Chapter 6 Palpation
Palpation is an important part of a lameness examination. In some sports horses, it becomes more important because, for example, suspensory desmitis often is not associated with overt lameness but may compromise performance. The veterinarian must develop a system to evaluate comprehensively all parts of the musculoskeletal system. I palpate in order each forelimb, the neck, the back, the pelvic regions, and then the hindlimbs. Each limb should be assessed when bearing weight and then again with the limb elevated from the ground. Deep palpation is used to describe direct, digital palpation, with the limb in an elevated position.
If time permits, palpation should be completed before the horse is moved, because if the lame limb is identified first, the other limbs may be overlooked and compensatory problems may be missed. For example, in a Thoroughbred (TB) racehorse, superficial digital flexor (SDF) tendonitis is a common compensatory problem caused by contralateral forelimb lameness resulting in overload. If a lame horse with left forelimb lameness is first examined while the horse is moving, and subsequent palpation of the limb reveals signs of possible fetlock osteoarthritis, mild swelling of the right forelimb SDF tendon (SDFT) may be missed. Comprehensive palpation may allow the clinician to make predictions about lameness, to “read” the horse. Palpation before exercise also facilitates identification of localized heat or swelling, because limb temperature increases with exercise, and swelling often decreases.
The Art of Palpation
The veterinarian should palpate and manipulate every possible anatomical structure, using the fingers and hands to push, prod, and feel. Interpretation of an abnormal response requires appreciation of the normal response. There are nerves beneath or adjacent to many structures, and direct pressure may elicit an apparently positive response. Such false-positive responses often occur during palpation of the origin of the suspensory ligament (SL) or the proximal sesamoid bones (PSBs). Care should be taken to apply pressure only in the desired location. During palpation of the PSBs, distal aspect of the SL, and digital flexor tendons, it is easy to apply pressure over the dorsal aspect of the third metacarpal bone (McIII), and a painful response may actually reflect sore shins.
The clinician should look for signs of inflammation: heat, pain, redness, swelling, and loss of function. One side of the horse should be compared with the other, but it should be remembered that both sides may be abnormal. Heat is one of the earliest clinical signs to develop with articular or nonarticular problems and may be the only sign. Subchondral remodeling and sclerosis of the third carpal bone often cause lameness in young racehorses, but effusion of the middle carpal joint and a positive response to flexion are found inconsistently. Usually prominent heat is detectable on the dorsal aspect of the carpus. It is important to recognize normality. A normal horse may have disparity in foot temperature. Horses often have two or three cold feet, but the other foot or feet feel warm. A few hours later, feet that previously were cool may feel warm. Foot temperature often reflects variations in ambient temperature, and care must be taken not to overinterpret this normal finding. In general, palpation is done with the palm side of the hand, although the back of the hand may be more sensitive to detection of warmth.
The veterinarian should assess the quality or strength of the digital pulse. In a normal horse, reliable detection of a digital pulse may be difficult, especially in cold weather or in horses with a thick hair coat. Increased or elevated digital pulse refers to the detection of increased strength (amplitude) or the bounding nature of the digital pulse. Inflammatory conditions in the foot or pastern region, such as abscesses, laminitis, hoof avulsions, or cracks, are the most common causes of increased digital pulse amplitude. Complete absence of hindlimb digital pulse may occur with aortoiliac thromboembolism or other vascular problems, but care should be taken when interpreting weak or near absent hindlimb digital pulses, because hindlimb digital pulses can be difficult to feel in normal horses.
Redness is difficult to perceive in the horse because of skin pigmentation, but in the foot, solar bruising or redness at the coronary band can be observed, especially in horses with nonpigmented feet. Swelling is often detected by observation, but subtle enlargement of structures such as the SL, or presence of effusion may be determined only by careful palpation.
Loss of function of tissues and regions can be assessed during palpation. Manipulation, flexion, and extension of the joints or soft tissues provide a better idea of function or loss of function. Static flexion and extension determine the range of motion of a joint and the horse’s response to the procedure. Chronic osteoarthritis of the fetlock or carpal joints often results in reduced range of flexion. However, many horses in work but without lameness resent hard flexion of the lower limbs. Good correlation between a reduction in fetlock flexion range, lameness, and severity of osteoarthritis was found in TB racehorses.1 A reduction in fetlock flexibility in young Warmbloods may be a predictor of future lameness.2 The response to rotation of joints also should be assessed.
Crepitus, the grating or crackling sound made by bone rubbing on bone, is an unusual and ominous clinical sign usually determined by palpation, although in horses with prominent osteoarthritis or fractures a grating sound may be heard. A stethoscope may be useful for detection of subtle crepitus.
Other factors may confound the results of palpation. Clipped areas usually are warmer than an adjacent area with normal hair length. Blistering or freeze firing can cause localized pain for weeks after application, even if lameness has resolved. Any type of skin lesion, such as those found in horses with scratches or boot rubs, can cause extreme soreness to palpation but no signs of lameness. Some individual horses are more sensitive to palpation than others, and interpretation of apparent pain can be frustrating.
Palpation of the Forelimb
Foot
The importance of the foot cannot be overemphasized, and it is for this reason that palpation of the forelimb begins here. The feet are included in evaluation of conformation, symmetry, and posture. Detailed static examination (examination at rest) of the foot must always be supplemented with, and correlated to, dynamic observations of foot flight and foot striking patterns. Some horses continually attempt to pick up the limb as the clinician tries to evaluate it with the horse in the standing position; it may be necessary to stroke the contralateral limb to divert attention. A hoof pick, wire brush, hoof knife, shoe-removing equipment, and hoof testers are required (Figure 6-1). The sole and frog and wall of the foot should be cleaned thoroughly. Removal of the shoe at this stage in the examination usually is indicated only if a subsolar abscess is suspected. The veterinarian should take care to preserve the hoof wall, and if it is cracked, protect it with tape.

Fig. 6-1 Instruments needed to examine the hoof, remove a shoe without tearing the hoof wall, and prepare the hoof for radiographic examination. Shown are apron, rasp, shoe pullers, nail pullers, clinch tool, hoof knife, hammer and hoof pick, and wire brush.
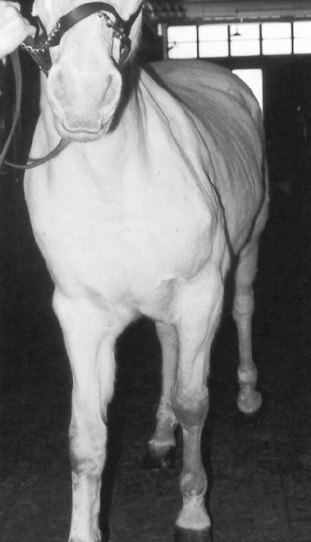
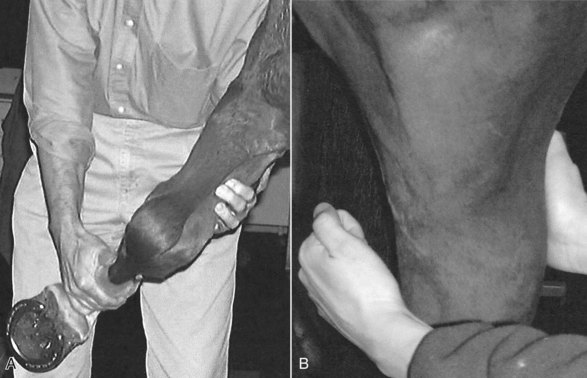
Foot and hoof balance are assessed by evaluating toe and heel length, hoof capsule conformation, condition and integrity, type of shoe and shoe position relative to the hoof capsule, hoof and pastern angle (axis), medial-to-lateral hoof balance, coronary band conformation, and distal interphalangeal (coffin) joint capsule distention and response to hoof testers. The coronary band should normally be parallel to the ground surface. Deviation from parallel often indicates mediolateral foot imbalance (Figure 6-2). Medial and lateral wall lengths should be assessed while the horse is standing and again with the limb off the ground, with the foot viewed from palmar to dorsal along the solar aspect. The limb is lifted and held in neutral position so the solar surface is perpendicular to the ground. Sheared and underrun heels are commonly associated with lameness (Figure 6-3). Deformation of the hoof capsule is not necessarily a cause of lameness. Many horses with proximal displacement of the medial heel bulb have level foot strikes and otherwise balanced feet. Toe and heel length should be assessed, and the hoof-pastern axis should be determined. The angle of the hoof and pastern should be equal to allow equal loading of all portions of the foot. Forelimb hoof-pastern angles normally range from 48 to 55 degrees, but the absolute angle should not be overemphasized. A straight (parallel) pastern-foot axis is more important. A long-toe, underrun-heel foot conformation causes a broken foot axis and predisposes to palmar foot pain (Figure 6-4).

