Genitourinary medicine
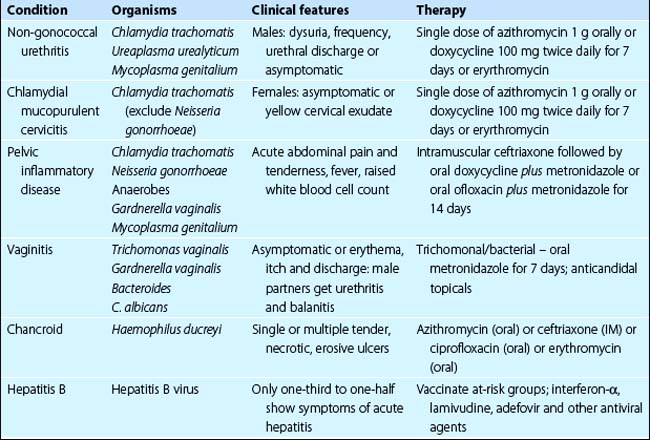
In the UK and Ireland, genitourinary medicine has traditionally been a separate specialty from dermatology, but the two are combined as ‘dermatovenereology’ in many countries. It has become increasingly important for those treating skin disease to know more about genitourinary disorders. Genitourinary diseases range as follows (see also Table 1): syphilis, gonorrhoea, human immunodeficiency virus (HIV) infection (p. 56), chlamydial infection, pelvic inflammatory disease, vaginitis, chancroid viral warts (p. 52), genital herpes simplex (p. 54), hepatitis B and hepatitis C, vulval/perianal dermatoses, penile/scrotal dermatoses.
Syphilis (lues)
Syphilis is a chronic infectious disease due to Treponema pallidum. Skin signs are seen in all three stages.
Clinical presentation
T. pallidum may rarely be acquired congenitally or from a contaminated blood transfusion, but the normal mode of transmission is through sexual intercourse.
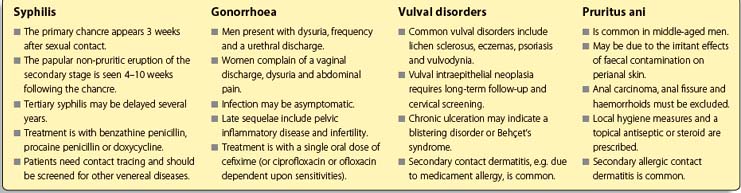
 Primary chancre. About 3 weeks after sexual contact, a primary chancre, a painless ulcerated button-like papule, develops at the site of inoculation. This is usually genital (Fig. 1), but oral and anal chancres are seen in men who have sex with men. Regional lymphadenopathy is common. Without treatment, the chancre clears spontaneously in 3–10 weeks. Serology is not positive until 4 weeks after infection, but spirochaetes can be isolated from the chancre.
Primary chancre. About 3 weeks after sexual contact, a primary chancre, a painless ulcerated button-like papule, develops at the site of inoculation. This is usually genital (Fig. 1), but oral and anal chancres are seen in men who have sex with men. Regional lymphadenopathy is common. Without treatment, the chancre clears spontaneously in 3–10 weeks. Serology is not positive until 4 weeks after infection, but spirochaetes can be isolated from the chancre.
 Secondary stage. This phase starts 4–10 weeks after the onset of the chancre. It is characterized by a non-itchy pink or copper-coloured papular eruption on the trunk, limbs, palms and soles (p. 42). Untreated, the eruption resolves in 1–3 months. Serology is positive.
Secondary stage. This phase starts 4–10 weeks after the onset of the chancre. It is characterized by a non-itchy pink or copper-coloured papular eruption on the trunk, limbs, palms and soles (p. 42). Untreated, the eruption resolves in 1–3 months. Serology is positive.
 Tertiary stage. About 30% of patients with untreated syphilis will develop late lesions, usually after a latent period of years. Painless nodules, sometimes with scaling, develop in annular or arcuate patterns on the face or back. Subcutaneous granulomatous gumma – usually on the face, neck or calf – ulcerate, scar and never heal completely (Fig. 2). Cardiovascular syphilis and neurosyphilis may coexist.
Tertiary stage. About 30% of patients with untreated syphilis will develop late lesions, usually after a latent period of years. Painless nodules, sometimes with scaling, develop in annular or arcuate patterns on the face or back. Subcutaneous granulomatous gumma – usually on the face, neck or calf – ulcerate, scar and never heal completely (Fig. 2). Cardiovascular syphilis and neurosyphilis may coexist.
Management
Primary or secondary syphilis is treated with a single dose of benzathine penicillin G (unlicensed) or procaine penicillin (unlicensed) intramuscularly daily for 10 days as first-line therapy. Doxycycline, azithromycin and erythromycin are alternatives. Patients need contact tracing and assessment for other venereal diseases, and should be managed in a genitourinary medicine department.
Gonorrhoea
Gonorrhoea is caused by the Gram-negative diplococcus Neisseria gonorrhoeae. Infection may be symptomatic or asymptomatic.
