Chapter 8 Manipulation
Flexion or other manipulative tests often are used to induce or exacerbate lameness during lameness or prepurchase examinations.
Induced and Baseline Lameness
It is important to understand the concept of induced lameness and the possible difference between lameness seen at this stage and baseline lameness. During lameness examination, baseline lameness is established before any form of manipulation is performed. This may be difficult if more than one limb is involved, if lameness is subtle or sub-clinical, or if lameness is bilaterally symmetrical, which causes a gait abnormality without overt lameness. Lameness provocation is performed to exacerbate the baseline lameness or to provoke a hidden gait abnormality and attempt to localize the source of pain within a limb or limbs.
Provocative tests create induced lameness that may not have any clinical relevance to the baseline lameness observed during initial movement. These tests are not sensitive or specific and often result in false-positive and false-negative findings. Many horses with palmar foot pain respond positively to the “fetlock flexion test” (or lower limb flexion test, see following text) and could erroneously be thought to have lameness of the metacarpophalangeal joint. Similarly, a horse with proximal suspensory desmitis (PSD) may show exacerbation of lameness after distal limb flexion. A racehorse with baseline lameness as the result of a carpal chip fracture may have preexisting low-grade osteoarthritis of the metacarpophalangeal joint and respond positively to lower limb flexion but response to carpal flexion may be equivocal. Diagnostic analgesia is essential to localize the source or sources of pain. In the hindlimb, hock flexion, the so-called “spavin test,” causes many false-positive reactions.
Flexion Tests
Flexion tests were first described early in the twentieth century, but information regarding the degree of flexion, force, or duration of the tests was lacking.1 Variations in technique persist and produce variable responses that can be misleading. There appear to be more false-positive reactions to flexion than there are false negatives, but the latter do occur. Flexion tests are useful during prepurchase examinations because the horses being examined usually are relatively sound, and the tests are useful at uncovering hidden sources of pain. Flexion tests may be useful in exacerbating lameness, particularly when the primary or baseline lameness is in the region being flexed, but sensitivity is doubtful. Horses judged to be clinically sound underwent a “normal” and then a “firm” lower limb flexion test (fetlock flexion).2 Of the 50 horses tested, 20 had a positive response to normal flexion, and 10 of these horses were judged to be lame while trotting for about 15 m (50 feet) or more. Forty-nine of 50 horses had a positive response to firm flexion, and 35 of these remained lame for a minimum of 15 m. In this study the force applied was not calibrated, 7 of the 50 horses developed lameness within 60 days of completion of the study, and 24 horses had radiological abnormalities that could have contributed to a positive response to flexion.2 Although there may be an explanation for a positive response in some horses, the high percentage of positive results in the study is in agreement with my clinical impression. In a study using the Flextest (Krypton Electronic Engineering NV, Leuven, Belgium), an apparatus designed to control traction force and time during a lower limb flexion test, the optimal force and time for flexion were 100 N and 1 minute, respectively. There was a positive response to flexion in many horses that were considered sound, and a positive response in sound horses was more likely in those in active work than in horses that had been rested or turned out on pasture. Horses were more likely to manifest a positive response to flexion as the force used in the test was increased.3 A false-positive response to flexion can be observed in clinically normal horses and in those with unimportant low-grade problems. Lameness induced by flexion in these horses may have little clinical relevance.