Fig. 6-2 The coronary band is uneven compared with the ground in this trotter’s unbalanced left forelimb hoof. The medial wall (right) appears to be shorter than the lateral wall. A toe weight and bariun point are also shown.

Fig. 6-3 Elevated foot viewed from the palmar aspects shows that the hairline at the medial bulb of heel (on the right) is displaced proximally compared with the lateral heel bulb. The medial wall is longer. Note also the prominent cleft between the heel bulbs. These features are typical of a sheared heel.
The conformation, condition, and integrity of the hoof capsule should be assessed. It is easy to miss hoof wall defects on the medial aspect. Small quarter or heel cracks and defects at the coronary band should not be overlooked. The clinician should evaluate the solar surface, bars, and frog. Thrush, although a reflection of poor management, rarely causes lameness.
The shoe type, shoe wear patterns, and the shoe size relative to the foot need to be assessed. The clinician should note the presence of pads or additions to the shoe, such as toe grabs, borium, and heel caulks. There is an association between toe grabs and suspensory apparatus failure in TB racehorses.3 Low heel angle also has been associated with injury.4 Shoe wear is important, because it reflects how the horse has been moving over the last several weeks. The clinician should note the breakover point and whether one branch of the shoe is worn more than the other. Shoe size should be assessed relative to foot size and the fit of the shoe. A shoe that is too small or set too close to the frog may predispose to lameness.
Careful palpation of the coronary band in the standing and non–weight-bearing position is critical in detecting foot soreness (Figure 6-5). In horses with sore feet, heat and pain often are detected on the sore side of the foot, and a prominent digital pulse usually is present. Effusion of the distal interphalangeal joint capsule accompanies many abnormalities of the foot, from early synovitis to chronic osteoarthritis of the distal interphalangeal joint, and those with non-specific foot soreness. The clinician places one finger lateral to, and another medial to, the common digital extensor tendon and gently pushes in on the joint capsule, first laterally and then medially. Ballottement is a useful technique to detect effusion in many synovial structures: with effusion, pushing in on the capsule on one side of the tendon causes elevation of the capsule on the other side. The region of the collateral ligaments of the distal interphalangeal joint should be assessed carefully; focal heat or mild swelling may signify acute injury.

Fig. 6-5 Palpation of the coronary band should include assessing the dorsal joint pouch of the distal interphalangeal joint. In this horse, distal interphalangeal effusion and fibrosis appear as a bulge just proximal to the coronary band, dorsally.
The clinician should palpate the cartilages of the foot, either with the horse standing or with the limb elevated. Sidebone, mineralization of the cartilages of the foot, rarely causes lameness. The cartilages of the foot normally are pliable and readily compressed axially. Fracture at the attachment of the cartilage of the foot to the distal phalanx is an occasional cause of lameness, and compression of the heel with hoof testers may elicit pain in some horses. Horses with sidebone often have medial-to-lateral hoof imbalance.
Hoof Tester Examination
“… I feel naked going into a stall without my hoof testers!”5 Hoof testers are essential for evaluation of the foot and are a basic requirement for all lameness examinations. Many types of hoof testers are available (Figure 6-6), but I favor one that is adjustable and can be applied with one hand. A proper evaluation of the foot with hoof testers cannot be done with a pad in place, although useful information can be acquired. The instrument can be applied with or without a shoe in place. The amount of force to apply varies from horse to horse and by region of the hoof, and both false-positive and false-negative responses occur. More force is required when the instrument is used across the heel than when used from sole to quarter. The foot should be held between the clinician’s legs in a relaxed manner. The clinician must be able to feel the horse react to subtle pressure, and if the limb is held too tightly or the horse is not calm during the examination, it is difficult to feel a response. The veterinarian should be careful not to place the outside jaw of the instrument too close to the coronary band, because this may cause a false-positive result. Sole sensitivity is assessed by applying the instrument to three to five sites from heel to toe, on both the medial and lateral aspects of the foot, starting from the angle of the sole (seat of the corn) and proceeding dorsally (Figure 6-7). The responses should be compared. If the sole is readily compressible, pain from bruising, a subsolar abscess, laminitis, fracture of the distal phalanx, and other injuries may be elicited, but in horses with hard horn the response may be negative. To evaluate sensitivity of the frog and underlying deeper structures, the hoof testers should be applied from the lateral aspect of the frog to the medial wall, and from the medial aspect of the frog to the lateral wall, each in the palmar, midportion, and dorsal aspects of the frog (Figure 6-8). Pain over the middle third of the frog has been attributed to navicular disease or navicular syndrome, but the specificity of this association is questionable and there are many false-negative responses. Horses with generalized foot soreness or any other cause of palmar foot pain may respond positively or not at all. Only 19 of 42 horses with navicular region pain responded positively to hoof tester examination in the middle third of the frog, with 50% specificity, 50% positive predictive value, and 48% accuracy.6 Horses with palmar foot pain caused by other conditions were as likely to respond to the test, a finding that obviously prompts questioning of the value of hoof tester examination.6 It is difficult if not impossible to create adequate pressure to cause pain in large breed horses or if the horn is hard. Application of a poultice or soaking the foot may be necessary to soften a hard foot, and reexamination after several days may be rewarding. Hoof tester application to the small feet of foals or ponies may elicit a false-positive response, and hoof tester size or amount of compression may require adjustment.

Fig. 6-6 A variety of hoof testers are available for lameness examinations. I prefer hoof testers that are easily adjusted and used in one hand (two pairs on the right). Large hoof testers (left) can be applied only with two hands, and small hoof testers (bottom) are inappropriate for medium to large hooves.

Fig. 6-7 Hoof testers should be applied from the sole to the wall, from heel to toe, and to both sides of the hoof.

Fig. 6-8 Hoof testers applied from the middle of the frog to the contralateral hoof wall put pressure on the navicular region. Horses with many abnormal conditions of the hoof may manifest a positive response.
Application of hoof testers across the heel may cause pain in horses with palmar foot pain but is not specific (Figure 6-9). Application of the hoof tester to the area of the sole adjacent to each nail, nail hole, or defect in the sole or white line is useful to detect a subsolar abscess or a close nail (Figure 6-10). Areas of pain can be gently explored with a hoof knife, but unless clearly indicated, the veterinarian should refrain from digging too deeply. The hoof tester can then be used as a hammer to percuss each nail in the shoe and the frog and toe regions.

