Other bacterial infections
Diseases due to commensal overgrowth
Sometimes, ‘normal’ commensals can result in disease. Among the most common are the following:
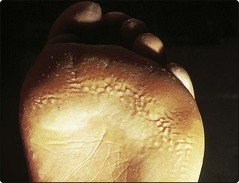
 Pitted keratolysis. Overgrowth of resident micro-organisms, that digest keratin; occurs with occluding footwear and sweaty feet (Fig. 1). Malodorous pitted erosions and punched out, discoloured areas result. Better hygiene, topical neomycin or soaks with 0.01% aqueous potassium permanganate or 3% aqueous formaldehyde usually help.
Pitted keratolysis. Overgrowth of resident micro-organisms, that digest keratin; occurs with occluding footwear and sweaty feet (Fig. 1). Malodorous pitted erosions and punched out, discoloured areas result. Better hygiene, topical neomycin or soaks with 0.01% aqueous potassium permanganate or 3% aqueous formaldehyde usually help.
 Erythrasma. A dry, reddish–brown, slightly scaly and usually asymptomatic eruption that affects the body folds (Fig. 2). It fluoresces coral pink with Wood’s light, owing to the production of porphyrins by the corynebacteria. Imidazole creams, topical fusidic acid or oral erythromycin are effective.
Erythrasma. A dry, reddish–brown, slightly scaly and usually asymptomatic eruption that affects the body folds (Fig. 2). It fluoresces coral pink with Wood’s light, owing to the production of porphyrins by the corynebacteria. Imidazole creams, topical fusidic acid or oral erythromycin are effective.
 Trichomycosis axillaris. Overgrowths of corynebacteria form yellow concretions on axillary hair. Topical antimicrobials usually effect a cure.
Trichomycosis axillaris. Overgrowths of corynebacteria form yellow concretions on axillary hair. Topical antimicrobials usually effect a cure.
Mycobacterial infections
Mycobacterium tuberculosis and M. leprae (p. 60) are the most important mycobacteria in human disease, although other species can cause infections. In western countries, tuberculosis (TB) has recently shown resurgence, related to immigration and co-infection with HIV. In the developing world, 50% of HIV-infected individuals also have TB. TB can produce a number of cutaneous manifestations (Table 1).
Table 1 Skin manifestations of tuberculosis
Lupus vulgaris
Reddish–brown plaques, often on the head or neck, characterize lupus vulgaris. It is the commonest M. tuberculosis skin infection.
Clinical presentation
Lupus vulgaris follows primary inoculation and develops in individuals with some immunity. It begins as painless reddish–brown nodules that slowly enlarge to form a plaque (Fig. 3), leaving scarring and sometimes destruction of deeper tissues such as cartilage. Presentation in the elderly is often due to reactivation of inadequately treated pre-existing disease.
Differential diagnosis and complications
Papules of lupus vulgaris typically show an ‘apple-jelly’ colour when compressed with a glass slide (diascopy). A biopsy will reveal tuberculoid granulomata with a few bacilli. The Mantoux test is positive. Sometimes it is necessary to consider:
Squamous cell carcinoma may develop in longstanding scarred lesions. The presence of M. tuberculosis somewhere in the body can induce cutaneous reactions called ‘tuberculides’. Erythema nodosum (p. 83) is the best known example. Another is erythema induratum, which occurs as painful ulcerating nodules on the lower legs of women and is thought to be a hypersensitivity response to TB.
Management
Four drugs, normally rifampicin, isoniazid, pyrazinamide and ethambutol, are given for the initial 8 weeks. After this, isoniazid and rifampicin are continued to complete a 6-month course. Directly observed therapy, in which ingestion of drugs is witnessed, improves cure rates if compliance could be a problem. Adverse reactions to TB drugs are common.
Scrofuloderma
A tuberculous lymph node or joint can directly involve the overlying skin, often on the neck and in children. Fistulae and scarring result.
Warty tuberculosis
A warty reddish or brown plaque, frequently on the hands, knees or buttock, results from inoculation of TB bacilli into the skin of someone with immunity from previous infection. It is rare in western countries, but is a common form of cutaneous TB in the developing world.
Other cutaneous mycobacterial infections
Fish tank granuloma
Typically, this is a reddish, slightly scaly plaque on the hand or arm of someone who keeps tropical fish. It is due to Mycobacterium marinum, which infects fish and is also found in swimming pools, sea water and fresh water.