However, other evidence suggests that a positive response to lower limb flexion in sound horses may be useful to predict future lameness. In a retrospective study, 151 initially sound horses were followed for 6 months. Twenty-one percent of horses with a positive forelimb flexion test result developed lameness in the area being flexed, whereas only 5% of horses with a negative flexion test result subsequently developed lameness. In young Swedish Warmbloods there was a positive correlation between a positive response to flexion and a subsequent insurance claim related to lameness.4
In a more recent study the predictive value of the lower limb flexion test was debated.5 Sixty percent of sound horses responded positively to the flexion test. There was no influence of body weight, height, or range of motion, but outcome of the flexion test increased significantly with age and in mares. Over a 6-month period the number of horses responding positively decreased significantly, a finding that casts doubt on the possible predictive value of the test.5
Flexion tests lack specificity because it is nearly impossible to flex a single joint without flexing other joints or nearby tissues, particularly in any hindlimb or distal forelimb flexion tests. Elevation of a limb without flexion in severely lame horses may exacerbate the baseline lameness, because horses guard the limb or need to warm out of the lameness for a number of steps while trotting, thus complicating interpretation. Hindlimb flexion tests are less specific than forelimb tests because the reciprocal apparatus prevents flexion of any joint without concomitant flexion of other joints. Hindlimb flexion tests are useful in exacerbating baseline lameness, but positive responses to individual lower limb and upper limb tests, in my opinion, only localize pain causing lameness to the entire hindlimb. I believe that flexion tests are useful in exacerbating lameness, and in some horses it is the baseline or relevant lameness that is being worsened. In general, unless the horse’s response is clearly pronounced and different from that of other manipulation, lameness cannot be localized based on response to flexion alone. Diagnostic analgesia should always be used, when possible, to localize pain.
Order, Duration, Force, and Venue during Flexion Tests
Consistency in technique is essential. Although force exerted by individuals varies, the flexion technique of experienced practitioners is sufficient to objectively assess response to flexion.6 Response to flexion can and should be compared with response in the contralateral limb. Ideally the flexion test should be performed in the contralateral sound limb first before being performed in the suspect limb, to determine the horse’s response. Accurate assessment of response to flexion in the contralateral nonlame limb may not be possible if the horse is severely lame after flexion of the lame limb and lameness persists. In some instances, baseline lameness is actually increased by forcing the horse to stand for the contralateral flexion test, a useful observation seen most commonly in horses with forelimb lameness (see following text). Horses with nearly bilaterally symmetrical lameness may have a similar positive test result in the less-lame contralateral limb.
Duration of flexion is somewhat controversial and may be an individual choice. In a study evaluating lower limb flexion, duration of 1 minute was considered ideal, because normal horses that underwent flexion at 100 N for 1 minute had few false-positive responses.3 Maintaining firm flexion for 1 minute while performing all flexion tests and repeating the tests in the contralateral limbs can make this portion of the lameness examination time-consuming. On the other hand, if the clinician takes the time to perform these tests, optimum chances of success are improved. A false-positive result is more useful than a false-negative test result. Some clinicians prefer to perform flexion tests with more force but for a shorter duration. This technique works well for lower limb flexion tests. Seldom is it possible to maintain some upper limb manipulative procedures for 1 minute. Thus some latitude is necessary. I believe that duration of flexion of 45 seconds to 1 minute is enough to elicit an accurate response in most horses.
Force used during flexion varies considerably, but excessive force induces lameness in most normal horses. Forces in the range of 100 to 150 N represent a moderate degree of force for lower limb flexion tests. In studies using a dynamometer, the maximum amount of force that could be used without a consistent withdrawal response in normal horses was 150 N.7 The amount of force also depends on the size of the horse or the joint being flexed. The amount of force used in adult horses cannot be used in foals. Horses with obvious osteoarthritis or articular fracture, or those with substantial soft tissue injury likely to be affected by the flexion test, do not tolerate the same force as horses with more mild conditions. In a study of healthy and injured Thoroughbred (TB) racehorses, a positive correlation existed between decreased range of motion and joint injury.8 Loss of joint motion was most likely caused by joint capsule fibrosis, but pain associated with increased intraarticular pressure from effusion or flexion also may have limited joint motion.8 I recommend flexing a joint as much as possible with an amount of force just slightly less than the force that consistently causes a withdrawal response. Consistency should be applied between horses, paying attention to how the horse reacts; obvious resistance to sustained passive flexion may be clinically significant.
Proper evaluation of the results of flexion tests requires that the horse be observed while trotting in a straight line on a firm, nonslip surface. Evaluation during trotting is important to differentiate those horses resistant to static flexion from those with an authentic positive flexion test result. Horses usually are trotted in hand, although occasionally a horse’s response to flexion is evaluated while it is being ridden. The horse should be trotted immediately after the limb is placed to the ground, with care taken to avoid scaring the horse or providing any excessive encouragement to trot, because many horses will slip initially, gallop off, or balk, all of which necessitate test repetition. If possible, the horse should be trotted away from the examiner for a minimum of 12 to 15 m.