Fig. 6-9 Adjustable hoof testers are easily placed across the heel. I prefer to apply hoof testers in this manner to assess horses for palmar foot pain during static examination and as a provocative test for lameness.
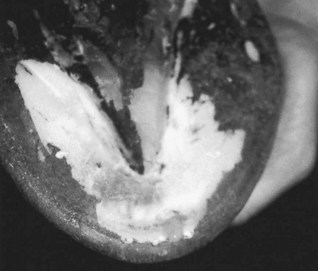
Fig. 6-10 Acute, severe lameness causing increase in digital pulse and profound hoof tester sensitivity in the toe region resulted from this hoof abscess. Exudate drains from the pared region at the toe.
(Courtesy Greg Staller, Pottersville, New Jersey.)
After completing the hoof tester examination, the clinician should reassess the digital pulses. In horses with foot pain the digital pulse may now be bounding. Horses that have recently been shod or trimmed or have raced or performed recently, especially on hard surfaces, may have mild elevations in digital pulse amplitude and may show hoof tester sensitivity normally. Pain causing lameness may not be in the foot.
Wedge Test and Other Forms of Static Manipulation
The wedge test is used most commonly as a dynamic procedure to induce lameness during the movement phase of the examination, but can be used to assess the static response of a horse to dramatic changes in dorsal-to-palmar or medial-to-lateral hoof angles (see Chapter 8, Figure 8-12). A digital extension device, with which the author gauged static painful responses to changes in hoof angle to make shoeing recommendations, was recently described.7
Pastern
The proximal interphalangeal (pastern) joint capsule is assessed by ballottement, although severe effusion must be present for fluid distention to be perceived. Bony swelling associated with this joint, proximal or high ringbone, is a classic cause of lameness yet an unusual clinical finding. Osteoarthritis of the proximal interphalangeal joint is a common diagnosis, but one made by a combination of clinical findings, diagnostic analgesia, radiography, and sometimes scintigraphy. The distal extent of the digital flexor tendon sheath (DFTS), deep digital flexor tendon (DDFT), and distal sesamoidean ligaments are palpated. Deep pain associated with the origin and insertion of the distal sesamoidean ligaments is assessed by palpation with the limb in flexion (Figure 6-11). In some horses with lesions of the DDFT within the hoof capsule a positive response to compression of the palmar pastern region is present, but this finding is inconsistent and many false-negative responses occur. The oblique sesamoidean ligaments are difficult to differentiate from the branches of the SDFT, but injury of the SDFT is more common. Distal sesamoidean desmitis or chronic suspensory desmitis may result in subluxation of the proximal interphalangeal joint (Figure 6-12). Swelling should prompt ultrasonographic examination if relevance has been confirmed using diagnostic analgesia. The proximal interphalangeal joint is manipulated in a medial-to-lateral direction to assess pain and collateral ligament integrity and is flexed independently of the fetlock joint. The proximal, dorsal aspect of the proximal phalanx is palpated (Figure 6-13). Horses with short, midsagittal fractures or dorsal frontal fractures of the proximal phalanx or proliferation at the attachment of the common digital extensor tendon may show pain. Enthesophyte formation at the common digital extensor tendon attachment, seen most commonly in older ex-racehorses with chronic osteoarthritis of the fetlock joint, results in prominent bony and soft tissue swelling and pain on palpation.
Fetlock
The clinician palpates the joint capsule of the metacarpophalangeal (fetlock) joint with the limb bearing weight, keeping in mind that pain associated with the joint can be present without localizing clinical signs. The dorsal aspect is palpated using ballottement on either side of the common digital extensor tendon. The clinician should determine whether localized heat is present. Osselets is a North American term used to describe early osteoarthritis of the metacarpophalangeal joint in young racehorses, with firm bony and soft tissue swelling on the dorsal, medial aspect of the proximal phalanx, and the distal aspect of the McIII, caused by traumatic capsulitis and early enthesophyte formation. Occasionally in horses with prominent effusion of the metacarpophalangeal joint, a soft tissue swelling can be palpated in the proximal, dorsal aspect of the joint from excessive proliferation of the dorsal synovial pads, called proliferative or villonodular synovitis. The palmar pouch of the metacarpophalangeal joint is palpated dorsal to the SL branches, both medially and laterally. Mild effusion may be present without associated lameness, especially in older performance horses. The PSBs are palpated and assessed for mild swelling and heat, clinical signs of sesamoiditis, or SL avulsion injury. The digital pulse amplitude is reassessed by placing fingers both medially and laterally, abaxial to both PSBs (Figure 6-14).
The DFTS extends from the distal metacarpal region to the distal palmar aspect of the pastern. Usually no palpable fluid is found. Effusion of the DFTS (tenosynovitis) causes swelling in the palmar fetlock region that must be differentiated from effusion of the metacarpophalangeal joint. Tenosynovitis causes swelling palmar to the branches of the SL, medially and laterally. Fluid can be compressed from medial to lateral. With severe effusion, distention is found in the palmar aspect of the pastern, but there may be distention proximal to the palmar annular ligament without obvious distention distally. Wind puffs or windgalls describe incidental fluid distention of the DFTS, commonly seen in older performance horses unassociated with lameness. Tenosynovitis can cause lameness, but additional diagnostic techniques are required to confirm the diagnosis.
The limb is elevated to assess range of joint motion and the horse’s response to flexion. Normally the fetlock can be flexed to 90 degrees (the angle between the proximal phalanx and the McIII) or slightly more. A reduction in fetlock flexion range is indicative of chronic fibrosis but is not necessarily a cause for concern. A pronounced response to static flexion is noteworthy, although many horses resent static flexion but do not show a positive response to dynamic flexion (lower limb or fetlock flexion tests; see Chapter 8). Horses with clinically relevant tenosynovitis usually strongly resent fetlock flexion. With the limb in flexion, the clinician palpates the PSBs and the branches of the SL, avoiding compression of the palmar digital nerves.
Metacarpal Region
The clinician should assess the dorsal aspect of the McIII for heat and swelling. This is a common area for traumatic injury (barked shins) or stress-related bone injury (bucked shin syndrome). Many ex-racehorses have incidental, prominent, chronic, and nonpainful swelling of the McIII caused by extensive modeling and remodeling of the dorsal cortex while in race training. Racehorses currently in training may have heat and pain on deep palpation (performed with the limb elevated), but prominent swelling may be lacking. Any combination of palpation findings is possible in horses with stress-related bone injury of the McIII. It is difficult to apply deep pressure to the dorsal aspect of the McIII without concomitant pressure to the palmar soft tissue structures or PSBs, so the responses should be assessed carefully.
The entire length (abaxial surface) of the second and fourth metacarpal bones (McII/IV) should be palpated with the horse in the standing position to detect exostoses, callus, or fractures. Swelling of the SL branches or body may make this difficult. Palpation of the McII and the McIV should be repeated with the limb elevated, because the axial aspect of these bones is impossible to assess in the weight-bearing position. Splint exostoses are common, particularly in young horses. Therefore the presence of even large bony swellings is not unusual. Exostoses detected axially, possibly impinging on the SL or causing adhesions to the SL (or so-called “blind splints”) should be carefully noted. Both false-positive and false-negative results can occur when palpating a splint exostosis and results of palpation and compression should be confirmed using perineural analgesia. Pain from even small exostoses of the McII and the McIV usually is more accurately assessed immediately after training or racing, because pain and lameness resulting from these swellings can be subtle and transient. The clinician should carefully palpate the SL branches. Differentiation of branch or SL body injuries is important: the latter injuries usually are more serious and have a worse prognosis.
The medial and lateral palmar digital vein, artery, and nerve, in dorsal-to-palmar orientation, respectively, are located between the SL and DDFT. The accessory ligament (distal or inferior check ligament) of the DDFT (ALDDFT) normally is difficult to palpate and even when enlarged cannot easily be differentiated from the DDFT, but injuries of the ALDDFT are more common. All soft tissue structures should be palpated carefully, using digital compression, with the limb elevated (Figure 6-15). Acute or chronic swelling should be assessed, as should the horse’s response to deep palpation. Obvious swelling and pain indicate the presence of tendonitis or desmitis. In some horses with acute severe tendonitis or desmitis the structure feels “mushy” or soft in the area of fiber damage. This finding, especially in horses with fetlock drop, indicates near rupture of the structure. There are many false-positive and even false-negative responses to palpation of the digital flexor tendons and SL. In most ridden performance horses a mild painful response (false-positive) to deep palpation of the SL is normal. However, in racehorses, false-positive responses are less common, and a painful response to deep palpation may indicate the presence of early desmitis or tendonitis. In many horses with foot lameness, secondary, mild suspensory desmitis is common. There is a painful response to palpation of the body and origin of the SL. It may be difficult to decide whether this is a true or false-positive response, a determination that often is made in hindsight after the lameness examination is finished. False-positive and false-negative responses to palpation of the proximal palmar metacarpal region also occur. This is a common site of lameness and should be examined carefully. Palpation must be done with the limb in flexion, and the presence of swelling and pain must be carefully interpreted (Figure 6-16). Horses with acute injuries, such as proximal suspensory desmitis (PSD), avulsion or longitudinal fracture of the McIII, and stress reaction of the McIII at the origin of the SL, may have swelling and pain. Deep palpation may create pressure on the palmar metacarpal nerves resulting in a false-positive pain response, and many horses with PSD have no localizing signs. The most proximal aspect of the SDFT is difficult to palpate with the limb in a flexed position, and mild swelling from tendonitis can easily be missed. When the limb is weight bearing, the expected convex profile associated with SDF tendonitis in the mid-to-distal regions of the metacarpal region is usually not seen because of pressure from the overlying metacarpal fascia. Careful palpation of the proximal aspect of the SDFT, particularly in horses that negotiate fences or in ponies, is necessary to avoid missing subtle lesions. This injury is particularly hard to recognize in horses or ponies with long hair coats.

Fig. 6-15 The soft tissue structures in the palmar metacarpal region should be carefully palpated with the horse in standing and flexed (shown) positions for heat, pain on compression, and swelling. Most ridden horses have mild pain, but in racehorses a painful response is an early sign of tendonitis or desmitis.

Fig. 6-16 Palpation of the proximopalmar metacarpal region is essential in diagnosing proximal suspensory desmitis and other conditions of the suspensory origin and differentiating lameness in the region from carpal lameness.
(Courtesy Ross Rich, Cave Creek, Arizona.)
The proximal dorsal aspect of the McIII should be palpated in a flexed position (Figure 6-17). Occasionally, dorsomedial articular fracture of the McIII results in a subtle painful swelling. Swelling (effusion) of the carpal sheath may be detected in the proximal medial metacarpal region, but large veins (medial palmar, accessory cephalic, and cephalic veins) may interfere with accurate palpation. With mild tenosynovitis, effusion may be difficult to discern.
Carpus
Detection of warmth on the dorsal aspect of the carpus is a reliable indicator of underlying inflammation. Obviously, one side should be compared with the other, but bilateral conditions exist commonly. Previous application of counterirritants interferes with the reliable detection of warmth. Carpal joint lameness without obvious signs of synovitis is common, but if present, effusion is easily palpated using ballottement. With the horse in the standing position, a finger is placed dorsolaterally between the extensor carpi radialis and common digital extensor tendons, and another finger is placed just medial to the extensor carpi radialis tendon. These openings are used for palpation and arthrocentesis of both the middle carpal and the antebrachiocarpal joints. The middle carpal and the carpometacarpal joints always communicate, but a small synovial compartment and dense overlying soft tissue structures limit palpation of the carpometacarpal joint. Both the middle carpal and the antebrachiocarpal joints have a palmarolateral pouch that may be distended if effusion is severe. If swelling is detected just caudal to the radius, it is necessary to differentiate distention of the palmarolateral pouch of the antebrachiocarpal joint from the carpal sheath (Figure 6-18). In horses with antebrachiocarpal joint effusion the dorsal outpouchings also should be prominent, whereas in those with carpal sheath effusion, fluid distention is restricted to the palmar aspect and also detected medially, both proximal and distal to the accessory carpal bone.

