Chapter 24 Tenoscopy and Bursoscopy
The advantages of arthroscopy as a diagnostic and therapeutic approach to joints1 have prompted the development of applications for other synovial cavities (see Chapter 23). Tenoscopy is the term used to describe endoscopy of synovial tendon sheaths, usually using a rigid arthroscope.2 Bursoscopy is used for endoscopy of bursae.
Tenoscopy has many advantages. Traditional approaches to tendon sheaths, requiring long incisions over highly mobile areas, are associated with substantial postoperative risks, including wound dehiscence and ascending sheath infection.3 These techniques are invasive, time consuming, and offer limited visibility of tendovaginal structures.2,3 Endoscopic approaches to the carpal tunnel in people have been described4,5 and have provided substantial improvements in terms of decreased morbidity, scarring, and loss of function compared with open techniques.4,6 Tenoscopy in the horse was first described for the examination of the digital flexor tendon sheath (DFTS).1,2 Since the early 1990s, other applications have been described.7-11
General Principles of Tenoscopy and Bursoscopy
Equipment
Standard arthroscopic equipment is used, including arthroscope, sleeve, and obturators; arthroscopic cannulae; probes; grasping forceps; and Ferris-Smith rongeurs. Sharp tenotomes, curettes, and meniscectomy scissors should also be available. A standard 4.0-mm, 25- to 35-degree forward angle arthroscopic endoscope is adequate for most sheaths and bursae, although thinner endoscopes may be useful for extensor sheaths. Light source and video camera apparatuses are as for arthroscopy. Motorized synovial resectors are particularly useful because debridement or synovectomy using hand-operated instruments can be tedious in large tendon sheaths.
Coblation technology (ArthroCare Corporation, Austin, Texas, United States) is a new technology that uses radiofrequency to vaporize soft tissues. I now use radiofrequency probes (Arthrowands, ArthroCare Corporation) to remove proliferative synovial tissue and masses, and a hook radiofrequency blade (Saber 30, ArthroCare Corporation) to carry out annular or retinaculum desmotomy. An added advantage is improved hemostasis.
Surgical Principles and Techniques
The basic principles of arthroscopy are also valid in tendon sheaths and bursae (see Chapter 23). The sheath usually is distended with fluids to facilitate insertion of the cannula. However, this is not necessary for the carpal and tarsal sheaths, which are not approached through distended pouches.9,10 It is generally recommended that the portal be created with a scalpel and the cannula inserted using a blunt, conical obturator to avoid damaging the tendons. A thorough knowledge of the normal endoscopic anatomy of the sheath is paramount for several reasons. First, all the surfaces are covered by synovium and look alike, making identification of the structures difficult. Second, normal anatomical structures such as vinculae and plicae (adhesion-like formations carrying blood vessels to the tendon from the parietal sheath), endotendon (reflection of the synovial membrane, which forms a continuous band attaching the tendon to the sheath along its length), and synovial folds are apparent. These should not be damaged because they participate in the blood supply of tendons within the sheathed portion.12-14
Triangulation techniques are applied for instruments using separate portals. These should be created as close as possible to the lesion, although the shape of the sheath often dictates the position of the portals. The longitudinal arrangement of the sheaths and tunnel-like enclosures within retinacula often make triangulation difficult; therefore it may be useful to perform retinaculum desmotomy to improve access to some lesions, or to create instrument portals so that instruments are inserted opposite and toward the endoscope lens.
Tenoscopy
Tenoscopy of the Digital Flexor Tendon Sheath
The DFTS is the most common site of tenosynovitis. Endoscopy is indicated as a diagnostic procedure to examine lesions of the surfaces of the deep digital flexor tendon (DDFT), superficial digital flexor tendon (SDFT), and parietal surface of the sheath. High-definition ultrasonography allows noninvasive examination of the sheath, its contents, and peripheral tissues, and provides more accurate information about the internal architecture of tendons.15 However, differentiating some adhesions, tears, and superficial fraying of the tendons may be difficult ultrasonographically.16-19 Tenoscopy is useful for debridement of masses, such as proliferative (villonodular) synovitis-like lesions and other lesions within the sheath, adhesiolysis, removal of debris, and synovectomy in infectious tenosynovitis.2,19,20 A technique for desmotomy of the palmar annular ligament under endoscopic control has been described to avoid inadvertent damage to the tendons, manica flexoria, and other peritendovaginal structures.21
The advantages of tenoscopy over traditional open surgery are similar to those recognized for arthroscopy over arthrotomy. They include decreased morbidity and more rapid return to normal function of the sheath and reduced risks of complications, such as wound breakdown, infection, fibrosis, and ankylosis.
