CHAPTER 39 Local Anesthesia
 Describe anesthetic agents and vasoconstrictors used in dentistry, and discuss the rationale for using a particular agent.
Describe anesthetic agents and vasoconstrictors used in dentistry, and discuss the rationale for using a particular agent. Assess clients' health and pharmacologic history to determine their suitability to receive local anesthetics or vasoconstrictors.
Assess clients' health and pharmacologic history to determine their suitability to receive local anesthetics or vasoconstrictors. Assemble, disassemble, and properly maintain the armamentarium required for local anesthetic administration.
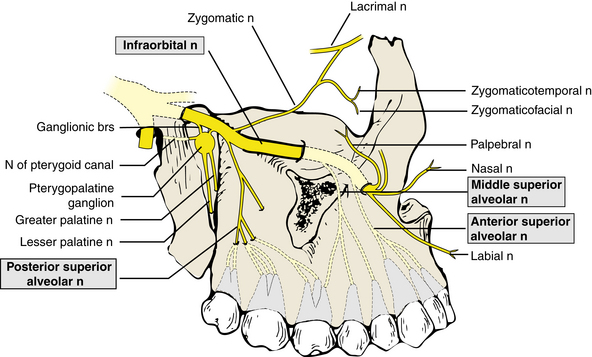
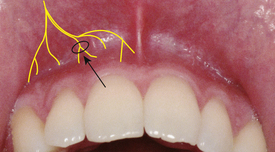
Assemble, disassemble, and properly maintain the armamentarium required for local anesthetic administration. Identify the anatomic landmarks on both a skull and a client for the following injections: supraperiosteal, anterior superior alveolar nerve block, infraorbital nerve block, middle superior alveolar nerve block, posterior superior alveolar nerve block, greater palatine nerve block, nasopalatine nerve block, inferior alveolar nerve block, lingual nerve block, buccal nerve block, mental nerve block, incisive nerve block.
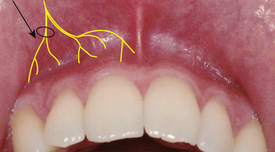
Identify the anatomic landmarks on both a skull and a client for the following injections: supraperiosteal, anterior superior alveolar nerve block, infraorbital nerve block, middle superior alveolar nerve block, posterior superior alveolar nerve block, greater palatine nerve block, nasopalatine nerve block, inferior alveolar nerve block, lingual nerve block, buccal nerve block, mental nerve block, incisive nerve block.Local anesthesia is the loss of sensation in a circumscribed area of the body as a result of the depression of excitation in nerve endings or the inhibition of the conduction process in peripheral nerves.1 Local anesthetic agents used in clinical practice today prevent both the generation and conduction of nerve impulses. Essentially the local anesthetic agent provides a chemical roadblock between the source of the impulse (e.g., a periodontal abscess) and the brain. The impulse is unable to reach the brain and is therefore not interpreted as pain or discomfort by the client. Local anesthesia differs dramatically from general anesthesia in that local anesthesia produces loss of sensation without inducing a loss of consciousness.1
Not all dental hygiene clients require local anesthesia. Those receiving preventive oral prophylaxis or even periodontal maintenance care may experience little or no discomfort; however, local anesthetic administration usually is required if the dental hygiene care plan includes therapeutic scaling and root planing, or if a client is simply experiencing undue tooth or soft-tissue sensitivity. In addition, a dental hygienist working in collaboration with a dentist may be called on to anesthetize individuals for the dentist in preparation for restorative or surgical periodontal therapy.
PHYSIOLOGY OF NERVE CONDUCTION
To understand how local anesthetic agents work, the dental hygienist needs to be familiar with the physiology of nerve conduction. Two principal ions are needed for nerve conduction: potassium (K+) and sodium (Na+). Because these two molecules are positively charged, they normally exist in equal concentration across a membrane; however, in a nerve cell this equilibrium does not exist (Figure 39-1, Phase 1). Because of a sodium pump located within the cell membrane, the positively charged sodium molecules are forced outside the nerve cell. As the sodium leaves the intracellular fluid, a state of negativity is created inside the nerve cell. At the same time the extracellular fluid, which has received the sodium, becomes positive. Once the sodium ion is transported out of the cell, it is not able to diffuse back into the intracellular fluids because of the relative impermeability of the nerve membrane to this ion. Although the nerve membrane is freely permeable to the potassium, this ion remains within the nerve cell because the negative charge of the nerve membrane restrains the positively charged ion by electrostatic attraction. The nerve is polarized or in a resting state or at resting potential when this balance exists between positive sodium ions on the outside of the nerve membrane and negative potassium ions on the inside of the membrane. Polarization of the membrane continues as long as the nerve remains undisturbed.
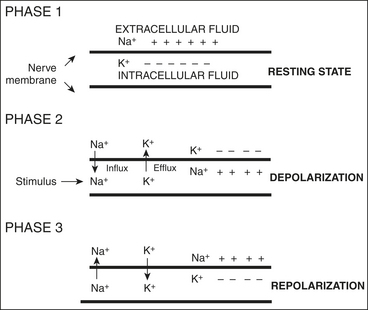
Figure 39-1 Rapid sequence of changes, depolarization and repolarization, is termed action potential.
A stimulus, which may be chemical, thermal, mechanical, or electrical in nature (such as pain), produces excitation of the nerve fiber and therefore a change in the ion balance (see Figure 39-1, Phase 2). During this phase, referred to as depolarization, the nerve membrane becomes more permeable to the sodium ion. Consequently the positive sodium ions move rapidly across the nerve membrane to the inside of the nerve cell. During this influx of sodium the potassium ions diffuse from the inside to the outside of the nerve membrane. Thus during depolarization the ion balance of the nerve cell reverses. On the interior of the nerve membrane are the positive sodium ions, whereas on the exterior of the nerve cell are the potassium ions. The inside of the nerve is now electrically positive compared with the outside of the nerve.
Immediately after depolarization, the permeability of the membrane to the sodium ion once again decreases (see Figure 39-1, Phase 3). This situation is referred to as repolarization. During this phase, the sodium pump actively transports the sodium ion out of the nerve cell, while potassium ions diffuse and are pumped to the inside of the nerve cell. Thus the nerve's resting potential is reestablished, whereby the interior of the nerve cell is negative and the exterior of the nerve cell consists of the positive sodium ions. This rapid sequence of changes, depolarization and repolarization, is termed action potential.
Once the resting potential of the nerve membrane is disrupted by a stimulus, such as pain, and depolarization occurs, the impulse must be transmitted along the nerve fiber. This impulse propagation is achieved when the ion changes during depolarization produce a new electrical equilibrium (the interior of the cell changing from negative to positive, the exterior of the cell changing from positive to negative). These ion changes in turn produce local currents that flow from the depolarized segment of the nerve to the adjacent resting area. As a result of this electrical current flow, depolarization begins in this previously resting area and continues propagating itself along the entire length of the nerve fiber. Thus the depolarization step begins a chain reaction that continues the action potential along the nerve. In this manner, the impulse is propelled along the nerve fiber to the central nervous system (CNS).1
Mechanism of Action of Local Anesthetic Agents
Although there are several theories on how local anesthetics work, it is commonly accepted that the primary action of these drugs is in reducing the nerve membrane permeability to the sodium ions (Na+). The nerve membrane remains impermeable to the sodium ions despite the introduction of a stimulus to the nerve. Because the sodium ions remain on the outside of the nerve cell and are unable to enter the nerve membrane, an action potential never occurs. The nerve cell remains in a polarized state (resting state) because the ionic movements responsible for the action potential do not develop. Thus the action of depolarization that is required to initiate or to continue nerve impulse transmission (propagation) is blocked. An impulse that arrives at the blocked nerve segment is unable to be transmitted to the brain and is therefore not interpreted as pain or discomfort by the client.
LOCAL ANESTHETIC AGENTS
Although many drugs are classified as local anesthetics, only a few are used in dentistry. Ester-type local anesthetics continue to be used as topical anesthetics (primarily benzocaine), but the injectable ester-type local anesthetics have been taken off the market. Currently the injectable local anesthetic agents employed in North America consist exclusively of amides1 (Table 39-1).
TABLE 39-1 Amide Local Anesthetics
| Generic Name | Proprietary Name |
|---|---|
| Articaine | Septocaine |
| Bupivacaine | Marcaine |
| Lidocaine | Xylocaine, Alphacaine, Octocaine |
| Mepivacaine | Carbocaine, Arestocaine, Isocaine, Polocaine |
| Prilocaine | Citanest |
Metabolism (Biotransformation) and Excretion
The mechanism by which local anesthetic agents are metabolized is important because the overall toxicity of an agent depends on the balance between the agent's rate of absorption into the bloodstream at the injection site and the rate of the agent's removal from the blood through the processes of tissue uptake and metabolism.
Amide local anesthetics undergo biotransformation in the liver by microsomal enzymes. Therefore the liver function of a client influences the rate of biotransformation of an amide drug. Those clients with impaired liver function are unable to metabolize amide local anesthetics at a normal rate, thereby leading to excessive levels of the agent in the blood, which increases the potential for toxic overdose (see the later discussions of preanesthetic client assessment and systemic complications).
The metabolic products of amide local anesthetics are almost entirely excreted by the kidneys. In addition, a small amount of a given dose of local anesthetic agent is excreted unchanged in the urine. Amides are usually excreted in their original form in small concentrations in the urine. Clients with significant renal impairment or those undergoing renal dialysis may be unable to efficiently remove the unchanged form of the local anesthetic compound or its breakdown products from their blood, leading to elevated local anesthetic levels and an increased potential for toxicity (see the later discussions of preanesthetic client assessment and systemic complications).1
VASOCONSTRICTORS
All local anesthetic agents presently used in dentistry produce some degree of vasodilation (relaxation of the blood vessel wall resulting in increased blood flow to the injection site). After local anesthetic injection into the tissues the following reactions occur1:
 Accelerated rate of absorption of the local anesthetic into the bloodstream, causing the anesthetic to be carried away from the injection site
Accelerated rate of absorption of the local anesthetic into the bloodstream, causing the anesthetic to be carried away from the injection site Higher amounts of local anesthetic in the blood, with the attendant greater risk for an overdose reaction
Higher amounts of local anesthetic in the blood, with the attendant greater risk for an overdose reaction Decreased duration of action and decreased effectiveness of the local anesthetic because it diffuses away from the site of administration more rapidly
Decreased duration of action and decreased effectiveness of the local anesthetic because it diffuses away from the site of administration more rapidlyTo counteract the vasodilating properties of local anesthetic agents, vasoconstrictors are added to the local anesthetic solution. Vasoconstrictors are drugs that constrict the blood vessels and thus control blood flow in the area of the injection. Vasoconstrictors are important additions to a local anesthetic solution because vasoconstriction leads to the following1:
 Slowed rate of absorption of the local anesthetic into the bloodstream, thus keeping it at the injection site longer and producing lower levels in the bloodstream
Slowed rate of absorption of the local anesthetic into the bloodstream, thus keeping it at the injection site longer and producing lower levels in the bloodstream Lower amounts of local anesthetic in the blood, thereby decreasing the risk for an overdose reaction (or reducing the potential for systemic toxicity)
Lower amounts of local anesthetic in the blood, thereby decreasing the risk for an overdose reaction (or reducing the potential for systemic toxicity) Increased duration of action and increased effectiveness of the local anesthetic as higher concentrations of the agent remain in and around the nerve for a longer period
Increased duration of action and increased effectiveness of the local anesthetic as higher concentrations of the agent remain in and around the nerve for a longer periodVasoconstrictors are an important addition to a local anesthetic solution because they decrease the potential toxicity of the anesthetic solution while increasing the duration and effectiveness of pain control. For example, the addition of 1:100,000 or 1:200,000 epinephrine to 2% lidocaine increases the duration of pulpal and hard-tissue anesthesia from approximately 10 minutes to 60 minutes. Dental hygiene appointments are frequently 60 minutes in length, and therefore vasoconstrictors are necessary to provide a pain-free state for clients during completion of dental hygiene care.