Fig. 6-18 Carpal tenosynovitis must be differentiated from effusion of the antebrachiocarpal joint. This horse with severe superficial digital flexor tendonitis has moderate distention of the carpal sheath (arrow) in the caudal, distal aspect of the antebrachium and medially in the proximal metacarpal region (not shown).
Tenosynovitis of the extensor carpi radialis, common digital extensor, or lateral digital extensor sheaths results in vertically oriented swellings that traverse the carpal joints, may extend proximal or distal to the carpus, and usually are multilobed, being divided by bands of extensor retinaculum located dorsally and laterally.
Normally the carpus can easily be flexed completely, so that the palmar metacarpal region and bulbs of the heel touch the caudal aspect of the antebrachium. Reduced flexion may be caused by pain, with or without chronic fibrosis, associated with osteoarthritis. Pain during carpal flexion is a reliable indicator of carpal region pain but does not indicate the cause. The carpal sheath is compressed and the extensor tendons are stretched during this maneuver, and conditions involving these structures and the accessory carpal bone can cause pain during flexion. The elbow joint is flexed simultaneously; therefore a positive response to carpal flexion can rarely result from elbow pain. The examiner should palpate the dorsal surfaces of the carpal bones with the limb in partial flexion (Figure 6-19). Many pathological conditions associated with the carpus are manifested dorsally, and pain associated with osteochondral fragmentation, slab fractures or other severe injuries, or osteoarthritis can be assessed with the limb in this position. Focal pain can be identified, and loose fragments associated with the third carpal bone or distal lateral radius occasionally can be identified.
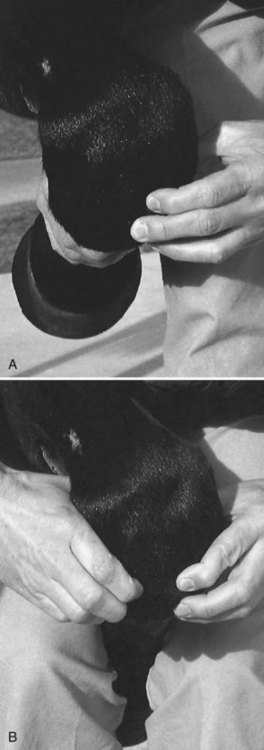
Fig. 6-19 Careful palpation of the dorsal aspect of each carpal bone can be done with one hand (A) or by placing the distal limb between the clinician’s legs and using both hands (B). A pain response indicates an osteochondral fragment or an osteophyte. Occasionally a loose osteochondral fragment can be palpated.
Antebrachium (Forearm)
Digital palpation of the forearm usually is performed with the limb bearing weight. The examiner should look primarily for muscle atrophy, wounds, or mild swelling associated with the radius. Small wounds in the antebrachium may look innocuous, but inappropriately severe lameness and pain on palpation may reflect a spiral radial fracture. The examiner should pay particular attention to the medial aspect of the limb; this area is easily overlooked when palpating from the lateral side. Distally, fluid distention of the carpal sheath or acute swelling associated with injury of the accessory ligament (proximal or superior check ligament) of the SDFT, or the flexor muscles and tendons can occur. The amount of muscle in the extensors and flexors should be compared with that in the contralateral limb, because subtle atrophy may be missed during observation.
Elbow
Frank swelling and prominent lameness accompany many injuries of the elbow region, but other problems of the elbow joint are discovered only after diagnostic analgesia has localized pain to this area or by use of advanced imaging modalities. It is nearly impossible to use diagnostic analgesic techniques to abolish pain in the distal aspect of the humerus and proximal aspects of the radius and ulna; therefore advanced imaging techniques are often required to identify problems in these structures. The clinician should palpate the olecranon process and the lateral and medial collateral ligaments with the limb bearing weight. Effusion is difficult to detect, but excess fluid occasionally can be found using ballottement, by placing fingers both cranial and caudal to the lateral collateral ligament. The elbow is flexed by pulling the distal limb in a cranial and proximal direction and then extended by pulling the lower limb in a caudal direction. The shoulder joint is undergoing the opposite reaction during this manipulation, and pain associated with that joint or the bicipital bursa can cause a positive response during elbow manipulation.
Brachium (Arm) and Shoulder
The shoulder and intertubercular (bicipital) bursa are regularly blamed as the cause of lameness yet are seldom involved. Normal horses may resent palpation of this area. Pain in the muscles surrounding the shoulder joint may develop secondary to primary lower limb lameness. In Standardbred (STB) racehorses with carpal lameness, secondary pain often is detected when the bicipital bursa is palpated. A rare cause of lameness is infection as a result of a previous deep injection of the “shoulder bursae,” and horses may have only subtle pain on palpation and manipulation of the shoulder region.![]() Infectious bicipital bursitis generally causes severe lameness, a marked shortened cranial phase of the stride, and a marked painful response to shoulder joint flexion.
Infectious bicipital bursitis generally causes severe lameness, a marked shortened cranial phase of the stride, and a marked painful response to shoulder joint flexion.
Palpation of the arm is limited because overlying muscles obscure much of the humerus. Horses with displaced humeral fractures usually are unwilling to bear weight and have severe soft tissue swelling. Those with humeral stress fractures usually have no localizing signs except a positive response to upper limb manipulation. A normal intertubercular bursa is not palpable. Horses with bicipital bursitis usually resent direct compression of the greater tubercle of the humerus, and fluid distention may be palpable, but ballottement is usually limited. Effusion of the scapulohumeral (shoulder) joint is palpable only if severe and even then is easily overlooked.
Upper limb manipulation, including static flexion and extension to assess the range of motion of the shoulder and elbow joints and the presence of a painful response, should always be performed. This can be done during palpation of the elbow or later when the clinician finishes the shoulder region. Most horses with shoulder joint lameness or bicipital bursitis show a painful response when the limb is pulled backward (shoulder flexion, elbow extension), whereas those with elbow lameness may show a painful response when the limb is pulled forward (shoulder extension, elbow flexion).
The examiner should palpate the scapular area and move the mane if necessary. Atrophy of the infraspinatus and supraspinatus muscles may indicate suprascapular nerve or brachial plexus injury (Figure 6-20). Muscle atrophy of these and other forelimb muscles can be caused by other neurogenic causes or by disuse. Upper limb palpation often is used to confirm those findings recognized during observation of the horse. Scapular height is compared manually. Although rare, damage to the innervation of the serratus ventralis muscle or direct trauma to the muscle itself allows abnormal elevation of the injured side when the horse is standing or during movement. Pectoral muscle atrophy can easily be missed during observation, and the pectoral region should be palpated to assess pectoral muscle mass and identify swellings or wounds that may cause lameness.
Palpation of the Cervical and Thoracolumbar Spine
Cervical Spine (Neck)
Palpation of the neck is limited. I usually palpate the brachiocephalicus muscle after shoulder palpation and manipulation, a procedure thought to have predictive but nonspecific value in horses with forelimb lameness.8 The muscle is squeezed just cranial to the shoulder joint; most horses flinch, but some horses with ipsilateral forelimb lameness show a marked pain response. The examiner should palpate both sides of the neck, noting any swelling or muscle atrophy. Cervical abscessation can cause signs of neck pain and forelimb lameness. Muscle atrophy may indicate long-standing cervical pain or ipsilateral forelimb lameness. Muscle development of the neck may be asymmetrical, especially if viewed from above (the perspective of a rider).2 Palpation of the poll region is important because undue soreness cranial to the wings of the atlas may be associated with poor performance.2 The head should be moved from side to side to evaluate the horse’s willingness to move the neck. One hand is placed on the midcervical region to use as a fulcrum, and the other hand is used to bend the head and neck toward the examiner. Food also can be used to entice the horse to move the head and neck from side to side. Normally a horse can reach around to the girth region on either side to ingest food, and reluctance to do so may indicate neck pain. This procedure may more closely mimic the horse’s natural head and neck movement than using a hand in the midcervical area as a fulcrum. A more comprehensive examination, including neurological or chiropractic evaluations, may be necessary after completion of the lameness examination. Up-and-down movement of the head also should be assessed. Although usually not a part of a routine lameness examination, evaluation of the temporomandibular joints and the mouth may be necessary in horses with poor performance.2
Thoracolumbar Spine (Back)
Additional detailed palpation of the back and pelvis may be necessary once the lameness examination has been completed. Chiropractic manipulation and assessment of acupuncture points may be useful but usually are reserved for specific horses or when history and clinical signs warrant such an examination and if the clinician is qualified to complete it. The cranial thoracic spine has already been briefly evaluated during examination of the shoulder for scapular symmetry. The withers should be examined closely for conformational abnormalities, such as those seen with fracture of the dorsal spinous processes or fistulous withers. The presence of sores may indicate an ill-fitting saddle and can cause performance-related problems. Using a hand on each side of the spine, the examiner should apply digital pressure to assess vertebral height, presence of pain, and muscle atrophy and to confirm symmetry (Figure 6-21). Many horses resent deep and aggressive palpation of the epaxial muscles, and the response of normal horses should be learned before a pathological response is presumed. Most horses readily become mildly lordotic (“scootch”) during deep digital palpation or when a blunt object, such as a pen, is used. Some clinicians prefer to use the ends of the fingers to “run” (apply digital pressure while moving the fingers caudally) the muscles from cranial to caudal, parallel to the spinal column. When this is continued along the gluteal muscles and rump, most normal horses become somewhat kyphotic and move forward slightly. Aggressive use of blunt or sharp objects to assess pain should be avoided. Some horses are stoic during palpation, and it may be impossible to stimulate them to extend and flex the thoracolumbar region without the use of a blunt instrument.2 In these horses, firmly stroking the ventral abdomen may stimulate movement.2 With one hand on the horse’s back during movement of the thoracolumbar spine, the clinician may be able to feel muscle “cracking” during the release of tension in the epaxial muscles.2 The observation of muscle fasciculations during or after palpation usually indicates a degree of muscle pain. Failure to exhibit the normal lordotic or kyphotic responses, assumption of a guarded posture, and vocalization during the examination are further signs of back pain.
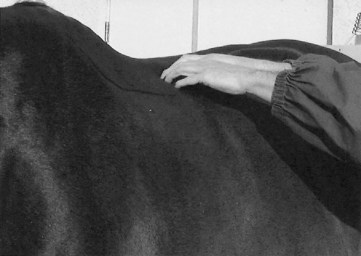
Fig. 6-21 Palpation of the thoracolumbar region should be performed in a quiet, careful manner. Many horses object to sudden or sharp stimuli applied to this region. Direct, even pressure is applied to the epaxial muscles (shown) and the summits of the dorsal spinous processes.
In many horses, back pain, and more specifically muscle pain, is secondary to hindlimb lameness, resulting from altered gait and posture. Any site of pain in the hindlimb may alter the gait to cause secondary upper limb or back muscle pain. The use of diagnostic analgesia to confirm the primary source of pain (in the hindlimb, or locally in the back) may be required to make the true diagnosis. Back pain often is complex and may be caused by many factors including ill-fitting saddles, poor riding, and other primary problems, such as overriding of dorsal spinous processes or other bony causes. The clinician should palpate carefully to detect localized swelling in the area of the saddle. Even small areas of hair loss without swelling may indicate a loose or ill-fitting saddle, abnormal movement of the saddle associated with hindlimb lameness, or a rider sitting crookedly.2
It is doubtful that muscular pain alone can cause unilateral hindlimb lameness. Back pain was induced in STB horses by injection of lactic acid into the left longissimus dorsi muscle and subsequently exercised and observed with high-speed cinematography.9 Frank lameness was not observed, but there was slight modification of left hindlimb stride and reduced performance. This supports the clinical observation that back pain usually is the result, not the cause, of obvious hindlimb lameness, although it may result in slight alterations in gait. Severe vertebral abnormalities or an abscess in the epaxial muscles may result in lameness or neurological dysfunction.
Palpation of the Lateral and Ventral Thorax and Abdomen
History or observation of lameness, performance, or behavioral abnormalities seen only when a horse is ridden or wearing tack should prompt examination of the thoracic region. Irritation from an ill-fitting girth or other sores or wounds can contribute to poor performance, and injury of the sternum or ribs can cause pain associated with saddling or being ridden. Traumatically induced hernias of the ventral abdomen can cause gait deficits or guarding of the abdomen.
Palpation of the External Genitalia
Testicular or inguinal pain should be considered as a cause of gait modification. Swelling, infection from previous castration, scirrhous cord, and mastitis can cause a change in gait. The veterinarian should determine the sex of the horse and the presence of one or both testicles.
Palpation of the Pelvis
Palpation of the pelvis is performed to confirm previous observations. The horse should stand as squarely as possible. The clinician should palpate all bony protuberances, including the tubera coxae, tubera sacrale, and tubera ischii. The examiner stands behind the horse and palpates these paired protuberances simultaneously if it is safe to do so (Figure 6-22). Fracture of a tuber coxae or an ilial shaft may result in asymmetry, but if the ventral aspect of the tuber coxae is fractured, the height of the dorsal aspect may be equal to that of the contralateral side. The anatomy of the ventral aspect of the tuber coxae is distorted. Small muscle defects may be associated with fracture or enthesopathy of the tubera ischii, but even with a displaced fracture, palpation of this area may be unrewarding (Figure 6-23). If a pelvic injury or fracture is suspected, the clinician should gently rock (move) the horse from side to side. Subtle crepitus may be detected, but in many horses with pelvic fractures this is not apparent until days to weeks after injury and only during the initial portions of the examination before muscle guarding supervenes. The veterinarian should grasp the tail and elevate it. Many horses resist this, but in those with fractures of the base of the tail (most commonly from sitting in the starting gate or trailer), a true pain response is elicited. Subtle swelling also may be present. Lack of tail tone may indicate neurological disease.
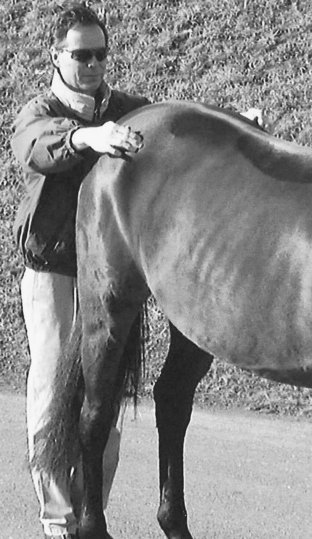
Fig. 6-22 Although the veterinarian must take care when standing behind any horse, this perspective is crucial in determining pelvic heights and widths. The height of each tuber coxae is compared in this photograph. Alternatively, an assistant on each side can be asked to point to a comparable location, or tape can be applied.

