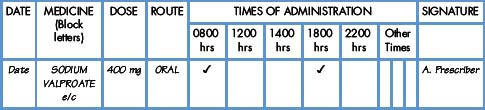
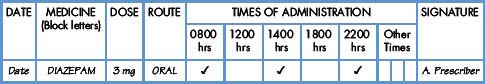
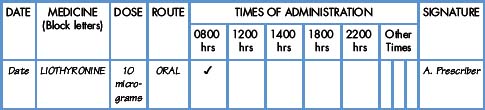
Exercise 4.4
Level I: further exercises
In the following examples, calculate what you should give the patient.
| ‘Prescription’ | ‘Medicine label’ | |
|---|---|---|
| 4.6 | Aspirin dispersible 150 mg oral | 75 mg tablets |
| 4.7 | Bisoprolol fumarate 20 mg oral | 5 mg tablets |
| 4.8 | Furosemide 30 mg oral | 20 mg tablets |
| 4.9 | Bisacodyl 10 mg oral | 5 mg tablets |
| 4.10 | Doxepin 50 mg oral | 25 mg capsules as hydrochloride |
| 4.11 | Mirtazapine 45 mg oral | 15 mg orodispersible tablets |
| 4.12 | Phenytoin 300 mg oral | 100 mg tablets |
| 4.13 | Ranitidine 300 mg oral | 150 mg tablets as hydrochloride |
| 4.14 | Atenolol 75 mg oral | 25 mg tablets |
| 4.15 | Betahistine 16 mg oral with food | 8 mg tablets betahistine dihydrochloride |
| 4.16 | Codeine phosphate 60 mg oral | 30 mg tablets |
| 4.17 | Allopurinol 200 mg oral | 100 mg tablets |
| 4.18 | Amlodipine 10 mg oral | 5 mg tablets as maleate |
| 4.19 | Soluble aspirin 900 mg oral | 300 mg tablets |
| 4.20 | Lormetazepam 750 microgram oral | 500 microgram tablets |
| 4.21 | Lansoprazole 60 mg oral | 15 mg capsules |
| 4.22 | Hydrocortisone 20 mg oral | 10 mg tablets |
| 4.23 | Megestrol 80 mg oral | 160 mg tablets |
| 4.24 | Venlafaxine 75 mg oral | 37.5 mg tablets |
| 4.25 | Acamprosate calcium 666 mg oral | 333 mg tablets |
| 4.26 | Nimodipine 60 mg oral | 30 mg tablets |
| 4.27 | Fludrocortisone 150 micrograms oral | 100 microgram tablets |
| 4.28 | Lofexidine 800 micrograms oral | 200 microgram tablets |
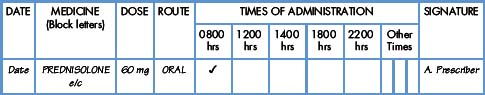
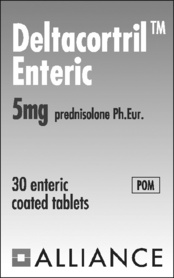
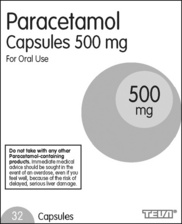
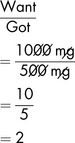
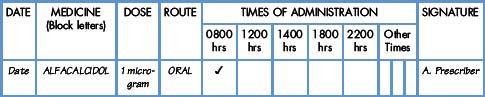
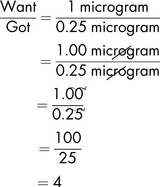
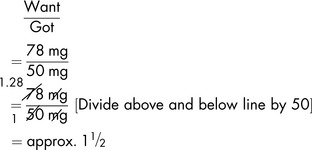
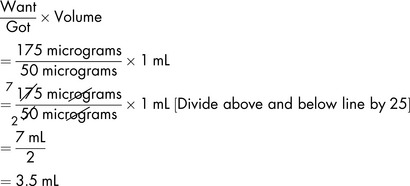
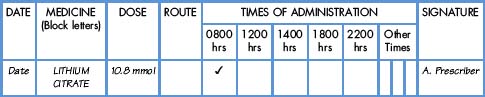
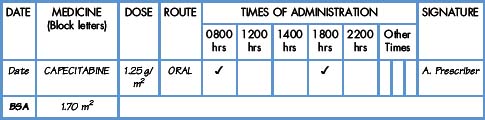
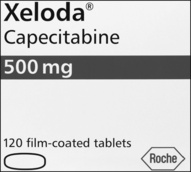
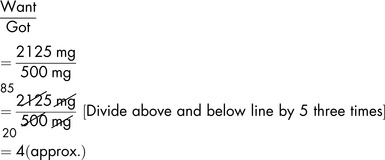
Level II: Demonstration
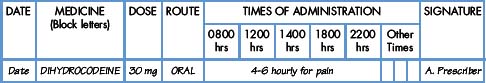
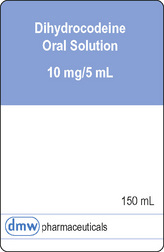
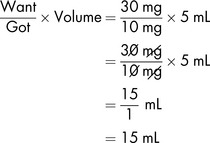
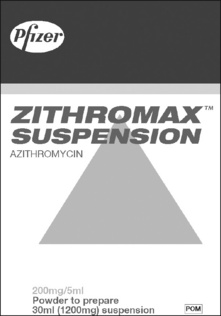
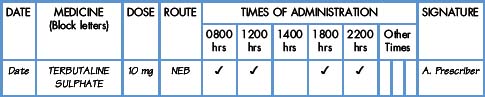
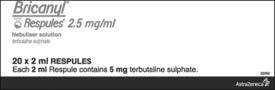
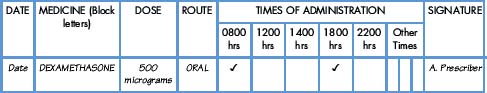
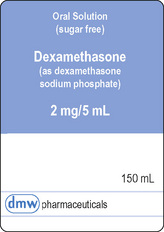
Demonstration 4.5
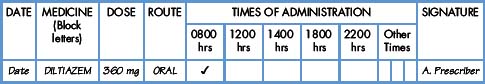
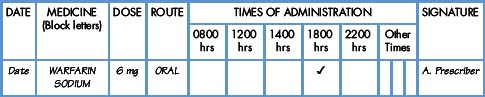
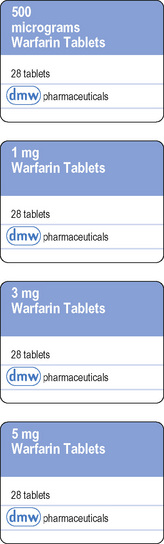
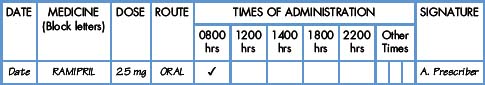
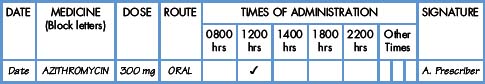
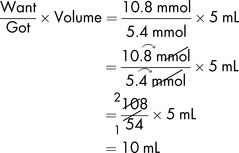
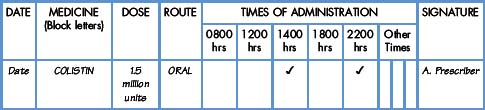
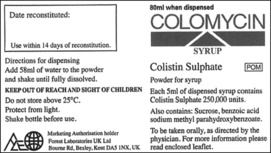