Causes of Pain during Flexion and Positive Flexion Test Results
Forced flexion of a joint can induce pain in many potential sites. Force is being applied to both articular structures and surrounding soft tissues. The tissues on the flexion side of the joint are being compressed, whereas tissues on the extension side are under tension. During flexion, intraarticular pressure and intraosseous pressure in subchondral bone are increased.3,8 Stretching or compression of the joint capsule, vascular constriction, and activation of pain receptors in the joints and surrounding soft tissues also can occur during flexion.3 It is rarely possible to attribute pain on static flexion or during movement after flexion to an individual articular surface. The “fetlock flexion test” is a misnomer because as it is commonly performed it includes the interphalangeal joints and stresses surrounding soft tissue. Thus the names lower limb flexion test or fetlock region flexion test are more appropriate.
Positive Responses to Flexion
Positive responses to flexion can be seen with static flexion (see Chapter 6) and when movement follows flexion. A positive flexion test result is defined as obvious lameness or an increase over baseline lameness that is observed for more than three to five strides while the horse trots in a straight line after flexion. A mild response, even in sound horses, often is seen in the first few strides, a finding that should be compared with the contralateral limb. Sound horses warm out of this mild response quickly. Of 100 sound horses 50% had a slight response, 35% had mild lameness and 15% had distinct lameness after a lower limb flexion test.5 A persistent, one- to two-grade increase over baseline lameness for several steps is a positive response. In horses with hindlimb lameness a marked positive response often is accompanied by reluctance to place the heel on the ground, and the horse may land only on the toe for several strides.
Forelimb Flexion Tests
Lower Limb Flexion Test
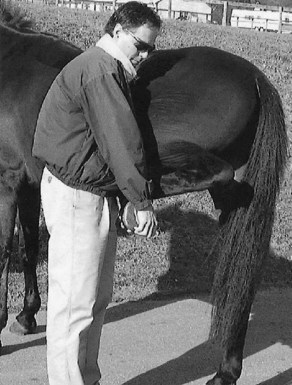
The lower limb flexion test often has been equated erroneously with the fetlock flexion test. The fetlock region can be flexed independently of interphalangeal joints (see following text). The lower limb flexion test is the most common test performed in the forelimb and involves placing a hand on the toe and forcing the fetlock and both interphalangeal joints into firm flexion (Figure 8-1). A positive response to flexion can be observed with any condition of the distal interphalangeal, proximal interphalangeal, and metacarpophalangeal joints or the navicular bone or bursa; other causes of palmar foot pain; digital flexor tenosynovitis; any soft tissue problem in the palmar pastern region; and lameness associated with the branches or proximal aspect of the suspensory ligament (SL) or proximal sesamoid bones (PSBs). Horses with lesions of the PSBs usually have markedly positive responses to this test. This test is not specific for lameness of the metacarpophalangeal joint. I have seen marked responses in horses with navicular disease or osteoarthritis of the interphalangeal joints. However, horses with osteoarthritis, fractures of the metacarpophalangeal joint, or tenosynovitis usually also show a marked positive response. In a recent study of clinically sound horses in which lameness could consistently be induced by flexion with 250 N for 1 minute, lameness was alleviated by intraarticular analgesia of the metacarpophalangeal joint, but not by intraarticular analgesia of the proximal interphalangeal or distal interphalangeal joints or intrathecal analgesia of the navicular bursa.9 Exacerbation of lameness associated with pain arising from the SL after lower limb flexion is probably caused by relaxation of the SL during flexion and then sudden loading of the ligament when the horse starts to load the limb.

Fig. 8-1 The lower limb flexion test is often erroneously called the fetlock flexion test. During the lower limb flexion test the fetlock, proximal interphalangeal, and distal interphalangeal joints are flexed; the palmar pastern and fetlock region soft tissue structures are compressed; and the dorsal structures are stretched.