Fig. 6-23 The tubera ischii (shown) and third trochanters are palpated carefully. Enthesopathy or fracture causes lameness that is difficult to locate without careful palpation or scintigraphic examination. Occasionally, horses with small muscle defects located distal to the tubera ischii have chronic lameness from previous fracture.
(Courtesy Carolyn Arnold, College Station, TX.)
Muscle pain and muscle atrophy should be assessed. The clinician carefully examines the gluteal musculature, the origin of the caudal thigh muscles, and the tensor fasciae latae (see Chapter 47 for further discussion of muscle assessment and palpation of the greater trochanter of the femur). Pain or soreness noted during palpation of the semimembranosus and semitendinosus muscles may be associated with injury of the ipsilateral tuber ischium.2
Palpation of the Pelvis per Rectum
Rectal examination is not part of the routine lameness examination and should be reserved as a special examination procedure if pelvic fracture or aortoiliac thrombosis is suspected. With the wrist just inside the anus the veterinarian should palpate the medial and dorsal aspects of the acetabulum, comparing sides. In young horses, there is a membranous junction between pelvic bones in the center of the acetabulum; a defect and a small amount of motion normally can be felt. Just cranial to the acetabulum is the cranial aspect of the pubis (brim of the pelvis). With the arm at elbow depth the examiner should sweep the arm dorsally on each side to palpate the medial aspect of each ilium. The ventral aspect of the sacrum and sacroiliac region are compared. The clinician should compare the pulse quality between the right and left external iliac arteries and evaluate conformation and pulse quality of the terminal aorta and branches. Horses with aortoiliac thromboembolism have abnormal conformation and altered pulse quality. Crepitus may be felt more easily by gently rocking the horse from side to side, picking up one hindlimb, or walking the horse a short distance with the veterinarian’s arm still within the rectum.
Asymmetry, swelling, actual fracture lines, fragments or callus, and crepitus are assessed. In horses with acute pelvic fractures, crepitus, fracture fragments or lines, and callus usually are not detectable, but hematoma and soft tissue swelling usually can be felt. In horses with ilial wing or shaft fractures, large fracture hematomas often are present, but the absence of swelling does not preclude presence of ilial fractures. These horses are at risk to develop fatal hemorrhage. Edges of fracture fragments may be evident with comminuted or grossly displaced fractures. With chronic pelvic fractures, crepitus and callus may be more obvious.
Palpation of the Hindlimb
For safety reasons, I prefer to start proximally and work distally in a hindlimb, allowing the horse to become accustomed to palpation. Horses often object to palpation of the flank and stifle regions, and this should not be misinterpreted as a sign of pain. The clinician should grasp the tail and pull it gently toward himself or herself to keep the ipsilateral hindlimb bearing weight and reduce the chance of the horse kicking. It may be useful to pick up the ipsilateral forelimb. In the large majority of horses the entire limb can be safely examined while bearing weight, but pain in the lame limb or contralateral limb or the horse’s behavior may make it difficult or impossible to pick up the limb. Reluctance to pick up the hindlimbs has been attributed to unilateral or bilateral sacroiliac pain.2 Horses with shivers often are reluctant or anxious to pick up one or both hindlimbs. It may be necessary to spend a small amount of time coaxing the horse to elevate the hindlimb, at first just high enough to examine or pick out the hind foot and then progressing to full flexion. Although historically the hock and stifle joints have been regarded as the principal sources of pain causing hindlimb lameness, there are many other potential sites, and the metatarsal and fetlock regions in particular should be examined with care.
Thigh
The clinician should assess the thigh for swelling, muscle atrophy, or scarring. Horses with femoral fractures usually have obvious severe swelling, crepitus, and instability of the limb. The third trochanter of the femur is difficult to feel, and clinical abnormalities associated with enthesopathy of the insertion of the superficial gluteal muscle or a fracture usually are impossible to detect. Scarring associated with the semitendinosus, the semimembranosus, and rarely the biceps femoris can lead to mechanical gait deficits, known as fibrotic myopathy. ![]() The gastrocnemius muscle arises from the distal caudal aspect of the femur, and acute tearing of this muscle may cause swelling in the caudal stifle area. This is difficult to perceive, but severe muscle injury results in a marked postural change, which should provoke more careful assessment of this region.
The gastrocnemius muscle arises from the distal caudal aspect of the femur, and acute tearing of this muscle may cause swelling in the caudal stifle area. This is difficult to perceive, but severe muscle injury results in a marked postural change, which should provoke more careful assessment of this region. ![]()
Stifle
Palpation of the stifle is limited to the cranial, lateral, and medial aspects; unfortunately, the caudal and proximal aspects of the joint are inaccessible. Many horses, especially fillies, object to palpation of the stifle, a normal response often misinterpreted as a painful reaction.
The veterinarian should palpate the stifle with the limb bearing weight. The foot should be flat on the ground. This may be impossible if the horse has severe pain prohibiting complete assessment of the stifle. The limb should be in a neutral and not in an abducted position and should be perpendicular to the spine or slightly ahead of the other hindlimb. If the limb is retracted, it is more difficult to palpate the patellar ligaments and joint outpouchings. The middle patellar ligament is identified and followed proximally to the distal aspect of the patella. The clinician should feel the femoropatellar joint capsule between either the middle and medial or the middle and lateral patellar ligaments and should determine the presence of effusion. In horses with osteochondritis dissecans (OCD), fluid distention can be pronounced. However, normal young horses (weanlings to early 2-year-olds) often have prominent bilateral fluid distention of the femoropatellar joint capsules.
The clinician should find the medial patellar ligament and follow it proximally and distally. At the proximal extent, the medial fibrocartilage of the patella can be felt medial to the medial trochlear ridge of the femur. It is this normal arrangement of the medial aspect of the patella and the medial trochlear ridge that allows the veterinarian to determine whether a horse has patellar luxation. The position of the patella is difficult to confirm if the horse is standing with the stifle flexed. True patellar luxation is rare. The examiner should determine if the medial patellar ligament is enlarged, which usually reflects previous desmotomy or dermoplasty. Usually a distinct depression is present between the medial patellar ligament and the medial collateral ligament, but effusion of the medial femorotibial (MFT) joint may result in a substantial “bulge” (Figure 6-24). This may be the only clinical sign indicative of MFT joint injury.