Moreover, dental hygiene care often involves soft-tissue manipulation, and hemorrhage is a frequent result, especially when inflammation is present. The use of local anesthetics without vasoconstrictors is problematic because the vasodilating properties of the anesthetic actually increase bleeding at the site of the injection. Vasoconstrictors are added to the anesthetic solution to counteract this unwanted action by preventing or minimizing bleeding during dental hygiene care.
For pain control when providing dental hygiene care, nerve blocks, such as the posterior superior alveolar (PSA) or inferior alveolar nerve block, are frequently the technique of choice. To derive the benefits of bleeding control from the vasoconstrictor, however, the drug must be administered, via local infiltration, directly into the area where the bleeding is occurring or is expected to occur. For example, to provide pain control to the maxillary molars and the buccal tissue over these teeth, a PSA nerve block is administered. The anesthetic agent is deposited posterior and superior to the posterior border of the maxilla, some distance from the area being anesthetized. If hemostasis is needed on the buccal tissue over any of the molars, however, the administration of a local infiltration into the area is necessary even though the anesthesia may be profound. Fortunately, only small volumes of solution are required (approximately 1 mL) for hemostatic purposes.1
Mechanism of Action
The sympathetic nervous system component of the autonomic nervous system, in addition to other functions, controls the dilation and constriction of various blood vessels throughout the body. Adrenalin, also known as epinephrine, is one of the naturally occurring agents responsible for sympathetic nervous system activity.1 The vasoconstrictors used with local anesthetics are chemically identical to or very similar to adrenalin produced naturally during sympathetic nervous system stimulation. Therefore, because the actions of the vasoconstrictors so closely mimic the action of the sympathetic autonomic nervous system, they are referred to as sympathomimetic or adrenergic agents.
Throughout the tissues of the body, adrenergic receptors are found that are stimulated by the chemicals released by the sympathetic nervous system or a sympathomimetic agent (drug). These receptor sites are divided into two major categories: alpha and beta. Activation of the alpha receptors by a sympathomimetic agent (drug) results in contraction of the smooth muscle in blood vessels. This contraction produces a constriction of the vessels referred to as vasoconstriction. The primary reason sympathomimetic agents are added to local anesthetic solutions is to produce this desirable vasoconstriction.
Activation of the beta receptors by a sympathomimetic agent (drug) produces smooth muscle relaxation and cardiac stimulation. Beta receptors have been further characterized as beta1 and beta2. Activation of beta1 receptors increases cardiac rate and force, whereas beta2 receptors are responsible for bronchodilation and vasodilation. Those changes resulting from beta-receptor stimulation are undesirable side effects of sympathomimetic drug incorporation into local anesthetic solutions. These beta effects are potentially hazardous.2
Concentrations
Vasoconstrictor concentrations are most often expressed as a ratio, such as one part per 100,000. This ratio appears as 1:100,000 in a written format. Table 39-2 lists the vasoconstrictors and their concentrations that are incorporated into dental local anesthetic solutions in the United States and Canada. The least concentrated solution that produces effective pain control should be used.1
TABLE 39-2 Vasoconstrictors Used in Dental Local Anesthetic Solutions
| Generic Name | Proprietary Name | Concentrations |
|---|---|---|
| Epinephrine | Adrenalin | |
| Levonordefrin∗ | Neo-Cobefrin | 1:20,000 |
| Norepinephrine (levarterenol)† | Levophed | 1:30,000 |
Epinephrine
Epinephrine is available as a synthetic and is also obtained from the adrenal medulla of animals. Whereas a variety of vasoconstrictors are used presently in oral healthcare, epinephrine is the most potent and widely employed and is the standard by which all other vasoconstrictors are measured. Epinephrine 1:100,000 is the most commonly used concentration; however, it is thought that the optimal concentration for prolongation of pain control is 1:200,000 or even 1:250,000. The use of 1:50,000 epinephrine for pain control is neither necessary nor recommended. The 1:50,000 dilution contains twice the epinephrine per milliliter as a 1:100,000 dilution and four times that contained in a 1:200,000 concentration and does not increase the quality or duration of pain control. Although the 1:50,000 dilution may be more effective in the control of bleeding, effective hemostasis also may be obtained with concentrations of 1:100,000 epinephrine.
There are few contraindications to vasoconstrictor administration in the concentrations in which they are found in dental local anesthetics. Because there is always concern about the systemic effects, however, it is recommended that the less-concentrated solution be used, particularly with clients known to be cardiovascularly compromised.3 For all clients, however, the benefits and risks of including a vasoconstrictor in the local anesthetic solution must be weighed against the benefits and risks of using an anesthetic solution without a vasoconstrictor. (See later sections on preanesthetic client assessment and systemic complications.)
Side Effects and Overdose
Epinephrine overdose (due to high amounts in the blood) relates to CNS stimulation. Clinical manifestations include increasing fear and anxiety, tension, restlessness, throbbing headache, tremor, weakness, dizziness, pallor, respiratory difficulty, and palpitation. With increasing levels of epinephrine in the blood, cardiac dysrhythmias, ventricular fibrillation, dramatic increase in blood pressure, and stroke are rare but possible. Because of epinephrine's rapid inactivation, overdose reactions are usually brief. Nevertheless, in cardiovascularly compromised clients, it is prudent to limit or avoid exposure to vasoconstrictors if possible. Table 39-3 lists the maximum doses of epinephrine recommended by Malamed and others.1
TABLE 39-3 Recommended Maximum Doses of Epinephrine
| Epinephrine Concentration (mcg/Cartridge) | CARTRIDGES (ROUNDED OFF) | |
|---|---|---|
| Normal, Healthy Patient (ASA I)∗ | Patient with Clinically Significant Cardiovascular Disease (ASA III or IV)† | |
| 1:50,000 (36) | 5.5 | 1 |
| 1:100,000 (18) | 11‡ | 2 |
| 1:200,000 (9) | 22‡ | 4 |
ASA, American Society of Anesthesiologists.
∗ Maximum epinephrine dose of 0.2 mg or 200 mcg per appointment.
† Maximum recommended dose of 0.04 or 40 mcg per appointment.
‡ Actual maximum volume of administration is limited by the dose of local anesthetic drug.
From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.
Norepinephrine (Levarterenol)
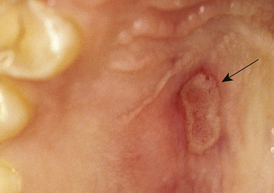
Norepinephrine (levarterenol) is one fourth as potent as epinephrine and is used clinically in a 1:30,000 dilution. Norepinephrine's clinical manifestations of overdose are similar to those of epinephrine but occur less frequently. The extravascular injection of norepinephrine, however, produces necrosis and sloughing (Figure 39-2). In the United States norepinephrine is no longer available in local anesthetic solutions used in dentistry.1
Levonordefrin
Levonordefrin is approximately one sixth (15%) as potent a vasoconstrictor as epinephrine and therefore is used in a greater concentration of 1:20,000. In 2003, local anesthetics containing levonordefrin were withdrawn from the market in the United States and Canada.1
SELECTION OF A LOCAL ANESTHETIC AGENT
Table 39-4 lists the local anesthetics and the combinations of vasoconstrictors that are currently available in the United States and Canada. The dental hygienist must weigh the following factors when determining the appropriate anesthetic agent to use during dental hygiene care:
 The duration of action of the local anesthetic agent and the length of time that pain control is needed
The duration of action of the local anesthetic agent and the length of time that pain control is neededTABLE 39-4 Local Anesthetic Agents and Duration of Pulpal and Soft-Tissue Anesthesia
| Agent | DURATION (APPROXIMATE MINUTES)∗ | |
|---|---|---|
| Pulpal | Soft Tissue | |
| Short Duration | ||
| Lidocaine HCl 2% | 5-10 | 60-120 |
| Prilocaine HCl 4% (by infiltration) | 5-10 | 90-120 |
| Mepivacaine HCl 3% | 20-40 | 120-180 |
| Intermediate Duration | ||
| Lidocaine HCl 2%, epinephrine 1:50,000 | 60 | 180-240 |
| Lidocaine HCl 2%, epinephrine 1:100,000 | 60 | 180-240 |
| Prilocaine HCl 4% (block) | 60 | 120-240 |
| Articaine HCl 4%, epinephrine 1:100,000 | 75 | 180-300 |
| Prilocaine HCl 4%, epinephrine 1:200,000 | 60-90 | 120-240 |
| Long Duration | ||
| Bupivacaine HCl 0.5%, epinephrine 1:200,000 | >90 | 240-540 |
HCl, Hydrochloride.
∗ Short-duration agents provide pulpal anesthesia for 30 minutes or less; intermediate-duration agents for approximately 60 minutes; long-term duration agents for longer than 90 minutes. The classification of duration is approximate. Variations may be noted.
Adapted from Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.
Duration of Action and Length of Time That Pain Control Is Needed
An important consideration when selecting a local anesthetic agent for pain control during dental hygiene care is the approximate duration of action of the local anesthetic agent, coupled with the length of time that pain control is needed. Table 39-4 lists the local anesthetic agents and their approximate duration of pulpal and soft-tissue anesthesia.
Box 39-1 classifies the local anesthetics more generally as short-, intermediate-, or long-acting. These time categories are approximations, and the actual duration of clinical anesthesia may vary. In addition to the presence or absence of a vasoconstrictor, several other factors described in the following sections may affect both the duration and depth of the anesthetic agent's action, either increasing or, more commonly, decreasing the drug's effectiveness.4
BOX 39-1 Approximate Duration of Action of Local Anesthetics
From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.
Variation in Response to the Agent Administered
Although most individuals respond predictably to an anesthetic agent (e.g., the duration of pulpal anesthesia after administration of 2% lidocaine with epinephrine 1:100,000 is approximately 60 minutes), some clients exhibit either a longer or a shorter duration of action than anticipated. This variation in response is normal and is simply a variation in the individual's reaction to the anesthetic agent.
Accuracy of the Administration of the Agent
Accuracy becomes significant when a substantial amount of soft tissue must be penetrated to reach the nerve to be anesthetized. For example, the inferior alveolar nerve block involves advancing through 20 to 25 mm of soft tissue before reaching the nerve, thereby influencing the accuracy of the injection. When injecting where it is not necessary to penetrate a large amount of tissue to block the nerve, however, such as with an infiltration, accuracy is seldom a problem.
Condition of the Soft Tissues at the Site of Drug Deposition
Anesthetic duration is increased in areas of decreased vascularity. Conversely, the presence of inflammation or infection increases vascularity and often decreases the anesthetic agent's duration of action as a result of more rapid absorption.