Anatomy
The DFTS is organized primarily around the DDFT, which it completely surrounds from the junction between the third and distal quarters of the metacarpal or metatarsal region to the level of the proximal interphalangeal joint, before tapering dorsally to the DDFT to the proximal border of the distal sesamoid bone.12,13,15,22 At the level of the metacarpophalangeal joint, the DFTS also surrounds the SDFT, except for a wide mesotendon over the palmar/plantar aspect of the tendon. At this level the DFTS is bound dorsally by the proximal scutum, a fibrocartilage covering the palmar (plantar) surfaces of the proximal sesamoid bones (PSBs) and intersesamoidean ligament, and palmarly by a tough transverse ligament, the palmar (plantar) annular ligament (PAL), thus forming a nonelastic canal through which both digital flexor tendons run independently. In the pastern region the SDFT separates into two branches and is no longer within the DFTS. The DFTS is bound dorsally by the distal sesamoidean ligaments and palmarly (plantarly) by two broad digital annular ligaments.
The proximal pouch bulges when distended proximal to the PAL and PSBs and contains a number of long villi in normal horses. Several small, subcutaneous pouches appear between the insertions of the PAL and digital annular ligaments abaxially and over the palmar (plantar) aspect of the DDFT in the midpastern region. A number of vascular structures are found, including two large vinculae forming a V-shaped adhesion-like structure between the dorsal surface of the DDFT and the dorsal sheath wall in the proximal pastern. Densely packed villi often are found in that area. The wide palmar mesotendon prevents examination of the palmar aspect of the SDFT in the fetlock region. Immediately proximal to this level, the manica flexoria forms a smooth, thin membrane originating from the axial surfaces of the SDFT and surrounding the DDFT dorsally.
Surgical Technique
The technique for tenoscopic exploration of the DFTS has been described in detail.2 The term palmar is used in the following description for either palmar or plantar. The horse may be placed in lateral recumbency with the affected limb uppermost for a lateral approach or lowermost for a medial approach. The choice of a lateral or medial portal is dictated by the site of the suspected lesion. However, if no definite lesion has been observed ultrasonographically and if a potential tear is suspected, the horse is best placed in dorsal recumbency with the limb attached to a frame or hoist so that the digit is in slight flexion. This decreases hemorrhage during the procedure. An Esmarch bandage and tourniquet may also be used.
The DFTS is distended with 10 to 20 mL of physiological solution through a needle inserted in the palmar aspect of the midpastern region. Overdistention of the DFTS is avoided because it causes flexion of the digit. A 5-mm longitudinal incision is made through the skin, immediately distal to the PAL, lateral or medial to the DDFT, and 0.5 to 1 cm palmar to the neurovascular bundle, which must be carefully avoided. A stab incision is made into the DFTS, taking care to avoid damaging the DDFT, and the cannula, with a conical obturator inserted in a proximal direction, between the DDFT and dorsal sheath wall (Figure 24-1). The DFTS is lavaged through an 18-gauge needle inserted in the proximal pouch. The obturator is replaced with the endoscope, and examination is carried out from proximal to the level of the portal by rotation and gradual withdrawal. The proximal pouch is examined, followed by the abaxial aspects of the two tendons. Flexion of the fetlock joint allows insertion of the endoscope between the SDFT and DDFT without damage to the manica flexoria. The endoscope is finally rotated around the SDFT on the side of the portal to inspect the mesotendon. Examination of the opposite side is made possible by flexion of the fetlock and rotation of the arthroscope window palmarly.
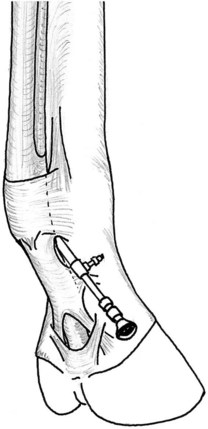
Fig. 24-1 Digital sheath tenoscopy. The arthroscope is inserted lateral to the deep digital flexor tendon, immediately distal to the palmar annular ligament.