The limb should be held as close to the ground as possible, and forced carpal flexion should be avoided (see Figure 8-1). All soft tissue and bony structures in the palmar aspect of the distal limb are severely compressed, resulting in low specificity for the metacarpophalangeal joint. Some people use a hand as a fulcrum or grab the toe with both hands (Figure 8-2), but this technique may result in application of excessive force, although it otherwise produces similar results.
Fetlock Flexion Test
The specificity of the lower limb flexion test can be improved by applying force to the metacarpophalangeal joint and avoiding forced flexion of the interphalangeal joints. The fetlock flexion test is performed by placing one hand along the dorsal aspect of the pastern region and one hand along the dorsal aspect of the metacarpal region, while avoiding flexion of the carpus (Figure 8-3). When compared with lower limb flexion this test is more difficult to perform because it requires more force and the clinician’s effort to maintain a similar degree of flexion. The test is not specific for articular lameness of the metacarpophalangeal joint, and horses with soft tissue problems respond positively.

Fig. 8-3 A true fetlock flexion test can be performed by carefully flexing only the fetlock joint. The clinician’s hand grasps only the pastern and not the toe of the hoof while avoiding forced flexion of the proximal and distal interphalangeal joints (see Figure 8-1).
Flexion of Interphalangeal Joints
In my opinion, flexion of either the proximal interphalangeal or distal interphalangeal joint without concomitant flexion of the other, or of the metacarpophalangeal joint, is impossible. Varus or valgus stress can be applied to the interphalangeal joints, and when followed by trotting, this stress can be a suitable provocative test in horses with osteoarthritis or soft tissue injuries of these joints.
Carpal Flexion Test
The carpal flexion test is the most specific of all forelimb flexion tests, and a positive response usually reflects baseline lameness associated with the carpal region. Few false-positive results occur. A positive response may reflect intraarticular pain, but a positive response also is seen in horses with carpal tenosynovitis, accessory carpal bone fractures, proximally located superficial digital flexor (SDF) and deep digital flexor (DDF) tendonitis, PSD, or avulsion fracture of the third metacarpal bone (McIII) at the SL origin. Rarely, a horse with a problem in the scapulohumeral and cubital joints or the antebrachium responds positively. A negative response does not preclude an articular lesion of the carpus, including incomplete fractures or sclerosis of the carpal bones.
The limb is elevated, and the carpus is forced into full flexion by pushing the metacarpal region directly underneath the radius (Figure 8-4). The distal limb can be pulled laterally to place the carpal joints in valgus stress or torsion.
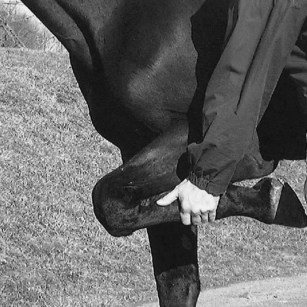
Fig. 8-4 The carpal flexion test is the most specific of all flexion tests, but it applies concomitant mild flexion of the elbow and shoulder joints. Although false-negative results are possible, a positive carpal flexion test result usually means that lameness originates from the carpal region.
Horses sometimes trot off lame on the contralateral limb after the carpal flexion test is performed. I have seen this most commonly in young Standardbred or TB racehorses with subchondral bone pain in the middle carpal joint and call it the “Ross crossed-extensor phenomenon.” I believe that this reflects bilateral lameness, and flexion of the ipsilateral carpus causes less pain than making the horse stand for 1 minute on the contralateral limb. I have observed this response most commonly in horses with bilateral carpal lameness, but exacerbation of contralateral lameness is not restricted to carpal lesions. Dyson10 has called this a “paradoxical response to flexion” and has observed exacerbation of contralateral lameness in horses with navicular syndrome, DDF tendon lesions in the digit, and distal hock joint pain.