Anatomic Variation
The injection techniques described in this chapter are based on a “normal” anatomy. Of course, anatomic variations from this “norm” exist and can decrease the duration of local anesthetic action. Anatomic variations in the maxilla that may account for failed effectiveness and shortened duration include the following:
 Palatal roots of maxillary molars that flare more than normal to the midline of the palate, thus affecting the anesthetic's action on these roots
Palatal roots of maxillary molars that flare more than normal to the midline of the palate, thus affecting the anesthetic's action on these roots An unusually low zygomatic arch, common in children, which prevents anesthesia or lessens its duration in the first and second molars
An unusually low zygomatic arch, common in children, which prevents anesthesia or lessens its duration in the first and second molarsAnatomic variations in the mandible that are cause for concern include the following1,4:
Suggestions for overcoming these variations in anatomy when administering anesthetic solution are discussed in the section on injection techniques.
Type of Injection Administered
For any anesthetic solution administered, both pulpal and soft-tissue anesthesia are sustained for a longer period when a nerve block rather than a supraperiosteal infiltration injection is administered. For example, if 2% lidocaine with 1:100,000 epinephrine is administered, a PSA nerve block provides approximately 60 minutes of pulpal anesthesia, whereas a supraperiosteal injection (an infiltration) allows only 40 minutes of anesthesia. In order to achieve the desired duration, the recommended minimal volume of anesthetic must be administered.
Need for Pain Control after Treatment
Although the need for pain control after dental hygiene care may be limited, the dental hygienist should be advised that long-duration agents may be administered if posttreatment discomfort is a factor. Anesthetic agents, such as 4% prilocaine with 1:200,000 epinephrine, can provide 5 to 8 hours of soft-tissue anesthesia, whereas 0.5% bupivacaine or 1.5% etidocaine with 1:200,000 epinephrine can alleviate posttreatment discomfort for 8 to 12 hours. These agents can be administered before dental hygiene care is begun or even at the end of the care to allow for maximal posttreatment anesthesia. These drugs should not be given to children or to people who are mentally or physically disabled because these individuals may accidentally chew or bite the lip or tongue.
MAXIMAL SAFE DOSES OF LOCAL ANESTHETICS
All drugs, if administered in excess, are capable of producing an overdose reaction. The exact dose or the blood level at which a toxic reaction occurs is impossible to predict because biologic variability greatly influences how individuals respond to a drug. Recommended maximal doses, however, can be calculated to serve as a guideline for the dental hygienist. A maximal safe dose is the maximal amount of a drug that can be safely administered to a healthy individual. Maximal doses of injectable local anesthetics should be determined after consideration of the following factors1:
 Client's age. Individuals on both ends of the age spectrum (i.e., the young child or the elderly adult) may be unable to tolerate normal doses. Therefore the dose of local anesthetic should be decreased accordingly.
Client's age. Individuals on both ends of the age spectrum (i.e., the young child or the elderly adult) may be unable to tolerate normal doses. Therefore the dose of local anesthetic should be decreased accordingly. Client's physical status. The calculated dose must be adjusted for clients with compromised health. For example, a client with significant liver or renal dysfunction may be given a reduced dose of local anesthetics.
Client's physical status. The calculated dose must be adjusted for clients with compromised health. For example, a client with significant liver or renal dysfunction may be given a reduced dose of local anesthetics. Client's weight. The larger the individual (within limits), the greater the drug distribution. When administering a normal dose of local anesthetic to a large individual, the blood level of the drug is lower than that in a small person. Therefore a larger dose can be safely given. Although this rule is generally true, there may be exceptions, and care must always be exercised.
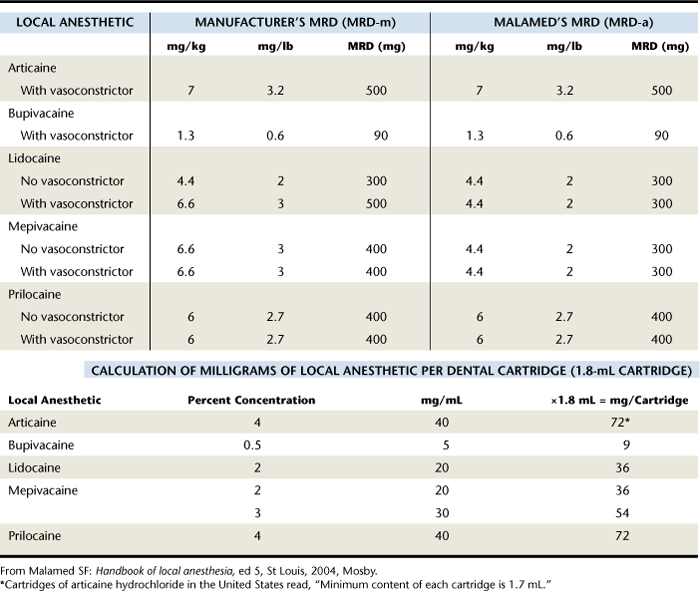
Client's weight. The larger the individual (within limits), the greater the drug distribution. When administering a normal dose of local anesthetic to a large individual, the blood level of the drug is lower than that in a small person. Therefore a larger dose can be safely given. Although this rule is generally true, there may be exceptions, and care must always be exercised.Table 39-5 lists the maximal safe doses recommended by manufacturers and by Malamed. The latter represents the most conservative of those recommended by the Council on Scientific Affairs of the American Dental Association (ADA), the United States Pharmacopeia, and the drugs' manufacturers.1 Table 39-5 also includes the milligrams of local anesthetic per cartridge for the available local anesthetic agents. It is important to note that the maximal doses are expressed in terms of milligrams per pound of body weight. Therefore the dental hygienist must be familiar with the relationship among solution percentage, the number of milligrams of solution contained per cartridge, the client's body weight, and the maximum recommended dose per pound. With this information the hygienist can calculate the maximum dose and the number of cartridges that could be administered.
Box 39-2 provides examples of how to calculate maximum doses and numbers of local anesthetic cartridges to be administered to various clients when only one local anesthetic is used. Box 39-3 provides similar calculation examples for when multiple drugs are used.1
BOX 39-2 Calculation of Maximum Doses and Number of Cartridges (Single Drug)
From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.
Patient: 6 Years Old, Healthy, Male, 40 lb
BOX 39-3 Calculation of Maximum Doses and Number of Cartridges (Multiple Drugs)
From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.
Patient: 100-lb Female, Healthy
How much lidocaine can this patient receive?
MRD-a, Author's maximum recommended dose; MRD-m, manufacturer's maximum recommended dose.
Fortunately, maximum doses are unlikely to be reached for most dental hygiene procedures. If the dental hygiene care plan involves scaling and root planing a quadrant, the administration of one to two cartridges often suffices. There is seldom a need to administer more than four cartridges during any appointment involving dental hygiene care.
In addition to considering the recommended maximal safe doses, the dental hygienist must follow other procedural guidelines to increase safety during administration of local anesthetics and prevent an overdose reaction. These include the following:
A more detailed discussion of these guidelines can be found later, in the section on procedures for a successful injection and complications.
PREANESTHETIC CLIENT ASSESSMENT
To meet the human need for protection from health risks, an evaluation of the client's health history and current health status is an essential prerequisite to dental hygiene care. The dental hygienist must ascertain if any conditions represent contraindications or require alterations to the dental hygiene care plan to eliminate or decrease client risk. The administration of local anesthetic and vasoconstricting agents provides an additional rationale for a thorough health history and health status review. Local anesthetics and vasoconstrictors, like all drugs, exert actions on multiple body systems. It is important to evaluate, through the health history, the client's ability to physically tolerate them, to determine a history of allergic responses, and to identify current medications. Collection of these data guides the dental hygienist in determining the appropriateness of administering a local anesthetic or vasoconstrictor, of seeking medical consultation, and of modifying the dental hygiene care plan. A thorough preanesthetic client assessment helps prevent or minimize complications and emergencies.2
Contraindications to local anesthetics and vasoconstrictors are divided into two categories: absolute and relative. Absolute contraindications require that the drug in question not be administered to the individual under any circumstances.1 The administration of such a drug is contraindicated in all situations because it substantially increases the possibility of a life-threatening risk for the client. An example is a documented local anesthetic allergic reaction.
A relative contraindication means that the drug in question may be administered to the client after careful weighing of the risk of using the drug against its potential benefit, and if an acceptable alternative drug is not available. However, the smallest clinically effective dose always should be used.
Client Health Status
Although local anesthetics and vasoconstrictors are considered relatively safe drugs when administered properly, certain health conditions require limiting or eliminating their use. Table 39-6 summarizes those health conditions that may affect the selection of a local anesthetic or vasoconstrictor and appropriate actions that the dental hygienist may follow.1
TABLE 39-6 Health Conditions That Require Special Consideration When Local Anesthetics Are Administered
| Health Condition | Reason for Modification | Recommended Action |
|---|---|---|
| Hyperthyroidism | Possible exaggerated response to vasoconstrictors | Avoid or limit use (uncontrolled) of vasoconstrictors; use 3% mepivacaine or 4% prilocaine. |
| Atypical plasma cholinesterase | Toxic overdose to esters | Use amide anesthetic agents. |
| Methemoglobinemia | Potential for cyanosis-like state, respiratory distress, and lethargy in response to prilocaine and articaine | Use other anesthetic agents. |
| Malignant hyperthermia | Life-threatening syndrome caused by administration of certain drugs in combination with amide agents | Use amides or esters in normal doses; seek medical consultation. |
| Significant liver dysfunction | Difficulty metabolizing amide agents, potential for overdose | Seek medical consultation; use amide agents judiciously. |
| Significant renal dysfunction | Difficulty excreting local anesthetic agents, potential for overdose | Seek medical consultation; use anesthetic agents judiciously. |
| Pregnancy | Potential for complications with pregnancy | Avoid elective treatment during first trimester; use local anesthetics judiciously. |
Few health conditions, such as documented allergy, are absolute contraindications to vasoconstrictors in the concentrations found in local anesthetic solutions used in oral healthcare; however, the dental hygienist must carefully consider the benefits versus the risks of administering a vasoconstrictor to clients with a history of hypertension, cardiovascular disease, or hyperthyroidism because often the risks outweigh the benefits.
Current Client Medications
A drug interaction occurs when one drug modifies the action of another drug. A drug may potentiate or diminish the action of another drug and may alter the way in which another drug is absorbed, metabolized, or eliminated from the body.1,2 Although local anesthetics and vasoconstrictors exhibit few interactions with other drugs, the dental hygienist should consult the Physicians' Desk Reference or a comparable reference when a client reports being treated with any medication. This practice enables the clinician to assess both the drug's activity and the drug-to-drug interactions between the local anesthetic and vasoconstrictor and the prescribed medication. In doing so, the dental hygienist meets the client's human need for protection from health risks. If further questions remain regarding the use of a local anesthetic or vasoconstrictor while a prescribed medication is being taken, the dentist or the individual's physician should be consulted.