Fig. 6-24 The medial femorotibial joint (right stifle, cranial view) is the most common location for osteoarthritis of the stifle joint and is palpated medially (needle in joint) between the medial patellar ligament and the medial collateral ligament. Normally a depression is present at this location, but a bulge from effusion can be palpated in this horse.
The lateral and middle patellar ligaments are palpated from their origin to insertion. Patellar desmitis is unusual but does occur; it usually involves the middle patellar ligament and may cause mild swelling. Previous injection with counterirritants causes firm, fibrous areas over the patellar ligaments, a common finding in racehorses. Gently rocking the horse from side to side to assess motion of the patella may give some indication of the potential for intermittent upward fixation of the patella (IUFP). In horses prone to IUFP, jerky rather than the normal smooth motion of the patella sometimes is detected.2 The lateral femorotibial (LFT) joint capsule is accessed between the lateral patellar and lateral collateral ligaments, but even with severe effusion it may be difficult to palpate. Overlying and adjacent soft tissue structures obscure palpation. Effusion of the LFT joint, although rare, is an important palpation finding that should be investigated carefully.
Deep palpation of the medial collateral ligament and the medial patellar ligament with the limb in flexion may elicit a pain response in horses with stifle lameness, but it probably is not specific for the source of pain in the stifle. The medial collateral stress test is perhaps the most reliable manipulative test of the stifle, although horses with lower limb lameness also may respond. With the leg in partial flexion, the shoulder or one hand is used as a fulcrum on the lateral aspect of the stifle, and the distal extremity is pulled laterally, thus placing valgus stress on the stifle (Figure 6-25). Care should be taken because horses may resent this manipulative test. If possible, the valgus motion should be applied by using the shoulder as a fulcrum and both hands on the crus, thus eliminating possible false-positive results from the lower limb. Patellar manipulation may cause a pain response, particularly in horses with femorotibial joint disease. During this procedure, caudal movement of the femur also may exacerbate cruciate injuries. With the limb on the ground in a weight-bearing position, the clinician’s hand is placed on the distal aspect of the patella, and the patella is forced upward (Figure 6-26). Theoretically during this test, numerous movements of the stifle are induced. The patellar ligaments are stretched, the patella is forced proximally, and on release the patella rapidly moves distally against the trochlear ridges, and the femur is forced caudally. Tests to assess cruciate ligament damage have been described but are dangerous to perform, and I have not found them particularly useful.10 Complete tearing of the cruciate or collateral ligaments is rare, and partial tearing does not cause clinically detectable instability. In horses with severe lameness and gross stifle instability, it is obvious that the stifle is the source of lameness, and pain usually prohibits manipulation.

Fig. 6-25 The valgus stress test of the stifle is difficult to perform and is accomplished by using a hand (shown) or shoulder as a fulcrum. This test can be done during static examination or a provocative test followed by trotting (see Chapter 8).
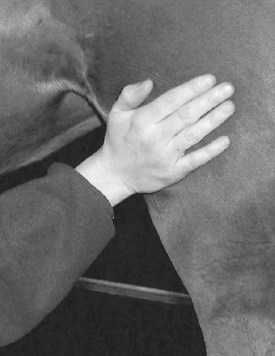
Fig. 6-26 Used as a static or provocative test, patellar manipulation is performed by placing the palm of the hand over the cranial aspect of the patella and manually forcing the patella proximally several times in succession. This maneuver can exacerbate pain from conditions of the patella and femoropatellar joint and forces the distal femur in a caudal direction. Pain from soft tissue injuries such as patellar, cruciate, or collateral ligament tears and osteoarthritis of the femorotibial joints can be exacerbated, but false-negative and false-positive results are common.
(Courtesy Carolyn Arnold, College Station, TX.)
Crus
The examiner should palpate the crus using both hands with the limb bearing weight. Subtle swelling of the medial aspect of the tibia can be palpated, but palpation of the caudolateral aspect of the tibia, the area in which stress fractures are diagnosed most frequently, is limited. Often no palpable abnormality is associated with a stress fracture. Any small wound or any form of swelling should be thoroughly investigated for the possibility of underlying bone damage, such as an occult tibial fracture. The veterinarian should palpate the caudal soft tissues. Proximally, the musculotendonous junction of the gastrocnemius muscle is a rare site of pain. The common calcaneal tendon is assessed. Swelling may indicate damage to any one of the contributing tendons. Effusion of the tarsal sheath causes swelling just proximal to the tarsus, at the caudal aspect of the crus, and should be differentiated from bog spavin. Deep palpation of the medial and caudal aspects of the crus is performed with the limb elevated (Figure 6-27). Horses with tibial stress fractures or those with spiral fracture or other tibial trauma may show a pain response, but false-positive responses are frequent. Tibial percussion, performed medially by using a clenched fist (knuckles) as a hammer, may elicit a pain response in horses with stress fractures, but many normal horses resent this test.
Tarsus
Five common swellings of the hock are important to differentiate, but hock swelling is not synonymous with hock pain. Capped hock is swelling located at the point of the hock (the proximal aspect of the calcaneus) and usually is an incidental finding, but in some horses the condition does cause lameness (Figure 6-28). The most common form involves the development of firm, fibrous subcutaneous tissue in the false bursa that lies over the point of the hock. This is a common area for abrasions and excoriation, and fibrous tissue formation results in a blemish but usually no lameness. Horses may be sensitive to palpation if the area has been traumatized recently. Infection or trauma leading to osteitis of the calcaneus can cause a clinically important capped hock and severe lameness. In these horses the problem involves the calcaneal bursa, located between the common calcaneal tendon and the calcaneus. If surrounding soft tissue swelling is minimal, fluid distention of the calcaneal bursa may be felt by ballottement. The bursa can be felt both medially and laterally at the proximal aspect of the calcaneus. Lateral, or less commonly, medial dislocation (luxation) of the SDFT results in similar swelling, but in an acute situation, lameness is present. Careful palpation may reveal the SDFT coursing laterally (Figure 6-29), unless excessive soft tissue swelling is present.