The endoscope is then pushed across the DFTS, between the DDFT and dorsal sheath wall, to avoid exiting the DFTS. The endoscope is then redirected distally. The distal part of the DFTS is examined by gradual withdrawal of the endoscope. The vinculae are visible in the proximal pastern region, between the dorsal surface of the DDFT and dorsal wall (Figure 24-2). Palmarly and farther distally, bifurcation of the SDFT branches forms a manica-like ring around the DDFT (Figure 24-3).

Fig. 24-2 Tenoscopic view of the dorsal aspect of the deep digital flexor tendon (DDFT) in the proximal pastern region, showing one of the vinculae (V) between the DDFT and dorsal wall (Sh) of the digital flexor tendon sheath.
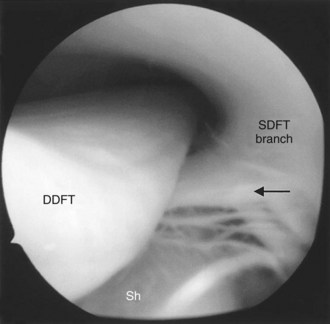
Fig. 24-3 Tenoscopic view of the palmar aspect of the deep digital flexor tendon (DDFT) in the proximal pastern region, showing the manica-like ring (arrow) surrounding the DDFT, between the two superficial digital flexor tendon (SDFT) branches (within the abaxial sheath walls). The dorsal wall (Sh) of the digital flexor tendon sheath is rich in long villi.
Debridement of potential lesions is carried out through separate instrument portals made as close as possible to the lesion to allow for adequate triangulation. At the end of surgery the DFTS is lavaged through a large-bore cannula, and the skin incisions are closed. It is recommended that a pressure bandage be applied for 2 weeks postoperatively. In horses with infection with substantial debris accumulation, it is possible to place a drain, exiting in the distal palmar recess through a separate incision. A drainage portal may also be created in the distal palmar aspect of the DFTS to allow for continuous drainage postoperatively. The incision is then left to heal by contraction and epithelialization.
A technique for transection (desmotomy) of the PAL under endoscopic guidance was described,18,20 using a desmotomy kit designed for palmar carpal ligament transection in people.4,5 This permits adequate examination of the DFTS before PAL transection and prevents inadvertent damage to the tendons and manica flexoria. Although the use of a specific cannula facilitates the procedure, I use a grooved director for the same purpose. A radiofrequency hook blade (Saber 30, ArthroCare Corporation) facilitates the technique because there is minimal hemorrhage and less risk of inadvertent damage to peripheral structures and tendons during insertion and manipulation of the knife.
I have used an alternative technique for digital tenoscopy using an endoscopic portal made proximal to the PAL and dorsolateral to the DDFT. This technique allows adequate examination of the entire DFTS, is useful to examine lesions in the proximal phalangeal region, and provides improved triangulation when surgically treating such lesions. Using a wound as an initial endoscopic portal is often possible, although creating a new endoscope portal and using the wound for instruments is usually preferable after examination is completed.
Postoperative Care
At the end of surgery the DFTS is emptied of fluid and the skin portals are closed with staples or sutures of the surgeon’s choice. Damage to the neurovascular bundle by needles and sutures is carefully avoided. The horse recovers with the limb in a pressure bandage from the foot to the distal aspect of the carpus (or tarsus) to prevent DFTS swelling and to reduce motion. Postoperative antibiotics are only necessary in horses with infectious tenosynovitis, but systemic nonsteroidal antiinflammatory drugs (NSAIDs) should be given for several days after surgery. The horse should be restricted to box rest for 3 days, and then it may be walked out in hand to decrease restrictive adhesion formation. Box stall rest with controlled exercise should be continued for 2 weeks until the sutures are removed, and then at the surgeon’s discretion exercise is increased progressively. Hyaluronan has been advocated as an adjunctive therapy2,17 but should be avoided if infection is present. Passive limb motion with repeated flexion/extension of the fetlock helps reduce stiffness in the initial stages. Cold hosing of the limb is useful to decrease potential swelling and hemorrhage after handwalking.