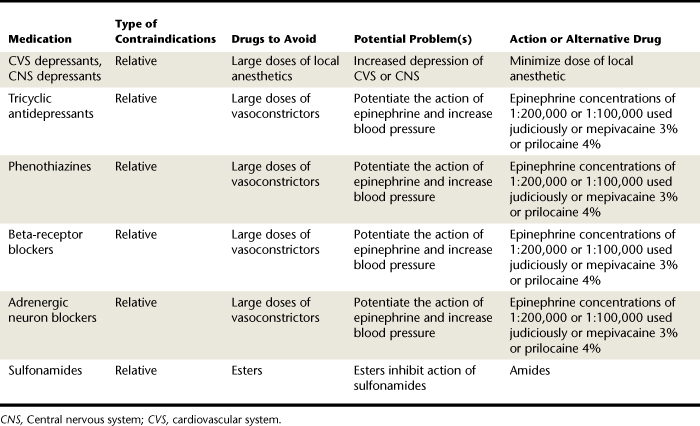
Table 39-7 summarizes those medications that may affect the selection of a local anesthetic or vasoconstrictor and appropriate actions the dental hygienist may choose.
Local anesthetics have proven to have few interactions with other prescribed drugs. Procaine has been cited as interfering with the action of anti-infective sulfonamide drugs. When CNS depressants or cardiovascular system (CVS) depressants are being taken by an individual, it is recommended that doses of local anesthetics be kept to a minimum because they may cause further depression.1,2
There are many conflicting reports of drug-to-drug interactions between vasoconstrictors and prescribed medications, but it is recommended that the dental hygienist proceed cautiously when administering a vasopressor to a person who is being treated with any of the following groups of drugs:
Currently, none of these drugs (described in the following paragraphs) poses an absolute contraindication to the administration of a vasoconstrictor; however, it is recommended that the dental hygienist exercise caution by administering the smallest dose that is clinically effective (such as that recommended for persons at cardiovascular risk) or eliminating the vasopressor entirely. If the dental hygienist is uncertain about the inclusion of a vasoconstrictor in the local anesthetic solution, consultation with the client's physician is advisable.
Tricyclic Antidepressants
Tricyclic antidepressant medications (e.g., amitriptyline, clomipramine, imipramine) have been cited as possibly potentiating the action of epinephrine and norepinephrine and resulting in an increase in blood pressure.2 Phenothiazines such as prochlorperazine are categorized as antipsychotic drugs but also are often prescribed for treatment of nausea. There is concern that these drugs, when combined with vasoconstrictors, may cause an exaggerated response to the vasopressor.
Beta-Receptor Blockers
Beta-receptor blockers such as propranolol, nadolol, timolol, pindolol, or penbutolol decrease systolic and diastolic blood pressures.3 (Note that these generic drugs end in “-olol.”) When these drugs are combined with epinephrine from a local anesthetic injection, however, significant increases in blood pressure may result.
Adrenergic Neuron Blockers
Adrenergic neuron blockers such as guanethidine and reserpine also are used to lower blood pressure through interference with the normal release of norepinephrine.1 When these drugs are combined with a vasoconstrictor, the effects of the vasopressor may be exaggerated, resulting in an increase in blood pressure.
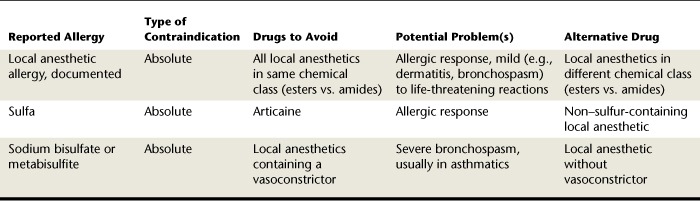
Allergies
An allergy is a hypersensitive reaction acquired through exposure to a specific substance (allergen); reexposure to the allergen increases one's potential to react. Approximately 1% of all reactions that occur during local anesthetic administration are true allergic reactions.1 A documented local anesthetic allergy, however, represents an absolute contraindication and must be investigated for authenticity. Table 39-8 summarizes allergies that affect the selection of a local anesthetic agent or vasoconstrictor and appropriate alternative drugs the dental hygienist may choose. A true allergic response to a pure amide drug is extremely rare. A true allergy to amides may exist; however, a verifiable occurrence is virtually nonexistent.
Allergic reactions have been documented for various contents of the dental cartridge. Sodium bisulfite and metabisulfite are antioxidants that are incorporated into local anesthetic solutions to act as preservatives for the vasoconstrictor. In addition to their use in local anesthetic cartridges, these agents are often sprayed on fruits and vegetables to keep them appearing fresh. They also are included in a variety of canned foods. Allergy to the bisulfites has been reported.5-8 Clients with a history of asthma may be particularly susceptible to an allergic response. The U.S. Food and Drug Administration (FDA) estimates that 5% of the 9 million allergy sufferers in the United States may be hypersensitive to sulfites.1 The FDA has enacted regulations limiting the use of bisulfites on food. If a client reports a history of sulfite sensitivity, the dental hygienist should be alerted to the possibility of a similar response if a sulfite is included in the dental cartridge. Although sodium bisulfite or metabisulfite is found in all dental cartridges containing a vasoconstrictor, these agents are not included in solutions in which there is no vasopressor. Therefore it is recommended that the dental hygienist administer local anesthetics containing no vasoconstrictor to clients with a history of sulfite sensitivity.1
ARMAMENTARIUM
The equipment essential for the administration of a local anesthetic agent includes the following:
Syringe
The syringe is that component of the local anesthetic armamentarium that holds the needle and cartridge of anesthetic (thus allowing the solution to be delivered to the client). Several types of syringes may be used for local anesthetic administration, as follows1:
The syringes most often employed in oral healthcare are the reusable aspirating syringe and the self-aspirating syringe.
Reusable Breech-Loading Metallic Cartridge-Type Aspirating Syringe
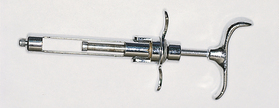
The reusable breech-loading metallic cartridge-type aspirating syringe is the most commonly used syringe for administration of an intraoral local anesthetic agent (Figure 39-3).
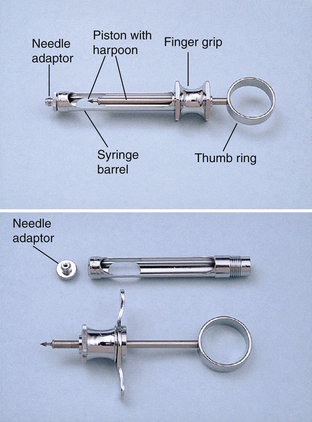
Figure 39-3 Breech-loading metallic cartridge-type syringe.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
The needle is affixed to the threaded portion (or needle adaptor) at one end of the syringe. At the other end a thumb ring and finger rest provide the dental hygienist with a means to grasp and control the syringe. The body of the syringe holds the cartridge of anesthetic solution. The aspirating syringe is characterized by a barbed piston also referred to as the harpoon. The harpoon engages the rubber or silicone stopper of the cartridge of anesthetic. The harpoon allows the dental hygienist to exert negative pressure on the thumb ring to assess the location of the lumen of the needle, a procedure referred to as aspiration. If the needle lumen rests within a blood vessel, blood appears in the cartridge after negative pressure is applied to the thumb ring. If this should occur, the dental hygienist needs to withdraw the needle, replace the cartridge of anesthetic solution, and repeat the procedure. Positive pressure on the thumb ring injects the anesthetic solution into the tissues. Advantages and disadvantages are listed in Box 39-4.
Reusable Breech-Loading Metallic Cartridge-Type Nonaspirating Syringe
The reusable breech-loading metallic cartridge-type nonaspirating syringe does not have a harpoon on the end of the piston, and therefore the dental hygienist is unable to aspirate before depositing the anesthetic solution (Figure 39-4).
It is impossible for the dental hygienist to ascertain the precise location of the needle tip with a nonaspirating syringe, and therefore this type of instrument should never be employed when a local anesthetic is administered during dental hygiene care.
Reusable Breech-Loading Metallic Cartridge-Type, Self-Aspirating Syringe
The importance of aspirating before injecting an anesthetic solution is widely accepted, and the self-aspirating syringe was developed to aid the oral healthcare provider in completing this important step. This type of syringe achieves the negative pressure necessary for aspiration via the elasticity of the rubber diaphragm in the cartridge of anesthetic. When the cartridge is placed in the syringe, the diaphragm rests against a metal projection inside the syringe; this projection also directs the needle into the cartridge (Figure 39-5).

Figure 39-5 A metal projection within the barrel depresses the diaphragm of the local anesthetic cartridge.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
Pressure exerted by the dental hygienist on the thumb disk (Figure 39-6) or on the plunger by way of the thumb ring moves the cartridge slightly toward the metal projection, thereby stretching the rubber diaphragm. When the pressure is released, the cartridge rebounds slightly, thus producing enough negative pressure within the cartridge to achieve aspiration. Therefore the dental hygienist does not need to pull back on the thumb ring to aspirate, as is necessary with an aspirating syringe.

Figure 39-6 Pressure exerted on the thumb disk (as shown in figure), or the thumb ring increases pressure within the cartridge. Aspiration occurs when the pressure is released.
Box 39-5 lists advantages and disadvantages of the metallic, self-aspirating syringe.
BOX 39-5 Advantages and Disadvantages of the Wand or CompuDent System
From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.
| Advantages | Disadvantages |
|---|---|
Computer-Controlled Local Anesthetic Delivery
The CompuDent (formerly known as the Wand) is a computer-controlled local anesthetic delivery system that can be used instead of the traditional breech-loading aspirating syringe (Figure 39-7). The CompuDent has several unique features. The handpiece is light and ergonomic; it is held in a pen grasp instead of a palm grasp, allowing a higher level of comfort and control for the clinician (Figure 39-8). The handpiece is also good for use with fearful clients because it looks nothing like the traditional syringe and therefore is much less threatening. The local anesthetic delivery is controlled by a computer that regulates the flow rate of the agent and the pressure of the deposition. The computer-controlled rate allows for creation of an anesthetic pathway immediately in front of the needle as it moves through the soft tissues, resulting in a high level of comfort for the client. Particularly with administration of palatal injections, the CompuDent can greatly increase client comfort and acceptance of local anesthetic procedures.
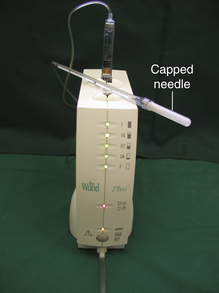
Figure 39-7 Computer-controlled local anesthetic delivery system: the Wand or CompuDent.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
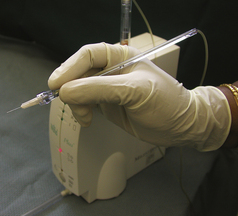
Figure 39-8 Lightweight handpiece.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
To initiate anesthetic delivery and aspiration, the clinician controls the computer via a foot pedal (Figure 39-9). The pedal allows for two levels of deposition: (1) a slow rate—one drop of anesthetic every 2 seconds, and (2) a fast rate—a steady stream of anesthetic. Removing the foot from the pedal, the clinician can initiate a 5-second aspiration cycle. By allowing the clinician to control the needle with the fine muscles of the hand rather than the large muscles required to operate a traditional syringe, the clinician can penetrate the soft tissues by gently rotating the needle back and forth between the thumb and fingers (bidirectional rotation) rather than by the typical linear penetration. This technique has two advantages: (1) by allowing the bevel to cut into the tissues by rotating, the technique causes no tearing of the tissue on penetration; (2) the bidirectional rotation results in less needle deflection as the tissue is penetrated. The lessened needle deflection can increase the effectiveness of the injection because the needle is more likely to be at the desired deposition site.1 Advantages and disadvantages of this computer-controlled local anesthetic delivery system are listed in Box 39-6.