Fig. 6-28 Capped hock, a firm fibrous swelling of the proximal aspect of the calcaneus (point of the hock), is considered a blemish, but with effusion of the calcaneal bursa (not shown), lameness is substantial.

Fig. 6-29 Lateral dislocation (luxation) of the superficial digital flexor tendon. Instead of attaching to the tuber calcanei, the superficial digital flexor tendon (arrows) is now located lateral to the point of the hock. Initial swelling makes this diagnosis difficult.
Effusion of the tarsal sheath, thoroughpin, must be differentiated from bog spavin (see following text). Tarsal tenosynovitis causes swelling both medially and laterally in the depression between the calcaneal tendon and the caudal aspect of the tibia (Figure 6-30). With severe effusion of the tarsal sheath, fluid distention can be palpated distal to the hock on the medial aspect. Thoroughpin usually is an incidental finding, seen most commonly in Western performance horses, but acute lameness accompanied by tarsal tenosynovitis can indicate strain or injury of the sheath, often associated with adjacent bony injury. Unusually, swelling in the distal, caudal aspect of the crus identical to that seen with classic thoroughpin is seen, but communication with and concomitant swelling of the tarsal sheath are absent.

Fig. 6-30 Thoroughpin, swelling located in the distal, caudal aspect of the crus, usually is caused by distention of the tarsal sheath and must be differentiated from effusion of the plantarolateral pouch of the tarsocrural joint (bog spavin).
The term spavin refers to “any disease of the hock joint of horses in which enlargements occur, often causing lameness … the enlargement may be due to collection of fluids or to bony growth.”11 Bog spavin is fluid distention of the tarsocrural joint capsule. The tarsocrural joint has four outpouchings: dorsolateral, dorsomedial, plantarolateral, and plantaromedial. All joint pouches may be distended, although the dorsomedial and plantarolateral pouches are large and most prominent (Figure 6-31). With ballottement, fluid can be pushed between pouches on the dorsal or plantar aspects, thus differentiating this condition from thoroughpin.

Fig. 6-31 Moderate-to-severe tarsocrural effusion, bog spavin, in this draft filly was caused by osteochondritis dissecans of the cranial intermediate ridge of the distal aspect of the tibia. Distention of the large dorsomedial pouch and swelling of the dorsolateral, plantarolateral, and plantaromedial pouches was present.
Bone spavin refers to fibrous and bony swelling that results from chronic osteoarthritis of the proximal intertarsal, centrodistal, and tarsometatarsal joints. This swelling usually is seen in older horses and can be palpated and observed on the medial side of the hock (Figure 6-32). Although the bony enlargement is the result of proliferation, it does not necessarily mean that the horse is lame as the result of the condition. Most horses with distal hock joint pain do not have palpable enlargement medially, and based on radiological evaluation, the most common area of proliferation and bony change is the dorsolateral aspect of the joints. Blood spavin is an old term usually meaning enlargement of the saphenous vein,3 but it also may have been used to describe a prominent saphenous vein in horses with bog spavin. Saphenous distention is rare, and the term is not used today. Occult or blind spavin is an obsolete term used to describe horses with clinical signs of hock lameness but no observable bony swelling.3 High spavin is also an obsolete term used to describe bone spavin located close to the tarsocrural joint.3
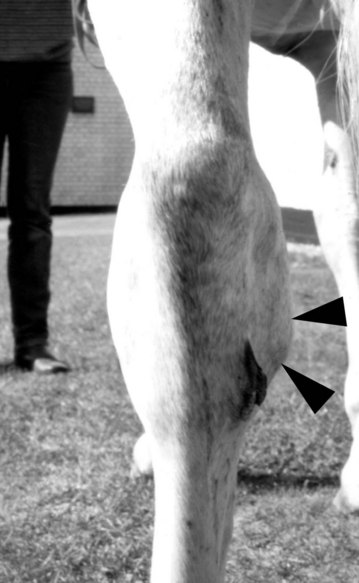
Fig. 6-32 Bone spavin (arrows), fibrous and bony swelling on the medial aspect of the distal hock joint (left hindlimb) caused by chronic osteoarthritis of the distal hock joints, sometimes appears in older sports horses but is rare in young racehorses. The presence of bone spavin should be noted, and this area should be palpated carefully, but horses can have distal hock pain without bone spavin, and horses with bone spavin can have lameness elsewhere in the limb. Previous cunean tenectomy causes chronic fibrosis in this region.
Curb describes swelling along the distal, plantar aspect of the hock and has often erroneously been blamed on long plantar desmitis. In most horses the swelling is actually enlargement of the SDFT or subcutaneous tissues. The swelling is often firm, but in some horses subcutaneous fluid can be present (see Figure 78-1). In horses with acute severe injury the swelling may feel soft and mushy. In some normal horses the proximal aspect of the MtIV is prominent and should not be confused with curb.
Swelling restricted to the medial or lateral aspect of the hock may reflect collateral ligament injury. Localized heat on the medial aspect of the hock or on the proximal aspect of the metatarsal region may be an important finding.
The Churchill Hock Test
The Churchill hock test was developed by Dr. E.A. Churchill in the 1950s as a rapid, noninvasive, specific method to screen and identify distal tarsal pain in athletic horses. Although the test has been used by Dr. Churchill and me primarily in STBs, TBs, endurance horses, and Three Day Event horses, it is equally reliable when applied to other equine athletes.
Digital pressure is applied on the plantar aspect of the head of the second metatarsal bone (MtII) and fused first and second tarsal bones with the limb in a non–weight-bearing position. Abduction of the limb is a positive response. To examine the left tarsus, the clinician approaches the horse facing caudally. The left hindlimb is picked up and brought forward, supported by the clinician’s right hand cupped under the fetlock or hoof. Holding the limb so that the hoof is approximately 25 to 30 cm above the ground is most comfortable for the horse. The heel of the left hand is positioned on the proximodorsal surface of the third metatarsal bone (MtIII) while the third phalanges of the index and middle or middle and ring fingers are placed around the medial side of the tarsus to engage the bony ridge formed by the head of the MtII and the first and second tarsal bones (the area of insertion of the cunean tendon) (Figure 6-33). The thumb is rested on the dorsal lateral aspect of the tarsus and the proximal aspect of the MtIII. Gentle, firm pressure is applied to the bony ridge by flexing the phalanges of only the index and middle fingers (Figure 6-34). The hand does not squeeze the hock. Pressure is applied three times approximately 1 second apart, each time with increasing intensity to a maximum effort on the third time.

Fig. 6-33 Correct left hand placement in the left proximal metatarsal region to perform the Churchill hock test.
(Courtesy Dan L. Hawkins, Gainesville, FL.)