Demonstration 4.6
Level II: exercises
In each of the following exercises, calculate what you should give the patient.
Level II: further exercises
In the following examples, calculate what you should give the patient.
| ‘Prescription’ | ‘Medicine label’ | |
|---|---|---|
| 4.32 | Erythromycin 250 mg oral | 500 mg/5 mL suspension |
| 4.33 | Procyclidine 2.5 mg oral | 5 mg tablets |
| 4.34 | Valproate 300 mg oral | 200 mg/5 mL oral solution |
| 4.35 | Haloperidol 1 mg oral | 500 micrograms tablets |
| 4.36 | Risperidone 500 micrograms oral | 0.5 mg tablets |
| 4.37 | Amoxicillin 500 mg oral | 250 mg/5 mL suspension |
| 4.38 | Colchicine 1 mg oral | 500 micrograms tablets |
| 4.39 | Pizotifen 200 micrograms oral | 250 micrograms/5 mL elixir |
| 4.40 | Trimethoprim 200 mg oral | 50 mg/5 mL suspension |
| 4.41 | Carbamazepine 300 mg oral | 100 mg/5 mL suspension |
| 4.42 | Cefradine 1 g oral | 250 mg/5 mL syrup |
| 4.43 | Montelukast 10 mg oral | 4 mg chewable tablets |
| 4.44 | Ondansetron 16 mg oral | 4 mg/5 mL syrup |
| 4.45 | Aciclovir 800 mg oral | 200 mg/5 mL suspension |
| 4.46 | Methadone 70 mg oral | 1 mg/mL oral solution |
| 4.47 | Ciprofloxacin 750 mg oral | 250 mg/5 mL suspension |
| 4.48 | Sunitinib 50 mg oral | 12.5 mg capsules |
| 4.49 | Nalidixic acid 900 mg oral | 300 mg/5 mL suspension |
| 4.50 | Selenium 75 micrograms oral | 50 micrograms/mL oral solution |
| 4.51 | Iodine 26 mg oral | 130 mg/mL oral solution |
| 4.52 | Oseltamivir 75 mg oral | 12 mg/mL oral suspension |
| 4.53 | Salbutamol 200 micrograms inhal | 100 micrograms/actuation |
| 4.54 | Promazine 200 mg oral | 50 mg/5 mL oral solution |
| 4.55 | Flupentixol 500 micrograms oral | 0.5 mg tablets |
| 4.56 | Paracetamol 375 mg oral | 250 mg/5 mL oral suspension |
| 4.57 | Digoxin 75 micrograms oral | 50 micrograms/mL elixir |
| 4.58 | Folic acid 5 mg oral | 2.5 mg/5 mL syrup |
| 4.59 | Carbocisteine 2.25 g oral | 375 mg capsules |
| 4.60 | Escitalopram 7.5 mg oral | 10 mg/mL oral drops |
| 4.61 | Buprenorphine HCl 2 mg | 400 microgram tablets |
| 4.62 | Memantine HCl 5 mg oral | 10 mg/g oral drops (2 drops/mg) |
| 4.63 | Sodium chloride 1.6 g oral | 400 mg capsules |
| 4.64 A patient has been taking 7.5 mg diazepam twice daily but has developed an allergy to the drug. The prescriber wishes to change to an equivalent dose of lorazepam. 5 mg diazepam is equivalent to 500 micrograms of lorazepam. What dose of lorazepam should be prescribed? | ||
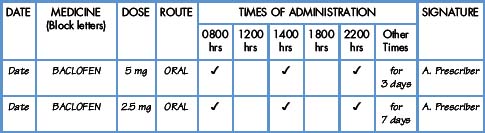
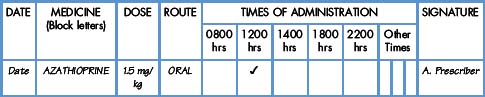
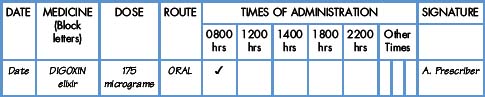
Level III: Demonstration
Demonstration 4.10
The medicine
Digoxin (Lanoxin-PG) tablets and elixir are available. The label of the elixir states that it contains 0.05 mg in 1 mL
Demonstration 4.11
Commentary