Upper Limb Manipulation
Because of the inverse but simultaneous movement of the elbow and shoulder joints, it is difficult to accurately name the flexion tests of these joints. For instance, when the limb is pulled in a caudal direction, the shoulder joint is flexed but the elbow joint is extended. I call this manipulation upper limb flexion (Figure 8-5). This maneuver requires both hands, one hand grasping the pastern region and one grasping the cranial aspect of the antebrachium to force the entire limb in a caudal direction. When the limb is pulled in a cranial direction, resulting in upper limb extension, the shoulder joint is extended, but the elbow joint is flexed (Figure 8-6). Both hands are placed around the pastern region while forcing the entire forelimb into maximal extension. Maintenance of upper limb extension or flexion for even 45 seconds is difficult, so I try to maintain this position for as long as possible and then evaluate the horse while trotting. Many normal horses resist upper limb manipulation, and an alternative is to force the limb into hard flexion or extension in a rhythmical fashion six to eight times and then trot the horse. Even though the entire limb is being manipulated, there are few false-positive test results. A horse with a positive response to carpal flexion may have a similar response to upper limb manipulation because it is difficult to perform upper limb flexion without simultaneously flexing the carpus. False-negative test results can occur, probably because of the inability to place either the shoulder or the elbow joints in hard flexion. In my experience, horses with lameness originating from the elbow region are more likely to respond to upper limb extension, whereas those with lameness originating from the shoulder region are more likely to respond to upper limb flexion.
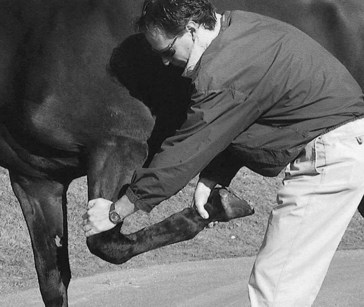
Fig. 8-5 Upper forelimb flexion is performed by grasping the antebrachium and pulling the entire limb caudally and slightly proximally. This maneuver flexes the shoulder joint and extends the elbow joint. Horses with shoulder region lameness often respond positively to this manipulative test.
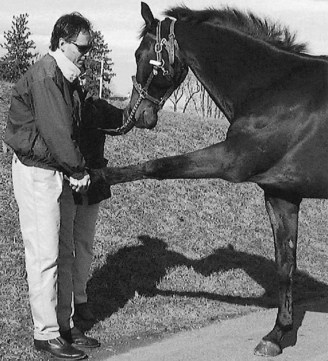
Fig. 8-6 The upper limb extension test is performed by pulling the forelimb out in front of the horse and forcing it proximally. This places the elbow joint in flexion and the shoulder joint in extension. In my experience, lameness of the elbow region is exacerbated by this technique, but occasionally shoulder joint lameness also is worsened.
Hindlimb Flexion Tests
Hindlimb flexion tests are not specific, but they may be useful to exacerbate the baseline lameness or detect hidden sources of potential lameness. I do not believe that hindlimb flexion tests are useful in differentiating the source of pain causing lameness in most horses unless the response is dramatic, and diagnostic analgesia usually is required in all horses.
Lower Limb Flexion Test
The lower limb flexion test is performed similarly to the forelimb flexion test, but with similar force the metatarsophalangeal joint can be flexed more extremely. The veterinarian should try to keep the limb as low as possible to avoid placing hard flexion on the upper limb, although all joints are flexed to a degree. The lower limb flexion test also affects the proximal interphalangeal and distal interphalangeal joints and the surrounding soft tissues (Figure 8-7). Horses with digital flexor tenosynovitis or DDF tendonitis show a marked response to the lower limb flexion test. False-positive results can occur, but these are less common in a hindlimb than in a forelimb, even in horses in active work. Horses with pain in the upper limb may show a mild or moderate response to lower limb flexion. This test is not specific for pain located in the lower limb, and lameness in horses with stifle pain often is worse after the lower limb flexion test.10 Horses with subchondral bone pain from maladaptive or nonadaptive bone remodeling of the distal aspect of the third metatarsal bone (MtIII) or those with incomplete fractures of the MtIII or incomplete midsagittal fractures of the proximal phalanx may show little response to this test (false-negative result). Coupled with lack of effusion of the metatarsophalangeal joint, a false-negative response to lower limb flexion may sidetrack the clinician into thinking pain originates elsewhere. Diagnostic analgesia is required to determine the source of pain.