Tarsal Sheath
Injuries to the tarsal sheath are relatively common (see Chapter 76). Open surgery has been associated with a high rate of postoperative complications,3,10,24 but early results indicate that the morbidity may be greatly reduced with tenoscopy.10
Anatomy
The tarsal sheath is the sheath of the lateral digital flexor tendon (LDFT), the largest of the two tendons (lateral and medial digital flexor tendons), the fusion of which in the proximal metatarsal region forms the DDFT (see Chapter 76).10,22,25 It is paramount to recognize the anatomical location of the plantar nerves and vessels that pass within the plantar flexor retinaculum and the presence of a continuous mesotendon, passing longitudinally along the plantaromedial aspect of the LDFT. However, accidental damage to these structures does not appear to have major consequences.
Surgical Technique
A technique allowing examination of the entire tarsal sheath has been described.10 Previous distention of the tarsal sheath is not necessary. The medial edge of the sustentaculum tali and medial insertion of the retinaculum are located, and an 8-mm vertical incision is made in the skin and underlying fascia, 8 mm plantar to the edge of the bone at the point where the tendon changes direction over the sustentaculum tali. The absence of blood vessels in the retinaculum deep to the incision is ascertained using hypodermic needles before making a 5-mm stab incision through the retinaculum. Care is taken to avoid damage to the underlying LDFT. The endoscope sleeve and conical, blunt obturator are inserted dorsal to the LDFT in a proximal direction. The obturator is replaced with an endoscope; the tarsal sheath is distended moderately with fluid; and examination is carried out as described for the DFTS by rotation of the window of the arthroscope and gradual withdrawal. After examination of the proximal half of the tarsal sheath, the endoscope is redirected into the distal pouch. The proximal pouch is large and lined by a thin wall (Figure 24-4, A). Muscle fibers from the lateral digital flexor muscle and separate head of the tibialis caudalis muscle may be seen by transillumination through the synovial membrane. Within the tight, rigid canal formed by the sustentaculum tali and retinaculum, the fibrocartilage appears glistening white, and small vessels are seen within the parietal membrane plantarly and in the mesotendon. In the distal half of the tarsal sheath, a fold of synovial membrane forming a small, blind pouch medially is seen dorsomedial to the LDFT at the level of the tarsometatarsal joint (Figure 24-4, B). Distal to this fold, the tarsal sheath continues as a cylindrical, blind recess dorsal to the tendon and contains small villi. The separate sheath of the medial digital flexor tendon is not visible from the tarsal sheath.
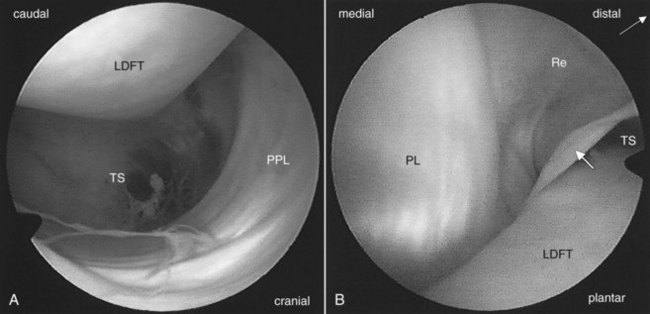
Fig. 24-4 Tenoscopic views of the tarsal sheath. A, Proximal pouch of the tarsal sheath (TS) showing the cranial aspect of the lateral digital flexor tendon (LDFT) and the proximal plantar ligament (PPL) thickening of the plantar capsule of the tarsocrural joint. B, Distal recess of the tarsal sheath (TS). At the tarsometatarsal joint, the end of the plantar ligament (PL) is visible. A synovial fold (white arrow) forms a small recess dorsomedially (Re).
If a wound exists, most commonly at the plantaromedial edge of the sustentaculum tali, it may be used as an endoscope portal. Instruments may be inserted as required close to lesions to allow for triangulation. Needles are used to determine the optimal location for the instrument portal.
Carpal Sheath
Tenosynovitis of the carpal flexor tendon sheath (carpal sheath) is relatively rare in horses but can cause severe lameness associated with carpal canal syndrome (see Chapter 75). Wounds leading to contamination of the carpal sheath are rare but possible. Common causes of noninfectious tenosynovitis include lesions of the SDFT in the carpal region, fractured accessory carpal bone, osteochondromata of the caudal distal aspect of the radius, exostoses of the caudal perimeter of the distal radial physis, and sprain injuries to the carpal sheath,26-28 although other causes may exist.29 Effusion may be secondary to lesions outside the carpal sheath, such as desmitis of the accessory ligament of the DDFT (ALDDFT), accessory ligament of the SDFT (ALSDFT), limb edema, and unassociated wounds. Ultrasonography is the technique of choice for investigating carpal sheath distention, but adhesions and subtle fraying of the tendons may not be visible.28,30 Radiography is also mandatory to rule out fractures, exostoses, and osteochondromata.27-29,31
Tenoscopy may be useful as a diagnostic tool if lameness is associated with pain localized to the carpal sheath by intrathecal analgesia but where no lesions are visible with other imaging methods. The main indication for tenoscopy of the carpal sheath is debridement and repair of structures within the sheath or transection of the ALSDFT.