Demonstration 4.12
Commentary
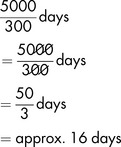
How long will a bottle last the patient (assuming no wastage) to the nearest day?
Level III: exercises
In the following exercises, calculate what you should give the patient.
Level III: further exercises
In the following examples, calculate what you should give the patient.
| ‘Prescription’ | ‘Medicine label’ | |
|---|---|---|
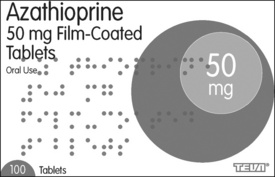
| 4.67 | Azathioprine 3 mg/kg oral daily | 25 mg tablet |
| Adult female 45 kg | ||
| 4.68 | Tacrolimus 300 micrograms/kg oral daily in two divided doses | 500 micrograms, 1 mg, 5 mg capsules |
| Adult male 55 kg | ||
| 4.69 | Chlorambucil 150 micrograms/kg daily | 2 mg tablets |
| Adult male 80 kg | ||
| Then, depending on leucocyte count, 100 micrograms/kg daily | ||
| 4.70 | Melphalan 125 micrograms/kg daily | 2 mg tablets |
| Adult female 50 kg | ||
| 4.71 | Mycophenolate mofetil 600 mg/m2 oral | 1 g/5 mL oral suspension |
| The patient’s BSA is 1.6 m2 | ||
Dilution of non-parenteral products
The dilution of solutions for topical use will seldom be required. Pre-packed single-use sachets are generally preferred.
Two examples of a dilution involving a calculation follow.
Example 4.1
The BNF gives specific guidance on the dilution of potassium permanganate solution. The standard solution is 1 in 1000 (0.1% w/v). A 1 in 10 000 solution is the required strength.
The standard solution must be diluted 1 in 10, i.e. 10 mL in 100 mL.
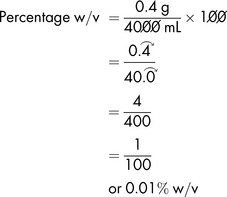
As an alternative, a tablet containing 400 mg (0.4 g) can be dissolved in 4 litres to produce a 0.01% w/v solution.
It should not be necessary to dilute antiseptic solutions for topical use. Individual sterile packs are the norm. However, the calculations involved are quite straightforward. It should be noted that this is a calculation involving percentages and so it is necessary to convert milligrams to grams.
Baxter K., Sharp J., Marshall, et al. Drug interactions. The Pharmaceutical Journal. 2008;281:333.
Blanch R. Confusion over eye drop prescriptions. The Pharmaceutical Journal (Letters). 2008;280(7502):594.
BMA (British Medical Association) and RPSGB (Royal Pharmaceutical Society of Great Britain). British National Formulary. London: BMJ Group and RPS Publishing, 2009.
Mental Welfare Commission for Scotland. Covert medication: a legal and practical guide. Edinburgh: Mental Welfare Commission for Scotland, 2007.
White R., Bradnam V. Handbook of drug administration via enteral feeding tubes. Biggleswade, Bedfordshire: Pharmaceutical Press, 2006.
Wright D., Chapman N., Foundling-Miah M., et al. Consensus guideline on the medication management of adults with swallowing difficulties. Connectmedical, a division of Medendium Group Publishing Ltd, 2006.