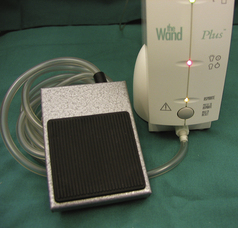
Figure 39-9 Foot-activated control.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
Pressure-Type Syringe
Another type of syringe that the dental hygienist may encounter is a pressure-type syringe (Figure 39-10).

Figure 39-10 Second-generation pressure syringes for periodontal ligament injection.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
This type of instrument is presently used for the administration of a periodontal ligament (PDL) injection or an intraligamentary injection (ILI), which provides pulpal anesthesia to one tooth on the mandible. A standard aspirating syringe can be used for this type of injection, but the pressure-type syringe is equipped with a trigger mechanism that delivers a measured dose (0.2 mL) of anesthetic solution and allows the administrator to more easily express the solution despite significant tissue resistance. This type of syringe permits easy administration of the solution; however, the dental hygienist must take care to slowly inject even this small measured dose of anesthetic agent. If deposition of the agent is done too rapidly, client discomfort may ensue during the injection and after the anesthesia has worn off. See Box 39-7 for advantages and disadvantages of the pressure-type syringe.1
Jet Injector Syringe
The jet injector syringe delivers 0.05 to 0.2 mL of anesthetic agent to the mucous membranes at a high pressure (2000 psi) via small openings called jets (Figure 39-11). The jet injector is used primarily to obtain topical anesthesia before insertion of a needle or to achieve soft-tissue anesthesia of the palate. To acquire complete anesthesia, nerve blocks or supraperiosteal injections also must be administered with a conventional syringe and needle. With the jet injector the anesthetic solution is delivered without the use of a needle; therefore it becomes a needleless injection. Clients may dislike the jolt of the jet injection, however, and postinjection discomfort may follow. Properly applied topical anesthetics accomplish the same objectives as the jet injector.1
Disposable Syringe
Disposable plastic syringes are most often used for intramuscular or intravenous drug administration, but they may be employed during intraoral injections. These syringes do not accept standard dental cartridges, and therefore it is necessary to insert the attached needle into a vial or cartridge of local anesthetic drug and eject the appropriate amount of solution. Furthermore, because these syringes have no thumb ring, aspiration is difficult and may require two hands. Because the disadvantages of the disposable syringe far outweigh the advantages, this type of syringe is not recommended for routine use.
Care and Handling of the Syringe
Recommendations for the care of reusable syringes used for local anesthetic administration follow1:
 The syringe should be sterilized after each use, following the appropriate infection-control protocol. Deposits resembling rust may accumulate on the syringe and interfere with function and appearance. Such deposits may be removed by ultrasonic cleaning or scrubbing (see Chapter 7).
The syringe should be sterilized after each use, following the appropriate infection-control protocol. Deposits resembling rust may accumulate on the syringe and interfere with function and appearance. Such deposits may be removed by ultrasonic cleaning or scrubbing (see Chapter 7).Problems with the Syringe
 Bent harpoon. The syringe harpoon must be sharp and straight to embed the rubber stopper of the cartridge. If the harpoon becomes bent, it may fail to engage the rubber stopper of the cartridge accurately. Consequently, aspiration may be unreliable.
Bent harpoon. The syringe harpoon must be sharp and straight to embed the rubber stopper of the cartridge. If the harpoon becomes bent, it may fail to engage the rubber stopper of the cartridge accurately. Consequently, aspiration may be unreliable. Disengagement of the harpoon from the rubber stopper of the cartridge during aspiration. Disengagement may ensue if the harpoon is dull or if the dental hygienist applies excessive pressure to the thumb ring during aspiration. With regard to aspiration, only a gentle retraction of the thumb ring is needed; forceful action is not required.
Disengagement of the harpoon from the rubber stopper of the cartridge during aspiration. Disengagement may ensue if the harpoon is dull or if the dental hygienist applies excessive pressure to the thumb ring during aspiration. With regard to aspiration, only a gentle retraction of the thumb ring is needed; forceful action is not required. Difficulty aspirating because of practitioner's hand size. When using an aspirating syringe, the dental hygienist must be able to stretch her or his fingers and thumb to retract the thumb ring of the syringe. If this cannot be done effectively, reliable aspiration does not occur. Therefore it is important that the syringe fit the practitioner's hand. Most syringes are similar in their dimensions, but variations do exist. When selecting an aspirating syringe, it is beneficial to hold the syringe and test your ability to aspirate efficiently. If this is not possible, other syringes should be tested so that aspiration is easy to perform. A practitioner with small hands may use a self-aspirating syringe and thus avoid the step of pulling back on the thumb ring.
Difficulty aspirating because of practitioner's hand size. When using an aspirating syringe, the dental hygienist must be able to stretch her or his fingers and thumb to retract the thumb ring of the syringe. If this cannot be done effectively, reliable aspiration does not occur. Therefore it is important that the syringe fit the practitioner's hand. Most syringes are similar in their dimensions, but variations do exist. When selecting an aspirating syringe, it is beneficial to hold the syringe and test your ability to aspirate efficiently. If this is not possible, other syringes should be tested so that aspiration is easy to perform. A practitioner with small hands may use a self-aspirating syringe and thus avoid the step of pulling back on the thumb ring.Needle
The needle is the component of the armamentarium that delivers the anesthetic agent from the cartridge to the tissues surrounding the needle tip. Virtually all needles used in oral healthcare today are made of stainless steel, are presterilized by the manufacturer, and are disposable.
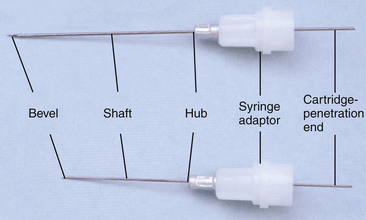
Parts of the Needle
Needles used for local anesthetic administration have several components (Figure 39-12). The bevel (Figure 39-13) is the angled surface of the needle point that is directed into the tissues. The shank is the length of the needle from the point to the hub. The hub or syringe adaptor is a plastic or metal piece that attaches the needle onto the syringe. The interior surface of metallic syringe adaptors is prethreaded. Plastic syringe adaptors are not prethreaded. Consequently, to attach a plastic-hubbed needle to a syringe, the dental hygienist must concurrently push and screw the needle onto the syringe. The syringe or cartridge-penetrating end enters the needle adaptor component of the syringe and engages the rubber diaphragm of the local anesthetic cartridge. This sterile needle is packaged in a plastic encasement consisting of two protective shields. A colored shield protects the part of the needle that is inserted into the tissues, and a clear or white shield covers the syringe and cartridge end of the needle.
Gauge
The gauge is the diameter of the lumen of the needle. The higher the gauge number, the smaller the diameter of the lumen. Therefore a 30-gauge needle has a smaller internal diameter than a 27-gauge needle. The most commonly employed needles in oral healthcare are the 25-, 27-, and 30-gauge needles.
A common assumption is that a larger-diameter needle (e.g., 25-gauge) is more uncomfortable to the client on insertion than a smaller-diameter needle (e.g., 30-gauge); however, this assumption is untrue. Research suggests that people cannot distinguish among a 25-, a 27-, and a 30-gauge needle when injected with each.1
Actually, larger-gauge needles (e.g., 25-gauge) have several advantages over smaller-gauge needles. Less deflection occurs when the larger-gauge needle passes through the tissues. Because it is larger and more rigid, it can be guided to the deposition site with minimal deviation, thus ensuring greater accuracy and a higher rate of injection success. This needle rigidity is particularly important with injections requiring significant penetration of the soft tissues, such as the inferior alveolar nerve block. Although needle breakage is uncommon with disposable needles, it is less likely to occur with a larger-gauge needle. Another advantage of larger-gauge needles is the ability to aspirate and thereby reduce the possibility of intravascular injections.
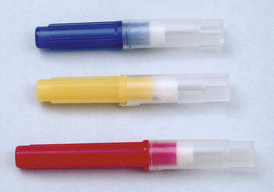
Opinions vary, but many authorities conclude that aspiration is easier and more reliable through the larger lumen, and smaller-gauge needles (e.g., 30-gauge) have diameters too narrow to adequately aspirate.1 Blood may be aspirated through a 25-, 27-, or 30-gauge needle, but more pressure is required when a smaller-gauge needle is employed. This difficulty in aspirating may decrease the reliability of the aspiration and increase the likelihood of the harpoon of the aspirating syringe becoming disengaged from the rubber stopper. Therefore it is recommended that the dental hygienist use a 25-gauge needle for those injections that pose a high risk for aspiration or when a significant depth of soft tissue must be penetrated (e.g., inferior alveolar, PSA, or mental or incisive nerve blocks). The 27-gauge needle may be used for all other injections, provided the possibility of aspiration and the depth of tissue penetration are minimal. The 30-gauge needle is not recommended. In the United States, needles are color-coded by gauge (Figure 39-14).
Length
The most common needle lengths used in oral healthcare are the short (approximately 1 inch or 25 mm) and the long (approximately 1⅝ inches or 40 mm), as measured from the hub to the needle tip. Choice of needle length depends on accessibility of the area to be anesthetized. Long needles are preferred for those injections that require penetration of a significant thickness of soft tissue (e.g., inferior alveolar nerve block). Short needles are indicated for injections in which smaller amounts of tissue are to be entered (see Figure 39-12).
Care and Handling of the Needle
Recommendations for the care and handling of disposable needles used for local anesthetic administration follow1:
 The needle should be changed after the administration of approximately three or four injections on the same client. Some clinicians recommend changing the needle even more often. The stainless steel becomes dull after several injections, causing each succeeding tissue penetration to be potentially traumatic and causing postinjection soreness.
The needle should be changed after the administration of approximately three or four injections on the same client. Some clinicians recommend changing the needle even more often. The stainless steel becomes dull after several injections, causing each succeeding tissue penetration to be potentially traumatic and causing postinjection soreness. The needle should be covered with a protective sheath when it is not being used—both before the injection and immediately on completion of the injection.
The needle should be covered with a protective sheath when it is not being used—both before the injection and immediately on completion of the injection. The position of the uncovered needle tip should be watched at all times to prevent needle injury to both the client and the operator.
The position of the uncovered needle tip should be watched at all times to prevent needle injury to both the client and the operator. Needles should be disposed of in an approved sharps container. These rigid, puncture-proof, leak-resistant containers should be disposed of in accordance with federal, state, and local regulations (see Chapter 7).
Needles should be disposed of in an approved sharps container. These rigid, puncture-proof, leak-resistant containers should be disposed of in accordance with federal, state, and local regulations (see Chapter 7).Problems with the Needle
The following are problems the dental hygienist may encounter with the needle when administering local anesthetic agents:
 Pain on insertion. Clients may experience discomfort of the tissues during insertion if the needle is dull; therefore the clinician should change the needle after three or four insertions if necessary
Pain on insertion. Clients may experience discomfort of the tissues during insertion if the needle is dull; therefore the clinician should change the needle after three or four insertions if necessary Pain on withdrawal. Client discomfort may occur when the needle is being withdrawn from the tissues if any barbs are on the needle tip. Barbs may be a result of the manufacturing process; however, they are more likely to occur if the needle tip contacts bone or any hard surface with too much force. To check for needle sharpness during preparation of the armamentarium, the practitioner may draw the needle tip backward across a sterile piece of gauze. A needle barb snags the gauze, indicating the need for replacement with a new needle. In addition, a needle should never be pushed forcefully against bone.