Anatomy
The anatomy of the carpal sheath has been described elsewhere in detail.14,21,30 Briefly, the carpal sheath is organized around the DDFT from the distal caudal aspect of the antebrachium, 4 to 7 cm proximal to the accessory carpal bone, to the metacarpal region. The carpal sheath extends around the DDFT and SDFT in the carpal region, where it is enclosed within a tight canal (the carpal canal) formed by a thick palmar carpal flexor retinaculum palmarly and medially, the accessory carpal bone laterally, and the palmar carpal ligament dorsally. At this level the SDFT is attached palmarly to the sheath wall by a thick mesotendon that contains the median artery and medial palmar nerve. A thinner mesotendon links the DDFT to the SDFT medially. Proximal to the carpal canal a large pouch occurs dorsal to the flexor muscles, bulging laterally and medially caudal to the radius if distended. Distal to the carpometacarpal joint the carpal sheath continues as a blind sack between the DDFT and ALDDFT and bulges dorsolaterally to the DDFT in the proximal third of the metacarpal area. The lateral palmar nerve and palmar veins pass within the retinaculum.
Surgical Technique
Several techniques have been described depending on the lesions identified before surgery. Removal of osteochondromata from the caudal distal aspect of the radius has been described using a lateral approach through the distended proximal pouch.8,33 The horse is anesthetized and placed either in lateral recumbency with the affected limb uppermost or in dorsal recumbency with the foot attached to a hoist, so that carpal position may be altered during the procedure. This latter position decreases hemorrhage, which may substantially decrease visibility. The carpal sheath is distended with 40 to 60 mL of balanced electrolyte solution, and the endoscopic portal is made between the lateral digital extensor and ulnaris lateralis tendons, 3.5 cm proximal to the distal radial physeal scar. The cannula and blunt obturator are inserted proximomedially into the carpal sheath. The instrument portal is made on the same side as the arthroscope portal, 2 cm distal to it. A medial approach has also been described but appears less practical because of the presence of the ALSDFT and the median nerve and artery.7
This lateral proximal approach is generally recommended for desmotomy of the ALSDFT and removal of osteochondromata or caudal radial physeal exostoses. Desmotomy of the ALSDFT is carried out easily via tenoscopy.32,33 This approach offers several advantages over the standard “open” medial approach: postoperative swelling is decreased, and the incidence of wound breakdown or seroma is nearly abolished. Intrathecal hemorrhage seems to be better tolerated than with the standard approach. Hence return to training is dramatically shortened (4 to 6 weeks). After insertion of the cannula through a portal 2.5 to 3 cm proximal to the distal radial physeal scar as described above, an instrument portal is created immediately proximal and caudal to the palpable physeal scar. The ALSDFT is easly identified by palpation with a blunt arthroscopic probe. In some horses, I use intraoperative ultrasonographic guidance to place needles at the proximal and distal borders of the ligament at the level of the flexor carpi radialis tendon. This also permits identification of the median artery and the small transverse artery, which are best avoided to reduce perioperative hemorrhage. The needles are used as landmarks for desmotomy. I use a radiofrequency hook blade (Saber 30, ArthroCare Corporation) as described for annular desmotomy, but the technique may also be performed using an arthroscopic hook blade, a tenotomy knife, or a No. 15 scalpel blade on a long No. 3 handle. After identifying the distal edge of the ligament, section is commenced at that level in a proximal direction and through the ligament until the sheath of the flexor carpi radialis tendon is entered. The section is continued proximally. The proximal quarter to third of the ligament is located outside the proximal boundaries of the carpal sheath, and this is where the transverse artery may be inadvertently severed. The radial head of the DDFT is reclined dorsally with the endoscope, and the desmotomy is continued until all identifiable fibers are severed. Using the coagulation setting on the coblation device during the procedure helps avoid hemorrhage. When the section is completed, the cut ends of the ligament separate, showing the large communication with the flexor carpi radialis sheath. There may be tremendous postoperative swelling of the carpal sheath and the flexor carpi radialis sheath; therefore it is recommended that a pressure bandage be placed over the carpal area (see below).