Fetlock Flexion and Interphalangeal Joint Tests
The metatarsophalangeal joint region can be flexed independently of the interphalangeal joints in the hindlimb, or the interphalangeal joints can be flexed independently, but these tests are difficult to perform and of limited value.
Upper Limb Flexion Test
The so-called “spavin test” or “hock flexion test,” misnomers for the upper limb flexion test, is not specific for lameness of the hock because the stifle and coxofemoral joints also are stressed hard, and mild flexion of the lower joints is inevitable. The terms spavin test and hock flexion test are deep-rooted in our profession but it is important to recognize that a positive response is not synonymous with distal hock joint pain.
The limb is held in hard flexion for at least 1 minute, but additional time for this test may improve its clinical value (Figure 8-8). It may be necessary to have an assistant place a hand on the contralateral hip to steady the horse, because proper performance of this test requires that the limb be elevated substantially, and the horse may lose its balance. The position of the hands in the metatarsal region is important to consider, because the force required to hold the hindlimb in this position may cause compression and pain in structures along the plantar aspect, potentially contributing to a false-positive response.
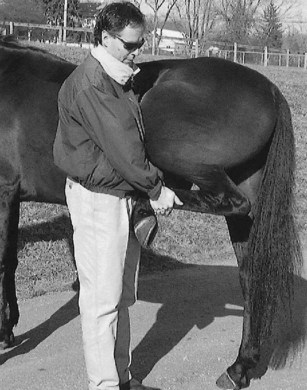
Fig. 8-8 The hindlimb upper limb flexion test is demonstrated. This test has been called the spavin test or hock flexion test, but it is not specific for lameness of the hock. The hock and stifle joints are in forced flexion, the lower limb joints are flexed, the metatarsal region is compressed, and a small amount of forced flexion of the coxofemoral joint is induced.
Hindlimb Flexion Test
Alternatively, the entire hindlimb can be flexed simultaneously. This test is useless in differentiating potential sources of pain in a limb, but it is quite useful in exacerbating baseline lameness or uncovering occult lameness conditions. The clinician’s hands are placed on the toe and the entire limb is held in extreme flexion (Figure 8-9). An assistant may be necessary to steady the opposite hip while the limb is elevated.
“Hock” Extension Test
Hock extension may be useful in placing selective stress on the hock, independent of the stifle. Forced extension causes tension on the soft tissue structures on the dorsal, medial, and lateral aspects of the hock. Seldom is it possible to perform this test for 1 minute; six to eight attempts at forced extension followed by trotting the horse can be substituted for more lengthy manipulation (Figure 8-10). False-positive and false-negative responses occur, which are caused mostly by the inelastic reciprocal apparatus. This maneuver can reveal laxity of a damaged fibularis (peroneus) tertius.
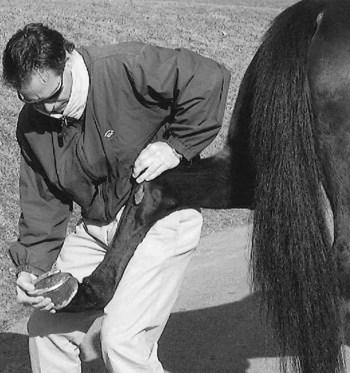
Fig. 8-10 During the hock extension test the clinician forces the hock into extension by pushing down on the calcaneus while pulling up on the distal limb by using both the right arm and left leg. Pain from hock lameness can be exacerbated, but false-positive results from pain in other locations also can occur.
“Stifle Flexion” Test
A modification of the upper limb flexion test can be used to place hard flexion on the stifle, independent of the hock (Figure 8-11). This test can be somewhat difficult to perform but may exacerbate lameness in horses with osteoarthritis or other conditions of the stifle. Other proximal limb joints are also in flexion; therefore some false-positive results occur. See page 87 for other manipulation of the stifle.