Pain on withdrawal. Client discomfort may occur when the needle is being withdrawn from the tissues if any barbs are on the needle tip. Barbs may be a result of the manufacturing process; however, they are more likely to occur if the needle tip contacts bone or any hard surface with too much force. To check for needle sharpness during preparation of the armamentarium, the practitioner may draw the needle tip backward across a sterile piece of gauze. A needle barb snags the gauze, indicating the need for replacement with a new needle. In addition, a needle should never be pushed forcefully against bone. Needle stick exposure of the administrator. For prevention of an accidental needle stick injury, the needle should remain capped with a protective shield before being used and immediately on termination of the injection. Should a needle stick exposure occur, follow the percutaneous exposure protocol and postexposure evaluation procedure outlined in Chapter 7.
Needle stick exposure of the administrator. For prevention of an accidental needle stick injury, the needle should remain capped with a protective shield before being used and immediately on termination of the injection. Should a needle stick exposure occur, follow the percutaneous exposure protocol and postexposure evaluation procedure outlined in Chapter 7.Cartridge
The cartridge is the component of the armamentarium that contains the local anesthetic drug in addition to other ingredients. The local anesthetic cartridge is often referred to as a carpule by oral health professionals; however, this term is a registered trademark name for the anesthetic cartridge manufactured by Cook-Waite Laboratories.1
Parts of the Cartridge
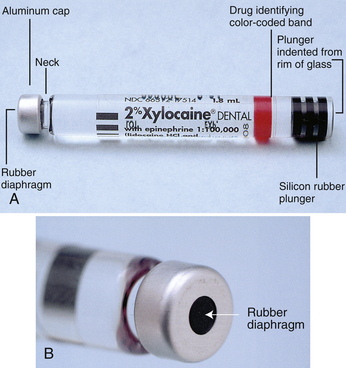
The cartridges used for local anesthetic administration have four components (Figure 39-15):
 The rubber stopper or plunger is located on one end of the cartridge and is the part in which the harpoon of an aspirating syringe is embedded. This component is pushed into the glass cylinder by pressure on the thumb ring of the syringe, thereby ejecting the local anesthetic solution through the needle. During manufacturing the rubber stopper is often treated with silicone to allow it to transverse the glass cylinder without sticking. In an unused local anesthetic cartridge the end of the rubber stopper is slightly indented from the rim of the glass cylinder (Figure 39-16). Cartridges that do not exhibit this characteristic should not be used because it is an indication that the solution has been contaminated. This topic is discussed more fully under the later section on problems.
The rubber stopper or plunger is located on one end of the cartridge and is the part in which the harpoon of an aspirating syringe is embedded. This component is pushed into the glass cylinder by pressure on the thumb ring of the syringe, thereby ejecting the local anesthetic solution through the needle. During manufacturing the rubber stopper is often treated with silicone to allow it to transverse the glass cylinder without sticking. In an unused local anesthetic cartridge the end of the rubber stopper is slightly indented from the rim of the glass cylinder (Figure 39-16). Cartridges that do not exhibit this characteristic should not be used because it is an indication that the solution has been contaminated. This topic is discussed more fully under the later section on problems. On the opposite end of the cartridge is a diaphragm into which the needle penetrates. The diaphragm is made of a semipermeable material, usually rubber, that allows solutions to diffuse into the cartridge if it is stored improperly (see Figure 39-15, B).
On the opposite end of the cartridge is a diaphragm into which the needle penetrates. The diaphragm is made of a semipermeable material, usually rubber, that allows solutions to diffuse into the cartridge if it is stored improperly (see Figure 39-15, B). The glass cylinder makes up the body of the cartridge on which the contents of the cartridge, the amount of solution, and the manufacturer's name are imprinted. Also, several manufacturers now place a color-coding band around the glass cylinder to aid in identification of the drug.
The glass cylinder makes up the body of the cartridge on which the contents of the cartridge, the amount of solution, and the manufacturer's name are imprinted. Also, several manufacturers now place a color-coding band around the glass cylinder to aid in identification of the drug.Ingredients
Several ingredients collectively form the anesthetic solution. The local anesthetic drug or combination of drugs is, of course, the primary reason for the dental cartridge. The local anesthetic molecule is stable and can withstand being boiled or processed in an autoclave without breaking down. Unfortunately, other ingredients and components of the dental cartridge are more fragile.
A vasoconstricting drug in various concentrations is included in some anesthetic cartridges. This component increases the safety and duration of action of the local anesthetic agent. Those cartridges that include a vasoconstrictor also contain a preservative for the vasoconstrictor. The agent most often employed is sodium bisulfite, which prevents biodegradation of the vasoconstrictor by oxygen.
Sodium chloride is added to the dental cartridge to make the solution isotonic with the body tissues. Finally, distilled water is incorporated into the anesthetic solution to produce a sufficient volume of solution in the cartridge. Cartridges available in the United States contain a total of 1.8 mL of solution.
Care and Handling of the Cartridge
Local anesthetic cartridges are packaged either in a vacuum-sealed metal canister containing 50 cartridges or in boxes that include 10 sealed units of 10 cartridges each, referred to as a blister pack. Regardless of how the cartridges are packaged, it is recommended that the cartridges be stored in their original container at room temperature in a dark place. Exposure to prolonged heat or direct sunlight results in an accelerated deterioration of the solution, particularly the vasoconstrictor. In addition, if kept in these original containers, the cartridges remain clean and uncontaminated.
It is not necessary to prepare a cartridge before use. The local anesthetic solution is sterilized during the manufacturing process, and bacterial cultures taken from exterior cartridge surfaces immediately after opening a container usually fail to produce bacterial growth.1 If the oral healthcare provider is concerned about the exterior of the cartridge, however, all components may be wiped with a disinfectant approved by the ADA and Environmental Protection Agency (EPA). Plastic cartridge dispensers are also available to aid in disinfecting cartridges. They can hold 1 day's supply of cartridges with the diaphragm or aluminum cap placed downward. Gauze moistened with a disinfectant is placed in the center. When assembling the armamentarium for local anesthetic administration, the oral healthcare provider may wipe the diaphragm end of the cartridge against the moistened gauze.
Cartridges should never be immersed in liquid disinfectant or sterilant. These solutions may diffuse through the semipermeable material of the diaphragm and contaminate the contents of the cartridge or may corrode the aluminum cap. In addition, local anesthetic cartridges should not be processed in the autoclave. Neither the labile vasoconstrictor nor the seals of the cartridge can withstand the extreme temperatures.
Cartridge warmers that bring the local anesthetic solution to body temperature to promote client comfort during administration are commercially available; however, they are neither necessary nor recommended. Local anesthetics stored and injected at room temperature are not uncomfortable to clients. Indeed, an overheated cartridge may cause a burning sensation during the injection and may destroy the heat-sensitive vasoconstrictor, thus producing a shorter duration of anesthesia.
Each box or canister is marked with an expiration date by the manufacturer. This expiration date also appears on the individual cartridges. Cartridges should not be used beyond the expiration date because injection with an outdated local anesthetic solution may result in client discomfort and unreliable anesthesia.
A product identification package insert is placed in all local anesthetic containers. It includes important information about the local anesthetic agent, including dosages, contraindications, warnings, care and handling, and more. It is imperative that the dental hygienist be familiar with this material to ensure client safety and comfort.
Problems
Problems are seldom encountered with cartridges, but the following may be noted1:
 Bubble in the cartridge. Small bubbles (1 to 2 mm in diameter) may at times be seen in a cartridge. These bubbles consist of nitrogen gas that was bubbled into the anesthetic solution during the manufacturing process to preclude oxygen, which destroys the vasoconstrictor, from being trapped in the cartridge. The bubbles are harmless and may be ignored. A larger bubble (larger than 2 mm) in the cartridge, however, is an indication that the solution has been frozen. In this case the stopper may also extend beyond the end of the cartridge (extruded). Because sterility of the solution is no longer guaranteed, the cartridge should not be used.
Bubble in the cartridge. Small bubbles (1 to 2 mm in diameter) may at times be seen in a cartridge. These bubbles consist of nitrogen gas that was bubbled into the anesthetic solution during the manufacturing process to preclude oxygen, which destroys the vasoconstrictor, from being trapped in the cartridge. The bubbles are harmless and may be ignored. A larger bubble (larger than 2 mm) in the cartridge, however, is an indication that the solution has been frozen. In this case the stopper may also extend beyond the end of the cartridge (extruded). Because sterility of the solution is no longer guaranteed, the cartridge should not be used. Extruded stopper. As noted previously, an extruded rubber stopper accompanied by a large bubble in the cartridge is an indication the solution has been frozen. Having a stopper that extends beyond the rim of the glass cylinder with no bubble present is often a sign that the cartridge was stored in a disinfectant and the solution has diffused through the diaphragm into the cartridge. When this occurs, the contents are contaminated and the cartridge should be discarded.
Extruded stopper. As noted previously, an extruded rubber stopper accompanied by a large bubble in the cartridge is an indication the solution has been frozen. Having a stopper that extends beyond the rim of the glass cylinder with no bubble present is often a sign that the cartridge was stored in a disinfectant and the solution has diffused through the diaphragm into the cartridge. When this occurs, the contents are contaminated and the cartridge should be discarded. Sticky stopper. A sticky stopper does not advance smoothly through the glass cylinder when pressure is applied to the thumb ring of the syringe. Because rubber stoppers are more frequently being treated with silicone during manufacturing, this has become less of a problem. If, however, paraffin is being employed by the manufacturer, difficulty may be encountered. To minimize the problem, cartridges should be stored at room temperature. If the problem persists, the healthcare provider should consider using only cartridges that have a silicone-treated stopper to facilitate a smooth, even deposition of solution.
Sticky stopper. A sticky stopper does not advance smoothly through the glass cylinder when pressure is applied to the thumb ring of the syringe. Because rubber stoppers are more frequently being treated with silicone during manufacturing, this has become less of a problem. If, however, paraffin is being employed by the manufacturer, difficulty may be encountered. To minimize the problem, cartridges should be stored at room temperature. If the problem persists, the healthcare provider should consider using only cartridges that have a silicone-treated stopper to facilitate a smooth, even deposition of solution. Corroded cap. Corrosion of the aluminum cap may be observed if the cap has been immersed in quaternary compounds such as benzalkonium chloride. If disinfecting the cartridge is necessary, an ADA- and EPA-approved disinfectant is recommended. Cartridges exhibiting corrosion should not be used.
Corroded cap. Corrosion of the aluminum cap may be observed if the cap has been immersed in quaternary compounds such as benzalkonium chloride. If disinfecting the cartridge is necessary, an ADA- and EPA-approved disinfectant is recommended. Cartridges exhibiting corrosion should not be used. Rust on the aluminum cap. The presence of rust signifies that a cartridge has broken or leaked in the metal container. The metal container rusts, and deposits appear on the cap of the cartridge. A cartridge that has a rust deposit should not be used, and each cartridge in the container should be carefully inspected.