These techniques do not permit examination of the distal half of the carpal sheath. Therefore another technique has been developed to facilitate endoscopic examination of most of the carpal sheath.9 The horse may be placed in lateral recumbency with the affected limb uppermost or in dorsal recumbency with the affected limb suspended loosely, so that the carpus is slightly flexed. An 8-mm longitudinal skin incision is made without previous distention of the carpal sheath 1.5 to 2 cm distal to the distal border of the accessory carpal bone along the lateral aspect of the DDFT. A medial approach is not recommended because examination is restricted by the mesotendons and the risk of injury to the median artery and medial palmar nerve. A needle is used to ensure that no vessels are present in the fascia deep to the incision. The incision is extended with a scalpel through the fascia into the carpal sheath. The arthroscope is inserted proximally, between the DDFT and dorsal wall of the sheath. The proximal pouch is large and contains small villi. The radial head of the DDFT forms a conical prominence in the medial aspect of this pouch. Rotation of the endoscope and manipulation around the tendons allow examination of the DDFT and SDFT surfaces, caudal surface of the distal radius, and fibrocartilaginous sheath wall in the carpal canal. Minimal fluid pressure should be used to avoid flexion of the carpus. The endoscope may be inserted between the tendons to view the surfaces and the lateral aspect of the mesotendon, covered by short, thin villi. Redirecting the endoscope distally permits examination of the distal recess. A normal, longitudinal synovial fold appears dorsomedially in the carpal sheath in the distal carpal region. Instrument portals are made where necessary to allow for adequate triangulation.
Improved triangulation is obtained for removal of osteochondromata of the distal caudal radius with this method, although the endoscope may occasionally be too short.
Desmotomy of the carpal palmar retinaculum has been advocated for carpal canal syndrome associated with constriction syndrome or functional carpal ankylosis. The technique may be performed using tenoscopy.35 I use electrosurgery because hemorrhage is often marked, particularly because there is frequently substantial concurrent synovial swelling.
Postoperative care is similar to that described for other sheaths, but postoperative hemorrhage and swelling are very common in the carpal sheath. It may not be practical to apply a pressure bandage for any length of time over the carpus. I usually apply a pressure bandage for recovery from general anesthesia and then replace it after the horse stands. The limb remains bandaged for only 48 hours because of the risk of pressure sores. The horse must be restricted to stall rest for at least 2 to 3 weeks.
Other Tendon Sheaths
Most tendon sheaths may be examined by tenoscopy, including extensor tendon sheaths in the dorsal carpal and tarsal regions. However, no published reports indicate the use of tenoscopy for these smaller synovial cavities, possibly because acceptable results have been obtained with traditional surgical exposure.36 I have attempted tenoscopy of the carpal extensor sheaths experimentally in isolated limbs, using a 4-mm, 30-degree forward endoscope inserted medially or laterally to the tendons, proximal to the carpus. This technique provides acceptable examination of the sheath and tendon surfaces, but little movement is possible because of the tight extensor retinacula.
Bursoscopy
Reports of bursoscopy in horses are limited,11,37 but it is probable that the technique would yield similar advantages to tenoscopy in horses with masses or infection in normal or acquired bursae. Surgical exposure and debridement of hygromas, capped hocks, and metacarpophalangeal subtendonous bursae are often associated with wound dehiscence and chronic infection.38 However, I am unaware of published data describing bursoscopic examination in these locations. A technique for bursoscopy of the calcaneal bursa of the SDFT has been described and advocated for diagnosis and treatment of injuries to this structure and is probably most useful in horses with infectious bursitis.37
Bursoscopy of the Intertubercular Bursa
Bursoscopic surgery has been used for the management of infectious intertubercular (bicipital) bursitis,39 and a report describes its use as a diagnostic method in a horse with traumatic bicipital bursitis.11 The horse is placed in lateral recumbency with the affected limb uppermost. The endoscope is introduced through a craniolateral skin portal, made over the point of the shoulder, immediately cranial to the lateral (greater) tubercle of the humerus. The bicipital bursa is distended with 40 mL of fluid. The skin incision is continued through the brachiocephalicus muscle and into the bicipital bursa, and the endoscope sleeve and conical obturator are inserted in a caudoproximal direction. A technique using two separate portals has been described to improve visibility.40 The first portal is made into the distal recess through an incision immediately proximal to the deltoid tuberosity. For the second portal, an incision is made cranioproximal to the lateral humeral tubercle to view the proximal half of the bicipital bursa. Experience with these techniques is currently limited, but they should provide similar advantages to tenoscopy, including easier access to the bicipital bursa, improved visibility, and decreased postoperative morbidity. This needs to be confirmed by more extensive reviews.