Direct or Local Palpation Followed by Movement
Static palpation, in which the horse’s response to compression during palpation while standing is assessed, reveals useful information (see Chapter 6). Additional information can be gained by evaluating movement after palpation and dynamic provocation to induce lameness. Dynamic provocation usually is performed by digital palpation or use of hoof testers. Many horses manifest a positive response during static palpation, but the primary pain is located elsewhere. However, if lameness can be induced or baseline lameness can be increased by one or two grades by deep palpation, then the area may be relevant to the current cause of lameness. False-positive results do occur, but in my opinion these are less frequent than with most flexion tests. There are few false-negative results.
Digital Compression of a Painful Area
The veterinarian should elevate the limb and compress the painful or otherwise inflamed area for 15 to 30 seconds and then evaluate the horse at a trot in hand. Exacerbation of the baseline lameness by one or more grades is considered a positive response. This procedure is useful in differentiating the cause of lameness in both the forelimb and hindlimb. In the forelimb, I find it useful to compress the dorsal proximal aspect of the proximal phalanx (if a midsagittal fracture is suspected), the dorsal cortex of the McIII (for bucked shins or a dorsal cortical fracture), exostoses involving the small metacarpal bones (for splints), the suspensory branches or digital flexor tendons, and the proximal palmar metacarpal region (for PSD or longitudinal or avulsion fracture of the McIII). In horses with mild SDF tendonitis, baseline lameness usually is mild or nonexistent, but obvious lameness after digital compression suggests tendonitis as a clinically significant problem.
In the hindlimbs, compression of the dorsal proximal aspect of the proximal phalanx can increase lameness from midsagittal or dorsal frontal fracture, but trauma from interference injury (of particular importance in trotters) or other forms can lead to a false-positive response. A dynamic Churchill test, compression followed by trotting (see Chapter 6), is useful in the diagnosis of lameness of the proximal metatarsal region and tarsus. In the hindlimb, compression of the proximal aspects of both the second and fourth metatarsal bones puts indirect pressure on the origin of the SL, and a positive response may indicate PSD. False-positive results to this provocative test are common because the entire hindlimb is in flexion, similar to upper limb flexion without compression. Compression of a “curb” followed by trotting may increase lameness.
In some horses with tibial stress fractures, an induced lameness can be seen after deep palpation of the caudal tibial cortex. With the limb elevated, the veterinarian should apply deep pressure to the caudal cortex by wrapping the fingers around the tibia from the medial aspect (see Figure 6-27). Most horses object to this maneuver, but in those with tibial stress fractures, the positive static response is followed by an exacerbation of the baseline lameness.
Axial Skeleton
Application of direct local pressure to many parts of the axial skeleton is difficult, but in some instances this procedure can lead to the detection of pain both statically and while the horse is trotting (see Chapters 6, 93, 95, and 97). In the cervical area, forced lateral bending followed by walking or trotting may exacerbate neurological signs or gait deficits in horses with cervical instability or proliferative changes. Deep palpation over the thoracolumbar spine followed by trotting can induce hindlimb stiffness or other mild gait abnormalities. Direct and deep palpation over the tubera sacrale and tubera coxae can induce hindlimb lameness in horses with stress fractures or those with chronic lameness as a result of pelvic asymmetry from old fractures. Sacroiliac compression, or manipulation of the sacrum or tail head, can induce hindlimb stiffness or lameness in horses with injuries in these areas.
Induced Lameness after Hoof Tester Examination
The hoof testers are applied in a suspected area for 15 to 30 seconds and the horse is evaluated for lameness while trotting. False-positive test results are quite common, but a marked difference between limbs can be an important clinical sign. Shoes and pad combinations may preclude complete hoof tester examination of the sole, so I often apply pressure across the heel. I have found this position to yield the most useful information in horses with palmar foot pain from most causes, but it also induces a positive response in horses with nonspecific foot pain (sore feet). Most normal horses object to firm pressure placed across the heel using hoof testers, particularly in a hindlimb, and mild lameness on the initial few steps is common, but severe lameness after this test is a useful indication that the foot is the source of baseline lameness.