Rust on the aluminum cap. The presence of rust signifies that a cartridge has broken or leaked in the metal container. The metal container rusts, and deposits appear on the cap of the cartridge. A cartridge that has a rust deposit should not be used, and each cartridge in the container should be carefully inspected. Broken cartridge. Cartridge breakage may occur if the cartridge has been fractured during handling. Damaged containers should be returned to the supplier. Before being used, each cartridge should be checked for signs of cracked or chipped glass. The area surrounding the stopper and the cylinder-cap interface need to be carefully examined. If a fractured cartridge is subjected to the pressure of an injection, it may shatter. Fortunately, the introduction of the color-coding band around the glass cylinder has minimized such occurrences by reinforcing the glass.
Broken cartridge. Cartridge breakage may occur if the cartridge has been fractured during handling. Damaged containers should be returned to the supplier. Before being used, each cartridge should be checked for signs of cracked or chipped glass. The area surrounding the stopper and the cylinder-cap interface need to be carefully examined. If a fractured cartridge is subjected to the pressure of an injection, it may shatter. Fortunately, the introduction of the color-coding band around the glass cylinder has minimized such occurrences by reinforcing the glass.
 Leakage during injection. An off-center perforation of the needle into the diaphragm of the cartridge produces an oval-shaped puncture. When positive pressure is applied to the plunger, anesthetic solution may leak through the perforation. It is important to carefully insert the needle into the cartridge diaphragm so a centric perforation occurs and leakage during the injection is prevented.
Leakage during injection. An off-center perforation of the needle into the diaphragm of the cartridge produces an oval-shaped puncture. When positive pressure is applied to the plunger, anesthetic solution may leak through the perforation. It is important to carefully insert the needle into the cartridge diaphragm so a centric perforation occurs and leakage during the injection is prevented.Supplementary Armamentarium
In addition to the syringe, needle, and cartridge, other items are needed to effectively administer local anesthetics. These include topical antiseptic, topical anesthetic, applicator sticks, gauze, and a hemostat or cotton pliers.
Topical Antiseptics
Topical antiseptics may be applied to the surface of the mucosa at the injection site to reduce the risk of introducing surface microorganisms into the tissue, which could result in inflammation and infection. Betadine (povidone-iodine) and Merthiolate (thimerosal) are agents commonly used for this purpose.1 A small quantity of the agent is placed at the site of the injection for 15 to 30 seconds before placement of the topical anesthetic and the initial needle penetration. The use of sterile gauze for wiping the surface has been suggested as an adequate alternative, with topical antiseptic application as an option for further microbe reduction. Because postinjection infections may occur, however, the use of a topical antiseptic should be considered, especially when local anesthetic agents are administered to individuals who may be immunosuppressed.1
Topical Anesthetic Agents
Topical anesthetic agents are applied to the mucous membrane before the initial needle penetration to anesthetize the terminal nerve endings, and thus promote client comfort during the injection procedures (Figure 39-17). For maximal effectiveness, the topical anesthetic agent should be placed at the penetration site, on dried tissue, for 1 to 2 minutes.

Figure 39-17 A, Example of a topical anesthetic containing benzocaine. B, Example of a topical anesthetic containing lidocaine (Thames Pharmaceuticals).
(A, Courtesy Beautlich LP, Pharmaceuticals, Waukegan, Illinois.)
The concentration of agents used for topical application is high to facilitate diffusion of the drug through the mucous membranes (usually 2 to 3 mm). Therefore only small amounts applied to a limited area should be used to avoid toxicity. Both ester and amide topical anesthetic agents are available. They are prepared in the form of gels, ointments, solutions, or sprays. Topical anesthetic sprays that when activated deliver a continuous stream until deactivated may potentially deliver a very high dose of the anesthetic agent and are therefore not recommended. Those sprays that deliver a measured dose limit the amount that can be expelled and are much preferred.
Cotton-Tipped Applicator Sticks
Cotton-tipped applicator sticks are needed for topical antiseptic and anesthetic agent application. They also may be used to apply pressure to the tissue before and during palatal injections (Figure 39-18).
Gauze
Gauze is used to wipe the tissue at the injection site before application of the topical antiseptic and anesthetic agents and again before insertion of the needle. This procedure removes the saliva and debris from the injection site. It also may serve as a suitable, although not as effective, replacement for the topical antiseptic (see preceding section on topical antiseptic). In addition, the gauze aids in retraction, visibility, and stability during the injection procedures (Figure 39-19).
Hemostat, Forceps, Cotton Pliers
A hemostat, forceps, or cotton pliers should be a component of the armamentarium in the unlikely event a needle breaks during administration and must be retrieved from the soft tissues (Figure 39-20).

Figure 39-21 Armamentarium. From top: needle, cartridge, syringe.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)

Figure 39-22 Retract the piston.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)

Figure 39-23 Insert the cartridge.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)

Figure 39-24 Engage the harpoon in the plunger with gentle finger pressure.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
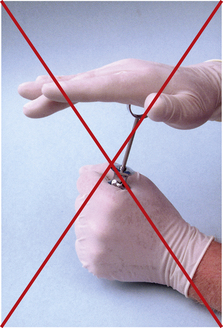
Figure 39-25 Do not exert force on the plunger.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)

Figure 39-26 Remove the clear plastic protective cap from the opposite end of the colored plastic cap that hubs the needle.
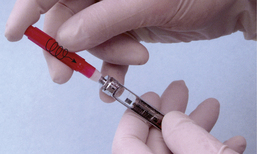
Figure 39-27 A plastic hubbed needle must be screwed onto the syringe while simultaneously being pushed into the metal needle adaptor of the syringe (arrow).
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
PREPARATION OF ARMAMENTARIUM
Loading and Unloading the Metallic or Plastic Cartridge-Type Syringe
Proper loading of the syringe is essential to prevent complications associated with the syringe, cartridge, and needle, and to ensure client safety and comfort during local anesthetic administration (Procedure 39-1).
Procedure 39-1 LOADING THE METALLIC OR PLASTIC CARTRIDGE-TYPE SYRINGE
STEPS
Unsheathing and Resheathing the Needle
A needle should be covered with a colored protective shield when it is not being used. Concerns regarding the possibility of a needle stick exposure have led to the formulation of guidelines for resheathing needles. Oral healthcare providers are most often injured with needles when the needle is being resheathed after an injection.1 At this time the needle is contaminated with blood, saliva, and debris, and the potential for disease transmission exists. A variety of techniques have been suggested, but currently a one-handed “scoop” technique for sheathing the needle is recommended and described in Procedure 39-1.
Mechanical devices such as shields and needle sheath props are available to aid in preventing accidental needle stick exposure (Figure 39-31). Dental hygienists should be familiar with the devices available and determine which technique or mechanical device is most acceptable to them. The one-handed resheathing technique or an approved mechanical device should be consistently used by the dental hygienist whether or not the needle has been contaminated.
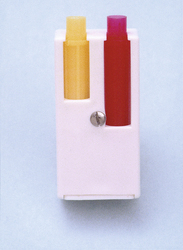
Figure 39-31 Plastic needle cap holders.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
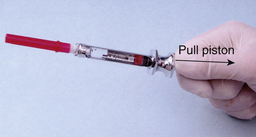
Figure 39-32 Retract the piston.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)

Figure 39-33 Remove the used cartridge.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
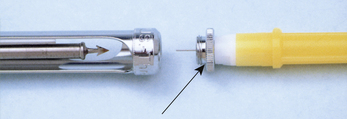
Figure 39-34 When discarding needle, check to be sure that the metal needle adaptor from the syringe is not inadvertently discarded too (arrow).
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
Dismantling the Armamentarium
At the completion of the dental hygiene care appointment, the local anesthesia armamentarium needs to be dismantled. Procedure 39-2 describes the sequence for properly unloading the syringe.
Procedure 39-2 UNLOADING THE BREECH-LOADING METALLIC OR PLASTIC CARTRIDGE-TYPE SYRINGE
STEPS
TRIGEMINAL NERVE
The trigeminal nerve is the fifth and largest of the 12 cranial nerves (Figure 39-37). The three divisions of the trigeminal nerve include the ophthalmic (V1), the maxillary (V2), and the mandibular (V3) divisions. The ophthalmic and maxillary divisions are completely sensory; the mandibular division is sensory and also carries the motor root to the muscles of the mandible.
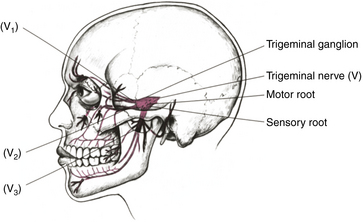
Figure 39-37 Trigeminal nerve distribution.
(From Fehrenbach MJ, Herring SW: Illustrated anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
Ophthalmic Division (V1)
The ophthalmic nerve, the first and smallest division of the trigeminal nerve, branches off the trigeminal (semilunar or gasserian) ganglion and forms three branches: the nasociliary nerve, the frontal nerve, and the lacrimal nerve. This division of the trigeminal nerve innervates tissues superior to the oral structures, including the eye, nose, and frontal cutaneous tissues. It has only sensory function. Of the three divisions of the trigeminal nerve, the ophthalmic is the least important to intraoral local anesthetic administration.
Maxillary Division (V2)
The maxillary division of the trigeminal nerve, which is entirely sensory in function, arises from the trigeminal (semilunar or gasserian) ganglion, exits the cranium via the foramen rotundum, and then passes into the pterygopalatine fossa, where it gives off several branches (Figure 39-38). Only those branches pertinent to intraoral local anesthesia are discussed.
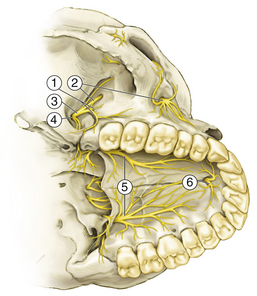
Figure 39-38 Distribution of the maxillary division (V2). 1, Posterior superior alveolar branches; 2, infraorbital nerve; 3, maxillary nerve; 4, foramen rotundum; 5, greater palatine nerve; 6, nasopalatine nerve.
(Data from Haglund J, Evers H: Local anaesthesia in dentistry, ed 2, Södertälje, Sweden, 1975, Astra Läkemedel.)
Pterygopalatine Nerves
Two branches pass through the pterygopalatine ganglion and form the greater (anterior) palatine nerve and the nasopalatine nerve (see Figure 39-38). The greater palatine nerve enters the oral cavity on the hard palate via the greater palatine foramen and innervates the palatal soft tissues and bone of the posterior teeth. The nasopalatine nerve leaves the pterygopalatine ganglion and passes forward and downward, entering the oral cavity through the incisive foramen. This nerve provides sensory innervation to the lingual bone and soft tissues in the premaxilla (canine to canine).
Posterior Superior Alveolar Nerve
The PSA nerve (Figure 39-39) descends from the main trunk of the maxillary nerve just before it enters the infraorbital canal. Most often there are two PSA branches that pass downward on the posterior surface of the maxilla. An internal branch enters the PSA foramen located on the superior portion of the maxillary tuberosity. This branch provides sensory innervation to the pulpal and osseous tissues and the PDLs of the maxillary third, second, and first molars (usually with the exception of the mesiobuccal root of the first molar). An external branch of the PSA nerve remains on the outer surface of the maxilla and continues downward to innervate the facial gingiva of the maxillary molars and the adjacent vestibular mucosa.
Branches of the Infraorbital Nerve
The maxillary nerve continues anteriorly after having given off the PSA nerve and enters the infraorbital canal. At this point the maxillary nerve is referred to as the infraorbital nerve (see Figure 39-39). Two branches may descend from the infraorbital nerve: the middle superior alveolar (MSA) and the anterior superior alveolar (ASA) nerves.