Buruli ulcer
In tropical zones, Mycobacterium ulcerans – acquired from vegetation or water after trauma – produces a painless erythematous nodule usually on the leg or forearm. The nodule becomes necrotic and ulceration results.
Disseminated infection with Mycobacterium avium complex is seen in patients with HIV infection (p. 56).
Spirochaetal infections
Spirochaetes are thin, spiral and motile organisms. Syphilis (p. 120), due to Treponema pallidum, is the best known spirochaetal disease, but other spirochaetes, e.g. Borrelia burgdorferi, can be pathogenic.
Non-venereal treponemal infections
Non-venereal treponemal infections are endemic in tropical and subtropical areas where people live in conditions of extreme poverty. They are caused by spirochaetes that are very similar to T. pallidum. Serological tests for syphilis are positive. All three of the following diseases respond to long-acting penicillins.
 Yaws occurs in central Africa, central America and southeast Asia. In children, the treponeme enters the skin through an abrasion and, after a few weeks, results in an ulcerated papilloma that heals with scarring. Secondary lesions follow and, in the late stage, bone deformities develop.
Yaws occurs in central Africa, central America and southeast Asia. In children, the treponeme enters the skin through an abrasion and, after a few weeks, results in an ulcerated papilloma that heals with scarring. Secondary lesions follow and, in the late stage, bone deformities develop.
 Bejel (endemic syphilis), found in rural Middle Eastern tribes living in unhygienic conditions, is similar to yaws but starts around the mouth. It is transmitted by skin contact.
Bejel (endemic syphilis), found in rural Middle Eastern tribes living in unhygienic conditions, is similar to yaws but starts around the mouth. It is transmitted by skin contact.
 Pinta is confined to central and south America. It results in hyperkeratoses over extensor aspects of joints with both hypo- and hyperpigmentation.
Pinta is confined to central and south America. It results in hyperkeratoses over extensor aspects of joints with both hypo- and hyperpigmentation.
Lyme disease
Lyme disease is a cutaneous and systemic infection caused by the spirochaete Borrelia burgdorferi and spread by tick bite. Most cases have been reported in the USA and Europe. At the site of the tick bite, usually a limb, a slowly expanding erythematous ring (erythema chronicum migrans) develops (Fig. 4). Arthritis and neurological and cardiac disease may follow. A response to high-dose amoxicillin or doxycycline is usual.
Further bacterial infections
Anthrax
A haemorrhagic bulla, associated with oedema and fever, forms at the site of inoculation of the skin with Bacillus anthracis, usually from contaminated animal products. It is now rare. Ciprofloxacin or amoxicillin is curative.
Gram-negative infections
Bacilli such as Pseudomonas aeruginosa can infect skin wounds, notably leg ulcers. They may also cause folliculitis and cellulitis.
Cellulitis
Cellulitis is an infection of the subcutaneous tissues. It is often due to streptococci, but is deeper and more extensive than erysipelas. The cardinal features are swelling, redness and local pain with systemic upset and fever. The leg is often affected (Fig. 5). The organism may gain entry through fissures between the toes or via a leg ulcer. Lymphangitis is common, and lymphatic damage may result. Hospital admission is usually indicated, particularly if the leg is involved. Antistreptococcal antibiotics are given for straightforward cases. However, a broad-spectrum antibiotic is prescribed for cellulitis complicating a leg ulcer, because a selection of organisms may be responsible. Blood cultures and ulcer swabs may give some guidance.
Other bacterial infections
 Overgrowth of commensal organisms can result in minor skin ‘disease’.
Overgrowth of commensal organisms can result in minor skin ‘disease’.
 Cutaneous mycobacterial infection is mainly due to M. tuberculosis, but occasionally ‘atypical’ mycobacteria such as M. marinum cause disease.
Cutaneous mycobacterial infection is mainly due to M. tuberculosis, but occasionally ‘atypical’ mycobacteria such as M. marinum cause disease.
 Non-venereal treponematoses, e.g. yaws, are still important diseases of rural people living in poor conditions in the developing world.
Non-venereal treponematoses, e.g. yaws, are still important diseases of rural people living in poor conditions in the developing world.
 Lyme disease is a tick-transmitted infection with Borrelia burgdorferi; the skin signs are often associated with arthritis or neurological disease.
Lyme disease is a tick-transmitted infection with Borrelia burgdorferi; the skin signs are often associated with arthritis or neurological disease.
 Cellulitis often affects the leg and is frequently caused by streptococci, although other organisms may be involved.
Cellulitis often affects the leg and is frequently caused by streptococci, although other organisms may be involved.