The Wedge Test
The wedge test is a form of manipulation similar to the flexion or other varus or valgus stress tests, but it is used specifically to evaluate the digit and associated soft tissues. The wedge can be used to dramatically change the dorsal-to-palmar (heel) or medial-to-lateral hoof angles. Collateral ligaments, joint capsules, subchondral bone and articular surfaces, and surrounding soft tissues can be stretched or compressed when the horse stands on the wedge. Changes in hoof angles of this magnitude can greatly change the stress placed on the DDF tendon, SDF tendon, and SL. Raising the heel reduces stress on the DDF tendon but increases stress on the SL. Raising the toe reduces stress on the SL but increases stress on the DDF tendon, navicular bone, and associated ligaments and bursa. The number of tissues affected by the wedge accounts for the lack of specificity of this test, and it likely accounts for many false-positive results. The wedge is placed in the desired position, and the horse is made to stand in this position for 30 to 60 seconds with the contralateral limb elevated (Figure 8-12). The horse is then trotted in a straight line on a firm surface. The test can be used in any limb but is performed most commonly in the forelimbs. In some horses, it is difficult to attain the desired duration regardless of whether they are lame. The horse’s response to simply standing on the wedge may not give an accurate indication of how lame it will be when it is trotted. In horses content to stand in such an abnormal position, a dramatic lameness may be seen at the trot. Horses with navicular syndrome or sore feet from many causes of palmar foot pain are most likely to manifest a positive response. In my experience and that of others, the direction of the wedge that elicits the most positive response from horses with palmar foot pain is with the apex (low end) directed medially (see Figure 8-12).11 This substantial change in the medial-to-lateral hoof angle is likely to cause stretching of the suspensory apparatus of the navicular bone and collateral ligaments of the distal interphalangeal joint or compression on articular structures. Horses with palmar foot pain may show severe lameness, but diagnostic analgesia is required to confirm the foot as a source of pain. Horses with injuries of the DDF tendon, SDF tendon, and SL may show a milder response.

Fig. 8-12 A 15- to 20-degree wedge can be used to manipulate the joints and soft tissue structures of the digit. The most consistent response is elicited by directing the apex (low end) of the wedge medially (as shown). The wedge also can be used to raise the heel and toe.
(Wedge courtesy Norman G. Ducharme, Ithaca, New York.)
Varus or Valgus Stress Tests
Evaluation for lameness after placing varus or valgus stress on an individual joint may incriminate this area as a potential source of pain and is used most commonly in the stifle. To perform the stifle valgus stress test, the clinician’s shoulder (or hand) is used as a fulcrum against the distal femur, and the distal limb is pulled laterally several times before the horse is trotted (see Figure 6-25). False-positive results can be obtained because the entire distal extremity is manipulated during this test. Valgus or varus stress tests can be used in many joints in the distal limb, particularly the interphalangeal joints.
Patellar manipulation followed by trotting (see Figure 6-26) may be helpful but can be difficult to perform when horses resist forced proximal movement of the patella (frequently, the veterinarian’s wrist is forced into hyperextension). Although cranial and caudal draw tests can be used to exacerbate stifle lameness, I have not found them particularly helpful, and they are dangerous to perform.
Flexion Tests and Diagnostic Analgesia
I do not generally recommend combining the results of flexion tests and diagnostic analgesia (called “blocking the flexion test”). I often hear that baseline lameness abated after a block, but the horse still had positive flexion test results. My usual comment is, “Why bother to flex the horse if baseline lameness has been abolished?” Flexion tests induce lameness that may be unrelated to the baseline lameness, a concept that is confusing to the inexperienced and to lay people. Thus it is not unusual that a horse might have residual lameness after flexion, even if the baseline lameness has been eliminated.4 I usually do not recommend further investigation once baseline lameness has been eliminated.
If baseline lameness is not obvious but a low-grade gait deficit is present, or if a horse has bilaterally symmetrical lameness, flexion tests or other forms of manipulation or provocation may be the only way of “seeing” lameness. In this instance, induced lameness from manipulation can be assumed to be the baseline lameness, and diagnostic analgesia can proceed. All involved parties should be well informed about the potential for misdiagnosis, but in certain circumstances this pathway may lead to a successful diagnosis.