The MSA nerve branches off the infraorbital nerve within the infraorbital canal. This nerve provides sensory innervation to the maxillary premolars, the mesiofacial root of the first molar, the periodontal tissues, and the facial soft tissue and bone in the premolar area. The MSA nerve is not present in approximately 60% of individuals.9 In its absence, these areas are innervated by the PSA nerve or, more commonly, the ASA nerve.
The ASA nerve descends from the infraorbital nerve just before the latter's exit from the infraorbital foramen. The ASA nerve provides innervation to the central and lateral incisors, the canine, the periodontal tissues, and facial soft tissue and bone over these teeth. In those individuals without an MSA nerve, the ASA nerve most often provides innervation to the premolars and possibly the mesiofacial root of the first molar.
Mandibular Division (V3)
The mandibular nerve, the third and largest division of the trigeminal nerve, both has a sensory root and carries the motor root for the trigeminal nerve (Figure 39-40). The sensory root arises from the trigeminal ganglion, after which it is joined by the motor root. Both roots emerge from the cranium via the foramen ovale, and at this point, they unite to form the main trunk of the mandibular nerve.
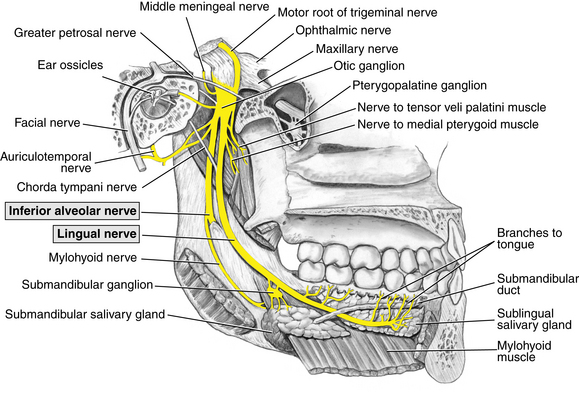
Figure 39-40 Medial view of the mandible showing the motor and sensory branches of the mandibular nerve.
(From Fehrenbach MJ, Herring SW: Illustrated anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
The trunk then divides into an anterior branch and a posterior branch. The nerves arising from these branches that relate to intraoral local anesthesia are described in the following paragraphs.
Branches of the Anterior Division
The anterior division is smaller than its posterior counterpart and contains primarily motor fibers. The motor component innervates the muscles of mastication: the masseter, the temporalis, and the lateral and medial pterygoid. The sensory component of the anterior division is the buccal nerve. At the level of the occlusal plane of the mandibular molars, it crosses the anterior border of the ramus and branches to innervate the buccal gingiva of the mandibular molars.
Branches of the Posterior Division
The posterior division of the mandibular nerve is primarily sensory, but it also has a small motor component. The branches of the posterior division related to mandibular anesthesia are the lingual and inferior alveolar nerves (Figure 39-41).
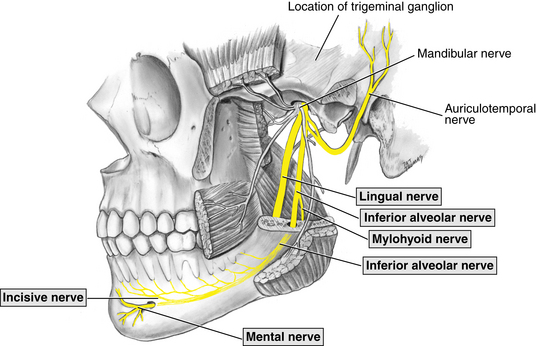
Figure 39-41 The pathway of the posterior trunk of the mandibular division of the trigeminal nerve.
(From Fehrenbach MJ, Herring SW: Illustrated anatomy of the head and neck, ed 3, St Louis, 2007, Saunders.)
The lingual nerve emerges between the lower head of the lateral pterygoid and medial pterygoid muscles and lies between the ramus and the medial pterygoid muscle in the pterygomandibular space. It turns anteriorly, where it enters the oral cavity and innervates the anterior two thirds of the tongue, the mucous membranes of the floor of the mouth, and the lingual gingiva of the mandible.
The inferior alveolar nerve runs posterior and parallel to the lingual nerve within the pterygomandibular space, where it enters the mandibular foramen. Within the mandible the inferior alveolar nerve travels in the mandibular canal and innervates the pulpal and osseous tissues of the mandibular teeth in the quadrant and facial soft tissues anterior to the first molar. Throughout its course the inferior alveolar nerve is accompanied by the inferior alveolar artery and vein.
As the inferior alveolar nerve reaches the mental foramen, it divides into two terminal branches. The incisive nerve is a direct extension of the inferior alveolar nerve, continuing anteriorly within the mandibular canal. It innervates the pulpal and osseous tissues of the mandibular first premolar, canine, and lateral and central incisors and the facial periodontal tissues of the teeth.
The mental nerve branches from the inferior alveolar nerve, exits the mandible via the mental foramen, and provides sensory innervation to the mucous membranes and skin of the lower lip and chin.
The mylohyoid nerve branches from the inferior alveolar nerve before the latter enters into the mandibular foramen. It advances downward and forward in the mylohyoid groove on the medial side of the ramus and provides motor innervation to the mylohyoid and anterior digastric muscles. In some individuals the mylohyoid nerve may supply accessory sensory innervation to the mandible in the premolar and molar areas.
LOCAL ANESTHESIA TECHNIQUES
When choosing the appropriate injection to be administered, the dental hygienist needs to consider the area to be treated, the procedure to be performed, the extent of anesthesia necessary, and the client's needs and comfort. In oral healthcare there are three major types of injections used to obtain local anesthesia:
These are differentiated by the site of anesthetic solution deposition relative to the area to receive treatment.
Local Infiltration
A local infiltration injection involves placement of the anesthetic solution close to the smaller terminal endings of the nerve fibers in the immediate area to be treated (Figure 39-42). An example would be the injection of anesthetic solution into an interproximal papilla before therapeutic scaling and root planing.
Field Block
The field block method of obtaining anesthesia involves the deposition of solution near large terminal nerve branches (Figure 39-43). The resulting anesthesia is more circumscribed, most often involving one tooth and the tissues surrounding the tooth. Treatment is away from the site of the injection. The deposition of anesthetic solution above the apex of a maxillary tooth, such as the maxillary right central incisor, is an example of a field block. In oral healthcare a field block is often incorrectly referred to as a local infiltration.
Nerve Block
The nerve block involves the deposition of anesthetic solution close to a main nerve trunk, often at some distance from the treatment area (Figure 39-44). This type of injection most often anesthetizes a larger area than that of a field block. Examples include a PSA nerve block and an inferior alveolar nerve block.
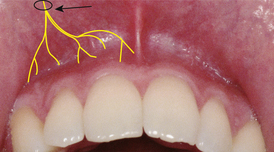
Figure 39-44 Nerve block. Local anesthetic is deposited close to the main nerve trunk, located at a distance from the site of injection.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
When dental hygiene care is to be performed in a small, isolated area, infiltration anesthesia may be the best choice, whereas a field block is the injection of choice when one or two teeth are to be treated. When the dental hygiene care plan involves a sextant or quadrant, nerve block anesthesia is recommended.
The term anesthesia is often preceded by either local or regional. Either phrase is correct; each indicates that a specific area is anesthetized and that the client is conscious, unlike in general anesthesia, in which the client is unconscious. Therefore the use of either term is appropriate, and they can be used interchangeably, although local anesthesia appears to be more commonly used.
PROCEDURES FOR A SUCCESSFUL INJECTION
The goal for each administration of local anesthetic is, of course, to give a safe, comfortable injection for control and elimination of painful sensations during and after dental hygiene care. It is ironic, however, that a procedure meant to control pain for clients is often reported to be the most dreaded. Although the prospect of receiving an intraoral injection provokes fear and apprehension in many individuals, local anesthetic agent administration need not be painful. There are technical and communication components to an atraumatic injection.
Technical Aspects
Technical strategies include using a topical anesthetic before needle insertion, depositing a few drops of anesthetic solution, waiting 5 seconds before cautiously advancing the needle, and slowly depositing the anesthetic solution; these techniques help minimize or eliminate discomfort. Also, it is essential to maintain complete control over the syringe at all times so that tissue penetration may be accomplished readily, accurately, and without inadvertent nicking of tissues. Figure 39-45 presents hand positions for injections.
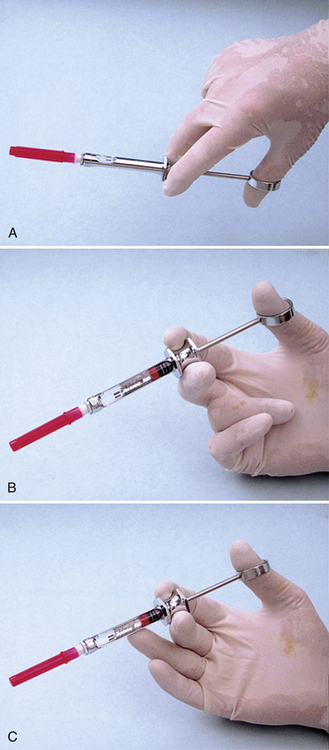
Figure 39-45 Hand positions for injections. A, Palm down: poor control over the syringe; not recommended. B, Palm up: better control over the syringe because it is supported by the wrist; recommended. C, Palm up and finger support: greatest stabilization; highly recommended.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
Figures 39-46 and 39-47 illustrate some hand rests and finger rests that can be used to stabilize syringes.
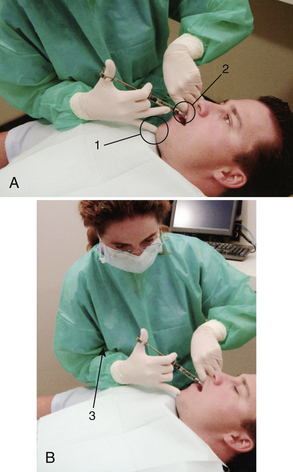
Figure 39-46 A, Use of the chin (1) as a finger rest, with the syringe barrel stabilized by the client's lip (2) during a right inferior alveolar nerve block. B, When necessary, stabilization may be increased by drawing the clinician's arm in against his or her chest (3).
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)

Figure 39-47 Syringe stabilization of a right posterior superior alveolar nerve block: syringe barrel on the client's lip, one finger resting on the chin and one on the syringe barrel (arrows). Upper arm kept close to the clinician's chest to maximize stability.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)
Figure 39-48 presents incorrect techniques to be avoided.
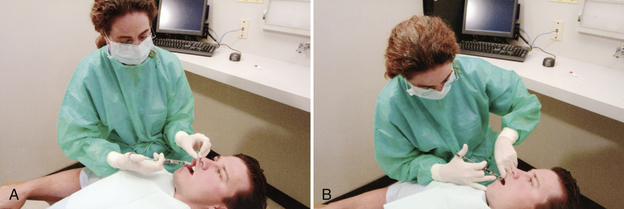
Figure 39-48 A, Incorrect position: no hand or finger rest for stabilization of syringe. B, Incorrect: clinician resting elbow on client's arm.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)

Figure 39-49 Physiologic position of patient for receipt of local anesthetic injection.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)

Figure 39-50 Sterilized gauze is used to gently wipe tissue at site of needle.
(From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.)