Fig. 6-34 The Churchill test is demonstrated on an anatomy specimen. The index and middle fingers are flexed and positioned on the bony ridge formed by the third metatarsal bone and the fused first and second tarsal bones, and the heel of the hand rests on the proximodorsal aspect of the third metatarsal bone. The thumb rests against the dorsolateral aspect of the tarsus.
(Courtesy Dan L. Hawkins, Gainesville, FL.)
Proficiency requires patience and routine practice. Consistent diagnostic information can be obtained safely from more than 90% of fit racehorses. If the limb cannot be picked up, the test cannot be performed. Fussing and repeatedly flexing the hock and limb in an agitated manner while the procedure is performed should not be misinterpreted as a positive response.
The Churchill hock test is useful for horses that are not visibly lame but for which the trainer or rider has a complaint that the horse is doing something uncharacteristic during work or competition associated with decreased performance. The horse may have a changed attitude toward work, lugs in or out, is rough in the turns, refuses to change leads, stops at jumps, jumps to one side, or is stiff going in one direction. Although these horses cannot be blocked out at a slow gait, the Churchill hock test may suggest the presence of distal hock joint pain.
Saphenous Filling Time
The veterinarian should assess the saphenous vein filling time. Blood flow in the saphenous vein is prevented using digital compression in the proximal metatarsal region, and the blood accumulated in the vein over the tarsocrural joint is pushed proximally to completely collapse the vein. The finger compressing the vein distal to the hock is then removed, and the time it takes for the saphenous vein to fill is observed. Normally, it takes less than 1 second for the vein to fill, but in horses with reduced circulation, prolonged filling time is seen. Pulse quality of the dorsal metatarsal artery, located on the dorsolateral aspect of the MtIII just dorsal to the fourth metatarsal bone (MtIV), can be useful, especially if the history suggests lameness is caused by vascular compromise. The arterial pulse quality is compared with that in the contralateral limb.
Metatarsal Region
The veterinarian should palpate the digital flexor tendons and SL. Tendonitis is unusual in the hindlimb, but occasionally SDF tendonitis occurs in the proximal metatarsal region. This is most common in horses with curb, and tendonitis progresses distally to involve the metatarsal area. The hock angle is evaluated carefully. Occasionally horses with severe curb or those with SDF tendonitis of the metatarsal region have a reduced hock angle (obvious unilateral sickle-hocked conformation), indicating loss of support in the SDFT. Once a general palpation for the presence of heat, swelling, and exostoses associated with the MtIII, the MtII, the MtIV, and the proximal aspect of the DFTS has been completed, the limb is lifted and deep palpation is performed. The clinician should carefully palpate the origin and body of the SL, keeping in mind that both false-positive and false-negative responses can occur (Figure 6-35). Much of the palpation of the SL laterally is indirect, because the MtIV hides the origin and proximal aspect of the body. Because the presence of the splint bones and dense metatarsal fascia prevents substantial swelling, or at least the clinical recognition of swelling of the SL, even mild swelling in the proximal, medial metatarsal region should be carefully interpreted. With the limb in flexion, the axial borders of splint bones are palpated. The dorsal aspect of the MtIII should also be assessed with the limb in flexion, because bony injury of the MtIII does occur and includes dorsal cortical trauma from external injury or interference, dorsal cortical and spiral fractures, and proximal dorsolateral fractures.

Fig. 6-35 Deep palpation of the proximal aspect of the suspensory ligament can be performed only with the limb in flexion. The close association of the suspensory origin to the Churchill site explains the need to differentiate proximal plantar metatarsal pain from distal hock joint pain using diagnostic analgesia.
(Courtesy Howard “Gene” Gill, Pine Bush, New York.)
Metatarsophalangeal Joint
Many of the common problems of the metatarsophalangeal (MTP) joint, such as short, midsagittal fractures of the proximal phalanx, sesamoiditis, maladaptive or nonadaptive remodeling of the MtIII, and osteochondrosis, cause very few clinical signs, and although palpation is quite important, diagnostic analgesia is often needed to localize pain to this area. Nonetheless, careful palpation of the fetlock region is mandatory. Some horses have concurrent MTP joint and stifle pain, and when suspicious findings exist in one site, the veterinarian should look carefully at the other for additional, secondary, or complementary problems.
The MTP or hind fetlock joint is evaluated with the limb bearing weight and in flexion. The clinician should assess the MTP joint capsule and the DFTS for the presence of effusion or fibrosis (Figure 6-36). Incidental effusion of both the MTP joint and the DFTS is common in the hindlimb of older performance horses; therefore this finding should not be overinterpreted. In younger horses, particularly racehorses, the presence of effusion can be an important clinical sign associated with osteoarthritis or other problems and should be interpreted accordingly. The clinician should carefully palpate for the presence of heat and mild swelling over the surface of both PSBs, subtle but important signs of sesamoiditis. Sesamoiditis is more prevalent in the hindlimb but can be difficult to detect, and advanced imaging often is necessary for diagnosis. The digital pulse amplitude should be assessed.

Fig. 6-36 The metatarsophalangeal joint region often is overlooked during lameness examination. This joint should be palpated carefully with the limb in the standing and flexed (shown) positions.
(Courtesy Ross Rich, Cave Creek, Arizona.)
With the fetlock joint in flexion, the veterinarian should palpate the proximal, dorsal aspect of the proximal phalanx for the presence of pain or exostoses (Figure 6-37) and should apply pressure to the PSBs, avoiding aggressive compression, which may cause false-positive results. The range of motion of the MTP joint is noted.

Fig. 6-37 Palpation of the proximal, dorsal aspect of the proximal phalanx can elicit pain in horses with incomplete mid-sagittal fracture of the proximal phalanx. In trotters, interference injury from the ipsilateral front foot causes pain and swelling in this region.
(Courtesy Ross Rich, Cave Creek, Arizona.)
Pastern
When the limb is elevated, the reciprocal apparatus causes constant flexion of the digit, which makes palpation of the plantar aspect of the pastern exceedingly difficult. Subtle swelling in the plantar aspect of the pastern is easy to miss. Bony and soft tissue structures should be palpated with the horse in the standing position, and the veterinarian should note the same clinically important areas that were pointed out for the forelimb. High and low ringbone (osteoarthritis of the proximal interphalangeal and distal interphalangeal joints, respectively), osteochondrosis of the pastern joint, and soft tissue problems such as SDF branch tendonitis, distal sesamoidean desmitis, and plantar injury of the pastern joint occur, but with reduced frequency when compared with the forelimb.
Foot
A similar approach to the evaluation of the hind foot as that described for the front foot is used. I spend considerably less time evaluating the hind foot than the front foot, unless the history or horse type dictates otherwise, because this area is relatively infrequently the source of pain. In the draft horse, hind foot pain is as common as in the forelimb, and therefore the hind feet merit considerable attention. Unless specifically indicated by the lameness history, or the horse is severely lame without an obvious cause in the upper limb, I do not routinely perform a hoof tester examination of the hind feet. Pressure with hoof testers over the frog and across the heel in a hind foot often causes a false-positive response in normal horses. The position needed to perform an unassisted hoof tester examination in the hindlimb can be dangerous. The presence of an assistant to elevate the limb may obviate some of the risk.
The examiner should assess the shape, balance, and contour of the foot and observe the shoe (or lack of one) carefully. Hoof angle in the hindlimb ranges from 48 to 58 degrees, and the hoof and pastern axis should be straight. A common finding is a low or underrun heel. An interesting relationship between a low heel and the presence of PSD has been noted.2 In these horses a lateral radiographic image of the foot shows that the plantar aspect of the distal phalanx is lower than the dorsal aspect.2 Shoe wear is extremely important in the hindlimb and can give clues to the source of lameness. For instance, horses with distal hock joint pain tend to stab the lower hindlimb during advancement, causing excessive wear of the lateral branch of the shoe (Figure 6-38). Other causes of lower hindlimb lameness, such as osteoarthritis of the MTP joint, can cause a similar gait, but usually abnormal shoe wear is less pronounced. Horses with stifle lameness often wear the medial branch of the shoe. The presence of heel and toe caulks or borium causes additional shear stress on many of the lower limb joints and can exacerbate lameness.

Fig. 6-38 It is imperative to observe the hind shoes for wear during lameness examination. This right hind shoe (lateral is to the right) has wear along the dorsal and lateral aspects (lateral aspect of toe grab and fullering are worn) consistent with a lower hindlimb lameness, such as distal hock joint or proximal metatarsal region pain.
The Role of Physical Examination in the Lameness Examination
Body temperature may assist with a clinical diagnosis. The normal temperature range is 37.5° to 38.6° C (99.5° to 101.3° F), although in a foal the upper limit may normally be slightly higher. Body temperature in foals rises more abruptly than in adult horses in response to stress, infection, and inflammation. Thus transport of a foal may cause transient low-grade pyrexia, but fever in an adult horse after transport is abnormal. Localized infection in a foal usually causes pyrexia but rarely does so in an adult. The examiner should not exclude infectious arthritis in an adult horse simply because fever is not present. However, adult horses usually are pyrexic during the early stages of cellulitis or lymphangitis.
Elevation in the pulse and respiratory rates often accompanies severe lameness because of pain. Systemic diseases such as endotoxemia may cause abnormal vital parameter findings in any horse and can lead to conditions such as laminitis.
It is important to remember that diseases of other body systems can cause clinical signs that mimic lameness or cause true gait deficits. For instance, abnormal or stiff gaits can be seen in horses with pleuritis and peritonitis, abdominal, sublumbar, inguinal, thoracic inlet, and pectoral abscesses or tumors. Proliferative new bone associated with hypertrophic osteopathy may be associated with a thoracic or abdominal mass. If an unusual situation arises, the veterinarian should step back and think of the exception rather than the rule, because the “red herring” may be just around the corner.