Bursoscopy of the Navicular Bursa
Endoscopic examination of the navicular bursa (bursa podotrochlearis)41 recently has been described as an alternative to the traditional street-nail procedure.42,43 It is the technique of choice for treating infectious navicular bursitis.
The main indication for navicular bursoscopy is for management of a contaminated or infected bursa.41 Other indications include diagnostic examination in horses with pain localized to the palmar aspect of the foot but with no lesions identifiable using other imaging modalities and the debridement of adhesions between the navicular bone and the dorsal surface of the DDFT.44
Surgical Technique
The technique has been described elsewhere.41,44-46 Standard arthroscopic equipment is used, although a thinner, 4-mm diameter or less, endoscope is more practical. The horse is placed in lateral recumbency with the metacarpal or metatarsal region supported and the digit moving loosely. A medial approach with the affected limb lowermost or a lateral approach with the limb uppermost may be used. A vertical, 5-mm skin incision is made along the abaxial border of the DDFT, 1 cm proximal to the cartilage of the foot, and palmar/plantar to the neurovascular bundle. The cannula, with a conical obturator, is inserted distally and slightly axially, dorsal to the DDFT. The obturator is replaced with the endoscope. Rotation of the endoscope allows examination of the entire proximal recess of the navicular bursa and sometimes the distal recess, including the smooth dorsal aspect of the DDFT and palmar fibrocartilage of the navicular bone. The collateral sesamoidean ligaments, blending over the proximal surface of the navicular bone into the fibrocartilage and the distal sesamoidean impar ligament, in the distal recess of the navicular bursa, are covered by synovium with thin villi. The larger proximal pouch and the T-ligament are also covered by synovium.
A wound in the sole, sulci, or frog can be used for insertion of cannulae or instruments into the navicular bursa. Some enlargement of the tract using curettes or a motorized synovial resector may be required but should be minimal to limit damage to the DDFT. If access through the wound is difficult, or to reach a lesion that cannot be accessed this way, a similar approach to that used for the endoscope may be made on the opposite side of the limb.
The navicular bursa is lavaged, and any lesions are debrided sharply. Partial synovectomy may be carried out if necessary. The use of motorized synovial resectors is recommended. At the end of the procedure the opening of a sinus tract on the solar surface of the foot may be enlarged and debrided to avoid abscess formation. Debridement of the defect through the DDFT should be minimal. An aminoglycoside antibiotic may be placed in the navicular bursa, and the skin incisions are closed routinely. A bandage including the whole hoof and extending to the proximal metacarpal or metatarsal region is applied.
Postoperative Management and Results
Postoperative use of antibiotics and NSAIDs is at the surgeon’s discretion. The horse can be walked out in hand after 2 or 3 days, and exercise can be gradually resumed after healing of the wound is complete, in the absence of complications.
Complications of infection include recurrence, extension of the infection into adjacent synovial structures, and osteitis or fracture of the navicular bone.41,43 Contamination of the distal interphalangeal joint or DFTS may be treated during the initial surgery by an endoscopic approach using the same skin portal.41 If infection recurs, lavage through needles or bursoscopy may be performed, and an open approach through the solar surface may be used, but the prognosis should then be considered graver.
The prognosis for horses with infectious navicular bursitis using this approach41 appears to be greatly improved compared with the more invasive street-nail procedure.43 Seventy-five percent of horses returned to the initial use after bursoscopy versus 31.5% using the open technique, although the criteria used to judge success may be slightly different.41 Bursoscopy is considered to be the technique of choice for infectious navicular bursitis, although I recommend using a street-nail approach for the salvage of horses with chronic bursitis with extensive damage to the podotrochlear structures.