Clinical presentation
Symptomatic males usually present with dysuria, frequency of micturition and a purulent urethral discharge. Females, when symptomatic, can have an abnormal vaginal discharge, dysuria, intermenstrual bleeding, menorrhagia or abdominal pain. Pharyngeal and anorectal infection may produce symptoms, or may be asymptomatic. The diagnosis relies on the microscopic identification of Gram-negative intracellular diplococci from urethral (males and females) or endocervical (females) smears, and culture for N. gonorrhoeae. Serological tests are unreliable. Women with untreated gonorrhoea are at risk of developing pelvic inflammatory disease and infertility. In men, complications include urethral stricture, infertility and epididymitis.
Gonococcaemia is rare but, when observed, results in fever, arthritis and pustules that are few in number and generally distributed on the hands, feet or near the large joints. This is a type of septic vasculitis which, like some other systemic infections (e.g. Neisseria meningitidis), may be purpuric.
Management
Uncomplicated acute gonorrhoea should be treated with single-dose cefixime (oral) or ceftriaxone (intramuscular) for pharyngeal infections. Single doses of ciprofloxacin or ofloxacin are alternatives as determined by microbiological sensitivities. Infection acquired abroad should be presumed to be multiantibiotic resistant. Pharyngeal and rectal infection may be particularly difficult to eliminate. A repeated culture to test for a cure is made 4–7 days after treatment. Patients with gonorrhoea should be screened for coexisting sexually transmitted diseases, e.g. chlamydia. Management is most appropriate in a department of genitourinary medicine where contact tracing can be organized.
Vulval disorders
The vulva can be involved in many conditions, and itching (pruritus vulvae), often followed by secondary lichenification, is frequent. Commonly seen dermatoses include:
 lichen sclerosus (p. 41)
lichen sclerosus (p. 41)
 eczemas including allergic contact dermatitis (Fig. 3) and seborrhoeic dermatitis (p. 38)
eczemas including allergic contact dermatitis (Fig. 3) and seborrhoeic dermatitis (p. 38)
 psoriasis (p. 28)
psoriasis (p. 28)
 lichen planus (p. 40).
lichen planus (p. 40).
Herpes simplex (p. 54), viral warts (p. 52), candidiasis (p. 58), venereal infections (see above) and extramammary Paget’s disease (p. 88) also occur. Other specific disorders include the following:
 Vulval intraepithelial neoplasia (VIN): includes in situ squamous cell carcinoma and Bowenoid papulosis (Fig. 4). Cervical intraepithelial neoplasia can coexist and screening is required. Human papillomavirus infection may predispose to the precancerous change. There is a small risk of progression to invasive squamous cell carcinoma. Treatment is by cryosurgery or excision (for small areas), topical fluorouracil and laser therapy. Follow-up is needed.
Vulval intraepithelial neoplasia (VIN): includes in situ squamous cell carcinoma and Bowenoid papulosis (Fig. 4). Cervical intraepithelial neoplasia can coexist and screening is required. Human papillomavirus infection may predispose to the precancerous change. There is a small risk of progression to invasive squamous cell carcinoma. Treatment is by cryosurgery or excision (for small areas), topical fluorouracil and laser therapy. Follow-up is needed.
 Vulvodynia: a chronic vulval discomfort, often with burning and soreness. It is sometimes due to erosive vulvitis, e.g. from lichen planus or VIN. Some patients have underlying psychological problems.
Vulvodynia: a chronic vulval discomfort, often with burning and soreness. It is sometimes due to erosive vulvitis, e.g. from lichen planus or VIN. Some patients have underlying psychological problems.
 Genital ulceration: may occur with pemphigoid or pemphigus (p. 78), or acutely with erythema multiforme. It is also seen with Behçet’s syndrome, a multisystem disorder in which recurrent oral aphthous ulceration and iridocyclitis also occur.
Genital ulceration: may occur with pemphigoid or pemphigus (p. 78), or acutely with erythema multiforme. It is also seen with Behçet’s syndrome, a multisystem disorder in which recurrent oral aphthous ulceration and iridocyclitis also occur.
Penile and scrotal eruptions
Balanitis (inflammation of the penile skin; Fig. 5) and scrotal eruptions can be caused by a similar list of conditions to those outlined above for vulval dermatoses. Specific disorders include:
 circinate balanitis, an eroded or crusted penile eruption seen in Reiter’s syndrome (p. 42)
circinate balanitis, an eroded or crusted penile eruption seen in Reiter’s syndrome (p. 42)
 scrotal gangrene, a necrotizing cellulitis of rapid onset, seen in diabetics. It has a mortality rateof 45%.
scrotal gangrene, a necrotizing cellulitis of rapid onset, seen in diabetics. It has a mortality rateof 45%.
Pruritus ani
The perianal skin is frequently involved in infective, inflammatory and occasionally neoplastic conditions, as for the genitalia. Pruritus ani is common in middle-aged men. Whatever the underlying dermatosis, faecal contamination of the perianal skin with bacteria, enzymes and allergens causes inflammation and itch. Persistent rubbing induces lichen simplex (p. 39) or maceration, and secondary infection with bacteria or fungi. A compounding contact dermatitis due to allergy to ‘over-the-counter’ creams is common. Anal carcinoma, fissure or haemorrhoids, and threadworm infestation in children, should be excluded.
Treatment requires attention to personal hygiene (daily baths are helpful but avoid the use of soap) and the topical application of an emollient, antiseptic or steroid preparation.